User login
Fourth U.S. case of mcr-1–resistance gene reported
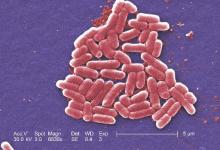
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
A fourth case of bacterial infection harboring the mcr-1 gene has been reported in a child recently returned from a visit to the Caribbean, according to a case report published Sept. 9 in Morbidity and Mortality Weekly Report.
The mcr-1 gene, which confers resistance to the last-resort antibiotic colistin, was first reported in China and is the first plasmid-mediated colistin-resistance mechanism to be identified. Since its discovery in 2015, cases have been reported in Africa, Asia, Europe, South America, and North America.
In this case report, a young patient developed fever and bloody diarrhea 2 days before returning to the United States from a 2-week visit to the Caribbean. The child were treated with the paromomycin and a stool specimen was collected on June 16, with follow-up cultures on June 18 and June 23.
All revealed Escherichia coli O157 harboring mcr-1. The isolates also carried a plasmid blaCMY-2 gene, which confers resistance to third-generation cephalosporins. Stool cultures taken on June 24 and July 1 were negative for E. coli O157 (MMWR. 2016 Sep 9. http://dx.doi.org/10.15585/mmwr.mm6536e3).
Family members in close contact with the patient also were tested; all were found to be negative. Similarly, 16 environmental samples collected from the kitchen and diaper-changing area of the patient’s home were negative for mcr-1.
Researchers reported that the patient was “typically healthy,” and the child’s diet included fruit, dairy products, and meat. While on vacation in the Caribbean, the child ate meat purchased at a live animal market but did not visit the market personally. The child also had contact with a pet dog and cat.
“At this time, CDC recommends that Enterobacteriaceae isolates with a colistin or polymyxin B MIC plus or minus 4 mcg/mL be tested for the presence of mcr-1; testing is available through CDC,” wrote Dr. Amber M. Vasquez and her colleagues from the Centers for Disease Control and Prevention. “Prompt reporting of mcr-1–carrying isolates to public health officials allows for a rapid response to identify transmission and limit further spread.”
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Gluten-free adherence triples while celiac disease prevalence remains stable
The number of people adhering to a gluten-free diet more than tripled between 2009 and 2014, despite the fact that the prevalence of celiac disease has remained largely stable over the same period, according to data from the National Health and Nutrition Examination Survey.
Hyun-seok Kim, MD, MPH, and colleagues from Rutgers New Jersey Medical School noted that there is a popular trend of people choosing gluten-free diets, which exceeds the numbers that would be solely attributable to an increasing prevalence of celiac disease.
In a report published online Sept. 6 in JAMA Internal Medicine, the researchers noted that of 22,278 persons aged 6 years or older for whom data were available on celiac disease status and gluten-free diet status, 106 (0.69%) had a diagnosis of celiac disease, and 213 (1.08%) followed a gluten-free diet but did not have celiac disease.
At a U.S. population level, this would correspond to an estimated 1.76 million individuals with celiac disease, and 2.7 million individuals without celiac disease who follow a gluten-free diet.
The prevalence of celiac disease ranged from 0.70% during 2009-2010, to 0.77% during 2011-2012, and 0.58% during 2013-2014 (JAMA Intern Med. 2016 Sept 6. doi: 10.1001/jamainternmed.2016.5254).
In contrast, the prevalence of a gluten-free diet without celiac disease increased from 0.52% during 2009-2010 to 0.99% during 2011-2012 and 1.69% during 2013-2014, although the increase was even greater among non-Hispanic whites.
“The two trends may be related because gluten consumption has been identified as a risk factor of celiac disease, such that steady or even decreasing gluten consumption may be contributing to a plateau in celiac disease,” they reported.
The authors suggested that there were a number of reasons why individuals without celiac disease might choose to follow a gluten-free diet. “The public perception is that gluten-free diets are healthier and may provide benefits to nonspecific gastrointestinal symptoms,” they wrote, pointing out that gluten-free products are now also more widely available in supermarkets and online.
“There is also an increasing number of individuals with self-diagnosed gluten sensitivity but not the typical enteropathic or serologic features of celiac disease who have improved gastrointestinal health after avoidance of gluten-containing products.”
They stressed that the numbers of individuals in the survey with celiac disease or adhering to a gluten-free diet were relatively small, and that a diagnosis of celiac disease was not confirmed by intestinal biopsy, relying instead on serological tests and prior diagnosis by a health professional.
No conflicts of interest were declared.
Part of what may be driving this gluten-free diet trend is simply a belief, fueled by marketing and media, that these foods are healthier. However, surveys suggest that many individuals who adhere to a gluten-free diet believe that the exclusion of gluten has resulted in subjective health benefits from weight loss to reduced symptoms of inflammation and gastrointestinal distress.
Because a gluten-free diet may have negative social, financial, and health repercussions, it is important for clinicians to understand whether, in most cases, it is the elimination of the protein gluten that is responsible for symptom improvement or whether following a gluten-free diet is simply a marker of other dietary choices that are creating positive effects.
Although the choice to be gluten free may be driven in part by marketing and a misperception that gluten free is healthier, it is important that this choice not be dismissed as an unfounded trend except for those with celiac disease and wheat allergy.
Dr. Daphne Miller is from the department of family and community medicine at the University of California, San Francisco. The comments are taken from an editorial (JAMA Intern Med. 2016 Sept 6. doi: 10.1001/jamainternmed.2016.5271). No conflicts of interest were declared.
Part of what may be driving this gluten-free diet trend is simply a belief, fueled by marketing and media, that these foods are healthier. However, surveys suggest that many individuals who adhere to a gluten-free diet believe that the exclusion of gluten has resulted in subjective health benefits from weight loss to reduced symptoms of inflammation and gastrointestinal distress.
Because a gluten-free diet may have negative social, financial, and health repercussions, it is important for clinicians to understand whether, in most cases, it is the elimination of the protein gluten that is responsible for symptom improvement or whether following a gluten-free diet is simply a marker of other dietary choices that are creating positive effects.
Although the choice to be gluten free may be driven in part by marketing and a misperception that gluten free is healthier, it is important that this choice not be dismissed as an unfounded trend except for those with celiac disease and wheat allergy.
Dr. Daphne Miller is from the department of family and community medicine at the University of California, San Francisco. The comments are taken from an editorial (JAMA Intern Med. 2016 Sept 6. doi: 10.1001/jamainternmed.2016.5271). No conflicts of interest were declared.
Part of what may be driving this gluten-free diet trend is simply a belief, fueled by marketing and media, that these foods are healthier. However, surveys suggest that many individuals who adhere to a gluten-free diet believe that the exclusion of gluten has resulted in subjective health benefits from weight loss to reduced symptoms of inflammation and gastrointestinal distress.
Because a gluten-free diet may have negative social, financial, and health repercussions, it is important for clinicians to understand whether, in most cases, it is the elimination of the protein gluten that is responsible for symptom improvement or whether following a gluten-free diet is simply a marker of other dietary choices that are creating positive effects.
Although the choice to be gluten free may be driven in part by marketing and a misperception that gluten free is healthier, it is important that this choice not be dismissed as an unfounded trend except for those with celiac disease and wheat allergy.
Dr. Daphne Miller is from the department of family and community medicine at the University of California, San Francisco. The comments are taken from an editorial (JAMA Intern Med. 2016 Sept 6. doi: 10.1001/jamainternmed.2016.5271). No conflicts of interest were declared.
The number of people adhering to a gluten-free diet more than tripled between 2009 and 2014, despite the fact that the prevalence of celiac disease has remained largely stable over the same period, according to data from the National Health and Nutrition Examination Survey.
Hyun-seok Kim, MD, MPH, and colleagues from Rutgers New Jersey Medical School noted that there is a popular trend of people choosing gluten-free diets, which exceeds the numbers that would be solely attributable to an increasing prevalence of celiac disease.
In a report published online Sept. 6 in JAMA Internal Medicine, the researchers noted that of 22,278 persons aged 6 years or older for whom data were available on celiac disease status and gluten-free diet status, 106 (0.69%) had a diagnosis of celiac disease, and 213 (1.08%) followed a gluten-free diet but did not have celiac disease.
At a U.S. population level, this would correspond to an estimated 1.76 million individuals with celiac disease, and 2.7 million individuals without celiac disease who follow a gluten-free diet.
The prevalence of celiac disease ranged from 0.70% during 2009-2010, to 0.77% during 2011-2012, and 0.58% during 2013-2014 (JAMA Intern Med. 2016 Sept 6. doi: 10.1001/jamainternmed.2016.5254).
In contrast, the prevalence of a gluten-free diet without celiac disease increased from 0.52% during 2009-2010 to 0.99% during 2011-2012 and 1.69% during 2013-2014, although the increase was even greater among non-Hispanic whites.
“The two trends may be related because gluten consumption has been identified as a risk factor of celiac disease, such that steady or even decreasing gluten consumption may be contributing to a plateau in celiac disease,” they reported.
The authors suggested that there were a number of reasons why individuals without celiac disease might choose to follow a gluten-free diet. “The public perception is that gluten-free diets are healthier and may provide benefits to nonspecific gastrointestinal symptoms,” they wrote, pointing out that gluten-free products are now also more widely available in supermarkets and online.
“There is also an increasing number of individuals with self-diagnosed gluten sensitivity but not the typical enteropathic or serologic features of celiac disease who have improved gastrointestinal health after avoidance of gluten-containing products.”
They stressed that the numbers of individuals in the survey with celiac disease or adhering to a gluten-free diet were relatively small, and that a diagnosis of celiac disease was not confirmed by intestinal biopsy, relying instead on serological tests and prior diagnosis by a health professional.
No conflicts of interest were declared.
The number of people adhering to a gluten-free diet more than tripled between 2009 and 2014, despite the fact that the prevalence of celiac disease has remained largely stable over the same period, according to data from the National Health and Nutrition Examination Survey.
Hyun-seok Kim, MD, MPH, and colleagues from Rutgers New Jersey Medical School noted that there is a popular trend of people choosing gluten-free diets, which exceeds the numbers that would be solely attributable to an increasing prevalence of celiac disease.
In a report published online Sept. 6 in JAMA Internal Medicine, the researchers noted that of 22,278 persons aged 6 years or older for whom data were available on celiac disease status and gluten-free diet status, 106 (0.69%) had a diagnosis of celiac disease, and 213 (1.08%) followed a gluten-free diet but did not have celiac disease.
