User login
USPSTF: Screen all adults for depression
All adults, including pregnant and postpartum women, should be screened for depression, according to new recommendations of the U.S. Preventive Services Task Force.
The recommendation also calls for screening to be coupled with “adequate systems” to ensure diagnosis, treatment, and follow-up (JAMA. 2016 Jan 26;315[4]:380-7).
The depression screening recommendation, authored by Dr. Albert L. Siu and the other members of the USPSTF, is a level B recommendation, meaning that it has either high certainty of moderate net benefit, or moderate certainty of moderate to substantial net benefit.
The new guidance in screening for depression helps address a disorder that is “the leading cause of disability among adults in high-income countries,” said Dr. Siu and his coauthors. Lost productivity attributable to depression cost $23 billion in the United States in 2011, and $22.8 billion was spent on treatments for depression in 2009, the last year for which figures are available.
Dr. Siu, chair of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and his coauthors cited “convincing evidence that screening improves the accurate identification of adult patients with depression in primary care settings, including pregnant and postpartum women.”
In addition, the task force found convincing evidence that for older adults as well as the general adult population, treatment of “depression identified through screening in primary care settings with antidepressants, psychotherapy, or both decreases clinical morbidity.”
For pregnant and postpartum women with depression, Dr. Siu and his coauthors found “adequate” evidence that cognitive behavioral therapy (CBT) improves outcomes.
The recommendation does not identify optimal timing and intervals for depression screening, citing a need for more research in this area. However, “a pragmatic approach might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” explained Dr. Siu and his coauthors.
The new depression screening recommendation from USPSTF updates the 2009 recommendation, which recommended universal screening if “staff-assisted depression care supports” were in place, and targeted screening based on clinical judgment and patient preference if such support were unavailable.
The rationale for the current recommendation of universal screening for those 18 years and older is the “recognition that such support is now much more widely available and accepted as part of mental health care,” the task force members said.
Any potential harms of screening, said Dr. Siu and his coauthors, were minimal to nonexistent.
Overall, the USPSTF assigned a small to moderate risk to the use of medication in depression. However, the use of “second-generation” antidepressants – mostly SSRIs – was associated with some harms, including increased risk of suicidal behavior in young adults and of gastrointestinal bleeding in older adults, as well as potential fetal harms in pregnant women taking antidepressants.
Using CBT to treat depression in pregnant and postpartum women was also associated with minimal to no harm.
The USPSTF screening recommendation is aligned with the American Academy of Family Physicians’ recommendation to screen the general adult population for depression, and with the American Academy of Pediatrics’ recommendation that pediatricians screen mothers for depression at their babies’ 1-, 2-, and 4-month office visits.
Released in draft form in July 2015, the depression screening recommendation was available for public comment for a period of 4 weeks. In response to public input, the final recommendation’s implementation section clarifies and characterizes an “adequate system” of screening, and gives more resources for evidence-based depression screening and treatment.
The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
On Twitter @karioakes
The new USPSTF recommendations carry a B grade, reflecting both the heterogeneous nature of the diagnosis of depression and the many areas of uncertainty in screening and treatment of the disorder. Major depressive disorder (MDD) is a varied condition that may respond to a variety of treatments, including medication and various forms of therapy. The clinical spectrum of MDD may range from a mild, self-limited course to disabling depression that interferes with daily function and that may persist for long periods of time.
Even the nine-item depression scale of the Patient Health Questionnaire (PHQ-9), considered the first choice of many in primary care, only has a positive predictive value of about 50%, and will miss about one in five cases of true depression. This means that screening must be followed by clinically appropriate evaluation to assure accurate diagnosis of MDD.

|
Dr. Michael E. Thase |
No biomarker has been identified that will predict which treatment will work for which patient with depression, and first-line antidepressants will only help about 50% of an intent-to-treat population.
Against that backdrop, clinicians should take patient preference into account, especially for patients with more severe depression, for whom preference may matter more. Individuals with more severe illness may require multiple adjustments to their pharmacologic and therapeutic regimen, so care systems should be built to anticipate this need.
Early warning systems that use technology to assess patient adherence and response may help effective tailoring of a therapeutic approach: Patients could complete online symptom diaries to assess early response to therapies, and a missed prescription refill – or failure to fill an initial prescription – could trigger prompt intervention by the care team.
Dr. Michael E. Thase is professor of psychiatry and chief of the mood and anxiety disorders treatment and research program at the University of Pennsylvania, Philadelphia. The comments above were summarized from Dr. Thase’s editorial accompanying the USPSTF depression screening recommendation (JAMA. 2016 Jan 26;315[4]:349-50).
The new USPSTF recommendations carry a B grade, reflecting both the heterogeneous nature of the diagnosis of depression and the many areas of uncertainty in screening and treatment of the disorder. Major depressive disorder (MDD) is a varied condition that may respond to a variety of treatments, including medication and various forms of therapy. The clinical spectrum of MDD may range from a mild, self-limited course to disabling depression that interferes with daily function and that may persist for long periods of time.
Even the nine-item depression scale of the Patient Health Questionnaire (PHQ-9), considered the first choice of many in primary care, only has a positive predictive value of about 50%, and will miss about one in five cases of true depression. This means that screening must be followed by clinically appropriate evaluation to assure accurate diagnosis of MDD.

|
Dr. Michael E. Thase |
No biomarker has been identified that will predict which treatment will work for which patient with depression, and first-line antidepressants will only help about 50% of an intent-to-treat population.
Against that backdrop, clinicians should take patient preference into account, especially for patients with more severe depression, for whom preference may matter more. Individuals with more severe illness may require multiple adjustments to their pharmacologic and therapeutic regimen, so care systems should be built to anticipate this need.
Early warning systems that use technology to assess patient adherence and response may help effective tailoring of a therapeutic approach: Patients could complete online symptom diaries to assess early response to therapies, and a missed prescription refill – or failure to fill an initial prescription – could trigger prompt intervention by the care team.
Dr. Michael E. Thase is professor of psychiatry and chief of the mood and anxiety disorders treatment and research program at the University of Pennsylvania, Philadelphia. The comments above were summarized from Dr. Thase’s editorial accompanying the USPSTF depression screening recommendation (JAMA. 2016 Jan 26;315[4]:349-50).
The new USPSTF recommendations carry a B grade, reflecting both the heterogeneous nature of the diagnosis of depression and the many areas of uncertainty in screening and treatment of the disorder. Major depressive disorder (MDD) is a varied condition that may respond to a variety of treatments, including medication and various forms of therapy. The clinical spectrum of MDD may range from a mild, self-limited course to disabling depression that interferes with daily function and that may persist for long periods of time.
Even the nine-item depression scale of the Patient Health Questionnaire (PHQ-9), considered the first choice of many in primary care, only has a positive predictive value of about 50%, and will miss about one in five cases of true depression. This means that screening must be followed by clinically appropriate evaluation to assure accurate diagnosis of MDD.

|
Dr. Michael E. Thase |
No biomarker has been identified that will predict which treatment will work for which patient with depression, and first-line antidepressants will only help about 50% of an intent-to-treat population.
Against that backdrop, clinicians should take patient preference into account, especially for patients with more severe depression, for whom preference may matter more. Individuals with more severe illness may require multiple adjustments to their pharmacologic and therapeutic regimen, so care systems should be built to anticipate this need.
Early warning systems that use technology to assess patient adherence and response may help effective tailoring of a therapeutic approach: Patients could complete online symptom diaries to assess early response to therapies, and a missed prescription refill – or failure to fill an initial prescription – could trigger prompt intervention by the care team.
Dr. Michael E. Thase is professor of psychiatry and chief of the mood and anxiety disorders treatment and research program at the University of Pennsylvania, Philadelphia. The comments above were summarized from Dr. Thase’s editorial accompanying the USPSTF depression screening recommendation (JAMA. 2016 Jan 26;315[4]:349-50).
All adults, including pregnant and postpartum women, should be screened for depression, according to new recommendations of the U.S. Preventive Services Task Force.
The recommendation also calls for screening to be coupled with “adequate systems” to ensure diagnosis, treatment, and follow-up (JAMA. 2016 Jan 26;315[4]:380-7).
The depression screening recommendation, authored by Dr. Albert L. Siu and the other members of the USPSTF, is a level B recommendation, meaning that it has either high certainty of moderate net benefit, or moderate certainty of moderate to substantial net benefit.
The new guidance in screening for depression helps address a disorder that is “the leading cause of disability among adults in high-income countries,” said Dr. Siu and his coauthors. Lost productivity attributable to depression cost $23 billion in the United States in 2011, and $22.8 billion was spent on treatments for depression in 2009, the last year for which figures are available.
Dr. Siu, chair of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and his coauthors cited “convincing evidence that screening improves the accurate identification of adult patients with depression in primary care settings, including pregnant and postpartum women.”
In addition, the task force found convincing evidence that for older adults as well as the general adult population, treatment of “depression identified through screening in primary care settings with antidepressants, psychotherapy, or both decreases clinical morbidity.”
For pregnant and postpartum women with depression, Dr. Siu and his coauthors found “adequate” evidence that cognitive behavioral therapy (CBT) improves outcomes.
The recommendation does not identify optimal timing and intervals for depression screening, citing a need for more research in this area. However, “a pragmatic approach might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” explained Dr. Siu and his coauthors.
The new depression screening recommendation from USPSTF updates the 2009 recommendation, which recommended universal screening if “staff-assisted depression care supports” were in place, and targeted screening based on clinical judgment and patient preference if such support were unavailable.
The rationale for the current recommendation of universal screening for those 18 years and older is the “recognition that such support is now much more widely available and accepted as part of mental health care,” the task force members said.
Any potential harms of screening, said Dr. Siu and his coauthors, were minimal to nonexistent.
Overall, the USPSTF assigned a small to moderate risk to the use of medication in depression. However, the use of “second-generation” antidepressants – mostly SSRIs – was associated with some harms, including increased risk of suicidal behavior in young adults and of gastrointestinal bleeding in older adults, as well as potential fetal harms in pregnant women taking antidepressants.
Using CBT to treat depression in pregnant and postpartum women was also associated with minimal to no harm.
The USPSTF screening recommendation is aligned with the American Academy of Family Physicians’ recommendation to screen the general adult population for depression, and with the American Academy of Pediatrics’ recommendation that pediatricians screen mothers for depression at their babies’ 1-, 2-, and 4-month office visits.
Released in draft form in July 2015, the depression screening recommendation was available for public comment for a period of 4 weeks. In response to public input, the final recommendation’s implementation section clarifies and characterizes an “adequate system” of screening, and gives more resources for evidence-based depression screening and treatment.
The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
On Twitter @karioakes
All adults, including pregnant and postpartum women, should be screened for depression, according to new recommendations of the U.S. Preventive Services Task Force.
The recommendation also calls for screening to be coupled with “adequate systems” to ensure diagnosis, treatment, and follow-up (JAMA. 2016 Jan 26;315[4]:380-7).
The depression screening recommendation, authored by Dr. Albert L. Siu and the other members of the USPSTF, is a level B recommendation, meaning that it has either high certainty of moderate net benefit, or moderate certainty of moderate to substantial net benefit.
The new guidance in screening for depression helps address a disorder that is “the leading cause of disability among adults in high-income countries,” said Dr. Siu and his coauthors. Lost productivity attributable to depression cost $23 billion in the United States in 2011, and $22.8 billion was spent on treatments for depression in 2009, the last year for which figures are available.
Dr. Siu, chair of geriatrics and palliative medicine at Icahn School of Medicine at Mount Sinai, New York, and his coauthors cited “convincing evidence that screening improves the accurate identification of adult patients with depression in primary care settings, including pregnant and postpartum women.”
In addition, the task force found convincing evidence that for older adults as well as the general adult population, treatment of “depression identified through screening in primary care settings with antidepressants, psychotherapy, or both decreases clinical morbidity.”
For pregnant and postpartum women with depression, Dr. Siu and his coauthors found “adequate” evidence that cognitive behavioral therapy (CBT) improves outcomes.
The recommendation does not identify optimal timing and intervals for depression screening, citing a need for more research in this area. However, “a pragmatic approach might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” explained Dr. Siu and his coauthors.
The new depression screening recommendation from USPSTF updates the 2009 recommendation, which recommended universal screening if “staff-assisted depression care supports” were in place, and targeted screening based on clinical judgment and patient preference if such support were unavailable.
The rationale for the current recommendation of universal screening for those 18 years and older is the “recognition that such support is now much more widely available and accepted as part of mental health care,” the task force members said.
Any potential harms of screening, said Dr. Siu and his coauthors, were minimal to nonexistent.
Overall, the USPSTF assigned a small to moderate risk to the use of medication in depression. However, the use of “second-generation” antidepressants – mostly SSRIs – was associated with some harms, including increased risk of suicidal behavior in young adults and of gastrointestinal bleeding in older adults, as well as potential fetal harms in pregnant women taking antidepressants.
Using CBT to treat depression in pregnant and postpartum women was also associated with minimal to no harm.
The USPSTF screening recommendation is aligned with the American Academy of Family Physicians’ recommendation to screen the general adult population for depression, and with the American Academy of Pediatrics’ recommendation that pediatricians screen mothers for depression at their babies’ 1-, 2-, and 4-month office visits.
Released in draft form in July 2015, the depression screening recommendation was available for public comment for a period of 4 weeks. In response to public input, the final recommendation’s implementation section clarifies and characterizes an “adequate system” of screening, and gives more resources for evidence-based depression screening and treatment.
The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
On Twitter @karioakes
FROM JAMA
Key clinical point: Screen all adults for depression, including pregnant and postpartum women.
Major finding: All adults should be screened for depression, with adequate systems in place for diagnosis, treatment, and follow-up.
Data source: New recommendations of the U.S. Preventive Services Task Force.
Disclosures: The Agency for Healthcare Research and Quality supports the operations of the USPSTF, but the task force’s recommendations are independent of the federal government. Dr. Siu and the other task force members reported no conflicts of interest.
Maternal immunization during pregnancy: lessons learned, and emerging opportunities
Pediatricians and our teams are the immunization experts. We educate, advocate, and incorporate vaccines into much of our daily routine. As such, we recognize the importance of working with our colleagues in family medicine, internal medicine, and obstetrics to optimize immunization programs for high-risk individuals, including pregnant women. Recent advances in vaccine recommendations during pregnancy are a result of the collaborative efforts of the health care providers for these women, and from systematic evaluation of immunization programs, vaccine pregnancy registries, and disease epidemiology.
Vaccinating women during pregnancy should be considered when a vaccine is known to be safe and when the following apply:
• The risk of severe infection is high during or augmented by pregnancy.
• The specific infection during pregnancy threatens the fetus.
• Maternal protection against infection benefits the newborn.
• Passive transfer of antibody from mother to fetus benefits the newborn.
Examples of safe vaccines immediately come to mind that fulfill one of more of these criteria, yet substantial obstacles exist even where safety and effectiveness data are robust. Because clinical vaccine trials traditionally exclude pregnant women, safety and effectiveness data for this group and their newborns are limited and often must come through experience. In a climate of increased vaccine hesitancy in general, both among providers and patients, vaccine delivery can be fragmented and particularly difficult to streamline. Additional obstacles that exist for any immunization program, including one that targets pregnant women specifically, are immunization delivery logistics and cost.
One of the major success stories of maternal immunization that is easily forgotten or overlooked in developed parts of the world is in the prevention of maternal and neonatal tetanus (MNT). A review of recent history reminds us that between the years 2000 and 2014, 35 countries were finally successful in eliminating MNT, including China, Turkey, Egypt, and South Africa. In addition, 24 of 36 states in the country of India, 30 of 34 provinces of Indonesia, and most of Ethiopia have met with success. This has been accomplished through aggressive tetanus vaccination programs, and through education programs targeted at optimal umbilical cord stump care after delivery.
In the United States, the Advisory Committee on Immunization Practices recommends that all pregnant women should receive inactivated influenza vaccine and Tdap vaccine. In addition, several other vaccines are recommended under certain circumstances. Live attenuated vaccines are considered contraindicated, although yellow fever vaccine is an exception during epidemics, or when travel to a highly endemic area during pregnancy cannot be avoided.
Influenza vaccine administered during pregnancy reduces maternal morbidity and mortality. Moreover, safety and benefits for the fetus are clearly documented. Both retrospective cohort analysis studies and randomized controlled trials have consistently demonstrated lower risk of preterm birth and lower risk for delivering newborns small for gestational age among women who received inactivated influenza vaccine during pregnancy. The benefit extends to term healthy infants who are less likely to be hospitalized during the first months of life if their mother was vaccinated against influenza during pregnancy. Because the mother was immunized during pregnancy, it reduces her risk of infection, thereby reducing the potential that the newborn will be exposed to a mother who is contagious. Perhaps more importantly, infants born at or near term have the benefit of transplacental antibody endowment from their mother, including vaccine induced anti-influenza antibodies. This passive protection is expected to last for several months. Active immunization against influenza during infancy begins at 6 months of age.
Tdap vaccine is also recommended during each pregnancy. In the United States, MNT is eliminated. Here, as in other developed countries, Tdap is administered to reduce infant pertussis morbidity. Pertussis remains endemic to the United States, and infants who develop whooping cough during the first 2-3 months of life are at the highest risk for morbidity and mortality.
