User login
Official Newspaper of the American College of Surgeons
VIDEO: More routine use of unilateral thyroidectomy advocated for papillary thyroid microcarcinoma
BOSTON – A study of over 60 years of patient data from the Mayo Clinic suggests a reconsideration of the routine use of unilateral thyroid lobectomy (UL) as the initial treatment for papillary thyroid microcarcinoma.
“Papillary thyroid microcarcinoma [PTM] patients have a normal life expectancy and typically are cured by adequate tumor resection. More than 99% of PTM patients are not at risk of either distant spread or mortality from cancer,” said Dr. Ian D. Hay of the Mayo Clinic, Rochester, Minn. Unilateral thyroid lobectomy is one treatment option for papillary thyroid microcarcinoma along with conventional bilateral nodal resection approaches of near-total thyroidectomy (NT) or total thyroidectomy (TT), or selective radioactive iodine remnant ablation (RRA).
Awareness of PTM is not new; examination of thyroid glands at autopsy going back decades has revealed their presence in 6%-36% of samples. A more recent development is the use of high-resolution ultrasound-guided biopsies of papillary thyroid carcinoma (PTC) lesions as small as 3 cm. For example, at the Mayo Clinic the diagnosis of PTM was about one annually from 1935 to 1944, while from 2005 to 2014 the average was close to one per day. “At Mayo, 34% of PTCs seen since 1995 are PTMs,” Dr. Hay said at the annual meeting of the Endocrine Society.
The best initial management of PTMs is disputed, with observation favored by some, TT and RRA favored by others, and ethanol ablation having been found to be effective by institutions including the Mayo Clinic. UL has been deemphasized, despite the 2015 American Thyroid Association Guidelines recommendation of UL as the usual surgical procedure for adults with PTM.
Dr. Hay and his colleagues sought to provide some clarity to the issue by taking advantage of the institute’s database of adult (18+ years) PTM patients who were consecutively treated from 1935 to 2014. The decades of data allowed a long-term look at patient outcomes. They examined data from 1,345 patients, 954 women and 391 men with a median age at surgery of 48 years. The mean follow-up was 15.4 years, representing almost 21,000 patient years. Data on tumor recurrence and cause-specific mortality were derived from a data base of over 4,300 PTC patients representing over 66,000 patient-years of observation.
Median tumor size was 7 mm (range, 0.08-1.0 cm). Extrathyroid invasion was evident in 18 (1.3%) cases and 298 tumors (26%) were multifocal. There were 399 (30%) node-positive tumors at diagnosis and 4 (0.3%) cases featuring initial distant metastases.
The mean MACIS (metastasis, age at presentation, completeness of surgical resection, invasion [extrathyroidal], size) score was 4.25 with little variation in score over time. Almost all (96%) patients had a MACIS score of under 6. Bilateral lobar resection was done in 1,132 (95%) patients, with NT or TT comprising 80% of the cases. UL was done in only 202 (15%) cases. The use of TT skyrocketed from 3% of the cases done in the first 2 decades to 40% in the last 2 decades. Regional nodes were removed at surgery in 743 (55%) cases, either by “node picking” (23%) or compartmental dissection (32%).
Overall survival following surgery in PTM patients was similar to age- and gender-matched controls (397 deaths observed, 431 deaths expected; P = .16). Only four (0.3%) patients died of PTM. The rates of locoregional recurrence were similar for the unilateral and bilateral approaches (P = .90). In 1,148 patients with potentially curable PTM, defined as the absence of metastasis at diagnosis and no gross residual disease, the rates of tumor recurrence 10, 20, and 40 years after surgery were 6%, 7%, and 10%, respectively. In these 1,148 patients, the 30-year locoregional recurrence rates after UL alone were similar to those seen after NT or TT followed by RRA (P = .99).
UL did not result in permanent unilateral vocal cord paresis or permanent hypoparathyroidism. These adversities were more likely to develop following bilateral lobectomy.
“Since [UL] produces comparable recurrence results when compared to bilateral surgery and is not associated with either cord paresis or hypoparathyroidism, then perhaps it is overdue for institutions like Mayo to individualize our treatment policies and more often employ UL when surgery, and not observation or ultrasound-guided percutaneous ethanol ablation, is chosen to treat PTM,” said Dr. Hay.
Dr. Hay was adamant on the overuse of ultrasound in the detection of small-diameter carcinomas in the decision for bilateral surgery. “It’s embarrassing how much we are wasting resources and doing too much ultrasound too often,” he said in an interview.
Dr. Hay had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – A study of over 60 years of patient data from the Mayo Clinic suggests a reconsideration of the routine use of unilateral thyroid lobectomy (UL) as the initial treatment for papillary thyroid microcarcinoma.
“Papillary thyroid microcarcinoma [PTM] patients have a normal life expectancy and typically are cured by adequate tumor resection. More than 99% of PTM patients are not at risk of either distant spread or mortality from cancer,” said Dr. Ian D. Hay of the Mayo Clinic, Rochester, Minn. Unilateral thyroid lobectomy is one treatment option for papillary thyroid microcarcinoma along with conventional bilateral nodal resection approaches of near-total thyroidectomy (NT) or total thyroidectomy (TT), or selective radioactive iodine remnant ablation (RRA).
Awareness of PTM is not new; examination of thyroid glands at autopsy going back decades has revealed their presence in 6%-36% of samples. A more recent development is the use of high-resolution ultrasound-guided biopsies of papillary thyroid carcinoma (PTC) lesions as small as 3 cm. For example, at the Mayo Clinic the diagnosis of PTM was about one annually from 1935 to 1944, while from 2005 to 2014 the average was close to one per day. “At Mayo, 34% of PTCs seen since 1995 are PTMs,” Dr. Hay said at the annual meeting of the Endocrine Society.
The best initial management of PTMs is disputed, with observation favored by some, TT and RRA favored by others, and ethanol ablation having been found to be effective by institutions including the Mayo Clinic. UL has been deemphasized, despite the 2015 American Thyroid Association Guidelines recommendation of UL as the usual surgical procedure for adults with PTM.
Dr. Hay and his colleagues sought to provide some clarity to the issue by taking advantage of the institute’s database of adult (18+ years) PTM patients who were consecutively treated from 1935 to 2014. The decades of data allowed a long-term look at patient outcomes. They examined data from 1,345 patients, 954 women and 391 men with a median age at surgery of 48 years. The mean follow-up was 15.4 years, representing almost 21,000 patient years. Data on tumor recurrence and cause-specific mortality were derived from a data base of over 4,300 PTC patients representing over 66,000 patient-years of observation.
Median tumor size was 7 mm (range, 0.08-1.0 cm). Extrathyroid invasion was evident in 18 (1.3%) cases and 298 tumors (26%) were multifocal. There were 399 (30%) node-positive tumors at diagnosis and 4 (0.3%) cases featuring initial distant metastases.
The mean MACIS (metastasis, age at presentation, completeness of surgical resection, invasion [extrathyroidal], size) score was 4.25 with little variation in score over time. Almost all (96%) patients had a MACIS score of under 6. Bilateral lobar resection was done in 1,132 (95%) patients, with NT or TT comprising 80% of the cases. UL was done in only 202 (15%) cases. The use of TT skyrocketed from 3% of the cases done in the first 2 decades to 40% in the last 2 decades. Regional nodes were removed at surgery in 743 (55%) cases, either by “node picking” (23%) or compartmental dissection (32%).
Overall survival following surgery in PTM patients was similar to age- and gender-matched controls (397 deaths observed, 431 deaths expected; P = .16). Only four (0.3%) patients died of PTM. The rates of locoregional recurrence were similar for the unilateral and bilateral approaches (P = .90). In 1,148 patients with potentially curable PTM, defined as the absence of metastasis at diagnosis and no gross residual disease, the rates of tumor recurrence 10, 20, and 40 years after surgery were 6%, 7%, and 10%, respectively. In these 1,148 patients, the 30-year locoregional recurrence rates after UL alone were similar to those seen after NT or TT followed by RRA (P = .99).
UL did not result in permanent unilateral vocal cord paresis or permanent hypoparathyroidism. These adversities were more likely to develop following bilateral lobectomy.
“Since [UL] produces comparable recurrence results when compared to bilateral surgery and is not associated with either cord paresis or hypoparathyroidism, then perhaps it is overdue for institutions like Mayo to individualize our treatment policies and more often employ UL when surgery, and not observation or ultrasound-guided percutaneous ethanol ablation, is chosen to treat PTM,” said Dr. Hay.
Dr. Hay was adamant on the overuse of ultrasound in the detection of small-diameter carcinomas in the decision for bilateral surgery. “It’s embarrassing how much we are wasting resources and doing too much ultrasound too often,” he said in an interview.
Dr. Hay had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – A study of over 60 years of patient data from the Mayo Clinic suggests a reconsideration of the routine use of unilateral thyroid lobectomy (UL) as the initial treatment for papillary thyroid microcarcinoma.
“Papillary thyroid microcarcinoma [PTM] patients have a normal life expectancy and typically are cured by adequate tumor resection. More than 99% of PTM patients are not at risk of either distant spread or mortality from cancer,” said Dr. Ian D. Hay of the Mayo Clinic, Rochester, Minn. Unilateral thyroid lobectomy is one treatment option for papillary thyroid microcarcinoma along with conventional bilateral nodal resection approaches of near-total thyroidectomy (NT) or total thyroidectomy (TT), or selective radioactive iodine remnant ablation (RRA).
Awareness of PTM is not new; examination of thyroid glands at autopsy going back decades has revealed their presence in 6%-36% of samples. A more recent development is the use of high-resolution ultrasound-guided biopsies of papillary thyroid carcinoma (PTC) lesions as small as 3 cm. For example, at the Mayo Clinic the diagnosis of PTM was about one annually from 1935 to 1944, while from 2005 to 2014 the average was close to one per day. “At Mayo, 34% of PTCs seen since 1995 are PTMs,” Dr. Hay said at the annual meeting of the Endocrine Society.
The best initial management of PTMs is disputed, with observation favored by some, TT and RRA favored by others, and ethanol ablation having been found to be effective by institutions including the Mayo Clinic. UL has been deemphasized, despite the 2015 American Thyroid Association Guidelines recommendation of UL as the usual surgical procedure for adults with PTM.
Dr. Hay and his colleagues sought to provide some clarity to the issue by taking advantage of the institute’s database of adult (18+ years) PTM patients who were consecutively treated from 1935 to 2014. The decades of data allowed a long-term look at patient outcomes. They examined data from 1,345 patients, 954 women and 391 men with a median age at surgery of 48 years. The mean follow-up was 15.4 years, representing almost 21,000 patient years. Data on tumor recurrence and cause-specific mortality were derived from a data base of over 4,300 PTC patients representing over 66,000 patient-years of observation.
Median tumor size was 7 mm (range, 0.08-1.0 cm). Extrathyroid invasion was evident in 18 (1.3%) cases and 298 tumors (26%) were multifocal. There were 399 (30%) node-positive tumors at diagnosis and 4 (0.3%) cases featuring initial distant metastases.
The mean MACIS (metastasis, age at presentation, completeness of surgical resection, invasion [extrathyroidal], size) score was 4.25 with little variation in score over time. Almost all (96%) patients had a MACIS score of under 6. Bilateral lobar resection was done in 1,132 (95%) patients, with NT or TT comprising 80% of the cases. UL was done in only 202 (15%) cases. The use of TT skyrocketed from 3% of the cases done in the first 2 decades to 40% in the last 2 decades. Regional nodes were removed at surgery in 743 (55%) cases, either by “node picking” (23%) or compartmental dissection (32%).
Overall survival following surgery in PTM patients was similar to age- and gender-matched controls (397 deaths observed, 431 deaths expected; P = .16). Only four (0.3%) patients died of PTM. The rates of locoregional recurrence were similar for the unilateral and bilateral approaches (P = .90). In 1,148 patients with potentially curable PTM, defined as the absence of metastasis at diagnosis and no gross residual disease, the rates of tumor recurrence 10, 20, and 40 years after surgery were 6%, 7%, and 10%, respectively. In these 1,148 patients, the 30-year locoregional recurrence rates after UL alone were similar to those seen after NT or TT followed by RRA (P = .99).
UL did not result in permanent unilateral vocal cord paresis or permanent hypoparathyroidism. These adversities were more likely to develop following bilateral lobectomy.
“Since [UL] produces comparable recurrence results when compared to bilateral surgery and is not associated with either cord paresis or hypoparathyroidism, then perhaps it is overdue for institutions like Mayo to individualize our treatment policies and more often employ UL when surgery, and not observation or ultrasound-guided percutaneous ethanol ablation, is chosen to treat PTM,” said Dr. Hay.
Dr. Hay was adamant on the overuse of ultrasound in the detection of small-diameter carcinomas in the decision for bilateral surgery. “It’s embarrassing how much we are wasting resources and doing too much ultrasound too often,” he said in an interview.
Dr. Hay had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ENDO 2016
Key clinical point: Unilateral thryoidectomy should be reconsidered as a routine strategy in treatment of papillary thyroid microcarcinoma.
Major finding: Data compiled from over 80 years at a single institution indicates the value of unilateral thyroidectomy in terms of recurrence and morbidity.
Data source: Retrospective analysis of data from 1,153 adult patients.
Disclosures: Dr. Hay had no disclosures.
New vulvar cancer guidelines stress regional disease control
HOLLYWOOD, FLA. – The National Comprehensive Cancer Network has issued new guidelines for the diagnosis and management of vulvar cancer.
Vulvar cancers are rare neoplasms, with an estimated U.S. annual incidence of 5,950 cases, and 1,110 deaths. The majority of cases (about 90%) are of squamous cell histology.
Treatment of vulvar cancer has evolved from en bloc resections used throughout most of the 20th century, to more refined techniques, said Dr. Benjamin E. Greer, professor of gynecological oncology at the University of Washington in Seattle.
“In the 1980s, we started to modify treatment to reduce morbidity,” he said at the annual conference of the National Comprehensive Cancer Network.
With older, more radical techniques, groin breakdown, leg edema, and impaired sexual function were common post-surgery consequences. Current practice, however, is to perform regional lymph node management for unilateral cancers, radical local excision rather than en bloc resections, separate groin incisions, lymphatic mapping, radiation, chemotherapy, and, if necessary, exenteration, Dr. Greer noted.
The guidelines note that adequate surgical margins – 1 to 2 cm – at the time of primary surgery appear to be essential for reducing risk of local recurrence, and that if margins are within 8 mm of tumor, the surgeon should consider re-excision or adjuvant radiation.
Lymph node status is the most important determinant of survival, with historical reports showing overall survival following surgery of 70% to 80% among patients with negative nodes, compared with 30% to 40% of those with positive nodes, he said.
Evaluation of bilateral inguinofemoral groin nodes should be performed in patients with lesions in the vulvar midline, and ipsilateral groin node evaluation should be performed for those with lateral lesions lying more than 2 cm from the vulvar midline. Additionally, select patients may require sentinel lymph node biopsy, the guidelines state.
