User login
FDA Rejects GI Cancer Drug Over Manufacturing Issues
the company announced January 8.
The monoclonal antibody was under priority review as the first agent specifically for locally advanced unresectable or metastatic HER2-negative gastric or gastroesophageal junction adenocarcinoma that is claudin 18.2-positive. Overexpression of claudin 18.2 in gastric cancer cells is associated with tumor growth and progression.
The FDA, however, could not approve zolbetuximab by the planned decision date of January 12, 2024, because of “unresolved deficiencies following its pre-license inspection of a third-party manufacturing facility for zolbetuximab,” according to the company press release.
Astellas “is working closely with the FDA and the third-party manufacturer to establish a timeline to quickly resolve” the issues, the company said.
Astellas also clarified that the FDA isn’t asking for additional efficacy and safety data. In phase 3 testing, zolbetuximab improved median progression-free and overall survival by about 2-3 months over chemotherapy alone.
If zolbetuximab is approved, “pathologists will have to be facile with claudin 18.2 testing as a companion diagnostic before [it] can be used,” Mark Lewis, MD, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, told this news organization.
The agent is also under review in Japan, Europe, and China.
A version of this article appeared on Medscape.com.
the company announced January 8.
The monoclonal antibody was under priority review as the first agent specifically for locally advanced unresectable or metastatic HER2-negative gastric or gastroesophageal junction adenocarcinoma that is claudin 18.2-positive. Overexpression of claudin 18.2 in gastric cancer cells is associated with tumor growth and progression.
The FDA, however, could not approve zolbetuximab by the planned decision date of January 12, 2024, because of “unresolved deficiencies following its pre-license inspection of a third-party manufacturing facility for zolbetuximab,” according to the company press release.
Astellas “is working closely with the FDA and the third-party manufacturer to establish a timeline to quickly resolve” the issues, the company said.
Astellas also clarified that the FDA isn’t asking for additional efficacy and safety data. In phase 3 testing, zolbetuximab improved median progression-free and overall survival by about 2-3 months over chemotherapy alone.
If zolbetuximab is approved, “pathologists will have to be facile with claudin 18.2 testing as a companion diagnostic before [it] can be used,” Mark Lewis, MD, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, told this news organization.
The agent is also under review in Japan, Europe, and China.
A version of this article appeared on Medscape.com.
the company announced January 8.
The monoclonal antibody was under priority review as the first agent specifically for locally advanced unresectable or metastatic HER2-negative gastric or gastroesophageal junction adenocarcinoma that is claudin 18.2-positive. Overexpression of claudin 18.2 in gastric cancer cells is associated with tumor growth and progression.
The FDA, however, could not approve zolbetuximab by the planned decision date of January 12, 2024, because of “unresolved deficiencies following its pre-license inspection of a third-party manufacturing facility for zolbetuximab,” according to the company press release.
Astellas “is working closely with the FDA and the third-party manufacturer to establish a timeline to quickly resolve” the issues, the company said.
Astellas also clarified that the FDA isn’t asking for additional efficacy and safety data. In phase 3 testing, zolbetuximab improved median progression-free and overall survival by about 2-3 months over chemotherapy alone.
If zolbetuximab is approved, “pathologists will have to be facile with claudin 18.2 testing as a companion diagnostic before [it] can be used,” Mark Lewis, MD, a gastrointestinal oncologist at Intermountain Healthcare in Murray, Utah, told this news organization.
The agent is also under review in Japan, Europe, and China.
A version of this article appeared on Medscape.com.
Panel Recommends Small Bump in 2025 Medicare Physician Pay
An influential panel is seeking an increase in Medicare’s 2025 payments for clinicians, adding to pressure on Congress to reconsider how the largest US purchaser of health services pays for office visits and related care of the nation’s older citizens and those with disabilities.
The Medicare Payment Advisory Commission (MedPAC) on Thursday voted unanimously in favor of a two-part recommendation on changes to the 2025 physician fee schedule:
- An increase in the base rate equal to half of the projected change in the Medicare Economic Index (MEI). Recent estimates have projected a 2.6% increase in MEI for 2025, which is intended to show how inflation affects the costs of running a medical practice.
- The creation of a safety-net add-on payment under the physician fee schedule to cover care of people with low incomes.
These recommendations echo the calls MedPAC made in a 2023 report to Congress.
Lawmakers and the Centers for Medicare and Medicaid Services (CMS) rely on MedPAC’s work in deciding how much to pay for services. About 1.3 million clinicians bill Medicare for their work, including about 670,000 physicians.
Thursday’s MedPAC vote comes amid continuing uncertainty about how much the federal government will actually pay clinicians this year through the physician fee schedule.
There are serious efforts underway to undo cuts already demanded by previously passed federal law. In an email, Rep. Larry Buchson, MD, (R-IN) said he remains committed to “eliminating the full 3.37% cut this year while also working toward a permanent solution to halt the downward spiral of physician reimbursement.”
“The Medicare payment cut to physicians will impede patients’ access to care and further accelerate the current path toward consolidation, physician burnout, and closure of medical practices,” Buchson told this news organization. “It’s past time that Congress provides much needed and deserved stability for America’s doctors.”
Congress this month is attempting to complete overdue budget legislation needed to fund federal operations for fiscal 2024, which began October 1, 2023. The pending expiration of a short-term stopgap continuing resolution could provide a vehicle that could also carry legislation that would address the physician fee schedule.
In a Thursday statement, Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association, commended MedPAC for its recommendations and urged lawmakers to act.
“Long-term reforms from Congress are overdue to close the unsustainable gap between what Medicare pays physicians and the actual costs of delivering high-quality care,” Dr. Ehrenfeld said. “When adjusted for inflation in practice costs, Medicare physician pay declined 26% from 2001 to 2023.”
Continual Struggles
Congress has struggled for years in its attempts to set Medicare payments for office visits and other services covered by the physician fee schedule. A 1990s budget law set the stage for what proved to be untenable reductions in payment through the sustainable growth rate mechanism.
Between 2003 through April 2014, lawmakers passed “doc-fix” legislation 17 times to block the slated cuts, according to the Congressional Research Service. In 2015, Congress passed an intended overhaul of the physician fee schedule through the Medicare Access and CHIP Reauthorization Act (MACRA). As part of this law, Congress eliminated a base automatic inflation adjuster for the physician fee schedule.
In recent years, Congress has acted repeatedly to address MACRA’s mandates for flat base pay. MedPAC and members of both parties in Congress have called for a broad new look at how Medicare pays physicians.
At Thursday’s meeting, MedPAC member Lawrence Casalino, MD, PhD, MPH, noted that the struggles to keep up with inflation and the “unpredictability of what the payment rates are going to be from year to year really do affect physician morale.”
A version of this article appeared on Medscape.com.
An influential panel is seeking an increase in Medicare’s 2025 payments for clinicians, adding to pressure on Congress to reconsider how the largest US purchaser of health services pays for office visits and related care of the nation’s older citizens and those with disabilities.
The Medicare Payment Advisory Commission (MedPAC) on Thursday voted unanimously in favor of a two-part recommendation on changes to the 2025 physician fee schedule:
- An increase in the base rate equal to half of the projected change in the Medicare Economic Index (MEI). Recent estimates have projected a 2.6% increase in MEI for 2025, which is intended to show how inflation affects the costs of running a medical practice.
- The creation of a safety-net add-on payment under the physician fee schedule to cover care of people with low incomes.
These recommendations echo the calls MedPAC made in a 2023 report to Congress.
Lawmakers and the Centers for Medicare and Medicaid Services (CMS) rely on MedPAC’s work in deciding how much to pay for services. About 1.3 million clinicians bill Medicare for their work, including about 670,000 physicians.
Thursday’s MedPAC vote comes amid continuing uncertainty about how much the federal government will actually pay clinicians this year through the physician fee schedule.
There are serious efforts underway to undo cuts already demanded by previously passed federal law. In an email, Rep. Larry Buchson, MD, (R-IN) said he remains committed to “eliminating the full 3.37% cut this year while also working toward a permanent solution to halt the downward spiral of physician reimbursement.”
“The Medicare payment cut to physicians will impede patients’ access to care and further accelerate the current path toward consolidation, physician burnout, and closure of medical practices,” Buchson told this news organization. “It’s past time that Congress provides much needed and deserved stability for America’s doctors.”
Congress this month is attempting to complete overdue budget legislation needed to fund federal operations for fiscal 2024, which began October 1, 2023. The pending expiration of a short-term stopgap continuing resolution could provide a vehicle that could also carry legislation that would address the physician fee schedule.
In a Thursday statement, Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association, commended MedPAC for its recommendations and urged lawmakers to act.
“Long-term reforms from Congress are overdue to close the unsustainable gap between what Medicare pays physicians and the actual costs of delivering high-quality care,” Dr. Ehrenfeld said. “When adjusted for inflation in practice costs, Medicare physician pay declined 26% from 2001 to 2023.”
Continual Struggles
Congress has struggled for years in its attempts to set Medicare payments for office visits and other services covered by the physician fee schedule. A 1990s budget law set the stage for what proved to be untenable reductions in payment through the sustainable growth rate mechanism.
Between 2003 through April 2014, lawmakers passed “doc-fix” legislation 17 times to block the slated cuts, according to the Congressional Research Service. In 2015, Congress passed an intended overhaul of the physician fee schedule through the Medicare Access and CHIP Reauthorization Act (MACRA). As part of this law, Congress eliminated a base automatic inflation adjuster for the physician fee schedule.
In recent years, Congress has acted repeatedly to address MACRA’s mandates for flat base pay. MedPAC and members of both parties in Congress have called for a broad new look at how Medicare pays physicians.
At Thursday’s meeting, MedPAC member Lawrence Casalino, MD, PhD, MPH, noted that the struggles to keep up with inflation and the “unpredictability of what the payment rates are going to be from year to year really do affect physician morale.”
A version of this article appeared on Medscape.com.
An influential panel is seeking an increase in Medicare’s 2025 payments for clinicians, adding to pressure on Congress to reconsider how the largest US purchaser of health services pays for office visits and related care of the nation’s older citizens and those with disabilities.
The Medicare Payment Advisory Commission (MedPAC) on Thursday voted unanimously in favor of a two-part recommendation on changes to the 2025 physician fee schedule:
- An increase in the base rate equal to half of the projected change in the Medicare Economic Index (MEI). Recent estimates have projected a 2.6% increase in MEI for 2025, which is intended to show how inflation affects the costs of running a medical practice.
- The creation of a safety-net add-on payment under the physician fee schedule to cover care of people with low incomes.
These recommendations echo the calls MedPAC made in a 2023 report to Congress.
Lawmakers and the Centers for Medicare and Medicaid Services (CMS) rely on MedPAC’s work in deciding how much to pay for services. About 1.3 million clinicians bill Medicare for their work, including about 670,000 physicians.
Thursday’s MedPAC vote comes amid continuing uncertainty about how much the federal government will actually pay clinicians this year through the physician fee schedule.
There are serious efforts underway to undo cuts already demanded by previously passed federal law. In an email, Rep. Larry Buchson, MD, (R-IN) said he remains committed to “eliminating the full 3.37% cut this year while also working toward a permanent solution to halt the downward spiral of physician reimbursement.”
“The Medicare payment cut to physicians will impede patients’ access to care and further accelerate the current path toward consolidation, physician burnout, and closure of medical practices,” Buchson told this news organization. “It’s past time that Congress provides much needed and deserved stability for America’s doctors.”
Congress this month is attempting to complete overdue budget legislation needed to fund federal operations for fiscal 2024, which began October 1, 2023. The pending expiration of a short-term stopgap continuing resolution could provide a vehicle that could also carry legislation that would address the physician fee schedule.
In a Thursday statement, Jesse M. Ehrenfeld, MD, MPH, president of the American Medical Association, commended MedPAC for its recommendations and urged lawmakers to act.
“Long-term reforms from Congress are overdue to close the unsustainable gap between what Medicare pays physicians and the actual costs of delivering high-quality care,” Dr. Ehrenfeld said. “When adjusted for inflation in practice costs, Medicare physician pay declined 26% from 2001 to 2023.”
Continual Struggles
Congress has struggled for years in its attempts to set Medicare payments for office visits and other services covered by the physician fee schedule. A 1990s budget law set the stage for what proved to be untenable reductions in payment through the sustainable growth rate mechanism.
Between 2003 through April 2014, lawmakers passed “doc-fix” legislation 17 times to block the slated cuts, according to the Congressional Research Service. In 2015, Congress passed an intended overhaul of the physician fee schedule through the Medicare Access and CHIP Reauthorization Act (MACRA). As part of this law, Congress eliminated a base automatic inflation adjuster for the physician fee schedule.
In recent years, Congress has acted repeatedly to address MACRA’s mandates for flat base pay. MedPAC and members of both parties in Congress have called for a broad new look at how Medicare pays physicians.
At Thursday’s meeting, MedPAC member Lawrence Casalino, MD, PhD, MPH, noted that the struggles to keep up with inflation and the “unpredictability of what the payment rates are going to be from year to year really do affect physician morale.”
A version of this article appeared on Medscape.com.
BC axillary dissection may be unnecessary for isolated tumor cells after NAC
SAN ANTONIO — Axillary lymph node dissection is the current standard of care in breast cancer when metastases are found in sentinel lymph nodes after neoadjuvant chemotherapy.
However, what to do when isolated tumor cells instead of outright metastases are found in sentinel nodes is an open question. Some surgeons opt for a full axillary dissection while others do not, and there is no standard of care, explained Giacomo Montagna, MD, a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York City.
The study led and presented by Dr. Montagna at the San Antonio Breast Cancer Symposium brings some much-needed clarity to the issue.
The findings argue strongly against “routine axillary lymph node dissection” — with its considerable morbidities — “in patients with residual isolated tumor cells after neoadjuvant chemotherapy,” Dr. Montagna said.
Study discussant Elizabeth Mittendorf, MD, PhD, a breast cancer surgeon at Brigham and Women’s Hospital, Boston, agreed.
“It appears that the presence of isolated tumor cells in the sentinel nodes does not negatively impact oncologic outcomes. These additional data allow us to debunk some of the surgical dogma we grew up with, specifically that lymph node dissection is required for either survival or local control,” Dr. Mittendorf said.
However, there was concern among audience members that the information gleaned from a full dissection might still be needed to guide follow-on adjuvant therapy decisions.
Dr. Mittendorf didn’t think so. Although additional positive lymph nodes were found in almost a third of women who had axillary dissections in the review, the majority of involved nodes simply had more isolated tumor cells; macrometastases were found in just 5% of cases.
So, for most patients, additional information from axillary dissections is “unlikely needed to inform adjuvant therapy, and in fact,” based on the 5% figure, “we are thinking we would have to do well over a hundred lymph node dissections in such patients to inform treatment recommendations for fewer than five. This comes at the cost of fair morbidity,” she said.
Study details
The retrospective study, dubbed OPBC05/EUBREAST-14R/ICARO, included 583 women with cT1-4 N0-3 breast cancer treated at 62 centers in 18 countries. The majority of subjects were from the United States and Europe.
Every patient was found to have isolated tumor cells (ITCs) in their sentinel lymph nodes after neoadjuvant chemotherapy (NAC), which generally included anthracycline and taxane-based regimens. The majority of patients did not have a pathologic complete response to NAC.
Overall, 182 patients (31%) had a subsequent axillary lymph node dissection; the rest did not.
Dissections were more common in the presence of lymphovascular invasion and N2/N3 disease as well as when fewer lymph nodes were removed and when ITCs were found during surgery on frozen section, which was the case in a quarter of patients.
Additional positive nodes were found in 30% of patients in the dissection group and consisted of more nodes with ITCs in 18%, micrometastases in 7%, and macrometastases in 5%. Receptor status and nodal status at presentation did not have an impact on the likelihood of finding macrometastases.
