User login
Insurance, location, income drive breast cancer surgery choices
The rates of breast-conserving surgery have increased over the last 2 decades among women with early-stage breast cancers in the United States, but disparities persist, based on an analysis of data from the National Cancer Data Base.
The rate of breast-conserving surgery has risen from approximately 54% in 1998 to 60% in 2011, but this rate may have been affected by “technical advances and changes in societal norms [that] include genetic testing for BRCA1 and BRCA2 mutation, advances in reconstruction techniques, breast magnetic resonance imaging, and increased patient interest in contralateral prophylactic mastectomy,” Dr. Meeghan Lautner and her colleagues at University of Texas MD Anderson Cancer Care Center, Houston, wrote.
“Among the most encouraging findings from our analysis is the considerable improvement of disparities based on facility type and the options afforded to older populations … however, insurance, income, and travel distance to treatment facilities persist as key barriers to [breast-conserving therapy] use,” the researchers said.
Their analysis of a cohort of 727,927 women, published online June 17 in JAMA Surgery, showed that women with early breast cancer were less likely to receive breast-conserving surgery if they had a low educational level, public or no health insurance, and low income.
Women aged 52-61 years were 14% more likely to be treated with breast-conserving surgery, compared with younger women. White race, fewer comorbidities, and living closer to a treatment facility were all positively associated with being treated with breast-conserving surgery.
Those in southern regions of the United States were significantly less likely to receive breast-conserving surgery, compared with those in the Northeast. The researchers said their data suggest the lower rates are because of the greater travel distances to treatment facilities in the South.
Women with no insurance were 25% less likely than those with private insurance to have breast-conserving therapy (JAMA Surgery 2015 June 17 [doi:10.1001/jamasurg.2015.1102]).
The researchers declared no conflicts of interest.
Optimal breast-conserving surgery for most lumpectomy-eligible patients requires a commitment to whole-breast radiation, which also requires access to a radiation oncologist and specialized treatment facility. This is an often insurmountable barrier for patients who lack transportation, have job or family responsibilities, or who live a considerable distance from a radiation facility.
Document
|
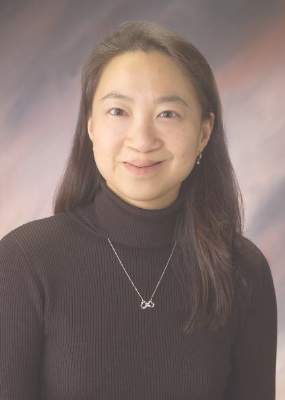
Dr. Lisa A. Newman |
Socioeconomically disadvantaged patients are typically the ones who face these obstacles, and these burdens of financial deprivation are disproportionately faced by minority racial/ethnic groups and rural communities.
Tragically, disadvantage will continue to breed more disadvantage.
Dr. Lisa A. Newman is director of the Breast Care Center at the University of Michigan Comprehensive Cancer Care Center, Ann Arbor, Mich. These comments are taken from an accompanying editorial (JAMA Surgery 2015 June 17 [doi:10.1001/jamasurg.2015.1114]). Dr. Newman declared no conflicts of interest.
Optimal breast-conserving surgery for most lumpectomy-eligible patients requires a commitment to whole-breast radiation, which also requires access to a radiation oncologist and specialized treatment facility. This is an often insurmountable barrier for patients who lack transportation, have job or family responsibilities, or who live a considerable distance from a radiation facility.
Document
|
Dr. Lisa A. Newman |
Socioeconomically disadvantaged patients are typically the ones who face these obstacles, and these burdens of financial deprivation are disproportionately faced by minority racial/ethnic groups and rural communities.
Tragically, disadvantage will continue to breed more disadvantage.
Dr. Lisa A. Newman is director of the Breast Care Center at the University of Michigan Comprehensive Cancer Care Center, Ann Arbor, Mich. These comments are taken from an accompanying editorial (JAMA Surgery 2015 June 17 [doi:10.1001/jamasurg.2015.1114]). Dr. Newman declared no conflicts of interest.
Optimal breast-conserving surgery for most lumpectomy-eligible patients requires a commitment to whole-breast radiation, which also requires access to a radiation oncologist and specialized treatment facility. This is an often insurmountable barrier for patients who lack transportation, have job or family responsibilities, or who live a considerable distance from a radiation facility.
Document
|
Dr. Lisa A. Newman |
Socioeconomically disadvantaged patients are typically the ones who face these obstacles, and these burdens of financial deprivation are disproportionately faced by minority racial/ethnic groups and rural communities.
Tragically, disadvantage will continue to breed more disadvantage.
Dr. Lisa A. Newman is director of the Breast Care Center at the University of Michigan Comprehensive Cancer Care Center, Ann Arbor, Mich. These comments are taken from an accompanying editorial (JAMA Surgery 2015 June 17 [doi:10.1001/jamasurg.2015.1114]). Dr. Newman declared no conflicts of interest.
The rates of breast-conserving surgery have increased over the last 2 decades among women with early-stage breast cancers in the United States, but disparities persist, based on an analysis of data from the National Cancer Data Base.
The rate of breast-conserving surgery has risen from approximately 54% in 1998 to 60% in 2011, but this rate may have been affected by “technical advances and changes in societal norms [that] include genetic testing for BRCA1 and BRCA2 mutation, advances in reconstruction techniques, breast magnetic resonance imaging, and increased patient interest in contralateral prophylactic mastectomy,” Dr. Meeghan Lautner and her colleagues at University of Texas MD Anderson Cancer Care Center, Houston, wrote.
“Among the most encouraging findings from our analysis is the considerable improvement of disparities based on facility type and the options afforded to older populations … however, insurance, income, and travel distance to treatment facilities persist as key barriers to [breast-conserving therapy] use,” the researchers said.
Their analysis of a cohort of 727,927 women, published online June 17 in JAMA Surgery, showed that women with early breast cancer were less likely to receive breast-conserving surgery if they had a low educational level, public or no health insurance, and low income.
Women aged 52-61 years were 14% more likely to be treated with breast-conserving surgery, compared with younger women. White race, fewer comorbidities, and living closer to a treatment facility were all positively associated with being treated with breast-conserving surgery.
Those in southern regions of the United States were significantly less likely to receive breast-conserving surgery, compared with those in the Northeast. The researchers said their data suggest the lower rates are because of the greater travel distances to treatment facilities in the South.
Women with no insurance were 25% less likely than those with private insurance to have breast-conserving therapy (JAMA Surgery 2015 June 17 [doi:10.1001/jamasurg.2015.1102]).
The researchers declared no conflicts of interest.
The rates of breast-conserving surgery have increased over the last 2 decades among women with early-stage breast cancers in the United States, but disparities persist, based on an analysis of data from the National Cancer Data Base.
The rate of breast-conserving surgery has risen from approximately 54% in 1998 to 60% in 2011, but this rate may have been affected by “technical advances and changes in societal norms [that] include genetic testing for BRCA1 and BRCA2 mutation, advances in reconstruction techniques, breast magnetic resonance imaging, and increased patient interest in contralateral prophylactic mastectomy,” Dr. Meeghan Lautner and her colleagues at University of Texas MD Anderson Cancer Care Center, Houston, wrote.
“Among the most encouraging findings from our analysis is the considerable improvement of disparities based on facility type and the options afforded to older populations … however, insurance, income, and travel distance to treatment facilities persist as key barriers to [breast-conserving therapy] use,” the researchers said.
Their analysis of a cohort of 727,927 women, published online June 17 in JAMA Surgery, showed that women with early breast cancer were less likely to receive breast-conserving surgery if they had a low educational level, public or no health insurance, and low income.
Women aged 52-61 years were 14% more likely to be treated with breast-conserving surgery, compared with younger women. White race, fewer comorbidities, and living closer to a treatment facility were all positively associated with being treated with breast-conserving surgery.
Those in southern regions of the United States were significantly less likely to receive breast-conserving surgery, compared with those in the Northeast. The researchers said their data suggest the lower rates are because of the greater travel distances to treatment facilities in the South.
Women with no insurance were 25% less likely than those with private insurance to have breast-conserving therapy (JAMA Surgery 2015 June 17 [doi:10.1001/jamasurg.2015.1102]).
The researchers declared no conflicts of interest.
FROM JAMA SURGERY
Key clinical point: Insurance status, income, and travel distance to treatment facilities are associated with the likelihood of having breast-conserving surgery.
Major finding: Women with no health insurance were 25% less likely than those with private insurance to receive breast-conserving surgery.
Data source: Analysis of data from 727,927 women in the National Cancer Data Base.
Disclosures: The researchers declared no conflicts of interest.
AUA: Renal mass biopsy trend tied to nonsurgical RCC treatment
NEW ORLEANS – Renal mass biopsy has traditionally played a restricted diagnostic role, but with its improved diagnostic accuracy, it is becoming a viable clinical tool in the modern era, according to Dr. Matthew Maurice.
“We were seeking to understand the current role of biopsy in the management of renal masses, said Dr. Maurice, a urology resident at University Hospitals Case Medical Center in Cleveland. “We used the National Cancer Database and looked at data from 2003 to 2011; what we saw was a rise in renal mass biopsy in the final 3 years of the study. It’s a very small increase, but a statistically significant increase, with people in 2011 having 1.3 times higher odds of being biopsied than they would have had in 2003.”
Dr. Maurice and his colleagues at Case Medical conducted a study examining renal mass biopsy use in the modern era, and presented their findings in a poster at the annual meeting of the American Urological Association.
Using the National Cancer Database (NCDB), Dr. Maurice and his colleagues identified all patients diagnosed with renal cell carcinoma (RCC) between 2003 and 2011. Patients within the RCC cohort were then classified as having undergone renal biopsy or not. Renal biopsy utilization rates were plotted over time, and patient, disease, provider, and treatment variables were evaluated via univariate and multivariate logistic regression models to determine the predictors of renal biopsy.
Out of 304,583 patients with kidney cancer, 35,942 patients (11.8%) underwent renal mass biopsy. From 2009 to 2011, Dr. Maurice and his coinvestigators observed a significant increase in biopsy use; patients diagnosed with a renal mass in 2011 had 1.3 times higher odds of being biopsied compared with those diagnosed in 2003 (odds radio, 1.3, confidence interval, 1.3-1.4, P < .01).
Eventual treatment was the strongest predictor of biopsy utilization. “Patients receiving observation or thermal ablative therapy (either cryoablation or radiofrequency ablation) were much more likely to receive biopsy than were those who received surgical therapy such as radical or partial nephrectomy,” Dr. Maurice explained. “So it seems like those treatments are driving the use of renal biopsy utilization in contemporary patients.”
Compared to patients treated with partial nephrectomy, patients managed with observation, cryoablation, or radiofrequency ablation had 4.2, 8.0, and 19.1 times the odds of being biopsied, respectively (OR, 4.2, CI, 4.0-4.5, P < .01; OR, 8.0, CI, 8.0-8.1, P < .01; OR, 19.1, CI, 18.4-19.7, P < .01). Patients with other known cancers, bulky lymph node involvement, or small masses ranging from 2 to 4 cm in size were also more likely to be biopsied (P < .01).
“Nonacademic hospitals were more likely to biopsy,” he added. “It could be that these hospitals are using observation and thermal ablative therapies more frequently.” Conversely, wealthier patients, patients treated at academic hospitals, and patients treated in the Northeast were significantly less likely to be biopsied. (P < .01).
On the basis of the data analyzed in this study, Dr. Maurice and his colleagues concluded that there is a trend in use of renal mass biopsy in nonacademic centers in recent years, particularly among patients with small renal masses and in those who eventually undergo observation or focal ablative therapies. Lesser indications predicting the usage of renal mass biopsy include the existence of other primary cancers and bulky lymph nodes.
Dr. Maurice reported no relevant financial relationships.
