User login
Study confirms link between PAP apnea treatment and dementia onset
Obstructive sleep apnea (OSA) treatment with positive airway pressure (PAP) therapy was associated with a lower odds of incident Alzheimer’s disease and other dementia in a large retrospective cohort study of Medicare patients with the sleep disorder.
The study builds on research linking OSA to poor cognitive outcomes and dementia syndromes. With use of a 5% random sample of Medicare beneficiaries (more than 2.7 million) and their claims data, investigators identified approximately 53,000 who had an OSA diagnosis prior to 2011.
Of these Medicare beneficiaries, 78% with OSA were identified as “PAP-treated” based on having at least one durable medical equipment claim for PAP equipment. And of those treated, 74% were identified as “PAP adherent” based on having more than two PAP equipment claims separated by at least a month, said Galit Levi Dunietz, PhD, MPH, at the virtual annual meeting of the Associated Professional Sleep Societies.
Dr. Dunietz and her coinvestigators used logistic regression to examine the associations between PAP treatment and PAP treatment adherence, and incident ICD-9 diagnoses of Alzheimer’s disease (AD), mild cognitive impairment (MCI), and dementia not otherwise specified (DNOS) over the period 2011-2013.
After adjustments for potential confounders (age, sex, race, stroke, hypertension, cardiovascular disease, and depression), OSA treatment was associated with a significantly lower odds of a diagnosis of AD (odds ratio, 0.78; 95% confidence interval 0.69-0.89) or DNOS (OR, 0.69; 95% CI, 0.55-0.85), as well as nonsignificantly lower odds of MCI diagnosis (OR, 0.82; 95% CI, 0.66-1.02).
“People who are treated for OSA have a 22% reduced odds of being diagnosed with AD and a 31% reduced odds of getting DNOS,” said Dr. Dunietz, from the University of Michigan in Ann Arbor, in an interview after the meeting. “The 18% reduced odds of mild cognitive disorder is not really significant because the upper bound is 1.02, but we consider it approaching significance.”
Adherence to treatment was significantly associated with lower odds of AD, but not with significantly lower odds of DNOS or MCI, she said. OSA was confirmed by ICD-9 diagnosis codes plus the presence of relevant polysomnography current procedural terminology code.
All told, the findings “suggest that PAP therapy for OSA may lower short-term risk for dementia in older persons,” Dr. Dunietz and her co-nvestigators said in their poster presentation. “If a causal pathway exists between OSA and dementia, treatment of OSA may offer new opportunities to improve cognitive outcomes in older adults with OSA.”
Andrew W. Varga, MD, of the division of pulmonary, critical care, and sleep medicine at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Integrative Sleep Center, both in New York, said that cognitive impairment is now a recognized clinical consequence of OSA and that OSA treatment could be a target for the prevention of cognitive impairment and Alzheimer’s disease in particular.
“I absolutely bring it up with patients in their 60s and 70s. I’m honest – I say, there seems to be more and more evidence for links between apnea and Alzheimer’s in particular. I tell them we don’t know 100% whether PAP reverses any of this, but it stands to reason that it does,” said Dr. Varga, who was asked to comment on the study and related research.
An analysis published several years ago in Neurology from the Alzheimer’s Disease Neuroimaging Initiative cohort found that patients with self-reported sleep apnea had a younger age of MCI or AD onset (about 10 years) and that patients who used continuous positive airway pressure had a delayed age of onset. “Those who had a subjective diagnosis of sleep apnea and who also reported using CPAP as treatment seemed to go in the opposite direction,” said Dr. Varga, a coauthor of that study. “They had an onset of AD that looked just like people who had no sleep apnea.”
While this study was limited by sleep apnea being self-reported – and by the lack of severity data – the newly reported study may be limited by the use of ICD codes and the fact that OSA is often entered into patient’s chart before diagnosis is confirmed through a sleep study, Dr. Varga said.
“The field is mature enough that we should be thinking of doing honest and rigorous clinical trials for sleep apnea with cognitive outcomes being a main measure of interest,” he said. “The issue we’re struggling with in the field is that such a trial would not be short.”
There are several theories for the link between OSA and cognitive impairment, he said, including disruptions in sleep architecture leading to increased production of amyloid and tau and/or decreased “clearance” of extracellular amyloid, neuronal sensitivity to hypoxia, and cardiovascular comorbidities.
Dr. Dunietz’s study was supported by The American Academy of Sleep Medicine Foundation. She reported having no disclosures. Dr. Varga said he has no relevant disclosures.
Obstructive sleep apnea (OSA) treatment with positive airway pressure (PAP) therapy was associated with a lower odds of incident Alzheimer’s disease and other dementia in a large retrospective cohort study of Medicare patients with the sleep disorder.
The study builds on research linking OSA to poor cognitive outcomes and dementia syndromes. With use of a 5% random sample of Medicare beneficiaries (more than 2.7 million) and their claims data, investigators identified approximately 53,000 who had an OSA diagnosis prior to 2011.
Of these Medicare beneficiaries, 78% with OSA were identified as “PAP-treated” based on having at least one durable medical equipment claim for PAP equipment. And of those treated, 74% were identified as “PAP adherent” based on having more than two PAP equipment claims separated by at least a month, said Galit Levi Dunietz, PhD, MPH, at the virtual annual meeting of the Associated Professional Sleep Societies.
Dr. Dunietz and her coinvestigators used logistic regression to examine the associations between PAP treatment and PAP treatment adherence, and incident ICD-9 diagnoses of Alzheimer’s disease (AD), mild cognitive impairment (MCI), and dementia not otherwise specified (DNOS) over the period 2011-2013.
After adjustments for potential confounders (age, sex, race, stroke, hypertension, cardiovascular disease, and depression), OSA treatment was associated with a significantly lower odds of a diagnosis of AD (odds ratio, 0.78; 95% confidence interval 0.69-0.89) or DNOS (OR, 0.69; 95% CI, 0.55-0.85), as well as nonsignificantly lower odds of MCI diagnosis (OR, 0.82; 95% CI, 0.66-1.02).
“People who are treated for OSA have a 22% reduced odds of being diagnosed with AD and a 31% reduced odds of getting DNOS,” said Dr. Dunietz, from the University of Michigan in Ann Arbor, in an interview after the meeting. “The 18% reduced odds of mild cognitive disorder is not really significant because the upper bound is 1.02, but we consider it approaching significance.”
Adherence to treatment was significantly associated with lower odds of AD, but not with significantly lower odds of DNOS or MCI, she said. OSA was confirmed by ICD-9 diagnosis codes plus the presence of relevant polysomnography current procedural terminology code.
All told, the findings “suggest that PAP therapy for OSA may lower short-term risk for dementia in older persons,” Dr. Dunietz and her co-nvestigators said in their poster presentation. “If a causal pathway exists between OSA and dementia, treatment of OSA may offer new opportunities to improve cognitive outcomes in older adults with OSA.”
Andrew W. Varga, MD, of the division of pulmonary, critical care, and sleep medicine at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Integrative Sleep Center, both in New York, said that cognitive impairment is now a recognized clinical consequence of OSA and that OSA treatment could be a target for the prevention of cognitive impairment and Alzheimer’s disease in particular.
“I absolutely bring it up with patients in their 60s and 70s. I’m honest – I say, there seems to be more and more evidence for links between apnea and Alzheimer’s in particular. I tell them we don’t know 100% whether PAP reverses any of this, but it stands to reason that it does,” said Dr. Varga, who was asked to comment on the study and related research.
An analysis published several years ago in Neurology from the Alzheimer’s Disease Neuroimaging Initiative cohort found that patients with self-reported sleep apnea had a younger age of MCI or AD onset (about 10 years) and that patients who used continuous positive airway pressure had a delayed age of onset. “Those who had a subjective diagnosis of sleep apnea and who also reported using CPAP as treatment seemed to go in the opposite direction,” said Dr. Varga, a coauthor of that study. “They had an onset of AD that looked just like people who had no sleep apnea.”
While this study was limited by sleep apnea being self-reported – and by the lack of severity data – the newly reported study may be limited by the use of ICD codes and the fact that OSA is often entered into patient’s chart before diagnosis is confirmed through a sleep study, Dr. Varga said.
“The field is mature enough that we should be thinking of doing honest and rigorous clinical trials for sleep apnea with cognitive outcomes being a main measure of interest,” he said. “The issue we’re struggling with in the field is that such a trial would not be short.”
There are several theories for the link between OSA and cognitive impairment, he said, including disruptions in sleep architecture leading to increased production of amyloid and tau and/or decreased “clearance” of extracellular amyloid, neuronal sensitivity to hypoxia, and cardiovascular comorbidities.
Dr. Dunietz’s study was supported by The American Academy of Sleep Medicine Foundation. She reported having no disclosures. Dr. Varga said he has no relevant disclosures.
Obstructive sleep apnea (OSA) treatment with positive airway pressure (PAP) therapy was associated with a lower odds of incident Alzheimer’s disease and other dementia in a large retrospective cohort study of Medicare patients with the sleep disorder.
The study builds on research linking OSA to poor cognitive outcomes and dementia syndromes. With use of a 5% random sample of Medicare beneficiaries (more than 2.7 million) and their claims data, investigators identified approximately 53,000 who had an OSA diagnosis prior to 2011.
Of these Medicare beneficiaries, 78% with OSA were identified as “PAP-treated” based on having at least one durable medical equipment claim for PAP equipment. And of those treated, 74% were identified as “PAP adherent” based on having more than two PAP equipment claims separated by at least a month, said Galit Levi Dunietz, PhD, MPH, at the virtual annual meeting of the Associated Professional Sleep Societies.
Dr. Dunietz and her coinvestigators used logistic regression to examine the associations between PAP treatment and PAP treatment adherence, and incident ICD-9 diagnoses of Alzheimer’s disease (AD), mild cognitive impairment (MCI), and dementia not otherwise specified (DNOS) over the period 2011-2013.
After adjustments for potential confounders (age, sex, race, stroke, hypertension, cardiovascular disease, and depression), OSA treatment was associated with a significantly lower odds of a diagnosis of AD (odds ratio, 0.78; 95% confidence interval 0.69-0.89) or DNOS (OR, 0.69; 95% CI, 0.55-0.85), as well as nonsignificantly lower odds of MCI diagnosis (OR, 0.82; 95% CI, 0.66-1.02).
“People who are treated for OSA have a 22% reduced odds of being diagnosed with AD and a 31% reduced odds of getting DNOS,” said Dr. Dunietz, from the University of Michigan in Ann Arbor, in an interview after the meeting. “The 18% reduced odds of mild cognitive disorder is not really significant because the upper bound is 1.02, but we consider it approaching significance.”
Adherence to treatment was significantly associated with lower odds of AD, but not with significantly lower odds of DNOS or MCI, she said. OSA was confirmed by ICD-9 diagnosis codes plus the presence of relevant polysomnography current procedural terminology code.
All told, the findings “suggest that PAP therapy for OSA may lower short-term risk for dementia in older persons,” Dr. Dunietz and her co-nvestigators said in their poster presentation. “If a causal pathway exists between OSA and dementia, treatment of OSA may offer new opportunities to improve cognitive outcomes in older adults with OSA.”
Andrew W. Varga, MD, of the division of pulmonary, critical care, and sleep medicine at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Integrative Sleep Center, both in New York, said that cognitive impairment is now a recognized clinical consequence of OSA and that OSA treatment could be a target for the prevention of cognitive impairment and Alzheimer’s disease in particular.
“I absolutely bring it up with patients in their 60s and 70s. I’m honest – I say, there seems to be more and more evidence for links between apnea and Alzheimer’s in particular. I tell them we don’t know 100% whether PAP reverses any of this, but it stands to reason that it does,” said Dr. Varga, who was asked to comment on the study and related research.
An analysis published several years ago in Neurology from the Alzheimer’s Disease Neuroimaging Initiative cohort found that patients with self-reported sleep apnea had a younger age of MCI or AD onset (about 10 years) and that patients who used continuous positive airway pressure had a delayed age of onset. “Those who had a subjective diagnosis of sleep apnea and who also reported using CPAP as treatment seemed to go in the opposite direction,” said Dr. Varga, a coauthor of that study. “They had an onset of AD that looked just like people who had no sleep apnea.”
