User login
Official Newspaper of the American College of Surgeons
VIDEO: Proposed revision of medullary thyroid cancer staging improves risk-stratification analysis
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – An analysis of data from medullary thyroid cancer patients that partitioned the patients into groups with similar overall survival has spurred a rethink of the current American Joint Committee on Cancer (AJCC) staging system.
The results from researchers at Duke University, Durham, N.C., presented at the annual meeting of the Endocrine Society by Dr. Mohamed Abdelgadir Adam, are timely, as the AJCC has embarked on a reconsideration of the staging of cancers, including medullary thyroid cancer (MTC), as part revisions for the eighth edition of the staging system.
“The existing AJCC staging system for MTC appears to be less than optimal in discriminating the risk of mortality among disease stage groups,” said Dr. Adam, who discussed the findings in a video interview.
MTC, a neuroendocrine tumor that affects C cells of the thyroid, comprises 3%-5% of all cases of thyroid cancer and it can be a more aggressive disease than differentiated thyroid cancer. Yet the current AJCC MTC staging system has been extrapolated from differentiated thyroid cancer data.
“We sought to evaluate how well the current AJCC seventh edition stage groupings predict survival for patients with MTC, to suggest a possible staging revision to sharpen estimates of prognosis,” said Dr. Adam.
The researchers utilized the National Cancer Data Base, representing over 70% of incident cancer cases in the United States.
MTC patients who underwent thyroid surgery from 1998 to 2012 were identified. Patients with missing values for pathologic T, N, or M were excluded. The primary outcome in the 3,315 patients was survival.
The researchers used a form of decision-tree analysis called recursive partitioning. In general, recursive partitioning is able to classify a population by splitting subjects into subgroups, each of which is homogeneous based on the particular outcome. In this study, the subgroup allocations were based on T, N, and M stages, with the outcome being overall survival. Kaplan-Meier and adjusted survival analyses enabled survival differences among the four subgroups (groups I, II, III and IV) to be explored.
The four groups were distinct in terms of survival time and allowed more accurate risk stratification. In particular, groups I and II were markedly better distinguished from one another than is the case with the current staging system. Survival differences across the stages were more distinct with the newly created T, N, and M groupings, compared with the current AJCC staging system.
After adjustment, survival differences across TNM groups were more distinct with the newly created TNM groupings (compared to subgroup I, hazard ratio of 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV), compared with the current AJCC staging (compared to stage I, HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV).
“The AJCC is reevaluating all staging schemas, including MTC. The current AJCC staging system could be improved with the newly identified TNM groupings suggested here for more accurate patient risk stratification and possibly treatment selection,” said Dr. Adam.
Dr. Adam had no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Key clinical point: A proposed revision of the AJCC thyroid cancer staging system improves risk stratification analysis.
Major finding: In the proposed staging system, compared to subgroup I, hazard ratio for survival was 3.06 for subgroup II; HR, 6.79 for III; and HR, 17.03 for IV, compared with the current AJCC staging of HR, 1.45 for stage II; HR, 2.17 for III; and HR, 5.33 for IV.
Data source: Data from 3,315 patients with medullary thyroid cancer was drawn from the National Cancer Database.
Disclosures: Dr. Adam had no disclosures.
Standard incubation can miss P. acnes in infective endocarditis
AMSTERDAM – Accounting for less than 1% of cases, Propionibacterium acnes has been considered an uncommon cause of infective endocarditis.
But data presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases suggest that the common anaerobe may be responsible for many more cases than is now believed. The bacteria are difficult to culture and grow very slowly, Dr. Jona Banzon said at the meeting. Incubating it for the standard 5 days may simply not be long enough.
“Due to this slow-growing nature, the standard incubation period may not be enough to detect it,” said Dr. Banzon, an infectious disease fellow at the Cleveland Clinic. “And since P. acnes is part of our commensal flora, it’s frequently a contaminate in culture, and we might be inappropriately dismissing it as such. In fact, we now wonder if this lack of extended incubation may be accounting for a significant proportion of negative blood cultures, and whether more prosthetic valve endocarditis than we think is actually being caused by P. acnes.”
Dr. Banzon presented a series of 23 cases included in the Cleveland Clinic Infective Endocarditis Registry from the period of 2007-2015. All had P. acnes confirmed as the causative organism. The group comprises 3.3% of the institution’s entire infective endocarditis registry, “making infective carditis with P. acnes already much more common than it is said to be in the literature,” she noted.
All of the cases were confirmed by any of the following standards:
• Two or more blood cultures positive for P. acnes.
• Two or more valve cultures positive for P. acnes.
• Two or more valve sequencing rests positive for P. acnes.
• At least two of the following: a positive blood culture, a positive valve culture or valve sequencing, or histopathologic demonstration of microorganism consistent with P. acnes.
Of the cohort, 22 had prosthetic valve endocarditis. One patient had endocarditis on a native valve. This is an important point, Dr. Banzon said.
The organism is being increasingly recognized for causing infections of prosthetic material, including shoulder joint infections and shunts, but it rarely seems to affect native tissue. The patient who had native valve endocarditis had experienced an episode of Staphylococcus aureus endocarditis about 18 months earlier. He was not treated surgically, and ended up with a damaged valve. After the initial illness, he was readmitted several times with symptoms of endocarditis, but all of his blood cultures were negative. This was attributed to the receipt of antibiotics. “When he was finally operated on, there were three valve sequencing specimens and all were positive for P. acnes,” Dr. Banzon said.
The patients in the cohort were a mean of 74 years old; about 75% were men. All of the cases were left-sided endocarditis, with the majority (74%) involving the aortic valve. Other sites included the mitral valve (18%), aortic plus mitral (4%), and aortic plus tricuspid (4%).
The most common predisposing factor was having a prosthetic valve (96%). Other factors included having a cardiac implantable device (17%), and a prior episode of infective endocarditis (13%). None of the patients had indwelling vascular catheters or used injectable drugs.
The cases presented with severe disease, Dr. Banzon said. Almost half (48%) had a perivalvular abscess at presentation. A third (35%) had valve dehiscence, and 35% had severe valvular regurgitation. There was a vegetation of more than 1 cm in 9% of cases.
Emboli were not uncommon; 17% had emboli in the central nervous system, and 17% had peripheral emboli. Two of these patients had kidney and spleen infarcts and two had acute arterial thromboembolism that required thrombectomy.
All of the patients underwent blood cultures; overall, 30% of the cultures were positive for P. acnes. But there were “striking differences” when the tests were broken down by incubation time, Dr. Banzon said.
Most of the cultures (16) were incubated for the standard of 5 days or less. Among these, 12.5% were positive. However, cultures on seven patients were incubated for more than 5 days and in this group, 71.4% were positive for P. acnes. The median time to positivity overall was 7 days, with a range of 3-9 days.
Other diagnostic methods were important in closing this gap, she said. Valve culturing was positive in 57% of the cases, while valve sequencing was positive in 95%. The median time to positive for valve culture was somewhat shorter than for blood culture (5.5 days).
In nine cases, no organism would have been identified without valve sequencing, Dr. Banzon said.
Because they presented with severe disease, almost all of the patients (22) underwent surgery as their intimal treatment. At the time of surgery, everyone was taking an antibiotic that covered P. acnes. Single-agent therapy was the definitive treatment for most, with vancomycin being most commonly employed (59%), followed by ceftriaxone (25%). A few patients had a combination of both drugs or a combination of vancomycin and rifampin. One patient took penicillin.
The single patient who was medically treated received 6 weeks of intravenous ceftriaxone. After 1 month, he was readmitted with blood cultures positive for P. acnes. He underwent surgery and a valve sequencing confirmed P. acnes as the infective agent.
There were two in-hospital deaths, but the rest of the patients were discharged on antibiotic therapy and recovered with no additional deaths or relapses.
The extended time P. acnes required to show in culture was enough for the Cleveland Clinic to reconsider incubation guidelines for the microorganism, Dr. Banzon said.
“There are enough cases taking 9 or 10 days that we now always hold these cultures for at least 10 days when we’re looking for P. acnes.”
She had no financial disclosures.
AMSTERDAM – Accounting for less than 1% of cases, Propionibacterium acnes has been considered an uncommon cause of infective endocarditis.
But data presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases suggest that the common anaerobe may be responsible for many more cases than is now believed. The bacteria are difficult to culture and grow very slowly, Dr. Jona Banzon said at the meeting. Incubating it for the standard 5 days may simply not be long enough.
“Due to this slow-growing nature, the standard incubation period may not be enough to detect it,” said Dr. Banzon, an infectious disease fellow at the Cleveland Clinic. “And since P. acnes is part of our commensal flora, it’s frequently a contaminate in culture, and we might be inappropriately dismissing it as such. In fact, we now wonder if this lack of extended incubation may be accounting for a significant proportion of negative blood cultures, and whether more prosthetic valve endocarditis than we think is actually being caused by P. acnes.”
Dr. Banzon presented a series of 23 cases included in the Cleveland Clinic Infective Endocarditis Registry from the period of 2007-2015. All had P. acnes confirmed as the causative organism. The group comprises 3.3% of the institution’s entire infective endocarditis registry, “making infective carditis with P. acnes already much more common than it is said to be in the literature,” she noted.
All of the cases were confirmed by any of the following standards:
• Two or more blood cultures positive for P. acnes.
• Two or more valve cultures positive for P. acnes.
• Two or more valve sequencing rests positive for P. acnes.
• At least two of the following: a positive blood culture, a positive valve culture or valve sequencing, or histopathologic demonstration of microorganism consistent with P. acnes.
Of the cohort, 22 had prosthetic valve endocarditis. One patient had endocarditis on a native valve. This is an important point, Dr. Banzon said.
The organism is being increasingly recognized for causing infections of prosthetic material, including shoulder joint infections and shunts, but it rarely seems to affect native tissue. The patient who had native valve endocarditis had experienced an episode of Staphylococcus aureus endocarditis about 18 months earlier. He was not treated surgically, and ended up with a damaged valve. After the initial illness, he was readmitted several times with symptoms of endocarditis, but all of his blood cultures were negative. This was attributed to the receipt of antibiotics. “When he was finally operated on, there were three valve sequencing specimens and all were positive for P. acnes,” Dr. Banzon said.
The patients in the cohort were a mean of 74 years old; about 75% were men. All of the cases were left-sided endocarditis, with the majority (74%) involving the aortic valve. Other sites included the mitral valve (18%), aortic plus mitral (4%), and aortic plus tricuspid (4%).