NEW ORLEANS – Renal mass biopsy has traditionally played a restricted diagnostic role, but with its improved diagnostic accuracy, it is becoming a viable clinical tool in the modern era, according to Dr. Matthew Maurice.
“We were seeking to understand the current role of biopsy in the management of renal masses, said Dr. Maurice, a urology resident at University Hospitals Case Medical Center in Cleveland. “We used the National Cancer Database and looked at data from 2003 to 2011; what we saw was a rise in renal mass biopsy in the final 3 years of the study. It’s a very small increase, but a statistically significant increase, with people in 2011 having 1.3 times higher odds of being biopsied than they would have had in 2003.”
Dr. Maurice and his colleagues at Case Medical conducted a study examining renal mass biopsy use in the modern era, and presented their findings in a poster at the annual meeting of the American Urological Association.
Using the National Cancer Database (NCDB), Dr. Maurice and his colleagues identified all patients diagnosed with renal cell carcinoma (RCC) between 2003 and 2011. Patients within the RCC cohort were then classified as having undergone renal biopsy or not. Renal biopsy utilization rates were plotted over time, and patient, disease, provider, and treatment variables were evaluated via univariate and multivariate logistic regression models to determine the predictors of renal biopsy.
Out of 304,583 patients with kidney cancer, 35,942 patients (11.8%) underwent renal mass biopsy. From 2009 to 2011, Dr. Maurice and his coinvestigators observed a significant increase in biopsy use; patients diagnosed with a renal mass in 2011 had 1.3 times higher odds of being biopsied compared with those diagnosed in 2003 (odds radio, 1.3, confidence interval, 1.3-1.4, P < .01).
Eventual treatment was the strongest predictor of biopsy utilization. “Patients receiving observation or thermal ablative therapy (either cryoablation or radiofrequency ablation) were much more likely to receive biopsy than were those who received surgical therapy such as radical or partial nephrectomy,” Dr. Maurice explained. “So it seems like those treatments are driving the use of renal biopsy utilization in contemporary patients.”
Compared to patients treated with partial nephrectomy, patients managed with observation, cryoablation, or radiofrequency ablation had 4.2, 8.0, and 19.1 times the odds of being biopsied, respectively (OR, 4.2, CI, 4.0-4.5, P < .01; OR, 8.0, CI, 8.0-8.1, P < .01; OR, 19.1, CI, 18.4-19.7, P < .01). Patients with other known cancers, bulky lymph node involvement, or small masses ranging from 2 to 4 cm in size were also more likely to be biopsied (P < .01).
“Nonacademic hospitals were more likely to biopsy,” he added. “It could be that these hospitals are using observation and thermal ablative therapies more frequently.” Conversely, wealthier patients, patients treated at academic hospitals, and patients treated in the Northeast were significantly less likely to be biopsied. (P < .01).
On the basis of the data analyzed in this study, Dr. Maurice and his colleagues concluded that there is a trend in use of renal mass biopsy in nonacademic centers in recent years, particularly among patients with small renal masses and in those who eventually undergo observation or focal ablative therapies. Lesser indications predicting the usage of renal mass biopsy include the existence of other primary cancers and bulky lymph nodes.
Dr. Maurice reported no relevant financial relationships.
NEW ORLEANS – Renal mass biopsy has traditionally played a restricted diagnostic role, but with its improved diagnostic accuracy, it is becoming a viable clinical tool in the modern era, according to Dr. Matthew Maurice.
“We were seeking to understand the current role of biopsy in the management of renal masses, said Dr. Maurice, a urology resident at University Hospitals Case Medical Center in Cleveland. “We used the National Cancer Database and looked at data from 2003 to 2011; what we saw was a rise in renal mass biopsy in the final 3 years of the study. It’s a very small increase, but a statistically significant increase, with people in 2011 having 1.3 times higher odds of being biopsied than they would have had in 2003.”
Dr. Maurice and his colleagues at Case Medical conducted a study examining renal mass biopsy use in the modern era, and presented their findings in a poster at the annual meeting of the American Urological Association.
Using the National Cancer Database (NCDB), Dr. Maurice and his colleagues identified all patients diagnosed with renal cell carcinoma (RCC) between 2003 and 2011. Patients within the RCC cohort were then classified as having undergone renal biopsy or not. Renal biopsy utilization rates were plotted over time, and patient, disease, provider, and treatment variables were evaluated via univariate and multivariate logistic regression models to determine the predictors of renal biopsy.
Out of 304,583 patients with kidney cancer, 35,942 patients (11.8%) underwent renal mass biopsy. From 2009 to 2011, Dr. Maurice and his coinvestigators observed a significant increase in biopsy use; patients diagnosed with a renal mass in 2011 had 1.3 times higher odds of being biopsied compared with those diagnosed in 2003 (odds radio, 1.3, confidence interval, 1.3-1.4, P < .01).
Eventual treatment was the strongest predictor of biopsy utilization. “Patients receiving observation or thermal ablative therapy (either cryoablation or radiofrequency ablation) were much more likely to receive biopsy than were those who received surgical therapy such as radical or partial nephrectomy,” Dr. Maurice explained. “So it seems like those treatments are driving the use of renal biopsy utilization in contemporary patients.”
Compared to patients treated with partial nephrectomy, patients managed with observation, cryoablation, or radiofrequency ablation had 4.2, 8.0, and 19.1 times the odds of being biopsied, respectively (OR, 4.2, CI, 4.0-4.5, P < .01; OR, 8.0, CI, 8.0-8.1, P < .01; OR, 19.1, CI, 18.4-19.7, P < .01). Patients with other known cancers, bulky lymph node involvement, or small masses ranging from 2 to 4 cm in size were also more likely to be biopsied (P < .01).
“Nonacademic hospitals were more likely to biopsy,” he added. “It could be that these hospitals are using observation and thermal ablative therapies more frequently.” Conversely, wealthier patients, patients treated at academic hospitals, and patients treated in the Northeast were significantly less likely to be biopsied. (P < .01).
On the basis of the data analyzed in this study, Dr. Maurice and his colleagues concluded that there is a trend in use of renal mass biopsy in nonacademic centers in recent years, particularly among patients with small renal masses and in those who eventually undergo observation or focal ablative therapies. Lesser indications predicting the usage of renal mass biopsy include the existence of other primary cancers and bulky lymph nodes.
Dr. Maurice reported no relevant financial relationships.
AT THE AUA ANNUAL MEETING
Key clinical point: Use of renal mass biopsy is increasing and the increase is likely linked to choice of treatment (observation or thermal ablative therapy).
Major finding: Patients diagnosed with renal mass had 1.3 times higher odds of being biopsied in 2011 than they would have had in 2003.
Data source: Sample from 2003-2011 National Cancer Database of 304,583 patients with kidney cancer, 35,942 of whom underwent renal mass biopsy.
Disclosures: Dr. Maurice reported no relevant financial relationships.
ICOO: Opioid self-dosing falls short of pain control
BOSTON – Many cancer patients do not pursue or at least do not achieve complete freedom from pain when permitted control over their opioid dose, according to a comprehensive analysis of published studies that evaluated patient-controlled analgesia.
“We do not know why. Patients were encouraged in these studies to titrate opioids until they were pain free or until they had side effects. Although this could be an issue of side effects, another interpretation is that complete pain control is not the goal for many individuals,” reported Dr. Brian H. Wetherington of the University of Kentucky, Lexington.
The data from this analysis were presented at the International Conference on Opioids from a comprehensive literature search that included 905 potentially relevant articles. Of these, 62 met inclusion criteria, particularly an assessment of patient-controlled opioids in patients with cancer pain. The studies also had to assess pain control with a visual analog scale (VAS) or the Neuropathy Pain Scale (NPS) using a 10-point system with 10 being the greatest level of pain imaginable.
“We were interested in evaluating whether patients, when given complete control over their opioids, would take sufficient doses to provide complete pain relief, which is often stated as the goal in pain management,” explained Dr. Wetherington, who was coauthor of a study led by his colleague at University of Kentucky, Dr. Michael Harned.
The answer was no. When the data from the 62 studies, which included 5,251 patients with cancer pain were collated, the average pain score at baseline was 5.4. At the time of assessment of pain control, the mean pain score was 2.7.
“The mean pain score for patients managing their own cancer pain on opioids was reduced from study entry but remained at the moderate to severe pain level or higher than what many health care providers would recommend,” Dr. Wetherington reported.
This review of published studies does not explain why lower pain scores are not reached, but the Dr. Wetherington and his coauthors hypothesized that patients are demonstrating their own benefit-to-risk ratio assessment.
This is thought to be the first systematic review to find that patients do not seek complete control of pain when given access to unrestricted analgesia, but several individual studies have made the same point. In one study cited by the authors, patients on a fentanyl patch only reduced their pain scores to 3.0 on average when given unlimited access to oral morphine for breakthroughs (J. Pain Symptom Manage. 1998;16:102-11).
“We think this deserves further study, because there may be lessons regarding how we think of optimal pain control. While the therapeutic target is often described as complete pain relief, these data suggest that this may not be the goal for patients when they are left to select their own level of pain control,” Dr. Wetherington explained.
The same observation regarding the failure of patients to eliminate all pain on patient-controlled analgesia has been made anecdotally by Dr. William G. Brose of Stanford (Calif.) University. However, he suggested in an interview that patients might be reluctant to rate themselves completely pain free on a subjective scale. He also believes that level of analgesia may not be the most relevant endpoint.
“We are increasingly evaluating change in patient function, which may be a more useful tool for evaluating the efficacy of pain control,” Dr. Brose said.
BOSTON – Many cancer patients do not pursue or at least do not achieve complete freedom from pain when permitted control over their opioid dose, according to a comprehensive analysis of published studies that evaluated patient-controlled analgesia.
“We do not know why. Patients were encouraged in these studies to titrate opioids until they were pain free or until they had side effects. Although this could be an issue of side effects, another interpretation is that complete pain control is not the goal for many individuals,” reported Dr. Brian H. Wetherington of the University of Kentucky, Lexington.
The data from this analysis were presented at the International Conference on Opioids from a comprehensive literature search that included 905 potentially relevant articles. Of these, 62 met inclusion criteria, particularly an assessment of patient-controlled opioids in patients with cancer pain. The studies also had to assess pain control with a visual analog scale (VAS) or the Neuropathy Pain Scale (NPS) using a 10-point system with 10 being the greatest level of pain imaginable.
“We were interested in evaluating whether patients, when given complete control over their opioids, would take sufficient doses to provide complete pain relief, which is often stated as the goal in pain management,” explained Dr. Wetherington, who was coauthor of a study led by his colleague at University of Kentucky, Dr. Michael Harned.
The answer was no. When the data from the 62 studies, which included 5,251 patients with cancer pain were collated, the average pain score at baseline was 5.4. At the time of assessment of pain control, the mean pain score was 2.7.
“The mean pain score for patients managing their own cancer pain on opioids was reduced from study entry but remained at the moderate to severe pain level or higher than what many health care providers would recommend,” Dr. Wetherington reported.
This review of published studies does not explain why lower pain scores are not reached, but the Dr. Wetherington and his coauthors hypothesized that patients are demonstrating their own benefit-to-risk ratio assessment.
This is thought to be the first systematic review to find that patients do not seek complete control of pain when given access to unrestricted analgesia, but several individual studies have made the same point. In one study cited by the authors, patients on a fentanyl patch only reduced their pain scores to 3.0 on average when given unlimited access to oral morphine for breakthroughs (J. Pain Symptom Manage. 1998;16:102-11).
“We think this deserves further study, because there may be lessons regarding how we think of optimal pain control. While the therapeutic target is often described as complete pain relief, these data suggest that this may not be the goal for patients when they are left to select their own level of pain control,” Dr. Wetherington explained.