At a U.S. population level, this would correspond to an estimated 1.76 million individuals with celiac disease, and 2.7 million individuals without celiac disease who follow a gluten-free diet.
The prevalence of celiac disease ranged from 0.70% during 2009-2010, to 0.77% during 2011-2012, and 0.58% during 2013-2014 (JAMA Intern Med. 2016 Sept 6. doi: 10.1001/jamainternmed.2016.5254).
In contrast, the prevalence of a gluten-free diet without celiac disease increased from 0.52% during 2009-2010 to 0.99% during 2011-2012 and 1.69% during 2013-2014, although the increase was even greater among non-Hispanic whites.
“The two trends may be related because gluten consumption has been identified as a risk factor of celiac disease, such that steady or even decreasing gluten consumption may be contributing to a plateau in celiac disease,” they reported.
The authors suggested that there were a number of reasons why individuals without celiac disease might choose to follow a gluten-free diet. “The public perception is that gluten-free diets are healthier and may provide benefits to nonspecific gastrointestinal symptoms,” they wrote, pointing out that gluten-free products are now also more widely available in supermarkets and online.
“There is also an increasing number of individuals with self-diagnosed gluten sensitivity but not the typical enteropathic or serologic features of celiac disease who have improved gastrointestinal health after avoidance of gluten-containing products.”
They stressed that the numbers of individuals in the survey with celiac disease or adhering to a gluten-free diet were relatively small, and that a diagnosis of celiac disease was not confirmed by intestinal biopsy, relying instead on serological tests and prior diagnosis by a health professional.
No conflicts of interest were declared.
FROM JAMA INTERNAL MEDICINE
Key clinical point: The number of people adhering to a gluten-free diet more than tripled between 2009 and 2014, while the prevalence of celiac disease has remained largely stable over the same period.
Major finding: The prevalence of celiac disease ranged from 0.70% during 2009-2010 to 0.58% in 2013-2014, while the prevalence of a gluten-free diet without celiac disease increased from 0.52% in 2009-2010 to 1.69% during 2013-2014.
Data source: Analysis of data from 22,278 participants in the National Health and Nutrition Examination Survey.
Disclosures: No conflicts of interest were disclosed.
September 2016: Click for Credit
Here are 5 articles in the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Women With BRCA1 Mutations at Higher Risk for Endometrial Cancers
To take the posttest, go to: http://bit.ly/2t6SPIY
Expires June 30, 2017
VITALSKey clinical point: Clinicians may wish to discuss the option of hysterectomy at the time of salpingo-oophorectomy in women with deleterious BRCA1 mutations.
Major finding: Among women with BRCA1 but not BRCA2 mutations there was increased risk for serous/serous-like endometrial carcinomas.
Data source: Prospective multicenter follow-up study of 1,083 women with BRCA mutations who underwent salpingo-oophorectomy without hysterectomy.
Disclosures: The study was supported by grants from the Department of Defense, National Institutes of Health, and public and private foundations. Coauthor Robert Soslow, MD, disclosed consulting for EMD Serono. No others reported conflicts of interest. The editorialists reported no conflicts of interest related to the study.
2. Cochrane Review: Topical Steroid—Vitamin D Combo Best for Scalp Psoriasis
To take the posttest, go to: http://bit.ly/2sIyLNI
Expires July 14, 2017
VITALSKey clinical point: The combination of a topical steroid and topical vitamin D is marginally better but with a similar safety profile to steroids alone as a treatment for psoriasis on the scalp.
Major finding: The combination of a topical steroid and vitamin D showed a small but statistically significant advantage over steroids alone, and a greater advantage over vitamin D alone.
Data source: A systematic review of 59 randomized controlled studies in 11,561 patients.
Disclosures: The study was supported by the Universidade Federal de São Paulo, Brazil; the Universidade Federal do Rio Grande do Norte, Brazil; and the National Institute for Health Research, United Kingdom. Six authors and one clinical referee declared speakers' fees, research grants, and funding from the pharmaceutical industry. One author had no conflicts of interest to disclose.
3. Study Finds Emergence of Azithromycin-resistant Gonorrhea
To take the posttest, go to: http://bit.ly/2u1nMmb
Expires July 16, 2017
VITALSKey clinical point:Resistance to azithromycin is emerging among patients diagnosed with gonorrhea.
Major finding: Among patients with gonorrhea, resistance to azithromycin increased from 0.6% in 2013 to 2.5% in 2014, predominantly in the Midwest.
Data source: An analysis of 5,093 Neisseria gonorrhoeae isolates from 27 clinics as part of the CDC's Gonococcal Isolate Surveillance Project.
Disclosures: The researchers had no financial disclosures.
4. Statins Improve Ovarian Cancer Survival
To take the posttest, go to: http://bit.ly/2t6swCF
Expires June 16, 2017
VITALSKey clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
5. Common Surgeries Linked to Chronic Opioid Use Among Opioid-naive Patients
To take the posttest, go to: http://bit.ly/2ub9fFg
Expires June 18, 2017
VITALSKey clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Here are 5 articles in the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Women With BRCA1 Mutations at Higher Risk for Endometrial Cancers
To take the posttest, go to: http://bit.ly/2t6SPIY
Expires June 30, 2017
VITALSKey clinical point: Clinicians may wish to discuss the option of hysterectomy at the time of salpingo-oophorectomy in women with deleterious BRCA1 mutations.
Major finding: Among women with BRCA1 but not BRCA2 mutations there was increased risk for serous/serous-like endometrial carcinomas.
Data source: Prospective multicenter follow-up study of 1,083 women with BRCA mutations who underwent salpingo-oophorectomy without hysterectomy.
Disclosures: The study was supported by grants from the Department of Defense, National Institutes of Health, and public and private foundations. Coauthor Robert Soslow, MD, disclosed consulting for EMD Serono. No others reported conflicts of interest. The editorialists reported no conflicts of interest related to the study.
2. Cochrane Review: Topical Steroid—Vitamin D Combo Best for Scalp Psoriasis
To take the posttest, go to: http://bit.ly/2sIyLNI
Expires July 14, 2017
VITALSKey clinical point: The combination of a topical steroid and topical vitamin D is marginally better but with a similar safety profile to steroids alone as a treatment for psoriasis on the scalp.
Major finding: The combination of a topical steroid and vitamin D showed a small but statistically significant advantage over steroids alone, and a greater advantage over vitamin D alone.
Data source: A systematic review of 59 randomized controlled studies in 11,561 patients.
Disclosures: The study was supported by the Universidade Federal de São Paulo, Brazil; the Universidade Federal do Rio Grande do Norte, Brazil; and the National Institute for Health Research, United Kingdom. Six authors and one clinical referee declared speakers' fees, research grants, and funding from the pharmaceutical industry. One author had no conflicts of interest to disclose.
3. Study Finds Emergence of Azithromycin-resistant Gonorrhea
To take the posttest, go to: http://bit.ly/2u1nMmb
Expires July 16, 2017
VITALSKey clinical point:Resistance to azithromycin is emerging among patients diagnosed with gonorrhea.
Major finding: Among patients with gonorrhea, resistance to azithromycin increased from 0.6% in 2013 to 2.5% in 2014, predominantly in the Midwest.
Data source: An analysis of 5,093 Neisseria gonorrhoeae isolates from 27 clinics as part of the CDC's Gonococcal Isolate Surveillance Project.
Disclosures: The researchers had no financial disclosures.
4. Statins Improve Ovarian Cancer Survival
To take the posttest, go to: http://bit.ly/2t6swCF
Expires June 16, 2017
VITALSKey clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
5. Common Surgeries Linked to Chronic Opioid Use Among Opioid-naive Patients
To take the posttest, go to: http://bit.ly/2ub9fFg
Expires June 18, 2017
VITALSKey clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Here are 5 articles in the August issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Women With BRCA1 Mutations at Higher Risk for Endometrial Cancers
To take the posttest, go to: http://bit.ly/2t6SPIY
Expires June 30, 2017
VITALSKey clinical point: Clinicians may wish to discuss the option of hysterectomy at the time of salpingo-oophorectomy in women with deleterious BRCA1 mutations.
Major finding: Among women with BRCA1 but not BRCA2 mutations there was increased risk for serous/serous-like endometrial carcinomas.
Data source: Prospective multicenter follow-up study of 1,083 women with BRCA mutations who underwent salpingo-oophorectomy without hysterectomy.
Disclosures: The study was supported by grants from the Department of Defense, National Institutes of Health, and public and private foundations. Coauthor Robert Soslow, MD, disclosed consulting for EMD Serono. No others reported conflicts of interest. The editorialists reported no conflicts of interest related to the study.
2. Cochrane Review: Topical Steroid—Vitamin D Combo Best for Scalp Psoriasis
To take the posttest, go to: http://bit.ly/2sIyLNI
Expires July 14, 2017
VITALSKey clinical point: The combination of a topical steroid and topical vitamin D is marginally better but with a similar safety profile to steroids alone as a treatment for psoriasis on the scalp.
Major finding: The combination of a topical steroid and vitamin D showed a small but statistically significant advantage over steroids alone, and a greater advantage over vitamin D alone.
Data source: A systematic review of 59 randomized controlled studies in 11,561 patients.
Disclosures: The study was supported by the Universidade Federal de São Paulo, Brazil; the Universidade Federal do Rio Grande do Norte, Brazil; and the National Institute for Health Research, United Kingdom. Six authors and one clinical referee declared speakers' fees, research grants, and funding from the pharmaceutical industry. One author had no conflicts of interest to disclose.
3. Study Finds Emergence of Azithromycin-resistant Gonorrhea
To take the posttest, go to: http://bit.ly/2u1nMmb
Expires July 16, 2017
VITALSKey clinical point:Resistance to azithromycin is emerging among patients diagnosed with gonorrhea.
Major finding: Among patients with gonorrhea, resistance to azithromycin increased from 0.6% in 2013 to 2.5% in 2014, predominantly in the Midwest.
Data source: An analysis of 5,093 Neisseria gonorrhoeae isolates from 27 clinics as part of the CDC's Gonococcal Isolate Surveillance Project.
Disclosures: The researchers had no financial disclosures.
4. Statins Improve Ovarian Cancer Survival
To take the posttest, go to: http://bit.ly/2t6swCF
Expires June 16, 2017
VITALSKey clinical point: The risk of all-cause mortality in ovarian cancer patients on statin therapy was reduced by one-third.
