User login
The challenge of poverty to health and success: What should pediatricians do?
Some days it feels like more than half of the journal articles I encounter report data suggesting that poverty is associated with some disease entity. I realize that young postgraduates are under some pressure to publish, but I’m ready for a break. I and most pediatricians already know, or at least have assumed, that in general and with few exceptions unwellness and poverty are closely linked. Whether that association is causal or not is a more interesting question. The answer, I suspect, depends on which health condition we are talking about. For the moment I think we should assume that poverty is more likely a major contributor and not merely a fellow traveler of poor health.
Some other questions: What are we as pediatricians expected to do about poverty? Is awareness sufficient? Should I be content with having an elevated awareness that a certain patient has a given disease because I know his family is economically challenged? Or, conversely, should I be satisfied that I have asked about a family’s economic distress when I have just diagnosed a child with asthma? The answer to those questions is a very personal one for each of us to ponder and may depend on where we feel we can best invest our time and skill set.
Like me, you may feel that the focus of your professional life is better spent diagnosing and treating the collateral damage of poverty and addressing economic inequities in your philanthropic activities and your choices at the polls. On the other hand, you may choose to use your public persona as a physician to more actively address poverty whether it is on a local, national, or global stage. There is no correct answer and a hybrid may work best for you.
On the other hand, while you agree that there is some link between poverty and unwellness, perhaps the issue is overblown and we should pay more attention to other factors such as the sad state of the family in both disadvantaged and advantaged populations. Maybe if we worked harder to foster and support two-parent families the drag of economic disadvantage would be reduced.
I recently encountered a study that explores this very question. Christina Cross, PhD, a postdoctoral fellow in the department of sociology at Harvard University, reports on her soon-to-be-published study of a nationally representative sample in which she found that, using a selection of academic metrics including earned grades, likelihood of grade repetition, and rates of suspension, in low-income families there was no difference in achievement between Black youth raised in single-parent households and Black youth raised in two-parent households. However, in well-off families, Black youth raised in two-parent households had better academic metrics. (“Why living in a two-parent home isn’t a cure-all for Black students.” Christina Cross. The Harvard Gazette. 2021 Jun 3).
I guess few of us are surprised that living in a two-parent household can provide a child with some advantages. However, it is disappointing and again not surprising that poverty can rob a child of these advantages. While it may make us feel like we are doing something when we offer counseling that promotes two-family households, this may be no more valuable than supporting apple pie and motherhood. Dr. Cross concludes that President Biden’s proposed American Families Plan is more likely to succeed than those focused on counseling because it will offer direct financial support with its tax credits and subsidies.*
Let’s hope she is correct.
* This story was updated on July 6, 2021.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Some days it feels like more than half of the journal articles I encounter report data suggesting that poverty is associated with some disease entity. I realize that young postgraduates are under some pressure to publish, but I’m ready for a break. I and most pediatricians already know, or at least have assumed, that in general and with few exceptions unwellness and poverty are closely linked. Whether that association is causal or not is a more interesting question. The answer, I suspect, depends on which health condition we are talking about. For the moment I think we should assume that poverty is more likely a major contributor and not merely a fellow traveler of poor health.
Some other questions: What are we as pediatricians expected to do about poverty? Is awareness sufficient? Should I be content with having an elevated awareness that a certain patient has a given disease because I know his family is economically challenged? Or, conversely, should I be satisfied that I have asked about a family’s economic distress when I have just diagnosed a child with asthma? The answer to those questions is a very personal one for each of us to ponder and may depend on where we feel we can best invest our time and skill set.
Like me, you may feel that the focus of your professional life is better spent diagnosing and treating the collateral damage of poverty and addressing economic inequities in your philanthropic activities and your choices at the polls. On the other hand, you may choose to use your public persona as a physician to more actively address poverty whether it is on a local, national, or global stage. There is no correct answer and a hybrid may work best for you.
On the other hand, while you agree that there is some link between poverty and unwellness, perhaps the issue is overblown and we should pay more attention to other factors such as the sad state of the family in both disadvantaged and advantaged populations. Maybe if we worked harder to foster and support two-parent families the drag of economic disadvantage would be reduced.
I recently encountered a study that explores this very question. Christina Cross, PhD, a postdoctoral fellow in the department of sociology at Harvard University, reports on her soon-to-be-published study of a nationally representative sample in which she found that, using a selection of academic metrics including earned grades, likelihood of grade repetition, and rates of suspension, in low-income families there was no difference in achievement between Black youth raised in single-parent households and Black youth raised in two-parent households. However, in well-off families, Black youth raised in two-parent households had better academic metrics. (“Why living in a two-parent home isn’t a cure-all for Black students.” Christina Cross. The Harvard Gazette. 2021 Jun 3).
I guess few of us are surprised that living in a two-parent household can provide a child with some advantages. However, it is disappointing and again not surprising that poverty can rob a child of these advantages. While it may make us feel like we are doing something when we offer counseling that promotes two-family households, this may be no more valuable than supporting apple pie and motherhood. Dr. Cross concludes that President Biden’s proposed American Families Plan is more likely to succeed than those focused on counseling because it will offer direct financial support with its tax credits and subsidies.*
Let’s hope she is correct.
* This story was updated on July 6, 2021.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Some days it feels like more than half of the journal articles I encounter report data suggesting that poverty is associated with some disease entity. I realize that young postgraduates are under some pressure to publish, but I’m ready for a break. I and most pediatricians already know, or at least have assumed, that in general and with few exceptions unwellness and poverty are closely linked. Whether that association is causal or not is a more interesting question. The answer, I suspect, depends on which health condition we are talking about. For the moment I think we should assume that poverty is more likely a major contributor and not merely a fellow traveler of poor health.
Some other questions: What are we as pediatricians expected to do about poverty? Is awareness sufficient? Should I be content with having an elevated awareness that a certain patient has a given disease because I know his family is economically challenged? Or, conversely, should I be satisfied that I have asked about a family’s economic distress when I have just diagnosed a child with asthma? The answer to those questions is a very personal one for each of us to ponder and may depend on where we feel we can best invest our time and skill set.
Like me, you may feel that the focus of your professional life is better spent diagnosing and treating the collateral damage of poverty and addressing economic inequities in your philanthropic activities and your choices at the polls. On the other hand, you may choose to use your public persona as a physician to more actively address poverty whether it is on a local, national, or global stage. There is no correct answer and a hybrid may work best for you.
On the other hand, while you agree that there is some link between poverty and unwellness, perhaps the issue is overblown and we should pay more attention to other factors such as the sad state of the family in both disadvantaged and advantaged populations. Maybe if we worked harder to foster and support two-parent families the drag of economic disadvantage would be reduced.
I recently encountered a study that explores this very question. Christina Cross, PhD, a postdoctoral fellow in the department of sociology at Harvard University, reports on her soon-to-be-published study of a nationally representative sample in which she found that, using a selection of academic metrics including earned grades, likelihood of grade repetition, and rates of suspension, in low-income families there was no difference in achievement between Black youth raised in single-parent households and Black youth raised in two-parent households. However, in well-off families, Black youth raised in two-parent households had better academic metrics. (“Why living in a two-parent home isn’t a cure-all for Black students.” Christina Cross. The Harvard Gazette. 2021 Jun 3).
I guess few of us are surprised that living in a two-parent household can provide a child with some advantages. However, it is disappointing and again not surprising that poverty can rob a child of these advantages. While it may make us feel like we are doing something when we offer counseling that promotes two-family households, this may be no more valuable than supporting apple pie and motherhood. Dr. Cross concludes that President Biden’s proposed American Families Plan is more likely to succeed than those focused on counseling because it will offer direct financial support with its tax credits and subsidies.*
Let’s hope she is correct.
* This story was updated on July 6, 2021.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Opioid prescriptions decrease in young kids, long dosages increase
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
The opioid prescription rates have significantly decreased for children, teens, and younger adults between 2006 and 2018, according to new research.
“What’s important about this new study is that it documented that these improvements were also occurring for children and young adults specifically,” said Kao-Ping Chua, MD, PhD, primary care physician and assistant professor of pediatrics at the University of Michigan, Ann Arbor, who was not involved in the study. “The reason that’s important is that changes in medical practice for adults aren’t always reflected in pediatrics.”
The study, published in JAMA Pediatrics, found that dispensed opioid prescriptions for this population have decreased by 15% annually since 2013. However, the study also examined specific prescribing variables, such as duration of opioid prescription and high-dosage prescriptions. Researchers found reduced rates of high-dosage and long-duration prescriptions for adolescents and younger adults. However, these types of prescription practices increased in children aged 0-5 years.
“I think [the findings are] promising, suggesting that opiate prescribing practices may be improving,” study author Madeline Renny, MD, pediatric emergency medicine doctor at New York University Langone Health, said in an interview. “But we did find that there were increases in the young children for the practice variables, which we didn’t expect. I think that was kind of one of the findings that we were a bit surprised about and want to explore further.”
Previous studies have linked prescription opioid use in children and teens to an increased risk of future opioid misuse. A 2015 study published in Pediatrics found that using prescribed opioids before the 12th grade is associated with a 33% increase in the risk of future opioid misuse by the age of 23. The study also found that for those with a low predicted risk of future opioid misuse, an opioid prescription increases the risk for misuse after high school threefold.
Furthermore, a 2018 study published in JAMA Network Open found that, between 1999 and 2016, the annual estimated mortality rate for all children and adolescents from prescription and illicit opioid use rose 268.2%.
In the new study, Dr. Renny and colleagues examined data from 2006 to 2018 from IQVIA Longitudinal Prescription Data, which captured 74%-92% of U.S. retail outpatient opioid prescriptions dispensed to people up to the age of 24. Researchers also examined prescribing practice variables, which included opioid dispensing rates, average amount of opioid dispensed per prescription, duration of opioid prescription, high-dosage opioid prescription for individuals, and the rate in which extended-release or long-acting opioids are prescribed.
Researchers found that between 2006 and 2018, the total U.S. annual opioid prescriptions dispensed to patients younger than 25 years was highest in 2007 at 15,689,779 prescriptions, and since 2012 has steadily decreased to 6,705,478 in 2018.
“Our study did show that there were declines, but opioids remain readily dispensed,” Dr. Renny said. “And I think it’s good that rates have gone down, but I think opioids are still commonly dispensed to children and adolescents and young adults and all of our age groups.”
Dr. Chua said that the study was important, but when it came to younger children, it didn’t account for the fact that “the underlying population of patients who were getting opioids changed because it’s not the same group of children.”
“Maybe at the beginning there were more surgical patients who are getting shorter duration, lower dosage opioids,” he added. “Now some of those surgical exceptions kind of went away and who’s left in the population of people who get opioids is a sicker population.”
“Who are the 0 to 5-year-olds who are getting opioids now?” Dr. Chua asked. “Well, some of them are going to be cancer or surgical patients. If you think about it, over time their surgeons may be more judicious and they stop prescribing opioids for some things like circumcision or something like that. So that means that who’s left in the population of children who get opiate prescriptions are the cancer patients. Cancer patients’ opioid dosages are going to be higher because they have chronic pain.”
Dr. Chua said it is important to remember that the number of children who are affected by those high-risk prescriptions are lower because the overall number of opioid prescriptions has gone down. He added that the key piece of missing information is the absolute number of prescriptions that were high risk.
Researchers of the current study suggested that, because of the differences between pediatric and adult pain and indications for opioid prescribing, there should be national guidelines on general opioid prescribing for children and adolescents.
Experts did not disclose relevant financial relationships.
FROM JAMA PEDIATRICS
New COVID-19 vaccinations decline again in 12- to 15-year-olds
Even though less than 21% of all children aged 12-15 years are fully vaccinated against COVID-19, the number seeking first vaccinations continues to decline, according to data from the Centers for Disease Control and Prevention.

and 462,000 during the week ending June 14. Collectively, 30.2% of 12- to 15-year-olds have gotten at least one dose of vaccine so far and 20.7% are now fully vaccinated, the CDC said on its COVID Data Tracker site.
Among children aged 16-17 years, who were able to start the vaccination process earlier, 42.9% have received at least one dose and 34.0% have completed the COVID-19 vaccine regimen. Vaccine initiation – measured as the proportion of all individuals getting a first shot over the previous 2 weeks – has been consistently around 4.8% during the month of June for this age group but has dropped from 17.9% on June 7 to 14.3% on June 28 for those aged 12-15, the CDC data show.
Looking at the same measure for vaccine completion, 16.7% of all those who reached full vaccination status in the 14 days ending June 28 were 12- to 15-years-olds, down from 21.5% on June 21 and 19.6% on June 14. The numbers for those aged 15-16 were, respectively, 4.6%, 4.5%, and 4.2%, the CDC reported.
Fortunately, in the wake of recent vaccination trends, new cases of COVID-19 in children were down to their lowest level – just 8,447 for the week ending June 24 – since May of 2020, according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
New cases had been well over 15,000 the previous week (June 17), following weeks of 14,000 (June 10) and 16,000 (June 3) new cases, so the latest drop down to just four digits represents a 1-week decline of over 46% in the 49 states (excluding New York) that are reporting age distribution, along with the District of Columbia, New York City, Puerto Rico, and Guam.
The cumulative number of child COVID-19 cases in those jurisdictions is about 4.03 million since the beginning of the pandemic, which represents 14.2% of all cases in the United States. At the state level, the cumulative rate of cases in children is highest in Vermont (22.7%) and lowest in Florida (8.9%), which uses an age range of 0-14 years for children, compared with 0-17 or 0-19 for most states, the AAP and CHA said.
Severe illness has been rare in children, which is reflected in the proportion of children among all hospitalizations, 2.2% in 24 jurisdictions, and the proportion of deaths, 0.06% in 46 jurisdictions, since the start of the pandemic, the AAP and CHA said, with a total of 336 COVID-19–related deaths reported.
Even though less than 21% of all children aged 12-15 years are fully vaccinated against COVID-19, the number seeking first vaccinations continues to decline, according to data from the Centers for Disease Control and Prevention.