The same observation regarding the failure of patients to eliminate all pain on patient-controlled analgesia has been made anecdotally by Dr. William G. Brose of Stanford (Calif.) University. However, he suggested in an interview that patients might be reluctant to rate themselves completely pain free on a subjective scale. He also believes that level of analgesia may not be the most relevant endpoint.
“We are increasingly evaluating change in patient function, which may be a more useful tool for evaluating the efficacy of pain control,” Dr. Brose said.
BOSTON – Many cancer patients do not pursue or at least do not achieve complete freedom from pain when permitted control over their opioid dose, according to a comprehensive analysis of published studies that evaluated patient-controlled analgesia.
“We do not know why. Patients were encouraged in these studies to titrate opioids until they were pain free or until they had side effects. Although this could be an issue of side effects, another interpretation is that complete pain control is not the goal for many individuals,” reported Dr. Brian H. Wetherington of the University of Kentucky, Lexington.
The data from this analysis were presented at the International Conference on Opioids from a comprehensive literature search that included 905 potentially relevant articles. Of these, 62 met inclusion criteria, particularly an assessment of patient-controlled opioids in patients with cancer pain. The studies also had to assess pain control with a visual analog scale (VAS) or the Neuropathy Pain Scale (NPS) using a 10-point system with 10 being the greatest level of pain imaginable.
“We were interested in evaluating whether patients, when given complete control over their opioids, would take sufficient doses to provide complete pain relief, which is often stated as the goal in pain management,” explained Dr. Wetherington, who was coauthor of a study led by his colleague at University of Kentucky, Dr. Michael Harned.
The answer was no. When the data from the 62 studies, which included 5,251 patients with cancer pain were collated, the average pain score at baseline was 5.4. At the time of assessment of pain control, the mean pain score was 2.7.
“The mean pain score for patients managing their own cancer pain on opioids was reduced from study entry but remained at the moderate to severe pain level or higher than what many health care providers would recommend,” Dr. Wetherington reported.
This review of published studies does not explain why lower pain scores are not reached, but the Dr. Wetherington and his coauthors hypothesized that patients are demonstrating their own benefit-to-risk ratio assessment.
This is thought to be the first systematic review to find that patients do not seek complete control of pain when given access to unrestricted analgesia, but several individual studies have made the same point. In one study cited by the authors, patients on a fentanyl patch only reduced their pain scores to 3.0 on average when given unlimited access to oral morphine for breakthroughs (J. Pain Symptom Manage. 1998;16:102-11).
“We think this deserves further study, because there may be lessons regarding how we think of optimal pain control. While the therapeutic target is often described as complete pain relief, these data suggest that this may not be the goal for patients when they are left to select their own level of pain control,” Dr. Wetherington explained.
The same observation regarding the failure of patients to eliminate all pain on patient-controlled analgesia has been made anecdotally by Dr. William G. Brose of Stanford (Calif.) University. However, he suggested in an interview that patients might be reluctant to rate themselves completely pain free on a subjective scale. He also believes that level of analgesia may not be the most relevant endpoint.
“We are increasingly evaluating change in patient function, which may be a more useful tool for evaluating the efficacy of pain control,” Dr. Brose said.
AT ICOO 2015
Key clinical point: Given the opportunity, patients do not titrate opioid therapy to a point of complete pain control, according to a comprehensive survey of published studies.
Major finding: In a survey of 62 published studies of cancer patients who were provided unlimited access to opioids for pain control, the average pain control was 2.7 on a scale of 10, indicating that most patients do not seek or are unable to achieve complete control with an acceptable benefit-to-risk ratio.
Data source: Retrospective data review.
Disclosures: The study was investigator initiated. Dr. Wetherington reported having no financial disclosures.
ASCO: Omitting adjuvant radiation after pCR ups locoregional recurrence risk
CHICAGO – Women with breast cancer treated with neoadjuvant chemotherapy and surgery are more likely to have a recurrence in the breast, chest wall, or axilla or to die if they don’t receive adjuvant radiation therapy, even if they had a pathologic complete response to the chemotherapy, new data show.
In a meta-analysis of three Gepar trials conducted by the German Breast Group, radiation therapy was associated with a 38% lower multivariate risk of locoregional recurrence or death, investigators reported at the annual meeting of the American Society of Clinical Oncology. Significant benefit was seen regardless of pathologic complete response, although findings across other subgroups were not consistent, possibly due to selection bias or underlying confounders.
“Radiotherapy is an independent prognostic factor for locoregional recurrence–free survival after neoadjuvant chemotherapy in breast cancer. However, the optimal selection criteria remain unclear,” commented first author Dr. David Krug of University Hospital Heidelberg (Germany).
“We are eagerly awaiting the results of prospective studies that are currently recruiting patients,” he added, referring to the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-51 trial and the Radiotherapy After Primary Chemotherapy for Breast Cancer (RAPCHEM) trial.
Findings of this meta-analysis are not practice changing, according to invited discussant Dr. Monica Morrow, chief of the breast service, department of surgery, and the Anne Burnett Windfohr Chair of Clinical Oncology at the Memorial Sloan Kettering Cancer Center in New York. “The Gepar data is not consistent enough across subsets to draw any different conclusions other than we need more data,” she said.
Focusing on the women who underwent mastectomy, she noted that only a small number who had a pathologic complete response did not receive radiation therapy, “so this study unfortunately lacks the power to tell us anything about the ability to eliminate radiation in this group.”
“What we’d really like to know about local control after neoadjuvant therapy is what’s the relative contribution of pretreatment stage and posttreatment stage to the risk of locoregional recurrence, especially in patients who achieve pathologic complete response? And if we try to address that question with this study, the results were a little murky,” Dr. Morrow further noted. For example, patients with higher–T stage primary tumors benefited from postmastectomy radiation, but patients who were clinically node positive did not.
“I think right now, what we have to say is we need to continue to do what we have been doing up until the present time, namely, patients whose presenting stage clearly indicates the need for radiotherapy should receive it, and patients who have lower-stage disease perhaps not,” she concluded, agreeing that the NSABP B-51 trial should help put this issue to rest.
Dr. Krug and his colleagues performed a pooled meta-analysis of data from the GeparTrio, GeparQuattro, and GeparQuinto trials of neoadjuvant chemotherapy, in which guidelines specified when adjuvant radiation therapy should be used. Those guidelines called for whole-breast radiation therapy with a boost after breast-conserving surgery (with omission of the boost in low-risk patients); radiation therapy after mastectomy for patients having more extensive disease before neoadjuvant chemotherapy; and radiation therapy for those with greater involvement of the regional lymphatics.
The meta-analysis was based on a total of 3,370 women. Overall, 94% received radiation therapy (99% of those who had undergone breast-conserving surgery and 85% of those who had undergone mastectomy).
With a median follow-up of 4.2 years, the 5-year rate of locoregional recurrence–free survival was 89.2% in the entire study population, according to Dr. Krug.
Women who did not receive radiation therapy had a significantly elevated risk of such recurrence or death compared with peers who received it. In subgroups analyses, benefit was significant whether women had had a pathologic complete response to neoadjuvant chemotherapy or not. Greatest absolute benefit was seen in those with a pathologic complete response, clinically positive nodes, or pathologically negative nodes.
The 5-year rate of disease-free survival was 74.0% in the entire study population. Here, there was only a trend toward a higher risk of events for women who did not receive radiation therapy.
In multivariate analyses, radiation therapy independently predicted better locoregional recurrence–free survival (hazard ratio, 0.62; P = .038) but not disease-free survival.
When analyses were restricted to women who had undergone mastectomy, radiation therapy was associated with significantly better locoregional recurrence–free survival among those with clinical stage T3/4 disease, pathologically negative nodes, a conversion from clinically positive to pathologically negative nodes, or hormone receptor–negative, HER2-positive disease.
It was associated with poorer disease-free survival for patients who did not achieve a pathologic complete response, had clinical stage T1/2 disease, or were clinically node negative.
Multivariate analysis here again showed that radiation therapy independently predicted better locoregional recurrence–free survival (HR, 0.56; P = .029) but not disease-free survival.
CHICAGO – Women with breast cancer treated with neoadjuvant chemotherapy and surgery are more likely to have a recurrence in the breast, chest wall, or axilla or to die if they don’t receive adjuvant radiation therapy, even if they had a pathologic complete response to the chemotherapy, new data show.
In a meta-analysis of three Gepar trials conducted by the German Breast Group, radiation therapy was associated with a 38% lower multivariate risk of locoregional recurrence or death, investigators reported at the annual meeting of the American Society of Clinical Oncology. Significant benefit was seen regardless of pathologic complete response, although findings across other subgroups were not consistent, possibly due to selection bias or underlying confounders.
“Radiotherapy is an independent prognostic factor for locoregional recurrence–free survival after neoadjuvant chemotherapy in breast cancer. However, the optimal selection criteria remain unclear,” commented first author Dr. David Krug of University Hospital Heidelberg (Germany).
“We are eagerly awaiting the results of prospective studies that are currently recruiting patients,” he added, referring to the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-51 trial and the Radiotherapy After Primary Chemotherapy for Breast Cancer (RAPCHEM) trial.
Findings of this meta-analysis are not practice changing, according to invited discussant Dr. Monica Morrow, chief of the breast service, department of surgery, and the Anne Burnett Windfohr Chair of Clinical Oncology at the Memorial Sloan Kettering Cancer Center in New York. “The Gepar data is not consistent enough across subsets to draw any different conclusions other than we need more data,” she said.
Focusing on the women who underwent mastectomy, she noted that only a small number who had a pathologic complete response did not receive radiation therapy, “so this study unfortunately lacks the power to tell us anything about the ability to eliminate radiation in this group.”
“What we’d really like to know about local control after neoadjuvant therapy is what’s the relative contribution of pretreatment stage and posttreatment stage to the risk of locoregional recurrence, especially in patients who achieve pathologic complete response? And if we try to address that question with this study, the results were a little murky,” Dr. Morrow further noted. For example, patients with higher–T stage primary tumors benefited from postmastectomy radiation, but patients who were clinically node positive did not.
“I think right now, what we have to say is we need to continue to do what we have been doing up until the present time, namely, patients whose presenting stage clearly indicates the need for radiotherapy should receive it, and patients who have lower-stage disease perhaps not,” she concluded, agreeing that the NSABP B-51 trial should help put this issue to rest.
Dr. Krug and his colleagues performed a pooled meta-analysis of data from the GeparTrio, GeparQuattro, and GeparQuinto trials of neoadjuvant chemotherapy, in which guidelines specified when adjuvant radiation therapy should be used. Those guidelines called for whole-breast radiation therapy with a boost after breast-conserving surgery (with omission of the boost in low-risk patients); radiation therapy after mastectomy for patients having more extensive disease before neoadjuvant chemotherapy; and radiation therapy for those with greater involvement of the regional lymphatics.
The meta-analysis was based on a total of 3,370 women. Overall, 94% received radiation therapy (99% of those who had undergone breast-conserving surgery and 85% of those who had undergone mastectomy).
With a median follow-up of 4.2 years, the 5-year rate of locoregional recurrence–free survival was 89.2% in the entire study population, according to Dr. Krug.
Women who did not receive radiation therapy had a significantly elevated risk of such recurrence or death compared with peers who received it. In subgroups analyses, benefit was significant whether women had had a pathologic complete response to neoadjuvant chemotherapy or not. Greatest absolute benefit was seen in those with a pathologic complete response, clinically positive nodes, or pathologically negative nodes.
The 5-year rate of disease-free survival was 74.0% in the entire study population. Here, there was only a trend toward a higher risk of events for women who did not receive radiation therapy.
In multivariate analyses, radiation therapy independently predicted better locoregional recurrence–free survival (hazard ratio, 0.62; P = .038) but not disease-free survival.