The most common predisposing factor was having a prosthetic valve (96%). Other factors included having a cardiac implantable device (17%), and a prior episode of infective endocarditis (13%). None of the patients had indwelling vascular catheters or used injectable drugs.
The cases presented with severe disease, Dr. Banzon said. Almost half (48%) had a perivalvular abscess at presentation. A third (35%) had valve dehiscence, and 35% had severe valvular regurgitation. There was a vegetation of more than 1 cm in 9% of cases.
Emboli were not uncommon; 17% had emboli in the central nervous system, and 17% had peripheral emboli. Two of these patients had kidney and spleen infarcts and two had acute arterial thromboembolism that required thrombectomy.
All of the patients underwent blood cultures; overall, 30% of the cultures were positive for P. acnes. But there were “striking differences” when the tests were broken down by incubation time, Dr. Banzon said.
Most of the cultures (16) were incubated for the standard of 5 days or less. Among these, 12.5% were positive. However, cultures on seven patients were incubated for more than 5 days and in this group, 71.4% were positive for P. acnes. The median time to positivity overall was 7 days, with a range of 3-9 days.
Other diagnostic methods were important in closing this gap, she said. Valve culturing was positive in 57% of the cases, while valve sequencing was positive in 95%. The median time to positive for valve culture was somewhat shorter than for blood culture (5.5 days).
In nine cases, no organism would have been identified without valve sequencing, Dr. Banzon said.
Because they presented with severe disease, almost all of the patients (22) underwent surgery as their intimal treatment. At the time of surgery, everyone was taking an antibiotic that covered P. acnes. Single-agent therapy was the definitive treatment for most, with vancomycin being most commonly employed (59%), followed by ceftriaxone (25%). A few patients had a combination of both drugs or a combination of vancomycin and rifampin. One patient took penicillin.
The single patient who was medically treated received 6 weeks of intravenous ceftriaxone. After 1 month, he was readmitted with blood cultures positive for P. acnes. He underwent surgery and a valve sequencing confirmed P. acnes as the infective agent.
There were two in-hospital deaths, but the rest of the patients were discharged on antibiotic therapy and recovered with no additional deaths or relapses.
The extended time P. acnes required to show in culture was enough for the Cleveland Clinic to reconsider incubation guidelines for the microorganism, Dr. Banzon said.
“There are enough cases taking 9 or 10 days that we now always hold these cultures for at least 10 days when we’re looking for P. acnes.”
She had no financial disclosures.
AMSTERDAM – Accounting for less than 1% of cases, Propionibacterium acnes has been considered an uncommon cause of infective endocarditis.
But data presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases suggest that the common anaerobe may be responsible for many more cases than is now believed. The bacteria are difficult to culture and grow very slowly, Dr. Jona Banzon said at the meeting. Incubating it for the standard 5 days may simply not be long enough.
“Due to this slow-growing nature, the standard incubation period may not be enough to detect it,” said Dr. Banzon, an infectious disease fellow at the Cleveland Clinic. “And since P. acnes is part of our commensal flora, it’s frequently a contaminate in culture, and we might be inappropriately dismissing it as such. In fact, we now wonder if this lack of extended incubation may be accounting for a significant proportion of negative blood cultures, and whether more prosthetic valve endocarditis than we think is actually being caused by P. acnes.”
Dr. Banzon presented a series of 23 cases included in the Cleveland Clinic Infective Endocarditis Registry from the period of 2007-2015. All had P. acnes confirmed as the causative organism. The group comprises 3.3% of the institution’s entire infective endocarditis registry, “making infective carditis with P. acnes already much more common than it is said to be in the literature,” she noted.
All of the cases were confirmed by any of the following standards:
• Two or more blood cultures positive for P. acnes.
• Two or more valve cultures positive for P. acnes.
• Two or more valve sequencing rests positive for P. acnes.
• At least two of the following: a positive blood culture, a positive valve culture or valve sequencing, or histopathologic demonstration of microorganism consistent with P. acnes.
Of the cohort, 22 had prosthetic valve endocarditis. One patient had endocarditis on a native valve. This is an important point, Dr. Banzon said.
The organism is being increasingly recognized for causing infections of prosthetic material, including shoulder joint infections and shunts, but it rarely seems to affect native tissue. The patient who had native valve endocarditis had experienced an episode of Staphylococcus aureus endocarditis about 18 months earlier. He was not treated surgically, and ended up with a damaged valve. After the initial illness, he was readmitted several times with symptoms of endocarditis, but all of his blood cultures were negative. This was attributed to the receipt of antibiotics. “When he was finally operated on, there were three valve sequencing specimens and all were positive for P. acnes,” Dr. Banzon said.
The patients in the cohort were a mean of 74 years old; about 75% were men. All of the cases were left-sided endocarditis, with the majority (74%) involving the aortic valve. Other sites included the mitral valve (18%), aortic plus mitral (4%), and aortic plus tricuspid (4%).
The most common predisposing factor was having a prosthetic valve (96%). Other factors included having a cardiac implantable device (17%), and a prior episode of infective endocarditis (13%). None of the patients had indwelling vascular catheters or used injectable drugs.
The cases presented with severe disease, Dr. Banzon said. Almost half (48%) had a perivalvular abscess at presentation. A third (35%) had valve dehiscence, and 35% had severe valvular regurgitation. There was a vegetation of more than 1 cm in 9% of cases.
Emboli were not uncommon; 17% had emboli in the central nervous system, and 17% had peripheral emboli. Two of these patients had kidney and spleen infarcts and two had acute arterial thromboembolism that required thrombectomy.
All of the patients underwent blood cultures; overall, 30% of the cultures were positive for P. acnes. But there were “striking differences” when the tests were broken down by incubation time, Dr. Banzon said.
Most of the cultures (16) were incubated for the standard of 5 days or less. Among these, 12.5% were positive. However, cultures on seven patients were incubated for more than 5 days and in this group, 71.4% were positive for P. acnes. The median time to positivity overall was 7 days, with a range of 3-9 days.
Other diagnostic methods were important in closing this gap, she said. Valve culturing was positive in 57% of the cases, while valve sequencing was positive in 95%. The median time to positive for valve culture was somewhat shorter than for blood culture (5.5 days).
In nine cases, no organism would have been identified without valve sequencing, Dr. Banzon said.
Because they presented with severe disease, almost all of the patients (22) underwent surgery as their intimal treatment. At the time of surgery, everyone was taking an antibiotic that covered P. acnes. Single-agent therapy was the definitive treatment for most, with vancomycin being most commonly employed (59%), followed by ceftriaxone (25%). A few patients had a combination of both drugs or a combination of vancomycin and rifampin. One patient took penicillin.
The single patient who was medically treated received 6 weeks of intravenous ceftriaxone. After 1 month, he was readmitted with blood cultures positive for P. acnes. He underwent surgery and a valve sequencing confirmed P. acnes as the infective agent.
There were two in-hospital deaths, but the rest of the patients were discharged on antibiotic therapy and recovered with no additional deaths or relapses.
The extended time P. acnes required to show in culture was enough for the Cleveland Clinic to reconsider incubation guidelines for the microorganism, Dr. Banzon said.
“There are enough cases taking 9 or 10 days that we now always hold these cultures for at least 10 days when we’re looking for P. acnes.”
She had no financial disclosures.
AT ECCMID 2016
Key clinical point: P. acnes’ slow growth may result in false negative blood cultures in infective endocarditis.
Major finding: Just 12% of blood cultures incubated for 5 days were positive, while 71% of those incubated for more than 5 days were positive.
Data source: The Cleveland Clinic Infective Endocarditis Registry.
Disclosures: Dr. Banzon had no financial disclosures.
Drug-eluting stent recipients can safely have surgery sooner
CHICAGO – Current U.S. and European guidelines recommending postponement of noncardiac surgery for 6-12 months after drug-eluting stent implantation appear to be excessive, Dr. Gro Egholm reported at the annual meeting of the American College of Cardiology.
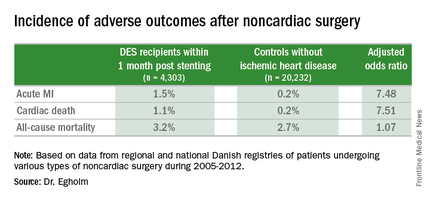
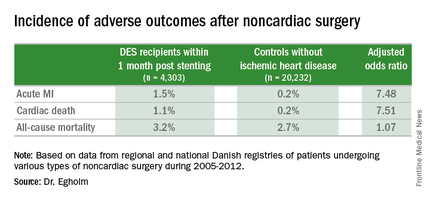
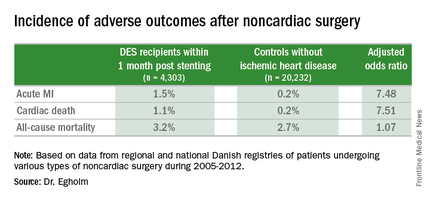
She presented a large retrospective observational study of outcomes in patients undergoing various types of noncardiac surgery in western Denmark during 2005-2012. Among 4,303 patients who had noncardiac surgery within 12 months after receiving a drug-eluting stent (DES), only those whose operations took place during the first month post stenting had increased risks of acute MI and cardiac death within 30 days post surgery.
Risks of major adverse cardiac events among the DES recipients who had noncardiac surgery within that first month post–percutaneous coronary intervention were increased roughly 7.5-fold compared with controls, but for surgery performed after that the risks of MI and cardiac death dropped off abruptly and were no different from rates in 20,232 controls without ischemic heart disease or stents who were matched for age, gender, surgical procedure, and Charlson Comorbidity Index, according to Dr. Egholm of Aarhus (Denmark) University.
Moreover, even in DES recipients undergoing noncardiac surgery during the first month post stenting, all-cause mortality was no greater than in controls.
“Surgery could be performed much earlier than recommended,” she concluded.
Her study was carried out by linking data from comprehensive regional and national Danish health care registries. Most patients with DES remained on dual antiplatelet therapy periprocedurally. The exceptions were neurosurgical operations and others where it’s standard that dual antiplatelet therapy must be stopped.
“If you can continue only one antiplatelet agent, aspirin would be the most appealing,” she said.
Of the DES participants, 56% received their device as treatment for an acute coronary syndrome. The average time from stent placement to noncardiac surgery in this large series was 147 days.