Historically, one-third of infants infected with pertussis were infected by their mother, although more recent evidence suggests that older siblings are at least as likely a source. Looking back to the paradigm for protection against influenza infection in the first few months of life, it becomes clear why the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention has recommended Tdap vaccine for all mothers during each pregnancy.
The first goal is to prevent pertussis in the mother so that she will not transmit the infection to her newborn. The additional goal, and the rationale for vaccinating pregnant women during every pregnancy, is to optimize levels of anti-pertussis antibody in the mother, so that the transplacental endowment to the infant is as robust as possible.
Serologic studies have demonstrated that Tdap vaccine induces high anti-pertussis antibodies when administered during pregnancy, but that the half-life of those antibodies is brief. When Tdap is given during pregnancy, and the infant is born at or near term, the antibody transfer to the infant is expected to provide passive protection for several months. Maternal immunization during pregnancy thereby reduces the risk that the mother will develop pertussis and transmit it to her newborn, while at the same time allows a degree of passive immunoprotection to the infant during the most vulnerable period of life. Active immunization against pertussis in the infant begins between 6-8 weeks of age.
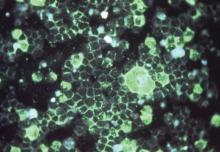
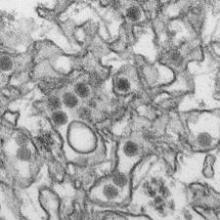
Another infection that is exceedingly common during the first several months of life is respiratory syncytial virus (RSV). RSV remains the most common reason for infant hospitalization in the United States and other developed countries. The source of the virus can be any other person with a mild or moderate respiratory tract infection as the virus is ubiquitous, and can re-infect individuals throughout their lifetime. The first infection, however, is the worst. It is estimated that between 3% and 4% of the U.S. birth cohort is hospitalized with RSV. With a U.S. birth cohort of about 4 million, the result is 120,000-160,000 infant admissions annually.
The RSV epidemic is seasonal, fairly predictable, and dreaded by primary care pediatricians and hospitalists alike. Lower respiratory tract infection with RSV, in the form of RSV bronchiolitis, presents all too commonly in the young infant with cough, coryza, tachypnea, and wheezing. When the work of breathing increases, and the cough symptoms predominate, the infant is unable to feed efficiently. Hospitalizations may be for dehydration, concerns for impending respiratory failure, or for the administration of supplemental oxygen or other respiratory support. No specific therapeutic interventions reliably reduce the symptoms or the length of hospital stay, nor do they reduce the possibility that intensive care with mechanical ventilation may be required. Treatments are only supportive. An effective vaccine remains elusive.
All other common infections that once resulted in high rates of hospitalization in the first year of life are now substantially reduced through vaccination. Why not this one? The development of a safe and effective vaccine to prevent infant RSV infection or to reduce RSV-associated hospitalizations is especially challenging for multiple reasons.
Some of these reasons have met with substantial advances quite recently, including the discovery of antigen structures needed to induce neutralizing antibody responses. There also are challenges specific to the infant group we need most to protect. Infant RSV infection itself confers only modest protection against subsequent infection. Repeated infections over time are necessary for protection against illness when re-exposed. A vaccine that is able to induce a response similar to natural infection would therefore require multiple doses, presumably over time (the so called ‘primary series’) before a substantial clinical benefit would be expected. This is particularly important because most RSV-associated hospitalizations occur during the first several months of life, reducing the timeline for which a protective vaccine series could be administered.
The challenges are parallel to the issues described earlier for protection against both influenza and pertussis. Infant protection against both of these infections are now addressed, at least to start with, by vaccinating the mother during her pregnancy. In the infant, the pertussis vaccine primary series is then initiated between 6 and 8 weeks of age, and the influenza series initiated at 6 months of age. It is the passive protection, in the form of transplacental maternal antibody, that offers the interim protection during the highest-risk first months of life.
For infants at very high risk of serious RSV infection, passive antibody protection is already administered in the form of the pharmacobiologic medication palivizumab. Its half-life dictates monthly injections for those eligible, and its cost precludes its use for any but the highest risk infants (those born prematurely, and those with chronic lung disease and/or congenital heart disease). This strategy, however, has proven effective in preventing RSV-associated hospitalization in every group in which it has been studied. This “proof of concept” strongly suggests that if the right RSV vaccine is given to women during pregnancy to induce a robust neutralizing anti-RSV antibody response, and that antibody is transferred to the fetus prior to birth, the newborn will benefit from protection against RSV for a period of time.
Several questions emerge. If RSV is ubiquitous, and can re-infect individuals throughout their lifetime, then some women will be infected during their pregnancy. Do their infants benefit? As a re-infection, the maternal symptoms would be expected to be mild, but the infection could boost the women’s natural immunity with a robust anamnestic antibody response. This possibility has not been studied systematically, but might help to explain why some healthy term infants exposed to RSV develop little or no symptoms, while others (mothers who have not recently had a natural RSV infection) develop severe illness requiring hospitalization.
There are data to support the contention that term infants born to mothers with higher naturally occurring anti-RSV neutralizing antibodies benefit from those antibodies. In a large prospective cohort study performed in Kenya, cord blood anti-RSV antibody concentrations correlated directly with the length of time before the infant’s first RSV infection. It’s therefore logical to conclude that administering an effective RSV vaccine during pregnancy could augment that natural antibody response, be transferred to the infant at birth, and offer protection against RSV when exposed.
Several candidate vaccines for study already exist and have undergone phase I testing in nonpregnant adults. Once safety is demonstrated, the next step is to identify the vaccine formulation resulting in the most robust anti-RSV neutralizing antibody concentrations. Such a candidate vaccine will be chosen for future phase III trials during pregnancy. Safety, and maternal/cord blood RSV antibody titers will be of interest during that clinical trial, but the rates and timing of RSV infection and RSV-associated hospitalizations among the infants born to those mothers will be the most instructive.
Ideally, a candidate RSV vaccine shown to be as safe and as effective during pregnancy as inactivated influenza vaccines and/or Tdap vaccines would be implemented immediately and universally. Unfortunately, substantial vaccine hesitancy for the use of influenza and Tdap vaccines continues among pregnant patients and their providers. Acceptance of an RSV vaccine for use during pregnancy will not come easily, or immediately. As with all of our successful vaccine programs, launching such an effort will require education, patience, and careful post-licensure documentation of the impact that the intervention has in the real world.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University, Syracuse, N.Y. Dr. Domachowske is performing clinical trials and has grants in the area of RSV prevention with Astra Zeneca, Regeneron, and Glaxo Smith Kline.
Pediatricians and our teams are the immunization experts. We educate, advocate, and incorporate vaccines into much of our daily routine. As such, we recognize the importance of working with our colleagues in family medicine, internal medicine, and obstetrics to optimize immunization programs for high-risk individuals, including pregnant women. Recent advances in vaccine recommendations during pregnancy are a result of the collaborative efforts of the health care providers for these women, and from systematic evaluation of immunization programs, vaccine pregnancy registries, and disease epidemiology.
Vaccinating women during pregnancy should be considered when a vaccine is known to be safe and when the following apply:
• The risk of severe infection is high during or augmented by pregnancy.
• The specific infection during pregnancy threatens the fetus.
• Maternal protection against infection benefits the newborn.
• Passive transfer of antibody from mother to fetus benefits the newborn.
Examples of safe vaccines immediately come to mind that fulfill one of more of these criteria, yet substantial obstacles exist even where safety and effectiveness data are robust. Because clinical vaccine trials traditionally exclude pregnant women, safety and effectiveness data for this group and their newborns are limited and often must come through experience. In a climate of increased vaccine hesitancy in general, both among providers and patients, vaccine delivery can be fragmented and particularly difficult to streamline. Additional obstacles that exist for any immunization program, including one that targets pregnant women specifically, are immunization delivery logistics and cost.
One of the major success stories of maternal immunization that is easily forgotten or overlooked in developed parts of the world is in the prevention of maternal and neonatal tetanus (MNT). A review of recent history reminds us that between the years 2000 and 2014, 35 countries were finally successful in eliminating MNT, including China, Turkey, Egypt, and South Africa. In addition, 24 of 36 states in the country of India, 30 of 34 provinces of Indonesia, and most of Ethiopia have met with success. This has been accomplished through aggressive tetanus vaccination programs, and through education programs targeted at optimal umbilical cord stump care after delivery.
In the United States, the Advisory Committee on Immunization Practices recommends that all pregnant women should receive inactivated influenza vaccine and Tdap vaccine. In addition, several other vaccines are recommended under certain circumstances. Live attenuated vaccines are considered contraindicated, although yellow fever vaccine is an exception during epidemics, or when travel to a highly endemic area during pregnancy cannot be avoided.
Influenza vaccine administered during pregnancy reduces maternal morbidity and mortality. Moreover, safety and benefits for the fetus are clearly documented. Both retrospective cohort analysis studies and randomized controlled trials have consistently demonstrated lower risk of preterm birth and lower risk for delivering newborns small for gestational age among women who received inactivated influenza vaccine during pregnancy. The benefit extends to term healthy infants who are less likely to be hospitalized during the first months of life if their mother was vaccinated against influenza during pregnancy. Because the mother was immunized during pregnancy, it reduces her risk of infection, thereby reducing the potential that the newborn will be exposed to a mother who is contagious. Perhaps more importantly, infants born at or near term have the benefit of transplacental antibody endowment from their mother, including vaccine induced anti-influenza antibodies. This passive protection is expected to last for several months. Active immunization against influenza during infancy begins at 6 months of age.
Tdap vaccine is also recommended during each pregnancy. In the United States, MNT is eliminated. Here, as in other developed countries, Tdap is administered to reduce infant pertussis morbidity. Pertussis remains endemic to the United States, and infants who develop whooping cough during the first 2-3 months of life are at the highest risk for morbidity and mortality.
Historically, one-third of infants infected with pertussis were infected by their mother, although more recent evidence suggests that older siblings are at least as likely a source. Looking back to the paradigm for protection against influenza infection in the first few months of life, it becomes clear why the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention has recommended Tdap vaccine for all mothers during each pregnancy.
The first goal is to prevent pertussis in the mother so that she will not transmit the infection to her newborn. The additional goal, and the rationale for vaccinating pregnant women during every pregnancy, is to optimize levels of anti-pertussis antibody in the mother, so that the transplacental endowment to the infant is as robust as possible.
Serologic studies have demonstrated that Tdap vaccine induces high anti-pertussis antibodies when administered during pregnancy, but that the half-life of those antibodies is brief. When Tdap is given during pregnancy, and the infant is born at or near term, the antibody transfer to the infant is expected to provide passive protection for several months. Maternal immunization during pregnancy thereby reduces the risk that the mother will develop pertussis and transmit it to her newborn, while at the same time allows a degree of passive immunoprotection to the infant during the most vulnerable period of life. Active immunization against pertussis in the infant begins between 6-8 weeks of age.
Another infection that is exceedingly common during the first several months of life is respiratory syncytial virus (RSV). RSV remains the most common reason for infant hospitalization in the United States and other developed countries. The source of the virus can be any other person with a mild or moderate respiratory tract infection as the virus is ubiquitous, and can re-infect individuals throughout their lifetime. The first infection, however, is the worst. It is estimated that between 3% and 4% of the U.S. birth cohort is hospitalized with RSV. With a U.S. birth cohort of about 4 million, the result is 120,000-160,000 infant admissions annually.
The RSV epidemic is seasonal, fairly predictable, and dreaded by primary care pediatricians and hospitalists alike. Lower respiratory tract infection with RSV, in the form of RSV bronchiolitis, presents all too commonly in the young infant with cough, coryza, tachypnea, and wheezing. When the work of breathing increases, and the cough symptoms predominate, the infant is unable to feed efficiently. Hospitalizations may be for dehydration, concerns for impending respiratory failure, or for the administration of supplemental oxygen or other respiratory support. No specific therapeutic interventions reliably reduce the symptoms or the length of hospital stay, nor do they reduce the possibility that intensive care with mechanical ventilation may be required. Treatments are only supportive. An effective vaccine remains elusive.
All other common infections that once resulted in high rates of hospitalization in the first year of life are now substantially reduced through vaccination. Why not this one? The development of a safe and effective vaccine to prevent infant RSV infection or to reduce RSV-associated hospitalizations is especially challenging for multiple reasons.
Some of these reasons have met with substantial advances quite recently, including the discovery of antigen structures needed to induce neutralizing antibody responses. There also are challenges specific to the infant group we need most to protect. Infant RSV infection itself confers only modest protection against subsequent infection. Repeated infections over time are necessary for protection against illness when re-exposed. A vaccine that is able to induce a response similar to natural infection would therefore require multiple doses, presumably over time (the so called ‘primary series’) before a substantial clinical benefit would be expected. This is particularly important because most RSV-associated hospitalizations occur during the first several months of life, reducing the timeline for which a protective vaccine series could be administered.
The challenges are parallel to the issues described earlier for protection against both influenza and pertussis. Infant protection against both of these infections are now addressed, at least to start with, by vaccinating the mother during her pregnancy. In the infant, the pertussis vaccine primary series is then initiated between 6 and 8 weeks of age, and the influenza series initiated at 6 months of age. It is the passive protection, in the form of transplacental maternal antibody, that offers the interim protection during the highest-risk first months of life.
For infants at very high risk of serious RSV infection, passive antibody protection is already administered in the form of the pharmacobiologic medication palivizumab. Its half-life dictates monthly injections for those eligible, and its cost precludes its use for any but the highest risk infants (those born prematurely, and those with chronic lung disease and/or congenital heart disease). This strategy, however, has proven effective in preventing RSV-associated hospitalization in every group in which it has been studied. This “proof of concept” strongly suggests that if the right RSV vaccine is given to women during pregnancy to induce a robust neutralizing anti-RSV antibody response, and that antibody is transferred to the fetus prior to birth, the newborn will benefit from protection against RSV for a period of time.
Several questions emerge. If RSV is ubiquitous, and can re-infect individuals throughout their lifetime, then some women will be infected during their pregnancy. Do their infants benefit? As a re-infection, the maternal symptoms would be expected to be mild, but the infection could boost the women’s natural immunity with a robust anamnestic antibody response. This possibility has not been studied systematically, but might help to explain why some healthy term infants exposed to RSV develop little or no symptoms, while others (mothers who have not recently had a natural RSV infection) develop severe illness requiring hospitalization.
There are data to support the contention that term infants born to mothers with higher naturally occurring anti-RSV neutralizing antibodies benefit from those antibodies. In a large prospective cohort study performed in Kenya, cord blood anti-RSV antibody concentrations correlated directly with the length of time before the infant’s first RSV infection. It’s therefore logical to conclude that administering an effective RSV vaccine during pregnancy could augment that natural antibody response, be transferred to the infant at birth, and offer protection against RSV when exposed.
Several candidate vaccines for study already exist and have undergone phase I testing in nonpregnant adults. Once safety is demonstrated, the next step is to identify the vaccine formulation resulting in the most robust anti-RSV neutralizing antibody concentrations. Such a candidate vaccine will be chosen for future phase III trials during pregnancy. Safety, and maternal/cord blood RSV antibody titers will be of interest during that clinical trial, but the rates and timing of RSV infection and RSV-associated hospitalizations among the infants born to those mothers will be the most instructive.
Ideally, a candidate RSV vaccine shown to be as safe and as effective during pregnancy as inactivated influenza vaccines and/or Tdap vaccines would be implemented immediately and universally. Unfortunately, substantial vaccine hesitancy for the use of influenza and Tdap vaccines continues among pregnant patients and their providers. Acceptance of an RSV vaccine for use during pregnancy will not come easily, or immediately. As with all of our successful vaccine programs, launching such an effort will require education, patience, and careful post-licensure documentation of the impact that the intervention has in the real world.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University, Syracuse, N.Y. Dr. Domachowske is performing clinical trials and has grants in the area of RSV prevention with Astra Zeneca, Regeneron, and Glaxo Smith Kline.
Pediatricians and our teams are the immunization experts. We educate, advocate, and incorporate vaccines into much of our daily routine. As such, we recognize the importance of working with our colleagues in family medicine, internal medicine, and obstetrics to optimize immunization programs for high-risk individuals, including pregnant women. Recent advances in vaccine recommendations during pregnancy are a result of the collaborative efforts of the health care providers for these women, and from systematic evaluation of immunization programs, vaccine pregnancy registries, and disease epidemiology.
Vaccinating women during pregnancy should be considered when a vaccine is known to be safe and when the following apply:
• The risk of severe infection is high during or augmented by pregnancy.
• The specific infection during pregnancy threatens the fetus.
• Maternal protection against infection benefits the newborn.
• Passive transfer of antibody from mother to fetus benefits the newborn.
Examples of safe vaccines immediately come to mind that fulfill one of more of these criteria, yet substantial obstacles exist even where safety and effectiveness data are robust. Because clinical vaccine trials traditionally exclude pregnant women, safety and effectiveness data for this group and their newborns are limited and often must come through experience. In a climate of increased vaccine hesitancy in general, both among providers and patients, vaccine delivery can be fragmented and particularly difficult to streamline. Additional obstacles that exist for any immunization program, including one that targets pregnant women specifically, are immunization delivery logistics and cost.