When analyses were restricted to women who had undergone mastectomy, radiation therapy was associated with significantly better locoregional recurrence–free survival among those with clinical stage T3/4 disease, pathologically negative nodes, a conversion from clinically positive to pathologically negative nodes, or hormone receptor–negative, HER2-positive disease.
It was associated with poorer disease-free survival for patients who did not achieve a pathologic complete response, had clinical stage T1/2 disease, or were clinically node negative.
Multivariate analysis here again showed that radiation therapy independently predicted better locoregional recurrence–free survival (HR, 0.56; P = .029) but not disease-free survival.
CHICAGO – Women with breast cancer treated with neoadjuvant chemotherapy and surgery are more likely to have a recurrence in the breast, chest wall, or axilla or to die if they don’t receive adjuvant radiation therapy, even if they had a pathologic complete response to the chemotherapy, new data show.
In a meta-analysis of three Gepar trials conducted by the German Breast Group, radiation therapy was associated with a 38% lower multivariate risk of locoregional recurrence or death, investigators reported at the annual meeting of the American Society of Clinical Oncology. Significant benefit was seen regardless of pathologic complete response, although findings across other subgroups were not consistent, possibly due to selection bias or underlying confounders.
“Radiotherapy is an independent prognostic factor for locoregional recurrence–free survival after neoadjuvant chemotherapy in breast cancer. However, the optimal selection criteria remain unclear,” commented first author Dr. David Krug of University Hospital Heidelberg (Germany).
“We are eagerly awaiting the results of prospective studies that are currently recruiting patients,” he added, referring to the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-51 trial and the Radiotherapy After Primary Chemotherapy for Breast Cancer (RAPCHEM) trial.
Findings of this meta-analysis are not practice changing, according to invited discussant Dr. Monica Morrow, chief of the breast service, department of surgery, and the Anne Burnett Windfohr Chair of Clinical Oncology at the Memorial Sloan Kettering Cancer Center in New York. “The Gepar data is not consistent enough across subsets to draw any different conclusions other than we need more data,” she said.
Focusing on the women who underwent mastectomy, she noted that only a small number who had a pathologic complete response did not receive radiation therapy, “so this study unfortunately lacks the power to tell us anything about the ability to eliminate radiation in this group.”
“What we’d really like to know about local control after neoadjuvant therapy is what’s the relative contribution of pretreatment stage and posttreatment stage to the risk of locoregional recurrence, especially in patients who achieve pathologic complete response? And if we try to address that question with this study, the results were a little murky,” Dr. Morrow further noted. For example, patients with higher–T stage primary tumors benefited from postmastectomy radiation, but patients who were clinically node positive did not.
“I think right now, what we have to say is we need to continue to do what we have been doing up until the present time, namely, patients whose presenting stage clearly indicates the need for radiotherapy should receive it, and patients who have lower-stage disease perhaps not,” she concluded, agreeing that the NSABP B-51 trial should help put this issue to rest.
Dr. Krug and his colleagues performed a pooled meta-analysis of data from the GeparTrio, GeparQuattro, and GeparQuinto trials of neoadjuvant chemotherapy, in which guidelines specified when adjuvant radiation therapy should be used. Those guidelines called for whole-breast radiation therapy with a boost after breast-conserving surgery (with omission of the boost in low-risk patients); radiation therapy after mastectomy for patients having more extensive disease before neoadjuvant chemotherapy; and radiation therapy for those with greater involvement of the regional lymphatics.
The meta-analysis was based on a total of 3,370 women. Overall, 94% received radiation therapy (99% of those who had undergone breast-conserving surgery and 85% of those who had undergone mastectomy).
With a median follow-up of 4.2 years, the 5-year rate of locoregional recurrence–free survival was 89.2% in the entire study population, according to Dr. Krug.
Women who did not receive radiation therapy had a significantly elevated risk of such recurrence or death compared with peers who received it. In subgroups analyses, benefit was significant whether women had had a pathologic complete response to neoadjuvant chemotherapy or not. Greatest absolute benefit was seen in those with a pathologic complete response, clinically positive nodes, or pathologically negative nodes.
The 5-year rate of disease-free survival was 74.0% in the entire study population. Here, there was only a trend toward a higher risk of events for women who did not receive radiation therapy.
In multivariate analyses, radiation therapy independently predicted better locoregional recurrence–free survival (hazard ratio, 0.62; P = .038) but not disease-free survival.
When analyses were restricted to women who had undergone mastectomy, radiation therapy was associated with significantly better locoregional recurrence–free survival among those with clinical stage T3/4 disease, pathologically negative nodes, a conversion from clinically positive to pathologically negative nodes, or hormone receptor–negative, HER2-positive disease.
It was associated with poorer disease-free survival for patients who did not achieve a pathologic complete response, had clinical stage T1/2 disease, or were clinically node negative.
Multivariate analysis here again showed that radiation therapy independently predicted better locoregional recurrence–free survival (HR, 0.56; P = .029) but not disease-free survival.
AT THE 2015 ASCO ANNUAL MEETING
Key clinical point: Adjuvant radiation therapy improves locoregional recurrence–free survival after neoadjuvant chemo and surgery for breast cancer.
Major finding: Women who received adjuvant radiation therapy had a 38% lower risk of locoregional recurrence or death.
Data source: A meta-analysis of three randomized trials among 3,370 women who underwent neoadjuvant chemotherapy and surgery for breast cancer.
Disclosures: Dr. Krug disclosed that he receives travel expenses from Accuray.
Prostate cancer screening for men over 50 has declined
Subsequent to the 2012 U.S. Preventative Services Task Force recommendation discouraging prostate-specific antigen (PSA)-based screening, prostate cancer screening significantly declined among men age 50 years and older in the United States, according to a study published online in the Journal of Clinical Oncology.
Based on National Health Interview Surveys in 2005, 2010, and 2013, self-reported PSA-testing levels decreased most among men aged 50-59 years, from 33.2% in 2010 to 24.8% in 2013 (odds ratio, 0.66; P < .01). Declines from 2010 to 2013 were also observed among men aged 60-74 years (51.2%-43.6%; OR, 0.74; P < .01); and aged 75 and older (43.9%-37.1%, OR, 0.75; P = .03). Among men aged 40-49 years, the decline from 12.5% to 11.2% was not significant (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2015.61.6532]).
The declines may reflect increased adherence by physicians to USPSTF guidelines; nevertheless, in 2013 approximately one-third of men aged 65 or older who had high risk for 9-year mortality (about 1.4 million individuals) were screened.
“Persistently elevated screening rates among men with limited remaining life expectancies are troubling and merit further interventions,” wrote Dr. Michael Drazer of the University of Chicago Medical Center and colleagues. “These may include increasing awareness of initiatives such as Choosing Wisely recommendations from the American Society of Clinical Oncology and recommendations from the American Geriatrics Society,” they wrote.
If these efforts prove unsuccessful, reducing or eliminating reimbursements for screening and interventions may be considered, the authors suggest.
A multivariate model identified factors that predict which men over age 65 are likely to be screened, and these are men who went to college, were married, consumed alcohol, and received a colonoscopy in the last 10 years. They found no significant predictors in the patient population for declines in screening from 2010 to 2013.
Several studies support the use of extended screening intervals (every 2-3 years) for patients at low risk for prostate cancer. Annual screening of men aged 55-67 years has been estimated to result in a 50% overdiagnosis rate.
Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
Subsequent to the 2012 U.S. Preventative Services Task Force recommendation discouraging prostate-specific antigen (PSA)-based screening, prostate cancer screening significantly declined among men age 50 years and older in the United States, according to a study published online in the Journal of Clinical Oncology.
Based on National Health Interview Surveys in 2005, 2010, and 2013, self-reported PSA-testing levels decreased most among men aged 50-59 years, from 33.2% in 2010 to 24.8% in 2013 (odds ratio, 0.66; P < .01). Declines from 2010 to 2013 were also observed among men aged 60-74 years (51.2%-43.6%; OR, 0.74; P < .01); and aged 75 and older (43.9%-37.1%, OR, 0.75; P = .03). Among men aged 40-49 years, the decline from 12.5% to 11.2% was not significant (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2015.61.6532]).
The declines may reflect increased adherence by physicians to USPSTF guidelines; nevertheless, in 2013 approximately one-third of men aged 65 or older who had high risk for 9-year mortality (about 1.4 million individuals) were screened.
“Persistently elevated screening rates among men with limited remaining life expectancies are troubling and merit further interventions,” wrote Dr. Michael Drazer of the University of Chicago Medical Center and colleagues. “These may include increasing awareness of initiatives such as Choosing Wisely recommendations from the American Society of Clinical Oncology and recommendations from the American Geriatrics Society,” they wrote.
If these efforts prove unsuccessful, reducing or eliminating reimbursements for screening and interventions may be considered, the authors suggest.
A multivariate model identified factors that predict which men over age 65 are likely to be screened, and these are men who went to college, were married, consumed alcohol, and received a colonoscopy in the last 10 years. They found no significant predictors in the patient population for declines in screening from 2010 to 2013.
Several studies support the use of extended screening intervals (every 2-3 years) for patients at low risk for prostate cancer. Annual screening of men aged 55-67 years has been estimated to result in a 50% overdiagnosis rate.
Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
Subsequent to the 2012 U.S. Preventative Services Task Force recommendation discouraging prostate-specific antigen (PSA)-based screening, prostate cancer screening significantly declined among men age 50 years and older in the United States, according to a study published online in the Journal of Clinical Oncology.
Based on National Health Interview Surveys in 2005, 2010, and 2013, self-reported PSA-testing levels decreased most among men aged 50-59 years, from 33.2% in 2010 to 24.8% in 2013 (odds ratio, 0.66; P < .01). Declines from 2010 to 2013 were also observed among men aged 60-74 years (51.2%-43.6%; OR, 0.74; P < .01); and aged 75 and older (43.9%-37.1%, OR, 0.75; P = .03). Among men aged 40-49 years, the decline from 12.5% to 11.2% was not significant (Journ. Clin. Onc. 2015 June 8 [doi:10.1200/JCO.2015.61.6532]).
The declines may reflect increased adherence by physicians to USPSTF guidelines; nevertheless, in 2013 approximately one-third of men aged 65 or older who had high risk for 9-year mortality (about 1.4 million individuals) were screened.
“Persistently elevated screening rates among men with limited remaining life expectancies are troubling and merit further interventions,” wrote Dr. Michael Drazer of the University of Chicago Medical Center and colleagues. “These may include increasing awareness of initiatives such as Choosing Wisely recommendations from the American Society of Clinical Oncology and recommendations from the American Geriatrics Society,” they wrote.
If these efforts prove unsuccessful, reducing or eliminating reimbursements for screening and interventions may be considered, the authors suggest.
A multivariate model identified factors that predict which men over age 65 are likely to be screened, and these are men who went to college, were married, consumed alcohol, and received a colonoscopy in the last 10 years. They found no significant predictors in the patient population for declines in screening from 2010 to 2013.
Several studies support the use of extended screening intervals (every 2-3 years) for patients at low risk for prostate cancer. Annual screening of men aged 55-67 years has been estimated to result in a 50% overdiagnosis rate.
Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Prostate cancer screening rates among men aged 50 years and older declined nationwide from 2010 to 2013.
Major finding: From 2010 to 2013 screening rates significantly declined among men aged 50-59 (33.2%-24.8%, P < .01); aged 60-74 (51.2%-43.6%, P < .01); and aged 75 and older (43.9%-37.1%, P = .03).
Data source: The National Health Interview Survey is a face-to-face, cross-sectional survey that included men ≥ 40 years who had seen a physician in the previous year, representing over 60,000,000 men.