Unilateral carcinomas of the vulva can be treated with limited radical vulvectomy and ipsilateral inguinal femoral node dissection. Lymph node dissection can be performed through a separate incision. For patients with positive nodes, adjuvant radiation may aid in disease control. Patients with inoperable carcinomas are recommended to receive radiation and chemotherapy.
Radiation for vulvar cancer
“For early stage tumors, adjuvant radiotherapy is an effective treatment modality that significantly decreases recurrence, especially in surgically resected groins, and it leads to improvement in relapse-free and overall survival,” said Dr. Wui-Jin Koh, medical director for radiation oncology at the Fred Hutchinson Cancer Research Center in Seattle.
Concurrent chemotherapy and radiation may provide additional therapeutic benefit, especially for patients with advanced, unresectable tumors, and it may help to address systemic risk in patients with multiple positive lymph nodes, Dr. Koh said.
The guidelines state that radiation can be given with external beam radiation delivered via a 3D-conformal or intensity modulated (IMRT) technique, with brachytherapy boost for some tumors where the anatomy permits.
“Careful attention should be taken to ensure adequate tumor coverage by combining clinical examination, imaging findings, and appropriate nodal volumes at risk to define the target volume,” the guideline states.
For adjuvant therapy, doses of 50.4 Gy divided in 1.8 Gy fractions should be delivered once daily 5 days per week, with minimal treatment breaks.
For treatment of unresectable tumors, doses range from 59.4 Gy to 64.8 Gy in 1.8 Gy fractions, with a boost dose to approximately 70 Gy for large lymph nodes in select cases.
Residual disease
The decision to provide additional treatment following surgery is based on whether the patient is clinically negative for residual tumor at the primary site and nodes.
“If one has negative margins and negative nodes? Observation, absolutely,” Dr. Koh said. “If one has positive margins for invasive disease, our recommendation is to re-excise and not go straight to radiation, and if one can do it and get negative margins, again observe the majority of them.”
“Use radiation very judiciously,” he added. “Only if patients have positive margins or have unresectable primary disease do we routinely recommend radiation.”
Locally advanced disease
For patients who cannot be treated with conventional or sphincter-sparing, organ preserving surgery upfront, the recommendation is to provide chemoradiation, with initial radiation to the primary site, groins, and pelvis, and concurrent week cisplatin at a dose of 30-40 mg/m2 per week. The recommended radiation doses are 45 Gy to at-risk, microscopic clinical tumor volume, and 57.6 to 60 Gy to gross tumor volume (primary site and nodes).
“If one uses IMRT, you need to be very generous with the volumes,” Dr. Koh said.
The panelists also recommend re-imaging and re-evaluating patients 6 to 8 weeks after the completion of chemoradiation, with possible resection or biopsy of the primary tumor site, and limited groin resection of imaged residual disease.
For patients with clearly node-positive disease, “my general preference is to give upfront chemoradiation therapy to avoid delay of primary therapy, and then resect residual nodes after the chemoradiation is done,” he said.
HOLLYWOOD, FLA. – The National Comprehensive Cancer Network has issued new guidelines for the diagnosis and management of vulvar cancer.
Vulvar cancers are rare neoplasms, with an estimated U.S. annual incidence of 5,950 cases, and 1,110 deaths. The majority of cases (about 90%) are of squamous cell histology.
Treatment of vulvar cancer has evolved from en bloc resections used throughout most of the 20th century, to more refined techniques, said Dr. Benjamin E. Greer, professor of gynecological oncology at the University of Washington in Seattle.
“In the 1980s, we started to modify treatment to reduce morbidity,” he said at the annual conference of the National Comprehensive Cancer Network.
With older, more radical techniques, groin breakdown, leg edema, and impaired sexual function were common post-surgery consequences. Current practice, however, is to perform regional lymph node management for unilateral cancers, radical local excision rather than en bloc resections, separate groin incisions, lymphatic mapping, radiation, chemotherapy, and, if necessary, exenteration, Dr. Greer noted.
The guidelines note that adequate surgical margins – 1 to 2 cm – at the time of primary surgery appear to be essential for reducing risk of local recurrence, and that if margins are within 8 mm of tumor, the surgeon should consider re-excision or adjuvant radiation.
Lymph node status is the most important determinant of survival, with historical reports showing overall survival following surgery of 70% to 80% among patients with negative nodes, compared with 30% to 40% of those with positive nodes, he said.
Evaluation of bilateral inguinofemoral groin nodes should be performed in patients with lesions in the vulvar midline, and ipsilateral groin node evaluation should be performed for those with lateral lesions lying more than 2 cm from the vulvar midline. Additionally, select patients may require sentinel lymph node biopsy, the guidelines state.
Unilateral carcinomas of the vulva can be treated with limited radical vulvectomy and ipsilateral inguinal femoral node dissection. Lymph node dissection can be performed through a separate incision. For patients with positive nodes, adjuvant radiation may aid in disease control. Patients with inoperable carcinomas are recommended to receive radiation and chemotherapy.
Radiation for vulvar cancer
“For early stage tumors, adjuvant radiotherapy is an effective treatment modality that significantly decreases recurrence, especially in surgically resected groins, and it leads to improvement in relapse-free and overall survival,” said Dr. Wui-Jin Koh, medical director for radiation oncology at the Fred Hutchinson Cancer Research Center in Seattle.
Concurrent chemotherapy and radiation may provide additional therapeutic benefit, especially for patients with advanced, unresectable tumors, and it may help to address systemic risk in patients with multiple positive lymph nodes, Dr. Koh said.
The guidelines state that radiation can be given with external beam radiation delivered via a 3D-conformal or intensity modulated (IMRT) technique, with brachytherapy boost for some tumors where the anatomy permits.
“Careful attention should be taken to ensure adequate tumor coverage by combining clinical examination, imaging findings, and appropriate nodal volumes at risk to define the target volume,” the guideline states.
For adjuvant therapy, doses of 50.4 Gy divided in 1.8 Gy fractions should be delivered once daily 5 days per week, with minimal treatment breaks.
For treatment of unresectable tumors, doses range from 59.4 Gy to 64.8 Gy in 1.8 Gy fractions, with a boost dose to approximately 70 Gy for large lymph nodes in select cases.
Residual disease
The decision to provide additional treatment following surgery is based on whether the patient is clinically negative for residual tumor at the primary site and nodes.
“If one has negative margins and negative nodes? Observation, absolutely,” Dr. Koh said. “If one has positive margins for invasive disease, our recommendation is to re-excise and not go straight to radiation, and if one can do it and get negative margins, again observe the majority of them.”
“Use radiation very judiciously,” he added. “Only if patients have positive margins or have unresectable primary disease do we routinely recommend radiation.”
Locally advanced disease
For patients who cannot be treated with conventional or sphincter-sparing, organ preserving surgery upfront, the recommendation is to provide chemoradiation, with initial radiation to the primary site, groins, and pelvis, and concurrent week cisplatin at a dose of 30-40 mg/m2 per week. The recommended radiation doses are 45 Gy to at-risk, microscopic clinical tumor volume, and 57.6 to 60 Gy to gross tumor volume (primary site and nodes).
“If one uses IMRT, you need to be very generous with the volumes,” Dr. Koh said.
The panelists also recommend re-imaging and re-evaluating patients 6 to 8 weeks after the completion of chemoradiation, with possible resection or biopsy of the primary tumor site, and limited groin resection of imaged residual disease.
For patients with clearly node-positive disease, “my general preference is to give upfront chemoradiation therapy to avoid delay of primary therapy, and then resect residual nodes after the chemoradiation is done,” he said.
HOLLYWOOD, FLA. – The National Comprehensive Cancer Network has issued new guidelines for the diagnosis and management of vulvar cancer.
Vulvar cancers are rare neoplasms, with an estimated U.S. annual incidence of 5,950 cases, and 1,110 deaths. The majority of cases (about 90%) are of squamous cell histology.
Treatment of vulvar cancer has evolved from en bloc resections used throughout most of the 20th century, to more refined techniques, said Dr. Benjamin E. Greer, professor of gynecological oncology at the University of Washington in Seattle.
“In the 1980s, we started to modify treatment to reduce morbidity,” he said at the annual conference of the National Comprehensive Cancer Network.
With older, more radical techniques, groin breakdown, leg edema, and impaired sexual function were common post-surgery consequences. Current practice, however, is to perform regional lymph node management for unilateral cancers, radical local excision rather than en bloc resections, separate groin incisions, lymphatic mapping, radiation, chemotherapy, and, if necessary, exenteration, Dr. Greer noted.
The guidelines note that adequate surgical margins – 1 to 2 cm – at the time of primary surgery appear to be essential for reducing risk of local recurrence, and that if margins are within 8 mm of tumor, the surgeon should consider re-excision or adjuvant radiation.
Lymph node status is the most important determinant of survival, with historical reports showing overall survival following surgery of 70% to 80% among patients with negative nodes, compared with 30% to 40% of those with positive nodes, he said.
Evaluation of bilateral inguinofemoral groin nodes should be performed in patients with lesions in the vulvar midline, and ipsilateral groin node evaluation should be performed for those with lateral lesions lying more than 2 cm from the vulvar midline. Additionally, select patients may require sentinel lymph node biopsy, the guidelines state.
Unilateral carcinomas of the vulva can be treated with limited radical vulvectomy and ipsilateral inguinal femoral node dissection. Lymph node dissection can be performed through a separate incision. For patients with positive nodes, adjuvant radiation may aid in disease control. Patients with inoperable carcinomas are recommended to receive radiation and chemotherapy.
Radiation for vulvar cancer
“For early stage tumors, adjuvant radiotherapy is an effective treatment modality that significantly decreases recurrence, especially in surgically resected groins, and it leads to improvement in relapse-free and overall survival,” said Dr. Wui-Jin Koh, medical director for radiation oncology at the Fred Hutchinson Cancer Research Center in Seattle.
Concurrent chemotherapy and radiation may provide additional therapeutic benefit, especially for patients with advanced, unresectable tumors, and it may help to address systemic risk in patients with multiple positive lymph nodes, Dr. Koh said.
The guidelines state that radiation can be given with external beam radiation delivered via a 3D-conformal or intensity modulated (IMRT) technique, with brachytherapy boost for some tumors where the anatomy permits.
“Careful attention should be taken to ensure adequate tumor coverage by combining clinical examination, imaging findings, and appropriate nodal volumes at risk to define the target volume,” the guideline states.
For adjuvant therapy, doses of 50.4 Gy divided in 1.8 Gy fractions should be delivered once daily 5 days per week, with minimal treatment breaks.
For treatment of unresectable tumors, doses range from 59.4 Gy to 64.8 Gy in 1.8 Gy fractions, with a boost dose to approximately 70 Gy for large lymph nodes in select cases.
Residual disease
The decision to provide additional treatment following surgery is based on whether the patient is clinically negative for residual tumor at the primary site and nodes.
“If one has negative margins and negative nodes? Observation, absolutely,” Dr. Koh said. “If one has positive margins for invasive disease, our recommendation is to re-excise and not go straight to radiation, and if one can do it and get negative margins, again observe the majority of them.”
“Use radiation very judiciously,” he added. “Only if patients have positive margins or have unresectable primary disease do we routinely recommend radiation.”
Locally advanced disease
For patients who cannot be treated with conventional or sphincter-sparing, organ preserving surgery upfront, the recommendation is to provide chemoradiation, with initial radiation to the primary site, groins, and pelvis, and concurrent week cisplatin at a dose of 30-40 mg/m2 per week. The recommended radiation doses are 45 Gy to at-risk, microscopic clinical tumor volume, and 57.6 to 60 Gy to gross tumor volume (primary site and nodes).
“If one uses IMRT, you need to be very generous with the volumes,” Dr. Koh said.
The panelists also recommend re-imaging and re-evaluating patients 6 to 8 weeks after the completion of chemoradiation, with possible resection or biopsy of the primary tumor site, and limited groin resection of imaged residual disease.
For patients with clearly node-positive disease, “my general preference is to give upfront chemoradiation therapy to avoid delay of primary therapy, and then resect residual nodes after the chemoradiation is done,” he said.
AT THE NCCN ANNUAL CONFERENCE
Key clinical point: Nodal status is an important determinant of survival of patients with vulvar carcinomas.
Major finding: Historically, reported overall survival following surgery is 70% to 80% among patients with negative nodes, compared with 30% to 40% of those with positive nodes.
Data source: Review of new clinical guidelines for the management of patients with vulvar cancer.
Disclosures: Dr. Greer and Dr. Koh reported having no relevant clinical disclosures.
Less symptomatic patients ‘worse off’ after knee surgery
AMSTERDAM – Patients with milder knee osteoarthritis symptoms or better quality of life before undergoing total knee replacement surgery gained less benefit from the surgery than did those who had more severe symptoms in two separate analyses of British and U.S. patients.
Additional evidence from total knee replacements (TKRs) performed on U.S. participants of the Osteoarthritis Initiative also suggest that as the use of TKR has increased to include less symptomatic patients, the overall cost-effectiveness of the procedure has declined.
“Knee replacements are one of those interventions that are known to be very effective and very cost-effective,” Rafael Pinedo-Villanueva, Ph.D., of the University of Oxford (England) said during his presentation of National Health Service data from England at the World Congress on Osteoarthritis. Indeed, knee replacements are associated with significant improvements in pain, function, and quality of life, he said, but that is if you look at the mean values.
As the deciles for baseline knee pain and function decrease in severity, there are diminishing mean improvements and an increasing proportion of patients who do worse after the operation, he reported. Up to 17% of patients had unchanged or improved knee pain scores and up to 27% had lower quality of life scores. If minimally important differences were considered, these percentages rose to 40% and 48% of patients being worse off, respectively.
“The significant improvements seem to be overshadowing what happens to those patients who are doing worse,” Dr. Pinedo-Villanueva suggested. “So essentially cost-effectiveness is being driven by the magnitude of the change in those who do improve, and we don’t really see much about what is happening to those who are doing worse.”
Of over 215,000 records of knee replacement collected from all patients undergoing TKR in England during 2008-2012, Dr. Pinedo-Villanueva and his study coauthors found 117,844 had data on pre- and post-operative knee pain assessed using the Oxford Knee Score (OKS) and quality of life measured with the EQ-5D instrument. The majority of replacements were in women (55%) and almost three quarters of patients had one or no comorbidities. Overall, the mean change in OKS was 15 points, improving from 19 to 34 (the higher the score the lesser the knee pain). EQ-5D scores also improved by a mean difference of 0.30 (from 0.41 to 0.70 where 1.0 is perfect health). Although the vast majority of patients had improved OKS and EQ-5D scores after surgery, unchanged or decreased scores were seen in 8% and 22% of patients, respectively.
“As we breakdown these data by deciles of baseline pain and function we see clearly that those starting at the lower decile improved the most, and that’s to be expected; they’ve a lot more to improve than the ones that came into the operation at the higher decile,” Dr. Pinedo-Villanueva said at the Congress, sponsored by the Osteoarthritis Research Society International. But there were patients who fared worse at every decile, he noted.
Dr. Pinedo-Villanueva concluded that outcome prediction models were needed to try to reduce the number of patients who are apparently worse off after knee replacement and improve the efficiency of resource allocation.
