User login
Understanding the cervicovaginal microbiome and how it affects preterm birth
Prematurity remains the leading cause of neonatal morbidity and mortality, accounting for $26 billion a year in immediate costs, despite the implementation in obstetrics of a host of risk stratification algorithms and strategies for risk reduction, including the use of some medications.
It now is questionable whether injectable 17-alpha hydroxyprogesterone caproate (Makena) truly is efficacious in women who’ve had a prior spontaneous preterm birth (sPTB) – a Food and Drug Administration advisory committee last year recommended withdrawing it from the market based on results of an FDA confirmatory study. Even if the drug were efficacious, only a small percentage of the women who have an sPTB have had a prior one. The majority of sPTB occurs among women without such a history.
Vaginal progesterone appears to confer some protection in women found to have a short cervix during the second trimester, but this approach also has limited reach: Only 9% of women with sPTB had an antecedent short cervix in a 2017 study.1 Like a history of sPTB, screening for short cervical length is a potentially helpful strategy for risk reduction, but it is not a strategy that will significantly impact the overall rate of prematurity.
We’ve fallen short in our goals to significantly reduce the public health impact of prematurity partly because we still do not understand the exact pathways and mechanisms by which sPTB occurs. The main working paradigm for myself and many other researchers over the past 2 decades has centered on infection in the uterus triggering inflammation, followed by cervical remodeling and ripening. Research in animal models, as well as human clinical trials targeting various infections and inflammation, have led to some insights and discoveries, but no successful interventions.
In the past decade, however, our research framework for understanding sPTB incorporates new questions about immunologic, microbiological, and molecular/cellular events that happen in the cervicovaginal space. We’ve learned more about the cervicovaginal microbiota, and most recently, our research at the University of Pennsylvania has elucidated the role that nonoptimal bacteria play in disrupting the cervical endothelial barrier and initiating the process of cervical remodeling that likely precedes sPTB.
We also know that this association is stronger in black women and may help explain some of the observed racial disparities in sPTB. Although more research is needed to determine specific therapeutic strategies, new doors are open.
Host immune-microbial interactions
This new research paradigm has involved stepping back and asking basic questions, such as, what do we really know about the cervicovaginal space? In actuality, we know very little. We know little about the immune function of the vaginal and cervical epithelial cells in pregnancy, for instance, and there is a large gap in knowledge regarding the biomechanics of the cervix – a remarkable organ that can change shape and function in a matter of minutes. Studies on the biomechanics of the cervix during pregnancy and in labor are still in their infancy.
However, lessons can be drawn from research on inflammatory bowel disease and other disorders involving the gut. In the gastrointestinal tract, epithelial cells have been found to act as sentinels, forming a mucosal barrier against bacterial pathogens and secreting various immune factors. Research in this field also has shown that microbes living in the gut produce metabolites; that these microbial metabolites may be the key messengers from the microbial communities to the epithelial barrier; and that the microbes, microbial metabolites, and immune responses are responsible for triggering inflammatory processes in the tissues underneath.
In 2011, Jacques Ravel, PhD, who was part of the National Institutes of Health’s Human Microbiome Project, characterized the vaginal microbiome of reproductive-age women for the first time.2 His paper classified the vaginal microbial communities of approximately 400 asymptomatic women of various ethnicities into five “community state types” (CSTs) based on the predominant bacteria found in the cervicovaginal space.3
On the heels of his research, Dr. Ravel and I launched an NIH-funded study involving a prospective cohort of 2,000 women with singleton pregnancies – the Motherhood & Microbiome cohort – to look at the cervicovaginal microbiota, the local immune response, and the risk of sPTB.4 Cervicovaginal samples were collected at 16-20 weeks’ gestation and during two subsequent clinical visits. From this cohort, which was composed mostly of African American women (74.5%), we conducted a nested case-controlled study of 103 cases of sPTB and 432 women who delivered at term, matched for race.
We carefully adjudicated the deliveries in our 2,000-person cohort so that we homed in on sPTB as opposed to preterm births that are medically indicated for reasons such as fetal distress or preeclampsia. (Several prior studies looking at the associations between the cervicovaginal microbiome had a heterogeneous phenotyping of PTB that made it hard to draw definitive conclusions.)
Our focus in assessing the microbiome and immunologic profiles was on the samples collected at the earliest time points in pregnancy because we hoped to detect a “signature” that could predict an outcome months later. Indeed, we found that the nonoptimal microbiota, known in microbiological terms as CST IV, was associated with about a 150% increased risk of sPTB. This community comprises a dominant array of anaerobic bacteria and a paucity of Lactobacillus species.
We also found that a larger proportion of African American women, compared with non–African American women, had this nonoptimal microbiota early in pregnancy (40% vs. 15%), which is consistent with previous studies in pregnancy and nonpregnancy showing lower levels of Lactobacillus species in the cervicovaginal microbiome of African American women.
Even more interesting was the finding that, although the rate of sPTB was higher in African American women and the effect of CST IV on sPTB was stronger in these women, the risk of sPTB couldn’t be explained solely by the presence of CST IV. Some women with this nonoptimal microbiome delivered at term, whereas others with more optimal microbiome types had sPTBs. This suggests that other factors contribute to African American women having a nonoptimal microbiota and being especially predisposed to sPTB.
Through the study’s immunologic profiling, we found a significant difference in the cervicovaginal levels of an immune factor, beta-defensin 2, between African American women who delivered at term and those who had a sPTB. Women who had a sPTB, even those who had higher levels of Lactobacillus species, had lower levels of beta-defensin 2. This association was not found in non–African American women.
Beta-defensin 2 is a host-derived antimicrobial peptide that, like other antimicrobial peptides, works at epithelial-mucosal barriers to combat bacteria; we have knowledge of its action from research on the gut, as well as some studies of the vaginal space in nonpregnant women that have focused on sexually transmitted infections.
Most exciting for us was the finding that higher levels of beta-defensin 2 appeared to lower the risk of sPTB in women who had a nonoptimal cervicovaginal microbiota. There’s an interplay between the host and the microbiota, in other words, and it’s one that could be essential to manipulate as we seek to reduce sPTB.
The cervical epithelial barrier
In the laboratory, meanwhile, we are learning how certain microbes are mechanistically involved in the pathogenesis of sPTB. Research over the last decade has suggested that disruption or breakdown of the cervical epithelial barrier drives cervical remodeling processes that precede sPTB. The question now is, do cervicovaginal bacteria associated with sPTB, or a nonoptimal cervicovaginal microbiota, cause disruption of the vaginal and cervical epithelial barrier – and how?
Using an in vitro model system, we found that Mobiluncus curtisii/mulieris, the bacterial taxa with the strongest association with sPTB in our Motherhood & Microbiome cohort and one that has long been associated with bacterial vaginosis, had a plethora of effects. It increased cell permeability and the expression of inflammatory mediators associated with cervical epithelial breakdown, and it altered expression of microRNAs that have been associated with sPTB in human studies.
Our study on Mobiluncus has served as proof of concept to us that, not only is the bacteria associated with sPTB, but that there are multiple mechanisms by which it can disrupt the cervicovaginal barrier and lead to cervical remodeling.5
The findings echo previous in vitro research on Gardnerella vaginalis, another anaerobic bacterium that has been associated with bacterial vaginosis and adverse obstetric outcomes, including sPTB.6 Using similar models, we found that G. vaginalis disrupts the cervical epithelial barrier through diverse mechanisms including the cleavage of certain proteins, the up-regulation of proinflammatory immune mediators, and altered gene expression.
Lactobacillus crispatus, on the other hand, conferred protection to the cervical epithelial barrier in this study by mitigating various G. vaginalis–induced effects.
Learning more about host-microbe interactions and the role of microbial metabolites in these interactions, as well as the role of altered gene expression in cervical function, will help us to more fully understand the biological mechanisms regulating cervicovaginal epithelial cells. At this point, we know that, as in the gut, bacteria commonly found in the cervicovaginal space play a significant role in regulating the function of epithelial cells (in both optimal and nonoptimal microbiota), and that various bacteria associated with sPTB contribute to poor outcomes by breaking down the cervical epithelium.
Therapeutic implications
Our growing knowledge of the cervicovaginal microbiota does not yet support screening or any particular interventions. We don’t know, for instance, that administering probiotics or prebiotics orally or vaginally will have any effect on rates of sPTB.
Ongoing research at all levels holds promise, however, for the development of diagnostics to identify women at risk for sPTB, and for the development of therapeutic strategies that aim to modify the microbiome and/or modify the immune response. We know from other areas of medicine that there are realistic ways to modulate the immune response and/or microbiota in a system to alter risk.
We need to more thoroughly understand the risk of particular microbiota and immune response factors – and how they vary by race and ethnicity – and we need to study the cervicovaginal microbiota of women before and during pregnancy to learn whether there is something about pregnancy or even about intercourse that can change one’s microbiome to a less favorable state.
It may well be possible in the near future to identify high-risk states of nonoptimal microbiota before conception – microbiota that, in and of themselves, may not be pathogenic but that become detrimental during pregnancy – and it should be possible to screen women early in pregnancy for microbial or immune signatures or both.
The question often arises in medicine of the validity of screening without having achieved certainty about treatments. However, in obstetrics, where we have different levels of care and the ability to personalize monitoring and care, identifying those at greatest risk still has value. Ultimately, with enough investment in all levels of research (basic, translational, and clinical), we can develop interventions and therapeutics that address a biologically plausible mechanism of sPTB and, as a result, achieve significant reductions in the rate of prematurity.
Dr. Elovitz is the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health, vice chair of translational research, and director of the Maternal and Child Health Research Center, department of obstetrics and gynecology, at the University of Pennsylvania, Philadelphia. She disclosed holding a patent on a method to determine risk of preterm birth that relates to the microbiome. Email her at [email protected].
References
1. JAMA. 2017 Mar 14;317(10):1047-56.
2. NIH Human Microbiome Project. https://hmpdacc.org/.
3. PNAS. 2011 Mar 15;108 (Supplement 1):4680-7.
4. Nat Commun. 2019 Mar 21. doi: 10.1038/s41467-019-09285-9.
5. Anaerobe. 2019 Nov 21. doi: 10.1016/j.anaerobe.2019.102127.
6. Front Microbiol. 2018 Oct 8. doi: 10.3389/fmicb.2018.02181.
Prematurity remains the leading cause of neonatal morbidity and mortality, accounting for $26 billion a year in immediate costs, despite the implementation in obstetrics of a host of risk stratification algorithms and strategies for risk reduction, including the use of some medications.
It now is questionable whether injectable 17-alpha hydroxyprogesterone caproate (Makena) truly is efficacious in women who’ve had a prior spontaneous preterm birth (sPTB) – a Food and Drug Administration advisory committee last year recommended withdrawing it from the market based on results of an FDA confirmatory study. Even if the drug were efficacious, only a small percentage of the women who have an sPTB have had a prior one. The majority of sPTB occurs among women without such a history.
Vaginal progesterone appears to confer some protection in women found to have a short cervix during the second trimester, but this approach also has limited reach: Only 9% of women with sPTB had an antecedent short cervix in a 2017 study.1 Like a history of sPTB, screening for short cervical length is a potentially helpful strategy for risk reduction, but it is not a strategy that will significantly impact the overall rate of prematurity.
We’ve fallen short in our goals to significantly reduce the public health impact of prematurity partly because we still do not understand the exact pathways and mechanisms by which sPTB occurs. The main working paradigm for myself and many other researchers over the past 2 decades has centered on infection in the uterus triggering inflammation, followed by cervical remodeling and ripening. Research in animal models, as well as human clinical trials targeting various infections and inflammation, have led to some insights and discoveries, but no successful interventions.
In the past decade, however, our research framework for understanding sPTB incorporates new questions about immunologic, microbiological, and molecular/cellular events that happen in the cervicovaginal space. We’ve learned more about the cervicovaginal microbiota, and most recently, our research at the University of Pennsylvania has elucidated the role that nonoptimal bacteria play in disrupting the cervical endothelial barrier and initiating the process of cervical remodeling that likely precedes sPTB.
We also know that this association is stronger in black women and may help explain some of the observed racial disparities in sPTB. Although more research is needed to determine specific therapeutic strategies, new doors are open.
Host immune-microbial interactions
This new research paradigm has involved stepping back and asking basic questions, such as, what do we really know about the cervicovaginal space? In actuality, we know very little. We know little about the immune function of the vaginal and cervical epithelial cells in pregnancy, for instance, and there is a large gap in knowledge regarding the biomechanics of the cervix – a remarkable organ that can change shape and function in a matter of minutes. Studies on the biomechanics of the cervix during pregnancy and in labor are still in their infancy.
However, lessons can be drawn from research on inflammatory bowel disease and other disorders involving the gut. In the gastrointestinal tract, epithelial cells have been found to act as sentinels, forming a mucosal barrier against bacterial pathogens and secreting various immune factors. Research in this field also has shown that microbes living in the gut produce metabolites; that these microbial metabolites may be the key messengers from the microbial communities to the epithelial barrier; and that the microbes, microbial metabolites, and immune responses are responsible for triggering inflammatory processes in the tissues underneath.
In 2011, Jacques Ravel, PhD, who was part of the National Institutes of Health’s Human Microbiome Project, characterized the vaginal microbiome of reproductive-age women for the first time.2 His paper classified the vaginal microbial communities of approximately 400 asymptomatic women of various ethnicities into five “community state types” (CSTs) based on the predominant bacteria found in the cervicovaginal space.3
On the heels of his research, Dr. Ravel and I launched an NIH-funded study involving a prospective cohort of 2,000 women with singleton pregnancies – the Motherhood & Microbiome cohort – to look at the cervicovaginal microbiota, the local immune response, and the risk of sPTB.4 Cervicovaginal samples were collected at 16-20 weeks’ gestation and during two subsequent clinical visits. From this cohort, which was composed mostly of African American women (74.5%), we conducted a nested case-controlled study of 103 cases of sPTB and 432 women who delivered at term, matched for race.
We carefully adjudicated the deliveries in our 2,000-person cohort so that we homed in on sPTB as opposed to preterm births that are medically indicated for reasons such as fetal distress or preeclampsia. (Several prior studies looking at the associations between the cervicovaginal microbiome had a heterogeneous phenotyping of PTB that made it hard to draw definitive conclusions.)
Our focus in assessing the microbiome and immunologic profiles was on the samples collected at the earliest time points in pregnancy because we hoped to detect a “signature” that could predict an outcome months later. Indeed, we found that the nonoptimal microbiota, known in microbiological terms as CST IV, was associated with about a 150% increased risk of sPTB. This community comprises a dominant array of anaerobic bacteria and a paucity of Lactobacillus species.
We also found that a larger proportion of African American women, compared with non–African American women, had this nonoptimal microbiota early in pregnancy (40% vs. 15%), which is consistent with previous studies in pregnancy and nonpregnancy showing lower levels of Lactobacillus species in the cervicovaginal microbiome of African American women.
Even more interesting was the finding that, although the rate of sPTB was higher in African American women and the effect of CST IV on sPTB was stronger in these women, the risk of sPTB couldn’t be explained solely by the presence of CST IV. Some women with this nonoptimal microbiome delivered at term, whereas others with more optimal microbiome types had sPTBs. This suggests that other factors contribute to African American women having a nonoptimal microbiota and being especially predisposed to sPTB.
Through the study’s immunologic profiling, we found a significant difference in the cervicovaginal levels of an immune factor, beta-defensin 2, between African American women who delivered at term and those who had a sPTB. Women who had a sPTB, even those who had higher levels of Lactobacillus species, had lower levels of beta-defensin 2. This association was not found in non–African American women.
Beta-defensin 2 is a host-derived antimicrobial peptide that, like other antimicrobial peptides, works at epithelial-mucosal barriers to combat bacteria; we have knowledge of its action from research on the gut, as well as some studies of the vaginal space in nonpregnant women that have focused on sexually transmitted infections.
Most exciting for us was the finding that higher levels of beta-defensin 2 appeared to lower the risk of sPTB in women who had a nonoptimal cervicovaginal microbiota. There’s an interplay between the host and the microbiota, in other words, and it’s one that could be essential to manipulate as we seek to reduce sPTB.
The cervical epithelial barrier
In the laboratory, meanwhile, we are learning how certain microbes are mechanistically involved in the pathogenesis of sPTB. Research over the last decade has suggested that disruption or breakdown of the cervical epithelial barrier drives cervical remodeling processes that precede sPTB. The question now is, do cervicovaginal bacteria associated with sPTB, or a nonoptimal cervicovaginal microbiota, cause disruption of the vaginal and cervical epithelial barrier – and how?
Using an in vitro model system, we found that Mobiluncus curtisii/mulieris, the bacterial taxa with the strongest association with sPTB in our Motherhood & Microbiome cohort and one that has long been associated with bacterial vaginosis, had a plethora of effects. It increased cell permeability and the expression of inflammatory mediators associated with cervical epithelial breakdown, and it altered expression of microRNAs that have been associated with sPTB in human studies.
Our study on Mobiluncus has served as proof of concept to us that, not only is the bacteria associated with sPTB, but that there are multiple mechanisms by which it can disrupt the cervicovaginal barrier and lead to cervical remodeling.5
The findings echo previous in vitro research on Gardnerella vaginalis, another anaerobic bacterium that has been associated with bacterial vaginosis and adverse obstetric outcomes, including sPTB.6 Using similar models, we found that G. vaginalis disrupts the cervical epithelial barrier through diverse mechanisms including the cleavage of certain proteins, the up-regulation of proinflammatory immune mediators, and altered gene expression.
Lactobacillus crispatus, on the other hand, conferred protection to the cervical epithelial barrier in this study by mitigating various G. vaginalis–induced effects.
Learning more about host-microbe interactions and the role of microbial metabolites in these interactions, as well as the role of altered gene expression in cervical function, will help us to more fully understand the biological mechanisms regulating cervicovaginal epithelial cells. At this point, we know that, as in the gut, bacteria commonly found in the cervicovaginal space play a significant role in regulating the function of epithelial cells (in both optimal and nonoptimal microbiota), and that various bacteria associated with sPTB contribute to poor outcomes by breaking down the cervical epithelium.
Therapeutic implications
Our growing knowledge of the cervicovaginal microbiota does not yet support screening or any particular interventions. We don’t know, for instance, that administering probiotics or prebiotics orally or vaginally will have any effect on rates of sPTB.
Ongoing research at all levels holds promise, however, for the development of diagnostics to identify women at risk for sPTB, and for the development of therapeutic strategies that aim to modify the microbiome and/or modify the immune response. We know from other areas of medicine that there are realistic ways to modulate the immune response and/or microbiota in a system to alter risk.
We need to more thoroughly understand the risk of particular microbiota and immune response factors – and how they vary by race and ethnicity – and we need to study the cervicovaginal microbiota of women before and during pregnancy to learn whether there is something about pregnancy or even about intercourse that can change one’s microbiome to a less favorable state.
It may well be possible in the near future to identify high-risk states of nonoptimal microbiota before conception – microbiota that, in and of themselves, may not be pathogenic but that become detrimental during pregnancy – and it should be possible to screen women early in pregnancy for microbial or immune signatures or both.
The question often arises in medicine of the validity of screening without having achieved certainty about treatments. However, in obstetrics, where we have different levels of care and the ability to personalize monitoring and care, identifying those at greatest risk still has value. Ultimately, with enough investment in all levels of research (basic, translational, and clinical), we can develop interventions and therapeutics that address a biologically plausible mechanism of sPTB and, as a result, achieve significant reductions in the rate of prematurity.
Dr. Elovitz is the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health, vice chair of translational research, and director of the Maternal and Child Health Research Center, department of obstetrics and gynecology, at the University of Pennsylvania, Philadelphia. She disclosed holding a patent on a method to determine risk of preterm birth that relates to the microbiome. Email her at [email protected].