Major finding: Mean survival in a large cohort of women with stage III ovarian cancer was 5.8 months longer among those on statin therapy.
Data source: A retrospective study of 1,510 women diagnosed with epithelial ovarian cancer during 2007-2009.
Disclosures: Dr. Vogel reported having no financial conflicts regarding this study, conducted without commercial support.
5. Common Surgeries Linked to Chronic Opioid Use Among Opioid-naive Patients
To take the posttest, go to: http://bit.ly/2ub9fFg
Expires June 18, 2017
VITALSKey clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Major depressive disorder increases acute MI risk in HIV
Major depressive disorder is associated with a significant increase in the risk of acute myocardial infarction in adults infected with HIV, even after accounting for existing cardiovascular and HIV-related risk factors, according to research published online Aug. 24 in JAMA Cardiology.
Researchers conducted a retrospective analysis of data from 26,144 HIV-infected veterans participating in the U.S. Department of Veterans Affairs Veterans Aging Cohort Study. Among these veterans, 4,853 (19%) had major depressive disorder and 2,296 (9%) had dysthymic disorder.
After adjustment for cardiovascular risk factors such as hypertension and lipid levels, HIV-infected individuals with major depressive disorder had a 29% higher risk of acute MI compared with HIV-infected individuals without major depressive disorder.
This association remained at the same level but lost its statistical significance after adjustment for hepatitis C infection, renal disease, and alcohol or cocaine dependence (JAMA Cardiology 2016, Aug 24. doi: 10.1001/jamacardio.2016.2716).
Acute myocardial event risk was not significantly increased in HIV-infected individuals with dysthymic disorder, although the hazard ratios themselves were only slightly smaller than those of people with major depressive disorder.
Depression is a known independent risk factor for cardiovascular disease; the authors cited one meta-analysis of 16 studies in the general population that suggested a 57% increase in cardiovascular risk associated with depression.
“Similar to the general population, MDD may be independently associated with incident atherosclerotic CVD in the HIV infected population,” wrote Tasneem Khambaty, PhD, of the University of Miami, and coauthors.
“Given the greater risk for CVD of HIV-infected adults and adults with depression separately and the high prevalence (24%-40%) of depressive disorders in those with HIV, a key remaining question is the following: Is depression independently associated with incident atherosclerotic CVD in the HIV infected population?” the authors asked.
The same mechanisms that increase the risk of cardiovascular disease with depression in the general population also appear to be at play in individuals with HIV, the authors said.
Certain HIV medications such as efavirenz have been independently associated with depression, suicidality, and an increased risk of acute MI events, although researchers said this would not have accounted for the increase in risk observed in this study.
The Veterans Aging Cohort Study was funded by the National Institute on Alcohol Abuse and Alcoholism, and Veterans Health Administration Public Health Strategic Health Core Group, and this analysis was partly supported by funding from the National Institutes of Health. Two authors declared grants and other funding from pharmaceutical companies, two declared grants from the National Institutes of Health, and one author disclosed a grant from General Electric. No other conflicts of interest were disclosed.
Major depressive disorder is associated with a significant increase in the risk of acute myocardial infarction in adults infected with HIV, even after accounting for existing cardiovascular and HIV-related risk factors, according to research published online Aug. 24 in JAMA Cardiology.
Researchers conducted a retrospective analysis of data from 26,144 HIV-infected veterans participating in the U.S. Department of Veterans Affairs Veterans Aging Cohort Study. Among these veterans, 4,853 (19%) had major depressive disorder and 2,296 (9%) had dysthymic disorder.
After adjustment for cardiovascular risk factors such as hypertension and lipid levels, HIV-infected individuals with major depressive disorder had a 29% higher risk of acute MI compared with HIV-infected individuals without major depressive disorder.
This association remained at the same level but lost its statistical significance after adjustment for hepatitis C infection, renal disease, and alcohol or cocaine dependence (JAMA Cardiology 2016, Aug 24. doi: 10.1001/jamacardio.2016.2716).
Acute myocardial event risk was not significantly increased in HIV-infected individuals with dysthymic disorder, although the hazard ratios themselves were only slightly smaller than those of people with major depressive disorder.
Depression is a known independent risk factor for cardiovascular disease; the authors cited one meta-analysis of 16 studies in the general population that suggested a 57% increase in cardiovascular risk associated with depression.
“Similar to the general population, MDD may be independently associated with incident atherosclerotic CVD in the HIV infected population,” wrote Tasneem Khambaty, PhD, of the University of Miami, and coauthors.
“Given the greater risk for CVD of HIV-infected adults and adults with depression separately and the high prevalence (24%-40%) of depressive disorders in those with HIV, a key remaining question is the following: Is depression independently associated with incident atherosclerotic CVD in the HIV infected population?” the authors asked.
The same mechanisms that increase the risk of cardiovascular disease with depression in the general population also appear to be at play in individuals with HIV, the authors said.
Certain HIV medications such as efavirenz have been independently associated with depression, suicidality, and an increased risk of acute MI events, although researchers said this would not have accounted for the increase in risk observed in this study.
The Veterans Aging Cohort Study was funded by the National Institute on Alcohol Abuse and Alcoholism, and Veterans Health Administration Public Health Strategic Health Core Group, and this analysis was partly supported by funding from the National Institutes of Health. Two authors declared grants and other funding from pharmaceutical companies, two declared grants from the National Institutes of Health, and one author disclosed a grant from General Electric. No other conflicts of interest were disclosed.
Major depressive disorder is associated with a significant increase in the risk of acute myocardial infarction in adults infected with HIV, even after accounting for existing cardiovascular and HIV-related risk factors, according to research published online Aug. 24 in JAMA Cardiology.
Researchers conducted a retrospective analysis of data from 26,144 HIV-infected veterans participating in the U.S. Department of Veterans Affairs Veterans Aging Cohort Study. Among these veterans, 4,853 (19%) had major depressive disorder and 2,296 (9%) had dysthymic disorder.
After adjustment for cardiovascular risk factors such as hypertension and lipid levels, HIV-infected individuals with major depressive disorder had a 29% higher risk of acute MI compared with HIV-infected individuals without major depressive disorder.
This association remained at the same level but lost its statistical significance after adjustment for hepatitis C infection, renal disease, and alcohol or cocaine dependence (JAMA Cardiology 2016, Aug 24. doi: 10.1001/jamacardio.2016.2716).
Acute myocardial event risk was not significantly increased in HIV-infected individuals with dysthymic disorder, although the hazard ratios themselves were only slightly smaller than those of people with major depressive disorder.
Depression is a known independent risk factor for cardiovascular disease; the authors cited one meta-analysis of 16 studies in the general population that suggested a 57% increase in cardiovascular risk associated with depression.
“Similar to the general population, MDD may be independently associated with incident atherosclerotic CVD in the HIV infected population,” wrote Tasneem Khambaty, PhD, of the University of Miami, and coauthors.
“Given the greater risk for CVD of HIV-infected adults and adults with depression separately and the high prevalence (24%-40%) of depressive disorders in those with HIV, a key remaining question is the following: Is depression independently associated with incident atherosclerotic CVD in the HIV infected population?” the authors asked.
The same mechanisms that increase the risk of cardiovascular disease with depression in the general population also appear to be at play in individuals with HIV, the authors said.
Certain HIV medications such as efavirenz have been independently associated with depression, suicidality, and an increased risk of acute MI events, although researchers said this would not have accounted for the increase in risk observed in this study.
The Veterans Aging Cohort Study was funded by the National Institute on Alcohol Abuse and Alcoholism, and Veterans Health Administration Public Health Strategic Health Core Group, and this analysis was partly supported by funding from the National Institutes of Health. Two authors declared grants and other funding from pharmaceutical companies, two declared grants from the National Institutes of Health, and one author disclosed a grant from General Electric. No other conflicts of interest were disclosed.
FROM JAMA Cardiology
Key clinical point: Major depressive disorder is associated with a significant increase in the risk of acute myocardial infarction in adults infected with HIV, even after accounting for existing cardiovascular risk factors.
Major finding: HIV-infected individuals with major depressive disorder have a 29% increased risk of acute MI compared to HIV-infected individuals without major depressive disorder.
Data source: Analysis of data from 26,144 HIV-infected veterans participating in the U.S. Department of Veterans Affairs Veterans Aging Cohort Study.
Disclosures: The Veterans Aging Cohort Study was funded by the National Institute on Alcohol Abuse and Alcoholism, and Veterans Health Administration Public Health Strategic Health Core Group, while this analysis was partly supported by funding from the National Institutes of Health. Two authors declared grants and other funding from pharmaceutical companies, two declared grants from the National Institutes of Health, and one author declared a grant from General Electric.
AHA: Limit children’s added sugar intake to 25 g/day
The American Heart Association has set its sights on the high levels of sugar in children’s diets, recommending that consumption of added sugars be limited to 25 grams or less per day to minimize the increased risk of cardiovascular disease, according to a scientific statement published Aug. 22 in Circulation.
“In part because of the lack of clarity and consensus on how much sugar is considered safe for children, sugars remain a commonly added ingredient in foods and drinks, and overall consumption by children and adults remains high,” wrote Miriam B. Vos, MD, of Emory University, Atlanta, and her coauthors.
The group conducted a literature search of the available evidence on sugar intake and its effects on blood pressure, lipids, insulin resistance and diabetes mellitus, nonalcoholic fatty liver disease, and obesity. They also used dietary data from the 2009-2012 National Health and Nutrition Examination Survey (NHANES) to estimate added sugar consumption (Circulation 2016 Aug 22. doi: 10.1161/cir.0000000000000439).
The NHANES data revealed that on average, 2- to 5-year-olds consume 53.3 g of added sugar, defined as all sugars used as ingredients in processed and prepared foods, eaten separately or added to foods at the table, per day; 6- to 11-year-olds consume 78.7 grams a day; and 12- to 19-year-olds consume 92.9 grams per day.
The writing group found there was evidence supporting links between added sugars and increased energy intake, adiposity, central adiposity, and dyslipidemia, which are all known risk factors for cardiovascular disease. They also found that added sugars were particularly harmful when introduced during infancy.
In particular, they found that consumption of sugar-sweetened beverages was strongly associated with an increased risk of obesity across all ages, and there was also a clear dose-response relationship between increased sugar consumption and increased cardiovascular risk.
Based on this, they recommended that children and adolescents drink no more than one 8-oz. sugar-sweetened beverage per week, and limit their overall added sugar intake to 25 g (around 6 teaspoons) or less per day, while added sugars should be avoided entirely for children aged under 2 years.