The main finding of the study was that there were no statistically significant differences in recurrence outcomes between the two groups.
The 5-year rate of isolated axillary recurrence was 1.7% with axillary lymph node dissection (ALND) versus 1.1% without it. The 5-year rate of any invasive recurrence was 16% in the ALND arm and 19% in the no-dissection group.
The median age in the study was 48 years. The majority of patients (57%) had clinical T2 tumors. Most were HR positive and either HER2 negative (41%) or HER2 positive (28%).
Regional nodal radiation was more common in the ALND group, 82% versus 75%. The dissection arm had a mean of 2.8 sentinel lymph nodes removed versus 3.5 in the no-dissection group.
“The likelihood of finding additional positive lymph nodes in patients with residual ITCs after NAC is lower than in patients with residual micro- and macrometastases. In the majority of cases, they contain ITCs. Nodal recurrence after omission of ALND is rare in this population,” the investigators concluded in their abstract.
The work was funded by EUBREAST. Dr. Montagna doesn’t have any disclosures. Dr. Mittendorf has several industry ties, including being an advisor for Roche, AstraZeneca, and Moderna and a speaker for Merck.
SAN ANTONIO — Axillary lymph node dissection is the current standard of care in breast cancer when metastases are found in sentinel lymph nodes after neoadjuvant chemotherapy.
However, what to do when isolated tumor cells instead of outright metastases are found in sentinel nodes is an open question. Some surgeons opt for a full axillary dissection while others do not, and there is no standard of care, explained Giacomo Montagna, MD, a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York City.
The study led and presented by Dr. Montagna at the San Antonio Breast Cancer Symposium brings some much-needed clarity to the issue.
The findings argue strongly against “routine axillary lymph node dissection” — with its considerable morbidities — “in patients with residual isolated tumor cells after neoadjuvant chemotherapy,” Dr. Montagna said.
Study discussant Elizabeth Mittendorf, MD, PhD, a breast cancer surgeon at Brigham and Women’s Hospital, Boston, agreed.
“It appears that the presence of isolated tumor cells in the sentinel nodes does not negatively impact oncologic outcomes. These additional data allow us to debunk some of the surgical dogma we grew up with, specifically that lymph node dissection is required for either survival or local control,” Dr. Mittendorf said.
However, there was concern among audience members that the information gleaned from a full dissection might still be needed to guide follow-on adjuvant therapy decisions.
Dr. Mittendorf didn’t think so. Although additional positive lymph nodes were found in almost a third of women who had axillary dissections in the review, the majority of involved nodes simply had more isolated tumor cells; macrometastases were found in just 5% of cases.
So, for most patients, additional information from axillary dissections is “unlikely needed to inform adjuvant therapy, and in fact,” based on the 5% figure, “we are thinking we would have to do well over a hundred lymph node dissections in such patients to inform treatment recommendations for fewer than five. This comes at the cost of fair morbidity,” she said.
Study details
The retrospective study, dubbed OPBC05/EUBREAST-14R/ICARO, included 583 women with cT1-4 N0-3 breast cancer treated at 62 centers in 18 countries. The majority of subjects were from the United States and Europe.
Every patient was found to have isolated tumor cells (ITCs) in their sentinel lymph nodes after neoadjuvant chemotherapy (NAC), which generally included anthracycline and taxane-based regimens. The majority of patients did not have a pathologic complete response to NAC.
Overall, 182 patients (31%) had a subsequent axillary lymph node dissection; the rest did not.
Dissections were more common in the presence of lymphovascular invasion and N2/N3 disease as well as when fewer lymph nodes were removed and when ITCs were found during surgery on frozen section, which was the case in a quarter of patients.
Additional positive nodes were found in 30% of patients in the dissection group and consisted of more nodes with ITCs in 18%, micrometastases in 7%, and macrometastases in 5%. Receptor status and nodal status at presentation did not have an impact on the likelihood of finding macrometastases.
The main finding of the study was that there were no statistically significant differences in recurrence outcomes between the two groups.
The 5-year rate of isolated axillary recurrence was 1.7% with axillary lymph node dissection (ALND) versus 1.1% without it. The 5-year rate of any invasive recurrence was 16% in the ALND arm and 19% in the no-dissection group.
The median age in the study was 48 years. The majority of patients (57%) had clinical T2 tumors. Most were HR positive and either HER2 negative (41%) or HER2 positive (28%).
Regional nodal radiation was more common in the ALND group, 82% versus 75%. The dissection arm had a mean of 2.8 sentinel lymph nodes removed versus 3.5 in the no-dissection group.
“The likelihood of finding additional positive lymph nodes in patients with residual ITCs after NAC is lower than in patients with residual micro- and macrometastases. In the majority of cases, they contain ITCs. Nodal recurrence after omission of ALND is rare in this population,” the investigators concluded in their abstract.
The work was funded by EUBREAST. Dr. Montagna doesn’t have any disclosures. Dr. Mittendorf has several industry ties, including being an advisor for Roche, AstraZeneca, and Moderna and a speaker for Merck.
SAN ANTONIO — Axillary lymph node dissection is the current standard of care in breast cancer when metastases are found in sentinel lymph nodes after neoadjuvant chemotherapy.
However, what to do when isolated tumor cells instead of outright metastases are found in sentinel nodes is an open question. Some surgeons opt for a full axillary dissection while others do not, and there is no standard of care, explained Giacomo Montagna, MD, a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York City.
The study led and presented by Dr. Montagna at the San Antonio Breast Cancer Symposium brings some much-needed clarity to the issue.
The findings argue strongly against “routine axillary lymph node dissection” — with its considerable morbidities — “in patients with residual isolated tumor cells after neoadjuvant chemotherapy,” Dr. Montagna said.
Study discussant Elizabeth Mittendorf, MD, PhD, a breast cancer surgeon at Brigham and Women’s Hospital, Boston, agreed.
“It appears that the presence of isolated tumor cells in the sentinel nodes does not negatively impact oncologic outcomes. These additional data allow us to debunk some of the surgical dogma we grew up with, specifically that lymph node dissection is required for either survival or local control,” Dr. Mittendorf said.
However, there was concern among audience members that the information gleaned from a full dissection might still be needed to guide follow-on adjuvant therapy decisions.
Dr. Mittendorf didn’t think so. Although additional positive lymph nodes were found in almost a third of women who had axillary dissections in the review, the majority of involved nodes simply had more isolated tumor cells; macrometastases were found in just 5% of cases.
So, for most patients, additional information from axillary dissections is “unlikely needed to inform adjuvant therapy, and in fact,” based on the 5% figure, “we are thinking we would have to do well over a hundred lymph node dissections in such patients to inform treatment recommendations for fewer than five. This comes at the cost of fair morbidity,” she said.
Study details
The retrospective study, dubbed OPBC05/EUBREAST-14R/ICARO, included 583 women with cT1-4 N0-3 breast cancer treated at 62 centers in 18 countries. The majority of subjects were from the United States and Europe.
Every patient was found to have isolated tumor cells (ITCs) in their sentinel lymph nodes after neoadjuvant chemotherapy (NAC), which generally included anthracycline and taxane-based regimens. The majority of patients did not have a pathologic complete response to NAC.
Overall, 182 patients (31%) had a subsequent axillary lymph node dissection; the rest did not.
Dissections were more common in the presence of lymphovascular invasion and N2/N3 disease as well as when fewer lymph nodes were removed and when ITCs were found during surgery on frozen section, which was the case in a quarter of patients.
Additional positive nodes were found in 30% of patients in the dissection group and consisted of more nodes with ITCs in 18%, micrometastases in 7%, and macrometastases in 5%. Receptor status and nodal status at presentation did not have an impact on the likelihood of finding macrometastases.
The main finding of the study was that there were no statistically significant differences in recurrence outcomes between the two groups.
The 5-year rate of isolated axillary recurrence was 1.7% with axillary lymph node dissection (ALND) versus 1.1% without it. The 5-year rate of any invasive recurrence was 16% in the ALND arm and 19% in the no-dissection group.
The median age in the study was 48 years. The majority of patients (57%) had clinical T2 tumors. Most were HR positive and either HER2 negative (41%) or HER2 positive (28%).
Regional nodal radiation was more common in the ALND group, 82% versus 75%. The dissection arm had a mean of 2.8 sentinel lymph nodes removed versus 3.5 in the no-dissection group.
“The likelihood of finding additional positive lymph nodes in patients with residual ITCs after NAC is lower than in patients with residual micro- and macrometastases. In the majority of cases, they contain ITCs. Nodal recurrence after omission of ALND is rare in this population,” the investigators concluded in their abstract.
The work was funded by EUBREAST. Dr. Montagna doesn’t have any disclosures. Dr. Mittendorf has several industry ties, including being an advisor for Roche, AstraZeneca, and Moderna and a speaker for Merck.
AT SABCS 2023
Healthcare Violence: Doctors and Nurses Are Bearing the Brunt of Business Pressures
This transcript has been edited for clarity.
This month, I want to tackle the difficult subject of violence toward healthcare workers. There’s a reason this is top of mind for me in my practice, but I want to start by acknowledging that this has been a much larger issue for our profession and one that has been growing for a number of years now.
They also estimate that that rate doubled between 2011 and 2018. I think that range is important because it proves this was a problem, and a crescendoing problem, even before COVID.
Another thing I think is relevant is to look at where in the healthcare system are these attacks most likely. In the emergency room, ER staff have seen hostility toward them rise by at least 25% over the past several years. Some of the seeds of mistrust that were sown between the general public and the scientific and medical communities around the pandemic. I think there’s some explanation there for why that might be a particular crucible.
Perhaps most disturbingly of all, 60% of the victims of healthcare workplace violence are bedside nurses. There is something about the intensity of the inpatient setting that makes nerves particularly frayed and unfortunately makes patients and family members more likely to lash out. I think it’s actually the heightened sense of mortality.
I’m not excusing any of these behaviors, but maybe it’s akin to road rage. On the road, behind the wheel, tiny gestures can actually be, on some level, perceived as threats to our survival. Another driver swerving into your lane activates a fight-or-flight response, you feel threatened, and you might respond in the moment very rashly. I wonder if we’re not seeing that, quite unfairly, play out against bedside staff in our hospitals.
Here’s the thing. Those of us who practice in the outpatient setting — 95% of my work, for instance, happens in clinic — are not immune to this either. There are some very harrowing recent examples of physicians being killed, typically at gunpoint, often by patients, sometimes by aggrieved family members, in their offices. An orthopedist in Tennessee, a back surgeon in Tulsa, along with three of their colleagues. In the latter case, the assailant specifically blamed the surgeon for their pain.
This is where I think things get even more scary. We have to be the bearers of bad news in our profession. This has long been the task of the oncologist, in particular, to convey things that people don’t want to hear.
I think what brought this to my mind in terms of my reading was an incredible article in The ASCO Post and also in the Journal of Clinical Oncology by Dr. Noelle LoConte, who’s a medical oncologist in Wisconsin. The article is called, “I Want to Kill You,” and it recounts her telling a previously stage III colon cancer patient, with whom she thought she had good rapport, that the disease had recurred. The patient’s immediate reaction in the heat of that moment was to say, Dr LoConte, I want to kill you. I want to blow your face off.
Already, there’s clearly tension when we are telling people what they don’t want to hear. I think the final piece of the puzzle goes back to the intrusion of the business of healthcare on the practice of medicine. This is what I witnessed very recently. One of the things that’s interesting to think about is how what we do is now framed as customer service. I know there’s deriding of this model, but if perception is reality, we have a system where patients are set up to view themselves as consumers.
Let’s say, for instance, you’re in the unfortunate circumstance of being diagnosed with cancer and your insurer gives you the option to go to multiple oncologists. If you’re online browsing for oncologists, how do you differentiate me from some of my colleagues? The answer on these rating websites often has to do with domains that are about the overall experience — not just the patient-doctor interaction but also things like wait time, friendliness of staff, and promptness of care delivery.
That, I think, is the final piece of the puzzle, because what I really risk when I sit down with a patient and lay out a treatment plan is overpromising and underdelivering. I am long used to citing median overall survival for expectation of outcome. Of course, every patient wants to be an exceptional responder. Most patients want to be on the latter half of median survival. No one wants to be on the disappointingly shorter half.
My point is that I’ve long been able to mitigate that uncertainty for patients. What is getting harder and harder to explain away is the delay incurred between someone’s diagnosis, my meeting them and laying out a treatment plan, and their actual initiation of that therapy.
This finally brings me to my recent personal encounter. I have long taken care of a patient, much like Dr LoConte’s, with an extremely calm demeanor. I thought we had a great therapeutic alliance. I had to tell the patient that the disease had recurred, and then I laid out a treatment plan. It took weeks and then months for the insurer to approve this plan despite my providing my note in a timely fashion with a mountain of evidence behind the regimen that I’d selected.
This is where I think insurers — when they deny, deflect, and delay — are not taking adequate responsibility for the impact that has on the therapeutic alliance between a patient and their doctor. These people are trusting us with their lives. As an oncologist, I’ve already told them something they didn’t want to hear, and now I’m compounding that with the uncertainty of when we can actually begin treatment.
This gentleman — who, again, is normally extremely kind and affable — showed up at my office and was incredibly hostile toward me and my staff because of the delay that he was encountering. We literally couldn’t tell him when his insurer was going to approve his treatment, which would have been financially disastrous if he had tried to pay for it himself out of pocket. He needed his insurer’s approval before we could start, but we didn’t know when he could start. That uncertainty and not knowing was gnawing away at him until he was at the end of his rope.
What I’m here to say is that this has been a difficult couple of years in healthcare. I’m well aware that our ER staff are on the front lines, as are our bedside and inpatient teams. Even in the outpatient setting, I think we’re seeing this crucible and we’re seeing the pressure just grow, and grow, and grow. It’s like fracking. The more you increase the pressure, the more eventually you’re going to find out where the cracks are.
These patients are the ultimate stakeholders. It’s their lives on the line, and we should be concerned, but perhaps ultimately not surprised, that they’re lashing out to be heard. Given no other resort, they are taking out their frustration and their aggression on us. It›s not fair, but I am newly aware of it because, in a patient with whom I thought we had a superb rapport, I saw that vanish. As soon as he thought that his life was at risk, his fight-or-flight response kicked in. I was not dealing with the same man I knew. I was dealing with someone who was desperate and who just wanted to know when he could get the treatment.
I think this has taken the likelihood of workplace hostility to a whole other level for those of us in healthcare.
For any patients listening, I beg of you, please don’t shoot the messenger. We are here to serve you the best we can, but there are many external factors at play. We are doing our best to mitigate those for you so we can deliver the care that we promised in as timely a fashion as we can.
I hope everyone out there can stay safe. Thank you.
Dr. Lewis is director of gastrointestinal oncology at Intermountain Healthcare in Salt Lake City, Utah. He has an interest in neuroendocrine tumors, hereditary cancer syndromes, and patient-physician communication. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
This month, I want to tackle the difficult subject of violence toward healthcare workers. There’s a reason this is top of mind for me in my practice, but I want to start by acknowledging that this has been a much larger issue for our profession and one that has been growing for a number of years now.
They also estimate that that rate doubled between 2011 and 2018. I think that range is important because it proves this was a problem, and a crescendoing problem, even before COVID.
Another thing I think is relevant is to look at where in the healthcare system are these attacks most likely. In the emergency room, ER staff have seen hostility toward them rise by at least 25% over the past several years. Some of the seeds of mistrust that were sown between the general public and the scientific and medical communities around the pandemic. I think there’s some explanation there for why that might be a particular crucible.