Session co-chair Dr. Sunil V. Rao of Duke University in Durham, N.C., called this work “a very important study that’s relevant to daily practice.” However, he found the 23% incidence of noncardiac surgery within 12 months following DES implantation reported in Dr. Egholm’s study to be “shockingly high.” She agreed, noting that rates in some non-Danish registries she’s looked at are more in the 8%-15% range. But Denmark’s health care registries are known for rigorous accuracy and completeness.
Dr. Egholm reported having no financial conflicts regarding her study.
CHICAGO – Current U.S. and European guidelines recommending postponement of noncardiac surgery for 6-12 months after drug-eluting stent implantation appear to be excessive, Dr. Gro Egholm reported at the annual meeting of the American College of Cardiology.
She presented a large retrospective observational study of outcomes in patients undergoing various types of noncardiac surgery in western Denmark during 2005-2012. Among 4,303 patients who had noncardiac surgery within 12 months after receiving a drug-eluting stent (DES), only those whose operations took place during the first month post stenting had increased risks of acute MI and cardiac death within 30 days post surgery.
Risks of major adverse cardiac events among the DES recipients who had noncardiac surgery within that first month post–percutaneous coronary intervention were increased roughly 7.5-fold compared with controls, but for surgery performed after that the risks of MI and cardiac death dropped off abruptly and were no different from rates in 20,232 controls without ischemic heart disease or stents who were matched for age, gender, surgical procedure, and Charlson Comorbidity Index, according to Dr. Egholm of Aarhus (Denmark) University.
Moreover, even in DES recipients undergoing noncardiac surgery during the first month post stenting, all-cause mortality was no greater than in controls.
“Surgery could be performed much earlier than recommended,” she concluded.
Her study was carried out by linking data from comprehensive regional and national Danish health care registries. Most patients with DES remained on dual antiplatelet therapy periprocedurally. The exceptions were neurosurgical operations and others where it’s standard that dual antiplatelet therapy must be stopped.
“If you can continue only one antiplatelet agent, aspirin would be the most appealing,” she said.
Of the DES participants, 56% received their device as treatment for an acute coronary syndrome. The average time from stent placement to noncardiac surgery in this large series was 147 days.
Session co-chair Dr. Sunil V. Rao of Duke University in Durham, N.C., called this work “a very important study that’s relevant to daily practice.” However, he found the 23% incidence of noncardiac surgery within 12 months following DES implantation reported in Dr. Egholm’s study to be “shockingly high.” She agreed, noting that rates in some non-Danish registries she’s looked at are more in the 8%-15% range. But Denmark’s health care registries are known for rigorous accuracy and completeness.
Dr. Egholm reported having no financial conflicts regarding her study.
CHICAGO – Current U.S. and European guidelines recommending postponement of noncardiac surgery for 6-12 months after drug-eluting stent implantation appear to be excessive, Dr. Gro Egholm reported at the annual meeting of the American College of Cardiology.
She presented a large retrospective observational study of outcomes in patients undergoing various types of noncardiac surgery in western Denmark during 2005-2012. Among 4,303 patients who had noncardiac surgery within 12 months after receiving a drug-eluting stent (DES), only those whose operations took place during the first month post stenting had increased risks of acute MI and cardiac death within 30 days post surgery.
Risks of major adverse cardiac events among the DES recipients who had noncardiac surgery within that first month post–percutaneous coronary intervention were increased roughly 7.5-fold compared with controls, but for surgery performed after that the risks of MI and cardiac death dropped off abruptly and were no different from rates in 20,232 controls without ischemic heart disease or stents who were matched for age, gender, surgical procedure, and Charlson Comorbidity Index, according to Dr. Egholm of Aarhus (Denmark) University.
Moreover, even in DES recipients undergoing noncardiac surgery during the first month post stenting, all-cause mortality was no greater than in controls.
“Surgery could be performed much earlier than recommended,” she concluded.
Her study was carried out by linking data from comprehensive regional and national Danish health care registries. Most patients with DES remained on dual antiplatelet therapy periprocedurally. The exceptions were neurosurgical operations and others where it’s standard that dual antiplatelet therapy must be stopped.
“If you can continue only one antiplatelet agent, aspirin would be the most appealing,” she said.
Of the DES participants, 56% received their device as treatment for an acute coronary syndrome. The average time from stent placement to noncardiac surgery in this large series was 147 days.
Session co-chair Dr. Sunil V. Rao of Duke University in Durham, N.C., called this work “a very important study that’s relevant to daily practice.” However, he found the 23% incidence of noncardiac surgery within 12 months following DES implantation reported in Dr. Egholm’s study to be “shockingly high.” She agreed, noting that rates in some non-Danish registries she’s looked at are more in the 8%-15% range. But Denmark’s health care registries are known for rigorous accuracy and completeness.
Dr. Egholm reported having no financial conflicts regarding her study.
AT ACC 16
Key clinical point: The risk of noncardiac surgery is elevated only when the operation occurs during the first month after stenting.
Major finding: Danish drug-eluting stent recipients who underwent noncardiac surgery within 1 month after stent placement were at 7.5-fold increased risks of acute MI and cardiac death, but surgery performed 2-12 months post stenting carried no increased risks.
Data source: This retrospective observational study based upon large Danish patient registries compared outcomes of noncardiac surgery performed within 12 months after drug-eluting stent placement in 4,303 patients with 20,232 matched controls without ischemic heart disease who underwent the same operations.
Disclosures: The study was supported by Danish research funds. The presenter reported having no financial conflicts of interest.
DANAMI 3-DEFER: No benefit with delayed stenting for STEMI
CHICAGO – Delaying stent implantation in patients with ST-segment elevation myocardial infarction failed to reduce the rate of mortality, heart failure, myocardial infarction, or repeat revascularization, compared with conventional percutaneous intervention in the randomized, controlled DANAMI 3-DEFER trial.
Among 1,215 patients with ST-segment elevation MI (STEMI) who were randomized to receive either standard primary percutaneous coronary intervention (PCI) with immediate stent implantation or deferred stent implantation 48 hours after the index procedure, the rate of the primary composite endpoint of all-cause mortality, hospital admission for heart failure, recurrent infarction, or any unplanned revascularization of the target vessel within 2 years was 18% in the immediate treatment group and 17% in the deferred stent implantation group, a nonsignificant difference, Dr. Henning Kelbæk reported at the annual meeting of the American College of Cardiology.
Procedure-related myocardial infarction, bleeding requiring transfusion or surgery, contrast-induced nephropathy, or stroke occurred in 5% and 4% of patients in the groups, respectively, he said.
Although some might be relieved to know there won’t be a need for doing a second procedure, the findings are a disappointment in that preliminary findings suggested a benefit when stenting is delayed for several hours to several days after angioplasty, said Dr. Kelbæk of Roskilde Hospital (Denmark).
The thinking was that medication given during the delay might help diminish residual blood clots, thereby reducing the risk of distal embolization, which occurs in 7% of cases, and which can occur despite successful treatment of the culprit artery lesion by primary PCI with stent implantation, he explained, noting that slow- or no-flow occurs in 10% of cases.
It is possible that the study may not have been large enough to detect overall differences in the two treatment groups. It is also possible that patients at the highest risk for developing another arterial blockage could potentially benefit from a delay, especially given that a small but significant improvement in left ventricular function was detected 18 months after treatment among patients who underwent deferred stenting (left ventricular ejection fraction, 60% vs. 57% in the immediate treatment group), but such patients were excluded from DANAMI 3-DEFER (the Third Danish Study of Optimal Acute Treatment of Patients with ST-segment Elevation Myocardial Infarction: Deferred stent implantation in connection with primary PCI), he said.
He added that he and his coinvestigators will “look carefully for possible ‘hypothesis-generating’ findings in subsets of patients – both those who might have benefited from the deferred-treatment strategy and, equally important, those in whom this strategy might have worsened their condition.”
Patients were enrolled into DANAMI 3-DEFER during March 2011–February 2014 at four primary PCI centers in Denmark. All were adults with acute onset symptoms lasting 12 hours or less, and ST-segment elevation of 0.1 mV or more in at least 2 contiguous electrocardiographic leads, or newly developed left bundle branch block. Those in the deferred treatment group were only randomized to that group if stabilized flow could be obtained in the infarct-related artery. Median follow-up was 42 months.
The findings indicate that at this point, deferred stent implantation cannot be recommended as a routine procedure for STEMI patients treated with primary PCI, Dr. Kelbæk concluded. The findings were published online simultaneously with the presentation (Lancet. 2016 Apr 3. doi: 10.1016/S0140-6736[16]30072-1).
The DANAMI-3-DEFER trial was funded by the Danish Agency for Science, Technology and Innovation and Danish Council for Strategic Research. Dr. Kelbæk reported having no disclosures.
CHICAGO – Delaying stent implantation in patients with ST-segment elevation myocardial infarction failed to reduce the rate of mortality, heart failure, myocardial infarction, or repeat revascularization, compared with conventional percutaneous intervention in the randomized, controlled DANAMI 3-DEFER trial.
Among 1,215 patients with ST-segment elevation MI (STEMI) who were randomized to receive either standard primary percutaneous coronary intervention (PCI) with immediate stent implantation or deferred stent implantation 48 hours after the index procedure, the rate of the primary composite endpoint of all-cause mortality, hospital admission for heart failure, recurrent infarction, or any unplanned revascularization of the target vessel within 2 years was 18% in the immediate treatment group and 17% in the deferred stent implantation group, a nonsignificant difference, Dr. Henning Kelbæk reported at the annual meeting of the American College of Cardiology.
Procedure-related myocardial infarction, bleeding requiring transfusion or surgery, contrast-induced nephropathy, or stroke occurred in 5% and 4% of patients in the groups, respectively, he said.
Although some might be relieved to know there won’t be a need for doing a second procedure, the findings are a disappointment in that preliminary findings suggested a benefit when stenting is delayed for several hours to several days after angioplasty, said Dr. Kelbæk of Roskilde Hospital (Denmark).
The thinking was that medication given during the delay might help diminish residual blood clots, thereby reducing the risk of distal embolization, which occurs in 7% of cases, and which can occur despite successful treatment of the culprit artery lesion by primary PCI with stent implantation, he explained, noting that slow- or no-flow occurs in 10% of cases.
It is possible that the study may not have been large enough to detect overall differences in the two treatment groups. It is also possible that patients at the highest risk for developing another arterial blockage could potentially benefit from a delay, especially given that a small but significant improvement in left ventricular function was detected 18 months after treatment among patients who underwent deferred stenting (left ventricular ejection fraction, 60% vs. 57% in the immediate treatment group), but such patients were excluded from DANAMI 3-DEFER (the Third Danish Study of Optimal Acute Treatment of Patients with ST-segment Elevation Myocardial Infarction: Deferred stent implantation in connection with primary PCI), he said.