Disclosures: Drs. Drazer and Huo reported having no financial disclosures. Dr. Eggener reported having consulting or advisory roles with Myriad Genetics, Medivation, Janssen Pharmaceuticals, Genomic Health, OPKO Diagnostics, and MDxHealth.
ASCO: Research IDs new subtype of refractory prostate cancer
CHICAGO – Researchers have identified a new histologic subset of metastatic castration-resistant prostate cancer called intermediate atypical carcinoma.
“Despite being cytologically bland, this is an aggressive cancer with shortened survival similar to that seen with small-cell neuroendocrine cancer,” study author Dr. Eric J. Small said at the annual meeting of the American Society of Clinical Oncology.
Therapies targeting the androgen receptor (AR) like abiraterone and enzalutamide have revolutionized the treatment of metastatic castration-resistant prostate cancer (mCRPC), but resistance to these agents is near-universal and leads to progressive disease and death. At the same time, clinicians are seeing an increasing number of patients with small cell neuroendocrine prostate cancer (SCNC), Dr. Small, professor of medicine at the University of California, San Francisco, said.
As part of a larger project designed to understand the mechanisms of resistance to abiraterone (Zytiga) and enzalutamide (Xtandi) undertaken by the West Coast Prostate Cancer Dream Team, biopsies were performed of a metastatic site in about 160 eligible men with mCRPC.Most (58%) had a Gleason score of 8 or more at diagnosis; 40% had been treated with abiraterone, 10% with enzalutamide, and 17% with both.
Formalin-fixed paraffin-embedded tissue was collected for histologic evaluation by three independent pathologists. Fresh frozen tissue, which underwent laser capture microdissection, was used for genomic analysis.
As of May 1, 173 of 300 planned biopsies have been conducted. In the 160 samples evaluated to date, there was adequate tissue for analysis in 124, for a 78% biopsy success rate, he said.
Among the 124 evaluable biopsies, 35% were classified as pure adenocarcinoma and 13% as pure SCNC.
A novel subtype was identified in another 26% that “consisted of a pure population of cells that was distinct from adenocarcinoma and distinct from small cell neuroendocrine cancer. We have termed this group intermediate atypical carcinoma (IAC),” Dr. Small said.
The remaining quarter of biopsies was composed of mixed populations.
In addition to the independent review, a consensus meeting with two additional pathologists confirmed that this was a new, highly reproducible pathologic subclass, he said.
The researchers next sought to determine whether IAC is phenotypically distinct. A survival analysis was performed based on biopsy pathology and revealed that men who develop IAC have poor survival.
Indeed, survival with IAC (median 11.9 months) tracks with that of SCNC (median 6.6 months) and is distinct from adenocarcinoma, with a log-rank P value of .041, Dr. Small said. Further, when IAC and SCNC were grouped together, there was a dramatically different survival curve (median 8.9 months) than that seen with adenocarcinoma (P = .006).
An analysis using microresected samples indicated that IAC is also genomically distinct, he said. Small cell nuclear clusters showed enrichment of neuronal and cell cycle elements and downregulation of androgen-receptor elements and the immune system.
Based on these findings, machine learning was used to develop a 50-gene signature, with 88.3% accuracy to distinguish small cell from non–small cell histology and 78.5% accuracy to distinguish small cell or IAC histology from adenocarcinoma. The test is not clinically available at this time, but is being used to identify new therapeutic targets.
“We are actively identifying the unique features of this subtype that can be targeted with therapy,” Dr. Small said in an interview. “There is a huge unmet need, since no one knows how to treat these patients, who comprise a significant portion of patients.”
Indeed, in the analysis, IAC represented a fourth of all metastatic castration-resistant biopsies and when combined with small cell neuroendocrine cancer accounted for 40% of all samples.
“This comprises the single largest group of abiraterone- and enzalutamide-refractory patients,” he concluded. “The increasing use of highly potent AR-targeted therapy may contribute to the increasing frequency of this entity, although that is conjecture at this point and certainly ascertainment bias may play a role.”
Discussant Dr. Scott Tomlins, a pathologist from the University of Michigan in Ann Arbor, said one of the study’s major findings is that collecting tissue for comprehensive molecular analysis is feasible in the context of a well-funded, team-based infrastructure, adding that this will likely have to be the way going forward. Despite limited sample numbers, there also appears to be a “strong signal” that gene expression signatures can discriminate various subtypes.
The study was funded by StandUpToCancer, the Prostate Cancer Foundation, and American Association for Cancer Research. Dr. Small reported having no disclosures.
On Twitter @pwendl
CHICAGO – Researchers have identified a new histologic subset of metastatic castration-resistant prostate cancer called intermediate atypical carcinoma.
“Despite being cytologically bland, this is an aggressive cancer with shortened survival similar to that seen with small-cell neuroendocrine cancer,” study author Dr. Eric J. Small said at the annual meeting of the American Society of Clinical Oncology.
Therapies targeting the androgen receptor (AR) like abiraterone and enzalutamide have revolutionized the treatment of metastatic castration-resistant prostate cancer (mCRPC), but resistance to these agents is near-universal and leads to progressive disease and death. At the same time, clinicians are seeing an increasing number of patients with small cell neuroendocrine prostate cancer (SCNC), Dr. Small, professor of medicine at the University of California, San Francisco, said.
As part of a larger project designed to understand the mechanisms of resistance to abiraterone (Zytiga) and enzalutamide (Xtandi) undertaken by the West Coast Prostate Cancer Dream Team, biopsies were performed of a metastatic site in about 160 eligible men with mCRPC.Most (58%) had a Gleason score of 8 or more at diagnosis; 40% had been treated with abiraterone, 10% with enzalutamide, and 17% with both.
Formalin-fixed paraffin-embedded tissue was collected for histologic evaluation by three independent pathologists. Fresh frozen tissue, which underwent laser capture microdissection, was used for genomic analysis.
As of May 1, 173 of 300 planned biopsies have been conducted. In the 160 samples evaluated to date, there was adequate tissue for analysis in 124, for a 78% biopsy success rate, he said.
Among the 124 evaluable biopsies, 35% were classified as pure adenocarcinoma and 13% as pure SCNC.
A novel subtype was identified in another 26% that “consisted of a pure population of cells that was distinct from adenocarcinoma and distinct from small cell neuroendocrine cancer. We have termed this group intermediate atypical carcinoma (IAC),” Dr. Small said.
The remaining quarter of biopsies was composed of mixed populations.
In addition to the independent review, a consensus meeting with two additional pathologists confirmed that this was a new, highly reproducible pathologic subclass, he said.
The researchers next sought to determine whether IAC is phenotypically distinct. A survival analysis was performed based on biopsy pathology and revealed that men who develop IAC have poor survival.
Indeed, survival with IAC (median 11.9 months) tracks with that of SCNC (median 6.6 months) and is distinct from adenocarcinoma, with a log-rank P value of .041, Dr. Small said. Further, when IAC and SCNC were grouped together, there was a dramatically different survival curve (median 8.9 months) than that seen with adenocarcinoma (P = .006).
An analysis using microresected samples indicated that IAC is also genomically distinct, he said. Small cell nuclear clusters showed enrichment of neuronal and cell cycle elements and downregulation of androgen-receptor elements and the immune system.
Based on these findings, machine learning was used to develop a 50-gene signature, with 88.3% accuracy to distinguish small cell from non–small cell histology and 78.5% accuracy to distinguish small cell or IAC histology from adenocarcinoma. The test is not clinically available at this time, but is being used to identify new therapeutic targets.
“We are actively identifying the unique features of this subtype that can be targeted with therapy,” Dr. Small said in an interview. “There is a huge unmet need, since no one knows how to treat these patients, who comprise a significant portion of patients.”
Indeed, in the analysis, IAC represented a fourth of all metastatic castration-resistant biopsies and when combined with small cell neuroendocrine cancer accounted for 40% of all samples.
“This comprises the single largest group of abiraterone- and enzalutamide-refractory patients,” he concluded. “The increasing use of highly potent AR-targeted therapy may contribute to the increasing frequency of this entity, although that is conjecture at this point and certainly ascertainment bias may play a role.”
Discussant Dr. Scott Tomlins, a pathologist from the University of Michigan in Ann Arbor, said one of the study’s major findings is that collecting tissue for comprehensive molecular analysis is feasible in the context of a well-funded, team-based infrastructure, adding that this will likely have to be the way going forward. Despite limited sample numbers, there also appears to be a “strong signal” that gene expression signatures can discriminate various subtypes.
The study was funded by StandUpToCancer, the Prostate Cancer Foundation, and American Association for Cancer Research. Dr. Small reported having no disclosures.
On Twitter @pwendl
CHICAGO – Researchers have identified a new histologic subset of metastatic castration-resistant prostate cancer called intermediate atypical carcinoma.
“Despite being cytologically bland, this is an aggressive cancer with shortened survival similar to that seen with small-cell neuroendocrine cancer,” study author Dr. Eric J. Small said at the annual meeting of the American Society of Clinical Oncology.
Therapies targeting the androgen receptor (AR) like abiraterone and enzalutamide have revolutionized the treatment of metastatic castration-resistant prostate cancer (mCRPC), but resistance to these agents is near-universal and leads to progressive disease and death. At the same time, clinicians are seeing an increasing number of patients with small cell neuroendocrine prostate cancer (SCNC), Dr. Small, professor of medicine at the University of California, San Francisco, said.
As part of a larger project designed to understand the mechanisms of resistance to abiraterone (Zytiga) and enzalutamide (Xtandi) undertaken by the West Coast Prostate Cancer Dream Team, biopsies were performed of a metastatic site in about 160 eligible men with mCRPC.Most (58%) had a Gleason score of 8 or more at diagnosis; 40% had been treated with abiraterone, 10% with enzalutamide, and 17% with both.
Formalin-fixed paraffin-embedded tissue was collected for histologic evaluation by three independent pathologists. Fresh frozen tissue, which underwent laser capture microdissection, was used for genomic analysis.
As of May 1, 173 of 300 planned biopsies have been conducted. In the 160 samples evaluated to date, there was adequate tissue for analysis in 124, for a 78% biopsy success rate, he said.
Among the 124 evaluable biopsies, 35% were classified as pure adenocarcinoma and 13% as pure SCNC.
A novel subtype was identified in another 26% that “consisted of a pure population of cells that was distinct from adenocarcinoma and distinct from small cell neuroendocrine cancer. We have termed this group intermediate atypical carcinoma (IAC),” Dr. Small said.
The remaining quarter of biopsies was composed of mixed populations.
In addition to the independent review, a consensus meeting with two additional pathologists confirmed that this was a new, highly reproducible pathologic subclass, he said.
The researchers next sought to determine whether IAC is phenotypically distinct. A survival analysis was performed based on biopsy pathology and revealed that men who develop IAC have poor survival.
Indeed, survival with IAC (median 11.9 months) tracks with that of SCNC (median 6.6 months) and is distinct from adenocarcinoma, with a log-rank P value of .041, Dr. Small said. Further, when IAC and SCNC were grouped together, there was a dramatically different survival curve (median 8.9 months) than that seen with adenocarcinoma (P = .006).
An analysis using microresected samples indicated that IAC is also genomically distinct, he said. Small cell nuclear clusters showed enrichment of neuronal and cell cycle elements and downregulation of androgen-receptor elements and the immune system.
Based on these findings, machine learning was used to develop a 50-gene signature, with 88.3% accuracy to distinguish small cell from non–small cell histology and 78.5% accuracy to distinguish small cell or IAC histology from adenocarcinoma. The test is not clinically available at this time, but is being used to identify new therapeutic targets.
“We are actively identifying the unique features of this subtype that can be targeted with therapy,” Dr. Small said in an interview. “There is a huge unmet need, since no one knows how to treat these patients, who comprise a significant portion of patients.”