The group also identified significant gaps in the literature around certain issues such as whether there is a lower threshold for added sugars below which there is no negative impact on cardiovascular health, whether added sugars in food are better or worse than added sugars in drinks, and whether the sugars in 100% fruit juice have biological and cardiovascular effects in children that are similar to those of added sugars in sugar-sweetened beverages.
“Although added sugars can mostly likely be safely consumed in low amounts as part of a healthy diet, little research has been done to establish a threshold between adverse effects and health, making this an important future research topic,” wrote Dr. Vos and her colleagues.
One author reported a consultancy to the Milk Processor Education Program, and another reported having advised the Sugar Board. No other conflicts of interest were declared.
The American Heart Association has set its sights on the high levels of sugar in children’s diets, recommending that consumption of added sugars be limited to 25 grams or less per day to minimize the increased risk of cardiovascular disease, according to a scientific statement published Aug. 22 in Circulation.
“In part because of the lack of clarity and consensus on how much sugar is considered safe for children, sugars remain a commonly added ingredient in foods and drinks, and overall consumption by children and adults remains high,” wrote Miriam B. Vos, MD, of Emory University, Atlanta, and her coauthors.
The group conducted a literature search of the available evidence on sugar intake and its effects on blood pressure, lipids, insulin resistance and diabetes mellitus, nonalcoholic fatty liver disease, and obesity. They also used dietary data from the 2009-2012 National Health and Nutrition Examination Survey (NHANES) to estimate added sugar consumption (Circulation 2016 Aug 22. doi: 10.1161/cir.0000000000000439).
The NHANES data revealed that on average, 2- to 5-year-olds consume 53.3 g of added sugar, defined as all sugars used as ingredients in processed and prepared foods, eaten separately or added to foods at the table, per day; 6- to 11-year-olds consume 78.7 grams a day; and 12- to 19-year-olds consume 92.9 grams per day.
The writing group found there was evidence supporting links between added sugars and increased energy intake, adiposity, central adiposity, and dyslipidemia, which are all known risk factors for cardiovascular disease. They also found that added sugars were particularly harmful when introduced during infancy.
In particular, they found that consumption of sugar-sweetened beverages was strongly associated with an increased risk of obesity across all ages, and there was also a clear dose-response relationship between increased sugar consumption and increased cardiovascular risk.
Based on this, they recommended that children and adolescents drink no more than one 8-oz. sugar-sweetened beverage per week, and limit their overall added sugar intake to 25 g (around 6 teaspoons) or less per day, while added sugars should be avoided entirely for children aged under 2 years.
The group also identified significant gaps in the literature around certain issues such as whether there is a lower threshold for added sugars below which there is no negative impact on cardiovascular health, whether added sugars in food are better or worse than added sugars in drinks, and whether the sugars in 100% fruit juice have biological and cardiovascular effects in children that are similar to those of added sugars in sugar-sweetened beverages.
“Although added sugars can mostly likely be safely consumed in low amounts as part of a healthy diet, little research has been done to establish a threshold between adverse effects and health, making this an important future research topic,” wrote Dr. Vos and her colleagues.
One author reported a consultancy to the Milk Processor Education Program, and another reported having advised the Sugar Board. No other conflicts of interest were declared.
The American Heart Association has set its sights on the high levels of sugar in children’s diets, recommending that consumption of added sugars be limited to 25 grams or less per day to minimize the increased risk of cardiovascular disease, according to a scientific statement published Aug. 22 in Circulation.
“In part because of the lack of clarity and consensus on how much sugar is considered safe for children, sugars remain a commonly added ingredient in foods and drinks, and overall consumption by children and adults remains high,” wrote Miriam B. Vos, MD, of Emory University, Atlanta, and her coauthors.
The group conducted a literature search of the available evidence on sugar intake and its effects on blood pressure, lipids, insulin resistance and diabetes mellitus, nonalcoholic fatty liver disease, and obesity. They also used dietary data from the 2009-2012 National Health and Nutrition Examination Survey (NHANES) to estimate added sugar consumption (Circulation 2016 Aug 22. doi: 10.1161/cir.0000000000000439).
The NHANES data revealed that on average, 2- to 5-year-olds consume 53.3 g of added sugar, defined as all sugars used as ingredients in processed and prepared foods, eaten separately or added to foods at the table, per day; 6- to 11-year-olds consume 78.7 grams a day; and 12- to 19-year-olds consume 92.9 grams per day.
The writing group found there was evidence supporting links between added sugars and increased energy intake, adiposity, central adiposity, and dyslipidemia, which are all known risk factors for cardiovascular disease. They also found that added sugars were particularly harmful when introduced during infancy.
In particular, they found that consumption of sugar-sweetened beverages was strongly associated with an increased risk of obesity across all ages, and there was also a clear dose-response relationship between increased sugar consumption and increased cardiovascular risk.
Based on this, they recommended that children and adolescents drink no more than one 8-oz. sugar-sweetened beverage per week, and limit their overall added sugar intake to 25 g (around 6 teaspoons) or less per day, while added sugars should be avoided entirely for children aged under 2 years.
The group also identified significant gaps in the literature around certain issues such as whether there is a lower threshold for added sugars below which there is no negative impact on cardiovascular health, whether added sugars in food are better or worse than added sugars in drinks, and whether the sugars in 100% fruit juice have biological and cardiovascular effects in children that are similar to those of added sugars in sugar-sweetened beverages.
“Although added sugars can mostly likely be safely consumed in low amounts as part of a healthy diet, little research has been done to establish a threshold between adverse effects and health, making this an important future research topic,” wrote Dr. Vos and her colleagues.
One author reported a consultancy to the Milk Processor Education Program, and another reported having advised the Sugar Board. No other conflicts of interest were declared.
FROM CIRCULATION
Key clinical point: The American Heart Association has recommended that children consume no more than 25 grams of added sugar per day and that added sugars be avoided altogether for children aged under 2 years to limit the consequences for cardiovascular health.
Major finding: On average, American children consume 80 grams of added sugar per day, and increased added sugar consumption is associated with increased adiposity, central adiposity, and dyslipidemia.
Data source: Scientific statement from the American Heart Association.
Disclosures: One author reported a consultancy to the Milk Processor Education Program, and another reported having advised the Sugar Board. No other conflicts of interest were declared.
TEP hernia repair patients have significant QOL improvements
The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation, results of a large prospective study indicate.
Researchers assessed 293 patients – 93% of whom were male – who underwent laparoscopic totally extraperitoneal (TEP) groin hernia repair, both before and 3 weeks, 6 months, 1 year, and 2 years after their operation, using the 36-Item Short Form Survey (v2), Surgical Outcomes Measurement System, and Carolinas Comfort Scale.
The study, published in the July issue of the Journal of the American College of Surgeons, found that 98% of individuals reported no or nonbothersome symptoms of sensation of mesh, 95% reported the same for pain, and 97% reported the same for movement limitations when assessed using the Carolinas Comfort Scale 2 years after surgery.
Pain scores, as measured by the Surgical Outcomes Measurement System, also improved significantly from baseline to 2 years after surgery (10 vs. 7.5; P = .025), and at all postoperative points, patients said they were highly satisfied with their quality of life.
“This study found that laparoscopic TEP groin hernia repair improves patient quality of life significantly, as evidenced by two generic and one procedure-specific quality of life instruments,” wrote Matthew E. Gitelis and his colleagues at the department of surgery at NorthShore University HealthSystem, Evanston, Ill. “Additionally, the procedure can be performed safely with minimal morbidity and low recurrence rates.”
According to the 36-Item Short Form Survey, patients showed significant improvements in physical functioning at 2 years after surgery, but not at 3 weeks, 6 months, or 1 year postoperatively. Pain scores initially increased at 3 weeks after surgery, compared with baseline, decreased to baseline levels at 6 months, then improved significantly at 1 and 2 years after surgery.
While surgery did not appear to affect energy/fatigue scores or emotional well-being, patients did report significant improvements in social functioning and role limitations (J Am Coll Surg. 2016 Jul;223:153-161). On average, patients used narcotic pain medication for 2.5 days after surgery, and returned to work and daily activities after 5.4 days.
The study also examined the technical outcomes of the operations, which were all performed by four surgeons specializing in minimally invasive and bariatric surgery at three sites across an academic-affiliated hospital system.
The authors said the decision was made to study the outcomes from more experienced surgeons because of the steep learning curves and specialized skill set required for laparoscopic techniques.
“Looking at the technical outcomes of our cohort as they relate to recurrence rates and complications, we continue to show the importance of reporting the experience of high-volume centers,” they wrote. “Our goal is to better understand the details and duration of quality of life outcomes so that we can better address patient expectations and provide important information used in the decision-making process for patients undergoing an elective procedure.”
There were 66 complications overall, most of which were from seroma (25 patients), hematoma (13 patients), and urinary retention (21 patients), with 7 cases of wound infection reported. Eight patients (2.2%) experienced a hernia recurrence.
“It is worth noting that, in the middle of our study, in an effort to decrease long-term postoperative pain, we switched to lighter-weight mesh (Physiomesh) from the polyester mesh (Parietex anatomical) used previously,” the authors reported. “Carolinas Comfort Scale scores at 1 year did confirm decreased pain scores; however, we also saw significantly higher rates of recurrence during that period.”
No conflicts of interest were declared.
The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation, results of a large prospective study indicate.
Researchers assessed 293 patients – 93% of whom were male – who underwent laparoscopic totally extraperitoneal (TEP) groin hernia repair, both before and 3 weeks, 6 months, 1 year, and 2 years after their operation, using the 36-Item Short Form Survey (v2), Surgical Outcomes Measurement System, and Carolinas Comfort Scale.
The study, published in the July issue of the Journal of the American College of Surgeons, found that 98% of individuals reported no or nonbothersome symptoms of sensation of mesh, 95% reported the same for pain, and 97% reported the same for movement limitations when assessed using the Carolinas Comfort Scale 2 years after surgery.
Pain scores, as measured by the Surgical Outcomes Measurement System, also improved significantly from baseline to 2 years after surgery (10 vs. 7.5; P = .025), and at all postoperative points, patients said they were highly satisfied with their quality of life.
“This study found that laparoscopic TEP groin hernia repair improves patient quality of life significantly, as evidenced by two generic and one procedure-specific quality of life instruments,” wrote Matthew E. Gitelis and his colleagues at the department of surgery at NorthShore University HealthSystem, Evanston, Ill. “Additionally, the procedure can be performed safely with minimal morbidity and low recurrence rates.”