Perhaps most disturbingly of all, 60% of the victims of healthcare workplace violence are bedside nurses. There is something about the intensity of the inpatient setting that makes nerves particularly frayed and unfortunately makes patients and family members more likely to lash out. I think it’s actually the heightened sense of mortality.
I’m not excusing any of these behaviors, but maybe it’s akin to road rage. On the road, behind the wheel, tiny gestures can actually be, on some level, perceived as threats to our survival. Another driver swerving into your lane activates a fight-or-flight response, you feel threatened, and you might respond in the moment very rashly. I wonder if we’re not seeing that, quite unfairly, play out against bedside staff in our hospitals.
Here’s the thing. Those of us who practice in the outpatient setting — 95% of my work, for instance, happens in clinic — are not immune to this either. There are some very harrowing recent examples of physicians being killed, typically at gunpoint, often by patients, sometimes by aggrieved family members, in their offices. An orthopedist in Tennessee, a back surgeon in Tulsa, along with three of their colleagues. In the latter case, the assailant specifically blamed the surgeon for their pain.
This is where I think things get even more scary. We have to be the bearers of bad news in our profession. This has long been the task of the oncologist, in particular, to convey things that people don’t want to hear.
I think what brought this to my mind in terms of my reading was an incredible article in The ASCO Post and also in the Journal of Clinical Oncology by Dr. Noelle LoConte, who’s a medical oncologist in Wisconsin. The article is called, “I Want to Kill You,” and it recounts her telling a previously stage III colon cancer patient, with whom she thought she had good rapport, that the disease had recurred. The patient’s immediate reaction in the heat of that moment was to say, Dr LoConte, I want to kill you. I want to blow your face off.
Already, there’s clearly tension when we are telling people what they don’t want to hear. I think the final piece of the puzzle goes back to the intrusion of the business of healthcare on the practice of medicine. This is what I witnessed very recently. One of the things that’s interesting to think about is how what we do is now framed as customer service. I know there’s deriding of this model, but if perception is reality, we have a system where patients are set up to view themselves as consumers.
Let’s say, for instance, you’re in the unfortunate circumstance of being diagnosed with cancer and your insurer gives you the option to go to multiple oncologists. If you’re online browsing for oncologists, how do you differentiate me from some of my colleagues? The answer on these rating websites often has to do with domains that are about the overall experience — not just the patient-doctor interaction but also things like wait time, friendliness of staff, and promptness of care delivery.
That, I think, is the final piece of the puzzle, because what I really risk when I sit down with a patient and lay out a treatment plan is overpromising and underdelivering. I am long used to citing median overall survival for expectation of outcome. Of course, every patient wants to be an exceptional responder. Most patients want to be on the latter half of median survival. No one wants to be on the disappointingly shorter half.
My point is that I’ve long been able to mitigate that uncertainty for patients. What is getting harder and harder to explain away is the delay incurred between someone’s diagnosis, my meeting them and laying out a treatment plan, and their actual initiation of that therapy.
This finally brings me to my recent personal encounter. I have long taken care of a patient, much like Dr LoConte’s, with an extremely calm demeanor. I thought we had a great therapeutic alliance. I had to tell the patient that the disease had recurred, and then I laid out a treatment plan. It took weeks and then months for the insurer to approve this plan despite my providing my note in a timely fashion with a mountain of evidence behind the regimen that I’d selected.
This is where I think insurers — when they deny, deflect, and delay — are not taking adequate responsibility for the impact that has on the therapeutic alliance between a patient and their doctor. These people are trusting us with their lives. As an oncologist, I’ve already told them something they didn’t want to hear, and now I’m compounding that with the uncertainty of when we can actually begin treatment.
This gentleman — who, again, is normally extremely kind and affable — showed up at my office and was incredibly hostile toward me and my staff because of the delay that he was encountering. We literally couldn’t tell him when his insurer was going to approve his treatment, which would have been financially disastrous if he had tried to pay for it himself out of pocket. He needed his insurer’s approval before we could start, but we didn’t know when he could start. That uncertainty and not knowing was gnawing away at him until he was at the end of his rope.
What I’m here to say is that this has been a difficult couple of years in healthcare. I’m well aware that our ER staff are on the front lines, as are our bedside and inpatient teams. Even in the outpatient setting, I think we’re seeing this crucible and we’re seeing the pressure just grow, and grow, and grow. It’s like fracking. The more you increase the pressure, the more eventually you’re going to find out where the cracks are.
These patients are the ultimate stakeholders. It’s their lives on the line, and we should be concerned, but perhaps ultimately not surprised, that they’re lashing out to be heard. Given no other resort, they are taking out their frustration and their aggression on us. It›s not fair, but I am newly aware of it because, in a patient with whom I thought we had a superb rapport, I saw that vanish. As soon as he thought that his life was at risk, his fight-or-flight response kicked in. I was not dealing with the same man I knew. I was dealing with someone who was desperate and who just wanted to know when he could get the treatment.
I think this has taken the likelihood of workplace hostility to a whole other level for those of us in healthcare.
For any patients listening, I beg of you, please don’t shoot the messenger. We are here to serve you the best we can, but there are many external factors at play. We are doing our best to mitigate those for you so we can deliver the care that we promised in as timely a fashion as we can.
I hope everyone out there can stay safe. Thank you.
Dr. Lewis is director of gastrointestinal oncology at Intermountain Healthcare in Salt Lake City, Utah. He has an interest in neuroendocrine tumors, hereditary cancer syndromes, and patient-physician communication. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
This month, I want to tackle the difficult subject of violence toward healthcare workers. There’s a reason this is top of mind for me in my practice, but I want to start by acknowledging that this has been a much larger issue for our profession and one that has been growing for a number of years now.
They also estimate that that rate doubled between 2011 and 2018. I think that range is important because it proves this was a problem, and a crescendoing problem, even before COVID.
Another thing I think is relevant is to look at where in the healthcare system are these attacks most likely. In the emergency room, ER staff have seen hostility toward them rise by at least 25% over the past several years. Some of the seeds of mistrust that were sown between the general public and the scientific and medical communities around the pandemic. I think there’s some explanation there for why that might be a particular crucible.
Perhaps most disturbingly of all, 60% of the victims of healthcare workplace violence are bedside nurses. There is something about the intensity of the inpatient setting that makes nerves particularly frayed and unfortunately makes patients and family members more likely to lash out. I think it’s actually the heightened sense of mortality.
I’m not excusing any of these behaviors, but maybe it’s akin to road rage. On the road, behind the wheel, tiny gestures can actually be, on some level, perceived as threats to our survival. Another driver swerving into your lane activates a fight-or-flight response, you feel threatened, and you might respond in the moment very rashly. I wonder if we’re not seeing that, quite unfairly, play out against bedside staff in our hospitals.
Here’s the thing. Those of us who practice in the outpatient setting — 95% of my work, for instance, happens in clinic — are not immune to this either. There are some very harrowing recent examples of physicians being killed, typically at gunpoint, often by patients, sometimes by aggrieved family members, in their offices. An orthopedist in Tennessee, a back surgeon in Tulsa, along with three of their colleagues. In the latter case, the assailant specifically blamed the surgeon for their pain.
This is where I think things get even more scary. We have to be the bearers of bad news in our profession. This has long been the task of the oncologist, in particular, to convey things that people don’t want to hear.
I think what brought this to my mind in terms of my reading was an incredible article in The ASCO Post and also in the Journal of Clinical Oncology by Dr. Noelle LoConte, who’s a medical oncologist in Wisconsin. The article is called, “I Want to Kill You,” and it recounts her telling a previously stage III colon cancer patient, with whom she thought she had good rapport, that the disease had recurred. The patient’s immediate reaction in the heat of that moment was to say, Dr LoConte, I want to kill you. I want to blow your face off.
Already, there’s clearly tension when we are telling people what they don’t want to hear. I think the final piece of the puzzle goes back to the intrusion of the business of healthcare on the practice of medicine. This is what I witnessed very recently. One of the things that’s interesting to think about is how what we do is now framed as customer service. I know there’s deriding of this model, but if perception is reality, we have a system where patients are set up to view themselves as consumers.
Let’s say, for instance, you’re in the unfortunate circumstance of being diagnosed with cancer and your insurer gives you the option to go to multiple oncologists. If you’re online browsing for oncologists, how do you differentiate me from some of my colleagues? The answer on these rating websites often has to do with domains that are about the overall experience — not just the patient-doctor interaction but also things like wait time, friendliness of staff, and promptness of care delivery.
That, I think, is the final piece of the puzzle, because what I really risk when I sit down with a patient and lay out a treatment plan is overpromising and underdelivering. I am long used to citing median overall survival for expectation of outcome. Of course, every patient wants to be an exceptional responder. Most patients want to be on the latter half of median survival. No one wants to be on the disappointingly shorter half.
My point is that I’ve long been able to mitigate that uncertainty for patients. What is getting harder and harder to explain away is the delay incurred between someone’s diagnosis, my meeting them and laying out a treatment plan, and their actual initiation of that therapy.
This finally brings me to my recent personal encounter. I have long taken care of a patient, much like Dr LoConte’s, with an extremely calm demeanor. I thought we had a great therapeutic alliance. I had to tell the patient that the disease had recurred, and then I laid out a treatment plan. It took weeks and then months for the insurer to approve this plan despite my providing my note in a timely fashion with a mountain of evidence behind the regimen that I’d selected.
This is where I think insurers — when they deny, deflect, and delay — are not taking adequate responsibility for the impact that has on the therapeutic alliance between a patient and their doctor. These people are trusting us with their lives. As an oncologist, I’ve already told them something they didn’t want to hear, and now I’m compounding that with the uncertainty of when we can actually begin treatment.
This gentleman — who, again, is normally extremely kind and affable — showed up at my office and was incredibly hostile toward me and my staff because of the delay that he was encountering. We literally couldn’t tell him when his insurer was going to approve his treatment, which would have been financially disastrous if he had tried to pay for it himself out of pocket. He needed his insurer’s approval before we could start, but we didn’t know when he could start. That uncertainty and not knowing was gnawing away at him until he was at the end of his rope.
What I’m here to say is that this has been a difficult couple of years in healthcare. I’m well aware that our ER staff are on the front lines, as are our bedside and inpatient teams. Even in the outpatient setting, I think we’re seeing this crucible and we’re seeing the pressure just grow, and grow, and grow. It’s like fracking. The more you increase the pressure, the more eventually you’re going to find out where the cracks are.
These patients are the ultimate stakeholders. It’s their lives on the line, and we should be concerned, but perhaps ultimately not surprised, that they’re lashing out to be heard. Given no other resort, they are taking out their frustration and their aggression on us. It›s not fair, but I am newly aware of it because, in a patient with whom I thought we had a superb rapport, I saw that vanish. As soon as he thought that his life was at risk, his fight-or-flight response kicked in. I was not dealing with the same man I knew. I was dealing with someone who was desperate and who just wanted to know when he could get the treatment.
I think this has taken the likelihood of workplace hostility to a whole other level for those of us in healthcare.
For any patients listening, I beg of you, please don’t shoot the messenger. We are here to serve you the best we can, but there are many external factors at play. We are doing our best to mitigate those for you so we can deliver the care that we promised in as timely a fashion as we can.
I hope everyone out there can stay safe. Thank you.
Dr. Lewis is director of gastrointestinal oncology at Intermountain Healthcare in Salt Lake City, Utah. He has an interest in neuroendocrine tumors, hereditary cancer syndromes, and patient-physician communication. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
New Prior Auth Policy Tied to Delays, Discontinuation of Oral Cancer Meds
TOPLINE:
Imposing a new prior authorization requirement increased the likelihood that older patients with cancer will delay or stop filling their prescription for oral anticancer drugs, a new study showed.
METHODOLOGY:
- Prior authorization requirements, especially in oncology, continue to increase, but how these policies affect patients’ access to care remains less clear.
- Researchers analyzed Medicare Part D claims from 2010 to 2020 to assess the effects of prior authorization changes on prescriptions fills for 1 of 11 oral anticancer drugs.
- The study included 2495 patients filling a prescription for these medications prior to their health plan imposing a new prior authorization policy and 22,641 patients filling prescriptions for the same drugs with no change in prior authorization policy (control).
- Beneficiaries had at least three 30-day fills in the 120 days before the new prior authorization policy was established on January 1 and continued to be enrolled in the same plan 120 days after the policy change.
- The researchers focused on how often patients discontinued their therapy within 120 days following a prior authorization policy change, as well as the time to fill a prescription after this change.
TAKEAWAY:
- Patients subjected to a new prior authorization policy on an established drug had a sevenfold higher likelihood of stopping the drug within 120 days than those who had no change in prior authorization requirements (adjusted odds ratio, 7.1).
- The adjusted probability of discontinuing an oral cancer regimen within 120 days after an index date of January 1 (when most health plan policy changes occur) was 5.8% for those with a new prior authorization policy vs 1.4% for the control group.
- A new prior authorization requirement was also associated with an average 10-day delay to refill the first prescription following the policy change (P < .001).
- The probability of a delay of more than 30 days was 22% after a policy change vs 7% after no policy change.
IN PRACTICE:
“Our results suggest concerns about delayed and foregone care related to prior authorization are warranted,” the authors said. Overall, this study found that “prior authorization wasted time and undermined the policy priorities of access to care and oral anticancer drug adherence for patients who were regular users of a particular medication.”
SOURCE:
The study by Michael Anna Kyle, PhD, RN, and Nancy Keating, MD, MPH, with Harvard Medical School, Boston, was published online in the Journal of Clinical Oncology.
LIMITATIONS:
The study did not look at patients starting new oral anticancer drugs, which may come with more complex prior authorization processes and create more significant access issues. The results are also limited to patients taking 1 of 11 oral anticancer agents in Medicare Part D.
DISCLOSURES:
Funding for the study was provided by the National Cancer Institute. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Imposing a new prior authorization requirement increased the likelihood that older patients with cancer will delay or stop filling their prescription for oral anticancer drugs, a new study showed.
METHODOLOGY:
- Prior authorization requirements, especially in oncology, continue to increase, but how these policies affect patients’ access to care remains less clear.
- Researchers analyzed Medicare Part D claims from 2010 to 2020 to assess the effects of prior authorization changes on prescriptions fills for 1 of 11 oral anticancer drugs.
- The study included 2495 patients filling a prescription for these medications prior to their health plan imposing a new prior authorization policy and 22,641 patients filling prescriptions for the same drugs with no change in prior authorization policy (control).
- Beneficiaries had at least three 30-day fills in the 120 days before the new prior authorization policy was established on January 1 and continued to be enrolled in the same plan 120 days after the policy change.
- The researchers focused on how often patients discontinued their therapy within 120 days following a prior authorization policy change, as well as the time to fill a prescription after this change.
TAKEAWAY:
- Patients subjected to a new prior authorization policy on an established drug had a sevenfold higher likelihood of stopping the drug within 120 days than those who had no change in prior authorization requirements (adjusted odds ratio, 7.1).
- The adjusted probability of discontinuing an oral cancer regimen within 120 days after an index date of January 1 (when most health plan policy changes occur) was 5.8% for those with a new prior authorization policy vs 1.4% for the control group.
- A new prior authorization requirement was also associated with an average 10-day delay to refill the first prescription following the policy change (P < .001).
- The probability of a delay of more than 30 days was 22% after a policy change vs 7% after no policy change.
IN PRACTICE:
“Our results suggest concerns about delayed and foregone care related to prior authorization are warranted,” the authors said. Overall, this study found that “prior authorization wasted time and undermined the policy priorities of access to care and oral anticancer drug adherence for patients who were regular users of a particular medication.”
SOURCE:
The study by Michael Anna Kyle, PhD, RN, and Nancy Keating, MD, MPH, with Harvard Medical School, Boston, was published online in the Journal of Clinical Oncology.