The value of TKR in a contemporary U.S. population was the focus of a separate presentation by Dr. Bart Ferket of Mount Sinai Hospital in New York. Dr. Ferket reported the results of a study looking at the impact of TKR on patients’ quality of life, lifetime costs, and quality-adjusted life years (QALYs) while varying the use of TKR by patients’ functional status at baseline.
“In the United States, the rate at which total knee replacement is performed has doubled in the last two decades,” Dr. Ferket observed. This “disproportionate” increase has been attributed to expanding the eligibility criteria to include less symptomatic patients.
Using data collected over an 8-year period on 1,327 participants from the Osteoarthritis Initiative, Dr. Ferket and his associates at Mount Sinai and Erasmus University Medical Center in Rotterdam (The Netherlands) discovered that the increased uptake of TKR might have affected the likely benefit and reduced the overall cost-effectiveness of the procedure.
At baseline, 17% of the participants, who all had knee osteoarthritis, had had a prior knee replacement.
Quality of life measured on the physical component scores (PCS) of the 12-item Short Form (SF-12) were generally improved after TKR but decreased in those who did not have a knee replaced. The effect on the mental component of the SF-12 was less clear, with possibly a decrease seen in some patients. Changes on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Knee injury and Osteoarthritis Outcome Score (KOOS) showed a considerable benefit for knee replacement and there was a general decrease in pain medication over time in those who had surgery. The overall effect was more pronounced if patients with greater baseline symptoms were considered.
Cost-effectiveness modeling showed that reserving TKR for more seriously affected patients may make it more economically attractive. The QALYs gained from TKR was about 11 but as the number of QALYs increased, so did the relative lifetime cost, with increasing incremental cost-effectiveness ratios (ICERs) as SF-12 PCS rose. ICERs were around $143,000, $160,000, $217,000, $385,000, and $1,175,000 considering patients with SF-12 PCS of less than 30, 35, 40, 45, and 50, respectively.
“The more lenient the eligibility criteria are, the higher the effectiveness, but also the higher the costs,” Dr. Ferket said. “The most cost-effective scenarios are actually more restrictive that what is currently seen in current practice in the U.S.”
Dr. Pinedo-Villanueva and Dr. Ferket reported having no financial disclosures.
AMSTERDAM – Patients with milder knee osteoarthritis symptoms or better quality of life before undergoing total knee replacement surgery gained less benefit from the surgery than did those who had more severe symptoms in two separate analyses of British and U.S. patients.
Additional evidence from total knee replacements (TKRs) performed on U.S. participants of the Osteoarthritis Initiative also suggest that as the use of TKR has increased to include less symptomatic patients, the overall cost-effectiveness of the procedure has declined.
“Knee replacements are one of those interventions that are known to be very effective and very cost-effective,” Rafael Pinedo-Villanueva, Ph.D., of the University of Oxford (England) said during his presentation of National Health Service data from England at the World Congress on Osteoarthritis. Indeed, knee replacements are associated with significant improvements in pain, function, and quality of life, he said, but that is if you look at the mean values.
As the deciles for baseline knee pain and function decrease in severity, there are diminishing mean improvements and an increasing proportion of patients who do worse after the operation, he reported. Up to 17% of patients had unchanged or improved knee pain scores and up to 27% had lower quality of life scores. If minimally important differences were considered, these percentages rose to 40% and 48% of patients being worse off, respectively.
“The significant improvements seem to be overshadowing what happens to those patients who are doing worse,” Dr. Pinedo-Villanueva suggested. “So essentially cost-effectiveness is being driven by the magnitude of the change in those who do improve, and we don’t really see much about what is happening to those who are doing worse.”
Of over 215,000 records of knee replacement collected from all patients undergoing TKR in England during 2008-2012, Dr. Pinedo-Villanueva and his study coauthors found 117,844 had data on pre- and post-operative knee pain assessed using the Oxford Knee Score (OKS) and quality of life measured with the EQ-5D instrument. The majority of replacements were in women (55%) and almost three quarters of patients had one or no comorbidities. Overall, the mean change in OKS was 15 points, improving from 19 to 34 (the higher the score the lesser the knee pain). EQ-5D scores also improved by a mean difference of 0.30 (from 0.41 to 0.70 where 1.0 is perfect health). Although the vast majority of patients had improved OKS and EQ-5D scores after surgery, unchanged or decreased scores were seen in 8% and 22% of patients, respectively.
“As we breakdown these data by deciles of baseline pain and function we see clearly that those starting at the lower decile improved the most, and that’s to be expected; they’ve a lot more to improve than the ones that came into the operation at the higher decile,” Dr. Pinedo-Villanueva said at the Congress, sponsored by the Osteoarthritis Research Society International. But there were patients who fared worse at every decile, he noted.
Dr. Pinedo-Villanueva concluded that outcome prediction models were needed to try to reduce the number of patients who are apparently worse off after knee replacement and improve the efficiency of resource allocation.
The value of TKR in a contemporary U.S. population was the focus of a separate presentation by Dr. Bart Ferket of Mount Sinai Hospital in New York. Dr. Ferket reported the results of a study looking at the impact of TKR on patients’ quality of life, lifetime costs, and quality-adjusted life years (QALYs) while varying the use of TKR by patients’ functional status at baseline.
“In the United States, the rate at which total knee replacement is performed has doubled in the last two decades,” Dr. Ferket observed. This “disproportionate” increase has been attributed to expanding the eligibility criteria to include less symptomatic patients.
Using data collected over an 8-year period on 1,327 participants from the Osteoarthritis Initiative, Dr. Ferket and his associates at Mount Sinai and Erasmus University Medical Center in Rotterdam (The Netherlands) discovered that the increased uptake of TKR might have affected the likely benefit and reduced the overall cost-effectiveness of the procedure.
At baseline, 17% of the participants, who all had knee osteoarthritis, had had a prior knee replacement.
Quality of life measured on the physical component scores (PCS) of the 12-item Short Form (SF-12) were generally improved after TKR but decreased in those who did not have a knee replaced. The effect on the mental component of the SF-12 was less clear, with possibly a decrease seen in some patients. Changes on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Knee injury and Osteoarthritis Outcome Score (KOOS) showed a considerable benefit for knee replacement and there was a general decrease in pain medication over time in those who had surgery. The overall effect was more pronounced if patients with greater baseline symptoms were considered.
Cost-effectiveness modeling showed that reserving TKR for more seriously affected patients may make it more economically attractive. The QALYs gained from TKR was about 11 but as the number of QALYs increased, so did the relative lifetime cost, with increasing incremental cost-effectiveness ratios (ICERs) as SF-12 PCS rose. ICERs were around $143,000, $160,000, $217,000, $385,000, and $1,175,000 considering patients with SF-12 PCS of less than 30, 35, 40, 45, and 50, respectively.
“The more lenient the eligibility criteria are, the higher the effectiveness, but also the higher the costs,” Dr. Ferket said. “The most cost-effective scenarios are actually more restrictive that what is currently seen in current practice in the U.S.”
Dr. Pinedo-Villanueva and Dr. Ferket reported having no financial disclosures.
AMSTERDAM – Patients with milder knee osteoarthritis symptoms or better quality of life before undergoing total knee replacement surgery gained less benefit from the surgery than did those who had more severe symptoms in two separate analyses of British and U.S. patients.
Additional evidence from total knee replacements (TKRs) performed on U.S. participants of the Osteoarthritis Initiative also suggest that as the use of TKR has increased to include less symptomatic patients, the overall cost-effectiveness of the procedure has declined.
“Knee replacements are one of those interventions that are known to be very effective and very cost-effective,” Rafael Pinedo-Villanueva, Ph.D., of the University of Oxford (England) said during his presentation of National Health Service data from England at the World Congress on Osteoarthritis. Indeed, knee replacements are associated with significant improvements in pain, function, and quality of life, he said, but that is if you look at the mean values.
As the deciles for baseline knee pain and function decrease in severity, there are diminishing mean improvements and an increasing proportion of patients who do worse after the operation, he reported. Up to 17% of patients had unchanged or improved knee pain scores and up to 27% had lower quality of life scores. If minimally important differences were considered, these percentages rose to 40% and 48% of patients being worse off, respectively.
“The significant improvements seem to be overshadowing what happens to those patients who are doing worse,” Dr. Pinedo-Villanueva suggested. “So essentially cost-effectiveness is being driven by the magnitude of the change in those who do improve, and we don’t really see much about what is happening to those who are doing worse.”
Of over 215,000 records of knee replacement collected from all patients undergoing TKR in England during 2008-2012, Dr. Pinedo-Villanueva and his study coauthors found 117,844 had data on pre- and post-operative knee pain assessed using the Oxford Knee Score (OKS) and quality of life measured with the EQ-5D instrument. The majority of replacements were in women (55%) and almost three quarters of patients had one or no comorbidities. Overall, the mean change in OKS was 15 points, improving from 19 to 34 (the higher the score the lesser the knee pain). EQ-5D scores also improved by a mean difference of 0.30 (from 0.41 to 0.70 where 1.0 is perfect health). Although the vast majority of patients had improved OKS and EQ-5D scores after surgery, unchanged or decreased scores were seen in 8% and 22% of patients, respectively.
“As we breakdown these data by deciles of baseline pain and function we see clearly that those starting at the lower decile improved the most, and that’s to be expected; they’ve a lot more to improve than the ones that came into the operation at the higher decile,” Dr. Pinedo-Villanueva said at the Congress, sponsored by the Osteoarthritis Research Society International. But there were patients who fared worse at every decile, he noted.
Dr. Pinedo-Villanueva concluded that outcome prediction models were needed to try to reduce the number of patients who are apparently worse off after knee replacement and improve the efficiency of resource allocation.
The value of TKR in a contemporary U.S. population was the focus of a separate presentation by Dr. Bart Ferket of Mount Sinai Hospital in New York. Dr. Ferket reported the results of a study looking at the impact of TKR on patients’ quality of life, lifetime costs, and quality-adjusted life years (QALYs) while varying the use of TKR by patients’ functional status at baseline.
“In the United States, the rate at which total knee replacement is performed has doubled in the last two decades,” Dr. Ferket observed. This “disproportionate” increase has been attributed to expanding the eligibility criteria to include less symptomatic patients.
Using data collected over an 8-year period on 1,327 participants from the Osteoarthritis Initiative, Dr. Ferket and his associates at Mount Sinai and Erasmus University Medical Center in Rotterdam (The Netherlands) discovered that the increased uptake of TKR might have affected the likely benefit and reduced the overall cost-effectiveness of the procedure.
At baseline, 17% of the participants, who all had knee osteoarthritis, had had a prior knee replacement.
Quality of life measured on the physical component scores (PCS) of the 12-item Short Form (SF-12) were generally improved after TKR but decreased in those who did not have a knee replaced. The effect on the mental component of the SF-12 was less clear, with possibly a decrease seen in some patients. Changes on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Knee injury and Osteoarthritis Outcome Score (KOOS) showed a considerable benefit for knee replacement and there was a general decrease in pain medication over time in those who had surgery. The overall effect was more pronounced if patients with greater baseline symptoms were considered.
Cost-effectiveness modeling showed that reserving TKR for more seriously affected patients may make it more economically attractive. The QALYs gained from TKR was about 11 but as the number of QALYs increased, so did the relative lifetime cost, with increasing incremental cost-effectiveness ratios (ICERs) as SF-12 PCS rose. ICERs were around $143,000, $160,000, $217,000, $385,000, and $1,175,000 considering patients with SF-12 PCS of less than 30, 35, 40, 45, and 50, respectively.
“The more lenient the eligibility criteria are, the higher the effectiveness, but also the higher the costs,” Dr. Ferket said. “The most cost-effective scenarios are actually more restrictive that what is currently seen in current practice in the U.S.”
Dr. Pinedo-Villanueva and Dr. Ferket reported having no financial disclosures.
AT OARSI 2016
Key clinical point: Patients with milder osteoarthritis can fare worse after knee replacement surgery, and the cost-effectiveness of the procedure is lower.
Major finding: Knee pain and quality of life scores were unchanged or worse after the operation in 8% and 22% of patients, respectively.
Data source: Two separate studies looking at the value of knee replacement in patients with knee osteoarthritis.
Disclosures: Dr. Pinedo-Villanueva and Dr. Ferket reported having no financial disclosures.
FDA allows marketing of morcellation containment system
The Food and Drug Administration has cleared for marketing a novel tissue containment system for use with certain laparoscopic power morcellators.
The PneumoLiner system is intended to be used to contain morcellated uterine tissue in a limited population of patients, including women without uterine fibroids undergoing hysterectomy and some premenopausal women with fibroids who want to maintain their fertility, according to the FDA. The agency is requiring the manufacturer to warn patients and physicians that the device has not been proven to reduce the risk of spreading cancer during surgery.
This approval – through the FDA’s de novo classification process for novel, low- and moderate-risk medical devices – comes about 2 years after the FDA first warned physicians and patients about the risk of spreading unsuspected uterine sarcomas during laparoscopic power morcellation in hysterectomy or myomectomy.
“This new device does not change our position on the risks associated with power morcellation,” Dr. William Maisel, deputy director for science and chief scientist at the FDA’s Center for Devices and Radiological Health, said in an April 7 statement. “We are continuing to warn against the use of power morcellators for the vast majority of women undergoing removal of the uterus or uterine fibroids.”
The device, which is manufactured by Advanced Surgical Concepts of Bray, Ireland, consists of a containment bag and a tube-like plunger to deliver the device into the abdominal cavity. The tissue being removed is placed in the bag and the bag is sealed and inflated. The inflation is intended to create working space around the tissue and better visualization during morcellation to prevent the morcellator tip or other surgical instruments from puncturing the bag. During laboratory testing, the containment bag was found to be impermeable to substances similar in molecular size to tissues, cells, and body fluids, according to the FDA.
Risks associated with the device include dissemination of morcellated tissue, injury to surrounding tissues or organs, infections, and a potentially longer surgical time. The FDA is requiring that the device’s label state that use of the PneumoLiner system is limited to physicians who have successfully completed the manufacturer’s validated training program.
On Twitter @maryellenny
The Food and Drug Administration has cleared for marketing a novel tissue containment system for use with certain laparoscopic power morcellators.
The PneumoLiner system is intended to be used to contain morcellated uterine tissue in a limited population of patients, including women without uterine fibroids undergoing hysterectomy and some premenopausal women with fibroids who want to maintain their fertility, according to the FDA. The agency is requiring the manufacturer to warn patients and physicians that the device has not been proven to reduce the risk of spreading cancer during surgery.
This approval – through the FDA’s de novo classification process for novel, low- and moderate-risk medical devices – comes about 2 years after the FDA first warned physicians and patients about the risk of spreading unsuspected uterine sarcomas during laparoscopic power morcellation in hysterectomy or myomectomy.
“This new device does not change our position on the risks associated with power morcellation,” Dr. William Maisel, deputy director for science and chief scientist at the FDA’s Center for Devices and Radiological Health, said in an April 7 statement. “We are continuing to warn against the use of power morcellators for the vast majority of women undergoing removal of the uterus or uterine fibroids.”