References
1. JAMA. 2017 Mar 14;317(10):1047-56.
2. NIH Human Microbiome Project. https://hmpdacc.org/.
3. PNAS. 2011 Mar 15;108 (Supplement 1):4680-7.
4. Nat Commun. 2019 Mar 21. doi: 10.1038/s41467-019-09285-9.
5. Anaerobe. 2019 Nov 21. doi: 10.1016/j.anaerobe.2019.102127.
6. Front Microbiol. 2018 Oct 8. doi: 10.3389/fmicb.2018.02181.
Prematurity remains the leading cause of neonatal morbidity and mortality, accounting for $26 billion a year in immediate costs, despite the implementation in obstetrics of a host of risk stratification algorithms and strategies for risk reduction, including the use of some medications.
It now is questionable whether injectable 17-alpha hydroxyprogesterone caproate (Makena) truly is efficacious in women who’ve had a prior spontaneous preterm birth (sPTB) – a Food and Drug Administration advisory committee last year recommended withdrawing it from the market based on results of an FDA confirmatory study. Even if the drug were efficacious, only a small percentage of the women who have an sPTB have had a prior one. The majority of sPTB occurs among women without such a history.
Vaginal progesterone appears to confer some protection in women found to have a short cervix during the second trimester, but this approach also has limited reach: Only 9% of women with sPTB had an antecedent short cervix in a 2017 study.1 Like a history of sPTB, screening for short cervical length is a potentially helpful strategy for risk reduction, but it is not a strategy that will significantly impact the overall rate of prematurity.
We’ve fallen short in our goals to significantly reduce the public health impact of prematurity partly because we still do not understand the exact pathways and mechanisms by which sPTB occurs. The main working paradigm for myself and many other researchers over the past 2 decades has centered on infection in the uterus triggering inflammation, followed by cervical remodeling and ripening. Research in animal models, as well as human clinical trials targeting various infections and inflammation, have led to some insights and discoveries, but no successful interventions.
In the past decade, however, our research framework for understanding sPTB incorporates new questions about immunologic, microbiological, and molecular/cellular events that happen in the cervicovaginal space. We’ve learned more about the cervicovaginal microbiota, and most recently, our research at the University of Pennsylvania has elucidated the role that nonoptimal bacteria play in disrupting the cervical endothelial barrier and initiating the process of cervical remodeling that likely precedes sPTB.
We also know that this association is stronger in black women and may help explain some of the observed racial disparities in sPTB. Although more research is needed to determine specific therapeutic strategies, new doors are open.
Host immune-microbial interactions
This new research paradigm has involved stepping back and asking basic questions, such as, what do we really know about the cervicovaginal space? In actuality, we know very little. We know little about the immune function of the vaginal and cervical epithelial cells in pregnancy, for instance, and there is a large gap in knowledge regarding the biomechanics of the cervix – a remarkable organ that can change shape and function in a matter of minutes. Studies on the biomechanics of the cervix during pregnancy and in labor are still in their infancy.
However, lessons can be drawn from research on inflammatory bowel disease and other disorders involving the gut. In the gastrointestinal tract, epithelial cells have been found to act as sentinels, forming a mucosal barrier against bacterial pathogens and secreting various immune factors. Research in this field also has shown that microbes living in the gut produce metabolites; that these microbial metabolites may be the key messengers from the microbial communities to the epithelial barrier; and that the microbes, microbial metabolites, and immune responses are responsible for triggering inflammatory processes in the tissues underneath.
In 2011, Jacques Ravel, PhD, who was part of the National Institutes of Health’s Human Microbiome Project, characterized the vaginal microbiome of reproductive-age women for the first time.2 His paper classified the vaginal microbial communities of approximately 400 asymptomatic women of various ethnicities into five “community state types” (CSTs) based on the predominant bacteria found in the cervicovaginal space.3
On the heels of his research, Dr. Ravel and I launched an NIH-funded study involving a prospective cohort of 2,000 women with singleton pregnancies – the Motherhood & Microbiome cohort – to look at the cervicovaginal microbiota, the local immune response, and the risk of sPTB.4 Cervicovaginal samples were collected at 16-20 weeks’ gestation and during two subsequent clinical visits. From this cohort, which was composed mostly of African American women (74.5%), we conducted a nested case-controlled study of 103 cases of sPTB and 432 women who delivered at term, matched for race.
We carefully adjudicated the deliveries in our 2,000-person cohort so that we homed in on sPTB as opposed to preterm births that are medically indicated for reasons such as fetal distress or preeclampsia. (Several prior studies looking at the associations between the cervicovaginal microbiome had a heterogeneous phenotyping of PTB that made it hard to draw definitive conclusions.)
Our focus in assessing the microbiome and immunologic profiles was on the samples collected at the earliest time points in pregnancy because we hoped to detect a “signature” that could predict an outcome months later. Indeed, we found that the nonoptimal microbiota, known in microbiological terms as CST IV, was associated with about a 150% increased risk of sPTB. This community comprises a dominant array of anaerobic bacteria and a paucity of Lactobacillus species.
We also found that a larger proportion of African American women, compared with non–African American women, had this nonoptimal microbiota early in pregnancy (40% vs. 15%), which is consistent with previous studies in pregnancy and nonpregnancy showing lower levels of Lactobacillus species in the cervicovaginal microbiome of African American women.
Even more interesting was the finding that, although the rate of sPTB was higher in African American women and the effect of CST IV on sPTB was stronger in these women, the risk of sPTB couldn’t be explained solely by the presence of CST IV. Some women with this nonoptimal microbiome delivered at term, whereas others with more optimal microbiome types had sPTBs. This suggests that other factors contribute to African American women having a nonoptimal microbiota and being especially predisposed to sPTB.
Through the study’s immunologic profiling, we found a significant difference in the cervicovaginal levels of an immune factor, beta-defensin 2, between African American women who delivered at term and those who had a sPTB. Women who had a sPTB, even those who had higher levels of Lactobacillus species, had lower levels of beta-defensin 2. This association was not found in non–African American women.
Beta-defensin 2 is a host-derived antimicrobial peptide that, like other antimicrobial peptides, works at epithelial-mucosal barriers to combat bacteria; we have knowledge of its action from research on the gut, as well as some studies of the vaginal space in nonpregnant women that have focused on sexually transmitted infections.
Most exciting for us was the finding that higher levels of beta-defensin 2 appeared to lower the risk of sPTB in women who had a nonoptimal cervicovaginal microbiota. There’s an interplay between the host and the microbiota, in other words, and it’s one that could be essential to manipulate as we seek to reduce sPTB.
The cervical epithelial barrier
In the laboratory, meanwhile, we are learning how certain microbes are mechanistically involved in the pathogenesis of sPTB. Research over the last decade has suggested that disruption or breakdown of the cervical epithelial barrier drives cervical remodeling processes that precede sPTB. The question now is, do cervicovaginal bacteria associated with sPTB, or a nonoptimal cervicovaginal microbiota, cause disruption of the vaginal and cervical epithelial barrier – and how?
Using an in vitro model system, we found that Mobiluncus curtisii/mulieris, the bacterial taxa with the strongest association with sPTB in our Motherhood & Microbiome cohort and one that has long been associated with bacterial vaginosis, had a plethora of effects. It increased cell permeability and the expression of inflammatory mediators associated with cervical epithelial breakdown, and it altered expression of microRNAs that have been associated with sPTB in human studies.
Our study on Mobiluncus has served as proof of concept to us that, not only is the bacteria associated with sPTB, but that there are multiple mechanisms by which it can disrupt the cervicovaginal barrier and lead to cervical remodeling.5
The findings echo previous in vitro research on Gardnerella vaginalis, another anaerobic bacterium that has been associated with bacterial vaginosis and adverse obstetric outcomes, including sPTB.6 Using similar models, we found that G. vaginalis disrupts the cervical epithelial barrier through diverse mechanisms including the cleavage of certain proteins, the up-regulation of proinflammatory immune mediators, and altered gene expression.
Lactobacillus crispatus, on the other hand, conferred protection to the cervical epithelial barrier in this study by mitigating various G. vaginalis–induced effects.
Learning more about host-microbe interactions and the role of microbial metabolites in these interactions, as well as the role of altered gene expression in cervical function, will help us to more fully understand the biological mechanisms regulating cervicovaginal epithelial cells. At this point, we know that, as in the gut, bacteria commonly found in the cervicovaginal space play a significant role in regulating the function of epithelial cells (in both optimal and nonoptimal microbiota), and that various bacteria associated with sPTB contribute to poor outcomes by breaking down the cervical epithelium.
Therapeutic implications
Our growing knowledge of the cervicovaginal microbiota does not yet support screening or any particular interventions. We don’t know, for instance, that administering probiotics or prebiotics orally or vaginally will have any effect on rates of sPTB.
Ongoing research at all levels holds promise, however, for the development of diagnostics to identify women at risk for sPTB, and for the development of therapeutic strategies that aim to modify the microbiome and/or modify the immune response. We know from other areas of medicine that there are realistic ways to modulate the immune response and/or microbiota in a system to alter risk.
We need to more thoroughly understand the risk of particular microbiota and immune response factors – and how they vary by race and ethnicity – and we need to study the cervicovaginal microbiota of women before and during pregnancy to learn whether there is something about pregnancy or even about intercourse that can change one’s microbiome to a less favorable state.
It may well be possible in the near future to identify high-risk states of nonoptimal microbiota before conception – microbiota that, in and of themselves, may not be pathogenic but that become detrimental during pregnancy – and it should be possible to screen women early in pregnancy for microbial or immune signatures or both.
The question often arises in medicine of the validity of screening without having achieved certainty about treatments. However, in obstetrics, where we have different levels of care and the ability to personalize monitoring and care, identifying those at greatest risk still has value. Ultimately, with enough investment in all levels of research (basic, translational, and clinical), we can develop interventions and therapeutics that address a biologically plausible mechanism of sPTB and, as a result, achieve significant reductions in the rate of prematurity.
Dr. Elovitz is the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health, vice chair of translational research, and director of the Maternal and Child Health Research Center, department of obstetrics and gynecology, at the University of Pennsylvania, Philadelphia. She disclosed holding a patent on a method to determine risk of preterm birth that relates to the microbiome. Email her at [email protected].
References
1. JAMA. 2017 Mar 14;317(10):1047-56.
2. NIH Human Microbiome Project. https://hmpdacc.org/.
3. PNAS. 2011 Mar 15;108 (Supplement 1):4680-7.
4. Nat Commun. 2019 Mar 21. doi: 10.1038/s41467-019-09285-9.
5. Anaerobe. 2019 Nov 21. doi: 10.1016/j.anaerobe.2019.102127.
6. Front Microbiol. 2018 Oct 8. doi: 10.3389/fmicb.2018.02181.
Preterm birth: Under the microscope
Preventing infant mortality remains a significant challenge for ob.gyns. Despite the availability of a multitude of preventive and treatment options and some of the best possible medical care offered in the world, the United States lags behind many other developed and developing countries in its rate of infant deaths, which was an estimated 5.8 deaths per 1,000 live births in 2017. We can, and must, do better.
One of the major contributing factors to infant mortality is preterm birth. Defined as birth occurring prior to 37 weeks’ gestation, preterm birth is associated with a myriad of severe neonatal sequelae: low birth weight, bacterial sepsis, neonatal hemorrhage, and respiratory distress syndrome, among others. Therefore, many within the clinical and biomedical research spheres recognize that preventing preterm birth means reducing infant deaths.
However, therein lies the conundrum. We know very little about what causes preterm birth, which renders the current therapeutic strategies – such as use of progesterone supplements or cerclage placement – good for some but not all patients. It is thus vital to continue research to unravel the underlying mechanisms of preterm birth.
A promising area of investigation is the field of microbiome research, which has made great strides in advancing our awareness of the critical role of the millions of organisms living on and within us in maintaining health and fighting disease. For example, we now realize that eradicating all the commensals in our gastrointestinal tract has unintended and very negative consequences and, for patients whose good bacteria have been eliminated, fecal transplant is a therapeutic option. Therefore, it stands to reason that the microbes found in the vagina contribute significantly to women’s overall reproductive health.
The publication of the groundbreaking study characterizing the vaginal microbiome species in reproductive-age women opened new avenues of research into how these organisms contribute to women’s health. Importantly, this work, led initially by Jacques Ravel, PhD, a professor in the department of microbiology & immunology and associate director of the Institute for Genome Sciences at the University of Maryland School of Medicine, has spawned additional investigations into the potential role of the vaginal microbiome in preterm birth.
To provide some insight into the research around how the microorganisms in the vagina may induce or prevent preterm birth is our guest author, Michal A. Elovitz, MD, the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health, vice chair of translational research, and director of the Maternal and Child Health Research Center, department of obstetrics and gynecology, at the University of Pennsylvania, Philadelphia.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Preventing infant mortality remains a significant challenge for ob.gyns. Despite the availability of a multitude of preventive and treatment options and some of the best possible medical care offered in the world, the United States lags behind many other developed and developing countries in its rate of infant deaths, which was an estimated 5.8 deaths per 1,000 live births in 2017. We can, and must, do better.
One of the major contributing factors to infant mortality is preterm birth. Defined as birth occurring prior to 37 weeks’ gestation, preterm birth is associated with a myriad of severe neonatal sequelae: low birth weight, bacterial sepsis, neonatal hemorrhage, and respiratory distress syndrome, among others. Therefore, many within the clinical and biomedical research spheres recognize that preventing preterm birth means reducing infant deaths.
However, therein lies the conundrum. We know very little about what causes preterm birth, which renders the current therapeutic strategies – such as use of progesterone supplements or cerclage placement – good for some but not all patients. It is thus vital to continue research to unravel the underlying mechanisms of preterm birth.
A promising area of investigation is the field of microbiome research, which has made great strides in advancing our awareness of the critical role of the millions of organisms living on and within us in maintaining health and fighting disease. For example, we now realize that eradicating all the commensals in our gastrointestinal tract has unintended and very negative consequences and, for patients whose good bacteria have been eliminated, fecal transplant is a therapeutic option. Therefore, it stands to reason that the microbes found in the vagina contribute significantly to women’s overall reproductive health.
The publication of the groundbreaking study characterizing the vaginal microbiome species in reproductive-age women opened new avenues of research into how these organisms contribute to women’s health. Importantly, this work, led initially by Jacques Ravel, PhD, a professor in the department of microbiology & immunology and associate director of the Institute for Genome Sciences at the University of Maryland School of Medicine, has spawned additional investigations into the potential role of the vaginal microbiome in preterm birth.
To provide some insight into the research around how the microorganisms in the vagina may induce or prevent preterm birth is our guest author, Michal A. Elovitz, MD, the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health, vice chair of translational research, and director of the Maternal and Child Health Research Center, department of obstetrics and gynecology, at the University of Pennsylvania, Philadelphia.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Preventing infant mortality remains a significant challenge for ob.gyns. Despite the availability of a multitude of preventive and treatment options and some of the best possible medical care offered in the world, the United States lags behind many other developed and developing countries in its rate of infant deaths, which was an estimated 5.8 deaths per 1,000 live births in 2017. We can, and must, do better.
One of the major contributing factors to infant mortality is preterm birth. Defined as birth occurring prior to 37 weeks’ gestation, preterm birth is associated with a myriad of severe neonatal sequelae: low birth weight, bacterial sepsis, neonatal hemorrhage, and respiratory distress syndrome, among others. Therefore, many within the clinical and biomedical research spheres recognize that preventing preterm birth means reducing infant deaths.
However, therein lies the conundrum. We know very little about what causes preterm birth, which renders the current therapeutic strategies – such as use of progesterone supplements or cerclage placement – good for some but not all patients. It is thus vital to continue research to unravel the underlying mechanisms of preterm birth.
A promising area of investigation is the field of microbiome research, which has made great strides in advancing our awareness of the critical role of the millions of organisms living on and within us in maintaining health and fighting disease. For example, we now realize that eradicating all the commensals in our gastrointestinal tract has unintended and very negative consequences and, for patients whose good bacteria have been eliminated, fecal transplant is a therapeutic option. Therefore, it stands to reason that the microbes found in the vagina contribute significantly to women’s overall reproductive health.
The publication of the groundbreaking study characterizing the vaginal microbiome species in reproductive-age women opened new avenues of research into how these organisms contribute to women’s health. Importantly, this work, led initially by Jacques Ravel, PhD, a professor in the department of microbiology & immunology and associate director of the Institute for Genome Sciences at the University of Maryland School of Medicine, has spawned additional investigations into the potential role of the vaginal microbiome in preterm birth.
To provide some insight into the research around how the microorganisms in the vagina may induce or prevent preterm birth is our guest author, Michal A. Elovitz, MD, the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health, vice chair of translational research, and director of the Maternal and Child Health Research Center, department of obstetrics and gynecology, at the University of Pennsylvania, Philadelphia.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Macrolides early in pregnancy linked to greater malformation risk
Children exposed to macrolides during the first trimester of pregnancy had an increased risk of major malformations, compared with first-trimester penicillin exposure, according to an observational study.
Use of antibiotics is common in pregnancy, and macrolides commonly are used if a penicillin allergy is reported.
Hypospadias and other genital malformations also were more likely with exposure during any trimester to macrolides, although this association lost significance when limited to the first trimester. The researchers did not identify any associations with macrolides exposure and neurodevelopmental disorders.
The observational study could not establish causality, but the researchers calculated an estimate of likely excess malformations if the association were found to be causal: “For every 1,000 mothers prescribed macrolides instead of penicillins during the first trimester, an additional 4.1 children would have cardiovascular malformations,” Heng Fan, a PhD student at the University College London, and colleagues wrote in the BMJ. “The corresponding figures for prescriptions during any trimester and genital malformations would be 1.7.”
The researchers used records from the U.K. Clinical Practice Research Datalink to analyze outcomes in 104,605 children born between 1990 and 2016 to mothers who received at least one prescription of erythromycin, clarithromycin, azithromycin, or penicillin monotherapy between their fourth week of pregnancy and delivery. Women prescribed any known teratogenic medications were excluded.
The majority of the mothers (92%) had been prescribed penicillin once, and 8% were prescribed a macrolide antibiotic once during pregnancy.
The researchers tallied and calculated the children’s risk of major malformations; cerebral palsy; epilepsy; ADHD; autism spectrum disorder; and any nervous, cardiovascular, gastrointestinal, genital, or urinary malformations. The children were tracked through a median 6 years of age.
In comparing risk of malformations or neurodevelopmental disorders among children, the researchers chose to compare exposure to macrolides and penicillin to reduce the likelihood of confounding by indication for infections. (They also included two negative control groups: unexposed siblings and women prescribed antibiotics before conception.) The authors acknowledged, however, that residual confounding still may occur “if macrolides were prescribed for specific indications (e.g., chlamydia), or when potential risk factors for malformations or neurodevelopmental outcomes differed between treatment groups.”
The overall rate of malformations was 22 per 1,000 children prenatally exposed to macrolides (28 in first trimester and 20 in second or third trimester) and 17 per 1,000 children prenatally exposed to penicillin. The risk and type of malformations varied, however, according to the trimester.
The researchers made adjustments to account for differences in a wide range of maternal factors: age at delivery, calendar year of delivery, alcohol misuse, illegal drug use, tobacco use, obesity, hypertension, diabetes, anxiety, depression, and epilepsy. They also adjusted for parity, multiples, and chronic medical treatments, as well as genitourinary tract infections or STIs during pregnancy, both of which are linked to preterm labor.
Compared with children exposed to penicillin during the first trimester of pregnancy, risk of malformations was 1.6 times greater in those exposed to macrolides in the first trimester (risk ratio, 1.55; 28 vs. 18 per 1,000). Erythromycin exposure in the first trimester also was linked to a 50% greater likelihood of any major malformation compared with penicillin (RR, 1.5; 27 vs. 18 per 1,000).
Cardiovascular malformations in particular were more likely in those exposed to macrolides (11 per 1,000), compared with penicillin (7 per 1,000) in the first trimester (RR, 1.62). Meanwhile, genital malformations, primarily hypospadias, occurred more frequently in children whose mothers were prescribed macrolides (5 per 1,000), compared with penicillin (3 per 1,000) in any trimester (RR, 1.58).
No increased risk of major malformations was associated with macrolides prescribed only in the second or third trimester, although a borderline significant association existed with gastrointestinal malformations. The authors also found no links between macrolides exposure and increased risk of cerebral palsy, epilepsy, ADHD, or autism spectrum disorder.