One of the major success stories of maternal immunization that is easily forgotten or overlooked in developed parts of the world is in the prevention of maternal and neonatal tetanus (MNT). A review of recent history reminds us that between the years 2000 and 2014, 35 countries were finally successful in eliminating MNT, including China, Turkey, Egypt, and South Africa. In addition, 24 of 36 states in the country of India, 30 of 34 provinces of Indonesia, and most of Ethiopia have met with success. This has been accomplished through aggressive tetanus vaccination programs, and through education programs targeted at optimal umbilical cord stump care after delivery.
In the United States, the Advisory Committee on Immunization Practices recommends that all pregnant women should receive inactivated influenza vaccine and Tdap vaccine. In addition, several other vaccines are recommended under certain circumstances. Live attenuated vaccines are considered contraindicated, although yellow fever vaccine is an exception during epidemics, or when travel to a highly endemic area during pregnancy cannot be avoided.
Influenza vaccine administered during pregnancy reduces maternal morbidity and mortality. Moreover, safety and benefits for the fetus are clearly documented. Both retrospective cohort analysis studies and randomized controlled trials have consistently demonstrated lower risk of preterm birth and lower risk for delivering newborns small for gestational age among women who received inactivated influenza vaccine during pregnancy. The benefit extends to term healthy infants who are less likely to be hospitalized during the first months of life if their mother was vaccinated against influenza during pregnancy. Because the mother was immunized during pregnancy, it reduces her risk of infection, thereby reducing the potential that the newborn will be exposed to a mother who is contagious. Perhaps more importantly, infants born at or near term have the benefit of transplacental antibody endowment from their mother, including vaccine induced anti-influenza antibodies. This passive protection is expected to last for several months. Active immunization against influenza during infancy begins at 6 months of age.
Tdap vaccine is also recommended during each pregnancy. In the United States, MNT is eliminated. Here, as in other developed countries, Tdap is administered to reduce infant pertussis morbidity. Pertussis remains endemic to the United States, and infants who develop whooping cough during the first 2-3 months of life are at the highest risk for morbidity and mortality.
Historically, one-third of infants infected with pertussis were infected by their mother, although more recent evidence suggests that older siblings are at least as likely a source. Looking back to the paradigm for protection against influenza infection in the first few months of life, it becomes clear why the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention has recommended Tdap vaccine for all mothers during each pregnancy.
The first goal is to prevent pertussis in the mother so that she will not transmit the infection to her newborn. The additional goal, and the rationale for vaccinating pregnant women during every pregnancy, is to optimize levels of anti-pertussis antibody in the mother, so that the transplacental endowment to the infant is as robust as possible.
Serologic studies have demonstrated that Tdap vaccine induces high anti-pertussis antibodies when administered during pregnancy, but that the half-life of those antibodies is brief. When Tdap is given during pregnancy, and the infant is born at or near term, the antibody transfer to the infant is expected to provide passive protection for several months. Maternal immunization during pregnancy thereby reduces the risk that the mother will develop pertussis and transmit it to her newborn, while at the same time allows a degree of passive immunoprotection to the infant during the most vulnerable period of life. Active immunization against pertussis in the infant begins between 6-8 weeks of age.
Another infection that is exceedingly common during the first several months of life is respiratory syncytial virus (RSV). RSV remains the most common reason for infant hospitalization in the United States and other developed countries. The source of the virus can be any other person with a mild or moderate respiratory tract infection as the virus is ubiquitous, and can re-infect individuals throughout their lifetime. The first infection, however, is the worst. It is estimated that between 3% and 4% of the U.S. birth cohort is hospitalized with RSV. With a U.S. birth cohort of about 4 million, the result is 120,000-160,000 infant admissions annually.
The RSV epidemic is seasonal, fairly predictable, and dreaded by primary care pediatricians and hospitalists alike. Lower respiratory tract infection with RSV, in the form of RSV bronchiolitis, presents all too commonly in the young infant with cough, coryza, tachypnea, and wheezing. When the work of breathing increases, and the cough symptoms predominate, the infant is unable to feed efficiently. Hospitalizations may be for dehydration, concerns for impending respiratory failure, or for the administration of supplemental oxygen or other respiratory support. No specific therapeutic interventions reliably reduce the symptoms or the length of hospital stay, nor do they reduce the possibility that intensive care with mechanical ventilation may be required. Treatments are only supportive. An effective vaccine remains elusive.
All other common infections that once resulted in high rates of hospitalization in the first year of life are now substantially reduced through vaccination. Why not this one? The development of a safe and effective vaccine to prevent infant RSV infection or to reduce RSV-associated hospitalizations is especially challenging for multiple reasons.
Some of these reasons have met with substantial advances quite recently, including the discovery of antigen structures needed to induce neutralizing antibody responses. There also are challenges specific to the infant group we need most to protect. Infant RSV infection itself confers only modest protection against subsequent infection. Repeated infections over time are necessary for protection against illness when re-exposed. A vaccine that is able to induce a response similar to natural infection would therefore require multiple doses, presumably over time (the so called ‘primary series’) before a substantial clinical benefit would be expected. This is particularly important because most RSV-associated hospitalizations occur during the first several months of life, reducing the timeline for which a protective vaccine series could be administered.
The challenges are parallel to the issues described earlier for protection against both influenza and pertussis. Infant protection against both of these infections are now addressed, at least to start with, by vaccinating the mother during her pregnancy. In the infant, the pertussis vaccine primary series is then initiated between 6 and 8 weeks of age, and the influenza series initiated at 6 months of age. It is the passive protection, in the form of transplacental maternal antibody, that offers the interim protection during the highest-risk first months of life.
For infants at very high risk of serious RSV infection, passive antibody protection is already administered in the form of the pharmacobiologic medication palivizumab. Its half-life dictates monthly injections for those eligible, and its cost precludes its use for any but the highest risk infants (those born prematurely, and those with chronic lung disease and/or congenital heart disease). This strategy, however, has proven effective in preventing RSV-associated hospitalization in every group in which it has been studied. This “proof of concept” strongly suggests that if the right RSV vaccine is given to women during pregnancy to induce a robust neutralizing anti-RSV antibody response, and that antibody is transferred to the fetus prior to birth, the newborn will benefit from protection against RSV for a period of time.
Several questions emerge. If RSV is ubiquitous, and can re-infect individuals throughout their lifetime, then some women will be infected during their pregnancy. Do their infants benefit? As a re-infection, the maternal symptoms would be expected to be mild, but the infection could boost the women’s natural immunity with a robust anamnestic antibody response. This possibility has not been studied systematically, but might help to explain why some healthy term infants exposed to RSV develop little or no symptoms, while others (mothers who have not recently had a natural RSV infection) develop severe illness requiring hospitalization.
There are data to support the contention that term infants born to mothers with higher naturally occurring anti-RSV neutralizing antibodies benefit from those antibodies. In a large prospective cohort study performed in Kenya, cord blood anti-RSV antibody concentrations correlated directly with the length of time before the infant’s first RSV infection. It’s therefore logical to conclude that administering an effective RSV vaccine during pregnancy could augment that natural antibody response, be transferred to the infant at birth, and offer protection against RSV when exposed.
Several candidate vaccines for study already exist and have undergone phase I testing in nonpregnant adults. Once safety is demonstrated, the next step is to identify the vaccine formulation resulting in the most robust anti-RSV neutralizing antibody concentrations. Such a candidate vaccine will be chosen for future phase III trials during pregnancy. Safety, and maternal/cord blood RSV antibody titers will be of interest during that clinical trial, but the rates and timing of RSV infection and RSV-associated hospitalizations among the infants born to those mothers will be the most instructive.
Ideally, a candidate RSV vaccine shown to be as safe and as effective during pregnancy as inactivated influenza vaccines and/or Tdap vaccines would be implemented immediately and universally. Unfortunately, substantial vaccine hesitancy for the use of influenza and Tdap vaccines continues among pregnant patients and their providers. Acceptance of an RSV vaccine for use during pregnancy will not come easily, or immediately. As with all of our successful vaccine programs, launching such an effort will require education, patience, and careful post-licensure documentation of the impact that the intervention has in the real world.
Dr. Domachowske is professor of pediatrics and professor of microbiology and immunology at the State University of New York Upstate Medical University, Syracuse, N.Y. Dr. Domachowske is performing clinical trials and has grants in the area of RSV prevention with Astra Zeneca, Regeneron, and Glaxo Smith Kline.
Practice guideline released for treating opioid use disorder
The American Society of Addiction Medicine has released a practice guideline to help clinicians evaluate and treat opioid use disorder, with the ultimate goal of getting more physicians to provide effective treatment.
Effective treatment of opioid use disorder “requires skill and time that are not generally available to primary care doctors in most practice models,” so much of the treatment provided in primary care has been “suboptimal.” This has probably worsened what the Centers for Disease Control and Prevention has described as an epidemic of opioid misuse and related deaths, said Dr. Kyle Kampman and Dr. Margaret Jarvis, cochairs of the ASAM’s guideline committee.
“At the same time, access to competent treatment is profoundly restricted because few physicians are willing and able to provide it,” they noted.
This guideline “is primarily intended for clinicians involved in evaluating patients and providing authorization for pharmacologic treatments at any level,” said Dr. Kampman of the University of Pennsylvania, Philadelphia, and Dr. Jarvis, of the Marworth Alcohol & Chemical Dependency Center, an entity of the Geisinger Health System, Waverly, Pa.
To develop the guideline, the committee – experts and researchers in internal medicine, family medicine, addiction medicine, addiction psychiatry, general psychiatry, obstetrics, pharmacology, and neurobiology, including some with allopathic or osteopathic training – first reviewed 34 existing clinical guidelines and 27 recent studies in the literature assessing medications used with psychosocial interventions. None of the existing guidelines included all the medications currently in use, and few addressed critical special populations such as pregnant women, patients with comorbid psychiatric disorders, and patients with chronic pain.
The ASAM guideline specifically addresses these and other special populations (for example, adolescents, patients in the criminal justice system). It includes detailed sections on treating opioid withdrawal and opioid overdose, as well as comprehensive discussions of methadone, buprenorphine, naltrexone, and psychosocial therapies.
The guideline offers numerous clinical recommendations regarding patient assessment and diagnosis (J Addict Med. 2015;9:358:67).
First, “addiction should be considered a bio-psycho-social-spiritual illness, for which the use of medication(s) is but only one component of overall treatment.” In addition to a thorough history and physical exam (including specific laboratory tests needed for this patient population), patients should undergo a mental health assessment with particular attention to possible psychiatric comorbidities. And since opioid use often co-occurs with other substance-related disorders, “the totality of substances that surround the addiction” should be assessed before treatment is considered.
Notably, the concomitant use of alcohol, sedatives, hypnotics, or anxiolytics with opioids can cause respiratory depression. Patients who use these agents may automatically require a higher level of care than that offered in typical primary care practices.
As well, social and environmental factors should be assessed, to identify both barriers to and facilitators for addiction treatment in general and pharmacotherapy in particular. “At a minimum, psychosocial treatment should include the following: psychosocial needs assessment, supportive counseling, links to existing family supports, and referrals to community services.” Physicians should be prepared to collaborate with qualified behavioral health care providers, the guideline states.
Urinary drug testing is recommended, both during the assessment process and frequently throughout treatment.
Regarding treatment, the guideline recommends considering the patient’s preferences, past treatment history, and the treatment setting when deciding whether to prescribe methadone, bupenorphrine, or naltrexone. The treatment venue is as important as the specific medication selected. Office-based treatment, which provides medication prescribed either weekly or monthly, is limited to buprenorphine only. It might not be suitable for patients who regularly use alcohol or other substances.
In contrast, treatment programs provide daily supervised dosing of methadone and, increasingly, buprenorphine. Methadone is recommended for patients who fail on buprenorphine or who would benefit from daily dosing and supervision.
Naltrexone can be prescribed in any setting by any clinician, but prescribers must be aware that adherence to oral naltrexone is generally poor, which often leads to treatment failure. Extended-release injectable naltrexone reduces but doesn’t eliminate adherence issues. Clinicians should reserve naltrexone “for patients who would be able to comply with special techniques to enhance their adherence, such as observed dosing.”
Dr. Kampton disclosed research ties with Braeburn Pharmaceuticals; Dr. Jarvis disclosed business ties with U.S. Preventive Medicine.
The American Society of Addiction Medicine has released a practice guideline to help clinicians evaluate and treat opioid use disorder, with the ultimate goal of getting more physicians to provide effective treatment.
Effective treatment of opioid use disorder “requires skill and time that are not generally available to primary care doctors in most practice models,” so much of the treatment provided in primary care has been “suboptimal.” This has probably worsened what the Centers for Disease Control and Prevention has described as an epidemic of opioid misuse and related deaths, said Dr. Kyle Kampman and Dr. Margaret Jarvis, cochairs of the ASAM’s guideline committee.
“At the same time, access to competent treatment is profoundly restricted because few physicians are willing and able to provide it,” they noted.
This guideline “is primarily intended for clinicians involved in evaluating patients and providing authorization for pharmacologic treatments at any level,” said Dr. Kampman of the University of Pennsylvania, Philadelphia, and Dr. Jarvis, of the Marworth Alcohol & Chemical Dependency Center, an entity of the Geisinger Health System, Waverly, Pa.
To develop the guideline, the committee – experts and researchers in internal medicine, family medicine, addiction medicine, addiction psychiatry, general psychiatry, obstetrics, pharmacology, and neurobiology, including some with allopathic or osteopathic training – first reviewed 34 existing clinical guidelines and 27 recent studies in the literature assessing medications used with psychosocial interventions. None of the existing guidelines included all the medications currently in use, and few addressed critical special populations such as pregnant women, patients with comorbid psychiatric disorders, and patients with chronic pain.
The ASAM guideline specifically addresses these and other special populations (for example, adolescents, patients in the criminal justice system). It includes detailed sections on treating opioid withdrawal and opioid overdose, as well as comprehensive discussions of methadone, buprenorphine, naltrexone, and psychosocial therapies.
The guideline offers numerous clinical recommendations regarding patient assessment and diagnosis (J Addict Med. 2015;9:358:67).
First, “addiction should be considered a bio-psycho-social-spiritual illness, for which the use of medication(s) is but only one component of overall treatment.” In addition to a thorough history and physical exam (including specific laboratory tests needed for this patient population), patients should undergo a mental health assessment with particular attention to possible psychiatric comorbidities. And since opioid use often co-occurs with other substance-related disorders, “the totality of substances that surround the addiction” should be assessed before treatment is considered.
Notably, the concomitant use of alcohol, sedatives, hypnotics, or anxiolytics with opioids can cause respiratory depression. Patients who use these agents may automatically require a higher level of care than that offered in typical primary care practices.
As well, social and environmental factors should be assessed, to identify both barriers to and facilitators for addiction treatment in general and pharmacotherapy in particular. “At a minimum, psychosocial treatment should include the following: psychosocial needs assessment, supportive counseling, links to existing family supports, and referrals to community services.” Physicians should be prepared to collaborate with qualified behavioral health care providers, the guideline states.
Urinary drug testing is recommended, both during the assessment process and frequently throughout treatment.
Regarding treatment, the guideline recommends considering the patient’s preferences, past treatment history, and the treatment setting when deciding whether to prescribe methadone, bupenorphrine, or naltrexone. The treatment venue is as important as the specific medication selected. Office-based treatment, which provides medication prescribed either weekly or monthly, is limited to buprenorphine only. It might not be suitable for patients who regularly use alcohol or other substances.
In contrast, treatment programs provide daily supervised dosing of methadone and, increasingly, buprenorphine. Methadone is recommended for patients who fail on buprenorphine or who would benefit from daily dosing and supervision.
Naltrexone can be prescribed in any setting by any clinician, but prescribers must be aware that adherence to oral naltrexone is generally poor, which often leads to treatment failure. Extended-release injectable naltrexone reduces but doesn’t eliminate adherence issues. Clinicians should reserve naltrexone “for patients who would be able to comply with special techniques to enhance their adherence, such as observed dosing.”
Dr. Kampton disclosed research ties with Braeburn Pharmaceuticals; Dr. Jarvis disclosed business ties with U.S. Preventive Medicine.
The American Society of Addiction Medicine has released a practice guideline to help clinicians evaluate and treat opioid use disorder, with the ultimate goal of getting more physicians to provide effective treatment.
Effective treatment of opioid use disorder “requires skill and time that are not generally available to primary care doctors in most practice models,” so much of the treatment provided in primary care has been “suboptimal.” This has probably worsened what the Centers for Disease Control and Prevention has described as an epidemic of opioid misuse and related deaths, said Dr. Kyle Kampman and Dr. Margaret Jarvis, cochairs of the ASAM’s guideline committee.
“At the same time, access to competent treatment is profoundly restricted because few physicians are willing and able to provide it,” they noted.
This guideline “is primarily intended for clinicians involved in evaluating patients and providing authorization for pharmacologic treatments at any level,” said Dr. Kampman of the University of Pennsylvania, Philadelphia, and Dr. Jarvis, of the Marworth Alcohol & Chemical Dependency Center, an entity of the Geisinger Health System, Waverly, Pa.
To develop the guideline, the committee – experts and researchers in internal medicine, family medicine, addiction medicine, addiction psychiatry, general psychiatry, obstetrics, pharmacology, and neurobiology, including some with allopathic or osteopathic training – first reviewed 34 existing clinical guidelines and 27 recent studies in the literature assessing medications used with psychosocial interventions. None of the existing guidelines included all the medications currently in use, and few addressed critical special populations such as pregnant women, patients with comorbid psychiatric disorders, and patients with chronic pain.