According to the 36-Item Short Form Survey, patients showed significant improvements in physical functioning at 2 years after surgery, but not at 3 weeks, 6 months, or 1 year postoperatively. Pain scores initially increased at 3 weeks after surgery, compared with baseline, decreased to baseline levels at 6 months, then improved significantly at 1 and 2 years after surgery.
While surgery did not appear to affect energy/fatigue scores or emotional well-being, patients did report significant improvements in social functioning and role limitations (J Am Coll Surg. 2016 Jul;223:153-161). On average, patients used narcotic pain medication for 2.5 days after surgery, and returned to work and daily activities after 5.4 days.
The study also examined the technical outcomes of the operations, which were all performed by four surgeons specializing in minimally invasive and bariatric surgery at three sites across an academic-affiliated hospital system.
The authors said the decision was made to study the outcomes from more experienced surgeons because of the steep learning curves and specialized skill set required for laparoscopic techniques.
“Looking at the technical outcomes of our cohort as they relate to recurrence rates and complications, we continue to show the importance of reporting the experience of high-volume centers,” they wrote. “Our goal is to better understand the details and duration of quality of life outcomes so that we can better address patient expectations and provide important information used in the decision-making process for patients undergoing an elective procedure.”
There were 66 complications overall, most of which were from seroma (25 patients), hematoma (13 patients), and urinary retention (21 patients), with 7 cases of wound infection reported. Eight patients (2.2%) experienced a hernia recurrence.
“It is worth noting that, in the middle of our study, in an effort to decrease long-term postoperative pain, we switched to lighter-weight mesh (Physiomesh) from the polyester mesh (Parietex anatomical) used previously,” the authors reported. “Carolinas Comfort Scale scores at 1 year did confirm decreased pain scores; however, we also saw significantly higher rates of recurrence during that period.”
No conflicts of interest were declared.
The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation, results of a large prospective study indicate.
Researchers assessed 293 patients – 93% of whom were male – who underwent laparoscopic totally extraperitoneal (TEP) groin hernia repair, both before and 3 weeks, 6 months, 1 year, and 2 years after their operation, using the 36-Item Short Form Survey (v2), Surgical Outcomes Measurement System, and Carolinas Comfort Scale.
The study, published in the July issue of the Journal of the American College of Surgeons, found that 98% of individuals reported no or nonbothersome symptoms of sensation of mesh, 95% reported the same for pain, and 97% reported the same for movement limitations when assessed using the Carolinas Comfort Scale 2 years after surgery.
Pain scores, as measured by the Surgical Outcomes Measurement System, also improved significantly from baseline to 2 years after surgery (10 vs. 7.5; P = .025), and at all postoperative points, patients said they were highly satisfied with their quality of life.
“This study found that laparoscopic TEP groin hernia repair improves patient quality of life significantly, as evidenced by two generic and one procedure-specific quality of life instruments,” wrote Matthew E. Gitelis and his colleagues at the department of surgery at NorthShore University HealthSystem, Evanston, Ill. “Additionally, the procedure can be performed safely with minimal morbidity and low recurrence rates.”
According to the 36-Item Short Form Survey, patients showed significant improvements in physical functioning at 2 years after surgery, but not at 3 weeks, 6 months, or 1 year postoperatively. Pain scores initially increased at 3 weeks after surgery, compared with baseline, decreased to baseline levels at 6 months, then improved significantly at 1 and 2 years after surgery.
While surgery did not appear to affect energy/fatigue scores or emotional well-being, patients did report significant improvements in social functioning and role limitations (J Am Coll Surg. 2016 Jul;223:153-161). On average, patients used narcotic pain medication for 2.5 days after surgery, and returned to work and daily activities after 5.4 days.
The study also examined the technical outcomes of the operations, which were all performed by four surgeons specializing in minimally invasive and bariatric surgery at three sites across an academic-affiliated hospital system.
The authors said the decision was made to study the outcomes from more experienced surgeons because of the steep learning curves and specialized skill set required for laparoscopic techniques.
“Looking at the technical outcomes of our cohort as they relate to recurrence rates and complications, we continue to show the importance of reporting the experience of high-volume centers,” they wrote. “Our goal is to better understand the details and duration of quality of life outcomes so that we can better address patient expectations and provide important information used in the decision-making process for patients undergoing an elective procedure.”
There were 66 complications overall, most of which were from seroma (25 patients), hematoma (13 patients), and urinary retention (21 patients), with 7 cases of wound infection reported. Eight patients (2.2%) experienced a hernia recurrence.
“It is worth noting that, in the middle of our study, in an effort to decrease long-term postoperative pain, we switched to lighter-weight mesh (Physiomesh) from the polyester mesh (Parietex anatomical) used previously,” the authors reported. “Carolinas Comfort Scale scores at 1 year did confirm decreased pain scores; however, we also saw significantly higher rates of recurrence during that period.”
No conflicts of interest were declared.
FROM JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: The majority of patients who have undergone laparoscopic totally extraperitoneal groin hernia repair report mild or no symptoms 2 years after the operation.
Major finding: More 90% of patients experience no or nonbothersome symptoms of sensation of mesh, pain or movement limitations at 2 years after laparoscopic totally extraperitoneal groin hernia repair.
Data source: Prospective study in 293 patients undergoing laparoscopic totally extraperitoneal groin hernia repair.
Disclosures: No conflicts of interest were declared.
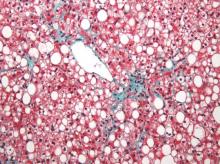
Metabolic factors link NAFLD with carotid atherosclerosis
Nonalcoholic fatty liver disease (NAFLD) is associated with a significant increase in the risk of carotid atherosclerosis that appears to be mediated by metabolic factors, according to a retrospective cohort study published in Gastroenterology.
The study of 8,020 adult Korean men without carotid atherosclerosis at baseline showed that men with persistent NAFLD had a 13% greater risk of subclinical carotid atherosclerosis compared with those without NAFLD, after adjustment for age, smoking, alcohol, body mass index, and weight change (95% confidence interval [CI], 1.13-1.35, P less than .001).
However, this increase in risk was entirely accounted for by metabolic variables including systolic blood pressure, fasting blood glucose, LDL and HDL cholesterol, and triglycerides (Gastroenterology 2016; http://dx.doi.org/10.1053/j.gastro.2016.06.001).
The analysis also showed a significant relationship between the degree of fibrosis and the risk of atherosclerosis; individuals with an NAFLD fibrosis score greater than –1.455 had a 29% higher risk of subclinical carotid atherosclerosis compared to those with a score less than –1.455. Those with a high FIB-4 score had a 43% greater risk of atherosclerosis than did those with a low FIB-4 score, even after adjustment for metabolic factors.
Individuals with a high gamma-glutamyl transferase level also had a higher risk of subclinical carotid atherosclerosis, but this became nonsignificant after adjustment for metabolic variables.
“Although the primary abnormality in NAFLD affects liver structure and function and may result in cirrhosis, liver failure, and hepatocellular carcinoma, the clinical burden of NAFLD is not confined to liver-related morbidity and mortality,” wrote Dong Hyun Sinn, MD, PhD, of Samsung Medical Center in Seoul, South Korea, and coauthors. “In our study, the association of persistent NAFLD with the development of carotid atherosclerosis was attenuated after adjusting for metabolic risk factors.”
Overall, 16.8% of individuals with persistent NAFLD developed subclinical carotid atherosclerosis over 3 years, compared to 11.4% of those with regressed NAFLD, 12.2% with developed NAFLD and 13.6% of those with no NAFLD.
The authors noted that regression of NAFLD appeared to reduce the risk of subclinical carotid atherosclerosis to a level that was comparable to that of individuals without NAFLD at baseline.
“This observation highlights the importance of persistent NAFLD as a risk factor and suggests that resolution of NAFLD may reduce the risk of atherosclerotic CVD,” they wrote. “Because lifestyle changes reduce CVD risk, it is possible that the reduced risk of CVD among participants with resolved NAFLD in the present study may be the consequence of lifestyle changes and not the direct consequence of NAFLD resolution.”
No conflicts of interest were declared.
Nonalcoholic fatty liver disease (NAFLD) is associated with a significant increase in the risk of carotid atherosclerosis that appears to be mediated by metabolic factors, according to a retrospective cohort study published in Gastroenterology.
The study of 8,020 adult Korean men without carotid atherosclerosis at baseline showed that men with persistent NAFLD had a 13% greater risk of subclinical carotid atherosclerosis compared with those without NAFLD, after adjustment for age, smoking, alcohol, body mass index, and weight change (95% confidence interval [CI], 1.13-1.35, P less than .001).
However, this increase in risk was entirely accounted for by metabolic variables including systolic blood pressure, fasting blood glucose, LDL and HDL cholesterol, and triglycerides (Gastroenterology 2016; http://dx.doi.org/10.1053/j.gastro.2016.06.001).
The analysis also showed a significant relationship between the degree of fibrosis and the risk of atherosclerosis; individuals with an NAFLD fibrosis score greater than –1.455 had a 29% higher risk of subclinical carotid atherosclerosis compared to those with a score less than –1.455. Those with a high FIB-4 score had a 43% greater risk of atherosclerosis than did those with a low FIB-4 score, even after adjustment for metabolic factors.
Individuals with a high gamma-glutamyl transferase level also had a higher risk of subclinical carotid atherosclerosis, but this became nonsignificant after adjustment for metabolic variables.
“Although the primary abnormality in NAFLD affects liver structure and function and may result in cirrhosis, liver failure, and hepatocellular carcinoma, the clinical burden of NAFLD is not confined to liver-related morbidity and mortality,” wrote Dong Hyun Sinn, MD, PhD, of Samsung Medical Center in Seoul, South Korea, and coauthors. “In our study, the association of persistent NAFLD with the development of carotid atherosclerosis was attenuated after adjusting for metabolic risk factors.”
Overall, 16.8% of individuals with persistent NAFLD developed subclinical carotid atherosclerosis over 3 years, compared to 11.4% of those with regressed NAFLD, 12.2% with developed NAFLD and 13.6% of those with no NAFLD.
The authors noted that regression of NAFLD appeared to reduce the risk of subclinical carotid atherosclerosis to a level that was comparable to that of individuals without NAFLD at baseline.