and 462,000 during the week ending June 14. Collectively, 30.2% of 12- to 15-year-olds have gotten at least one dose of vaccine so far and 20.7% are now fully vaccinated, the CDC said on its COVID Data Tracker site.
Among children aged 16-17 years, who were able to start the vaccination process earlier, 42.9% have received at least one dose and 34.0% have completed the COVID-19 vaccine regimen. Vaccine initiation – measured as the proportion of all individuals getting a first shot over the previous 2 weeks – has been consistently around 4.8% during the month of June for this age group but has dropped from 17.9% on June 7 to 14.3% on June 28 for those aged 12-15, the CDC data show.
Looking at the same measure for vaccine completion, 16.7% of all those who reached full vaccination status in the 14 days ending June 28 were 12- to 15-years-olds, down from 21.5% on June 21 and 19.6% on June 14. The numbers for those aged 15-16 were, respectively, 4.6%, 4.5%, and 4.2%, the CDC reported.
Fortunately, in the wake of recent vaccination trends, new cases of COVID-19 in children were down to their lowest level – just 8,447 for the week ending June 24 – since May of 2020, according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
New cases had been well over 15,000 the previous week (June 17), following weeks of 14,000 (June 10) and 16,000 (June 3) new cases, so the latest drop down to just four digits represents a 1-week decline of over 46% in the 49 states (excluding New York) that are reporting age distribution, along with the District of Columbia, New York City, Puerto Rico, and Guam.
The cumulative number of child COVID-19 cases in those jurisdictions is about 4.03 million since the beginning of the pandemic, which represents 14.2% of all cases in the United States. At the state level, the cumulative rate of cases in children is highest in Vermont (22.7%) and lowest in Florida (8.9%), which uses an age range of 0-14 years for children, compared with 0-17 or 0-19 for most states, the AAP and CHA said.
Severe illness has been rare in children, which is reflected in the proportion of children among all hospitalizations, 2.2% in 24 jurisdictions, and the proportion of deaths, 0.06% in 46 jurisdictions, since the start of the pandemic, the AAP and CHA said, with a total of 336 COVID-19–related deaths reported.
Even though less than 21% of all children aged 12-15 years are fully vaccinated against COVID-19, the number seeking first vaccinations continues to decline, according to data from the Centers for Disease Control and Prevention.

and 462,000 during the week ending June 14. Collectively, 30.2% of 12- to 15-year-olds have gotten at least one dose of vaccine so far and 20.7% are now fully vaccinated, the CDC said on its COVID Data Tracker site.
Among children aged 16-17 years, who were able to start the vaccination process earlier, 42.9% have received at least one dose and 34.0% have completed the COVID-19 vaccine regimen. Vaccine initiation – measured as the proportion of all individuals getting a first shot over the previous 2 weeks – has been consistently around 4.8% during the month of June for this age group but has dropped from 17.9% on June 7 to 14.3% on June 28 for those aged 12-15, the CDC data show.
Looking at the same measure for vaccine completion, 16.7% of all those who reached full vaccination status in the 14 days ending June 28 were 12- to 15-years-olds, down from 21.5% on June 21 and 19.6% on June 14. The numbers for those aged 15-16 were, respectively, 4.6%, 4.5%, and 4.2%, the CDC reported.
Fortunately, in the wake of recent vaccination trends, new cases of COVID-19 in children were down to their lowest level – just 8,447 for the week ending June 24 – since May of 2020, according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
New cases had been well over 15,000 the previous week (June 17), following weeks of 14,000 (June 10) and 16,000 (June 3) new cases, so the latest drop down to just four digits represents a 1-week decline of over 46% in the 49 states (excluding New York) that are reporting age distribution, along with the District of Columbia, New York City, Puerto Rico, and Guam.
The cumulative number of child COVID-19 cases in those jurisdictions is about 4.03 million since the beginning of the pandemic, which represents 14.2% of all cases in the United States. At the state level, the cumulative rate of cases in children is highest in Vermont (22.7%) and lowest in Florida (8.9%), which uses an age range of 0-14 years for children, compared with 0-17 or 0-19 for most states, the AAP and CHA said.
Severe illness has been rare in children, which is reflected in the proportion of children among all hospitalizations, 2.2% in 24 jurisdictions, and the proportion of deaths, 0.06% in 46 jurisdictions, since the start of the pandemic, the AAP and CHA said, with a total of 336 COVID-19–related deaths reported.
‘Treat youth with gender dysphoria as individuals’
Young people with gender dysphoria should be considered as individuals rather than fall into an age-defined bracket when assessing their understanding to consent to hormone treatment, according to the Tavistock and Portman NHS Foundation Trust, as it awaits the verdict of its recent appeal in London against a High Court ruling.
The High Court ruling, made in December 2020 as reported by this news organization, stated that adolescents with gender dysphoria were unlikely to fully understand the consequences of hormone treatment for gender reassignment and was the result of a case brought by 24-year-old Keira Bell, who transitioned from female to male at the Gender Identity Development Service (GIDS), starting at the age of 16, but later “detransitioned.”
Along with changes made to rules around prescribing puberty blockers and cross-sex hormones to minors with gender dysphoria in countries such as Finland and Sweden, the English ruling signals a more cautious approach to any medical treatment for such children, as detailed in a feature published in April.
However, during the appeal, The Trust argued once more that puberty blockers give children time to “consider options” about their bodies and that the decision (the December ruling) was inconsistent with the law that “entitles children under the age of 16 to make decisions for themselves after being assessed as competent to do so by their doctor.”
Alongside other organizations, the United States–based Endocrine Society submitted written evidence in support of the Tavistock. “The High Court’s decision, if it is allowed to stand, would set a harmful precedent preventing physicians from providing transgender and gender diverse youth with high-quality medical care,” it noted in a statement.
Defending the High Court’s ruling, the lawyer for Ms. Bell said its conclusion was that puberty blockers for gender dysphoria are an “experimental” treatment with a very limited evidence base.
“The judgment of the [High Court] is entirely correct, and there is no proper basis for overturning it,” he asserted.
The 2-day appeal hearing ended on June 24, and a ruling will be made at a later date.
Do children understand the consequences of hormone treatment?
One central aspect of the overall case is the fact that Ms. Bell regrets her decision to transition at age 16, saying she only received three counseling sessions prior to endocrinology referral. And she consequently had a mastectomy at age 20, which she also bitterly regrets.
So a key concern is whether young people fully understand the consequences of taking puberty blockers and therapies that may follow, including cross-sex hormones.
Witness for the appeal Gary Butler, MD, consultant in pediatric and adolescent endocrinology at University College Hospital, London, where children are referred to from GIDS for hormone treatment, said the number of children who go on to cross-sex hormones from puberty blockers is “over 80%.”
But the actual number of children who are referred to endocrinology services (where puberty blockers are initiated) from GIDS is low, at approximately 16%, according to 2019-2020 data, said a GIDS spokesperson.
“Once at the endocrinology service, young people either participate in a group education session, or if under 15 years, an individualized session between the clinician and the patient and family members,” she added. The Trust also maintained that initiation of cross-sex hormones “is separate from the prescription of puberty blockers.”
Since the December ruling, The Trust has put in place multidisciplinary clinical reviews (MDCR) of cases, and in July, NHS England will start implementing an independent multidisciplinary professional review (MDPR) to check that the GIDS has followed due process with each case.
Slow the process down, give appropriate psychotherapy
Stella O’Malley is a psychotherapist who works with transitioners and detransitioners and is a founding member of the International Association of Therapists for Desisters and Detransitioners (IATDD).
Whatever the outcome of the appeal process, Ms. O’Malley said she would like to see the Tavistock slow down and take a broader approach to counseling children before referral to endocrinology services.
In discussing therapy prior to transition, Ms. O’Malley stated that her clients often say they did not explore their inner motivations or other possible reasons for their distress, and the therapy was focused more on when they transition, rather than being sure it was something they wanted to do.
“We need to learn from the mistakes made with people like Keira Bell. , especially when [children are] ... young and especially when they’re traumatized,” Ms. O’Malley said.
“Had they received a more conventional therapy, they might have thought about their decision from different perspectives and in the process acquired more self-awareness, which would have been more beneficial.”
“The ‘affirmative’ approach to gender therapy is too narrow; we need to look at the whole individual. Therapy in other areas would never disregard other, nongender issues such as attention deficit hyperactivity disorder or anxiety [which often co-exist with gender dysphoria] – issues bleed into each other,” Ms. O’Malley pointed out. “We need a more exploratory approach.”
“I’d also like to see other therapists all over the [U.K.] who are perfectly qualified and capable of working with gender actually start working with gender issues,” she said, noting that such an approach might also help reduce the long waiting list at the Tavistock.
The latter had been overwhelmed, and this led to a speeding up of the assessment process, which led to a number of professionals resigning from the service in recent years, saying children were being “fast-tracked” to medical transition.
Fertility and sexual function are complex issues for kids
Also asked to comment was Claire Graham, from Genspect, a group that describes itself as a voice for parents of gender-questioning kids.
She told this news organization that “parents are rightly concerned about their children’s ability to consent to treatments that may lead to infertility and issues surrounding sexual function.” She added that other countries in Europe were changing their approach. “Look to Sweden and Finland, who have both rowed back on puberty blockers and no longer recommend them.”
Ms. Graham, who has worked with children with differences in sexual development, added that it was very difficult for children and young people to understand the life-long implications of decisions made at an early age.
“How can children understand what it is to live with impaired sexual functioning if they have never had sex? Likewise, fertility is a complex issue. Most people do not want to become parents as teenagers, but we understand that this will often change as they grow,” said Ms. Graham.
“Many parents worry that their child is not being considered in the whole [and] that their child’s ability to consent to medical interventions for gender dysphoria is impacted by comorbidities, such as a diagnosis of autism or a history of mental health issues. These children are particularly vulnerable.”
“At Genspect, we hope that the decision from the ... court is upheld,” Ms. Graham concluded.
A version of this article first appeared on Medscape.com.
Young people with gender dysphoria should be considered as individuals rather than fall into an age-defined bracket when assessing their understanding to consent to hormone treatment, according to the Tavistock and Portman NHS Foundation Trust, as it awaits the verdict of its recent appeal in London against a High Court ruling.
The High Court ruling, made in December 2020 as reported by this news organization, stated that adolescents with gender dysphoria were unlikely to fully understand the consequences of hormone treatment for gender reassignment and was the result of a case brought by 24-year-old Keira Bell, who transitioned from female to male at the Gender Identity Development Service (GIDS), starting at the age of 16, but later “detransitioned.”
Along with changes made to rules around prescribing puberty blockers and cross-sex hormones to minors with gender dysphoria in countries such as Finland and Sweden, the English ruling signals a more cautious approach to any medical treatment for such children, as detailed in a feature published in April.
However, during the appeal, The Trust argued once more that puberty blockers give children time to “consider options” about their bodies and that the decision (the December ruling) was inconsistent with the law that “entitles children under the age of 16 to make decisions for themselves after being assessed as competent to do so by their doctor.”
Alongside other organizations, the United States–based Endocrine Society submitted written evidence in support of the Tavistock. “The High Court’s decision, if it is allowed to stand, would set a harmful precedent preventing physicians from providing transgender and gender diverse youth with high-quality medical care,” it noted in a statement.
Defending the High Court’s ruling, the lawyer for Ms. Bell said its conclusion was that puberty blockers for gender dysphoria are an “experimental” treatment with a very limited evidence base.
“The judgment of the [High Court] is entirely correct, and there is no proper basis for overturning it,” he asserted.
The 2-day appeal hearing ended on June 24, and a ruling will be made at a later date.
Do children understand the consequences of hormone treatment?
One central aspect of the overall case is the fact that Ms. Bell regrets her decision to transition at age 16, saying she only received three counseling sessions prior to endocrinology referral. And she consequently had a mastectomy at age 20, which she also bitterly regrets.
So a key concern is whether young people fully understand the consequences of taking puberty blockers and therapies that may follow, including cross-sex hormones.
Witness for the appeal Gary Butler, MD, consultant in pediatric and adolescent endocrinology at University College Hospital, London, where children are referred to from GIDS for hormone treatment, said the number of children who go on to cross-sex hormones from puberty blockers is “over 80%.”
But the actual number of children who are referred to endocrinology services (where puberty blockers are initiated) from GIDS is low, at approximately 16%, according to 2019-2020 data, said a GIDS spokesperson.
“Once at the endocrinology service, young people either participate in a group education session, or if under 15 years, an individualized session between the clinician and the patient and family members,” she added. The Trust also maintained that initiation of cross-sex hormones “is separate from the prescription of puberty blockers.”
Since the December ruling, The Trust has put in place multidisciplinary clinical reviews (MDCR) of cases, and in July, NHS England will start implementing an independent multidisciplinary professional review (MDPR) to check that the GIDS has followed due process with each case.
Slow the process down, give appropriate psychotherapy
Stella O’Malley is a psychotherapist who works with transitioners and detransitioners and is a founding member of the International Association of Therapists for Desisters and Detransitioners (IATDD).
Whatever the outcome of the appeal process, Ms. O’Malley said she would like to see the Tavistock slow down and take a broader approach to counseling children before referral to endocrinology services.
In discussing therapy prior to transition, Ms. O’Malley stated that her clients often say they did not explore their inner motivations or other possible reasons for their distress, and the therapy was focused more on when they transition, rather than being sure it was something they wanted to do.
“We need to learn from the mistakes made with people like Keira Bell. , especially when [children are] ... young and especially when they’re traumatized,” Ms. O’Malley said.
“Had they received a more conventional therapy, they might have thought about their decision from different perspectives and in the process acquired more self-awareness, which would have been more beneficial.”
“The ‘affirmative’ approach to gender therapy is too narrow; we need to look at the whole individual. Therapy in other areas would never disregard other, nongender issues such as attention deficit hyperactivity disorder or anxiety [which often co-exist with gender dysphoria] – issues bleed into each other,” Ms. O’Malley pointed out. “We need a more exploratory approach.”