While this study was limited by sleep apnea being self-reported – and by the lack of severity data – the newly reported study may be limited by the use of ICD codes and the fact that OSA is often entered into patient’s chart before diagnosis is confirmed through a sleep study, Dr. Varga said.
“The field is mature enough that we should be thinking of doing honest and rigorous clinical trials for sleep apnea with cognitive outcomes being a main measure of interest,” he said. “The issue we’re struggling with in the field is that such a trial would not be short.”
There are several theories for the link between OSA and cognitive impairment, he said, including disruptions in sleep architecture leading to increased production of amyloid and tau and/or decreased “clearance” of extracellular amyloid, neuronal sensitivity to hypoxia, and cardiovascular comorbidities.
Dr. Dunietz’s study was supported by The American Academy of Sleep Medicine Foundation. She reported having no disclosures. Dr. Varga said he has no relevant disclosures.
FROM SLEEP 2020
Social distancing impacts other infectious diseases
Diagnoses of 12 common pediatric infectious diseases in a large pediatric primary care network declined significantly in the weeks after COVID-19 social distancing (SD) was enacted in Massachusetts, compared with the same time period in 2019, an analysis of EHR data has shown.
While declines in infectious disease transmission with SD are not surprising, “these data demonstrate the extent to which transmission of common pediatric infections can be altered when close contact with other children is eliminated,” Jonathan Hatoun, MD, MPH of the Pediatric Physicians’ Organization at Children’s in Brookline, Mass., and coauthors wrote in Pediatrics . “Notably, three of the studied diseases, namely, influenza, croup, and bronchiolitis, essentially disappeared with [social distancing].”
The researchers analyzed the weekly incidence of each diagnosis for similar calendar periods in 2019 and 2020. A pre-SD period was defined as week 1-9, starting on Jan. 1, and a post-SD period was defined as week 13-18. (The several-week gap represented an implementation period as social distancing was enacted in the state earlier in 2020, from a declared statewide state of emergency through school closures and stay-at-home advisories.)
To isolate the effect of widespread SD, they performed a “difference-in-differences regression analysis, with diagnosis count as a function of calendar year, time period (pre-SD versus post-SD) and the interaction between the two.” The Massachusetts pediatric network provides care for approximately 375,000 children in 100 locations around the state.
In their research brief, Dr. Hatoun and coauthors presented weekly rates expressed as diagnoses per 100,000 patients per day. The rate of bronchiolitis, for instance, was 18 and 8 in the pre- and post-SD–equivalent weeks of 2019, respectively, and 20 and 0.6 in the pre- and post-SD weeks of 2020. Their analysis showed the rate in the 2020 post-SD period to be 10 diagnoses per 100,000 patients per day lower than they would have expected based on the 2019 trend.
Rates of pneumonia, acute otitis media, and streptococcal pharyngitis were similarly 14, 85, and 31 diagnoses per 100,000 patients per day lower, respectively. The prevalence of each of the other conditions analyzed – the common cold, croup, gastroenteritis, nonstreptococcal pharyngitis, sinusitis, skin and soft tissue infections, and urinary tract infection (UTI) – also was significantly lower in the 2020 post-SD period than would be expected based on 2019 data (P < .001 for all diagnoses).
Putting things in perspective
“This study puts numbers to the sense that we have all had in pediatrics – that social distancing appears to have had a dramatic impact on the transmission of common childhood infectious diseases, especially other respiratory viral pathogens,” Audrey R. John, MD, PhD, chief of the division of pediatric infectious disease at Children’s Hospital of Philadelphia, said in an interview.
The authors acknowledged the possible role of families not seeking care, but said that a smaller decrease in diagnoses of UTI – generally not a contagious disease – “suggests that changes in care-seeking behavior had a relatively modest effect on the other observed declines.” (The rate of UTI for the pre- and post-SD periods was 3.3 and 3.7 per 100,000 patients per day in 2019, and 3.4 and 2.4 in 2020, for a difference in differences of –1.5).
In an accompanying editorial, David W. Kimberlin, MD and Erica C. Bjornstad, MD, PhD, MPH, of the University of Alabama at Birmingham, called the report “provocative” and wrote that similar observations of infections dropping during periods of isolation – namely, dramatic declines in influenza and other respiratory viruses in Seattle after a record snowstorm in 2019 – combined with findings from other modeling studies “suggest that the decline [reported in Boston] is indeed real” (Pediatrics 2020. doi: 10.1542/peds.2020-019232).
However, “we also now know that immunization rates for American children have plummeted since the onset of the SARS-CoV-2 pandemic [because of a] ... dramatic decrease in the use of health care during the first months of the pandemic,” they wrote. “Viewed through this lens,” the declines reported in Boston may reflect inflections going “undiagnosed and untreated.”
Ultimately, Dr. Kimberlin and Dr. Bjornstad said, “the verdict remains out.”
Dr. John said that she and others are “concerned about children not seeking care in a timely manner, and [concerned] that reductions in reported infections might be due to a lack of recognition rather than a lack of transmission.”
In Philadelphia, however, declines in admissions for asthma exacerbations, “which are often caused by respiratory viral infections, suggests that this may not be the case,” said Dr. John, who was asked to comment on the study.
In addition, she said, the Massachusetts data showing that UTI diagnoses “are nearly as common this year as in 2019” are “reassuring.”
Are there lessons for the future?
Coauthor Louis Vernacchio, MD, MSc, chief medical officer of the Pediatric Physicians’ Organization at Children’s network, said in an interview that beyond the pandemic, it’s likely that “more careful attention to proven infection control practices in daycares and schools could reduce the burden of common infectious diseases in children.”
Dr. John similarly sees a long-term value of quantifying the impact of social distancing. “We’ve always known [for instance] that bronchiolitis is the result of viral infection.” Findings like the Massachusetts data “will help us advise families who might be trying to protect their premature infants (at risk for severe bronchiolitis) through social distancing.”
The analysis covered both in-person and telemedicine encounters occurring on weekdays.
The authors of the research brief indicated they have no relevant financial disclosures and there was no external funding. The authors of the commentary also reported they have no relevant financial disclosures, and Dr. John said she had no relevant financial disclosures.
SOURCE: Hatoun J et al. Pediatrics. 2020. doi: 10.1542/peds.2020-006460.
Diagnoses of 12 common pediatric infectious diseases in a large pediatric primary care network declined significantly in the weeks after COVID-19 social distancing (SD) was enacted in Massachusetts, compared with the same time period in 2019, an analysis of EHR data has shown.
While declines in infectious disease transmission with SD are not surprising, “these data demonstrate the extent to which transmission of common pediatric infections can be altered when close contact with other children is eliminated,” Jonathan Hatoun, MD, MPH of the Pediatric Physicians’ Organization at Children’s in Brookline, Mass., and coauthors wrote in Pediatrics . “Notably, three of the studied diseases, namely, influenza, croup, and bronchiolitis, essentially disappeared with [social distancing].”
The researchers analyzed the weekly incidence of each diagnosis for similar calendar periods in 2019 and 2020. A pre-SD period was defined as week 1-9, starting on Jan. 1, and a post-SD period was defined as week 13-18. (The several-week gap represented an implementation period as social distancing was enacted in the state earlier in 2020, from a declared statewide state of emergency through school closures and stay-at-home advisories.)
To isolate the effect of widespread SD, they performed a “difference-in-differences regression analysis, with diagnosis count as a function of calendar year, time period (pre-SD versus post-SD) and the interaction between the two.” The Massachusetts pediatric network provides care for approximately 375,000 children in 100 locations around the state.
In their research brief, Dr. Hatoun and coauthors presented weekly rates expressed as diagnoses per 100,000 patients per day. The rate of bronchiolitis, for instance, was 18 and 8 in the pre- and post-SD–equivalent weeks of 2019, respectively, and 20 and 0.6 in the pre- and post-SD weeks of 2020. Their analysis showed the rate in the 2020 post-SD period to be 10 diagnoses per 100,000 patients per day lower than they would have expected based on the 2019 trend.
Rates of pneumonia, acute otitis media, and streptococcal pharyngitis were similarly 14, 85, and 31 diagnoses per 100,000 patients per day lower, respectively. The prevalence of each of the other conditions analyzed – the common cold, croup, gastroenteritis, nonstreptococcal pharyngitis, sinusitis, skin and soft tissue infections, and urinary tract infection (UTI) – also was significantly lower in the 2020 post-SD period than would be expected based on 2019 data (P < .001 for all diagnoses).
Putting things in perspective
“This study puts numbers to the sense that we have all had in pediatrics – that social distancing appears to have had a dramatic impact on the transmission of common childhood infectious diseases, especially other respiratory viral pathogens,” Audrey R. John, MD, PhD, chief of the division of pediatric infectious disease at Children’s Hospital of Philadelphia, said in an interview.
The authors acknowledged the possible role of families not seeking care, but said that a smaller decrease in diagnoses of UTI – generally not a contagious disease – “suggests that changes in care-seeking behavior had a relatively modest effect on the other observed declines.” (The rate of UTI for the pre- and post-SD periods was 3.3 and 3.7 per 100,000 patients per day in 2019, and 3.4 and 2.4 in 2020, for a difference in differences of –1.5).
In an accompanying editorial, David W. Kimberlin, MD and Erica C. Bjornstad, MD, PhD, MPH, of the University of Alabama at Birmingham, called the report “provocative” and wrote that similar observations of infections dropping during periods of isolation – namely, dramatic declines in influenza and other respiratory viruses in Seattle after a record snowstorm in 2019 – combined with findings from other modeling studies “suggest that the decline [reported in Boston] is indeed real” (Pediatrics 2020. doi: 10.1542/peds.2020-019232).
However, “we also now know that immunization rates for American children have plummeted since the onset of the SARS-CoV-2 pandemic [because of a] ... dramatic decrease in the use of health care during the first months of the pandemic,” they wrote. “Viewed through this lens,” the declines reported in Boston may reflect inflections going “undiagnosed and untreated.”
Ultimately, Dr. Kimberlin and Dr. Bjornstad said, “the verdict remains out.”
Dr. John said that she and others are “concerned about children not seeking care in a timely manner, and [concerned] that reductions in reported infections might be due to a lack of recognition rather than a lack of transmission.”
In Philadelphia, however, declines in admissions for asthma exacerbations, “which are often caused by respiratory viral infections, suggests that this may not be the case,” said Dr. John, who was asked to comment on the study.
In addition, she said, the Massachusetts data showing that UTI diagnoses “are nearly as common this year as in 2019” are “reassuring.”
Are there lessons for the future?
Coauthor Louis Vernacchio, MD, MSc, chief medical officer of the Pediatric Physicians’ Organization at Children’s network, said in an interview that beyond the pandemic, it’s likely that “more careful attention to proven infection control practices in daycares and schools could reduce the burden of common infectious diseases in children.”
Dr. John similarly sees a long-term value of quantifying the impact of social distancing. “We’ve always known [for instance] that bronchiolitis is the result of viral infection.” Findings like the Massachusetts data “will help us advise families who might be trying to protect their premature infants (at risk for severe bronchiolitis) through social distancing.”
The analysis covered both in-person and telemedicine encounters occurring on weekdays.
The authors of the research brief indicated they have no relevant financial disclosures and there was no external funding. The authors of the commentary also reported they have no relevant financial disclosures, and Dr. John said she had no relevant financial disclosures.
SOURCE: Hatoun J et al. Pediatrics. 2020. doi: 10.1542/peds.2020-006460.
Diagnoses of 12 common pediatric infectious diseases in a large pediatric primary care network declined significantly in the weeks after COVID-19 social distancing (SD) was enacted in Massachusetts, compared with the same time period in 2019, an analysis of EHR data has shown.