“This observation highlights the importance of persistent NAFLD as a risk factor and suggests that resolution of NAFLD may reduce the risk of atherosclerotic CVD,” they wrote. “Because lifestyle changes reduce CVD risk, it is possible that the reduced risk of CVD among participants with resolved NAFLD in the present study may be the consequence of lifestyle changes and not the direct consequence of NAFLD resolution.”
No conflicts of interest were declared.
Nonalcoholic fatty liver disease (NAFLD) is associated with a significant increase in the risk of carotid atherosclerosis that appears to be mediated by metabolic factors, according to a retrospective cohort study published in Gastroenterology.
The study of 8,020 adult Korean men without carotid atherosclerosis at baseline showed that men with persistent NAFLD had a 13% greater risk of subclinical carotid atherosclerosis compared with those without NAFLD, after adjustment for age, smoking, alcohol, body mass index, and weight change (95% confidence interval [CI], 1.13-1.35, P less than .001).
However, this increase in risk was entirely accounted for by metabolic variables including systolic blood pressure, fasting blood glucose, LDL and HDL cholesterol, and triglycerides (Gastroenterology 2016; http://dx.doi.org/10.1053/j.gastro.2016.06.001).
The analysis also showed a significant relationship between the degree of fibrosis and the risk of atherosclerosis; individuals with an NAFLD fibrosis score greater than –1.455 had a 29% higher risk of subclinical carotid atherosclerosis compared to those with a score less than –1.455. Those with a high FIB-4 score had a 43% greater risk of atherosclerosis than did those with a low FIB-4 score, even after adjustment for metabolic factors.
Individuals with a high gamma-glutamyl transferase level also had a higher risk of subclinical carotid atherosclerosis, but this became nonsignificant after adjustment for metabolic variables.
“Although the primary abnormality in NAFLD affects liver structure and function and may result in cirrhosis, liver failure, and hepatocellular carcinoma, the clinical burden of NAFLD is not confined to liver-related morbidity and mortality,” wrote Dong Hyun Sinn, MD, PhD, of Samsung Medical Center in Seoul, South Korea, and coauthors. “In our study, the association of persistent NAFLD with the development of carotid atherosclerosis was attenuated after adjusting for metabolic risk factors.”
Overall, 16.8% of individuals with persistent NAFLD developed subclinical carotid atherosclerosis over 3 years, compared to 11.4% of those with regressed NAFLD, 12.2% with developed NAFLD and 13.6% of those with no NAFLD.
The authors noted that regression of NAFLD appeared to reduce the risk of subclinical carotid atherosclerosis to a level that was comparable to that of individuals without NAFLD at baseline.
“This observation highlights the importance of persistent NAFLD as a risk factor and suggests that resolution of NAFLD may reduce the risk of atherosclerotic CVD,” they wrote. “Because lifestyle changes reduce CVD risk, it is possible that the reduced risk of CVD among participants with resolved NAFLD in the present study may be the consequence of lifestyle changes and not the direct consequence of NAFLD resolution.”
No conflicts of interest were declared.
FROM GASTROENTEROLOGY
Key clinical point: Nonalcoholic fatty liver disease is associated with a significant increase in the risk of carotid atherosclerosis that appears to be mediated by metabolic factors.
Major finding: Men with persistent nonalcoholic fatty liver disease have a 13% greater risk of subclinical carotid atherosclerosis compared with those without NAFLD, but this association disappears after adjustment for metabolic variables such as cholesterol and blood glucose levels.
Data source: Retrospective cohort study of 8,020 adult men without carotid atherosclerosis at baseline.
Disclosures: No conflicts of interest were declared.
Psychotropic drug use similar in cosmetic and medical dermatology patients
The use of psychotropic medications was similar between patients seeking cosmetic dermatology treatment and those presenting with medical dermatologic conditions in a study published in the Journal of Drugs in Dermatology.
A retrospective chart review of 154 adult female patients presenting for cosmetic dermatology and 156 presenting for medical reasons to a suburban dermatology private practice found that 26.8% of the cosmetic group and 22.2% of the medical group reported taking psychotropic medications (P = .09).
The most common medication type was a selective serotonin reuptake inhibitor antidepressant, reported Dr. Heather K. Hamilton, a dermatologist in Chestnut Hill, Mass., at the time of the study, and her associates. An SSRI was used by 23 patients (56.1%) in the cosmetic group and 25 (71.4%) of the general dermatology patients, followed by benzodiazepines, tricyclic antidepressants, and attention-deficit/hyperactivity disorder medications (J Drugs Dermatol. 2016; 15 9[7]:858-61).
The study also found no significant difference between the two groups in self-reported record of a psychiatric disorder, with four such cases in the medical group and six in the cosmetic group (P = .139).
Cosmetic patients presenting for appearance-related dermatologic therapy are often perceived as being more difficult to satisfy than those with dermatologic problems, the authors noted. “While the reasons for this perception are many, some have hypothesized that this may be related to a higher rate of anxiety, mild depression, or body image issues among this patient population,” they wrote.
The authors referred to the high proportion of patients in both groups taking psychotropic medications in the study, a finding that was “even more striking” since the study excluded patients with conditions known to be associated with psychopathology, such as vitiligo, psoriasis, and neurotic excoriations.
“This finding serves as a reminder that we should take full medical histories as mental health may play a role in compliance and satisfaction with treatment,” the authors stated.
They acknowledged that there were limitations of the study, including using psychotropic medication as a marker for mental health problems and the use of self-reported data.
No conflicts of interest were declared. Dr. Hamilton now practices outside of New York.
The use of psychotropic medications was similar between patients seeking cosmetic dermatology treatment and those presenting with medical dermatologic conditions in a study published in the Journal of Drugs in Dermatology.
A retrospective chart review of 154 adult female patients presenting for cosmetic dermatology and 156 presenting for medical reasons to a suburban dermatology private practice found that 26.8% of the cosmetic group and 22.2% of the medical group reported taking psychotropic medications (P = .09).
The most common medication type was a selective serotonin reuptake inhibitor antidepressant, reported Dr. Heather K. Hamilton, a dermatologist in Chestnut Hill, Mass., at the time of the study, and her associates. An SSRI was used by 23 patients (56.1%) in the cosmetic group and 25 (71.4%) of the general dermatology patients, followed by benzodiazepines, tricyclic antidepressants, and attention-deficit/hyperactivity disorder medications (J Drugs Dermatol. 2016; 15 9[7]:858-61).
The study also found no significant difference between the two groups in self-reported record of a psychiatric disorder, with four such cases in the medical group and six in the cosmetic group (P = .139).
Cosmetic patients presenting for appearance-related dermatologic therapy are often perceived as being more difficult to satisfy than those with dermatologic problems, the authors noted. “While the reasons for this perception are many, some have hypothesized that this may be related to a higher rate of anxiety, mild depression, or body image issues among this patient population,” they wrote.
The authors referred to the high proportion of patients in both groups taking psychotropic medications in the study, a finding that was “even more striking” since the study excluded patients with conditions known to be associated with psychopathology, such as vitiligo, psoriasis, and neurotic excoriations.
“This finding serves as a reminder that we should take full medical histories as mental health may play a role in compliance and satisfaction with treatment,” the authors stated.
They acknowledged that there were limitations of the study, including using psychotropic medication as a marker for mental health problems and the use of self-reported data.
No conflicts of interest were declared. Dr. Hamilton now practices outside of New York.
The use of psychotropic medications was similar between patients seeking cosmetic dermatology treatment and those presenting with medical dermatologic conditions in a study published in the Journal of Drugs in Dermatology.
A retrospective chart review of 154 adult female patients presenting for cosmetic dermatology and 156 presenting for medical reasons to a suburban dermatology private practice found that 26.8% of the cosmetic group and 22.2% of the medical group reported taking psychotropic medications (P = .09).
The most common medication type was a selective serotonin reuptake inhibitor antidepressant, reported Dr. Heather K. Hamilton, a dermatologist in Chestnut Hill, Mass., at the time of the study, and her associates. An SSRI was used by 23 patients (56.1%) in the cosmetic group and 25 (71.4%) of the general dermatology patients, followed by benzodiazepines, tricyclic antidepressants, and attention-deficit/hyperactivity disorder medications (J Drugs Dermatol. 2016; 15 9[7]:858-61).
The study also found no significant difference between the two groups in self-reported record of a psychiatric disorder, with four such cases in the medical group and six in the cosmetic group (P = .139).
Cosmetic patients presenting for appearance-related dermatologic therapy are often perceived as being more difficult to satisfy than those with dermatologic problems, the authors noted. “While the reasons for this perception are many, some have hypothesized that this may be related to a higher rate of anxiety, mild depression, or body image issues among this patient population,” they wrote.
The authors referred to the high proportion of patients in both groups taking psychotropic medications in the study, a finding that was “even more striking” since the study excluded patients with conditions known to be associated with psychopathology, such as vitiligo, psoriasis, and neurotic excoriations.
“This finding serves as a reminder that we should take full medical histories as mental health may play a role in compliance and satisfaction with treatment,” the authors stated.
They acknowledged that there were limitations of the study, including using psychotropic medication as a marker for mental health problems and the use of self-reported data.
No conflicts of interest were declared. Dr. Hamilton now practices outside of New York.
FROM JOURNAL OF DRUGS IN DERMATOLOGY
Key clinical point: The use of psychotropic medications is high among cosmetic and medical dermatology patients.
Major finding: About one-quarter of patients presenting for cosmetic or medical dermatology consultations reported taking psychotropic medications.
Data source: A retrospective chart review of 154 adult female patients presenting for cosmetic dermatology and 156 presenting for medical reasons at a suburban comprehensive dermatology private practice.
Disclosures: No conflicts of interest were declared.
Links found between NAFLD, type 2 diabetes, and NASH in children
Nearly one in three children with nonalcoholic fatty liver disease have abnormal glucose metabolism, and this co-morbidity is also associated with a greater risk of nonalcoholic steatohepatitis, according to a cross-sectional study published online Aug. 1 in JAMA Pediatrics.
The study used data from 675 children with biopsy-confirmed nonalcoholic fatty liver disease (NAFLD) who were enrolled in the NASH Clinical Research Network. The mean age of the children was 12.6 years, and they had a mean BMI of 32.5. Most of the children in the study were boys and Hispanic.