“I’d also like to see other therapists all over the [U.K.] who are perfectly qualified and capable of working with gender actually start working with gender issues,” she said, noting that such an approach might also help reduce the long waiting list at the Tavistock.
The latter had been overwhelmed, and this led to a speeding up of the assessment process, which led to a number of professionals resigning from the service in recent years, saying children were being “fast-tracked” to medical transition.
Fertility and sexual function are complex issues for kids
Also asked to comment was Claire Graham, from Genspect, a group that describes itself as a voice for parents of gender-questioning kids.
She told this news organization that “parents are rightly concerned about their children’s ability to consent to treatments that may lead to infertility and issues surrounding sexual function.” She added that other countries in Europe were changing their approach. “Look to Sweden and Finland, who have both rowed back on puberty blockers and no longer recommend them.”
Ms. Graham, who has worked with children with differences in sexual development, added that it was very difficult for children and young people to understand the life-long implications of decisions made at an early age.
“How can children understand what it is to live with impaired sexual functioning if they have never had sex? Likewise, fertility is a complex issue. Most people do not want to become parents as teenagers, but we understand that this will often change as they grow,” said Ms. Graham.
“Many parents worry that their child is not being considered in the whole [and] that their child’s ability to consent to medical interventions for gender dysphoria is impacted by comorbidities, such as a diagnosis of autism or a history of mental health issues. These children are particularly vulnerable.”
“At Genspect, we hope that the decision from the ... court is upheld,” Ms. Graham concluded.
A version of this article first appeared on Medscape.com.
Young people with gender dysphoria should be considered as individuals rather than fall into an age-defined bracket when assessing their understanding to consent to hormone treatment, according to the Tavistock and Portman NHS Foundation Trust, as it awaits the verdict of its recent appeal in London against a High Court ruling.
The High Court ruling, made in December 2020 as reported by this news organization, stated that adolescents with gender dysphoria were unlikely to fully understand the consequences of hormone treatment for gender reassignment and was the result of a case brought by 24-year-old Keira Bell, who transitioned from female to male at the Gender Identity Development Service (GIDS), starting at the age of 16, but later “detransitioned.”
Along with changes made to rules around prescribing puberty blockers and cross-sex hormones to minors with gender dysphoria in countries such as Finland and Sweden, the English ruling signals a more cautious approach to any medical treatment for such children, as detailed in a feature published in April.
However, during the appeal, The Trust argued once more that puberty blockers give children time to “consider options” about their bodies and that the decision (the December ruling) was inconsistent with the law that “entitles children under the age of 16 to make decisions for themselves after being assessed as competent to do so by their doctor.”
Alongside other organizations, the United States–based Endocrine Society submitted written evidence in support of the Tavistock. “The High Court’s decision, if it is allowed to stand, would set a harmful precedent preventing physicians from providing transgender and gender diverse youth with high-quality medical care,” it noted in a statement.
Defending the High Court’s ruling, the lawyer for Ms. Bell said its conclusion was that puberty blockers for gender dysphoria are an “experimental” treatment with a very limited evidence base.
“The judgment of the [High Court] is entirely correct, and there is no proper basis for overturning it,” he asserted.
The 2-day appeal hearing ended on June 24, and a ruling will be made at a later date.
Do children understand the consequences of hormone treatment?
One central aspect of the overall case is the fact that Ms. Bell regrets her decision to transition at age 16, saying she only received three counseling sessions prior to endocrinology referral. And she consequently had a mastectomy at age 20, which she also bitterly regrets.
So a key concern is whether young people fully understand the consequences of taking puberty blockers and therapies that may follow, including cross-sex hormones.
Witness for the appeal Gary Butler, MD, consultant in pediatric and adolescent endocrinology at University College Hospital, London, where children are referred to from GIDS for hormone treatment, said the number of children who go on to cross-sex hormones from puberty blockers is “over 80%.”
But the actual number of children who are referred to endocrinology services (where puberty blockers are initiated) from GIDS is low, at approximately 16%, according to 2019-2020 data, said a GIDS spokesperson.
“Once at the endocrinology service, young people either participate in a group education session, or if under 15 years, an individualized session between the clinician and the patient and family members,” she added. The Trust also maintained that initiation of cross-sex hormones “is separate from the prescription of puberty blockers.”
Since the December ruling, The Trust has put in place multidisciplinary clinical reviews (MDCR) of cases, and in July, NHS England will start implementing an independent multidisciplinary professional review (MDPR) to check that the GIDS has followed due process with each case.
Slow the process down, give appropriate psychotherapy
Stella O’Malley is a psychotherapist who works with transitioners and detransitioners and is a founding member of the International Association of Therapists for Desisters and Detransitioners (IATDD).
Whatever the outcome of the appeal process, Ms. O’Malley said she would like to see the Tavistock slow down and take a broader approach to counseling children before referral to endocrinology services.
In discussing therapy prior to transition, Ms. O’Malley stated that her clients often say they did not explore their inner motivations or other possible reasons for their distress, and the therapy was focused more on when they transition, rather than being sure it was something they wanted to do.
“We need to learn from the mistakes made with people like Keira Bell. , especially when [children are] ... young and especially when they’re traumatized,” Ms. O’Malley said.
“Had they received a more conventional therapy, they might have thought about their decision from different perspectives and in the process acquired more self-awareness, which would have been more beneficial.”
“The ‘affirmative’ approach to gender therapy is too narrow; we need to look at the whole individual. Therapy in other areas would never disregard other, nongender issues such as attention deficit hyperactivity disorder or anxiety [which often co-exist with gender dysphoria] – issues bleed into each other,” Ms. O’Malley pointed out. “We need a more exploratory approach.”
“I’d also like to see other therapists all over the [U.K.] who are perfectly qualified and capable of working with gender actually start working with gender issues,” she said, noting that such an approach might also help reduce the long waiting list at the Tavistock.
The latter had been overwhelmed, and this led to a speeding up of the assessment process, which led to a number of professionals resigning from the service in recent years, saying children were being “fast-tracked” to medical transition.
Fertility and sexual function are complex issues for kids
Also asked to comment was Claire Graham, from Genspect, a group that describes itself as a voice for parents of gender-questioning kids.
She told this news organization that “parents are rightly concerned about their children’s ability to consent to treatments that may lead to infertility and issues surrounding sexual function.” She added that other countries in Europe were changing their approach. “Look to Sweden and Finland, who have both rowed back on puberty blockers and no longer recommend them.”
Ms. Graham, who has worked with children with differences in sexual development, added that it was very difficult for children and young people to understand the life-long implications of decisions made at an early age.
“How can children understand what it is to live with impaired sexual functioning if they have never had sex? Likewise, fertility is a complex issue. Most people do not want to become parents as teenagers, but we understand that this will often change as they grow,” said Ms. Graham.
“Many parents worry that their child is not being considered in the whole [and] that their child’s ability to consent to medical interventions for gender dysphoria is impacted by comorbidities, such as a diagnosis of autism or a history of mental health issues. These children are particularly vulnerable.”
“At Genspect, we hope that the decision from the ... court is upheld,” Ms. Graham concluded.
A version of this article first appeared on Medscape.com.
Even a pandemic can’t stop teens’ alcohol and marijuana use
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
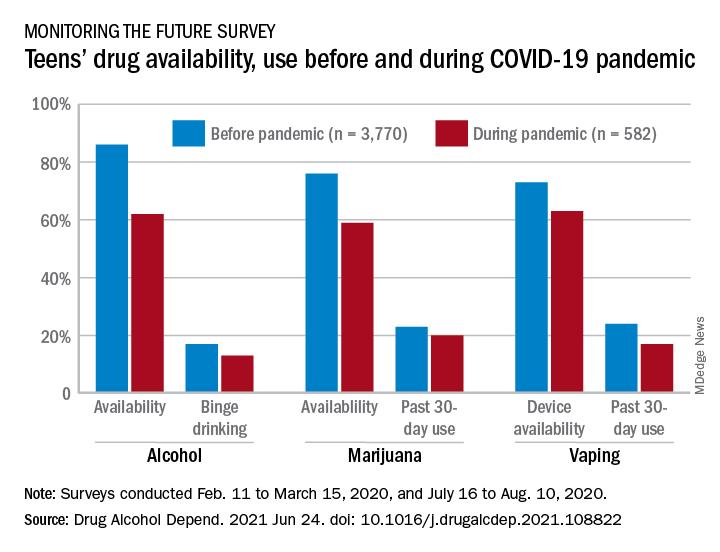
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
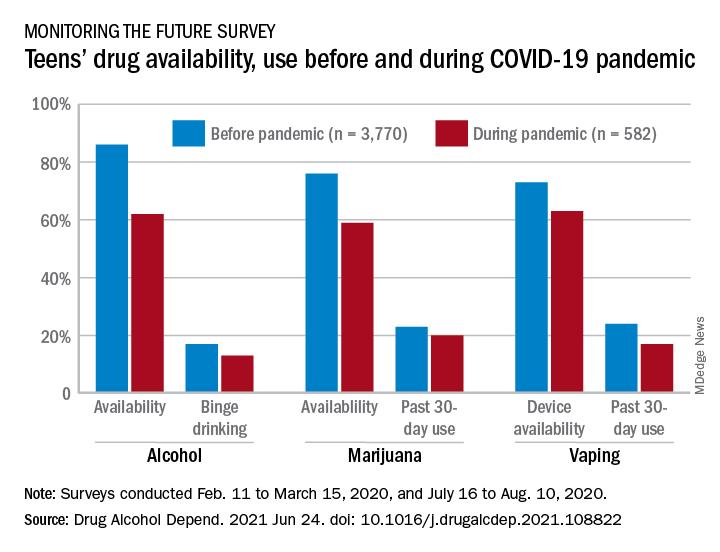
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
Despite record-breaking decreases in perceived availability of alcohol and marijuana among 12th-grade students, their use of these substances did not change significantly during the COVID-19 pandemic, according to two surveys conducted in 2020.
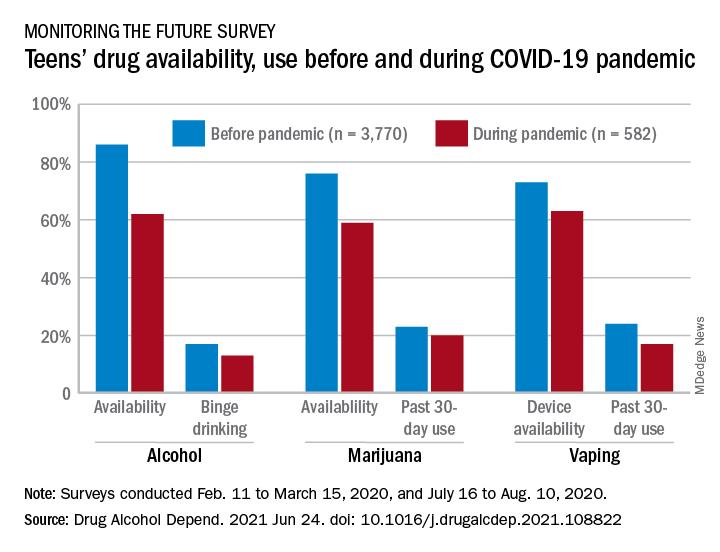
Vaping, however, did not show the same pattern. A decline in use over the previous 30 days was seen between the two surveys – conducted from Feb. 11 to March 15 and July 16 to Aug. 10 – along with a perceived reduction in the supply of vaping devices, Richard A. Miech, PhD, and associates said in Drug and Alcohol Dependence.
“Last year brought dramatic changes to adolescents’ lives, as many teens remained home with parents and other family members full time,” Nora D. Volkow, director of the National Institute on Drug Abuse, said in a separate written statement. “It is striking that, despite this monumental shift and teens’ perceived decreases in availability of marijuana and alcohol, usage rates held steady for these substances. This indicates that teens were able to obtain them despite barriers caused by the pandemic and despite not being of age to legally purchase them.”
In the first poll, conducted as part of the Monitoring the Future survey largely before the national emergency was declared, 86% of 12th-graders said that it was “fairly easy” or “very easy” to get alcohol, but that dropped to 62% in the second survey. For marijuana, prevalence of that level of availability was 76% before and 59% during the pandemic, Dr. Miech of the University of Michigan, Ann Arbor, and associates reported.
These results “indicate the largest decreases in substance use availability ever recorded in the 46 consecutive years it has been monitored by Monitoring the Future,” the investigators wrote.
The prevalence of marijuana use in the past 30 days declined from 23% before the pandemic to 20% during, with the respective figures for binge drinking in the past 2 weeks at 17% and 13%, and neither of those reductions reached significance, they noted.
“Adolescents may redouble their substance procurement efforts so that they can continue using substances at the levels at which they used in the past. In addition, adolescents may move to more solitary substance use. Social distancing policies might even increase substance use to the extent that they lead to feelings of isolation and loneliness that some adolescents address through increased substance use,” they suggested.
This hypothesis does not apply to vaping. The significant decline in availability – 73% before and 63% during – was accompanied by a significant drop in prevalence of past 30-day use from 24% to 17%, based on the survey data, which came from 3,770 responses to the first poll and 582 to the second.
In the case of vaping, the decline in use may have been caused by the decreased “exposure to substance-using peer networks ... and adults who provide opportunities for youth to initiate and continue use of substances,” Dr. Miech and associates said.
The findings of this analysis “suggest that reducing adolescent substance use through attempts to restrict supply alone would be a difficult undertaking,” Dr. Miech said in the NIDA statement. “The best strategy is likely to be one that combines approaches to limit the supply of these substances with efforts to decrease demand, through educational and public health campaigns.”
The research was funded by a NIDA grant. The investigators did not declare any conflicts of interest.
