User login
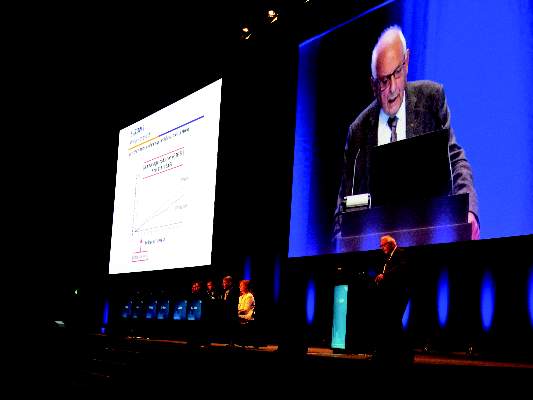
Levosimendan does not reduce organ dysfunction risk in sepsis
Levosimendan does not reduce the likelihood of severe organ dysfunction in adults with sepsis, nor does it lower the mortality rate, according to research presented at the annual congress of the European Society of Intensive Care Medicine and published in the New England Journal of Medicine.
Levosimendan is a calcium-sensitizing drug with inotropic and vasodilatory properties, which is commonly used to treat decompensated heart failure. “Small studies that have investigated the use of levosimendan in patients with septic shock have shown improvements in hemodynamic variables, microcirculatory flow, and renal and hepatic function, as compared with dobutamine,” wrote Anthony C. Gordon, MD, of Imperial College London and Imperial College Healthcare NHS Trust and his coauthors.
In the Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis (LeoPARDS) trial, 516 patients were randomized to 24 hours of a blinded infusion either of levosimendan (.05-0.2 mcg per kilogram of body weight per minute) or placebo in addition to standard care.
Researchers saw no significant difference in the mean daily Sequential Organ Failure Assessment (SOFA) score between the two groups (mean difference, 0.61; 95% confidence interval, −0.07 to 1.29; P = .053). When the SOFA score was analyzed by system, the mean daily cardiovascular score was significantly higher in the levosimendan group, compared with the placebo group, indicating greater dysfunction in that system.
“The cardiovascular SOFA score was higher in the levosimendan group than in the placebo group, which reflects the higher doses of norepinephrine that were required to maintain the mean arterial pressure,” researchers reported.
There was no significant difference in 28-day mortality between the levosimendan and placebo groups (34.5% vs. 30.9%; 95% CI, −4.5 to 11.7; P = .43), and both groups had a similar number of catecholamine-free days. However, among the patients who required ventilation at baseline, those treated with levosimendan were less likely than those given placebo to be successfully weaned from ventilation over the 28-day follow-up.
Patients treated with levosimendan also had a higher incidence of serious adverse events, and supraventricular tachyarrhythmia was significantly more common in the levosimendan group than in the placebo group (3.1% vs. 0.4%; 95% CI, 0.1- 5.3; P = .04).
The two groups showed similar cardiac index, stroke volume, central venous oxygen saturations or pressure, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, and serum creatinine and bilirubin levels.
The authors drew attention to several limitations of the study, including the fact that levosimendan was added to standard care rather than being compared with an alternative inotrope such as dobutamine.
“Less than 10% of the patients in the placebo group received dobutamine, although the rate of use in the placebo group was higher than in the levosimendan group and may explain in part why the cardiac index and stroke volume were not higher in the levosimendan group than in the placebo group,” they wrote.
The study did not include echocardiographic analysis to discover any changes in myocardial function with levosimendan, and there were only a small number of patients with low cardiac index.
“Therefore, this trial cannot provide guidance as to which inotrope is best to use in the management of sepsis if a low cardiac index is present,” the authors said. “The target mean arterial pressure of 65-70 mm Hg, which was recommended in the protocol and reiterated at investigator meetings, was frequently exceeded (as in other trials involving patients with shock), which suggests that the norepinephrine doses that were administered could have been reduced in the two trial groups.”
The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions, and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Levosimendan does not reduce the likelihood of severe organ dysfunction in adults with sepsis, nor does it lower the mortality rate, according to research presented at the annual congress of the European Society of Intensive Care Medicine and published in the New England Journal of Medicine.
Levosimendan is a calcium-sensitizing drug with inotropic and vasodilatory properties, which is commonly used to treat decompensated heart failure. “Small studies that have investigated the use of levosimendan in patients with septic shock have shown improvements in hemodynamic variables, microcirculatory flow, and renal and hepatic function, as compared with dobutamine,” wrote Anthony C. Gordon, MD, of Imperial College London and Imperial College Healthcare NHS Trust and his coauthors.
In the Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis (LeoPARDS) trial, 516 patients were randomized to 24 hours of a blinded infusion either of levosimendan (.05-0.2 mcg per kilogram of body weight per minute) or placebo in addition to standard care.
Researchers saw no significant difference in the mean daily Sequential Organ Failure Assessment (SOFA) score between the two groups (mean difference, 0.61; 95% confidence interval, −0.07 to 1.29; P = .053). When the SOFA score was analyzed by system, the mean daily cardiovascular score was significantly higher in the levosimendan group, compared with the placebo group, indicating greater dysfunction in that system.
“The cardiovascular SOFA score was higher in the levosimendan group than in the placebo group, which reflects the higher doses of norepinephrine that were required to maintain the mean arterial pressure,” researchers reported.
There was no significant difference in 28-day mortality between the levosimendan and placebo groups (34.5% vs. 30.9%; 95% CI, −4.5 to 11.7; P = .43), and both groups had a similar number of catecholamine-free days. However, among the patients who required ventilation at baseline, those treated with levosimendan were less likely than those given placebo to be successfully weaned from ventilation over the 28-day follow-up.
Patients treated with levosimendan also had a higher incidence of serious adverse events, and supraventricular tachyarrhythmia was significantly more common in the levosimendan group than in the placebo group (3.1% vs. 0.4%; 95% CI, 0.1- 5.3; P = .04).
The two groups showed similar cardiac index, stroke volume, central venous oxygen saturations or pressure, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, and serum creatinine and bilirubin levels.
The authors drew attention to several limitations of the study, including the fact that levosimendan was added to standard care rather than being compared with an alternative inotrope such as dobutamine.
“Less than 10% of the patients in the placebo group received dobutamine, although the rate of use in the placebo group was higher than in the levosimendan group and may explain in part why the cardiac index and stroke volume were not higher in the levosimendan group than in the placebo group,” they wrote.
The study did not include echocardiographic analysis to discover any changes in myocardial function with levosimendan, and there were only a small number of patients with low cardiac index.
“Therefore, this trial cannot provide guidance as to which inotrope is best to use in the management of sepsis if a low cardiac index is present,” the authors said. “The target mean arterial pressure of 65-70 mm Hg, which was recommended in the protocol and reiterated at investigator meetings, was frequently exceeded (as in other trials involving patients with shock), which suggests that the norepinephrine doses that were administered could have been reduced in the two trial groups.”
The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions, and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Levosimendan does not reduce the likelihood of severe organ dysfunction in adults with sepsis, nor does it lower the mortality rate, according to research presented at the annual congress of the European Society of Intensive Care Medicine and published in the New England Journal of Medicine.
Levosimendan is a calcium-sensitizing drug with inotropic and vasodilatory properties, which is commonly used to treat decompensated heart failure. “Small studies that have investigated the use of levosimendan in patients with septic shock have shown improvements in hemodynamic variables, microcirculatory flow, and renal and hepatic function, as compared with dobutamine,” wrote Anthony C. Gordon, MD, of Imperial College London and Imperial College Healthcare NHS Trust and his coauthors.
In the Levosimendan for the Prevention of Acute Organ Dysfunction in Sepsis (LeoPARDS) trial, 516 patients were randomized to 24 hours of a blinded infusion either of levosimendan (.05-0.2 mcg per kilogram of body weight per minute) or placebo in addition to standard care.
Researchers saw no significant difference in the mean daily Sequential Organ Failure Assessment (SOFA) score between the two groups (mean difference, 0.61; 95% confidence interval, −0.07 to 1.29; P = .053). When the SOFA score was analyzed by system, the mean daily cardiovascular score was significantly higher in the levosimendan group, compared with the placebo group, indicating greater dysfunction in that system.
“The cardiovascular SOFA score was higher in the levosimendan group than in the placebo group, which reflects the higher doses of norepinephrine that were required to maintain the mean arterial pressure,” researchers reported.
There was no significant difference in 28-day mortality between the levosimendan and placebo groups (34.5% vs. 30.9%; 95% CI, −4.5 to 11.7; P = .43), and both groups had a similar number of catecholamine-free days. However, among the patients who required ventilation at baseline, those treated with levosimendan were less likely than those given placebo to be successfully weaned from ventilation over the 28-day follow-up.
Patients treated with levosimendan also had a higher incidence of serious adverse events, and supraventricular tachyarrhythmia was significantly more common in the levosimendan group than in the placebo group (3.1% vs. 0.4%; 95% CI, 0.1- 5.3; P = .04).
The two groups showed similar cardiac index, stroke volume, central venous oxygen saturations or pressure, the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen, and serum creatinine and bilirubin levels.
The authors drew attention to several limitations of the study, including the fact that levosimendan was added to standard care rather than being compared with an alternative inotrope such as dobutamine.
“Less than 10% of the patients in the placebo group received dobutamine, although the rate of use in the placebo group was higher than in the levosimendan group and may explain in part why the cardiac index and stroke volume were not higher in the levosimendan group than in the placebo group,” they wrote.
The study did not include echocardiographic analysis to discover any changes in myocardial function with levosimendan, and there were only a small number of patients with low cardiac index.
“Therefore, this trial cannot provide guidance as to which inotrope is best to use in the management of sepsis if a low cardiac index is present,” the authors said. “The target mean arterial pressure of 65-70 mm Hg, which was recommended in the protocol and reiterated at investigator meetings, was frequently exceeded (as in other trials involving patients with shock), which suggests that the norepinephrine doses that were administered could have been reduced in the two trial groups.”
The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions, and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Key clinical point: Levosimendan does not reduce the likelihood of severe organ dysfunction or lower the mortality rate in adults with sepsis.
Major finding: There were no significant differences in mean daily Sequential Organ Failure Assessment score or mortality between patients treated with levosimendan or placebo in addition to standard care.
Data source: Randomized, placebo-controlled LeoPARDS trial in 516 adults with sepsis.
Disclosures: The study was supported by the Medical Research Council and National Institute for Health Research, United Kingdom, and Tenax Therapeutics. Four authors declared grants, personal fees, advisory board positions and other funding from the pharmaceutical industry, including one author receiving support from Tenax Therapeutics. No other conflicts of interest were declared.
Acoustic pharyngometry no additional benefit in OSA diagnosis
Assessment of upper airway cross-sectional area using acoustic pharyngometry is no better than the use of clinical variables to diagnose obstructive sleep apnea (OSA), according to a study in the Annals of the American Thoracic Society.
Tetyana Kendzerska, PhD, of the Institute for Clinical Evaluative Sciences, Toronto, and her colleagues found that the median upper airway cross-sectional area at functional residual capacity when sitting was significantly reduced in individuals with OSA, compared with those without the condition (3.3 cm2 vs. 3.7 cm2).
The researchers found that, at a cut-off value of 3.75 cm2, which struck the best balance of sensitivity and specificity, upper airway cross-sectional area had a sensitivity of 73% and specificity of 46%. Varying the apnea-hypopnea index to define OSA or varying the analysis of upper airway cross-sectional area did not improve its predictive or discriminative ability, nor was there any benefit to measuring upper airway cross-sectional area when an individual was supine, compared with sitting.