The device, which is manufactured by Advanced Surgical Concepts of Bray, Ireland, consists of a containment bag and a tube-like plunger to deliver the device into the abdominal cavity. The tissue being removed is placed in the bag and the bag is sealed and inflated. The inflation is intended to create working space around the tissue and better visualization during morcellation to prevent the morcellator tip or other surgical instruments from puncturing the bag. During laboratory testing, the containment bag was found to be impermeable to substances similar in molecular size to tissues, cells, and body fluids, according to the FDA.
Risks associated with the device include dissemination of morcellated tissue, injury to surrounding tissues or organs, infections, and a potentially longer surgical time. The FDA is requiring that the device’s label state that use of the PneumoLiner system is limited to physicians who have successfully completed the manufacturer’s validated training program.
On Twitter @maryellenny
The Food and Drug Administration has cleared for marketing a novel tissue containment system for use with certain laparoscopic power morcellators.
The PneumoLiner system is intended to be used to contain morcellated uterine tissue in a limited population of patients, including women without uterine fibroids undergoing hysterectomy and some premenopausal women with fibroids who want to maintain their fertility, according to the FDA. The agency is requiring the manufacturer to warn patients and physicians that the device has not been proven to reduce the risk of spreading cancer during surgery.
This approval – through the FDA’s de novo classification process for novel, low- and moderate-risk medical devices – comes about 2 years after the FDA first warned physicians and patients about the risk of spreading unsuspected uterine sarcomas during laparoscopic power morcellation in hysterectomy or myomectomy.
“This new device does not change our position on the risks associated with power morcellation,” Dr. William Maisel, deputy director for science and chief scientist at the FDA’s Center for Devices and Radiological Health, said in an April 7 statement. “We are continuing to warn against the use of power morcellators for the vast majority of women undergoing removal of the uterus or uterine fibroids.”
The device, which is manufactured by Advanced Surgical Concepts of Bray, Ireland, consists of a containment bag and a tube-like plunger to deliver the device into the abdominal cavity. The tissue being removed is placed in the bag and the bag is sealed and inflated. The inflation is intended to create working space around the tissue and better visualization during morcellation to prevent the morcellator tip or other surgical instruments from puncturing the bag. During laboratory testing, the containment bag was found to be impermeable to substances similar in molecular size to tissues, cells, and body fluids, according to the FDA.
Risks associated with the device include dissemination of morcellated tissue, injury to surrounding tissues or organs, infections, and a potentially longer surgical time. The FDA is requiring that the device’s label state that use of the PneumoLiner system is limited to physicians who have successfully completed the manufacturer’s validated training program.
On Twitter @maryellenny
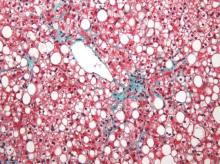
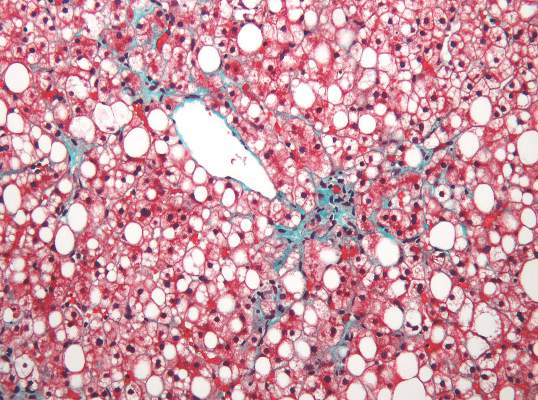
Fatty liver risk rises in years after transplant
Steatosis may be present in at least half of liver transplant recipients, and the prevalence increases significantly over time, according to data from a retrospective study of 548 adult patients.
Although steatosis is common after transplantation, the prevalence, risk factors, and impact on patient survival has not been well studied, wrote Dr. Irena Hejlova of the Institute for Clinical and Experimental Medicine in Prague, Czech Republic, and her colleagues.
“Our study was the first to document that the prevalence of steatosis in LT [liver transplant] recipients may be far higher than previously reported,” they said.
The researchers reviewed liver biopsies and patient survival data and found steatosis in 309 (56%) of the patients, including 93 (17%) with significant steatosis (defined as greater than 33%). Pretransplant factors associated with significant steatosis included cirrhosis caused by alcohol consumption as well as a high body mass index. Post-transplant risk factors associated with increased risk of significant steatosis included increased body mass index, increased serum triglycerides, alcohol consumption, and type 2 diabetes. However, “Although patients transplanted for alcoholic cirrhosis are at an increased risk, the vast majority of post-transplant steatosis is nonalcohol-related,” the researchers noted.
The overall prevalence of steatosis increased from 30% at 1 year after transplant to 48% at 10 years after transplant. Post-transplant steatosis was not associated with worse patient survival in the short term, but the long-term survival of patients with significant steatosis tended to be worse.
Read the full study here (Liver Transpl. 2016 Apr 5. doi: 10.1002/lt.24393).
Steatosis may be present in at least half of liver transplant recipients, and the prevalence increases significantly over time, according to data from a retrospective study of 548 adult patients.
Although steatosis is common after transplantation, the prevalence, risk factors, and impact on patient survival has not been well studied, wrote Dr. Irena Hejlova of the Institute for Clinical and Experimental Medicine in Prague, Czech Republic, and her colleagues.
“Our study was the first to document that the prevalence of steatosis in LT [liver transplant] recipients may be far higher than previously reported,” they said.
The researchers reviewed liver biopsies and patient survival data and found steatosis in 309 (56%) of the patients, including 93 (17%) with significant steatosis (defined as greater than 33%). Pretransplant factors associated with significant steatosis included cirrhosis caused by alcohol consumption as well as a high body mass index. Post-transplant risk factors associated with increased risk of significant steatosis included increased body mass index, increased serum triglycerides, alcohol consumption, and type 2 diabetes. However, “Although patients transplanted for alcoholic cirrhosis are at an increased risk, the vast majority of post-transplant steatosis is nonalcohol-related,” the researchers noted.
The overall prevalence of steatosis increased from 30% at 1 year after transplant to 48% at 10 years after transplant. Post-transplant steatosis was not associated with worse patient survival in the short term, but the long-term survival of patients with significant steatosis tended to be worse.
Read the full study here (Liver Transpl. 2016 Apr 5. doi: 10.1002/lt.24393).
Steatosis may be present in at least half of liver transplant recipients, and the prevalence increases significantly over time, according to data from a retrospective study of 548 adult patients.
Although steatosis is common after transplantation, the prevalence, risk factors, and impact on patient survival has not been well studied, wrote Dr. Irena Hejlova of the Institute for Clinical and Experimental Medicine in Prague, Czech Republic, and her colleagues.
“Our study was the first to document that the prevalence of steatosis in LT [liver transplant] recipients may be far higher than previously reported,” they said.
The researchers reviewed liver biopsies and patient survival data and found steatosis in 309 (56%) of the patients, including 93 (17%) with significant steatosis (defined as greater than 33%). Pretransplant factors associated with significant steatosis included cirrhosis caused by alcohol consumption as well as a high body mass index. Post-transplant risk factors associated with increased risk of significant steatosis included increased body mass index, increased serum triglycerides, alcohol consumption, and type 2 diabetes. However, “Although patients transplanted for alcoholic cirrhosis are at an increased risk, the vast majority of post-transplant steatosis is nonalcohol-related,” the researchers noted.
The overall prevalence of steatosis increased from 30% at 1 year after transplant to 48% at 10 years after transplant. Post-transplant steatosis was not associated with worse patient survival in the short term, but the long-term survival of patients with significant steatosis tended to be worse.
Read the full study here (Liver Transpl. 2016 Apr 5. doi: 10.1002/lt.24393).
FROM LIVER TRANSPLANTATION
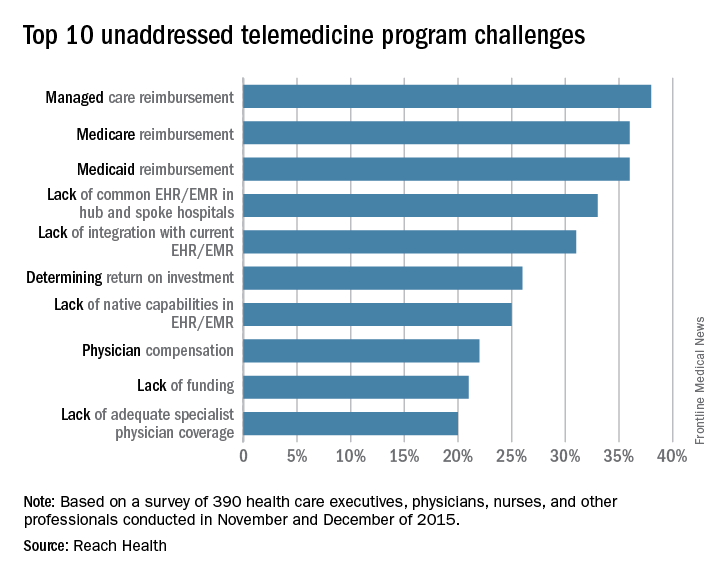
SURVEY: Telemedicine high priority, but reimbursement remains challenging
Nearly two-thirds of health care providers rank telemedicine as a top priority in 2016, a 10% increase from last year, according to a survey.
Telemedicine software company REACH Health surveyed 390 U.S. health care professionals between November 2015 and December 2015, including physicians, nurses, and health care executives. Participants answered questions related to their objectives, challenges, telemedicine program models, and management structures, among other inquiries.
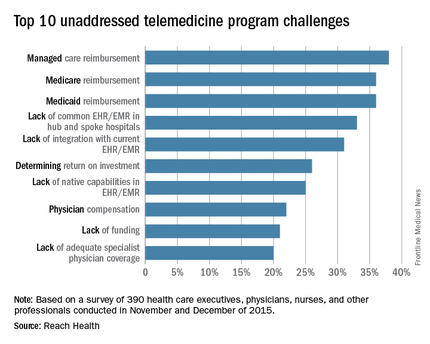
Of those polled, 96% of respondents said improving patient outcome was a top objective in developing telemedicine programs, according to the survey. Increasing patient convenience (87%) and improving patient engagement (86%) also rated highly. Other objectives included providing remote and rural patients with access to specialists (83%) and improving leverage of limited physician resources (81%). Percentages do not equal 100% because respondents could choose more than one objective.
The maturity of telemedicine programs varied widely depending on care setting. In general, settings requiring highly specialized treatment had more mature telemedicine programs than those requiring more generalized treatment. Stroke, neurology, and psychiatric/behavioral health settings had the most mature telemedicine programs, according to the survey.
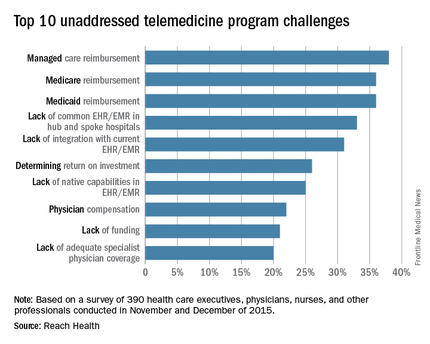
Reimbursement ranked as the top barrier to telemedicine. Respondents rated private plan payment as the No. 1 challenge (38%), followed by Medicare reimbursement (36%) and Medicaid reimbursement (36%). Electronic health record incapabilities and liability risks also ranked as primary challenges.
“Telemedicine reimbursement poses the primary obstacle to success, but EMR-related challenges are persistent and widely noted in the survey,” Steve McGraw, president and CEO of REACH Health said in a statement. “There is clearly a high demand in the industry for EMR integration, specifically the two-way flow of individual data elements between telemedicine platforms and EMR systems.”
On Twitter @legal_med
Nearly two-thirds of health care providers rank telemedicine as a top priority in 2016, a 10% increase from last year, according to a survey.
Telemedicine software company REACH Health surveyed 390 U.S. health care professionals between November 2015 and December 2015, including physicians, nurses, and health care executives. Participants answered questions related to their objectives, challenges, telemedicine program models, and management structures, among other inquiries.
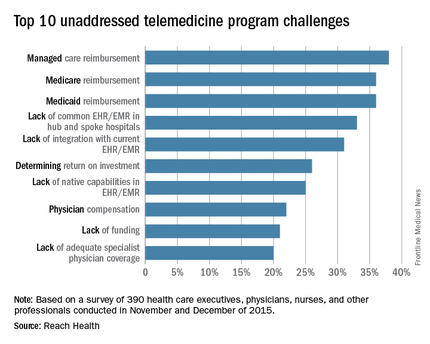
Of those polled, 96% of respondents said improving patient outcome was a top objective in developing telemedicine programs, according to the survey. Increasing patient convenience (87%) and improving patient engagement (86%) also rated highly. Other objectives included providing remote and rural patients with access to specialists (83%) and improving leverage of limited physician resources (81%). Percentages do not equal 100% because respondents could choose more than one objective.
The maturity of telemedicine programs varied widely depending on care setting. In general, settings requiring highly specialized treatment had more mature telemedicine programs than those requiring more generalized treatment. Stroke, neurology, and psychiatric/behavioral health settings had the most mature telemedicine programs, according to the survey.
Reimbursement ranked as the top barrier to telemedicine. Respondents rated private plan payment as the No. 1 challenge (38%), followed by Medicare reimbursement (36%) and Medicaid reimbursement (36%). Electronic health record incapabilities and liability risks also ranked as primary challenges.
“Telemedicine reimbursement poses the primary obstacle to success, but EMR-related challenges are persistent and widely noted in the survey,” Steve McGraw, president and CEO of REACH Health said in a statement. “There is clearly a high demand in the industry for EMR integration, specifically the two-way flow of individual data elements between telemedicine platforms and EMR systems.”
On Twitter @legal_med
Nearly two-thirds of health care providers rank telemedicine as a top priority in 2016, a 10% increase from last year, according to a survey.
Telemedicine software company REACH Health surveyed 390 U.S. health care professionals between November 2015 and December 2015, including physicians, nurses, and health care executives. Participants answered questions related to their objectives, challenges, telemedicine program models, and management structures, among other inquiries.
Of those polled, 96% of respondents said improving patient outcome was a top objective in developing telemedicine programs, according to the survey. Increasing patient convenience (87%) and improving patient engagement (86%) also rated highly. Other objectives included providing remote and rural patients with access to specialists (83%) and improving leverage of limited physician resources (81%). Percentages do not equal 100% because respondents could choose more than one objective.
The maturity of telemedicine programs varied widely depending on care setting. In general, settings requiring highly specialized treatment had more mature telemedicine programs than those requiring more generalized treatment. Stroke, neurology, and psychiatric/behavioral health settings had the most mature telemedicine programs, according to the survey.
Reimbursement ranked as the top barrier to telemedicine. Respondents rated private plan payment as the No. 1 challenge (38%), followed by Medicare reimbursement (36%) and Medicaid reimbursement (36%). Electronic health record incapabilities and liability risks also ranked as primary challenges.
“Telemedicine reimbursement poses the primary obstacle to success, but EMR-related challenges are persistent and widely noted in the survey,” Steve McGraw, president and CEO of REACH Health said in a statement. “There is clearly a high demand in the industry for EMR integration, specifically the two-way flow of individual data elements between telemedicine platforms and EMR systems.”