While declines in infectious disease transmission with SD are not surprising, “these data demonstrate the extent to which transmission of common pediatric infections can be altered when close contact with other children is eliminated,” Jonathan Hatoun, MD, MPH of the Pediatric Physicians’ Organization at Children’s in Brookline, Mass., and coauthors wrote in Pediatrics . “Notably, three of the studied diseases, namely, influenza, croup, and bronchiolitis, essentially disappeared with [social distancing].”
The researchers analyzed the weekly incidence of each diagnosis for similar calendar periods in 2019 and 2020. A pre-SD period was defined as week 1-9, starting on Jan. 1, and a post-SD period was defined as week 13-18. (The several-week gap represented an implementation period as social distancing was enacted in the state earlier in 2020, from a declared statewide state of emergency through school closures and stay-at-home advisories.)
To isolate the effect of widespread SD, they performed a “difference-in-differences regression analysis, with diagnosis count as a function of calendar year, time period (pre-SD versus post-SD) and the interaction between the two.” The Massachusetts pediatric network provides care for approximately 375,000 children in 100 locations around the state.
In their research brief, Dr. Hatoun and coauthors presented weekly rates expressed as diagnoses per 100,000 patients per day. The rate of bronchiolitis, for instance, was 18 and 8 in the pre- and post-SD–equivalent weeks of 2019, respectively, and 20 and 0.6 in the pre- and post-SD weeks of 2020. Their analysis showed the rate in the 2020 post-SD period to be 10 diagnoses per 100,000 patients per day lower than they would have expected based on the 2019 trend.
Rates of pneumonia, acute otitis media, and streptococcal pharyngitis were similarly 14, 85, and 31 diagnoses per 100,000 patients per day lower, respectively. The prevalence of each of the other conditions analyzed – the common cold, croup, gastroenteritis, nonstreptococcal pharyngitis, sinusitis, skin and soft tissue infections, and urinary tract infection (UTI) – also was significantly lower in the 2020 post-SD period than would be expected based on 2019 data (P < .001 for all diagnoses).
Putting things in perspective
“This study puts numbers to the sense that we have all had in pediatrics – that social distancing appears to have had a dramatic impact on the transmission of common childhood infectious diseases, especially other respiratory viral pathogens,” Audrey R. John, MD, PhD, chief of the division of pediatric infectious disease at Children’s Hospital of Philadelphia, said in an interview.
The authors acknowledged the possible role of families not seeking care, but said that a smaller decrease in diagnoses of UTI – generally not a contagious disease – “suggests that changes in care-seeking behavior had a relatively modest effect on the other observed declines.” (The rate of UTI for the pre- and post-SD periods was 3.3 and 3.7 per 100,000 patients per day in 2019, and 3.4 and 2.4 in 2020, for a difference in differences of –1.5).
In an accompanying editorial, David W. Kimberlin, MD and Erica C. Bjornstad, MD, PhD, MPH, of the University of Alabama at Birmingham, called the report “provocative” and wrote that similar observations of infections dropping during periods of isolation – namely, dramatic declines in influenza and other respiratory viruses in Seattle after a record snowstorm in 2019 – combined with findings from other modeling studies “suggest that the decline [reported in Boston] is indeed real” (Pediatrics 2020. doi: 10.1542/peds.2020-019232).
However, “we also now know that immunization rates for American children have plummeted since the onset of the SARS-CoV-2 pandemic [because of a] ... dramatic decrease in the use of health care during the first months of the pandemic,” they wrote. “Viewed through this lens,” the declines reported in Boston may reflect inflections going “undiagnosed and untreated.”
Ultimately, Dr. Kimberlin and Dr. Bjornstad said, “the verdict remains out.”
Dr. John said that she and others are “concerned about children not seeking care in a timely manner, and [concerned] that reductions in reported infections might be due to a lack of recognition rather than a lack of transmission.”
In Philadelphia, however, declines in admissions for asthma exacerbations, “which are often caused by respiratory viral infections, suggests that this may not be the case,” said Dr. John, who was asked to comment on the study.
In addition, she said, the Massachusetts data showing that UTI diagnoses “are nearly as common this year as in 2019” are “reassuring.”
Are there lessons for the future?
Coauthor Louis Vernacchio, MD, MSc, chief medical officer of the Pediatric Physicians’ Organization at Children’s network, said in an interview that beyond the pandemic, it’s likely that “more careful attention to proven infection control practices in daycares and schools could reduce the burden of common infectious diseases in children.”
Dr. John similarly sees a long-term value of quantifying the impact of social distancing. “We’ve always known [for instance] that bronchiolitis is the result of viral infection.” Findings like the Massachusetts data “will help us advise families who might be trying to protect their premature infants (at risk for severe bronchiolitis) through social distancing.”
The analysis covered both in-person and telemedicine encounters occurring on weekdays.
The authors of the research brief indicated they have no relevant financial disclosures and there was no external funding. The authors of the commentary also reported they have no relevant financial disclosures, and Dr. John said she had no relevant financial disclosures.
SOURCE: Hatoun J et al. Pediatrics. 2020. doi: 10.1542/peds.2020-006460.
FROM PEDIATRICS
Obesity-related hypoventilation increased morbidity risk after bariatric surgery
Patients with obesity-associated sleep hypoventilation had a heightened risk of postoperative morbidities after bariatric surgery, according to a retrospective study.
Reena Mehra, MD, director of sleep disorders research for the Sleep Disorders Center at the Cleveland Clinic, led the team and the findings were presented at the virtual annual meeting of the Associated Professional Sleep Societies. Her research team examined the outcomes of 1,665 patients who underwent polysomnography prior to bariatric surgery performed at the Cleveland Clinic from 2011 to 2018.
More than two-thirds – 68.5% – had obesity-associated sleep hypoventilation as defined by body mass index (BMI) of ≥30 kg/m2 and either polysomnography-based end-tidal CO2 ≥45 mm Hg or serum bicarbonate ≥27 mEq/L.
These patients represent “a subset, if you will, of obesity hypoventilation syndrome – a subset that we were able to capture from our sleep studies … [because] we do CO2 monitoring during sleep studies uniformly,” Dr. Mehra said in an interview after the meeting.
Pornprapa Chindamporn, MD, a former fellow at the center and first author on the abstract, presented the findings. Patients in the study had a mean age of 45.2 ± 12.0 years and a BMI of 48.7 ± 9.0. Approximately 20% were male and 63.6% were White.
Those with obesity-associated sleep hypoventilation were more likely to be male and have a higher BMI and higher hemoglobin A1c than those without the condition. They also had a significantly higher apnea-hypopnea index (17.0 vs. 13.8) in those without the condition, she reported.
A number of outcomes (ICU stay, intubation, tracheostomy, discharge disposition, and 30-day readmission) were compared individually and as a composite outcome between those with and without obesity-associated sleep hypoventilation. While some of these postoperative morbidities were more common in patients with the condition, the differences between those with and without OHS were not statistically significant for intubation (1.5% vs. 1.3%, P = .81) and 30-day readmission (13.8% vs. 11.3%, P = .16). However, the composite outcome was significantly higher: 18.9% vs. 14.3% (P = .021), including in multivariable analysis that considered age, gender, BMI, Apnea Hypopnea Index, and diabetes.
All-cause mortality was not significantly different between the groups, likely because of its low overall rate (hazard ratio, 1.39; 95% confidence interval, 0.56-3.42).
“In this largest sample to date of systematically phenotyped obesity-associated sleep hypoventilation in patients undergoing bariatric surgery, we identified increased postoperative morbidity,” said Dr. Chindamporn, now a pulmonologist and sleep specialist practicing in Bangkok.
Dr. Mehra said in the interview that patients considering bariatric surgery are typically assessed for obstructive sleep apnea, but “not so much obesity hypoventilation syndrome or obesity-associated sleep-related hypoventilation syndrome.” The findings, “support the notion that we should be closely examining sleep-related hypoventilation in these patients.”
At the Cleveland Clinic, “clinically, we make sure we’re identifying these individuals and communicating the findings to bariatric surgery colleagues and to anesthesia,” said Dr. Mehra, also professor of medicine at Case Western Reserve University, Cleveland.
OHS is defined, according to the 2019 American Thoracic Society clinical practice guideline on evaluation and management of OHS, by the combination of obesity, sleep-disordered breathing, and awake daytime hypercapnia, after excluding other causes for hypoventilation (Am J Respir Crit Care Med. 2019;200[3]:e6-24).
A European Respiratory Society task force has proposed severity grading for OHS, with early stages defined by sleep-related hypoventilation and the highest grade of severity defined by morbidity-associated daytime hypercapnia (Eur Respir Rev. 2019;28:180097). However, Dr. Mehra said she is “not sure that we know enough [from long-term studies of OHS] to say definitively that there’s such an evolution.”
Certainly, she said, future research on OHS should consider its heterogeneity. It is possible that a subset of patients with OHS, “maybe these individuals with sleep-related hypoventilation,” are most likely to have adverse postsurgical outcomes.
Atul Malhotra, MD, professor of medicine at the University of California, San Diego, who was asked to comment on the study, said that OHS is understudied in general and particularly in the perioperative setting. “With the obesity pandemic, issues around OHS are likely to be [increasingly] important. And with increasing [use of] bariatric surgery, strategies to minimize risks are clearly needed,” he said, adding that the potential risks of nonbariatric surgery in patients with OHS require further study.
He noted that mortality rates in good hospitals “have become quite low for many elective surgeries, making it hard to show mortality benefit to most interventions.”
The ATS guideline on OHS states that it is the most severe form of obesity-induced respiratory compromise and leads to serious sequelae, including increased rates of mortality, chronic heart failure, pulmonary hypertension, and hospitalization caused by acute-on-chronic hypercapnic respiratory failure.
Dr. Chindamporn said in her presentation that she had no disclosures. Dr. Mehra’s research program is funded by the National Institute of Health, but she has also procured funding from the American College of Chest Physicians, American Heart Association, Clinical Translational Science Collaborative, and Central Society of Clinical Research. Dr. Malhotra disclosed that he is funded by the NIH and has received income from Merck and LIvanova related to medical education.
CORRECTION 9/15/2020: The original story misstated the presenter of the study. Dr. Chindamporn presented the findings.
Patients with obesity-associated sleep hypoventilation had a heightened risk of postoperative morbidities after bariatric surgery, according to a retrospective study.
Reena Mehra, MD, director of sleep disorders research for the Sleep Disorders Center at the Cleveland Clinic, led the team and the findings were presented at the virtual annual meeting of the Associated Professional Sleep Societies. Her research team examined the outcomes of 1,665 patients who underwent polysomnography prior to bariatric surgery performed at the Cleveland Clinic from 2011 to 2018.
More than two-thirds – 68.5% – had obesity-associated sleep hypoventilation as defined by body mass index (BMI) of ≥30 kg/m2 and either polysomnography-based end-tidal CO2 ≥45 mm Hg or serum bicarbonate ≥27 mEq/L.
These patients represent “a subset, if you will, of obesity hypoventilation syndrome – a subset that we were able to capture from our sleep studies … [because] we do CO2 monitoring during sleep studies uniformly,” Dr. Mehra said in an interview after the meeting.
Pornprapa Chindamporn, MD, a former fellow at the center and first author on the abstract, presented the findings. Patients in the study had a mean age of 45.2 ± 12.0 years and a BMI of 48.7 ± 9.0. Approximately 20% were male and 63.6% were White.
Those with obesity-associated sleep hypoventilation were more likely to be male and have a higher BMI and higher hemoglobin A1c than those without the condition. They also had a significantly higher apnea-hypopnea index (17.0 vs. 13.8) in those without the condition, she reported.
A number of outcomes (ICU stay, intubation, tracheostomy, discharge disposition, and 30-day readmission) were compared individually and as a composite outcome between those with and without obesity-associated sleep hypoventilation. While some of these postoperative morbidities were more common in patients with the condition, the differences between those with and without OHS were not statistically significant for intubation (1.5% vs. 1.3%, P = .81) and 30-day readmission (13.8% vs. 11.3%, P = .16). However, the composite outcome was significantly higher: 18.9% vs. 14.3% (P = .021), including in multivariable analysis that considered age, gender, BMI, Apnea Hypopnea Index, and diabetes.
