User login
Official Newspaper of the American College of Surgeons
Study Spotlights Disparities in Specialized Epilepsy Care
SAN DIEGO – People with epilepsy who lacked health insurance were less likely to receive specialized epilepsy care in the form of video EEG monitoring and surgery, as were those on Medicaid or who were elderly, black, Hispanic, or had comorbidities, a study of nearly 200,000 adults in California demonstrated.
"Specialized epilepsy care can provide proper diagnosis and therapeutic interventions to control seizures and improve quality of life," Nicholas K. Schiltz said in an interview in advance of the annual meeting of the American Epilepsy Society, where the work was presented. "Previous studies have found evidence of disparities in access to epilepsy specialists among persons with low socioeconomic status and among racial and ethnic minorities. Other studies have found patients with Medicaid have difficulty accessing specialty care. This is the first report that explores the impact of both individual and community characteristics on disparities in access to specialized epilepsy care in persons with epilepsy."
For the study, Mr. Schiltz, a PhD candidate in the department of epidemiology and biostatistics at Case Western Reserve University, Cleveland, and his associates performed a cross-sectional analysis using data between 2005 and 2009 from the California State Inpatient Sample, the State Ambulatory Surgery Database, and the State Emergency Department Database, which provided information on all hospital discharges, ambulatory surgeries, and emergency department visits. The researchers linked these datasets to a 2009 Area Resource File, which provided health resource information and socioeconomic characteristics at the county level, and used a two-level hierarchical logistic regression model to determine the probability that an individual would receive video EEG monitoring or surgery. Individual-level predictors included insurance status, age, race/ethnicity, gender, and comorbidities, while county level predictors included proximity to a comprehensive epilepsy center and social and economic characteristics.
Of the 195,166 adults with epilepsy who were included in the study, 4,707 had video EEG monitoring and 779 underwent surgery during the study period. Mr. Schiltz reported that uninsured individuals were less likely to have video EEG monitoring (adjusted odds ratio [AOR] 0.16) or surgery (AOR 0.05). Similarly, those on Medicaid had significantly lower odds of receiving video EEG monitoring (AOR 0.65) and surgery (AOR 0.38), compared with individuals who had private insurance.
Other individual characteristics significantly associated with a low likelihood of having video EEG monitoring including being black (AOR 0.56), Hispanic (AOR 0.81), older (AOR 0.51), and having comorbid conditions (AOR 0.62).
Other individual characteristics associated with a low likelihood of having surgery including being black (AOR 0.22), older (AOR 0.44), and having comorbid conditions (AOR 0.47).
The researchers also found that adults who routinely received their services in an area where epilepsy centers are located were more likely to undergo video EEG monitoring (AOR 1.61) and surgery (AOR 2.64) than were those who had a regular source of care elsewhere.
This effect size "was surprising to us as it shows that receiving care in the area proximate to an epilepsy center is as important a factor as individual factors in determining access to specialty care," Mr. Schiltz said. "It is possible that neurologists or physicians who are in the area close to epilepsy centers are more aware and therefore refer patients to the epilepsy centers. We were also surprised that other community-level characteristics such as the poverty and employment rate were not significant predictors of access, as studies in other areas of clinical and health services research have found this to be the case."
The study’s overall findings, he added, make continued emphasis on highlighting awareness of epilepsy management among general neurologists and primary care physicians "as important as ever, as they serve as the main gatekeepers for patients to access specialized epilepsy care."
Mr. Schiltz acknowledged certain limitations of the study, including the fact that it relied on hospital billing records, which "do not contain detailed clinical information," he said. "In addition, we only identify specialized epilepsy centers based on the data from the National Association of Epilepsy Centers (NAEC). Some of the hospitals that provide specialized epilepsy care might not be a member of the NAEC. We looked at geographic factors at the county level, which may be somewhat crude in a state like California with diverse populations within counties."
Support for the study was provided by the Epilepsy Foundation, a training grant from the Agency for Healthcare Research and Quality, and a grant from the National Center for Research Resources. Mr. Schiltz received support for travel to the meeting from his receipt of an American Epilepsy Society Young Investigator Award.
Mr. Schiltz said that he had no relevant financial conflicts to disclose.
SAN DIEGO – People with epilepsy who lacked health insurance were less likely to receive specialized epilepsy care in the form of video EEG monitoring and surgery, as were those on Medicaid or who were elderly, black, Hispanic, or had comorbidities, a study of nearly 200,000 adults in California demonstrated.
"Specialized epilepsy care can provide proper diagnosis and therapeutic interventions to control seizures and improve quality of life," Nicholas K. Schiltz said in an interview in advance of the annual meeting of the American Epilepsy Society, where the work was presented. "Previous studies have found evidence of disparities in access to epilepsy specialists among persons with low socioeconomic status and among racial and ethnic minorities. Other studies have found patients with Medicaid have difficulty accessing specialty care. This is the first report that explores the impact of both individual and community characteristics on disparities in access to specialized epilepsy care in persons with epilepsy."
For the study, Mr. Schiltz, a PhD candidate in the department of epidemiology and biostatistics at Case Western Reserve University, Cleveland, and his associates performed a cross-sectional analysis using data between 2005 and 2009 from the California State Inpatient Sample, the State Ambulatory Surgery Database, and the State Emergency Department Database, which provided information on all hospital discharges, ambulatory surgeries, and emergency department visits. The researchers linked these datasets to a 2009 Area Resource File, which provided health resource information and socioeconomic characteristics at the county level, and used a two-level hierarchical logistic regression model to determine the probability that an individual would receive video EEG monitoring or surgery. Individual-level predictors included insurance status, age, race/ethnicity, gender, and comorbidities, while county level predictors included proximity to a comprehensive epilepsy center and social and economic characteristics.
Of the 195,166 adults with epilepsy who were included in the study, 4,707 had video EEG monitoring and 779 underwent surgery during the study period. Mr. Schiltz reported that uninsured individuals were less likely to have video EEG monitoring (adjusted odds ratio [AOR] 0.16) or surgery (AOR 0.05). Similarly, those on Medicaid had significantly lower odds of receiving video EEG monitoring (AOR 0.65) and surgery (AOR 0.38), compared with individuals who had private insurance.
Other individual characteristics significantly associated with a low likelihood of having video EEG monitoring including being black (AOR 0.56), Hispanic (AOR 0.81), older (AOR 0.51), and having comorbid conditions (AOR 0.62).
Other individual characteristics associated with a low likelihood of having surgery including being black (AOR 0.22), older (AOR 0.44), and having comorbid conditions (AOR 0.47).
The researchers also found that adults who routinely received their services in an area where epilepsy centers are located were more likely to undergo video EEG monitoring (AOR 1.61) and surgery (AOR 2.64) than were those who had a regular source of care elsewhere.
This effect size "was surprising to us as it shows that receiving care in the area proximate to an epilepsy center is as important a factor as individual factors in determining access to specialty care," Mr. Schiltz said. "It is possible that neurologists or physicians who are in the area close to epilepsy centers are more aware and therefore refer patients to the epilepsy centers. We were also surprised that other community-level characteristics such as the poverty and employment rate were not significant predictors of access, as studies in other areas of clinical and health services research have found this to be the case."
The study’s overall findings, he added, make continued emphasis on highlighting awareness of epilepsy management among general neurologists and primary care physicians "as important as ever, as they serve as the main gatekeepers for patients to access specialized epilepsy care."
Mr. Schiltz acknowledged certain limitations of the study, including the fact that it relied on hospital billing records, which "do not contain detailed clinical information," he said. "In addition, we only identify specialized epilepsy centers based on the data from the National Association of Epilepsy Centers (NAEC). Some of the hospitals that provide specialized epilepsy care might not be a member of the NAEC. We looked at geographic factors at the county level, which may be somewhat crude in a state like California with diverse populations within counties."
Support for the study was provided by the Epilepsy Foundation, a training grant from the Agency for Healthcare Research and Quality, and a grant from the National Center for Research Resources. Mr. Schiltz received support for travel to the meeting from his receipt of an American Epilepsy Society Young Investigator Award.
Mr. Schiltz said that he had no relevant financial conflicts to disclose.
SAN DIEGO – People with epilepsy who lacked health insurance were less likely to receive specialized epilepsy care in the form of video EEG monitoring and surgery, as were those on Medicaid or who were elderly, black, Hispanic, or had comorbidities, a study of nearly 200,000 adults in California demonstrated.
"Specialized epilepsy care can provide proper diagnosis and therapeutic interventions to control seizures and improve quality of life," Nicholas K. Schiltz said in an interview in advance of the annual meeting of the American Epilepsy Society, where the work was presented. "Previous studies have found evidence of disparities in access to epilepsy specialists among persons with low socioeconomic status and among racial and ethnic minorities. Other studies have found patients with Medicaid have difficulty accessing specialty care. This is the first report that explores the impact of both individual and community characteristics on disparities in access to specialized epilepsy care in persons with epilepsy."
For the study, Mr. Schiltz, a PhD candidate in the department of epidemiology and biostatistics at Case Western Reserve University, Cleveland, and his associates performed a cross-sectional analysis using data between 2005 and 2009 from the California State Inpatient Sample, the State Ambulatory Surgery Database, and the State Emergency Department Database, which provided information on all hospital discharges, ambulatory surgeries, and emergency department visits. The researchers linked these datasets to a 2009 Area Resource File, which provided health resource information and socioeconomic characteristics at the county level, and used a two-level hierarchical logistic regression model to determine the probability that an individual would receive video EEG monitoring or surgery. Individual-level predictors included insurance status, age, race/ethnicity, gender, and comorbidities, while county level predictors included proximity to a comprehensive epilepsy center and social and economic characteristics.
Of the 195,166 adults with epilepsy who were included in the study, 4,707 had video EEG monitoring and 779 underwent surgery during the study period. Mr. Schiltz reported that uninsured individuals were less likely to have video EEG monitoring (adjusted odds ratio [AOR] 0.16) or surgery (AOR 0.05). Similarly, those on Medicaid had significantly lower odds of receiving video EEG monitoring (AOR 0.65) and surgery (AOR 0.38), compared with individuals who had private insurance.
Other individual characteristics significantly associated with a low likelihood of having video EEG monitoring including being black (AOR 0.56), Hispanic (AOR 0.81), older (AOR 0.51), and having comorbid conditions (AOR 0.62).
Other individual characteristics associated with a low likelihood of having surgery including being black (AOR 0.22), older (AOR 0.44), and having comorbid conditions (AOR 0.47).
The researchers also found that adults who routinely received their services in an area where epilepsy centers are located were more likely to undergo video EEG monitoring (AOR 1.61) and surgery (AOR 2.64) than were those who had a regular source of care elsewhere.
This effect size "was surprising to us as it shows that receiving care in the area proximate to an epilepsy center is as important a factor as individual factors in determining access to specialty care," Mr. Schiltz said. "It is possible that neurologists or physicians who are in the area close to epilepsy centers are more aware and therefore refer patients to the epilepsy centers. We were also surprised that other community-level characteristics such as the poverty and employment rate were not significant predictors of access, as studies in other areas of clinical and health services research have found this to be the case."
The study’s overall findings, he added, make continued emphasis on highlighting awareness of epilepsy management among general neurologists and primary care physicians "as important as ever, as they serve as the main gatekeepers for patients to access specialized epilepsy care."
Mr. Schiltz acknowledged certain limitations of the study, including the fact that it relied on hospital billing records, which "do not contain detailed clinical information," he said. "In addition, we only identify specialized epilepsy centers based on the data from the National Association of Epilepsy Centers (NAEC). Some of the hospitals that provide specialized epilepsy care might not be a member of the NAEC. We looked at geographic factors at the county level, which may be somewhat crude in a state like California with diverse populations within counties."
Support for the study was provided by the Epilepsy Foundation, a training grant from the Agency for Healthcare Research and Quality, and a grant from the National Center for Research Resources. Mr. Schiltz received support for travel to the meeting from his receipt of an American Epilepsy Society Young Investigator Award.
Mr. Schiltz said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN EPILEPSY SOCIETY
Major Finding: Adults with epilepsy who routinely received their services in an area where epilepsy centers are located were more likely to undergo video EEG monitoring (adjusted odds ratio [AOR] 1.61) or surgery (AOR 2.64) than were those who had a regular source of care elsewhere.
Data Source: This was a cross-sectional analysis study of 195,166 California adults with epilepsy conducted between 2005 and 2009.
Disclosures: Support for the study was provided by the Epilepsy Foundation, a training grant from the Agency for Healthcare Research and Quality, and a grant from the National Center for Research Resources. Mr. Schiltz received support for travel to the meeting from his receipt of an American Epilepsy Society Young Investigator Award.
Avoiding the Fiscal Cliff: The Policy & Practice Podcast
The fiscal cliff looms. The country faces a combination of spending cuts and tax increases on Jan. 1 if Congress can’t broker a deal to stop them. But what does that mean for doctors? Well, they'll face a 2% across-the-board cut, in addition to the impending 27% cut to their Medicare reimbursements. Some experts say a 2% cut is the best deal physicians are going to get.
In other news, the ACA could be heading back to court. A lower court was recently asked to take a second look at the law’s requirement that employers offer contraceptive coverage without cost sharing. The plaintiff, Liberty University, claims the provision violates First Amendment guarantees of religious freedom. If the court accepts that argument, the case could head to the Supreme Court next year. For more details on that, check out this week’s Policy & Practice podcast.