Dr. Kendzerska and her colleagues had hypothesized that acoustic pharyngometry could play a role in screening for OSA, based on previous studies suggesting significant differences in upper airway cross-sectional area measures in individuals with and without the condition. Their cross-sectional study included 576 subjects with suspected OSA who underwent acoustic pharyngometry within 35 days of standard diagnostic polysomnography (Ann Am Thorac Soc. 2016 Aug 16. doi: 10.1513/AnnalsATS.201601-056OC).
“Although the mean [upper airway cross-sectional area] at [functional residual capacity] when sitting was a significant predictor of OSA controlling for important confounders, it had only fair discriminant validity for identifying those with OSA in a clinic population and had no significantly greater discriminant value than the use of clinical variables,” the researchers reported. “Therefore, it is probably of no clinical utility in this setting.”
The investigators said that they had no conflicts of interest.
Assessment of upper airway cross-sectional area using acoustic pharyngometry is no better than the use of clinical variables to diagnose obstructive sleep apnea (OSA), according to a study in the Annals of the American Thoracic Society.
Tetyana Kendzerska, PhD, of the Institute for Clinical Evaluative Sciences, Toronto, and her colleagues found that the median upper airway cross-sectional area at functional residual capacity when sitting was significantly reduced in individuals with OSA, compared with those without the condition (3.3 cm2 vs. 3.7 cm2).
The researchers found that, at a cut-off value of 3.75 cm2, which struck the best balance of sensitivity and specificity, upper airway cross-sectional area had a sensitivity of 73% and specificity of 46%. Varying the apnea-hypopnea index to define OSA or varying the analysis of upper airway cross-sectional area did not improve its predictive or discriminative ability, nor was there any benefit to measuring upper airway cross-sectional area when an individual was supine, compared with sitting.
Dr. Kendzerska and her colleagues had hypothesized that acoustic pharyngometry could play a role in screening for OSA, based on previous studies suggesting significant differences in upper airway cross-sectional area measures in individuals with and without the condition. Their cross-sectional study included 576 subjects with suspected OSA who underwent acoustic pharyngometry within 35 days of standard diagnostic polysomnography (Ann Am Thorac Soc. 2016 Aug 16. doi: 10.1513/AnnalsATS.201601-056OC).
“Although the mean [upper airway cross-sectional area] at [functional residual capacity] when sitting was a significant predictor of OSA controlling for important confounders, it had only fair discriminant validity for identifying those with OSA in a clinic population and had no significantly greater discriminant value than the use of clinical variables,” the researchers reported. “Therefore, it is probably of no clinical utility in this setting.”
The investigators said that they had no conflicts of interest.
Assessment of upper airway cross-sectional area using acoustic pharyngometry is no better than the use of clinical variables to diagnose obstructive sleep apnea (OSA), according to a study in the Annals of the American Thoracic Society.
Tetyana Kendzerska, PhD, of the Institute for Clinical Evaluative Sciences, Toronto, and her colleagues found that the median upper airway cross-sectional area at functional residual capacity when sitting was significantly reduced in individuals with OSA, compared with those without the condition (3.3 cm2 vs. 3.7 cm2).
The researchers found that, at a cut-off value of 3.75 cm2, which struck the best balance of sensitivity and specificity, upper airway cross-sectional area had a sensitivity of 73% and specificity of 46%. Varying the apnea-hypopnea index to define OSA or varying the analysis of upper airway cross-sectional area did not improve its predictive or discriminative ability, nor was there any benefit to measuring upper airway cross-sectional area when an individual was supine, compared with sitting.
Dr. Kendzerska and her colleagues had hypothesized that acoustic pharyngometry could play a role in screening for OSA, based on previous studies suggesting significant differences in upper airway cross-sectional area measures in individuals with and without the condition. Their cross-sectional study included 576 subjects with suspected OSA who underwent acoustic pharyngometry within 35 days of standard diagnostic polysomnography (Ann Am Thorac Soc. 2016 Aug 16. doi: 10.1513/AnnalsATS.201601-056OC).
“Although the mean [upper airway cross-sectional area] at [functional residual capacity] when sitting was a significant predictor of OSA controlling for important confounders, it had only fair discriminant validity for identifying those with OSA in a clinic population and had no significantly greater discriminant value than the use of clinical variables,” the researchers reported. “Therefore, it is probably of no clinical utility in this setting.”
The investigators said that they had no conflicts of interest.
Key clinical point: .
Major finding: The addition of upper airway cross-sectional area to the clinical variables of age; sex; BMI; and heart, kidney, and lung disease only led to a very small and nonsignificant increase in predictive ability for obstructive sleep apnea.
Data source: Cross-sectional study in 576 subjects with suspected obstructive sleep apnea.
Disclosures: No conflicts of interest were declared.
Patient-specific model takes variability out of blood glucose average
Researchers have identified a patient-specific correction factor based on the age of a patient’s red blood cells that can improve the accuracy of average blood glucose estimations from hemoglobin A1c measures in patients with diabetes.
“The true average glucose concentration of a nondiabetic and a poorly controlled diabetic may differ by less than 15 mg/dL, but patients with identical HbA1c values may have true average glucose concentrations that differ by more than 60 mg/dL,” wrote Roy Malka, PhD, a mathematician and research fellow at Massachusetts General Hospital, Boston, and his associates.
In an article published in the Oct. 5 online edition of Science Translational Medicine, the researchers reported the development of a mathematical model for HbA1c formation inside the red blood cell, based on the chemical contributions of glycemic and nonglycemic factors, as well as the average age of a patient’s red blood cells.
Using existing continuous glucose monitoring (CGM) data from four different groups – totaling more than 200 diabetes patients – the researchers then personalized the parameters of the model to each patient to see the impact of patient-specific variation in the relationship between average concentration of glucose in the blood and HbA1c.
Finally, they applied the personalized model to data from each patient to determine its accuracy in estimating future blood glucose from future HbA1c measurements, and compared the blood glucose estimates with those made using the current standard method (Sci Transl Med. 2016, Oct 5. http://stm.sciencemag.org/lookup/doi/10.1126/scitranslmed.aaf9304).
This showed that their patient-specific model reduced the median absolute error in estimated average blood glucose from more than 15 mg/dL to less than 5 mg/dL, representing an error reduction of more than 66%.
“The model would require one pair of CGM-measured AG [average blood glucose] and an HbA1c measurement that would be used to determine the patient’s [mean red blood cell count (MRBC)],” the researchers wrote. “MRBC would then be used going forward to refine the future [average glucose (AG)] calculated on the basis of HbA1c.”
The researchers pointed out that work was still needed to calculate the duration of CGM that would allow sufficient calibration of MRBC. However, their analysis suggested that no more than 30 days would be needed, and significant improvements could be achieved within just 21 days.
In patients with stable monthly glucose averages, the prior month would be enough for calibration, and even a single week of stable weekly glucose averages might be sufficient.
“The improvement in AG calculation afforded by our model should improve medical care and provide for a personalized approach to determining AG from HbA1c.”
The ADAG study was supported by the American Diabetes Association, the European Association for the Study of Diabetes, Abbott Diabetes Care, Bayer Healthcare, GlaxoSmithKline, Sanofi-Aventis Netherlands, Merck, LifeScan, Medtronic MiniMed, and HemoCue. Two authors were supported by the National Institutes of Health, and Abbott Diagnostics. The authors are also listed as inventors on a patent application related to this work submitted by Partners HealthCare.
Researchers have identified a patient-specific correction factor based on the age of a patient’s red blood cells that can improve the accuracy of average blood glucose estimations from hemoglobin A1c measures in patients with diabetes.
“The true average glucose concentration of a nondiabetic and a poorly controlled diabetic may differ by less than 15 mg/dL, but patients with identical HbA1c values may have true average glucose concentrations that differ by more than 60 mg/dL,” wrote Roy Malka, PhD, a mathematician and research fellow at Massachusetts General Hospital, Boston, and his associates.
In an article published in the Oct. 5 online edition of Science Translational Medicine, the researchers reported the development of a mathematical model for HbA1c formation inside the red blood cell, based on the chemical contributions of glycemic and nonglycemic factors, as well as the average age of a patient’s red blood cells.
Using existing continuous glucose monitoring (CGM) data from four different groups – totaling more than 200 diabetes patients – the researchers then personalized the parameters of the model to each patient to see the impact of patient-specific variation in the relationship between average concentration of glucose in the blood and HbA1c.
Finally, they applied the personalized model to data from each patient to determine its accuracy in estimating future blood glucose from future HbA1c measurements, and compared the blood glucose estimates with those made using the current standard method (Sci Transl Med. 2016, Oct 5. http://stm.sciencemag.org/lookup/doi/10.1126/scitranslmed.aaf9304).
This showed that their patient-specific model reduced the median absolute error in estimated average blood glucose from more than 15 mg/dL to less than 5 mg/dL, representing an error reduction of more than 66%.
“The model would require one pair of CGM-measured AG [average blood glucose] and an HbA1c measurement that would be used to determine the patient’s [mean red blood cell count (MRBC)],” the researchers wrote. “MRBC would then be used going forward to refine the future [average glucose (AG)] calculated on the basis of HbA1c.”
The researchers pointed out that work was still needed to calculate the duration of CGM that would allow sufficient calibration of MRBC. However, their analysis suggested that no more than 30 days would be needed, and significant improvements could be achieved within just 21 days.
In patients with stable monthly glucose averages, the prior month would be enough for calibration, and even a single week of stable weekly glucose averages might be sufficient.
“The improvement in AG calculation afforded by our model should improve medical care and provide for a personalized approach to determining AG from HbA1c.”
The ADAG study was supported by the American Diabetes Association, the European Association for the Study of Diabetes, Abbott Diabetes Care, Bayer Healthcare, GlaxoSmithKline, Sanofi-Aventis Netherlands, Merck, LifeScan, Medtronic MiniMed, and HemoCue. Two authors were supported by the National Institutes of Health, and Abbott Diagnostics. The authors are also listed as inventors on a patent application related to this work submitted by Partners HealthCare.
Researchers have identified a patient-specific correction factor based on the age of a patient’s red blood cells that can improve the accuracy of average blood glucose estimations from hemoglobin A1c measures in patients with diabetes.
“The true average glucose concentration of a nondiabetic and a poorly controlled diabetic may differ by less than 15 mg/dL, but patients with identical HbA1c values may have true average glucose concentrations that differ by more than 60 mg/dL,” wrote Roy Malka, PhD, a mathematician and research fellow at Massachusetts General Hospital, Boston, and his associates.
In an article published in the Oct. 5 online edition of Science Translational Medicine, the researchers reported the development of a mathematical model for HbA1c formation inside the red blood cell, based on the chemical contributions of glycemic and nonglycemic factors, as well as the average age of a patient’s red blood cells.
Using existing continuous glucose monitoring (CGM) data from four different groups – totaling more than 200 diabetes patients – the researchers then personalized the parameters of the model to each patient to see the impact of patient-specific variation in the relationship between average concentration of glucose in the blood and HbA1c.
Finally, they applied the personalized model to data from each patient to determine its accuracy in estimating future blood glucose from future HbA1c measurements, and compared the blood glucose estimates with those made using the current standard method (Sci Transl Med. 2016, Oct 5. http://stm.sciencemag.org/lookup/doi/10.1126/scitranslmed.aaf9304).
This showed that their patient-specific model reduced the median absolute error in estimated average blood glucose from more than 15 mg/dL to less than 5 mg/dL, representing an error reduction of more than 66%.
“The model would require one pair of CGM-measured AG [average blood glucose] and an HbA1c measurement that would be used to determine the patient’s [mean red blood cell count (MRBC)],” the researchers wrote. “MRBC would then be used going forward to refine the future [average glucose (AG)] calculated on the basis of HbA1c.”