LIMITATIONS:
The study did not look at patients starting new oral anticancer drugs, which may come with more complex prior authorization processes and create more significant access issues. The results are also limited to patients taking 1 of 11 oral anticancer agents in Medicare Part D.
DISCLOSURES:
Funding for the study was provided by the National Cancer Institute. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
Imposing a new prior authorization requirement increased the likelihood that older patients with cancer will delay or stop filling their prescription for oral anticancer drugs, a new study showed.
METHODOLOGY:
- Prior authorization requirements, especially in oncology, continue to increase, but how these policies affect patients’ access to care remains less clear.
- Researchers analyzed Medicare Part D claims from 2010 to 2020 to assess the effects of prior authorization changes on prescriptions fills for 1 of 11 oral anticancer drugs.
- The study included 2495 patients filling a prescription for these medications prior to their health plan imposing a new prior authorization policy and 22,641 patients filling prescriptions for the same drugs with no change in prior authorization policy (control).
- Beneficiaries had at least three 30-day fills in the 120 days before the new prior authorization policy was established on January 1 and continued to be enrolled in the same plan 120 days after the policy change.
- The researchers focused on how often patients discontinued their therapy within 120 days following a prior authorization policy change, as well as the time to fill a prescription after this change.
TAKEAWAY:
- Patients subjected to a new prior authorization policy on an established drug had a sevenfold higher likelihood of stopping the drug within 120 days than those who had no change in prior authorization requirements (adjusted odds ratio, 7.1).
- The adjusted probability of discontinuing an oral cancer regimen within 120 days after an index date of January 1 (when most health plan policy changes occur) was 5.8% for those with a new prior authorization policy vs 1.4% for the control group.
- A new prior authorization requirement was also associated with an average 10-day delay to refill the first prescription following the policy change (P < .001).
- The probability of a delay of more than 30 days was 22% after a policy change vs 7% after no policy change.
IN PRACTICE:
“Our results suggest concerns about delayed and foregone care related to prior authorization are warranted,” the authors said. Overall, this study found that “prior authorization wasted time and undermined the policy priorities of access to care and oral anticancer drug adherence for patients who were regular users of a particular medication.”
SOURCE:
The study by Michael Anna Kyle, PhD, RN, and Nancy Keating, MD, MPH, with Harvard Medical School, Boston, was published online in the Journal of Clinical Oncology.
LIMITATIONS:
The study did not look at patients starting new oral anticancer drugs, which may come with more complex prior authorization processes and create more significant access issues. The results are also limited to patients taking 1 of 11 oral anticancer agents in Medicare Part D.
DISCLOSURES:
Funding for the study was provided by the National Cancer Institute. The authors reported no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
‘Left in the Dark’: Prior Authorization Erodes Trust, Costs More
Mark Lewis, MD, saw the pain in his patient’s body. The man’s gastrointestinal tumor had metastasized to his bones. Even breathing had become agonizing.
It was a Friday afternoon. Dr. Lewis could see his patient would struggle to make it through the weekend without some pain relief.
When this happens, “the clock is ticking,” said Dr. Lewis, director of gastrointestinal oncology at Intermountain Health in Salt Lake City, Utah. “A patient, especially one with more advanced disease, only has so much time to wait for care.”
Dr. Lewis sent in an electronic request for an opioid prescription to help ease his patient’s pain through the weekend. Once the prescription had gone through, Dr. Lewis told his patient the medication should be ready to pick up at his local pharmacy.
Dr. Lewis left work that Friday feeling a little lighter, knowing the pain medication would help his patient over the weekend.
Moments after walking into the clinic on Monday morning, Dr. Lewis received an unexpected message: “Your patient is in the hospital.”
The events of the weekend soon unfolded.
Dr. Lewis learned that when his patient went to the pharmacy to pick up his pain medication, the pharmacist told him the prescription required prior authorization.
The patient left the pharmacy empty-handed. Hours later, he was in the emergency room (ER) in extreme pain — the exact situation Dr. Lewis had been trying to avoid.
Dr. Lewis felt a sense of powerlessness in that moment.
“I had been left in the dark,” he said. The oncologist-patient relationship is predicated on trust and “that trust is eroded when I can’t give my patients the care they need,” he explained. “I can’t stand overpromising and underdelivering to them.”
Dr. Lewis had received no communication from the insurer that the prescription required prior authorization, no red flag that the request had been denied, and no notification to call the insurer.
Although physicians may need to tread carefully when prescribing opioids over the long term, “this was simply a prescription for 2-3 days of opioids for the exact patient who the drugs were developed to benefit,” Dr. Lewis said. But instead, “he ended up in ER with a pain crisis.”
Prior authorization delays like this often mean patients pay the price.
“These delays are not trivial,” Dr. Lewis said.
A recent study, presented at the ASCO Quality Care Symposium in October, found that among 3304 supportive care prescriptions requiring prior authorization, insurance companies denied 8% of requests, with final denials taking as long as 78 days. Among approved prescriptions, about 40% happened on the same day, while the remaining took anywhere from 1 to 54 days.
Denying or delaying necessary and cost-effective care, even briefly, can harm patients and lead to higher costs. A 2022 survey from the American Medical Association found that instead of reducing low-value care as insurance companies claim, prior authorization often leads to higher overall use of healthcare resources. More specifically, almost half of physicians surveyed said that prior authorization led to an ER visit or need for immediate care.
In this patient’s case, filling the opioid prescription that Friday would have cost no more than $300, possibly as little as $30. The ER visit to manage the patient’s pain crisis costs thousands.
The major issue overall, Dr. Lewis said, is the disconnect between the time spent waiting for prior authorization approvals and the necessity of these treatments. Dr. Lewis says even standard chemotherapy often requires prior authorization.
“The currency we all share is time,” Dr. Lewis said. “But it often feels like there’s very little urgency on insurance company side to approve a treatment, which places a heavy weight on patients and physicians.”
“It just shouldn’t be this hard,” he said.
A version of this article appeared on Medscape.com as part of the Gatekeepers of Care series on issues oncologists and people with cancer face navigating health insurance company requirements. Read more about the series here. Please email [email protected] to share experiences with prior authorization or other challenges receiving care.
Mark Lewis, MD, saw the pain in his patient’s body. The man’s gastrointestinal tumor had metastasized to his bones. Even breathing had become agonizing.
It was a Friday afternoon. Dr. Lewis could see his patient would struggle to make it through the weekend without some pain relief.
When this happens, “the clock is ticking,” said Dr. Lewis, director of gastrointestinal oncology at Intermountain Health in Salt Lake City, Utah. “A patient, especially one with more advanced disease, only has so much time to wait for care.”
Dr. Lewis sent in an electronic request for an opioid prescription to help ease his patient’s pain through the weekend. Once the prescription had gone through, Dr. Lewis told his patient the medication should be ready to pick up at his local pharmacy.
Dr. Lewis left work that Friday feeling a little lighter, knowing the pain medication would help his patient over the weekend.
Moments after walking into the clinic on Monday morning, Dr. Lewis received an unexpected message: “Your patient is in the hospital.”
The events of the weekend soon unfolded.
Dr. Lewis learned that when his patient went to the pharmacy to pick up his pain medication, the pharmacist told him the prescription required prior authorization.
The patient left the pharmacy empty-handed. Hours later, he was in the emergency room (ER) in extreme pain — the exact situation Dr. Lewis had been trying to avoid.
Dr. Lewis felt a sense of powerlessness in that moment.
“I had been left in the dark,” he said. The oncologist-patient relationship is predicated on trust and “that trust is eroded when I can’t give my patients the care they need,” he explained. “I can’t stand overpromising and underdelivering to them.”
Dr. Lewis had received no communication from the insurer that the prescription required prior authorization, no red flag that the request had been denied, and no notification to call the insurer.
Although physicians may need to tread carefully when prescribing opioids over the long term, “this was simply a prescription for 2-3 days of opioids for the exact patient who the drugs were developed to benefit,” Dr. Lewis said. But instead, “he ended up in ER with a pain crisis.”
Prior authorization delays like this often mean patients pay the price.
“These delays are not trivial,” Dr. Lewis said.
A recent study, presented at the ASCO Quality Care Symposium in October, found that among 3304 supportive care prescriptions requiring prior authorization, insurance companies denied 8% of requests, with final denials taking as long as 78 days. Among approved prescriptions, about 40% happened on the same day, while the remaining took anywhere from 1 to 54 days.
Denying or delaying necessary and cost-effective care, even briefly, can harm patients and lead to higher costs. A 2022 survey from the American Medical Association found that instead of reducing low-value care as insurance companies claim, prior authorization often leads to higher overall use of healthcare resources. More specifically, almost half of physicians surveyed said that prior authorization led to an ER visit or need for immediate care.
In this patient’s case, filling the opioid prescription that Friday would have cost no more than $300, possibly as little as $30. The ER visit to manage the patient’s pain crisis costs thousands.
The major issue overall, Dr. Lewis said, is the disconnect between the time spent waiting for prior authorization approvals and the necessity of these treatments. Dr. Lewis says even standard chemotherapy often requires prior authorization.
“The currency we all share is time,” Dr. Lewis said. “But it often feels like there’s very little urgency on insurance company side to approve a treatment, which places a heavy weight on patients and physicians.”
“It just shouldn’t be this hard,” he said.
A version of this article appeared on Medscape.com as part of the Gatekeepers of Care series on issues oncologists and people with cancer face navigating health insurance company requirements. Read more about the series here. Please email [email protected] to share experiences with prior authorization or other challenges receiving care.
Mark Lewis, MD, saw the pain in his patient’s body. The man’s gastrointestinal tumor had metastasized to his bones. Even breathing had become agonizing.
It was a Friday afternoon. Dr. Lewis could see his patient would struggle to make it through the weekend without some pain relief.
When this happens, “the clock is ticking,” said Dr. Lewis, director of gastrointestinal oncology at Intermountain Health in Salt Lake City, Utah. “A patient, especially one with more advanced disease, only has so much time to wait for care.”
Dr. Lewis sent in an electronic request for an opioid prescription to help ease his patient’s pain through the weekend. Once the prescription had gone through, Dr. Lewis told his patient the medication should be ready to pick up at his local pharmacy.
Dr. Lewis left work that Friday feeling a little lighter, knowing the pain medication would help his patient over the weekend.
Moments after walking into the clinic on Monday morning, Dr. Lewis received an unexpected message: “Your patient is in the hospital.”
The events of the weekend soon unfolded.
Dr. Lewis learned that when his patient went to the pharmacy to pick up his pain medication, the pharmacist told him the prescription required prior authorization.
The patient left the pharmacy empty-handed. Hours later, he was in the emergency room (ER) in extreme pain — the exact situation Dr. Lewis had been trying to avoid.
Dr. Lewis felt a sense of powerlessness in that moment.
“I had been left in the dark,” he said. The oncologist-patient relationship is predicated on trust and “that trust is eroded when I can’t give my patients the care they need,” he explained. “I can’t stand overpromising and underdelivering to them.”
Dr. Lewis had received no communication from the insurer that the prescription required prior authorization, no red flag that the request had been denied, and no notification to call the insurer.
Although physicians may need to tread carefully when prescribing opioids over the long term, “this was simply a prescription for 2-3 days of opioids for the exact patient who the drugs were developed to benefit,” Dr. Lewis said. But instead, “he ended up in ER with a pain crisis.”
Prior authorization delays like this often mean patients pay the price.
“These delays are not trivial,” Dr. Lewis said.
A recent study, presented at the ASCO Quality Care Symposium in October, found that among 3304 supportive care prescriptions requiring prior authorization, insurance companies denied 8% of requests, with final denials taking as long as 78 days. Among approved prescriptions, about 40% happened on the same day, while the remaining took anywhere from 1 to 54 days.
Denying or delaying necessary and cost-effective care, even briefly, can harm patients and lead to higher costs. A 2022 survey from the American Medical Association found that instead of reducing low-value care as insurance companies claim, prior authorization often leads to higher overall use of healthcare resources. More specifically, almost half of physicians surveyed said that prior authorization led to an ER visit or need for immediate care.
In this patient’s case, filling the opioid prescription that Friday would have cost no more than $300, possibly as little as $30. The ER visit to manage the patient’s pain crisis costs thousands.
The major issue overall, Dr. Lewis said, is the disconnect between the time spent waiting for prior authorization approvals and the necessity of these treatments. Dr. Lewis says even standard chemotherapy often requires prior authorization.
“The currency we all share is time,” Dr. Lewis said. “But it often feels like there’s very little urgency on insurance company side to approve a treatment, which places a heavy weight on patients and physicians.”
“It just shouldn’t be this hard,” he said.
A version of this article appeared on Medscape.com as part of the Gatekeepers of Care series on issues oncologists and people with cancer face navigating health insurance company requirements. Read more about the series here. Please email [email protected] to share experiences with prior authorization or other challenges receiving care.
Why Do MDs Have Such a High Rate of Eating Disorders?
Ten years ago, Clare Gerada, FRCGP, an advocate for physician well-being and today president of the UK’s Royal College of General Practitioners, made a prediction to the audience at the International Conference on Physician Health.
“We have seen a massive increase in eating disorders [among doctors],” she said. “I’m not sure anybody is quite aware of the tsunami of eating disorders,” she believed would soon strike predominantly female physicians.
That was 2014. Did the tsunami hit?
Quite possibly. Data are limited on the prevalence of eating disorders (EDs) among healthcare workers, but studies do exist. A 2019 global review and meta-analysis determined “the summary prevalence of eating disorder (ED) risk among medical students was 10.4%.”
A 2022 update of that review boosted the estimate to 17.35%.
Tsunami or not, that’s nearly double the 9% rate within the US general public (from a 2020 report from STRIPED and the Academy of Eating Disorders). And while the following stat isn’t an indicator of EDs per se,
To her credit, Dr. Gerada, awarded a damehood in 2020, was in a position to know what was coming. Her statement was informed by research showing an increasing number of young doctors seeking treatment for mental health issues, including EDs, through the NHS Practitioner Health program, a mental health service she established in 2008.
So ... what puts doctors at such a high risk for EDs?
Be Careful of ‘Overlap Traits’
As with many mental health issues, EDs have no single cause. Researchers believe they stem from a complex interaction of genetic, biological, behavioral, psychological, and social factors. But the medical field should take note: Some personality traits commonly associated with EDs are often shared by successful physicians.
“I think some of the overlap traits would be being highly driven, goal-oriented and self-critical,” said Lesley Williams, MD, a family medicine physician at the Mayo Clinic in Phoenix, Arizona. “A lot of those traits can make you a very successful physician and physician-in-training but could also potentially spill over into body image and rigidity around food.”
Of course, we want physicians to strive for excellence, and the majority of diligent, driven doctors will not develop an ED.
But when pushed too far, those admirable qualities can easily become perfectionism — which has long been recognized as a risk factor for EDs, an association supported by decades of research.
Medical School: Where EDs Begin and Little Education About Them Happens
“I think medicine in general attracts people that often share similar characteristics to those who struggle with EDs — high-achieving, hardworking perfectionists who put a lot of pressure on themselves,” said Elizabeth McNaught, MD, a general practitioner and medical director at Family Mental Wealth.
Diagnosed with an ED at 14, Dr. McNaught has experienced this firsthand and shared her story in a 2020 memoir, Life Hurts: A Doctor’s Personal Journey Through Anorexia.
Competitive, high-stress environments can also be a trigger, Dr. McNaught explained. “The pressure of medical school,” for example, “can perpetuate an eating disorder if that’s something that you’re struggling with,” she said.
Pressure to perform may not be the only problem. Medical students are taught to view weight as a key indicator of health. Multiple studies suggested that not only does weight stigma exist in healthcare but also it has increased over time and negatively affects patients’ psychological well-being and physical health.