All-cause mortality was not significantly different between the groups, likely because of its low overall rate (hazard ratio, 1.39; 95% confidence interval, 0.56-3.42).
“In this largest sample to date of systematically phenotyped obesity-associated sleep hypoventilation in patients undergoing bariatric surgery, we identified increased postoperative morbidity,” said Dr. Chindamporn, now a pulmonologist and sleep specialist practicing in Bangkok.
Dr. Mehra said in the interview that patients considering bariatric surgery are typically assessed for obstructive sleep apnea, but “not so much obesity hypoventilation syndrome or obesity-associated sleep-related hypoventilation syndrome.” The findings, “support the notion that we should be closely examining sleep-related hypoventilation in these patients.”
At the Cleveland Clinic, “clinically, we make sure we’re identifying these individuals and communicating the findings to bariatric surgery colleagues and to anesthesia,” said Dr. Mehra, also professor of medicine at Case Western Reserve University, Cleveland.
OHS is defined, according to the 2019 American Thoracic Society clinical practice guideline on evaluation and management of OHS, by the combination of obesity, sleep-disordered breathing, and awake daytime hypercapnia, after excluding other causes for hypoventilation (Am J Respir Crit Care Med. 2019;200[3]:e6-24).
A European Respiratory Society task force has proposed severity grading for OHS, with early stages defined by sleep-related hypoventilation and the highest grade of severity defined by morbidity-associated daytime hypercapnia (Eur Respir Rev. 2019;28:180097). However, Dr. Mehra said she is “not sure that we know enough [from long-term studies of OHS] to say definitively that there’s such an evolution.”
Certainly, she said, future research on OHS should consider its heterogeneity. It is possible that a subset of patients with OHS, “maybe these individuals with sleep-related hypoventilation,” are most likely to have adverse postsurgical outcomes.
Atul Malhotra, MD, professor of medicine at the University of California, San Diego, who was asked to comment on the study, said that OHS is understudied in general and particularly in the perioperative setting. “With the obesity pandemic, issues around OHS are likely to be [increasingly] important. And with increasing [use of] bariatric surgery, strategies to minimize risks are clearly needed,” he said, adding that the potential risks of nonbariatric surgery in patients with OHS require further study.
He noted that mortality rates in good hospitals “have become quite low for many elective surgeries, making it hard to show mortality benefit to most interventions.”
The ATS guideline on OHS states that it is the most severe form of obesity-induced respiratory compromise and leads to serious sequelae, including increased rates of mortality, chronic heart failure, pulmonary hypertension, and hospitalization caused by acute-on-chronic hypercapnic respiratory failure.
Dr. Chindamporn said in her presentation that she had no disclosures. Dr. Mehra’s research program is funded by the National Institute of Health, but she has also procured funding from the American College of Chest Physicians, American Heart Association, Clinical Translational Science Collaborative, and Central Society of Clinical Research. Dr. Malhotra disclosed that he is funded by the NIH and has received income from Merck and LIvanova related to medical education.
CORRECTION 9/15/2020: The original story misstated the presenter of the study. Dr. Chindamporn presented the findings.
Patients with obesity-associated sleep hypoventilation had a heightened risk of postoperative morbidities after bariatric surgery, according to a retrospective study.
Reena Mehra, MD, director of sleep disorders research for the Sleep Disorders Center at the Cleveland Clinic, led the team and the findings were presented at the virtual annual meeting of the Associated Professional Sleep Societies. Her research team examined the outcomes of 1,665 patients who underwent polysomnography prior to bariatric surgery performed at the Cleveland Clinic from 2011 to 2018.
More than two-thirds – 68.5% – had obesity-associated sleep hypoventilation as defined by body mass index (BMI) of ≥30 kg/m2 and either polysomnography-based end-tidal CO2 ≥45 mm Hg or serum bicarbonate ≥27 mEq/L.
These patients represent “a subset, if you will, of obesity hypoventilation syndrome – a subset that we were able to capture from our sleep studies … [because] we do CO2 monitoring during sleep studies uniformly,” Dr. Mehra said in an interview after the meeting.
Pornprapa Chindamporn, MD, a former fellow at the center and first author on the abstract, presented the findings. Patients in the study had a mean age of 45.2 ± 12.0 years and a BMI of 48.7 ± 9.0. Approximately 20% were male and 63.6% were White.
Those with obesity-associated sleep hypoventilation were more likely to be male and have a higher BMI and higher hemoglobin A1c than those without the condition. They also had a significantly higher apnea-hypopnea index (17.0 vs. 13.8) in those without the condition, she reported.
A number of outcomes (ICU stay, intubation, tracheostomy, discharge disposition, and 30-day readmission) were compared individually and as a composite outcome between those with and without obesity-associated sleep hypoventilation. While some of these postoperative morbidities were more common in patients with the condition, the differences between those with and without OHS were not statistically significant for intubation (1.5% vs. 1.3%, P = .81) and 30-day readmission (13.8% vs. 11.3%, P = .16). However, the composite outcome was significantly higher: 18.9% vs. 14.3% (P = .021), including in multivariable analysis that considered age, gender, BMI, Apnea Hypopnea Index, and diabetes.
All-cause mortality was not significantly different between the groups, likely because of its low overall rate (hazard ratio, 1.39; 95% confidence interval, 0.56-3.42).
“In this largest sample to date of systematically phenotyped obesity-associated sleep hypoventilation in patients undergoing bariatric surgery, we identified increased postoperative morbidity,” said Dr. Chindamporn, now a pulmonologist and sleep specialist practicing in Bangkok.
Dr. Mehra said in the interview that patients considering bariatric surgery are typically assessed for obstructive sleep apnea, but “not so much obesity hypoventilation syndrome or obesity-associated sleep-related hypoventilation syndrome.” The findings, “support the notion that we should be closely examining sleep-related hypoventilation in these patients.”
At the Cleveland Clinic, “clinically, we make sure we’re identifying these individuals and communicating the findings to bariatric surgery colleagues and to anesthesia,” said Dr. Mehra, also professor of medicine at Case Western Reserve University, Cleveland.
OHS is defined, according to the 2019 American Thoracic Society clinical practice guideline on evaluation and management of OHS, by the combination of obesity, sleep-disordered breathing, and awake daytime hypercapnia, after excluding other causes for hypoventilation (Am J Respir Crit Care Med. 2019;200[3]:e6-24).
A European Respiratory Society task force has proposed severity grading for OHS, with early stages defined by sleep-related hypoventilation and the highest grade of severity defined by morbidity-associated daytime hypercapnia (Eur Respir Rev. 2019;28:180097). However, Dr. Mehra said she is “not sure that we know enough [from long-term studies of OHS] to say definitively that there’s such an evolution.”
Certainly, she said, future research on OHS should consider its heterogeneity. It is possible that a subset of patients with OHS, “maybe these individuals with sleep-related hypoventilation,” are most likely to have adverse postsurgical outcomes.
Atul Malhotra, MD, professor of medicine at the University of California, San Diego, who was asked to comment on the study, said that OHS is understudied in general and particularly in the perioperative setting. “With the obesity pandemic, issues around OHS are likely to be [increasingly] important. And with increasing [use of] bariatric surgery, strategies to minimize risks are clearly needed,” he said, adding that the potential risks of nonbariatric surgery in patients with OHS require further study.
He noted that mortality rates in good hospitals “have become quite low for many elective surgeries, making it hard to show mortality benefit to most interventions.”
The ATS guideline on OHS states that it is the most severe form of obesity-induced respiratory compromise and leads to serious sequelae, including increased rates of mortality, chronic heart failure, pulmonary hypertension, and hospitalization caused by acute-on-chronic hypercapnic respiratory failure.
Dr. Chindamporn said in her presentation that she had no disclosures. Dr. Mehra’s research program is funded by the National Institute of Health, but she has also procured funding from the American College of Chest Physicians, American Heart Association, Clinical Translational Science Collaborative, and Central Society of Clinical Research. Dr. Malhotra disclosed that he is funded by the NIH and has received income from Merck and LIvanova related to medical education.
CORRECTION 9/15/2020: The original story misstated the presenter of the study. Dr. Chindamporn presented the findings.
FROM SLEEP 2020
Insomnia + COPD linked to more outpatient, ED visits
Insomnia is “highly prevalent” in veterans with chronic pulmonary obstructive disease and is significantly associated with greater COPD-related health care utilization, according to an analysis of national Veterans Health Administration data.
“The study highlights the importance of exploring potential sleep disturbances and disorders in this population and suggests that a targeted treatment for insomnia may help to improve COPD outcomes in veterans with COPD and insomnia,” said Faith Luyster, PhD, assistant professor at the University of Pittsburgh, in an interview after the virtual annual meeting of the Associated Professional Sleep Societies, where she presented the findings.
Dr. Luyster and coinvestigators used an administrative database from the Veterans Affairs Corporate Data Warehouse to identify more than 1.5 million patients with COPD who used VHA services over a 6-year period (fiscal years 2011-2017). Insomnia was defined by ICD-9/10 diagnostic codes and/or a sedative-hypnotic prescription for at least 30 doses during any of these years.
Insomnia with COPD was prevalent in this sample of veterans at 37.3%. Compared with veterans without comorbid insomnia, those who had both COPD and insomnia (575,539 of the total 1,542,642) were older (69 vs. 64 years), more likely to be female (6.3% vs. 3.7%), more likely to be Black (14% vs. 11%) and more likely to be a current smoker (46.1% vs. 35.5%).
Those with both COPD and insomnia were also more likely to have a service-connected disability rating of 50% of greater; use supplemental oxygen; be divorced, widowed, or separated; have a higher body mass index; or have other medical or psychiatric conditions – in particular obstructive sleep apnea (39% vs. 7%), depression (21% vs. 5%), and PTSD (33% vs. 3%).
P values were < .001 for all of these demographic and clinical variables, Dr. Luyster reported at the meeting.
Comorbid insomnia clearly impacted health care utilization, she said. Veterans with insomnia in addition to COPD had more outpatient and ED visits (10.5 vs 6.9, and 1.6 vs. 1.4, respectively) and more hospitalizations (2.2 vs. 1.8) with a primary diagnostic code for COPD or COPD exacerbation (P < .001).
A negative binomial regression analysis (P < .001) showed that “even after controlling for demographic and other medical conditions, COPD patients with insomnia had greater rates of health care utilization relative to COPD patients without insomnia,” Dr. Luyster said in the interview.
Prior studies have suggested that disturbed sleep is a predictor of poorer longitudinal outcomes in COPD, even after controlling for COPD severity, but have not looked specifically at insomnia, she said.
Commenting on the study Octavian C. Ioachimescu, MD, PhD, of Emory University, Atlanta, and the Atlanta VA Medical Center in Decatur, said the criteria used to define insomnia – unadjudicated ICD diagnoses as well as sedative-hypnotic prescriptions – may explain part of the reported prevalence of insomnia. Even so, the findings add to existing literature demonstrating that COPD and insomnia are both common disorders among VHA patients, and that their frequent coexistence “could have adverse consequences on the overall health, functional status, long-term outcomes, and quality of life of these patients.”
Questions of causation are yet to be answered, he said. “Is it that uncontrolled or severe airflow obstruction causing frequent nocturnal arousals, dyspnea, orthopnea, overuse of inhaled sympathomimetics and heightened anxiety leads to insomnia? Or is it that insomnia – possibly in a cluster with other affective disorders such as depression, anxiety disorders, or PTSD – elicits more frequent or more severe symptoms of shortness of breath in those with smoking-induced airway and parenchymal lung disease, making the latter diagnosis more overt than in others?
“My bet is on a bidirectional causal relationship,” said Dr. Ioachimescu, an editorial board advisor of CHEST Physician.
“Regardless of the etiology [of insomnia in veterans with COPD],” Dr. Luyster said, “it’s important that [insomnia] be addressed and treated appropriately, whether that be through pharmacological treatment, or probably more ideally through [cognitive behavioral therapy] for insomnia.”