The ASAM guideline specifically addresses these and other special populations (for example, adolescents, patients in the criminal justice system). It includes detailed sections on treating opioid withdrawal and opioid overdose, as well as comprehensive discussions of methadone, buprenorphine, naltrexone, and psychosocial therapies.
The guideline offers numerous clinical recommendations regarding patient assessment and diagnosis (J Addict Med. 2015;9:358:67).
First, “addiction should be considered a bio-psycho-social-spiritual illness, for which the use of medication(s) is but only one component of overall treatment.” In addition to a thorough history and physical exam (including specific laboratory tests needed for this patient population), patients should undergo a mental health assessment with particular attention to possible psychiatric comorbidities. And since opioid use often co-occurs with other substance-related disorders, “the totality of substances that surround the addiction” should be assessed before treatment is considered.
Notably, the concomitant use of alcohol, sedatives, hypnotics, or anxiolytics with opioids can cause respiratory depression. Patients who use these agents may automatically require a higher level of care than that offered in typical primary care practices.
As well, social and environmental factors should be assessed, to identify both barriers to and facilitators for addiction treatment in general and pharmacotherapy in particular. “At a minimum, psychosocial treatment should include the following: psychosocial needs assessment, supportive counseling, links to existing family supports, and referrals to community services.” Physicians should be prepared to collaborate with qualified behavioral health care providers, the guideline states.
Urinary drug testing is recommended, both during the assessment process and frequently throughout treatment.
Regarding treatment, the guideline recommends considering the patient’s preferences, past treatment history, and the treatment setting when deciding whether to prescribe methadone, bupenorphrine, or naltrexone. The treatment venue is as important as the specific medication selected. Office-based treatment, which provides medication prescribed either weekly or monthly, is limited to buprenorphine only. It might not be suitable for patients who regularly use alcohol or other substances.
In contrast, treatment programs provide daily supervised dosing of methadone and, increasingly, buprenorphine. Methadone is recommended for patients who fail on buprenorphine or who would benefit from daily dosing and supervision.
Naltrexone can be prescribed in any setting by any clinician, but prescribers must be aware that adherence to oral naltrexone is generally poor, which often leads to treatment failure. Extended-release injectable naltrexone reduces but doesn’t eliminate adherence issues. Clinicians should reserve naltrexone “for patients who would be able to comply with special techniques to enhance their adherence, such as observed dosing.”
Dr. Kampton disclosed research ties with Braeburn Pharmaceuticals; Dr. Jarvis disclosed business ties with U.S. Preventive Medicine.
FROM JOURNAL OF ADDICTION MEDICINE
Key clinical point: The American Society of Addiction Medicine has released a clinical practice guideline that discusses all of the medications used in treating opioid use disorder as well as treating special populations.
Major finding: Access to competent treatment of opioid use disorder has been “profoundly restricted,” because few physicians are willing and able to provide it.
Data source: A review of 34 existing clinical guidelines and 27 studies of treatments, and a compilation of clinical recommendations for treating opioid use disorder.
Disclosures: Dr. Kampton disclosed research ties with Braeburn Pharmaceuticals; Dr. Jarvis disclosed business ties with U.S. Preventive Medicine.
Zika virus: What clinicians must know
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr. St. John said, the more exposure a Zika virus–infected individual has to the outside world, the more likely he or she is to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the U.S., despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr. St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr. Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr. Senanayake added that advanced research is currently underway in mosquito-control efforts, including the idea of releasing mosquitoes into the wild which have been genetically modified so they can’t breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin and Guadeloupe and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr. Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
*This story was updated 1/25/2016.
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr. St. John said, the more exposure a Zika virus–infected individual has to the outside world, the more likely he or she is to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the U.S., despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr. St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr. Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr. Senanayake added that advanced research is currently underway in mosquito-control efforts, including the idea of releasing mosquitoes into the wild which have been genetically modified so they can’t breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin and Guadeloupe and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr. Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
*This story was updated 1/25/2016.
The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.
Those who are infected are also advised to stay indoors and remain as isolated as possible for at least a week after symptoms first present. While the risk of a domestic outbreak is probably low, Dr. St. John said, the more exposure a Zika virus–infected individual has to the outside world, the more likely he or she is to be bitten by another mosquito, which can then carry and transmit the virus to another person.
“Chikungunya and dengue virus, which are transmitted by the same vectors [as Zika virus], have not managed to establish ongoing transmission in the U.S., despite repeated importations, [so] it is likely that Zika virus’ spread would follow a similar pattern,” Dr. St. John noted.
Though rare, sexual transmission of Zika virus has also been found in at least one case, although it had been previously suspected for some time. In December 2013, a 44-year-old Tahitian man sought treatment for hematospermia. Analysis of his sperm, however, found Zika virus, indicating possible sexual transmission of the virus.
“The observation that [Zika virus] RNA was detectable in urine after viremia clearance in blood suggests that, as found for [dengue] and [West Nile virus] infections, urine samples can yield evidence of [Zika virus] for late diagnosis, but more investigation is needed,” the study concluded.
“The best way to control all this is to control the mosquito,” said Dr. Senanayake. “You get a four-for-one deal; not only do you get rid of Zika virus, but also chikungunya, dengue, and yellow fever.” Dr. Senanayake added that advanced research is currently underway in mosquito-control efforts, including the idea of releasing mosquitoes into the wild which have been genetically modified so they can’t breed.
Now that the Illinois Department of Health has confirmed two new cases of Zika virus infection in that state, with other new cases cropping up in Saint Martin and Guadeloupe and El Salvador, providers should remain vigilant, taking note of patients who have traveled to afflicted regions and show mosquito bites. Person-to-person transmission is “rare as hen’s teeth,” said Dr. Senanayake, which is to say, it is highly unlikely to occur. Nonetheless, he said information and communication is the best way to ensure that Zika virus does not spread widely in the United States.
*This story was updated 1/25/2016.
CDC expands Zika virus travel warnings; more U.S. cases confirmed
Officials at the Centers for Disease Control and Prevention have issued an expanded travel alert for regions where travelers may be at risk of contracting Zika virus.
The mosquito-borne flavivirus may be associated with an increased risk of microcephaly and other intracranial and neurologic abnormalities in infants whose mothers were infected with Zika virus during pregnancy. Women who are pregnant or considering becoming pregnant should consider avoiding travel to countries included in the Zika virus alert.
The CDC’s expanded warning includes Barbados, Bolivia, Ecuador, Guadeloupe, Saint Martin, Guyana, Cape Verde, and Samoa. This is in addition to the previous travel alert for Puerto Rico (a U.S. territory), Brazil, Colombia, El Salvador, French Guiana, Guatemala, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Suriname, and Venezuela.
In the United States, about a dozen cases of Zika virus have been reported, according to the CDC. States thus far where individuals have tested positive for the virus are Texas, Florida, Illinois, New Jersey, and Hawaii. These dozen cases include two pregnant women who tested positive for the Zika virus in Illinois this week. In Hawaii, a woman who had lived in Brazil while pregnant has given birth to a baby with microcephaly and congenital Zika virus infection. To date, all confirmed cases of Zika virus in the U.S. have been in individuals who traveled to areas with Zika virus transmission.
Zika virus, a member of the family of viruses that includes dengue fever, is spread by mosquitoes of the Aedes species, according to Dr. Amesh Adalja.
Dr. Adalja, a member of the public health committee of the Infectious Disease Society of America and an instructor in the department of infectious diseases at the University of Pittsburgh Medical Center, noted that though the virus has been known since the 1940s, “it was not considered a major public health threat” because of the generally mild course of the disease.
Infection is asymptomatic in 80% of individuals, he said. Symptoms of Zika virus infection, if they appear, include initial fever, a maculopapular rash, arthralgia, and sometimes conjunctivitis. There is no treatment for the disease and care is supportive.
A recent explosion of Zika virus cases in Brazil, however, has been associated with a large increase in cases of microcephaly in newborns. Though the association has not been confirmed, Zika virus has been found in infants born with microcephaly and in the placentas of mothers of babies with microcephaly.
The CDC has issued interim guidance for diagnosis, treatment, and management of suspected Zika virus in pregnant women. All pregnant women should be asked about travel to countries with known Zika virus exposure, with surveillance by fetal ultrasound and, in some cases, testing for Zika virus guided by symptoms and likelihood of exposure.
The CDC recommends vigilance against mosquito bites for pregnant women who do travel to areas with Zika virus activity, including the use of effective insect repellent, protective clothing, and remaining in and sleeping in air-conditioned rooms when possible.
In the United States, there is reason to be concerned about Zika virus, since “the scale of travel is very, very high” to the Central and South American and Caribbean countries where Zika virus transmission is active, Dr. Adalja said. However, since the same vector also transmits dengue fever and the Chikungunya virus – currently the focus of increasing concern in the U.S. – aggressive vector control measures are already underway in parts of the country where Aedes species mosquitoes are resident.
Though the consequences of the apparent association between maternal Zika virus infection and infant microcephaly are devastating, said Dr. Adalja, “it’s important that people put this in the proper public health perspective. Dengue fever kills thousands of people each year.”*
Dr. Adalja said that he expects commercially available testing for Zika virus to be developed; currently, testing is currently only available from the CDC and from some states’ departments of public health.
Additional resources for physicians
American College of Obstetricians and Gynecologists: www.acog.org/About-ACOG/News-Room/Practice-Advisories
CDC: www.cdc.gov/zika/
*Correction, 1/25/2016: An earlier version of this story misstated the number of deaths from dengue fever.
On Twitter @karioakes
Officials at the Centers for Disease Control and Prevention have issued an expanded travel alert for regions where travelers may be at risk of contracting Zika virus.
The mosquito-borne flavivirus may be associated with an increased risk of microcephaly and other intracranial and neurologic abnormalities in infants whose mothers were infected with Zika virus during pregnancy. Women who are pregnant or considering becoming pregnant should consider avoiding travel to countries included in the Zika virus alert.
The CDC’s expanded warning includes Barbados, Bolivia, Ecuador, Guadeloupe, Saint Martin, Guyana, Cape Verde, and Samoa. This is in addition to the previous travel alert for Puerto Rico (a U.S. territory), Brazil, Colombia, El Salvador, French Guiana, Guatemala, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Suriname, and Venezuela.
In the United States, about a dozen cases of Zika virus have been reported, according to the CDC. States thus far where individuals have tested positive for the virus are Texas, Florida, Illinois, New Jersey, and Hawaii. These dozen cases include two pregnant women who tested positive for the Zika virus in Illinois this week. In Hawaii, a woman who had lived in Brazil while pregnant has given birth to a baby with microcephaly and congenital Zika virus infection. To date, all confirmed cases of Zika virus in the U.S. have been in individuals who traveled to areas with Zika virus transmission.
Zika virus, a member of the family of viruses that includes dengue fever, is spread by mosquitoes of the Aedes species, according to Dr. Amesh Adalja.
Dr. Adalja, a member of the public health committee of the Infectious Disease Society of America and an instructor in the department of infectious diseases at the University of Pittsburgh Medical Center, noted that though the virus has been known since the 1940s, “it was not considered a major public health threat” because of the generally mild course of the disease.
Infection is asymptomatic in 80% of individuals, he said. Symptoms of Zika virus infection, if they appear, include initial fever, a maculopapular rash, arthralgia, and sometimes conjunctivitis. There is no treatment for the disease and care is supportive.
A recent explosion of Zika virus cases in Brazil, however, has been associated with a large increase in cases of microcephaly in newborns. Though the association has not been confirmed, Zika virus has been found in infants born with microcephaly and in the placentas of mothers of babies with microcephaly.
The CDC has issued interim guidance for diagnosis, treatment, and management of suspected Zika virus in pregnant women. All pregnant women should be asked about travel to countries with known Zika virus exposure, with surveillance by fetal ultrasound and, in some cases, testing for Zika virus guided by symptoms and likelihood of exposure.
The CDC recommends vigilance against mosquito bites for pregnant women who do travel to areas with Zika virus activity, including the use of effective insect repellent, protective clothing, and remaining in and sleeping in air-conditioned rooms when possible.
In the United States, there is reason to be concerned about Zika virus, since “the scale of travel is very, very high” to the Central and South American and Caribbean countries where Zika virus transmission is active, Dr. Adalja said. However, since the same vector also transmits dengue fever and the Chikungunya virus – currently the focus of increasing concern in the U.S. – aggressive vector control measures are already underway in parts of the country where Aedes species mosquitoes are resident.
Though the consequences of the apparent association between maternal Zika virus infection and infant microcephaly are devastating, said Dr. Adalja, “it’s important that people put this in the proper public health perspective. Dengue fever kills thousands of people each year.”*
Dr. Adalja said that he expects commercially available testing for Zika virus to be developed; currently, testing is currently only available from the CDC and from some states’ departments of public health.
Additional resources for physicians
American College of Obstetricians and Gynecologists: www.acog.org/About-ACOG/News-Room/Practice-Advisories
CDC: www.cdc.gov/zika/
*Correction, 1/25/2016: An earlier version of this story misstated the number of deaths from dengue fever.
On Twitter @karioakes
Officials at the Centers for Disease Control and Prevention have issued an expanded travel alert for regions where travelers may be at risk of contracting Zika virus.
The mosquito-borne flavivirus may be associated with an increased risk of microcephaly and other intracranial and neurologic abnormalities in infants whose mothers were infected with Zika virus during pregnancy. Women who are pregnant or considering becoming pregnant should consider avoiding travel to countries included in the Zika virus alert.
The CDC’s expanded warning includes Barbados, Bolivia, Ecuador, Guadeloupe, Saint Martin, Guyana, Cape Verde, and Samoa. This is in addition to the previous travel alert for Puerto Rico (a U.S. territory), Brazil, Colombia, El Salvador, French Guiana, Guatemala, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Suriname, and Venezuela.
In the United States, about a dozen cases of Zika virus have been reported, according to the CDC. States thus far where individuals have tested positive for the virus are Texas, Florida, Illinois, New Jersey, and Hawaii. These dozen cases include two pregnant women who tested positive for the Zika virus in Illinois this week. In Hawaii, a woman who had lived in Brazil while pregnant has given birth to a baby with microcephaly and congenital Zika virus infection. To date, all confirmed cases of Zika virus in the U.S. have been in individuals who traveled to areas with Zika virus transmission.
Zika virus, a member of the family of viruses that includes dengue fever, is spread by mosquitoes of the Aedes species, according to Dr. Amesh Adalja.
Dr. Adalja, a member of the public health committee of the Infectious Disease Society of America and an instructor in the department of infectious diseases at the University of Pittsburgh Medical Center, noted that though the virus has been known since the 1940s, “it was not considered a major public health threat” because of the generally mild course of the disease.
Infection is asymptomatic in 80% of individuals, he said. Symptoms of Zika virus infection, if they appear, include initial fever, a maculopapular rash, arthralgia, and sometimes conjunctivitis. There is no treatment for the disease and care is supportive.
A recent explosion of Zika virus cases in Brazil, however, has been associated with a large increase in cases of microcephaly in newborns. Though the association has not been confirmed, Zika virus has been found in infants born with microcephaly and in the placentas of mothers of babies with microcephaly.
The CDC has issued interim guidance for diagnosis, treatment, and management of suspected Zika virus in pregnant women. All pregnant women should be asked about travel to countries with known Zika virus exposure, with surveillance by fetal ultrasound and, in some cases, testing for Zika virus guided by symptoms and likelihood of exposure.
The CDC recommends vigilance against mosquito bites for pregnant women who do travel to areas with Zika virus activity, including the use of effective insect repellent, protective clothing, and remaining in and sleeping in air-conditioned rooms when possible.
In the United States, there is reason to be concerned about Zika virus, since “the scale of travel is very, very high” to the Central and South American and Caribbean countries where Zika virus transmission is active, Dr. Adalja said. However, since the same vector also transmits dengue fever and the Chikungunya virus – currently the focus of increasing concern in the U.S. – aggressive vector control measures are already underway in parts of the country where Aedes species mosquitoes are resident.
Though the consequences of the apparent association between maternal Zika virus infection and infant microcephaly are devastating, said Dr. Adalja, “it’s important that people put this in the proper public health perspective. Dengue fever kills thousands of people each year.”*
Dr. Adalja said that he expects commercially available testing for Zika virus to be developed; currently, testing is currently only available from the CDC and from some states’ departments of public health.
Additional resources for physicians
American College of Obstetricians and Gynecologists: www.acog.org/About-ACOG/News-Room/Practice-Advisories
CDC: www.cdc.gov/zika/
*Correction, 1/25/2016: An earlier version of this story misstated the number of deaths from dengue fever.
On Twitter @karioakes
Understanding stillbirth
When a couple learns that “they are pregnant,” it is often one of the most joyous moments in their lives. However, despite the modern prenatal care available to women in the United States, pregnancy loss remains a real concern. Miscarriage is estimated to occur in 15%-20% of pregnancies; recurrent pregnancy loss in about 1%-2% of pregnancies; and stillbirth in as many as 1% of pregnancies. The causes of pregnancy loss can range from those we can diagnose, such as genetic factors, anatomic complications, and thrombophilia, to those that elude us completely.