The findings did not change in several sensitivity analyses, including one that restricted analysis to antibiotics prescribed only for respiratory tract infections.
Dr. Fan and associates discussed several potential biological mechanisms for causation, including the arrhythmic effect of macrolides that may relate to cardiovascular malformations or contribute to fetal hypoxia. They noted that “macrolide prescribing during pregnancy warrants caution,” and recommend including on drug safety labels “that there is uncertainty about the safety of macrolides, including erythromycin” and alternative antibiotics should be used when possible.
Iris Krishna, MD, MPH, assistant professor of maternal-fetal medicine at Emory University, Atlanta, agreed with the study authors that use of macrolides in the first trimester warrants further investigation, and if an appropriate alternative antibiotic is available, then it should be preferentially considered when treating infections in the first trimester.
“However, if macrolides are the only treatment option, pregnant women can be reassured that the absolute risk of a birth defect is low, and this should not discourage them from taking a macrolide when needed as untreated infections pose a greater risk in pregnancy,” she said in an interview.
“This study does not establish that macrolide antibiotics cause birth defects, but it suggests a potential association. Previous studies examining the use of macrolides, such as erythromycin, have not demonstrated a consistent pattern of birth defects, and heart defects identified were classified as mostly mild. The authors suggest that the potential biologic mechanism based on rat models may be that macrolides might induce fetal cardiac arrhythmias and short-term fetal hypoxia. This study was underpowered to examine macrolide exposure for specific malformations. To avoid underpowered comparisons, the authors’ categorized malformations by organ systems, so the spectrum of cardiac defects is unclear,” commented Dr. Krishna, who also is a member of the Ob.Gyn. News editorial advisory board.
“Current recommendations for macrolide antibiotic use in pregnancy in the second and third trimester of pregnancy, and in particular when used for obstetric indications, such as prelabor rupture of membranes to prolong the latency period to delivery, should not be altered based on the findings of this study,” she concluded.
The research was funded by Child Health Research CIO Trust, the China Scholarship Council, Health Data Research UK, and the National Institute for Health Research. Dr. Fan and associates had no industry disclosures. Dr. Krishna had no relevant financial disclosures.
SOURCE: Fan H et al. BMJ. 2020;368:m331.
Children exposed to macrolides during the first trimester of pregnancy had an increased risk of major malformations, compared with first-trimester penicillin exposure, according to an observational study.
Use of antibiotics is common in pregnancy, and macrolides commonly are used if a penicillin allergy is reported.
Hypospadias and other genital malformations also were more likely with exposure during any trimester to macrolides, although this association lost significance when limited to the first trimester. The researchers did not identify any associations with macrolides exposure and neurodevelopmental disorders.
The observational study could not establish causality, but the researchers calculated an estimate of likely excess malformations if the association were found to be causal: “For every 1,000 mothers prescribed macrolides instead of penicillins during the first trimester, an additional 4.1 children would have cardiovascular malformations,” Heng Fan, a PhD student at the University College London, and colleagues wrote in the BMJ. “The corresponding figures for prescriptions during any trimester and genital malformations would be 1.7.”
The researchers used records from the U.K. Clinical Practice Research Datalink to analyze outcomes in 104,605 children born between 1990 and 2016 to mothers who received at least one prescription of erythromycin, clarithromycin, azithromycin, or penicillin monotherapy between their fourth week of pregnancy and delivery. Women prescribed any known teratogenic medications were excluded.
The majority of the mothers (92%) had been prescribed penicillin once, and 8% were prescribed a macrolide antibiotic once during pregnancy.
The researchers tallied and calculated the children’s risk of major malformations; cerebral palsy; epilepsy; ADHD; autism spectrum disorder; and any nervous, cardiovascular, gastrointestinal, genital, or urinary malformations. The children were tracked through a median 6 years of age.
In comparing risk of malformations or neurodevelopmental disorders among children, the researchers chose to compare exposure to macrolides and penicillin to reduce the likelihood of confounding by indication for infections. (They also included two negative control groups: unexposed siblings and women prescribed antibiotics before conception.) The authors acknowledged, however, that residual confounding still may occur “if macrolides were prescribed for specific indications (e.g., chlamydia), or when potential risk factors for malformations or neurodevelopmental outcomes differed between treatment groups.”
The overall rate of malformations was 22 per 1,000 children prenatally exposed to macrolides (28 in first trimester and 20 in second or third trimester) and 17 per 1,000 children prenatally exposed to penicillin. The risk and type of malformations varied, however, according to the trimester.
The researchers made adjustments to account for differences in a wide range of maternal factors: age at delivery, calendar year of delivery, alcohol misuse, illegal drug use, tobacco use, obesity, hypertension, diabetes, anxiety, depression, and epilepsy. They also adjusted for parity, multiples, and chronic medical treatments, as well as genitourinary tract infections or STIs during pregnancy, both of which are linked to preterm labor.
Compared with children exposed to penicillin during the first trimester of pregnancy, risk of malformations was 1.6 times greater in those exposed to macrolides in the first trimester (risk ratio, 1.55; 28 vs. 18 per 1,000). Erythromycin exposure in the first trimester also was linked to a 50% greater likelihood of any major malformation compared with penicillin (RR, 1.5; 27 vs. 18 per 1,000).
Cardiovascular malformations in particular were more likely in those exposed to macrolides (11 per 1,000), compared with penicillin (7 per 1,000) in the first trimester (RR, 1.62). Meanwhile, genital malformations, primarily hypospadias, occurred more frequently in children whose mothers were prescribed macrolides (5 per 1,000), compared with penicillin (3 per 1,000) in any trimester (RR, 1.58).
No increased risk of major malformations was associated with macrolides prescribed only in the second or third trimester, although a borderline significant association existed with gastrointestinal malformations. The authors also found no links between macrolides exposure and increased risk of cerebral palsy, epilepsy, ADHD, or autism spectrum disorder.
The findings did not change in several sensitivity analyses, including one that restricted analysis to antibiotics prescribed only for respiratory tract infections.
Dr. Fan and associates discussed several potential biological mechanisms for causation, including the arrhythmic effect of macrolides that may relate to cardiovascular malformations or contribute to fetal hypoxia. They noted that “macrolide prescribing during pregnancy warrants caution,” and recommend including on drug safety labels “that there is uncertainty about the safety of macrolides, including erythromycin” and alternative antibiotics should be used when possible.
Iris Krishna, MD, MPH, assistant professor of maternal-fetal medicine at Emory University, Atlanta, agreed with the study authors that use of macrolides in the first trimester warrants further investigation, and if an appropriate alternative antibiotic is available, then it should be preferentially considered when treating infections in the first trimester.
“However, if macrolides are the only treatment option, pregnant women can be reassured that the absolute risk of a birth defect is low, and this should not discourage them from taking a macrolide when needed as untreated infections pose a greater risk in pregnancy,” she said in an interview.
“This study does not establish that macrolide antibiotics cause birth defects, but it suggests a potential association. Previous studies examining the use of macrolides, such as erythromycin, have not demonstrated a consistent pattern of birth defects, and heart defects identified were classified as mostly mild. The authors suggest that the potential biologic mechanism based on rat models may be that macrolides might induce fetal cardiac arrhythmias and short-term fetal hypoxia. This study was underpowered to examine macrolide exposure for specific malformations. To avoid underpowered comparisons, the authors’ categorized malformations by organ systems, so the spectrum of cardiac defects is unclear,” commented Dr. Krishna, who also is a member of the Ob.Gyn. News editorial advisory board.
“Current recommendations for macrolide antibiotic use in pregnancy in the second and third trimester of pregnancy, and in particular when used for obstetric indications, such as prelabor rupture of membranes to prolong the latency period to delivery, should not be altered based on the findings of this study,” she concluded.
The research was funded by Child Health Research CIO Trust, the China Scholarship Council, Health Data Research UK, and the National Institute for Health Research. Dr. Fan and associates had no industry disclosures. Dr. Krishna had no relevant financial disclosures.
SOURCE: Fan H et al. BMJ. 2020;368:m331.
Children exposed to macrolides during the first trimester of pregnancy had an increased risk of major malformations, compared with first-trimester penicillin exposure, according to an observational study.
Use of antibiotics is common in pregnancy, and macrolides commonly are used if a penicillin allergy is reported.
Hypospadias and other genital malformations also were more likely with exposure during any trimester to macrolides, although this association lost significance when limited to the first trimester. The researchers did not identify any associations with macrolides exposure and neurodevelopmental disorders.
The observational study could not establish causality, but the researchers calculated an estimate of likely excess malformations if the association were found to be causal: “For every 1,000 mothers prescribed macrolides instead of penicillins during the first trimester, an additional 4.1 children would have cardiovascular malformations,” Heng Fan, a PhD student at the University College London, and colleagues wrote in the BMJ. “The corresponding figures for prescriptions during any trimester and genital malformations would be 1.7.”
The researchers used records from the U.K. Clinical Practice Research Datalink to analyze outcomes in 104,605 children born between 1990 and 2016 to mothers who received at least one prescription of erythromycin, clarithromycin, azithromycin, or penicillin monotherapy between their fourth week of pregnancy and delivery. Women prescribed any known teratogenic medications were excluded.
The majority of the mothers (92%) had been prescribed penicillin once, and 8% were prescribed a macrolide antibiotic once during pregnancy.
The researchers tallied and calculated the children’s risk of major malformations; cerebral palsy; epilepsy; ADHD; autism spectrum disorder; and any nervous, cardiovascular, gastrointestinal, genital, or urinary malformations. The children were tracked through a median 6 years of age.
In comparing risk of malformations or neurodevelopmental disorders among children, the researchers chose to compare exposure to macrolides and penicillin to reduce the likelihood of confounding by indication for infections. (They also included two negative control groups: unexposed siblings and women prescribed antibiotics before conception.) The authors acknowledged, however, that residual confounding still may occur “if macrolides were prescribed for specific indications (e.g., chlamydia), or when potential risk factors for malformations or neurodevelopmental outcomes differed between treatment groups.”
The overall rate of malformations was 22 per 1,000 children prenatally exposed to macrolides (28 in first trimester and 20 in second or third trimester) and 17 per 1,000 children prenatally exposed to penicillin. The risk and type of malformations varied, however, according to the trimester.
The researchers made adjustments to account for differences in a wide range of maternal factors: age at delivery, calendar year of delivery, alcohol misuse, illegal drug use, tobacco use, obesity, hypertension, diabetes, anxiety, depression, and epilepsy. They also adjusted for parity, multiples, and chronic medical treatments, as well as genitourinary tract infections or STIs during pregnancy, both of which are linked to preterm labor.
Compared with children exposed to penicillin during the first trimester of pregnancy, risk of malformations was 1.6 times greater in those exposed to macrolides in the first trimester (risk ratio, 1.55; 28 vs. 18 per 1,000). Erythromycin exposure in the first trimester also was linked to a 50% greater likelihood of any major malformation compared with penicillin (RR, 1.5; 27 vs. 18 per 1,000).
Cardiovascular malformations in particular were more likely in those exposed to macrolides (11 per 1,000), compared with penicillin (7 per 1,000) in the first trimester (RR, 1.62). Meanwhile, genital malformations, primarily hypospadias, occurred more frequently in children whose mothers were prescribed macrolides (5 per 1,000), compared with penicillin (3 per 1,000) in any trimester (RR, 1.58).
No increased risk of major malformations was associated with macrolides prescribed only in the second or third trimester, although a borderline significant association existed with gastrointestinal malformations. The authors also found no links between macrolides exposure and increased risk of cerebral palsy, epilepsy, ADHD, or autism spectrum disorder.
The findings did not change in several sensitivity analyses, including one that restricted analysis to antibiotics prescribed only for respiratory tract infections.
Dr. Fan and associates discussed several potential biological mechanisms for causation, including the arrhythmic effect of macrolides that may relate to cardiovascular malformations or contribute to fetal hypoxia. They noted that “macrolide prescribing during pregnancy warrants caution,” and recommend including on drug safety labels “that there is uncertainty about the safety of macrolides, including erythromycin” and alternative antibiotics should be used when possible.
Iris Krishna, MD, MPH, assistant professor of maternal-fetal medicine at Emory University, Atlanta, agreed with the study authors that use of macrolides in the first trimester warrants further investigation, and if an appropriate alternative antibiotic is available, then it should be preferentially considered when treating infections in the first trimester.
“However, if macrolides are the only treatment option, pregnant women can be reassured that the absolute risk of a birth defect is low, and this should not discourage them from taking a macrolide when needed as untreated infections pose a greater risk in pregnancy,” she said in an interview.
“This study does not establish that macrolide antibiotics cause birth defects, but it suggests a potential association. Previous studies examining the use of macrolides, such as erythromycin, have not demonstrated a consistent pattern of birth defects, and heart defects identified were classified as mostly mild. The authors suggest that the potential biologic mechanism based on rat models may be that macrolides might induce fetal cardiac arrhythmias and short-term fetal hypoxia. This study was underpowered to examine macrolide exposure for specific malformations. To avoid underpowered comparisons, the authors’ categorized malformations by organ systems, so the spectrum of cardiac defects is unclear,” commented Dr. Krishna, who also is a member of the Ob.Gyn. News editorial advisory board.
“Current recommendations for macrolide antibiotic use in pregnancy in the second and third trimester of pregnancy, and in particular when used for obstetric indications, such as prelabor rupture of membranes to prolong the latency period to delivery, should not be altered based on the findings of this study,” she concluded.
The research was funded by Child Health Research CIO Trust, the China Scholarship Council, Health Data Research UK, and the National Institute for Health Research. Dr. Fan and associates had no industry disclosures. Dr. Krishna had no relevant financial disclosures.
SOURCE: Fan H et al. BMJ. 2020;368:m331.
FROM THE BMJ
Genetic risk score may flag post-GDM incidence of type 2 disease
Women who had gestational diabetes mellitus had an increased risk for later type 2 diabetes if they carried certain genetic risk factors for the disease, according to a new analysis in BMJ Open Diabetes Research & Care of data from two independent populations.
A higher genetic risk score (GRS) had a modest association with developing type 2 diabetes, but a healthier diet may mitigate this risk, as Mengying Li, PhD, and her colleagues found for participants in the Nurses’ Health Study and members of the Danish National Birth Cohort who developed gestational diabetes mellitus (GDM).
Of 1,884 white women with a history of GDM in the Nurses’ Health Study II (NHSII), 446 (23.7%) went on to develop type 2 diabetes, and of the 550 women who had GDM in the Danish National Birth Cohort (DNBC), 155 (28.2%) developed the disease. The researchers calculated a GRS for type 2 diabetes for the full cohort. Genome-wide association studies completed in European populations were used to identify 59 single-nucleotide polymorphisms (SNPs) associated with the disease.
Dr. Li, an epidemiologist and postdoctoral researcher at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md., and her coauthors found that women whose GRS was in the highest quartile had a relative risk of 1.19 for type 2 diabetes. The relative risks for the three lower quartiles were 1.25, 0.97, and 1.00, respectively (P value for trend = .02). For each increase of five risk alleles in the GRS, NHSII participants had a 7% increased risk for type 2 diabetes, and DNBC participants saw a 9% increased risk.
Comparing these findings with other studies looking at genetic risk and type 2 diabetes in the general population, Dr. Li and her coauthors noted that the increase in relative risk for type 2 disease with increase in GRS was actually slightly weaker in the GDM cohort they studied. “The smaller effect size among women with GDM likely reflects an already higher baseline genetic risk for [type 2 diabetes] than the general population, as we have demonstrated,” they explained.
Though 11 individual SNPs had a significant individual association with the risk for type 2 diabetes initially, that association disappeared after correction for a false-discovery rate. Dr. Li and her coinvestigators conducted a sensitivity analysis that included only 42 SNPs that were later definitively associated with type 2 disease and they saw essentially unchanged results.
The researchers also investigated how dietary quality affected the GRS–type 2 diabetes association by dichotomizing self-reported diet quality in both cohorts into healthier diet quality and less healthy diet quality. They found a tighter association between GRS and type 2 diabetes for women with diet quality below the median, whereas women with higher diet quality did not have such a strong association between GRS and type 2 disease. The researchers wrote that there was “suggestive evidence that a healthful diet might mitigate the excessive risk of T2D [type 2 diabetes] related to greater genetic susceptibility, which supports public health efforts of encouraging a healthful diet” for diabetes prevention in this high-risk population.
Patients in the NHSII were followed for a mean 21.3 years, and those in the DNBC were followed for a mean 12.7 years. Mean age at index pregnancy was 30.5 years for the NHSII cohort and 31.7 for the DNBC cohort. In the NHSII cohort, just 8.4% of participants reported smoking before pregnancy, compared with 26.4% of those in the DNBC cohort. The NHSII cohort participants, wrote Dr. Li and her coauthors, “were also less likely to have a family history of diabetes, less likely to smoke, and be leaner than women in the DNBC.”
Dr. Li and her coauthors noted that, “despite being the largest genetic study by far on [type 2 diabetes] among women with GDM, our study may not be sufficiently powered to examine the associations of individual T2D SNPs in relation to the risk of developing T2D.” Another limitation was that for the Danish cohort, information about diet was drawn from a one-time questionnaire administered between 9 and 16 years after the index pregnancy, so full data about dietary quality over time was not available. Also of note is that the study included only white participants, limiting generalizability to women of color. The authors called for expanding this research into more racially diverse populations.
The study was supported by the National Institutes of Health. The authors reported that they had no conflicts of interest.
SOURCE: Li M et al. BMJ Open Diab Res Care. 2020 Feb 13. doi: 10.1136/bmjdrc-2019-000850.
Women who had gestational diabetes mellitus had an increased risk for later type 2 diabetes if they carried certain genetic risk factors for the disease, according to a new analysis in BMJ Open Diabetes Research & Care of data from two independent populations.
A higher genetic risk score (GRS) had a modest association with developing type 2 diabetes, but a healthier diet may mitigate this risk, as Mengying Li, PhD, and her colleagues found for participants in the Nurses’ Health Study and members of the Danish National Birth Cohort who developed gestational diabetes mellitus (GDM).
Of 1,884 white women with a history of GDM in the Nurses’ Health Study II (NHSII), 446 (23.7%) went on to develop type 2 diabetes, and of the 550 women who had GDM in the Danish National Birth Cohort (DNBC), 155 (28.2%) developed the disease. The researchers calculated a GRS for type 2 diabetes for the full cohort. Genome-wide association studies completed in European populations were used to identify 59 single-nucleotide polymorphisms (SNPs) associated with the disease.
Dr. Li, an epidemiologist and postdoctoral researcher at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md., and her coauthors found that women whose GRS was in the highest quartile had a relative risk of 1.19 for type 2 diabetes. The relative risks for the three lower quartiles were 1.25, 0.97, and 1.00, respectively (P value for trend = .02). For each increase of five risk alleles in the GRS, NHSII participants had a 7% increased risk for type 2 diabetes, and DNBC participants saw a 9% increased risk.
Comparing these findings with other studies looking at genetic risk and type 2 diabetes in the general population, Dr. Li and her coauthors noted that the increase in relative risk for type 2 disease with increase in GRS was actually slightly weaker in the GDM cohort they studied. “The smaller effect size among women with GDM likely reflects an already higher baseline genetic risk for [type 2 diabetes] than the general population, as we have demonstrated,” they explained.
Though 11 individual SNPs had a significant individual association with the risk for type 2 diabetes initially, that association disappeared after correction for a false-discovery rate. Dr. Li and her coinvestigators conducted a sensitivity analysis that included only 42 SNPs that were later definitively associated with type 2 disease and they saw essentially unchanged results.
The researchers also investigated how dietary quality affected the GRS–type 2 diabetes association by dichotomizing self-reported diet quality in both cohorts into healthier diet quality and less healthy diet quality. They found a tighter association between GRS and type 2 diabetes for women with diet quality below the median, whereas women with higher diet quality did not have such a strong association between GRS and type 2 disease. The researchers wrote that there was “suggestive evidence that a healthful diet might mitigate the excessive risk of T2D [type 2 diabetes] related to greater genetic susceptibility, which supports public health efforts of encouraging a healthful diet” for diabetes prevention in this high-risk population.