He added that he and his coinvestigators will “look carefully for possible ‘hypothesis-generating’ findings in subsets of patients – both those who might have benefited from the deferred-treatment strategy and, equally important, those in whom this strategy might have worsened their condition.”
Patients were enrolled into DANAMI 3-DEFER during March 2011–February 2014 at four primary PCI centers in Denmark. All were adults with acute onset symptoms lasting 12 hours or less, and ST-segment elevation of 0.1 mV or more in at least 2 contiguous electrocardiographic leads, or newly developed left bundle branch block. Those in the deferred treatment group were only randomized to that group if stabilized flow could be obtained in the infarct-related artery. Median follow-up was 42 months.
The findings indicate that at this point, deferred stent implantation cannot be recommended as a routine procedure for STEMI patients treated with primary PCI, Dr. Kelbæk concluded. The findings were published online simultaneously with the presentation (Lancet. 2016 Apr 3. doi: 10.1016/S0140-6736[16]30072-1).
The DANAMI-3-DEFER trial was funded by the Danish Agency for Science, Technology and Innovation and Danish Council for Strategic Research. Dr. Kelbæk reported having no disclosures.
CHICAGO – Delaying stent implantation in patients with ST-segment elevation myocardial infarction failed to reduce the rate of mortality, heart failure, myocardial infarction, or repeat revascularization, compared with conventional percutaneous intervention in the randomized, controlled DANAMI 3-DEFER trial.
Among 1,215 patients with ST-segment elevation MI (STEMI) who were randomized to receive either standard primary percutaneous coronary intervention (PCI) with immediate stent implantation or deferred stent implantation 48 hours after the index procedure, the rate of the primary composite endpoint of all-cause mortality, hospital admission for heart failure, recurrent infarction, or any unplanned revascularization of the target vessel within 2 years was 18% in the immediate treatment group and 17% in the deferred stent implantation group, a nonsignificant difference, Dr. Henning Kelbæk reported at the annual meeting of the American College of Cardiology.
Procedure-related myocardial infarction, bleeding requiring transfusion or surgery, contrast-induced nephropathy, or stroke occurred in 5% and 4% of patients in the groups, respectively, he said.
Although some might be relieved to know there won’t be a need for doing a second procedure, the findings are a disappointment in that preliminary findings suggested a benefit when stenting is delayed for several hours to several days after angioplasty, said Dr. Kelbæk of Roskilde Hospital (Denmark).
The thinking was that medication given during the delay might help diminish residual blood clots, thereby reducing the risk of distal embolization, which occurs in 7% of cases, and which can occur despite successful treatment of the culprit artery lesion by primary PCI with stent implantation, he explained, noting that slow- or no-flow occurs in 10% of cases.
It is possible that the study may not have been large enough to detect overall differences in the two treatment groups. It is also possible that patients at the highest risk for developing another arterial blockage could potentially benefit from a delay, especially given that a small but significant improvement in left ventricular function was detected 18 months after treatment among patients who underwent deferred stenting (left ventricular ejection fraction, 60% vs. 57% in the immediate treatment group), but such patients were excluded from DANAMI 3-DEFER (the Third Danish Study of Optimal Acute Treatment of Patients with ST-segment Elevation Myocardial Infarction: Deferred stent implantation in connection with primary PCI), he said.
He added that he and his coinvestigators will “look carefully for possible ‘hypothesis-generating’ findings in subsets of patients – both those who might have benefited from the deferred-treatment strategy and, equally important, those in whom this strategy might have worsened their condition.”
Patients were enrolled into DANAMI 3-DEFER during March 2011–February 2014 at four primary PCI centers in Denmark. All were adults with acute onset symptoms lasting 12 hours or less, and ST-segment elevation of 0.1 mV or more in at least 2 contiguous electrocardiographic leads, or newly developed left bundle branch block. Those in the deferred treatment group were only randomized to that group if stabilized flow could be obtained in the infarct-related artery. Median follow-up was 42 months.
The findings indicate that at this point, deferred stent implantation cannot be recommended as a routine procedure for STEMI patients treated with primary PCI, Dr. Kelbæk concluded. The findings were published online simultaneously with the presentation (Lancet. 2016 Apr 3. doi: 10.1016/S0140-6736[16]30072-1).
The DANAMI-3-DEFER trial was funded by the Danish Agency for Science, Technology and Innovation and Danish Council for Strategic Research. Dr. Kelbæk reported having no disclosures.
AT ACC 16
Key clinical point: Delaying stent implantation in patients with STEMI failed to improve outcomes, compared with conventional percutaneous intervention in the randomized, controlled DANAMI 3-DEFER trial.
Major finding: The rate of the primary composite endpoint was 18% in the immediate treatment group and 17% in the deferred stent implantation group.
Data source: The open-label, randomized, controlled DANAMI 3-DEFER trial of 1,215 patients.
Disclosures: The DANAMI 3-DEFER trial was funded by the Danish Agency for Science, Technology, and Innovation, and the Danish Council for Strategic Research. Dr. Kelbæk reported having no disclosures.
Androgen deprivation therapy linked to depression
Men on androgen deprivation therapy for prostate cancer are at significantly increased risk for depression, a risk that increases with duration of therapy, investigators report.
A review of Surveillance, Epidemiology, and End Results (SEER) Medicare data on nearly 79,000 men older than 65 years with a diagnosis of prostate cancer showed that those who received androgen deprivation therapy (ADT) had a 23% increased risk for depression, compared with men who were not on ADT, reported Kathryn T. Dinh of Harvard Medical School, Boston, and her colleagues.
“We observed a significantly increased risk of depression and inpatient psychiatric treatment in men treated with ADT for prostate cancer, as well as a duration-response effect such that more ADT was linked to an increasing risk of depression and inpatient and outpatient psychiatric treatment. The possible psychiatric effects of ADT should be recognized by physicians and discussed with patients before initiating treatment,” they wrote (J Clin Oncol. 2016 Apr 11. doi: 10.1200/JCO.2015.64.1969).
Although ADT has been identified in some studies as a risk factor for clinical depression, evidence for such a relationship has been spotty, the investigators said, prompting them to conduct a population-based retrospective study to get a better handle on the issue.
They reviewed SEER Medicare data on 78,552 men older than 65 years with a diagnosis of stage I-III prostate cancer treated with ADT from 1992 through 2006, excluding from the sample those patients who had a psychiatric diagnosis within the past 12 months.
Ms. Dinh and her associates found that the 33,882 patients (43%) who received ADT had a significantly higher 3-year cumulative incidence of depression than patients who did not have ADT (7.1% vs. 5.2%, P less than .001), and a significantly higher proportion had either inpatient psychiatric treatment (2.8% vs. 1.9%, P less than .001) or outpatient psychiatric therapy (3.4% vs. 2.5%, P less than .001).
In proportional hazard models controlling for demographic and clinical factors, receipt of ADT was associated with adjusted hazard ratios of 1.23 for depression and 1.29 (P less than .001 for both) for inpatient psychiatric treatment. There was no significant increase in risk for outpatient psychiatric treatment in this analysis, however.
In addition, the longer patients that were on ADT, the greater the risk for depression. The risk of depression was 12% for patients treated for 6 months or less, 26% for those on ADT for 7-11 months, and 37% for those on ADT for at least 1 year.
“The impact of ADT on depression may plausibly occur via deregulation of neurochemicals, such as serotonin, in addition to the well-described physical effects,” Ms. Dinh and her associates wrote.
Side effects of ADT that can impair quality of life also may contribute to clinical depression, they noted.
The study was supported by charitable grants and internal institutional sources. One investigator reported consulting or advisory roles with Medivation, GenomeDx, and Ferring. Three of the other ten coauthors also reported financial disclosures.
Men on androgen deprivation therapy for prostate cancer are at significantly increased risk for depression, a risk that increases with duration of therapy, investigators report.
A review of Surveillance, Epidemiology, and End Results (SEER) Medicare data on nearly 79,000 men older than 65 years with a diagnosis of prostate cancer showed that those who received androgen deprivation therapy (ADT) had a 23% increased risk for depression, compared with men who were not on ADT, reported Kathryn T. Dinh of Harvard Medical School, Boston, and her colleagues.
“We observed a significantly increased risk of depression and inpatient psychiatric treatment in men treated with ADT for prostate cancer, as well as a duration-response effect such that more ADT was linked to an increasing risk of depression and inpatient and outpatient psychiatric treatment. The possible psychiatric effects of ADT should be recognized by physicians and discussed with patients before initiating treatment,” they wrote (J Clin Oncol. 2016 Apr 11. doi: 10.1200/JCO.2015.64.1969).
Although ADT has been identified in some studies as a risk factor for clinical depression, evidence for such a relationship has been spotty, the investigators said, prompting them to conduct a population-based retrospective study to get a better handle on the issue.
They reviewed SEER Medicare data on 78,552 men older than 65 years with a diagnosis of stage I-III prostate cancer treated with ADT from 1992 through 2006, excluding from the sample those patients who had a psychiatric diagnosis within the past 12 months.
Ms. Dinh and her associates found that the 33,882 patients (43%) who received ADT had a significantly higher 3-year cumulative incidence of depression than patients who did not have ADT (7.1% vs. 5.2%, P less than .001), and a significantly higher proportion had either inpatient psychiatric treatment (2.8% vs. 1.9%, P less than .001) or outpatient psychiatric therapy (3.4% vs. 2.5%, P less than .001).
In proportional hazard models controlling for demographic and clinical factors, receipt of ADT was associated with adjusted hazard ratios of 1.23 for depression and 1.29 (P less than .001 for both) for inpatient psychiatric treatment. There was no significant increase in risk for outpatient psychiatric treatment in this analysis, however.
In addition, the longer patients that were on ADT, the greater the risk for depression. The risk of depression was 12% for patients treated for 6 months or less, 26% for those on ADT for 7-11 months, and 37% for those on ADT for at least 1 year.
“The impact of ADT on depression may plausibly occur via deregulation of neurochemicals, such as serotonin, in addition to the well-described physical effects,” Ms. Dinh and her associates wrote.
Side effects of ADT that can impair quality of life also may contribute to clinical depression, they noted.