There is far less public discourse about how weight stigma can be harmful to medical students and physicians themselves. Dr. Williams believed the weight-centric paradigm was key.
“For so long, we believed that health presents itself within these confines on a BMI chart and anything outside of that is unhealthy and must be fixed,” she said. “I can say from having gone through medical education, having that continual messaging does make someone feel that if I myself am not within those confines, then I need to do something to fix that immediately if I’m going to continue to care for patients.”
In general, Dr. Williams, and Dr. McNaught agreed that medical training around EDs is lacking, producing doctors who are ill-equipped to diagnose, treat, or even discuss them with patients. Dr. Williams recalled only one lecture on the topic in med school.
“And yet, anorexia carries the second highest death rate of all mental illnesses after opioid-use disorders,” she said, “so it’s astonishing that that just wasn’t included.”
MDs Hiding Mental Health Issues
Claire Anderson, MD (a pseudonym), emphatically stated she would never tell anyone at the hospital where she works in the emergency department that she has an ED.
“There is still a lot of misunderstanding about mental health, and I never want people to doubt my ability to care for people,” Dr. Anderson said. “There’s so much stigma around eating disorders, and I also feel like once it’s out there, I can’t take it back, and I don’t want to feel like people are watching me.”
Melissa Klein, PhD, a clinical psychologist specializing in EDs, has more than 25 years of experience working the inpatient ED unit at New York Presbyterian. Having treated medical professionals, Dr. Klein said they have legitimate concerns about revealing their struggles.
“Sometimes, they do get reported to higher ups — the boards,” Dr. Klein said, “and they’re told that they have to get help in order for them to continue to work in their profession. I think people might be scared to ask for help because of that reason.”
Doctors Often Ignore EDs or Teach ‘Bad Habits’
Dr. Anderson firmly believed that if her early treatment from doctors had been better, she might not be struggling so much today.
The first time Dr. Anderson’s mother brought up her daughter’s sudden weight loss at 14, their family doctor conferred with a chart and said there was no reason to worry; Dr. Anderson’s weight was “normal.” “I was eating like 500 calories a day and swimming for 3 hours, and [by saying that], they assured me I was fine,” she recalls.
At 15, when Dr. Anderson went in for an initial assessment for an ED, she thought she’d be connected with a nutritionist and sent home. “I didn’t have a lot of classic thoughts of wanting to be thin or wanting to lose weight,” she said.
Instead, Dr. Anderson was sent to inpatient care, which she credits with escalating her ED. “I picked up on a lot of really bad habits when I went there — I sort of learned how to have an eating disorder,” she said. “When I left, it was very different than when I went in, which is kind of sad.”
Throughout high school, Dr. Anderson went in and out of so many hospitals and treatment programs that she’s lost track of them. Then, in 2008, she left formal treatment altogether. “I had been really angry with the treatment programs for trying to fit me into their box with a rigid schedule of inpatient and outpatient care,” she recalled. “I didn’t want to live in that world anymore.”
After working with a new psychiatrist, Dr. Anderson’s situation improved until a particularly stressful second year of residency. “That’s when I just tanked,” she said. “Residency, and especially being on my own and with COVID, things have not been great for me.”
Dr. Anderson now sees an eating disorder specialist, but she pays for this out-of-pocket. “I have terrible insurance,” she said with a laugh, aware of that irony.
If You Are Struggling, Don’t Be Ashamed
Some physicians who’ve experienced EDs firsthand are working to improve training on diagnosing and treating the conditions. Dr. McNaught has developed and launched a new eLearning program for healthcare workers on how to recognize the early signs and symptoms of an ED and provide support.
“It’s not only so they can recognize it in their patients but also if colleagues and family and friends are struggling,” she said.
In 2021, the American Psychiatric Association (APA) approved the APA Practice Guideline for the Treatment of Patients With Eating Disorders, which aims to improve patient care and treatment outcomes.
But Dr. Klein is concerned that increased stress since the COVID-19 pandemic may be putting healthcare workers at even greater risk.
“When people are under stress or when they feel like there are things in their life that maybe they can’t control, sometimes turning to an eating disorder is a way to cope,” she said, “In that sense, the stress on medical professionals is something that could lead to eating disorder behaviors.”
Dr. Klein’s message to healthcare workers: Don’t be ashamed. She described an ED as “a monster that takes over your brain. Once it starts, it’s very hard to turn it around on your own. So, I hope anyone who is suffering, in whatever field they’re in, that they are able to ask for help.”
A version of this article appeared on Medscape.com.
Ten years ago, Clare Gerada, FRCGP, an advocate for physician well-being and today president of the UK’s Royal College of General Practitioners, made a prediction to the audience at the International Conference on Physician Health.
“We have seen a massive increase in eating disorders [among doctors],” she said. “I’m not sure anybody is quite aware of the tsunami of eating disorders,” she believed would soon strike predominantly female physicians.
That was 2014. Did the tsunami hit?
Quite possibly. Data are limited on the prevalence of eating disorders (EDs) among healthcare workers, but studies do exist. A 2019 global review and meta-analysis determined “the summary prevalence of eating disorder (ED) risk among medical students was 10.4%.”
A 2022 update of that review boosted the estimate to 17.35%.
Tsunami or not, that’s nearly double the 9% rate within the US general public (from a 2020 report from STRIPED and the Academy of Eating Disorders). And while the following stat isn’t an indicator of EDs per se,
To her credit, Dr. Gerada, awarded a damehood in 2020, was in a position to know what was coming. Her statement was informed by research showing an increasing number of young doctors seeking treatment for mental health issues, including EDs, through the NHS Practitioner Health program, a mental health service she established in 2008.
So ... what puts doctors at such a high risk for EDs?
Be Careful of ‘Overlap Traits’
As with many mental health issues, EDs have no single cause. Researchers believe they stem from a complex interaction of genetic, biological, behavioral, psychological, and social factors. But the medical field should take note: Some personality traits commonly associated with EDs are often shared by successful physicians.
“I think some of the overlap traits would be being highly driven, goal-oriented and self-critical,” said Lesley Williams, MD, a family medicine physician at the Mayo Clinic in Phoenix, Arizona. “A lot of those traits can make you a very successful physician and physician-in-training but could also potentially spill over into body image and rigidity around food.”
Of course, we want physicians to strive for excellence, and the majority of diligent, driven doctors will not develop an ED.
But when pushed too far, those admirable qualities can easily become perfectionism — which has long been recognized as a risk factor for EDs, an association supported by decades of research.
Medical School: Where EDs Begin and Little Education About Them Happens
“I think medicine in general attracts people that often share similar characteristics to those who struggle with EDs — high-achieving, hardworking perfectionists who put a lot of pressure on themselves,” said Elizabeth McNaught, MD, a general practitioner and medical director at Family Mental Wealth.
Diagnosed with an ED at 14, Dr. McNaught has experienced this firsthand and shared her story in a 2020 memoir, Life Hurts: A Doctor’s Personal Journey Through Anorexia.
Competitive, high-stress environments can also be a trigger, Dr. McNaught explained. “The pressure of medical school,” for example, “can perpetuate an eating disorder if that’s something that you’re struggling with,” she said.
Pressure to perform may not be the only problem. Medical students are taught to view weight as a key indicator of health. Multiple studies suggested that not only does weight stigma exist in healthcare but also it has increased over time and negatively affects patients’ psychological well-being and physical health.
There is far less public discourse about how weight stigma can be harmful to medical students and physicians themselves. Dr. Williams believed the weight-centric paradigm was key.
“For so long, we believed that health presents itself within these confines on a BMI chart and anything outside of that is unhealthy and must be fixed,” she said. “I can say from having gone through medical education, having that continual messaging does make someone feel that if I myself am not within those confines, then I need to do something to fix that immediately if I’m going to continue to care for patients.”
In general, Dr. Williams, and Dr. McNaught agreed that medical training around EDs is lacking, producing doctors who are ill-equipped to diagnose, treat, or even discuss them with patients. Dr. Williams recalled only one lecture on the topic in med school.
“And yet, anorexia carries the second highest death rate of all mental illnesses after opioid-use disorders,” she said, “so it’s astonishing that that just wasn’t included.”
MDs Hiding Mental Health Issues
Claire Anderson, MD (a pseudonym), emphatically stated she would never tell anyone at the hospital where she works in the emergency department that she has an ED.
“There is still a lot of misunderstanding about mental health, and I never want people to doubt my ability to care for people,” Dr. Anderson said. “There’s so much stigma around eating disorders, and I also feel like once it’s out there, I can’t take it back, and I don’t want to feel like people are watching me.”
Melissa Klein, PhD, a clinical psychologist specializing in EDs, has more than 25 years of experience working the inpatient ED unit at New York Presbyterian. Having treated medical professionals, Dr. Klein said they have legitimate concerns about revealing their struggles.
“Sometimes, they do get reported to higher ups — the boards,” Dr. Klein said, “and they’re told that they have to get help in order for them to continue to work in their profession. I think people might be scared to ask for help because of that reason.”
Doctors Often Ignore EDs or Teach ‘Bad Habits’
Dr. Anderson firmly believed that if her early treatment from doctors had been better, she might not be struggling so much today.
The first time Dr. Anderson’s mother brought up her daughter’s sudden weight loss at 14, their family doctor conferred with a chart and said there was no reason to worry; Dr. Anderson’s weight was “normal.” “I was eating like 500 calories a day and swimming for 3 hours, and [by saying that], they assured me I was fine,” she recalls.
At 15, when Dr. Anderson went in for an initial assessment for an ED, she thought she’d be connected with a nutritionist and sent home. “I didn’t have a lot of classic thoughts of wanting to be thin or wanting to lose weight,” she said.
Instead, Dr. Anderson was sent to inpatient care, which she credits with escalating her ED. “I picked up on a lot of really bad habits when I went there — I sort of learned how to have an eating disorder,” she said. “When I left, it was very different than when I went in, which is kind of sad.”
Throughout high school, Dr. Anderson went in and out of so many hospitals and treatment programs that she’s lost track of them. Then, in 2008, she left formal treatment altogether. “I had been really angry with the treatment programs for trying to fit me into their box with a rigid schedule of inpatient and outpatient care,” she recalled. “I didn’t want to live in that world anymore.”
After working with a new psychiatrist, Dr. Anderson’s situation improved until a particularly stressful second year of residency. “That’s when I just tanked,” she said. “Residency, and especially being on my own and with COVID, things have not been great for me.”
Dr. Anderson now sees an eating disorder specialist, but she pays for this out-of-pocket. “I have terrible insurance,” she said with a laugh, aware of that irony.
If You Are Struggling, Don’t Be Ashamed
Some physicians who’ve experienced EDs firsthand are working to improve training on diagnosing and treating the conditions. Dr. McNaught has developed and launched a new eLearning program for healthcare workers on how to recognize the early signs and symptoms of an ED and provide support.
“It’s not only so they can recognize it in their patients but also if colleagues and family and friends are struggling,” she said.
In 2021, the American Psychiatric Association (APA) approved the APA Practice Guideline for the Treatment of Patients With Eating Disorders, which aims to improve patient care and treatment outcomes.
But Dr. Klein is concerned that increased stress since the COVID-19 pandemic may be putting healthcare workers at even greater risk.
“When people are under stress or when they feel like there are things in their life that maybe they can’t control, sometimes turning to an eating disorder is a way to cope,” she said, “In that sense, the stress on medical professionals is something that could lead to eating disorder behaviors.”
Dr. Klein’s message to healthcare workers: Don’t be ashamed. She described an ED as “a monster that takes over your brain. Once it starts, it’s very hard to turn it around on your own. So, I hope anyone who is suffering, in whatever field they’re in, that they are able to ask for help.”
A version of this article appeared on Medscape.com.
Ten years ago, Clare Gerada, FRCGP, an advocate for physician well-being and today president of the UK’s Royal College of General Practitioners, made a prediction to the audience at the International Conference on Physician Health.
“We have seen a massive increase in eating disorders [among doctors],” she said. “I’m not sure anybody is quite aware of the tsunami of eating disorders,” she believed would soon strike predominantly female physicians.
That was 2014. Did the tsunami hit?
Quite possibly. Data are limited on the prevalence of eating disorders (EDs) among healthcare workers, but studies do exist. A 2019 global review and meta-analysis determined “the summary prevalence of eating disorder (ED) risk among medical students was 10.4%.”
A 2022 update of that review boosted the estimate to 17.35%.
Tsunami or not, that’s nearly double the 9% rate within the US general public (from a 2020 report from STRIPED and the Academy of Eating Disorders). And while the following stat isn’t an indicator of EDs per se,
To her credit, Dr. Gerada, awarded a damehood in 2020, was in a position to know what was coming. Her statement was informed by research showing an increasing number of young doctors seeking treatment for mental health issues, including EDs, through the NHS Practitioner Health program, a mental health service she established in 2008.
So ... what puts doctors at such a high risk for EDs?
Be Careful of ‘Overlap Traits’
As with many mental health issues, EDs have no single cause. Researchers believe they stem from a complex interaction of genetic, biological, behavioral, psychological, and social factors. But the medical field should take note: Some personality traits commonly associated with EDs are often shared by successful physicians.
“I think some of the overlap traits would be being highly driven, goal-oriented and self-critical,” said Lesley Williams, MD, a family medicine physician at the Mayo Clinic in Phoenix, Arizona. “A lot of those traits can make you a very successful physician and physician-in-training but could also potentially spill over into body image and rigidity around food.”
Of course, we want physicians to strive for excellence, and the majority of diligent, driven doctors will not develop an ED.
But when pushed too far, those admirable qualities can easily become perfectionism — which has long been recognized as a risk factor for EDs, an association supported by decades of research.
Medical School: Where EDs Begin and Little Education About Them Happens
“I think medicine in general attracts people that often share similar characteristics to those who struggle with EDs — high-achieving, hardworking perfectionists who put a lot of pressure on themselves,” said Elizabeth McNaught, MD, a general practitioner and medical director at Family Mental Wealth.
Diagnosed with an ED at 14, Dr. McNaught has experienced this firsthand and shared her story in a 2020 memoir, Life Hurts: A Doctor’s Personal Journey Through Anorexia.
Competitive, high-stress environments can also be a trigger, Dr. McNaught explained. “The pressure of medical school,” for example, “can perpetuate an eating disorder if that’s something that you’re struggling with,” she said.
Pressure to perform may not be the only problem. Medical students are taught to view weight as a key indicator of health. Multiple studies suggested that not only does weight stigma exist in healthcare but also it has increased over time and negatively affects patients’ psychological well-being and physical health.
There is far less public discourse about how weight stigma can be harmful to medical students and physicians themselves. Dr. Williams believed the weight-centric paradigm was key.
“For so long, we believed that health presents itself within these confines on a BMI chart and anything outside of that is unhealthy and must be fixed,” she said. “I can say from having gone through medical education, having that continual messaging does make someone feel that if I myself am not within those confines, then I need to do something to fix that immediately if I’m going to continue to care for patients.”
In general, Dr. Williams, and Dr. McNaught agreed that medical training around EDs is lacking, producing doctors who are ill-equipped to diagnose, treat, or even discuss them with patients. Dr. Williams recalled only one lecture on the topic in med school.
“And yet, anorexia carries the second highest death rate of all mental illnesses after opioid-use disorders,” she said, “so it’s astonishing that that just wasn’t included.”
MDs Hiding Mental Health Issues
Claire Anderson, MD (a pseudonym), emphatically stated she would never tell anyone at the hospital where she works in the emergency department that she has an ED.
“There is still a lot of misunderstanding about mental health, and I never want people to doubt my ability to care for people,” Dr. Anderson said. “There’s so much stigma around eating disorders, and I also feel like once it’s out there, I can’t take it back, and I don’t want to feel like people are watching me.”
