User login
Official Newspaper of the American College of Surgeons
Appendix linked to Parkinson’s disease in series of unexpected findings
Appendectomy has been associated with a reduced risk of Parkinson’s disease (PD), which supports the potential for a reservoir of aggregated alpha-synuclein in the appendix to affect risk of the condition, according to new epidemiologic and translational evidence from two data sets that promotes a new and emerging theory for PD etiology.
When placed into the context of other recent studies, these epidemiologic data “point to the appendix as a site of origin for Parkinson’s and provide a path forward for devising new treatment strategies,” reported senior author Viviane Labrie, PhD, of the Van Andel Research Institute (VARI) in Grand Rapids, Mich.
The epidemiologic data was the most recent step in a series of findings summarized in a newly published paper in Science Translational Medicine. As the researchers explained, it is relevant to a separate body of evidence that alpha-synuclein, a protein that serves as the hallmark of PD when it appears in Lewy bodies, can be isolated in the nerve fibers and nerve cells of the appendix.
“We have shown that alpha-synuclein proteins, including the truncated forms observed in Lewy bodies, are abundant in the appendix,” reported first author Bryan A. Killinger, PhD, also at VARI, in a press teleconference. He said this finding is likely to explain the reduced risk of PD from appendectomy.
In the largest of the epidemiologic studies, the effect of appendectomy on subsequent risk of PD was evaluated through the health records from more than 1.6 million individuals in Sweden. The incidence of PD was found to be 19.3% lower among 551,647 patients who had an appendectomy, compared with controls.
In addition, the data showed that when PD did occur after appendectomy, it was delayed on average by 3.6 years. It is notable that appendectomy was not associated with protection from PD in patients with a familial link to PD, a group they said comprises less than 10% of cases.
In patients with PD, nonmotor symptoms often include GI tract dysfunction, which can, in some cases, be part of a prodromal presentation that precedes the onset of classical PD symptoms by several years, the authors reported. However, the new research upends previous conceptions of disease. The demonstration of abundant alpha-synuclein in the appendix coupled with the protective effect of appendectomy, suggests that PD may originate in the GI tract and then spread to the central nervous system (CNS) rather than the other way around.
“The vermiform appendix was once considered to be an unnecessary organ. Although there is now good evidence that the appendix plays a major role in the regulation of the immune system, including the regulation of gut bacteria, our work suggests it is also mediates risk of Parkinson’s,” Dr. Labrie said in the teleconference.
In the paper, numerous pieces of the puzzle are brought together to suggest that alpha-synuclein in the appendix is linked to alpha-synuclein in the CNS. Many of the findings along this investigative pathway were described as surprising. For example, immunohistochemistry studies revealed high amounts of alpha-synuclein in nearly every sample of appendiceal tissue examined, including normal and inflamed tissue, tissue from individuals with PD and those without, and tissues from young and old individuals.
“The normal tissue, as well as appendiceal tissue from PD patients, contained high levels of alpha-synuclein in the truncated forms analogous to those seen in Lewy body pathology,” Dr. Killinger said. Based on these and other findings, he believes that alpha-synuclein in the appendix forms a reservoir for seeding the aggregates involved in the pathology of PD, although he acknowledged that it is not yet clear how the proteins in the appendix find their way to the brain.
From these data, it appears that most individuals with an intact appendix have alpha-synuclein in the nerve fibers, but Dr. Labrie pointed out that the only about 1% of the population develops PD. She speculated that there is “some confluence of events,” such as an environmental trigger altering the GI microbiome, that mediates ultimate risk of PD, but she noted that these events may take place decades before signs and symptoms of PD develop. The data appear to be a substantial reorientation in understanding PD.
“We have shown that the appendix is a hub for the accumulation of clumped forms of alpha-synuclein proteins, which are implicated in Parkinson’s,” Dr. Killinger said. “This knowledge will be invaluable as we explore new prevention and treatment strategies.”
The research was funded by a variety of governmental and private grants to individual authors. Dr. Killinger and Dr. Labrie report no financial relationships relevant to this study.
SOURCE: Killinger BA et al. Sci Transl Med. 2018;10:eaar5380.
Appendectomy has been associated with a reduced risk of Parkinson’s disease (PD), which supports the potential for a reservoir of aggregated alpha-synuclein in the appendix to affect risk of the condition, according to new epidemiologic and translational evidence from two data sets that promotes a new and emerging theory for PD etiology.
When placed into the context of other recent studies, these epidemiologic data “point to the appendix as a site of origin for Parkinson’s and provide a path forward for devising new treatment strategies,” reported senior author Viviane Labrie, PhD, of the Van Andel Research Institute (VARI) in Grand Rapids, Mich.
The epidemiologic data was the most recent step in a series of findings summarized in a newly published paper in Science Translational Medicine. As the researchers explained, it is relevant to a separate body of evidence that alpha-synuclein, a protein that serves as the hallmark of PD when it appears in Lewy bodies, can be isolated in the nerve fibers and nerve cells of the appendix.
“We have shown that alpha-synuclein proteins, including the truncated forms observed in Lewy bodies, are abundant in the appendix,” reported first author Bryan A. Killinger, PhD, also at VARI, in a press teleconference. He said this finding is likely to explain the reduced risk of PD from appendectomy.
In the largest of the epidemiologic studies, the effect of appendectomy on subsequent risk of PD was evaluated through the health records from more than 1.6 million individuals in Sweden. The incidence of PD was found to be 19.3% lower among 551,647 patients who had an appendectomy, compared with controls.
In addition, the data showed that when PD did occur after appendectomy, it was delayed on average by 3.6 years. It is notable that appendectomy was not associated with protection from PD in patients with a familial link to PD, a group they said comprises less than 10% of cases.
In patients with PD, nonmotor symptoms often include GI tract dysfunction, which can, in some cases, be part of a prodromal presentation that precedes the onset of classical PD symptoms by several years, the authors reported. However, the new research upends previous conceptions of disease. The demonstration of abundant alpha-synuclein in the appendix coupled with the protective effect of appendectomy, suggests that PD may originate in the GI tract and then spread to the central nervous system (CNS) rather than the other way around.
“The vermiform appendix was once considered to be an unnecessary organ. Although there is now good evidence that the appendix plays a major role in the regulation of the immune system, including the regulation of gut bacteria, our work suggests it is also mediates risk of Parkinson’s,” Dr. Labrie said in the teleconference.
In the paper, numerous pieces of the puzzle are brought together to suggest that alpha-synuclein in the appendix is linked to alpha-synuclein in the CNS. Many of the findings along this investigative pathway were described as surprising. For example, immunohistochemistry studies revealed high amounts of alpha-synuclein in nearly every sample of appendiceal tissue examined, including normal and inflamed tissue, tissue from individuals with PD and those without, and tissues from young and old individuals.
“The normal tissue, as well as appendiceal tissue from PD patients, contained high levels of alpha-synuclein in the truncated forms analogous to those seen in Lewy body pathology,” Dr. Killinger said. Based on these and other findings, he believes that alpha-synuclein in the appendix forms a reservoir for seeding the aggregates involved in the pathology of PD, although he acknowledged that it is not yet clear how the proteins in the appendix find their way to the brain.
From these data, it appears that most individuals with an intact appendix have alpha-synuclein in the nerve fibers, but Dr. Labrie pointed out that the only about 1% of the population develops PD. She speculated that there is “some confluence of events,” such as an environmental trigger altering the GI microbiome, that mediates ultimate risk of PD, but she noted that these events may take place decades before signs and symptoms of PD develop. The data appear to be a substantial reorientation in understanding PD.
“We have shown that the appendix is a hub for the accumulation of clumped forms of alpha-synuclein proteins, which are implicated in Parkinson’s,” Dr. Killinger said. “This knowledge will be invaluable as we explore new prevention and treatment strategies.”
The research was funded by a variety of governmental and private grants to individual authors. Dr. Killinger and Dr. Labrie report no financial relationships relevant to this study.
SOURCE: Killinger BA et al. Sci Transl Med. 2018;10:eaar5380.
Appendectomy has been associated with a reduced risk of Parkinson’s disease (PD), which supports the potential for a reservoir of aggregated alpha-synuclein in the appendix to affect risk of the condition, according to new epidemiologic and translational evidence from two data sets that promotes a new and emerging theory for PD etiology.
When placed into the context of other recent studies, these epidemiologic data “point to the appendix as a site of origin for Parkinson’s and provide a path forward for devising new treatment strategies,” reported senior author Viviane Labrie, PhD, of the Van Andel Research Institute (VARI) in Grand Rapids, Mich.
The epidemiologic data was the most recent step in a series of findings summarized in a newly published paper in Science Translational Medicine. As the researchers explained, it is relevant to a separate body of evidence that alpha-synuclein, a protein that serves as the hallmark of PD when it appears in Lewy bodies, can be isolated in the nerve fibers and nerve cells of the appendix.
“We have shown that alpha-synuclein proteins, including the truncated forms observed in Lewy bodies, are abundant in the appendix,” reported first author Bryan A. Killinger, PhD, also at VARI, in a press teleconference. He said this finding is likely to explain the reduced risk of PD from appendectomy.
In the largest of the epidemiologic studies, the effect of appendectomy on subsequent risk of PD was evaluated through the health records from more than 1.6 million individuals in Sweden. The incidence of PD was found to be 19.3% lower among 551,647 patients who had an appendectomy, compared with controls.
In addition, the data showed that when PD did occur after appendectomy, it was delayed on average by 3.6 years. It is notable that appendectomy was not associated with protection from PD in patients with a familial link to PD, a group they said comprises less than 10% of cases.
In patients with PD, nonmotor symptoms often include GI tract dysfunction, which can, in some cases, be part of a prodromal presentation that precedes the onset of classical PD symptoms by several years, the authors reported. However, the new research upends previous conceptions of disease. The demonstration of abundant alpha-synuclein in the appendix coupled with the protective effect of appendectomy, suggests that PD may originate in the GI tract and then spread to the central nervous system (CNS) rather than the other way around.
“The vermiform appendix was once considered to be an unnecessary organ. Although there is now good evidence that the appendix plays a major role in the regulation of the immune system, including the regulation of gut bacteria, our work suggests it is also mediates risk of Parkinson’s,” Dr. Labrie said in the teleconference.
In the paper, numerous pieces of the puzzle are brought together to suggest that alpha-synuclein in the appendix is linked to alpha-synuclein in the CNS. Many of the findings along this investigative pathway were described as surprising. For example, immunohistochemistry studies revealed high amounts of alpha-synuclein in nearly every sample of appendiceal tissue examined, including normal and inflamed tissue, tissue from individuals with PD and those without, and tissues from young and old individuals.
“The normal tissue, as well as appendiceal tissue from PD patients, contained high levels of alpha-synuclein in the truncated forms analogous to those seen in Lewy body pathology,” Dr. Killinger said. Based on these and other findings, he believes that alpha-synuclein in the appendix forms a reservoir for seeding the aggregates involved in the pathology of PD, although he acknowledged that it is not yet clear how the proteins in the appendix find their way to the brain.
From these data, it appears that most individuals with an intact appendix have alpha-synuclein in the nerve fibers, but Dr. Labrie pointed out that the only about 1% of the population develops PD. She speculated that there is “some confluence of events,” such as an environmental trigger altering the GI microbiome, that mediates ultimate risk of PD, but she noted that these events may take place decades before signs and symptoms of PD develop. The data appear to be a substantial reorientation in understanding PD.
“We have shown that the appendix is a hub for the accumulation of clumped forms of alpha-synuclein proteins, which are implicated in Parkinson’s,” Dr. Killinger said. “This knowledge will be invaluable as we explore new prevention and treatment strategies.”
The research was funded by a variety of governmental and private grants to individual authors. Dr. Killinger and Dr. Labrie report no financial relationships relevant to this study.
SOURCE: Killinger BA et al. Sci Transl Med. 2018;10:eaar5380.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: A 19.3% reduction in risk of PD from appendectomy may relate to alpha-synuclein in the appendix.
Study details: Series of related epidemiologic and translational studies.
Disclosures: The research was funded by a variety of governmental and private grants to individual authors. Dr. Killinger and Dr. Labrie report no financial relationships relevant to this study.
Source: Killinger BA et al. Sci Transl Med. 2018;10:eaar5380.
The election’s impact on health care: Some bellwether races to watch
Voters this year have told pollsters in no uncertain terms that health care is important to them. In particular, maintaining insurance protections for preexisting conditions is the top issue to many.
But the results of the midterm elections are likely to have a major impact on a broad array of other health issues that touch every single American. And how those issues are addressed will depend in large part on which party controls the U.S. House and Senate, governors’ mansions, and state legislatures around the country.
All politics is local, and no single race is likely to determine national or even state action. But some key contests can provide something of a barometer of what’s likely to happen – or not happen – over the next 2 years.
For example, keep an eye on Kansas. The razor-tight race for governor could determine whether the state expands Medicaid to all people with low incomes, as allowed under the Affordable Care Act. The legislature in that deep-red state passed a bill to accept expansion in 2017, but it could not override the veto of then-Gov. Sam Brownback. Of the candidates running for governor in 2018, Democrat Laura Kelly supports expansion, while Republican Kris Kobach does not.
Here are three big health issues that could be dramatically affected by Tuesday’s vote.
1. The Affordable Care Act
Protections for preexisting conditions are only a small part of the ACA. The law also made big changes to Medicare and Medicaid, employer-provided health plans, and the generic drug approval process, among other things.
Republicans ran hard on promises to get rid of the law in every election since it passed in 2010. But when the GOP finally got control of the House, the Senate, and the White House in 2017, Republicans found they could not reach agreement on how to “repeal and replace” the law.
This year has Democrats on the attack over the votes Republicans took on various proposals to remake the health law. Probably the most endangered Democrat in the Senate, Heidi Heitkamp of North Dakota, has hammered her Republican opponent, U.S. Rep. Kevin Cramer, over his votes in the House for the unsuccessful repeal-and-replace bills. Rep. Cramer said that despite his votes he supports protections for preexisting conditions, but he has not said what he would do or get behind that could have that effect.
Polls suggest Rep. Cramer has a healthy lead in that race, but if Sen. Heitkamp pulled off a surprise win, health care might well get some of the credit.
And in New Jersey, Rep. Tom MacArthur, the moderate Republican who wrote the language that got the GOP health bill passed in the House in 2017, is in a heated race with Democrat Andy Kim, who has never held elective office. The overriding issue in that race, too, is health care.
It is not just congressional action that has Republicans playing defense on the ACA. In February, 18 GOP attorneys general and 2 GOP governors filed a lawsuit seeking a judgment that the law is now unconstitutional because Congress in the 2017 tax bill repealed the penalty for not having insurance. Two of those attorneys general – Missouri’s Josh Hawley and West Virginia’s Patrick Morrisey – are running for the Senate. Both states overwhelmingly supported President Donald Trump in 2016.
The attorneys general are running against Democratic incumbents – Claire McCaskill of Missouri and Joe Manchin of West Virginia. And both Republicans are being hotly criticized by their opponents for their participation in the lawsuit.
Although Sen. Manchin appears to have taken a lead, the Hawley-McCaskill race is rated a toss-up by political analysts.