The researchers pointed out that work was still needed to calculate the duration of CGM that would allow sufficient calibration of MRBC. However, their analysis suggested that no more than 30 days would be needed, and significant improvements could be achieved within just 21 days.
In patients with stable monthly glucose averages, the prior month would be enough for calibration, and even a single week of stable weekly glucose averages might be sufficient.
“The improvement in AG calculation afforded by our model should improve medical care and provide for a personalized approach to determining AG from HbA1c.”
The ADAG study was supported by the American Diabetes Association, the European Association for the Study of Diabetes, Abbott Diabetes Care, Bayer Healthcare, GlaxoSmithKline, Sanofi-Aventis Netherlands, Merck, LifeScan, Medtronic MiniMed, and HemoCue. Two authors were supported by the National Institutes of Health, and Abbott Diagnostics. The authors are also listed as inventors on a patent application related to this work submitted by Partners HealthCare.
Key clinical point:
Major finding: A patient-specific model of the relationship between HbA1c and average blood sugar reduced the median absolute error in estimated average blood glucose from more than 15 mg/dL to less than 5 mg/dL, representing an error reduction of more than 66%.
Data source: Mathematical modeling validated via four sets of patient continuous glucose monitoring data.
Disclosures: The ADAG study was supported by the American Diabetes Association, the European Association for the Study of Diabetes, Abbott Diabetes Care, Bayer Healthcare, GlaxoSmithKline, Sanofi-Aventis Netherlands, Merck, LifeScan, Medtronic MiniMed, and HemoCue. Two authors were supported by the National Institutes of Health, and Abbott Diagnostics. The authors are also listed as inventors on a patent application related to this work submitted by Partners HealthCare.
No increase in CV events with long-acting bronchodilators in COPD
Long-acting bronchodilators, including tiotropium, do not appear to increase the risk of cardiovascular events in the first year of use, according to a study in patients with chronic obstructive pulmonary disease.
Long-acting bronchodilators are recommended as first-line maintenance therapy for chronic obstructive pulmonary disease (COPD), but they can cause cardiac complications, wrote Samy Suissa, PhD, and his colleagues at the Centre for Clinical Epidemiology, Lady Davis Institute, Montreal.
“Indeed, long-acting anticholinergics are believed to suppress parasympathetic control, while LABAs [long-acting beta2-agonists] stimulate sympathetic tone, possibly leading to tachyarrhythmia and coronary insufficiency,” the authors wrote (Chest. 2016 Aug 20. doi: 10.1016/j.chest.2016.08.001). “Furthermore, these pharmacologic effects would be expected to occur immediately at initiation of therapy.”
However, the observational studies and randomized trials comparing the safety of LABAs and the long-acting anticholinergic tiotropium have shown inconclusive results, possibly because of insufficient numbers, short follow-ups or “treatment-experienced” patients.
Dr. Suissa and his colleagues analyzed data from 26,442 new tiotropium users and 26,442 LABA initiators from a U.K. primary care database. Participants in each arm were matched on high-dimensional propensity scores and prior inhaled corticosteroid use, and followed for 1 year for occurrence of acute myocardial infarction, stroke, heart failure, arrhythmia, and pneumonia.
The researchers saw no significant difference between tiotropium and LABA users in the risk of acute myocardial infarction (hazard ratio, 1.10; 95% CI, 0.88-1.38), stroke (HR, 1.02; 95% CI, 0.78-1.34), arrhythmia (HR, 0.81; 95% CI, 0.60-1.09), or heart failure (HR, 0.90; 95% CI, 0.79-1.02). This was the case even when the current exposure time window was varied from 60-day periods to 30- or 90-day periods.
There was a significantly lower incidence of pneumonia in individuals treated with tiotropium (HR, 0.81; 95% CI, 0.72-0.92), which the authors suggested was likely due to the presence of inhaled corticosteroids in many LABAs.
“In our study, 78% of the LABA users were receiving a combined inhaler that included an inhaled corticosteroid, two-thirds of which were for fluticasone, which has been associated with an up to twofold increase in the risk of pneumonia,” they reported.
The authors acknowledged that the presence of an inhaled corticosteroid in combination with many of the LABAs could attract criticism that the study was therefore not a strict comparison between tiotropium and a LABA. However, they noted that the study aimed to represent the real-world experience of clinical practice.
“In this real-world–setting study of the treatment of COPD, the initiation of maintenance treatment with tiotropium compared with a LABA does not increase cardiovascular risk, but reduces significantly the risk of pneumonia, albeit a likely adverse effect of the inhaled corticosteroid component present in many LABA inhalers,” the authors wrote.
“This differential risk that appears to confer a safety advantage to tiotropium as the initial long-acting bronchodilator in COPD should be considered against the comparative effectiveness of these two treatments at initiation,” they noted.
The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Long-acting bronchodilators, including tiotropium, do not appear to increase the risk of cardiovascular events in the first year of use, according to a study in patients with chronic obstructive pulmonary disease.
Long-acting bronchodilators are recommended as first-line maintenance therapy for chronic obstructive pulmonary disease (COPD), but they can cause cardiac complications, wrote Samy Suissa, PhD, and his colleagues at the Centre for Clinical Epidemiology, Lady Davis Institute, Montreal.
“Indeed, long-acting anticholinergics are believed to suppress parasympathetic control, while LABAs [long-acting beta2-agonists] stimulate sympathetic tone, possibly leading to tachyarrhythmia and coronary insufficiency,” the authors wrote (Chest. 2016 Aug 20. doi: 10.1016/j.chest.2016.08.001). “Furthermore, these pharmacologic effects would be expected to occur immediately at initiation of therapy.”
However, the observational studies and randomized trials comparing the safety of LABAs and the long-acting anticholinergic tiotropium have shown inconclusive results, possibly because of insufficient numbers, short follow-ups or “treatment-experienced” patients.
Dr. Suissa and his colleagues analyzed data from 26,442 new tiotropium users and 26,442 LABA initiators from a U.K. primary care database. Participants in each arm were matched on high-dimensional propensity scores and prior inhaled corticosteroid use, and followed for 1 year for occurrence of acute myocardial infarction, stroke, heart failure, arrhythmia, and pneumonia.
The researchers saw no significant difference between tiotropium and LABA users in the risk of acute myocardial infarction (hazard ratio, 1.10; 95% CI, 0.88-1.38), stroke (HR, 1.02; 95% CI, 0.78-1.34), arrhythmia (HR, 0.81; 95% CI, 0.60-1.09), or heart failure (HR, 0.90; 95% CI, 0.79-1.02). This was the case even when the current exposure time window was varied from 60-day periods to 30- or 90-day periods.
There was a significantly lower incidence of pneumonia in individuals treated with tiotropium (HR, 0.81; 95% CI, 0.72-0.92), which the authors suggested was likely due to the presence of inhaled corticosteroids in many LABAs.
“In our study, 78% of the LABA users were receiving a combined inhaler that included an inhaled corticosteroid, two-thirds of which were for fluticasone, which has been associated with an up to twofold increase in the risk of pneumonia,” they reported.
The authors acknowledged that the presence of an inhaled corticosteroid in combination with many of the LABAs could attract criticism that the study was therefore not a strict comparison between tiotropium and a LABA. However, they noted that the study aimed to represent the real-world experience of clinical practice.
“In this real-world–setting study of the treatment of COPD, the initiation of maintenance treatment with tiotropium compared with a LABA does not increase cardiovascular risk, but reduces significantly the risk of pneumonia, albeit a likely adverse effect of the inhaled corticosteroid component present in many LABA inhalers,” the authors wrote.
“This differential risk that appears to confer a safety advantage to tiotropium as the initial long-acting bronchodilator in COPD should be considered against the comparative effectiveness of these two treatments at initiation,” they noted.
The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Long-acting bronchodilators, including tiotropium, do not appear to increase the risk of cardiovascular events in the first year of use, according to a study in patients with chronic obstructive pulmonary disease.
Long-acting bronchodilators are recommended as first-line maintenance therapy for chronic obstructive pulmonary disease (COPD), but they can cause cardiac complications, wrote Samy Suissa, PhD, and his colleagues at the Centre for Clinical Epidemiology, Lady Davis Institute, Montreal.
“Indeed, long-acting anticholinergics are believed to suppress parasympathetic control, while LABAs [long-acting beta2-agonists] stimulate sympathetic tone, possibly leading to tachyarrhythmia and coronary insufficiency,” the authors wrote (Chest. 2016 Aug 20. doi: 10.1016/j.chest.2016.08.001). “Furthermore, these pharmacologic effects would be expected to occur immediately at initiation of therapy.”
However, the observational studies and randomized trials comparing the safety of LABAs and the long-acting anticholinergic tiotropium have shown inconclusive results, possibly because of insufficient numbers, short follow-ups or “treatment-experienced” patients.
Dr. Suissa and his colleagues analyzed data from 26,442 new tiotropium users and 26,442 LABA initiators from a U.K. primary care database. Participants in each arm were matched on high-dimensional propensity scores and prior inhaled corticosteroid use, and followed for 1 year for occurrence of acute myocardial infarction, stroke, heart failure, arrhythmia, and pneumonia.
The researchers saw no significant difference between tiotropium and LABA users in the risk of acute myocardial infarction (hazard ratio, 1.10; 95% CI, 0.88-1.38), stroke (HR, 1.02; 95% CI, 0.78-1.34), arrhythmia (HR, 0.81; 95% CI, 0.60-1.09), or heart failure (HR, 0.90; 95% CI, 0.79-1.02). This was the case even when the current exposure time window was varied from 60-day periods to 30- or 90-day periods.
There was a significantly lower incidence of pneumonia in individuals treated with tiotropium (HR, 0.81; 95% CI, 0.72-0.92), which the authors suggested was likely due to the presence of inhaled corticosteroids in many LABAs.
“In our study, 78% of the LABA users were receiving a combined inhaler that included an inhaled corticosteroid, two-thirds of which were for fluticasone, which has been associated with an up to twofold increase in the risk of pneumonia,” they reported.
The authors acknowledged that the presence of an inhaled corticosteroid in combination with many of the LABAs could attract criticism that the study was therefore not a strict comparison between tiotropium and a LABA. However, they noted that the study aimed to represent the real-world experience of clinical practice.
“In this real-world–setting study of the treatment of COPD, the initiation of maintenance treatment with tiotropium compared with a LABA does not increase cardiovascular risk, but reduces significantly the risk of pneumonia, albeit a likely adverse effect of the inhaled corticosteroid component present in many LABA inhalers,” the authors wrote.
“This differential risk that appears to confer a safety advantage to tiotropium as the initial long-acting bronchodilator in COPD should be considered against the comparative effectiveness of these two treatments at initiation,” they noted.
The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Key clinical point: Long-acting bronchodilators do not appear to increase the risk of cardiovascular events in the first year of use in individuals with chronic obstructive pulmonary disease.
Major finding: Tiotropium and long-acting beta2-agonists were not associated with any significant increases in the risk of acute myocardial infarction, stroke, heart failure, or arrhythmia in the first year of use.
Data source: Population-based cohort study of 26,442 new tiotropium users and 26,442 LABA initiators.
Disclosures: The Canadian Institutes of Health Research, the Canadian Foundation for Innovation, and Boehringer Ingelheim supported the study. One author disclosed ties with Boehringer Ingelheim, AstraZeneca, Novartis, and Pfizer. No other conflicts of interest were declared.
Nonalcoholic fatty liver disease estimated to cost $103 billion annually
Nonalcoholic fatty liver disease (NAFLD) is estimated to affect over 64 million people each year in the United States, leading to medical costs of more than $100 billion, according to a new analysis.