In December 2015, investigators from Karolinska Institutet in Stockholm published a study indicating that women who gained weight between their first and second pregnancies, but who were a healthy weight prior to their first pregnancy, had an increased risk of experiencing a stillbirth (30%-50%), or having an infant who died within the first year (27%-60%) (Lancet 2015. doi: 10.1016/S0140-6736(15)00990-3). We have devoted a number of Master Class columns to the link between obesity and pregnancy complications, and this study further reinforces the influence of a healthy weight on pregnancy outcomes.
In addition to lifestyle modifications, evidence has suggested that low-molecular-weight heparin, aspirin, or vitamin supplements, in combination with appropriate surveillance and management, may reduce risk of pregnancy loss. However, more work is needed to fully understand why fetal death occurs if we are to better equip ourselves, and our patients, with all the information necessary to prevent loss from happening.
For this reason, we have invited Dr. Uma M. Reddy of the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health, to address one of the most devastating types of pregnancy losses: stillbirth. As a program scientist for large research studies, such as the Stillbirth Collaborative Research Network, Dr. Reddy’s unique perspective will add greatly to our understanding of pregnancy loss.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece reported having no relevant financial disclosures. He is the medical editor of this column.
When a couple learns that “they are pregnant,” it is often one of the most joyous moments in their lives. However, despite the modern prenatal care available to women in the United States, pregnancy loss remains a real concern. Miscarriage is estimated to occur in 15%-20% of pregnancies; recurrent pregnancy loss in about 1%-2% of pregnancies; and stillbirth in as many as 1% of pregnancies. The causes of pregnancy loss can range from those we can diagnose, such as genetic factors, anatomic complications, and thrombophilia, to those that elude us completely.
In December 2015, investigators from Karolinska Institutet in Stockholm published a study indicating that women who gained weight between their first and second pregnancies, but who were a healthy weight prior to their first pregnancy, had an increased risk of experiencing a stillbirth (30%-50%), or having an infant who died within the first year (27%-60%) (Lancet 2015. doi: 10.1016/S0140-6736(15)00990-3). We have devoted a number of Master Class columns to the link between obesity and pregnancy complications, and this study further reinforces the influence of a healthy weight on pregnancy outcomes.
In addition to lifestyle modifications, evidence has suggested that low-molecular-weight heparin, aspirin, or vitamin supplements, in combination with appropriate surveillance and management, may reduce risk of pregnancy loss. However, more work is needed to fully understand why fetal death occurs if we are to better equip ourselves, and our patients, with all the information necessary to prevent loss from happening.
For this reason, we have invited Dr. Uma M. Reddy of the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health, to address one of the most devastating types of pregnancy losses: stillbirth. As a program scientist for large research studies, such as the Stillbirth Collaborative Research Network, Dr. Reddy’s unique perspective will add greatly to our understanding of pregnancy loss.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece reported having no relevant financial disclosures. He is the medical editor of this column.
When a couple learns that “they are pregnant,” it is often one of the most joyous moments in their lives. However, despite the modern prenatal care available to women in the United States, pregnancy loss remains a real concern. Miscarriage is estimated to occur in 15%-20% of pregnancies; recurrent pregnancy loss in about 1%-2% of pregnancies; and stillbirth in as many as 1% of pregnancies. The causes of pregnancy loss can range from those we can diagnose, such as genetic factors, anatomic complications, and thrombophilia, to those that elude us completely.
In December 2015, investigators from Karolinska Institutet in Stockholm published a study indicating that women who gained weight between their first and second pregnancies, but who were a healthy weight prior to their first pregnancy, had an increased risk of experiencing a stillbirth (30%-50%), or having an infant who died within the first year (27%-60%) (Lancet 2015. doi: 10.1016/S0140-6736(15)00990-3). We have devoted a number of Master Class columns to the link between obesity and pregnancy complications, and this study further reinforces the influence of a healthy weight on pregnancy outcomes.
In addition to lifestyle modifications, evidence has suggested that low-molecular-weight heparin, aspirin, or vitamin supplements, in combination with appropriate surveillance and management, may reduce risk of pregnancy loss. However, more work is needed to fully understand why fetal death occurs if we are to better equip ourselves, and our patients, with all the information necessary to prevent loss from happening.
For this reason, we have invited Dr. Uma M. Reddy of the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health, to address one of the most devastating types of pregnancy losses: stillbirth. As a program scientist for large research studies, such as the Stillbirth Collaborative Research Network, Dr. Reddy’s unique perspective will add greatly to our understanding of pregnancy loss.
Dr. Reece, who specializes in maternal-fetal medicine, is vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. Dr. Reece reported having no relevant financial disclosures. He is the medical editor of this column.
Research adds insight on stillbirth risk factors
Stillbirth is a major public health problem, occurring in approximately 1 of every 160 pregnancies in the United States. The rate has remained stagnant since 2006. Prior to that time, from 1990 to 2006, the rate declined somewhat, but only half as much as the decline in infant mortality during this time period. Racial disparities also have persisted, with non-Hispanic black women having more than a twofold increase in risk (Natl Vital Stat Rep. 2012;60:1-22).
Research conducted by the Stillbirth Collaborative Research Network (SCRN) and others has provided us with insight on risk factors and on probable and possible causes of death among stillbirths, which are defined as fetal deaths at 20 or more weeks’ gestation. We know from SCRN data, for instance, that black women are more likely to have stillbirths associated with obstetric complications and infections than white and Hispanic women. However, we still cannot explain a substantial proportion of stillbirths, despite a complete evaluation, or predict who will have a stillbirth.
What we can do as obstetricians is be aware that stillbirth is one of the most common adverse pregnancy outcomes in the United States and counsel women regarding risk factors that are modifiable. Moreover, when stillbirth happens, a complete postmortem evaluation that includes autopsy, placental pathology, karyotype or microarray analysis, and fetal-maternal hemorrhage testing is recommended (Obstet Gynecol. 2009;113[3]:748-61). Recent data show that each of these four components is valuable and should be considered the basic work-up for stillbirth.
Risks and causes
Pregnancy history was the strongest baseline risk factor for stillbirth in an analysis of 614 stillbirths and 1,816 live births in the SCRN’s population-based, case-control study conducted between 2006 and 2008. The SCRN was initiated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in 2003. This critical population-based study was conducted at 59 U.S. tertiary care and community hospitals in five catchment areas and has been analyzed in more than 15 published reports.
Women with a previous stillbirth have been known to be at 5- to 10-fold increased risk of a recurrence of stillbirth, and the SCRN findings confirmed this. The study added to our knowledge, however, with the finding that even a prior pregnancy loss at less than 20 weeks’ gestation increased the risk for stillbirth.
Other risk factors identified in the study, in addition to race, included having a multifetal pregnancy (adjusted odds ratio of 4.59), diabetes (AOR of 2.50), maternal age of 40 years or older (AOR of 2.41), maternal AB blood type (AOR of 1.96, compared with type O), a history of drug addiction (AOR of 2.08), smoking during the 3 months prior to pregnancy (AOR of 1.55-1.57, depending on amount), and being unmarried and not cohabitating (AOR of 1.69). Regarding racial disparity, the study showed that elevated risk of stillbirth for non-Hispanic blacks occurred predominantly prior to 24 weeks of gestation.
As in prior research, overweight and obesity also conferred elevated risks in the SCRN study (AORs of 1.43 and 1.72, respectively), and these risks were not explained by either diabetes or hypertension (JAMA. 2011;306:2469-79).
The use of assisted reproductive technology was not included in the study’s multivariate model, but previous research has shown a fourfold increased risk of stillbirth for singleton IVF/ICSI pregnancies. The reason is unclear, but the risk appears to be more related to IVF/ICSI rather than the underlying infertility (Hum Reprod. 2010 May;25[5]:1312-6).
A previous preterm or small-for-gestational-age birth has also been shown in prior research to be a significant risk factor for stillbirth. Less clear is the role of previous cesarean delivery in stillbirth risk. An association has been demonstrated in several studies, however, including one involving about 180,000 singleton pregnancies of 23 or more weeks’ gestation. Women in this cohort who had a previous cesarean delivery had a 1.3-fold increased risk of antepartum stillbirth, after controlling for important factors such as race, body mass index (BMI), and maternal disease (Obstet Gynecol. 2010 Nov;116[5]:1119-26).
In another analysis of the SCRN study looking specifically at causes of stillbirth, a “probable” cause of death was found in 61% of cases and a “possible or probable” cause of death in more than 76% of cases. The most common causes were obstetric complications (29.3%), placental abnormalities (23.6%), fetal genetic/structural abnormalities (13.7%), infection (12.9%), umbilical cord abnormalities (10.4%), hypertensive disorders (9.2%), and other maternal medical conditions (7.8%).
A higher proportion of stillbirths in non-Hispanic black women, compared with non-Hispanic white women and Hispanic women was associated with obstetric complications (43.5%) and infections (25.2%). This finding combined with the finding that stillbirth in black women often occurs at less than 24 weeks’ gestation suggests that measures aimed at reducing the rate of spontaneous preterm birth in black women could potentially reduce the rate of stillbirth as well (JAMA. 2011 Dec 14;306[22]:2459-68).
Work-up and prevention
Prevention of stillbirth requires that we identify the women at highest risk, and thus far this ability still eludes us. Apart from occurrence of previous stillbirth or pregnancy loss, other risk factors have had limited predictive value in the SCRN analyses and other research.
Biomarkers such as a low PAPP-A during the first trimester and a high AFP in the second trimester – as well as Doppler imaging of the uterine artery – have also been associated with stillbirth, but again, the positive predictive value has been shown to be low (Clin Obstet Gynecol. 2010 Sep;53[3]:597-606). More research is needed to determine if some combination of biochemical markers, imaging, and other risk factors can predict which women are at highest risk.
In the meantime, attention can be paid – in the preconception period if possible – to modifiable risk factors such as maternal obesity, diabetes, and smoking. About 10% of stillbirths are associated with maternal conditions such as hypertension and diabetes, and late stillbirths in particular (28 weeks or later) are associated with maternal medical conditions that are potentially preventable.
Normalization of prepregnancy weight should be a goal, since the overall risk of stillbirth appears to increase independently with increasing BMI. Glycemic control should also be achieved: A recent meta-analysis of preconception and prenatal care of diabetic women estimated “conservatively” that 10% of diabetes-associated stillbirths could be prevented with early detection and glycemic control (BMC Public Health. 2011;11 Suppl 3:S2). Research has also shown that women who quit smoking between their first and second pregnancy reduce their stillbirth risk to that of nonsmokers in the second pregnancy (BJOG. 2007 Jun;114[6]:699-704).
When stillbirth happens, a thorough work-up is recommended in order to counsel for future pregnancies and decrease the risk of recurrence. Evaluations for causes of stillbirth are too often incomplete in the United States for various reasons, including emotional, cultural, and resource factors. Even if a cause is not found, many families appreciate knowing that every effort has been made to determine a cause of death.
Four components of evaluation – autopsy, placental examination, karyotype or microarray analysis, and fetal-maternal hemorrhage testing – have proven to be high-yield tests when performed in all cases of stillbirth.
In the SCRN study, of 512 stillbirths undergoing a complete evaluation, 66.4% had a positive result – defined as abnormalities contributing to a probable or possible cause – for at least one of the first three tests (JAMA. 2011 Dec 14;306[22]:2459-68).
A Dutch study of 1,025 stillbirths similarly demonstrated that all four tests are justified. A test was defined as valuable in this study if it established or excluded a cause of stillbirth. Placental examination was determined to be the most valuable test, helping to determine a cause of death in 95.7% of cases. Autopsy was valuable 72.6% of the time, and cytogenetic analysis was valuable in 29% of cases.
Kleihauer-Betke testing for fetal-maternal hemorrhage was positive in 11.9% of women. However, fetal maternal hemorrhage was considered the cause of death in only 1.3%.of cases because, beyond a positive Kleihauer-Betke test, evidence of fetal anemia confirmed by placental examination and/or autopsy was required for hemorrhage to be considered the cause of death (Am. J. Obstet. Gynecol. 2012;206:53.e1-12). Because Kleihauer-Betke testing is ideally performed before induction, authors of both the SCRN study and the Dutch study believe it is a valuable test to be offered in all cases.
In both studies, the yield of other stillbirth diagnostic tests (for example, maternal serology, hormone assessment, and toxicology screen) was low, indicating that these tests are considered sequential and can be performed only when the clinical history or findings of the four core tests raise suspicion of particular potential causes. Antinuclear antibody testing and TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers have an extremely low yield and are generally not useful.
For detecting genetic abnormalities after stillbirth, it appears that microarray analysis is superior to karyotype analysis. In a SCRN analysis of samples from 532 stillbirths, microarray yielded results more often and identified more genetic abnormalities. Unlike karyotype, it does not require live cells, which makes it preferable for stillbirth evaluation (N Engl J Med. 2012 Dec 6;367[23]:2185-93).
Current research
One of the more significant studies underway on prevention is looking at labor induction as an intervention for reducing stillbirths and improving other perinatal outcomes. The ARRIVE trial (“A Randomized Trial of Induction Versus Expectant Management”), currently in the recruitment stage, will examine outcomes after induction at 39 weeks’ gestation, compared with expectant management in 6,000 patients (clinicaltrials.gov/ct2/show/NCT01990612).
Common wisdom informed by retrospective cohort studies has long told us that inducing labor prior to 41 weeks’ gestation is associated with a higher risk of cesarean delivery in nulliparous women. However, recent observational data have suggested that women whose labor is induced actually have fewer cesarean deliveries and better perinatal outcomes, including a lower risk of stillbirth (AJOG 2012;207:502.e1-8).
In addition, a meta-analysis published in 2014, as the ARRIVE trial was taking shape, reported a 12% reduction in cesarean delivery, and a reduced risk of stillbirth, among women whose labor was induced. The initial cervical score did not impact the main findings (CMAJ. 2014 Jun 10;186[9]:665-73). If these findings are confirmed in the ARRIVE trial, we could see a new opportunity for stillbirth prevention.
Another ongoing study of 10,000 singleton pregnancies – the Nulliparous Pregnancy Outcomes: Monitoring Mothers-to-Be (nuMoM2b) study – may also lead to prevention strategies in women for whom the current pregnancy will lead to their first delivery. Among the questions being examined in this eight-site study are whether sleep-disordered breathing, or apnea, and a supine sleep position are risk factors for adverse pregnancy outcomes including stillbirth.
Supine sleeping in the last month of pregnancy was strongly associated with stillbirth in a recent analysis from the Sydney Stillbirth Study (Obstet Gynecol. 2015 Feb;125[2]:347-55), and an early analysis of a nuMoM2b subset has shown associations between sleep-disordered breathing in midpregnancy and the development of hypertensive disorders of pregnancy, and between sleep-disordered breathing in early- and mid-pregnancy and gestational diabetes (Am J Obstet Gynecol. 2015;212:S424-425).
The possible role of low-dose aspirin in preventing stillbirth also needs more exploration. A recent randomized trial of women attempting to become pregnant after having had one or two prior pregnancy losses found no difference overall in live birth rates between those who took low-dose aspirin and those assigned to placebo. However, there was one subgroup – women with a single loss at less than 20 weeks’ gestation during the previous year – in which live birth rates were higher in the aspirin group (Lancet. 2014 Jul 5;384[9937]:29-36). More research is necessary to determine if low-dose aspirin administration in women with a previous stillbirth improves pregnancy outcome.
Dr. Reddy is a member at the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. She is a board-certified ob.gyn. and maternal-fetal medicine specialist. She is the program scientist for the Maternal-Fetal Medicine Units Network and for the Stillbirth Collaborative Research Network. The comments and views of the author do not necessarily represent the views of the NICHD.
Stillbirth is a major public health problem, occurring in approximately 1 of every 160 pregnancies in the United States. The rate has remained stagnant since 2006. Prior to that time, from 1990 to 2006, the rate declined somewhat, but only half as much as the decline in infant mortality during this time period. Racial disparities also have persisted, with non-Hispanic black women having more than a twofold increase in risk (Natl Vital Stat Rep. 2012;60:1-22).
Research conducted by the Stillbirth Collaborative Research Network (SCRN) and others has provided us with insight on risk factors and on probable and possible causes of death among stillbirths, which are defined as fetal deaths at 20 or more weeks’ gestation. We know from SCRN data, for instance, that black women are more likely to have stillbirths associated with obstetric complications and infections than white and Hispanic women. However, we still cannot explain a substantial proportion of stillbirths, despite a complete evaluation, or predict who will have a stillbirth.
What we can do as obstetricians is be aware that stillbirth is one of the most common adverse pregnancy outcomes in the United States and counsel women regarding risk factors that are modifiable. Moreover, when stillbirth happens, a complete postmortem evaluation that includes autopsy, placental pathology, karyotype or microarray analysis, and fetal-maternal hemorrhage testing is recommended (Obstet Gynecol. 2009;113[3]:748-61). Recent data show that each of these four components is valuable and should be considered the basic work-up for stillbirth.
Risks and causes
Pregnancy history was the strongest baseline risk factor for stillbirth in an analysis of 614 stillbirths and 1,816 live births in the SCRN’s population-based, case-control study conducted between 2006 and 2008. The SCRN was initiated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in 2003. This critical population-based study was conducted at 59 U.S. tertiary care and community hospitals in five catchment areas and has been analyzed in more than 15 published reports.