FROM DRUG AND ALCOHOL DEPENDENCE
Omnipod 5 ‘artificial pancreas’ shows benefit in type 1 diabetes
Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes aged as young as 2 years, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2-5.9 years with type 1 diabetes were presented during the annual scientific sessions of the American Diabetes Association.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7, 2021, in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the FDA, the Omnipod 5 would be the third commercially available automated insulin delivery system – also called hybrid closed-loop or artificial pancreas systems – in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
‘No-tubing’ feature will be a draw for parents of young children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, said in an interview: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the U.S.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Dr. Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t ... the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Dr. Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal data show benefit in ‘difficult-to-manage’ preschool children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale University, New Haven, Conn.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average hemoglobin A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs. –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Dr. Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Dr. Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing benefit seen in older children and adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Dr. Carlson and colleagues concluded.
Reduced diabetes distress, don’t forget parents’ quality of life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford (Calif.) University, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Dr. Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization–5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Dr. Hood said.
Dr. Jacobsen has reported no relevant financial relationships. Dr. Sherr has reported being an adviser for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
A version of this article first appeared on Medscape.com.
Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes aged as young as 2 years, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2-5.9 years with type 1 diabetes were presented during the annual scientific sessions of the American Diabetes Association.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7, 2021, in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the FDA, the Omnipod 5 would be the third commercially available automated insulin delivery system – also called hybrid closed-loop or artificial pancreas systems – in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
‘No-tubing’ feature will be a draw for parents of young children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, said in an interview: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the U.S.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Dr. Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t ... the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Dr. Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal data show benefit in ‘difficult-to-manage’ preschool children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale University, New Haven, Conn.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average hemoglobin A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs. –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Dr. Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Dr. Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing benefit seen in older children and adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Dr. Carlson and colleagues concluded.
Reduced diabetes distress, don’t forget parents’ quality of life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford (Calif.) University, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Dr. Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization–5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Dr. Hood said.
Dr. Jacobsen has reported no relevant financial relationships. Dr. Sherr has reported being an adviser for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
A version of this article first appeared on Medscape.com.
Insulet’s investigational Omnipod 5 automated insulin delivery system improves glycemic control in people with type 1 diabetes aged as young as 2 years, new data suggest.
The Omnipod 5 system combines a tubing-free insulin-filled delivery “Pod” with the Dexcom G6 continuous glucose monitor and an algorithm built into the Pod connecting the two devices via a smartphone app to semiautomate insulin delivery. It is currently under review by the Food and Drug Administration. The company expects to launch it in limited release during the second half of 2021.
Results from a pivotal trial of the system in children aged 2-5.9 years with type 1 diabetes were presented during the annual scientific sessions of the American Diabetes Association.
Follow-up data at 6 months were also presented for another pivotal study of 112 children aged 6-13.9 years and 129 adults aged 14-70 years. Those primary 3-month data were reported earlier this year at the Endocrine Society’s annual meeting and subsequently published online June 7, 2021, in Diabetes Care. Another study presented at ADA looked at quality of life in children using Omnipod 5 and their caregivers.
If approved by the FDA, the Omnipod 5 would be the third commercially available automated insulin delivery system – also called hybrid closed-loop or artificial pancreas systems – in the United States. It would be the second approved for children as young as 2 years of age and the first to deliver insulin subcutaneously without tubing.
‘No-tubing’ feature will be a draw for parents of young children
Asked to comment, pediatric endocrinologist Laura M. Jacobsen, MD, of the University of Florida, Gainesville, said in an interview: “I think the big advantage for the Omnipod 5 is that [if approved it will be] the only tubeless automated insulin delivery system in the U.S.”
“The automated delivery systems have just been wonderful for helping patients achieve time in range, especially overnight. And the fact that this goes down to such a young age where that can be very difficult is wonderful.”
Another difference between the Omnipod 5 and other systems is the ability to adjust glucose targets (from 110 to 150 mg/dL), although newer versions of the currently available hybrid closed-loop systems are expected to include that feature as well. “They’re all slightly different in the way the algorithms work, but I think the end result is similar,” Dr. Jacobsen said.
But, she said, the no-tubing feature might be particularly helpful for some very active young kids. “A lot of small kids do use the tubed pumps, and you can make it work with a lot of kids, but with some kids it just won’t ... the tubing gets caught. I think this really helps parents make the step. A lot of them don’t want to try the tubing whereas they see the Omnipod and might feel a little more confidence to try a pump.”
Overall, said Dr. Jacobsen, who has no financial disclosures with Insulet, Dexcom, or any of their competitors, “I think any addition to the technology field to improve quality of life for people with type 1 diabetes is important and people need choices.”
Pivotal data show benefit in ‘difficult-to-manage’ preschool children
Pivotal 3-month data for the Omnipod 5 in children aged 2-5.9 years with type 1 diabetes were presented on June 26 by pediatric endocrinologist Jennifer Sherr, MD, PhD, Yale University, New Haven, Conn.
“As a pediatric endocrinologist, I can attest to the difficulty of managing this age group, due to grazing eating patterns and erratic physical activity. Oftentimes, care providers may fear hypoglycemia as these youth can not verbalize or self-treat lows,” she remarked.
A total of 80 children were enrolled at 10 institutions across the United Sates. There was a single 14-day standard therapy phase (baseline), followed by 3 months of automated insulin delivery during which the children’s eating and exercise were unrestricted.
At 3 months, average hemoglobin A1c had fallen from 7.4% at baseline to 6.9%, a significant difference (P < .05). The proportions achieving the target A1c of less than 7% were 54% at 3 months versus 31% at baseline. The reduction was even greater among the 25 with baseline A1c of 8% or greater, although it was significant even among the 55 who started with a lower A1c (–1.06 vs. –0.31 percentage points; both P < .05).
Time in range rose from 57.2% at baseline to 68.1% at 3 months (P < .05).
“These youngsters are spending an average of 2.6 more hours/day in range,” Dr. Sherr commented, noting that the difference became apparent shortly after study start and was maintained during the 3 months.
Dr. Sherr noted that this 10.9% improvement in time in range with Omnipod 5 was similar to improvements in the previously reported pivotal study of older children and adults. Data from that study showed improvement in time in range from a gain of 15.6% for the 6 to 13.9 year olds to 8.0% for those aged 26-49 years. Interestingly, improvements in time in range were seen even in the oldest group, aged 50-70, who increased from an already high baseline of 69.9% to 79.1% with Omnipod 5 after 3 months.
In her current study, in the youngest age group, the improvement in time in range was achieved primarily by a reduction of time above range, from 2.4 fewer hours/day above 180 mg/dL, while time below 70 mg/dL was reduced by 4 minutes/day. Overnight time in range improved by 1.4 hours/night, with most of the improvements in reduction of hyperglycemia.
The proportions meeting the combined goals of less than 4% time below range and greater than 60% time in range rose from 29% to 65%.
There were no episodes of severe hypoglycemia or diabetic ketoacidosis during the 3-month study phase.
Another important related metric, sleep quality for parents/caregivers, also improved. The percentage reporting overall sleep quality of “very good” or “fairly good” increased from 65% at baseline to 90% with Omnipod 5, while “very bad” sleep quality fell from 8.8% to 0%.
All 80 patients completed the study and elected to continue in a 12-month extension phase.
Ongoing benefit seen in older children and adults
In a late-breaking poster presented on June 25, Anders L. Carlson, MD, medical director at the International Diabetes Center at Park Nicollet, Minneapolis, presented more follow-up data to the previously reported 3-month pivotal study, including 108 older children and 109 adults from the original study.
A1c remained lower after 6 months than at baseline for both children and adults (P < .001). In the children, A1c levels weren’t significantly different at the end of 6 versus 3 months, while in the adults there was an additional 0.1 percentage point decrease (P < .01).
There was one episode of diabetic ketoacidosis and no severe hypoglycemic episodes in the 3-month extension. “Sustained reduction of A1c indicates the potential long-term benefit of the Omnipod 5 System,” Dr. Carlson and colleagues concluded.
Reduced diabetes distress, don’t forget parents’ quality of life
Meanwhile, psychologist Korey K. Hood, PhD, of Stanford (Calif.) University, presented quality of life data at the meeting for 83 children aged 6-11.9 years and 42 teens aged 12-17.9 years using the Omnipod 5 from the larger study population and their parents.
Significant improvements were seen for both the youth and their caregivers in the Problem Areas in Diabetes score, a measure of diabetes-related emotional distress. Changes were less dramatic on the Hypoglycemic Confidence Scale, although improvements were significant for the caregivers of the younger children.
“We know this is a group that is really worried about hypoglycemia across a lot of situations, not just sleep but also school and outside of the home. So, to increase their confidence to this extent I think is a pretty important finding,” Dr. Hood commented.
There were nonsignificant trends in improvement across groups on the Pittsburgh Sleep Quality Index, but overall sleep quality did significantly improve among parents of the younger children. And on the World Health Organization–5 quality of life survey, significant improvements again were seen among the caregivers of young children.
“Reduced diabetes distress and improved quality of life are key benefits of using the Omnipod 5 [automated insulin delivery] system that are complementary to the glycemic benefits achieved,” Dr. Hood said.
Dr. Jacobsen has reported no relevant financial relationships. Dr. Sherr has reported being an adviser for, consultant for, and/or grant recipient from Bigfoot Biomedical, Cecelia Health, Insulet, Medtronic Diabetes, Eli Lilly, Lexicon, Sanofi, and the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Hood has reported being a consultant for Cecelia Health, Havas, and Cercacor.
A version of this article first appeared on Medscape.com.
Intervention opens access to care for minority youths with type 1 diabetes
For racial or ethnic minority youths with type 1 diabetes, participating in an interventional program improves access to care, new research shows.
Youth categorized as Black, Indigenous, and other people of color (BIPOC) had significantly improved outpatient attendance during and after participating in Novel Interventions in Children’s Healthcare (NICH), a systems intervention for children with chronic health conditions and their families.
By comparison, no improvements in care access were observed among BIPOC children who were not able to access the program because of insurance or other reasons, David V. Wagner, PhD, Associate Professor and NICH research director at Oregon Health & Science University, Portland, reported at the annual scientific sessions of the American Diabetes Association.
The findings demonstrate a need for intensive, home-based services that aim to correct health inequities, said Dr. Wagner, who presented the findings along with Winniebhelle Cadiz, a scholar in the BUILD EXITO undergraduate research training program at Portland (Ore.) State University.
The NICH program hinges on trained interventionists who visit families at home, attend clinic visits, and work with schools and other contacts to help solve problems that keep children from following medical instructions, according to a program description.
“Families report having somebody by their side to help them navigate the system, address the transportation difficulties experienced, and help them and build that relationship with their health care provider seems to be hugely influential in terms of helping them navigate and access care,” Dr. Wagner said in a presentation of the study.
A NICH for youths with chronic health conditions
The NICH program differs from some other programs that have been developed in an attempt to improve health outcomes among youths in the community, according to Dr. Wagner.
“Many of the programs that exist out there are often piloted on, and seemingly built for, those who have more resources,” he said in his presentation. “Those who are in greatest need often have difficulty accessing and responding to the services.”
NICH doesn’t take the place of existing services, but is “an addition to the continuum of care” for youths and families who are struggling because of lack of resources or marginalization in the health care system, Dr. Wagner said.
While NICH is not specific to any one chronic health condition, several previous investigations have specifically looked at the impact of the NICH program on access to care in youths with type 1 diabetes.
Youths participating in the program for a year had fewer ED visits, including fewer visits with diabetic ketoacidosis (DKA), as well as fewer and shorter admissions as compared with the year prior to participating in the program, Dr. Wagner said.
In another study, youths had fewer admissions for diabetes or DKA and less frequent pediatric ICU contact during the NICH program, as compared with before the program.
Another study showed that, while NICH had no impact overall on access to care among youths with type 1 diabetes, BIPOC youths had an improvement in the mean number of outpatient visits as compared with preprogram levels. However, because none of those studies included a control group, Dr. Wagner said, it remained unclear whether this systems intervention might improve outpatient access among youths with type 1 diabetes as compared with those who did not participate.
Intervention linked to increased BIPOC care access
The latest study includes 144 youths with type 1 diabetes referred for the program. The mean age was 13.7 years, 58% were female, and 81% were non-Hispanic White. While 51 youths were able to participate in NICH, the remaining 93 were not served by the program because of insurance denial or nonresponse, according to investigators.
While participation in the program made no difference in access to care overall, results of this study suggest NICH reduced access disparities among BIPOC youths, the investigators said.
Those BIPOC youth, 28 in total, had significantly worse access to care prior to referral. However, BIPOC youth participation in NICH was associated with improved attendance at endocrinology appointments and outpatient attendance overall.
A mean change of 1.9 more appointments per year was seen among BIPOC youth who participated in NICH, compared with a mean decrease of 0.5 appointments per year among BIPOC youth not served by the program (P = .03), according to the study abstract.
Prior to NICH participation, outpatient attendance among BIPOC youths was about 2.5 visits per year, data presented by the investigators show.
Systemic changes needed
This study is representative of systemic changes that are needed to improve access to quality care for BIPOC youth, according Cynthia E. Muñoz, PhD, MPH, ADA’s president of health care and education.
“We know that there are increased risks for poor health outcomes for these children and youths, and we know that there is a risk for mental health and psychosocial challenges for youth from these communities,” said Dr. Muñoz, a bilingual licensed psychologist and assistant professor of clinical pediatrics at the University of Southern California, Los Angeles.
In his presentation, Dr. Wagner said lumping racial and ethnic minority participants under a single BIPOC header probably wasn’t ideal because of the diversity and differences among racial and ethnic minorities. However, it was necessary in this particular study because of limited sample size.
Dr. Wagner and coauthors disclosed no conflicts of interest related to the research, which was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
For racial or ethnic minority youths with type 1 diabetes, participating in an interventional program improves access to care, new research shows.
Youth categorized as Black, Indigenous, and other people of color (BIPOC) had significantly improved outpatient attendance during and after participating in Novel Interventions in Children’s Healthcare (NICH), a systems intervention for children with chronic health conditions and their families.