Using a steady-state prevalence model, Zobair M. Younossi, MD, MPH, from the Center for Liver Diseases at Inova Fairfax (Va.) Hospital, and his coauthors, sought to estimate the prevalence and economic burden of NAFLD in the United States, Germany, France, Italy, and the United Kingdom.
Their models, which were calibrated against real-world prevalence rates, predicted an estimated 58 million prevalent cases and 12 million new cases of NAFLD each year in the US alone (Hepatology. 2016 Sep 26. doi: 10.1002/hep.28785).
The models also incorporated the transition of patients between nine health states, from NAFLD through nonalcoholic steatohepatitis (NASH) to NASH fibrosis, compensated and decompensated cirrhosis, hepatocellular carcinoma, liver transplantation, posttransplant, and death.
They forecast an overall prevalence of 64 million cases of NAFLD annually in the United States, which includes more than 5.5 million prevalent cases – and 600,000 incident cases – of NASH. The number of incident cases of NAFLD were highest in the patients aged 45-64 years, while the incident cases of NASH and hepatocellular carcinoma peaked in the patients aged 65 years and older.
The results were proportionally similar for the four European countries, although when it came to the analysis of economic burden, researchers found the direct costs of NAFLD were much higher in the United States.
Overall, NAFLD costs $103 billion each year in the United States, compared with EU 27.7 billion in Germany, France, and Italy, and GBP 5.24 billion in the United Kingdom. The authors attributed these greater costs to a larger population, as well as higher costs of managing disease-related complications.
“However, if we assume the annual rate of increase in the costs due to NAFLD to parallel the annual growth in the prevalence of obesity in the United States since 1994, the expected 10-year burden of NAFLD could increase substantially – to an estimated $1.005 trillion in the United States and EU334 billion in the Europe-4,” they noted.
Total costs were highest in the group aged 45-65 years, but per-patient costs were highest in the group aged 65 years and older, which the authors said reflected the higher proportion of these patients in more advanced stages of disease.
The authors also argued that these cost estimates do not take into account the societal costs related to the loss of quality years of life to NAFLD and its complications.
“By assigning a monetary value to societal costs and adding these to the annual direct cost of NAFLD for the United States and the Europe-4, the total annual cost of NAFLD can be estimated at $292.19 billion and EU227.84 billion, respectively,” they wrote. “Furthermore, these cost calculations do not take into account other indirect costs of NAFLD, which are related to work-productivity loss and its economic impact.”
The study was partly funded by Gilead Sciences. Four authors declared consultancies and advisory positions for the pharmaceutical industry, including Gilead.
Nonalcoholic fatty liver disease (NAFLD) is estimated to affect over 64 million people each year in the United States, leading to medical costs of more than $100 billion, according to a new analysis.
Using a steady-state prevalence model, Zobair M. Younossi, MD, MPH, from the Center for Liver Diseases at Inova Fairfax (Va.) Hospital, and his coauthors, sought to estimate the prevalence and economic burden of NAFLD in the United States, Germany, France, Italy, and the United Kingdom.
Their models, which were calibrated against real-world prevalence rates, predicted an estimated 58 million prevalent cases and 12 million new cases of NAFLD each year in the US alone (Hepatology. 2016 Sep 26. doi: 10.1002/hep.28785).
The models also incorporated the transition of patients between nine health states, from NAFLD through nonalcoholic steatohepatitis (NASH) to NASH fibrosis, compensated and decompensated cirrhosis, hepatocellular carcinoma, liver transplantation, posttransplant, and death.
They forecast an overall prevalence of 64 million cases of NAFLD annually in the United States, which includes more than 5.5 million prevalent cases – and 600,000 incident cases – of NASH. The number of incident cases of NAFLD were highest in the patients aged 45-64 years, while the incident cases of NASH and hepatocellular carcinoma peaked in the patients aged 65 years and older.
The results were proportionally similar for the four European countries, although when it came to the analysis of economic burden, researchers found the direct costs of NAFLD were much higher in the United States.
Overall, NAFLD costs $103 billion each year in the United States, compared with EU 27.7 billion in Germany, France, and Italy, and GBP 5.24 billion in the United Kingdom. The authors attributed these greater costs to a larger population, as well as higher costs of managing disease-related complications.
“However, if we assume the annual rate of increase in the costs due to NAFLD to parallel the annual growth in the prevalence of obesity in the United States since 1994, the expected 10-year burden of NAFLD could increase substantially – to an estimated $1.005 trillion in the United States and EU334 billion in the Europe-4,” they noted.
Total costs were highest in the group aged 45-65 years, but per-patient costs were highest in the group aged 65 years and older, which the authors said reflected the higher proportion of these patients in more advanced stages of disease.
The authors also argued that these cost estimates do not take into account the societal costs related to the loss of quality years of life to NAFLD and its complications.
“By assigning a monetary value to societal costs and adding these to the annual direct cost of NAFLD for the United States and the Europe-4, the total annual cost of NAFLD can be estimated at $292.19 billion and EU227.84 billion, respectively,” they wrote. “Furthermore, these cost calculations do not take into account other indirect costs of NAFLD, which are related to work-productivity loss and its economic impact.”
The study was partly funded by Gilead Sciences. Four authors declared consultancies and advisory positions for the pharmaceutical industry, including Gilead.
Nonalcoholic fatty liver disease (NAFLD) is estimated to affect over 64 million people each year in the United States, leading to medical costs of more than $100 billion, according to a new analysis.
Using a steady-state prevalence model, Zobair M. Younossi, MD, MPH, from the Center for Liver Diseases at Inova Fairfax (Va.) Hospital, and his coauthors, sought to estimate the prevalence and economic burden of NAFLD in the United States, Germany, France, Italy, and the United Kingdom.
Their models, which were calibrated against real-world prevalence rates, predicted an estimated 58 million prevalent cases and 12 million new cases of NAFLD each year in the US alone (Hepatology. 2016 Sep 26. doi: 10.1002/hep.28785).
The models also incorporated the transition of patients between nine health states, from NAFLD through nonalcoholic steatohepatitis (NASH) to NASH fibrosis, compensated and decompensated cirrhosis, hepatocellular carcinoma, liver transplantation, posttransplant, and death.
They forecast an overall prevalence of 64 million cases of NAFLD annually in the United States, which includes more than 5.5 million prevalent cases – and 600,000 incident cases – of NASH. The number of incident cases of NAFLD were highest in the patients aged 45-64 years, while the incident cases of NASH and hepatocellular carcinoma peaked in the patients aged 65 years and older.
The results were proportionally similar for the four European countries, although when it came to the analysis of economic burden, researchers found the direct costs of NAFLD were much higher in the United States.
Overall, NAFLD costs $103 billion each year in the United States, compared with EU 27.7 billion in Germany, France, and Italy, and GBP 5.24 billion in the United Kingdom. The authors attributed these greater costs to a larger population, as well as higher costs of managing disease-related complications.
“However, if we assume the annual rate of increase in the costs due to NAFLD to parallel the annual growth in the prevalence of obesity in the United States since 1994, the expected 10-year burden of NAFLD could increase substantially – to an estimated $1.005 trillion in the United States and EU334 billion in the Europe-4,” they noted.
Total costs were highest in the group aged 45-65 years, but per-patient costs were highest in the group aged 65 years and older, which the authors said reflected the higher proportion of these patients in more advanced stages of disease.
The authors also argued that these cost estimates do not take into account the societal costs related to the loss of quality years of life to NAFLD and its complications.
“By assigning a monetary value to societal costs and adding these to the annual direct cost of NAFLD for the United States and the Europe-4, the total annual cost of NAFLD can be estimated at $292.19 billion and EU227.84 billion, respectively,” they wrote. “Furthermore, these cost calculations do not take into account other indirect costs of NAFLD, which are related to work-productivity loss and its economic impact.”
The study was partly funded by Gilead Sciences. Four authors declared consultancies and advisory positions for the pharmaceutical industry, including Gilead.
FROM HEPATOLOGY
Key clinical point:
Major finding: Models have predicted an estimated 58 million prevalent cases and 12 million new cases of nonalcoholic fatty liver each year in the United States.
Data source: Analysis using a steady-state prevalence model calibrated with real-world prevalence data.
Disclosures: The study was partly funded by Gilead Sciences. Four authors declared consultancies and advisory positions for the pharmaceutical industry, including Gilead.
Congenital Zika syndrome includes range of neurologic abnormalities
Researchers have proposed the term “congenital Zika syndrome” to cover the range of severe damage and developmental abnormalities – including microcephaly – caused by Zika virus infection.
In the Oct. 3 online edition of JAMA Neurology, Adriana Suely de Oliveira Melo, MD, PhD, of the Instituto de Pesquisa Professor Amorim Neto in Campina Grande, Brazil, and her coauthors report on 11 babies with congenital Zika virus infection who were followed from gestation to 6 months of age.
Researchers observed hypoplasia of the cerebellar vermis and cerebellum in nine patients, while MRI and CT imaging also found that all patients showed callosal hypoplasia, reduced cerebral volume, abnormal cortical development, and subcortical calcifications.
Four of the infants showed gyral disorganization, five showed evidence of pachygyria, and two had lissencephaly (JAMA Neurol. 2016 Oct 3. doi: 10.1001/jamaneurol.2016.3720).
“Although there was variable damage resulting from brain lesions associated with [Zika virus] congenital infection, a common pattern of brain atrophy and changes associated with disturbances in neuronal migration were observed,” the authors wrote. “Some patients presented with mild brain atrophy and calcifications, and others presented with more severe malformations, such as the absence of the thalamus and lissencephaly.”
Three of the infants died after delivery, representing a fatality rate of 27.3%. All three were found to have akinesia deformation sequence or arthrogryposis. One of the three pregnancies also involved polyhydramnios, and the infant was delivered at 36 weeks because of severe maternal respiratory distress.
All but one of the pregnant women had reported a skin rash at a median of 9.5 weeks in the pregnancy, suggesting Zika virus infection was acquired early.
Postmortem tissue analysis of two of the infants who died found Zika virus genome in the brain, cerebellum, spinal cord, and lung; a higher viral load in the tissue of one of the infants was associated with more severe brain damage.
Overall, nine patients tested positive for Zika virus using real-time reverse-transcription polymerase chain
reactions during gestation and/or after birth, while two patients only had serologic evidence of infection.
“It was interesting to note that the viral sequences amplified from patients 1 and 7 after birth gained a new substitution, V23I, which is located in the envelope domain I and may be implicated in viral tropism to different tissues.”
The study was supported by Consellho Nacional de Desenvolvimento e Pesquisa, Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, and Prefeitura Municipal de Campina Grande. No conflicts of interest were declared.
Many unanswered questions remain about Zika virus: How frequently does asymptomatic infection or second- and third-trimester infection lead to CNS disease? What are the long-term sequelae of intrauterine Zika virus infection? What is the reason for the substantial size, severity, and unexpected complications of the recent Zika virus outbreak in the Americas, compared with what has been seen with this virus in the past? And a broader question: How many CNS birth defects presently of unclear cause will be found to be virus induced?
It would be valuable to have adult and pediatric neurologists network with the U.S. Centers for Disease Control and Prevention to establish a surveillance system that could track Zika virus–induced Guillain-Barré syndrome and CNS disease. This would facilitate the identification and characterization of disorders, the formation of a registry, and the mounting of comprehensive epidemiological studies.
Dr. Raymond P. Roos is with the Department of Neurology at the University of Chicago. These comments are adapted from an accompanying editorial (JAMA Neurol. 2016 Oct 3. doi: 10.1001/jamaneurol.2016.3677). No conflicts of interest were declared.