The study did not control for COPD severity, she said, because of the difficulty of extracting this data from the VA Corporate Data Warehouse. The study was funded by the VA Competitive Career Development Fund.Dr. Luyster reported that she had no disclosures. Dr. Ioachimescu also said he had no relevant disclosures.
Insomnia is “highly prevalent” in veterans with chronic pulmonary obstructive disease and is significantly associated with greater COPD-related health care utilization, according to an analysis of national Veterans Health Administration data.
“The study highlights the importance of exploring potential sleep disturbances and disorders in this population and suggests that a targeted treatment for insomnia may help to improve COPD outcomes in veterans with COPD and insomnia,” said Faith Luyster, PhD, assistant professor at the University of Pittsburgh, in an interview after the virtual annual meeting of the Associated Professional Sleep Societies, where she presented the findings.
Dr. Luyster and coinvestigators used an administrative database from the Veterans Affairs Corporate Data Warehouse to identify more than 1.5 million patients with COPD who used VHA services over a 6-year period (fiscal years 2011-2017). Insomnia was defined by ICD-9/10 diagnostic codes and/or a sedative-hypnotic prescription for at least 30 doses during any of these years.
Insomnia with COPD was prevalent in this sample of veterans at 37.3%. Compared with veterans without comorbid insomnia, those who had both COPD and insomnia (575,539 of the total 1,542,642) were older (69 vs. 64 years), more likely to be female (6.3% vs. 3.7%), more likely to be Black (14% vs. 11%) and more likely to be a current smoker (46.1% vs. 35.5%).
Those with both COPD and insomnia were also more likely to have a service-connected disability rating of 50% of greater; use supplemental oxygen; be divorced, widowed, or separated; have a higher body mass index; or have other medical or psychiatric conditions – in particular obstructive sleep apnea (39% vs. 7%), depression (21% vs. 5%), and PTSD (33% vs. 3%).
P values were < .001 for all of these demographic and clinical variables, Dr. Luyster reported at the meeting.
Comorbid insomnia clearly impacted health care utilization, she said. Veterans with insomnia in addition to COPD had more outpatient and ED visits (10.5 vs 6.9, and 1.6 vs. 1.4, respectively) and more hospitalizations (2.2 vs. 1.8) with a primary diagnostic code for COPD or COPD exacerbation (P < .001).
A negative binomial regression analysis (P < .001) showed that “even after controlling for demographic and other medical conditions, COPD patients with insomnia had greater rates of health care utilization relative to COPD patients without insomnia,” Dr. Luyster said in the interview.
Prior studies have suggested that disturbed sleep is a predictor of poorer longitudinal outcomes in COPD, even after controlling for COPD severity, but have not looked specifically at insomnia, she said.
Commenting on the study Octavian C. Ioachimescu, MD, PhD, of Emory University, Atlanta, and the Atlanta VA Medical Center in Decatur, said the criteria used to define insomnia – unadjudicated ICD diagnoses as well as sedative-hypnotic prescriptions – may explain part of the reported prevalence of insomnia. Even so, the findings add to existing literature demonstrating that COPD and insomnia are both common disorders among VHA patients, and that their frequent coexistence “could have adverse consequences on the overall health, functional status, long-term outcomes, and quality of life of these patients.”
Questions of causation are yet to be answered, he said. “Is it that uncontrolled or severe airflow obstruction causing frequent nocturnal arousals, dyspnea, orthopnea, overuse of inhaled sympathomimetics and heightened anxiety leads to insomnia? Or is it that insomnia – possibly in a cluster with other affective disorders such as depression, anxiety disorders, or PTSD – elicits more frequent or more severe symptoms of shortness of breath in those with smoking-induced airway and parenchymal lung disease, making the latter diagnosis more overt than in others?
“My bet is on a bidirectional causal relationship,” said Dr. Ioachimescu, an editorial board advisor of CHEST Physician.
“Regardless of the etiology [of insomnia in veterans with COPD],” Dr. Luyster said, “it’s important that [insomnia] be addressed and treated appropriately, whether that be through pharmacological treatment, or probably more ideally through [cognitive behavioral therapy] for insomnia.”
The study did not control for COPD severity, she said, because of the difficulty of extracting this data from the VA Corporate Data Warehouse. The study was funded by the VA Competitive Career Development Fund.Dr. Luyster reported that she had no disclosures. Dr. Ioachimescu also said he had no relevant disclosures.
Insomnia is “highly prevalent” in veterans with chronic pulmonary obstructive disease and is significantly associated with greater COPD-related health care utilization, according to an analysis of national Veterans Health Administration data.
“The study highlights the importance of exploring potential sleep disturbances and disorders in this population and suggests that a targeted treatment for insomnia may help to improve COPD outcomes in veterans with COPD and insomnia,” said Faith Luyster, PhD, assistant professor at the University of Pittsburgh, in an interview after the virtual annual meeting of the Associated Professional Sleep Societies, where she presented the findings.
Dr. Luyster and coinvestigators used an administrative database from the Veterans Affairs Corporate Data Warehouse to identify more than 1.5 million patients with COPD who used VHA services over a 6-year period (fiscal years 2011-2017). Insomnia was defined by ICD-9/10 diagnostic codes and/or a sedative-hypnotic prescription for at least 30 doses during any of these years.
Insomnia with COPD was prevalent in this sample of veterans at 37.3%. Compared with veterans without comorbid insomnia, those who had both COPD and insomnia (575,539 of the total 1,542,642) were older (69 vs. 64 years), more likely to be female (6.3% vs. 3.7%), more likely to be Black (14% vs. 11%) and more likely to be a current smoker (46.1% vs. 35.5%).
Those with both COPD and insomnia were also more likely to have a service-connected disability rating of 50% of greater; use supplemental oxygen; be divorced, widowed, or separated; have a higher body mass index; or have other medical or psychiatric conditions – in particular obstructive sleep apnea (39% vs. 7%), depression (21% vs. 5%), and PTSD (33% vs. 3%).
P values were < .001 for all of these demographic and clinical variables, Dr. Luyster reported at the meeting.
Comorbid insomnia clearly impacted health care utilization, she said. Veterans with insomnia in addition to COPD had more outpatient and ED visits (10.5 vs 6.9, and 1.6 vs. 1.4, respectively) and more hospitalizations (2.2 vs. 1.8) with a primary diagnostic code for COPD or COPD exacerbation (P < .001).
A negative binomial regression analysis (P < .001) showed that “even after controlling for demographic and other medical conditions, COPD patients with insomnia had greater rates of health care utilization relative to COPD patients without insomnia,” Dr. Luyster said in the interview.
Prior studies have suggested that disturbed sleep is a predictor of poorer longitudinal outcomes in COPD, even after controlling for COPD severity, but have not looked specifically at insomnia, she said.
Commenting on the study Octavian C. Ioachimescu, MD, PhD, of Emory University, Atlanta, and the Atlanta VA Medical Center in Decatur, said the criteria used to define insomnia – unadjudicated ICD diagnoses as well as sedative-hypnotic prescriptions – may explain part of the reported prevalence of insomnia. Even so, the findings add to existing literature demonstrating that COPD and insomnia are both common disorders among VHA patients, and that their frequent coexistence “could have adverse consequences on the overall health, functional status, long-term outcomes, and quality of life of these patients.”
Questions of causation are yet to be answered, he said. “Is it that uncontrolled or severe airflow obstruction causing frequent nocturnal arousals, dyspnea, orthopnea, overuse of inhaled sympathomimetics and heightened anxiety leads to insomnia? Or is it that insomnia – possibly in a cluster with other affective disorders such as depression, anxiety disorders, or PTSD – elicits more frequent or more severe symptoms of shortness of breath in those with smoking-induced airway and parenchymal lung disease, making the latter diagnosis more overt than in others?
“My bet is on a bidirectional causal relationship,” said Dr. Ioachimescu, an editorial board advisor of CHEST Physician.
“Regardless of the etiology [of insomnia in veterans with COPD],” Dr. Luyster said, “it’s important that [insomnia] be addressed and treated appropriately, whether that be through pharmacological treatment, or probably more ideally through [cognitive behavioral therapy] for insomnia.”
The study did not control for COPD severity, she said, because of the difficulty of extracting this data from the VA Corporate Data Warehouse. The study was funded by the VA Competitive Career Development Fund.Dr. Luyster reported that she had no disclosures. Dr. Ioachimescu also said he had no relevant disclosures.
FROM SLEEP 2020
Psoriasis, PsA, and pregnancy: Tailoring treatment with increasing data
With an average age of diagnosis of 28 years, and one of two incidence peaks occurring at 15-30 years, psoriasis affects many women in the midst of their reproductive years. The prospect of pregnancy – or the reality of a surprise pregnancy – drives questions about heritability of the disease in offspring, the impact of the disease on pregnancy outcomes and breastfeeding, and how to best balance risks of treatments with risks of uncontrolled psoriasis and/or psoriatic arthritis (PsA).
While answers to these questions are not always clear, discussions about pregnancy and psoriasis management “shouldn’t be scary,” said Jenny E. Murase, MD, a dermatologist who speaks and writes widely about her research and experience with psoriasis and pregnancy. “We have access to information and data and educational resources to [work with] and reassure our patients – we just need to use it. Right now, there’s unnecessary suffering [with some patients unnecessarily stopping all treatment].”
Much has been learned in the past 2 decades about the course of psoriasis in pregnancy, and pregnancy outcomes data on the safety of biologics during pregnancy are increasingly emerging – particularly for tumor necrosis factor (TNF)–alpha inhibitors.
Ideally, since half of all pregnancies are unplanned, the implications of therapeutic options should be discussed with all women with psoriasis who are of reproductive age, whether they are sexually active or not. “The onus is on us to make sure that we’re considering the possibility [that our patient] could become pregnant without consulting us first,” said Dr. Murase, associate professor of dermatology at the University of California, San Francisco, and director of medical consultative dermatology for the Palo Alto Foundation Medical Group in Mountain View, Calif.
Lisa R. Sammaritano, MD, associate professor of clinical medicine at Weill Cornell Medicine and a rheumatologist at the Hospital for Special Surgery, both in New York, urges similar attention for PsA. “Pregnancy is best planned while patients have quiescent disease on pregnancy-compatible medications,” she said. “We encourage [more] rheumatologists to be actively involved in pregnancy planning [in order] to guide therapy.”
The impact of estrogen
Dr. Murase was inspired to study psoriasis and pregnancy in part by a patient she met as a medical student. “She had severe psoriasis covering her body, and she said that the only times her psoriasis cleared was during her three pregnancies,” Dr. Murase recalled. “I wondered: What about the pregnancies resulted in such a substantial reduction of her psoriasis?”
She subsequently led a study, published in 2005, of 47 pregnant and 27 nonpregnant patients with psoriasis. More than half of the patients – 55% – reported improvements in their psoriasis during pregnancy, 21% reported no change, and 23% reported worsening. Among the 16 patients who had 10% or greater psoriatic body surface area (BSA) involvement and reported improvements, lesions decreased by 84%.
In the postpartum period, only 9% reported improvement, 26% reported no change, and 65% reported worsening. The increased BSA values observed 6 weeks postpartum did not exceed those of the first trimester, suggesting a return to the patients’ baseline status.
Earlier and smaller retrospective studies had also shown that approximately half of patients improve during pregnancy, and it was believed that progesterone was most likely responsible for this improvement. Dr. Murase’s study moved the needle in that it examined BSA in pregnancy and the postpartum period. It also turned the spotlight on estrogen: Patients who had higher levels of improvement also had higher levels of estradiol, estrone, and the ratio of estrogen to progesterone. However, there was no correlation between psoriatic change and levels of progesterone.
To promote fetal survival, pregnancy triggers a shift from Th1 cell–mediated immunity – and Th17 immunity – to Th2 immunity. While there’s no proof of a causative effect, increased estrogen appears to play a role in this shift and in the reduced production of Th1 and Th17 cytokines. Psoriasis is believed to be primarily a Th17-mediated disease, with some Th1 involvement, so this down-regulation can result in improved disease status, Dr. Murase said. (A host of other autoimmune diseases categorized as Th1 mediated similarly tend to improve during pregnancy, she added.)