By comparison, no improvements in care access were observed among BIPOC children who were not able to access the program because of insurance or other reasons, David V. Wagner, PhD, Associate Professor and NICH research director at Oregon Health & Science University, Portland, reported at the annual scientific sessions of the American Diabetes Association.
The findings demonstrate a need for intensive, home-based services that aim to correct health inequities, said Dr. Wagner, who presented the findings along with Winniebhelle Cadiz, a scholar in the BUILD EXITO undergraduate research training program at Portland (Ore.) State University.
The NICH program hinges on trained interventionists who visit families at home, attend clinic visits, and work with schools and other contacts to help solve problems that keep children from following medical instructions, according to a program description.
“Families report having somebody by their side to help them navigate the system, address the transportation difficulties experienced, and help them and build that relationship with their health care provider seems to be hugely influential in terms of helping them navigate and access care,” Dr. Wagner said in a presentation of the study.
A NICH for youths with chronic health conditions
The NICH program differs from some other programs that have been developed in an attempt to improve health outcomes among youths in the community, according to Dr. Wagner.
“Many of the programs that exist out there are often piloted on, and seemingly built for, those who have more resources,” he said in his presentation. “Those who are in greatest need often have difficulty accessing and responding to the services.”
NICH doesn’t take the place of existing services, but is “an addition to the continuum of care” for youths and families who are struggling because of lack of resources or marginalization in the health care system, Dr. Wagner said.
While NICH is not specific to any one chronic health condition, several previous investigations have specifically looked at the impact of the NICH program on access to care in youths with type 1 diabetes.
Youths participating in the program for a year had fewer ED visits, including fewer visits with diabetic ketoacidosis (DKA), as well as fewer and shorter admissions as compared with the year prior to participating in the program, Dr. Wagner said.
In another study, youths had fewer admissions for diabetes or DKA and less frequent pediatric ICU contact during the NICH program, as compared with before the program.
Another study showed that, while NICH had no impact overall on access to care among youths with type 1 diabetes, BIPOC youths had an improvement in the mean number of outpatient visits as compared with preprogram levels. However, because none of those studies included a control group, Dr. Wagner said, it remained unclear whether this systems intervention might improve outpatient access among youths with type 1 diabetes as compared with those who did not participate.
Intervention linked to increased BIPOC care access
The latest study includes 144 youths with type 1 diabetes referred for the program. The mean age was 13.7 years, 58% were female, and 81% were non-Hispanic White. While 51 youths were able to participate in NICH, the remaining 93 were not served by the program because of insurance denial or nonresponse, according to investigators.
While participation in the program made no difference in access to care overall, results of this study suggest NICH reduced access disparities among BIPOC youths, the investigators said.
Those BIPOC youth, 28 in total, had significantly worse access to care prior to referral. However, BIPOC youth participation in NICH was associated with improved attendance at endocrinology appointments and outpatient attendance overall.
A mean change of 1.9 more appointments per year was seen among BIPOC youth who participated in NICH, compared with a mean decrease of 0.5 appointments per year among BIPOC youth not served by the program (P = .03), according to the study abstract.
Prior to NICH participation, outpatient attendance among BIPOC youths was about 2.5 visits per year, data presented by the investigators show.
Systemic changes needed
This study is representative of systemic changes that are needed to improve access to quality care for BIPOC youth, according Cynthia E. Muñoz, PhD, MPH, ADA’s president of health care and education.
“We know that there are increased risks for poor health outcomes for these children and youths, and we know that there is a risk for mental health and psychosocial challenges for youth from these communities,” said Dr. Muñoz, a bilingual licensed psychologist and assistant professor of clinical pediatrics at the University of Southern California, Los Angeles.
In his presentation, Dr. Wagner said lumping racial and ethnic minority participants under a single BIPOC header probably wasn’t ideal because of the diversity and differences among racial and ethnic minorities. However, it was necessary in this particular study because of limited sample size.
Dr. Wagner and coauthors disclosed no conflicts of interest related to the research, which was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
For racial or ethnic minority youths with type 1 diabetes, participating in an interventional program improves access to care, new research shows.
Youth categorized as Black, Indigenous, and other people of color (BIPOC) had significantly improved outpatient attendance during and after participating in Novel Interventions in Children’s Healthcare (NICH), a systems intervention for children with chronic health conditions and their families.
By comparison, no improvements in care access were observed among BIPOC children who were not able to access the program because of insurance or other reasons, David V. Wagner, PhD, Associate Professor and NICH research director at Oregon Health & Science University, Portland, reported at the annual scientific sessions of the American Diabetes Association.
The findings demonstrate a need for intensive, home-based services that aim to correct health inequities, said Dr. Wagner, who presented the findings along with Winniebhelle Cadiz, a scholar in the BUILD EXITO undergraduate research training program at Portland (Ore.) State University.
The NICH program hinges on trained interventionists who visit families at home, attend clinic visits, and work with schools and other contacts to help solve problems that keep children from following medical instructions, according to a program description.
“Families report having somebody by their side to help them navigate the system, address the transportation difficulties experienced, and help them and build that relationship with their health care provider seems to be hugely influential in terms of helping them navigate and access care,” Dr. Wagner said in a presentation of the study.
A NICH for youths with chronic health conditions
The NICH program differs from some other programs that have been developed in an attempt to improve health outcomes among youths in the community, according to Dr. Wagner.
“Many of the programs that exist out there are often piloted on, and seemingly built for, those who have more resources,” he said in his presentation. “Those who are in greatest need often have difficulty accessing and responding to the services.”
NICH doesn’t take the place of existing services, but is “an addition to the continuum of care” for youths and families who are struggling because of lack of resources or marginalization in the health care system, Dr. Wagner said.
While NICH is not specific to any one chronic health condition, several previous investigations have specifically looked at the impact of the NICH program on access to care in youths with type 1 diabetes.
Youths participating in the program for a year had fewer ED visits, including fewer visits with diabetic ketoacidosis (DKA), as well as fewer and shorter admissions as compared with the year prior to participating in the program, Dr. Wagner said.
In another study, youths had fewer admissions for diabetes or DKA and less frequent pediatric ICU contact during the NICH program, as compared with before the program.
Another study showed that, while NICH had no impact overall on access to care among youths with type 1 diabetes, BIPOC youths had an improvement in the mean number of outpatient visits as compared with preprogram levels. However, because none of those studies included a control group, Dr. Wagner said, it remained unclear whether this systems intervention might improve outpatient access among youths with type 1 diabetes as compared with those who did not participate.
Intervention linked to increased BIPOC care access
The latest study includes 144 youths with type 1 diabetes referred for the program. The mean age was 13.7 years, 58% were female, and 81% were non-Hispanic White. While 51 youths were able to participate in NICH, the remaining 93 were not served by the program because of insurance denial or nonresponse, according to investigators.
While participation in the program made no difference in access to care overall, results of this study suggest NICH reduced access disparities among BIPOC youths, the investigators said.
Those BIPOC youth, 28 in total, had significantly worse access to care prior to referral. However, BIPOC youth participation in NICH was associated with improved attendance at endocrinology appointments and outpatient attendance overall.
A mean change of 1.9 more appointments per year was seen among BIPOC youth who participated in NICH, compared with a mean decrease of 0.5 appointments per year among BIPOC youth not served by the program (P = .03), according to the study abstract.
Prior to NICH participation, outpatient attendance among BIPOC youths was about 2.5 visits per year, data presented by the investigators show.
Systemic changes needed
This study is representative of systemic changes that are needed to improve access to quality care for BIPOC youth, according Cynthia E. Muñoz, PhD, MPH, ADA’s president of health care and education.
“We know that there are increased risks for poor health outcomes for these children and youths, and we know that there is a risk for mental health and psychosocial challenges for youth from these communities,” said Dr. Muñoz, a bilingual licensed psychologist and assistant professor of clinical pediatrics at the University of Southern California, Los Angeles.
In his presentation, Dr. Wagner said lumping racial and ethnic minority participants under a single BIPOC header probably wasn’t ideal because of the diversity and differences among racial and ethnic minorities. However, it was necessary in this particular study because of limited sample size.
Dr. Wagner and coauthors disclosed no conflicts of interest related to the research, which was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
FROM ADA 2021
‘Staggering’ doubling of type 2 diabetes in children during pandemic
The incidence of type 2 diabetes in children appears to have doubled during the COVID-19 pandemic, data from two new U.S. studies suggest, with the lead investigator of one saying she was “surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Findings from the two separate retrospective chart reviews – one conducted in Washington, D.C., and the other in Baton Rouge, La. – were presented June 25 at the annual scientific sessions of the American Diabetes Association.
Although the two studies differed somewhat in the clinical parameters examined, both revealed a similar doubling of the rates of hospitalizations for type 2 diabetes among youth during 2020, compared with the same time period in 2019, as well as greater severity of metabolic disturbance.
And, as has been previously described with type 2 diabetes in youth, African American ethnicity predominated in both cohorts.
“Although we could not assess the cause of the increases in type 2 diabetes from our data, these disparities suggest that indirect effects of social distancing measures, including school closure and unemployment, are placing undue burden on underserved communities. Decreases in well-child care and fears of seeking medical care during the pandemic may have also contributed,” lead investigator of one of the studies, pediatric endocrinologist Brynn E. Marks, MD, Children’s National Hospital, Washington, said in an interview.
More hospitalizations, racial disparities aggravated by COVID-19
Lead author of the other study, Daniel S. Hsia, MD, Pennington Biomedical Research Center, Baton Rouge, said in an interview: “Since the pandemic, our data suggest that more children may be diagnosed with type 2 diabetes and may require hospitalization when they are diagnosed. Looking at both datasets, there appears to be a racial disparity in type 2 diabetes diagnoses that has only been exacerbated by the COVID-19 pandemic.”
Of concern, Dr. Hsia said, “The incidence rate of type 2 diabetes in children was already on the rise before the pandemic. While there may be a brief leveling off now that children are getting regular health care and going back to school in person, I believe these rates will continue to rise especially in light of the childhood obesity rates not improving.”
Their dataset captured all youth who were newly diagnosed with type 2 diabetes during the first full year of the COVID-19 pandemic, from March 11, 2020, to March 10, 2021, and compared those data with the time period from March 11, 2019, to March 10, 2020.
During the pandemic, the number of cases of type 2 diabetes increased by 182%, from 50 in 2019 to 141 in 2020. The average age at diagnosis was about 14 years in both time periods.
In the prepandemic period, 18 (36%) diagnosed with type 2 diabetes required inpatient admission, compared with 85 (60.3%) during the pandemic. At Children’s National, youth with suspected new-onset type 2 diabetes aren’t typically hospitalized unless they have severe hyperglycemia, ketosis, or are unable to schedule urgent outpatient follow-up, Dr. Marks noted.
The proportions of youth with new-onset type 2 diabetes who presented in diabetic ketoacidosis (DKA) rose from 2 (4%) prepandemic to 33 (23.4%) during the pandemic. Presentation with hyperosmolar DKA rose from 0 to 13 (9.2%).
However, during the pandemic only five youth were actively infected with SARS-CoV-2 at the time of type 2 diabetes diagnosis among the 90 tested.
Dr. Marks said: “We believe the increase in inpatient admissions was due to more severe presentation during the pandemic. ...We were surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Shift in diagnoses to type 2 diabetes
The pandemic also appears to have shifted the proportion of youth diagnosed with type 2 diabetes, compared with type 1 diabetes. Whereas 24% of youth with new-onset diabetes prepandemic had type 2 diabetes and the rest had type 1 diabetes, during pandemic the proportion with type 2 diabetes rose to 44%.
“Rates of type 2 diabetes rose steadily at a rate of 1.45 cases per month throughout the course of the pandemic, suggesting a cumulative effect of the indirect effects of social distancing measures,” Dr. Marks said.
Furthermore, she added, whereas 60% of youth diagnosed with type 2 diabetes before the pandemic were female, the rate fell to 40% during the pandemic. This trend might be because of activity levels in that, while male adolescents are typically more active, rates of exercise fell in both sexes during the pandemic but declined more sharply in males such that activity levels between the sexes became equal.
Although type 2 diabetes in youth has always been more common in ethnic minorities, the pandemic appears to have exacerbated these disparities.
While 58% of youth diagnosed with type 2 diabetes prepandemic identified as non-Hispanic Black, that proportion rose to 76.7% during the pandemic. Among Black youth with new-onset type 2 diabetes, 31 of 33 presented in DKA, and 12 of the 13 who presented in hyperosmolar DKA during the pandemic were Black.
“Strategies to promote health equity and address the undue burden of the COVID-19 pandemic on underserved communities must be developed to avoid worsening disparities and long-term health outcomes,” Dr. Marks said.
‘A microcosm’: Similar findings in a smaller population
Dr. Hsia and colleagues looked at a smaller number of patients in a shorter time period. In March–December 2019, the hospitalization rate for new-onset type 2 diabetes was 0.27% (8 out of 2,964 hospitalizations), compared with 0.62% (17 out of 2,729 hospitalizations) during the same period in 2020 (P < .048) – also more than a doubling. Age at admission, sex, and body mass index didn’t differ between the two groups.
Criteria for DKA were met by three children in 2019 versus eight in 2020, and hyperosmolar hyperglycemic syndrome in zero versus two, respectively. Mean hemoglobin A1c on admission was 12.4% in 2019 versus 13.1% in 2020 (P = .59), and mean serum glucose was 441 mg/dL versus 669 mg/dL (P = .14), respectively. Serum osmolality on admission was 314 mmol/kg in 2019 versus 335 mmol/kg in 2020 (P = .19).
“Clinically speaking the differences in the lab values were significant, but we did not have enough numbers ... to see a statistically significant difference. I think by looking at more centers, our site likely represents a microcosm of what is happening across the country,” Dr. Hsia said.
In 2019, 7 of the 8 children were African American, as were 16 of the 17 children in 2020. The other single child in each group was White.