The study was supported by charitable grants and internal institutional sources. One investigator reported consulting or advisory roles with Medivation, GenomeDx, and Ferring. Three of the other ten coauthors also reported financial disclosures.
Men on androgen deprivation therapy for prostate cancer are at significantly increased risk for depression, a risk that increases with duration of therapy, investigators report.
A review of Surveillance, Epidemiology, and End Results (SEER) Medicare data on nearly 79,000 men older than 65 years with a diagnosis of prostate cancer showed that those who received androgen deprivation therapy (ADT) had a 23% increased risk for depression, compared with men who were not on ADT, reported Kathryn T. Dinh of Harvard Medical School, Boston, and her colleagues.
“We observed a significantly increased risk of depression and inpatient psychiatric treatment in men treated with ADT for prostate cancer, as well as a duration-response effect such that more ADT was linked to an increasing risk of depression and inpatient and outpatient psychiatric treatment. The possible psychiatric effects of ADT should be recognized by physicians and discussed with patients before initiating treatment,” they wrote (J Clin Oncol. 2016 Apr 11. doi: 10.1200/JCO.2015.64.1969).
Although ADT has been identified in some studies as a risk factor for clinical depression, evidence for such a relationship has been spotty, the investigators said, prompting them to conduct a population-based retrospective study to get a better handle on the issue.
They reviewed SEER Medicare data on 78,552 men older than 65 years with a diagnosis of stage I-III prostate cancer treated with ADT from 1992 through 2006, excluding from the sample those patients who had a psychiatric diagnosis within the past 12 months.
Ms. Dinh and her associates found that the 33,882 patients (43%) who received ADT had a significantly higher 3-year cumulative incidence of depression than patients who did not have ADT (7.1% vs. 5.2%, P less than .001), and a significantly higher proportion had either inpatient psychiatric treatment (2.8% vs. 1.9%, P less than .001) or outpatient psychiatric therapy (3.4% vs. 2.5%, P less than .001).
In proportional hazard models controlling for demographic and clinical factors, receipt of ADT was associated with adjusted hazard ratios of 1.23 for depression and 1.29 (P less than .001 for both) for inpatient psychiatric treatment. There was no significant increase in risk for outpatient psychiatric treatment in this analysis, however.
In addition, the longer patients that were on ADT, the greater the risk for depression. The risk of depression was 12% for patients treated for 6 months or less, 26% for those on ADT for 7-11 months, and 37% for those on ADT for at least 1 year.
“The impact of ADT on depression may plausibly occur via deregulation of neurochemicals, such as serotonin, in addition to the well-described physical effects,” Ms. Dinh and her associates wrote.
Side effects of ADT that can impair quality of life also may contribute to clinical depression, they noted.
The study was supported by charitable grants and internal institutional sources. One investigator reported consulting or advisory roles with Medivation, GenomeDx, and Ferring. Three of the other ten coauthors also reported financial disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Androgen deprivation therapy for prostate cancer is associated with increased risk for clinical depression.
Major finding: Men who received androgen deprivation therapy (ADT) had a 23% increased risk for depression compared with men who were not on ADT.
Data source: Review of SEER Medicare data on 78,552 men with stage I-III prostate cancer.
Disclosures: The study was supported by charitable grants and internal institutional sources. One investigator reported consulting or advisory roles with Medivation, GenomeDx, and Ferring. Three of the other ten coauthors also reported financial disclosures.
FDA approves first leadless pacemaker
The Food and Drug Administration has approved the first leadless pacemaker, the Micra transcatheter pacing system, the FDA stated in a release accompanying its approval.
The Micra pacemaker eliminates the need for wired leads and the risk of associated complications. The single-chamber ventricular pacemaker is 93% smaller than traditional pacemakers, according to a summary document submitted to the FDA by Medtronic, which makes the device. Like other ventricular pacemakers, Micra provides rate-adaptive pacing, with automated pacing capture threshold management to maximize battery life, which the company estimates at about 10 years.
The pacemaker is inserted directly into the right ventricle through the femoral vein by means of a steerable catheter. Pressing a button on the distal end of the catheter releases four flexible, electrically inactive nitinol tines that hook into the myocardium to secure the device. Engagement by two tines exerts 15 times the amount of force needed to secure the device in place, according to Medtronic.
The device’s approval was based on a pivotal prospective, nonrandomized uncontrolled study of 719 patients at 56 investigational sites in North America, Europe, Asia, Australia, and Africa. The primary efficacy endpoint, low and stable pacing capture thresholds at 6 months (up to 2.0 V at a pulse width of 0.24 milliseconds and an increase of up to 1.5 V from the time of implantation) was achieved for 98% of patients (95% confidence interval, 96%-99.5%), reported Dr. Dwight Reynolds of the University of Oklahoma Health Sciences Center in Oklahoma City and his associates (N Engl J Med. 2016 Feb. 11. doi: 10.1056/NEJMoa1511643).
The researchers also compared safety outcomes among Micra recipients and 2,667 historical controls from six previously published studies. The Micra pacemaker was associated with significantly lower hospitalization and system revision rates, with “no systemic infections, no pneumothoraxes, and no radiographically visible dislodgements or device emboli,” they said. In all, 4% of Micra recipients had complications leading to death or requiring invasive revision, treatment cessation, or hospitalization, which resembled recent reports of transvenous systems and was significantly lower than the rate for historical controls, according to the investigators. However, the rate of cardiac perforation or effusion was 1.6%, slightly higher than the rate of 1.1% for historical controls. Other major complications included cardiac failure (0.9% of study patients), atrioventricular fistula or pseudoaneurysm at the groin puncture site (0.7%), and deep vein thrombosis or pulmonary thromboembolism (0.3%).
Medtronic funded the pivotal study on which approval of the Micra pacemaker was based. Dr. Reynolds had no relevant financial disclosures. Several coinvestigators reported financial relationships with Medtronic and several other cardiac device manufacturers.
The Food and Drug Administration has approved the first leadless pacemaker, the Micra transcatheter pacing system, the FDA stated in a release accompanying its approval.
The Micra pacemaker eliminates the need for wired leads and the risk of associated complications. The single-chamber ventricular pacemaker is 93% smaller than traditional pacemakers, according to a summary document submitted to the FDA by Medtronic, which makes the device. Like other ventricular pacemakers, Micra provides rate-adaptive pacing, with automated pacing capture threshold management to maximize battery life, which the company estimates at about 10 years.
The pacemaker is inserted directly into the right ventricle through the femoral vein by means of a steerable catheter. Pressing a button on the distal end of the catheter releases four flexible, electrically inactive nitinol tines that hook into the myocardium to secure the device. Engagement by two tines exerts 15 times the amount of force needed to secure the device in place, according to Medtronic.
The device’s approval was based on a pivotal prospective, nonrandomized uncontrolled study of 719 patients at 56 investigational sites in North America, Europe, Asia, Australia, and Africa. The primary efficacy endpoint, low and stable pacing capture thresholds at 6 months (up to 2.0 V at a pulse width of 0.24 milliseconds and an increase of up to 1.5 V from the time of implantation) was achieved for 98% of patients (95% confidence interval, 96%-99.5%), reported Dr. Dwight Reynolds of the University of Oklahoma Health Sciences Center in Oklahoma City and his associates (N Engl J Med. 2016 Feb. 11. doi: 10.1056/NEJMoa1511643).
The researchers also compared safety outcomes among Micra recipients and 2,667 historical controls from six previously published studies. The Micra pacemaker was associated with significantly lower hospitalization and system revision rates, with “no systemic infections, no pneumothoraxes, and no radiographically visible dislodgements or device emboli,” they said. In all, 4% of Micra recipients had complications leading to death or requiring invasive revision, treatment cessation, or hospitalization, which resembled recent reports of transvenous systems and was significantly lower than the rate for historical controls, according to the investigators. However, the rate of cardiac perforation or effusion was 1.6%, slightly higher than the rate of 1.1% for historical controls. Other major complications included cardiac failure (0.9% of study patients), atrioventricular fistula or pseudoaneurysm at the groin puncture site (0.7%), and deep vein thrombosis or pulmonary thromboembolism (0.3%).
Medtronic funded the pivotal study on which approval of the Micra pacemaker was based. Dr. Reynolds had no relevant financial disclosures. Several coinvestigators reported financial relationships with Medtronic and several other cardiac device manufacturers.
The Food and Drug Administration has approved the first leadless pacemaker, the Micra transcatheter pacing system, the FDA stated in a release accompanying its approval.
The Micra pacemaker eliminates the need for wired leads and the risk of associated complications. The single-chamber ventricular pacemaker is 93% smaller than traditional pacemakers, according to a summary document submitted to the FDA by Medtronic, which makes the device. Like other ventricular pacemakers, Micra provides rate-adaptive pacing, with automated pacing capture threshold management to maximize battery life, which the company estimates at about 10 years.
The pacemaker is inserted directly into the right ventricle through the femoral vein by means of a steerable catheter. Pressing a button on the distal end of the catheter releases four flexible, electrically inactive nitinol tines that hook into the myocardium to secure the device. Engagement by two tines exerts 15 times the amount of force needed to secure the device in place, according to Medtronic.
The device’s approval was based on a pivotal prospective, nonrandomized uncontrolled study of 719 patients at 56 investigational sites in North America, Europe, Asia, Australia, and Africa. The primary efficacy endpoint, low and stable pacing capture thresholds at 6 months (up to 2.0 V at a pulse width of 0.24 milliseconds and an increase of up to 1.5 V from the time of implantation) was achieved for 98% of patients (95% confidence interval, 96%-99.5%), reported Dr. Dwight Reynolds of the University of Oklahoma Health Sciences Center in Oklahoma City and his associates (N Engl J Med. 2016 Feb. 11. doi: 10.1056/NEJMoa1511643).
The researchers also compared safety outcomes among Micra recipients and 2,667 historical controls from six previously published studies. The Micra pacemaker was associated with significantly lower hospitalization and system revision rates, with “no systemic infections, no pneumothoraxes, and no radiographically visible dislodgements or device emboli,” they said. In all, 4% of Micra recipients had complications leading to death or requiring invasive revision, treatment cessation, or hospitalization, which resembled recent reports of transvenous systems and was significantly lower than the rate for historical controls, according to the investigators. However, the rate of cardiac perforation or effusion was 1.6%, slightly higher than the rate of 1.1% for historical controls. Other major complications included cardiac failure (0.9% of study patients), atrioventricular fistula or pseudoaneurysm at the groin puncture site (0.7%), and deep vein thrombosis or pulmonary thromboembolism (0.3%).