On Twitter @legal_med
FIRE AND ICE trial called a win for cryoablation of AF
CHICAGO – The largest-ever randomized trial of catheter ablation of atrial fibrillation has ended in a draw between radiofrequency and cryoballoon ablation in safety and efficacy – and that actually represents a win for cryoablation, a simpler and far more easily mastered procedure, Dr. Karl-Heinz Kuck said at the annual meeting of the American College of Cardiology.
“We can teach physicians how to do cryoablation much more easily. That will allow more patients with atrial fibrillation to get access to catheter ablation, which is what we really need,” according to Dr. Kuck, principal investigator in the poetically named FIRE AND ICE trial and head of cardiology at St. Georg Hospital in Hamburg (Germany).
FIRE AND ICE included 769 patients in eight European countries. The participants, all of whom had antiarrhythmic drug–refractory paroxysmal atrial fibrillation (AF), were randomized to radiofrequency ablation – the long-time standard – or to cryoablation, a newer technology. Radiofrequency ablation was guided by three-dimensional electroanatomic mapping, while cryoablation utilized fluoroscopic guidance.
The primary efficacy endpoint was the 1-year rate of clinical failure, defined as an occurrence of AF, atrial flutter, or atrial tachycardia lasting for at least 30 seconds, or repeat ablation or the use of antiarrhythmic drugs following a 90-day postprocedural blanking period. The clinical failure rate was 34.6% in the cryoballoon group and similar at 35.9% in the radiofrequency group.
Serious treatment-related adverse events occurred in 10.2% of the cryoballoon group and 12.8% of the radiofrequency group, a nonsignificant difference. No procedural deaths occurred in the study.
There were, however, several significant procedural differences. Procedure time averaged 124 minutes in the cryoablation group, nearly 20 minutes less than the 142 minutes for radiofrequency ablation. However, the 17-minute fluoroscopy time in the radiofrequency group was 5 minutes shorter than for cryoablation.
Dr. Kuck said the study underestimates the true procedural differences because FIRE AND ICE was carried out by extremely experienced operators. In routine clinical practice involving non-elite operators, it’s not unusual for radiofrequency ablation fluoroscopy times to be two or even three times longer than the 17 minutes seen in the study. Plus, FIRE AND ICE was conducted when the procedure entailed two applications of the cryoballoon. Now only one application is recommended, cutting an additional 12 minutes off the total procedure time, he added.
Radiofrequency ablation takes longer because it entails creating a series of point-to-point lesions in a circle to isolate the pulmonary veins. With cryoablation, the balloon is moved into position, inflated, and a 3-minute-freeze is administered to create a circle of necrotic tissue in a single-step procedure.
Discussant Dr. Hugh G. Calkins praised the FIRE AND ICE investigators’ use of a rigorous definition of recurrence that required as little as a 30-second episode of atrial arrhythmia.
“That’s a very high bar, so I think the results are very impressive,” said Dr. Calkins, professor of medicine and of pediatrics and director of the cardiac arrhythmia service at Johns Hopkins University, Baltimore.
He commented that “this study is a clear reminder that 90% success rates just don’t happen in this field,” despite what some practitioners have claimed.
Asked how he predicts the study results will influence the field of AF ablation, Dr. Kuck replied that he foresees much wider adoption of cryoablation and a stronger endorsement of the technology in updated guideline recommendations.
“I personally believe this will be the most important development in our field in the next several years,” he added.
The electrophysiologist noted that even though current guidelines give a class Ia recommendation to catheter ablation of paroxysmal AF that’s refractory to at least one antiarrhythmic drug, at present only 4% of such patients actually undergo the procedure.
“Having just 4% of patients with AF undergo catheter ablation cannot be what we are looking for as physicians,” Dr. Kuck said. “I believe if we want to roll out catheter ablation for AF, we need simple and safe tools. This trial elegantly shows that with a simpler device that allows single-shot isolation of the pulmonary veins, we can get the same safety and efficacy as with radiofrequency ablation. I often tell people that radiofrequency ablation of atrial fibrillation is the most challenging procedure in all cardiology. We do this procedure from the groin in a moving heart. It’s a very complex technology.”
His dream, he continued, is that cryoablation will eventually enable patients with atrial fibrillation to be managed the same way electrophysiologists treat patients with Wolff-Parkinson-White syndrome; with the first episode, the patient goes to the electrophysiology catheterization lab for an ablation procedure.
“I think there’s a great message here: The cryoballoon will move catheter ablation from a niche procedure performed in specialized centers by the few guys in the world who can do it really well out into the broader world. To do that you need a tool that is safe, simple, and can be handled by the average doctor,” Dr. Kuck said.
Discussant Dr. Anthony DeMaria commented that it would be premature at this point to start thinking about cryoablation as a first approach to new-onset AF, given the roughly 35% clinical failure rate at 1 year seen in FIRE AND ICE. That rate doubtless would have been even higher had patients been equipped with implantable loop recorders, added Dr. DeMaria, professor of medicine at the University of California, San Diego.
Dr. Kuck conceded that the high recurrence rate is one of the great unsolved limitations of catheter ablation of AF.
“We don’t know how to get the pulmonary veins permanently isolated,” he said. “We can create acute lesions, but over time what we’ve seen is recovery of tissue and then reconduction by the pulmonary veins. I believe that 20% of the 40% recurrence rate is due to reconduction from the pulmonary veins, and the rest is probably due to triggers coming from other sites.”
The FIRE AND ICE trial was funded in part by Medtronic, which markets the Arctic Front Advance cryoablation catheter used in the study. Dr. Kuck reported serving on a speakers’ bureau for Medtronic and acting as a consultant to Biosense Webster, Edwards, and St. Jude.
Simultaneous with Dr. Kuck’s presentation at ACC 16, the results of FIRE AND ICE were published online (N Engl J Med. 2016 Apr 4. doi: 10.1056/NEJMoa1602014).
CHICAGO – The largest-ever randomized trial of catheter ablation of atrial fibrillation has ended in a draw between radiofrequency and cryoballoon ablation in safety and efficacy – and that actually represents a win for cryoablation, a simpler and far more easily mastered procedure, Dr. Karl-Heinz Kuck said at the annual meeting of the American College of Cardiology.
“We can teach physicians how to do cryoablation much more easily. That will allow more patients with atrial fibrillation to get access to catheter ablation, which is what we really need,” according to Dr. Kuck, principal investigator in the poetically named FIRE AND ICE trial and head of cardiology at St. Georg Hospital in Hamburg (Germany).
FIRE AND ICE included 769 patients in eight European countries. The participants, all of whom had antiarrhythmic drug–refractory paroxysmal atrial fibrillation (AF), were randomized to radiofrequency ablation – the long-time standard – or to cryoablation, a newer technology. Radiofrequency ablation was guided by three-dimensional electroanatomic mapping, while cryoablation utilized fluoroscopic guidance.
The primary efficacy endpoint was the 1-year rate of clinical failure, defined as an occurrence of AF, atrial flutter, or atrial tachycardia lasting for at least 30 seconds, or repeat ablation or the use of antiarrhythmic drugs following a 90-day postprocedural blanking period. The clinical failure rate was 34.6% in the cryoballoon group and similar at 35.9% in the radiofrequency group.
Serious treatment-related adverse events occurred in 10.2% of the cryoballoon group and 12.8% of the radiofrequency group, a nonsignificant difference. No procedural deaths occurred in the study.
There were, however, several significant procedural differences. Procedure time averaged 124 minutes in the cryoablation group, nearly 20 minutes less than the 142 minutes for radiofrequency ablation. However, the 17-minute fluoroscopy time in the radiofrequency group was 5 minutes shorter than for cryoablation.
Dr. Kuck said the study underestimates the true procedural differences because FIRE AND ICE was carried out by extremely experienced operators. In routine clinical practice involving non-elite operators, it’s not unusual for radiofrequency ablation fluoroscopy times to be two or even three times longer than the 17 minutes seen in the study. Plus, FIRE AND ICE was conducted when the procedure entailed two applications of the cryoballoon. Now only one application is recommended, cutting an additional 12 minutes off the total procedure time, he added.
Radiofrequency ablation takes longer because it entails creating a series of point-to-point lesions in a circle to isolate the pulmonary veins. With cryoablation, the balloon is moved into position, inflated, and a 3-minute-freeze is administered to create a circle of necrotic tissue in a single-step procedure.
Discussant Dr. Hugh G. Calkins praised the FIRE AND ICE investigators’ use of a rigorous definition of recurrence that required as little as a 30-second episode of atrial arrhythmia.
“That’s a very high bar, so I think the results are very impressive,” said Dr. Calkins, professor of medicine and of pediatrics and director of the cardiac arrhythmia service at Johns Hopkins University, Baltimore.
He commented that “this study is a clear reminder that 90% success rates just don’t happen in this field,” despite what some practitioners have claimed.
Asked how he predicts the study results will influence the field of AF ablation, Dr. Kuck replied that he foresees much wider adoption of cryoablation and a stronger endorsement of the technology in updated guideline recommendations.
“I personally believe this will be the most important development in our field in the next several years,” he added.
The electrophysiologist noted that even though current guidelines give a class Ia recommendation to catheter ablation of paroxysmal AF that’s refractory to at least one antiarrhythmic drug, at present only 4% of such patients actually undergo the procedure.
“Having just 4% of patients with AF undergo catheter ablation cannot be what we are looking for as physicians,” Dr. Kuck said. “I believe if we want to roll out catheter ablation for AF, we need simple and safe tools. This trial elegantly shows that with a simpler device that allows single-shot isolation of the pulmonary veins, we can get the same safety and efficacy as with radiofrequency ablation. I often tell people that radiofrequency ablation of atrial fibrillation is the most challenging procedure in all cardiology. We do this procedure from the groin in a moving heart. It’s a very complex technology.”
His dream, he continued, is that cryoablation will eventually enable patients with atrial fibrillation to be managed the same way electrophysiologists treat patients with Wolff-Parkinson-White syndrome; with the first episode, the patient goes to the electrophysiology catheterization lab for an ablation procedure.
“I think there’s a great message here: The cryoballoon will move catheter ablation from a niche procedure performed in specialized centers by the few guys in the world who can do it really well out into the broader world. To do that you need a tool that is safe, simple, and can be handled by the average doctor,” Dr. Kuck said.
Discussant Dr. Anthony DeMaria commented that it would be premature at this point to start thinking about cryoablation as a first approach to new-onset AF, given the roughly 35% clinical failure rate at 1 year seen in FIRE AND ICE. That rate doubtless would have been even higher had patients been equipped with implantable loop recorders, added Dr. DeMaria, professor of medicine at the University of California, San Diego.
Dr. Kuck conceded that the high recurrence rate is one of the great unsolved limitations of catheter ablation of AF.
“We don’t know how to get the pulmonary veins permanently isolated,” he said. “We can create acute lesions, but over time what we’ve seen is recovery of tissue and then reconduction by the pulmonary veins. I believe that 20% of the 40% recurrence rate is due to reconduction from the pulmonary veins, and the rest is probably due to triggers coming from other sites.”
The FIRE AND ICE trial was funded in part by Medtronic, which markets the Arctic Front Advance cryoablation catheter used in the study. Dr. Kuck reported serving on a speakers’ bureau for Medtronic and acting as a consultant to Biosense Webster, Edwards, and St. Jude.
Simultaneous with Dr. Kuck’s presentation at ACC 16, the results of FIRE AND ICE were published online (N Engl J Med. 2016 Apr 4. doi: 10.1056/NEJMoa1602014).
CHICAGO – The largest-ever randomized trial of catheter ablation of atrial fibrillation has ended in a draw between radiofrequency and cryoballoon ablation in safety and efficacy – and that actually represents a win for cryoablation, a simpler and far more easily mastered procedure, Dr. Karl-Heinz Kuck said at the annual meeting of the American College of Cardiology.
“We can teach physicians how to do cryoablation much more easily. That will allow more patients with atrial fibrillation to get access to catheter ablation, which is what we really need,” according to Dr. Kuck, principal investigator in the poetically named FIRE AND ICE trial and head of cardiology at St. Georg Hospital in Hamburg (Germany).
FIRE AND ICE included 769 patients in eight European countries. The participants, all of whom had antiarrhythmic drug–refractory paroxysmal atrial fibrillation (AF), were randomized to radiofrequency ablation – the long-time standard – or to cryoablation, a newer technology. Radiofrequency ablation was guided by three-dimensional electroanatomic mapping, while cryoablation utilized fluoroscopic guidance.
The primary efficacy endpoint was the 1-year rate of clinical failure, defined as an occurrence of AF, atrial flutter, or atrial tachycardia lasting for at least 30 seconds, or repeat ablation or the use of antiarrhythmic drugs following a 90-day postprocedural blanking period. The clinical failure rate was 34.6% in the cryoballoon group and similar at 35.9% in the radiofrequency group.
Serious treatment-related adverse events occurred in 10.2% of the cryoballoon group and 12.8% of the radiofrequency group, a nonsignificant difference. No procedural deaths occurred in the study.
There were, however, several significant procedural differences. Procedure time averaged 124 minutes in the cryoablation group, nearly 20 minutes less than the 142 minutes for radiofrequency ablation. However, the 17-minute fluoroscopy time in the radiofrequency group was 5 minutes shorter than for cryoablation.
Dr. Kuck said the study underestimates the true procedural differences because FIRE AND ICE was carried out by extremely experienced operators. In routine clinical practice involving non-elite operators, it’s not unusual for radiofrequency ablation fluoroscopy times to be two or even three times longer than the 17 minutes seen in the study. Plus, FIRE AND ICE was conducted when the procedure entailed two applications of the cryoballoon. Now only one application is recommended, cutting an additional 12 minutes off the total procedure time, he added.
Radiofrequency ablation takes longer because it entails creating a series of point-to-point lesions in a circle to isolate the pulmonary veins. With cryoablation, the balloon is moved into position, inflated, and a 3-minute-freeze is administered to create a circle of necrotic tissue in a single-step procedure.
Discussant Dr. Hugh G. Calkins praised the FIRE AND ICE investigators’ use of a rigorous definition of recurrence that required as little as a 30-second episode of atrial arrhythmia.
“That’s a very high bar, so I think the results are very impressive,” said Dr. Calkins, professor of medicine and of pediatrics and director of the cardiac arrhythmia service at Johns Hopkins University, Baltimore.
He commented that “this study is a clear reminder that 90% success rates just don’t happen in this field,” despite what some practitioners have claimed.
Asked how he predicts the study results will influence the field of AF ablation, Dr. Kuck replied that he foresees much wider adoption of cryoablation and a stronger endorsement of the technology in updated guideline recommendations.
“I personally believe this will be the most important development in our field in the next several years,” he added.
The electrophysiologist noted that even though current guidelines give a class Ia recommendation to catheter ablation of paroxysmal AF that’s refractory to at least one antiarrhythmic drug, at present only 4% of such patients actually undergo the procedure.