Melissa Klein, PhD, a clinical psychologist specializing in EDs, has more than 25 years of experience working the inpatient ED unit at New York Presbyterian. Having treated medical professionals, Dr. Klein said they have legitimate concerns about revealing their struggles.
“Sometimes, they do get reported to higher ups — the boards,” Dr. Klein said, “and they’re told that they have to get help in order for them to continue to work in their profession. I think people might be scared to ask for help because of that reason.”
Doctors Often Ignore EDs or Teach ‘Bad Habits’
Dr. Anderson firmly believed that if her early treatment from doctors had been better, she might not be struggling so much today.
The first time Dr. Anderson’s mother brought up her daughter’s sudden weight loss at 14, their family doctor conferred with a chart and said there was no reason to worry; Dr. Anderson’s weight was “normal.” “I was eating like 500 calories a day and swimming for 3 hours, and [by saying that], they assured me I was fine,” she recalls.
At 15, when Dr. Anderson went in for an initial assessment for an ED, she thought she’d be connected with a nutritionist and sent home. “I didn’t have a lot of classic thoughts of wanting to be thin or wanting to lose weight,” she said.
Instead, Dr. Anderson was sent to inpatient care, which she credits with escalating her ED. “I picked up on a lot of really bad habits when I went there — I sort of learned how to have an eating disorder,” she said. “When I left, it was very different than when I went in, which is kind of sad.”
Throughout high school, Dr. Anderson went in and out of so many hospitals and treatment programs that she’s lost track of them. Then, in 2008, she left formal treatment altogether. “I had been really angry with the treatment programs for trying to fit me into their box with a rigid schedule of inpatient and outpatient care,” she recalled. “I didn’t want to live in that world anymore.”
After working with a new psychiatrist, Dr. Anderson’s situation improved until a particularly stressful second year of residency. “That’s when I just tanked,” she said. “Residency, and especially being on my own and with COVID, things have not been great for me.”
Dr. Anderson now sees an eating disorder specialist, but she pays for this out-of-pocket. “I have terrible insurance,” she said with a laugh, aware of that irony.
If You Are Struggling, Don’t Be Ashamed
Some physicians who’ve experienced EDs firsthand are working to improve training on diagnosing and treating the conditions. Dr. McNaught has developed and launched a new eLearning program for healthcare workers on how to recognize the early signs and symptoms of an ED and provide support.
“It’s not only so they can recognize it in their patients but also if colleagues and family and friends are struggling,” she said.
In 2021, the American Psychiatric Association (APA) approved the APA Practice Guideline for the Treatment of Patients With Eating Disorders, which aims to improve patient care and treatment outcomes.
But Dr. Klein is concerned that increased stress since the COVID-19 pandemic may be putting healthcare workers at even greater risk.
“When people are under stress or when they feel like there are things in their life that maybe they can’t control, sometimes turning to an eating disorder is a way to cope,” she said, “In that sense, the stress on medical professionals is something that could lead to eating disorder behaviors.”
Dr. Klein’s message to healthcare workers: Don’t be ashamed. She described an ED as “a monster that takes over your brain. Once it starts, it’s very hard to turn it around on your own. So, I hope anyone who is suffering, in whatever field they’re in, that they are able to ask for help.”
A version of this article appeared on Medscape.com.
Nodal Radiation May Make BC Axillary Dissection Unnecessary
SAN ANTONIO — Axillary lymph node dissection may be unnecessary if breast cancer patients with one or two positive sentinel lymph nodes plan to have adjuvant nodal radiation, according to a major Scandinavian trial presented at the San Antonio Breast Cancer Symposium.
“It means that you don’t need to dissect the axilla if you” are going to “radiate the axilla.” “For the U.S., that’s the conclusion because there are still centers that do both, and that’s out,” lead investigator Jana de Boniface, MD, PhD, a breast cancer surgeon at the Karolinska Institutet, Stockholm, said in an interview.
Some even wondered if 5 years of endocrine therapy is necessary.
Dr. Boniface shared her thoughts after presenting the Scandinavian trial, SENOMAC, which she led.
SENOMAC randomized 1,204 patients with one or two positive sentinel lymph nodes to axillary dissection; 1,335 with the same finding were randomized to no dissection.
Subjects had clinically T1-3, N0 primary breast cancer. About 89% in both arms went on to adjuvant radiation, including nodal radiation, and almost all also went on to systemic therapy, which included endocrine therapy in over 90%. Only about 2% of subjects had neoadjuvant therapy.
At a median follow-up of nearly 4 years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection arm and 7.1% in the no-dissection group having recurrences. Estimated 5-year recurrence-free survival was just shy of 90% in both groups. Skipping dissection was strongly non-inferior to having one (P < .001).
SENOMAC “clearly shows that you don’t need to dissect the axilla if you have one to two positive sentinel lymph nodes” so long as patients have adjuvant nodal radiation. Recurrence-free survival “curves practically overlap, and we cannot see any difference between the two groups,” Dr. Boniface said.
Meanwhile, the dissection group fared worse on patient reported outcomes. Overall survival outcomes, the primary endpoint of the trial, are expected within 2 years.
The goal of the trial, the largest to date to look into the issue, was to fill gaps in the literature. Similar outcomes were reported around a decade ago in patients with low sentinel lymph node burdens, but the extensive exclusion criteria raised questions about general applicability.
In contrast, SENOMAC was widely inclusive. Over a third of patients had mastectomies, over a third had sentinel lymph node extracapsular extension, almost 6% had T3 disease, almost 20% had lobular carcinoma, 40% were 65 years or older, and tumors were as large as 15.5 cm.
The findings held regardless of those and other factors on subgroup analyses, including estrogen receptor and HER2 status and the number of additional positive nodes retrieved in the dissection group.
Andrea V. Barrio, MD, the study discussant and a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York, agreed with the message from SENOMAC.
“Based on this, ALND [axillary lymph node dissection] should not be considered standard in patients with clinical T1-3, N0 breast cancer with one to two positive sentinel nodes, with or without microscopic extracapsular extension, undergoing lumpectomy or mastectomy,” provided nodal adjuvant radiotherapy is indicated, she said.
Although adjuvant nodal radiation for patients with one to three positive sentinel nodes is standard of care in Denmark and Sweden, where most of the patients in SENOMAC were located, practices vary widely in the United States. If adjuvant radiation isn’t used, “then ALND [is still] indicated,” Dr. Barrio said, but in either case, “only one is needed.”
In keeping with the de-escalation theme at the 2023 symposium, both Dr. Boniface and Dr. Barrio noted that trials are now underway to find patients who can avoid any axillary treatment at all if they have just one or two positive sentinel lymph nodes.
Preoperative axillary ultrasound was mandatory in SENOMAC and patients with non-palpable suspicious axillary lymph nodes were enrolled.
Thirty-six were positive on fine needle aspiration and randomized into the study, but when asked, Dr. Boniface didn’t have the data immediately at hand on how they fared.
The work was funded by the Swedish Research Council, Nordic Cancer Union, and others. Dr. Boniface and Dr. Barrio didn’t have any disclosures.
SAN ANTONIO — Axillary lymph node dissection may be unnecessary if breast cancer patients with one or two positive sentinel lymph nodes plan to have adjuvant nodal radiation, according to a major Scandinavian trial presented at the San Antonio Breast Cancer Symposium.
“It means that you don’t need to dissect the axilla if you” are going to “radiate the axilla.” “For the U.S., that’s the conclusion because there are still centers that do both, and that’s out,” lead investigator Jana de Boniface, MD, PhD, a breast cancer surgeon at the Karolinska Institutet, Stockholm, said in an interview.
Some even wondered if 5 years of endocrine therapy is necessary.
Dr. Boniface shared her thoughts after presenting the Scandinavian trial, SENOMAC, which she led.
SENOMAC randomized 1,204 patients with one or two positive sentinel lymph nodes to axillary dissection; 1,335 with the same finding were randomized to no dissection.
Subjects had clinically T1-3, N0 primary breast cancer. About 89% in both arms went on to adjuvant radiation, including nodal radiation, and almost all also went on to systemic therapy, which included endocrine therapy in over 90%. Only about 2% of subjects had neoadjuvant therapy.
At a median follow-up of nearly 4 years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection arm and 7.1% in the no-dissection group having recurrences. Estimated 5-year recurrence-free survival was just shy of 90% in both groups. Skipping dissection was strongly non-inferior to having one (P < .001).
SENOMAC “clearly shows that you don’t need to dissect the axilla if you have one to two positive sentinel lymph nodes” so long as patients have adjuvant nodal radiation. Recurrence-free survival “curves practically overlap, and we cannot see any difference between the two groups,” Dr. Boniface said.
Meanwhile, the dissection group fared worse on patient reported outcomes. Overall survival outcomes, the primary endpoint of the trial, are expected within 2 years.
The goal of the trial, the largest to date to look into the issue, was to fill gaps in the literature. Similar outcomes were reported around a decade ago in patients with low sentinel lymph node burdens, but the extensive exclusion criteria raised questions about general applicability.
In contrast, SENOMAC was widely inclusive. Over a third of patients had mastectomies, over a third had sentinel lymph node extracapsular extension, almost 6% had T3 disease, almost 20% had lobular carcinoma, 40% were 65 years or older, and tumors were as large as 15.5 cm.
The findings held regardless of those and other factors on subgroup analyses, including estrogen receptor and HER2 status and the number of additional positive nodes retrieved in the dissection group.
Andrea V. Barrio, MD, the study discussant and a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York, agreed with the message from SENOMAC.
“Based on this, ALND [axillary lymph node dissection] should not be considered standard in patients with clinical T1-3, N0 breast cancer with one to two positive sentinel nodes, with or without microscopic extracapsular extension, undergoing lumpectomy or mastectomy,” provided nodal adjuvant radiotherapy is indicated, she said.
Although adjuvant nodal radiation for patients with one to three positive sentinel nodes is standard of care in Denmark and Sweden, where most of the patients in SENOMAC were located, practices vary widely in the United States. If adjuvant radiation isn’t used, “then ALND [is still] indicated,” Dr. Barrio said, but in either case, “only one is needed.”
In keeping with the de-escalation theme at the 2023 symposium, both Dr. Boniface and Dr. Barrio noted that trials are now underway to find patients who can avoid any axillary treatment at all if they have just one or two positive sentinel lymph nodes.
Preoperative axillary ultrasound was mandatory in SENOMAC and patients with non-palpable suspicious axillary lymph nodes were enrolled.
Thirty-six were positive on fine needle aspiration and randomized into the study, but when asked, Dr. Boniface didn’t have the data immediately at hand on how they fared.
The work was funded by the Swedish Research Council, Nordic Cancer Union, and others. Dr. Boniface and Dr. Barrio didn’t have any disclosures.
SAN ANTONIO — Axillary lymph node dissection may be unnecessary if breast cancer patients with one or two positive sentinel lymph nodes plan to have adjuvant nodal radiation, according to a major Scandinavian trial presented at the San Antonio Breast Cancer Symposium.
“It means that you don’t need to dissect the axilla if you” are going to “radiate the axilla.” “For the U.S., that’s the conclusion because there are still centers that do both, and that’s out,” lead investigator Jana de Boniface, MD, PhD, a breast cancer surgeon at the Karolinska Institutet, Stockholm, said in an interview.
Some even wondered if 5 years of endocrine therapy is necessary.
Dr. Boniface shared her thoughts after presenting the Scandinavian trial, SENOMAC, which she led.
SENOMAC randomized 1,204 patients with one or two positive sentinel lymph nodes to axillary dissection; 1,335 with the same finding were randomized to no dissection.
Subjects had clinically T1-3, N0 primary breast cancer. About 89% in both arms went on to adjuvant radiation, including nodal radiation, and almost all also went on to systemic therapy, which included endocrine therapy in over 90%. Only about 2% of subjects had neoadjuvant therapy.
At a median follow-up of nearly 4 years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection arm and 7.1% in the no-dissection group having recurrences. Estimated 5-year recurrence-free survival was just shy of 90% in both groups. Skipping dissection was strongly non-inferior to having one (P < .001).
SENOMAC “clearly shows that you don’t need to dissect the axilla if you have one to two positive sentinel lymph nodes” so long as patients have adjuvant nodal radiation. Recurrence-free survival “curves practically overlap, and we cannot see any difference between the two groups,” Dr. Boniface said.
Meanwhile, the dissection group fared worse on patient reported outcomes. Overall survival outcomes, the primary endpoint of the trial, are expected within 2 years.
The goal of the trial, the largest to date to look into the issue, was to fill gaps in the literature. Similar outcomes were reported around a decade ago in patients with low sentinel lymph node burdens, but the extensive exclusion criteria raised questions about general applicability.
In contrast, SENOMAC was widely inclusive. Over a third of patients had mastectomies, over a third had sentinel lymph node extracapsular extension, almost 6% had T3 disease, almost 20% had lobular carcinoma, 40% were 65 years or older, and tumors were as large as 15.5 cm.
The findings held regardless of those and other factors on subgroup analyses, including estrogen receptor and HER2 status and the number of additional positive nodes retrieved in the dissection group.
Andrea V. Barrio, MD, the study discussant and a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York, agreed with the message from SENOMAC.
“Based on this, ALND [axillary lymph node dissection] should not be considered standard in patients with clinical T1-3, N0 breast cancer with one to two positive sentinel nodes, with or without microscopic extracapsular extension, undergoing lumpectomy or mastectomy,” provided nodal adjuvant radiotherapy is indicated, she said.
Although adjuvant nodal radiation for patients with one to three positive sentinel nodes is standard of care in Denmark and Sweden, where most of the patients in SENOMAC were located, practices vary widely in the United States. If adjuvant radiation isn’t used, “then ALND [is still] indicated,” Dr. Barrio said, but in either case, “only one is needed.”
In keeping with the de-escalation theme at the 2023 symposium, both Dr. Boniface and Dr. Barrio noted that trials are now underway to find patients who can avoid any axillary treatment at all if they have just one or two positive sentinel lymph nodes.
Preoperative axillary ultrasound was mandatory in SENOMAC and patients with non-palpable suspicious axillary lymph nodes were enrolled.
Thirty-six were positive on fine needle aspiration and randomized into the study, but when asked, Dr. Boniface didn’t have the data immediately at hand on how they fared.
The work was funded by the Swedish Research Council, Nordic Cancer Union, and others. Dr. Boniface and Dr. Barrio didn’t have any disclosures.
FROM SABCS 2023
Male Surgeons Linked With Higher Subsequent Healthcare Costs
, data suggested.
A retrospective, population-based cohort study that included more than 1 million adults undergoing any of 25 common surgical procedures found that total healthcare costs assessed at 1 year following surgery were more than $6000 higher when the surgery was performed by a male surgeon. Costs were also higher at 30 and 90 days for patients treated by male surgeons.
“As a male surgeon, I think our results should cause me and my colleagues to pause and consider why this may be,” said lead author Christopher J. D. Wallis, MD, PhD, assistant professor of surgery at the University of Toronto.
“None of us believe that the presence of a Y chromosome in surgeons means there are worse outcomes, it’s just that generally speaking, men and women, as we have known for decades, practice medicine a little differently. Things like communication style, time they spend with their patients, and even things like guideline adherence are different, and understanding how those differences translate into patient outcomes is the goal of this whole body of work,” said Wallis.
The study was published online November 29 in JAMA Surgery.
Explanation Is Elusive
In earlier work, Dr. Wallis and his team reported that patients treated by female surgeons had a small but statistically significant decrease in 30-day mortality, were less likely to be readmitted to the hospital, and had fewer complications than those treated by male surgeons. In another study, they found worse outcomes among female patients treated by male surgeons.