Patients in the NHSII were followed for a mean 21.3 years, and those in the DNBC were followed for a mean 12.7 years. Mean age at index pregnancy was 30.5 years for the NHSII cohort and 31.7 for the DNBC cohort. In the NHSII cohort, just 8.4% of participants reported smoking before pregnancy, compared with 26.4% of those in the DNBC cohort. The NHSII cohort participants, wrote Dr. Li and her coauthors, “were also less likely to have a family history of diabetes, less likely to smoke, and be leaner than women in the DNBC.”
Dr. Li and her coauthors noted that, “despite being the largest genetic study by far on [type 2 diabetes] among women with GDM, our study may not be sufficiently powered to examine the associations of individual T2D SNPs in relation to the risk of developing T2D.” Another limitation was that for the Danish cohort, information about diet was drawn from a one-time questionnaire administered between 9 and 16 years after the index pregnancy, so full data about dietary quality over time was not available. Also of note is that the study included only white participants, limiting generalizability to women of color. The authors called for expanding this research into more racially diverse populations.
The study was supported by the National Institutes of Health. The authors reported that they had no conflicts of interest.
SOURCE: Li M et al. BMJ Open Diab Res Care. 2020 Feb 13. doi: 10.1136/bmjdrc-2019-000850.
Women who had gestational diabetes mellitus had an increased risk for later type 2 diabetes if they carried certain genetic risk factors for the disease, according to a new analysis in BMJ Open Diabetes Research & Care of data from two independent populations.
A higher genetic risk score (GRS) had a modest association with developing type 2 diabetes, but a healthier diet may mitigate this risk, as Mengying Li, PhD, and her colleagues found for participants in the Nurses’ Health Study and members of the Danish National Birth Cohort who developed gestational diabetes mellitus (GDM).
Of 1,884 white women with a history of GDM in the Nurses’ Health Study II (NHSII), 446 (23.7%) went on to develop type 2 diabetes, and of the 550 women who had GDM in the Danish National Birth Cohort (DNBC), 155 (28.2%) developed the disease. The researchers calculated a GRS for type 2 diabetes for the full cohort. Genome-wide association studies completed in European populations were used to identify 59 single-nucleotide polymorphisms (SNPs) associated with the disease.
Dr. Li, an epidemiologist and postdoctoral researcher at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md., and her coauthors found that women whose GRS was in the highest quartile had a relative risk of 1.19 for type 2 diabetes. The relative risks for the three lower quartiles were 1.25, 0.97, and 1.00, respectively (P value for trend = .02). For each increase of five risk alleles in the GRS, NHSII participants had a 7% increased risk for type 2 diabetes, and DNBC participants saw a 9% increased risk.
Comparing these findings with other studies looking at genetic risk and type 2 diabetes in the general population, Dr. Li and her coauthors noted that the increase in relative risk for type 2 disease with increase in GRS was actually slightly weaker in the GDM cohort they studied. “The smaller effect size among women with GDM likely reflects an already higher baseline genetic risk for [type 2 diabetes] than the general population, as we have demonstrated,” they explained.
Though 11 individual SNPs had a significant individual association with the risk for type 2 diabetes initially, that association disappeared after correction for a false-discovery rate. Dr. Li and her coinvestigators conducted a sensitivity analysis that included only 42 SNPs that were later definitively associated with type 2 disease and they saw essentially unchanged results.
The researchers also investigated how dietary quality affected the GRS–type 2 diabetes association by dichotomizing self-reported diet quality in both cohorts into healthier diet quality and less healthy diet quality. They found a tighter association between GRS and type 2 diabetes for women with diet quality below the median, whereas women with higher diet quality did not have such a strong association between GRS and type 2 disease. The researchers wrote that there was “suggestive evidence that a healthful diet might mitigate the excessive risk of T2D [type 2 diabetes] related to greater genetic susceptibility, which supports public health efforts of encouraging a healthful diet” for diabetes prevention in this high-risk population.
Patients in the NHSII were followed for a mean 21.3 years, and those in the DNBC were followed for a mean 12.7 years. Mean age at index pregnancy was 30.5 years for the NHSII cohort and 31.7 for the DNBC cohort. In the NHSII cohort, just 8.4% of participants reported smoking before pregnancy, compared with 26.4% of those in the DNBC cohort. The NHSII cohort participants, wrote Dr. Li and her coauthors, “were also less likely to have a family history of diabetes, less likely to smoke, and be leaner than women in the DNBC.”
Dr. Li and her coauthors noted that, “despite being the largest genetic study by far on [type 2 diabetes] among women with GDM, our study may not be sufficiently powered to examine the associations of individual T2D SNPs in relation to the risk of developing T2D.” Another limitation was that for the Danish cohort, information about diet was drawn from a one-time questionnaire administered between 9 and 16 years after the index pregnancy, so full data about dietary quality over time was not available. Also of note is that the study included only white participants, limiting generalizability to women of color. The authors called for expanding this research into more racially diverse populations.
The study was supported by the National Institutes of Health. The authors reported that they had no conflicts of interest.
SOURCE: Li M et al. BMJ Open Diab Res Care. 2020 Feb 13. doi: 10.1136/bmjdrc-2019-000850.
FROM BMJ OPEN DIABETES RESEARCH & CARE
Vitamin D supplements in pregnancy boost bone health in offspring
Vitamin D supplementation during pregnancy is associated with higher bone mineral content in the offspring, even up to 6 years after birth, research suggests.
“The well-established tracking of bone mineralization from early life throughout childhood and early adulthood is a key factor for the final peak bone mass gained and the subsequent risk of fractures and osteoporosis later in life,” wrote Nicklas Brustad, MD, of the Herlev and Gentofte Hospital at the University of Copenhagen, and coauthors. Their report is in JAMA Pediatrics.This was a secondary analysis of a prospective, double-blind, randomized controlled trial of high versus standard dose vitamin D supplementation in 623 pregnant Danish women and the outcomes in their 584 children. The women were randomized either to a daily dose of 2,400 IU vitamin D3 (cholecalciferol) or matching placebo capsules from 24 weeks’ gestation until 1 week after birth. All women were advised to maintain a daily intake of 400 IU of vitamin D3.
The children underwent anthropometric growth assessments regularly up to age 6 years, and underwent whole-body dual-energy radiograph absorptiometry (DXA) scanning at 3 years and 6 years.
At 3 years, children of mothers who received the vitamin D supplements showed significantly higher mean total-body-less-head (TBLH) bone mineral content (BMC) compared with those who received placebo (294 g vs. 289 g) and total-body BMC (526 g vs. 514 g), respectively, after adjustment for age, sex, height, and weight.
The difference in total-body BMC was particularly evident in children of mothers who had insufficient vitamin D levels at baseline, compared with those with sufficient vitamin D levels (538 g vs. 514 g). The study also saw higher head bone mineral density (BMD) in children of mothers with insufficient vitamin D at baseline who received supplementation.
At 6 years, there still were significant differences in BMC between the supplementation and placebo groups. Children in the vitamin D group had an 8-g greater TBLH BMC compared with those in the placebo group, and a 14-g higher total BMC.
Among the children of mothers with insufficient preintervention vitamin D, there was an 18-g higher mean total BMC and 0.0125 g/cm2 greater total BMD, compared with those with sufficient vitamin D at baseline.
Overall, the children of mothers who received high-dose vitamin D supplementation had a mean 8-g higher TBLH BMC, a mean 0.023 g/cm2 higher head BMD, and a mean 12-g higher total BMC.
Dr. Brustad and associates noted that the head could represent the most sensitive compartment for intervention, because 80% of bone mineralization of the skull occurs by the age of 3 years.
The study also showed a seasonal effect, such that mothers who gave birth in winter showed the greatest effects of vitamin D supplementation on head BMC.
There was a nonsignificant trend toward a lower fracture rate among children in the supplementation group, compared with the placebo group.
“We speculate that these intervention effects could be of importance for bone health and osteoporosis risk in adult life, which is supported by our likely underpowered post hoc analysis on fracture risk, suggesting an almost 40% reduced incidence of fractures of the larger bones in the high-dose vitamin D group,” the authors wrote.
Vitamin D supplementation did not appear to affect the children’s growth. At 6 years, there were no significant differences between the two groups in body mass index, height, weight, or waist, head, and thorax circumference.
Neonatologist Carol Wagner, MD, said in an interview that the study provided an absolute reason for vitamin D supplementation during pregnancy.
“At the very least, a study like this argues for much more than is recommended by the European nutrition group or the U.S. group,” said Dr. Wagner, professor of pediatrics at the Medical University of South Carolina, Charleston. “Here you have a therapy that costs literally pennies a day, and no one should be deficient.”
She also pointed out that the study was able to show significant effects on BMC despite the fact that there would have been considerable variation in postnatal vitamin D intake from breast milk or formula.
Cristina Palacios, PhD, an associate professor in the department of dietetics and nutrition at Florida International University, Miami, said that vitamin D deficiency is increasingly prevalent worldwide, and is associated with a return of rickets – the skeletal disorder caused by vitamin D deficiency – in children.
“If women are deficient during pregnancy, providing vitamin D supplementation in pregnancy may promote bone health in their offspring,” Dr. Palacios said in an interview. “Because vitamin D is such an important component of bone metabolism, this could prevent future rickets in these children.”
Dr. Palacios coauthored a recent Cochrane review that examined the safety of high-dose vitamin D supplementation in pregnancy, and said the analysis found no evidence of safety concerns.
The study was supported by The Lundbeck Foundation, the Ministry of Health, Danish Council for Strategic Research, and the Capital Region Research Foundation. The authors declared no conflicts of interest.
SOURCE: Brustad N et al. JAMA Pediatrics 2020 Feb 24. doi: 10.1001/jamapediatrics.2019.6083.
Vitamin D supplementation during pregnancy is associated with higher bone mineral content in the offspring, even up to 6 years after birth, research suggests.
“The well-established tracking of bone mineralization from early life throughout childhood and early adulthood is a key factor for the final peak bone mass gained and the subsequent risk of fractures and osteoporosis later in life,” wrote Nicklas Brustad, MD, of the Herlev and Gentofte Hospital at the University of Copenhagen, and coauthors. Their report is in JAMA Pediatrics.This was a secondary analysis of a prospective, double-blind, randomized controlled trial of high versus standard dose vitamin D supplementation in 623 pregnant Danish women and the outcomes in their 584 children. The women were randomized either to a daily dose of 2,400 IU vitamin D3 (cholecalciferol) or matching placebo capsules from 24 weeks’ gestation until 1 week after birth. All women were advised to maintain a daily intake of 400 IU of vitamin D3.
The children underwent anthropometric growth assessments regularly up to age 6 years, and underwent whole-body dual-energy radiograph absorptiometry (DXA) scanning at 3 years and 6 years.
At 3 years, children of mothers who received the vitamin D supplements showed significantly higher mean total-body-less-head (TBLH) bone mineral content (BMC) compared with those who received placebo (294 g vs. 289 g) and total-body BMC (526 g vs. 514 g), respectively, after adjustment for age, sex, height, and weight.
The difference in total-body BMC was particularly evident in children of mothers who had insufficient vitamin D levels at baseline, compared with those with sufficient vitamin D levels (538 g vs. 514 g). The study also saw higher head bone mineral density (BMD) in children of mothers with insufficient vitamin D at baseline who received supplementation.
At 6 years, there still were significant differences in BMC between the supplementation and placebo groups. Children in the vitamin D group had an 8-g greater TBLH BMC compared with those in the placebo group, and a 14-g higher total BMC.
Among the children of mothers with insufficient preintervention vitamin D, there was an 18-g higher mean total BMC and 0.0125 g/cm2 greater total BMD, compared with those with sufficient vitamin D at baseline.
Overall, the children of mothers who received high-dose vitamin D supplementation had a mean 8-g higher TBLH BMC, a mean 0.023 g/cm2 higher head BMD, and a mean 12-g higher total BMC.
Dr. Brustad and associates noted that the head could represent the most sensitive compartment for intervention, because 80% of bone mineralization of the skull occurs by the age of 3 years.
The study also showed a seasonal effect, such that mothers who gave birth in winter showed the greatest effects of vitamin D supplementation on head BMC.
There was a nonsignificant trend toward a lower fracture rate among children in the supplementation group, compared with the placebo group.
“We speculate that these intervention effects could be of importance for bone health and osteoporosis risk in adult life, which is supported by our likely underpowered post hoc analysis on fracture risk, suggesting an almost 40% reduced incidence of fractures of the larger bones in the high-dose vitamin D group,” the authors wrote.
Vitamin D supplementation did not appear to affect the children’s growth. At 6 years, there were no significant differences between the two groups in body mass index, height, weight, or waist, head, and thorax circumference.
Neonatologist Carol Wagner, MD, said in an interview that the study provided an absolute reason for vitamin D supplementation during pregnancy.
“At the very least, a study like this argues for much more than is recommended by the European nutrition group or the U.S. group,” said Dr. Wagner, professor of pediatrics at the Medical University of South Carolina, Charleston. “Here you have a therapy that costs literally pennies a day, and no one should be deficient.”
She also pointed out that the study was able to show significant effects on BMC despite the fact that there would have been considerable variation in postnatal vitamin D intake from breast milk or formula.
Cristina Palacios, PhD, an associate professor in the department of dietetics and nutrition at Florida International University, Miami, said that vitamin D deficiency is increasingly prevalent worldwide, and is associated with a return of rickets – the skeletal disorder caused by vitamin D deficiency – in children.
“If women are deficient during pregnancy, providing vitamin D supplementation in pregnancy may promote bone health in their offspring,” Dr. Palacios said in an interview. “Because vitamin D is such an important component of bone metabolism, this could prevent future rickets in these children.”
Dr. Palacios coauthored a recent Cochrane review that examined the safety of high-dose vitamin D supplementation in pregnancy, and said the analysis found no evidence of safety concerns.
The study was supported by The Lundbeck Foundation, the Ministry of Health, Danish Council for Strategic Research, and the Capital Region Research Foundation. The authors declared no conflicts of interest.
SOURCE: Brustad N et al. JAMA Pediatrics 2020 Feb 24. doi: 10.1001/jamapediatrics.2019.6083.
Vitamin D supplementation during pregnancy is associated with higher bone mineral content in the offspring, even up to 6 years after birth, research suggests.
“The well-established tracking of bone mineralization from early life throughout childhood and early adulthood is a key factor for the final peak bone mass gained and the subsequent risk of fractures and osteoporosis later in life,” wrote Nicklas Brustad, MD, of the Herlev and Gentofte Hospital at the University of Copenhagen, and coauthors. Their report is in JAMA Pediatrics.This was a secondary analysis of a prospective, double-blind, randomized controlled trial of high versus standard dose vitamin D supplementation in 623 pregnant Danish women and the outcomes in their 584 children. The women were randomized either to a daily dose of 2,400 IU vitamin D3 (cholecalciferol) or matching placebo capsules from 24 weeks’ gestation until 1 week after birth. All women were advised to maintain a daily intake of 400 IU of vitamin D3.
The children underwent anthropometric growth assessments regularly up to age 6 years, and underwent whole-body dual-energy radiograph absorptiometry (DXA) scanning at 3 years and 6 years.
At 3 years, children of mothers who received the vitamin D supplements showed significantly higher mean total-body-less-head (TBLH) bone mineral content (BMC) compared with those who received placebo (294 g vs. 289 g) and total-body BMC (526 g vs. 514 g), respectively, after adjustment for age, sex, height, and weight.
The difference in total-body BMC was particularly evident in children of mothers who had insufficient vitamin D levels at baseline, compared with those with sufficient vitamin D levels (538 g vs. 514 g). The study also saw higher head bone mineral density (BMD) in children of mothers with insufficient vitamin D at baseline who received supplementation.
At 6 years, there still were significant differences in BMC between the supplementation and placebo groups. Children in the vitamin D group had an 8-g greater TBLH BMC compared with those in the placebo group, and a 14-g higher total BMC.
Among the children of mothers with insufficient preintervention vitamin D, there was an 18-g higher mean total BMC and 0.0125 g/cm2 greater total BMD, compared with those with sufficient vitamin D at baseline.
Overall, the children of mothers who received high-dose vitamin D supplementation had a mean 8-g higher TBLH BMC, a mean 0.023 g/cm2 higher head BMD, and a mean 12-g higher total BMC.
Dr. Brustad and associates noted that the head could represent the most sensitive compartment for intervention, because 80% of bone mineralization of the skull occurs by the age of 3 years.
The study also showed a seasonal effect, such that mothers who gave birth in winter showed the greatest effects of vitamin D supplementation on head BMC.
There was a nonsignificant trend toward a lower fracture rate among children in the supplementation group, compared with the placebo group.
“We speculate that these intervention effects could be of importance for bone health and osteoporosis risk in adult life, which is supported by our likely underpowered post hoc analysis on fracture risk, suggesting an almost 40% reduced incidence of fractures of the larger bones in the high-dose vitamin D group,” the authors wrote.
Vitamin D supplementation did not appear to affect the children’s growth. At 6 years, there were no significant differences between the two groups in body mass index, height, weight, or waist, head, and thorax circumference.
Neonatologist Carol Wagner, MD, said in an interview that the study provided an absolute reason for vitamin D supplementation during pregnancy.
“At the very least, a study like this argues for much more than is recommended by the European nutrition group or the U.S. group,” said Dr. Wagner, professor of pediatrics at the Medical University of South Carolina, Charleston. “Here you have a therapy that costs literally pennies a day, and no one should be deficient.”
She also pointed out that the study was able to show significant effects on BMC despite the fact that there would have been considerable variation in postnatal vitamin D intake from breast milk or formula.
Cristina Palacios, PhD, an associate professor in the department of dietetics and nutrition at Florida International University, Miami, said that vitamin D deficiency is increasingly prevalent worldwide, and is associated with a return of rickets – the skeletal disorder caused by vitamin D deficiency – in children.
“If women are deficient during pregnancy, providing vitamin D supplementation in pregnancy may promote bone health in their offspring,” Dr. Palacios said in an interview. “Because vitamin D is such an important component of bone metabolism, this could prevent future rickets in these children.”
Dr. Palacios coauthored a recent Cochrane review that examined the safety of high-dose vitamin D supplementation in pregnancy, and said the analysis found no evidence of safety concerns.
The study was supported by The Lundbeck Foundation, the Ministry of Health, Danish Council for Strategic Research, and the Capital Region Research Foundation. The authors declared no conflicts of interest.
SOURCE: Brustad N et al. JAMA Pediatrics 2020 Feb 24. doi: 10.1001/jamapediatrics.2019.6083.
FROM JAMA PEDIATRICS
June Medical Services v. Russo: Understanding this high-stakes abortion case
On March 4, 2020, the Supreme Court of the United States (SCOTUS) will hear opening arguments for June Medical Services v. Russo. (Please note that this case was originally referred to as June Medical Services v. Gee. However, Secretary Rebekah Gee resigned from her position on January 31, 2020, and was replaced by Interim Secretary Stephen Russo.) The case will examine a Louisiana law (Louisiana Act 620, or LA 620), originally passed in 2014, that requires physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.1 When LA 620 was signed into law in 2014, 5 of Louisiana’s 6 abortion clinics would not have met the standards created by this legislation and would have been forced to close, potentially leaving the vast majority of women in Louisiana without access to an abortion provider, and disproportionately impacting poor and rural women. Prior to enactment of this law, physicians at these 5 clinics attempted to obtain admitting privileges, and all were denied. The denials occurred due to two main reasons—because the providers admitted too few patients each year to qualify for hospital privileges or simply because they provided abortion care.2 Shortly after this legislation was signed into law, the Center for Reproductive Rights (CRR) challenged the law, citing the undue burden it created for patients attempting to access abortion care.