Information on the effect of pregnancy on PsA is “conflicting,” Dr. Sammaritano said. “Some [of a limited number of studies] suggest a beneficial effect as is generally seen for rheumatoid arthritis. Others, however, have found an increased risk of disease activity during pregnancy ... It may be that psoriatic arthritis can be quite variable from patient to patient in its clinical presentation.”
At least one study, Dr. Sammaritano added, “has shown that the arthritis in pregnancy patients with PsA did not improve, compared to control nonpregnant patients, while the psoriasis rash did improve.”
The mixed findings don’t surprise Dr. Murase. “It harder to quantify joint disease in general,” she said. “And during pregnancy, physiologic changes relating to the pregnancy itself can cause discomfort – your joints ache. The numbers [of improved] cases aren’t as high with PsA, but it’s a more complex question.”
In the postpartum period, however, research findings “all suggest an increased risk of flare” of PsA, Dr. Sammaritano said, just as with psoriasis.
Assessing risk of treatment
Understanding the immunologic effects of pregnancy on psoriasis and PsA – and appreciating the concept of a hormonal component – is an important part of treatment decision making. So is understanding pregnancy outcomes data.
Researchers have looked at a host of pregnancy outcomes – including congenital malformations, preterm birth, spontaneous abortion, low birth weight, macrosomia, and gestational diabetes and hypertension – in women with psoriasis or psoriasis/PsA, compared with control groups. Some studies have suggested a link between disease activity and pregnancy complications or adverse pregnancy outcomes, “just as a result of having moderate to severe disease,” while others have found no evidence of increased risk, Dr. Murase said.
“It’s a bit unclear and a difficult question to answer; it depends on what study you look at and what data you believe. It would be nice to have some clarity, but basically the jury is still out,” said Dr. Murase, who, with coauthors Alice B. Gottlieb, MD, PhD, of the department of dermatology at the Icahn School of Medicine at Mount Sinai, New York, and Caitriona Ryan, MD, of the Blackrock Clinic and Charles Institute of Dermatology, University College Dublin, discussed the pregnancy outcomes data in a recently published review of psoriasis in women.
“In my opinion, because we have therapies that are so low risk and well tolerated, it’s better to make sure that the inflammatory cascade and inflammation created by psoriasis is under control,” she said. “So whether or not the pregnancy itself causes the patient to go into remission, or whether you have to use therapy to help the patient stay in remission, it’s important to control the inflammation.”
Contraindicated in pregnancy are oral psoralen, methotrexate, and acitretin, the latter of which should be avoided for several years before pregnancy and “therefore shouldn’t be used in a woman of childbearing age,” said Dr. Murase. Methotrexate, said Dr. Sammaritano, should generally be stopped 1-3 months prior to conception.
For psoriasis, the therapy that’s “classically considered the safest in pregnancy is UVB light therapy, specifically the 300-nm wavelength of light, which works really well as an anti-inflammatory,” Dr. Murase said. Because of the potential for maternal folate degradation with phototherapy and the long-known association of folate deficiency with neural tube defects, women of childbearing age who are receiving light therapy should take daily folic acid supplementation. (She prescribes a daily prenatal vitamin containing at least 1 mg of folic acid for women who are utilizing light therapy.)
Many topical agents can be used during pregnancy, Dr. Murase said. Topical corticosteroids, she noted, have the most safety-affirming data of any topical medication.
Regarding oral therapies, Dr. Murase recommends against the use of apremilast (Otezla) for her patients. “It’s not contraindicated, but the animal studies don’t look promising, so I don’t use that one in women of childbearing age just in case. There’s just very little data to support the safety of this medication [in pregnancy].”
There are no therapeutic guidelines in the United States for guiding the management of psoriasis in women who are considering pregnancy. In 2012, the medical board of the National Psoriasis Foundation published a review of treatment options for psoriasis in pregnant or lactating women, the “closest thing to guidelines that we’ve had,” said Dr. Murase. (Now almost a decade old, the review addresses TNF inhibitors but does not cover the anti-interleukin agents more recently approved for moderate to severe psoriasis and PsA.)
For treating PsA, rheumatologists now have the American College of Rheumatology’s first guideline for the management of reproductive health in rheumatic and musculoskeletal diseases to reference. The 2020 guideline does not address PsA specifically, but its section on pregnancy and lactation includes recommendations on biologic and other therapies used to treat the disease.
Guidelines aside, physician-patient discussions over drug safety have the potential to be much more meaningful now that drug labels offer clinical summaries, data, and risk summaries regarding potential use in pregnancy. The labels have “more of a narrative, which is a more useful way to counsel patients and make risk-benefit decisions” than the former system of five-letter categories, said Dr. Murase. (The changes were made per the Pregnancy and Lactation Labeling Rule of 2015.)
MothertoBaby, a service of the nonprofit Organization of Teratology Information Specialists, also provides good evidence-based information to physicians and mothers, Dr. Sammaritano noted.
The use of biologic therapies
In a 2017 review of biologic safety for patients with psoriasis during pregnancy, Alexa B. Kimball, MD, MPH, professor of dermatology at Harvard Medical School, Boston; Martina L. Porter, MD, currently with the department of dermatology at Beth Israel Deaconess Medical Center, Boston; and Stephen J. Lockwood, MD, MPH, of the department of dermatology at Harvard Medical School, concluded that an increasing body of literature suggests that biologic agents can be used during pregnancy and breastfeeding. Anti-TNF agents “should be considered over IL-12/23 and IL-17 inhibitors due to the increased availability of long-term data,” they wrote.
“In general,” said Dr. Murase, “there’s more and more data coming out from gastroenterology and rheumatology to reassure patients and prescribing physicians that the TNF-blocker class is likely safe to use in pregnancy,” particularly during the first trimester and early second trimester, when the transport of maternal antibodies across the placenta is “essentially nonexistent.” In the third trimester, the active transport of IgG antibodies increases rapidly.
If possible, said Dr. Sammaritano, who served as lead author of the ACR’s reproductive health guideline, TNF inhibitors “will be stopped prior to the third trimester to avoid [the possibility of] high drug levels in the infant at birth, which raises concern for immunosuppression in the newborn. If disease is very active, however, they can be continued throughout the pregnancy.”
The TNF inhibitor certolizumab pegol (Cimzia) has the advantage of being transported only minimally across the placenta, if at all, she and Dr. Murase both explained. “To be actively carried across, antibodies need what’s called an Fc region for the placenta to grab onto,” Dr. Murase said. Certolizumab – a pegylated anti–binding fragment antibody – lacks this Fc region.
Two recent studies – CRIB and a UCB Pharma safety database analysis – showed “essentially no medication crossing – there were barely detectable levels,” Dr. Murase said. Certolizumab’s label contains this information and other clinical trial data as well as findings from safety database analyses/surveillance registries.
“Before we had much data for the biologics, I’d advise transitioning patients to light therapy from their biologics and a lot of times their psoriasis would improve, but it was more of a dance,” she said. “Now we tend to look at [certolizumab] when they’re of childbearing age and keep them on the treatment. I know that the baby is not being immunosuppressed.”
Consideration of the use of certolizumab when treatment with biologic agents is required throughout the pregnancy is a recommendation included in Dr. Kimball’s 2017 review.
As newer anti-interleukin agents – the IL-12/23 and IL-17 inhibitors – play a growing role in the treatment of psoriasis and PsA, questions loom about their safety profile. Dr. Murase and Dr. Sammaritano are waiting for more data. “In general,” Dr. Sammaritano said, “we recommend stopping them at the time pregnancy is detected, based on a lack of data at this time.”
Small-molecule drugs are also less well studied, she noted. “Because of their low molecular weight, we anticipate they will easily cross the placenta, so we recommend avoiding use during pregnancy until more information is available.”
Postpartum care
The good news, both experts say, is that the vast majority of medications, including biologics, are safe to use during breastfeeding. Methotrexate should be avoided, Dr. Sammaritano pointed out, and the impact of novel small-molecule therapies on breast milk has not been studied.
In her 2019 review of psoriasis in women, Dr. Murase and coauthors wrote that too many dermatologists believe that breastfeeding women should either not be on biologics or are uncertain about biologic use during breastfeeding. However, “biologics are considered compatible for use while breastfeeding due to their large molecular size and the proteolytic environment in the neonatal gastrointestinal tract,” they added.
Counseling and support for breastfeeding is especially important for women with psoriasis, Dr. Murase emphasized. “Breastfeeding is very traumatizing to the skin, and psoriasis can form in skin that’s injured. I have my patients set up an office visit very soon after the pregnancy to make sure they’re doing alright with their breastfeeding and that they’re coating their nipple area with some type of moisturizer and keeping the health of their nipples in good shape.”
Timely reviews of therapy and adjustments are also a priority, she said. “We need to prepare for 6 weeks post partum” when psoriasis will often flare without treatment.
Dr. Murase disclosed that she is a consultant for Dermira, UCB Pharma, Sanofi, Ferndale, and Regeneron. She is also coeditor in chief of the International Journal of Women’s Dermatology. Dr. Sammaritano reported that she has no disclosures relating to the treatment of PsA.
With an average age of diagnosis of 28 years, and one of two incidence peaks occurring at 15-30 years, psoriasis affects many women in the midst of their reproductive years. The prospect of pregnancy – or the reality of a surprise pregnancy – drives questions about heritability of the disease in offspring, the impact of the disease on pregnancy outcomes and breastfeeding, and how to best balance risks of treatments with risks of uncontrolled psoriasis and/or psoriatic arthritis (PsA).
While answers to these questions are not always clear, discussions about pregnancy and psoriasis management “shouldn’t be scary,” said Jenny E. Murase, MD, a dermatologist who speaks and writes widely about her research and experience with psoriasis and pregnancy. “We have access to information and data and educational resources to [work with] and reassure our patients – we just need to use it. Right now, there’s unnecessary suffering [with some patients unnecessarily stopping all treatment].”
Much has been learned in the past 2 decades about the course of psoriasis in pregnancy, and pregnancy outcomes data on the safety of biologics during pregnancy are increasingly emerging – particularly for tumor necrosis factor (TNF)–alpha inhibitors.
Ideally, since half of all pregnancies are unplanned, the implications of therapeutic options should be discussed with all women with psoriasis who are of reproductive age, whether they are sexually active or not. “The onus is on us to make sure that we’re considering the possibility [that our patient] could become pregnant without consulting us first,” said Dr. Murase, associate professor of dermatology at the University of California, San Francisco, and director of medical consultative dermatology for the Palo Alto Foundation Medical Group in Mountain View, Calif.
Lisa R. Sammaritano, MD, associate professor of clinical medicine at Weill Cornell Medicine and a rheumatologist at the Hospital for Special Surgery, both in New York, urges similar attention for PsA. “Pregnancy is best planned while patients have quiescent disease on pregnancy-compatible medications,” she said. “We encourage [more] rheumatologists to be actively involved in pregnancy planning [in order] to guide therapy.”
The impact of estrogen
Dr. Murase was inspired to study psoriasis and pregnancy in part by a patient she met as a medical student. “She had severe psoriasis covering her body, and she said that the only times her psoriasis cleared was during her three pregnancies,” Dr. Murase recalled. “I wondered: What about the pregnancies resulted in such a substantial reduction of her psoriasis?”
She subsequently led a study, published in 2005, of 47 pregnant and 27 nonpregnant patients with psoriasis. More than half of the patients – 55% – reported improvements in their psoriasis during pregnancy, 21% reported no change, and 23% reported worsening. Among the 16 patients who had 10% or greater psoriatic body surface area (BSA) involvement and reported improvements, lesions decreased by 84%.
In the postpartum period, only 9% reported improvement, 26% reported no change, and 65% reported worsening. The increased BSA values observed 6 weeks postpartum did not exceed those of the first trimester, suggesting a return to the patients’ baseline status.