Medtronic funded the pivotal study on which approval of the Micra pacemaker was based. Dr. Reynolds had no relevant financial disclosures. Several coinvestigators reported financial relationships with Medtronic and several other cardiac device manufacturers.
Study raises questions about cost effectiveness of robot-assisted hysterectomy
With few exceptions, the rates of complications, readmissions, and reoperations were similar among patients who underwent robotic hysterectomy for benign indications, compared with those who underwent the procedure by other minimally invasive routes, results from a large analysis demonstrated.
Yet the price tag for nonrobotic, minimally invasive approaches to hysterectomy was 24% lower overall per case.
“In general, people tend to favor newer technologies over older ones because the assumption is that because it’s new, it’s better,” Dr. Carolyn W. Swenson, lead study author, said in an interview before the annual scientific meeting of the Society of Gynecologic Surgeons. “Physicians are not immune to this kind of thinking. But in medicine, we have an obligation to use evidence-based practices to try and optimize outcomes for our patients. If study after study is concluding that, for benign hysterectomy, the additional cost of the robot doesn’t produce better outcomes, then we should be seriously evaluating why and how we choose to use this tool.”
In the past 10 years, use of the robot for benign hysterectomy has increased by more than 25-fold in the Unites States, while other routes of minimally invasive hysterectomy (vaginal and conventional laparoscopic) have decreased, according to Dr. Swenson, a specialist in female pelvic medicine and reconstructive surgery at the University of Michigan, Ann Arbor.
“We know that robot-assisted technology adds, on average, $2,000 to $3,000 per hysterectomy, but that major complications are no different when compared to conventional laparoscopy,” she said. “Vaginal hysterectomy is actually the most minimally invasive and most cost-effective route and it’s also associated with lower complications compared to abdominal and conventional laparoscopic routes. But vaginal hysterectomy is often left out of comparative studies with robotic hysterectomy. So what we’ve been missing up to this point is a study comparing outcomes between robot-assisted laparoscopy and all other routes of minimally invasive hysterectomy, including vaginal and vaginal-assisted laparoscopic routes in addition to conventional laparoscopy.”
In an effort to compare the clinical outcomes and the estimated cost of robot-assisted hysterectomy to all other routes of minimally invasive hysterectomy for benign indications, the researchers analyzed records from a statewide database in Michigan for all such procedures performed from July 1, 2012, to July 1, 2014. They used propensity-matched scoring to control for demographic, clinical, and hospital factors and went on to perform a one-to-one match between women who had a hysterectomy with robotic assistance, and those had a hysterectomy by other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Next, they compared the two cohorts for perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmission, and reoperation.
Dr. Swenson reported results from 11,004 hysterectomy cases. Of these, 6,222 were performed with robotic assistance, while the remaining 4,782 were performed via other minimally-invasive surgical routes. Over the study period, the proportion of hysterectomies performed with robotic assistance ranged from 43% to 45%, while rates of laparoscopy were 10%-13%, and rates of vaginal hysterectomy (with or without laparoscopy) were 19%-24%.
“I was surprised at how many robotic hysterectomies are being done in the state of Michigan for benign indications,” she said. “The rate is over three times the national average.”
After the propensity score analysis was done, 1,338 hysterectomies from each group were successfully matched and the researchers found that compared with the other minimally invasive routes, hysterectomy cases done with robotic assistance had lower estimated blood loss (94.2 vs. 175.3 mL, respectively; P less than .0001); longer surgical time (2.3 vs. 2 hours; P less .0001), and larger specimen weights (178.9 vs. 160.6 grams; P less than .0001). Intraoperative and bladder complications were similar between the two groups.
Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01) and was driven by lower rates of superficial surgical site infections (SSIs) (.07% vs. .7%; P = .01) and blood transfusion (.8% vs. 1.9%; P = .02). However, rates of major complications including deep/organ space SSI, thromboembolic events, MI/stroke, pneumonia, sepsis or death, and readmission and reoperation rates did not differ between the two groups.
After applying hospital cost estimates drawn from published data to results from the hysterectomies included in the propensity match, Dr. Swenson and her associates estimated that the nonrobotic minimally invasive hysterectomy routes led to a 24% lower overall cost per case ($10,160, compared with $13,429 per case performed with robotic assistance), even when considering the cost of additional cases of superficial SSI and blood transfusion. This calculation excluded maintenance costs of the robot.
“Because utilization of robotic hysterectomy for benign indications in Michigan is so much higher than the national average, the generalizability our findings might be limited,” she said. “Also, our cost data were based on estimates from the literature and were not linked to cases in our database, which would have been ideal.”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Swenson reported having no financial disclosures.
With few exceptions, the rates of complications, readmissions, and reoperations were similar among patients who underwent robotic hysterectomy for benign indications, compared with those who underwent the procedure by other minimally invasive routes, results from a large analysis demonstrated.
Yet the price tag for nonrobotic, minimally invasive approaches to hysterectomy was 24% lower overall per case.
“In general, people tend to favor newer technologies over older ones because the assumption is that because it’s new, it’s better,” Dr. Carolyn W. Swenson, lead study author, said in an interview before the annual scientific meeting of the Society of Gynecologic Surgeons. “Physicians are not immune to this kind of thinking. But in medicine, we have an obligation to use evidence-based practices to try and optimize outcomes for our patients. If study after study is concluding that, for benign hysterectomy, the additional cost of the robot doesn’t produce better outcomes, then we should be seriously evaluating why and how we choose to use this tool.”
In the past 10 years, use of the robot for benign hysterectomy has increased by more than 25-fold in the Unites States, while other routes of minimally invasive hysterectomy (vaginal and conventional laparoscopic) have decreased, according to Dr. Swenson, a specialist in female pelvic medicine and reconstructive surgery at the University of Michigan, Ann Arbor.
“We know that robot-assisted technology adds, on average, $2,000 to $3,000 per hysterectomy, but that major complications are no different when compared to conventional laparoscopy,” she said. “Vaginal hysterectomy is actually the most minimally invasive and most cost-effective route and it’s also associated with lower complications compared to abdominal and conventional laparoscopic routes. But vaginal hysterectomy is often left out of comparative studies with robotic hysterectomy. So what we’ve been missing up to this point is a study comparing outcomes between robot-assisted laparoscopy and all other routes of minimally invasive hysterectomy, including vaginal and vaginal-assisted laparoscopic routes in addition to conventional laparoscopy.”
In an effort to compare the clinical outcomes and the estimated cost of robot-assisted hysterectomy to all other routes of minimally invasive hysterectomy for benign indications, the researchers analyzed records from a statewide database in Michigan for all such procedures performed from July 1, 2012, to July 1, 2014. They used propensity-matched scoring to control for demographic, clinical, and hospital factors and went on to perform a one-to-one match between women who had a hysterectomy with robotic assistance, and those had a hysterectomy by other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Next, they compared the two cohorts for perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmission, and reoperation.
Dr. Swenson reported results from 11,004 hysterectomy cases. Of these, 6,222 were performed with robotic assistance, while the remaining 4,782 were performed via other minimally-invasive surgical routes. Over the study period, the proportion of hysterectomies performed with robotic assistance ranged from 43% to 45%, while rates of laparoscopy were 10%-13%, and rates of vaginal hysterectomy (with or without laparoscopy) were 19%-24%.
“I was surprised at how many robotic hysterectomies are being done in the state of Michigan for benign indications,” she said. “The rate is over three times the national average.”
After the propensity score analysis was done, 1,338 hysterectomies from each group were successfully matched and the researchers found that compared with the other minimally invasive routes, hysterectomy cases done with robotic assistance had lower estimated blood loss (94.2 vs. 175.3 mL, respectively; P less than .0001); longer surgical time (2.3 vs. 2 hours; P less .0001), and larger specimen weights (178.9 vs. 160.6 grams; P less than .0001). Intraoperative and bladder complications were similar between the two groups.
Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01) and was driven by lower rates of superficial surgical site infections (SSIs) (.07% vs. .7%; P = .01) and blood transfusion (.8% vs. 1.9%; P = .02). However, rates of major complications including deep/organ space SSI, thromboembolic events, MI/stroke, pneumonia, sepsis or death, and readmission and reoperation rates did not differ between the two groups.
After applying hospital cost estimates drawn from published data to results from the hysterectomies included in the propensity match, Dr. Swenson and her associates estimated that the nonrobotic minimally invasive hysterectomy routes led to a 24% lower overall cost per case ($10,160, compared with $13,429 per case performed with robotic assistance), even when considering the cost of additional cases of superficial SSI and blood transfusion. This calculation excluded maintenance costs of the robot.
“Because utilization of robotic hysterectomy for benign indications in Michigan is so much higher than the national average, the generalizability our findings might be limited,” she said. “Also, our cost data were based on estimates from the literature and were not linked to cases in our database, which would have been ideal.”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Swenson reported having no financial disclosures.
With few exceptions, the rates of complications, readmissions, and reoperations were similar among patients who underwent robotic hysterectomy for benign indications, compared with those who underwent the procedure by other minimally invasive routes, results from a large analysis demonstrated.
Yet the price tag for nonrobotic, minimally invasive approaches to hysterectomy was 24% lower overall per case.
“In general, people tend to favor newer technologies over older ones because the assumption is that because it’s new, it’s better,” Dr. Carolyn W. Swenson, lead study author, said in an interview before the annual scientific meeting of the Society of Gynecologic Surgeons. “Physicians are not immune to this kind of thinking. But in medicine, we have an obligation to use evidence-based practices to try and optimize outcomes for our patients. If study after study is concluding that, for benign hysterectomy, the additional cost of the robot doesn’t produce better outcomes, then we should be seriously evaluating why and how we choose to use this tool.”
In the past 10 years, use of the robot for benign hysterectomy has increased by more than 25-fold in the Unites States, while other routes of minimally invasive hysterectomy (vaginal and conventional laparoscopic) have decreased, according to Dr. Swenson, a specialist in female pelvic medicine and reconstructive surgery at the University of Michigan, Ann Arbor.
“We know that robot-assisted technology adds, on average, $2,000 to $3,000 per hysterectomy, but that major complications are no different when compared to conventional laparoscopy,” she said. “Vaginal hysterectomy is actually the most minimally invasive and most cost-effective route and it’s also associated with lower complications compared to abdominal and conventional laparoscopic routes. But vaginal hysterectomy is often left out of comparative studies with robotic hysterectomy. So what we’ve been missing up to this point is a study comparing outcomes between robot-assisted laparoscopy and all other routes of minimally invasive hysterectomy, including vaginal and vaginal-assisted laparoscopic routes in addition to conventional laparoscopy.”