Many unanswered questions remain about Zika virus: How frequently does asymptomatic infection or second- and third-trimester infection lead to CNS disease? What are the long-term sequelae of intrauterine Zika virus infection? What is the reason for the substantial size, severity, and unexpected complications of the recent Zika virus outbreak in the Americas, compared with what has been seen with this virus in the past? And a broader question: How many CNS birth defects presently of unclear cause will be found to be virus induced?
It would be valuable to have adult and pediatric neurologists network with the U.S. Centers for Disease Control and Prevention to establish a surveillance system that could track Zika virus–induced Guillain-Barré syndrome and CNS disease. This would facilitate the identification and characterization of disorders, the formation of a registry, and the mounting of comprehensive epidemiological studies.
Dr. Raymond P. Roos is with the Department of Neurology at the University of Chicago. These comments are adapted from an accompanying editorial (JAMA Neurol. 2016 Oct 3. doi: 10.1001/jamaneurol.2016.3677). No conflicts of interest were declared.
Many unanswered questions remain about Zika virus: How frequently does asymptomatic infection or second- and third-trimester infection lead to CNS disease? What are the long-term sequelae of intrauterine Zika virus infection? What is the reason for the substantial size, severity, and unexpected complications of the recent Zika virus outbreak in the Americas, compared with what has been seen with this virus in the past? And a broader question: How many CNS birth defects presently of unclear cause will be found to be virus induced?
It would be valuable to have adult and pediatric neurologists network with the U.S. Centers for Disease Control and Prevention to establish a surveillance system that could track Zika virus–induced Guillain-Barré syndrome and CNS disease. This would facilitate the identification and characterization of disorders, the formation of a registry, and the mounting of comprehensive epidemiological studies.
Dr. Raymond P. Roos is with the Department of Neurology at the University of Chicago. These comments are adapted from an accompanying editorial (JAMA Neurol. 2016 Oct 3. doi: 10.1001/jamaneurol.2016.3677). No conflicts of interest were declared.
Researchers have proposed the term “congenital Zika syndrome” to cover the range of severe damage and developmental abnormalities – including microcephaly – caused by Zika virus infection.
In the Oct. 3 online edition of JAMA Neurology, Adriana Suely de Oliveira Melo, MD, PhD, of the Instituto de Pesquisa Professor Amorim Neto in Campina Grande, Brazil, and her coauthors report on 11 babies with congenital Zika virus infection who were followed from gestation to 6 months of age.
Researchers observed hypoplasia of the cerebellar vermis and cerebellum in nine patients, while MRI and CT imaging also found that all patients showed callosal hypoplasia, reduced cerebral volume, abnormal cortical development, and subcortical calcifications.
Four of the infants showed gyral disorganization, five showed evidence of pachygyria, and two had lissencephaly (JAMA Neurol. 2016 Oct 3. doi: 10.1001/jamaneurol.2016.3720).
“Although there was variable damage resulting from brain lesions associated with [Zika virus] congenital infection, a common pattern of brain atrophy and changes associated with disturbances in neuronal migration were observed,” the authors wrote. “Some patients presented with mild brain atrophy and calcifications, and others presented with more severe malformations, such as the absence of the thalamus and lissencephaly.”
Three of the infants died after delivery, representing a fatality rate of 27.3%. All three were found to have akinesia deformation sequence or arthrogryposis. One of the three pregnancies also involved polyhydramnios, and the infant was delivered at 36 weeks because of severe maternal respiratory distress.
All but one of the pregnant women had reported a skin rash at a median of 9.5 weeks in the pregnancy, suggesting Zika virus infection was acquired early.
Postmortem tissue analysis of two of the infants who died found Zika virus genome in the brain, cerebellum, spinal cord, and lung; a higher viral load in the tissue of one of the infants was associated with more severe brain damage.
Overall, nine patients tested positive for Zika virus using real-time reverse-transcription polymerase chain
reactions during gestation and/or after birth, while two patients only had serologic evidence of infection.
“It was interesting to note that the viral sequences amplified from patients 1 and 7 after birth gained a new substitution, V23I, which is located in the envelope domain I and may be implicated in viral tropism to different tissues.”
The study was supported by Consellho Nacional de Desenvolvimento e Pesquisa, Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, and Prefeitura Municipal de Campina Grande. No conflicts of interest were declared.
Researchers have proposed the term “congenital Zika syndrome” to cover the range of severe damage and developmental abnormalities – including microcephaly – caused by Zika virus infection.
In the Oct. 3 online edition of JAMA Neurology, Adriana Suely de Oliveira Melo, MD, PhD, of the Instituto de Pesquisa Professor Amorim Neto in Campina Grande, Brazil, and her coauthors report on 11 babies with congenital Zika virus infection who were followed from gestation to 6 months of age.
Researchers observed hypoplasia of the cerebellar vermis and cerebellum in nine patients, while MRI and CT imaging also found that all patients showed callosal hypoplasia, reduced cerebral volume, abnormal cortical development, and subcortical calcifications.
Four of the infants showed gyral disorganization, five showed evidence of pachygyria, and two had lissencephaly (JAMA Neurol. 2016 Oct 3. doi: 10.1001/jamaneurol.2016.3720).
“Although there was variable damage resulting from brain lesions associated with [Zika virus] congenital infection, a common pattern of brain atrophy and changes associated with disturbances in neuronal migration were observed,” the authors wrote. “Some patients presented with mild brain atrophy and calcifications, and others presented with more severe malformations, such as the absence of the thalamus and lissencephaly.”
Three of the infants died after delivery, representing a fatality rate of 27.3%. All three were found to have akinesia deformation sequence or arthrogryposis. One of the three pregnancies also involved polyhydramnios, and the infant was delivered at 36 weeks because of severe maternal respiratory distress.
All but one of the pregnant women had reported a skin rash at a median of 9.5 weeks in the pregnancy, suggesting Zika virus infection was acquired early.
Postmortem tissue analysis of two of the infants who died found Zika virus genome in the brain, cerebellum, spinal cord, and lung; a higher viral load in the tissue of one of the infants was associated with more severe brain damage.
Overall, nine patients tested positive for Zika virus using real-time reverse-transcription polymerase chain
reactions during gestation and/or after birth, while two patients only had serologic evidence of infection.
“It was interesting to note that the viral sequences amplified from patients 1 and 7 after birth gained a new substitution, V23I, which is located in the envelope domain I and may be implicated in viral tropism to different tissues.”
The study was supported by Consellho Nacional de Desenvolvimento e Pesquisa, Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, and Prefeitura Municipal de Campina Grande. No conflicts of interest were declared.
Key clinical point:
Major finding: Congenital Zika syndrome is associated with microcephaly, reduced cerebral volume, cerebellar hypoplasia, lissencephaly with hydrocephalus, and fetal akinesia deformation sequence.
Data source: Prospective study of 11 Zika-affected infants followed from gestation to 6 months of age.
Disclosures: The study was supported by Consellho Nacional de Desenvolvimento e Pesquisa, Fundação de Amparo a Pesquisa do Estado do Rio de Janeiro, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, and Prefeitura Municipal de Campina Grande. No conflicts of interest were declared.
Morning sickness linked to lower risk of pregnancy loss
Nausea and vomiting in early pregnancy were associated with a substantially reduced risk of pregnancy loss in a prospective preconception cohort of almost 800 pregnant women.
Although there has long been the suggestion that nausea is a sign of a healthy pregnancy, the evidence supporting this idea has been limited.
“Much of the published literature reports on studies that enrolled women after a clinically recognized pregnancy, thereby failing to include women with early pregnancy losses or relying on participant recall of nausea and/or loss,” wrote Stefanie N. Hinkle, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and her colleagues.
In this study, the researchers examined data from 797 women with one or two prior pregnancy losses and a current pregnancy confirmed by an HCG pregnancy test. They all were enrolled in a randomized clinical trial on the effects of aspirin on gestation and reproduction (JAMA Intern Med. 2016 Sep 26. doi: 10.1001/jamainternmed.2016.5641).
Participants kept a daily record of nausea and vomiting symptoms for gestational weeks 2-8 and then monthly after that. At week 12, 86% of the women reported nausea and 35% reported nausea with vomiting at least once a week in the previous 4 weeks.
Overall, women with nausea and vomiting in any given week had a 75% lower risk of pregnancy loss during that week (hazard ratio, 0.25), while those with only nausea had a 50% reduction in pregnancy loss (HR, 0.50), compared with women with neither symptom.
For women who had a peri-implantation pregnancy loss, the researchers found a similar association but it did not reach statistical significance. The hazard ratio was 0.59 for women who had nausea only and 0.51 for women who experienced nausea with vomiting.
Among women who did not experience a peri-implantation pregnancy loss, nausea only and nausea with vomiting were associated with a 66% (HR, 0.44) and 80% (HR, 0.20) reduction in risk for pregnancy loss, respectively, compared with women with neither symptom. These reductions in risk were similar when the analysis was limited to first-trimester pregnancy loss and persisted even after accounting for lifestyle and fetal factors, such as number of prior pregnancy losses, body-mass index, fetal karyotype, and multiple fetal gestations.
“These findings overcome prior analytic and design limitations and represent the most definitive data available, to our knowledge, indicating the protective association of nausea and vomiting in early pregnancy on the risk for pregnancy loss and thus may provide reassurance to women experiencing these difficult symptoms in pregnancy,” researchers wrote.
The study was supported by the National Institutes of Health. The researchers reported having no financial disclosures.
This study’s contribution to the existing literature is valuable because investigators were able to compare nausea and vomiting among women who experienced an early pregnancy loss with those whose pregnancies continued. Furthermore, by collecting daily urine samples, it was possible to identify all pregnancies very early in gestation and thus definitively quantify the losses that occurred around the time of implantation in addition to those that occurred after ultrasonography.
As common as nausea and vomiting are in the first trimester, researchers and clinicians should be cautious about deeming it to have a protective effect against pregnancy loss. Although such a designation may provide reassurance to some women, they should not be discouraged from seeking treatment for a condition that can have a considerable negative effect on their quality of life.
Siripanth Nippita, MD, and Laura E. Dodge, ScD, are with the department of obstetrics and gynecology at Beth Israel Deaconess Medical Center, Boston. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2016 Sep 26. doi: 10.1001/jamainternmed.2016.6101). They reported having no financial disclosures.
This study’s contribution to the existing literature is valuable because investigators were able to compare nausea and vomiting among women who experienced an early pregnancy loss with those whose pregnancies continued. Furthermore, by collecting daily urine samples, it was possible to identify all pregnancies very early in gestation and thus definitively quantify the losses that occurred around the time of implantation in addition to those that occurred after ultrasonography.
As common as nausea and vomiting are in the first trimester, researchers and clinicians should be cautious about deeming it to have a protective effect against pregnancy loss. Although such a designation may provide reassurance to some women, they should not be discouraged from seeking treatment for a condition that can have a considerable negative effect on their quality of life.
Siripanth Nippita, MD, and Laura E. Dodge, ScD, are with the department of obstetrics and gynecology at Beth Israel Deaconess Medical Center, Boston. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2016 Sep 26. doi: 10.1001/jamainternmed.2016.6101). They reported having no financial disclosures.
This study’s contribution to the existing literature is valuable because investigators were able to compare nausea and vomiting among women who experienced an early pregnancy loss with those whose pregnancies continued. Furthermore, by collecting daily urine samples, it was possible to identify all pregnancies very early in gestation and thus definitively quantify the losses that occurred around the time of implantation in addition to those that occurred after ultrasonography.
As common as nausea and vomiting are in the first trimester, researchers and clinicians should be cautious about deeming it to have a protective effect against pregnancy loss. Although such a designation may provide reassurance to some women, they should not be discouraged from seeking treatment for a condition that can have a considerable negative effect on their quality of life.