But in the end the fate of the ACA depends less on an individual race than on which party winds up in control of Congress.
“If Democrats take the House ... then any attempt at repeal-and-replace will be kaput,” said John McDonough, a former Democratic Senate aide who helped write the ACA and now teaches at the Harvard School of Public Health, Boston.
Conservative health care strategist Chris Jacobs, who worked for Republicans on Capitol Hill, said a new repeal-and-replace effort might not happen even if Republicans are successful Tuesday.
“Republicans, if they maintain the majority in the House, will have a margin of a half-dozen seats – if they are lucky,” he said. That likely would not allow the party to push through another controversial effort to change the law. Currently there are 42 more Republicans than Democrats in the House. Even so, the GOP barely got its health bill passed out of the House in 2017.
And political strategists say that, when the dust clears after voting, the numbers in the Senate may not be much different so change could be hard there too. Republicans, even with a small majority last year, could not pass a repeal bill there.
2. Medicaid expansion
The Supreme Court in 2012 made optional the ACA’s expansion of Medicaid to cover all low-income Americans up to 138% of the poverty line ($16,753 for an individual in 2018). Most states have now expanded, particularly since the federal government is paying the vast majority of the cost: 94% in 2018, gradually dropping to 90% in 2020.
Still, 17 states, all with GOP governors or state legislatures (or both), have yet to expand Medicaid.
Mr. McDonough is confident that’s about to change. “I’m wondering if we’re on the cusp of a Medicaid wave,” he said.
Four states – Idaho, Montana, Nebraska, and Utah – have Medicaid expansion questions on their ballots. All but Montana have yet to expand the program. Montana’s question would eliminate the 2019 sunset date included in its expansion in 2016. But it will be interesting to watch results because the measure has run into big-pocketed opposition: the tobacco industry. The initiative would increase taxes on cigarettes and other tobacco products to fund the state’s increased Medicaid costs.
In Idaho, the ballot measure is being embraced by a number of Republican leaders. GOP Gov. Butch Otter, who is retiring after three terms, endorsed it Oct. 30.
But the issue is in play in other states, too. Several nonexpansion states have close or closer-than-expected races for governor where the Democrat has made Medicaid expansion a priority.
In Florida, one of the largest states not to have expanded Medicaid, the Republican candidate for governor, former U.S. Rep. Ron DeSantis, opposes expansion. His Democratic opponent, Tallahassee Mayor Andrew Gillum, supports it.
In Georgia, the gubernatorial candidates, Democrat Stacey Abrams and Republican Brian Kemp, are also on opposite sides of the Medicaid expansion debate.
However, the legislatures in both states have opposed the expansion, and it’s not clear if they would be swayed by arguments from a new governor.
3. Medicare
Until recently, Republicans have remained relatively quiet about efforts to change the popular Medicare program for seniors and people with disabilities.
Their new talking point is that proposals to expand the program – such as the often-touted “Medicare-for-all,” which an increasing number of Democrats are embracing – could threaten the existing program.
“Medicare is at significant risk of being cut if Democrats take over the House,” Rep. Greg Gianforte (R-Mont.) told the Lee Montana Newspapers. “Medicare-for-all is Medicare for none. It will gut Medicare, end the VA [Department of Veterans Affairs] as we know it, and force Montana seniors to the back of the line.”
Gianforte’s Democratic opponent, Kathleen Williams, is proposing another idea popular with Democrats: allowing people aged 55 years and over to “buy into” Medicare coverage. That race, too, is very tight.
Meanwhile, back in Washington, congressional Republicans are more concerned with how Medicare and other large government social programs are threatening the budget.
“Sooner or later we are going to run out of other people’s money,” said Mr. Jacobs.
Senate Majority Leader Mitch McConnell (R-Ky.) suggested in an Oct. 16 interview with Bloomberg News that entitlement programs like Medicare are “the real driver of the debt by any objective standard,” but that bipartisan cooperation will be needed to address that problem
Republican Mr. Jacobs and Democrat Mr. McDonough think that’s unlikely any time soon.
“Why would Democrats give that up as an issue heading into 2020?” asked Mr. McDonough, especially because Republicans in recent years have been proposing deep cuts to the Medicare program.
Agreed Mr. Jacobs, “Trump may not want that to be the centerpiece of a reelection campaign.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Voters this year have told pollsters in no uncertain terms that health care is important to them. In particular, maintaining insurance protections for preexisting conditions is the top issue to many.
But the results of the midterm elections are likely to have a major impact on a broad array of other health issues that touch every single American. And how those issues are addressed will depend in large part on which party controls the U.S. House and Senate, governors’ mansions, and state legislatures around the country.
All politics is local, and no single race is likely to determine national or even state action. But some key contests can provide something of a barometer of what’s likely to happen – or not happen – over the next 2 years.
For example, keep an eye on Kansas. The razor-tight race for governor could determine whether the state expands Medicaid to all people with low incomes, as allowed under the Affordable Care Act. The legislature in that deep-red state passed a bill to accept expansion in 2017, but it could not override the veto of then-Gov. Sam Brownback. Of the candidates running for governor in 2018, Democrat Laura Kelly supports expansion, while Republican Kris Kobach does not.
Here are three big health issues that could be dramatically affected by Tuesday’s vote.
1. The Affordable Care Act
Protections for preexisting conditions are only a small part of the ACA. The law also made big changes to Medicare and Medicaid, employer-provided health plans, and the generic drug approval process, among other things.
Republicans ran hard on promises to get rid of the law in every election since it passed in 2010. But when the GOP finally got control of the House, the Senate, and the White House in 2017, Republicans found they could not reach agreement on how to “repeal and replace” the law.
This year has Democrats on the attack over the votes Republicans took on various proposals to remake the health law. Probably the most endangered Democrat in the Senate, Heidi Heitkamp of North Dakota, has hammered her Republican opponent, U.S. Rep. Kevin Cramer, over his votes in the House for the unsuccessful repeal-and-replace bills. Rep. Cramer said that despite his votes he supports protections for preexisting conditions, but he has not said what he would do or get behind that could have that effect.
Polls suggest Rep. Cramer has a healthy lead in that race, but if Sen. Heitkamp pulled off a surprise win, health care might well get some of the credit.
And in New Jersey, Rep. Tom MacArthur, the moderate Republican who wrote the language that got the GOP health bill passed in the House in 2017, is in a heated race with Democrat Andy Kim, who has never held elective office. The overriding issue in that race, too, is health care.
It is not just congressional action that has Republicans playing defense on the ACA. In February, 18 GOP attorneys general and 2 GOP governors filed a lawsuit seeking a judgment that the law is now unconstitutional because Congress in the 2017 tax bill repealed the penalty for not having insurance. Two of those attorneys general – Missouri’s Josh Hawley and West Virginia’s Patrick Morrisey – are running for the Senate. Both states overwhelmingly supported President Donald Trump in 2016.
The attorneys general are running against Democratic incumbents – Claire McCaskill of Missouri and Joe Manchin of West Virginia. And both Republicans are being hotly criticized by their opponents for their participation in the lawsuit.
Although Sen. Manchin appears to have taken a lead, the Hawley-McCaskill race is rated a toss-up by political analysts.
But in the end the fate of the ACA depends less on an individual race than on which party winds up in control of Congress.
“If Democrats take the House ... then any attempt at repeal-and-replace will be kaput,” said John McDonough, a former Democratic Senate aide who helped write the ACA and now teaches at the Harvard School of Public Health, Boston.
Conservative health care strategist Chris Jacobs, who worked for Republicans on Capitol Hill, said a new repeal-and-replace effort might not happen even if Republicans are successful Tuesday.
“Republicans, if they maintain the majority in the House, will have a margin of a half-dozen seats – if they are lucky,” he said. That likely would not allow the party to push through another controversial effort to change the law. Currently there are 42 more Republicans than Democrats in the House. Even so, the GOP barely got its health bill passed out of the House in 2017.
And political strategists say that, when the dust clears after voting, the numbers in the Senate may not be much different so change could be hard there too. Republicans, even with a small majority last year, could not pass a repeal bill there.
2. Medicaid expansion
The Supreme Court in 2012 made optional the ACA’s expansion of Medicaid to cover all low-income Americans up to 138% of the poverty line ($16,753 for an individual in 2018). Most states have now expanded, particularly since the federal government is paying the vast majority of the cost: 94% in 2018, gradually dropping to 90% in 2020.
Still, 17 states, all with GOP governors or state legislatures (or both), have yet to expand Medicaid.
Mr. McDonough is confident that’s about to change. “I’m wondering if we’re on the cusp of a Medicaid wave,” he said.
Four states – Idaho, Montana, Nebraska, and Utah – have Medicaid expansion questions on their ballots. All but Montana have yet to expand the program. Montana’s question would eliminate the 2019 sunset date included in its expansion in 2016. But it will be interesting to watch results because the measure has run into big-pocketed opposition: the tobacco industry. The initiative would increase taxes on cigarettes and other tobacco products to fund the state’s increased Medicaid costs.
In Idaho, the ballot measure is being embraced by a number of Republican leaders. GOP Gov. Butch Otter, who is retiring after three terms, endorsed it Oct. 30.
But the issue is in play in other states, too. Several nonexpansion states have close or closer-than-expected races for governor where the Democrat has made Medicaid expansion a priority.
In Florida, one of the largest states not to have expanded Medicaid, the Republican candidate for governor, former U.S. Rep. Ron DeSantis, opposes expansion. His Democratic opponent, Tallahassee Mayor Andrew Gillum, supports it.
In Georgia, the gubernatorial candidates, Democrat Stacey Abrams and Republican Brian Kemp, are also on opposite sides of the Medicaid expansion debate.
However, the legislatures in both states have opposed the expansion, and it’s not clear if they would be swayed by arguments from a new governor.
3. Medicare
Until recently, Republicans have remained relatively quiet about efforts to change the popular Medicare program for seniors and people with disabilities.
Their new talking point is that proposals to expand the program – such as the often-touted “Medicare-for-all,” which an increasing number of Democrats are embracing – could threaten the existing program.
“Medicare is at significant risk of being cut if Democrats take over the House,” Rep. Greg Gianforte (R-Mont.) told the Lee Montana Newspapers. “Medicare-for-all is Medicare for none. It will gut Medicare, end the VA [Department of Veterans Affairs] as we know it, and force Montana seniors to the back of the line.”
Gianforte’s Democratic opponent, Kathleen Williams, is proposing another idea popular with Democrats: allowing people aged 55 years and over to “buy into” Medicare coverage. That race, too, is very tight.
Meanwhile, back in Washington, congressional Republicans are more concerned with how Medicare and other large government social programs are threatening the budget.
“Sooner or later we are going to run out of other people’s money,” said Mr. Jacobs.
Senate Majority Leader Mitch McConnell (R-Ky.) suggested in an Oct. 16 interview with Bloomberg News that entitlement programs like Medicare are “the real driver of the debt by any objective standard,” but that bipartisan cooperation will be needed to address that problem
Republican Mr. Jacobs and Democrat Mr. McDonough think that’s unlikely any time soon.
“Why would Democrats give that up as an issue heading into 2020?” asked Mr. McDonough, especially because Republicans in recent years have been proposing deep cuts to the Medicare program.
Agreed Mr. Jacobs, “Trump may not want that to be the centerpiece of a reelection campaign.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Voters this year have told pollsters in no uncertain terms that health care is important to them. In particular, maintaining insurance protections for preexisting conditions is the top issue to many.
But the results of the midterm elections are likely to have a major impact on a broad array of other health issues that touch every single American. And how those issues are addressed will depend in large part on which party controls the U.S. House and Senate, governors’ mansions, and state legislatures around the country.
All politics is local, and no single race is likely to determine national or even state action. But some key contests can provide something of a barometer of what’s likely to happen – or not happen – over the next 2 years.
For example, keep an eye on Kansas. The razor-tight race for governor could determine whether the state expands Medicaid to all people with low incomes, as allowed under the Affordable Care Act. The legislature in that deep-red state passed a bill to accept expansion in 2017, but it could not override the veto of then-Gov. Sam Brownback. Of the candidates running for governor in 2018, Democrat Laura Kelly supports expansion, while Republican Kris Kobach does not.
Here are three big health issues that could be dramatically affected by Tuesday’s vote.
1. The Affordable Care Act
Protections for preexisting conditions are only a small part of the ACA. The law also made big changes to Medicare and Medicaid, employer-provided health plans, and the generic drug approval process, among other things.
Republicans ran hard on promises to get rid of the law in every election since it passed in 2010. But when the GOP finally got control of the House, the Senate, and the White House in 2017, Republicans found they could not reach agreement on how to “repeal and replace” the law.
This year has Democrats on the attack over the votes Republicans took on various proposals to remake the health law. Probably the most endangered Democrat in the Senate, Heidi Heitkamp of North Dakota, has hammered her Republican opponent, U.S. Rep. Kevin Cramer, over his votes in the House for the unsuccessful repeal-and-replace bills. Rep. Cramer said that despite his votes he supports protections for preexisting conditions, but he has not said what he would do or get behind that could have that effect.
Polls suggest Rep. Cramer has a healthy lead in that race, but if Sen. Heitkamp pulled off a surprise win, health care might well get some of the credit.
And in New Jersey, Rep. Tom MacArthur, the moderate Republican who wrote the language that got the GOP health bill passed in the House in 2017, is in a heated race with Democrat Andy Kim, who has never held elective office. The overriding issue in that race, too, is health care.
It is not just congressional action that has Republicans playing defense on the ACA. In February, 18 GOP attorneys general and 2 GOP governors filed a lawsuit seeking a judgment that the law is now unconstitutional because Congress in the 2017 tax bill repealed the penalty for not having insurance. Two of those attorneys general – Missouri’s Josh Hawley and West Virginia’s Patrick Morrisey – are running for the Senate. Both states overwhelmingly supported President Donald Trump in 2016.
The attorneys general are running against Democratic incumbents – Claire McCaskill of Missouri and Joe Manchin of West Virginia. And both Republicans are being hotly criticized by their opponents for their participation in the lawsuit.
Although Sen. Manchin appears to have taken a lead, the Hawley-McCaskill race is rated a toss-up by political analysts.
But in the end the fate of the ACA depends less on an individual race than on which party winds up in control of Congress.
“If Democrats take the House ... then any attempt at repeal-and-replace will be kaput,” said John McDonough, a former Democratic Senate aide who helped write the ACA and now teaches at the Harvard School of Public Health, Boston.
Conservative health care strategist Chris Jacobs, who worked for Republicans on Capitol Hill, said a new repeal-and-replace effort might not happen even if Republicans are successful Tuesday.
“Republicans, if they maintain the majority in the House, will have a margin of a half-dozen seats – if they are lucky,” he said. That likely would not allow the party to push through another controversial effort to change the law. Currently there are 42 more Republicans than Democrats in the House. Even so, the GOP barely got its health bill passed out of the House in 2017.
And political strategists say that, when the dust clears after voting, the numbers in the Senate may not be much different so change could be hard there too. Republicans, even with a small majority last year, could not pass a repeal bill there.