Women with a previous stillbirth have been known to be at 5- to 10-fold increased risk of a recurrence of stillbirth, and the SCRN findings confirmed this. The study added to our knowledge, however, with the finding that even a prior pregnancy loss at less than 20 weeks’ gestation increased the risk for stillbirth.
Other risk factors identified in the study, in addition to race, included having a multifetal pregnancy (adjusted odds ratio of 4.59), diabetes (AOR of 2.50), maternal age of 40 years or older (AOR of 2.41), maternal AB blood type (AOR of 1.96, compared with type O), a history of drug addiction (AOR of 2.08), smoking during the 3 months prior to pregnancy (AOR of 1.55-1.57, depending on amount), and being unmarried and not cohabitating (AOR of 1.69). Regarding racial disparity, the study showed that elevated risk of stillbirth for non-Hispanic blacks occurred predominantly prior to 24 weeks of gestation.
As in prior research, overweight and obesity also conferred elevated risks in the SCRN study (AORs of 1.43 and 1.72, respectively), and these risks were not explained by either diabetes or hypertension (JAMA. 2011;306:2469-79).
The use of assisted reproductive technology was not included in the study’s multivariate model, but previous research has shown a fourfold increased risk of stillbirth for singleton IVF/ICSI pregnancies. The reason is unclear, but the risk appears to be more related to IVF/ICSI rather than the underlying infertility (Hum Reprod. 2010 May;25[5]:1312-6).
A previous preterm or small-for-gestational-age birth has also been shown in prior research to be a significant risk factor for stillbirth. Less clear is the role of previous cesarean delivery in stillbirth risk. An association has been demonstrated in several studies, however, including one involving about 180,000 singleton pregnancies of 23 or more weeks’ gestation. Women in this cohort who had a previous cesarean delivery had a 1.3-fold increased risk of antepartum stillbirth, after controlling for important factors such as race, body mass index (BMI), and maternal disease (Obstet Gynecol. 2010 Nov;116[5]:1119-26).
In another analysis of the SCRN study looking specifically at causes of stillbirth, a “probable” cause of death was found in 61% of cases and a “possible or probable” cause of death in more than 76% of cases. The most common causes were obstetric complications (29.3%), placental abnormalities (23.6%), fetal genetic/structural abnormalities (13.7%), infection (12.9%), umbilical cord abnormalities (10.4%), hypertensive disorders (9.2%), and other maternal medical conditions (7.8%).
A higher proportion of stillbirths in non-Hispanic black women, compared with non-Hispanic white women and Hispanic women was associated with obstetric complications (43.5%) and infections (25.2%). This finding combined with the finding that stillbirth in black women often occurs at less than 24 weeks’ gestation suggests that measures aimed at reducing the rate of spontaneous preterm birth in black women could potentially reduce the rate of stillbirth as well (JAMA. 2011 Dec 14;306[22]:2459-68).
Work-up and prevention
Prevention of stillbirth requires that we identify the women at highest risk, and thus far this ability still eludes us. Apart from occurrence of previous stillbirth or pregnancy loss, other risk factors have had limited predictive value in the SCRN analyses and other research.
Biomarkers such as a low PAPP-A during the first trimester and a high AFP in the second trimester – as well as Doppler imaging of the uterine artery – have also been associated with stillbirth, but again, the positive predictive value has been shown to be low (Clin Obstet Gynecol. 2010 Sep;53[3]:597-606). More research is needed to determine if some combination of biochemical markers, imaging, and other risk factors can predict which women are at highest risk.
In the meantime, attention can be paid – in the preconception period if possible – to modifiable risk factors such as maternal obesity, diabetes, and smoking. About 10% of stillbirths are associated with maternal conditions such as hypertension and diabetes, and late stillbirths in particular (28 weeks or later) are associated with maternal medical conditions that are potentially preventable.
Normalization of prepregnancy weight should be a goal, since the overall risk of stillbirth appears to increase independently with increasing BMI. Glycemic control should also be achieved: A recent meta-analysis of preconception and prenatal care of diabetic women estimated “conservatively” that 10% of diabetes-associated stillbirths could be prevented with early detection and glycemic control (BMC Public Health. 2011;11 Suppl 3:S2). Research has also shown that women who quit smoking between their first and second pregnancy reduce their stillbirth risk to that of nonsmokers in the second pregnancy (BJOG. 2007 Jun;114[6]:699-704).
When stillbirth happens, a thorough work-up is recommended in order to counsel for future pregnancies and decrease the risk of recurrence. Evaluations for causes of stillbirth are too often incomplete in the United States for various reasons, including emotional, cultural, and resource factors. Even if a cause is not found, many families appreciate knowing that every effort has been made to determine a cause of death.
Four components of evaluation – autopsy, placental examination, karyotype or microarray analysis, and fetal-maternal hemorrhage testing – have proven to be high-yield tests when performed in all cases of stillbirth.
In the SCRN study, of 512 stillbirths undergoing a complete evaluation, 66.4% had a positive result – defined as abnormalities contributing to a probable or possible cause – for at least one of the first three tests (JAMA. 2011 Dec 14;306[22]:2459-68).
A Dutch study of 1,025 stillbirths similarly demonstrated that all four tests are justified. A test was defined as valuable in this study if it established or excluded a cause of stillbirth. Placental examination was determined to be the most valuable test, helping to determine a cause of death in 95.7% of cases. Autopsy was valuable 72.6% of the time, and cytogenetic analysis was valuable in 29% of cases.
Kleihauer-Betke testing for fetal-maternal hemorrhage was positive in 11.9% of women. However, fetal maternal hemorrhage was considered the cause of death in only 1.3%.of cases because, beyond a positive Kleihauer-Betke test, evidence of fetal anemia confirmed by placental examination and/or autopsy was required for hemorrhage to be considered the cause of death (Am. J. Obstet. Gynecol. 2012;206:53.e1-12). Because Kleihauer-Betke testing is ideally performed before induction, authors of both the SCRN study and the Dutch study believe it is a valuable test to be offered in all cases.
In both studies, the yield of other stillbirth diagnostic tests (for example, maternal serology, hormone assessment, and toxicology screen) was low, indicating that these tests are considered sequential and can be performed only when the clinical history or findings of the four core tests raise suspicion of particular potential causes. Antinuclear antibody testing and TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers have an extremely low yield and are generally not useful.
For detecting genetic abnormalities after stillbirth, it appears that microarray analysis is superior to karyotype analysis. In a SCRN analysis of samples from 532 stillbirths, microarray yielded results more often and identified more genetic abnormalities. Unlike karyotype, it does not require live cells, which makes it preferable for stillbirth evaluation (N Engl J Med. 2012 Dec 6;367[23]:2185-93).
Current research
One of the more significant studies underway on prevention is looking at labor induction as an intervention for reducing stillbirths and improving other perinatal outcomes. The ARRIVE trial (“A Randomized Trial of Induction Versus Expectant Management”), currently in the recruitment stage, will examine outcomes after induction at 39 weeks’ gestation, compared with expectant management in 6,000 patients (clinicaltrials.gov/ct2/show/NCT01990612).
Common wisdom informed by retrospective cohort studies has long told us that inducing labor prior to 41 weeks’ gestation is associated with a higher risk of cesarean delivery in nulliparous women. However, recent observational data have suggested that women whose labor is induced actually have fewer cesarean deliveries and better perinatal outcomes, including a lower risk of stillbirth (AJOG 2012;207:502.e1-8).
In addition, a meta-analysis published in 2014, as the ARRIVE trial was taking shape, reported a 12% reduction in cesarean delivery, and a reduced risk of stillbirth, among women whose labor was induced. The initial cervical score did not impact the main findings (CMAJ. 2014 Jun 10;186[9]:665-73). If these findings are confirmed in the ARRIVE trial, we could see a new opportunity for stillbirth prevention.
Another ongoing study of 10,000 singleton pregnancies – the Nulliparous Pregnancy Outcomes: Monitoring Mothers-to-Be (nuMoM2b) study – may also lead to prevention strategies in women for whom the current pregnancy will lead to their first delivery. Among the questions being examined in this eight-site study are whether sleep-disordered breathing, or apnea, and a supine sleep position are risk factors for adverse pregnancy outcomes including stillbirth.
Supine sleeping in the last month of pregnancy was strongly associated with stillbirth in a recent analysis from the Sydney Stillbirth Study (Obstet Gynecol. 2015 Feb;125[2]:347-55), and an early analysis of a nuMoM2b subset has shown associations between sleep-disordered breathing in midpregnancy and the development of hypertensive disorders of pregnancy, and between sleep-disordered breathing in early- and mid-pregnancy and gestational diabetes (Am J Obstet Gynecol. 2015;212:S424-425).
The possible role of low-dose aspirin in preventing stillbirth also needs more exploration. A recent randomized trial of women attempting to become pregnant after having had one or two prior pregnancy losses found no difference overall in live birth rates between those who took low-dose aspirin and those assigned to placebo. However, there was one subgroup – women with a single loss at less than 20 weeks’ gestation during the previous year – in which live birth rates were higher in the aspirin group (Lancet. 2014 Jul 5;384[9937]:29-36). More research is necessary to determine if low-dose aspirin administration in women with a previous stillbirth improves pregnancy outcome.
Dr. Reddy is a member at the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. She is a board-certified ob.gyn. and maternal-fetal medicine specialist. She is the program scientist for the Maternal-Fetal Medicine Units Network and for the Stillbirth Collaborative Research Network. The comments and views of the author do not necessarily represent the views of the NICHD.
Stillbirth is a major public health problem, occurring in approximately 1 of every 160 pregnancies in the United States. The rate has remained stagnant since 2006. Prior to that time, from 1990 to 2006, the rate declined somewhat, but only half as much as the decline in infant mortality during this time period. Racial disparities also have persisted, with non-Hispanic black women having more than a twofold increase in risk (Natl Vital Stat Rep. 2012;60:1-22).
Research conducted by the Stillbirth Collaborative Research Network (SCRN) and others has provided us with insight on risk factors and on probable and possible causes of death among stillbirths, which are defined as fetal deaths at 20 or more weeks’ gestation. We know from SCRN data, for instance, that black women are more likely to have stillbirths associated with obstetric complications and infections than white and Hispanic women. However, we still cannot explain a substantial proportion of stillbirths, despite a complete evaluation, or predict who will have a stillbirth.
What we can do as obstetricians is be aware that stillbirth is one of the most common adverse pregnancy outcomes in the United States and counsel women regarding risk factors that are modifiable. Moreover, when stillbirth happens, a complete postmortem evaluation that includes autopsy, placental pathology, karyotype or microarray analysis, and fetal-maternal hemorrhage testing is recommended (Obstet Gynecol. 2009;113[3]:748-61). Recent data show that each of these four components is valuable and should be considered the basic work-up for stillbirth.
Risks and causes
Pregnancy history was the strongest baseline risk factor for stillbirth in an analysis of 614 stillbirths and 1,816 live births in the SCRN’s population-based, case-control study conducted between 2006 and 2008. The SCRN was initiated by the Eunice Kennedy Shriver National Institute of Child Health and Human Development in 2003. This critical population-based study was conducted at 59 U.S. tertiary care and community hospitals in five catchment areas and has been analyzed in more than 15 published reports.
Women with a previous stillbirth have been known to be at 5- to 10-fold increased risk of a recurrence of stillbirth, and the SCRN findings confirmed this. The study added to our knowledge, however, with the finding that even a prior pregnancy loss at less than 20 weeks’ gestation increased the risk for stillbirth.
Other risk factors identified in the study, in addition to race, included having a multifetal pregnancy (adjusted odds ratio of 4.59), diabetes (AOR of 2.50), maternal age of 40 years or older (AOR of 2.41), maternal AB blood type (AOR of 1.96, compared with type O), a history of drug addiction (AOR of 2.08), smoking during the 3 months prior to pregnancy (AOR of 1.55-1.57, depending on amount), and being unmarried and not cohabitating (AOR of 1.69). Regarding racial disparity, the study showed that elevated risk of stillbirth for non-Hispanic blacks occurred predominantly prior to 24 weeks of gestation.
As in prior research, overweight and obesity also conferred elevated risks in the SCRN study (AORs of 1.43 and 1.72, respectively), and these risks were not explained by either diabetes or hypertension (JAMA. 2011;306:2469-79).
The use of assisted reproductive technology was not included in the study’s multivariate model, but previous research has shown a fourfold increased risk of stillbirth for singleton IVF/ICSI pregnancies. The reason is unclear, but the risk appears to be more related to IVF/ICSI rather than the underlying infertility (Hum Reprod. 2010 May;25[5]:1312-6).
A previous preterm or small-for-gestational-age birth has also been shown in prior research to be a significant risk factor for stillbirth. Less clear is the role of previous cesarean delivery in stillbirth risk. An association has been demonstrated in several studies, however, including one involving about 180,000 singleton pregnancies of 23 or more weeks’ gestation. Women in this cohort who had a previous cesarean delivery had a 1.3-fold increased risk of antepartum stillbirth, after controlling for important factors such as race, body mass index (BMI), and maternal disease (Obstet Gynecol. 2010 Nov;116[5]:1119-26).
In another analysis of the SCRN study looking specifically at causes of stillbirth, a “probable” cause of death was found in 61% of cases and a “possible or probable” cause of death in more than 76% of cases. The most common causes were obstetric complications (29.3%), placental abnormalities (23.6%), fetal genetic/structural abnormalities (13.7%), infection (12.9%), umbilical cord abnormalities (10.4%), hypertensive disorders (9.2%), and other maternal medical conditions (7.8%).
A higher proportion of stillbirths in non-Hispanic black women, compared with non-Hispanic white women and Hispanic women was associated with obstetric complications (43.5%) and infections (25.2%). This finding combined with the finding that stillbirth in black women often occurs at less than 24 weeks’ gestation suggests that measures aimed at reducing the rate of spontaneous preterm birth in black women could potentially reduce the rate of stillbirth as well (JAMA. 2011 Dec 14;306[22]:2459-68).
Work-up and prevention
Prevention of stillbirth requires that we identify the women at highest risk, and thus far this ability still eludes us. Apart from occurrence of previous stillbirth or pregnancy loss, other risk factors have had limited predictive value in the SCRN analyses and other research.
Biomarkers such as a low PAPP-A during the first trimester and a high AFP in the second trimester – as well as Doppler imaging of the uterine artery – have also been associated with stillbirth, but again, the positive predictive value has been shown to be low (Clin Obstet Gynecol. 2010 Sep;53[3]:597-606). More research is needed to determine if some combination of biochemical markers, imaging, and other risk factors can predict which women are at highest risk.
In the meantime, attention can be paid – in the preconception period if possible – to modifiable risk factors such as maternal obesity, diabetes, and smoking. About 10% of stillbirths are associated with maternal conditions such as hypertension and diabetes, and late stillbirths in particular (28 weeks or later) are associated with maternal medical conditions that are potentially preventable.
Normalization of prepregnancy weight should be a goal, since the overall risk of stillbirth appears to increase independently with increasing BMI. Glycemic control should also be achieved: A recent meta-analysis of preconception and prenatal care of diabetic women estimated “conservatively” that 10% of diabetes-associated stillbirths could be prevented with early detection and glycemic control (BMC Public Health. 2011;11 Suppl 3:S2). Research has also shown that women who quit smoking between their first and second pregnancy reduce their stillbirth risk to that of nonsmokers in the second pregnancy (BJOG. 2007 Jun;114[6]:699-704).
When stillbirth happens, a thorough work-up is recommended in order to counsel for future pregnancies and decrease the risk of recurrence. Evaluations for causes of stillbirth are too often incomplete in the United States for various reasons, including emotional, cultural, and resource factors. Even if a cause is not found, many families appreciate knowing that every effort has been made to determine a cause of death.
Four components of evaluation – autopsy, placental examination, karyotype or microarray analysis, and fetal-maternal hemorrhage testing – have proven to be high-yield tests when performed in all cases of stillbirth.
In the SCRN study, of 512 stillbirths undergoing a complete evaluation, 66.4% had a positive result – defined as abnormalities contributing to a probable or possible cause – for at least one of the first three tests (JAMA. 2011 Dec 14;306[22]:2459-68).
A Dutch study of 1,025 stillbirths similarly demonstrated that all four tests are justified. A test was defined as valuable in this study if it established or excluded a cause of stillbirth. Placental examination was determined to be the most valuable test, helping to determine a cause of death in 95.7% of cases. Autopsy was valuable 72.6% of the time, and cytogenetic analysis was valuable in 29% of cases.
Kleihauer-Betke testing for fetal-maternal hemorrhage was positive in 11.9% of women. However, fetal maternal hemorrhage was considered the cause of death in only 1.3%.of cases because, beyond a positive Kleihauer-Betke test, evidence of fetal anemia confirmed by placental examination and/or autopsy was required for hemorrhage to be considered the cause of death (Am. J. Obstet. Gynecol. 2012;206:53.e1-12). Because Kleihauer-Betke testing is ideally performed before induction, authors of both the SCRN study and the Dutch study believe it is a valuable test to be offered in all cases.
In both studies, the yield of other stillbirth diagnostic tests (for example, maternal serology, hormone assessment, and toxicology screen) was low, indicating that these tests are considered sequential and can be performed only when the clinical history or findings of the four core tests raise suspicion of particular potential causes. Antinuclear antibody testing and TORCH (toxoplasmosis, rubella, cytomegalovirus, herpes simplex) titers have an extremely low yield and are generally not useful.