Prior case also considered question of hospital privileges for abortion providers
Interestingly, SCOTUS already has ruled on this very question. In 1992, the Court ruled in Planned Parenthood of Southeastern Pennsylvania v. Casey that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 And in 2016, when considering whether or not requiring abortion providers to obtain hospital privileges creates an undue burden in Whole Women’s Health (WWH) v. Hellerstedt, the Supreme Court’s answer was yes, it does. WWH, with legal aid from CRR, challenged Texas House Bill 2 (H.B. 2), which similar to LA 620, required abortion providers to have local admitting privileges. Based largely on the precedent set in Casey, SCOTUS ruled 5-3 in favor of WWH.
The Louisiana law currently in question was written and challenged in district court simultaneous to the Supreme Court’s review of WWH. The district court declared LA 620 invalid and permanently enjoined its enforcement, finding the law would “drastically burden women’s right to choose abortions.”4 However, the US Court of Appeals for the Fifth Circuit reviewed the case and overturned the district court decision, finding the lower court’s analysis erroneous and stating, “no clinics will likely be forced to close on account of [LA 620].” The Fifth Circuit panel ruled that, despite the precedent of WWH, LA 620 did not create an undue burden because of state-level differences in admitting privileges, demographics, and geography. They also found that only 30% of the 2 million women living in Louisiana would be impacted by the law, predominantly via longer wait times, and argued that this does not represent significant burden. The plaintiffs filed for an emergency stay with SCOTUS, who granted the stay pending a full hearing. On March 4, the Supreme Court will hear arguments to determine if the Fifth Circuit was correct in drawing a distinction between LA 620 and the SCOTUS verdict in WWH.
Targeted restrictions on abortion providers
LA 620 joins a long series of laws meant to enact targeted restrictions on abortion providers, or “TRAP” laws. TRAP laws are written to limit access to abortion under the guise of improving patient safety, despite ample evidence to the contrary, and include such various regulations as admitting privileges, facilities requirements, waiting periods, and parental or partner notification. Many such laws have been enacted in the last decade, and many struck down based on judicial precedent.
How the Supreme Court has ruled in the past
When a case is appealed to the Supreme Court, the court can either decline to hear the case, thereby leaving the lower courts’ ruling in place, or choose to hear the case in full and either affirm or overturn the lower court’s decision. After issuing a ruling in WWH, the 2016-2017 Roberts Court declined to hear challenges from other states with similarly overturned laws, leaving the laws struck down. In electing to hear June Medical Services v. Russo, the court has the opportunity to uphold or overturn the Fifth Circuit Court’s decision. However, today’s Supreme Court differs greatly from the Supreme Court in 2016.
In 2016, the court ruled 5-3 to overturn H.B. 2 in WWH shortly after the death of Justice Antonin Scalia. Scalia was replaced by Justice Neil Gorsuch, a Constitutional originalist who has never directly ruled on an abortion case.5 In 2018, Justice Anthony Kennedy, who authored the court’s majority opinion on Casey and was among the majority on WWH, retired, and was replaced by Justice Brett Kavanaugh. Kavanaugh has ruled once on the right to abortion in Garza v. Hargan in 2017, where he argued that precedent states that the government has “permissible interests in favoring fetal life…and refraining from facilitating abortion,” and that significant delay in care did not constitute undue burden.6 In regard to the 5-4 stay issued by the court in June Medical Services, Kavanaugh joined Gorsuch in voting to deny the application for stay, and was the only justice to issue an opinion alongside the ruling, arguing that because the doctors in question had not applied for and been denied admitting privileges since the WWH ruling, the case hinges on theoretical rather than demonstrable undue burden.7 Appointed by President Donald Trump, both Gorsuch and Kavanaugh are widely considered to be conservative judges, and while neither has a strong judicial record on abortion rights, both are anticipated to side with the conservative majority on the court.
The Supreme Court rarely overturns its own precedent, but concerns are high
The question of precedent will be central in SCOTUS hearing June Medical Services v. Russo so quickly after the WWH decision. Additionally, in hearing this case, the court will have the opportunity to reexamine all relevant precedent, including the Planned Parenthood of Southeastern Pennsylvania v. Casey decision and even Roe v. Wade. With a conservative court and an increasingly charged political environment, reproductive rights advocates fear that the June Medical Services v. Russo ruling may be the first step toward dismantling judicial protection of abortion rights in the United States.
If SCOTUS rules against June Medical Services, stating that admitting privileges do not cause an undue burden for women seeking to access abortion care, other states likely will introduce and enact similar legislation. These TRAP laws have the potential to limit or eliminate access to abortion for 25 million people of reproductive age. Numerous studies have demonstrated that limiting access to abortion care does not decrease the number of abortions but can result in patients using unsafe means to obtain an abortion.8
The medical community recognizes the danger of enacting restrictive legislation. The American College of Obstetricians and Gynecologists (ACOG), along with the American Medical Association, the Society of Maternal-Fetal Medicine, the Association for Sexual and Reproductive Medicine, the American Association of Family Practitioners, and many others, filed an amicus curiae in support of the June Medical Services plaintiffs.9 These brief filings are critical to ensuring the courts hear physician voices in this important legal decision, and ACOG’s briefs have been quoted in several previous Supreme Court opinions, concurrences, and dissents.
Action items
- Although June Medical Services v. Russo’s decision will not be made until early summer 2020, we can continue to use our voices and expertise to speak out against laws designed to limit access to abortion—at the state and federal levels. As women’s health clinicians, we see the impact abortion restrictions have on our patients, especially our low income and rural patients. Sharing these stories with our legislators, testifying for or against legislation, and speaking out in our communities can have a powerful impact. Check with your local ACOG chapter or with ACOG’s state and government affairs office for more information.
- Follow along with this case at SCOTUS Blog.
- Lastly, make sure you are registered to vote. We are in an election year, and using our voices in and out of the ballot box is critical. You can register here.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed February 19, 2020.
- Nash E, Donovan MK. Admitting priveleges are back at the U.S. Supreme Court with serious implications for abortion access. Guttmacher Institute. Updated December 3, 2019.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed February 20, 2020.
- June Medical Services LLC v Gee. Oyez. www.oyez.org/cases/2019/18-1323. Accessed February 20, 2020.
- Neil Gorsuch. Oyez. https://www.oyez.org/justices/neil_gorsuch. Accessed February 20, 2020.
- Judge Kavanaugh’s Judicial Record on the Right to Abortion. Center for Reproductive Rights. https://www.reproductiverights.org/sites/crr.civicactions.net/files/documents/factsheets/Judge-Kavanaugh-Judicial-Record-on-the-Right-to-Abortion2.pdf. Accessed February 20, 2020.
- Kavanaugh B. (2019, February 7). June Medical Services, L.L.C, v. Gee, 586 U.S. ____ (2019). Supreme Court of the United States. https://www.supremecourt.gov/opinions/18pdf/18a774_3ebh.pdf. Accessed February 20, 2020.
- Cohen SA. Facts and consequences: Legality, incidence and safety of abortion worldwide. November 20, 2009.
- June Medical Services, LLC v. Russo. SCOTUSblog. February 6, 2020. https://www.scotusblog.com/case-files/cases/june-medical-services-llc-v-russo/. Accessed February 20, 2020.
On March 4, 2020, the Supreme Court of the United States (SCOTUS) will hear opening arguments for June Medical Services v. Russo. (Please note that this case was originally referred to as June Medical Services v. Gee. However, Secretary Rebekah Gee resigned from her position on January 31, 2020, and was replaced by Interim Secretary Stephen Russo.) The case will examine a Louisiana law (Louisiana Act 620, or LA 620), originally passed in 2014, that requires physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.1 When LA 620 was signed into law in 2014, 5 of Louisiana’s 6 abortion clinics would not have met the standards created by this legislation and would have been forced to close, potentially leaving the vast majority of women in Louisiana without access to an abortion provider, and disproportionately impacting poor and rural women. Prior to enactment of this law, physicians at these 5 clinics attempted to obtain admitting privileges, and all were denied. The denials occurred due to two main reasons—because the providers admitted too few patients each year to qualify for hospital privileges or simply because they provided abortion care.2 Shortly after this legislation was signed into law, the Center for Reproductive Rights (CRR) challenged the law, citing the undue burden it created for patients attempting to access abortion care.
Prior case also considered question of hospital privileges for abortion providers
Interestingly, SCOTUS already has ruled on this very question. In 1992, the Court ruled in Planned Parenthood of Southeastern Pennsylvania v. Casey that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 And in 2016, when considering whether or not requiring abortion providers to obtain hospital privileges creates an undue burden in Whole Women’s Health (WWH) v. Hellerstedt, the Supreme Court’s answer was yes, it does. WWH, with legal aid from CRR, challenged Texas House Bill 2 (H.B. 2), which similar to LA 620, required abortion providers to have local admitting privileges. Based largely on the precedent set in Casey, SCOTUS ruled 5-3 in favor of WWH.
The Louisiana law currently in question was written and challenged in district court simultaneous to the Supreme Court’s review of WWH. The district court declared LA 620 invalid and permanently enjoined its enforcement, finding the law would “drastically burden women’s right to choose abortions.”4 However, the US Court of Appeals for the Fifth Circuit reviewed the case and overturned the district court decision, finding the lower court’s analysis erroneous and stating, “no clinics will likely be forced to close on account of [LA 620].” The Fifth Circuit panel ruled that, despite the precedent of WWH, LA 620 did not create an undue burden because of state-level differences in admitting privileges, demographics, and geography. They also found that only 30% of the 2 million women living in Louisiana would be impacted by the law, predominantly via longer wait times, and argued that this does not represent significant burden. The plaintiffs filed for an emergency stay with SCOTUS, who granted the stay pending a full hearing. On March 4, the Supreme Court will hear arguments to determine if the Fifth Circuit was correct in drawing a distinction between LA 620 and the SCOTUS verdict in WWH.
Targeted restrictions on abortion providers
LA 620 joins a long series of laws meant to enact targeted restrictions on abortion providers, or “TRAP” laws. TRAP laws are written to limit access to abortion under the guise of improving patient safety, despite ample evidence to the contrary, and include such various regulations as admitting privileges, facilities requirements, waiting periods, and parental or partner notification. Many such laws have been enacted in the last decade, and many struck down based on judicial precedent.
How the Supreme Court has ruled in the past
When a case is appealed to the Supreme Court, the court can either decline to hear the case, thereby leaving the lower courts’ ruling in place, or choose to hear the case in full and either affirm or overturn the lower court’s decision. After issuing a ruling in WWH, the 2016-2017 Roberts Court declined to hear challenges from other states with similarly overturned laws, leaving the laws struck down. In electing to hear June Medical Services v. Russo, the court has the opportunity to uphold or overturn the Fifth Circuit Court’s decision. However, today’s Supreme Court differs greatly from the Supreme Court in 2016.
In 2016, the court ruled 5-3 to overturn H.B. 2 in WWH shortly after the death of Justice Antonin Scalia. Scalia was replaced by Justice Neil Gorsuch, a Constitutional originalist who has never directly ruled on an abortion case.5 In 2018, Justice Anthony Kennedy, who authored the court’s majority opinion on Casey and was among the majority on WWH, retired, and was replaced by Justice Brett Kavanaugh. Kavanaugh has ruled once on the right to abortion in Garza v. Hargan in 2017, where he argued that precedent states that the government has “permissible interests in favoring fetal life…and refraining from facilitating abortion,” and that significant delay in care did not constitute undue burden.6 In regard to the 5-4 stay issued by the court in June Medical Services, Kavanaugh joined Gorsuch in voting to deny the application for stay, and was the only justice to issue an opinion alongside the ruling, arguing that because the doctors in question had not applied for and been denied admitting privileges since the WWH ruling, the case hinges on theoretical rather than demonstrable undue burden.7 Appointed by President Donald Trump, both Gorsuch and Kavanaugh are widely considered to be conservative judges, and while neither has a strong judicial record on abortion rights, both are anticipated to side with the conservative majority on the court.
The Supreme Court rarely overturns its own precedent, but concerns are high
The question of precedent will be central in SCOTUS hearing June Medical Services v. Russo so quickly after the WWH decision. Additionally, in hearing this case, the court will have the opportunity to reexamine all relevant precedent, including the Planned Parenthood of Southeastern Pennsylvania v. Casey decision and even Roe v. Wade. With a conservative court and an increasingly charged political environment, reproductive rights advocates fear that the June Medical Services v. Russo ruling may be the first step toward dismantling judicial protection of abortion rights in the United States.
If SCOTUS rules against June Medical Services, stating that admitting privileges do not cause an undue burden for women seeking to access abortion care, other states likely will introduce and enact similar legislation. These TRAP laws have the potential to limit or eliminate access to abortion for 25 million people of reproductive age. Numerous studies have demonstrated that limiting access to abortion care does not decrease the number of abortions but can result in patients using unsafe means to obtain an abortion.8
The medical community recognizes the danger of enacting restrictive legislation. The American College of Obstetricians and Gynecologists (ACOG), along with the American Medical Association, the Society of Maternal-Fetal Medicine, the Association for Sexual and Reproductive Medicine, the American Association of Family Practitioners, and many others, filed an amicus curiae in support of the June Medical Services plaintiffs.9 These brief filings are critical to ensuring the courts hear physician voices in this important legal decision, and ACOG’s briefs have been quoted in several previous Supreme Court opinions, concurrences, and dissents.
Action items
- Although June Medical Services v. Russo’s decision will not be made until early summer 2020, we can continue to use our voices and expertise to speak out against laws designed to limit access to abortion—at the state and federal levels. As women’s health clinicians, we see the impact abortion restrictions have on our patients, especially our low income and rural patients. Sharing these stories with our legislators, testifying for or against legislation, and speaking out in our communities can have a powerful impact. Check with your local ACOG chapter or with ACOG’s state and government affairs office for more information.
- Follow along with this case at SCOTUS Blog.
- Lastly, make sure you are registered to vote. We are in an election year, and using our voices in and out of the ballot box is critical. You can register here.
On March 4, 2020, the Supreme Court of the United States (SCOTUS) will hear opening arguments for June Medical Services v. Russo. (Please note that this case was originally referred to as June Medical Services v. Gee. However, Secretary Rebekah Gee resigned from her position on January 31, 2020, and was replaced by Interim Secretary Stephen Russo.) The case will examine a Louisiana law (Louisiana Act 620, or LA 620), originally passed in 2014, that requires physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.1 When LA 620 was signed into law in 2014, 5 of Louisiana’s 6 abortion clinics would not have met the standards created by this legislation and would have been forced to close, potentially leaving the vast majority of women in Louisiana without access to an abortion provider, and disproportionately impacting poor and rural women. Prior to enactment of this law, physicians at these 5 clinics attempted to obtain admitting privileges, and all were denied. The denials occurred due to two main reasons—because the providers admitted too few patients each year to qualify for hospital privileges or simply because they provided abortion care.2 Shortly after this legislation was signed into law, the Center for Reproductive Rights (CRR) challenged the law, citing the undue burden it created for patients attempting to access abortion care.
Prior case also considered question of hospital privileges for abortion providers
Interestingly, SCOTUS already has ruled on this very question. In 1992, the Court ruled in Planned Parenthood of Southeastern Pennsylvania v. Casey that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 And in 2016, when considering whether or not requiring abortion providers to obtain hospital privileges creates an undue burden in Whole Women’s Health (WWH) v. Hellerstedt, the Supreme Court’s answer was yes, it does. WWH, with legal aid from CRR, challenged Texas House Bill 2 (H.B. 2), which similar to LA 620, required abortion providers to have local admitting privileges. Based largely on the precedent set in Casey, SCOTUS ruled 5-3 in favor of WWH.
The Louisiana law currently in question was written and challenged in district court simultaneous to the Supreme Court’s review of WWH. The district court declared LA 620 invalid and permanently enjoined its enforcement, finding the law would “drastically burden women’s right to choose abortions.”4 However, the US Court of Appeals for the Fifth Circuit reviewed the case and overturned the district court decision, finding the lower court’s analysis erroneous and stating, “no clinics will likely be forced to close on account of [LA 620].” The Fifth Circuit panel ruled that, despite the precedent of WWH, LA 620 did not create an undue burden because of state-level differences in admitting privileges, demographics, and geography. They also found that only 30% of the 2 million women living in Louisiana would be impacted by the law, predominantly via longer wait times, and argued that this does not represent significant burden. The plaintiffs filed for an emergency stay with SCOTUS, who granted the stay pending a full hearing. On March 4, the Supreme Court will hear arguments to determine if the Fifth Circuit was correct in drawing a distinction between LA 620 and the SCOTUS verdict in WWH.
Targeted restrictions on abortion providers
LA 620 joins a long series of laws meant to enact targeted restrictions on abortion providers, or “TRAP” laws. TRAP laws are written to limit access to abortion under the guise of improving patient safety, despite ample evidence to the contrary, and include such various regulations as admitting privileges, facilities requirements, waiting periods, and parental or partner notification. Many such laws have been enacted in the last decade, and many struck down based on judicial precedent.
How the Supreme Court has ruled in the past
When a case is appealed to the Supreme Court, the court can either decline to hear the case, thereby leaving the lower courts’ ruling in place, or choose to hear the case in full and either affirm or overturn the lower court’s decision. After issuing a ruling in WWH, the 2016-2017 Roberts Court declined to hear challenges from other states with similarly overturned laws, leaving the laws struck down. In electing to hear June Medical Services v. Russo, the court has the opportunity to uphold or overturn the Fifth Circuit Court’s decision. However, today’s Supreme Court differs greatly from the Supreme Court in 2016.
In 2016, the court ruled 5-3 to overturn H.B. 2 in WWH shortly after the death of Justice Antonin Scalia. Scalia was replaced by Justice Neil Gorsuch, a Constitutional originalist who has never directly ruled on an abortion case.5 In 2018, Justice Anthony Kennedy, who authored the court’s majority opinion on Casey and was among the majority on WWH, retired, and was replaced by Justice Brett Kavanaugh. Kavanaugh has ruled once on the right to abortion in Garza v. Hargan in 2017, where he argued that precedent states that the government has “permissible interests in favoring fetal life…and refraining from facilitating abortion,” and that significant delay in care did not constitute undue burden.6 In regard to the 5-4 stay issued by the court in June Medical Services, Kavanaugh joined Gorsuch in voting to deny the application for stay, and was the only justice to issue an opinion alongside the ruling, arguing that because the doctors in question had not applied for and been denied admitting privileges since the WWH ruling, the case hinges on theoretical rather than demonstrable undue burden.7 Appointed by President Donald Trump, both Gorsuch and Kavanaugh are widely considered to be conservative judges, and while neither has a strong judicial record on abortion rights, both are anticipated to side with the conservative majority on the court.
The Supreme Court rarely overturns its own precedent, but concerns are high
The question of precedent will be central in SCOTUS hearing June Medical Services v. Russo so quickly after the WWH decision. Additionally, in hearing this case, the court will have the opportunity to reexamine all relevant precedent, including the Planned Parenthood of Southeastern Pennsylvania v. Casey decision and even Roe v. Wade. With a conservative court and an increasingly charged political environment, reproductive rights advocates fear that the June Medical Services v. Russo ruling may be the first step toward dismantling judicial protection of abortion rights in the United States.
If SCOTUS rules against June Medical Services, stating that admitting privileges do not cause an undue burden for women seeking to access abortion care, other states likely will introduce and enact similar legislation. These TRAP laws have the potential to limit or eliminate access to abortion for 25 million people of reproductive age. Numerous studies have demonstrated that limiting access to abortion care does not decrease the number of abortions but can result in patients using unsafe means to obtain an abortion.8
The medical community recognizes the danger of enacting restrictive legislation. The American College of Obstetricians and Gynecologists (ACOG), along with the American Medical Association, the Society of Maternal-Fetal Medicine, the Association for Sexual and Reproductive Medicine, the American Association of Family Practitioners, and many others, filed an amicus curiae in support of the June Medical Services plaintiffs.9 These brief filings are critical to ensuring the courts hear physician voices in this important legal decision, and ACOG’s briefs have been quoted in several previous Supreme Court opinions, concurrences, and dissents.