Indeed, in the analysis, IAC represented a fourth of all metastatic castration-resistant biopsies and when combined with small cell neuroendocrine cancer accounted for 40% of all samples.
“This comprises the single largest group of abiraterone- and enzalutamide-refractory patients,” he concluded. “The increasing use of highly potent AR-targeted therapy may contribute to the increasing frequency of this entity, although that is conjecture at this point and certainly ascertainment bias may play a role.”
Discussant Dr. Scott Tomlins, a pathologist from the University of Michigan in Ann Arbor, said one of the study’s major findings is that collecting tissue for comprehensive molecular analysis is feasible in the context of a well-funded, team-based infrastructure, adding that this will likely have to be the way going forward. Despite limited sample numbers, there also appears to be a “strong signal” that gene expression signatures can discriminate various subtypes.
The study was funded by StandUpToCancer, the Prostate Cancer Foundation, and American Association for Cancer Research. Dr. Small reported having no disclosures.
On Twitter @pwendl
AT THE 2015 ASCO ANNUAL MEETING
Key clinical point: Researchers have identified an aggressive new histologic subset of metastatic castration-resistant prostate cancer.
Major finding: Of 124 evaluable biopsies, 35% were pure adenocarcinoma, 13% pure small cell neuroendocrine cancer, and 26% intermediate atypical carcinoma.
Data source: Pathologic and genomic analyses in men with metastatic castration-resistant prostate cancer.
Disclosures: The study was funded by StandUpToCancer, the Prostate Cancer Foundation, and American Association for Cancer Research. Dr. Small reported having no disclosures.
VIDEO: Dr. Walter M. Stadler gives take-home messages from ASCO 2015 GU sessions
CHICAGO – Dr. Walter M. Stadler provides his take on ASCO 2015 presentations and discussions around genitourinary research, including practice-changing results on the use of chemotherapy for treating prostate cancer and the timing of androgen suppression. He also addresses the disappointing results for using precision medicine to treat bladder cancer versus the encouraging results from immunotherapy for both bladder and renal cell cancer. Dr. Stadler is the Fred C. Buffett Professor of Medicine and Surgery; associate dean for clinical research; chief, section of hematology/oncology; and director, genitourinary program, University of Chicago. He had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @nikolaideslaura
CHICAGO – Dr. Walter M. Stadler provides his take on ASCO 2015 presentations and discussions around genitourinary research, including practice-changing results on the use of chemotherapy for treating prostate cancer and the timing of androgen suppression. He also addresses the disappointing results for using precision medicine to treat bladder cancer versus the encouraging results from immunotherapy for both bladder and renal cell cancer. Dr. Stadler is the Fred C. Buffett Professor of Medicine and Surgery; associate dean for clinical research; chief, section of hematology/oncology; and director, genitourinary program, University of Chicago. He had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @nikolaideslaura
CHICAGO – Dr. Walter M. Stadler provides his take on ASCO 2015 presentations and discussions around genitourinary research, including practice-changing results on the use of chemotherapy for treating prostate cancer and the timing of androgen suppression. He also addresses the disappointing results for using precision medicine to treat bladder cancer versus the encouraging results from immunotherapy for both bladder and renal cell cancer. Dr. Stadler is the Fred C. Buffett Professor of Medicine and Surgery; associate dean for clinical research; chief, section of hematology/oncology; and director, genitourinary program, University of Chicago. He had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @nikolaideslaura
AT THE 2015 ASCO ANNUAL MEETING
ASA: Mutation testing aids decision making in thyroid cancer
SAN DIEGO – Routine preoperative use of genetic testing to detect mutations implicated in thyroid carcinogenesis can help guide perioperative decision making, though risks associated with mutations are not always clear-cut.
For individuals with thyroid cancer (TC), the presence of certain mutations was associated with higher risk of early recurrence of cancer as well as distant metastases, according to a recent study presented by Dr. Linwah Yip at the annual meeting of the American Surgical Association. She and her colleagues at the University of Pittsburgh built on their previous work to characterize how thyroid cancer genotype relates both to cancer histology and to disease-related outcomes.
Using data from the electronic medical record of a single institution, Dr. Yip and her colleagues examined data from consecutive patients who had initial surgery for histologically confirmed TC. Of the 1,510 patients in the study cohort, 77% were women, and patients had a mean age of 49 years. All of the cancers in the study were tested for mutations in seven genes known to be associated with thyroid carcinogenesis. Mutation testing was a routine part of preoperative care for thyroid cancer patients, often performed on preoperative fine needle aspiration (FNA) biopsy.
Outcomes tracked in the study, Dr. Yip said, included the type and stage of thyroid cancer identified and whether the cancer recurred.
Mutations were found in 1,039 patients (69%), and no more than one mutation was found in any one tumor. No tumor genotype was specifically associated with tumor size or whether the tumor was multifocal.
Overall, BRAF V600E was the most common mutation associated with TC, and patients with this mutation were the ones most likely to have a recurrence (P = .001). However, Dr. Yip noted that there is phenotypic heterogeneity in how the recurrences present. More distant metastatic disease and lateral lymph node metastases were most likely with RET/PTC1 and three mutations (P = .02).
By contrast, about 25% of thyroid cancers in the study showed mutations in RAS, PAX8/PPARG, or BRAF K601E. These mutations were associated with a more indolent disease course, with more encapsulated tumors and an overall disease-free survival of nearly 100% at 5 years after diagnosis. Dr. Yip said, “However, RAS variations can be associated with any histologic type of thyroid cancer, including anaplastic.”
Dr. Yip said that clinicians should consider conducting perioperative neck ultrasound with lymph node mapping if BRAF V600E or RET/PTC mutations are found. Her recommendation for these patients was a total thyroidectomy, with consideration of a central compartment neck dissection performed prophylactically, in light of the > 50% chance for lymph node involvement. Additionally, surveillance for distant metastases in the form of a chest CT should be considered when tumors are REC/PTC positive.
Study limitations include its retrospective nature and the fact that the treating physicians were not blinded to mutation testing results. Additionally, Dr. Yip noted, in patients with multifocal disease, only the most aggressive tumor was included.
Dr. Chris McHenry of Case Western Reserve University, Cleveland, noted in discussion that disease-specific survival was not related to mutation testing in this study. For patients with advanced thyroid cancer who have limited treatment options, however, mutation testing may help direct specific adjuvant therapies based on risk.
Dr. Nikiforov is a consultant for Quest Diagnostics. The others reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Routine preoperative use of genetic testing to detect mutations implicated in thyroid carcinogenesis can help guide perioperative decision making, though risks associated with mutations are not always clear-cut.
For individuals with thyroid cancer (TC), the presence of certain mutations was associated with higher risk of early recurrence of cancer as well as distant metastases, according to a recent study presented by Dr. Linwah Yip at the annual meeting of the American Surgical Association. She and her colleagues at the University of Pittsburgh built on their previous work to characterize how thyroid cancer genotype relates both to cancer histology and to disease-related outcomes.
Using data from the electronic medical record of a single institution, Dr. Yip and her colleagues examined data from consecutive patients who had initial surgery for histologically confirmed TC. Of the 1,510 patients in the study cohort, 77% were women, and patients had a mean age of 49 years. All of the cancers in the study were tested for mutations in seven genes known to be associated with thyroid carcinogenesis. Mutation testing was a routine part of preoperative care for thyroid cancer patients, often performed on preoperative fine needle aspiration (FNA) biopsy.
Outcomes tracked in the study, Dr. Yip said, included the type and stage of thyroid cancer identified and whether the cancer recurred.
Mutations were found in 1,039 patients (69%), and no more than one mutation was found in any one tumor. No tumor genotype was specifically associated with tumor size or whether the tumor was multifocal.
Overall, BRAF V600E was the most common mutation associated with TC, and patients with this mutation were the ones most likely to have a recurrence (P = .001). However, Dr. Yip noted that there is phenotypic heterogeneity in how the recurrences present. More distant metastatic disease and lateral lymph node metastases were most likely with RET/PTC1 and three mutations (P = .02).
By contrast, about 25% of thyroid cancers in the study showed mutations in RAS, PAX8/PPARG, or BRAF K601E. These mutations were associated with a more indolent disease course, with more encapsulated tumors and an overall disease-free survival of nearly 100% at 5 years after diagnosis. Dr. Yip said, “However, RAS variations can be associated with any histologic type of thyroid cancer, including anaplastic.”
Dr. Yip said that clinicians should consider conducting perioperative neck ultrasound with lymph node mapping if BRAF V600E or RET/PTC mutations are found. Her recommendation for these patients was a total thyroidectomy, with consideration of a central compartment neck dissection performed prophylactically, in light of the > 50% chance for lymph node involvement. Additionally, surveillance for distant metastases in the form of a chest CT should be considered when tumors are REC/PTC positive.
Study limitations include its retrospective nature and the fact that the treating physicians were not blinded to mutation testing results. Additionally, Dr. Yip noted, in patients with multifocal disease, only the most aggressive tumor was included.
Dr. Chris McHenry of Case Western Reserve University, Cleveland, noted in discussion that disease-specific survival was not related to mutation testing in this study. For patients with advanced thyroid cancer who have limited treatment options, however, mutation testing may help direct specific adjuvant therapies based on risk.
Dr. Nikiforov is a consultant for Quest Diagnostics. The others reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – Routine preoperative use of genetic testing to detect mutations implicated in thyroid carcinogenesis can help guide perioperative decision making, though risks associated with mutations are not always clear-cut.
For individuals with thyroid cancer (TC), the presence of certain mutations was associated with higher risk of early recurrence of cancer as well as distant metastases, according to a recent study presented by Dr. Linwah Yip at the annual meeting of the American Surgical Association. She and her colleagues at the University of Pittsburgh built on their previous work to characterize how thyroid cancer genotype relates both to cancer histology and to disease-related outcomes.
Using data from the electronic medical record of a single institution, Dr. Yip and her colleagues examined data from consecutive patients who had initial surgery for histologically confirmed TC. Of the 1,510 patients in the study cohort, 77% were women, and patients had a mean age of 49 years. All of the cancers in the study were tested for mutations in seven genes known to be associated with thyroid carcinogenesis. Mutation testing was a routine part of preoperative care for thyroid cancer patients, often performed on preoperative fine needle aspiration (FNA) biopsy.
Outcomes tracked in the study, Dr. Yip said, included the type and stage of thyroid cancer identified and whether the cancer recurred.
Mutations were found in 1,039 patients (69%), and no more than one mutation was found in any one tumor. No tumor genotype was specifically associated with tumor size or whether the tumor was multifocal.
Overall, BRAF V600E was the most common mutation associated with TC, and patients with this mutation were the ones most likely to have a recurrence (P = .001). However, Dr. Yip noted that there is phenotypic heterogeneity in how the recurrences present. More distant metastatic disease and lateral lymph node metastases were most likely with RET/PTC1 and three mutations (P = .02).
By contrast, about 25% of thyroid cancers in the study showed mutations in RAS, PAX8/PPARG, or BRAF K601E. These mutations were associated with a more indolent disease course, with more encapsulated tumors and an overall disease-free survival of nearly 100% at 5 years after diagnosis. Dr. Yip said, “However, RAS variations can be associated with any histologic type of thyroid cancer, including anaplastic.”
Dr. Yip said that clinicians should consider conducting perioperative neck ultrasound with lymph node mapping if BRAF V600E or RET/PTC mutations are found. Her recommendation for these patients was a total thyroidectomy, with consideration of a central compartment neck dissection performed prophylactically, in light of the > 50% chance for lymph node involvement. Additionally, surveillance for distant metastases in the form of a chest CT should be considered when tumors are REC/PTC positive.
Study limitations include its retrospective nature and the fact that the treating physicians were not blinded to mutation testing results. Additionally, Dr. Yip noted, in patients with multifocal disease, only the most aggressive tumor was included.