Overall, 23.4% of study participants had prediabetes and 6.5% met the clinical criteria for type 2 diabetes. However, girls with NAFLD had a 60% greater risk of prediabetes and a fivefold greater risk of type 2 diabetes than boys, even after controlling for BMI and waist circumference (JAMA Pediatr. 2016 Aug 1. doi: 10.1001/jamapediatrics.2016.1971), reported Dr. Kimberly P. Newton and her coauthors.
The researchers also noted a significant association between nonalcoholic steatohepatitis (NASH) and glucose metabolism. Individuals with type 2 diabetes were three times more likely to also have NASH, while those with prediabetes had a 90% higher incidence of NASH, compared with individuals with normal glucose metabolism. They also found that those with NASH had significantly higher mean fasting glucose and insulin concentrations than children without NASH.
Dr. Newton, of the University of California, San Diego, and her coauthors wrote that while abnormal glucose metabolism is known to be common in adults with NAFLD, and that type diabetes is a risk factor for progression to NASH and liver-related mortality, the association in children with NAFLD is less well understood.
“Among our cohort, the prevalence of children with type 2 diabetes was much higher than would be expected based on contributions from obesity alone,” they wrote. “Although systemic insulin resistance is believed be important in the pathogenesis of both pediatric NAFLD and type 2 diabetes, to our knowledge, there are no longitudinal studies that evaluate the cause-effect relationship between these two associated conditions.”
The authors drew particular attention to the threefold higher odds of NASH in children with NAFLD and type 2 diabetes, pointing out that while the prognostic implications of NASH in childhood are not fully known, the NASH phenotype is associated with a “substantially” greater risk of cirrhosis. This risk is likely to be compounded by the presence of type 2 diabetes.
“Our study advances the literature by showing that as early as childhood, prediabetes and type 2 diabetes emerge as clear risk factors for NASH with potential downstream implications for future morbidity and mortality.”
Commenting on the greater incidence of prediabetes and type 2 diabetes among girls with NAFLD, the authors said this had been observed in other studies and that sex differences represented a major unmet research need.
The Nonalcoholic Steatohepatitis Clinical Research Network is supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Additional support was received from the National Center for Advancing Translational Sciences. The researchers reported no conflicts of interest.
Nearly one in three children with nonalcoholic fatty liver disease have abnormal glucose metabolism, and this co-morbidity is also associated with a greater risk of nonalcoholic steatohepatitis, according to a cross-sectional study published online Aug. 1 in JAMA Pediatrics.
The study used data from 675 children with biopsy-confirmed nonalcoholic fatty liver disease (NAFLD) who were enrolled in the NASH Clinical Research Network. The mean age of the children was 12.6 years, and they had a mean BMI of 32.5. Most of the children in the study were boys and Hispanic.
Overall, 23.4% of study participants had prediabetes and 6.5% met the clinical criteria for type 2 diabetes. However, girls with NAFLD had a 60% greater risk of prediabetes and a fivefold greater risk of type 2 diabetes than boys, even after controlling for BMI and waist circumference (JAMA Pediatr. 2016 Aug 1. doi: 10.1001/jamapediatrics.2016.1971), reported Dr. Kimberly P. Newton and her coauthors.
The researchers also noted a significant association between nonalcoholic steatohepatitis (NASH) and glucose metabolism. Individuals with type 2 diabetes were three times more likely to also have NASH, while those with prediabetes had a 90% higher incidence of NASH, compared with individuals with normal glucose metabolism. They also found that those with NASH had significantly higher mean fasting glucose and insulin concentrations than children without NASH.
Dr. Newton, of the University of California, San Diego, and her coauthors wrote that while abnormal glucose metabolism is known to be common in adults with NAFLD, and that type diabetes is a risk factor for progression to NASH and liver-related mortality, the association in children with NAFLD is less well understood.
“Among our cohort, the prevalence of children with type 2 diabetes was much higher than would be expected based on contributions from obesity alone,” they wrote. “Although systemic insulin resistance is believed be important in the pathogenesis of both pediatric NAFLD and type 2 diabetes, to our knowledge, there are no longitudinal studies that evaluate the cause-effect relationship between these two associated conditions.”
The authors drew particular attention to the threefold higher odds of NASH in children with NAFLD and type 2 diabetes, pointing out that while the prognostic implications of NASH in childhood are not fully known, the NASH phenotype is associated with a “substantially” greater risk of cirrhosis. This risk is likely to be compounded by the presence of type 2 diabetes.
“Our study advances the literature by showing that as early as childhood, prediabetes and type 2 diabetes emerge as clear risk factors for NASH with potential downstream implications for future morbidity and mortality.”
Commenting on the greater incidence of prediabetes and type 2 diabetes among girls with NAFLD, the authors said this had been observed in other studies and that sex differences represented a major unmet research need.
The Nonalcoholic Steatohepatitis Clinical Research Network is supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Additional support was received from the National Center for Advancing Translational Sciences. The researchers reported no conflicts of interest.
Nearly one in three children with nonalcoholic fatty liver disease have abnormal glucose metabolism, and this co-morbidity is also associated with a greater risk of nonalcoholic steatohepatitis, according to a cross-sectional study published online Aug. 1 in JAMA Pediatrics.
The study used data from 675 children with biopsy-confirmed nonalcoholic fatty liver disease (NAFLD) who were enrolled in the NASH Clinical Research Network. The mean age of the children was 12.6 years, and they had a mean BMI of 32.5. Most of the children in the study were boys and Hispanic.
Overall, 23.4% of study participants had prediabetes and 6.5% met the clinical criteria for type 2 diabetes. However, girls with NAFLD had a 60% greater risk of prediabetes and a fivefold greater risk of type 2 diabetes than boys, even after controlling for BMI and waist circumference (JAMA Pediatr. 2016 Aug 1. doi: 10.1001/jamapediatrics.2016.1971), reported Dr. Kimberly P. Newton and her coauthors.
The researchers also noted a significant association between nonalcoholic steatohepatitis (NASH) and glucose metabolism. Individuals with type 2 diabetes were three times more likely to also have NASH, while those with prediabetes had a 90% higher incidence of NASH, compared with individuals with normal glucose metabolism. They also found that those with NASH had significantly higher mean fasting glucose and insulin concentrations than children without NASH.
Dr. Newton, of the University of California, San Diego, and her coauthors wrote that while abnormal glucose metabolism is known to be common in adults with NAFLD, and that type diabetes is a risk factor for progression to NASH and liver-related mortality, the association in children with NAFLD is less well understood.
“Among our cohort, the prevalence of children with type 2 diabetes was much higher than would be expected based on contributions from obesity alone,” they wrote. “Although systemic insulin resistance is believed be important in the pathogenesis of both pediatric NAFLD and type 2 diabetes, to our knowledge, there are no longitudinal studies that evaluate the cause-effect relationship between these two associated conditions.”
The authors drew particular attention to the threefold higher odds of NASH in children with NAFLD and type 2 diabetes, pointing out that while the prognostic implications of NASH in childhood are not fully known, the NASH phenotype is associated with a “substantially” greater risk of cirrhosis. This risk is likely to be compounded by the presence of type 2 diabetes.
“Our study advances the literature by showing that as early as childhood, prediabetes and type 2 diabetes emerge as clear risk factors for NASH with potential downstream implications for future morbidity and mortality.”
Commenting on the greater incidence of prediabetes and type 2 diabetes among girls with NAFLD, the authors said this had been observed in other studies and that sex differences represented a major unmet research need.
The Nonalcoholic Steatohepatitis Clinical Research Network is supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Additional support was received from the National Center for Advancing Translational Sciences. The researchers reported no conflicts of interest.
FROM JAMA PEDIATRICS
Key clinical point: Nearly one in three children with nonalcoholic fatty liver disease have abnormal glucose metabolism, and this combination also is associated with a greater risk of nonalcoholic steatohepatitis.
Major finding: Among children with biopsy-diagnosed non-alcoholic fatty liver disease, 23.4% had prediabetes and 6.5% met the clinical criteria for type 2 diabetes.
Data source: Cross-sectional study of 675 children with biopsy-confirmed nonalcoholic fatty liver disease enrolled in the NASH Clinical Research Network.
Disclosures: The Nonalcoholic Steatohepatitis Clinical Research Network is supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Additional support was received from the National Center for Advancing Translational Sciences. The researchers reported no conflicts of interest.
Two incretin-based drugs linked to increased bile duct disease but not pancreatitis
At least two incretin-based drugs – glucagon-like peptide 1 agonists and dipeptidyl peptidase 4 inhibitors – do not appear to increase the risk of acute pancreatitis in individuals with diabetes but are associated with an increased risk of bile duct and gallbladder disease.
Two studies examining the impact on the pancreas of incretin-based drugs, including dipeptidyl peptidase 4 (DPP-4) inhibitors and glucagon-like peptide 1 (GLP-1) agonists, have been published online August 1 in JAMA Internal Medicine.
Incretin-based drugs have been associated with increased risk of elevated pancreatic enzyme levels, while GLP-1 has been shown to increase the proliferation and activity of cholangiocytes, which have raised concerns of an impact on the bile duct, gallbladder, and pancreas.
The first study was an international, population-based cohort study using the health records of more than 1.5 million individuals with type 2 diabetes, who began treatment with antidiabetic drugs between January 2007 and June 2013.
Analysis of these data showed there was no difference in the risk of hospitalization for acute pancreatitis between those taking incretin-based drugs and those on two or more other oral antidiabetic medications (JAMA Intern Med. 2016 Aug 1. doi: 10.1001/jamainternmed.2016.1522).
The study also found no significant increase in the risk of acute pancreatitis either with DPP-4 inhibitors or GLP-1 agonists, nor was there any increase with a longer duration of use or in patients with a history of acute or chronic pancreatitis.
Most previous observational studies of incretin-based drugs and pancreatitis had reported null findings, but four studies did find a positive association. Laurent Azoulay, PhD, from the Lady Davis Institute at Montreal’s Jewish General Hospital, and his coauthors suggested this heterogeneity was likely the result of methodologic shortcomings such as the use of inappropriate comparator groups and confoundings.
“Although it remains possible that these drugs may be associated with acute pancreatitis, the upper limit of our 95% [confidence interval] suggests that this risk is likely to be small,” the authors wrote. “Thus, the findings of this study should provide some reassurance to patients treated with incretin-based drugs.”
Meanwhile, a second population-based cohort study in 71,368 patients starting an antidiabetic drug found the use of GLP-1 analogues was associated with a significant 79% increase in the risk of bile duct and gallbladder disease, compared with the use of at least two other oral antidiabetic medications.