--Frances Correa (@FMCReporting)
The fiscal cliff looms. The country faces a combination of spending cuts and tax increases on Jan. 1 if Congress can’t broker a deal to stop them. But what does that mean for doctors? Well, they'll face a 2% across-the-board cut, in addition to the impending 27% cut to their Medicare reimbursements. Some experts say a 2% cut is the best deal physicians are going to get.
In other news, the ACA could be heading back to court. A lower court was recently asked to take a second look at the law’s requirement that employers offer contraceptive coverage without cost sharing. The plaintiff, Liberty University, claims the provision violates First Amendment guarantees of religious freedom. If the court accepts that argument, the case could head to the Supreme Court next year. For more details on that, check out this week’s Policy & Practice podcast.
--Frances Correa (@FMCReporting)
The fiscal cliff looms. The country faces a combination of spending cuts and tax increases on Jan. 1 if Congress can’t broker a deal to stop them. But what does that mean for doctors? Well, they'll face a 2% across-the-board cut, in addition to the impending 27% cut to their Medicare reimbursements. Some experts say a 2% cut is the best deal physicians are going to get.
In other news, the ACA could be heading back to court. A lower court was recently asked to take a second look at the law’s requirement that employers offer contraceptive coverage without cost sharing. The plaintiff, Liberty University, claims the provision violates First Amendment guarantees of religious freedom. If the court accepts that argument, the case could head to the Supreme Court next year. For more details on that, check out this week’s Policy & Practice podcast.
--Frances Correa (@FMCReporting)
Teduglutide Trims Parenteral Support in Short Bowel Syndrome
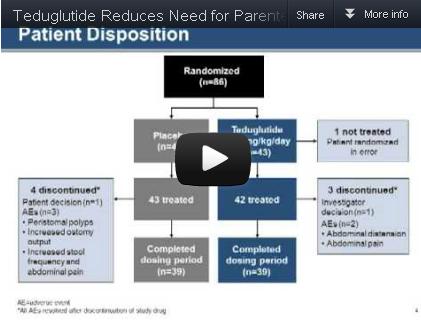
Teduglutide significantly reduced the need for parenteral support in patients with short bowel syndrome and intestinal failure, based on data from 85 adults in a randomized, controlled multicenter trial. The findings were published in the December issue of Gastroenterology.
Patients with short bowel syndrome and intestinal failure (SBS-IF) have inadequate intestinal absorption and require parenteral support (PS) to maintain fluids, electrolytes, trace elements, vitamins, and nutrient balances, said Dr. Palle Bekker Jeppesen of Rigshospitalet in Copenhagen and colleagues.
Source: American Gastroenterological Association
Data from previous open-label studies suggest an association between teduglutide and clinically meaningful reductions in wet weight and energy, which may reduce the need for PS in these patients, the investigators noted.
The researchers randomized 86 adults with SBS-IF to either 0.05 mg/kg per day of teduglutide or a placebo. One patient was randomized in error; complete data were available for 42 teduglutide patients and 43 placebo patients.
Significantly more patients in the teduglutide group responded to treatment, compared with the placebo group (63% vs. 30%). This response was defined as sustaining a 20%-100% reduction from baseline in weekly PS volume during weeks 20-24. "Small bowel length did not appear to be a predictor of response," the researchers noted.
The high placebo response may be explained by examining the fluid composite effect, a measure of the combined effects of teduglutide on PS volume reduction as well as the ability to reduce oral fluid intake and increase urine output volume, the researchers noted.
"In the current study, where protocol modifications encouraged earlier and more aggressive PS reductions, significantly larger PS reductions were also achieved in patients receiving placebo, but subsequently these patients had to increase their oral fluid intake significantly to maintain urine production and hydration constant," they said.
After 24 weeks, overall PS volume was reduced by 32% from baseline in teduglutide patients, compared with 21% in placebo patients. Although no patients in either group were completely weaned from parenteral support at 24 weeks, the difference in PS volume reduction was significantly greater in the teduglutide group.
The average weekly PS volume in teduglutide patients decreased significantly from 12.5 L/wk at baseline to 8.1 L/wk at week 24. The placebo patients also had a significant decrease in average weekly PS volume, from 13.4 L/wk at baseline to 11.1 L/wk at week 24.
Treatment-ending adverse events were similar between the two groups; 5% of teduglutide patients and 7% of placebo patients discontinued treatment because of such events during the study period. The most frequently reported treatment-emergent adverse events included abdominal pain, abdominal distension, nausea, and gastrointestinal stoma complications.
Although the study did not specifically assess quality of life measures, significantly more teduglutide patients had at least 1 day off PS, compared with placebo patients, which could help to "liberate considerable time for unhindered daytime activities or undisturbed sleep," the researchers said.
The study did not address the possible benefit of teduglutide therapy earlier in the course of SBS, or the duration of effect after patients discontinued teduglutide, the researchers added.
However, the findings indicate that teduglutide was safe and well tolerated, and "could positively add to the limited treatment armamentarium" for patients with SBS-IF.
Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
Patients with short bowel syndrome whose absorption is insufficient to maintain nutritional or fluid autonomy have intestinal failure. These patients, particularly those with proximal jejunostomies, who may actually secrete more fluid than they ingest, are among the most complex and challenging to manage of patients with any gastrointestinal disease. Patients with short bowel syndrome and intestinal failure are dependent on parenteral nutrition and/or fluid support (PS) to maintain life. This therapy has substantial implications for employment, activities, sleep, and finances. Numerous, often life-threatening, complications develop.

|
|
A myriad of growth factors may be involved in the process of postresection intestinal adaptation, including glucagonlike peptide-2 (GLP-2), wherein intestinal epithelial growth is promoted. Teduglutide is a long-acting analog of native GLP-2 and is somewhat more resistant to enzymatic degradation in the enterocyte than is the native enzyme. Dr. Jeppesen and colleagues reported a sustained 20%-100% decrease in PS volume requirements during weeks 20-24 of treatment in 63% of patients who received teduglutide, compared with 30% of placebo-treated patients. The mean drop in weekly PS volume from baseline to week 24 totaled 4.4 L in patients who received teduglutide, which equates to a decrease of 1-2 nights of infusion weekly, a very profound improvement for individual patients. The PS weaning protocol used was similar to that used in most centers experienced in the care of these patients.
As would be expected in the SBS-IF patient population, there were many adverse events, although these were equally distributed across teduglutide and placebo groups. Stomal changes, primarily related to enlargement, were evident in a significant minority of patients in the teduglutide group, as would be expected given the hyperplastic effect of the medication on intestinal epithelial tissue.Concern has been raised about GLP-2’s potential to stimulate the development of colonic adenomas in rodent models. Although the risk for malignancy is hypothetical in humans, colonoscopy should be considered at baseline for those patients with residual colons and perhaps as frequently as annually while the patients are on therapy until more long-term safety data are available.
Is teduglutide a "game changer"? The only patients who will be able to discontinue PS completely will be those who are on the borderline between nutritional autonomy and PS dependence. It is important to realize that teduglutide should be used to augment, not replace conventional management. What happens when teduglutide is stopped? Preliminary evidence suggests the effects on adaptation may be persistent, although earlier study noted that histologic changes trended toward baseline within 4 weeks of discontinuation. Perhaps longer treatment or maintenance will be required. The real future is an artificially grown and harvested intestine; even intestinal transplantation represents a bridge at best.
Dr. Alan L. Buchman is a former professor of medicine and surgery at the Feinberg School of Medicine at Northwestern University, Chicago. Within the past 12 months he has consulted for Takeda Pharmaceuticals and NPS Pharmaceuticals.
Patients with short bowel syndrome whose absorption is insufficient to maintain nutritional or fluid autonomy have intestinal failure. These patients, particularly those with proximal jejunostomies, who may actually secrete more fluid than they ingest, are among the most complex and challenging to manage of patients with any gastrointestinal disease. Patients with short bowel syndrome and intestinal failure are dependent on parenteral nutrition and/or fluid support (PS) to maintain life. This therapy has substantial implications for employment, activities, sleep, and finances. Numerous, often life-threatening, complications develop.

|
|
A myriad of growth factors may be involved in the process of postresection intestinal adaptation, including glucagonlike peptide-2 (GLP-2), wherein intestinal epithelial growth is promoted. Teduglutide is a long-acting analog of native GLP-2 and is somewhat more resistant to enzymatic degradation in the enterocyte than is the native enzyme. Dr. Jeppesen and colleagues reported a sustained 20%-100% decrease in PS volume requirements during weeks 20-24 of treatment in 63% of patients who received teduglutide, compared with 30% of placebo-treated patients. The mean drop in weekly PS volume from baseline to week 24 totaled 4.4 L in patients who received teduglutide, which equates to a decrease of 1-2 nights of infusion weekly, a very profound improvement for individual patients. The PS weaning protocol used was similar to that used in most centers experienced in the care of these patients.
As would be expected in the SBS-IF patient population, there were many adverse events, although these were equally distributed across teduglutide and placebo groups. Stomal changes, primarily related to enlargement, were evident in a significant minority of patients in the teduglutide group, as would be expected given the hyperplastic effect of the medication on intestinal epithelial tissue.Concern has been raised about GLP-2’s potential to stimulate the development of colonic adenomas in rodent models. Although the risk for malignancy is hypothetical in humans, colonoscopy should be considered at baseline for those patients with residual colons and perhaps as frequently as annually while the patients are on therapy until more long-term safety data are available.
Is teduglutide a "game changer"? The only patients who will be able to discontinue PS completely will be those who are on the borderline between nutritional autonomy and PS dependence. It is important to realize that teduglutide should be used to augment, not replace conventional management. What happens when teduglutide is stopped? Preliminary evidence suggests the effects on adaptation may be persistent, although earlier study noted that histologic changes trended toward baseline within 4 weeks of discontinuation. Perhaps longer treatment or maintenance will be required. The real future is an artificially grown and harvested intestine; even intestinal transplantation represents a bridge at best.
Dr. Alan L. Buchman is a former professor of medicine and surgery at the Feinberg School of Medicine at Northwestern University, Chicago. Within the past 12 months he has consulted for Takeda Pharmaceuticals and NPS Pharmaceuticals.
Patients with short bowel syndrome whose absorption is insufficient to maintain nutritional or fluid autonomy have intestinal failure. These patients, particularly those with proximal jejunostomies, who may actually secrete more fluid than they ingest, are among the most complex and challenging to manage of patients with any gastrointestinal disease. Patients with short bowel syndrome and intestinal failure are dependent on parenteral nutrition and/or fluid support (PS) to maintain life. This therapy has substantial implications for employment, activities, sleep, and finances. Numerous, often life-threatening, complications develop.

|
|
A myriad of growth factors may be involved in the process of postresection intestinal adaptation, including glucagonlike peptide-2 (GLP-2), wherein intestinal epithelial growth is promoted. Teduglutide is a long-acting analog of native GLP-2 and is somewhat more resistant to enzymatic degradation in the enterocyte than is the native enzyme. Dr. Jeppesen and colleagues reported a sustained 20%-100% decrease in PS volume requirements during weeks 20-24 of treatment in 63% of patients who received teduglutide, compared with 30% of placebo-treated patients. The mean drop in weekly PS volume from baseline to week 24 totaled 4.4 L in patients who received teduglutide, which equates to a decrease of 1-2 nights of infusion weekly, a very profound improvement for individual patients. The PS weaning protocol used was similar to that used in most centers experienced in the care of these patients.
As would be expected in the SBS-IF patient population, there were many adverse events, although these were equally distributed across teduglutide and placebo groups. Stomal changes, primarily related to enlargement, were evident in a significant minority of patients in the teduglutide group, as would be expected given the hyperplastic effect of the medication on intestinal epithelial tissue.Concern has been raised about GLP-2’s potential to stimulate the development of colonic adenomas in rodent models. Although the risk for malignancy is hypothetical in humans, colonoscopy should be considered at baseline for those patients with residual colons and perhaps as frequently as annually while the patients are on therapy until more long-term safety data are available.
Is teduglutide a "game changer"? The only patients who will be able to discontinue PS completely will be those who are on the borderline between nutritional autonomy and PS dependence. It is important to realize that teduglutide should be used to augment, not replace conventional management. What happens when teduglutide is stopped? Preliminary evidence suggests the effects on adaptation may be persistent, although earlier study noted that histologic changes trended toward baseline within 4 weeks of discontinuation. Perhaps longer treatment or maintenance will be required. The real future is an artificially grown and harvested intestine; even intestinal transplantation represents a bridge at best.
Dr. Alan L. Buchman is a former professor of medicine and surgery at the Feinberg School of Medicine at Northwestern University, Chicago. Within the past 12 months he has consulted for Takeda Pharmaceuticals and NPS Pharmaceuticals.
Teduglutide significantly reduced the need for parenteral support in patients with short bowel syndrome and intestinal failure, based on data from 85 adults in a randomized, controlled multicenter trial. The findings were published in the December issue of Gastroenterology.
Patients with short bowel syndrome and intestinal failure (SBS-IF) have inadequate intestinal absorption and require parenteral support (PS) to maintain fluids, electrolytes, trace elements, vitamins, and nutrient balances, said Dr. Palle Bekker Jeppesen of Rigshospitalet in Copenhagen and colleagues.