Dr. Hsia said: “Larger studies that include more patients are needed to confirm our initial findings. More research is needed to understand why this increasing trend of type 2 diabetes diagnoses in children may be occurring [and] to better understand how stay-at-home orders and other restrictions due to COVID-19 have worsened risk factors for type 2 diabetes.”
“These include decreased physical activity, more screen time, disturbed sleep, and increased intake of processed foods, which can all lead to weight gain,” he concluded.
Dr. Marks reported receiving research support from Tandem, Dexcom, and the Cystic Fibrosis Foundation. Dr. Hsia reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The incidence of type 2 diabetes in children appears to have doubled during the COVID-19 pandemic, data from two new U.S. studies suggest, with the lead investigator of one saying she was “surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Findings from the two separate retrospective chart reviews – one conducted in Washington, D.C., and the other in Baton Rouge, La. – were presented June 25 at the annual scientific sessions of the American Diabetes Association.
Although the two studies differed somewhat in the clinical parameters examined, both revealed a similar doubling of the rates of hospitalizations for type 2 diabetes among youth during 2020, compared with the same time period in 2019, as well as greater severity of metabolic disturbance.
And, as has been previously described with type 2 diabetes in youth, African American ethnicity predominated in both cohorts.
“Although we could not assess the cause of the increases in type 2 diabetes from our data, these disparities suggest that indirect effects of social distancing measures, including school closure and unemployment, are placing undue burden on underserved communities. Decreases in well-child care and fears of seeking medical care during the pandemic may have also contributed,” lead investigator of one of the studies, pediatric endocrinologist Brynn E. Marks, MD, Children’s National Hospital, Washington, said in an interview.
More hospitalizations, racial disparities aggravated by COVID-19
Lead author of the other study, Daniel S. Hsia, MD, Pennington Biomedical Research Center, Baton Rouge, said in an interview: “Since the pandemic, our data suggest that more children may be diagnosed with type 2 diabetes and may require hospitalization when they are diagnosed. Looking at both datasets, there appears to be a racial disparity in type 2 diabetes diagnoses that has only been exacerbated by the COVID-19 pandemic.”
Of concern, Dr. Hsia said, “The incidence rate of type 2 diabetes in children was already on the rise before the pandemic. While there may be a brief leveling off now that children are getting regular health care and going back to school in person, I believe these rates will continue to rise especially in light of the childhood obesity rates not improving.”
Their dataset captured all youth who were newly diagnosed with type 2 diabetes during the first full year of the COVID-19 pandemic, from March 11, 2020, to March 10, 2021, and compared those data with the time period from March 11, 2019, to March 10, 2020.
During the pandemic, the number of cases of type 2 diabetes increased by 182%, from 50 in 2019 to 141 in 2020. The average age at diagnosis was about 14 years in both time periods.
In the prepandemic period, 18 (36%) diagnosed with type 2 diabetes required inpatient admission, compared with 85 (60.3%) during the pandemic. At Children’s National, youth with suspected new-onset type 2 diabetes aren’t typically hospitalized unless they have severe hyperglycemia, ketosis, or are unable to schedule urgent outpatient follow-up, Dr. Marks noted.
The proportions of youth with new-onset type 2 diabetes who presented in diabetic ketoacidosis (DKA) rose from 2 (4%) prepandemic to 33 (23.4%) during the pandemic. Presentation with hyperosmolar DKA rose from 0 to 13 (9.2%).
However, during the pandemic only five youth were actively infected with SARS-CoV-2 at the time of type 2 diabetes diagnosis among the 90 tested.
Dr. Marks said: “We believe the increase in inpatient admissions was due to more severe presentation during the pandemic. ...We were surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Shift in diagnoses to type 2 diabetes
The pandemic also appears to have shifted the proportion of youth diagnosed with type 2 diabetes, compared with type 1 diabetes. Whereas 24% of youth with new-onset diabetes prepandemic had type 2 diabetes and the rest had type 1 diabetes, during pandemic the proportion with type 2 diabetes rose to 44%.
“Rates of type 2 diabetes rose steadily at a rate of 1.45 cases per month throughout the course of the pandemic, suggesting a cumulative effect of the indirect effects of social distancing measures,” Dr. Marks said.
Furthermore, she added, whereas 60% of youth diagnosed with type 2 diabetes before the pandemic were female, the rate fell to 40% during the pandemic. This trend might be because of activity levels in that, while male adolescents are typically more active, rates of exercise fell in both sexes during the pandemic but declined more sharply in males such that activity levels between the sexes became equal.
Although type 2 diabetes in youth has always been more common in ethnic minorities, the pandemic appears to have exacerbated these disparities.
While 58% of youth diagnosed with type 2 diabetes prepandemic identified as non-Hispanic Black, that proportion rose to 76.7% during the pandemic. Among Black youth with new-onset type 2 diabetes, 31 of 33 presented in DKA, and 12 of the 13 who presented in hyperosmolar DKA during the pandemic were Black.
“Strategies to promote health equity and address the undue burden of the COVID-19 pandemic on underserved communities must be developed to avoid worsening disparities and long-term health outcomes,” Dr. Marks said.
‘A microcosm’: Similar findings in a smaller population
Dr. Hsia and colleagues looked at a smaller number of patients in a shorter time period. In March–December 2019, the hospitalization rate for new-onset type 2 diabetes was 0.27% (8 out of 2,964 hospitalizations), compared with 0.62% (17 out of 2,729 hospitalizations) during the same period in 2020 (P < .048) – also more than a doubling. Age at admission, sex, and body mass index didn’t differ between the two groups.
Criteria for DKA were met by three children in 2019 versus eight in 2020, and hyperosmolar hyperglycemic syndrome in zero versus two, respectively. Mean hemoglobin A1c on admission was 12.4% in 2019 versus 13.1% in 2020 (P = .59), and mean serum glucose was 441 mg/dL versus 669 mg/dL (P = .14), respectively. Serum osmolality on admission was 314 mmol/kg in 2019 versus 335 mmol/kg in 2020 (P = .19).
“Clinically speaking the differences in the lab values were significant, but we did not have enough numbers ... to see a statistically significant difference. I think by looking at more centers, our site likely represents a microcosm of what is happening across the country,” Dr. Hsia said.
In 2019, 7 of the 8 children were African American, as were 16 of the 17 children in 2020. The other single child in each group was White.
Dr. Hsia said: “Larger studies that include more patients are needed to confirm our initial findings. More research is needed to understand why this increasing trend of type 2 diabetes diagnoses in children may be occurring [and] to better understand how stay-at-home orders and other restrictions due to COVID-19 have worsened risk factors for type 2 diabetes.”
“These include decreased physical activity, more screen time, disturbed sleep, and increased intake of processed foods, which can all lead to weight gain,” he concluded.
Dr. Marks reported receiving research support from Tandem, Dexcom, and the Cystic Fibrosis Foundation. Dr. Hsia reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The incidence of type 2 diabetes in children appears to have doubled during the COVID-19 pandemic, data from two new U.S. studies suggest, with the lead investigator of one saying she was “surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Findings from the two separate retrospective chart reviews – one conducted in Washington, D.C., and the other in Baton Rouge, La. – were presented June 25 at the annual scientific sessions of the American Diabetes Association.
Although the two studies differed somewhat in the clinical parameters examined, both revealed a similar doubling of the rates of hospitalizations for type 2 diabetes among youth during 2020, compared with the same time period in 2019, as well as greater severity of metabolic disturbance.
And, as has been previously described with type 2 diabetes in youth, African American ethnicity predominated in both cohorts.
“Although we could not assess the cause of the increases in type 2 diabetes from our data, these disparities suggest that indirect effects of social distancing measures, including school closure and unemployment, are placing undue burden on underserved communities. Decreases in well-child care and fears of seeking medical care during the pandemic may have also contributed,” lead investigator of one of the studies, pediatric endocrinologist Brynn E. Marks, MD, Children’s National Hospital, Washington, said in an interview.
More hospitalizations, racial disparities aggravated by COVID-19
Lead author of the other study, Daniel S. Hsia, MD, Pennington Biomedical Research Center, Baton Rouge, said in an interview: “Since the pandemic, our data suggest that more children may be diagnosed with type 2 diabetes and may require hospitalization when they are diagnosed. Looking at both datasets, there appears to be a racial disparity in type 2 diabetes diagnoses that has only been exacerbated by the COVID-19 pandemic.”
Of concern, Dr. Hsia said, “The incidence rate of type 2 diabetes in children was already on the rise before the pandemic. While there may be a brief leveling off now that children are getting regular health care and going back to school in person, I believe these rates will continue to rise especially in light of the childhood obesity rates not improving.”
Their dataset captured all youth who were newly diagnosed with type 2 diabetes during the first full year of the COVID-19 pandemic, from March 11, 2020, to March 10, 2021, and compared those data with the time period from March 11, 2019, to March 10, 2020.
During the pandemic, the number of cases of type 2 diabetes increased by 182%, from 50 in 2019 to 141 in 2020. The average age at diagnosis was about 14 years in both time periods.
In the prepandemic period, 18 (36%) diagnosed with type 2 diabetes required inpatient admission, compared with 85 (60.3%) during the pandemic. At Children’s National, youth with suspected new-onset type 2 diabetes aren’t typically hospitalized unless they have severe hyperglycemia, ketosis, or are unable to schedule urgent outpatient follow-up, Dr. Marks noted.
The proportions of youth with new-onset type 2 diabetes who presented in diabetic ketoacidosis (DKA) rose from 2 (4%) prepandemic to 33 (23.4%) during the pandemic. Presentation with hyperosmolar DKA rose from 0 to 13 (9.2%).
However, during the pandemic only five youth were actively infected with SARS-CoV-2 at the time of type 2 diabetes diagnosis among the 90 tested.
Dr. Marks said: “We believe the increase in inpatient admissions was due to more severe presentation during the pandemic. ...We were surprised by the staggering increase in cases of type 2 diabetes ... and the increase in severity of presentation.”
Shift in diagnoses to type 2 diabetes
The pandemic also appears to have shifted the proportion of youth diagnosed with type 2 diabetes, compared with type 1 diabetes. Whereas 24% of youth with new-onset diabetes prepandemic had type 2 diabetes and the rest had type 1 diabetes, during pandemic the proportion with type 2 diabetes rose to 44%.
“Rates of type 2 diabetes rose steadily at a rate of 1.45 cases per month throughout the course of the pandemic, suggesting a cumulative effect of the indirect effects of social distancing measures,” Dr. Marks said.
Furthermore, she added, whereas 60% of youth diagnosed with type 2 diabetes before the pandemic were female, the rate fell to 40% during the pandemic. This trend might be because of activity levels in that, while male adolescents are typically more active, rates of exercise fell in both sexes during the pandemic but declined more sharply in males such that activity levels between the sexes became equal.
Although type 2 diabetes in youth has always been more common in ethnic minorities, the pandemic appears to have exacerbated these disparities.
While 58% of youth diagnosed with type 2 diabetes prepandemic identified as non-Hispanic Black, that proportion rose to 76.7% during the pandemic. Among Black youth with new-onset type 2 diabetes, 31 of 33 presented in DKA, and 12 of the 13 who presented in hyperosmolar DKA during the pandemic were Black.
“Strategies to promote health equity and address the undue burden of the COVID-19 pandemic on underserved communities must be developed to avoid worsening disparities and long-term health outcomes,” Dr. Marks said.
‘A microcosm’: Similar findings in a smaller population
Dr. Hsia and colleagues looked at a smaller number of patients in a shorter time period. In March–December 2019, the hospitalization rate for new-onset type 2 diabetes was 0.27% (8 out of 2,964 hospitalizations), compared with 0.62% (17 out of 2,729 hospitalizations) during the same period in 2020 (P < .048) – also more than a doubling. Age at admission, sex, and body mass index didn’t differ between the two groups.
Criteria for DKA were met by three children in 2019 versus eight in 2020, and hyperosmolar hyperglycemic syndrome in zero versus two, respectively. Mean hemoglobin A1c on admission was 12.4% in 2019 versus 13.1% in 2020 (P = .59), and mean serum glucose was 441 mg/dL versus 669 mg/dL (P = .14), respectively. Serum osmolality on admission was 314 mmol/kg in 2019 versus 335 mmol/kg in 2020 (P = .19).
“Clinically speaking the differences in the lab values were significant, but we did not have enough numbers ... to see a statistically significant difference. I think by looking at more centers, our site likely represents a microcosm of what is happening across the country,” Dr. Hsia said.
In 2019, 7 of the 8 children were African American, as were 16 of the 17 children in 2020. The other single child in each group was White.
Dr. Hsia said: “Larger studies that include more patients are needed to confirm our initial findings. More research is needed to understand why this increasing trend of type 2 diabetes diagnoses in children may be occurring [and] to better understand how stay-at-home orders and other restrictions due to COVID-19 have worsened risk factors for type 2 diabetes.”
“These include decreased physical activity, more screen time, disturbed sleep, and increased intake of processed foods, which can all lead to weight gain,” he concluded.
Dr. Marks reported receiving research support from Tandem, Dexcom, and the Cystic Fibrosis Foundation. Dr. Hsia reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Average childbirth costs more than $3,000 out of pocket with private insurance
Families with private health insurance pay around $3,000 for newborn delivery and hospitalization, while adding neonatal intensive care can push the bill closer to $5,000, based on a retrospective look at almost 400,000 episodes.
The findings suggest that privately insured families need prenatal financial counseling, as well as screening for financial hardship after delivery, reported lead author Kao-Ping Chua, MD, PhD, assistant professor and health policy researcher in the department of pediatrics and the Susan B. Meister Child Health Evaluation and Research Center at the University of Michigan, Ann Arbor, and colleagues.
“Concern is growing regarding the high and rising financial burden of childbirth for privately insured families,” the investigators wrote in Pediatrics. “Previous studies assessing this burden have focused on out-of-pocket spending for maternal care, including hospitalizations for delivery. However, there are no recent national data on out-of-pocket spending across the childbirth episode, including both deliveries and newborn hospitalizations.”