2. Medicaid expansion
The Supreme Court in 2012 made optional the ACA’s expansion of Medicaid to cover all low-income Americans up to 138% of the poverty line ($16,753 for an individual in 2018). Most states have now expanded, particularly since the federal government is paying the vast majority of the cost: 94% in 2018, gradually dropping to 90% in 2020.
Still, 17 states, all with GOP governors or state legislatures (or both), have yet to expand Medicaid.
Mr. McDonough is confident that’s about to change. “I’m wondering if we’re on the cusp of a Medicaid wave,” he said.
Four states – Idaho, Montana, Nebraska, and Utah – have Medicaid expansion questions on their ballots. All but Montana have yet to expand the program. Montana’s question would eliminate the 2019 sunset date included in its expansion in 2016. But it will be interesting to watch results because the measure has run into big-pocketed opposition: the tobacco industry. The initiative would increase taxes on cigarettes and other tobacco products to fund the state’s increased Medicaid costs.
In Idaho, the ballot measure is being embraced by a number of Republican leaders. GOP Gov. Butch Otter, who is retiring after three terms, endorsed it Oct. 30.
But the issue is in play in other states, too. Several nonexpansion states have close or closer-than-expected races for governor where the Democrat has made Medicaid expansion a priority.
In Florida, one of the largest states not to have expanded Medicaid, the Republican candidate for governor, former U.S. Rep. Ron DeSantis, opposes expansion. His Democratic opponent, Tallahassee Mayor Andrew Gillum, supports it.
In Georgia, the gubernatorial candidates, Democrat Stacey Abrams and Republican Brian Kemp, are also on opposite sides of the Medicaid expansion debate.
However, the legislatures in both states have opposed the expansion, and it’s not clear if they would be swayed by arguments from a new governor.
3. Medicare
Until recently, Republicans have remained relatively quiet about efforts to change the popular Medicare program for seniors and people with disabilities.
Their new talking point is that proposals to expand the program – such as the often-touted “Medicare-for-all,” which an increasing number of Democrats are embracing – could threaten the existing program.
“Medicare is at significant risk of being cut if Democrats take over the House,” Rep. Greg Gianforte (R-Mont.) told the Lee Montana Newspapers. “Medicare-for-all is Medicare for none. It will gut Medicare, end the VA [Department of Veterans Affairs] as we know it, and force Montana seniors to the back of the line.”
Gianforte’s Democratic opponent, Kathleen Williams, is proposing another idea popular with Democrats: allowing people aged 55 years and over to “buy into” Medicare coverage. That race, too, is very tight.
Meanwhile, back in Washington, congressional Republicans are more concerned with how Medicare and other large government social programs are threatening the budget.
“Sooner or later we are going to run out of other people’s money,” said Mr. Jacobs.
Senate Majority Leader Mitch McConnell (R-Ky.) suggested in an Oct. 16 interview with Bloomberg News that entitlement programs like Medicare are “the real driver of the debt by any objective standard,” but that bipartisan cooperation will be needed to address that problem
Republican Mr. Jacobs and Democrat Mr. McDonough think that’s unlikely any time soon.
“Why would Democrats give that up as an issue heading into 2020?” asked Mr. McDonough, especially because Republicans in recent years have been proposing deep cuts to the Medicare program.
Agreed Mr. Jacobs, “Trump may not want that to be the centerpiece of a reelection campaign.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Rate of sling removal 9 years after MUS for SUI over 3%
a British study found.
Ipek Gurol-Urganci, PhD, of the London School of Hygiene and Tropical Medicine, and her coauthors said their study comes as a result of safety concerns around the procedure, which resulted in a suspension of the operation in the United Kingdom.
“There is concern about problems that some women experience following MUS insertion, including pain, dyspareunia, persistent urinary incontinence, and exposure or erosion. However, there is little randomized, clinical trial evidence on these longer-term outcomes,” they wrote in JAMA, noting that an estimated 250,000 MUS operations were performed in 2010 in the United States.
The current study involved 95,057 women in England who underwent an MUS insertion procedure for SUI for the first time in a National Health Service hospital between 2006 and 2015. Overall, 60,194 of the women had a retropubic insertion and 34,863 had a transobturator insertion.
At 9 years after the initial insertion, the mesh was removed in 3.3% of women. The risk of removal was higher for women who had a retropubic insertion (3.6%), compared with those who had a transobturator insertion (2.7%).
“The risk of a removal was about 30% lower if the mesh sling had been inserted via the transobturator route, which may be explained by the removal of transobturator sling being a more complicated procedure,” Dr. Gurol-Urganci and her associates noted.
Mesh sling removal risk decreased with age, with the risk at 4.4% for women aged 18-39 years, compared with 2.1% in women aged 70 years and older at 9 years after insertion.
The authors wrote that the risks of removal and any reoperation (mesh removal and/or reoperation for SUI) were higher among women from a white racial/ethnic background. However, it was not possible to “disentangle explanations” for these possible differences in risk seen with patient characteristics, which ranged from higher morbidity to differences in the reasons for surgery.
Results also showed that the risk of reoperation was 4.5% at 9 years after the initial insertion, and was slightly higher for a transobturator insertion at 5.3%, compared with 4.1% for a retropubic insertion.
The risk of any reoperation, including mesh removal and/or reoperation for SUI, following the initial MUS insertion was 6.9% at 9 years (95% confidence interval, 6.7%-7.1%), but no statistically significant difference was observed between retropubic and transobturator insertion.
“The present results demonstrate that removal and reoperation risks were associated with the insertion route and patient factors,” Dr. Gurol-Urganci and her associates wrote.
“These findings may guide women and their surgeons when making decisions about surgical treatment of stress urinary incontinence,” they concluded.
The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas.
SOURCE: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
a British study found.
Ipek Gurol-Urganci, PhD, of the London School of Hygiene and Tropical Medicine, and her coauthors said their study comes as a result of safety concerns around the procedure, which resulted in a suspension of the operation in the United Kingdom.
“There is concern about problems that some women experience following MUS insertion, including pain, dyspareunia, persistent urinary incontinence, and exposure or erosion. However, there is little randomized, clinical trial evidence on these longer-term outcomes,” they wrote in JAMA, noting that an estimated 250,000 MUS operations were performed in 2010 in the United States.
The current study involved 95,057 women in England who underwent an MUS insertion procedure for SUI for the first time in a National Health Service hospital between 2006 and 2015. Overall, 60,194 of the women had a retropubic insertion and 34,863 had a transobturator insertion.
At 9 years after the initial insertion, the mesh was removed in 3.3% of women. The risk of removal was higher for women who had a retropubic insertion (3.6%), compared with those who had a transobturator insertion (2.7%).
“The risk of a removal was about 30% lower if the mesh sling had been inserted via the transobturator route, which may be explained by the removal of transobturator sling being a more complicated procedure,” Dr. Gurol-Urganci and her associates noted.
Mesh sling removal risk decreased with age, with the risk at 4.4% for women aged 18-39 years, compared with 2.1% in women aged 70 years and older at 9 years after insertion.
The authors wrote that the risks of removal and any reoperation (mesh removal and/or reoperation for SUI) were higher among women from a white racial/ethnic background. However, it was not possible to “disentangle explanations” for these possible differences in risk seen with patient characteristics, which ranged from higher morbidity to differences in the reasons for surgery.
Results also showed that the risk of reoperation was 4.5% at 9 years after the initial insertion, and was slightly higher for a transobturator insertion at 5.3%, compared with 4.1% for a retropubic insertion.
The risk of any reoperation, including mesh removal and/or reoperation for SUI, following the initial MUS insertion was 6.9% at 9 years (95% confidence interval, 6.7%-7.1%), but no statistically significant difference was observed between retropubic and transobturator insertion.
“The present results demonstrate that removal and reoperation risks were associated with the insertion route and patient factors,” Dr. Gurol-Urganci and her associates wrote.
“These findings may guide women and their surgeons when making decisions about surgical treatment of stress urinary incontinence,” they concluded.
The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas.
SOURCE: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
a British study found.
Ipek Gurol-Urganci, PhD, of the London School of Hygiene and Tropical Medicine, and her coauthors said their study comes as a result of safety concerns around the procedure, which resulted in a suspension of the operation in the United Kingdom.
“There is concern about problems that some women experience following MUS insertion, including pain, dyspareunia, persistent urinary incontinence, and exposure or erosion. However, there is little randomized, clinical trial evidence on these longer-term outcomes,” they wrote in JAMA, noting that an estimated 250,000 MUS operations were performed in 2010 in the United States.
The current study involved 95,057 women in England who underwent an MUS insertion procedure for SUI for the first time in a National Health Service hospital between 2006 and 2015. Overall, 60,194 of the women had a retropubic insertion and 34,863 had a transobturator insertion.
At 9 years after the initial insertion, the mesh was removed in 3.3% of women. The risk of removal was higher for women who had a retropubic insertion (3.6%), compared with those who had a transobturator insertion (2.7%).
“The risk of a removal was about 30% lower if the mesh sling had been inserted via the transobturator route, which may be explained by the removal of transobturator sling being a more complicated procedure,” Dr. Gurol-Urganci and her associates noted.
Mesh sling removal risk decreased with age, with the risk at 4.4% for women aged 18-39 years, compared with 2.1% in women aged 70 years and older at 9 years after insertion.
The authors wrote that the risks of removal and any reoperation (mesh removal and/or reoperation for SUI) were higher among women from a white racial/ethnic background. However, it was not possible to “disentangle explanations” for these possible differences in risk seen with patient characteristics, which ranged from higher morbidity to differences in the reasons for surgery.
Results also showed that the risk of reoperation was 4.5% at 9 years after the initial insertion, and was slightly higher for a transobturator insertion at 5.3%, compared with 4.1% for a retropubic insertion.
The risk of any reoperation, including mesh removal and/or reoperation for SUI, following the initial MUS insertion was 6.9% at 9 years (95% confidence interval, 6.7%-7.1%), but no statistically significant difference was observed between retropubic and transobturator insertion.
“The present results demonstrate that removal and reoperation risks were associated with the insertion route and patient factors,” Dr. Gurol-Urganci and her associates wrote.
“These findings may guide women and their surgeons when making decisions about surgical treatment of stress urinary incontinence,” they concluded.
The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas.
SOURCE: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
FROM JAMA
Key clinical point: The findings of this study may inform decision making when choosing treatment for stress urinary incontinence.
Major finding: Within 9 years of a mesh insertion for stress urinary incontinence, the rate of sling removal was 3.3% and the rate of reoperation was 4.5%.
Study details: A prospective, observational study examining long-term mesh removal and reoperations in over 95,000 women who underwent midurethral mesh operations for stress urinary incontinence between 2006 and 2015.
Disclosures: The study was supported by a grant from the National Institute for Health Research Health Services and Delivery Research Programme and several of the authors reported receiving National Institute for Health Research research grants. One author reported providing consultancy services to Cambridge Medical Robotics, Femeda, and Astellas Pharma.
Source: Gurol-Urganci I et al. JAMA. 2018 Oct 23. doi:10.1001/jama.2018.14997.
Quality programs drive improvements in colorectal surgery outcomes
BOSTON – Rates of (ACS NSQIP), a recent analysis shows.
Reoperation rates have also decreased, while early-discharge rates have steadily increased, according to results of the analysis, presented at the annual clinical congress of the American College of Surgeons.
The findings underline the value of such ACS-led initiatives in improving patient care and surgical quality, said Ahmed M. Al-Mazrou, MD, a general surgery resident at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York.
“Over its first decade of introduction, ACS NSQIP was associated with improved outcomes after colorectal surgery, and also introduction of colectomy-targeted data was also associated with improved outcomes,” Dr. Al-Mazrou said in his presentation describing the results.
Prior to this study, the question of whether the introduction of ACS NSQIP has improved outcomes over time had not been well characterized, according to Dr. Al-Mazrou and his colleagues.
To evaluate the impact, the investigators looked at more than 310,000 nonemergency colorectal resections in ACS NSQIP, of which about 58% were done after the introduction of colectomy-targeted variables in 2013.
They found that, over time, incidence of most complications fell, including surgical site infections, urinary tract infections, sepsis and septic shock, and venous thromboembolism, while rates of early discharge increased.
For example, surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Introduction of colectomy-targeted data was associated with fewer surgical site infections (odds ratio, 0.78; 95% confidence interval, 0.77-0.80), multivariable analysis showed. Likewise, there were lower rates of systemic infections (OR, 0.94; 95% CI, 0.91-0.98) and urinary tract infections (OR, 0.70; 95% CI, 0.67-0.74) after introduction of the data.
Rates of reoperation also decreased (OR, 0.88; 95% CI, 0.85-0.91) while early-discharge rates increased (OR, 1.60; 95% CI, 1.57-1.63) after colectomy data was introduced, the multivariable analysis further showed.
Principal investigator P. Ravi Kiran, MD, FACS, professor of surgery at Columbia University and chief of the medical center’s division of colorectal surgery, said the improved outcomes were attributable to a few different factors.
First, the NSQIP national data allows participants to benchmark with peer hospitals and find areas for improvement, Dr. Kiran said in an ACS press release.
That benchmarking encourages participating centers to follow evidence-based recommendations, including ACS guidelines for preventing surgical site infections, he added.
The introduction of procedure-targeted datasets in NSQIP was done in response to user requests for more clinically detailed information, according to Clifford Y. Ko, MD, FACS, director of the ACS division of research and optimal patient care.
While the NSQIP data are important in improving surgical outcomes, credit also goes to the organizations that are leading the quality improvement efforts by effectively using the data, Dr. Ko said in the press release.
Dr. Ko was not involved in the study. Dr. Al-Mazrou and Dr. Kiran reported no disclosures relevant to the study.
SOURCE: Al-Mazrou AM et al. ACS Clinical Congress. Abstract SF330.
BOSTON – Rates of (ACS NSQIP), a recent analysis shows.
Reoperation rates have also decreased, while early-discharge rates have steadily increased, according to results of the analysis, presented at the annual clinical congress of the American College of Surgeons.
The findings underline the value of such ACS-led initiatives in improving patient care and surgical quality, said Ahmed M. Al-Mazrou, MD, a general surgery resident at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York.
“Over its first decade of introduction, ACS NSQIP was associated with improved outcomes after colorectal surgery, and also introduction of colectomy-targeted data was also associated with improved outcomes,” Dr. Al-Mazrou said in his presentation describing the results.
Prior to this study, the question of whether the introduction of ACS NSQIP has improved outcomes over time had not been well characterized, according to Dr. Al-Mazrou and his colleagues.
To evaluate the impact, the investigators looked at more than 310,000 nonemergency colorectal resections in ACS NSQIP, of which about 58% were done after the introduction of colectomy-targeted variables in 2013.
They found that, over time, incidence of most complications fell, including surgical site infections, urinary tract infections, sepsis and septic shock, and venous thromboembolism, while rates of early discharge increased.
For example, surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Introduction of colectomy-targeted data was associated with fewer surgical site infections (odds ratio, 0.78; 95% confidence interval, 0.77-0.80), multivariable analysis showed. Likewise, there were lower rates of systemic infections (OR, 0.94; 95% CI, 0.91-0.98) and urinary tract infections (OR, 0.70; 95% CI, 0.67-0.74) after introduction of the data.