Source: American Gastroenterological Association
Data from previous open-label studies suggest an association between teduglutide and clinically meaningful reductions in wet weight and energy, which may reduce the need for PS in these patients, the investigators noted.
The researchers randomized 86 adults with SBS-IF to either 0.05 mg/kg per day of teduglutide or a placebo. One patient was randomized in error; complete data were available for 42 teduglutide patients and 43 placebo patients.
Significantly more patients in the teduglutide group responded to treatment, compared with the placebo group (63% vs. 30%). This response was defined as sustaining a 20%-100% reduction from baseline in weekly PS volume during weeks 20-24. "Small bowel length did not appear to be a predictor of response," the researchers noted.
The high placebo response may be explained by examining the fluid composite effect, a measure of the combined effects of teduglutide on PS volume reduction as well as the ability to reduce oral fluid intake and increase urine output volume, the researchers noted.
"In the current study, where protocol modifications encouraged earlier and more aggressive PS reductions, significantly larger PS reductions were also achieved in patients receiving placebo, but subsequently these patients had to increase their oral fluid intake significantly to maintain urine production and hydration constant," they said.
After 24 weeks, overall PS volume was reduced by 32% from baseline in teduglutide patients, compared with 21% in placebo patients. Although no patients in either group were completely weaned from parenteral support at 24 weeks, the difference in PS volume reduction was significantly greater in the teduglutide group.
The average weekly PS volume in teduglutide patients decreased significantly from 12.5 L/wk at baseline to 8.1 L/wk at week 24. The placebo patients also had a significant decrease in average weekly PS volume, from 13.4 L/wk at baseline to 11.1 L/wk at week 24.
Treatment-ending adverse events were similar between the two groups; 5% of teduglutide patients and 7% of placebo patients discontinued treatment because of such events during the study period. The most frequently reported treatment-emergent adverse events included abdominal pain, abdominal distension, nausea, and gastrointestinal stoma complications.
Although the study did not specifically assess quality of life measures, significantly more teduglutide patients had at least 1 day off PS, compared with placebo patients, which could help to "liberate considerable time for unhindered daytime activities or undisturbed sleep," the researchers said.
The study did not address the possible benefit of teduglutide therapy earlier in the course of SBS, or the duration of effect after patients discontinued teduglutide, the researchers added.
However, the findings indicate that teduglutide was safe and well tolerated, and "could positively add to the limited treatment armamentarium" for patients with SBS-IF.
Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
Teduglutide significantly reduced the need for parenteral support in patients with short bowel syndrome and intestinal failure, based on data from 85 adults in a randomized, controlled multicenter trial. The findings were published in the December issue of Gastroenterology.
Patients with short bowel syndrome and intestinal failure (SBS-IF) have inadequate intestinal absorption and require parenteral support (PS) to maintain fluids, electrolytes, trace elements, vitamins, and nutrient balances, said Dr. Palle Bekker Jeppesen of Rigshospitalet in Copenhagen and colleagues.
Source: American Gastroenterological Association
Data from previous open-label studies suggest an association between teduglutide and clinically meaningful reductions in wet weight and energy, which may reduce the need for PS in these patients, the investigators noted.
The researchers randomized 86 adults with SBS-IF to either 0.05 mg/kg per day of teduglutide or a placebo. One patient was randomized in error; complete data were available for 42 teduglutide patients and 43 placebo patients.
Significantly more patients in the teduglutide group responded to treatment, compared with the placebo group (63% vs. 30%). This response was defined as sustaining a 20%-100% reduction from baseline in weekly PS volume during weeks 20-24. "Small bowel length did not appear to be a predictor of response," the researchers noted.
The high placebo response may be explained by examining the fluid composite effect, a measure of the combined effects of teduglutide on PS volume reduction as well as the ability to reduce oral fluid intake and increase urine output volume, the researchers noted.
"In the current study, where protocol modifications encouraged earlier and more aggressive PS reductions, significantly larger PS reductions were also achieved in patients receiving placebo, but subsequently these patients had to increase their oral fluid intake significantly to maintain urine production and hydration constant," they said.
After 24 weeks, overall PS volume was reduced by 32% from baseline in teduglutide patients, compared with 21% in placebo patients. Although no patients in either group were completely weaned from parenteral support at 24 weeks, the difference in PS volume reduction was significantly greater in the teduglutide group.
The average weekly PS volume in teduglutide patients decreased significantly from 12.5 L/wk at baseline to 8.1 L/wk at week 24. The placebo patients also had a significant decrease in average weekly PS volume, from 13.4 L/wk at baseline to 11.1 L/wk at week 24.
Treatment-ending adverse events were similar between the two groups; 5% of teduglutide patients and 7% of placebo patients discontinued treatment because of such events during the study period. The most frequently reported treatment-emergent adverse events included abdominal pain, abdominal distension, nausea, and gastrointestinal stoma complications.
Although the study did not specifically assess quality of life measures, significantly more teduglutide patients had at least 1 day off PS, compared with placebo patients, which could help to "liberate considerable time for unhindered daytime activities or undisturbed sleep," the researchers said.
The study did not address the possible benefit of teduglutide therapy earlier in the course of SBS, or the duration of effect after patients discontinued teduglutide, the researchers added.
However, the findings indicate that teduglutide was safe and well tolerated, and "could positively add to the limited treatment armamentarium" for patients with SBS-IF.
Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
FROM GASTROENTEROLOGY
Major Finding: Significantly more patients who received 0.05 mg/kg per day of teduglutide had a sustained response to treatment during weeks 20-24, compared with the placebo group (63% vs. 30%).
Data Source: The data come from a randomized, controlled multicenter trial of 85 adults with short bowel syndrome and intestinal failure.
Disclosures: Dr. Jeppesen and several coauthors have served on the advisory board of and as consultants to NPS Pharmaceuticals, the company that funded the study. One author is an employee of NPS Pharmaceuticals.
Recurrent Acute Pancreatitis No Better After Dual Sphincterotomy
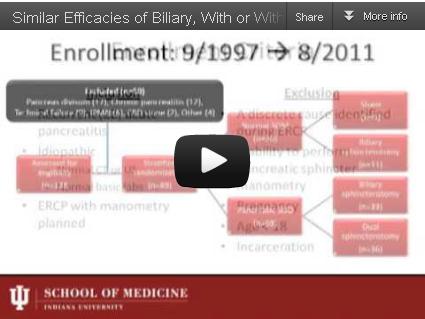
Performance of either biliary endoscopic sphincterotomy alone or dual biliary and pancreatic sphincterotomy similarly prevented approximately half of idiopathic recurrent acute pancreatitis cases in a trial in which 89 patients were randomized to treatments based on the presence or absence of sphincter of Oddi dysfunction.
The study is "the largest randomized clinical trial studying ERCP [endoscopic retrograde cholangiopancreatography] with SOM [sphincter of Oddi manometry] in this population" with long-term follow-up data, Dr. Gregory A. Coté of Indiana University in Indianapolis and his colleagues reported in the December issue of Gastroenterology (2012 [doi: 10.1053/j.gastro.2012.09.006]).
Source: American Gastroenterological Institute
Finding therapeutic equivalence between biliary endoscopic sphincterotomy (BES) and dual endoscopic sphincterotomy (DES) in preventing at least one episode of acute pancreatitis during follow-up is important, because the addition of pancreatic sphincterotomy to ERCP carries the risk of post-ERCP pancreatitis, bleeding, perforation, and sphincter restenosis, according to Dr. Coté and his associates.
To assess the therapeutic value of two types of sphincterotomy and the prognostic value of pancreatic SOD for patients with idiopathic recurrent acute pancreatitis (RAP), the researchers randomized 69 adults with SOD to BES or DES. The other 20 patients who did not have SOD were randomized to BES or a sham therapy. SOD was defined as basal pressure of 40 mm Hg or greater, "sustained for at least 30 seconds across two transducers," the researchers noted.
The patients were aged 18 years and older, and those with chronic pancreatitis or an identified cause of RAP were excluded from the study.
Of the 69 patients with SOD, RAP occurred in 49% of patients who underwent BES and 47% who underwent DES. There was no significant difference in rates of RAP between non-SOD patients who had BES and those who had a sham procedure (27% vs. 11%, respectively).
The risk of RAP was approximately four times higher in patients with SOD than in those without SOD, they added.
"Most RAP events occurred within 30 months of randomization in all subgroups," the researchers said.
Overall, chronic pancreatitis developed in 17% of all patients over a median of 78 months, and there was no difference in the probability of developing chronic pancreatitis in patients with and without SOD.
The study was limited by several factors, including its small sample size for the non-SOD population and the impact of environmental and genetic risk factors on idiopathic RAP, the researchers noted.
The small sample of patients with normal SOM meant that the researchers could draw no conclusions about the benefit of BES in these patients, but the results "represent preliminary data for estimating the sample size of a future definitive trial of ERCP with empiric biliary sphincterotomy," they noted.
In addition, the findings suggest that SOD "may be a secondary marker of more significant inflammation related to previous acute pancreatitis," and that pancreatic sphincterotomy "cannot be recommended as a curative treatment of unexplained RAP alone," they wrote.
None of the study authors had any financial conflicts to disclose.
Performance of either biliary endoscopic sphincterotomy alone or dual biliary and pancreatic sphincterotomy similarly prevented approximately half of idiopathic recurrent acute pancreatitis cases in a trial in which 89 patients were randomized to treatments based on the presence or absence of sphincter of Oddi dysfunction.
The study is "the largest randomized clinical trial studying ERCP [endoscopic retrograde cholangiopancreatography] with SOM [sphincter of Oddi manometry] in this population" with long-term follow-up data, Dr. Gregory A. Coté of Indiana University in Indianapolis and his colleagues reported in the December issue of Gastroenterology (2012 [doi: 10.1053/j.gastro.2012.09.006]).
Source: American Gastroenterological Institute
Finding therapeutic equivalence between biliary endoscopic sphincterotomy (BES) and dual endoscopic sphincterotomy (DES) in preventing at least one episode of acute pancreatitis during follow-up is important, because the addition of pancreatic sphincterotomy to ERCP carries the risk of post-ERCP pancreatitis, bleeding, perforation, and sphincter restenosis, according to Dr. Coté and his associates.
To assess the therapeutic value of two types of sphincterotomy and the prognostic value of pancreatic SOD for patients with idiopathic recurrent acute pancreatitis (RAP), the researchers randomized 69 adults with SOD to BES or DES. The other 20 patients who did not have SOD were randomized to BES or a sham therapy. SOD was defined as basal pressure of 40 mm Hg or greater, "sustained for at least 30 seconds across two transducers," the researchers noted.
The patients were aged 18 years and older, and those with chronic pancreatitis or an identified cause of RAP were excluded from the study.
Of the 69 patients with SOD, RAP occurred in 49% of patients who underwent BES and 47% who underwent DES. There was no significant difference in rates of RAP between non-SOD patients who had BES and those who had a sham procedure (27% vs. 11%, respectively).
The risk of RAP was approximately four times higher in patients with SOD than in those without SOD, they added.
"Most RAP events occurred within 30 months of randomization in all subgroups," the researchers said.
Overall, chronic pancreatitis developed in 17% of all patients over a median of 78 months, and there was no difference in the probability of developing chronic pancreatitis in patients with and without SOD.
The study was limited by several factors, including its small sample size for the non-SOD population and the impact of environmental and genetic risk factors on idiopathic RAP, the researchers noted.
The small sample of patients with normal SOM meant that the researchers could draw no conclusions about the benefit of BES in these patients, but the results "represent preliminary data for estimating the sample size of a future definitive trial of ERCP with empiric biliary sphincterotomy," they noted.
In addition, the findings suggest that SOD "may be a secondary marker of more significant inflammation related to previous acute pancreatitis," and that pancreatic sphincterotomy "cannot be recommended as a curative treatment of unexplained RAP alone," they wrote.
None of the study authors had any financial conflicts to disclose.
Performance of either biliary endoscopic sphincterotomy alone or dual biliary and pancreatic sphincterotomy similarly prevented approximately half of idiopathic recurrent acute pancreatitis cases in a trial in which 89 patients were randomized to treatments based on the presence or absence of sphincter of Oddi dysfunction.
The study is "the largest randomized clinical trial studying ERCP [endoscopic retrograde cholangiopancreatography] with SOM [sphincter of Oddi manometry] in this population" with long-term follow-up data, Dr. Gregory A. Coté of Indiana University in Indianapolis and his colleagues reported in the December issue of Gastroenterology (2012 [doi: 10.1053/j.gastro.2012.09.006]).
Source: American Gastroenterological Institute
Finding therapeutic equivalence between biliary endoscopic sphincterotomy (BES) and dual endoscopic sphincterotomy (DES) in preventing at least one episode of acute pancreatitis during follow-up is important, because the addition of pancreatic sphincterotomy to ERCP carries the risk of post-ERCP pancreatitis, bleeding, perforation, and sphincter restenosis, according to Dr. Coté and his associates.
To assess the therapeutic value of two types of sphincterotomy and the prognostic value of pancreatic SOD for patients with idiopathic recurrent acute pancreatitis (RAP), the researchers randomized 69 adults with SOD to BES or DES. The other 20 patients who did not have SOD were randomized to BES or a sham therapy. SOD was defined as basal pressure of 40 mm Hg or greater, "sustained for at least 30 seconds across two transducers," the researchers noted.