For detecting genetic abnormalities after stillbirth, it appears that microarray analysis is superior to karyotype analysis. In a SCRN analysis of samples from 532 stillbirths, microarray yielded results more often and identified more genetic abnormalities. Unlike karyotype, it does not require live cells, which makes it preferable for stillbirth evaluation (N Engl J Med. 2012 Dec 6;367[23]:2185-93).
Current research
One of the more significant studies underway on prevention is looking at labor induction as an intervention for reducing stillbirths and improving other perinatal outcomes. The ARRIVE trial (“A Randomized Trial of Induction Versus Expectant Management”), currently in the recruitment stage, will examine outcomes after induction at 39 weeks’ gestation, compared with expectant management in 6,000 patients (clinicaltrials.gov/ct2/show/NCT01990612).
Common wisdom informed by retrospective cohort studies has long told us that inducing labor prior to 41 weeks’ gestation is associated with a higher risk of cesarean delivery in nulliparous women. However, recent observational data have suggested that women whose labor is induced actually have fewer cesarean deliveries and better perinatal outcomes, including a lower risk of stillbirth (AJOG 2012;207:502.e1-8).
In addition, a meta-analysis published in 2014, as the ARRIVE trial was taking shape, reported a 12% reduction in cesarean delivery, and a reduced risk of stillbirth, among women whose labor was induced. The initial cervical score did not impact the main findings (CMAJ. 2014 Jun 10;186[9]:665-73). If these findings are confirmed in the ARRIVE trial, we could see a new opportunity for stillbirth prevention.
Another ongoing study of 10,000 singleton pregnancies – the Nulliparous Pregnancy Outcomes: Monitoring Mothers-to-Be (nuMoM2b) study – may also lead to prevention strategies in women for whom the current pregnancy will lead to their first delivery. Among the questions being examined in this eight-site study are whether sleep-disordered breathing, or apnea, and a supine sleep position are risk factors for adverse pregnancy outcomes including stillbirth.
Supine sleeping in the last month of pregnancy was strongly associated with stillbirth in a recent analysis from the Sydney Stillbirth Study (Obstet Gynecol. 2015 Feb;125[2]:347-55), and an early analysis of a nuMoM2b subset has shown associations between sleep-disordered breathing in midpregnancy and the development of hypertensive disorders of pregnancy, and between sleep-disordered breathing in early- and mid-pregnancy and gestational diabetes (Am J Obstet Gynecol. 2015;212:S424-425).
The possible role of low-dose aspirin in preventing stillbirth also needs more exploration. A recent randomized trial of women attempting to become pregnant after having had one or two prior pregnancy losses found no difference overall in live birth rates between those who took low-dose aspirin and those assigned to placebo. However, there was one subgroup – women with a single loss at less than 20 weeks’ gestation during the previous year – in which live birth rates were higher in the aspirin group (Lancet. 2014 Jul 5;384[9937]:29-36). More research is necessary to determine if low-dose aspirin administration in women with a previous stillbirth improves pregnancy outcome.
Dr. Reddy is a member at the Pregnancy and Perinatology Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. She is a board-certified ob.gyn. and maternal-fetal medicine specialist. She is the program scientist for the Maternal-Fetal Medicine Units Network and for the Stillbirth Collaborative Research Network. The comments and views of the author do not necessarily represent the views of the NICHD.
Biologic treatment in pregnancy requires balancing risks
The effectiveness of immunoglobulin biologic treatments in controlling chronic and potentially debilitating autoimmune diseases such as rheumatoid arthritis and ulcerative colitis means that more physicians are faced with the question of how to handle the use of these drugs in pregnancy.
While immunoglobulin G (IgG) biologicals are large molecules, there is no doubt that they cross the placenta through specific transport systems with a long half life in infants, creating potential risks for immunocompromise in early life. At the same time, these biologicals are essential, in many cases, for controlling the pregnant woman’s disease and allowing her to carry a pregnancy successfully by avoiding disease flare.
For ob.gyns., successful management of a pregnancy in which the woman is taking an immunoglobulin biological, such as an anti–tumor necrosis factor (TNF)-alpha agent, requires an understanding of not only which drugs cross the placenta, but when they do so and at what levels.
Crossing the placenta
Along with my student Juejing Ling, I recently reviewed the question of how the use of immunoglobulin biologicals in pregnancy affects the vaccination of infants in an article published in Expert Review of Vaccines (2015 Dec 7:1-18 doi: 10.1586/14760584.2016.1115351). Our analysis relates only to biologicals with partial or full IgG structure, as they are capable of crossing the placenta.
Data are still limited about the use of immunoglobulin biologicals in pregnancy, but measurement of umbilical cord blood has shown high levels of anti-TNF IgG in newborn serum, raising concerns about how these neonates will respond to vaccinations.
Neonates rely on maternal IgG transport to prevent infection in the first few months of life and that transport process begins around 12 weeks gestation. Fetal IgG levels begin to rise at 13-18 weeks and reach 120%-130% of maternal levels when the fetus reaches full term. In contrast, fusion proteins that contain the Fc portion and Fab fragment appear to have limited ability to cross the placenta. As a result, chimeric and full human IgG antibodies such as infliximab, adalimumab, and rituximab have demonstrated high levels of placental transport, while other agents, such as etanercept, appear to cross the placenta at lower levels.
Hence, due to the ineffective clearance, certain immunoglobulin biologicals actually have a higher concentration and a longer half life in neonates than in mothers. For instance, with infliximab, studies show that levels in the umbilical cord were up to fourfold higher than maternal levels, even when the drug was discontinued at 30 weeks of pregnancy or earlier. Due to long neonatal half life, infliximab levels became undetectable in infant serum only between 2-7 months, compared with 1-2 weeks in adults. Adalimumab is similar, where concentrations of the drug in neonates can be 150% of the maternal serum level and detectable for about 3 months after birth.
Transport of anti-TNFs is also possible through breastfeeding, although studies indicate that the levels are very low.
Infection risk
Due to the immunosuppressive effect of anti-TNF immunoglobulin biologicals, newborn infection is a real concern. Review of the literature showed that severe and moderate neutropenia and skin infection were reported in four neonates born to two women with ulcerative colitis who had taken infliximab throughout pregnancy.
Some other studies have followed infants who had detectable biological levels at birth after in utero exposure. In general, there is normal development in the first year without overt infection. However, there have been case reports of infections with varicella or upper respiratory infections in infants exposed to infliximab before 30 weeks’ gestation.
There is very little data on the long-term immune system impacts for infants exposed to immunoglobulin biologicals in utero. However, these agents are generally not at detectable levels after 1 year.
Impact on vaccination
Although these IgG biologicals will clear the infants’ systems after several months of life (generally by 8 months), another concern is for how their presence in the early months impacts neonatal vaccination, specifically live attenuated vaccines such as MMR (measles, mumps and rubella), BCG for tuberculosis, oral polio, rotavirus vaccine, and the intranasal influenza vaccine.
Generally, outcomes among infants exposed to anti-TNFs have been good. For instance, reports looking at 24 children with exposure to anti-TNFs found no complications with the MMR vaccine. But a famous case report identified one infant who died at 4.5 months after receiving the BCG vaccine at 3 months. The mother, who had Crohn’s disease, had been taking infliximab 10 mg/kg every 8 weeks throughout her pregnancy.
Another study of 15 infants in the Czech Republic who were exposed to infliximab in utero and received BCG vaccination within 1 week of birth found that three of the infants developed large local skin reactions. One of the three children also developed axillary lymphadenopathy. All of the children recovered without the need for anti-tuberculosis therapy.
So what do these complications mean for vaccination strategies? Both the European Crohn’s and Colitis Organisation and the World Congress of Gastroenterology recommend that in terms of non-live vaccines, it’s safe to follow the same vaccine schedule as infants not exposed to biologicals in utero. When it comes to live attenuated vaccines such as rotavirus, oral polio, and BCG, these infants should be treated as immunocompromised and not receive these vaccines until after 6 months of age, when the biologicals should be at undetectable levels.
Future directions
Given that most infections and other adverse events happen after late exposure in pregnancy, some have recommended discontinuing anti-TNF treatment before the third trimester. In fact, this has become a common management practice. However, this should be an individualized decision made after discussion between a woman and her physician or physicians. Any benefits from early discontinuation of an immunoglobulin biological therapy should be weighed against the risk of disease flare, which also has real potential to complicate pregnancy.
The evidence presented here not only shines a light on the possible risk to infants, but also on the need for more high-quality evidence on which physicians can base decisions. Most of the available evidence is drawn from case reports and registry databases. Both of these suffer from a lack of control groups. To answer these questions definitively, we need more well-controlled studies of large populations. I strongly urge readers to follow the amazing work led by Dr. Uma Mahadevan and her colleagues at the University of California, San Francisco on biological use in pregnancy and long-term outcomes. As we wait for more evidence, we all look forward to the development of newer biologic agents that can help women control autoimmune disease without crossing the placenta.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He reported having no financial disclosures related to this article. Email him at [email protected].
The effectiveness of immunoglobulin biologic treatments in controlling chronic and potentially debilitating autoimmune diseases such as rheumatoid arthritis and ulcerative colitis means that more physicians are faced with the question of how to handle the use of these drugs in pregnancy.
While immunoglobulin G (IgG) biologicals are large molecules, there is no doubt that they cross the placenta through specific transport systems with a long half life in infants, creating potential risks for immunocompromise in early life. At the same time, these biologicals are essential, in many cases, for controlling the pregnant woman’s disease and allowing her to carry a pregnancy successfully by avoiding disease flare.
For ob.gyns., successful management of a pregnancy in which the woman is taking an immunoglobulin biological, such as an anti–tumor necrosis factor (TNF)-alpha agent, requires an understanding of not only which drugs cross the placenta, but when they do so and at what levels.
Crossing the placenta
Along with my student Juejing Ling, I recently reviewed the question of how the use of immunoglobulin biologicals in pregnancy affects the vaccination of infants in an article published in Expert Review of Vaccines (2015 Dec 7:1-18 doi: 10.1586/14760584.2016.1115351). Our analysis relates only to biologicals with partial or full IgG structure, as they are capable of crossing the placenta.
Data are still limited about the use of immunoglobulin biologicals in pregnancy, but measurement of umbilical cord blood has shown high levels of anti-TNF IgG in newborn serum, raising concerns about how these neonates will respond to vaccinations.
Neonates rely on maternal IgG transport to prevent infection in the first few months of life and that transport process begins around 12 weeks gestation. Fetal IgG levels begin to rise at 13-18 weeks and reach 120%-130% of maternal levels when the fetus reaches full term. In contrast, fusion proteins that contain the Fc portion and Fab fragment appear to have limited ability to cross the placenta. As a result, chimeric and full human IgG antibodies such as infliximab, adalimumab, and rituximab have demonstrated high levels of placental transport, while other agents, such as etanercept, appear to cross the placenta at lower levels.
Hence, due to the ineffective clearance, certain immunoglobulin biologicals actually have a higher concentration and a longer half life in neonates than in mothers. For instance, with infliximab, studies show that levels in the umbilical cord were up to fourfold higher than maternal levels, even when the drug was discontinued at 30 weeks of pregnancy or earlier. Due to long neonatal half life, infliximab levels became undetectable in infant serum only between 2-7 months, compared with 1-2 weeks in adults. Adalimumab is similar, where concentrations of the drug in neonates can be 150% of the maternal serum level and detectable for about 3 months after birth.
Transport of anti-TNFs is also possible through breastfeeding, although studies indicate that the levels are very low.
Infection risk
Due to the immunosuppressive effect of anti-TNF immunoglobulin biologicals, newborn infection is a real concern. Review of the literature showed that severe and moderate neutropenia and skin infection were reported in four neonates born to two women with ulcerative colitis who had taken infliximab throughout pregnancy.
Some other studies have followed infants who had detectable biological levels at birth after in utero exposure. In general, there is normal development in the first year without overt infection. However, there have been case reports of infections with varicella or upper respiratory infections in infants exposed to infliximab before 30 weeks’ gestation.
There is very little data on the long-term immune system impacts for infants exposed to immunoglobulin biologicals in utero. However, these agents are generally not at detectable levels after 1 year.
Impact on vaccination
Although these IgG biologicals will clear the infants’ systems after several months of life (generally by 8 months), another concern is for how their presence in the early months impacts neonatal vaccination, specifically live attenuated vaccines such as MMR (measles, mumps and rubella), BCG for tuberculosis, oral polio, rotavirus vaccine, and the intranasal influenza vaccine.
Generally, outcomes among infants exposed to anti-TNFs have been good. For instance, reports looking at 24 children with exposure to anti-TNFs found no complications with the MMR vaccine. But a famous case report identified one infant who died at 4.5 months after receiving the BCG vaccine at 3 months. The mother, who had Crohn’s disease, had been taking infliximab 10 mg/kg every 8 weeks throughout her pregnancy.
Another study of 15 infants in the Czech Republic who were exposed to infliximab in utero and received BCG vaccination within 1 week of birth found that three of the infants developed large local skin reactions. One of the three children also developed axillary lymphadenopathy. All of the children recovered without the need for anti-tuberculosis therapy.
So what do these complications mean for vaccination strategies? Both the European Crohn’s and Colitis Organisation and the World Congress of Gastroenterology recommend that in terms of non-live vaccines, it’s safe to follow the same vaccine schedule as infants not exposed to biologicals in utero. When it comes to live attenuated vaccines such as rotavirus, oral polio, and BCG, these infants should be treated as immunocompromised and not receive these vaccines until after 6 months of age, when the biologicals should be at undetectable levels.
Future directions
Given that most infections and other adverse events happen after late exposure in pregnancy, some have recommended discontinuing anti-TNF treatment before the third trimester. In fact, this has become a common management practice. However, this should be an individualized decision made after discussion between a woman and her physician or physicians. Any benefits from early discontinuation of an immunoglobulin biological therapy should be weighed against the risk of disease flare, which also has real potential to complicate pregnancy.
The evidence presented here not only shines a light on the possible risk to infants, but also on the need for more high-quality evidence on which physicians can base decisions. Most of the available evidence is drawn from case reports and registry databases. Both of these suffer from a lack of control groups. To answer these questions definitively, we need more well-controlled studies of large populations. I strongly urge readers to follow the amazing work led by Dr. Uma Mahadevan and her colleagues at the University of California, San Francisco on biological use in pregnancy and long-term outcomes. As we wait for more evidence, we all look forward to the development of newer biologic agents that can help women control autoimmune disease without crossing the placenta.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He reported having no financial disclosures related to this article. Email him at [email protected].
The effectiveness of immunoglobulin biologic treatments in controlling chronic and potentially debilitating autoimmune diseases such as rheumatoid arthritis and ulcerative colitis means that more physicians are faced with the question of how to handle the use of these drugs in pregnancy.
While immunoglobulin G (IgG) biologicals are large molecules, there is no doubt that they cross the placenta through specific transport systems with a long half life in infants, creating potential risks for immunocompromise in early life. At the same time, these biologicals are essential, in many cases, for controlling the pregnant woman’s disease and allowing her to carry a pregnancy successfully by avoiding disease flare.
For ob.gyns., successful management of a pregnancy in which the woman is taking an immunoglobulin biological, such as an anti–tumor necrosis factor (TNF)-alpha agent, requires an understanding of not only which drugs cross the placenta, but when they do so and at what levels.
Crossing the placenta
Along with my student Juejing Ling, I recently reviewed the question of how the use of immunoglobulin biologicals in pregnancy affects the vaccination of infants in an article published in Expert Review of Vaccines (2015 Dec 7:1-18 doi: 10.1586/14760584.2016.1115351). Our analysis relates only to biologicals with partial or full IgG structure, as they are capable of crossing the placenta.
Data are still limited about the use of immunoglobulin biologicals in pregnancy, but measurement of umbilical cord blood has shown high levels of anti-TNF IgG in newborn serum, raising concerns about how these neonates will respond to vaccinations.
Neonates rely on maternal IgG transport to prevent infection in the first few months of life and that transport process begins around 12 weeks gestation. Fetal IgG levels begin to rise at 13-18 weeks and reach 120%-130% of maternal levels when the fetus reaches full term. In contrast, fusion proteins that contain the Fc portion and Fab fragment appear to have limited ability to cross the placenta. As a result, chimeric and full human IgG antibodies such as infliximab, adalimumab, and rituximab have demonstrated high levels of placental transport, while other agents, such as etanercept, appear to cross the placenta at lower levels.
Hence, due to the ineffective clearance, certain immunoglobulin biologicals actually have a higher concentration and a longer half life in neonates than in mothers. For instance, with infliximab, studies show that levels in the umbilical cord were up to fourfold higher than maternal levels, even when the drug was discontinued at 30 weeks of pregnancy or earlier. Due to long neonatal half life, infliximab levels became undetectable in infant serum only between 2-7 months, compared with 1-2 weeks in adults. Adalimumab is similar, where concentrations of the drug in neonates can be 150% of the maternal serum level and detectable for about 3 months after birth.
Transport of anti-TNFs is also possible through breastfeeding, although studies indicate that the levels are very low.
Infection risk
Due to the immunosuppressive effect of anti-TNF immunoglobulin biologicals, newborn infection is a real concern. Review of the literature showed that severe and moderate neutropenia and skin infection were reported in four neonates born to two women with ulcerative colitis who had taken infliximab throughout pregnancy.