Rates of reoperation also decreased (OR, 0.88; 95% CI, 0.85-0.91) while early-discharge rates increased (OR, 1.60; 95% CI, 1.57-1.63) after colectomy data was introduced, the multivariable analysis further showed.
Principal investigator P. Ravi Kiran, MD, FACS, professor of surgery at Columbia University and chief of the medical center’s division of colorectal surgery, said the improved outcomes were attributable to a few different factors.
First, the NSQIP national data allows participants to benchmark with peer hospitals and find areas for improvement, Dr. Kiran said in an ACS press release.
That benchmarking encourages participating centers to follow evidence-based recommendations, including ACS guidelines for preventing surgical site infections, he added.
The introduction of procedure-targeted datasets in NSQIP was done in response to user requests for more clinically detailed information, according to Clifford Y. Ko, MD, FACS, director of the ACS division of research and optimal patient care.
While the NSQIP data are important in improving surgical outcomes, credit also goes to the organizations that are leading the quality improvement efforts by effectively using the data, Dr. Ko said in the press release.
Dr. Ko was not involved in the study. Dr. Al-Mazrou and Dr. Kiran reported no disclosures relevant to the study.
SOURCE: Al-Mazrou AM et al. ACS Clinical Congress. Abstract SF330.
BOSTON – Rates of (ACS NSQIP), a recent analysis shows.
Reoperation rates have also decreased, while early-discharge rates have steadily increased, according to results of the analysis, presented at the annual clinical congress of the American College of Surgeons.
The findings underline the value of such ACS-led initiatives in improving patient care and surgical quality, said Ahmed M. Al-Mazrou, MD, a general surgery resident at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York.
“Over its first decade of introduction, ACS NSQIP was associated with improved outcomes after colorectal surgery, and also introduction of colectomy-targeted data was also associated with improved outcomes,” Dr. Al-Mazrou said in his presentation describing the results.
Prior to this study, the question of whether the introduction of ACS NSQIP has improved outcomes over time had not been well characterized, according to Dr. Al-Mazrou and his colleagues.
To evaluate the impact, the investigators looked at more than 310,000 nonemergency colorectal resections in ACS NSQIP, of which about 58% were done after the introduction of colectomy-targeted variables in 2013.
They found that, over time, incidence of most complications fell, including surgical site infections, urinary tract infections, sepsis and septic shock, and venous thromboembolism, while rates of early discharge increased.
For example, surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Introduction of colectomy-targeted data was associated with fewer surgical site infections (odds ratio, 0.78; 95% confidence interval, 0.77-0.80), multivariable analysis showed. Likewise, there were lower rates of systemic infections (OR, 0.94; 95% CI, 0.91-0.98) and urinary tract infections (OR, 0.70; 95% CI, 0.67-0.74) after introduction of the data.
Rates of reoperation also decreased (OR, 0.88; 95% CI, 0.85-0.91) while early-discharge rates increased (OR, 1.60; 95% CI, 1.57-1.63) after colectomy data was introduced, the multivariable analysis further showed.
Principal investigator P. Ravi Kiran, MD, FACS, professor of surgery at Columbia University and chief of the medical center’s division of colorectal surgery, said the improved outcomes were attributable to a few different factors.
First, the NSQIP national data allows participants to benchmark with peer hospitals and find areas for improvement, Dr. Kiran said in an ACS press release.
That benchmarking encourages participating centers to follow evidence-based recommendations, including ACS guidelines for preventing surgical site infections, he added.
The introduction of procedure-targeted datasets in NSQIP was done in response to user requests for more clinically detailed information, according to Clifford Y. Ko, MD, FACS, director of the ACS division of research and optimal patient care.
While the NSQIP data are important in improving surgical outcomes, credit also goes to the organizations that are leading the quality improvement efforts by effectively using the data, Dr. Ko said in the press release.
Dr. Ko was not involved in the study. Dr. Al-Mazrou and Dr. Kiran reported no disclosures relevant to the study.
SOURCE: Al-Mazrou AM et al. ACS Clinical Congress. Abstract SF330.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point: Rates of colorectal procedure complications have steadily decreased since the introduction of the American College of Surgeons National Surgical Quality Improvement Program.
Major finding: Surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Study details: Retrospective review of more than 310,000 nonemergency colorectal resections in ACS NSQIP from 2007 to 2016.
Disclosures: Study authors reported no conflicts of interest.
Source: Al-Mazrou AM et al. ACS Clinical Congress, Abstract SF330.
With midterm elections near, PhRMA continues to spend
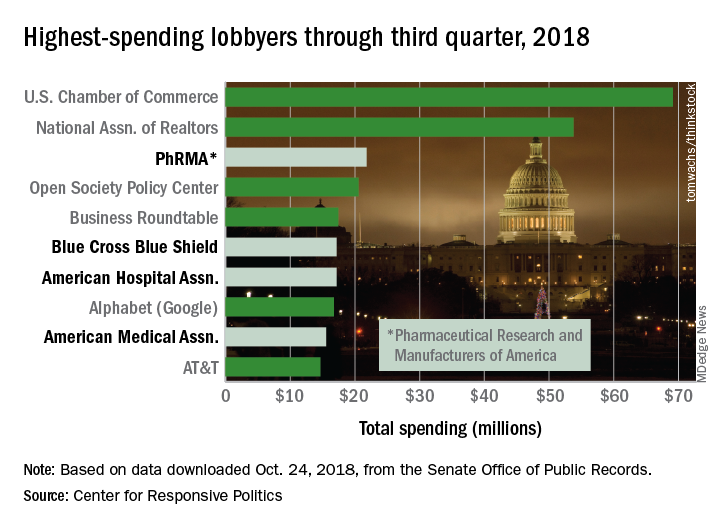
PhRMA’s $21.8 million worth of lobbying through September put it ahead of Blue Cross Blue Shield’s $17.2 million. PhRMA remains on pace to exceed its previous spending high of $27.2 million in 2009, and the health sector as a whole, with a lobbying bill of $421.5 million for three-quarters of 2018, is just slightly ahead of last year’s record of $561.3 million, the center reported on OpenSecrets.org.
PhRMA is third overall in lobbying spending so far this year, behind the U.S. Chamber of Commerce ($69.1 million) and the National Association of Realtors ($53.8 million). Blue Cross Blue Shield is sixth overall, with the American Hospital Association ($17.2 million, seventh) and the American Medical Association ($15.5 million, ninth) also in the top 10, according to the center’s analysis of data from the Senate Office of Public Records.
The pharmaceutical/health product industry leads health-sector lobbying with $216.1 million in spending so far in 2018, followed by hospitals/nursing homes at $73.6 million, health professionals at $68.6 million, and health services/HMOs at $57.5 million.
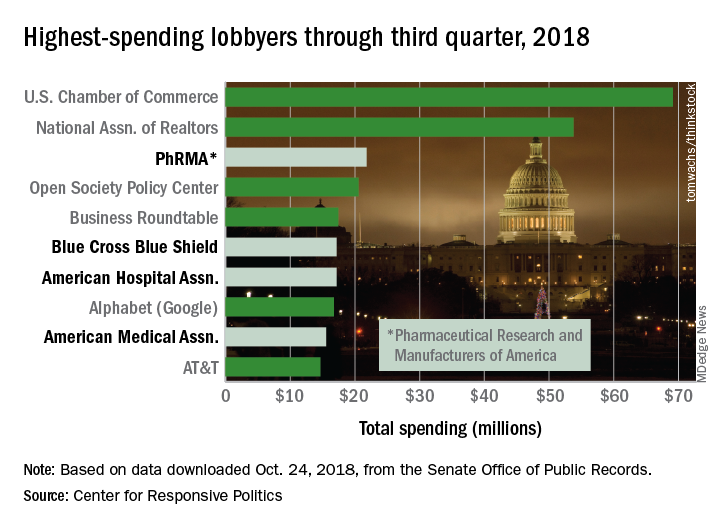
PhRMA’s $21.8 million worth of lobbying through September put it ahead of Blue Cross Blue Shield’s $17.2 million. PhRMA remains on pace to exceed its previous spending high of $27.2 million in 2009, and the health sector as a whole, with a lobbying bill of $421.5 million for three-quarters of 2018, is just slightly ahead of last year’s record of $561.3 million, the center reported on OpenSecrets.org.
PhRMA is third overall in lobbying spending so far this year, behind the U.S. Chamber of Commerce ($69.1 million) and the National Association of Realtors ($53.8 million). Blue Cross Blue Shield is sixth overall, with the American Hospital Association ($17.2 million, seventh) and the American Medical Association ($15.5 million, ninth) also in the top 10, according to the center’s analysis of data from the Senate Office of Public Records.
The pharmaceutical/health product industry leads health-sector lobbying with $216.1 million in spending so far in 2018, followed by hospitals/nursing homes at $73.6 million, health professionals at $68.6 million, and health services/HMOs at $57.5 million.
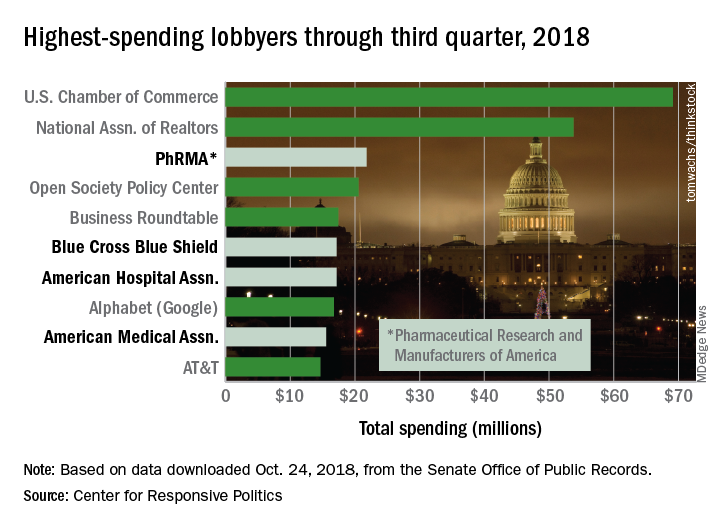
PhRMA’s $21.8 million worth of lobbying through September put it ahead of Blue Cross Blue Shield’s $17.2 million. PhRMA remains on pace to exceed its previous spending high of $27.2 million in 2009, and the health sector as a whole, with a lobbying bill of $421.5 million for three-quarters of 2018, is just slightly ahead of last year’s record of $561.3 million, the center reported on OpenSecrets.org.
PhRMA is third overall in lobbying spending so far this year, behind the U.S. Chamber of Commerce ($69.1 million) and the National Association of Realtors ($53.8 million). Blue Cross Blue Shield is sixth overall, with the American Hospital Association ($17.2 million, seventh) and the American Medical Association ($15.5 million, ninth) also in the top 10, according to the center’s analysis of data from the Senate Office of Public Records.
The pharmaceutical/health product industry leads health-sector lobbying with $216.1 million in spending so far in 2018, followed by hospitals/nursing homes at $73.6 million, health professionals at $68.6 million, and health services/HMOs at $57.5 million.
'Liver first' for select stage IV colon cancer gaining traction
BOSTON –
It’s an alternative to usual care, meaning simultaneous bowel and liver resection or bowel resection with liver surgery later on.
Systemic chemotherapy comes first, followed by liver resection. If margins are microscopically negative, the patient gets another round of chemotherapy. If no additional lesions emerge, the primary tumor is taken out. The entire process can take up to a year.
The approach was developed in the Netherlands for rectal cancer with advanced liver metastases. The idea was to get the liver lesions out before they became unresectable, then remove the primary tumor later on. It’s gaining traction now for colon cancer, and beginning to trickle into the United States at a few academic medical centers.
It comes down to what’s more dangerous, the metastases or the primary tumor? Tumor science hasn’t answered that question yet. There’s general agreement that metastases are what kill people with cancer, but it’s not known if they come mostly from previous metastases or from the primary tumor. The liver-first approach assumes the former.
Liver-first is “extremely controversial. For older surgeons who are not in tertiary care centers, liver-first doesn’t make sense, and it doesn’t seem to make sense to patients. They wonder why you would go after the liver when they were diagnosed with a colon tumor,” said Janice Rafferty, MD, FACS, professor of surgery at the University of Cincinnati, at the annual clinical congress of the American College of Surgeons.
“Well, it’s because the primary tumor doesn’t limit your life,” she continued. “The life-limiting disease is in the liver, not the colon. If you explain it to them that way, it makes sense. If we cannot get an R0 resection on the liver, it doesn’t make sense to go after the primary, unless it’s symptomatic with obstruction, bleeding, or fistula.”
There have been about 10 attempts at a randomized trial of this approach versus usual care, but they were not successful because of the difficulty of recruiting patients. Patients – and no doubt, some surgeons – may have some resistance to the logic of going after metastases first.
Dr. Rafferty moderated a review of research from Yale University, New Haven, Conn., that attempted to plug the evidence gap. The Yale investigators “presented really interesting data that shows that liver-first has improved survival,” she said.
The Yale team used the National Cancer Database to compare 2010-2015 outcomes from liver-first patients with patients who had simultaneous or bowel-first resections, followed by later liver resections. The database didn’t allow them to tease out simultaneous from bowel-first cases, so they lumped them together as usual care. To avoid confounding, rectal carcinomas and metastases to the lung, brain, and other organs were excluded.
Median survival was 34 months among 358 liver-first patients versus 24 months among 18,042 usual care patients in an intention-to-treat analysis. Among patients who completed their resections, median survival was 57 months among 140 liver-first patients versus 36 months with usual care in 3,988.
The benefit held after adjustment for patient and tumor characteristics (hazard ratio for death 0.77 in favor of liver first). When further adjusted for chemotherapy timing, there was a strong trend for liver-first but it was not statistically significant, suggesting that up-front chemotherapy contributed to the results (HR, 0.88; 95% confidence interval, 0.75-1.01; P = .09).
There were many caveats. The liver-first patients were younger, with over half under the age of 60 years versus just over 40% in usual care. They were also healthier based on Charlson comorbidity scores and more likely to have upfront chemotherapy and be treated at an academic center.
So, what should surgeons make of these findings? Lead investigator Vadim Kurbatov, MD, a Yale surgery resident, argued that, at the very least, they suggest that liver-first is a viable option for stage IV colon cancer with isolated liver metastases. Going further, they suggest that liver first may be the right way to go for younger, healthier patients at academic centers.
For sicker stage IV patients, however, the role of liver-first is unclear. “We really do need a randomized trial,” he said.
Dr. Kurbatov and Dr. Rafferty had no relevant disclosures to report. The work was funded in part by the National Institutes of Health.
BOSTON –
It’s an alternative to usual care, meaning simultaneous bowel and liver resection or bowel resection with liver surgery later on.
Systemic chemotherapy comes first, followed by liver resection. If margins are microscopically negative, the patient gets another round of chemotherapy. If no additional lesions emerge, the primary tumor is taken out. The entire process can take up to a year.
The approach was developed in the Netherlands for rectal cancer with advanced liver metastases. The idea was to get the liver lesions out before they became unresectable, then remove the primary tumor later on. It’s gaining traction now for colon cancer, and beginning to trickle into the United States at a few academic medical centers.