Siripanth Nippita, MD, and Laura E. Dodge, ScD, are with the department of obstetrics and gynecology at Beth Israel Deaconess Medical Center, Boston. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2016 Sep 26. doi: 10.1001/jamainternmed.2016.6101). They reported having no financial disclosures.
Nausea and vomiting in early pregnancy were associated with a substantially reduced risk of pregnancy loss in a prospective preconception cohort of almost 800 pregnant women.
Although there has long been the suggestion that nausea is a sign of a healthy pregnancy, the evidence supporting this idea has been limited.
“Much of the published literature reports on studies that enrolled women after a clinically recognized pregnancy, thereby failing to include women with early pregnancy losses or relying on participant recall of nausea and/or loss,” wrote Stefanie N. Hinkle, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and her colleagues.
In this study, the researchers examined data from 797 women with one or two prior pregnancy losses and a current pregnancy confirmed by an HCG pregnancy test. They all were enrolled in a randomized clinical trial on the effects of aspirin on gestation and reproduction (JAMA Intern Med. 2016 Sep 26. doi: 10.1001/jamainternmed.2016.5641).
Participants kept a daily record of nausea and vomiting symptoms for gestational weeks 2-8 and then monthly after that. At week 12, 86% of the women reported nausea and 35% reported nausea with vomiting at least once a week in the previous 4 weeks.
Overall, women with nausea and vomiting in any given week had a 75% lower risk of pregnancy loss during that week (hazard ratio, 0.25), while those with only nausea had a 50% reduction in pregnancy loss (HR, 0.50), compared with women with neither symptom.
For women who had a peri-implantation pregnancy loss, the researchers found a similar association but it did not reach statistical significance. The hazard ratio was 0.59 for women who had nausea only and 0.51 for women who experienced nausea with vomiting.
Among women who did not experience a peri-implantation pregnancy loss, nausea only and nausea with vomiting were associated with a 66% (HR, 0.44) and 80% (HR, 0.20) reduction in risk for pregnancy loss, respectively, compared with women with neither symptom. These reductions in risk were similar when the analysis was limited to first-trimester pregnancy loss and persisted even after accounting for lifestyle and fetal factors, such as number of prior pregnancy losses, body-mass index, fetal karyotype, and multiple fetal gestations.
“These findings overcome prior analytic and design limitations and represent the most definitive data available, to our knowledge, indicating the protective association of nausea and vomiting in early pregnancy on the risk for pregnancy loss and thus may provide reassurance to women experiencing these difficult symptoms in pregnancy,” researchers wrote.
The study was supported by the National Institutes of Health. The researchers reported having no financial disclosures.
Nausea and vomiting in early pregnancy were associated with a substantially reduced risk of pregnancy loss in a prospective preconception cohort of almost 800 pregnant women.
Although there has long been the suggestion that nausea is a sign of a healthy pregnancy, the evidence supporting this idea has been limited.
“Much of the published literature reports on studies that enrolled women after a clinically recognized pregnancy, thereby failing to include women with early pregnancy losses or relying on participant recall of nausea and/or loss,” wrote Stefanie N. Hinkle, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, Md., and her colleagues.
In this study, the researchers examined data from 797 women with one or two prior pregnancy losses and a current pregnancy confirmed by an HCG pregnancy test. They all were enrolled in a randomized clinical trial on the effects of aspirin on gestation and reproduction (JAMA Intern Med. 2016 Sep 26. doi: 10.1001/jamainternmed.2016.5641).
Participants kept a daily record of nausea and vomiting symptoms for gestational weeks 2-8 and then monthly after that. At week 12, 86% of the women reported nausea and 35% reported nausea with vomiting at least once a week in the previous 4 weeks.
Overall, women with nausea and vomiting in any given week had a 75% lower risk of pregnancy loss during that week (hazard ratio, 0.25), while those with only nausea had a 50% reduction in pregnancy loss (HR, 0.50), compared with women with neither symptom.
For women who had a peri-implantation pregnancy loss, the researchers found a similar association but it did not reach statistical significance. The hazard ratio was 0.59 for women who had nausea only and 0.51 for women who experienced nausea with vomiting.
Among women who did not experience a peri-implantation pregnancy loss, nausea only and nausea with vomiting were associated with a 66% (HR, 0.44) and 80% (HR, 0.20) reduction in risk for pregnancy loss, respectively, compared with women with neither symptom. These reductions in risk were similar when the analysis was limited to first-trimester pregnancy loss and persisted even after accounting for lifestyle and fetal factors, such as number of prior pregnancy losses, body-mass index, fetal karyotype, and multiple fetal gestations.
“These findings overcome prior analytic and design limitations and represent the most definitive data available, to our knowledge, indicating the protective association of nausea and vomiting in early pregnancy on the risk for pregnancy loss and thus may provide reassurance to women experiencing these difficult symptoms in pregnancy,” researchers wrote.
The study was supported by the National Institutes of Health. The researchers reported having no financial disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Nausea and vomiting in early pregnancy are associated with a reduced risk of pregnancy loss.
Major finding: Women with nausea and vomiting in any given week had a 75% lower risk of pregnancy loss during that week, while those with nausea only had a 50% reduction in pregnancy loss, compared with women with neither symptom.
Data source: Analysis of data from 797 pregnant women enrolled in a randomized clinical trial on the effects of aspirin on gestation and reproduction.
Disclosures: The study was supported by the National Institutes of Health. The researchers reported having no financial disclosures.
Racial gaps persist in lung cancer trial enrollment
Elderly women, blacks, Asians, Pacific Islanders, and Hispanics are all still underrepresented in lung cancer clinical trials, while gender- and age-based disparities have improved, according to a report published online in Journal of Clinical Oncology.
Herbert H. Pang, PhD, of the Li Ka Shing Faculty of Medicine, Hong Kong, and his coauthors noted that enrollment disparities in cancer clinical trials have existed for many years, with previous research showing underenrollment of the elderly, women, blacks, and racial and ethnic minorities.
In this study, they analyzed data from 23,006 participants in National Cancer Institute lung cancer trials, and 578,476 patients with lung cancer from the SEER registry (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.67.7088).
When they compared the proportion of each subgroup in the trial population with the proportion in the U.S. lung cancer population over time, they noted consistent underrepresentation of blacks, Asian/Pacific Islander, and Hispanic patients across the entire study period.
The enrollment disparity for patients aged 70 years or older with non–small-cell lung cancer improved significantly from 1990 to 2012, but while there has been an increase in the proportion of elderly patients with small-cell lung cancer in the U.S. population from 1990 to 2012, the proportion of elderly patients in trials for small-cell lung cancer remained static.
The authors suggested that this may have been the result of local enrollment patterns for the mostly smaller, phase II trials in small-cell lung cancer, but also the fact that the therapies investigated for small-cell lung cancer may have posed a greater risk of treatment toxicity, which would limit the enrollment of older patients.
Significant improvements were seen in the proportion of women enrolled in lung cancer trials, with the enrollment gap between the genders closing in 2012, although elderly women were still underrepresented in lung cancer clinical trials.
“These findings suggest a beneficial effect of the NIH Revitalization Act of 1993 that mandated the inclusion of women and minorities in all NIH-funded research,” the authors wrote. “However, other important enrollment disparities, especially for older patients with SCLC, elderly women, and racial/ethnic minorities, continue to persist and require ongoing work to eliminate underrepresentation in lung cancer treatment trials.”
Elderly women, blacks, Asians, Pacific Islanders, and Hispanics are all still underrepresented in lung cancer clinical trials, while gender- and age-based disparities have improved, according to a report published online in Journal of Clinical Oncology.
Herbert H. Pang, PhD, of the Li Ka Shing Faculty of Medicine, Hong Kong, and his coauthors noted that enrollment disparities in cancer clinical trials have existed for many years, with previous research showing underenrollment of the elderly, women, blacks, and racial and ethnic minorities.
In this study, they analyzed data from 23,006 participants in National Cancer Institute lung cancer trials, and 578,476 patients with lung cancer from the SEER registry (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.67.7088).
When they compared the proportion of each subgroup in the trial population with the proportion in the U.S. lung cancer population over time, they noted consistent underrepresentation of blacks, Asian/Pacific Islander, and Hispanic patients across the entire study period.
The enrollment disparity for patients aged 70 years or older with non–small-cell lung cancer improved significantly from 1990 to 2012, but while there has been an increase in the proportion of elderly patients with small-cell lung cancer in the U.S. population from 1990 to 2012, the proportion of elderly patients in trials for small-cell lung cancer remained static.
The authors suggested that this may have been the result of local enrollment patterns for the mostly smaller, phase II trials in small-cell lung cancer, but also the fact that the therapies investigated for small-cell lung cancer may have posed a greater risk of treatment toxicity, which would limit the enrollment of older patients.
Significant improvements were seen in the proportion of women enrolled in lung cancer trials, with the enrollment gap between the genders closing in 2012, although elderly women were still underrepresented in lung cancer clinical trials.
“These findings suggest a beneficial effect of the NIH Revitalization Act of 1993 that mandated the inclusion of women and minorities in all NIH-funded research,” the authors wrote. “However, other important enrollment disparities, especially for older patients with SCLC, elderly women, and racial/ethnic minorities, continue to persist and require ongoing work to eliminate underrepresentation in lung cancer treatment trials.”
Elderly women, blacks, Asians, Pacific Islanders, and Hispanics are all still underrepresented in lung cancer clinical trials, while gender- and age-based disparities have improved, according to a report published online in Journal of Clinical Oncology.
Herbert H. Pang, PhD, of the Li Ka Shing Faculty of Medicine, Hong Kong, and his coauthors noted that enrollment disparities in cancer clinical trials have existed for many years, with previous research showing underenrollment of the elderly, women, blacks, and racial and ethnic minorities.
In this study, they analyzed data from 23,006 participants in National Cancer Institute lung cancer trials, and 578,476 patients with lung cancer from the SEER registry (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.67.7088).
When they compared the proportion of each subgroup in the trial population with the proportion in the U.S. lung cancer population over time, they noted consistent underrepresentation of blacks, Asian/Pacific Islander, and Hispanic patients across the entire study period.
The enrollment disparity for patients aged 70 years or older with non–small-cell lung cancer improved significantly from 1990 to 2012, but while there has been an increase in the proportion of elderly patients with small-cell lung cancer in the U.S. population from 1990 to 2012, the proportion of elderly patients in trials for small-cell lung cancer remained static.
The authors suggested that this may have been the result of local enrollment patterns for the mostly smaller, phase II trials in small-cell lung cancer, but also the fact that the therapies investigated for small-cell lung cancer may have posed a greater risk of treatment toxicity, which would limit the enrollment of older patients.
Significant improvements were seen in the proportion of women enrolled in lung cancer trials, with the enrollment gap between the genders closing in 2012, although elderly women were still underrepresented in lung cancer clinical trials.
“These findings suggest a beneficial effect of the NIH Revitalization Act of 1993 that mandated the inclusion of women and minorities in all NIH-funded research,” the authors wrote. “However, other important enrollment disparities, especially for older patients with SCLC, elderly women, and racial/ethnic minorities, continue to persist and require ongoing work to eliminate underrepresentation in lung cancer treatment trials.”
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Elderly women, blacks, Asians, Pacific Islanders, and Hispanics are all still underrepresented in lung cancer clinical trials, while gender- and age-based disparities have improved.
Major finding: There is consistent underrepresentation of blacks, Asian/Pacific Islander, and Hispanic patients in lung cancer clinical trials, but the enrollment gap between genders has closed.
Data source: Analysis of data from 23,006 participants in National Cancer Institute lung cancer trials, and 578,476 patients with lung cancer from the SEER registry.