The patients were aged 18 years and older, and those with chronic pancreatitis or an identified cause of RAP were excluded from the study.
Of the 69 patients with SOD, RAP occurred in 49% of patients who underwent BES and 47% who underwent DES. There was no significant difference in rates of RAP between non-SOD patients who had BES and those who had a sham procedure (27% vs. 11%, respectively).
The risk of RAP was approximately four times higher in patients with SOD than in those without SOD, they added.
"Most RAP events occurred within 30 months of randomization in all subgroups," the researchers said.
Overall, chronic pancreatitis developed in 17% of all patients over a median of 78 months, and there was no difference in the probability of developing chronic pancreatitis in patients with and without SOD.
The study was limited by several factors, including its small sample size for the non-SOD population and the impact of environmental and genetic risk factors on idiopathic RAP, the researchers noted.
The small sample of patients with normal SOM meant that the researchers could draw no conclusions about the benefit of BES in these patients, but the results "represent preliminary data for estimating the sample size of a future definitive trial of ERCP with empiric biliary sphincterotomy," they noted.
In addition, the findings suggest that SOD "may be a secondary marker of more significant inflammation related to previous acute pancreatitis," and that pancreatic sphincterotomy "cannot be recommended as a curative treatment of unexplained RAP alone," they wrote.
None of the study authors had any financial conflicts to disclose.
FROM GASTROENTEROLOGY
Major Finding: Of 69 patients with sphincter of Oddi dysfunction, recurrent acute pancreatitis occurred in 49% of patients who underwent biliary endoscopic sphincterectomy and 47% who had dual biliary and pancreatic endoscopic sphincterectomy.
Data Source: The data come from a randomized trial of 89 adults with idiopathic recurrent acute pancreatitis.
Disclosures: None of the study authors had any financial conflicts to disclose.
Study: Uterus Preservation Feasible with Mesh POP Repair System
LAS VEGAS – The Elevate Anterior and Apical system – a transvaginal synthetic mesh repair system – was just as effective when pelvic organ prolapse repair was performed with or without uterine preservation in a prospective, multicenter trial.
Complication rates, including extrusion rates, were low, and there was long-term durability at 24 months, Dr. Edward J. Stanford said at the 41st AAGL Global Ccongress.
"In our opinion, the results support [the idea] that concomitant hysterectomy may not be, or is not, necessary in patients who, after informed consent, would like to preserve their uterus," he said.
The Elevate Anterior and Apical (EAA) transvaginal polypropylene mesh pelvic organ prolapse (POP) repair system is contraindicated in pregnant women and women planning future pregnancies, as the graft will not stretch significantly as the patient grows, according to the device manufacturer, American Medical Systems.
Concerns about the safety and efficacy of transvaginally placed synthetic mesh for POP prompted the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) in late 2011 to recommend that such repairs be reserved for "high-risk patients in whom the benefit of mesh placement may justify the risk, such as those with recurrent prolapse" (Obstet. Gynecol. 2011;118:1459-64).
Dr. Stanford and his fellow investigators at 10 U.S. and 6 European sites sought to prospectively explore the efficacy of the EAA system when utilized with or without uterine preservation in 142 women with anterior vaginal prolapse and/or apical descent of at least stage II.
The primary outcome was treatment failure, defined as at least stage II of the Pelvic Organ Prolapse Quantification system (leading edge of prolapse within 1 cm of the hymenal ring) during follow-up, using the last observation carried forward method.
Three subgroups were analyzed: 61 women with a baseline, prior hysterectomy; 29 with a concomitant hysterectomy; and 51 with no hysterectomy. The groups were well balanced, although 10% of the concomitant group was current smokers, compared with roughly 2% in the other groups. Median gravity was 3 and median parity 2. Their average age was 64 years.
For the apical compartment, success at 24 months was reported in 29 patients with a prior hysterectomy (93.5%), 17 with a concomitant hysterectomy (94.4%), and 24 with no hysterectomy (100%), reported Dr. Stanford, a health care consultant in Las Vegas. Notably, data were missing for 30 of the 61 prior hysterectomy patients, 11 of the 29 concomitant patients, and 27 of the 51 uterine preservation patients.
For the anterior compartment, success was slightly lower at 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17 patients), and 89% with uterine preservation (41 patients). Data were missing for 7, 5, and 5 patients, respectively.
There was no significant difference in success between the groups for the apical (P = .46) or anterior (P = .154) compartments, he said.
Dr. Stanford defended the use of the study’s methodology in an interview, and said that the last observation carried forward method was the best way to account for missing data.
"It penalized those groups with missing data, and our results were still good," he said.
Three patients in the prior and current hysterectomy groups experienced an intraoperative complication, as did seven patients with uterine preservation. Estimated blood loss was similar at a median of 50 mL in each group.
There was a nonsignificant trend toward higher mesh extrusion in women undergoing a concomitant hysterectomy (13.8%; 4 of 29), compared with those with a prior hysterectomy (5%; 3 of 61) or no hysterectomy (2%; 1 of 51), Dr. Stanford said.
"We are a little concerned that the higher extrusion rate with a concomitant hysterectomy, which has been seen in other studies, is coming true in this study as well," he added. "Perhaps, the higher number of smokers in that subgroup may be a factor."
Smoking and urogenital atrophy have been acknowledged as risk factors for mesh erosion. About 42% of patients were on vaginal or topical estrogen prior to surgery, and all received preoperative antibiotics, he said during a discussion of the study.
Almost all of the failures occurred early on, up to 3 months after surgery, with extrusion rates remaining stable from year 1 to year 2, Dr. Stanford said in an interview.
"A lot of experts are saying that late complications are happening on a regular basis, but we’re just not seeing it in our data or in other prolapse studies," he said.
Dr. Stanford contends that reported extrusion rates of 15% or more occurred primarily among surgeons still learning the technique. He credits the high success rate in the current study to the use of a standardized approach and the expertise of the surgeons, who were given specific training on the Elevate system and perform at least 100 vaginal mesh repairs annually.
"It’s a long learning curve, and you have to continue with an adequate volume and know how to do a proper dissection," he said. "You need about 25 to 50 cases to have a level of expertise, which is consistent with the surgical literature. We know that’s true of total laparoscopic hysterectomy as well."
In its joint communication, ACOG and AUGS recommended that surgeons placing vaginal mesh undergo training specific to each device, have experience with reconstructive surgical procedures, and have a thorough understanding of pelvic anatomy.
Based on the current limited data, the two groups said there is a "small, but significant group" of patients who experience permanent or life-altering sequelae as result of the transvaginal mesh placement.
In its updated July 2011 safety report, however, the Food and Drug Administration said that serious complications related to POP transvaginal mesh repair "are not rare," and that the procedure "may expose patients to greater risk" than traditional nonmesh repair.
The FDA’s Obstetrics and Gynecology Devices Panel subsequently called for postmarket studies to evaluate current products, and recommended that new vaginal mesh products for POP repair not be approved through the less rigorous Class II 501(k) process, but reclassified as Class III to ensure that premarket clinical studies are conducted.
Law firms are aggressively litigating cases against transvaginal mesh manufacturers, with commercials soliciting new clients airing on local television in Las Vegas throughout the AAGL meeting. American Medical Systems, which also manufactures the Apogee and Perigee mesh products, is one of several companies to be named in at least six ongoing multidistrict litigations.
Dr. Stanford said the current data are reassuring, and that there were no significant differences between women with or without uterine preservation in quality of life scores on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12), Pelvic Floor Incontinence Questionnaire-7 (PFIQ-7), and Pelvic Floor Distress Inventory (PFDI).
Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
LAS VEGAS – The Elevate Anterior and Apical system – a transvaginal synthetic mesh repair system – was just as effective when pelvic organ prolapse repair was performed with or without uterine preservation in a prospective, multicenter trial.
Complication rates, including extrusion rates, were low, and there was long-term durability at 24 months, Dr. Edward J. Stanford said at the 41st AAGL Global Ccongress.
"In our opinion, the results support [the idea] that concomitant hysterectomy may not be, or is not, necessary in patients who, after informed consent, would like to preserve their uterus," he said.
The Elevate Anterior and Apical (EAA) transvaginal polypropylene mesh pelvic organ prolapse (POP) repair system is contraindicated in pregnant women and women planning future pregnancies, as the graft will not stretch significantly as the patient grows, according to the device manufacturer, American Medical Systems.
Concerns about the safety and efficacy of transvaginally placed synthetic mesh for POP prompted the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) in late 2011 to recommend that such repairs be reserved for "high-risk patients in whom the benefit of mesh placement may justify the risk, such as those with recurrent prolapse" (Obstet. Gynecol. 2011;118:1459-64).
Dr. Stanford and his fellow investigators at 10 U.S. and 6 European sites sought to prospectively explore the efficacy of the EAA system when utilized with or without uterine preservation in 142 women with anterior vaginal prolapse and/or apical descent of at least stage II.
The primary outcome was treatment failure, defined as at least stage II of the Pelvic Organ Prolapse Quantification system (leading edge of prolapse within 1 cm of the hymenal ring) during follow-up, using the last observation carried forward method.
Three subgroups were analyzed: 61 women with a baseline, prior hysterectomy; 29 with a concomitant hysterectomy; and 51 with no hysterectomy. The groups were well balanced, although 10% of the concomitant group was current smokers, compared with roughly 2% in the other groups. Median gravity was 3 and median parity 2. Their average age was 64 years.
For the apical compartment, success at 24 months was reported in 29 patients with a prior hysterectomy (93.5%), 17 with a concomitant hysterectomy (94.4%), and 24 with no hysterectomy (100%), reported Dr. Stanford, a health care consultant in Las Vegas. Notably, data were missing for 30 of the 61 prior hysterectomy patients, 11 of the 29 concomitant patients, and 27 of the 51 uterine preservation patients.
For the anterior compartment, success was slightly lower at 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17 patients), and 89% with uterine preservation (41 patients). Data were missing for 7, 5, and 5 patients, respectively.
There was no significant difference in success between the groups for the apical (P = .46) or anterior (P = .154) compartments, he said.
Dr. Stanford defended the use of the study’s methodology in an interview, and said that the last observation carried forward method was the best way to account for missing data.
"It penalized those groups with missing data, and our results were still good," he said.
Three patients in the prior and current hysterectomy groups experienced an intraoperative complication, as did seven patients with uterine preservation. Estimated blood loss was similar at a median of 50 mL in each group.
There was a nonsignificant trend toward higher mesh extrusion in women undergoing a concomitant hysterectomy (13.8%; 4 of 29), compared with those with a prior hysterectomy (5%; 3 of 61) or no hysterectomy (2%; 1 of 51), Dr. Stanford said.
"We are a little concerned that the higher extrusion rate with a concomitant hysterectomy, which has been seen in other studies, is coming true in this study as well," he added. "Perhaps, the higher number of smokers in that subgroup may be a factor."
Smoking and urogenital atrophy have been acknowledged as risk factors for mesh erosion. About 42% of patients were on vaginal or topical estrogen prior to surgery, and all received preoperative antibiotics, he said during a discussion of the study.
Almost all of the failures occurred early on, up to 3 months after surgery, with extrusion rates remaining stable from year 1 to year 2, Dr. Stanford said in an interview.
"A lot of experts are saying that late complications are happening on a regular basis, but we’re just not seeing it in our data or in other prolapse studies," he said.
Dr. Stanford contends that reported extrusion rates of 15% or more occurred primarily among surgeons still learning the technique. He credits the high success rate in the current study to the use of a standardized approach and the expertise of the surgeons, who were given specific training on the Elevate system and perform at least 100 vaginal mesh repairs annually.
"It’s a long learning curve, and you have to continue with an adequate volume and know how to do a proper dissection," he said. "You need about 25 to 50 cases to have a level of expertise, which is consistent with the surgical literature. We know that’s true of total laparoscopic hysterectomy as well."
In its joint communication, ACOG and AUGS recommended that surgeons placing vaginal mesh undergo training specific to each device, have experience with reconstructive surgical procedures, and have a thorough understanding of pelvic anatomy.
Based on the current limited data, the two groups said there is a "small, but significant group" of patients who experience permanent or life-altering sequelae as result of the transvaginal mesh placement.
In its updated July 2011 safety report, however, the Food and Drug Administration said that serious complications related to POP transvaginal mesh repair "are not rare," and that the procedure "may expose patients to greater risk" than traditional nonmesh repair.
The FDA’s Obstetrics and Gynecology Devices Panel subsequently called for postmarket studies to evaluate current products, and recommended that new vaginal mesh products for POP repair not be approved through the less rigorous Class II 501(k) process, but reclassified as Class III to ensure that premarket clinical studies are conducted.
Law firms are aggressively litigating cases against transvaginal mesh manufacturers, with commercials soliciting new clients airing on local television in Las Vegas throughout the AAGL meeting. American Medical Systems, which also manufactures the Apogee and Perigee mesh products, is one of several companies to be named in at least six ongoing multidistrict litigations.
Dr. Stanford said the current data are reassuring, and that there were no significant differences between women with or without uterine preservation in quality of life scores on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12), Pelvic Floor Incontinence Questionnaire-7 (PFIQ-7), and Pelvic Floor Distress Inventory (PFDI).
Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
LAS VEGAS – The Elevate Anterior and Apical system – a transvaginal synthetic mesh repair system – was just as effective when pelvic organ prolapse repair was performed with or without uterine preservation in a prospective, multicenter trial.
Complication rates, including extrusion rates, were low, and there was long-term durability at 24 months, Dr. Edward J. Stanford said at the 41st AAGL Global Ccongress.
"In our opinion, the results support [the idea] that concomitant hysterectomy may not be, or is not, necessary in patients who, after informed consent, would like to preserve their uterus," he said.
The Elevate Anterior and Apical (EAA) transvaginal polypropylene mesh pelvic organ prolapse (POP) repair system is contraindicated in pregnant women and women planning future pregnancies, as the graft will not stretch significantly as the patient grows, according to the device manufacturer, American Medical Systems.
Concerns about the safety and efficacy of transvaginally placed synthetic mesh for POP prompted the American College of Obstetricians and Gynecologists (ACOG) and the American Urogynecologic Society (AUGS) in late 2011 to recommend that such repairs be reserved for "high-risk patients in whom the benefit of mesh placement may justify the risk, such as those with recurrent prolapse" (Obstet. Gynecol. 2011;118:1459-64).
Dr. Stanford and his fellow investigators at 10 U.S. and 6 European sites sought to prospectively explore the efficacy of the EAA system when utilized with or without uterine preservation in 142 women with anterior vaginal prolapse and/or apical descent of at least stage II.
The primary outcome was treatment failure, defined as at least stage II of the Pelvic Organ Prolapse Quantification system (leading edge of prolapse within 1 cm of the hymenal ring) during follow-up, using the last observation carried forward method.
Three subgroups were analyzed: 61 women with a baseline, prior hysterectomy; 29 with a concomitant hysterectomy; and 51 with no hysterectomy. The groups were well balanced, although 10% of the concomitant group was current smokers, compared with roughly 2% in the other groups. Median gravity was 3 and median parity 2. Their average age was 64 years.
For the apical compartment, success at 24 months was reported in 29 patients with a prior hysterectomy (93.5%), 17 with a concomitant hysterectomy (94.4%), and 24 with no hysterectomy (100%), reported Dr. Stanford, a health care consultant in Las Vegas. Notably, data were missing for 30 of the 61 prior hysterectomy patients, 11 of the 29 concomitant patients, and 27 of the 51 uterine preservation patients.
For the anterior compartment, success was slightly lower at 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17 patients), and 89% with uterine preservation (41 patients). Data were missing for 7, 5, and 5 patients, respectively.
There was no significant difference in success between the groups for the apical (P = .46) or anterior (P = .154) compartments, he said.
Dr. Stanford defended the use of the study’s methodology in an interview, and said that the last observation carried forward method was the best way to account for missing data.
"It penalized those groups with missing data, and our results were still good," he said.
Three patients in the prior and current hysterectomy groups experienced an intraoperative complication, as did seven patients with uterine preservation. Estimated blood loss was similar at a median of 50 mL in each group.
There was a nonsignificant trend toward higher mesh extrusion in women undergoing a concomitant hysterectomy (13.8%; 4 of 29), compared with those with a prior hysterectomy (5%; 3 of 61) or no hysterectomy (2%; 1 of 51), Dr. Stanford said.
"We are a little concerned that the higher extrusion rate with a concomitant hysterectomy, which has been seen in other studies, is coming true in this study as well," he added. "Perhaps, the higher number of smokers in that subgroup may be a factor."
Smoking and urogenital atrophy have been acknowledged as risk factors for mesh erosion. About 42% of patients were on vaginal or topical estrogen prior to surgery, and all received preoperative antibiotics, he said during a discussion of the study.
Almost all of the failures occurred early on, up to 3 months after surgery, with extrusion rates remaining stable from year 1 to year 2, Dr. Stanford said in an interview.
"A lot of experts are saying that late complications are happening on a regular basis, but we’re just not seeing it in our data or in other prolapse studies," he said.
Dr. Stanford contends that reported extrusion rates of 15% or more occurred primarily among surgeons still learning the technique. He credits the high success rate in the current study to the use of a standardized approach and the expertise of the surgeons, who were given specific training on the Elevate system and perform at least 100 vaginal mesh repairs annually.
"It’s a long learning curve, and you have to continue with an adequate volume and know how to do a proper dissection," he said. "You need about 25 to 50 cases to have a level of expertise, which is consistent with the surgical literature. We know that’s true of total laparoscopic hysterectomy as well."
In its joint communication, ACOG and AUGS recommended that surgeons placing vaginal mesh undergo training specific to each device, have experience with reconstructive surgical procedures, and have a thorough understanding of pelvic anatomy.
Based on the current limited data, the two groups said there is a "small, but significant group" of patients who experience permanent or life-altering sequelae as result of the transvaginal mesh placement.
In its updated July 2011 safety report, however, the Food and Drug Administration said that serious complications related to POP transvaginal mesh repair "are not rare," and that the procedure "may expose patients to greater risk" than traditional nonmesh repair.
The FDA’s Obstetrics and Gynecology Devices Panel subsequently called for postmarket studies to evaluate current products, and recommended that new vaginal mesh products for POP repair not be approved through the less rigorous Class II 501(k) process, but reclassified as Class III to ensure that premarket clinical studies are conducted.
Law firms are aggressively litigating cases against transvaginal mesh manufacturers, with commercials soliciting new clients airing on local television in Las Vegas throughout the AAGL meeting. American Medical Systems, which also manufactures the Apogee and Perigee mesh products, is one of several companies to be named in at least six ongoing multidistrict litigations.
Dr. Stanford said the current data are reassuring, and that there were no significant differences between women with or without uterine preservation in quality of life scores on the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-12 (PISQ-12), Pelvic Floor Incontinence Questionnaire-7 (PFIQ-7), and Pelvic Floor Distress Inventory (PFDI).
Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
AT THE 41st AAGL GLOBAL CONGRESS
Major Finding: For the apical compartment, success at 24 months was reported in 93.5% of patients with a prior hysterectomy (29 patients), 94.4% of those with a concomitant hysterectomy (17), and 100% with no hysterectomy (24). For the anterior compartment, success was 79.6% with a prior hysterectomy (43 patients), 70.8% with a concomitant hysterectomy (17), and 89% with uterine preservation (41).
Data Source: This was a prospective, international study of 142 women treated with the Elevate Anterior and Apical Prolapse Repair System.
Disclosures: Dr. Stanford disclosed a research grant from study sponsor American Medical Systems, maker of the Elevate system.
Older Docs Still Balking at Minimally Invasive Hysterectomy
LAS VEGAS – Gynecologists who completed their residency more than 20 years ago are half as likely as more recent graduates to perform a laparoscopic hysterectomy, a survey has shown.
Total abdominal hysterectomy was the most commonly performed route for 35% of respondents, with 24% preferring a vaginal approach, and only 8% reporting total laparoscopic hysterectomy as their preferred method.
"Rates of laparoscopic hysterectomy are increasing, but as seen in other studies, the abdominal approach is still the preferred method," Dr. Terri Febbraro said at the 41st AAGL Global Congress.
Both a 2009 American College of Obstetricians and Gynecologists (ACOG) committee opinion and a 2010 AAGL position statement favor vaginal hysterectomy as the preferred route. Laparoscopic hysterectomy can be used as an alternative in the minority of cases when the vaginal approach is not feasible or indicated.
Still, the disconnect continues.
Total abdominal surgeries account for roughly two-thirds of hysterectomies in the United States (Obstet. Gynecol. 2007;110;1091-5), although that number may be declining. Only 8% of gynecologists, however, would choose an abdominal hysterectomy for themselves or their spouse (J. Minim. Invasive Gynecol. 2010;17:167-75), said Dr. February, a fourth-year resident at Brown University in Providence, R.I.
To explore the perceived barriers and contraindications among gynecologists to providing minimally invasive surgery (MIS), Dr. Febbraro and her associates sent a cross-sectional survey via the Web and mail to 802 ACOG fellows from October 2008 to May 2009. A total of 417 surveys (52%) were returned.
The majority of respondents practiced general ob.gyn. (94%) and were in private practice (82%). Almost half, or 42%, graduated residency more than 20 years ago and 31% graduated in the last 10 years. There was an equal gender split, and all geographic districts were represented.
Three-fourths of respondents (78%) reported performing an average of one to five hysterectomies per month, and 8% performed six or more, which was defined as high volume for the analysis.
In addition to the three approaches described above, 19% of respondents preferred laparoscopic-assisted vaginal, 11% supracervical laparoscopic, and 3% supracervical abdominal (3%) hysterectomy.
Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P = .03).
The odds of performing MIS, either vaginally or laparoscopically, increased with surgical volume (OR, 8.37) and specialized training (OR, 9.37). This was even more pronounced among physicians who reported performing laparoscopic hysterectomies most often (OR, 12.0, and OR, 16.4), Dr. Febbraro said.
Providers graduating from residency more than 20 years ago were half as likely to prefer a laparoscopic approach as were those graduating less than 10 years ago (OR, 0.44).
Providers who preferred an open abdominal approach were significantly more likely than those using MIS to cite minimal descent, narrow introitus, and a uterus more than 12 weeks in size as perceived contraindications to a vaginal hysterectomy, she said.
Prior exploratory laparotomy, endometriosis, and a uterus larger than 12 or 16 weeks were significantly more likely to be cited as contraindications to laparoscopic hysterectomy by providers preferring an open approach.
Those providers who preferred an abdominal approach also reported significantly more contraindications than did MIS providers to vaginal hysterectomy (mean 4.4 vs. 3.4; P = .0003) and laparoscopic hysterectomy (mean, 1.5 vs. 0.8; P less than .0001). The lower number of contraindications to laparoscopic hysterectomy is noteworthy, given that this approach was preferred by fewer respondents than either open or vaginal surgery, Dr. Febbraro noted.
"As surgical volume and specialized training increase, it is likely that perceived barriers and contraindications will decrease, prompting providers to offer minimally invasive surgeries more readily," she said. "Training programs addressing these factors could have an impact on providers’ choice of surgical approach."
During a discussion of the study, Dr. Febbraro said that she and her colleagues did not distinguish between rural and urban providers, but that no regional differences were observed.
Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
LAS VEGAS – Gynecologists who completed their residency more than 20 years ago are half as likely as more recent graduates to perform a laparoscopic hysterectomy, a survey has shown.
Total abdominal hysterectomy was the most commonly performed route for 35% of respondents, with 24% preferring a vaginal approach, and only 8% reporting total laparoscopic hysterectomy as their preferred method.
"Rates of laparoscopic hysterectomy are increasing, but as seen in other studies, the abdominal approach is still the preferred method," Dr. Terri Febbraro said at the 41st AAGL Global Congress.
Both a 2009 American College of Obstetricians and Gynecologists (ACOG) committee opinion and a 2010 AAGL position statement favor vaginal hysterectomy as the preferred route. Laparoscopic hysterectomy can be used as an alternative in the minority of cases when the vaginal approach is not feasible or indicated.
Still, the disconnect continues.
Total abdominal surgeries account for roughly two-thirds of hysterectomies in the United States (Obstet. Gynecol. 2007;110;1091-5), although that number may be declining. Only 8% of gynecologists, however, would choose an abdominal hysterectomy for themselves or their spouse (J. Minim. Invasive Gynecol. 2010;17:167-75), said Dr. February, a fourth-year resident at Brown University in Providence, R.I.
To explore the perceived barriers and contraindications among gynecologists to providing minimally invasive surgery (MIS), Dr. Febbraro and her associates sent a cross-sectional survey via the Web and mail to 802 ACOG fellows from October 2008 to May 2009. A total of 417 surveys (52%) were returned.
The majority of respondents practiced general ob.gyn. (94%) and were in private practice (82%). Almost half, or 42%, graduated residency more than 20 years ago and 31% graduated in the last 10 years. There was an equal gender split, and all geographic districts were represented.
Three-fourths of respondents (78%) reported performing an average of one to five hysterectomies per month, and 8% performed six or more, which was defined as high volume for the analysis.
In addition to the three approaches described above, 19% of respondents preferred laparoscopic-assisted vaginal, 11% supracervical laparoscopic, and 3% supracervical abdominal (3%) hysterectomy.
Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P = .03).
The odds of performing MIS, either vaginally or laparoscopically, increased with surgical volume (OR, 8.37) and specialized training (OR, 9.37). This was even more pronounced among physicians who reported performing laparoscopic hysterectomies most often (OR, 12.0, and OR, 16.4), Dr. Febbraro said.
Providers graduating from residency more than 20 years ago were half as likely to prefer a laparoscopic approach as were those graduating less than 10 years ago (OR, 0.44).
Providers who preferred an open abdominal approach were significantly more likely than those using MIS to cite minimal descent, narrow introitus, and a uterus more than 12 weeks in size as perceived contraindications to a vaginal hysterectomy, she said.
Prior exploratory laparotomy, endometriosis, and a uterus larger than 12 or 16 weeks were significantly more likely to be cited as contraindications to laparoscopic hysterectomy by providers preferring an open approach.
Those providers who preferred an abdominal approach also reported significantly more contraindications than did MIS providers to vaginal hysterectomy (mean 4.4 vs. 3.4; P = .0003) and laparoscopic hysterectomy (mean, 1.5 vs. 0.8; P less than .0001). The lower number of contraindications to laparoscopic hysterectomy is noteworthy, given that this approach was preferred by fewer respondents than either open or vaginal surgery, Dr. Febbraro noted.