“Having just 4% of patients with AF undergo catheter ablation cannot be what we are looking for as physicians,” Dr. Kuck said. “I believe if we want to roll out catheter ablation for AF, we need simple and safe tools. This trial elegantly shows that with a simpler device that allows single-shot isolation of the pulmonary veins, we can get the same safety and efficacy as with radiofrequency ablation. I often tell people that radiofrequency ablation of atrial fibrillation is the most challenging procedure in all cardiology. We do this procedure from the groin in a moving heart. It’s a very complex technology.”
His dream, he continued, is that cryoablation will eventually enable patients with atrial fibrillation to be managed the same way electrophysiologists treat patients with Wolff-Parkinson-White syndrome; with the first episode, the patient goes to the electrophysiology catheterization lab for an ablation procedure.
“I think there’s a great message here: The cryoballoon will move catheter ablation from a niche procedure performed in specialized centers by the few guys in the world who can do it really well out into the broader world. To do that you need a tool that is safe, simple, and can be handled by the average doctor,” Dr. Kuck said.
Discussant Dr. Anthony DeMaria commented that it would be premature at this point to start thinking about cryoablation as a first approach to new-onset AF, given the roughly 35% clinical failure rate at 1 year seen in FIRE AND ICE. That rate doubtless would have been even higher had patients been equipped with implantable loop recorders, added Dr. DeMaria, professor of medicine at the University of California, San Diego.
Dr. Kuck conceded that the high recurrence rate is one of the great unsolved limitations of catheter ablation of AF.
“We don’t know how to get the pulmonary veins permanently isolated,” he said. “We can create acute lesions, but over time what we’ve seen is recovery of tissue and then reconduction by the pulmonary veins. I believe that 20% of the 40% recurrence rate is due to reconduction from the pulmonary veins, and the rest is probably due to triggers coming from other sites.”
The FIRE AND ICE trial was funded in part by Medtronic, which markets the Arctic Front Advance cryoablation catheter used in the study. Dr. Kuck reported serving on a speakers’ bureau for Medtronic and acting as a consultant to Biosense Webster, Edwards, and St. Jude.
Simultaneous with Dr. Kuck’s presentation at ACC 16, the results of FIRE AND ICE were published online (N Engl J Med. 2016 Apr 4. doi: 10.1056/NEJMoa1602014).
AT ACC 16
Key clinical point: Cryoablation of atrial fibrillation offers significant advantages over radiofrequency ablation.
Major finding: In a rigorous randomized trial, cryoablation of atrial fibrillation had a 34.6% clinical failure rate at 1 year, similar to the 35.9% rate for radiofrequency ablation.
Data source: The FIRE AND ICE trial, which randomized 769 patients with paroxysmal atrial fibrillation in eight European countries.
Disclosures: FIRE AND ICE was funded in part by Medtronic. The presenter reported serving on a speakers’ bureau for the company.
VIDEO: Sapien 3 TAVR bests surgery in intermediate-risk patients
CHICAGO – Transcatheter aortic valve replacement (TAVR) using Sapien 3 – the latest-generation valve – is associated with low mortality, stroke, and paravalvular regurgitation rates at 1 year in intermediate-risk patients, and is superior to surgical valve replacement, according to findings from the SAPIEN 3 study.
The mortality rate at 1 year in the 1,077 patients in the observational study was 7.4% overall and 6.5% in a transfemoral access subgroup, the disabling stroke rate was 2.3%, the aortic valve reintervention rate was 0.6%, and the moderate/severe paravalvular regurgitation rate was 1.5%, Dr. Vinod H. Thourani reported on behalf of the PARTNER trial investigators at the annual meeting of the American College of Cardiology. The findings were published simultaneously in The Lancet (2016 Apr 3. doi: 10.1016/So140-6736[19]30073-3).
A prespecified propensity score analysis comparing 963 SAPIEN 3 patients with 747 similar intermediate-risk patients from the PARTNER 2A trial who underwent surgical valve replacement showed that not only was Sapien 3 TAVR noninferior to surgery for the primary composite endpoint of mortality, strokes, and moderate or severe aortic regurgitation, it was also superior to surgery (pooled weighted proportion difference, –9.2% for each). The differences were highly statistically significant.
In fact, Sapien 3 TAVR “blew it out of the water” for both noninferiority and superiority vs. surgery, Dr. Thourani of Emory University, Atlanta said.
The propensity score incorporated 22 characteristics, and the analysis was conducted by blinded investigators. Even using the most conservative strategy for the analysis as approved by the Food and Drug Administration, with the heaviest weighting against TAVR, Sapien 3 TAVR was superior to surgery for the primary composite endpoint, he noted.
Of note, while Sapien 3 TAVR was superior for the individual components of mortality and stroke from the composite endpoint, surgery was superior to Sapien 3 TAVR for the component of moderate or greater aortic regurgitation, he said.
However, the findings represent “strong evidence that in intermediate-risk patients with severe aortic stenosis, SAPIEN 3, compared to surgery, improves clinical outcomes and is the preferred therapy,” he concluded.
In a video interview, he said that if approved by the FDA, “this will become the impetus for [use in] a lower-risk population of patients. Currently we have the inoperative and high-risk patients, and this will open up the intermediate-risk patients for having transcatheter valve therapies, and I think it becomes exceedingly powerful.”
Two ongoing industry-sponsored randomized trials in low-risk patients (those with a Society of Thoracic Surgeons score of less than 4) are underway, he noted.
Sapien 3 TAVR was previously shown to improve 30-day outcomes in intermediate-risk patients with severe aortic stenosis (Eur Heart J. 2016 Mar 31. doi: 10.1093/eurheartj/ehw112), but longer-term data were lacking, and no comparisons with surgery in intermediate-risk patients were available.
For the current study, patients with a mean age of 82 years were evaluated at 51 centers in the United States and Canada during February-September 2014. Subjects had a median Society of Thoracic Surgeons score of 5.2% (range, 4-8) and 73% had New York Heart Association class III/IV heart failure. Almost 90% were treated via the transfemoral route, Dr. Thourani said.
The Sapien 3 device is a balloon expandable valve that differs from prior-generation devices in that it has improved geometry of the trileaflet bovine pericardial valve, a longer cobalt alloy frame with more open outlet cells and denser inlet cells, a polyethylene terephthalate fabric skirt that provides an external circumferential seal to reduce paravalvular leak, four valve sizes, and lower-profile delivery catheters with more precise valve positioning inserted through 14 or 16 French sheaths for increased use of transfemoral access.
Discussant Dr. David E. Kandzari, director of interventional cardiology and chief scientific officer at Piedmont Heart Institute, Atlanta, congratulated Dr. Thourani and his colleagues on “a terrific trial and impactful result.”
“There are, with regard to the Sapien 3 technology, many reasons to believe that this could be an advancement above existing predicate technologies,” he said, specifically mentioning the improvements in the device, compared with prior generations, such as the modification to reduce paravalvular leak, which has been associated with worse outcomes for patients.
“In parallel, there were changes in practice, and one of them implemented in the context of SAPIEN 3 was the use of [computed tomography] imaging to help guide and inform the procedure itself,” he said, adding that the results of the trial “really open the door for at least two very broad pathways.”
First, they expand TAVR to intermediate-risk patients.
“Secondly, they lead the way even further with greater reassurance toward two large ongoing clinical trials in patients considered at low risk, as well,” he said.
The remarkable outcomes in regard to mortality and stroke are “clinically meaningful and some of the best outcomes we’ve ever witnessed with transcatheter therapy,” he said.
This study was funded by Edwards Lifesciences. Dr. Thourani disclosed that he has received consulting fees and/or research grants from Edwards Lifesciences, St. Jude Medical, Abbott Medical, Boston Scientific, Claret Medical, DirectFlow, Medtronic, and Sorin. Dr. Kandzari has received consultant fees and honoraria from Boston Scientific, The Medicines Company, and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Transcatheter aortic valve replacement (TAVR) using Sapien 3 – the latest-generation valve – is associated with low mortality, stroke, and paravalvular regurgitation rates at 1 year in intermediate-risk patients, and is superior to surgical valve replacement, according to findings from the SAPIEN 3 study.
The mortality rate at 1 year in the 1,077 patients in the observational study was 7.4% overall and 6.5% in a transfemoral access subgroup, the disabling stroke rate was 2.3%, the aortic valve reintervention rate was 0.6%, and the moderate/severe paravalvular regurgitation rate was 1.5%, Dr. Vinod H. Thourani reported on behalf of the PARTNER trial investigators at the annual meeting of the American College of Cardiology. The findings were published simultaneously in The Lancet (2016 Apr 3. doi: 10.1016/So140-6736[19]30073-3).
A prespecified propensity score analysis comparing 963 SAPIEN 3 patients with 747 similar intermediate-risk patients from the PARTNER 2A trial who underwent surgical valve replacement showed that not only was Sapien 3 TAVR noninferior to surgery for the primary composite endpoint of mortality, strokes, and moderate or severe aortic regurgitation, it was also superior to surgery (pooled weighted proportion difference, –9.2% for each). The differences were highly statistically significant.
In fact, Sapien 3 TAVR “blew it out of the water” for both noninferiority and superiority vs. surgery, Dr. Thourani of Emory University, Atlanta said.
The propensity score incorporated 22 characteristics, and the analysis was conducted by blinded investigators. Even using the most conservative strategy for the analysis as approved by the Food and Drug Administration, with the heaviest weighting against TAVR, Sapien 3 TAVR was superior to surgery for the primary composite endpoint, he noted.
Of note, while Sapien 3 TAVR was superior for the individual components of mortality and stroke from the composite endpoint, surgery was superior to Sapien 3 TAVR for the component of moderate or greater aortic regurgitation, he said.
However, the findings represent “strong evidence that in intermediate-risk patients with severe aortic stenosis, SAPIEN 3, compared to surgery, improves clinical outcomes and is the preferred therapy,” he concluded.
In a video interview, he said that if approved by the FDA, “this will become the impetus for [use in] a lower-risk population of patients. Currently we have the inoperative and high-risk patients, and this will open up the intermediate-risk patients for having transcatheter valve therapies, and I think it becomes exceedingly powerful.”
Two ongoing industry-sponsored randomized trials in low-risk patients (those with a Society of Thoracic Surgeons score of less than 4) are underway, he noted.
Sapien 3 TAVR was previously shown to improve 30-day outcomes in intermediate-risk patients with severe aortic stenosis (Eur Heart J. 2016 Mar 31. doi: 10.1093/eurheartj/ehw112), but longer-term data were lacking, and no comparisons with surgery in intermediate-risk patients were available.
For the current study, patients with a mean age of 82 years were evaluated at 51 centers in the United States and Canada during February-September 2014. Subjects had a median Society of Thoracic Surgeons score of 5.2% (range, 4-8) and 73% had New York Heart Association class III/IV heart failure. Almost 90% were treated via the transfemoral route, Dr. Thourani said.
The Sapien 3 device is a balloon expandable valve that differs from prior-generation devices in that it has improved geometry of the trileaflet bovine pericardial valve, a longer cobalt alloy frame with more open outlet cells and denser inlet cells, a polyethylene terephthalate fabric skirt that provides an external circumferential seal to reduce paravalvular leak, four valve sizes, and lower-profile delivery catheters with more precise valve positioning inserted through 14 or 16 French sheaths for increased use of transfemoral access.
Discussant Dr. David E. Kandzari, director of interventional cardiology and chief scientific officer at Piedmont Heart Institute, Atlanta, congratulated Dr. Thourani and his colleagues on “a terrific trial and impactful result.”
“There are, with regard to the Sapien 3 technology, many reasons to believe that this could be an advancement above existing predicate technologies,” he said, specifically mentioning the improvements in the device, compared with prior generations, such as the modification to reduce paravalvular leak, which has been associated with worse outcomes for patients.
“In parallel, there were changes in practice, and one of them implemented in the context of SAPIEN 3 was the use of [computed tomography] imaging to help guide and inform the procedure itself,” he said, adding that the results of the trial “really open the door for at least two very broad pathways.”
First, they expand TAVR to intermediate-risk patients.
“Secondly, they lead the way even further with greater reassurance toward two large ongoing clinical trials in patients considered at low risk, as well,” he said.
The remarkable outcomes in regard to mortality and stroke are “clinically meaningful and some of the best outcomes we’ve ever witnessed with transcatheter therapy,” he said.
This study was funded by Edwards Lifesciences. Dr. Thourani disclosed that he has received consulting fees and/or research grants from Edwards Lifesciences, St. Jude Medical, Abbott Medical, Boston Scientific, Claret Medical, DirectFlow, Medtronic, and Sorin. Dr. Kandzari has received consultant fees and honoraria from Boston Scientific, The Medicines Company, and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Transcatheter aortic valve replacement (TAVR) using Sapien 3 – the latest-generation valve – is associated with low mortality, stroke, and paravalvular regurgitation rates at 1 year in intermediate-risk patients, and is superior to surgical valve replacement, according to findings from the SAPIEN 3 study.
The mortality rate at 1 year in the 1,077 patients in the observational study was 7.4% overall and 6.5% in a transfemoral access subgroup, the disabling stroke rate was 2.3%, the aortic valve reintervention rate was 0.6%, and the moderate/severe paravalvular regurgitation rate was 1.5%, Dr. Vinod H. Thourani reported on behalf of the PARTNER trial investigators at the annual meeting of the American College of Cardiology. The findings were published simultaneously in The Lancet (2016 Apr 3. doi: 10.1016/So140-6736[19]30073-3).
A prespecified propensity score analysis comparing 963 SAPIEN 3 patients with 747 similar intermediate-risk patients from the PARTNER 2A trial who underwent surgical valve replacement showed that not only was Sapien 3 TAVR noninferior to surgery for the primary composite endpoint of mortality, strokes, and moderate or severe aortic regurgitation, it was also superior to surgery (pooled weighted proportion difference, –9.2% for each). The differences were highly statistically significant.
In fact, Sapien 3 TAVR “blew it out of the water” for both noninferiority and superiority vs. surgery, Dr. Thourani of Emory University, Atlanta said.
The propensity score incorporated 22 characteristics, and the analysis was conducted by blinded investigators. Even using the most conservative strategy for the analysis as approved by the Food and Drug Administration, with the heaviest weighting against TAVR, Sapien 3 TAVR was superior to surgery for the primary composite endpoint, he noted.
Of note, while Sapien 3 TAVR was superior for the individual components of mortality and stroke from the composite endpoint, surgery was superior to Sapien 3 TAVR for the component of moderate or greater aortic regurgitation, he said.
However, the findings represent “strong evidence that in intermediate-risk patients with severe aortic stenosis, SAPIEN 3, compared to surgery, improves clinical outcomes and is the preferred therapy,” he concluded.
In a video interview, he said that if approved by the FDA, “this will become the impetus for [use in] a lower-risk population of patients. Currently we have the inoperative and high-risk patients, and this will open up the intermediate-risk patients for having transcatheter valve therapies, and I think it becomes exceedingly powerful.”
Two ongoing industry-sponsored randomized trials in low-risk patients (those with a Society of Thoracic Surgeons score of less than 4) are underway, he noted.