To address this knowledge gap, Dr. Chua and colleagues turned to Optum’s deidentified Clinformatics Data Mart, comprising 12 million privately insured individuals across the United States. The investigators identified 398,410 childbirth episodes occurring between 2016 and 2019. Each episode was defined as one delivery and at least one newborn hospitalization under the same family plan.
Out-of-pocket cost included copayment plus coinsurance and deductibles. Primary outcomes included mean total out-of-pocket spending and proportion of episodes exceeding $5,000 or $10,000. Subgroup analyses compared differences in spending between episodes involving neonatal intensive care or cesarean birth.
The mean out-of-pocket spending was $2,281 for delivery and $788 for newborn hospitalization, giving a total of $3,068 per childbirth episode. Coinsurance and deductibles accounted for much of that cost, at 55.8% and 42.1%, respectively, whereas copayments accounted for a relatively minor portion (2.2%).
Almost all episodes (95%) cost more than zero dollars, while 17.1% cost more than $5,000 and 1.0% cost more than $10,000. Total mean out-of-pocket spending was higher for episodes involving cesarean birth ($3,389) or neonatal intensive care ($4,969), the latter of which cost more than $10,000 in 8.8% of episodes.
“Because details on plan benefit design were unavailable, the generalizability of findings to all privately insured Americans is unclear,” the investigators noted. “However, the proportion of childbirth episodes covered by high-deductible health plans in this study is consistent with the prevalence of such plans among Americans with employer-sponsored insurance.”
The findings suggest that financial reform is needed, Dr. Chua and colleagues concluded.
“To avoid imposing undue financial burden on families, private insurers should improve childbirth coverage,” they wrote. “An incremental step would be providing first-dollar coverage of deliveries and newborn hospitalizations before deductibles are met. Ideally, however, insurers would waive most or all cost-sharing for these hospitalizations, consistent with the approach taken by Medicaid programs and many developed countries.”
According to Madeline Sutton, MD, assistant professor of obstetrics and gynecology at Morehouse School of Medicine, Atlanta, the size of the study is commendable, but some details are lacking.
“Although the overall sample size allows for a robust analysis, deciding to not report the confidence intervals in this report does not allow for understanding of [the findings with] smaller sample sizes,” Dr. Sutton said in an interview.
(Dr. Chua and colleagues noted that they did not report confidence intervals because “all differences between subgroups were significant owing to large sample sizes.”)
“Still,” Dr. Sutton went on, “this is an important study that has implications for financial counseling that may need to be a part of preconceptional, prenatal, and postnatal visits for privately insured families to help with planning and to decrease the chances of childbirth-related financial hardships. Additionally, policy-level changes that decrease or eliminate these private insurance–related childbirth-episode costs that may negatively impact some families with lower incomes, are warranted.”
The study was funded by the National Institutes of Health. Dr. Chua disclosed a grant from the National Institute on Drug Abuse, while Dr. Moniz is supported by the Agency for Healthcare Research and Quality. Dr. Sutton had no relevant disclosures.
Families with private health insurance pay around $3,000 for newborn delivery and hospitalization, while adding neonatal intensive care can push the bill closer to $5,000, based on a retrospective look at almost 400,000 episodes.
The findings suggest that privately insured families need prenatal financial counseling, as well as screening for financial hardship after delivery, reported lead author Kao-Ping Chua, MD, PhD, assistant professor and health policy researcher in the department of pediatrics and the Susan B. Meister Child Health Evaluation and Research Center at the University of Michigan, Ann Arbor, and colleagues.
“Concern is growing regarding the high and rising financial burden of childbirth for privately insured families,” the investigators wrote in Pediatrics. “Previous studies assessing this burden have focused on out-of-pocket spending for maternal care, including hospitalizations for delivery. However, there are no recent national data on out-of-pocket spending across the childbirth episode, including both deliveries and newborn hospitalizations.”
To address this knowledge gap, Dr. Chua and colleagues turned to Optum’s deidentified Clinformatics Data Mart, comprising 12 million privately insured individuals across the United States. The investigators identified 398,410 childbirth episodes occurring between 2016 and 2019. Each episode was defined as one delivery and at least one newborn hospitalization under the same family plan.
Out-of-pocket cost included copayment plus coinsurance and deductibles. Primary outcomes included mean total out-of-pocket spending and proportion of episodes exceeding $5,000 or $10,000. Subgroup analyses compared differences in spending between episodes involving neonatal intensive care or cesarean birth.
The mean out-of-pocket spending was $2,281 for delivery and $788 for newborn hospitalization, giving a total of $3,068 per childbirth episode. Coinsurance and deductibles accounted for much of that cost, at 55.8% and 42.1%, respectively, whereas copayments accounted for a relatively minor portion (2.2%).
Almost all episodes (95%) cost more than zero dollars, while 17.1% cost more than $5,000 and 1.0% cost more than $10,000. Total mean out-of-pocket spending was higher for episodes involving cesarean birth ($3,389) or neonatal intensive care ($4,969), the latter of which cost more than $10,000 in 8.8% of episodes.
“Because details on plan benefit design were unavailable, the generalizability of findings to all privately insured Americans is unclear,” the investigators noted. “However, the proportion of childbirth episodes covered by high-deductible health plans in this study is consistent with the prevalence of such plans among Americans with employer-sponsored insurance.”
The findings suggest that financial reform is needed, Dr. Chua and colleagues concluded.
“To avoid imposing undue financial burden on families, private insurers should improve childbirth coverage,” they wrote. “An incremental step would be providing first-dollar coverage of deliveries and newborn hospitalizations before deductibles are met. Ideally, however, insurers would waive most or all cost-sharing for these hospitalizations, consistent with the approach taken by Medicaid programs and many developed countries.”
According to Madeline Sutton, MD, assistant professor of obstetrics and gynecology at Morehouse School of Medicine, Atlanta, the size of the study is commendable, but some details are lacking.
“Although the overall sample size allows for a robust analysis, deciding to not report the confidence intervals in this report does not allow for understanding of [the findings with] smaller sample sizes,” Dr. Sutton said in an interview.
(Dr. Chua and colleagues noted that they did not report confidence intervals because “all differences between subgroups were significant owing to large sample sizes.”)
“Still,” Dr. Sutton went on, “this is an important study that has implications for financial counseling that may need to be a part of preconceptional, prenatal, and postnatal visits for privately insured families to help with planning and to decrease the chances of childbirth-related financial hardships. Additionally, policy-level changes that decrease or eliminate these private insurance–related childbirth-episode costs that may negatively impact some families with lower incomes, are warranted.”
The study was funded by the National Institutes of Health. Dr. Chua disclosed a grant from the National Institute on Drug Abuse, while Dr. Moniz is supported by the Agency for Healthcare Research and Quality. Dr. Sutton had no relevant disclosures.
Families with private health insurance pay around $3,000 for newborn delivery and hospitalization, while adding neonatal intensive care can push the bill closer to $5,000, based on a retrospective look at almost 400,000 episodes.
The findings suggest that privately insured families need prenatal financial counseling, as well as screening for financial hardship after delivery, reported lead author Kao-Ping Chua, MD, PhD, assistant professor and health policy researcher in the department of pediatrics and the Susan B. Meister Child Health Evaluation and Research Center at the University of Michigan, Ann Arbor, and colleagues.
“Concern is growing regarding the high and rising financial burden of childbirth for privately insured families,” the investigators wrote in Pediatrics. “Previous studies assessing this burden have focused on out-of-pocket spending for maternal care, including hospitalizations for delivery. However, there are no recent national data on out-of-pocket spending across the childbirth episode, including both deliveries and newborn hospitalizations.”
To address this knowledge gap, Dr. Chua and colleagues turned to Optum’s deidentified Clinformatics Data Mart, comprising 12 million privately insured individuals across the United States. The investigators identified 398,410 childbirth episodes occurring between 2016 and 2019. Each episode was defined as one delivery and at least one newborn hospitalization under the same family plan.
Out-of-pocket cost included copayment plus coinsurance and deductibles. Primary outcomes included mean total out-of-pocket spending and proportion of episodes exceeding $5,000 or $10,000. Subgroup analyses compared differences in spending between episodes involving neonatal intensive care or cesarean birth.
The mean out-of-pocket spending was $2,281 for delivery and $788 for newborn hospitalization, giving a total of $3,068 per childbirth episode. Coinsurance and deductibles accounted for much of that cost, at 55.8% and 42.1%, respectively, whereas copayments accounted for a relatively minor portion (2.2%).
Almost all episodes (95%) cost more than zero dollars, while 17.1% cost more than $5,000 and 1.0% cost more than $10,000. Total mean out-of-pocket spending was higher for episodes involving cesarean birth ($3,389) or neonatal intensive care ($4,969), the latter of which cost more than $10,000 in 8.8% of episodes.
“Because details on plan benefit design were unavailable, the generalizability of findings to all privately insured Americans is unclear,” the investigators noted. “However, the proportion of childbirth episodes covered by high-deductible health plans in this study is consistent with the prevalence of such plans among Americans with employer-sponsored insurance.”
The findings suggest that financial reform is needed, Dr. Chua and colleagues concluded.
“To avoid imposing undue financial burden on families, private insurers should improve childbirth coverage,” they wrote. “An incremental step would be providing first-dollar coverage of deliveries and newborn hospitalizations before deductibles are met. Ideally, however, insurers would waive most or all cost-sharing for these hospitalizations, consistent with the approach taken by Medicaid programs and many developed countries.”
According to Madeline Sutton, MD, assistant professor of obstetrics and gynecology at Morehouse School of Medicine, Atlanta, the size of the study is commendable, but some details are lacking.
“Although the overall sample size allows for a robust analysis, deciding to not report the confidence intervals in this report does not allow for understanding of [the findings with] smaller sample sizes,” Dr. Sutton said in an interview.
(Dr. Chua and colleagues noted that they did not report confidence intervals because “all differences between subgroups were significant owing to large sample sizes.”)
“Still,” Dr. Sutton went on, “this is an important study that has implications for financial counseling that may need to be a part of preconceptional, prenatal, and postnatal visits for privately insured families to help with planning and to decrease the chances of childbirth-related financial hardships. Additionally, policy-level changes that decrease or eliminate these private insurance–related childbirth-episode costs that may negatively impact some families with lower incomes, are warranted.”
The study was funded by the National Institutes of Health. Dr. Chua disclosed a grant from the National Institute on Drug Abuse, while Dr. Moniz is supported by the Agency for Healthcare Research and Quality. Dr. Sutton had no relevant disclosures.
FROM PEDIATRICS
Dose-dependent effect of ‘internet addiction’ and sleep problems
More evidence suggests the severity of internet addiction (IA) is directly related to the severity of sleep problems in youth.
Results from a study of more than 4,000 adolescent students show IA severity was linked to less sleep and to daytime sleepiness. In addition, boys aged 12-14 years who were addicted to computer games versus social media networking were the most affected.
Sleep issues could be “easily detectable manifestations of pathological internet addiction,” investigator Sergey Tereshchenko, PhD, Scientific Research Institute for Medical Problems of the North, Krasnoyask State Medical University, Russia, told this news organization.
These sleep problems require attention and correction, Dr. Tereshchenko added.
The findings were presented at the virtual Congress of the European Academy of Neurology 2021.
New phenomenon
IA is a relatively new psychological phenomenon and is most prevalent in “socially vulnerable groups,” such as adolescents, Dr. Tereshchenko said.
He cited numerous studies that have “convincingly demonstrated” IA is comorbid with a broad range of psychopathologic conditions, including depression, anxiety, and attention deficit hyperactivity disorder.
There is also growing evidence, including from systematic reviews in 2014 and 2019, that IA affects a wide range of sleep parameters.
However, most studies in adolescents have used only one psychometric tool to assess addiction, revealing only the “general IA pattern” and not the type of IA, Dr. Tereshchenko noted.
Adolescents may not be addicted to the internet itself but to certain behaviors like gaming or social networking, he said.
The “undoubted advantage” of his team’s research is the use of more than one tool, making it possible to “verify the predominant content of the addiction,” he added.
The investigators previously assessed general prevalence of IA in adolescents in Siberia and found about 6.8% of participants displayed pathological IA behavior – and that gaming addiction is more common in boys whereas addiction to social networking is more common in girls.
This prevalence rate is lower than in the Philippines (21.1%), Hong Kong (16.4%), Malaysia (14.1%), China (11%), and South Korea (9.7%), but slightly higher than in Japan (6.2%).
IA prevalence among adolescents in Europe ranges from 1% to 11%, with an average of 4.4%, said Dr. Tereshchenko.
Siberian students’ sleep
The current study included 4,344 students aged 12-18 years (average age, about 15 years) from 10 public schools in three large cities of Central Siberia (Krasnoyarsk, Abakan, and Kyzyl). There were slightly more girls than boys in the study sample.
Participants completed the Russian language version of the Chen Internet Addiction Scale (CIAS), which covers five symptomatic criteria for addictive behavior: withdrawal symptoms, signs of tolerance, compulsive use, psychological or physical problems, and difficulty managing time.
In this questionnaire, respondents rate several statements regarding the effect of internet use, each on a 4-point Likert scale: not at all (1 point), a little bit (2 points), moderately (3 points) and extremely (4). The total score ranges from 26 to 104.
A CIAS score of 26-42 indicates adaptive internet use, 43-64 indicates maladaptive internet use, and 65 and above indicates pathological internet use (PIU), which was classified as “internet-addicted.”
The researchers also used the nine-item Social Media Disorder Scale, as well as the Pittsburgh Sleep Quality Index to assess nighttime sleep.
Among other questions, teens were asked how long it usually took them to fall asleep and when they typically went to bed and woke up on school nights.
For daytime sleepiness, investigators used the targeted Pediatric Daytime Sleepiness Scale questionnaire, making them among the few research groups to use this psychometric instrument, Dr. Tereshchenko noted.