When stratified by duration of use, individuals taking GLP-1 analogues for less than 180 days showed a twofold increase in the risk of bile duct and gallbladder disease (adjusted hazard ratio, 2.01; 95% CI, 1.23-3.29) but those taking the drugs for longer than 180 days did not show an increased risk.
The use of GLP-1 analogues was also associated with a two-fold increase in the risk of undergoing a cholecystectomy.
However, the study found no increased risk of bile duct or gallbladder disease with DPP-4 inhibitors (JAMA Intern Med. 2016 Aug 1. doi: 10.1001/jamainternmed.2016.1531).
Jean-Luc Faillie, MD, PhD, of the University of Montpellier (France) and his associates suggested that rapid weight loss associated with GLP-1 analogues may explain the association with bile duct and gallbladder disease, which would also account for the observation that the association did not occur in patients taking the drugs for a longer period of time.
“Weight loss leads to supersaturation of cholesterol in the bile, a known risk factor for gallstones,” the authors wrote.
DPP-4 inhibitors have different effects on the GLP-1 pharmacologic factors and a weaker incretin action, which the authors suggested may explain the lack of association with bile duct and gallbladder disease, as well as their lower incidence of gastrointestinal adverse events.
“Although further studies are needed to confirm our findings and the mechanisms involved, physicians prescribing GLP-1 analogues should be aware of this association and carefully monitor patients for biliary tract complications.”
The first study was enabled by data-sharing agreements with the Canadian Network for Observational Drug Effect Studies, which is funded by the Canadian Institutes of Health Research. Two authors declared consulting fees, grant support, or financial compensation from the pharmaceutical industry, but there were no other conflicts of interest declared.
The second study was funded by the Canadian Institutes of Health Research. No conflicts of interest were declared.
At least two incretin-based drugs – glucagon-like peptide 1 agonists and dipeptidyl peptidase 4 inhibitors – do not appear to increase the risk of acute pancreatitis in individuals with diabetes but are associated with an increased risk of bile duct and gallbladder disease.
Two studies examining the impact on the pancreas of incretin-based drugs, including dipeptidyl peptidase 4 (DPP-4) inhibitors and glucagon-like peptide 1 (GLP-1) agonists, have been published online August 1 in JAMA Internal Medicine.
Incretin-based drugs have been associated with increased risk of elevated pancreatic enzyme levels, while GLP-1 has been shown to increase the proliferation and activity of cholangiocytes, which have raised concerns of an impact on the bile duct, gallbladder, and pancreas.
The first study was an international, population-based cohort study using the health records of more than 1.5 million individuals with type 2 diabetes, who began treatment with antidiabetic drugs between January 2007 and June 2013.
Analysis of these data showed there was no difference in the risk of hospitalization for acute pancreatitis between those taking incretin-based drugs and those on two or more other oral antidiabetic medications (JAMA Intern Med. 2016 Aug 1. doi: 10.1001/jamainternmed.2016.1522).
The study also found no significant increase in the risk of acute pancreatitis either with DPP-4 inhibitors or GLP-1 agonists, nor was there any increase with a longer duration of use or in patients with a history of acute or chronic pancreatitis.
Most previous observational studies of incretin-based drugs and pancreatitis had reported null findings, but four studies did find a positive association. Laurent Azoulay, PhD, from the Lady Davis Institute at Montreal’s Jewish General Hospital, and his coauthors suggested this heterogeneity was likely the result of methodologic shortcomings such as the use of inappropriate comparator groups and confoundings.
“Although it remains possible that these drugs may be associated with acute pancreatitis, the upper limit of our 95% [confidence interval] suggests that this risk is likely to be small,” the authors wrote. “Thus, the findings of this study should provide some reassurance to patients treated with incretin-based drugs.”
Meanwhile, a second population-based cohort study in 71,368 patients starting an antidiabetic drug found the use of GLP-1 analogues was associated with a significant 79% increase in the risk of bile duct and gallbladder disease, compared with the use of at least two other oral antidiabetic medications.
When stratified by duration of use, individuals taking GLP-1 analogues for less than 180 days showed a twofold increase in the risk of bile duct and gallbladder disease (adjusted hazard ratio, 2.01; 95% CI, 1.23-3.29) but those taking the drugs for longer than 180 days did not show an increased risk.
The use of GLP-1 analogues was also associated with a two-fold increase in the risk of undergoing a cholecystectomy.
However, the study found no increased risk of bile duct or gallbladder disease with DPP-4 inhibitors (JAMA Intern Med. 2016 Aug 1. doi: 10.1001/jamainternmed.2016.1531).
Jean-Luc Faillie, MD, PhD, of the University of Montpellier (France) and his associates suggested that rapid weight loss associated with GLP-1 analogues may explain the association with bile duct and gallbladder disease, which would also account for the observation that the association did not occur in patients taking the drugs for a longer period of time.
“Weight loss leads to supersaturation of cholesterol in the bile, a known risk factor for gallstones,” the authors wrote.
DPP-4 inhibitors have different effects on the GLP-1 pharmacologic factors and a weaker incretin action, which the authors suggested may explain the lack of association with bile duct and gallbladder disease, as well as their lower incidence of gastrointestinal adverse events.
“Although further studies are needed to confirm our findings and the mechanisms involved, physicians prescribing GLP-1 analogues should be aware of this association and carefully monitor patients for biliary tract complications.”
The first study was enabled by data-sharing agreements with the Canadian Network for Observational Drug Effect Studies, which is funded by the Canadian Institutes of Health Research. Two authors declared consulting fees, grant support, or financial compensation from the pharmaceutical industry, but there were no other conflicts of interest declared.
The second study was funded by the Canadian Institutes of Health Research. No conflicts of interest were declared.
At least two incretin-based drugs – glucagon-like peptide 1 agonists and dipeptidyl peptidase 4 inhibitors – do not appear to increase the risk of acute pancreatitis in individuals with diabetes but are associated with an increased risk of bile duct and gallbladder disease.
Two studies examining the impact on the pancreas of incretin-based drugs, including dipeptidyl peptidase 4 (DPP-4) inhibitors and glucagon-like peptide 1 (GLP-1) agonists, have been published online August 1 in JAMA Internal Medicine.
Incretin-based drugs have been associated with increased risk of elevated pancreatic enzyme levels, while GLP-1 has been shown to increase the proliferation and activity of cholangiocytes, which have raised concerns of an impact on the bile duct, gallbladder, and pancreas.
The first study was an international, population-based cohort study using the health records of more than 1.5 million individuals with type 2 diabetes, who began treatment with antidiabetic drugs between January 2007 and June 2013.
Analysis of these data showed there was no difference in the risk of hospitalization for acute pancreatitis between those taking incretin-based drugs and those on two or more other oral antidiabetic medications (JAMA Intern Med. 2016 Aug 1. doi: 10.1001/jamainternmed.2016.1522).
The study also found no significant increase in the risk of acute pancreatitis either with DPP-4 inhibitors or GLP-1 agonists, nor was there any increase with a longer duration of use or in patients with a history of acute or chronic pancreatitis.
Most previous observational studies of incretin-based drugs and pancreatitis had reported null findings, but four studies did find a positive association. Laurent Azoulay, PhD, from the Lady Davis Institute at Montreal’s Jewish General Hospital, and his coauthors suggested this heterogeneity was likely the result of methodologic shortcomings such as the use of inappropriate comparator groups and confoundings.
“Although it remains possible that these drugs may be associated with acute pancreatitis, the upper limit of our 95% [confidence interval] suggests that this risk is likely to be small,” the authors wrote. “Thus, the findings of this study should provide some reassurance to patients treated with incretin-based drugs.”
Meanwhile, a second population-based cohort study in 71,368 patients starting an antidiabetic drug found the use of GLP-1 analogues was associated with a significant 79% increase in the risk of bile duct and gallbladder disease, compared with the use of at least two other oral antidiabetic medications.
When stratified by duration of use, individuals taking GLP-1 analogues for less than 180 days showed a twofold increase in the risk of bile duct and gallbladder disease (adjusted hazard ratio, 2.01; 95% CI, 1.23-3.29) but those taking the drugs for longer than 180 days did not show an increased risk.
The use of GLP-1 analogues was also associated with a two-fold increase in the risk of undergoing a cholecystectomy.
However, the study found no increased risk of bile duct or gallbladder disease with DPP-4 inhibitors (JAMA Intern Med. 2016 Aug 1. doi: 10.1001/jamainternmed.2016.1531).
Jean-Luc Faillie, MD, PhD, of the University of Montpellier (France) and his associates suggested that rapid weight loss associated with GLP-1 analogues may explain the association with bile duct and gallbladder disease, which would also account for the observation that the association did not occur in patients taking the drugs for a longer period of time.
“Weight loss leads to supersaturation of cholesterol in the bile, a known risk factor for gallstones,” the authors wrote.
DPP-4 inhibitors have different effects on the GLP-1 pharmacologic factors and a weaker incretin action, which the authors suggested may explain the lack of association with bile duct and gallbladder disease, as well as their lower incidence of gastrointestinal adverse events.
“Although further studies are needed to confirm our findings and the mechanisms involved, physicians prescribing GLP-1 analogues should be aware of this association and carefully monitor patients for biliary tract complications.”
The first study was enabled by data-sharing agreements with the Canadian Network for Observational Drug Effect Studies, which is funded by the Canadian Institutes of Health Research. Two authors declared consulting fees, grant support, or financial compensation from the pharmaceutical industry, but there were no other conflicts of interest declared.
The second study was funded by the Canadian Institutes of Health Research. No conflicts of interest were declared.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Glucagon-like peptide 1 agonists do not appear to increase the risk of acute pancreatitis in individuals with diabetes but are associated with an increased risk of bile duct and gallbladder disease.
Major finding: GLP-1 agonists are associated with a 79% increase in the risk of bile duct and gallbladder disease, compared with other oral antidiabetic medications, but do not increase the risk of acute pancreatitis.
Data source: Two population-based cohort studies; one involving more than 1.5 million individuals with type 2 diabetes across three countries, and the other involving 71,368 patients with type 2 diabetes.
Disclosures: The first study was enabled by data-sharing agreements with the Canadian Network for Observational Drug Effect Studies, which is funded by the Canadian Institutes of Health Research. Two authors declared consulting fees, grant support, or financial compensation from the pharmaceutical industry, but there were no other conflicts of interest declared. The second study was funded by the Canadian Institutes of Health Research. No conflicts of interest were declared.