Action items
- Although June Medical Services v. Russo’s decision will not be made until early summer 2020, we can continue to use our voices and expertise to speak out against laws designed to limit access to abortion—at the state and federal levels. As women’s health clinicians, we see the impact abortion restrictions have on our patients, especially our low income and rural patients. Sharing these stories with our legislators, testifying for or against legislation, and speaking out in our communities can have a powerful impact. Check with your local ACOG chapter or with ACOG’s state and government affairs office for more information.
- Follow along with this case at SCOTUS Blog.
- Lastly, make sure you are registered to vote. We are in an election year, and using our voices in and out of the ballot box is critical. You can register here.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed February 19, 2020.
- Nash E, Donovan MK. Admitting priveleges are back at the U.S. Supreme Court with serious implications for abortion access. Guttmacher Institute. Updated December 3, 2019.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed February 20, 2020.
- June Medical Services LLC v Gee. Oyez. www.oyez.org/cases/2019/18-1323. Accessed February 20, 2020.
- Neil Gorsuch. Oyez. https://www.oyez.org/justices/neil_gorsuch. Accessed February 20, 2020.
- Judge Kavanaugh’s Judicial Record on the Right to Abortion. Center for Reproductive Rights. https://www.reproductiverights.org/sites/crr.civicactions.net/files/documents/factsheets/Judge-Kavanaugh-Judicial-Record-on-the-Right-to-Abortion2.pdf. Accessed February 20, 2020.
- Kavanaugh B. (2019, February 7). June Medical Services, L.L.C, v. Gee, 586 U.S. ____ (2019). Supreme Court of the United States. https://www.supremecourt.gov/opinions/18pdf/18a774_3ebh.pdf. Accessed February 20, 2020.
- Cohen SA. Facts and consequences: Legality, incidence and safety of abortion worldwide. November 20, 2009.
- June Medical Services, LLC v. Russo. SCOTUSblog. February 6, 2020. https://www.scotusblog.com/case-files/cases/june-medical-services-llc-v-russo/. Accessed February 20, 2020.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed February 19, 2020.
- Nash E, Donovan MK. Admitting priveleges are back at the U.S. Supreme Court with serious implications for abortion access. Guttmacher Institute. Updated December 3, 2019.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed February 20, 2020.
- June Medical Services LLC v Gee. Oyez. www.oyez.org/cases/2019/18-1323. Accessed February 20, 2020.
- Neil Gorsuch. Oyez. https://www.oyez.org/justices/neil_gorsuch. Accessed February 20, 2020.
- Judge Kavanaugh’s Judicial Record on the Right to Abortion. Center for Reproductive Rights. https://www.reproductiverights.org/sites/crr.civicactions.net/files/documents/factsheets/Judge-Kavanaugh-Judicial-Record-on-the-Right-to-Abortion2.pdf. Accessed February 20, 2020.
- Kavanaugh B. (2019, February 7). June Medical Services, L.L.C, v. Gee, 586 U.S. ____ (2019). Supreme Court of the United States. https://www.supremecourt.gov/opinions/18pdf/18a774_3ebh.pdf. Accessed February 20, 2020.
- Cohen SA. Facts and consequences: Legality, incidence and safety of abortion worldwide. November 20, 2009.
- June Medical Services, LLC v. Russo. SCOTUSblog. February 6, 2020. https://www.scotusblog.com/case-files/cases/june-medical-services-llc-v-russo/. Accessed February 20, 2020.
After gestational diabetes, longer lactation tied to lower risk for type 2
Among women with a history of gestational diabetes, a longer period of breastfeeding was associated with a lower probability of going on to develop type 2 diabetes, as well as a more favorable glucose metabolic biomarker profile. Women who breastfed for 2 years or longer had a 27% lower risk than that of those who did not breastfeed at all, even after adjustment for age, ethnicity, family history of diabetes, parity, age at first birth, smoking, diet quality, physical activity, and prepregnancy body mass index, according to findings published in Diabetes Care.
It remains to be seen if the association is causal, and if so, what mechanisms might connect breastfeeding duration to risk for type 2 diabetes, wrote study leaders Sylvia Ley, PhD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, and the Harvard T.H. Chan School of Public Health, Boston, and Cuilin Zhang, MD, PhD, of the Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and colleagues.
“It’s really nice to see this consistency and the long-term association being borne out in a very large sample of women with gestational diabetes,” Erica P. Gunderson, PhD, said in an interview about the study. Dr. Gunderson has conducted similar studies of her own, including one published in 2018 that showed an independent association between lactation and reduced diabetes risk in women (JAMA Intern Med. 2018;178:328-37). That analysis showed no sign that the presence of gestational diabetes affected the reduction of diabetes risk associated with lactation.
Dr. Gunderson noted that pregnancy is a hyperlipidemic state, with triglyceride levels sometimes doubling, likely in response to the need to support the placenta and the growing fetus. Lactation may help restore lipid levels to the prepregnancy state by redirecting lipids to breast milk. She and others are working to produce more direct evidence of metabolic changes in the postpartum period associated with lactation. “That’s where we don’t have much mechanistic evidence right now,” said Dr. Gunderson, a senior research scientist and epidemiologist at Kaiser Permanente Northern California, Oakland.
Gestational diabetes occurs in an estimated 5%-9% of pregnancies in the United States, and women who experience this complication are at greater risk of developing type 2 diabetes in the future. Findings from other studies have shown that longer lactation periods are associated with lowered risk of future type 2 disease (JAMA. 2005;294:2601-10).
In the latest study, the researchers included 4,372 women with a history of gestational diabetes, identified through the Nurses’ Health Study II. Participants were excluded if they had a history of cancer, cardiovascular disease, or multiple-birth pregnancy before the pregnancy during which they were diagnosed with gestational diabetes. In all, 873 women developed type 2 diabetes over 87,411 person-years of follow-up. The median age at gestational diabetes diagnosis was 31.8 years, and 49.8 years for diagnoses of type 2 diabetes.
After adjustment, the researchers found a steadying decline of risk for type 2 diabetes with increasing length of lactation: for up to 6 months of lactation, the hazard ratio was 1.05 (95% confidence interval, 0.82-1.34); for 6-12 months, the HR was 0.91 (95% CI, 0.71-1.15); 12-24 months, 0.84 (95% CI, 0.67-1.06); more than 24 months, 0.73 (95% CI, 0.57-0.93; P for trend = .004). Age, parity, primipara, prepregnancy body mass index, and age had no statistically significant effect modification on the association.
At a follow-up blood collection taken at median age of 58.2 years and 26.3 years after the gestational-diabetes index pregnancy, the researchers found associations between longer breastfeeding (greater than 24 months vs. 0 months) and lower hemoglobin A1c percentage (5.58 vs. 5.68; P for trend = .04), lower insulin levels (53.1 vs. 64.7 pmol/L; P for trend = .02), and lower C-peptide levels (3.42 vs. 3.88 ng/mL; P for trend = .02).
The study was supported by the National Institutes of Health. Dr. Ley was supported by a National Institute of General Medical Sciences grant from the NIH. None of the study authors reported any conflicts of interest, and neither did Dr. Gunderson.
SOURCE: Ley S et al. Diabetes Care. 2020 Feb 10. doi: 10.2337/dc19-2237.
Among women with a history of gestational diabetes, a longer period of breastfeeding was associated with a lower probability of going on to develop type 2 diabetes, as well as a more favorable glucose metabolic biomarker profile. Women who breastfed for 2 years or longer had a 27% lower risk than that of those who did not breastfeed at all, even after adjustment for age, ethnicity, family history of diabetes, parity, age at first birth, smoking, diet quality, physical activity, and prepregnancy body mass index, according to findings published in Diabetes Care.
It remains to be seen if the association is causal, and if so, what mechanisms might connect breastfeeding duration to risk for type 2 diabetes, wrote study leaders Sylvia Ley, PhD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, and the Harvard T.H. Chan School of Public Health, Boston, and Cuilin Zhang, MD, PhD, of the Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and colleagues.
“It’s really nice to see this consistency and the long-term association being borne out in a very large sample of women with gestational diabetes,” Erica P. Gunderson, PhD, said in an interview about the study. Dr. Gunderson has conducted similar studies of her own, including one published in 2018 that showed an independent association between lactation and reduced diabetes risk in women (JAMA Intern Med. 2018;178:328-37). That analysis showed no sign that the presence of gestational diabetes affected the reduction of diabetes risk associated with lactation.
Dr. Gunderson noted that pregnancy is a hyperlipidemic state, with triglyceride levels sometimes doubling, likely in response to the need to support the placenta and the growing fetus. Lactation may help restore lipid levels to the prepregnancy state by redirecting lipids to breast milk. She and others are working to produce more direct evidence of metabolic changes in the postpartum period associated with lactation. “That’s where we don’t have much mechanistic evidence right now,” said Dr. Gunderson, a senior research scientist and epidemiologist at Kaiser Permanente Northern California, Oakland.
Gestational diabetes occurs in an estimated 5%-9% of pregnancies in the United States, and women who experience this complication are at greater risk of developing type 2 diabetes in the future. Findings from other studies have shown that longer lactation periods are associated with lowered risk of future type 2 disease (JAMA. 2005;294:2601-10).
In the latest study, the researchers included 4,372 women with a history of gestational diabetes, identified through the Nurses’ Health Study II. Participants were excluded if they had a history of cancer, cardiovascular disease, or multiple-birth pregnancy before the pregnancy during which they were diagnosed with gestational diabetes. In all, 873 women developed type 2 diabetes over 87,411 person-years of follow-up. The median age at gestational diabetes diagnosis was 31.8 years, and 49.8 years for diagnoses of type 2 diabetes.
After adjustment, the researchers found a steadying decline of risk for type 2 diabetes with increasing length of lactation: for up to 6 months of lactation, the hazard ratio was 1.05 (95% confidence interval, 0.82-1.34); for 6-12 months, the HR was 0.91 (95% CI, 0.71-1.15); 12-24 months, 0.84 (95% CI, 0.67-1.06); more than 24 months, 0.73 (95% CI, 0.57-0.93; P for trend = .004). Age, parity, primipara, prepregnancy body mass index, and age had no statistically significant effect modification on the association.
At a follow-up blood collection taken at median age of 58.2 years and 26.3 years after the gestational-diabetes index pregnancy, the researchers found associations between longer breastfeeding (greater than 24 months vs. 0 months) and lower hemoglobin A1c percentage (5.58 vs. 5.68; P for trend = .04), lower insulin levels (53.1 vs. 64.7 pmol/L; P for trend = .02), and lower C-peptide levels (3.42 vs. 3.88 ng/mL; P for trend = .02).
The study was supported by the National Institutes of Health. Dr. Ley was supported by a National Institute of General Medical Sciences grant from the NIH. None of the study authors reported any conflicts of interest, and neither did Dr. Gunderson.
SOURCE: Ley S et al. Diabetes Care. 2020 Feb 10. doi: 10.2337/dc19-2237.
Among women with a history of gestational diabetes, a longer period of breastfeeding was associated with a lower probability of going on to develop type 2 diabetes, as well as a more favorable glucose metabolic biomarker profile. Women who breastfed for 2 years or longer had a 27% lower risk than that of those who did not breastfeed at all, even after adjustment for age, ethnicity, family history of diabetes, parity, age at first birth, smoking, diet quality, physical activity, and prepregnancy body mass index, according to findings published in Diabetes Care.
It remains to be seen if the association is causal, and if so, what mechanisms might connect breastfeeding duration to risk for type 2 diabetes, wrote study leaders Sylvia Ley, PhD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, and the Harvard T.H. Chan School of Public Health, Boston, and Cuilin Zhang, MD, PhD, of the Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and colleagues.
“It’s really nice to see this consistency and the long-term association being borne out in a very large sample of women with gestational diabetes,” Erica P. Gunderson, PhD, said in an interview about the study. Dr. Gunderson has conducted similar studies of her own, including one published in 2018 that showed an independent association between lactation and reduced diabetes risk in women (JAMA Intern Med. 2018;178:328-37). That analysis showed no sign that the presence of gestational diabetes affected the reduction of diabetes risk associated with lactation.
Dr. Gunderson noted that pregnancy is a hyperlipidemic state, with triglyceride levels sometimes doubling, likely in response to the need to support the placenta and the growing fetus. Lactation may help restore lipid levels to the prepregnancy state by redirecting lipids to breast milk. She and others are working to produce more direct evidence of metabolic changes in the postpartum period associated with lactation. “That’s where we don’t have much mechanistic evidence right now,” said Dr. Gunderson, a senior research scientist and epidemiologist at Kaiser Permanente Northern California, Oakland.
Gestational diabetes occurs in an estimated 5%-9% of pregnancies in the United States, and women who experience this complication are at greater risk of developing type 2 diabetes in the future. Findings from other studies have shown that longer lactation periods are associated with lowered risk of future type 2 disease (JAMA. 2005;294:2601-10).
In the latest study, the researchers included 4,372 women with a history of gestational diabetes, identified through the Nurses’ Health Study II. Participants were excluded if they had a history of cancer, cardiovascular disease, or multiple-birth pregnancy before the pregnancy during which they were diagnosed with gestational diabetes. In all, 873 women developed type 2 diabetes over 87,411 person-years of follow-up. The median age at gestational diabetes diagnosis was 31.8 years, and 49.8 years for diagnoses of type 2 diabetes.
After adjustment, the researchers found a steadying decline of risk for type 2 diabetes with increasing length of lactation: for up to 6 months of lactation, the hazard ratio was 1.05 (95% confidence interval, 0.82-1.34); for 6-12 months, the HR was 0.91 (95% CI, 0.71-1.15); 12-24 months, 0.84 (95% CI, 0.67-1.06); more than 24 months, 0.73 (95% CI, 0.57-0.93; P for trend = .004). Age, parity, primipara, prepregnancy body mass index, and age had no statistically significant effect modification on the association.
At a follow-up blood collection taken at median age of 58.2 years and 26.3 years after the gestational-diabetes index pregnancy, the researchers found associations between longer breastfeeding (greater than 24 months vs. 0 months) and lower hemoglobin A1c percentage (5.58 vs. 5.68; P for trend = .04), lower insulin levels (53.1 vs. 64.7 pmol/L; P for trend = .02), and lower C-peptide levels (3.42 vs. 3.88 ng/mL; P for trend = .02).
The study was supported by the National Institutes of Health. Dr. Ley was supported by a National Institute of General Medical Sciences grant from the NIH. None of the study authors reported any conflicts of interest, and neither did Dr. Gunderson.
SOURCE: Ley S et al. Diabetes Care. 2020 Feb 10. doi: 10.2337/dc19-2237.
FROM DIABETES CARE
Newborn transfer may not reflect true rate of complications
Neonatal transfer was the factor most often associated with unexpected, severe complications at birth, particularly at hospitals that had the highest rates of complications, according to a cross-sectional study published online in JAMA Network Open (2020;3[2]:e1919498).
Mark A. Clapp, MD, MPH, of Massachusetts General Hospital in Boston, and colleagues wrote. “Thus, if this metric is to be used in its current form, it would appear that accreditors, regulatory bodies, and payers should consider adjusting for or stratifying by a hospital’s level of neonatal care to avoid disincentivizing against appropriate transfers.”
The Joint Commission recently included unexpected complications in term newborns as a marker of quality of obstetric care, but it does not currently recommend any risk adjustment for the metric. The authors aimed to learn which factors regarding patients and hospitals were associated with such complications. Severe, unexpected newborn complications include death, seizure, use of assisted ventilation for at least 6 hours, transfer to another facility, or a 5-minute Apgar score of 3 or less.
“This measure has been proposed to serve as a balancing measure to maternal metrics, such as the rate of nulliparous, term, singleton, vertex-presenting cesarean deliveries,” the authors explained.
This study was supported by a Health Policy Award from the Society for Maternal-Fetal Medicine. The authors reported no relevant financial disclosures.
This story first appeared on Medscape.
Neonatal transfer was the factor most often associated with unexpected, severe complications at birth, particularly at hospitals that had the highest rates of complications, according to a cross-sectional study published online in JAMA Network Open (2020;3[2]:e1919498).
Mark A. Clapp, MD, MPH, of Massachusetts General Hospital in Boston, and colleagues wrote. “Thus, if this metric is to be used in its current form, it would appear that accreditors, regulatory bodies, and payers should consider adjusting for or stratifying by a hospital’s level of neonatal care to avoid disincentivizing against appropriate transfers.”
The Joint Commission recently included unexpected complications in term newborns as a marker of quality of obstetric care, but it does not currently recommend any risk adjustment for the metric. The authors aimed to learn which factors regarding patients and hospitals were associated with such complications. Severe, unexpected newborn complications include death, seizure, use of assisted ventilation for at least 6 hours, transfer to another facility, or a 5-minute Apgar score of 3 or less.
“This measure has been proposed to serve as a balancing measure to maternal metrics, such as the rate of nulliparous, term, singleton, vertex-presenting cesarean deliveries,” the authors explained.
This study was supported by a Health Policy Award from the Society for Maternal-Fetal Medicine. The authors reported no relevant financial disclosures.
This story first appeared on Medscape.
Neonatal transfer was the factor most often associated with unexpected, severe complications at birth, particularly at hospitals that had the highest rates of complications, according to a cross-sectional study published online in JAMA Network Open (2020;3[2]:e1919498).
Mark A. Clapp, MD, MPH, of Massachusetts General Hospital in Boston, and colleagues wrote. “Thus, if this metric is to be used in its current form, it would appear that accreditors, regulatory bodies, and payers should consider adjusting for or stratifying by a hospital’s level of neonatal care to avoid disincentivizing against appropriate transfers.”
The Joint Commission recently included unexpected complications in term newborns as a marker of quality of obstetric care, but it does not currently recommend any risk adjustment for the metric. The authors aimed to learn which factors regarding patients and hospitals were associated with such complications. Severe, unexpected newborn complications include death, seizure, use of assisted ventilation for at least 6 hours, transfer to another facility, or a 5-minute Apgar score of 3 or less.
“This measure has been proposed to serve as a balancing measure to maternal metrics, such as the rate of nulliparous, term, singleton, vertex-presenting cesarean deliveries,” the authors explained.
This study was supported by a Health Policy Award from the Society for Maternal-Fetal Medicine. The authors reported no relevant financial disclosures.
This story first appeared on Medscape.
FROM JAMA NETWORK OPEN
ERAS for cesarean delivery: Intraoperative care



2020 Update on fertility
Although we are not able to cover all of the important developments in fertility medicine over the past year, there were 3 important articles published in the past 12 months that we highlight here. First, we discuss an American College of Obstetricians and Gynecologists (ACOG) committee opinion on genetic carrier screening that was reaffirmed in 2019. Second, we explore an interesting retrospective analysis of time-lapse videos and clinical outcomes of more than 10,000 embryos from 8 IVF clinics, across 4 countries. The authors assessed whether a deep learning model could predict the probability of pregnancy with fetal heart from time-lapse videos in the hopes that their research can improve prioritization of the most viable embryo for single embryo transfer. Last, we consider a review of the data on obstetric and reproductive health effects of preconception and prenatal exposure to several environmental toxicants, including heavy metals, endocrine-disrupting chemicals, pesticides, and air pollution.
Preconception genetic carrier screening: Standardize your counseling approach
American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 690: carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40.
With the rapid development of advanced and high throughput platforms for DNA sequencing in the past several years, the cost of genetic testing has decreased dramatically. Women's health care providers in general, and fertility specialists in particular, are uniquely positioned to take advantage of these novel and yet affordable technologies by counseling prospective parents during the preconception counseling, or early prenatal period, about the availability of genetic carrier screening and its potential to provide actionable information in a timely manner. The ultimate objective of genetic carrier screening is to enable individuals to make an informed decision regarding their reproductive choices based on their personal values. In a study by Larsen and colleagues, the uptake of genetic carrier screening was significantly higher when offered in the preconception period (68.7%), compared with during pregnancy (35.1%), which highlights the significance of early counseling.1
Based on the Centers for Disease Control and Prevention's Birth/Infant Death Data set, birth defects affect 1 in every 33 (about 3%) of all babies born in the United States each year and account for 20% of infant mortality.2 About 20% of birth defects are caused by single-gene (monogenic) disorders, and although some of these are due to dominant conditions or de novo mutations, a significant proportion are due to autosomal recessive, or X-chromosome linked conditions that are commonly assessed by genetic carrier screening.