Dr. Chris McHenry of Case Western Reserve University, Cleveland, noted in discussion that disease-specific survival was not related to mutation testing in this study. For patients with advanced thyroid cancer who have limited treatment options, however, mutation testing may help direct specific adjuvant therapies based on risk.
Dr. Nikiforov is a consultant for Quest Diagnostics. The others reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Genetic testing in those with thyroid cancer may aid perioperative decision making.
Major finding: Distant metastases were more common in thyroid cancer patients who were positive for the RET/PTC mutation (P = .02), while thyroid cancer expressing BRAF V600E or RET/PTC was associated with higher-grade cancer on presentation (P < .001) and early recurrence (P < .001).
Data source: Retrospective review of a consecutive series of 1,510 patients with thyroidectomy for thyroid cancer and testing for thyroid cancer-specific genetic alterations.
Disclosures: One of the researchers is a consultant for Quest Diagnostics. The others reported no disclosures.
AACE: How to safely skip radioactive iodine for low-grade thyroid cancer
NASHVILLE, TENN. – Patients with stage I or II differentiated thyroid cancers do not need radioactive iodine treatment if their nonsuppressed thyroglobulin level is less than 2 ng/mL 2 weeks after surgery, according to Dr. Kathleen Hands.
When that’s the case, “I know the patient had an excellent surgery and will have an excellent prognosis with an extremely low likelihood of recurrence over the next 10 years without radioactive iodine. These patients can be managed safely and effectively without radioactive iodine in a community setting,” said Dr. Hands, a thyroidologist who practices in San Antonio.
It’s common for patients in the United States to receive iodine-131 (I-131) after surgery for low-risk thyroid cancers “despite the abundance of evidence” showing that it does them no good and may cause harm and despite guidelines calling for conservative use of I-131, she said (World. J. Surg. 2002;26:879-85).
“It’s a habit,” a holdover from decades ago “when we didn’t actually have good surgical technique. We need to [heed recent data] and step away from what we did in the 60s, 70s, and 80s and get into the 21st century. We should stop using radioactive iodine in these low-risk patients,” Dr. Hands said at the American Association of Clinical Endocrinologists annual meeting.
Among radioactive iodine’s drawbacks are its expense and sometimes salivary and lacrimal problems associated with its use. Earlier in her career, “I personally had two of my cases” – 19 and 22 years old – “develop acute myelogenous leukemia [shortly] after I-131, one of whom succumbed. I took that very seriously. I’ve become very conservative in the use of this drug. Ablation should be restricted to patients with incomplete surgical excision or poor prognostic factors for recurrence or death,” she said.
This advice is backed up by findings from her review of 378 patients who underwent surgery for differentiated thyroid cancer, with MACIS (metastasis, age, completeness of resection, invasion, and size) scores below 7, meaning low-intermediate-risk disease. Patients ranged from 18 to 79 years old. The majority were women, and about a third had multifocal disease. Tumor sizes ranged from 0.8 mm to 4.0 cm. Twenty-one patients under 45 years old had lymph node metastases of less than 5 mm.
The patients had nonsuppressed thyroglobulin levels below 2 ng/mL 2 weeks after surgery. They opted against I-131, and were started on levothyroxine. There’s been no recurrence of disease in the group after 8 years’ follow-up; thyroglobulin was undetectable in 72% by 2 years. Those in whom thyroglobulin remained detectable had thyroglobulin velocities below 10% over a period of 5 years.
“Nonsuppressed thyroglobulin” means that the patients were not put on thyroxine right after surgery, so that Dr. Hands could get an idea if any tumor was left 2 weeks later. They also weren’t put on low-iodine diets in the interim, she said, because she had no intention of giving them I-131.
To get the most out of the approach, patients need excellent and complete surgeries. That means that endocrinologists should learn to perform preoperative neck ultrasounds – or refer to someone who can – to give surgeons a heads-up about tumor location, size, shape, and invasiveness, as well as lymph node involvement, calcifications, and other issues. “This is the kind of information your surgeon needs” to do a good job, Dr. Hands said.
She said she doesn’t worry about hypothyroidism when patients don’t get thyroxine right after surgery. Manipulation of the thyroid during surgery releases hormone into the system, and “I think that tides them over; It’s a long-acting hormone. Patients tolerate not having replacement immediately [after surgery],” Dr. Hands said.
There was no funding for the project, and Dr. Hands said she had no relevant financial disclosures.
NASHVILLE, TENN. – Patients with stage I or II differentiated thyroid cancers do not need radioactive iodine treatment if their nonsuppressed thyroglobulin level is less than 2 ng/mL 2 weeks after surgery, according to Dr. Kathleen Hands.
When that’s the case, “I know the patient had an excellent surgery and will have an excellent prognosis with an extremely low likelihood of recurrence over the next 10 years without radioactive iodine. These patients can be managed safely and effectively without radioactive iodine in a community setting,” said Dr. Hands, a thyroidologist who practices in San Antonio.
It’s common for patients in the United States to receive iodine-131 (I-131) after surgery for low-risk thyroid cancers “despite the abundance of evidence” showing that it does them no good and may cause harm and despite guidelines calling for conservative use of I-131, she said (World. J. Surg. 2002;26:879-85).
“It’s a habit,” a holdover from decades ago “when we didn’t actually have good surgical technique. We need to [heed recent data] and step away from what we did in the 60s, 70s, and 80s and get into the 21st century. We should stop using radioactive iodine in these low-risk patients,” Dr. Hands said at the American Association of Clinical Endocrinologists annual meeting.
Among radioactive iodine’s drawbacks are its expense and sometimes salivary and lacrimal problems associated with its use. Earlier in her career, “I personally had two of my cases” – 19 and 22 years old – “develop acute myelogenous leukemia [shortly] after I-131, one of whom succumbed. I took that very seriously. I’ve become very conservative in the use of this drug. Ablation should be restricted to patients with incomplete surgical excision or poor prognostic factors for recurrence or death,” she said.
This advice is backed up by findings from her review of 378 patients who underwent surgery for differentiated thyroid cancer, with MACIS (metastasis, age, completeness of resection, invasion, and size) scores below 7, meaning low-intermediate-risk disease. Patients ranged from 18 to 79 years old. The majority were women, and about a third had multifocal disease. Tumor sizes ranged from 0.8 mm to 4.0 cm. Twenty-one patients under 45 years old had lymph node metastases of less than 5 mm.
The patients had nonsuppressed thyroglobulin levels below 2 ng/mL 2 weeks after surgery. They opted against I-131, and were started on levothyroxine. There’s been no recurrence of disease in the group after 8 years’ follow-up; thyroglobulin was undetectable in 72% by 2 years. Those in whom thyroglobulin remained detectable had thyroglobulin velocities below 10% over a period of 5 years.
“Nonsuppressed thyroglobulin” means that the patients were not put on thyroxine right after surgery, so that Dr. Hands could get an idea if any tumor was left 2 weeks later. They also weren’t put on low-iodine diets in the interim, she said, because she had no intention of giving them I-131.
To get the most out of the approach, patients need excellent and complete surgeries. That means that endocrinologists should learn to perform preoperative neck ultrasounds – or refer to someone who can – to give surgeons a heads-up about tumor location, size, shape, and invasiveness, as well as lymph node involvement, calcifications, and other issues. “This is the kind of information your surgeon needs” to do a good job, Dr. Hands said.
She said she doesn’t worry about hypothyroidism when patients don’t get thyroxine right after surgery. Manipulation of the thyroid during surgery releases hormone into the system, and “I think that tides them over; It’s a long-acting hormone. Patients tolerate not having replacement immediately [after surgery],” Dr. Hands said.
There was no funding for the project, and Dr. Hands said she had no relevant financial disclosures.
NASHVILLE, TENN. – Patients with stage I or II differentiated thyroid cancers do not need radioactive iodine treatment if their nonsuppressed thyroglobulin level is less than 2 ng/mL 2 weeks after surgery, according to Dr. Kathleen Hands.
When that’s the case, “I know the patient had an excellent surgery and will have an excellent prognosis with an extremely low likelihood of recurrence over the next 10 years without radioactive iodine. These patients can be managed safely and effectively without radioactive iodine in a community setting,” said Dr. Hands, a thyroidologist who practices in San Antonio.
It’s common for patients in the United States to receive iodine-131 (I-131) after surgery for low-risk thyroid cancers “despite the abundance of evidence” showing that it does them no good and may cause harm and despite guidelines calling for conservative use of I-131, she said (World. J. Surg. 2002;26:879-85).
“It’s a habit,” a holdover from decades ago “when we didn’t actually have good surgical technique. We need to [heed recent data] and step away from what we did in the 60s, 70s, and 80s and get into the 21st century. We should stop using radioactive iodine in these low-risk patients,” Dr. Hands said at the American Association of Clinical Endocrinologists annual meeting.
Among radioactive iodine’s drawbacks are its expense and sometimes salivary and lacrimal problems associated with its use. Earlier in her career, “I personally had two of my cases” – 19 and 22 years old – “develop acute myelogenous leukemia [shortly] after I-131, one of whom succumbed. I took that very seriously. I’ve become very conservative in the use of this drug. Ablation should be restricted to patients with incomplete surgical excision or poor prognostic factors for recurrence or death,” she said.
This advice is backed up by findings from her review of 378 patients who underwent surgery for differentiated thyroid cancer, with MACIS (metastasis, age, completeness of resection, invasion, and size) scores below 7, meaning low-intermediate-risk disease. Patients ranged from 18 to 79 years old. The majority were women, and about a third had multifocal disease. Tumor sizes ranged from 0.8 mm to 4.0 cm. Twenty-one patients under 45 years old had lymph node metastases of less than 5 mm.
The patients had nonsuppressed thyroglobulin levels below 2 ng/mL 2 weeks after surgery. They opted against I-131, and were started on levothyroxine. There’s been no recurrence of disease in the group after 8 years’ follow-up; thyroglobulin was undetectable in 72% by 2 years. Those in whom thyroglobulin remained detectable had thyroglobulin velocities below 10% over a period of 5 years.
“Nonsuppressed thyroglobulin” means that the patients were not put on thyroxine right after surgery, so that Dr. Hands could get an idea if any tumor was left 2 weeks later. They also weren’t put on low-iodine diets in the interim, she said, because she had no intention of giving them I-131.
To get the most out of the approach, patients need excellent and complete surgeries. That means that endocrinologists should learn to perform preoperative neck ultrasounds – or refer to someone who can – to give surgeons a heads-up about tumor location, size, shape, and invasiveness, as well as lymph node involvement, calcifications, and other issues. “This is the kind of information your surgeon needs” to do a good job, Dr. Hands said.
She said she doesn’t worry about hypothyroidism when patients don’t get thyroxine right after surgery. Manipulation of the thyroid during surgery releases hormone into the system, and “I think that tides them over; It’s a long-acting hormone. Patients tolerate not having replacement immediately [after surgery],” Dr. Hands said.
There was no funding for the project, and Dr. Hands said she had no relevant financial disclosures.
AT AACE 2015
Key clinical point: Thyroid cancer patients do not need radioactive iodine treatment if their nonsuppressed thyroglobulin is less than 2 ng/mL 2 weeks after surgery.
Major finding: Among 378 patients whose nonsuppressed thyroglobulin levels were below 2 ng/mL 2 weeks after removal of low-risk differentiated thyroid cancers, there were zero recurrences over 8 years of follow-up.
Data source: A single-center, retrospective study.
Disclosures: The investigator said she had no relevant financial disclosures and no outside funding.
ASCO: Precision medicine initiatives take wing
CHICAGO – It’s getting very personal in oncology, and that’s a very good thing.
At the annual meeting of the American Society of Clinical Oncology, major cancer organizations announced new precision medicine initiatives that will attempt to match patients who have advanced cancers with the best available therapies based not on the location or histologic subtypes of their tumors, but on specific molecular abnormalities.