After parental consent was given, students completed the tests at the end of the day’s lessons. Total test time was about 45 minutes.
Sleep disturbance
Initial study results showed that compared with the other groups, adolescents with PIU tended to go to bed later, wake up later, take longer to fall asleep, sleep less at night, have more nighttime awakenings, and have more daytime sleepiness.
Sleep quality was the most impaired in boys aged 12-14 years who are addicted to internet computer games.
“In this group, 5 of the 6 sleep assessment parameters we studied were changed,” Dr. Tereshchenko reported.
Decreased total nighttime sleep was more common in older adolescents.
On average, boys and girls aged 15-18 years got less than the recommended 8 hours of sleep per night. Boys with IA got only about 6.4 hours per night and girls with IA got about 6.6 hours.
Interestingly, IA is generally more prevalent among teen girls than boys in Russia, which is not the case in Europe and North America, Dr. Tereshchenko noted.
Mechanisms linking IA and sleep disorders are not clear, but the relationship is probably multifactorial and perhaps interrelated, creating something of a “vicious circle,” he said.
“Sleep disturbances, which reflect psychosocial problems, depression, and anxiety-phobic disorders, can precede and contribute to IA. On the other hand, sleep disturbances such as insomnia can lead to increased use of the internet in the evening and at night, further exacerbating the problem,” said Dr. Tereshchenko.
Research is lacking on useful treatments for youth with IA, but these kids would likely benefit from behavioral therapy approaches, he added.
No escape?
Commenting on the study for this news organization, Maurice M. Ohayon, MD, DSc, PhD, director of the Stanford Sleep Epidemiology Research Center, Stanford University, California, said the topic of youth IA is “very important.”
Previous research in this field has shown a major impact from IA not only on sleep but also on mood – with irritability, depression, and even thoughts of suicide being possible red flags, said Dr. Ohayon, who was not involved in the current study.
Interestingly, his own research has also found that young teenage boys are most at risk for gaming addiction.
Although internet gaming has some positive effects, such as fostering leadership skills and relationships, it has become increasingly violent and isolating, with more adult professional gamers preying on younger players, Dr. Ohayon said.
“The major problem is that it’s putting children in a virtual world from which it’s difficult to escape,” he added.
Dr. Ohayon also noted concern about future developmental effects in kids who play video games for hours on end without coming out of their bedroom and with no physical contact with fellow players.
Parents should intervene before this situation occurs and limit the time their children spend on the gaming console, he said.
A version of this article first appeared on Medscape.com.
More evidence suggests the severity of internet addiction (IA) is directly related to the severity of sleep problems in youth.
Results from a study of more than 4,000 adolescent students show IA severity was linked to less sleep and to daytime sleepiness. In addition, boys aged 12-14 years who were addicted to computer games versus social media networking were the most affected.
Sleep issues could be “easily detectable manifestations of pathological internet addiction,” investigator Sergey Tereshchenko, PhD, Scientific Research Institute for Medical Problems of the North, Krasnoyask State Medical University, Russia, told this news organization.
These sleep problems require attention and correction, Dr. Tereshchenko added.
The findings were presented at the virtual Congress of the European Academy of Neurology 2021.
New phenomenon
IA is a relatively new psychological phenomenon and is most prevalent in “socially vulnerable groups,” such as adolescents, Dr. Tereshchenko said.
He cited numerous studies that have “convincingly demonstrated” IA is comorbid with a broad range of psychopathologic conditions, including depression, anxiety, and attention deficit hyperactivity disorder.
There is also growing evidence, including from systematic reviews in 2014 and 2019, that IA affects a wide range of sleep parameters.
However, most studies in adolescents have used only one psychometric tool to assess addiction, revealing only the “general IA pattern” and not the type of IA, Dr. Tereshchenko noted.
Adolescents may not be addicted to the internet itself but to certain behaviors like gaming or social networking, he said.
The “undoubted advantage” of his team’s research is the use of more than one tool, making it possible to “verify the predominant content of the addiction,” he added.
The investigators previously assessed general prevalence of IA in adolescents in Siberia and found about 6.8% of participants displayed pathological IA behavior – and that gaming addiction is more common in boys whereas addiction to social networking is more common in girls.
This prevalence rate is lower than in the Philippines (21.1%), Hong Kong (16.4%), Malaysia (14.1%), China (11%), and South Korea (9.7%), but slightly higher than in Japan (6.2%).
IA prevalence among adolescents in Europe ranges from 1% to 11%, with an average of 4.4%, said Dr. Tereshchenko.
Siberian students’ sleep
The current study included 4,344 students aged 12-18 years (average age, about 15 years) from 10 public schools in three large cities of Central Siberia (Krasnoyarsk, Abakan, and Kyzyl). There were slightly more girls than boys in the study sample.
Participants completed the Russian language version of the Chen Internet Addiction Scale (CIAS), which covers five symptomatic criteria for addictive behavior: withdrawal symptoms, signs of tolerance, compulsive use, psychological or physical problems, and difficulty managing time.
In this questionnaire, respondents rate several statements regarding the effect of internet use, each on a 4-point Likert scale: not at all (1 point), a little bit (2 points), moderately (3 points) and extremely (4). The total score ranges from 26 to 104.
A CIAS score of 26-42 indicates adaptive internet use, 43-64 indicates maladaptive internet use, and 65 and above indicates pathological internet use (PIU), which was classified as “internet-addicted.”
The researchers also used the nine-item Social Media Disorder Scale, as well as the Pittsburgh Sleep Quality Index to assess nighttime sleep.
Among other questions, teens were asked how long it usually took them to fall asleep and when they typically went to bed and woke up on school nights.
For daytime sleepiness, investigators used the targeted Pediatric Daytime Sleepiness Scale questionnaire, making them among the few research groups to use this psychometric instrument, Dr. Tereshchenko noted.
After parental consent was given, students completed the tests at the end of the day’s lessons. Total test time was about 45 minutes.
Sleep disturbance
Initial study results showed that compared with the other groups, adolescents with PIU tended to go to bed later, wake up later, take longer to fall asleep, sleep less at night, have more nighttime awakenings, and have more daytime sleepiness.
Sleep quality was the most impaired in boys aged 12-14 years who are addicted to internet computer games.
“In this group, 5 of the 6 sleep assessment parameters we studied were changed,” Dr. Tereshchenko reported.
Decreased total nighttime sleep was more common in older adolescents.
On average, boys and girls aged 15-18 years got less than the recommended 8 hours of sleep per night. Boys with IA got only about 6.4 hours per night and girls with IA got about 6.6 hours.
Interestingly, IA is generally more prevalent among teen girls than boys in Russia, which is not the case in Europe and North America, Dr. Tereshchenko noted.
Mechanisms linking IA and sleep disorders are not clear, but the relationship is probably multifactorial and perhaps interrelated, creating something of a “vicious circle,” he said.
“Sleep disturbances, which reflect psychosocial problems, depression, and anxiety-phobic disorders, can precede and contribute to IA. On the other hand, sleep disturbances such as insomnia can lead to increased use of the internet in the evening and at night, further exacerbating the problem,” said Dr. Tereshchenko.
Research is lacking on useful treatments for youth with IA, but these kids would likely benefit from behavioral therapy approaches, he added.
No escape?
Commenting on the study for this news organization, Maurice M. Ohayon, MD, DSc, PhD, director of the Stanford Sleep Epidemiology Research Center, Stanford University, California, said the topic of youth IA is “very important.”
Previous research in this field has shown a major impact from IA not only on sleep but also on mood – with irritability, depression, and even thoughts of suicide being possible red flags, said Dr. Ohayon, who was not involved in the current study.
Interestingly, his own research has also found that young teenage boys are most at risk for gaming addiction.
Although internet gaming has some positive effects, such as fostering leadership skills and relationships, it has become increasingly violent and isolating, with more adult professional gamers preying on younger players, Dr. Ohayon said.
“The major problem is that it’s putting children in a virtual world from which it’s difficult to escape,” he added.
Dr. Ohayon also noted concern about future developmental effects in kids who play video games for hours on end without coming out of their bedroom and with no physical contact with fellow players.
Parents should intervene before this situation occurs and limit the time their children spend on the gaming console, he said.
A version of this article first appeared on Medscape.com.
More evidence suggests the severity of internet addiction (IA) is directly related to the severity of sleep problems in youth.
Results from a study of more than 4,000 adolescent students show IA severity was linked to less sleep and to daytime sleepiness. In addition, boys aged 12-14 years who were addicted to computer games versus social media networking were the most affected.
Sleep issues could be “easily detectable manifestations of pathological internet addiction,” investigator Sergey Tereshchenko, PhD, Scientific Research Institute for Medical Problems of the North, Krasnoyask State Medical University, Russia, told this news organization.
These sleep problems require attention and correction, Dr. Tereshchenko added.
The findings were presented at the virtual Congress of the European Academy of Neurology 2021.
New phenomenon
IA is a relatively new psychological phenomenon and is most prevalent in “socially vulnerable groups,” such as adolescents, Dr. Tereshchenko said.
He cited numerous studies that have “convincingly demonstrated” IA is comorbid with a broad range of psychopathologic conditions, including depression, anxiety, and attention deficit hyperactivity disorder.
There is also growing evidence, including from systematic reviews in 2014 and 2019, that IA affects a wide range of sleep parameters.
However, most studies in adolescents have used only one psychometric tool to assess addiction, revealing only the “general IA pattern” and not the type of IA, Dr. Tereshchenko noted.
Adolescents may not be addicted to the internet itself but to certain behaviors like gaming or social networking, he said.
The “undoubted advantage” of his team’s research is the use of more than one tool, making it possible to “verify the predominant content of the addiction,” he added.
The investigators previously assessed general prevalence of IA in adolescents in Siberia and found about 6.8% of participants displayed pathological IA behavior – and that gaming addiction is more common in boys whereas addiction to social networking is more common in girls.
This prevalence rate is lower than in the Philippines (21.1%), Hong Kong (16.4%), Malaysia (14.1%), China (11%), and South Korea (9.7%), but slightly higher than in Japan (6.2%).
IA prevalence among adolescents in Europe ranges from 1% to 11%, with an average of 4.4%, said Dr. Tereshchenko.
Siberian students’ sleep
The current study included 4,344 students aged 12-18 years (average age, about 15 years) from 10 public schools in three large cities of Central Siberia (Krasnoyarsk, Abakan, and Kyzyl). There were slightly more girls than boys in the study sample.
Participants completed the Russian language version of the Chen Internet Addiction Scale (CIAS), which covers five symptomatic criteria for addictive behavior: withdrawal symptoms, signs of tolerance, compulsive use, psychological or physical problems, and difficulty managing time.
In this questionnaire, respondents rate several statements regarding the effect of internet use, each on a 4-point Likert scale: not at all (1 point), a little bit (2 points), moderately (3 points) and extremely (4). The total score ranges from 26 to 104.
A CIAS score of 26-42 indicates adaptive internet use, 43-64 indicates maladaptive internet use, and 65 and above indicates pathological internet use (PIU), which was classified as “internet-addicted.”
The researchers also used the nine-item Social Media Disorder Scale, as well as the Pittsburgh Sleep Quality Index to assess nighttime sleep.
Among other questions, teens were asked how long it usually took them to fall asleep and when they typically went to bed and woke up on school nights.
For daytime sleepiness, investigators used the targeted Pediatric Daytime Sleepiness Scale questionnaire, making them among the few research groups to use this psychometric instrument, Dr. Tereshchenko noted.
After parental consent was given, students completed the tests at the end of the day’s lessons. Total test time was about 45 minutes.
Sleep disturbance
Initial study results showed that compared with the other groups, adolescents with PIU tended to go to bed later, wake up later, take longer to fall asleep, sleep less at night, have more nighttime awakenings, and have more daytime sleepiness.
Sleep quality was the most impaired in boys aged 12-14 years who are addicted to internet computer games.
“In this group, 5 of the 6 sleep assessment parameters we studied were changed,” Dr. Tereshchenko reported.
Decreased total nighttime sleep was more common in older adolescents.
On average, boys and girls aged 15-18 years got less than the recommended 8 hours of sleep per night. Boys with IA got only about 6.4 hours per night and girls with IA got about 6.6 hours.
Interestingly, IA is generally more prevalent among teen girls than boys in Russia, which is not the case in Europe and North America, Dr. Tereshchenko noted.
Mechanisms linking IA and sleep disorders are not clear, but the relationship is probably multifactorial and perhaps interrelated, creating something of a “vicious circle,” he said.
“Sleep disturbances, which reflect psychosocial problems, depression, and anxiety-phobic disorders, can precede and contribute to IA. On the other hand, sleep disturbances such as insomnia can lead to increased use of the internet in the evening and at night, further exacerbating the problem,” said Dr. Tereshchenko.
Research is lacking on useful treatments for youth with IA, but these kids would likely benefit from behavioral therapy approaches, he added.
No escape?
Commenting on the study for this news organization, Maurice M. Ohayon, MD, DSc, PhD, director of the Stanford Sleep Epidemiology Research Center, Stanford University, California, said the topic of youth IA is “very important.”
Previous research in this field has shown a major impact from IA not only on sleep but also on mood – with irritability, depression, and even thoughts of suicide being possible red flags, said Dr. Ohayon, who was not involved in the current study.
Interestingly, his own research has also found that young teenage boys are most at risk for gaming addiction.
Although internet gaming has some positive effects, such as fostering leadership skills and relationships, it has become increasingly violent and isolating, with more adult professional gamers preying on younger players, Dr. Ohayon said.
“The major problem is that it’s putting children in a virtual world from which it’s difficult to escape,” he added.
Dr. Ohayon also noted concern about future developmental effects in kids who play video games for hours on end without coming out of their bedroom and with no physical contact with fellow players.
Parents should intervene before this situation occurs and limit the time their children spend on the gaming console, he said.
A version of this article first appeared on Medscape.com.