ACOG published a committee opinion on "Carrier Screening in the Age of Genomic Medicine" in March 2017, which was reaffirmed in 2019.3
Residual risk. Several points discussed in this document are of paramount importance, including the need for pretest and posttest counseling and consent, as well as a discussion of "residual risk." Newer platforms employ sequencing techniques that potentially can detect most, if not all, of the disease-causing variants in the tested genes, such as the gene for cystic fibrosis and, therefore, have a higher detection rate compared with the older PCR-based techniques for a limited number of specific mutations included in the panel. Due to a variety of technical and biological limitations, however, such as allelic dropouts and the occurrence of de novo mutations, the detection rate is not 100%; there is always a residual risk that needs to be estimated and provided to individuals based on the existing knowledge on frequency of gene, penetrance of phenotype, and prevalence of condition in the general and specific ethnic populations.
Continue to: Expanded vs panethnic screening...
Expanded vs panethnic screening. Furthermore, although sequencing technology has made "expanded carrier screening" for several hundred conditions, simultaneous to and independent of ethnicity and family history, more easily available and affordable, ethnic-specific and panethnic screening for a more limited number of conditions are still acceptable approaches. Having said this, when the first partner screened is identified to be a carrier, his/her reproductive partners must be offered next-generation sequencing to identify less common disease-causing variants.4
A cautionary point to consider when expanded carrier screening panels are requested is the significant variability among commercial laboratories with regard to the conditions included in their panels. In addition, consider the absence of a well-defined or predictable phenotype for some of the included conditions.
Perhaps the most important matter when it comes to genetic carrier screening is to have a standard counseling approach that is persistently followed and offers the opportunity for individuals to know about their genetic testing options and available reproductive choices, including the use of donor gametes, preimplantation genetic testing for monogenic disease (PGT-M, formerly known as preimplantation genetic diagnosis, or PGD), prenatal testing, and pregnancy management options. For couples and/or individuals who decide to proceed with an affected pregnancy, earlier diagnosis can assist with postnatal management.
Medicolegal responsibility. Genetic carrier screening also is of specific relevance to the field of fertility medicine and assisted reproductive technology (ART) as a potential liability issue. Couples and individuals who are undergoing fertility treatment with in vitro fertilization (IVF) for a variety of medical or personal reasons are a specific group that certainly should be offered genetic carrier screening, as they have the option of "adding on" PGT-M (PGD) to their existing treatment plan at a fraction of the cost and treatment burden that would have otherwise been needed if they were not undergoing IVF. After counseling, some individuals and couples may ultimately opt out of genetic carrier screening. The counseling discussion needs to be clearly documented in the medical chart.
The preconception period is the perfect time to have a discussion about genetic carrier screening; it offers the opportunity for timely interventions if desired by the couples or individuals.
Continue to: Artificial intelligence and embryo selection...
Artificial intelligence and embryo selection
With continued improvements in embryo culture conditions and cryopreservation technology, there has been a tremendous amount of interest in developing better methods for embryo selection. These efforts are aimed at encouraging elective single embryo transfer (eSET) for women of all ages, thereby lowering the risk of multiple pregnancy and its associated adverse neonatal and obstetric outcomes—without compromising the pregnancy rates per transfer or lengthening the time to pregnancy.
One of the most extensively studied methods for this purpose is preimplantation genetic testing for aneuploidy (PGT-A, formerly known as PGS), but emerging data from large multicenter randomized clinical trials (RCTs) have again cast significant doubt on PGT-A's efficacy and utility.5 Meanwhile, alternative methods for embryo selection are currently under investigation, including noninvasive PGT-A and morphokinetic assessment of embryo development via analysis of images obtained by time-lapse imaging.
The potential of time-lapse imaging
Despite the initial promising results from time-lapse imaging, subsequent RCTs have not shown a significant clinical benefit.6 However, these early methods of morphokinetic assessment are mainly dependent on the embryologists' subjective assessment of individual static frames and "annotation" of observed spatial and temporal features of embryo development. In addition to being a very time-consuming task, this process is subject to significant interobserver and intraobserver variability.
Considering these limitations, even machine-based algorithms that incorporate these annotations along with such other clinical variables as parental age and prior obstetric history, have a low predictive power for the outcome of embryo transfer, with an area under the curve (AUC) of the ROC curve of 0.65 to 0.74. (An AUC of 0.5 represents completely random prediction and an AUC of 1.0 suggests perfect prediction.)7
A recent study by Tran and colleagues has employed a deep learning (neural network) model to analyze the entire raw time-lapse videos in an automated manner without prior annotation by embryologists. After analysis of 10,638 embryos from 8 different IVF clinics in 4 different countries, they have reported an AUC of 0.93 (95% confidence interval, 0.92-0.94) for prediction of fetal heart rate activity detected at 7 weeks of gestation or beyond. Although these data are very preliminary and have not yet been validated prospectively in larger datasets for live birth, it may herald the beginning of a new era for the automation and standardization of embryo assessment with artificial intelligence—similar to the rapidly increasing role of facial recognition technology for various applications.
Improved standardization of noninvasive embryo selection with growing use of artificial intelligence is a promising new tool to improve the safety and efficacy of ART.
Continue to: Environmental toxicants: The hidden danger...
Environmental toxicants: The hidden danger
Segal TR, Giudice LC. Before the beginning: environmental exposures and reproductive and obstetrical outcomes. Fertil Steril. 2019;112:613-621.
We receive news daily about the existential risk to humans of climate change. However, a risk that is likely as serious goes almost unseen by the public and most health care providers. That risk is environmental toxicants.8
More than 80,000 chemicals are registered in the United States, most in the last 75 years. These chemicals are ubiquitous. All of us are continuously exposed to and suffused with these toxicants and their metabolites. Air pollution adds insult to injury. Since this exposure has especially significant implications for fertility, infertility, pregnancy, perinatal health, childhood development, adult diseases, and later generational reproduction, it is imperative that reproductive health professionals take responsibility for helping mitigate this environmental crisis.
The problem is exceptionally complicated
The risks posed by environmental toxicants are much less visible than those for climate change, so the public, policymakers, and providers are largely unaware or may even seem uncaring. Few health professionals have sufficient knowledge to deliver care in this area, know which questions to ask, or have adequate information/medical record tools to assist them in care—and what are the possible interventions?
Addressing risk posed by individual toxicants
Addressing the problem clinically requires asking patients questions about exposure and recommending interventions. Toxicant chemicals include the neurotoxin mercury, which can be addressed by limiting intake of fish, especially certain types.
Lead was used before 1978 in paint, it also was used in gas and in water pipes. People living in older homes may be exposed, as well as those in occupations exposed to lead. Others with lead exposure risk include immigrants from areas without lead regulations and people using pica- or lead-glazed pottery. Lead exposure has been associated with multiple pregnancy complications and permanently impaired intellectual development in children. If lead testing reveals high levels, chelation therapy can help.
Cadmium is a heavy metal used in rechargeable batteries, paint pigment, and plastic production. Exposure results from food intake, smoking, and second-hand smoke. Cadmium accumulates in the liver, kidneys, testes, ovaries, and placenta. Exposure causes itai-itai disease, which is characterized by osteomalacia and renal tubular dysfunction as well as epigenetic changes in placental DNA and damage to the reproductive system. Eating organic food and reducing industrial exposure to cadmium are preventive strategies.
Pesticides are ubiquitous, with 90% of the US population having detectable levels. Exposure during the preconception period can lead to intrauterine growth restriction, low birth weight, subsequent cancers, and other problems. Eating organic food can reduce risk, as can frequent hand washing when exposed to pesticides, using protective gear, and removing shoes in the home.
Endocrine-disrupting chemicals (EDCs) are chemicals that can mimic or block endogenous hormones, which leads to adverse health outcomes. In addition to heavy metals, 3 important EDCs are bisphenol A (BPA), phthalates, and polybrominated diethyl ethers (PBDEs). Exposure is ubiquitous from industrial food processing, personal care products, cosmetics, and dust. Phthalates and BPA have short half-lives of hours to days, while PBDEs can persist in adipose tissue for months. Abnormal urogenital and neurologic development and thyroid disruption can result. Eating organic food, eating at home, and decreasing processed food intake can reduce exposure.
BPA is used in plastics, canned food liners, cash register receipts, and epoxy resins. Exposure is through inhalation, ingestion, and dermal absorption and affects semen quality, fertilization, placentation, and early reproduction. Limiting the use of plastic containers, not microwaving food in plastic, and avoiding thermal paper cash register receipts can reduce exposure.
Phthalates are synthetically derived and used as plasticizers in personal and medical products. The major source of phthalate exposure is food; exposure causes sperm, egg, and DNA damage. Phthalate avoidance involves replacing plastic bottles with glass or stainless steel, avoiding reheating food in plastic containers, and choosing "fragrance free" products.
PBDEs are used in flame retardants on upholstery, textiles, carpeting, and some electronics. Most PBDEs have been replaced by alternatives; however, their half-life is up to 12 years. Complications caused by PBDEs include thyroid disruption, resulting in abnormal fetal brain development. Avoiding dust and furniture that contain PBDEs, as well as hand washing, reduces exposure risk.
Air pollutants are associated with adverse obstetric outcomes and lower cognitive function in children. Avoiding areas with heavy traffic, staying indoors when air is heavily polluted, and using a HEPA filter in the home can reduce chemicals from air pollution.
Recommendations
The magnitude of the problem that environmental toxicant exposure creates requires health care providers to take action. The table in the publication by Segal and Giudice can be used as a tool that patients can answer first themselves before review by their provider.2 It can be added to your electronic health record and/or patient portal. Even making general comments to raise awareness, asking questions regarding exposure, and making recommendations can be helpful (TABLES 1 and 2). When possible, we also should advocate for public awareness and policy changes that address this significant health issue.
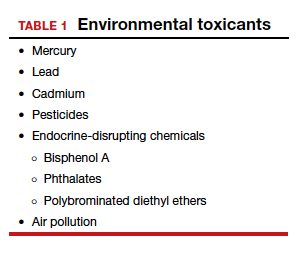
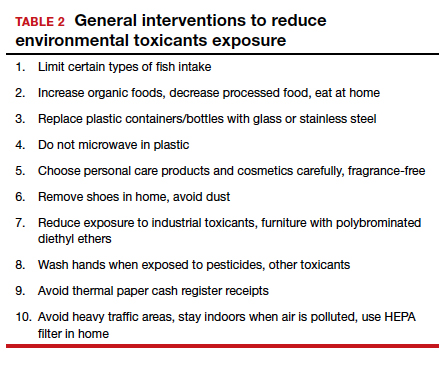
Environmental toxicants are a significant health problem that can be effectively mitigated through patient questions and recommended interventions.
- Larsen D, Ma J, Strassberg M, et al. The uptake of pan-ethnic expanded carrier screening is higher when offered during preconception or early prenatal genetic counseling. Prenat Diagn. 2019;39:319-323.
- Matthews TJ, MacDorman MF, Thoma ME. Infant Mortality Statistics From the 2013 Period Linked Birth/Infant Death Data Set. Natl Vital Stat Rep. 2015;64:1-30.
- American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 690: carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40.
- Gregg AR, Edwards JG. Prenatal genetic carrier screening in the genomic age. Semin Perinatol. 2018;42:303-306.
- Munné S, Kaplan B, Frattarelli JL, et al; STAR Study Group. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112:1071-1079. e7.
- Goodman LR, Goldberg J, Falcone T, et al. Does the addition of time-lapse morphokinetics in the selection of embryos for transfer improve pregnancy rates? A randomized controlled trial. Fertil Steril. 2016;105:275-285.e10.
- Blank C, Wildeboer RR, DeCroo I, et al. Prediction of implantation after blastocyst transfer in in vitro fertilization: a machine-learning perspective. Fertil Steril. 2019;111:318- 326.
- The American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women; American Society for Reproductive Medicine Practice Committee; The University of California, San Francisco Program on Reproductive Health and the Environment. ACOG Committee Opinion No. 575. Exposure to environmental toxic agents. Fertil Steril. 2013;100:931-934.
Although we are not able to cover all of the important developments in fertility medicine over the past year, there were 3 important articles published in the past 12 months that we highlight here. First, we discuss an American College of Obstetricians and Gynecologists (ACOG) committee opinion on genetic carrier screening that was reaffirmed in 2019. Second, we explore an interesting retrospective analysis of time-lapse videos and clinical outcomes of more than 10,000 embryos from 8 IVF clinics, across 4 countries. The authors assessed whether a deep learning model could predict the probability of pregnancy with fetal heart from time-lapse videos in the hopes that their research can improve prioritization of the most viable embryo for single embryo transfer. Last, we consider a review of the data on obstetric and reproductive health effects of preconception and prenatal exposure to several environmental toxicants, including heavy metals, endocrine-disrupting chemicals, pesticides, and air pollution.
Preconception genetic carrier screening: Standardize your counseling approach
American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 690: carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40.
With the rapid development of advanced and high throughput platforms for DNA sequencing in the past several years, the cost of genetic testing has decreased dramatically. Women's health care providers in general, and fertility specialists in particular, are uniquely positioned to take advantage of these novel and yet affordable technologies by counseling prospective parents during the preconception counseling, or early prenatal period, about the availability of genetic carrier screening and its potential to provide actionable information in a timely manner. The ultimate objective of genetic carrier screening is to enable individuals to make an informed decision regarding their reproductive choices based on their personal values. In a study by Larsen and colleagues, the uptake of genetic carrier screening was significantly higher when offered in the preconception period (68.7%), compared with during pregnancy (35.1%), which highlights the significance of early counseling.1
Based on the Centers for Disease Control and Prevention's Birth/Infant Death Data set, birth defects affect 1 in every 33 (about 3%) of all babies born in the United States each year and account for 20% of infant mortality.2 About 20% of birth defects are caused by single-gene (monogenic) disorders, and although some of these are due to dominant conditions or de novo mutations, a significant proportion are due to autosomal recessive, or X-chromosome linked conditions that are commonly assessed by genetic carrier screening.
ACOG published a committee opinion on "Carrier Screening in the Age of Genomic Medicine" in March 2017, which was reaffirmed in 2019.3
Residual risk. Several points discussed in this document are of paramount importance, including the need for pretest and posttest counseling and consent, as well as a discussion of "residual risk." Newer platforms employ sequencing techniques that potentially can detect most, if not all, of the disease-causing variants in the tested genes, such as the gene for cystic fibrosis and, therefore, have a higher detection rate compared with the older PCR-based techniques for a limited number of specific mutations included in the panel. Due to a variety of technical and biological limitations, however, such as allelic dropouts and the occurrence of de novo mutations, the detection rate is not 100%; there is always a residual risk that needs to be estimated and provided to individuals based on the existing knowledge on frequency of gene, penetrance of phenotype, and prevalence of condition in the general and specific ethnic populations.
Continue to: Expanded vs panethnic screening...
Expanded vs panethnic screening. Furthermore, although sequencing technology has made "expanded carrier screening" for several hundred conditions, simultaneous to and independent of ethnicity and family history, more easily available and affordable, ethnic-specific and panethnic screening for a more limited number of conditions are still acceptable approaches. Having said this, when the first partner screened is identified to be a carrier, his/her reproductive partners must be offered next-generation sequencing to identify less common disease-causing variants.4
A cautionary point to consider when expanded carrier screening panels are requested is the significant variability among commercial laboratories with regard to the conditions included in their panels. In addition, consider the absence of a well-defined or predictable phenotype for some of the included conditions.
Perhaps the most important matter when it comes to genetic carrier screening is to have a standard counseling approach that is persistently followed and offers the opportunity for individuals to know about their genetic testing options and available reproductive choices, including the use of donor gametes, preimplantation genetic testing for monogenic disease (PGT-M, formerly known as preimplantation genetic diagnosis, or PGD), prenatal testing, and pregnancy management options. For couples and/or individuals who decide to proceed with an affected pregnancy, earlier diagnosis can assist with postnatal management.
Medicolegal responsibility. Genetic carrier screening also is of specific relevance to the field of fertility medicine and assisted reproductive technology (ART) as a potential liability issue. Couples and individuals who are undergoing fertility treatment with in vitro fertilization (IVF) for a variety of medical or personal reasons are a specific group that certainly should be offered genetic carrier screening, as they have the option of "adding on" PGT-M (PGD) to their existing treatment plan at a fraction of the cost and treatment burden that would have otherwise been needed if they were not undergoing IVF. After counseling, some individuals and couples may ultimately opt out of genetic carrier screening. The counseling discussion needs to be clearly documented in the medical chart.
The preconception period is the perfect time to have a discussion about genetic carrier screening; it offers the opportunity for timely interventions if desired by the couples or individuals.
Continue to: Artificial intelligence and embryo selection...
Artificial intelligence and embryo selection
With continued improvements in embryo culture conditions and cryopreservation technology, there has been a tremendous amount of interest in developing better methods for embryo selection. These efforts are aimed at encouraging elective single embryo transfer (eSET) for women of all ages, thereby lowering the risk of multiple pregnancy and its associated adverse neonatal and obstetric outcomes—without compromising the pregnancy rates per transfer or lengthening the time to pregnancy.
One of the most extensively studied methods for this purpose is preimplantation genetic testing for aneuploidy (PGT-A, formerly known as PGS), but emerging data from large multicenter randomized clinical trials (RCTs) have again cast significant doubt on PGT-A's efficacy and utility.5 Meanwhile, alternative methods for embryo selection are currently under investigation, including noninvasive PGT-A and morphokinetic assessment of embryo development via analysis of images obtained by time-lapse imaging.
The potential of time-lapse imaging
Despite the initial promising results from time-lapse imaging, subsequent RCTs have not shown a significant clinical benefit.6 However, these early methods of morphokinetic assessment are mainly dependent on the embryologists' subjective assessment of individual static frames and "annotation" of observed spatial and temporal features of embryo development. In addition to being a very time-consuming task, this process is subject to significant interobserver and intraobserver variability.
Considering these limitations, even machine-based algorithms that incorporate these annotations along with such other clinical variables as parental age and prior obstetric history, have a low predictive power for the outcome of embryo transfer, with an area under the curve (AUC) of the ROC curve of 0.65 to 0.74. (An AUC of 0.5 represents completely random prediction and an AUC of 1.0 suggests perfect prediction.)7
A recent study by Tran and colleagues has employed a deep learning (neural network) model to analyze the entire raw time-lapse videos in an automated manner without prior annotation by embryologists. After analysis of 10,638 embryos from 8 different IVF clinics in 4 different countries, they have reported an AUC of 0.93 (95% confidence interval, 0.92-0.94) for prediction of fetal heart rate activity detected at 7 weeks of gestation or beyond. Although these data are very preliminary and have not yet been validated prospectively in larger datasets for live birth, it may herald the beginning of a new era for the automation and standardization of embryo assessment with artificial intelligence—similar to the rapidly increasing role of facial recognition technology for various applications.
Improved standardization of noninvasive embryo selection with growing use of artificial intelligence is a promising new tool to improve the safety and efficacy of ART.
Continue to: Environmental toxicants: The hidden danger...
Environmental toxicants: The hidden danger
Segal TR, Giudice LC. Before the beginning: environmental exposures and reproductive and obstetrical outcomes. Fertil Steril. 2019;112:613-621.
We receive news daily about the existential risk to humans of climate change. However, a risk that is likely as serious goes almost unseen by the public and most health care providers. That risk is environmental toxicants.8
More than 80,000 chemicals are registered in the United States, most in the last 75 years. These chemicals are ubiquitous. All of us are continuously exposed to and suffused with these toxicants and their metabolites. Air pollution adds insult to injury. Since this exposure has especially significant implications for fertility, infertility, pregnancy, perinatal health, childhood development, adult diseases, and later generational reproduction, it is imperative that reproductive health professionals take responsibility for helping mitigate this environmental crisis.