In an effort to compare the clinical outcomes and the estimated cost of robot-assisted hysterectomy to all other routes of minimally invasive hysterectomy for benign indications, the researchers analyzed records from a statewide database in Michigan for all such procedures performed from July 1, 2012, to July 1, 2014. They used propensity-matched scoring to control for demographic, clinical, and hospital factors and went on to perform a one-to-one match between women who had a hysterectomy with robotic assistance, and those had a hysterectomy by other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Next, they compared the two cohorts for perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmission, and reoperation.
Dr. Swenson reported results from 11,004 hysterectomy cases. Of these, 6,222 were performed with robotic assistance, while the remaining 4,782 were performed via other minimally-invasive surgical routes. Over the study period, the proportion of hysterectomies performed with robotic assistance ranged from 43% to 45%, while rates of laparoscopy were 10%-13%, and rates of vaginal hysterectomy (with or without laparoscopy) were 19%-24%.
“I was surprised at how many robotic hysterectomies are being done in the state of Michigan for benign indications,” she said. “The rate is over three times the national average.”
After the propensity score analysis was done, 1,338 hysterectomies from each group were successfully matched and the researchers found that compared with the other minimally invasive routes, hysterectomy cases done with robotic assistance had lower estimated blood loss (94.2 vs. 175.3 mL, respectively; P less than .0001); longer surgical time (2.3 vs. 2 hours; P less .0001), and larger specimen weights (178.9 vs. 160.6 grams; P less than .0001). Intraoperative and bladder complications were similar between the two groups.
Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01) and was driven by lower rates of superficial surgical site infections (SSIs) (.07% vs. .7%; P = .01) and blood transfusion (.8% vs. 1.9%; P = .02). However, rates of major complications including deep/organ space SSI, thromboembolic events, MI/stroke, pneumonia, sepsis or death, and readmission and reoperation rates did not differ between the two groups.
After applying hospital cost estimates drawn from published data to results from the hysterectomies included in the propensity match, Dr. Swenson and her associates estimated that the nonrobotic minimally invasive hysterectomy routes led to a 24% lower overall cost per case ($10,160, compared with $13,429 per case performed with robotic assistance), even when considering the cost of additional cases of superficial SSI and blood transfusion. This calculation excluded maintenance costs of the robot.
“Because utilization of robotic hysterectomy for benign indications in Michigan is so much higher than the national average, the generalizability our findings might be limited,” she said. “Also, our cost data were based on estimates from the literature and were not linked to cases in our database, which would have been ideal.”
The meeting was jointly sponsored by the American College of Surgeons.
Dr. Swenson reported having no financial disclosures.
FROM SGS 2016
Key clinical point: Major complication rates were similar for hysterectomies performed for benign indications using robotic assistance, compared with those performed via other MIS routes, but the robotic costs were higher.
Major finding: Compared with the other minimally invasive hysterectomy routes, the rate of any postoperative complication was lower among cases performed with robotic assistance (3.5% vs. 5.6%; P = .01), but rates for major complications did not differ between the groups.
Data source: An analysis of state records from 11,004 hysterectomies performed in Michigan from July 1, 2012, to July 1, 2014.
Disclosures: Dr. Swenson reported having no financial disclosures.
Surgeons commonly off the mark in estimating blood loss
MONTREAL – Surgeons, nurses, and anesthesia providers were all pretty bad at estimating surgical blood loss in a small study. And more experience doesn’t improve accuracy, though experienced providers were more confident in their estimates.
These were the findings from a study that simulated operating room scenarios and asked providers to estimate blood loss. “Estimation of blood loss is inaccurate and unreliable,” Dr. Luke Rothermel said at the Central Surgical Association’s annual meeting.
Dr. Rothermel, a resident at Case Western Reserve University, Cleveland, noted that although the Joint Commission requires operative notes to contain estimated blood loss, “no study in the United States has compared the characteristics of operating room personnel or conditions associated with improved accuracy or reliability of blood loss estimation.”
Beyond the required reporting, estimating blood loss (EBL) also provides important guidance in perioperative care. Still, said Dr. Rothermel, previous studies have shown that EBL is typically inaccurate.
To assess providers’ ability to be accurate and reliable in estimating blood loss, Dr. Rothermel and his collaborator, Dr. Jeremy Lipman, assistant residency director at MetroHealth, Cleveland, designed a study to simulate three different operating room scenarios, involving high, medium, and low blood loss volumes. The materials used, such as blood-soaked sponges and suction canisters, were identical to what’s actually used in the operating room (porcine blood was used in the simulations).
Before the study, Dr. Rothermel said that he and Dr. Lipman hypothesized that those providers who had more experience and those who were working at the operating field would be more accurate in estimating blood loss. They also hypothesized that estimations in procedures with lower volumes of blood loss would be more accurate.
The study recruited providers from the surgery, anesthesia, and nursing services at an urban level 1 trauma center. Each scenario included a written description of the procedure performed and the course of surgery, and participants could handle study materials for each scenario under the supervision of study staff.
A total of 60 participants (22 from surgery, 17 from anesthesia, and 21 from nursing) participated; they had an average of 12.8 years of experience. The surgical participants included surgical scrub techs, trainees, and attending physicians. Anesthesia participants included anesthesia assistants, CRNAs, trainees, and attending physicians. Nursing participants were all RNs.
The findings? All over the board: “There was no association between specialty, years of experience, or confidence in ability with the consistency or accuracy of estimated blood loss,” said Dr. Rothermel.
Most participants were far shy of the mark, with just 5% of study participants overall able to come within 25% accuracy in judging EBL in all scenarios. Just over a quarter were consistent in over- or underestimating blood loss.
These findings held true across scenarios, across disciplines, and regardless of the number of years of experience. “Increased years of experience trended toward increased error,” said Dr. Rothermel, though the difference was not statistically significant. However, those with more years of experience tended to be more confident of their judgments.
Dr. Rothermel noted the small study size and single institution studied as limitations. Also, “this model was not a high fidelity representation of the OR experience, “ he said, explaining that during surgery, caregivers continually assess intraoperative blood loss and may form an estimate in a different – and potentially more accurate – manner than occurs when presented with the contrived presentation of a scenario.
The study calls into question the validity of using EBL as a quality indicator in assessing physician performance and patient outcomes, said Dr. Rothermel, who had no financial disclosures.
On Twitter @karioakes
MONTREAL – Surgeons, nurses, and anesthesia providers were all pretty bad at estimating surgical blood loss in a small study. And more experience doesn’t improve accuracy, though experienced providers were more confident in their estimates.
These were the findings from a study that simulated operating room scenarios and asked providers to estimate blood loss. “Estimation of blood loss is inaccurate and unreliable,” Dr. Luke Rothermel said at the Central Surgical Association’s annual meeting.
Dr. Rothermel, a resident at Case Western Reserve University, Cleveland, noted that although the Joint Commission requires operative notes to contain estimated blood loss, “no study in the United States has compared the characteristics of operating room personnel or conditions associated with improved accuracy or reliability of blood loss estimation.”
Beyond the required reporting, estimating blood loss (EBL) also provides important guidance in perioperative care. Still, said Dr. Rothermel, previous studies have shown that EBL is typically inaccurate.
To assess providers’ ability to be accurate and reliable in estimating blood loss, Dr. Rothermel and his collaborator, Dr. Jeremy Lipman, assistant residency director at MetroHealth, Cleveland, designed a study to simulate three different operating room scenarios, involving high, medium, and low blood loss volumes. The materials used, such as blood-soaked sponges and suction canisters, were identical to what’s actually used in the operating room (porcine blood was used in the simulations).
Before the study, Dr. Rothermel said that he and Dr. Lipman hypothesized that those providers who had more experience and those who were working at the operating field would be more accurate in estimating blood loss. They also hypothesized that estimations in procedures with lower volumes of blood loss would be more accurate.
The study recruited providers from the surgery, anesthesia, and nursing services at an urban level 1 trauma center. Each scenario included a written description of the procedure performed and the course of surgery, and participants could handle study materials for each scenario under the supervision of study staff.
A total of 60 participants (22 from surgery, 17 from anesthesia, and 21 from nursing) participated; they had an average of 12.8 years of experience. The surgical participants included surgical scrub techs, trainees, and attending physicians. Anesthesia participants included anesthesia assistants, CRNAs, trainees, and attending physicians. Nursing participants were all RNs.
The findings? All over the board: “There was no association between specialty, years of experience, or confidence in ability with the consistency or accuracy of estimated blood loss,” said Dr. Rothermel.
Most participants were far shy of the mark, with just 5% of study participants overall able to come within 25% accuracy in judging EBL in all scenarios. Just over a quarter were consistent in over- or underestimating blood loss.
These findings held true across scenarios, across disciplines, and regardless of the number of years of experience. “Increased years of experience trended toward increased error,” said Dr. Rothermel, though the difference was not statistically significant. However, those with more years of experience tended to be more confident of their judgments.
Dr. Rothermel noted the small study size and single institution studied as limitations. Also, “this model was not a high fidelity representation of the OR experience, “ he said, explaining that during surgery, caregivers continually assess intraoperative blood loss and may form an estimate in a different – and potentially more accurate – manner than occurs when presented with the contrived presentation of a scenario.
The study calls into question the validity of using EBL as a quality indicator in assessing physician performance and patient outcomes, said Dr. Rothermel, who had no financial disclosures.
On Twitter @karioakes
MONTREAL – Surgeons, nurses, and anesthesia providers were all pretty bad at estimating surgical blood loss in a small study. And more experience doesn’t improve accuracy, though experienced providers were more confident in their estimates.
These were the findings from a study that simulated operating room scenarios and asked providers to estimate blood loss. “Estimation of blood loss is inaccurate and unreliable,” Dr. Luke Rothermel said at the Central Surgical Association’s annual meeting.
Dr. Rothermel, a resident at Case Western Reserve University, Cleveland, noted that although the Joint Commission requires operative notes to contain estimated blood loss, “no study in the United States has compared the characteristics of operating room personnel or conditions associated with improved accuracy or reliability of blood loss estimation.”
Beyond the required reporting, estimating blood loss (EBL) also provides important guidance in perioperative care. Still, said Dr. Rothermel, previous studies have shown that EBL is typically inaccurate.