Sapien 3 TAVR was previously shown to improve 30-day outcomes in intermediate-risk patients with severe aortic stenosis (Eur Heart J. 2016 Mar 31. doi: 10.1093/eurheartj/ehw112), but longer-term data were lacking, and no comparisons with surgery in intermediate-risk patients were available.
For the current study, patients with a mean age of 82 years were evaluated at 51 centers in the United States and Canada during February-September 2014. Subjects had a median Society of Thoracic Surgeons score of 5.2% (range, 4-8) and 73% had New York Heart Association class III/IV heart failure. Almost 90% were treated via the transfemoral route, Dr. Thourani said.
The Sapien 3 device is a balloon expandable valve that differs from prior-generation devices in that it has improved geometry of the trileaflet bovine pericardial valve, a longer cobalt alloy frame with more open outlet cells and denser inlet cells, a polyethylene terephthalate fabric skirt that provides an external circumferential seal to reduce paravalvular leak, four valve sizes, and lower-profile delivery catheters with more precise valve positioning inserted through 14 or 16 French sheaths for increased use of transfemoral access.
Discussant Dr. David E. Kandzari, director of interventional cardiology and chief scientific officer at Piedmont Heart Institute, Atlanta, congratulated Dr. Thourani and his colleagues on “a terrific trial and impactful result.”
“There are, with regard to the Sapien 3 technology, many reasons to believe that this could be an advancement above existing predicate technologies,” he said, specifically mentioning the improvements in the device, compared with prior generations, such as the modification to reduce paravalvular leak, which has been associated with worse outcomes for patients.
“In parallel, there were changes in practice, and one of them implemented in the context of SAPIEN 3 was the use of [computed tomography] imaging to help guide and inform the procedure itself,” he said, adding that the results of the trial “really open the door for at least two very broad pathways.”
First, they expand TAVR to intermediate-risk patients.
“Secondly, they lead the way even further with greater reassurance toward two large ongoing clinical trials in patients considered at low risk, as well,” he said.
The remarkable outcomes in regard to mortality and stroke are “clinically meaningful and some of the best outcomes we’ve ever witnessed with transcatheter therapy,” he said.
This study was funded by Edwards Lifesciences. Dr. Thourani disclosed that he has received consulting fees and/or research grants from Edwards Lifesciences, St. Jude Medical, Abbott Medical, Boston Scientific, Claret Medical, DirectFlow, Medtronic, and Sorin. Dr. Kandzari has received consultant fees and honoraria from Boston Scientific, The Medicines Company, and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACC 16
Key clinical point: Transcatheter aortic valve replacement using Sapien 3 is associated with low mortality, stroke, and paravalvular regurgitation rates at 1 year in intermediate-risk patients, and is superior to surgical valve replacement.
Major finding: A propensity score analysis showed that Sapien 3 TAVR was superior to surgical valve replacement (pooled weighted proportion difference, –9.2%).
Data source: An observational study of 1,077 SAPIEN 3 patients, and a propensity score analysis comparing 963 SAPIEN 3 patients and 747 surgical valve replacement patients.
Disclosures: SAPIEN 3 was funded by Edwards Lifesciences. Dr. Thourani disclosed that he has received consulting fees from Edwards Lifesciences and St. Jude Medical, and research grants from Abbott Medical, Boston Scientific, Claret Medical, DirectFlow, Medtronic, and Sorin.
Similarities seen in rate and rhythm control for postsurgical AF
CHICAGO – Rate and rhythm control proved equally effective for treatment of new-onset post–cardiac surgery atrial fibrillation in a randomized trial that was far and away the largest ever to examine the best way to address this common and costly arrhythmia, Dr. A. Marc Gillinov said at the annual meeting of the American College of Cardiology.
Thus, either strategy is acceptable. That being said, rate control gets the edge as the initial treatment strategy because it avoids the considerable toxicities accompanying amiodarone for rhythm control, most of which arise only after patients have been discharged from the hospital. In contrast, when rate control doesn’t work, it becomes evident while the patient is still in the hospital, according to Dr. Gillinov, a cardiothoracic surgeon at the Cleveland Clinic .
Atrial fibrillation (AF) is the most common complication of cardiac surgery, with an incidence variously reported at 20%-50%. It results in lengthier hospital stays, greater cost of care, and increased risks of mortality, stroke, heart failure, and infection. Postoperative AF adds an estimated $1 billion per year to health care costs in the United States.
While current ACC/AHA/Heart Rhythm Society joint guidelines recommend rate control with a beta-blocker as first-line therapy for patients with this postoperative complication, with a class I, level-of-evidence A rating, upon closer inspection the evidence cited mainly involves extrapolation from studies looking at how to prevent postoperative AF. Because no persuasive evidence existed as to how best to treat this common and economically and medically costly condition, Dr. Gillinov and his coinvestigators in the National Institutes of Health–funded Cardiothoracic Surgical Trials Network carried out a randomized trial 10-fold larger than anything prior.
The 23-site study included 2,109 patients enrolled prior to cardiac surgery, of whom 40% underwent isolated coronary artery bypass grafting (CABG) while the other 60% had valve surgery, either alone or with CABG. These proportions reflect current cardiac surgery treatment patterns nationally. Overall, 33% of the cardiac surgery patients experienced postoperative AF. The incidence was 28% in patients who underwent isolated CABG but rose with increasing surgical complexity to nearly 50% in patients who had combined CABG and valve operations. The average time to onset of postoperative AF was 2.4 days.
A total of 523 patients with postoperative AF were randomized to rate or rhythm control. Rate control most often entailed use of a beta-blocker, while amiodarone was prescribed for rhythm control.
The primary endpoint in the trial was a measure of health care resource utilization: total days in hospital during a 60-day period starting from the time of randomization. This endpoint was a draw: a median of 5.1 days with rate control and 5.0 days with rhythm control.
At hospital discharge, 89.9% of patients in the rate control group and 93.5% in the rhythm control group had a stable heart rhythm without AF. From discharge to 60 days, 84.2% of patients in the rate control group and a similar 86.9% of the rhythm control group remained free of AF.
Rates of serious adverse events were similar in the two groups: 24.8 per 100 patient-months in the rate control arm and 26.4 per 100 patient-months in the rhythm control arm. Three patients in the rate control arm died during the 60-day study period, and two died in the rhythm control group.
Of note, roughly one-quarter of patients in each study arm crossed over to the other arm. In the rate control group, this was typically due to drug ineffectiveness, while in the rhythm control arm the switch was most often made in response to amiodarone side effects.
Roughly 43% of patients in each group were placed on anticoagulation with warfarin for 60 days according to study protocol, which called for such action if a patient remained in AF 48 hours after randomization.
There were five strokes, one case of transient ischemic attack, and four noncerebral thromboembolisms. Also, 21 bleeding events occurred, 17 of which were classified as serious; 90% of the bleeding events happened in patients on warfarin.
“I found the results very striking and very reassuring,” said discussant Hugh G. Calkins. “To me, the clinical message is clearly that rate control is the preference.”
It was troubling, however, to see that 10 thromboembolic events occurred in 523 patients over the course of just 60 days. “Should we be anticoagulating these postsurgical atrial fibrillation patients a lot more frequently?” asked Dr. Calkins, professor of medicine and of pediatrics and director of the cardiac arrhythmia service at Johns Hopkins University, Baltimore.
Dr. Gillinov replied that he and his colleagues in the Cardiothoracic Surgical Trials Network consider that to be the key remaining question regarding postoperative AF. They are now planning a clinical trial aimed at finding the optimal balance between stroke protection via anticoagulation and bleeding risk.
The National Institutes of Health and the Canadian Institutes of Health Research funded the work. Dr. Gillinov reported serving as a consultant to five surgical device companies, none of which played any role in the study.
Simultaneously with Dr. Gillinov’s presentation at ACC 16, the study results were published in the New England Journal of Medicine (doi: 10.1056/NEJMoa1602002).
CHICAGO – Rate and rhythm control proved equally effective for treatment of new-onset post–cardiac surgery atrial fibrillation in a randomized trial that was far and away the largest ever to examine the best way to address this common and costly arrhythmia, Dr. A. Marc Gillinov said at the annual meeting of the American College of Cardiology.
Thus, either strategy is acceptable. That being said, rate control gets the edge as the initial treatment strategy because it avoids the considerable toxicities accompanying amiodarone for rhythm control, most of which arise only after patients have been discharged from the hospital. In contrast, when rate control doesn’t work, it becomes evident while the patient is still in the hospital, according to Dr. Gillinov, a cardiothoracic surgeon at the Cleveland Clinic .
Atrial fibrillation (AF) is the most common complication of cardiac surgery, with an incidence variously reported at 20%-50%. It results in lengthier hospital stays, greater cost of care, and increased risks of mortality, stroke, heart failure, and infection. Postoperative AF adds an estimated $1 billion per year to health care costs in the United States.
While current ACC/AHA/Heart Rhythm Society joint guidelines recommend rate control with a beta-blocker as first-line therapy for patients with this postoperative complication, with a class I, level-of-evidence A rating, upon closer inspection the evidence cited mainly involves extrapolation from studies looking at how to prevent postoperative AF. Because no persuasive evidence existed as to how best to treat this common and economically and medically costly condition, Dr. Gillinov and his coinvestigators in the National Institutes of Health–funded Cardiothoracic Surgical Trials Network carried out a randomized trial 10-fold larger than anything prior.
The 23-site study included 2,109 patients enrolled prior to cardiac surgery, of whom 40% underwent isolated coronary artery bypass grafting (CABG) while the other 60% had valve surgery, either alone or with CABG. These proportions reflect current cardiac surgery treatment patterns nationally. Overall, 33% of the cardiac surgery patients experienced postoperative AF. The incidence was 28% in patients who underwent isolated CABG but rose with increasing surgical complexity to nearly 50% in patients who had combined CABG and valve operations. The average time to onset of postoperative AF was 2.4 days.
A total of 523 patients with postoperative AF were randomized to rate or rhythm control. Rate control most often entailed use of a beta-blocker, while amiodarone was prescribed for rhythm control.
The primary endpoint in the trial was a measure of health care resource utilization: total days in hospital during a 60-day period starting from the time of randomization. This endpoint was a draw: a median of 5.1 days with rate control and 5.0 days with rhythm control.
At hospital discharge, 89.9% of patients in the rate control group and 93.5% in the rhythm control group had a stable heart rhythm without AF. From discharge to 60 days, 84.2% of patients in the rate control group and a similar 86.9% of the rhythm control group remained free of AF.
Rates of serious adverse events were similar in the two groups: 24.8 per 100 patient-months in the rate control arm and 26.4 per 100 patient-months in the rhythm control arm. Three patients in the rate control arm died during the 60-day study period, and two died in the rhythm control group.
Of note, roughly one-quarter of patients in each study arm crossed over to the other arm. In the rate control group, this was typically due to drug ineffectiveness, while in the rhythm control arm the switch was most often made in response to amiodarone side effects.
Roughly 43% of patients in each group were placed on anticoagulation with warfarin for 60 days according to study protocol, which called for such action if a patient remained in AF 48 hours after randomization.
There were five strokes, one case of transient ischemic attack, and four noncerebral thromboembolisms. Also, 21 bleeding events occurred, 17 of which were classified as serious; 90% of the bleeding events happened in patients on warfarin.
“I found the results very striking and very reassuring,” said discussant Hugh G. Calkins. “To me, the clinical message is clearly that rate control is the preference.”
It was troubling, however, to see that 10 thromboembolic events occurred in 523 patients over the course of just 60 days. “Should we be anticoagulating these postsurgical atrial fibrillation patients a lot more frequently?” asked Dr. Calkins, professor of medicine and of pediatrics and director of the cardiac arrhythmia service at Johns Hopkins University, Baltimore.
Dr. Gillinov replied that he and his colleagues in the Cardiothoracic Surgical Trials Network consider that to be the key remaining question regarding postoperative AF. They are now planning a clinical trial aimed at finding the optimal balance between stroke protection via anticoagulation and bleeding risk.
The National Institutes of Health and the Canadian Institutes of Health Research funded the work. Dr. Gillinov reported serving as a consultant to five surgical device companies, none of which played any role in the study.
Simultaneously with Dr. Gillinov’s presentation at ACC 16, the study results were published in the New England Journal of Medicine (doi: 10.1056/NEJMoa1602002).
CHICAGO – Rate and rhythm control proved equally effective for treatment of new-onset post–cardiac surgery atrial fibrillation in a randomized trial that was far and away the largest ever to examine the best way to address this common and costly arrhythmia, Dr. A. Marc Gillinov said at the annual meeting of the American College of Cardiology.
Thus, either strategy is acceptable. That being said, rate control gets the edge as the initial treatment strategy because it avoids the considerable toxicities accompanying amiodarone for rhythm control, most of which arise only after patients have been discharged from the hospital. In contrast, when rate control doesn’t work, it becomes evident while the patient is still in the hospital, according to Dr. Gillinov, a cardiothoracic surgeon at the Cleveland Clinic .
Atrial fibrillation (AF) is the most common complication of cardiac surgery, with an incidence variously reported at 20%-50%. It results in lengthier hospital stays, greater cost of care, and increased risks of mortality, stroke, heart failure, and infection. Postoperative AF adds an estimated $1 billion per year to health care costs in the United States.
While current ACC/AHA/Heart Rhythm Society joint guidelines recommend rate control with a beta-blocker as first-line therapy for patients with this postoperative complication, with a class I, level-of-evidence A rating, upon closer inspection the evidence cited mainly involves extrapolation from studies looking at how to prevent postoperative AF. Because no persuasive evidence existed as to how best to treat this common and economically and medically costly condition, Dr. Gillinov and his coinvestigators in the National Institutes of Health–funded Cardiothoracic Surgical Trials Network carried out a randomized trial 10-fold larger than anything prior.
The 23-site study included 2,109 patients enrolled prior to cardiac surgery, of whom 40% underwent isolated coronary artery bypass grafting (CABG) while the other 60% had valve surgery, either alone or with CABG. These proportions reflect current cardiac surgery treatment patterns nationally. Overall, 33% of the cardiac surgery patients experienced postoperative AF. The incidence was 28% in patients who underwent isolated CABG but rose with increasing surgical complexity to nearly 50% in patients who had combined CABG and valve operations. The average time to onset of postoperative AF was 2.4 days.
A total of 523 patients with postoperative AF were randomized to rate or rhythm control. Rate control most often entailed use of a beta-blocker, while amiodarone was prescribed for rhythm control.
The primary endpoint in the trial was a measure of health care resource utilization: total days in hospital during a 60-day period starting from the time of randomization. This endpoint was a draw: a median of 5.1 days with rate control and 5.0 days with rhythm control.
At hospital discharge, 89.9% of patients in the rate control group and 93.5% in the rhythm control group had a stable heart rhythm without AF. From discharge to 60 days, 84.2% of patients in the rate control group and a similar 86.9% of the rhythm control group remained free of AF.
Rates of serious adverse events were similar in the two groups: 24.8 per 100 patient-months in the rate control arm and 26.4 per 100 patient-months in the rhythm control arm. Three patients in the rate control arm died during the 60-day study period, and two died in the rhythm control group.