It comes down to what’s more dangerous, the metastases or the primary tumor? Tumor science hasn’t answered that question yet. There’s general agreement that metastases are what kill people with cancer, but it’s not known if they come mostly from previous metastases or from the primary tumor. The liver-first approach assumes the former.
Liver-first is “extremely controversial. For older surgeons who are not in tertiary care centers, liver-first doesn’t make sense, and it doesn’t seem to make sense to patients. They wonder why you would go after the liver when they were diagnosed with a colon tumor,” said Janice Rafferty, MD, FACS, professor of surgery at the University of Cincinnati, at the annual clinical congress of the American College of Surgeons.
“Well, it’s because the primary tumor doesn’t limit your life,” she continued. “The life-limiting disease is in the liver, not the colon. If you explain it to them that way, it makes sense. If we cannot get an R0 resection on the liver, it doesn’t make sense to go after the primary, unless it’s symptomatic with obstruction, bleeding, or fistula.”
There have been about 10 attempts at a randomized trial of this approach versus usual care, but they were not successful because of the difficulty of recruiting patients. Patients – and no doubt, some surgeons – may have some resistance to the logic of going after metastases first.
Dr. Rafferty moderated a review of research from Yale University, New Haven, Conn., that attempted to plug the evidence gap. The Yale investigators “presented really interesting data that shows that liver-first has improved survival,” she said.
The Yale team used the National Cancer Database to compare 2010-2015 outcomes from liver-first patients with patients who had simultaneous or bowel-first resections, followed by later liver resections. The database didn’t allow them to tease out simultaneous from bowel-first cases, so they lumped them together as usual care. To avoid confounding, rectal carcinomas and metastases to the lung, brain, and other organs were excluded.
Median survival was 34 months among 358 liver-first patients versus 24 months among 18,042 usual care patients in an intention-to-treat analysis. Among patients who completed their resections, median survival was 57 months among 140 liver-first patients versus 36 months with usual care in 3,988.
The benefit held after adjustment for patient and tumor characteristics (hazard ratio for death 0.77 in favor of liver first). When further adjusted for chemotherapy timing, there was a strong trend for liver-first but it was not statistically significant, suggesting that up-front chemotherapy contributed to the results (HR, 0.88; 95% confidence interval, 0.75-1.01; P = .09).
There were many caveats. The liver-first patients were younger, with over half under the age of 60 years versus just over 40% in usual care. They were also healthier based on Charlson comorbidity scores and more likely to have upfront chemotherapy and be treated at an academic center.
So, what should surgeons make of these findings? Lead investigator Vadim Kurbatov, MD, a Yale surgery resident, argued that, at the very least, they suggest that liver-first is a viable option for stage IV colon cancer with isolated liver metastases. Going further, they suggest that liver first may be the right way to go for younger, healthier patients at academic centers.
For sicker stage IV patients, however, the role of liver-first is unclear. “We really do need a randomized trial,” he said.
Dr. Kurbatov and Dr. Rafferty had no relevant disclosures to report. The work was funded in part by the National Institutes of Health.
BOSTON –
It’s an alternative to usual care, meaning simultaneous bowel and liver resection or bowel resection with liver surgery later on.
Systemic chemotherapy comes first, followed by liver resection. If margins are microscopically negative, the patient gets another round of chemotherapy. If no additional lesions emerge, the primary tumor is taken out. The entire process can take up to a year.
The approach was developed in the Netherlands for rectal cancer with advanced liver metastases. The idea was to get the liver lesions out before they became unresectable, then remove the primary tumor later on. It’s gaining traction now for colon cancer, and beginning to trickle into the United States at a few academic medical centers.
It comes down to what’s more dangerous, the metastases or the primary tumor? Tumor science hasn’t answered that question yet. There’s general agreement that metastases are what kill people with cancer, but it’s not known if they come mostly from previous metastases or from the primary tumor. The liver-first approach assumes the former.
Liver-first is “extremely controversial. For older surgeons who are not in tertiary care centers, liver-first doesn’t make sense, and it doesn’t seem to make sense to patients. They wonder why you would go after the liver when they were diagnosed with a colon tumor,” said Janice Rafferty, MD, FACS, professor of surgery at the University of Cincinnati, at the annual clinical congress of the American College of Surgeons.
“Well, it’s because the primary tumor doesn’t limit your life,” she continued. “The life-limiting disease is in the liver, not the colon. If you explain it to them that way, it makes sense. If we cannot get an R0 resection on the liver, it doesn’t make sense to go after the primary, unless it’s symptomatic with obstruction, bleeding, or fistula.”
There have been about 10 attempts at a randomized trial of this approach versus usual care, but they were not successful because of the difficulty of recruiting patients. Patients – and no doubt, some surgeons – may have some resistance to the logic of going after metastases first.
Dr. Rafferty moderated a review of research from Yale University, New Haven, Conn., that attempted to plug the evidence gap. The Yale investigators “presented really interesting data that shows that liver-first has improved survival,” she said.
The Yale team used the National Cancer Database to compare 2010-2015 outcomes from liver-first patients with patients who had simultaneous or bowel-first resections, followed by later liver resections. The database didn’t allow them to tease out simultaneous from bowel-first cases, so they lumped them together as usual care. To avoid confounding, rectal carcinomas and metastases to the lung, brain, and other organs were excluded.
Median survival was 34 months among 358 liver-first patients versus 24 months among 18,042 usual care patients in an intention-to-treat analysis. Among patients who completed their resections, median survival was 57 months among 140 liver-first patients versus 36 months with usual care in 3,988.
The benefit held after adjustment for patient and tumor characteristics (hazard ratio for death 0.77 in favor of liver first). When further adjusted for chemotherapy timing, there was a strong trend for liver-first but it was not statistically significant, suggesting that up-front chemotherapy contributed to the results (HR, 0.88; 95% confidence interval, 0.75-1.01; P = .09).
There were many caveats. The liver-first patients were younger, with over half under the age of 60 years versus just over 40% in usual care. They were also healthier based on Charlson comorbidity scores and more likely to have upfront chemotherapy and be treated at an academic center.
So, what should surgeons make of these findings? Lead investigator Vadim Kurbatov, MD, a Yale surgery resident, argued that, at the very least, they suggest that liver-first is a viable option for stage IV colon cancer with isolated liver metastases. Going further, they suggest that liver first may be the right way to go for younger, healthier patients at academic centers.
For sicker stage IV patients, however, the role of liver-first is unclear. “We really do need a randomized trial,” he said.
Dr. Kurbatov and Dr. Rafferty had no relevant disclosures to report. The work was funded in part by the National Institutes of Health.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point: The liver-first approach may be appropriate for younger, healthier patients at academic centers.
Major finding: Median survival was 34 months among 358 liver-first patients versus 24 months among 18,042 usual care patients in an intention-to-treat analysis.
Study details: A review of over 18,000 patients in the National Cancer Database
Disclosures: The lead investigator had no disclosures to report. The work was funded in part by the National Institutes of Health.
How to use transgastric necrosectomy for midline pancreatitis
BOSTON – When pancreatitis symptoms don’t resolve within a month, patients need some sort of surgical intervention, according to Steven Hughes, MD, FACS, professor and chief of surgical oncology at the University of Florida, Gainesville.
Pancreatitis management has been evolving in recent years. Prophylactic antibiotics and total parenteral nutrition are out; tube feeds are in, and there’s compelling evidence to take the gallbladder out, regardless of etiology, he said at the annual clinical congress of the American College of Surgeons.
However, too many patients get drains placed in the first 2 weeks; it’s the wrong move because it consigns to surgery a lot of patients who otherwise would have recovered on their own. “In the first 2 weeks, please do not place drains. Once you place the drain, you have committed the patient to a very different clinical course,” Dr. Hughes said.
Surgery generally comes a month or more after the initial presentation. Infection is inevitable at that point; the delay gives the lesion time to consolidate and wall itself off, making for a cleaner, safer operation.
It’s Dr. Hughes’s favored approach when the anatomy is appropriate; he shared his thoughts at the meeting.
Transgastric necrosectomy provides “single-stop shopping. You can get a thorough debridement in a single procedure,” and durable internal drainage. “Most importantly, from a patient’s perspective, it leaves them without external drains. You can transition a patient who’s been percutaneously drained to no external drainage at the time of this operation,” he said.
Additional pluses include cholecystectomy either before or after necrosectomy and the ability to place enteric feeding systems. “I like to use a combination G-J tube that allows drainage of the emptying stomach along with distal tube feeds,” he said.
Laparoscopic and endoscopic approaches are possible, but Dr. Hughes favors an open procedure “because the finger is the best debriding tool I have found.” There’s an anterior and then posterior gastric incision to dig out the necroma. The anterior incision is closed, but the posterior cut is sealed open to the necroma with a running hemostatic suture to allow for a “large cavity between the cavity and the stomach” for ongoing drainage.
“I have ultrasound on the field, but typically finding the necroma is like falling out of a canoe and finding water.” Even so, “I like to bring a 10-mm straight scope for direct viewing onto the field to explore the necrotic cavity and ensure I’ve done an adequate necrosectomy,” he said.
“I do think that this operation can be performed in patients who have some retrocolic extension even over into the pancreatic head and down the right paracolic gutter, but certainly if the collection extends down towards the pelvis, the notion that this is going to be adequate in and of itself requires further investigation,” he said.
In a cohort of 18 patients he and his colleagues followed for at least 2 years, “I was impressed that this operation is rather durable,” with rapid resolution of disease, Dr. Hughes said. Just a couple people needed additional operations. “The majority created persistent fistulas between the pancreatic body tail and the stomach.”
He cautioned that the procedure “is not for the faint of heart. The splenic vein and the splenic artery as well the celiac axis and portal vein are at risk during this procedure, and if you get into them, you have got a wolf by both ears. I would encourage you to consider referral for these patients.”
Dr. Hughes strongly encouraged surgeons to “ make sure your interventional radiologists and advanced endoscopists are on board, whether for the postop pseudoaneurysm bleeding or recurrent sepsis.”
Dr. Hughes had no relevant disclosures to report.
BOSTON – When pancreatitis symptoms don’t resolve within a month, patients need some sort of surgical intervention, according to Steven Hughes, MD, FACS, professor and chief of surgical oncology at the University of Florida, Gainesville.
Pancreatitis management has been evolving in recent years. Prophylactic antibiotics and total parenteral nutrition are out; tube feeds are in, and there’s compelling evidence to take the gallbladder out, regardless of etiology, he said at the annual clinical congress of the American College of Surgeons.
However, too many patients get drains placed in the first 2 weeks; it’s the wrong move because it consigns to surgery a lot of patients who otherwise would have recovered on their own. “In the first 2 weeks, please do not place drains. Once you place the drain, you have committed the patient to a very different clinical course,” Dr. Hughes said.
Surgery generally comes a month or more after the initial presentation. Infection is inevitable at that point; the delay gives the lesion time to consolidate and wall itself off, making for a cleaner, safer operation.
It’s Dr. Hughes’s favored approach when the anatomy is appropriate; he shared his thoughts at the meeting.
Transgastric necrosectomy provides “single-stop shopping. You can get a thorough debridement in a single procedure,” and durable internal drainage. “Most importantly, from a patient’s perspective, it leaves them without external drains. You can transition a patient who’s been percutaneously drained to no external drainage at the time of this operation,” he said.
Additional pluses include cholecystectomy either before or after necrosectomy and the ability to place enteric feeding systems. “I like to use a combination G-J tube that allows drainage of the emptying stomach along with distal tube feeds,” he said.
Laparoscopic and endoscopic approaches are possible, but Dr. Hughes favors an open procedure “because the finger is the best debriding tool I have found.” There’s an anterior and then posterior gastric incision to dig out the necroma. The anterior incision is closed, but the posterior cut is sealed open to the necroma with a running hemostatic suture to allow for a “large cavity between the cavity and the stomach” for ongoing drainage.
“I have ultrasound on the field, but typically finding the necroma is like falling out of a canoe and finding water.” Even so, “I like to bring a 10-mm straight scope for direct viewing onto the field to explore the necrotic cavity and ensure I’ve done an adequate necrosectomy,” he said.
“I do think that this operation can be performed in patients who have some retrocolic extension even over into the pancreatic head and down the right paracolic gutter, but certainly if the collection extends down towards the pelvis, the notion that this is going to be adequate in and of itself requires further investigation,” he said.
In a cohort of 18 patients he and his colleagues followed for at least 2 years, “I was impressed that this operation is rather durable,” with rapid resolution of disease, Dr. Hughes said. Just a couple people needed additional operations. “The majority created persistent fistulas between the pancreatic body tail and the stomach.”
He cautioned that the procedure “is not for the faint of heart. The splenic vein and the splenic artery as well the celiac axis and portal vein are at risk during this procedure, and if you get into them, you have got a wolf by both ears. I would encourage you to consider referral for these patients.”
Dr. Hughes strongly encouraged surgeons to “ make sure your interventional radiologists and advanced endoscopists are on board, whether for the postop pseudoaneurysm bleeding or recurrent sepsis.”
Dr. Hughes had no relevant disclosures to report.
BOSTON – When pancreatitis symptoms don’t resolve within a month, patients need some sort of surgical intervention, according to Steven Hughes, MD, FACS, professor and chief of surgical oncology at the University of Florida, Gainesville.
Pancreatitis management has been evolving in recent years. Prophylactic antibiotics and total parenteral nutrition are out; tube feeds are in, and there’s compelling evidence to take the gallbladder out, regardless of etiology, he said at the annual clinical congress of the American College of Surgeons.
However, too many patients get drains placed in the first 2 weeks; it’s the wrong move because it consigns to surgery a lot of patients who otherwise would have recovered on their own. “In the first 2 weeks, please do not place drains. Once you place the drain, you have committed the patient to a very different clinical course,” Dr. Hughes said.
Surgery generally comes a month or more after the initial presentation. Infection is inevitable at that point; the delay gives the lesion time to consolidate and wall itself off, making for a cleaner, safer operation.
It’s Dr. Hughes’s favored approach when the anatomy is appropriate; he shared his thoughts at the meeting.
Transgastric necrosectomy provides “single-stop shopping. You can get a thorough debridement in a single procedure,” and durable internal drainage. “Most importantly, from a patient’s perspective, it leaves them without external drains. You can transition a patient who’s been percutaneously drained to no external drainage at the time of this operation,” he said.
Additional pluses include cholecystectomy either before or after necrosectomy and the ability to place enteric feeding systems. “I like to use a combination G-J tube that allows drainage of the emptying stomach along with distal tube feeds,” he said.
Laparoscopic and endoscopic approaches are possible, but Dr. Hughes favors an open procedure “because the finger is the best debriding tool I have found.” There’s an anterior and then posterior gastric incision to dig out the necroma. The anterior incision is closed, but the posterior cut is sealed open to the necroma with a running hemostatic suture to allow for a “large cavity between the cavity and the stomach” for ongoing drainage.
“I have ultrasound on the field, but typically finding the necroma is like falling out of a canoe and finding water.” Even so, “I like to bring a 10-mm straight scope for direct viewing onto the field to explore the necrotic cavity and ensure I’ve done an adequate necrosectomy,” he said.