Some other studies have followed infants who had detectable biological levels at birth after in utero exposure. In general, there is normal development in the first year without overt infection. However, there have been case reports of infections with varicella or upper respiratory infections in infants exposed to infliximab before 30 weeks’ gestation.
There is very little data on the long-term immune system impacts for infants exposed to immunoglobulin biologicals in utero. However, these agents are generally not at detectable levels after 1 year.
Impact on vaccination
Although these IgG biologicals will clear the infants’ systems after several months of life (generally by 8 months), another concern is for how their presence in the early months impacts neonatal vaccination, specifically live attenuated vaccines such as MMR (measles, mumps and rubella), BCG for tuberculosis, oral polio, rotavirus vaccine, and the intranasal influenza vaccine.
Generally, outcomes among infants exposed to anti-TNFs have been good. For instance, reports looking at 24 children with exposure to anti-TNFs found no complications with the MMR vaccine. But a famous case report identified one infant who died at 4.5 months after receiving the BCG vaccine at 3 months. The mother, who had Crohn’s disease, had been taking infliximab 10 mg/kg every 8 weeks throughout her pregnancy.
Another study of 15 infants in the Czech Republic who were exposed to infliximab in utero and received BCG vaccination within 1 week of birth found that three of the infants developed large local skin reactions. One of the three children also developed axillary lymphadenopathy. All of the children recovered without the need for anti-tuberculosis therapy.
So what do these complications mean for vaccination strategies? Both the European Crohn’s and Colitis Organisation and the World Congress of Gastroenterology recommend that in terms of non-live vaccines, it’s safe to follow the same vaccine schedule as infants not exposed to biologicals in utero. When it comes to live attenuated vaccines such as rotavirus, oral polio, and BCG, these infants should be treated as immunocompromised and not receive these vaccines until after 6 months of age, when the biologicals should be at undetectable levels.
Future directions
Given that most infections and other adverse events happen after late exposure in pregnancy, some have recommended discontinuing anti-TNF treatment before the third trimester. In fact, this has become a common management practice. However, this should be an individualized decision made after discussion between a woman and her physician or physicians. Any benefits from early discontinuation of an immunoglobulin biological therapy should be weighed against the risk of disease flare, which also has real potential to complicate pregnancy.
The evidence presented here not only shines a light on the possible risk to infants, but also on the need for more high-quality evidence on which physicians can base decisions. Most of the available evidence is drawn from case reports and registry databases. Both of these suffer from a lack of control groups. To answer these questions definitively, we need more well-controlled studies of large populations. I strongly urge readers to follow the amazing work led by Dr. Uma Mahadevan and her colleagues at the University of California, San Francisco on biological use in pregnancy and long-term outcomes. As we wait for more evidence, we all look forward to the development of newer biologic agents that can help women control autoimmune disease without crossing the placenta.
Dr. Koren is professor of pharmacology and pharmacy at the University of Toronto. He is the founding director of the Motherisk Program. He reported having no financial disclosures related to this article. Email him at [email protected].
CDC: Ask Pregnant Women About Zika Virus Exposure
The Centers for Disease Control and Prevention has released interim guidelines for the care of pregnant women during a Zika virus outbreak.
The guidelines, developed in consultation with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, come on the heels of a Jan. 15 advisory warning pregnant women to avoid traveling to tropical countries and territories with outbreaks of the mosquito-borne virus. The virus is typically associated with only mild symptoms, but has been linked with cases of microcephaly and other poor outcomes in pregnancy.
“Health care providers should ask all pregnant women about recent travel. Pregnant women with a history of travel to an area with Zika virus transmission who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department,” according to the guidelines, which were published Jan. 19 in an early release of the Morbidity and Mortality Weekly Report (MMWR. 2016 Jan 19;65[Early Release]:1-4).
Testing is not indicated for women who have not traveled to areas with Zika virus transmission, according to CDC.
For women who test positive for the virus, serial ultrasounds to monitor fetal growth and anatomy should be considered, as well as referral to a maternal-fetal medicine specialist or infectious disease specialist with expertise in pregnancy management, according to the guidelines.
While a positive reverse-transcription polymerase chain reaction (RT-PCR) result on amniotic fluid would suggest intrauterine infection and could potentially be useful to pregnant women and their health care providers, it is currently not known how sensitive or specific the test is for congenital infection or whether a positive result is predictive of a subsequent fetal abnormality.
“Health care providers should discuss the risks and benefits of amniocentesis with their patients,” CDC officials wrote in the interim guidance.
The following tests are advised for live births with evidence of infection: histopathological examination of the placenta and umbilical cord, testing of frozen placental tissue and cord tissue for Zika virus RNA, and testing of cord serum for Zika and dengue virus IgM and neutralizing antibodies. Guidelines for infected infants are currently being developed.
No specific treatment exists for Zika virus infection; supportive care, including rest, fluids, use of analgesics and antipyretics, and acetaminophen for fever is advised.
The CDC continues to recommend that pregnant women avoid travel to areas where Zika virus transmission is ongoing. Strict steps to avoid mosquito bites are advised for those who do travel to such areas. This includes use of protective clothing and U.S. Environmental Protection Agency–registered insect repellents, as well as staying and sleeping in screened-in or air-conditioned rooms. Insect repellents containing DEET, picaridin, and IR3535 are safe for pregnant women when used as directed on the label, according to the CDC.
Updates on areas with ongoing Zika virus transmission are available on the CDC website.
The Centers for Disease Control and Prevention has released interim guidelines for the care of pregnant women during a Zika virus outbreak.
The guidelines, developed in consultation with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, come on the heels of a Jan. 15 advisory warning pregnant women to avoid traveling to tropical countries and territories with outbreaks of the mosquito-borne virus. The virus is typically associated with only mild symptoms, but has been linked with cases of microcephaly and other poor outcomes in pregnancy.
“Health care providers should ask all pregnant women about recent travel. Pregnant women with a history of travel to an area with Zika virus transmission who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department,” according to the guidelines, which were published Jan. 19 in an early release of the Morbidity and Mortality Weekly Report (MMWR. 2016 Jan 19;65[Early Release]:1-4).
Testing is not indicated for women who have not traveled to areas with Zika virus transmission, according to CDC.
For women who test positive for the virus, serial ultrasounds to monitor fetal growth and anatomy should be considered, as well as referral to a maternal-fetal medicine specialist or infectious disease specialist with expertise in pregnancy management, according to the guidelines.
While a positive reverse-transcription polymerase chain reaction (RT-PCR) result on amniotic fluid would suggest intrauterine infection and could potentially be useful to pregnant women and their health care providers, it is currently not known how sensitive or specific the test is for congenital infection or whether a positive result is predictive of a subsequent fetal abnormality.
“Health care providers should discuss the risks and benefits of amniocentesis with their patients,” CDC officials wrote in the interim guidance.
The following tests are advised for live births with evidence of infection: histopathological examination of the placenta and umbilical cord, testing of frozen placental tissue and cord tissue for Zika virus RNA, and testing of cord serum for Zika and dengue virus IgM and neutralizing antibodies. Guidelines for infected infants are currently being developed.
No specific treatment exists for Zika virus infection; supportive care, including rest, fluids, use of analgesics and antipyretics, and acetaminophen for fever is advised.
The CDC continues to recommend that pregnant women avoid travel to areas where Zika virus transmission is ongoing. Strict steps to avoid mosquito bites are advised for those who do travel to such areas. This includes use of protective clothing and U.S. Environmental Protection Agency–registered insect repellents, as well as staying and sleeping in screened-in or air-conditioned rooms. Insect repellents containing DEET, picaridin, and IR3535 are safe for pregnant women when used as directed on the label, according to the CDC.
Updates on areas with ongoing Zika virus transmission are available on the CDC website.
The Centers for Disease Control and Prevention has released interim guidelines for the care of pregnant women during a Zika virus outbreak.
The guidelines, developed in consultation with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, come on the heels of a Jan. 15 advisory warning pregnant women to avoid traveling to tropical countries and territories with outbreaks of the mosquito-borne virus. The virus is typically associated with only mild symptoms, but has been linked with cases of microcephaly and other poor outcomes in pregnancy.
“Health care providers should ask all pregnant women about recent travel. Pregnant women with a history of travel to an area with Zika virus transmission who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department,” according to the guidelines, which were published Jan. 19 in an early release of the Morbidity and Mortality Weekly Report (MMWR. 2016 Jan 19;65[Early Release]:1-4).
Testing is not indicated for women who have not traveled to areas with Zika virus transmission, according to CDC.
For women who test positive for the virus, serial ultrasounds to monitor fetal growth and anatomy should be considered, as well as referral to a maternal-fetal medicine specialist or infectious disease specialist with expertise in pregnancy management, according to the guidelines.
While a positive reverse-transcription polymerase chain reaction (RT-PCR) result on amniotic fluid would suggest intrauterine infection and could potentially be useful to pregnant women and their health care providers, it is currently not known how sensitive or specific the test is for congenital infection or whether a positive result is predictive of a subsequent fetal abnormality.
“Health care providers should discuss the risks and benefits of amniocentesis with their patients,” CDC officials wrote in the interim guidance.
The following tests are advised for live births with evidence of infection: histopathological examination of the placenta and umbilical cord, testing of frozen placental tissue and cord tissue for Zika virus RNA, and testing of cord serum for Zika and dengue virus IgM and neutralizing antibodies. Guidelines for infected infants are currently being developed.
No specific treatment exists for Zika virus infection; supportive care, including rest, fluids, use of analgesics and antipyretics, and acetaminophen for fever is advised.
The CDC continues to recommend that pregnant women avoid travel to areas where Zika virus transmission is ongoing. Strict steps to avoid mosquito bites are advised for those who do travel to such areas. This includes use of protective clothing and U.S. Environmental Protection Agency–registered insect repellents, as well as staying and sleeping in screened-in or air-conditioned rooms. Insect repellents containing DEET, picaridin, and IR3535 are safe for pregnant women when used as directed on the label, according to the CDC.
Updates on areas with ongoing Zika virus transmission are available on the CDC website.
FROM MMWR
CDC: Ask pregnant women about Zika virus exposure
The Centers for Disease Control and Prevention has released interim guidelines for the care of pregnant women during a Zika virus outbreak.
The guidelines, developed in consultation with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, come on the heels of a Jan. 15 advisory warning pregnant women to avoid traveling to tropical countries and territories with outbreaks of the mosquito-borne virus. The virus is typically associated with only mild symptoms, but has been linked with cases of microcephaly and other poor outcomes in pregnancy.
“Health care providers should ask all pregnant women about recent travel. Pregnant women with a history of travel to an area with Zika virus transmission who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department,” according to the guidelines, which were published Jan. 19 in an early release of the Morbidity and Mortality Weekly Report (MMWR. 2016 Jan 19;65[Early Release]:1-4).
Testing is not indicated for women who have not traveled to areas with Zika virus transmission, according to CDC.
For women who test positive for the virus, serial ultrasounds to monitor fetal growth and anatomy should be considered, as well as referral to a maternal-fetal medicine specialist or infectious disease specialist with expertise in pregnancy management, according to the guidelines.
While a positive reverse-transcription polymerase chain reaction (RT-PCR) result on amniotic fluid would suggest intrauterine infection and could potentially be useful to pregnant women and their health care providers, it is currently not known how sensitive or specific the test is for congenital infection or whether a positive result is predictive of a subsequent fetal abnormality.
“Health care providers should discuss the risks and benefits of amniocentesis with their patients,” CDC officials wrote in the interim guidance.
The following tests are advised for live births with evidence of infection: histopathological examination of the placenta and umbilical cord, testing of frozen placental tissue and cord tissue for Zika virus RNA, and testing of cord serum for Zika and dengue virus IgM and neutralizing antibodies. Guidelines for infected infants are currently being developed.
No specific treatment exists for Zika virus infection; supportive care, including rest, fluids, use of analgesics and antipyretics, and acetaminophen for fever is advised.
The CDC continues to recommend that pregnant women avoid travel to areas where Zika virus transmission is ongoing. Strict steps to avoid mosquito bites are advised for those who do travel to such areas. This includes use of protective clothing and U.S. Environmental Protection Agency–registered insect repellents, as well as staying and sleeping in screened-in or air-conditioned rooms. Insect repellents containing DEET, picaridin, and IR3535 are safe for pregnant women when used as directed on the label, according to the CDC.
Updates on areas with ongoing Zika virus transmission are available on the CDC website.
The Centers for Disease Control and Prevention has released interim guidelines for the care of pregnant women during a Zika virus outbreak.
The guidelines, developed in consultation with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, come on the heels of a Jan. 15 advisory warning pregnant women to avoid traveling to tropical countries and territories with outbreaks of the mosquito-borne virus. The virus is typically associated with only mild symptoms, but has been linked with cases of microcephaly and other poor outcomes in pregnancy.
“Health care providers should ask all pregnant women about recent travel. Pregnant women with a history of travel to an area with Zika virus transmission who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department,” according to the guidelines, which were published Jan. 19 in an early release of the Morbidity and Mortality Weekly Report (MMWR. 2016 Jan 19;65[Early Release]:1-4).
Testing is not indicated for women who have not traveled to areas with Zika virus transmission, according to CDC.
For women who test positive for the virus, serial ultrasounds to monitor fetal growth and anatomy should be considered, as well as referral to a maternal-fetal medicine specialist or infectious disease specialist with expertise in pregnancy management, according to the guidelines.
While a positive reverse-transcription polymerase chain reaction (RT-PCR) result on amniotic fluid would suggest intrauterine infection and could potentially be useful to pregnant women and their health care providers, it is currently not known how sensitive or specific the test is for congenital infection or whether a positive result is predictive of a subsequent fetal abnormality.
“Health care providers should discuss the risks and benefits of amniocentesis with their patients,” CDC officials wrote in the interim guidance.
The following tests are advised for live births with evidence of infection: histopathological examination of the placenta and umbilical cord, testing of frozen placental tissue and cord tissue for Zika virus RNA, and testing of cord serum for Zika and dengue virus IgM and neutralizing antibodies. Guidelines for infected infants are currently being developed.
No specific treatment exists for Zika virus infection; supportive care, including rest, fluids, use of analgesics and antipyretics, and acetaminophen for fever is advised.
The CDC continues to recommend that pregnant women avoid travel to areas where Zika virus transmission is ongoing. Strict steps to avoid mosquito bites are advised for those who do travel to such areas. This includes use of protective clothing and U.S. Environmental Protection Agency–registered insect repellents, as well as staying and sleeping in screened-in or air-conditioned rooms. Insect repellents containing DEET, picaridin, and IR3535 are safe for pregnant women when used as directed on the label, according to the CDC.
Updates on areas with ongoing Zika virus transmission are available on the CDC website.
The Centers for Disease Control and Prevention has released interim guidelines for the care of pregnant women during a Zika virus outbreak.
The guidelines, developed in consultation with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, come on the heels of a Jan. 15 advisory warning pregnant women to avoid traveling to tropical countries and territories with outbreaks of the mosquito-borne virus. The virus is typically associated with only mild symptoms, but has been linked with cases of microcephaly and other poor outcomes in pregnancy.
“Health care providers should ask all pregnant women about recent travel. Pregnant women with a history of travel to an area with Zika virus transmission who report two or more symptoms consistent with Zika virus disease (acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis) during or within 2 weeks of travel, or who have ultrasound findings of fetal microcephaly or intracranial calcifications, should be tested for Zika virus infection in consultation with their state or local health department,” according to the guidelines, which were published Jan. 19 in an early release of the Morbidity and Mortality Weekly Report (MMWR. 2016 Jan 19;65[Early Release]:1-4).
Testing is not indicated for women who have not traveled to areas with Zika virus transmission, according to CDC.
For women who test positive for the virus, serial ultrasounds to monitor fetal growth and anatomy should be considered, as well as referral to a maternal-fetal medicine specialist or infectious disease specialist with expertise in pregnancy management, according to the guidelines.
While a positive reverse-transcription polymerase chain reaction (RT-PCR) result on amniotic fluid would suggest intrauterine infection and could potentially be useful to pregnant women and their health care providers, it is currently not known how sensitive or specific the test is for congenital infection or whether a positive result is predictive of a subsequent fetal abnormality.
“Health care providers should discuss the risks and benefits of amniocentesis with their patients,” CDC officials wrote in the interim guidance.
The following tests are advised for live births with evidence of infection: histopathological examination of the placenta and umbilical cord, testing of frozen placental tissue and cord tissue for Zika virus RNA, and testing of cord serum for Zika and dengue virus IgM and neutralizing antibodies. Guidelines for infected infants are currently being developed.
No specific treatment exists for Zika virus infection; supportive care, including rest, fluids, use of analgesics and antipyretics, and acetaminophen for fever is advised.
The CDC continues to recommend that pregnant women avoid travel to areas where Zika virus transmission is ongoing. Strict steps to avoid mosquito bites are advised for those who do travel to such areas. This includes use of protective clothing and U.S. Environmental Protection Agency–registered insect repellents, as well as staying and sleeping in screened-in or air-conditioned rooms. Insect repellents containing DEET, picaridin, and IR3535 are safe for pregnant women when used as directed on the label, according to the CDC.
Updates on areas with ongoing Zika virus transmission are available on the CDC website.
FROM MMWR