Disclosures: The study was supported by the National Institutes of Health, National Institute on Aging, and the Health and Medical Research Fund of Hong Kong, and by the National Institute on Aging. Dr. Wang had no disclosures to report; several coauthors reported relationships with various pharmaceutical companies.
Novel GLP-1 receptor agonist shows reduction in cardiovascular risk
The novel glucagonlike peptide 1 (GLP-1) receptor agonist semaglutide may reduce the risk of cardiovascular events in patients with type 2 diabetes who are at elevated cardiovascular risk, according to data presented Sept. 16 at the annual meeting of the European Association for the Study of Diabetes and simultaneously published online in the New England Journal of Medicine.
“In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide,” wrote Steven P. Marso, MD, and his coinvestigators.
SUSTAIN-6 was a randomized, placebo-controlled, noninferiority trial in which 3,297 patients with type 2 diabetes, 85% of whom had established cardiovascular disease, were assigned to take either once-weekly semaglutide (0.5 mg or 1 mg) or placebo.
At the end of the 2-year study period, patients on semaglutide had a statistically significant, 26% lower risk of first occurrence of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, the study’s primary composite outcome, compared with those on placebo (P less than .001), Dr. Marso and his associates wrote. This outcome occurred in 108 of 1,648 patients (6.6%) in the semaglutide group and in 146 of 1,649 patients (8.9%) in the placebo group.
Specifically, the study showed a 26% reduction in the risk of nonfatal MI (P = .12) and 39% reduction in nonfatal stroke (P = .04) with semaglutide, while the rates of cardiovascular death and heart failure hospitalizations were similar between the two arms of the study.
Overall, 60.5% of the patients in the study had a history of cardiovascular disease, and nearly one-third had a history of MI (N Engl J Med. 2016 Sep 16. doi: 10.1056/NEJMoa1607141).
“In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide,” wrote Dr. Marso of the Research Medical Center in Kansas City, Mo., and coauthors. “The beneficial effect of semaglutide on cardiovascular outcomes may relate to modification of the progression of atherosclerosis.”
Semaglutide has a longer duration of action than the approved GLP-1 receptor agonists – liraglutide, exenatide, albiglutide, dulaglutide, and lixisenatide – allowing for once-weekly subcutaneous injection.
Patients enrolled in the study were all on a standard care regimen, but those taking semaglutide showed significant and sustained reductions in hemoglobin A1c levels, compared with placebo, as well as a higher incidence of clinically meaningful and sustained weight loss, and reductions in systolic blood pressure.
The reductions in HbA1c, body weight, and systolic blood pressure may all have contributed to the observed reduction in cardiovascular risk with semaglutide,” the authors noted.
The study did observe significantly higher rates of diabetic retinopathy complications in patients taking semaglutide. The overall incidence of these complications occurred in 50 patients (3.0%) in the semaglutide group and 29 (1.8%) of the placebo patients, yielding a hazard ratio of 1.76 (P = .02). More patients in the semaglutide group required retinal photocoagulation or the use of an intravitreal agent, had a vitreous hemorrhage, or had developed diabetes-related blindness.
However, patients taking semaglutide also had a 36% lower incidence of new or worsening nephropathy (P = .005), and the frequency of serious adverse events was also lower in the semaglutide group than in the placebo patients.
“With the exception of complications of retinopathy, semaglutide had a safety profile similar to that of other GLP-1 receptor agonists,” the authors reported. The rates of malignant neoplasms were similar in both arms of the study, and the rate of pancreatic cancer, which is known to be an event of interest for this class of drugs, was lower in the semaglutide arm, compared with placebo.
Semaglutide is in development and not yet approved for the treatment of type 2 diabetes.
Starting in 2008, all new drug applications to the Food and Drug Administration for antihyperglycemic agents must include evidence that therapy will not increase the risk of cardiovascular events; SUSTAIN-6 (Trial to Evaluate Cardiovascular and Other Long-Term Outcomes With Semaglutide in Subjects with Type 2 Diabetes) was designed to fill that need for semaglutide, and is being developed by Novo Nordisk.
The study was supported by Novo Nordisk. Thirteen authors declared consultancies, grants, fees, and other support from pharmaceutical companies, including Novo Nordisk, and three authors were employees of Novo Nordisk.
SUSTAIN-6 is a carefully planned, well-performed, and objectively reported trial that showed a meaningful reduction in the cardiovascular endpoint of first occurrence of cardiovascular death, nonfatal MI, or stroke of 26%.
Comparing the HbA1c attained across cardiovascular outcome trials of other antihyperglycemic drugs, semaglutide was more efficient in SUSTAIN-6 than in the two cardiovascular outcome trials that have thus far shown cardiovascular benefit, LEADER (N Engl J Med. 2016;375:311-32) in liraglutide and EMPA-REG (N Engl J Med. 2015;373:2117-128) in empagliflozin, lowering HbA1c to 7.3, compared with 7.7 and 8.0, respectively.

|
| Michele G. Sullivan Dr. Lars Rydén |
However, that doesn’t explain the greater absolute risk reduction in the primary outcome of 2.6% in SUSTAIN-6, compared with LEADER (1.9%) and EMPA-REG (1.6), even with a shorter trial duration. But duration of action may hold the key. Semaglutide has a half-life of 7 days, compared with 13 hours for liraglutide and roughly 4 hours for lixisenatide, so perhaps it’s very important to cover the full day before you start to get the impact.
Considering the slow onset of action and the impact on stroke, myocardial infarction, and revascularization, the delay of progress, or regression of atherosclerosis, is likely the important mechanism.
Dr. Lars Rydén is a cardiologist at the Karolinska Institute in Stockholm. He has received research support from Amgen, Bayer AG, Boehringer-Ingelheim, Merck, and Novo Nordisk, the developer of semaglutide. He made these comments as designated discussant for the SUSTAIN-6 report.
SUSTAIN-6 is a carefully planned, well-performed, and objectively reported trial that showed a meaningful reduction in the cardiovascular endpoint of first occurrence of cardiovascular death, nonfatal MI, or stroke of 26%.
Comparing the HbA1c attained across cardiovascular outcome trials of other antihyperglycemic drugs, semaglutide was more efficient in SUSTAIN-6 than in the two cardiovascular outcome trials that have thus far shown cardiovascular benefit, LEADER (N Engl J Med. 2016;375:311-32) in liraglutide and EMPA-REG (N Engl J Med. 2015;373:2117-128) in empagliflozin, lowering HbA1c to 7.3, compared with 7.7 and 8.0, respectively.

|
| Michele G. Sullivan Dr. Lars Rydén |
However, that doesn’t explain the greater absolute risk reduction in the primary outcome of 2.6% in SUSTAIN-6, compared with LEADER (1.9%) and EMPA-REG (1.6), even with a shorter trial duration. But duration of action may hold the key. Semaglutide has a half-life of 7 days, compared with 13 hours for liraglutide and roughly 4 hours for lixisenatide, so perhaps it’s very important to cover the full day before you start to get the impact.
Considering the slow onset of action and the impact on stroke, myocardial infarction, and revascularization, the delay of progress, or regression of atherosclerosis, is likely the important mechanism.
Dr. Lars Rydén is a cardiologist at the Karolinska Institute in Stockholm. He has received research support from Amgen, Bayer AG, Boehringer-Ingelheim, Merck, and Novo Nordisk, the developer of semaglutide. He made these comments as designated discussant for the SUSTAIN-6 report.
SUSTAIN-6 is a carefully planned, well-performed, and objectively reported trial that showed a meaningful reduction in the cardiovascular endpoint of first occurrence of cardiovascular death, nonfatal MI, or stroke of 26%.
Comparing the HbA1c attained across cardiovascular outcome trials of other antihyperglycemic drugs, semaglutide was more efficient in SUSTAIN-6 than in the two cardiovascular outcome trials that have thus far shown cardiovascular benefit, LEADER (N Engl J Med. 2016;375:311-32) in liraglutide and EMPA-REG (N Engl J Med. 2015;373:2117-128) in empagliflozin, lowering HbA1c to 7.3, compared with 7.7 and 8.0, respectively.

|
| Michele G. Sullivan Dr. Lars Rydén |
However, that doesn’t explain the greater absolute risk reduction in the primary outcome of 2.6% in SUSTAIN-6, compared with LEADER (1.9%) and EMPA-REG (1.6), even with a shorter trial duration. But duration of action may hold the key. Semaglutide has a half-life of 7 days, compared with 13 hours for liraglutide and roughly 4 hours for lixisenatide, so perhaps it’s very important to cover the full day before you start to get the impact.
Considering the slow onset of action and the impact on stroke, myocardial infarction, and revascularization, the delay of progress, or regression of atherosclerosis, is likely the important mechanism.
Dr. Lars Rydén is a cardiologist at the Karolinska Institute in Stockholm. He has received research support from Amgen, Bayer AG, Boehringer-Ingelheim, Merck, and Novo Nordisk, the developer of semaglutide. He made these comments as designated discussant for the SUSTAIN-6 report.
The novel glucagonlike peptide 1 (GLP-1) receptor agonist semaglutide may reduce the risk of cardiovascular events in patients with type 2 diabetes who are at elevated cardiovascular risk, according to data presented Sept. 16 at the annual meeting of the European Association for the Study of Diabetes and simultaneously published online in the New England Journal of Medicine.
“In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide,” wrote Steven P. Marso, MD, and his coinvestigators.
SUSTAIN-6 was a randomized, placebo-controlled, noninferiority trial in which 3,297 patients with type 2 diabetes, 85% of whom had established cardiovascular disease, were assigned to take either once-weekly semaglutide (0.5 mg or 1 mg) or placebo.
At the end of the 2-year study period, patients on semaglutide had a statistically significant, 26% lower risk of first occurrence of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, the study’s primary composite outcome, compared with those on placebo (P less than .001), Dr. Marso and his associates wrote. This outcome occurred in 108 of 1,648 patients (6.6%) in the semaglutide group and in 146 of 1,649 patients (8.9%) in the placebo group.
Specifically, the study showed a 26% reduction in the risk of nonfatal MI (P = .12) and 39% reduction in nonfatal stroke (P = .04) with semaglutide, while the rates of cardiovascular death and heart failure hospitalizations were similar between the two arms of the study.
Overall, 60.5% of the patients in the study had a history of cardiovascular disease, and nearly one-third had a history of MI (N Engl J Med. 2016 Sep 16. doi: 10.1056/NEJMoa1607141).
“In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide,” wrote Dr. Marso of the Research Medical Center in Kansas City, Mo., and coauthors. “The beneficial effect of semaglutide on cardiovascular outcomes may relate to modification of the progression of atherosclerosis.”
Semaglutide has a longer duration of action than the approved GLP-1 receptor agonists – liraglutide, exenatide, albiglutide, dulaglutide, and lixisenatide – allowing for once-weekly subcutaneous injection.
Patients enrolled in the study were all on a standard care regimen, but those taking semaglutide showed significant and sustained reductions in hemoglobin A1c levels, compared with placebo, as well as a higher incidence of clinically meaningful and sustained weight loss, and reductions in systolic blood pressure.
The reductions in HbA1c, body weight, and systolic blood pressure may all have contributed to the observed reduction in cardiovascular risk with semaglutide,” the authors noted.
The study did observe significantly higher rates of diabetic retinopathy complications in patients taking semaglutide. The overall incidence of these complications occurred in 50 patients (3.0%) in the semaglutide group and 29 (1.8%) of the placebo patients, yielding a hazard ratio of 1.76 (P = .02). More patients in the semaglutide group required retinal photocoagulation or the use of an intravitreal agent, had a vitreous hemorrhage, or had developed diabetes-related blindness.