“I do think that this operation can be performed in patients who have some retrocolic extension even over into the pancreatic head and down the right paracolic gutter, but certainly if the collection extends down towards the pelvis, the notion that this is going to be adequate in and of itself requires further investigation,” he said.
In a cohort of 18 patients he and his colleagues followed for at least 2 years, “I was impressed that this operation is rather durable,” with rapid resolution of disease, Dr. Hughes said. Just a couple people needed additional operations. “The majority created persistent fistulas between the pancreatic body tail and the stomach.”
He cautioned that the procedure “is not for the faint of heart. The splenic vein and the splenic artery as well the celiac axis and portal vein are at risk during this procedure, and if you get into them, you have got a wolf by both ears. I would encourage you to consider referral for these patients.”
Dr. Hughes strongly encouraged surgeons to “ make sure your interventional radiologists and advanced endoscopists are on board, whether for the postop pseudoaneurysm bleeding or recurrent sepsis.”
Dr. Hughes had no relevant disclosures to report.
EXPERT ANALYSIS FROM THE ACS CLINICAL CONGRESS
Cervical cancer survival higher with open surgery in LACC trial
based on findings from the randomized, controlled phase 3 Laparoscopic Approach to Cervical Cancer (LACC) trial of more than 600 women.

The alarming findings, which led to early study termination, also were supported by results from a second population-based study. Both studies were published concurrently in the Oct. 31 issue of the New England Journal of Medicine.
The disease-free survival at 4.5 years among 319 patients who underwent minimally invasive surgery in the LACC trial was 86.0% vs. 96.5% in 312 patients who underwent open surgery, Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395).
At 3 years, the disease-free survival rates were 91.2% in the minimally invasive surgery group and 97.1% in open surgery group (hazard ratio for disease recurrence or death from cervical cancer, 3.74).
The differences between the groups persisted after adjustment for age, body mass index, disease stage, lymphovascular invasion, and lymph-node involvement. In the minimally invasive surgery group, the findings were comparable for those who underwent laparoscopic vs. robot-assisted surgery, the investigators found.
Further, at 3 years, overall survival was 93.8% vs. 99.0% (HR for death from any cause, 6.00), death from cervical cancer was 4.4% vs. 0.6% (HR, 6.56), and the rate of locoregional recurrence-free survival was 94.3 vs. 98.3 (HR, 4.26) in the minimally invasive and open surgery groups, respectively.
Study participants were women with a mean age of 46 years with stage IA1, IA2, or IB1 cervical cancer, with most (91.9%) having IB1 disease, and either squamous-cell carcinoma, adenocarcinoma, or adenosquamous carcinoma. They were recruited from 33 centers worldwide between June 2008 and June 2017. Most of those assigned to minimally invasive surgery underwent laparoscopic surgery (84.4%), and the remaining patients underwent robot-assisted surgery.
The treatment groups were balanced with respect to baseline characteristics, they noted.
The minimally invasive approach is widely used given that guidelines from the National Comprehensive Cancer Network and European Society of Gynecological Oncology consider both surgical approaches acceptable, and since retrospective studies suggest laparoscopic radical hysterectomy is associated with lower complication rates and comparable outcomes. However, there are limited prospective data regarding survival outcomes in early stage disease with the two approaches, the researchers said.
“Our results call into question the findings in the literature suggesting that minimally invasive radical hysterectomy is associated with no difference in oncologic outcomes as compared with the open approach,” they wrote, noting that a number of factors may explain the differences, such as concurrent vs. sequential analyses in the current studies vs. prior studies (in sequential analyses, earlier procedures may have been performed under broader indications and less clearly defined radiotherapy guidelines), and the possibility that “routine use of a uterine manipulator might increase the propensity for tumor spillage” in minimally invasive surgery.
Strengths of the study include its prospective, randomized, international multicenter design and inclusion of a per-protocol analysis that was consistent with the intention-to-treat analysis, and limitations include the fact that intended enrollment wasn’t reached because of the “safety alert raised by the data and safety monitoring committee on the basis of the higher recurrence and death in the minimally invasive surgery groups,” as well as the inability to generalize the results to patients with low-risk disease as there was lack of power to evaluate outcomes in that context.
Even though the trial was initially powered on the assumption that there would be a 4.5 year follow-up for all patients, only 59.7% reached that length of follow-up. However, the trial still reached 84% power to detect noninferiority of the primary outcome (disease-free survival) with minimally invasive surgery, which was not found, they noted.
Similarly, in the population-based cohort study of 2,461 women who underwent radical hysterectomy for stage IA2 of IB1 cervical cancer between 2010 and 2013, 4-year mortality was 9.1% among 1,225 patients who underwent minimally invasive surgery vs. 5.3% among the 1,236 patients who underwent open surgery (HR, 1.65), Alexander Melamed, MD, of Harvard Medical School, Boston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1804923).
Of note, the 4-year relative survival rate following radical hysterectomy for cervical cancer remained stable prior to the widespread adoption of minimally invasive approaches; an interrupted time-series analysis involving women who underwent surgery during 2000-2010, which was also conducted as part of the study, showed a decline in 4-year survival of 0.8% per year after 2006, coinciding with increased use of minimally invasive surgery, the investigators said.
For the main patient-level analysis, the researchers used the National Cancer Database, and for the time-series analysis they used information from the Surveillance, Epidemiology, and End Results program database.
“Our findings suggest that minimally invasive surgery was associated with a higher risk of death than open surgery among women who underwent radical hysterectomy for early-stage cervical cancer. This association was apparent regardless of laparoscopic approach, tumor size, or histologic type,” they concluded.
The findings are unexpected, eye-opening, and should inform practice, according to Ritu Salani, MD, of the Ohio State University, Columbus.
“This is something we have to discuss with patients,” she said in an interview, noting that while these aren’t perfect studies, they “are the best information we have.
Data reported in September at a meeting of the International Gynecologic Cancer Society show that surgical complications and quality of life outcomes are similar with minimally invasive and open surgery, therefore the findings from these two new studies suggest a need to shift back toward open surgery for patients with cervical cancer, she said.
One “catch” is that survival in the open surgery group in the LACC trial was unusually high and recurrence rates unusually low, compared with what might be expected, and the explanation for this observation is unclear.
“There may be some missing pieces that they haven’t been able to explain, but it’s not clear that they would change the outcome,” she said.
Justin Chura, MD, director of gynecologic oncology and robotic surgery at Cancer Treatment Center of America’s Eastern Regional Medical Center in Philadelphia, said in an interview, “The results of the study by Ramirez et al. are certainly disappointing for those among us who are advocates of minimally invasive surgery (MIS). In my own practice, I transitioned to minimally invasive radical hysterectomy approximately 10 years ago. Now that approach has to be reconsidered. While there are likely subsets of patients who will still benefit from a MIS approach without worsening oncologic outcomes, we do not have robust data to reliably identify those patients.
“One factor that warrants further investigation is the use of a uterine manipulator. While I do not use a manipulator out of personal preference (one less step in the operating room), the idea of placing a device through the tumor or adjacent to it, has biologic plausibility in terms of displacing tumor cells into lymphatic channels,” he said. “Until we have more data, an open approach appears to be preferred.”*
Dr. Ramirez and Dr. Melamed each reported having no relevant disclosures. Dr. Salani and Dr. Chura are members of the Ob.Gyn. News editorial board, but reported having no other relevant disclosures.*
SOURCE: Ramirez P. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
*This article was updated 11/9/2018.
The findings by Ramirez et al. and Melamed et al. are striking in part because previous studies focused more on surgical than clinical outcomes.
They are powerful, but scientific scrutiny demands consideration of potential study-design or study-conduct issues. For example, all cancer recurrences in the LACC trial were clustered at 14 of 33 participating centers, raising questions about factors that contributed to recurrence at those centers .
Still, the findings are alarming and deal a blow to the use of minimally invasive surgical approaches in cervical cancer patients. They don’t necessarily “signal the death knell” of such approaches.
Select patients may still benefit from a less invasive approach; none of the patients with stage lA2 disease, and only one with stage lB1, grade 1 disease had a recurrence in the LACC trial.
Further, patients with tumors smaller than 2 cm also did not have worse outcomes with minimally invasive surgery in either study. However, until further details are known, surgeons should proceed cautiously and counsel patients regarding these study results.
Amanda N. Fader, MD , made her comments in an accompanying editorial (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395 ). Dr. Fader is with the Johns Hopkins University, Baltimore. She reported having no relevant disclosures.
The findings by Ramirez et al. and Melamed et al. are striking in part because previous studies focused more on surgical than clinical outcomes.
They are powerful, but scientific scrutiny demands consideration of potential study-design or study-conduct issues. For example, all cancer recurrences in the LACC trial were clustered at 14 of 33 participating centers, raising questions about factors that contributed to recurrence at those centers .
Still, the findings are alarming and deal a blow to the use of minimally invasive surgical approaches in cervical cancer patients. They don’t necessarily “signal the death knell” of such approaches.
Select patients may still benefit from a less invasive approach; none of the patients with stage lA2 disease, and only one with stage lB1, grade 1 disease had a recurrence in the LACC trial.
Further, patients with tumors smaller than 2 cm also did not have worse outcomes with minimally invasive surgery in either study. However, until further details are known, surgeons should proceed cautiously and counsel patients regarding these study results.
Amanda N. Fader, MD , made her comments in an accompanying editorial (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395 ). Dr. Fader is with the Johns Hopkins University, Baltimore. She reported having no relevant disclosures.
The findings by Ramirez et al. and Melamed et al. are striking in part because previous studies focused more on surgical than clinical outcomes.
They are powerful, but scientific scrutiny demands consideration of potential study-design or study-conduct issues. For example, all cancer recurrences in the LACC trial were clustered at 14 of 33 participating centers, raising questions about factors that contributed to recurrence at those centers .
Still, the findings are alarming and deal a blow to the use of minimally invasive surgical approaches in cervical cancer patients. They don’t necessarily “signal the death knell” of such approaches.
Select patients may still benefit from a less invasive approach; none of the patients with stage lA2 disease, and only one with stage lB1, grade 1 disease had a recurrence in the LACC trial.
Further, patients with tumors smaller than 2 cm also did not have worse outcomes with minimally invasive surgery in either study. However, until further details are known, surgeons should proceed cautiously and counsel patients regarding these study results.
Amanda N. Fader, MD , made her comments in an accompanying editorial (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395 ). Dr. Fader is with the Johns Hopkins University, Baltimore. She reported having no relevant disclosures.
based on findings from the randomized, controlled phase 3 Laparoscopic Approach to Cervical Cancer (LACC) trial of more than 600 women.

The alarming findings, which led to early study termination, also were supported by results from a second population-based study. Both studies were published concurrently in the Oct. 31 issue of the New England Journal of Medicine.
The disease-free survival at 4.5 years among 319 patients who underwent minimally invasive surgery in the LACC trial was 86.0% vs. 96.5% in 312 patients who underwent open surgery, Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395).
At 3 years, the disease-free survival rates were 91.2% in the minimally invasive surgery group and 97.1% in open surgery group (hazard ratio for disease recurrence or death from cervical cancer, 3.74).
The differences between the groups persisted after adjustment for age, body mass index, disease stage, lymphovascular invasion, and lymph-node involvement. In the minimally invasive surgery group, the findings were comparable for those who underwent laparoscopic vs. robot-assisted surgery, the investigators found.
Further, at 3 years, overall survival was 93.8% vs. 99.0% (HR for death from any cause, 6.00), death from cervical cancer was 4.4% vs. 0.6% (HR, 6.56), and the rate of locoregional recurrence-free survival was 94.3 vs. 98.3 (HR, 4.26) in the minimally invasive and open surgery groups, respectively.
Study participants were women with a mean age of 46 years with stage IA1, IA2, or IB1 cervical cancer, with most (91.9%) having IB1 disease, and either squamous-cell carcinoma, adenocarcinoma, or adenosquamous carcinoma. They were recruited from 33 centers worldwide between June 2008 and June 2017. Most of those assigned to minimally invasive surgery underwent laparoscopic surgery (84.4%), and the remaining patients underwent robot-assisted surgery.
The treatment groups were balanced with respect to baseline characteristics, they noted.
The minimally invasive approach is widely used given that guidelines from the National Comprehensive Cancer Network and European Society of Gynecological Oncology consider both surgical approaches acceptable, and since retrospective studies suggest laparoscopic radical hysterectomy is associated with lower complication rates and comparable outcomes. However, there are limited prospective data regarding survival outcomes in early stage disease with the two approaches, the researchers said.
“Our results call into question the findings in the literature suggesting that minimally invasive radical hysterectomy is associated with no difference in oncologic outcomes as compared with the open approach,” they wrote, noting that a number of factors may explain the differences, such as concurrent vs. sequential analyses in the current studies vs. prior studies (in sequential analyses, earlier procedures may have been performed under broader indications and less clearly defined radiotherapy guidelines), and the possibility that “routine use of a uterine manipulator might increase the propensity for tumor spillage” in minimally invasive surgery.
Strengths of the study include its prospective, randomized, international multicenter design and inclusion of a per-protocol analysis that was consistent with the intention-to-treat analysis, and limitations include the fact that intended enrollment wasn’t reached because of the “safety alert raised by the data and safety monitoring committee on the basis of the higher recurrence and death in the minimally invasive surgery groups,” as well as the inability to generalize the results to patients with low-risk disease as there was lack of power to evaluate outcomes in that context.
Even though the trial was initially powered on the assumption that there would be a 4.5 year follow-up for all patients, only 59.7% reached that length of follow-up. However, the trial still reached 84% power to detect noninferiority of the primary outcome (disease-free survival) with minimally invasive surgery, which was not found, they noted.
Similarly, in the population-based cohort study of 2,461 women who underwent radical hysterectomy for stage IA2 of IB1 cervical cancer between 2010 and 2013, 4-year mortality was 9.1% among 1,225 patients who underwent minimally invasive surgery vs. 5.3% among the 1,236 patients who underwent open surgery (HR, 1.65), Alexander Melamed, MD, of Harvard Medical School, Boston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1804923).
Of note, the 4-year relative survival rate following radical hysterectomy for cervical cancer remained stable prior to the widespread adoption of minimally invasive approaches; an interrupted time-series analysis involving women who underwent surgery during 2000-2010, which was also conducted as part of the study, showed a decline in 4-year survival of 0.8% per year after 2006, coinciding with increased use of minimally invasive surgery, the investigators said.
For the main patient-level analysis, the researchers used the National Cancer Database, and for the time-series analysis they used information from the Surveillance, Epidemiology, and End Results program database.
“Our findings suggest that minimally invasive surgery was associated with a higher risk of death than open surgery among women who underwent radical hysterectomy for early-stage cervical cancer. This association was apparent regardless of laparoscopic approach, tumor size, or histologic type,” they concluded.
The findings are unexpected, eye-opening, and should inform practice, according to Ritu Salani, MD, of the Ohio State University, Columbus.
“This is something we have to discuss with patients,” she said in an interview, noting that while these aren’t perfect studies, they “are the best information we have.