The National Cancer Institute’s Molecular Analysis for Therapy Choice (NCI-MATCH) trial will begin enrolling patients in July 2015. The study’s objective is “to understand the relative efficacy of the same therapy applied to oncogene-defined subsets across the entire cancer population as defined by site of origin or tumor histology,” said co–principal investigator Dr. Keith T. Flaherty of Harvard Medical School, Boston.
“This is the beginning, not the end, in terms of how we think about applying these therapies,” he said at a briefing that was held to announce the start of trial enrollment and a second initiative – the Targeted Agent and Profiling Utilization Registry (TAPUR) Study – by ASCO in cooperation with major pharmaceutical companies.
NCI-MATCH
NCI-MATCH is a phase II trial that will be operated through the National Clinical Trials Network. Oncologists at participating centers throughout the United States can enroll patients aged 18 years and older who have solid tumors or lymphomas that have relapsed or are refractory to conventional therapy, or who have a type of cancer for which no effective, consensus-based therapy is available.
Investigators plan to screen 3,000 patients initially, with the goal of enrolling 1,000 patients distributed among several substudies that will be evaluating specific drugs against specific molecular targets.
Patients will undergo biopsy at study entry, and their tumors will be subjected to genomic analysis to detect specific, targetable molecular abnormalities.
If a patient has a specific abnormality that is being explored in a current substudy, that patient will be further evaluated to determine whether he or she meets the eligibility criteria for that trial arm. Once enrolled, patients can remain on therapy until disease progression. The therapies will include both currently marketed agents and investigational therapies contributed by drug companies. Most of the trial arms will explore monotherapy with a targeted agent, but a few may investigate combinations which have accumulated enough safety and efficacy data to suggest that they might work against a specific molecular target.
The primary endpoint will be overall response rate, with a secondary endpoint of 6-month progression-free survival (PFS).
“This holds promise to bring faster cures to millions of Americans who so desperately need them,” ASCO past president Dr. Clifford A. Hudis said at the briefing.
TAPUR Trial
In cooperation with major pharmaceutical manufacturers (currently five, with more expected to sign on), ASCO has initiated a study designed to help answer the question, “I’ve got the tumor genome – now what do I do with it?”
The goal of the TAPUR trial, says ASCO Chief Medical Officer Dr. Richard Schilsky, is “to learn from the real world practice of prescribing targeted therapies to patients with advanced cancer whose tumor harbors a genomic variant known to be a drug target.”
The primary objectives are to describe the antitumor activity and toxicity profiles of targeted therapies, and to help patients get access to Food and Drug Administration–approved agents from which they may be able to benefit.
The trial will enroll patients with advanced solid tumors, B-cell non-Hodgkin’s lymphomas, and multiple myelomas for which there are no standard therapies. The patients must have adequate organ function and good performance status (0-2).
Patients will be matched by their personal physicians to specific therapies, if such a match exists; otherwise, they will be treated at the physician’s discretion.
The primary endpoint of the study will be overall response rates by Response Evaluation Criteria in Solid Tumors (RECIST). Secondary endpoints will be PFS, OS, time on treatment, grade 3 or greater adverse events, and serious adverse event. The investigators plan to begin patient enrollment in the fourth quarter of 2015.
Current industry partners include AstraZeneca, Bristol Myers Squibb, Eli Lilly, Genentech, and Pfizer.
The NCI-MATCH study is funded by the National Institutes of Health. Dr. Flaherty has received NIH research grants. Dr. Hudis disclosed ties to AstraZeneca, Sanofi-Aventis, Amgen, Bristol-Myers Squibb, Genentech, Eli Lilly, Novartis, Ortho Biotech, Pfizer, and Roche. Dr. Schilsky disclosed no relevant conflicts of interest.
CHICAGO – It’s getting very personal in oncology, and that’s a very good thing.
At the annual meeting of the American Society of Clinical Oncology, major cancer organizations announced new precision medicine initiatives that will attempt to match patients who have advanced cancers with the best available therapies based not on the location or histologic subtypes of their tumors, but on specific molecular abnormalities.
The National Cancer Institute’s Molecular Analysis for Therapy Choice (NCI-MATCH) trial will begin enrolling patients in July 2015. The study’s objective is “to understand the relative efficacy of the same therapy applied to oncogene-defined subsets across the entire cancer population as defined by site of origin or tumor histology,” said co–principal investigator Dr. Keith T. Flaherty of Harvard Medical School, Boston.
“This is the beginning, not the end, in terms of how we think about applying these therapies,” he said at a briefing that was held to announce the start of trial enrollment and a second initiative – the Targeted Agent and Profiling Utilization Registry (TAPUR) Study – by ASCO in cooperation with major pharmaceutical companies.
NCI-MATCH
NCI-MATCH is a phase II trial that will be operated through the National Clinical Trials Network. Oncologists at participating centers throughout the United States can enroll patients aged 18 years and older who have solid tumors or lymphomas that have relapsed or are refractory to conventional therapy, or who have a type of cancer for which no effective, consensus-based therapy is available.
Investigators plan to screen 3,000 patients initially, with the goal of enrolling 1,000 patients distributed among several substudies that will be evaluating specific drugs against specific molecular targets.
Patients will undergo biopsy at study entry, and their tumors will be subjected to genomic analysis to detect specific, targetable molecular abnormalities.
If a patient has a specific abnormality that is being explored in a current substudy, that patient will be further evaluated to determine whether he or she meets the eligibility criteria for that trial arm. Once enrolled, patients can remain on therapy until disease progression. The therapies will include both currently marketed agents and investigational therapies contributed by drug companies. Most of the trial arms will explore monotherapy with a targeted agent, but a few may investigate combinations which have accumulated enough safety and efficacy data to suggest that they might work against a specific molecular target.
The primary endpoint will be overall response rate, with a secondary endpoint of 6-month progression-free survival (PFS).
“This holds promise to bring faster cures to millions of Americans who so desperately need them,” ASCO past president Dr. Clifford A. Hudis said at the briefing.
TAPUR Trial
In cooperation with major pharmaceutical manufacturers (currently five, with more expected to sign on), ASCO has initiated a study designed to help answer the question, “I’ve got the tumor genome – now what do I do with it?”
The goal of the TAPUR trial, says ASCO Chief Medical Officer Dr. Richard Schilsky, is “to learn from the real world practice of prescribing targeted therapies to patients with advanced cancer whose tumor harbors a genomic variant known to be a drug target.”
The primary objectives are to describe the antitumor activity and toxicity profiles of targeted therapies, and to help patients get access to Food and Drug Administration–approved agents from which they may be able to benefit.
The trial will enroll patients with advanced solid tumors, B-cell non-Hodgkin’s lymphomas, and multiple myelomas for which there are no standard therapies. The patients must have adequate organ function and good performance status (0-2).
Patients will be matched by their personal physicians to specific therapies, if such a match exists; otherwise, they will be treated at the physician’s discretion.
The primary endpoint of the study will be overall response rates by Response Evaluation Criteria in Solid Tumors (RECIST). Secondary endpoints will be PFS, OS, time on treatment, grade 3 or greater adverse events, and serious adverse event. The investigators plan to begin patient enrollment in the fourth quarter of 2015.
Current industry partners include AstraZeneca, Bristol Myers Squibb, Eli Lilly, Genentech, and Pfizer.
The NCI-MATCH study is funded by the National Institutes of Health. Dr. Flaherty has received NIH research grants. Dr. Hudis disclosed ties to AstraZeneca, Sanofi-Aventis, Amgen, Bristol-Myers Squibb, Genentech, Eli Lilly, Novartis, Ortho Biotech, Pfizer, and Roche. Dr. Schilsky disclosed no relevant conflicts of interest.
CHICAGO – It’s getting very personal in oncology, and that’s a very good thing.
At the annual meeting of the American Society of Clinical Oncology, major cancer organizations announced new precision medicine initiatives that will attempt to match patients who have advanced cancers with the best available therapies based not on the location or histologic subtypes of their tumors, but on specific molecular abnormalities.
The National Cancer Institute’s Molecular Analysis for Therapy Choice (NCI-MATCH) trial will begin enrolling patients in July 2015. The study’s objective is “to understand the relative efficacy of the same therapy applied to oncogene-defined subsets across the entire cancer population as defined by site of origin or tumor histology,” said co–principal investigator Dr. Keith T. Flaherty of Harvard Medical School, Boston.
“This is the beginning, not the end, in terms of how we think about applying these therapies,” he said at a briefing that was held to announce the start of trial enrollment and a second initiative – the Targeted Agent and Profiling Utilization Registry (TAPUR) Study – by ASCO in cooperation with major pharmaceutical companies.
NCI-MATCH
NCI-MATCH is a phase II trial that will be operated through the National Clinical Trials Network. Oncologists at participating centers throughout the United States can enroll patients aged 18 years and older who have solid tumors or lymphomas that have relapsed or are refractory to conventional therapy, or who have a type of cancer for which no effective, consensus-based therapy is available.
Investigators plan to screen 3,000 patients initially, with the goal of enrolling 1,000 patients distributed among several substudies that will be evaluating specific drugs against specific molecular targets.
Patients will undergo biopsy at study entry, and their tumors will be subjected to genomic analysis to detect specific, targetable molecular abnormalities.
If a patient has a specific abnormality that is being explored in a current substudy, that patient will be further evaluated to determine whether he or she meets the eligibility criteria for that trial arm. Once enrolled, patients can remain on therapy until disease progression. The therapies will include both currently marketed agents and investigational therapies contributed by drug companies. Most of the trial arms will explore monotherapy with a targeted agent, but a few may investigate combinations which have accumulated enough safety and efficacy data to suggest that they might work against a specific molecular target.
The primary endpoint will be overall response rate, with a secondary endpoint of 6-month progression-free survival (PFS).
“This holds promise to bring faster cures to millions of Americans who so desperately need them,” ASCO past president Dr. Clifford A. Hudis said at the briefing.
TAPUR Trial
In cooperation with major pharmaceutical manufacturers (currently five, with more expected to sign on), ASCO has initiated a study designed to help answer the question, “I’ve got the tumor genome – now what do I do with it?”
The goal of the TAPUR trial, says ASCO Chief Medical Officer Dr. Richard Schilsky, is “to learn from the real world practice of prescribing targeted therapies to patients with advanced cancer whose tumor harbors a genomic variant known to be a drug target.”
The primary objectives are to describe the antitumor activity and toxicity profiles of targeted therapies, and to help patients get access to Food and Drug Administration–approved agents from which they may be able to benefit.
The trial will enroll patients with advanced solid tumors, B-cell non-Hodgkin’s lymphomas, and multiple myelomas for which there are no standard therapies. The patients must have adequate organ function and good performance status (0-2).
Patients will be matched by their personal physicians to specific therapies, if such a match exists; otherwise, they will be treated at the physician’s discretion.
The primary endpoint of the study will be overall response rates by Response Evaluation Criteria in Solid Tumors (RECIST). Secondary endpoints will be PFS, OS, time on treatment, grade 3 or greater adverse events, and serious adverse event. The investigators plan to begin patient enrollment in the fourth quarter of 2015.
Current industry partners include AstraZeneca, Bristol Myers Squibb, Eli Lilly, Genentech, and Pfizer.
The NCI-MATCH study is funded by the National Institutes of Health. Dr. Flaherty has received NIH research grants. Dr. Hudis disclosed ties to AstraZeneca, Sanofi-Aventis, Amgen, Bristol-Myers Squibb, Genentech, Eli Lilly, Novartis, Ortho Biotech, Pfizer, and Roche. Dr. Schilsky disclosed no relevant conflicts of interest.
AT THE 2015 ASCO ANNUAL MEETING