However, patients taking semaglutide also had a 36% lower incidence of new or worsening nephropathy (P = .005), and the frequency of serious adverse events was also lower in the semaglutide group than in the placebo patients.
“With the exception of complications of retinopathy, semaglutide had a safety profile similar to that of other GLP-1 receptor agonists,” the authors reported. The rates of malignant neoplasms were similar in both arms of the study, and the rate of pancreatic cancer, which is known to be an event of interest for this class of drugs, was lower in the semaglutide arm, compared with placebo.
Semaglutide is in development and not yet approved for the treatment of type 2 diabetes.
Starting in 2008, all new drug applications to the Food and Drug Administration for antihyperglycemic agents must include evidence that therapy will not increase the risk of cardiovascular events; SUSTAIN-6 (Trial to Evaluate Cardiovascular and Other Long-Term Outcomes With Semaglutide in Subjects with Type 2 Diabetes) was designed to fill that need for semaglutide, and is being developed by Novo Nordisk.
The study was supported by Novo Nordisk. Thirteen authors declared consultancies, grants, fees, and other support from pharmaceutical companies, including Novo Nordisk, and three authors were employees of Novo Nordisk.
The novel glucagonlike peptide 1 (GLP-1) receptor agonist semaglutide may reduce the risk of cardiovascular events in patients with type 2 diabetes who are at elevated cardiovascular risk, according to data presented Sept. 16 at the annual meeting of the European Association for the Study of Diabetes and simultaneously published online in the New England Journal of Medicine.
“In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide,” wrote Steven P. Marso, MD, and his coinvestigators.
SUSTAIN-6 was a randomized, placebo-controlled, noninferiority trial in which 3,297 patients with type 2 diabetes, 85% of whom had established cardiovascular disease, were assigned to take either once-weekly semaglutide (0.5 mg or 1 mg) or placebo.
At the end of the 2-year study period, patients on semaglutide had a statistically significant, 26% lower risk of first occurrence of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, the study’s primary composite outcome, compared with those on placebo (P less than .001), Dr. Marso and his associates wrote. This outcome occurred in 108 of 1,648 patients (6.6%) in the semaglutide group and in 146 of 1,649 patients (8.9%) in the placebo group.
Specifically, the study showed a 26% reduction in the risk of nonfatal MI (P = .12) and 39% reduction in nonfatal stroke (P = .04) with semaglutide, while the rates of cardiovascular death and heart failure hospitalizations were similar between the two arms of the study.
Overall, 60.5% of the patients in the study had a history of cardiovascular disease, and nearly one-third had a history of MI (N Engl J Med. 2016 Sep 16. doi: 10.1056/NEJMoa1607141).
“In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide,” wrote Dr. Marso of the Research Medical Center in Kansas City, Mo., and coauthors. “The beneficial effect of semaglutide on cardiovascular outcomes may relate to modification of the progression of atherosclerosis.”
Semaglutide has a longer duration of action than the approved GLP-1 receptor agonists – liraglutide, exenatide, albiglutide, dulaglutide, and lixisenatide – allowing for once-weekly subcutaneous injection.
Patients enrolled in the study were all on a standard care regimen, but those taking semaglutide showed significant and sustained reductions in hemoglobin A1c levels, compared with placebo, as well as a higher incidence of clinically meaningful and sustained weight loss, and reductions in systolic blood pressure.
The reductions in HbA1c, body weight, and systolic blood pressure may all have contributed to the observed reduction in cardiovascular risk with semaglutide,” the authors noted.
The study did observe significantly higher rates of diabetic retinopathy complications in patients taking semaglutide. The overall incidence of these complications occurred in 50 patients (3.0%) in the semaglutide group and 29 (1.8%) of the placebo patients, yielding a hazard ratio of 1.76 (P = .02). More patients in the semaglutide group required retinal photocoagulation or the use of an intravitreal agent, had a vitreous hemorrhage, or had developed diabetes-related blindness.
However, patients taking semaglutide also had a 36% lower incidence of new or worsening nephropathy (P = .005), and the frequency of serious adverse events was also lower in the semaglutide group than in the placebo patients.
“With the exception of complications of retinopathy, semaglutide had a safety profile similar to that of other GLP-1 receptor agonists,” the authors reported. The rates of malignant neoplasms were similar in both arms of the study, and the rate of pancreatic cancer, which is known to be an event of interest for this class of drugs, was lower in the semaglutide arm, compared with placebo.
Semaglutide is in development and not yet approved for the treatment of type 2 diabetes.
Starting in 2008, all new drug applications to the Food and Drug Administration for antihyperglycemic agents must include evidence that therapy will not increase the risk of cardiovascular events; SUSTAIN-6 (Trial to Evaluate Cardiovascular and Other Long-Term Outcomes With Semaglutide in Subjects with Type 2 Diabetes) was designed to fill that need for semaglutide, and is being developed by Novo Nordisk.
The study was supported by Novo Nordisk. Thirteen authors declared consultancies, grants, fees, and other support from pharmaceutical companies, including Novo Nordisk, and three authors were employees of Novo Nordisk.
AT EASD 2016
Key clinical point: The glucagonlike peptide 1 receptor agonist semaglutide may reduce the risk of cardiovascular events in patients with type 2 diabetes who are at elevated cardiovascular risk.
Major finding: Patients randomized to once-weekly semaglutide had a significant 26% lower risk of first occurrence of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, compared with those on placebo.
Data source: SUSTAIN-6, a randomized, placebo-controlled noninferiority study.
Disclosures: SUSTAIN-6 was supported by Novo Nordisk. Thirteen authors declared consultancies, grants, fees, and other support from pharmaceutical companies, including Novo Nordisk, and three authors were employees of Novo Nordisk.
Antibiotic stewardship lacking at many hospital nurseries
Nearly one-third of hospital newborn nurseries and neonatal ICUs do not have an antibiotic stewardship program, according to a survey of 146 hospital nursery centers across all 50 states.
Researchers randomly selected a level III NICU in each state using the 2014 American Hospital Association annual survey, then selected a level I and level II nursery in the same city. They collected data on the hospital, nursery, and antibiotic stewardship program characteristics and interviewed staff pharmacists and infectious diseases physicians (J Pediatric Infect Dis Soc. 2016 Jul 15. doi: 10.1093/jpids/piw040).
A total of 104 (71%) of responding hospitals had an antibiotic stewardship program in place for their nurseries. Hospitals with a nursery-based antibiotic stewardship programs tended to be larger, have more full-time equivalent staff dedicated to the antibiotic stewardship program, have higher level nurses, and be affiliated with a university, according to Joseph B. Cantey, MD, and his colleagues from the Texas A&M Health Science Center in Temple.
Geographic region and core stewardship strategies did not influence the likelihood of a nursery-based antibiotic stewardship program in place.
From the interviews, the researchers identified several barriers to implementation of antibiotic stewardship programs, and themes such as unwanted coverage, unnecessary coverage, and need for communication.
“Many [antibiotic stewardship program] and nursery representatives stated that nursery [antibiotic stewardship program] coverage was not important, either because antibiotic consumption was perceived as low (theme 1), narrow-spectrum (theme 2), or both,” the authors wrote.
Some nursery providers also argued that participating in stewardship programs was time consuming and not valuable, which the authors said was often related to a lack of pediatric expertise in the program providers. Some of those interviewed also spoke of issues relating to jurisdiction and responsibility for the programs, and there was also a common perception that antibiotic stewardship programs were more concerned with cost savings than patient care.
“Barriers to effective nursery stewardship are exacerbated by lack of communication between stewardship providers and their nursery counterparts,” the authors reported.
No conflicts of interest were declared.
Nearly one-third of hospital newborn nurseries and neonatal ICUs do not have an antibiotic stewardship program, according to a survey of 146 hospital nursery centers across all 50 states.
Researchers randomly selected a level III NICU in each state using the 2014 American Hospital Association annual survey, then selected a level I and level II nursery in the same city. They collected data on the hospital, nursery, and antibiotic stewardship program characteristics and interviewed staff pharmacists and infectious diseases physicians (J Pediatric Infect Dis Soc. 2016 Jul 15. doi: 10.1093/jpids/piw040).
A total of 104 (71%) of responding hospitals had an antibiotic stewardship program in place for their nurseries. Hospitals with a nursery-based antibiotic stewardship programs tended to be larger, have more full-time equivalent staff dedicated to the antibiotic stewardship program, have higher level nurses, and be affiliated with a university, according to Joseph B. Cantey, MD, and his colleagues from the Texas A&M Health Science Center in Temple.
Geographic region and core stewardship strategies did not influence the likelihood of a nursery-based antibiotic stewardship program in place.
From the interviews, the researchers identified several barriers to implementation of antibiotic stewardship programs, and themes such as unwanted coverage, unnecessary coverage, and need for communication.
“Many [antibiotic stewardship program] and nursery representatives stated that nursery [antibiotic stewardship program] coverage was not important, either because antibiotic consumption was perceived as low (theme 1), narrow-spectrum (theme 2), or both,” the authors wrote.
Some nursery providers also argued that participating in stewardship programs was time consuming and not valuable, which the authors said was often related to a lack of pediatric expertise in the program providers. Some of those interviewed also spoke of issues relating to jurisdiction and responsibility for the programs, and there was also a common perception that antibiotic stewardship programs were more concerned with cost savings than patient care.
“Barriers to effective nursery stewardship are exacerbated by lack of communication between stewardship providers and their nursery counterparts,” the authors reported.
No conflicts of interest were declared.
Nearly one-third of hospital newborn nurseries and neonatal ICUs do not have an antibiotic stewardship program, according to a survey of 146 hospital nursery centers across all 50 states.
Researchers randomly selected a level III NICU in each state using the 2014 American Hospital Association annual survey, then selected a level I and level II nursery in the same city. They collected data on the hospital, nursery, and antibiotic stewardship program characteristics and interviewed staff pharmacists and infectious diseases physicians (J Pediatric Infect Dis Soc. 2016 Jul 15. doi: 10.1093/jpids/piw040).
A total of 104 (71%) of responding hospitals had an antibiotic stewardship program in place for their nurseries. Hospitals with a nursery-based antibiotic stewardship programs tended to be larger, have more full-time equivalent staff dedicated to the antibiotic stewardship program, have higher level nurses, and be affiliated with a university, according to Joseph B. Cantey, MD, and his colleagues from the Texas A&M Health Science Center in Temple.
Geographic region and core stewardship strategies did not influence the likelihood of a nursery-based antibiotic stewardship program in place.
From the interviews, the researchers identified several barriers to implementation of antibiotic stewardship programs, and themes such as unwanted coverage, unnecessary coverage, and need for communication.
“Many [antibiotic stewardship program] and nursery representatives stated that nursery [antibiotic stewardship program] coverage was not important, either because antibiotic consumption was perceived as low (theme 1), narrow-spectrum (theme 2), or both,” the authors wrote.
Some nursery providers also argued that participating in stewardship programs was time consuming and not valuable, which the authors said was often related to a lack of pediatric expertise in the program providers. Some of those interviewed also spoke of issues relating to jurisdiction and responsibility for the programs, and there was also a common perception that antibiotic stewardship programs were more concerned with cost savings than patient care.
“Barriers to effective nursery stewardship are exacerbated by lack of communication between stewardship providers and their nursery counterparts,” the authors reported.
No conflicts of interest were declared.
FROM JOURNAL OF THE PEDIATRIC INFECTIOUS DISEASES SOCIETY
Key clinical point: Many hospital newborn nurseries or neonatal ICUs do not have an antibiotic stewardship program in place.
Major finding: 29% of hospital nurseries surveyed did not have an antibiotic stewardship program.
Data source: Survey of 146 hospital nursery centers in 50 states.
Disclosures: No conflicts of interest were declared.