"As surgical volume and specialized training increase, it is likely that perceived barriers and contraindications will decrease, prompting providers to offer minimally invasive surgeries more readily," she said. "Training programs addressing these factors could have an impact on providers’ choice of surgical approach."
During a discussion of the study, Dr. Febbraro said that she and her colleagues did not distinguish between rural and urban providers, but that no regional differences were observed.
Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
LAS VEGAS – Gynecologists who completed their residency more than 20 years ago are half as likely as more recent graduates to perform a laparoscopic hysterectomy, a survey has shown.
Total abdominal hysterectomy was the most commonly performed route for 35% of respondents, with 24% preferring a vaginal approach, and only 8% reporting total laparoscopic hysterectomy as their preferred method.
"Rates of laparoscopic hysterectomy are increasing, but as seen in other studies, the abdominal approach is still the preferred method," Dr. Terri Febbraro said at the 41st AAGL Global Congress.
Both a 2009 American College of Obstetricians and Gynecologists (ACOG) committee opinion and a 2010 AAGL position statement favor vaginal hysterectomy as the preferred route. Laparoscopic hysterectomy can be used as an alternative in the minority of cases when the vaginal approach is not feasible or indicated.
Still, the disconnect continues.
Total abdominal surgeries account for roughly two-thirds of hysterectomies in the United States (Obstet. Gynecol. 2007;110;1091-5), although that number may be declining. Only 8% of gynecologists, however, would choose an abdominal hysterectomy for themselves or their spouse (J. Minim. Invasive Gynecol. 2010;17:167-75), said Dr. February, a fourth-year resident at Brown University in Providence, R.I.
To explore the perceived barriers and contraindications among gynecologists to providing minimally invasive surgery (MIS), Dr. Febbraro and her associates sent a cross-sectional survey via the Web and mail to 802 ACOG fellows from October 2008 to May 2009. A total of 417 surveys (52%) were returned.
The majority of respondents practiced general ob.gyn. (94%) and were in private practice (82%). Almost half, or 42%, graduated residency more than 20 years ago and 31% graduated in the last 10 years. There was an equal gender split, and all geographic districts were represented.
Three-fourths of respondents (78%) reported performing an average of one to five hysterectomies per month, and 8% performed six or more, which was defined as high volume for the analysis.
In addition to the three approaches described above, 19% of respondents preferred laparoscopic-assisted vaginal, 11% supracervical laparoscopic, and 3% supracervical abdominal (3%) hysterectomy.
Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P = .03).
The odds of performing MIS, either vaginally or laparoscopically, increased with surgical volume (OR, 8.37) and specialized training (OR, 9.37). This was even more pronounced among physicians who reported performing laparoscopic hysterectomies most often (OR, 12.0, and OR, 16.4), Dr. Febbraro said.
Providers graduating from residency more than 20 years ago were half as likely to prefer a laparoscopic approach as were those graduating less than 10 years ago (OR, 0.44).
Providers who preferred an open abdominal approach were significantly more likely than those using MIS to cite minimal descent, narrow introitus, and a uterus more than 12 weeks in size as perceived contraindications to a vaginal hysterectomy, she said.
Prior exploratory laparotomy, endometriosis, and a uterus larger than 12 or 16 weeks were significantly more likely to be cited as contraindications to laparoscopic hysterectomy by providers preferring an open approach.
Those providers who preferred an abdominal approach also reported significantly more contraindications than did MIS providers to vaginal hysterectomy (mean 4.4 vs. 3.4; P = .0003) and laparoscopic hysterectomy (mean, 1.5 vs. 0.8; P less than .0001). The lower number of contraindications to laparoscopic hysterectomy is noteworthy, given that this approach was preferred by fewer respondents than either open or vaginal surgery, Dr. Febbraro noted.
"As surgical volume and specialized training increase, it is likely that perceived barriers and contraindications will decrease, prompting providers to offer minimally invasive surgeries more readily," she said. "Training programs addressing these factors could have an impact on providers’ choice of surgical approach."
During a discussion of the study, Dr. Febbraro said that she and her colleagues did not distinguish between rural and urban providers, but that no regional differences were observed.
Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: Physicians who reported performing laparoscopic hysterectomies most often were significantly more likely to have graduated from residency in the previous 10 years than were physicians who performed vaginal hysterectomies most often (52% vs. 26.2%; P value = .03).
Data Source: Data are from a mixed-mode, cross-sectional survey sent to 802 ACOG fellows; 52% responded.
Disclosures: Dr. Febbraro reported no relevant financial disclosures. One of her coauthors is an ACOG employee.
Suture Method Linked to Vaginal Cuff Complications
LAS VEGAS – The risk of vaginal cuff complications was not influenced by the type of hysterectomy performed, although suture technique was a factor, in a retrospective analysis of 604 patients.
"In our study, the intracorporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications of evisceration and dehiscence in total laparoscopic hysterectomy," Dr. Yoon Byoung Kim said at the 41st AAGL Global Congress.
Although vaginal cuff dehiscence is a rare complication of hysterectomy, concerns have been raised that total laparoscopic hysterectomies may be associated with an increased risk of this potentially morbid complication.
Researchers at Beth Israel Deaconess Medical Center recently reported an updated incidence of vaginal cuff dehiscence of 1.35% after total laparoscopic hysterectomy, the highest rate among all hysterectomy modes evaluated (Obstet. Gynecol. 2011;118:794-801). This was dramatically lower, however, than the 4.93% incidence the group reported in a previous study (J. Minim. Invasive Gynecol. 2007;14:311-7).
Dr. Kim and her associates looked at the risk factors for vaginal cuff complications for six types of hysterectomies performed in 604 women between June 2007 and June 2011 at Korea University Anam Hospital, Seoul, Korea. The approach was robotic hysterectomy in 7, robotic radical hysterectomy and node dissection (RRHND) in 9, total laparoscopic hysterectomy (TLH) in 276, laparoscopically assisted vaginal hysterectomy (LAVH) in 238, laparoscopic radical hysterectomy and node dissection (LRHND) in 11, and abdominal radical hysterectomy in 63.
The suture technique was intracorporeal continuous for robotic hysterectomy, RRHND, and LRHND; intracorporeal or vaginal continuous locking for total laparoscopic hysterectomy; vaginal continuous locking for LAVH; and a 5-point suture with figure-8 vaginal suture for abdominal radical hysterectomy. Two TLH patients closed with a 3-point intracorporeal suture and figure-8 vaginal suture were excluded from the TLH analysis.
Among the remaining 274 TLH women, there were 1 case of evisceration and 4 cases of dehiscence with the intracorporeal continuous suture, compared with 0 cases of evisceration and 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P = .02).
In addition, the duration between surgery and the vaginal cuff complication was significantly longer with the intracorporeal suture than the vaginal suture (72.8 days vs. 23.6 days; P = .01), Dr. Kim said.
"The possible reasons for this result can be infection or delicate layering of the submucosal layer," she said.
Among all 604 women, there were 3 eviscerations (0.49%) and 21 cases of dehiscence (3.43%).
The incidence of evisceration was 0% for robotic hysterectomy, 11.1% for RRHND, 0.36% for total laparoscopic hysterectomy, 0% for LAVH, 0% for LRHND, and 1.5% for abdominal radical hysterectomy. The incidence of vaginal dehiscence was 0% for radical hysterectomy, 0% for RRHND, 5.43% for total laparoscopic hysterectomy, 1.68% for LAVH, 0% for LRHND, and 3.17% for abdominal radical hysterectomy.
Although total laparoscopic hysterectomy was associated with a higher incidence of cuff complications, the finding was not statistically significant, Dr. Kim said. Overall, there was no significant correlation between the incidence of cuff complications and the type of operation or suture technique.
The investigators then performed a subgroup analysis that included age, body mass index, operation time, estimated blood loss, postoperative fever, and antibiotic use. None of these risk factors correlated with dehiscence or evisceration (P = 0.99, 0.32, 0.46, 0.32, .06, and 0.42, respectively), Dr. Kim reported.
The limitations of the study were its small sample size, significant heterogeneity, and variation in sample size between groups, she said.
Dr. Kim reported no relevant financial disclosures.
LAS VEGAS – The risk of vaginal cuff complications was not influenced by the type of hysterectomy performed, although suture technique was a factor, in a retrospective analysis of 604 patients.
"In our study, the intracorporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications of evisceration and dehiscence in total laparoscopic hysterectomy," Dr. Yoon Byoung Kim said at the 41st AAGL Global Congress.
Although vaginal cuff dehiscence is a rare complication of hysterectomy, concerns have been raised that total laparoscopic hysterectomies may be associated with an increased risk of this potentially morbid complication.
Researchers at Beth Israel Deaconess Medical Center recently reported an updated incidence of vaginal cuff dehiscence of 1.35% after total laparoscopic hysterectomy, the highest rate among all hysterectomy modes evaluated (Obstet. Gynecol. 2011;118:794-801). This was dramatically lower, however, than the 4.93% incidence the group reported in a previous study (J. Minim. Invasive Gynecol. 2007;14:311-7).
Dr. Kim and her associates looked at the risk factors for vaginal cuff complications for six types of hysterectomies performed in 604 women between June 2007 and June 2011 at Korea University Anam Hospital, Seoul, Korea. The approach was robotic hysterectomy in 7, robotic radical hysterectomy and node dissection (RRHND) in 9, total laparoscopic hysterectomy (TLH) in 276, laparoscopically assisted vaginal hysterectomy (LAVH) in 238, laparoscopic radical hysterectomy and node dissection (LRHND) in 11, and abdominal radical hysterectomy in 63.
The suture technique was intracorporeal continuous for robotic hysterectomy, RRHND, and LRHND; intracorporeal or vaginal continuous locking for total laparoscopic hysterectomy; vaginal continuous locking for LAVH; and a 5-point suture with figure-8 vaginal suture for abdominal radical hysterectomy. Two TLH patients closed with a 3-point intracorporeal suture and figure-8 vaginal suture were excluded from the TLH analysis.
Among the remaining 274 TLH women, there were 1 case of evisceration and 4 cases of dehiscence with the intracorporeal continuous suture, compared with 0 cases of evisceration and 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P = .02).
In addition, the duration between surgery and the vaginal cuff complication was significantly longer with the intracorporeal suture than the vaginal suture (72.8 days vs. 23.6 days; P = .01), Dr. Kim said.
"The possible reasons for this result can be infection or delicate layering of the submucosal layer," she said.
Among all 604 women, there were 3 eviscerations (0.49%) and 21 cases of dehiscence (3.43%).
The incidence of evisceration was 0% for robotic hysterectomy, 11.1% for RRHND, 0.36% for total laparoscopic hysterectomy, 0% for LAVH, 0% for LRHND, and 1.5% for abdominal radical hysterectomy. The incidence of vaginal dehiscence was 0% for radical hysterectomy, 0% for RRHND, 5.43% for total laparoscopic hysterectomy, 1.68% for LAVH, 0% for LRHND, and 3.17% for abdominal radical hysterectomy.
Although total laparoscopic hysterectomy was associated with a higher incidence of cuff complications, the finding was not statistically significant, Dr. Kim said. Overall, there was no significant correlation between the incidence of cuff complications and the type of operation or suture technique.
The investigators then performed a subgroup analysis that included age, body mass index, operation time, estimated blood loss, postoperative fever, and antibiotic use. None of these risk factors correlated with dehiscence or evisceration (P = 0.99, 0.32, 0.46, 0.32, .06, and 0.42, respectively), Dr. Kim reported.
The limitations of the study were its small sample size, significant heterogeneity, and variation in sample size between groups, she said.
Dr. Kim reported no relevant financial disclosures.
LAS VEGAS – The risk of vaginal cuff complications was not influenced by the type of hysterectomy performed, although suture technique was a factor, in a retrospective analysis of 604 patients.
"In our study, the intracorporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications of evisceration and dehiscence in total laparoscopic hysterectomy," Dr. Yoon Byoung Kim said at the 41st AAGL Global Congress.
Although vaginal cuff dehiscence is a rare complication of hysterectomy, concerns have been raised that total laparoscopic hysterectomies may be associated with an increased risk of this potentially morbid complication.
Researchers at Beth Israel Deaconess Medical Center recently reported an updated incidence of vaginal cuff dehiscence of 1.35% after total laparoscopic hysterectomy, the highest rate among all hysterectomy modes evaluated (Obstet. Gynecol. 2011;118:794-801). This was dramatically lower, however, than the 4.93% incidence the group reported in a previous study (J. Minim. Invasive Gynecol. 2007;14:311-7).
Dr. Kim and her associates looked at the risk factors for vaginal cuff complications for six types of hysterectomies performed in 604 women between June 2007 and June 2011 at Korea University Anam Hospital, Seoul, Korea. The approach was robotic hysterectomy in 7, robotic radical hysterectomy and node dissection (RRHND) in 9, total laparoscopic hysterectomy (TLH) in 276, laparoscopically assisted vaginal hysterectomy (LAVH) in 238, laparoscopic radical hysterectomy and node dissection (LRHND) in 11, and abdominal radical hysterectomy in 63.