Data reported in September at a meeting of the International Gynecologic Cancer Society show that surgical complications and quality of life outcomes are similar with minimally invasive and open surgery, therefore the findings from these two new studies suggest a need to shift back toward open surgery for patients with cervical cancer, she said.
One “catch” is that survival in the open surgery group in the LACC trial was unusually high and recurrence rates unusually low, compared with what might be expected, and the explanation for this observation is unclear.
“There may be some missing pieces that they haven’t been able to explain, but it’s not clear that they would change the outcome,” she said.
Justin Chura, MD, director of gynecologic oncology and robotic surgery at Cancer Treatment Center of America’s Eastern Regional Medical Center in Philadelphia, said in an interview, “The results of the study by Ramirez et al. are certainly disappointing for those among us who are advocates of minimally invasive surgery (MIS). In my own practice, I transitioned to minimally invasive radical hysterectomy approximately 10 years ago. Now that approach has to be reconsidered. While there are likely subsets of patients who will still benefit from a MIS approach without worsening oncologic outcomes, we do not have robust data to reliably identify those patients.
“One factor that warrants further investigation is the use of a uterine manipulator. While I do not use a manipulator out of personal preference (one less step in the operating room), the idea of placing a device through the tumor or adjacent to it, has biologic plausibility in terms of displacing tumor cells into lymphatic channels,” he said. “Until we have more data, an open approach appears to be preferred.”*
Dr. Ramirez and Dr. Melamed each reported having no relevant disclosures. Dr. Salani and Dr. Chura are members of the Ob.Gyn. News editorial board, but reported having no other relevant disclosures.*
SOURCE: Ramirez P. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
*This article was updated 11/9/2018.
based on findings from the randomized, controlled phase 3 Laparoscopic Approach to Cervical Cancer (LACC) trial of more than 600 women.

The alarming findings, which led to early study termination, also were supported by results from a second population-based study. Both studies were published concurrently in the Oct. 31 issue of the New England Journal of Medicine.
The disease-free survival at 4.5 years among 319 patients who underwent minimally invasive surgery in the LACC trial was 86.0% vs. 96.5% in 312 patients who underwent open surgery, Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395).
At 3 years, the disease-free survival rates were 91.2% in the minimally invasive surgery group and 97.1% in open surgery group (hazard ratio for disease recurrence or death from cervical cancer, 3.74).
The differences between the groups persisted after adjustment for age, body mass index, disease stage, lymphovascular invasion, and lymph-node involvement. In the minimally invasive surgery group, the findings were comparable for those who underwent laparoscopic vs. robot-assisted surgery, the investigators found.
Further, at 3 years, overall survival was 93.8% vs. 99.0% (HR for death from any cause, 6.00), death from cervical cancer was 4.4% vs. 0.6% (HR, 6.56), and the rate of locoregional recurrence-free survival was 94.3 vs. 98.3 (HR, 4.26) in the minimally invasive and open surgery groups, respectively.
Study participants were women with a mean age of 46 years with stage IA1, IA2, or IB1 cervical cancer, with most (91.9%) having IB1 disease, and either squamous-cell carcinoma, adenocarcinoma, or adenosquamous carcinoma. They were recruited from 33 centers worldwide between June 2008 and June 2017. Most of those assigned to minimally invasive surgery underwent laparoscopic surgery (84.4%), and the remaining patients underwent robot-assisted surgery.
The treatment groups were balanced with respect to baseline characteristics, they noted.
The minimally invasive approach is widely used given that guidelines from the National Comprehensive Cancer Network and European Society of Gynecological Oncology consider both surgical approaches acceptable, and since retrospective studies suggest laparoscopic radical hysterectomy is associated with lower complication rates and comparable outcomes. However, there are limited prospective data regarding survival outcomes in early stage disease with the two approaches, the researchers said.
“Our results call into question the findings in the literature suggesting that minimally invasive radical hysterectomy is associated with no difference in oncologic outcomes as compared with the open approach,” they wrote, noting that a number of factors may explain the differences, such as concurrent vs. sequential analyses in the current studies vs. prior studies (in sequential analyses, earlier procedures may have been performed under broader indications and less clearly defined radiotherapy guidelines), and the possibility that “routine use of a uterine manipulator might increase the propensity for tumor spillage” in minimally invasive surgery.
Strengths of the study include its prospective, randomized, international multicenter design and inclusion of a per-protocol analysis that was consistent with the intention-to-treat analysis, and limitations include the fact that intended enrollment wasn’t reached because of the “safety alert raised by the data and safety monitoring committee on the basis of the higher recurrence and death in the minimally invasive surgery groups,” as well as the inability to generalize the results to patients with low-risk disease as there was lack of power to evaluate outcomes in that context.
Even though the trial was initially powered on the assumption that there would be a 4.5 year follow-up for all patients, only 59.7% reached that length of follow-up. However, the trial still reached 84% power to detect noninferiority of the primary outcome (disease-free survival) with minimally invasive surgery, which was not found, they noted.
Similarly, in the population-based cohort study of 2,461 women who underwent radical hysterectomy for stage IA2 of IB1 cervical cancer between 2010 and 2013, 4-year mortality was 9.1% among 1,225 patients who underwent minimally invasive surgery vs. 5.3% among the 1,236 patients who underwent open surgery (HR, 1.65), Alexander Melamed, MD, of Harvard Medical School, Boston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1804923).
Of note, the 4-year relative survival rate following radical hysterectomy for cervical cancer remained stable prior to the widespread adoption of minimally invasive approaches; an interrupted time-series analysis involving women who underwent surgery during 2000-2010, which was also conducted as part of the study, showed a decline in 4-year survival of 0.8% per year after 2006, coinciding with increased use of minimally invasive surgery, the investigators said.
For the main patient-level analysis, the researchers used the National Cancer Database, and for the time-series analysis they used information from the Surveillance, Epidemiology, and End Results program database.
“Our findings suggest that minimally invasive surgery was associated with a higher risk of death than open surgery among women who underwent radical hysterectomy for early-stage cervical cancer. This association was apparent regardless of laparoscopic approach, tumor size, or histologic type,” they concluded.
The findings are unexpected, eye-opening, and should inform practice, according to Ritu Salani, MD, of the Ohio State University, Columbus.
“This is something we have to discuss with patients,” she said in an interview, noting that while these aren’t perfect studies, they “are the best information we have.
Data reported in September at a meeting of the International Gynecologic Cancer Society show that surgical complications and quality of life outcomes are similar with minimally invasive and open surgery, therefore the findings from these two new studies suggest a need to shift back toward open surgery for patients with cervical cancer, she said.
One “catch” is that survival in the open surgery group in the LACC trial was unusually high and recurrence rates unusually low, compared with what might be expected, and the explanation for this observation is unclear.
“There may be some missing pieces that they haven’t been able to explain, but it’s not clear that they would change the outcome,” she said.
Justin Chura, MD, director of gynecologic oncology and robotic surgery at Cancer Treatment Center of America’s Eastern Regional Medical Center in Philadelphia, said in an interview, “The results of the study by Ramirez et al. are certainly disappointing for those among us who are advocates of minimally invasive surgery (MIS). In my own practice, I transitioned to minimally invasive radical hysterectomy approximately 10 years ago. Now that approach has to be reconsidered. While there are likely subsets of patients who will still benefit from a MIS approach without worsening oncologic outcomes, we do not have robust data to reliably identify those patients.
“One factor that warrants further investigation is the use of a uterine manipulator. While I do not use a manipulator out of personal preference (one less step in the operating room), the idea of placing a device through the tumor or adjacent to it, has biologic plausibility in terms of displacing tumor cells into lymphatic channels,” he said. “Until we have more data, an open approach appears to be preferred.”*
Dr. Ramirez and Dr. Melamed each reported having no relevant disclosures. Dr. Salani and Dr. Chura are members of the Ob.Gyn. News editorial board, but reported having no other relevant disclosures.*
SOURCE: Ramirez P. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
*This article was updated 11/9/2018.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Cervical cancer recurrence and survival rates were worse with minimally invasive vs. open surgery in a prospective study.
Major finding: Disease-free survival at 4.5 years was 86% with minimally invasive vs. 96.5% with open surgery.
Study details: The phase 3 LACC trial of more than 600 women with cervical cancer, and a population based study of nearly 2,500 women with cervical cancer.
Disclosures: Dr. Ramirez and Dr. Melamed each reported having no relevant disclosures. Dr. Salani is a member of the OB.GYN. News editorial board, but reported having no other relevant disclosures.
Source: Ramirez P. N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395.
Palliative care update highlights role of nonspecialists
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
The new edition of providing care for critically ill patients, not just those clinicians actively specialized in palliative care.
The Clinical Practice Guidelines for Quality Palliative Care, 4th Edition, emphasizes the importance of palliative care provided by “clinicians in primary care and specialty care practices, such as oncologists,” the guideline authors stated.
The latest revision of the guideline aims to establish a foundation for “gold-standard” palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to the National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology and the Oncology Nurses Society.
One key reason for the update, according to the NCP, was to acknowledge that today’s health care system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on all clinicians who are not palliative specialists to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
This approach differs from the way palliative care is traditionally practiced, often by fellowship-trained physicians, trained nurses, and other specialists who provide that support.
The guidelines are organized into sections covering palliative care structure and processes, care for the patient nearing the end of life, and specific aspects of palliative care, including physical, psychological, and psychiatric; social; cultural, ethical, and legal; and spiritual, religious, and existential aspects.
“The expectation is that all clinicians caring for seriously ill patients will integrate palliative care competencies, such as safe and effective pain and symptom management and expert communication skills in their practice, and palliative care specialists will provide expertise for those with the most complex needs,” the guideline authors wrote.
Implications for treatment of oncology patients
These new guidelines represent a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, who is a medical oncologist, palliative care physician, and patient experience researcher at Duke University, Durham, N.C.
“Part of this report to is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” said Dr. LeBlanc.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who needs us the most, and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said in an interview.
That’s a major driver behind the emphasis in these latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, he added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists, and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Palliative care in surgical care
These guidelines are particularly useful to surgeons in part because of their focus on what’s known as primary palliative care, said to Geoffrey P. Dunn, MD, former chair of the American College of Surgeons Committee on Surgical Palliative Care. Palliative care, the new guidelines suggest, can be implemented by nonspecialists.
Primary palliative care includes diverse skills such as breaking adverse news to patients, managing uncomplicated pain, and being able to recognize signs and symptoms of imminent demise. “These are the minimum deliverables for all people dealing with seriously ill patients,” Dr. Dunn said in an interview. “It’s palliative care that any practicing physician should be able to handle.”
Dr. Dunn concurred with Dr. LaBlanc about the workforce shortage in the palliative field. The traditional model has created a shortage of specialized clinicians to meet palliative care needs. Across the board, “staffing for palliative teams is very inconsistent,” said Dr. Dunn. “It’s a classic unfunded mandate.”
While these guidelines are a step forward in recognizing the importance of palliative care outside of the palliative care specialty, there is no reference to surgery anywhere in the text of the 141-page prepublication draft provided by the NCP, Dr. Dunn noted in the interview.
“There’s still a danger of parallel universes, where surgery is developing its own understanding of this in parallel with the more general national palliative care movement,” he said. Despite that, there is a growing connection between surgery and the broader palliative care community. That linkage is especially important given the number of seriously ill patients with high symptom burden that are seen in surgery.
“I think where surgeons are beginning to find [palliative principles] very helpful is dealing with these protracted serial discussions with families in difficult circumstances, such as how long is the life support going to be prolonged in someone with a devastating head injury, or multiple system organ failure in the elderly,” Dr. Dunn added.
With one hand, administration boosts ACA marketplaces, weakens them with another
In the span of less than 12 hours, the Trump administration took two seemingly contradictory actions that could have profound effects on the insurance marketplaces set up by the Affordable Care Act.
First, officials issued guidance on the morning of Oct. 22 that could weaken the exchanges set up for people who buy their own insurance. The new approach makes it easier for states to get around some ACA requirements, including allowing the use of federal subsidies for skimpier plans that can reject people with preexisting conditions.
Yet, the other move – a proposed rule unveiled that evening – could bolster ACA marketplaces by sending millions of people with job-based coverage there, armed with tax-free money from their employers to buy individual plans.
Both efforts play into the parallel narratives dominating the bitter political debate over the ACA.
The administration, frustrated that Congress did not repeal the law, say some critics and policy experts, is working to undermine it by weakening the marketplaces and the law’s consumer protections. Those efforts make it easier for insurers to offer skimpier policies that bypass the law’s rules, such as its ban on annual or lifetime limits or its protections for people with preexisting conditions. Congress also zeroed out the tax penalty for not having coverage, effective next year. Combined, the moves could reduce enrollment in ACA plans, potentially driving up premiums for those who remain.
The administration and Republicans in Congress say they are looking to assist those left behind by the ACA – people who don’t get subsidies to help them buy coverage and are desperate for less expensive options – even if that means purchasing less robust coverage.
“These are people who were buying insurance before [the law] and then the rules changed and they could not buy it because they could not afford it,” said Joe Antos, a resident scholar at the conservative American Enterprise Institute. “They have been slowly dropping out of insurance coverage altogether.”
The efforts are dramatically reshaping the ACA and the individual insurance market to one that looks more as it did before the 2010 law, when regulation, coverage, and consumer protections varied widely across the country.
“Some states will do everything they can to keep individual markets strong and stable. Others won’t,” said Sabrina Corlette, research professor at the Center on Health Insurance Reforms at Georgetown University.
So what expectations should consumers have? Here are three key takeaways:
Protections for preexisting health problems are uncertain
Polls show that keeping the ACA’s guarantees on coverage for people with medical problems is a top concern for Americans, and Democrats have made their defense of the health law a key part of their midterm election campaigns.
Republicans have gotten that message and even those who voted to repeal the ACA or joined a lawsuit by 20 red states to overturn it now say they want to protect people with preexisting conditions. Still, GOP lawmakers have not introduced any plan that would be as protective as the current law.
In August, the administration released a rule allowing expanded use of short-term plans, which are less expensive than ACA policies. To get those lower prices, most of these plans do not cover prescription drugs, maternity care, mental health, or substance abuse treatments.
The move is unlikely to benefit people with health problems, as short-term plans can reject people with preexisting conditions or decline to cover care for those medical problems.
Under the rule, insurers can sell them starting in 2019 for up to a year’s duration, with an option to renew for up to 3 years, reversing an Obama-era directive that limited them to 90 days.
Administration officials estimate such plans could draw 600,000 new enrollees next year, and others have estimated the numbers could be far higher. The concern is if many healthy people in 2019 switch out of the ACA market and choose short-term plans, premiums will rise for those who remain, including those with preexisting conditions, or make the ACA market less attractive for insurers.
Where you live matters more
One of the biggest changes ushered in with the ACA was a standard set of rules across all states.
Before the law took effect, consumers buying their own coverage saw tremendous variation in what was offered and what protections they had, depending on the state where they lived.
Most states, for example, allowed insurers to reject people with medical conditions. A few states required insurers to charge similar premiums across the board, but most allowed wide variations based on age, gender or health. Some skimpy plans didn’t cover prescription drugs, chemotherapy, or other medical services.