Of note, roughly one-quarter of patients in each study arm crossed over to the other arm. In the rate control group, this was typically due to drug ineffectiveness, while in the rhythm control arm the switch was most often made in response to amiodarone side effects.
Roughly 43% of patients in each group were placed on anticoagulation with warfarin for 60 days according to study protocol, which called for such action if a patient remained in AF 48 hours after randomization.
There were five strokes, one case of transient ischemic attack, and four noncerebral thromboembolisms. Also, 21 bleeding events occurred, 17 of which were classified as serious; 90% of the bleeding events happened in patients on warfarin.
“I found the results very striking and very reassuring,” said discussant Hugh G. Calkins. “To me, the clinical message is clearly that rate control is the preference.”
It was troubling, however, to see that 10 thromboembolic events occurred in 523 patients over the course of just 60 days. “Should we be anticoagulating these postsurgical atrial fibrillation patients a lot more frequently?” asked Dr. Calkins, professor of medicine and of pediatrics and director of the cardiac arrhythmia service at Johns Hopkins University, Baltimore.
Dr. Gillinov replied that he and his colleagues in the Cardiothoracic Surgical Trials Network consider that to be the key remaining question regarding postoperative AF. They are now planning a clinical trial aimed at finding the optimal balance between stroke protection via anticoagulation and bleeding risk.
The National Institutes of Health and the Canadian Institutes of Health Research funded the work. Dr. Gillinov reported serving as a consultant to five surgical device companies, none of which played any role in the study.
Simultaneously with Dr. Gillinov’s presentation at ACC 16, the study results were published in the New England Journal of Medicine (doi: 10.1056/NEJMoa1602002).
AT ACC 16
Key clinical point: Rate control offers the advantage of simplicity over a rhythm control strategy in new-onset atrial fibrillation after cardiac surgery.
Major finding: Rate and rhythm control strategies for treatment of new-onset atrial fibrillation after cardiac surgery resulted in equal numbers of hospital days, similar serious complication rates, and low rates of persistent atrial fibrillation at 60 days of follow-up.
Data source: A randomized clinical trial of 523 patients with new-onset atrial fibrillation following cardiac surgery at 23 U.S. and Canadian academic medical centers.
Disclosures: The study was funded by the National Institutes of Health and the Canadian Institutes of Health Research and carried out through the Cardiothoracic Surgical Trials Network. The presenter reported having no relevant financial interests.
Could value-based care raise False Claims Act liability?
As you begin to consider the switch to value-based care systems, be sure to safeguard against risks that could fuel false claims scrutiny by the government, legal experts advise.
A primary consideration is arrangements that include shared savings through coordinated care, said George B. Breen, a Washington-based health law attorney. For example, he said that the Stark Law could be implicated if a physician within a shared savings model receives a bonus payment for referring patients to specific providers. The Stark Law prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician has a financial relationship.
“While there are a number of exceptions and safe harbors which would validate any such relationship, it’s something that needs to be thought through” from the start, Mr. Breen said in an interview. “You have to look at each factual circumstance separately because each is fact and circumstance dependent.”
The Anti-Kickback Statute also could come into play if value-based arrangements generate renumeration. The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business. Exceptions to the statute can be applied and should also be examined during arrangement development, Mr. Breen said.
Data collection and reporting also may present a problem, according to Seattle-based health law attorney Robert G. Homchick. Inaccurate data that become the basis for quality-based payments could lead to overpayment liability and indirect False Claims Act (FCA) exposure, he said.
In addition, “If the facts support that you were acting with intentional or deliberate ignorance or reckless disregard for how the data were gathered and reported that supported your value-based comp kicker, there could be direct False Claims Act liability,” Mr. Homchick said in an interview.
But Mr. Homchick stressed there are still many unknowns when it comes to how data-driven measurements will unfold.
“With MACRA, this is such a moving target as to exactly what type of data is going to form the basis for the metrics, and how the data need to be gathered and reported,” he said. “Many of those issues are still in play or still being developed at the agency level in terms of regulatory guidance.”
Current lawsuit could influence future cases
While it is too early to know every legal theory that could intersect with quality-based care, legal experts are closely watching a case that could offer insight into future claims.
In Duffy v. Lawrence Memorial Hospital, a former employee turned whistle-blower alleges that the Lawrence, Kan.–based hospital inflated its performance scores under the Hospital Value-Based Purchasing Program to increase federal incentive payments. Hospital leaders deny they falsified data and claim the allegations are based on the whistle-blower’s “improper understanding of acceptable reporting times for patient arrival,” according the hospital’s court response. The FCA lawsuit is before the U.S. District Court for the District of Kansas.
Notably, the government has declined to intervene in the lawsuit twice, Mr. Breen said. The case is continuing without government intervention, a trend that has become more common in recent years, he said. In 2015, whistle-blower cases in which U.S. Department of Justice declined to intervene led to $1.1 billion in recoveries for the government and $335 million in rewards for whistle-blowers, according to government data.
Mr. Homchick called the Lawrence Memorial lawsuit “troubling.”
“Providers are struggling with the complexity of the reporting requirements imposed by the layers of value-based payment programs implemented by both government and private payers,” he said. “The Lawrence Memorial case illustrates that the whistle-blower community will likely exploit the inevitable mistakes or missteps of providers attempting to comply with the increasingly byzantine quality-reporting requirements.”
The outcome of the Lawrence Memorial case could influence similar lawsuits involving value-based programs, Mr. Breen said.
“I think this theory that there is some false reporting, or false certification, is a theory that you will see being pursed in connection with some of these quality-based programs,” Mr. Breen said.
Early steps can curb legal risk
Asking questions and being proactive as new value-based models develop is key to mitigating legal dangers, experts said.
Ensure that new arrangements are analyzed for fraud and abuse risk exposure before finalizing, Mr. Breen advised.
“Have a comfort level about the arrangement” that’s being entered into, he added, and “have those arrangements vetted.”
Pay attention to data, added Michael E. Paulhus, an Atlanta-based health law attorney who specializes in FCA cases.
“The more data they collect, the more the government is paying attention to where you are in the range,” he said in an interview. “If you stick out on either end, that would be a risk profile that, as a physician, I would want to know. I would want to know where I sit in the data.”
When making reports regarding quality measures, include such reports in internal audits as part of regular compliance efforts, the experts suggested.
In addition, seek out resources early that can help prepare the practice for new quality-based regulations, Mr. Homchick said.
“There will be guidance coming out [regarding] eligibility for these value-based incentives,” he said. “That will require you and your staff to really pay attention and seek out resources and guidance to try to do this right. If you have the bandwidth to get out ahead of this, that would certainly be the best approach.”
On Twitter @legal_med
As you begin to consider the switch to value-based care systems, be sure to safeguard against risks that could fuel false claims scrutiny by the government, legal experts advise.
A primary consideration is arrangements that include shared savings through coordinated care, said George B. Breen, a Washington-based health law attorney. For example, he said that the Stark Law could be implicated if a physician within a shared savings model receives a bonus payment for referring patients to specific providers. The Stark Law prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician has a financial relationship.
“While there are a number of exceptions and safe harbors which would validate any such relationship, it’s something that needs to be thought through” from the start, Mr. Breen said in an interview. “You have to look at each factual circumstance separately because each is fact and circumstance dependent.”
The Anti-Kickback Statute also could come into play if value-based arrangements generate renumeration. The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business. Exceptions to the statute can be applied and should also be examined during arrangement development, Mr. Breen said.
Data collection and reporting also may present a problem, according to Seattle-based health law attorney Robert G. Homchick. Inaccurate data that become the basis for quality-based payments could lead to overpayment liability and indirect False Claims Act (FCA) exposure, he said.
In addition, “If the facts support that you were acting with intentional or deliberate ignorance or reckless disregard for how the data were gathered and reported that supported your value-based comp kicker, there could be direct False Claims Act liability,” Mr. Homchick said in an interview.
But Mr. Homchick stressed there are still many unknowns when it comes to how data-driven measurements will unfold.
“With MACRA, this is such a moving target as to exactly what type of data is going to form the basis for the metrics, and how the data need to be gathered and reported,” he said. “Many of those issues are still in play or still being developed at the agency level in terms of regulatory guidance.”
Current lawsuit could influence future cases
While it is too early to know every legal theory that could intersect with quality-based care, legal experts are closely watching a case that could offer insight into future claims.
In Duffy v. Lawrence Memorial Hospital, a former employee turned whistle-blower alleges that the Lawrence, Kan.–based hospital inflated its performance scores under the Hospital Value-Based Purchasing Program to increase federal incentive payments. Hospital leaders deny they falsified data and claim the allegations are based on the whistle-blower’s “improper understanding of acceptable reporting times for patient arrival,” according the hospital’s court response. The FCA lawsuit is before the U.S. District Court for the District of Kansas.
Notably, the government has declined to intervene in the lawsuit twice, Mr. Breen said. The case is continuing without government intervention, a trend that has become more common in recent years, he said. In 2015, whistle-blower cases in which U.S. Department of Justice declined to intervene led to $1.1 billion in recoveries for the government and $335 million in rewards for whistle-blowers, according to government data.
Mr. Homchick called the Lawrence Memorial lawsuit “troubling.”
“Providers are struggling with the complexity of the reporting requirements imposed by the layers of value-based payment programs implemented by both government and private payers,” he said. “The Lawrence Memorial case illustrates that the whistle-blower community will likely exploit the inevitable mistakes or missteps of providers attempting to comply with the increasingly byzantine quality-reporting requirements.”
The outcome of the Lawrence Memorial case could influence similar lawsuits involving value-based programs, Mr. Breen said.
“I think this theory that there is some false reporting, or false certification, is a theory that you will see being pursed in connection with some of these quality-based programs,” Mr. Breen said.
Early steps can curb legal risk
Asking questions and being proactive as new value-based models develop is key to mitigating legal dangers, experts said.
Ensure that new arrangements are analyzed for fraud and abuse risk exposure before finalizing, Mr. Breen advised.
“Have a comfort level about the arrangement” that’s being entered into, he added, and “have those arrangements vetted.”
Pay attention to data, added Michael E. Paulhus, an Atlanta-based health law attorney who specializes in FCA cases.
“The more data they collect, the more the government is paying attention to where you are in the range,” he said in an interview. “If you stick out on either end, that would be a risk profile that, as a physician, I would want to know. I would want to know where I sit in the data.”
When making reports regarding quality measures, include such reports in internal audits as part of regular compliance efforts, the experts suggested.
In addition, seek out resources early that can help prepare the practice for new quality-based regulations, Mr. Homchick said.
“There will be guidance coming out [regarding] eligibility for these value-based incentives,” he said. “That will require you and your staff to really pay attention and seek out resources and guidance to try to do this right. If you have the bandwidth to get out ahead of this, that would certainly be the best approach.”
On Twitter @legal_med
As you begin to consider the switch to value-based care systems, be sure to safeguard against risks that could fuel false claims scrutiny by the government, legal experts advise.
A primary consideration is arrangements that include shared savings through coordinated care, said George B. Breen, a Washington-based health law attorney. For example, he said that the Stark Law could be implicated if a physician within a shared savings model receives a bonus payment for referring patients to specific providers. The Stark Law prohibits a physician from referring Medicare patients for designated health services to an entity with which the physician has a financial relationship.
“While there are a number of exceptions and safe harbors which would validate any such relationship, it’s something that needs to be thought through” from the start, Mr. Breen said in an interview. “You have to look at each factual circumstance separately because each is fact and circumstance dependent.”
The Anti-Kickback Statute also could come into play if value-based arrangements generate renumeration. The Anti-Kickback Statute prohibits offering, paying, soliciting, or receiving anything of value to induce or reward referrals or generate federal health care program business. Exceptions to the statute can be applied and should also be examined during arrangement development, Mr. Breen said.
Data collection and reporting also may present a problem, according to Seattle-based health law attorney Robert G. Homchick. Inaccurate data that become the basis for quality-based payments could lead to overpayment liability and indirect False Claims Act (FCA) exposure, he said.
In addition, “If the facts support that you were acting with intentional or deliberate ignorance or reckless disregard for how the data were gathered and reported that supported your value-based comp kicker, there could be direct False Claims Act liability,” Mr. Homchick said in an interview.
But Mr. Homchick stressed there are still many unknowns when it comes to how data-driven measurements will unfold.
“With MACRA, this is such a moving target as to exactly what type of data is going to form the basis for the metrics, and how the data need to be gathered and reported,” he said. “Many of those issues are still in play or still being developed at the agency level in terms of regulatory guidance.”
Current lawsuit could influence future cases
While it is too early to know every legal theory that could intersect with quality-based care, legal experts are closely watching a case that could offer insight into future claims.
In Duffy v. Lawrence Memorial Hospital, a former employee turned whistle-blower alleges that the Lawrence, Kan.–based hospital inflated its performance scores under the Hospital Value-Based Purchasing Program to increase federal incentive payments. Hospital leaders deny they falsified data and claim the allegations are based on the whistle-blower’s “improper understanding of acceptable reporting times for patient arrival,” according the hospital’s court response. The FCA lawsuit is before the U.S. District Court for the District of Kansas.
Notably, the government has declined to intervene in the lawsuit twice, Mr. Breen said. The case is continuing without government intervention, a trend that has become more common in recent years, he said. In 2015, whistle-blower cases in which U.S. Department of Justice declined to intervene led to $1.1 billion in recoveries for the government and $335 million in rewards for whistle-blowers, according to government data.
Mr. Homchick called the Lawrence Memorial lawsuit “troubling.”
“Providers are struggling with the complexity of the reporting requirements imposed by the layers of value-based payment programs implemented by both government and private payers,” he said. “The Lawrence Memorial case illustrates that the whistle-blower community will likely exploit the inevitable mistakes or missteps of providers attempting to comply with the increasingly byzantine quality-reporting requirements.”
The outcome of the Lawrence Memorial case could influence similar lawsuits involving value-based programs, Mr. Breen said.
“I think this theory that there is some false reporting, or false certification, is a theory that you will see being pursed in connection with some of these quality-based programs,” Mr. Breen said.
Early steps can curb legal risk
Asking questions and being proactive as new value-based models develop is key to mitigating legal dangers, experts said.
Ensure that new arrangements are analyzed for fraud and abuse risk exposure before finalizing, Mr. Breen advised.
“Have a comfort level about the arrangement” that’s being entered into, he added, and “have those arrangements vetted.”
Pay attention to data, added Michael E. Paulhus, an Atlanta-based health law attorney who specializes in FCA cases.
“The more data they collect, the more the government is paying attention to where you are in the range,” he said in an interview. “If you stick out on either end, that would be a risk profile that, as a physician, I would want to know. I would want to know where I sit in the data.”
When making reports regarding quality measures, include such reports in internal audits as part of regular compliance efforts, the experts suggested.
In addition, seek out resources early that can help prepare the practice for new quality-based regulations, Mr. Homchick said.
“There will be guidance coming out [regarding] eligibility for these value-based incentives,” he said. “That will require you and your staff to really pay attention and seek out resources and guidance to try to do this right. If you have the bandwidth to get out ahead of this, that would certainly be the best approach.”
On Twitter @legal_med