To assess providers’ ability to be accurate and reliable in estimating blood loss, Dr. Rothermel and his collaborator, Dr. Jeremy Lipman, assistant residency director at MetroHealth, Cleveland, designed a study to simulate three different operating room scenarios, involving high, medium, and low blood loss volumes. The materials used, such as blood-soaked sponges and suction canisters, were identical to what’s actually used in the operating room (porcine blood was used in the simulations).
Before the study, Dr. Rothermel said that he and Dr. Lipman hypothesized that those providers who had more experience and those who were working at the operating field would be more accurate in estimating blood loss. They also hypothesized that estimations in procedures with lower volumes of blood loss would be more accurate.
The study recruited providers from the surgery, anesthesia, and nursing services at an urban level 1 trauma center. Each scenario included a written description of the procedure performed and the course of surgery, and participants could handle study materials for each scenario under the supervision of study staff.
A total of 60 participants (22 from surgery, 17 from anesthesia, and 21 from nursing) participated; they had an average of 12.8 years of experience. The surgical participants included surgical scrub techs, trainees, and attending physicians. Anesthesia participants included anesthesia assistants, CRNAs, trainees, and attending physicians. Nursing participants were all RNs.
The findings? All over the board: “There was no association between specialty, years of experience, or confidence in ability with the consistency or accuracy of estimated blood loss,” said Dr. Rothermel.
Most participants were far shy of the mark, with just 5% of study participants overall able to come within 25% accuracy in judging EBL in all scenarios. Just over a quarter were consistent in over- or underestimating blood loss.
These findings held true across scenarios, across disciplines, and regardless of the number of years of experience. “Increased years of experience trended toward increased error,” said Dr. Rothermel, though the difference was not statistically significant. However, those with more years of experience tended to be more confident of their judgments.
Dr. Rothermel noted the small study size and single institution studied as limitations. Also, “this model was not a high fidelity representation of the OR experience, “ he said, explaining that during surgery, caregivers continually assess intraoperative blood loss and may form an estimate in a different – and potentially more accurate – manner than occurs when presented with the contrived presentation of a scenario.
The study calls into question the validity of using EBL as a quality indicator in assessing physician performance and patient outcomes, said Dr. Rothermel, who had no financial disclosures.
On Twitter @karioakes
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Surgery, anesthesia, and nursing providers were inaccurate and unreliable in estimating surgical blood loss.
Major finding: Only 5% of providers could come within 25% accuracy of simulated surgical blood loss.
Data source: Simulations of surgical scenarios depicting varying amounts of blood loss using porcine blood, presented to 60 providers.
Disclosures: The study authors reported no relevant disclosures.
Patient-controlled epidural analgesia similar to intravenous
Patient-controlled epidural analgesia achieves pain control similar to that of patient-controlled intravenous analgesia after spinal fusion surgery, but is associated with a higher incidence of pruritus and paresthesia, a meta-analysis published in BMC Musculoskeletal Disorders has found.
The analysis of eight randomized controlled trials involving 482 patients found that patient-controlled epidural analgesia was associated with significantly better analgesic effects on day 1 and 2 after surgery (mean difference in visual analog scale scores of −0.47 and −0.66, respectively), but this difference was no longer statistically significant on day 3.
The study, conducted by Dr. Peng Tian of Tianjin (China) Hospital and colleagues showed that patient-controlled epidural analgesia was associated with a significant 53% higher incidence of pruritus and a threefold increase in paresthesia, compared with patient-controlled intravenous analgesia, although there were no significant differences in the rates of nausea or vomiting (BMC Musculoskeletal Disorders 2015 Dec 15. doi: 10.1186/s12891-015-0849-y).
Researchers noted that patient-controlled epidural analgesia achieves a faster analgesic effect than does patient-controlled intravenous analgesia because it acts directly on the near-operative region, but the analgesic effect of the intravenous administration lasts longer.
“The most important findings of the present meta-analysis are that the application of PCEA [patient-controlled epidural analgesia] does not more effectively relieve” pain in 3 postoperative days compared with patient-controlled intravenous analgesia, “meanwhile increasing the incidence of some complications such as pruritus and paresthesia,” wrote the investigators.
The National Natural Science Foundation of China supported the study. No conflicts of interest were declared.
Patient-controlled epidural analgesia achieves pain control similar to that of patient-controlled intravenous analgesia after spinal fusion surgery, but is associated with a higher incidence of pruritus and paresthesia, a meta-analysis published in BMC Musculoskeletal Disorders has found.
The analysis of eight randomized controlled trials involving 482 patients found that patient-controlled epidural analgesia was associated with significantly better analgesic effects on day 1 and 2 after surgery (mean difference in visual analog scale scores of −0.47 and −0.66, respectively), but this difference was no longer statistically significant on day 3.
The study, conducted by Dr. Peng Tian of Tianjin (China) Hospital and colleagues showed that patient-controlled epidural analgesia was associated with a significant 53% higher incidence of pruritus and a threefold increase in paresthesia, compared with patient-controlled intravenous analgesia, although there were no significant differences in the rates of nausea or vomiting (BMC Musculoskeletal Disorders 2015 Dec 15. doi: 10.1186/s12891-015-0849-y).
Researchers noted that patient-controlled epidural analgesia achieves a faster analgesic effect than does patient-controlled intravenous analgesia because it acts directly on the near-operative region, but the analgesic effect of the intravenous administration lasts longer.
“The most important findings of the present meta-analysis are that the application of PCEA [patient-controlled epidural analgesia] does not more effectively relieve” pain in 3 postoperative days compared with patient-controlled intravenous analgesia, “meanwhile increasing the incidence of some complications such as pruritus and paresthesia,” wrote the investigators.
The National Natural Science Foundation of China supported the study. No conflicts of interest were declared.
Patient-controlled epidural analgesia achieves pain control similar to that of patient-controlled intravenous analgesia after spinal fusion surgery, but is associated with a higher incidence of pruritus and paresthesia, a meta-analysis published in BMC Musculoskeletal Disorders has found.
The analysis of eight randomized controlled trials involving 482 patients found that patient-controlled epidural analgesia was associated with significantly better analgesic effects on day 1 and 2 after surgery (mean difference in visual analog scale scores of −0.47 and −0.66, respectively), but this difference was no longer statistically significant on day 3.
The study, conducted by Dr. Peng Tian of Tianjin (China) Hospital and colleagues showed that patient-controlled epidural analgesia was associated with a significant 53% higher incidence of pruritus and a threefold increase in paresthesia, compared with patient-controlled intravenous analgesia, although there were no significant differences in the rates of nausea or vomiting (BMC Musculoskeletal Disorders 2015 Dec 15. doi: 10.1186/s12891-015-0849-y).
Researchers noted that patient-controlled epidural analgesia achieves a faster analgesic effect than does patient-controlled intravenous analgesia because it acts directly on the near-operative region, but the analgesic effect of the intravenous administration lasts longer.
“The most important findings of the present meta-analysis are that the application of PCEA [patient-controlled epidural analgesia] does not more effectively relieve” pain in 3 postoperative days compared with patient-controlled intravenous analgesia, “meanwhile increasing the incidence of some complications such as pruritus and paresthesia,” wrote the investigators.
The National Natural Science Foundation of China supported the study. No conflicts of interest were declared.
FROM BMC MUSCULOSKELETAL DISORDERS
Key clinical point: Patient-controlled epidural analgesia achieves pain control similar to that of patient-controlled intravenous analgesia after spinal fusion surgery, but with more pruritus and paresthesia.
Major finding: Patient-controlled epidural analgesia achieved greater analgesic effects on day 1 and 2 after surgery but these differences were no longer significant by day 3.
Data source: A meta-analysis of eight randomized controlled trials in 482 patients undergoing spinal fusion surgery.
Disclosures: The National Natural Science Foundation of China supported the study. No conflicts of interest were declared.
Uterus transplant update: Fungal infection may have caused complication
The failure of the first U.S. uterus transplant may have been due a complication triggered by an infection of Candida, according to the Cleveland Clinic.
“Preliminary results suggest that the complication was due to an infection caused by an organism that is commonly found in a woman’s reproductive system,” officials at the Cleveland Clinic said in an April 8 statement. “The infection appears to have compromised the blood supply to the uterus, causing the need for its removal. There is an ongoing review of all the data and the team is modifying the protocol to reduce the chances of this complication occurring again in the future. The health of our patient is and has always been our primary concern.”
A team of surgeons at the Cleveland Clinic performed the first U.S. uterus transplant on a 26-year-old woman with uterine factor infertility on Feb. 24, but had to remove the transplanted uterus several days later following a sudden complication. The transplant is part of a study aimed at achieving pregnancy in women with uterine factor infertility. The study is still ongoing.
On Twitter @maryellenny
The failure of the first U.S. uterus transplant may have been due a complication triggered by an infection of Candida, according to the Cleveland Clinic.
“Preliminary results suggest that the complication was due to an infection caused by an organism that is commonly found in a woman’s reproductive system,” officials at the Cleveland Clinic said in an April 8 statement. “The infection appears to have compromised the blood supply to the uterus, causing the need for its removal. There is an ongoing review of all the data and the team is modifying the protocol to reduce the chances of this complication occurring again in the future. The health of our patient is and has always been our primary concern.”
A team of surgeons at the Cleveland Clinic performed the first U.S. uterus transplant on a 26-year-old woman with uterine factor infertility on Feb. 24, but had to remove the transplanted uterus several days later following a sudden complication. The transplant is part of a study aimed at achieving pregnancy in women with uterine factor infertility. The study is still ongoing.
On Twitter @maryellenny
The failure of the first U.S. uterus transplant may have been due a complication triggered by an infection of Candida, according to the Cleveland Clinic.
“Preliminary results suggest that the complication was due to an infection caused by an organism that is commonly found in a woman’s reproductive system,” officials at the Cleveland Clinic said in an April 8 statement. “The infection appears to have compromised the blood supply to the uterus, causing the need for its removal. There is an ongoing review of all the data and the team is modifying the protocol to reduce the chances of this complication occurring again in the future. The health of our patient is and has always been our primary concern.”
A team of surgeons at the Cleveland Clinic performed the first U.S. uterus transplant on a 26-year-old woman with uterine factor infertility on Feb. 24, but had to remove the transplanted uterus several days later following a sudden complication. The transplant is part of a study aimed at achieving pregnancy in women with uterine factor infertility. The study is still ongoing.
On Twitter @maryellenny