By standardizing the rules and benefits, the ACA barred insurers from rejecting applicants with medical conditions or charging them more. Women and men get the same premium rates and insurers could charge older people no more than three times what they charged younger ones.
Under the new guidance issued this week giving states more flexibility on what is offered, consumers could again see a wide variation on coverage, premium rules, and even subsidy eligibility.
“It shifts pressure to state politicians,” said Caroline Pearson, a senior fellow at NORC, a nonpartisan research institution at the University of Chicago. That could play into the calculus of whether a state will seek to make broad changes to help people who cannot afford ACA plans, even if the trade-off affects people with medical conditions.
“You risk making some worse off by threatening those markets,” said Pearson. “That is always going to be hard.”
Millions more will join the “buy-your-own” ranks
The proposed rule released Oct. 23 allows employers to fund tax-free accounts – called health reimbursement arrangements (HRAs) – that workers can use to buy their own coverage on the ACA marketplaces.
The administration estimates about 10 million people would do so by 2028 – a substantial boost for those exchanges, which policymakers say never hit the enrollment numbers needed to attract enough insurers and hold prices down.
John Barkett, senior director of policy affairs at Willis Towers Watson, a benefits consulting firm, said he expects employers to “seriously consider” the new market. The infusion of workers will improve options by attracting more insurers, he added.
“These people coming in will be employer-sponsored, they’ll have steady jobs,” Barkett noted, and will likely stick with coverage longer than those typically in the individual market.
Currently more than 14 million people buy their own insurance, with about 10 million of those using federal or state ACA marketplaces. The others buy private plans through brokers.
The proposed rule won’t be finalized for months, but it could result in new options by 2020.
If these workers seeking coverage are generally healthy, the infusion could slow premium increases in the overall ACA marketplace because it would improve the risk pool for insurers.
But, if employers with mainly higher-cost or older workers opt to move to the marketplaces, it could help drive up premiums.
In an odd twist, the administration notes in the proposed rule that the ACA has provisions that could protect the marketplace from that type of adverse selection, which can drive up prices. But most of the protective factors cited by the rule have been weakened, removed, or expired, such as the tax penalty for being uninsured and the federal subsidies for insurers to cover lower deductibles for certain low-income consumers.
Benefits consultants and policy experts are skeptical about how many companies will move to the HRA plan, given the tight labor market. Continued uncertainty about the fate of the ACA marketplace may keep them reluctant to send workers out on their own, they say.
Health benefits are a big factor in attracting and retaining workers, said Chris Condeluci, a Washington attorney who previously worked for Sen. Chuck Grassley (R-Iowa) and served as counsel to the Senate Finance Committee during the drafting of the ACA.
“Most employers believe their group health plan will provide better health coverage than an individual market plan,” he said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In the span of less than 12 hours, the Trump administration took two seemingly contradictory actions that could have profound effects on the insurance marketplaces set up by the Affordable Care Act.
First, officials issued guidance on the morning of Oct. 22 that could weaken the exchanges set up for people who buy their own insurance. The new approach makes it easier for states to get around some ACA requirements, including allowing the use of federal subsidies for skimpier plans that can reject people with preexisting conditions.
Yet, the other move – a proposed rule unveiled that evening – could bolster ACA marketplaces by sending millions of people with job-based coverage there, armed with tax-free money from their employers to buy individual plans.
Both efforts play into the parallel narratives dominating the bitter political debate over the ACA.
The administration, frustrated that Congress did not repeal the law, say some critics and policy experts, is working to undermine it by weakening the marketplaces and the law’s consumer protections. Those efforts make it easier for insurers to offer skimpier policies that bypass the law’s rules, such as its ban on annual or lifetime limits or its protections for people with preexisting conditions. Congress also zeroed out the tax penalty for not having coverage, effective next year. Combined, the moves could reduce enrollment in ACA plans, potentially driving up premiums for those who remain.
The administration and Republicans in Congress say they are looking to assist those left behind by the ACA – people who don’t get subsidies to help them buy coverage and are desperate for less expensive options – even if that means purchasing less robust coverage.
“These are people who were buying insurance before [the law] and then the rules changed and they could not buy it because they could not afford it,” said Joe Antos, a resident scholar at the conservative American Enterprise Institute. “They have been slowly dropping out of insurance coverage altogether.”
The efforts are dramatically reshaping the ACA and the individual insurance market to one that looks more as it did before the 2010 law, when regulation, coverage, and consumer protections varied widely across the country.
“Some states will do everything they can to keep individual markets strong and stable. Others won’t,” said Sabrina Corlette, research professor at the Center on Health Insurance Reforms at Georgetown University.
So what expectations should consumers have? Here are three key takeaways:
Protections for preexisting health problems are uncertain
Polls show that keeping the ACA’s guarantees on coverage for people with medical problems is a top concern for Americans, and Democrats have made their defense of the health law a key part of their midterm election campaigns.
Republicans have gotten that message and even those who voted to repeal the ACA or joined a lawsuit by 20 red states to overturn it now say they want to protect people with preexisting conditions. Still, GOP lawmakers have not introduced any plan that would be as protective as the current law.
In August, the administration released a rule allowing expanded use of short-term plans, which are less expensive than ACA policies. To get those lower prices, most of these plans do not cover prescription drugs, maternity care, mental health, or substance abuse treatments.
The move is unlikely to benefit people with health problems, as short-term plans can reject people with preexisting conditions or decline to cover care for those medical problems.
Under the rule, insurers can sell them starting in 2019 for up to a year’s duration, with an option to renew for up to 3 years, reversing an Obama-era directive that limited them to 90 days.
Administration officials estimate such plans could draw 600,000 new enrollees next year, and others have estimated the numbers could be far higher. The concern is if many healthy people in 2019 switch out of the ACA market and choose short-term plans, premiums will rise for those who remain, including those with preexisting conditions, or make the ACA market less attractive for insurers.
Where you live matters more
One of the biggest changes ushered in with the ACA was a standard set of rules across all states.
Before the law took effect, consumers buying their own coverage saw tremendous variation in what was offered and what protections they had, depending on the state where they lived.
Most states, for example, allowed insurers to reject people with medical conditions. A few states required insurers to charge similar premiums across the board, but most allowed wide variations based on age, gender or health. Some skimpy plans didn’t cover prescription drugs, chemotherapy, or other medical services.
By standardizing the rules and benefits, the ACA barred insurers from rejecting applicants with medical conditions or charging them more. Women and men get the same premium rates and insurers could charge older people no more than three times what they charged younger ones.
Under the new guidance issued this week giving states more flexibility on what is offered, consumers could again see a wide variation on coverage, premium rules, and even subsidy eligibility.
“It shifts pressure to state politicians,” said Caroline Pearson, a senior fellow at NORC, a nonpartisan research institution at the University of Chicago. That could play into the calculus of whether a state will seek to make broad changes to help people who cannot afford ACA plans, even if the trade-off affects people with medical conditions.
“You risk making some worse off by threatening those markets,” said Pearson. “That is always going to be hard.”
Millions more will join the “buy-your-own” ranks
The proposed rule released Oct. 23 allows employers to fund tax-free accounts – called health reimbursement arrangements (HRAs) – that workers can use to buy their own coverage on the ACA marketplaces.
The administration estimates about 10 million people would do so by 2028 – a substantial boost for those exchanges, which policymakers say never hit the enrollment numbers needed to attract enough insurers and hold prices down.
John Barkett, senior director of policy affairs at Willis Towers Watson, a benefits consulting firm, said he expects employers to “seriously consider” the new market. The infusion of workers will improve options by attracting more insurers, he added.
“These people coming in will be employer-sponsored, they’ll have steady jobs,” Barkett noted, and will likely stick with coverage longer than those typically in the individual market.
Currently more than 14 million people buy their own insurance, with about 10 million of those using federal or state ACA marketplaces. The others buy private plans through brokers.
The proposed rule won’t be finalized for months, but it could result in new options by 2020.
If these workers seeking coverage are generally healthy, the infusion could slow premium increases in the overall ACA marketplace because it would improve the risk pool for insurers.
But, if employers with mainly higher-cost or older workers opt to move to the marketplaces, it could help drive up premiums.
In an odd twist, the administration notes in the proposed rule that the ACA has provisions that could protect the marketplace from that type of adverse selection, which can drive up prices. But most of the protective factors cited by the rule have been weakened, removed, or expired, such as the tax penalty for being uninsured and the federal subsidies for insurers to cover lower deductibles for certain low-income consumers.
Benefits consultants and policy experts are skeptical about how many companies will move to the HRA plan, given the tight labor market. Continued uncertainty about the fate of the ACA marketplace may keep them reluctant to send workers out on their own, they say.
Health benefits are a big factor in attracting and retaining workers, said Chris Condeluci, a Washington attorney who previously worked for Sen. Chuck Grassley (R-Iowa) and served as counsel to the Senate Finance Committee during the drafting of the ACA.
“Most employers believe their group health plan will provide better health coverage than an individual market plan,” he said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In the span of less than 12 hours, the Trump administration took two seemingly contradictory actions that could have profound effects on the insurance marketplaces set up by the Affordable Care Act.
First, officials issued guidance on the morning of Oct. 22 that could weaken the exchanges set up for people who buy their own insurance. The new approach makes it easier for states to get around some ACA requirements, including allowing the use of federal subsidies for skimpier plans that can reject people with preexisting conditions.
Yet, the other move – a proposed rule unveiled that evening – could bolster ACA marketplaces by sending millions of people with job-based coverage there, armed with tax-free money from their employers to buy individual plans.
Both efforts play into the parallel narratives dominating the bitter political debate over the ACA.
The administration, frustrated that Congress did not repeal the law, say some critics and policy experts, is working to undermine it by weakening the marketplaces and the law’s consumer protections. Those efforts make it easier for insurers to offer skimpier policies that bypass the law’s rules, such as its ban on annual or lifetime limits or its protections for people with preexisting conditions. Congress also zeroed out the tax penalty for not having coverage, effective next year. Combined, the moves could reduce enrollment in ACA plans, potentially driving up premiums for those who remain.
The administration and Republicans in Congress say they are looking to assist those left behind by the ACA – people who don’t get subsidies to help them buy coverage and are desperate for less expensive options – even if that means purchasing less robust coverage.
“These are people who were buying insurance before [the law] and then the rules changed and they could not buy it because they could not afford it,” said Joe Antos, a resident scholar at the conservative American Enterprise Institute. “They have been slowly dropping out of insurance coverage altogether.”
The efforts are dramatically reshaping the ACA and the individual insurance market to one that looks more as it did before the 2010 law, when regulation, coverage, and consumer protections varied widely across the country.
“Some states will do everything they can to keep individual markets strong and stable. Others won’t,” said Sabrina Corlette, research professor at the Center on Health Insurance Reforms at Georgetown University.
So what expectations should consumers have? Here are three key takeaways:
Protections for preexisting health problems are uncertain
Polls show that keeping the ACA’s guarantees on coverage for people with medical problems is a top concern for Americans, and Democrats have made their defense of the health law a key part of their midterm election campaigns.
Republicans have gotten that message and even those who voted to repeal the ACA or joined a lawsuit by 20 red states to overturn it now say they want to protect people with preexisting conditions. Still, GOP lawmakers have not introduced any plan that would be as protective as the current law.
In August, the administration released a rule allowing expanded use of short-term plans, which are less expensive than ACA policies. To get those lower prices, most of these plans do not cover prescription drugs, maternity care, mental health, or substance abuse treatments.
The move is unlikely to benefit people with health problems, as short-term plans can reject people with preexisting conditions or decline to cover care for those medical problems.
Under the rule, insurers can sell them starting in 2019 for up to a year’s duration, with an option to renew for up to 3 years, reversing an Obama-era directive that limited them to 90 days.
Administration officials estimate such plans could draw 600,000 new enrollees next year, and others have estimated the numbers could be far higher. The concern is if many healthy people in 2019 switch out of the ACA market and choose short-term plans, premiums will rise for those who remain, including those with preexisting conditions, or make the ACA market less attractive for insurers.
Where you live matters more
One of the biggest changes ushered in with the ACA was a standard set of rules across all states.
Before the law took effect, consumers buying their own coverage saw tremendous variation in what was offered and what protections they had, depending on the state where they lived.
Most states, for example, allowed insurers to reject people with medical conditions. A few states required insurers to charge similar premiums across the board, but most allowed wide variations based on age, gender or health. Some skimpy plans didn’t cover prescription drugs, chemotherapy, or other medical services.
By standardizing the rules and benefits, the ACA barred insurers from rejecting applicants with medical conditions or charging them more. Women and men get the same premium rates and insurers could charge older people no more than three times what they charged younger ones.
Under the new guidance issued this week giving states more flexibility on what is offered, consumers could again see a wide variation on coverage, premium rules, and even subsidy eligibility.
“It shifts pressure to state politicians,” said Caroline Pearson, a senior fellow at NORC, a nonpartisan research institution at the University of Chicago. That could play into the calculus of whether a state will seek to make broad changes to help people who cannot afford ACA plans, even if the trade-off affects people with medical conditions.
“You risk making some worse off by threatening those markets,” said Pearson. “That is always going to be hard.”
Millions more will join the “buy-your-own” ranks
The proposed rule released Oct. 23 allows employers to fund tax-free accounts – called health reimbursement arrangements (HRAs) – that workers can use to buy their own coverage on the ACA marketplaces.
The administration estimates about 10 million people would do so by 2028 – a substantial boost for those exchanges, which policymakers say never hit the enrollment numbers needed to attract enough insurers and hold prices down.
John Barkett, senior director of policy affairs at Willis Towers Watson, a benefits consulting firm, said he expects employers to “seriously consider” the new market. The infusion of workers will improve options by attracting more insurers, he added.
“These people coming in will be employer-sponsored, they’ll have steady jobs,” Barkett noted, and will likely stick with coverage longer than those typically in the individual market.
Currently more than 14 million people buy their own insurance, with about 10 million of those using federal or state ACA marketplaces. The others buy private plans through brokers.
The proposed rule won’t be finalized for months, but it could result in new options by 2020.
If these workers seeking coverage are generally healthy, the infusion could slow premium increases in the overall ACA marketplace because it would improve the risk pool for insurers.
But, if employers with mainly higher-cost or older workers opt to move to the marketplaces, it could help drive up premiums.
In an odd twist, the administration notes in the proposed rule that the ACA has provisions that could protect the marketplace from that type of adverse selection, which can drive up prices. But most of the protective factors cited by the rule have been weakened, removed, or expired, such as the tax penalty for being uninsured and the federal subsidies for insurers to cover lower deductibles for certain low-income consumers.
Benefits consultants and policy experts are skeptical about how many companies will move to the HRA plan, given the tight labor market. Continued uncertainty about the fate of the ACA marketplace may keep them reluctant to send workers out on their own, they say.
Health benefits are a big factor in attracting and retaining workers, said Chris Condeluci, a Washington attorney who previously worked for Sen. Chuck Grassley (R-Iowa) and served as counsel to the Senate Finance Committee during the drafting of the ACA.
“Most employers believe their group health plan will provide better health coverage than an individual market plan,” he said.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.