Earlier and smaller retrospective studies had also shown that approximately half of patients improve during pregnancy, and it was believed that progesterone was most likely responsible for this improvement. Dr. Murase’s study moved the needle in that it examined BSA in pregnancy and the postpartum period. It also turned the spotlight on estrogen: Patients who had higher levels of improvement also had higher levels of estradiol, estrone, and the ratio of estrogen to progesterone. However, there was no correlation between psoriatic change and levels of progesterone.
To promote fetal survival, pregnancy triggers a shift from Th1 cell–mediated immunity – and Th17 immunity – to Th2 immunity. While there’s no proof of a causative effect, increased estrogen appears to play a role in this shift and in the reduced production of Th1 and Th17 cytokines. Psoriasis is believed to be primarily a Th17-mediated disease, with some Th1 involvement, so this down-regulation can result in improved disease status, Dr. Murase said. (A host of other autoimmune diseases categorized as Th1 mediated similarly tend to improve during pregnancy, she added.)
Information on the effect of pregnancy on PsA is “conflicting,” Dr. Sammaritano said. “Some [of a limited number of studies] suggest a beneficial effect as is generally seen for rheumatoid arthritis. Others, however, have found an increased risk of disease activity during pregnancy ... It may be that psoriatic arthritis can be quite variable from patient to patient in its clinical presentation.”
At least one study, Dr. Sammaritano added, “has shown that the arthritis in pregnancy patients with PsA did not improve, compared to control nonpregnant patients, while the psoriasis rash did improve.”
The mixed findings don’t surprise Dr. Murase. “It harder to quantify joint disease in general,” she said. “And during pregnancy, physiologic changes relating to the pregnancy itself can cause discomfort – your joints ache. The numbers [of improved] cases aren’t as high with PsA, but it’s a more complex question.”
In the postpartum period, however, research findings “all suggest an increased risk of flare” of PsA, Dr. Sammaritano said, just as with psoriasis.
Assessing risk of treatment
Understanding the immunologic effects of pregnancy on psoriasis and PsA – and appreciating the concept of a hormonal component – is an important part of treatment decision making. So is understanding pregnancy outcomes data.
Researchers have looked at a host of pregnancy outcomes – including congenital malformations, preterm birth, spontaneous abortion, low birth weight, macrosomia, and gestational diabetes and hypertension – in women with psoriasis or psoriasis/PsA, compared with control groups. Some studies have suggested a link between disease activity and pregnancy complications or adverse pregnancy outcomes, “just as a result of having moderate to severe disease,” while others have found no evidence of increased risk, Dr. Murase said.
“It’s a bit unclear and a difficult question to answer; it depends on what study you look at and what data you believe. It would be nice to have some clarity, but basically the jury is still out,” said Dr. Murase, who, with coauthors Alice B. Gottlieb, MD, PhD, of the department of dermatology at the Icahn School of Medicine at Mount Sinai, New York, and Caitriona Ryan, MD, of the Blackrock Clinic and Charles Institute of Dermatology, University College Dublin, discussed the pregnancy outcomes data in a recently published review of psoriasis in women.
“In my opinion, because we have therapies that are so low risk and well tolerated, it’s better to make sure that the inflammatory cascade and inflammation created by psoriasis is under control,” she said. “So whether or not the pregnancy itself causes the patient to go into remission, or whether you have to use therapy to help the patient stay in remission, it’s important to control the inflammation.”
Contraindicated in pregnancy are oral psoralen, methotrexate, and acitretin, the latter of which should be avoided for several years before pregnancy and “therefore shouldn’t be used in a woman of childbearing age,” said Dr. Murase. Methotrexate, said Dr. Sammaritano, should generally be stopped 1-3 months prior to conception.
For psoriasis, the therapy that’s “classically considered the safest in pregnancy is UVB light therapy, specifically the 300-nm wavelength of light, which works really well as an anti-inflammatory,” Dr. Murase said. Because of the potential for maternal folate degradation with phototherapy and the long-known association of folate deficiency with neural tube defects, women of childbearing age who are receiving light therapy should take daily folic acid supplementation. (She prescribes a daily prenatal vitamin containing at least 1 mg of folic acid for women who are utilizing light therapy.)
Many topical agents can be used during pregnancy, Dr. Murase said. Topical corticosteroids, she noted, have the most safety-affirming data of any topical medication.
Regarding oral therapies, Dr. Murase recommends against the use of apremilast (Otezla) for her patients. “It’s not contraindicated, but the animal studies don’t look promising, so I don’t use that one in women of childbearing age just in case. There’s just very little data to support the safety of this medication [in pregnancy].”
There are no therapeutic guidelines in the United States for guiding the management of psoriasis in women who are considering pregnancy. In 2012, the medical board of the National Psoriasis Foundation published a review of treatment options for psoriasis in pregnant or lactating women, the “closest thing to guidelines that we’ve had,” said Dr. Murase. (Now almost a decade old, the review addresses TNF inhibitors but does not cover the anti-interleukin agents more recently approved for moderate to severe psoriasis and PsA.)
For treating PsA, rheumatologists now have the American College of Rheumatology’s first guideline for the management of reproductive health in rheumatic and musculoskeletal diseases to reference. The 2020 guideline does not address PsA specifically, but its section on pregnancy and lactation includes recommendations on biologic and other therapies used to treat the disease.
Guidelines aside, physician-patient discussions over drug safety have the potential to be much more meaningful now that drug labels offer clinical summaries, data, and risk summaries regarding potential use in pregnancy. The labels have “more of a narrative, which is a more useful way to counsel patients and make risk-benefit decisions” than the former system of five-letter categories, said Dr. Murase. (The changes were made per the Pregnancy and Lactation Labeling Rule of 2015.)
MothertoBaby, a service of the nonprofit Organization of Teratology Information Specialists, also provides good evidence-based information to physicians and mothers, Dr. Sammaritano noted.
The use of biologic therapies
In a 2017 review of biologic safety for patients with psoriasis during pregnancy, Alexa B. Kimball, MD, MPH, professor of dermatology at Harvard Medical School, Boston; Martina L. Porter, MD, currently with the department of dermatology at Beth Israel Deaconess Medical Center, Boston; and Stephen J. Lockwood, MD, MPH, of the department of dermatology at Harvard Medical School, concluded that an increasing body of literature suggests that biologic agents can be used during pregnancy and breastfeeding. Anti-TNF agents “should be considered over IL-12/23 and IL-17 inhibitors due to the increased availability of long-term data,” they wrote.
“In general,” said Dr. Murase, “there’s more and more data coming out from gastroenterology and rheumatology to reassure patients and prescribing physicians that the TNF-blocker class is likely safe to use in pregnancy,” particularly during the first trimester and early second trimester, when the transport of maternal antibodies across the placenta is “essentially nonexistent.” In the third trimester, the active transport of IgG antibodies increases rapidly.
If possible, said Dr. Sammaritano, who served as lead author of the ACR’s reproductive health guideline, TNF inhibitors “will be stopped prior to the third trimester to avoid [the possibility of] high drug levels in the infant at birth, which raises concern for immunosuppression in the newborn. If disease is very active, however, they can be continued throughout the pregnancy.”
The TNF inhibitor certolizumab pegol (Cimzia) has the advantage of being transported only minimally across the placenta, if at all, she and Dr. Murase both explained. “To be actively carried across, antibodies need what’s called an Fc region for the placenta to grab onto,” Dr. Murase said. Certolizumab – a pegylated anti–binding fragment antibody – lacks this Fc region.
Two recent studies – CRIB and a UCB Pharma safety database analysis – showed “essentially no medication crossing – there were barely detectable levels,” Dr. Murase said. Certolizumab’s label contains this information and other clinical trial data as well as findings from safety database analyses/surveillance registries.
“Before we had much data for the biologics, I’d advise transitioning patients to light therapy from their biologics and a lot of times their psoriasis would improve, but it was more of a dance,” she said. “Now we tend to look at [certolizumab] when they’re of childbearing age and keep them on the treatment. I know that the baby is not being immunosuppressed.”
Consideration of the use of certolizumab when treatment with biologic agents is required throughout the pregnancy is a recommendation included in Dr. Kimball’s 2017 review.
As newer anti-interleukin agents – the IL-12/23 and IL-17 inhibitors – play a growing role in the treatment of psoriasis and PsA, questions loom about their safety profile. Dr. Murase and Dr. Sammaritano are waiting for more data. “In general,” Dr. Sammaritano said, “we recommend stopping them at the time pregnancy is detected, based on a lack of data at this time.”
Small-molecule drugs are also less well studied, she noted. “Because of their low molecular weight, we anticipate they will easily cross the placenta, so we recommend avoiding use during pregnancy until more information is available.”
Postpartum care
The good news, both experts say, is that the vast majority of medications, including biologics, are safe to use during breastfeeding. Methotrexate should be avoided, Dr. Sammaritano pointed out, and the impact of novel small-molecule therapies on breast milk has not been studied.
In her 2019 review of psoriasis in women, Dr. Murase and coauthors wrote that too many dermatologists believe that breastfeeding women should either not be on biologics or are uncertain about biologic use during breastfeeding. However, “biologics are considered compatible for use while breastfeeding due to their large molecular size and the proteolytic environment in the neonatal gastrointestinal tract,” they added.
Counseling and support for breastfeeding is especially important for women with psoriasis, Dr. Murase emphasized. “Breastfeeding is very traumatizing to the skin, and psoriasis can form in skin that’s injured. I have my patients set up an office visit very soon after the pregnancy to make sure they’re doing alright with their breastfeeding and that they’re coating their nipple area with some type of moisturizer and keeping the health of their nipples in good shape.”
Timely reviews of therapy and adjustments are also a priority, she said. “We need to prepare for 6 weeks post partum” when psoriasis will often flare without treatment.
Dr. Murase disclosed that she is a consultant for Dermira, UCB Pharma, Sanofi, Ferndale, and Regeneron. She is also coeditor in chief of the International Journal of Women’s Dermatology. Dr. Sammaritano reported that she has no disclosures relating to the treatment of PsA.
With an average age of diagnosis of 28 years, and one of two incidence peaks occurring at 15-30 years, psoriasis affects many women in the midst of their reproductive years. The prospect of pregnancy – or the reality of a surprise pregnancy – drives questions about heritability of the disease in offspring, the impact of the disease on pregnancy outcomes and breastfeeding, and how to best balance risks of treatments with risks of uncontrolled psoriasis and/or psoriatic arthritis (PsA).
While answers to these questions are not always clear, discussions about pregnancy and psoriasis management “shouldn’t be scary,” said Jenny E. Murase, MD, a dermatologist who speaks and writes widely about her research and experience with psoriasis and pregnancy. “We have access to information and data and educational resources to [work with] and reassure our patients – we just need to use it. Right now, there’s unnecessary suffering [with some patients unnecessarily stopping all treatment].”
Much has been learned in the past 2 decades about the course of psoriasis in pregnancy, and pregnancy outcomes data on the safety of biologics during pregnancy are increasingly emerging – particularly for tumor necrosis factor (TNF)–alpha inhibitors.
Ideally, since half of all pregnancies are unplanned, the implications of therapeutic options should be discussed with all women with psoriasis who are of reproductive age, whether they are sexually active or not. “The onus is on us to make sure that we’re considering the possibility [that our patient] could become pregnant without consulting us first,” said Dr. Murase, associate professor of dermatology at the University of California, San Francisco, and director of medical consultative dermatology for the Palo Alto Foundation Medical Group in Mountain View, Calif.
Lisa R. Sammaritano, MD, associate professor of clinical medicine at Weill Cornell Medicine and a rheumatologist at the Hospital for Special Surgery, both in New York, urges similar attention for PsA. “Pregnancy is best planned while patients have quiescent disease on pregnancy-compatible medications,” she said. “We encourage [more] rheumatologists to be actively involved in pregnancy planning [in order] to guide therapy.”
The impact of estrogen
Dr. Murase was inspired to study psoriasis and pregnancy in part by a patient she met as a medical student. “She had severe psoriasis covering her body, and she said that the only times her psoriasis cleared was during her three pregnancies,” Dr. Murase recalled. “I wondered: What about the pregnancies resulted in such a substantial reduction of her psoriasis?”