The suture technique was intracorporeal continuous for robotic hysterectomy, RRHND, and LRHND; intracorporeal or vaginal continuous locking for total laparoscopic hysterectomy; vaginal continuous locking for LAVH; and a 5-point suture with figure-8 vaginal suture for abdominal radical hysterectomy. Two TLH patients closed with a 3-point intracorporeal suture and figure-8 vaginal suture were excluded from the TLH analysis.
Among the remaining 274 TLH women, there were 1 case of evisceration and 4 cases of dehiscence with the intracorporeal continuous suture, compared with 0 cases of evisceration and 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P = .02).
In addition, the duration between surgery and the vaginal cuff complication was significantly longer with the intracorporeal suture than the vaginal suture (72.8 days vs. 23.6 days; P = .01), Dr. Kim said.
"The possible reasons for this result can be infection or delicate layering of the submucosal layer," she said.
Among all 604 women, there were 3 eviscerations (0.49%) and 21 cases of dehiscence (3.43%).
The incidence of evisceration was 0% for robotic hysterectomy, 11.1% for RRHND, 0.36% for total laparoscopic hysterectomy, 0% for LAVH, 0% for LRHND, and 1.5% for abdominal radical hysterectomy. The incidence of vaginal dehiscence was 0% for radical hysterectomy, 0% for RRHND, 5.43% for total laparoscopic hysterectomy, 1.68% for LAVH, 0% for LRHND, and 3.17% for abdominal radical hysterectomy.
Although total laparoscopic hysterectomy was associated with a higher incidence of cuff complications, the finding was not statistically significant, Dr. Kim said. Overall, there was no significant correlation between the incidence of cuff complications and the type of operation or suture technique.
The investigators then performed a subgroup analysis that included age, body mass index, operation time, estimated blood loss, postoperative fever, and antibiotic use. None of these risk factors correlated with dehiscence or evisceration (P = 0.99, 0.32, 0.46, 0.32, .06, and 0.42, respectively), Dr. Kim reported.
The limitations of the study were its small sample size, significant heterogeneity, and variation in sample size between groups, she said.
Dr. Kim reported no relevant financial disclosures.
AT THE 41ST AAGL GLOBAL CONGRESS
Major Finding: One case of evisceration and 4 cases of dehiscence occurred with the intracorporeal continuous suture vs. 11 cases of dehiscence with the vaginal continuous locking suture (2.63% vs. 10.47%; P value = .02)
Data Source: Data are from a retrospective, single-center analysis involving 604 women undergoing six types of hysterectomies.
Disclosures: Dr. Kim reported no relevant financial disclosures.
Patients' Worry, Not Risk, Drives Double Mastectomies
Among breast cancer patients, women who worry the most that localized cancer in one breast will spread to the other breast are twice as likely to choose a prophylactic double mastectomy – even though most of them have no clinical indication for the procedure, a study of 1,446 patients showed.
Approximately 80% of the 107 women in the study who chose prophylactic double mastectomy had a very low risk for contralateral disease, Sarah T. Hawley, Ph.D., said in a press conference sponsored by the American Society of Clinical Oncology (ASCO).
She is slated to present the results at a symposium on quality care sponsored by the American Society of Clinical Oncology, taking place Nov. 30 to Dec. 1 in San Diego.
Many women undergo unnecessary surgery out of ungrounded fear that cancer in one breast will lead to cancer in the other, said Dr. Hawley of the division of general medicine at the University of Michigan, Ann Arbor.
Women’s worry about cancer spreading from one breast to the other "really shouldn’t be a reason to get that procedure," she said.
Contralateral prophylactic mastectomy can be considered if a patient is positive for BRCA1 or BRCA2 mutations or has a family history of breast or ovarian cancer in two or more first-degree relatives, according to Society of Surgical Oncology guidelines.
"Despite the small number of women who meet these criteria, rates of contralateral prophylactic mastectomy have been increasing in recent years," Dr. Hawley noted.
Those traditional indications still were powerful drivers in the study – a positive genetic test increased the odds of contralateral prophylactic mastectomy 10-fold, and a family history increased the odds 5-fold.
The doubling in odds of contralateral prophylactic mastectomy in women with a high level of worry (compared with low worry level) is notable because the prophylactic surgery has not been known to reduce the risk of recurrence when those indications are not present, as was the case with the majority of women who chose the procedure in the study.
Among women who chose contralateral prophylactic mastectomy, 90% reported high levels of worry, compared with 80% of the 564 women who underwent single-breast mastectomy, a statistically significant difference, Dr. Hawley reported.
She and her associates studied 1,446 newly diagnosed breast cancer patients who completed two surveys 4 years apart, had not had a recurrence during that time, and had complete data on genetic testing and family history. Contralateral prophylactic mastectomy was considered by 35% of the whole cohort and chosen by 7%. Among women who underwent mastectomy of the cancerous breast, 53% considered contralateral prophylactic mastectomy and 19% underwent the procedure.
When women were considering any mastectomy vs. breast conservation surgery, family history and genetic test results did not significantly affect the odds that they would choose any mastectomy, but their level of worry did. High levels of worry significantly increased the odds of mastectomy by 69% in a subanalysis that controlled for the effects of age, race or ethnicity, education, and cancer stage.
A separate subanalysis found that both clinical indications and worry affected the likelihood of contralateral prophylactic mastectomy compared with unilateral mastectomy. The odds of having the prophylactic surgery increased more than 4-fold with a family history of at least two primary relatives with breast cancer, more than 10-fold with a positive genetic test, and more than 2-fold with a high degree of worry in the multivariate analysis, Dr. Hawley said.
Compared with previous studies on why women are getting contralateral prophylactic mastectomy, the current study is larger; is population-based; contains racial and ethnic samples; and includes data on patient attitudes, genetic testing, and type of family history (not just any family history), she said.
Dr. Jyoti D. Patel, moderator of the press conference, said the findings suggest that "we, as physicians, may not be adequately educating our patients about the risk for recurrent disease."
In general, women with localized breast cancer in one breast have less than a 1% chance of developing a new cancer in the unaffected breast and an 8% chance of recurrence in the affected breast or a nearby lymph node. The risk for developing a new cancer in the contralateral breast rises to approximately 10%-15% if the patient has a history of breast or ovarian cancer in two or more primary relatives, with a similar or slightly greater increased risk from a positive genetic mutation, Dr. Patel estimated. Having both clinical risk factors confers a 10- to 20-fold increase in risk.
Unfortunately, many women overestimate their risk of developing breast cancer in the contralateral breast and undergo unnecessary surgery, she commented. This study suggests that physicians re-examine how they communicate with their patients regarding the decision to undergo prophylactic mastectomy.
"Many women fear recurrence, and they also fear surveillance. They worry about, if they’re 35 years old, what a lifetime of screening for the contralateral breast might look like if they end up getting multiple biopsies. So how we put that in perspective for our young population will become vitally important," said Dr. Patell, a thoracic oncologist at Northwestern University in Chicago and a member of ASCO’s Cancer Communications Committee.
Dr. Hawley reported having no financial disclosures.
The findings suggest that "we, as physicians, may not be adequately educating our patients about the risk for recurrent disease," said Dr. Jyoti D. Patel, who moderated the press conference.
In general, women with localized breast cancer in one breast have less than a 1% chance of developing a new cancer in the unaffected breast and an 8% chance of recurrence in the affected breast or a nearby lymph node. The risk for developing a new cancer in the contralateral breast rises to approximately 10%-15% if the patient has a history of breast or ovarian cancer in two or more primary relatives, with a similar or slightly greater increased risk from a positive genetic mutation, Dr. Patel estimated. Having both clinical risk factors confers a 10- to 20-fold increase in risk.

|
| Dr. Jyoti Patel |
"Many women fear recurrence, and they also fear surveillance. They worry about, if they’re 35 years old, what a lifetime of screening for the contralateral breast might look like if they end up getting multiple biopsies. So how we put that in perspective for our young population will become vitally important," Dr. Patel said.
Dr. Patel, a thoracic oncologist at Northwestern University in Chicago, is a member of ASCO’s Cancer Communications Committee.
The findings suggest that "we, as physicians, may not be adequately educating our patients about the risk for recurrent disease," said Dr. Jyoti D. Patel, who moderated the press conference.
In general, women with localized breast cancer in one breast have less than a 1% chance of developing a new cancer in the unaffected breast and an 8% chance of recurrence in the affected breast or a nearby lymph node. The risk for developing a new cancer in the contralateral breast rises to approximately 10%-15% if the patient has a history of breast or ovarian cancer in two or more primary relatives, with a similar or slightly greater increased risk from a positive genetic mutation, Dr. Patel estimated. Having both clinical risk factors confers a 10- to 20-fold increase in risk.

|
| Dr. Jyoti Patel |
"Many women fear recurrence, and they also fear surveillance. They worry about, if they’re 35 years old, what a lifetime of screening for the contralateral breast might look like if they end up getting multiple biopsies. So how we put that in perspective for our young population will become vitally important," Dr. Patel said.
Dr. Patel, a thoracic oncologist at Northwestern University in Chicago, is a member of ASCO’s Cancer Communications Committee.
The findings suggest that "we, as physicians, may not be adequately educating our patients about the risk for recurrent disease," said Dr. Jyoti D. Patel, who moderated the press conference.
In general, women with localized breast cancer in one breast have less than a 1% chance of developing a new cancer in the unaffected breast and an 8% chance of recurrence in the affected breast or a nearby lymph node. The risk for developing a new cancer in the contralateral breast rises to approximately 10%-15% if the patient has a history of breast or ovarian cancer in two or more primary relatives, with a similar or slightly greater increased risk from a positive genetic mutation, Dr. Patel estimated. Having both clinical risk factors confers a 10- to 20-fold increase in risk.

|
| Dr. Jyoti Patel |
"Many women fear recurrence, and they also fear surveillance. They worry about, if they’re 35 years old, what a lifetime of screening for the contralateral breast might look like if they end up getting multiple biopsies. So how we put that in perspective for our young population will become vitally important," Dr. Patel said.
Dr. Patel, a thoracic oncologist at Northwestern University in Chicago, is a member of ASCO’s Cancer Communications Committee.
Among breast cancer patients, women who worry the most that localized cancer in one breast will spread to the other breast are twice as likely to choose a prophylactic double mastectomy – even though most of them have no clinical indication for the procedure, a study of 1,446 patients showed.
Approximately 80% of the 107 women in the study who chose prophylactic double mastectomy had a very low risk for contralateral disease, Sarah T. Hawley, Ph.D., said in a press conference sponsored by the American Society of Clinical Oncology (ASCO).
She is slated to present the results at a symposium on quality care sponsored by the American Society of Clinical Oncology, taking place Nov. 30 to Dec. 1 in San Diego.
Many women undergo unnecessary surgery out of ungrounded fear that cancer in one breast will lead to cancer in the other, said Dr. Hawley of the division of general medicine at the University of Michigan, Ann Arbor.
Women’s worry about cancer spreading from one breast to the other "really shouldn’t be a reason to get that procedure," she said.
Contralateral prophylactic mastectomy can be considered if a patient is positive for BRCA1 or BRCA2 mutations or has a family history of breast or ovarian cancer in two or more first-degree relatives, according to Society of Surgical Oncology guidelines.
"Despite the small number of women who meet these criteria, rates of contralateral prophylactic mastectomy have been increasing in recent years," Dr. Hawley noted.
Those traditional indications still were powerful drivers in the study – a positive genetic test increased the odds of contralateral prophylactic mastectomy 10-fold, and a family history increased the odds 5-fold.
The doubling in odds of contralateral prophylactic mastectomy in women with a high level of worry (compared with low worry level) is notable because the prophylactic surgery has not been known to reduce the risk of recurrence when those indications are not present, as was the case with the majority of women who chose the procedure in the study.
Among women who chose contralateral prophylactic mastectomy, 90% reported high levels of worry, compared with 80% of the 564 women who underwent single-breast mastectomy, a statistically significant difference, Dr. Hawley reported.
She and her associates studied 1,446 newly diagnosed breast cancer patients who completed two surveys 4 years apart, had not had a recurrence during that time, and had complete data on genetic testing and family history. Contralateral prophylactic mastectomy was considered by 35% of the whole cohort and chosen by 7%. Among women who underwent mastectomy of the cancerous breast, 53% considered contralateral prophylactic mastectomy and 19% underwent the procedure.
When women were considering any mastectomy vs. breast conservation surgery, family history and genetic test results did not significantly affect the odds that they would choose any mastectomy, but their level of worry did. High levels of worry significantly increased the odds of mastectomy by 69% in a subanalysis that controlled for the effects of age, race or ethnicity, education, and cancer stage.
A separate subanalysis found that both clinical indications and worry affected the likelihood of contralateral prophylactic mastectomy compared with unilateral mastectomy. The odds of having the prophylactic surgery increased more than 4-fold with a family history of at least two primary relatives with breast cancer, more than 10-fold with a positive genetic test, and more than 2-fold with a high degree of worry in the multivariate analysis, Dr. Hawley said.
Compared with previous studies on why women are getting contralateral prophylactic mastectomy, the current study is larger; is population-based; contains racial and ethnic samples; and includes data on patient attitudes, genetic testing, and type of family history (not just any family history), she said.
Dr. Jyoti D. Patel, moderator of the press conference, said the findings suggest that "we, as physicians, may not be adequately educating our patients about the risk for recurrent disease."