The problem is exceptionally complicated
The risks posed by environmental toxicants are much less visible than those for climate change, so the public, policymakers, and providers are largely unaware or may even seem uncaring. Few health professionals have sufficient knowledge to deliver care in this area, know which questions to ask, or have adequate information/medical record tools to assist them in care—and what are the possible interventions?
Addressing risk posed by individual toxicants
Addressing the problem clinically requires asking patients questions about exposure and recommending interventions. Toxicant chemicals include the neurotoxin mercury, which can be addressed by limiting intake of fish, especially certain types.
Lead was used before 1978 in paint, it also was used in gas and in water pipes. People living in older homes may be exposed, as well as those in occupations exposed to lead. Others with lead exposure risk include immigrants from areas without lead regulations and people using pica- or lead-glazed pottery. Lead exposure has been associated with multiple pregnancy complications and permanently impaired intellectual development in children. If lead testing reveals high levels, chelation therapy can help.
Cadmium is a heavy metal used in rechargeable batteries, paint pigment, and plastic production. Exposure results from food intake, smoking, and second-hand smoke. Cadmium accumulates in the liver, kidneys, testes, ovaries, and placenta. Exposure causes itai-itai disease, which is characterized by osteomalacia and renal tubular dysfunction as well as epigenetic changes in placental DNA and damage to the reproductive system. Eating organic food and reducing industrial exposure to cadmium are preventive strategies.
Pesticides are ubiquitous, with 90% of the US population having detectable levels. Exposure during the preconception period can lead to intrauterine growth restriction, low birth weight, subsequent cancers, and other problems. Eating organic food can reduce risk, as can frequent hand washing when exposed to pesticides, using protective gear, and removing shoes in the home.
Endocrine-disrupting chemicals (EDCs) are chemicals that can mimic or block endogenous hormones, which leads to adverse health outcomes. In addition to heavy metals, 3 important EDCs are bisphenol A (BPA), phthalates, and polybrominated diethyl ethers (PBDEs). Exposure is ubiquitous from industrial food processing, personal care products, cosmetics, and dust. Phthalates and BPA have short half-lives of hours to days, while PBDEs can persist in adipose tissue for months. Abnormal urogenital and neurologic development and thyroid disruption can result. Eating organic food, eating at home, and decreasing processed food intake can reduce exposure.
BPA is used in plastics, canned food liners, cash register receipts, and epoxy resins. Exposure is through inhalation, ingestion, and dermal absorption and affects semen quality, fertilization, placentation, and early reproduction. Limiting the use of plastic containers, not microwaving food in plastic, and avoiding thermal paper cash register receipts can reduce exposure.
Phthalates are synthetically derived and used as plasticizers in personal and medical products. The major source of phthalate exposure is food; exposure causes sperm, egg, and DNA damage. Phthalate avoidance involves replacing plastic bottles with glass or stainless steel, avoiding reheating food in plastic containers, and choosing "fragrance free" products.
PBDEs are used in flame retardants on upholstery, textiles, carpeting, and some electronics. Most PBDEs have been replaced by alternatives; however, their half-life is up to 12 years. Complications caused by PBDEs include thyroid disruption, resulting in abnormal fetal brain development. Avoiding dust and furniture that contain PBDEs, as well as hand washing, reduces exposure risk.
Air pollutants are associated with adverse obstetric outcomes and lower cognitive function in children. Avoiding areas with heavy traffic, staying indoors when air is heavily polluted, and using a HEPA filter in the home can reduce chemicals from air pollution.
Recommendations
The magnitude of the problem that environmental toxicant exposure creates requires health care providers to take action. The table in the publication by Segal and Giudice can be used as a tool that patients can answer first themselves before review by their provider.2 It can be added to your electronic health record and/or patient portal. Even making general comments to raise awareness, asking questions regarding exposure, and making recommendations can be helpful (TABLES 1 and 2). When possible, we also should advocate for public awareness and policy changes that address this significant health issue.
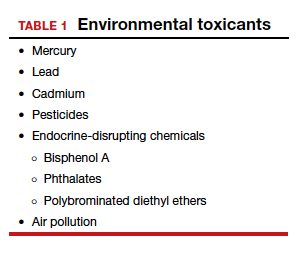
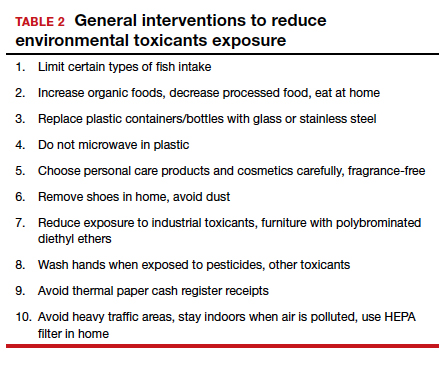
Environmental toxicants are a significant health problem that can be effectively mitigated through patient questions and recommended interventions.
Although we are not able to cover all of the important developments in fertility medicine over the past year, there were 3 important articles published in the past 12 months that we highlight here. First, we discuss an American College of Obstetricians and Gynecologists (ACOG) committee opinion on genetic carrier screening that was reaffirmed in 2019. Second, we explore an interesting retrospective analysis of time-lapse videos and clinical outcomes of more than 10,000 embryos from 8 IVF clinics, across 4 countries. The authors assessed whether a deep learning model could predict the probability of pregnancy with fetal heart from time-lapse videos in the hopes that their research can improve prioritization of the most viable embryo for single embryo transfer. Last, we consider a review of the data on obstetric and reproductive health effects of preconception and prenatal exposure to several environmental toxicants, including heavy metals, endocrine-disrupting chemicals, pesticides, and air pollution.
Preconception genetic carrier screening: Standardize your counseling approach
American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 690: carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40.
With the rapid development of advanced and high throughput platforms for DNA sequencing in the past several years, the cost of genetic testing has decreased dramatically. Women's health care providers in general, and fertility specialists in particular, are uniquely positioned to take advantage of these novel and yet affordable technologies by counseling prospective parents during the preconception counseling, or early prenatal period, about the availability of genetic carrier screening and its potential to provide actionable information in a timely manner. The ultimate objective of genetic carrier screening is to enable individuals to make an informed decision regarding their reproductive choices based on their personal values. In a study by Larsen and colleagues, the uptake of genetic carrier screening was significantly higher when offered in the preconception period (68.7%), compared with during pregnancy (35.1%), which highlights the significance of early counseling.1
Based on the Centers for Disease Control and Prevention's Birth/Infant Death Data set, birth defects affect 1 in every 33 (about 3%) of all babies born in the United States each year and account for 20% of infant mortality.2 About 20% of birth defects are caused by single-gene (monogenic) disorders, and although some of these are due to dominant conditions or de novo mutations, a significant proportion are due to autosomal recessive, or X-chromosome linked conditions that are commonly assessed by genetic carrier screening.
ACOG published a committee opinion on "Carrier Screening in the Age of Genomic Medicine" in March 2017, which was reaffirmed in 2019.3
Residual risk. Several points discussed in this document are of paramount importance, including the need for pretest and posttest counseling and consent, as well as a discussion of "residual risk." Newer platforms employ sequencing techniques that potentially can detect most, if not all, of the disease-causing variants in the tested genes, such as the gene for cystic fibrosis and, therefore, have a higher detection rate compared with the older PCR-based techniques for a limited number of specific mutations included in the panel. Due to a variety of technical and biological limitations, however, such as allelic dropouts and the occurrence of de novo mutations, the detection rate is not 100%; there is always a residual risk that needs to be estimated and provided to individuals based on the existing knowledge on frequency of gene, penetrance of phenotype, and prevalence of condition in the general and specific ethnic populations.
Continue to: Expanded vs panethnic screening...
Expanded vs panethnic screening. Furthermore, although sequencing technology has made "expanded carrier screening" for several hundred conditions, simultaneous to and independent of ethnicity and family history, more easily available and affordable, ethnic-specific and panethnic screening for a more limited number of conditions are still acceptable approaches. Having said this, when the first partner screened is identified to be a carrier, his/her reproductive partners must be offered next-generation sequencing to identify less common disease-causing variants.4
A cautionary point to consider when expanded carrier screening panels are requested is the significant variability among commercial laboratories with regard to the conditions included in their panels. In addition, consider the absence of a well-defined or predictable phenotype for some of the included conditions.
Perhaps the most important matter when it comes to genetic carrier screening is to have a standard counseling approach that is persistently followed and offers the opportunity for individuals to know about their genetic testing options and available reproductive choices, including the use of donor gametes, preimplantation genetic testing for monogenic disease (PGT-M, formerly known as preimplantation genetic diagnosis, or PGD), prenatal testing, and pregnancy management options. For couples and/or individuals who decide to proceed with an affected pregnancy, earlier diagnosis can assist with postnatal management.
Medicolegal responsibility. Genetic carrier screening also is of specific relevance to the field of fertility medicine and assisted reproductive technology (ART) as a potential liability issue. Couples and individuals who are undergoing fertility treatment with in vitro fertilization (IVF) for a variety of medical or personal reasons are a specific group that certainly should be offered genetic carrier screening, as they have the option of "adding on" PGT-M (PGD) to their existing treatment plan at a fraction of the cost and treatment burden that would have otherwise been needed if they were not undergoing IVF. After counseling, some individuals and couples may ultimately opt out of genetic carrier screening. The counseling discussion needs to be clearly documented in the medical chart.
The preconception period is the perfect time to have a discussion about genetic carrier screening; it offers the opportunity for timely interventions if desired by the couples or individuals.
Continue to: Artificial intelligence and embryo selection...
Artificial intelligence and embryo selection
With continued improvements in embryo culture conditions and cryopreservation technology, there has been a tremendous amount of interest in developing better methods for embryo selection. These efforts are aimed at encouraging elective single embryo transfer (eSET) for women of all ages, thereby lowering the risk of multiple pregnancy and its associated adverse neonatal and obstetric outcomes—without compromising the pregnancy rates per transfer or lengthening the time to pregnancy.
One of the most extensively studied methods for this purpose is preimplantation genetic testing for aneuploidy (PGT-A, formerly known as PGS), but emerging data from large multicenter randomized clinical trials (RCTs) have again cast significant doubt on PGT-A's efficacy and utility.5 Meanwhile, alternative methods for embryo selection are currently under investigation, including noninvasive PGT-A and morphokinetic assessment of embryo development via analysis of images obtained by time-lapse imaging.
The potential of time-lapse imaging
Despite the initial promising results from time-lapse imaging, subsequent RCTs have not shown a significant clinical benefit.6 However, these early methods of morphokinetic assessment are mainly dependent on the embryologists' subjective assessment of individual static frames and "annotation" of observed spatial and temporal features of embryo development. In addition to being a very time-consuming task, this process is subject to significant interobserver and intraobserver variability.
Considering these limitations, even machine-based algorithms that incorporate these annotations along with such other clinical variables as parental age and prior obstetric history, have a low predictive power for the outcome of embryo transfer, with an area under the curve (AUC) of the ROC curve of 0.65 to 0.74. (An AUC of 0.5 represents completely random prediction and an AUC of 1.0 suggests perfect prediction.)7
A recent study by Tran and colleagues has employed a deep learning (neural network) model to analyze the entire raw time-lapse videos in an automated manner without prior annotation by embryologists. After analysis of 10,638 embryos from 8 different IVF clinics in 4 different countries, they have reported an AUC of 0.93 (95% confidence interval, 0.92-0.94) for prediction of fetal heart rate activity detected at 7 weeks of gestation or beyond. Although these data are very preliminary and have not yet been validated prospectively in larger datasets for live birth, it may herald the beginning of a new era for the automation and standardization of embryo assessment with artificial intelligence—similar to the rapidly increasing role of facial recognition technology for various applications.
Improved standardization of noninvasive embryo selection with growing use of artificial intelligence is a promising new tool to improve the safety and efficacy of ART.
Continue to: Environmental toxicants: The hidden danger...
Environmental toxicants: The hidden danger
Segal TR, Giudice LC. Before the beginning: environmental exposures and reproductive and obstetrical outcomes. Fertil Steril. 2019;112:613-621.
We receive news daily about the existential risk to humans of climate change. However, a risk that is likely as serious goes almost unseen by the public and most health care providers. That risk is environmental toxicants.8
More than 80,000 chemicals are registered in the United States, most in the last 75 years. These chemicals are ubiquitous. All of us are continuously exposed to and suffused with these toxicants and their metabolites. Air pollution adds insult to injury. Since this exposure has especially significant implications for fertility, infertility, pregnancy, perinatal health, childhood development, adult diseases, and later generational reproduction, it is imperative that reproductive health professionals take responsibility for helping mitigate this environmental crisis.
The problem is exceptionally complicated
The risks posed by environmental toxicants are much less visible than those for climate change, so the public, policymakers, and providers are largely unaware or may even seem uncaring. Few health professionals have sufficient knowledge to deliver care in this area, know which questions to ask, or have adequate information/medical record tools to assist them in care—and what are the possible interventions?
Addressing risk posed by individual toxicants
Addressing the problem clinically requires asking patients questions about exposure and recommending interventions. Toxicant chemicals include the neurotoxin mercury, which can be addressed by limiting intake of fish, especially certain types.
Lead was used before 1978 in paint, it also was used in gas and in water pipes. People living in older homes may be exposed, as well as those in occupations exposed to lead. Others with lead exposure risk include immigrants from areas without lead regulations and people using pica- or lead-glazed pottery. Lead exposure has been associated with multiple pregnancy complications and permanently impaired intellectual development in children. If lead testing reveals high levels, chelation therapy can help.
Cadmium is a heavy metal used in rechargeable batteries, paint pigment, and plastic production. Exposure results from food intake, smoking, and second-hand smoke. Cadmium accumulates in the liver, kidneys, testes, ovaries, and placenta. Exposure causes itai-itai disease, which is characterized by osteomalacia and renal tubular dysfunction as well as epigenetic changes in placental DNA and damage to the reproductive system. Eating organic food and reducing industrial exposure to cadmium are preventive strategies.
Pesticides are ubiquitous, with 90% of the US population having detectable levels. Exposure during the preconception period can lead to intrauterine growth restriction, low birth weight, subsequent cancers, and other problems. Eating organic food can reduce risk, as can frequent hand washing when exposed to pesticides, using protective gear, and removing shoes in the home.
Endocrine-disrupting chemicals (EDCs) are chemicals that can mimic or block endogenous hormones, which leads to adverse health outcomes. In addition to heavy metals, 3 important EDCs are bisphenol A (BPA), phthalates, and polybrominated diethyl ethers (PBDEs). Exposure is ubiquitous from industrial food processing, personal care products, cosmetics, and dust. Phthalates and BPA have short half-lives of hours to days, while PBDEs can persist in adipose tissue for months. Abnormal urogenital and neurologic development and thyroid disruption can result. Eating organic food, eating at home, and decreasing processed food intake can reduce exposure.
BPA is used in plastics, canned food liners, cash register receipts, and epoxy resins. Exposure is through inhalation, ingestion, and dermal absorption and affects semen quality, fertilization, placentation, and early reproduction. Limiting the use of plastic containers, not microwaving food in plastic, and avoiding thermal paper cash register receipts can reduce exposure.
Phthalates are synthetically derived and used as plasticizers in personal and medical products. The major source of phthalate exposure is food; exposure causes sperm, egg, and DNA damage. Phthalate avoidance involves replacing plastic bottles with glass or stainless steel, avoiding reheating food in plastic containers, and choosing "fragrance free" products.
PBDEs are used in flame retardants on upholstery, textiles, carpeting, and some electronics. Most PBDEs have been replaced by alternatives; however, their half-life is up to 12 years. Complications caused by PBDEs include thyroid disruption, resulting in abnormal fetal brain development. Avoiding dust and furniture that contain PBDEs, as well as hand washing, reduces exposure risk.
Air pollutants are associated with adverse obstetric outcomes and lower cognitive function in children. Avoiding areas with heavy traffic, staying indoors when air is heavily polluted, and using a HEPA filter in the home can reduce chemicals from air pollution.
Recommendations
The magnitude of the problem that environmental toxicant exposure creates requires health care providers to take action. The table in the publication by Segal and Giudice can be used as a tool that patients can answer first themselves before review by their provider.2 It can be added to your electronic health record and/or patient portal. Even making general comments to raise awareness, asking questions regarding exposure, and making recommendations can be helpful (TABLES 1 and 2). When possible, we also should advocate for public awareness and policy changes that address this significant health issue.
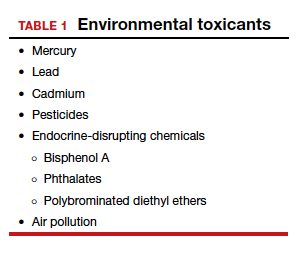
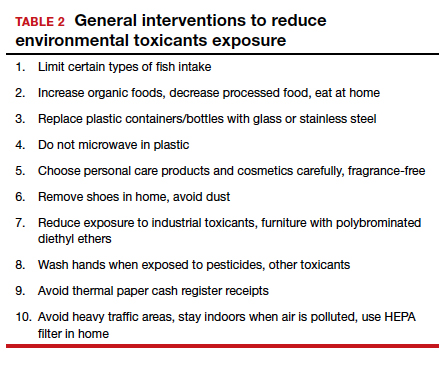
Environmental toxicants are a significant health problem that can be effectively mitigated through patient questions and recommended interventions.
- Larsen D, Ma J, Strassberg M, et al. The uptake of pan-ethnic expanded carrier screening is higher when offered during preconception or early prenatal genetic counseling. Prenat Diagn. 2019;39:319-323.
- Matthews TJ, MacDorman MF, Thoma ME. Infant Mortality Statistics From the 2013 Period Linked Birth/Infant Death Data Set. Natl Vital Stat Rep. 2015;64:1-30.
- American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 690: carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40.
- Gregg AR, Edwards JG. Prenatal genetic carrier screening in the genomic age. Semin Perinatol. 2018;42:303-306.
- Munné S, Kaplan B, Frattarelli JL, et al; STAR Study Group. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112:1071-1079. e7.
- Goodman LR, Goldberg J, Falcone T, et al. Does the addition of time-lapse morphokinetics in the selection of embryos for transfer improve pregnancy rates? A randomized controlled trial. Fertil Steril. 2016;105:275-285.e10.
- Blank C, Wildeboer RR, DeCroo I, et al. Prediction of implantation after blastocyst transfer in in vitro fertilization: a machine-learning perspective. Fertil Steril. 2019;111:318- 326.
- The American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women; American Society for Reproductive Medicine Practice Committee; The University of California, San Francisco Program on Reproductive Health and the Environment. ACOG Committee Opinion No. 575. Exposure to environmental toxic agents. Fertil Steril. 2013;100:931-934.
- Larsen D, Ma J, Strassberg M, et al. The uptake of pan-ethnic expanded carrier screening is higher when offered during preconception or early prenatal genetic counseling. Prenat Diagn. 2019;39:319-323.
- Matthews TJ, MacDorman MF, Thoma ME. Infant Mortality Statistics From the 2013 Period Linked Birth/Infant Death Data Set. Natl Vital Stat Rep. 2015;64:1-30.
- American College of Obstetricians and Gynecologists Committee on Genetics. Committee Opinion No. 690: carrier screening in the age of genomic medicine. Obstet Gynecol. 2017;129:e35-e40.
- Gregg AR, Edwards JG. Prenatal genetic carrier screening in the genomic age. Semin Perinatol. 2018;42:303-306.
- Munné S, Kaplan B, Frattarelli JL, et al; STAR Study Group. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112:1071-1079. e7.
- Goodman LR, Goldberg J, Falcone T, et al. Does the addition of time-lapse morphokinetics in the selection of embryos for transfer improve pregnancy rates? A randomized controlled trial. Fertil Steril. 2016;105:275-285.e10.
- Blank C, Wildeboer RR, DeCroo I, et al. Prediction of implantation after blastocyst transfer in in vitro fertilization: a machine-learning perspective. Fertil Steril. 2019;111:318- 326.
- The American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women; American Society for Reproductive Medicine Practice Committee; The University of California, San Francisco Program on Reproductive Health and the Environment. ACOG Committee Opinion No. 575. Exposure to environmental toxic agents. Fertil Steril. 2013;100:931-934.