In the current study, the researchers examined the association between surgeon sex and healthcare costs among patients undergoing various surgical procedures, including coronary artery bypass grafting, appendectomy, hysterectomy, anterior spinal decompression, and knee replacement. They included all adult patients who underwent these procedures at hospitals in Ontario, Canada, between January 2007 and December 2019 in their analysis.
The study sample included 1,165,711 patients. Of this group, 151,054 patients were treated by a female surgeon, and 1,014,657 were treated by a male surgeon.
After adjusting for patient-, surgeon-, anesthesiologist-, and hospital-related factors, they found that 1-year total healthcare costs were $24,882 for patients treated by male surgeons vs $18,517 for patients treated by female surgeons. Healthcare costs were also higher at 30 days (adjusted absolute difference, $3115) and at 90 days (adjusted absolute difference, $4228).
“This translates into a 9%-10% higher risk of costs with male surgeons compared with women surgeons at these time points,” said Dr. Wallis.
“This study cannot provide a specific answer as to why these differences are occurring,” Dr. Wallis said.
“We are currently undertaking more research to better understand the reasons. Our previous studies have shown that patients treated by male physicians have higher rates of death, readmission, and complications. Managing these adverse postoperative events is costly and likely contributes to these differences. Given the size of our study and similar training pathways, we do not think there are technical differences between male and female surgeons. Rather, we are hypothesizing that there may be differences in how physicians practice, make decisions, and consult with patients,” he said.
Ultimately, Dr. Wallis said he would like his research to prompt “a moment of introspection” among his surgical colleagues.
“Hopefully, these data will provide the impetus for further efforts to make surgery, and medicine in general, a field that is welcoming to women,” he said.
Potential Confounding Factors
This study expands the evidence suggesting significant practice differences between male and female surgeons, Ursula Adams, MD, a resident; Caprice C. Greenberg, MD, MPH, chair; and Jared Gallaher, MD, MPH, adjunct assistant professor, all from the Department of Surgery at the University of North Carolina in Chapel Hill, wrote in an accompanying editorial.
They cautioned, however, that “there are many potential confounding factors and possible explanatory mechanisms associated with surgeon sex that make it challenging to untangle influences on costs. Sex may be an easily captured data point, but is understanding the mechanism by which it affects cost the right next step? Surgeons control how and where they practice; they do not have control over their own demographics.”
The editorialists added that while recruiting and retaining women in surgery is important, it is not a solution to controlling costs.
“We must provide surgeons with better data to understand how practice approach and decisions affect cost and support for practice improvement. Only with these insights will we ensure patients of male surgeons receive care that is just as cost-effective as that provided by female surgeons, while also helping to bend the cost curve and improve the quality of surgical care,” they concluded.
‘Admirable’ Data Use
Commenting on the findings, Oluwadamilola “Lola” Fayanju, MD, chief of breast surgery at Penn Medicine in Philadelphia, said, “It is interesting that the study was performed in Canada with its different healthcare system.” Dr. Fayanju did not participate in the study.
“They used administrative data from a national database, and it is admirable that they were able to do that. These data allow us to make large-scale geographical assessments, although they are subject to errors and unmeasured confounders,” said Dr. Fayanju.
Women surgeons may do things that result in better outcomes, she suggested. “In this study, the women were younger and so perhaps were more up to date. They might have optimized management of their patients in the pre-op phase, including better patient selection, which led to better costs. Or in the post-op phase, they might have made themselves readily accessible. For instance, I remove all barriers about getting in touch with me, and I tell my students to make sure the patient can reach you easily,” said Dr. Fayanju.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care, and the Data Sciences Institute at the University of Toronto. Dr. Wallis, Dr. Adams, Dr. Greenberg, Dr. Gallaher, and Dr. Fayanju reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
, data suggested.
A retrospective, population-based cohort study that included more than 1 million adults undergoing any of 25 common surgical procedures found that total healthcare costs assessed at 1 year following surgery were more than $6000 higher when the surgery was performed by a male surgeon. Costs were also higher at 30 and 90 days for patients treated by male surgeons.
“As a male surgeon, I think our results should cause me and my colleagues to pause and consider why this may be,” said lead author Christopher J. D. Wallis, MD, PhD, assistant professor of surgery at the University of Toronto.
“None of us believe that the presence of a Y chromosome in surgeons means there are worse outcomes, it’s just that generally speaking, men and women, as we have known for decades, practice medicine a little differently. Things like communication style, time they spend with their patients, and even things like guideline adherence are different, and understanding how those differences translate into patient outcomes is the goal of this whole body of work,” said Wallis.
The study was published online November 29 in JAMA Surgery.
Explanation Is Elusive
In earlier work, Dr. Wallis and his team reported that patients treated by female surgeons had a small but statistically significant decrease in 30-day mortality, were less likely to be readmitted to the hospital, and had fewer complications than those treated by male surgeons. In another study, they found worse outcomes among female patients treated by male surgeons.
In the current study, the researchers examined the association between surgeon sex and healthcare costs among patients undergoing various surgical procedures, including coronary artery bypass grafting, appendectomy, hysterectomy, anterior spinal decompression, and knee replacement. They included all adult patients who underwent these procedures at hospitals in Ontario, Canada, between January 2007 and December 2019 in their analysis.
The study sample included 1,165,711 patients. Of this group, 151,054 patients were treated by a female surgeon, and 1,014,657 were treated by a male surgeon.
After adjusting for patient-, surgeon-, anesthesiologist-, and hospital-related factors, they found that 1-year total healthcare costs were $24,882 for patients treated by male surgeons vs $18,517 for patients treated by female surgeons. Healthcare costs were also higher at 30 days (adjusted absolute difference, $3115) and at 90 days (adjusted absolute difference, $4228).
“This translates into a 9%-10% higher risk of costs with male surgeons compared with women surgeons at these time points,” said Dr. Wallis.
“This study cannot provide a specific answer as to why these differences are occurring,” Dr. Wallis said.
“We are currently undertaking more research to better understand the reasons. Our previous studies have shown that patients treated by male physicians have higher rates of death, readmission, and complications. Managing these adverse postoperative events is costly and likely contributes to these differences. Given the size of our study and similar training pathways, we do not think there are technical differences between male and female surgeons. Rather, we are hypothesizing that there may be differences in how physicians practice, make decisions, and consult with patients,” he said.
Ultimately, Dr. Wallis said he would like his research to prompt “a moment of introspection” among his surgical colleagues.
“Hopefully, these data will provide the impetus for further efforts to make surgery, and medicine in general, a field that is welcoming to women,” he said.
Potential Confounding Factors
This study expands the evidence suggesting significant practice differences between male and female surgeons, Ursula Adams, MD, a resident; Caprice C. Greenberg, MD, MPH, chair; and Jared Gallaher, MD, MPH, adjunct assistant professor, all from the Department of Surgery at the University of North Carolina in Chapel Hill, wrote in an accompanying editorial.
They cautioned, however, that “there are many potential confounding factors and possible explanatory mechanisms associated with surgeon sex that make it challenging to untangle influences on costs. Sex may be an easily captured data point, but is understanding the mechanism by which it affects cost the right next step? Surgeons control how and where they practice; they do not have control over their own demographics.”
The editorialists added that while recruiting and retaining women in surgery is important, it is not a solution to controlling costs.
“We must provide surgeons with better data to understand how practice approach and decisions affect cost and support for practice improvement. Only with these insights will we ensure patients of male surgeons receive care that is just as cost-effective as that provided by female surgeons, while also helping to bend the cost curve and improve the quality of surgical care,” they concluded.
‘Admirable’ Data Use
Commenting on the findings, Oluwadamilola “Lola” Fayanju, MD, chief of breast surgery at Penn Medicine in Philadelphia, said, “It is interesting that the study was performed in Canada with its different healthcare system.” Dr. Fayanju did not participate in the study.
“They used administrative data from a national database, and it is admirable that they were able to do that. These data allow us to make large-scale geographical assessments, although they are subject to errors and unmeasured confounders,” said Dr. Fayanju.
Women surgeons may do things that result in better outcomes, she suggested. “In this study, the women were younger and so perhaps were more up to date. They might have optimized management of their patients in the pre-op phase, including better patient selection, which led to better costs. Or in the post-op phase, they might have made themselves readily accessible. For instance, I remove all barriers about getting in touch with me, and I tell my students to make sure the patient can reach you easily,” said Dr. Fayanju.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care, and the Data Sciences Institute at the University of Toronto. Dr. Wallis, Dr. Adams, Dr. Greenberg, Dr. Gallaher, and Dr. Fayanju reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
, data suggested.
A retrospective, population-based cohort study that included more than 1 million adults undergoing any of 25 common surgical procedures found that total healthcare costs assessed at 1 year following surgery were more than $6000 higher when the surgery was performed by a male surgeon. Costs were also higher at 30 and 90 days for patients treated by male surgeons.
“As a male surgeon, I think our results should cause me and my colleagues to pause and consider why this may be,” said lead author Christopher J. D. Wallis, MD, PhD, assistant professor of surgery at the University of Toronto.
“None of us believe that the presence of a Y chromosome in surgeons means there are worse outcomes, it’s just that generally speaking, men and women, as we have known for decades, practice medicine a little differently. Things like communication style, time they spend with their patients, and even things like guideline adherence are different, and understanding how those differences translate into patient outcomes is the goal of this whole body of work,” said Wallis.
The study was published online November 29 in JAMA Surgery.
Explanation Is Elusive
In earlier work, Dr. Wallis and his team reported that patients treated by female surgeons had a small but statistically significant decrease in 30-day mortality, were less likely to be readmitted to the hospital, and had fewer complications than those treated by male surgeons. In another study, they found worse outcomes among female patients treated by male surgeons.
In the current study, the researchers examined the association between surgeon sex and healthcare costs among patients undergoing various surgical procedures, including coronary artery bypass grafting, appendectomy, hysterectomy, anterior spinal decompression, and knee replacement. They included all adult patients who underwent these procedures at hospitals in Ontario, Canada, between January 2007 and December 2019 in their analysis.
The study sample included 1,165,711 patients. Of this group, 151,054 patients were treated by a female surgeon, and 1,014,657 were treated by a male surgeon.
After adjusting for patient-, surgeon-, anesthesiologist-, and hospital-related factors, they found that 1-year total healthcare costs were $24,882 for patients treated by male surgeons vs $18,517 for patients treated by female surgeons. Healthcare costs were also higher at 30 days (adjusted absolute difference, $3115) and at 90 days (adjusted absolute difference, $4228).
“This translates into a 9%-10% higher risk of costs with male surgeons compared with women surgeons at these time points,” said Dr. Wallis.
“This study cannot provide a specific answer as to why these differences are occurring,” Dr. Wallis said.
“We are currently undertaking more research to better understand the reasons. Our previous studies have shown that patients treated by male physicians have higher rates of death, readmission, and complications. Managing these adverse postoperative events is costly and likely contributes to these differences. Given the size of our study and similar training pathways, we do not think there are technical differences between male and female surgeons. Rather, we are hypothesizing that there may be differences in how physicians practice, make decisions, and consult with patients,” he said.
Ultimately, Dr. Wallis said he would like his research to prompt “a moment of introspection” among his surgical colleagues.
“Hopefully, these data will provide the impetus for further efforts to make surgery, and medicine in general, a field that is welcoming to women,” he said.
Potential Confounding Factors
This study expands the evidence suggesting significant practice differences between male and female surgeons, Ursula Adams, MD, a resident; Caprice C. Greenberg, MD, MPH, chair; and Jared Gallaher, MD, MPH, adjunct assistant professor, all from the Department of Surgery at the University of North Carolina in Chapel Hill, wrote in an accompanying editorial.
They cautioned, however, that “there are many potential confounding factors and possible explanatory mechanisms associated with surgeon sex that make it challenging to untangle influences on costs. Sex may be an easily captured data point, but is understanding the mechanism by which it affects cost the right next step? Surgeons control how and where they practice; they do not have control over their own demographics.”
The editorialists added that while recruiting and retaining women in surgery is important, it is not a solution to controlling costs.
“We must provide surgeons with better data to understand how practice approach and decisions affect cost and support for practice improvement. Only with these insights will we ensure patients of male surgeons receive care that is just as cost-effective as that provided by female surgeons, while also helping to bend the cost curve and improve the quality of surgical care,” they concluded.
‘Admirable’ Data Use
Commenting on the findings, Oluwadamilola “Lola” Fayanju, MD, chief of breast surgery at Penn Medicine in Philadelphia, said, “It is interesting that the study was performed in Canada with its different healthcare system.” Dr. Fayanju did not participate in the study.
“They used administrative data from a national database, and it is admirable that they were able to do that. These data allow us to make large-scale geographical assessments, although they are subject to errors and unmeasured confounders,” said Dr. Fayanju.
Women surgeons may do things that result in better outcomes, she suggested. “In this study, the women were younger and so perhaps were more up to date. They might have optimized management of their patients in the pre-op phase, including better patient selection, which led to better costs. Or in the post-op phase, they might have made themselves readily accessible. For instance, I remove all barriers about getting in touch with me, and I tell my students to make sure the patient can reach you easily,” said Dr. Fayanju.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care, and the Data Sciences Institute at the University of Toronto. Dr. Wallis, Dr. Adams, Dr. Greenberg, Dr. Gallaher, and Dr. Fayanju reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
AGA Tech Summit: Bridging the Gap Between Innovation, Industry, and Gastroenterologists
Medicine is transforming at a remarkable pace. It is therefore imperative for the future of the field that physicians understand innovation and collaborate with industry partners. Innovation can be defined as invention, adoption, and diffusion.1 During my training in gastroenterology and advanced fellowships, I learned about multiple endoscopic tools and techniques and became familiar with industry names that I frequently encountered in the endoscopy unit or clinic.
I was nominated to attend the AGA Tech Summit Fellows Program by my advanced endoscopy fellowship program director. A total of 22 fellows from around the United States at various stages of their training and interests in the field of gastroenterology and hepatology were selected for the program through an application process. The program included registration, travel, and accommodations to attend the AGA Tech Summit and Fellows Immersion Day at Medtronic.
The first event in the program was a visit to the Medtronic Santa Clara office, where our initial stop was at the research and development lab. We were introduced to design and biomedical engineers who reviewed with us the extensive testing that devices and endoscopy equipment undergo before coming to the market. These labs have a heavy focus on prototyping and experimentation and exist to promote in-house innovation and inventions.

During the day, we met physicians who shared their journeys on how they developed and advanced their careers in partnership with industry. Our visit also included a session with the business development and strategy manager at Medtronic, who discussed strategy and steps involved in product development — from the inception of an idea, institutional policies, and patents, to industry collaboration, and finally to successful commercialization. During medical school and training, we are focused on appropriately learning and applying medical knowledge to clinical care. The Medtronic Fellows Immersion Day experience offered a different perspective and showed other ways by which clinical knowledge and experience can be used to make an impact, in collaboration with industry and stakeholders. It also highlighted alternative career paths for medical professionals. The evening concluded with a meet and greet with the AGA Center for GI Innovation & Technology (CGIT) members and leadership.