In general, women with localized breast cancer in one breast have less than a 1% chance of developing a new cancer in the unaffected breast and an 8% chance of recurrence in the affected breast or a nearby lymph node. The risk for developing a new cancer in the contralateral breast rises to approximately 10%-15% if the patient has a history of breast or ovarian cancer in two or more primary relatives, with a similar or slightly greater increased risk from a positive genetic mutation, Dr. Patel estimated. Having both clinical risk factors confers a 10- to 20-fold increase in risk.
Unfortunately, many women overestimate their risk of developing breast cancer in the contralateral breast and undergo unnecessary surgery, she commented. This study suggests that physicians re-examine how they communicate with their patients regarding the decision to undergo prophylactic mastectomy.
"Many women fear recurrence, and they also fear surveillance. They worry about, if they’re 35 years old, what a lifetime of screening for the contralateral breast might look like if they end up getting multiple biopsies. So how we put that in perspective for our young population will become vitally important," said Dr. Patell, a thoracic oncologist at Northwestern University in Chicago and a member of ASCO’s Cancer Communications Committee.
Dr. Hawley reported having no financial disclosures.
Among breast cancer patients, women who worry the most that localized cancer in one breast will spread to the other breast are twice as likely to choose a prophylactic double mastectomy – even though most of them have no clinical indication for the procedure, a study of 1,446 patients showed.
Approximately 80% of the 107 women in the study who chose prophylactic double mastectomy had a very low risk for contralateral disease, Sarah T. Hawley, Ph.D., said in a press conference sponsored by the American Society of Clinical Oncology (ASCO).
She is slated to present the results at a symposium on quality care sponsored by the American Society of Clinical Oncology, taking place Nov. 30 to Dec. 1 in San Diego.
Many women undergo unnecessary surgery out of ungrounded fear that cancer in one breast will lead to cancer in the other, said Dr. Hawley of the division of general medicine at the University of Michigan, Ann Arbor.
Women’s worry about cancer spreading from one breast to the other "really shouldn’t be a reason to get that procedure," she said.
Contralateral prophylactic mastectomy can be considered if a patient is positive for BRCA1 or BRCA2 mutations or has a family history of breast or ovarian cancer in two or more first-degree relatives, according to Society of Surgical Oncology guidelines.
"Despite the small number of women who meet these criteria, rates of contralateral prophylactic mastectomy have been increasing in recent years," Dr. Hawley noted.
Those traditional indications still were powerful drivers in the study – a positive genetic test increased the odds of contralateral prophylactic mastectomy 10-fold, and a family history increased the odds 5-fold.
The doubling in odds of contralateral prophylactic mastectomy in women with a high level of worry (compared with low worry level) is notable because the prophylactic surgery has not been known to reduce the risk of recurrence when those indications are not present, as was the case with the majority of women who chose the procedure in the study.
Among women who chose contralateral prophylactic mastectomy, 90% reported high levels of worry, compared with 80% of the 564 women who underwent single-breast mastectomy, a statistically significant difference, Dr. Hawley reported.
She and her associates studied 1,446 newly diagnosed breast cancer patients who completed two surveys 4 years apart, had not had a recurrence during that time, and had complete data on genetic testing and family history. Contralateral prophylactic mastectomy was considered by 35% of the whole cohort and chosen by 7%. Among women who underwent mastectomy of the cancerous breast, 53% considered contralateral prophylactic mastectomy and 19% underwent the procedure.
When women were considering any mastectomy vs. breast conservation surgery, family history and genetic test results did not significantly affect the odds that they would choose any mastectomy, but their level of worry did. High levels of worry significantly increased the odds of mastectomy by 69% in a subanalysis that controlled for the effects of age, race or ethnicity, education, and cancer stage.
A separate subanalysis found that both clinical indications and worry affected the likelihood of contralateral prophylactic mastectomy compared with unilateral mastectomy. The odds of having the prophylactic surgery increased more than 4-fold with a family history of at least two primary relatives with breast cancer, more than 10-fold with a positive genetic test, and more than 2-fold with a high degree of worry in the multivariate analysis, Dr. Hawley said.
Compared with previous studies on why women are getting contralateral prophylactic mastectomy, the current study is larger; is population-based; contains racial and ethnic samples; and includes data on patient attitudes, genetic testing, and type of family history (not just any family history), she said.
Dr. Jyoti D. Patel, moderator of the press conference, said the findings suggest that "we, as physicians, may not be adequately educating our patients about the risk for recurrent disease."
In general, women with localized breast cancer in one breast have less than a 1% chance of developing a new cancer in the unaffected breast and an 8% chance of recurrence in the affected breast or a nearby lymph node. The risk for developing a new cancer in the contralateral breast rises to approximately 10%-15% if the patient has a history of breast or ovarian cancer in two or more primary relatives, with a similar or slightly greater increased risk from a positive genetic mutation, Dr. Patel estimated. Having both clinical risk factors confers a 10- to 20-fold increase in risk.
Unfortunately, many women overestimate their risk of developing breast cancer in the contralateral breast and undergo unnecessary surgery, she commented. This study suggests that physicians re-examine how they communicate with their patients regarding the decision to undergo prophylactic mastectomy.
"Many women fear recurrence, and they also fear surveillance. They worry about, if they’re 35 years old, what a lifetime of screening for the contralateral breast might look like if they end up getting multiple biopsies. So how we put that in perspective for our young population will become vitally important," said Dr. Patell, a thoracic oncologist at Northwestern University in Chicago and a member of ASCO’s Cancer Communications Committee.
Dr. Hawley reported having no financial disclosures.
FROM A PRESS CONFERENCE SPONSORED BY THE AMERICAN SOCIETY OF CLINICAL ONCOLOGY
Major Finding: Eighty percent of 107 women who underwent contralateral prophylactic mastectomy had no clinical indication for the procedure. A high level of worry doubled the odds of choosing the procedure.
Data Source: Investigators studied 1,446 newly diagnosed breast cancer patients who completed two surveys 4 years apart, had not had a recurrence during that time, and had complete data on genetic testing and family history.
Disclosures: Dr. Hawley reported having no financial disclosures.
Progress Limited in Transcatheter Repair of Mitral Regurgitation
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
EXPERT ANALYSIS FROM THE HEART VALVE SUMMIT 2012
In Type 1 Diabetes, Cardiac Measures Improved After Pancreas Transplant
BERLIN -- A pancreas-only transplant improved cardiac function and morphology in a group of patients with type 1 diabetes.
After 5 years, the patients showed significantly improved posterior wall and interventricular septal thickness, as well as a significantly increased left ventricular ejection fraction, Dr. Margherita Occhipinti said at the annual meeting of the European Societies for the Study of Diabetes.
She reported 5-year follow-up data on 35 patients with type 1 diabetes who underwent the procedure. The patients were a mean of 38 years old and had a mean disease duration of 25 years. Their mean insulin requirement was 43 U/day.
Most of the transplants (74%) were performed with a portal-enteric drain technique; the remainder had systemic-enteric drainage, said Dr. Occhipinti of the University of Pisa (Italy). The majority (77%) had induction therapy with basiliximab; the rest had antithymocyte globulin (rabbit) induction. The maintenance immunosuppressant regimen was a combination of mycophenolate mofetil, tacrolimus, and steroids.
At last follow-up, fasting plasma glucose level had normalized, hemoglobin A1c level had fallen from 9% to just under 6%, and C-peptide level had increased from under 1 ng/mL to almost 3 ng/mL.
There were no significant changes in either systolic or diastolic blood pressure. However, the number of patients taking ACE inhibitors or angiotensin receptor blockers decreased from 59% to 43%. Total and LDL cholesterol levels decreased significantly, although there were no significant changes in HDL cholesterol or triglycerides.
Cardiac morphology changed significantly, Dr. Occhipinti said, including a significant decrease in posterior wall thickness during diastole, from 8.1 mm to 7.0 mm, and interventricular septum thickness during diastole, from 9.3 mm to 8.7 mm. The left ventricular mass index decreased significantly, from 82 mg/m2 to 73 mg/m2; and the left ventricular ejection fraction increased significantly, from 55.3% to 57.9%.
Dr. Occhipinti compared these changes to 2-year findings in a group of 11 control patients who were on a transplant waiting list or who had a failed pancreatic transplant.
In this group, there were no significant changes in HbA1c, left ventricular ejection fraction, or any of the measures of cardiac morphology.
Dr. Occhipinti said she had no relevant financial disclosures.
BERLIN -- A pancreas-only transplant improved cardiac function and morphology in a group of patients with type 1 diabetes.
After 5 years, the patients showed significantly improved posterior wall and interventricular septal thickness, as well as a significantly increased left ventricular ejection fraction, Dr. Margherita Occhipinti said at the annual meeting of the European Societies for the Study of Diabetes.
She reported 5-year follow-up data on 35 patients with type 1 diabetes who underwent the procedure. The patients were a mean of 38 years old and had a mean disease duration of 25 years. Their mean insulin requirement was 43 U/day.
Most of the transplants (74%) were performed with a portal-enteric drain technique; the remainder had systemic-enteric drainage, said Dr. Occhipinti of the University of Pisa (Italy). The majority (77%) had induction therapy with basiliximab; the rest had antithymocyte globulin (rabbit) induction. The maintenance immunosuppressant regimen was a combination of mycophenolate mofetil, tacrolimus, and steroids.
At last follow-up, fasting plasma glucose level had normalized, hemoglobin A1c level had fallen from 9% to just under 6%, and C-peptide level had increased from under 1 ng/mL to almost 3 ng/mL.
There were no significant changes in either systolic or diastolic blood pressure. However, the number of patients taking ACE inhibitors or angiotensin receptor blockers decreased from 59% to 43%. Total and LDL cholesterol levels decreased significantly, although there were no significant changes in HDL cholesterol or triglycerides.
Cardiac morphology changed significantly, Dr. Occhipinti said, including a significant decrease in posterior wall thickness during diastole, from 8.1 mm to 7.0 mm, and interventricular septum thickness during diastole, from 9.3 mm to 8.7 mm. The left ventricular mass index decreased significantly, from 82 mg/m2 to 73 mg/m2; and the left ventricular ejection fraction increased significantly, from 55.3% to 57.9%.
Dr. Occhipinti compared these changes to 2-year findings in a group of 11 control patients who were on a transplant waiting list or who had a failed pancreatic transplant.
In this group, there were no significant changes in HbA1c, left ventricular ejection fraction, or any of the measures of cardiac morphology.
Dr. Occhipinti said she had no relevant financial disclosures.
BERLIN -- A pancreas-only transplant improved cardiac function and morphology in a group of patients with type 1 diabetes.
After 5 years, the patients showed significantly improved posterior wall and interventricular septal thickness, as well as a significantly increased left ventricular ejection fraction, Dr. Margherita Occhipinti said at the annual meeting of the European Societies for the Study of Diabetes.
She reported 5-year follow-up data on 35 patients with type 1 diabetes who underwent the procedure. The patients were a mean of 38 years old and had a mean disease duration of 25 years. Their mean insulin requirement was 43 U/day.
Most of the transplants (74%) were performed with a portal-enteric drain technique; the remainder had systemic-enteric drainage, said Dr. Occhipinti of the University of Pisa (Italy). The majority (77%) had induction therapy with basiliximab; the rest had antithymocyte globulin (rabbit) induction. The maintenance immunosuppressant regimen was a combination of mycophenolate mofetil, tacrolimus, and steroids.
At last follow-up, fasting plasma glucose level had normalized, hemoglobin A1c level had fallen from 9% to just under 6%, and C-peptide level had increased from under 1 ng/mL to almost 3 ng/mL.
There were no significant changes in either systolic or diastolic blood pressure. However, the number of patients taking ACE inhibitors or angiotensin receptor blockers decreased from 59% to 43%. Total and LDL cholesterol levels decreased significantly, although there were no significant changes in HDL cholesterol or triglycerides.
Cardiac morphology changed significantly, Dr. Occhipinti said, including a significant decrease in posterior wall thickness during diastole, from 8.1 mm to 7.0 mm, and interventricular septum thickness during diastole, from 9.3 mm to 8.7 mm. The left ventricular mass index decreased significantly, from 82 mg/m2 to 73 mg/m2; and the left ventricular ejection fraction increased significantly, from 55.3% to 57.9%.
Dr. Occhipinti compared these changes to 2-year findings in a group of 11 control patients who were on a transplant waiting list or who had a failed pancreatic transplant.
In this group, there were no significant changes in HbA1c, left ventricular ejection fraction, or any of the measures of cardiac morphology.
Dr. Occhipinti said she had no relevant financial disclosures.
AT THE ANNUAL MEETING OF THE EUROPEAN SOCIETIES FOR THE STUDY OF DIABETES
Major Finding: Cardiac morphology and function improved significantly after pancreas-only transplant: Posterior wall thickness and interventricular septum thickness decreased during diastole, from 8.1 mm to 7.0 mm and from 9.3 mm to 8.7 mm, respectively; left ventricular mass index decreased from 82 mg/m2 to 73 mg/m2; and left ventricular ejection fraction increased, from 55.3% to 57.9%.
Data Source: Data are from 35 patients with longstanding type 1 diabetes.
Disclosures: Dr. Occhipinti said she had no relevant financial disclosures.