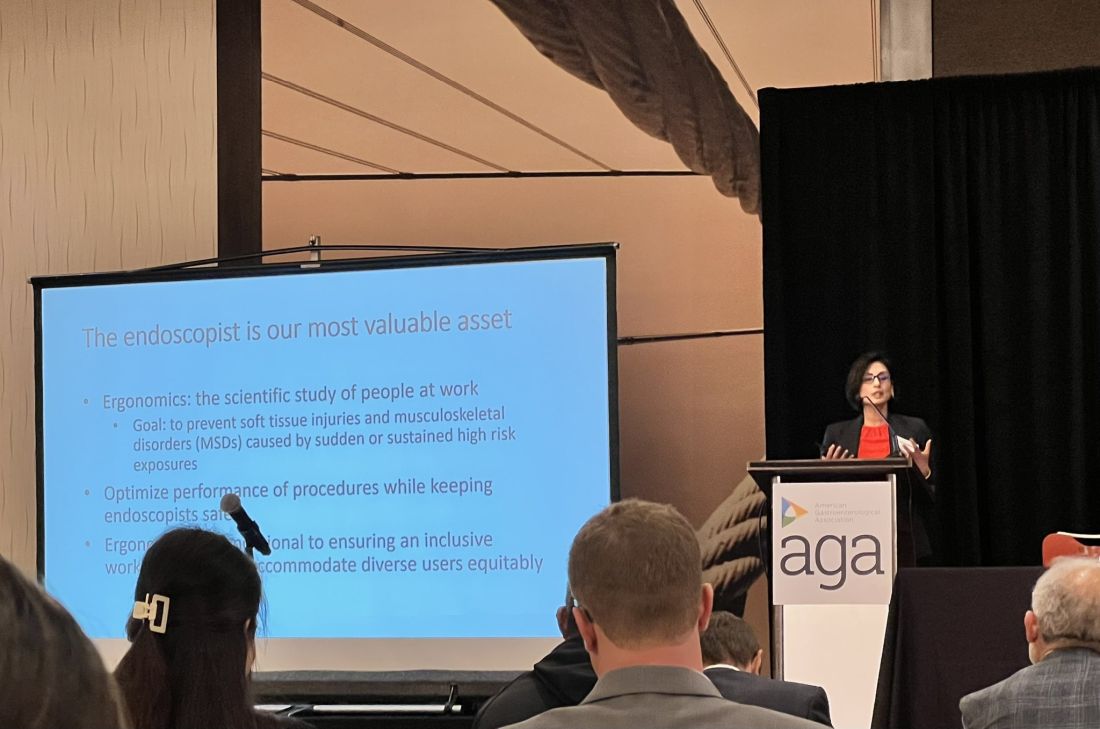
The AGA Tech Summit was unlike any conference I have been to in my 13 years of training in medicine (which included mostly clinically focused scientific meetings). Sessions involved ergonomics, applications of artificial intelligence, advances in imaging, environmental endoscopy, the role of the FDA, and innovations around the world. The audience included but was not limited to industry executives, AGA CGIT leadership, physician innovators, gastroenterologists, venture capitalists, and others. Attendees represented the diversity of our field in terms of organizational structures and backgrounds. This resulted in an opportunity to hear and learn different perspectives about products, emerging technology, and the costs involved for physicians, industry, and patients.
The final session of the summit, the AGA Shark Tank, was perhaps the most intriguing one of all. The session showcased landscape-changing technology to AGA investors and venture capitalists. The participants presented their own pitches and faced the sharks (judges). The winner received additional funding, tailored guidance from the AGA CGIT committee, partnering opportunities with interested parties, and the opportunity to represent AGA Shark Tank at the Digestive Disease Week (DDW).
The AGA Tech Summit Fellows Program is a learning platform that not only helps you find your niche in the world of GI innovation but also equips you with resources and connections to make an impact. It is also a great way to infuse new ideas into your practice or research. As healthcare professionals, we must create a culture where innovation can flourish, and where staff and patients feel empowered to contribute to the innovation process and help make change happen — to me, the AGA Tech Summit is one such avenue.
Reference
1. Kelly CJ and Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017 Jun. doi: 10.7861/futurehosp.4-2-121.
Dr. Umar is Assistant Professor of Medicine, Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, Texas, and a staff physician at Michael E. DeBakey VA Medical Center, Houston. Dr. Umar has no relevant financial conflicts and is on X, formerly Twitter, @shifaumarMD.
Medicine is transforming at a remarkable pace. It is therefore imperative for the future of the field that physicians understand innovation and collaborate with industry partners. Innovation can be defined as invention, adoption, and diffusion.1 During my training in gastroenterology and advanced fellowships, I learned about multiple endoscopic tools and techniques and became familiar with industry names that I frequently encountered in the endoscopy unit or clinic.
I was nominated to attend the AGA Tech Summit Fellows Program by my advanced endoscopy fellowship program director. A total of 22 fellows from around the United States at various stages of their training and interests in the field of gastroenterology and hepatology were selected for the program through an application process. The program included registration, travel, and accommodations to attend the AGA Tech Summit and Fellows Immersion Day at Medtronic.
The first event in the program was a visit to the Medtronic Santa Clara office, where our initial stop was at the research and development lab. We were introduced to design and biomedical engineers who reviewed with us the extensive testing that devices and endoscopy equipment undergo before coming to the market. These labs have a heavy focus on prototyping and experimentation and exist to promote in-house innovation and inventions.

During the day, we met physicians who shared their journeys on how they developed and advanced their careers in partnership with industry. Our visit also included a session with the business development and strategy manager at Medtronic, who discussed strategy and steps involved in product development — from the inception of an idea, institutional policies, and patents, to industry collaboration, and finally to successful commercialization. During medical school and training, we are focused on appropriately learning and applying medical knowledge to clinical care. The Medtronic Fellows Immersion Day experience offered a different perspective and showed other ways by which clinical knowledge and experience can be used to make an impact, in collaboration with industry and stakeholders. It also highlighted alternative career paths for medical professionals. The evening concluded with a meet and greet with the AGA Center for GI Innovation & Technology (CGIT) members and leadership.
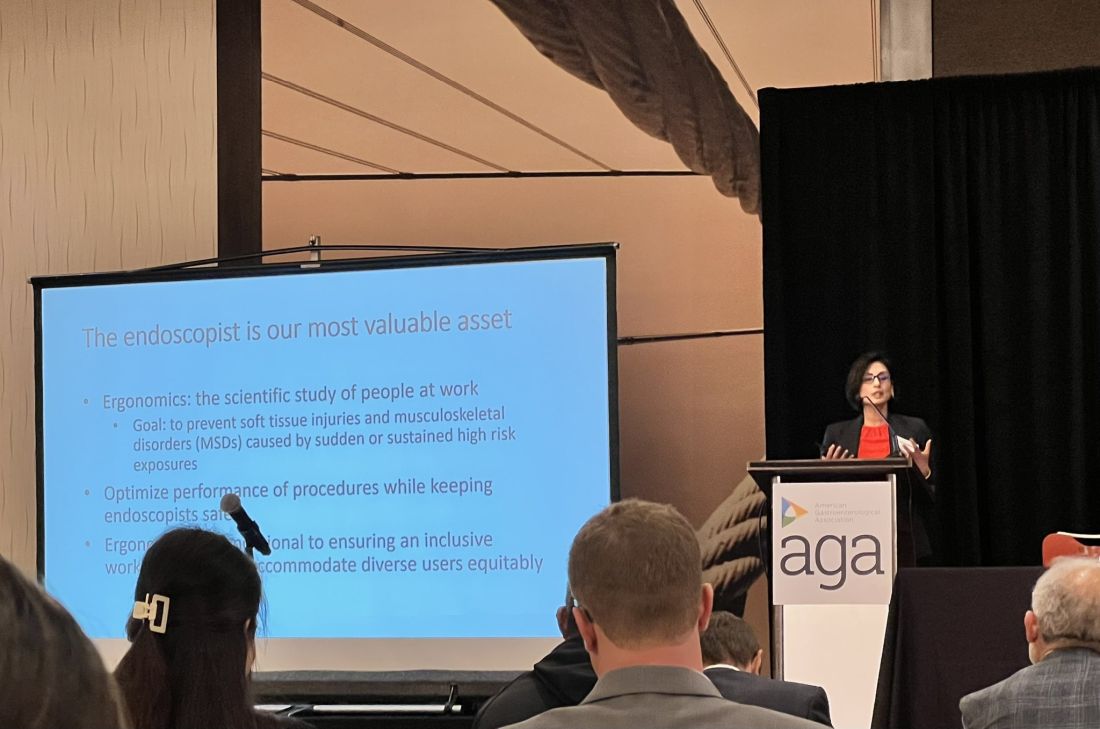
The AGA Tech Summit was unlike any conference I have been to in my 13 years of training in medicine (which included mostly clinically focused scientific meetings). Sessions involved ergonomics, applications of artificial intelligence, advances in imaging, environmental endoscopy, the role of the FDA, and innovations around the world. The audience included but was not limited to industry executives, AGA CGIT leadership, physician innovators, gastroenterologists, venture capitalists, and others. Attendees represented the diversity of our field in terms of organizational structures and backgrounds. This resulted in an opportunity to hear and learn different perspectives about products, emerging technology, and the costs involved for physicians, industry, and patients.
The final session of the summit, the AGA Shark Tank, was perhaps the most intriguing one of all. The session showcased landscape-changing technology to AGA investors and venture capitalists. The participants presented their own pitches and faced the sharks (judges). The winner received additional funding, tailored guidance from the AGA CGIT committee, partnering opportunities with interested parties, and the opportunity to represent AGA Shark Tank at the Digestive Disease Week (DDW).
The AGA Tech Summit Fellows Program is a learning platform that not only helps you find your niche in the world of GI innovation but also equips you with resources and connections to make an impact. It is also a great way to infuse new ideas into your practice or research. As healthcare professionals, we must create a culture where innovation can flourish, and where staff and patients feel empowered to contribute to the innovation process and help make change happen — to me, the AGA Tech Summit is one such avenue.
Reference
1. Kelly CJ and Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017 Jun. doi: 10.7861/futurehosp.4-2-121.
Dr. Umar is Assistant Professor of Medicine, Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, Texas, and a staff physician at Michael E. DeBakey VA Medical Center, Houston. Dr. Umar has no relevant financial conflicts and is on X, formerly Twitter, @shifaumarMD.
Medicine is transforming at a remarkable pace. It is therefore imperative for the future of the field that physicians understand innovation and collaborate with industry partners. Innovation can be defined as invention, adoption, and diffusion.1 During my training in gastroenterology and advanced fellowships, I learned about multiple endoscopic tools and techniques and became familiar with industry names that I frequently encountered in the endoscopy unit or clinic.
I was nominated to attend the AGA Tech Summit Fellows Program by my advanced endoscopy fellowship program director. A total of 22 fellows from around the United States at various stages of their training and interests in the field of gastroenterology and hepatology were selected for the program through an application process. The program included registration, travel, and accommodations to attend the AGA Tech Summit and Fellows Immersion Day at Medtronic.
The first event in the program was a visit to the Medtronic Santa Clara office, where our initial stop was at the research and development lab. We were introduced to design and biomedical engineers who reviewed with us the extensive testing that devices and endoscopy equipment undergo before coming to the market. These labs have a heavy focus on prototyping and experimentation and exist to promote in-house innovation and inventions.

During the day, we met physicians who shared their journeys on how they developed and advanced their careers in partnership with industry. Our visit also included a session with the business development and strategy manager at Medtronic, who discussed strategy and steps involved in product development — from the inception of an idea, institutional policies, and patents, to industry collaboration, and finally to successful commercialization. During medical school and training, we are focused on appropriately learning and applying medical knowledge to clinical care. The Medtronic Fellows Immersion Day experience offered a different perspective and showed other ways by which clinical knowledge and experience can be used to make an impact, in collaboration with industry and stakeholders. It also highlighted alternative career paths for medical professionals. The evening concluded with a meet and greet with the AGA Center for GI Innovation & Technology (CGIT) members and leadership.
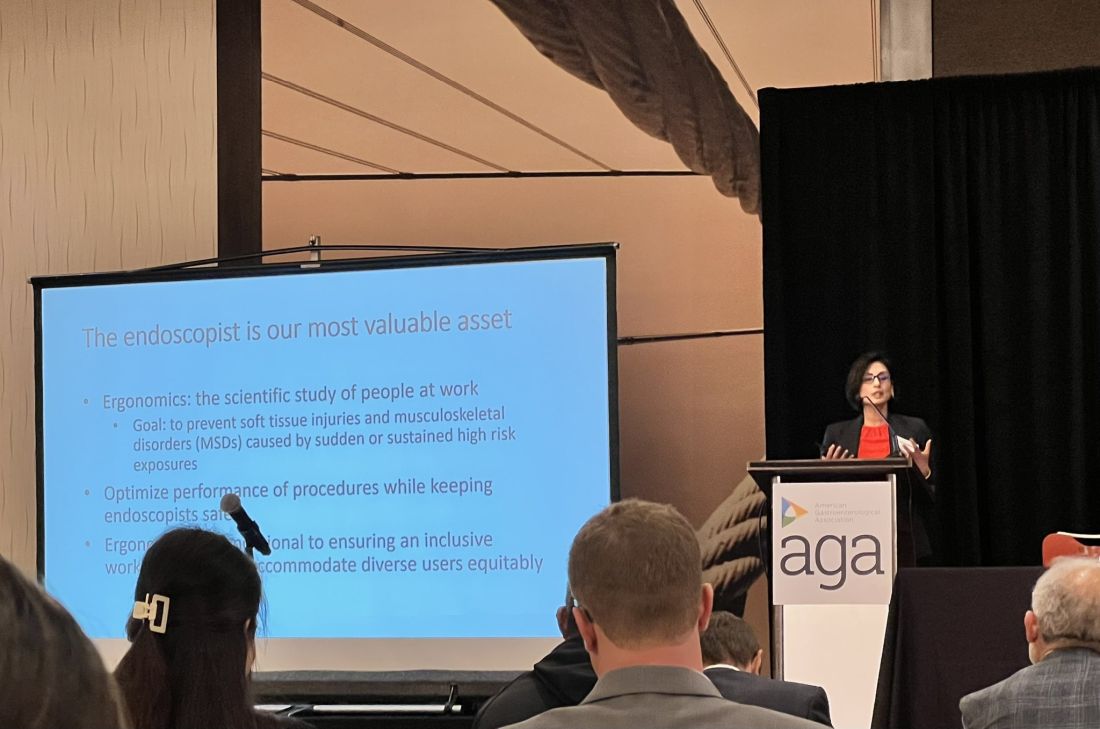
The AGA Tech Summit was unlike any conference I have been to in my 13 years of training in medicine (which included mostly clinically focused scientific meetings). Sessions involved ergonomics, applications of artificial intelligence, advances in imaging, environmental endoscopy, the role of the FDA, and innovations around the world. The audience included but was not limited to industry executives, AGA CGIT leadership, physician innovators, gastroenterologists, venture capitalists, and others. Attendees represented the diversity of our field in terms of organizational structures and backgrounds. This resulted in an opportunity to hear and learn different perspectives about products, emerging technology, and the costs involved for physicians, industry, and patients.
The final session of the summit, the AGA Shark Tank, was perhaps the most intriguing one of all. The session showcased landscape-changing technology to AGA investors and venture capitalists. The participants presented their own pitches and faced the sharks (judges). The winner received additional funding, tailored guidance from the AGA CGIT committee, partnering opportunities with interested parties, and the opportunity to represent AGA Shark Tank at the Digestive Disease Week (DDW).
The AGA Tech Summit Fellows Program is a learning platform that not only helps you find your niche in the world of GI innovation but also equips you with resources and connections to make an impact. It is also a great way to infuse new ideas into your practice or research. As healthcare professionals, we must create a culture where innovation can flourish, and where staff and patients feel empowered to contribute to the innovation process and help make change happen — to me, the AGA Tech Summit is one such avenue.
Reference
1. Kelly CJ and Young AJ. Promoting innovation in healthcare. Future Healthc J. 2017 Jun. doi: 10.7861/futurehosp.4-2-121.
Dr. Umar is Assistant Professor of Medicine, Section of Gastroenterology and Hepatology, Baylor College of Medicine, Houston, Texas, and a staff physician at Michael E. DeBakey VA Medical Center, Houston. Dr. Umar has no relevant financial conflicts and is on X, formerly Twitter, @shifaumarMD.