She subsequently led a study, published in 2005, of 47 pregnant and 27 nonpregnant patients with psoriasis. More than half of the patients – 55% – reported improvements in their psoriasis during pregnancy, 21% reported no change, and 23% reported worsening. Among the 16 patients who had 10% or greater psoriatic body surface area (BSA) involvement and reported improvements, lesions decreased by 84%.
In the postpartum period, only 9% reported improvement, 26% reported no change, and 65% reported worsening. The increased BSA values observed 6 weeks postpartum did not exceed those of the first trimester, suggesting a return to the patients’ baseline status.
Earlier and smaller retrospective studies had also shown that approximately half of patients improve during pregnancy, and it was believed that progesterone was most likely responsible for this improvement. Dr. Murase’s study moved the needle in that it examined BSA in pregnancy and the postpartum period. It also turned the spotlight on estrogen: Patients who had higher levels of improvement also had higher levels of estradiol, estrone, and the ratio of estrogen to progesterone. However, there was no correlation between psoriatic change and levels of progesterone.
To promote fetal survival, pregnancy triggers a shift from Th1 cell–mediated immunity – and Th17 immunity – to Th2 immunity. While there’s no proof of a causative effect, increased estrogen appears to play a role in this shift and in the reduced production of Th1 and Th17 cytokines. Psoriasis is believed to be primarily a Th17-mediated disease, with some Th1 involvement, so this down-regulation can result in improved disease status, Dr. Murase said. (A host of other autoimmune diseases categorized as Th1 mediated similarly tend to improve during pregnancy, she added.)
Information on the effect of pregnancy on PsA is “conflicting,” Dr. Sammaritano said. “Some [of a limited number of studies] suggest a beneficial effect as is generally seen for rheumatoid arthritis. Others, however, have found an increased risk of disease activity during pregnancy ... It may be that psoriatic arthritis can be quite variable from patient to patient in its clinical presentation.”
At least one study, Dr. Sammaritano added, “has shown that the arthritis in pregnancy patients with PsA did not improve, compared to control nonpregnant patients, while the psoriasis rash did improve.”
The mixed findings don’t surprise Dr. Murase. “It harder to quantify joint disease in general,” she said. “And during pregnancy, physiologic changes relating to the pregnancy itself can cause discomfort – your joints ache. The numbers [of improved] cases aren’t as high with PsA, but it’s a more complex question.”
In the postpartum period, however, research findings “all suggest an increased risk of flare” of PsA, Dr. Sammaritano said, just as with psoriasis.
Assessing risk of treatment
Understanding the immunologic effects of pregnancy on psoriasis and PsA – and appreciating the concept of a hormonal component – is an important part of treatment decision making. So is understanding pregnancy outcomes data.
Researchers have looked at a host of pregnancy outcomes – including congenital malformations, preterm birth, spontaneous abortion, low birth weight, macrosomia, and gestational diabetes and hypertension – in women with psoriasis or psoriasis/PsA, compared with control groups. Some studies have suggested a link between disease activity and pregnancy complications or adverse pregnancy outcomes, “just as a result of having moderate to severe disease,” while others have found no evidence of increased risk, Dr. Murase said.
“It’s a bit unclear and a difficult question to answer; it depends on what study you look at and what data you believe. It would be nice to have some clarity, but basically the jury is still out,” said Dr. Murase, who, with coauthors Alice B. Gottlieb, MD, PhD, of the department of dermatology at the Icahn School of Medicine at Mount Sinai, New York, and Caitriona Ryan, MD, of the Blackrock Clinic and Charles Institute of Dermatology, University College Dublin, discussed the pregnancy outcomes data in a recently published review of psoriasis in women.
“In my opinion, because we have therapies that are so low risk and well tolerated, it’s better to make sure that the inflammatory cascade and inflammation created by psoriasis is under control,” she said. “So whether or not the pregnancy itself causes the patient to go into remission, or whether you have to use therapy to help the patient stay in remission, it’s important to control the inflammation.”
Contraindicated in pregnancy are oral psoralen, methotrexate, and acitretin, the latter of which should be avoided for several years before pregnancy and “therefore shouldn’t be used in a woman of childbearing age,” said Dr. Murase. Methotrexate, said Dr. Sammaritano, should generally be stopped 1-3 months prior to conception.
For psoriasis, the therapy that’s “classically considered the safest in pregnancy is UVB light therapy, specifically the 300-nm wavelength of light, which works really well as an anti-inflammatory,” Dr. Murase said. Because of the potential for maternal folate degradation with phototherapy and the long-known association of folate deficiency with neural tube defects, women of childbearing age who are receiving light therapy should take daily folic acid supplementation. (She prescribes a daily prenatal vitamin containing at least 1 mg of folic acid for women who are utilizing light therapy.)
Many topical agents can be used during pregnancy, Dr. Murase said. Topical corticosteroids, she noted, have the most safety-affirming data of any topical medication.
Regarding oral therapies, Dr. Murase recommends against the use of apremilast (Otezla) for her patients. “It’s not contraindicated, but the animal studies don’t look promising, so I don’t use that one in women of childbearing age just in case. There’s just very little data to support the safety of this medication [in pregnancy].”
There are no therapeutic guidelines in the United States for guiding the management of psoriasis in women who are considering pregnancy. In 2012, the medical board of the National Psoriasis Foundation published a review of treatment options for psoriasis in pregnant or lactating women, the “closest thing to guidelines that we’ve had,” said Dr. Murase. (Now almost a decade old, the review addresses TNF inhibitors but does not cover the anti-interleukin agents more recently approved for moderate to severe psoriasis and PsA.)
For treating PsA, rheumatologists now have the American College of Rheumatology’s first guideline for the management of reproductive health in rheumatic and musculoskeletal diseases to reference. The 2020 guideline does not address PsA specifically, but its section on pregnancy and lactation includes recommendations on biologic and other therapies used to treat the disease.
Guidelines aside, physician-patient discussions over drug safety have the potential to be much more meaningful now that drug labels offer clinical summaries, data, and risk summaries regarding potential use in pregnancy. The labels have “more of a narrative, which is a more useful way to counsel patients and make risk-benefit decisions” than the former system of five-letter categories, said Dr. Murase. (The changes were made per the Pregnancy and Lactation Labeling Rule of 2015.)
MothertoBaby, a service of the nonprofit Organization of Teratology Information Specialists, also provides good evidence-based information to physicians and mothers, Dr. Sammaritano noted.
The use of biologic therapies
In a 2017 review of biologic safety for patients with psoriasis during pregnancy, Alexa B. Kimball, MD, MPH, professor of dermatology at Harvard Medical School, Boston; Martina L. Porter, MD, currently with the department of dermatology at Beth Israel Deaconess Medical Center, Boston; and Stephen J. Lockwood, MD, MPH, of the department of dermatology at Harvard Medical School, concluded that an increasing body of literature suggests that biologic agents can be used during pregnancy and breastfeeding. Anti-TNF agents “should be considered over IL-12/23 and IL-17 inhibitors due to the increased availability of long-term data,” they wrote.
“In general,” said Dr. Murase, “there’s more and more data coming out from gastroenterology and rheumatology to reassure patients and prescribing physicians that the TNF-blocker class is likely safe to use in pregnancy,” particularly during the first trimester and early second trimester, when the transport of maternal antibodies across the placenta is “essentially nonexistent.” In the third trimester, the active transport of IgG antibodies increases rapidly.
If possible, said Dr. Sammaritano, who served as lead author of the ACR’s reproductive health guideline, TNF inhibitors “will be stopped prior to the third trimester to avoid [the possibility of] high drug levels in the infant at birth, which raises concern for immunosuppression in the newborn. If disease is very active, however, they can be continued throughout the pregnancy.”
The TNF inhibitor certolizumab pegol (Cimzia) has the advantage of being transported only minimally across the placenta, if at all, she and Dr. Murase both explained. “To be actively carried across, antibodies need what’s called an Fc region for the placenta to grab onto,” Dr. Murase said. Certolizumab – a pegylated anti–binding fragment antibody – lacks this Fc region.
Two recent studies – CRIB and a UCB Pharma safety database analysis – showed “essentially no medication crossing – there were barely detectable levels,” Dr. Murase said. Certolizumab’s label contains this information and other clinical trial data as well as findings from safety database analyses/surveillance registries.
“Before we had much data for the biologics, I’d advise transitioning patients to light therapy from their biologics and a lot of times their psoriasis would improve, but it was more of a dance,” she said. “Now we tend to look at [certolizumab] when they’re of childbearing age and keep them on the treatment. I know that the baby is not being immunosuppressed.”
Consideration of the use of certolizumab when treatment with biologic agents is required throughout the pregnancy is a recommendation included in Dr. Kimball’s 2017 review.
As newer anti-interleukin agents – the IL-12/23 and IL-17 inhibitors – play a growing role in the treatment of psoriasis and PsA, questions loom about their safety profile. Dr. Murase and Dr. Sammaritano are waiting for more data. “In general,” Dr. Sammaritano said, “we recommend stopping them at the time pregnancy is detected, based on a lack of data at this time.”
Small-molecule drugs are also less well studied, she noted. “Because of their low molecular weight, we anticipate they will easily cross the placenta, so we recommend avoiding use during pregnancy until more information is available.”
Postpartum care
The good news, both experts say, is that the vast majority of medications, including biologics, are safe to use during breastfeeding. Methotrexate should be avoided, Dr. Sammaritano pointed out, and the impact of novel small-molecule therapies on breast milk has not been studied.
In her 2019 review of psoriasis in women, Dr. Murase and coauthors wrote that too many dermatologists believe that breastfeeding women should either not be on biologics or are uncertain about biologic use during breastfeeding. However, “biologics are considered compatible for use while breastfeeding due to their large molecular size and the proteolytic environment in the neonatal gastrointestinal tract,” they added.
Counseling and support for breastfeeding is especially important for women with psoriasis, Dr. Murase emphasized. “Breastfeeding is very traumatizing to the skin, and psoriasis can form in skin that’s injured. I have my patients set up an office visit very soon after the pregnancy to make sure they’re doing alright with their breastfeeding and that they’re coating their nipple area with some type of moisturizer and keeping the health of their nipples in good shape.”
Timely reviews of therapy and adjustments are also a priority, she said. “We need to prepare for 6 weeks post partum” when psoriasis will often flare without treatment.
Dr. Murase disclosed that she is a consultant for Dermira, UCB Pharma, Sanofi, Ferndale, and Regeneron. She is also coeditor in chief of the International Journal of Women’s Dermatology. Dr. Sammaritano reported that she has no disclosures relating to the treatment of PsA.
Study highlights role of structural racism in delayed autism diagnoses
An analysis of a large cohort of African American children with autism spectrum disorder (ASD) reveals a more than 3-year time lag between parental recognition of a development delay and an ASD diagnosis, reported John N. Constantino, MD, of the department of psychiatry at Washington University, St. Louis, and coauthors.
The analysis also highlights the need to further understand – and act on – the disproportionate burden of intellectual disability comorbidity among these children, the investigators say.
Their analysis, published in Pediatrics, builds on national community surveillance data from the Centers for Disease Control and Prevention published in 2018 showing near-equal rates of identification of ASD among African American (and other minorities) and non-Hispanic white children, but greater delays in diagnosis for African American children as well as twice the rate of comorbid intellectual disability, compared with non-Hispanic white children (44% vs. 22%).
To explore potential drivers of both diagnostic delays and the intellectual disability disparity, the investigators tapped into a repository of data on 584 African American children with ASD and their first-degree relatives who were consecutively enrolled in the National Institutes of Health–funded Autism Genetic Resource Exchange across four academic sites. The program aims to improve the representation of families of self-reported African ancestry in ASD genetics research.
The mean age of diagnosis was 65 months, which came at an average of more than 3 years after parents reported having concerns about their child’s language, behavior or development – and “the period when early developmental therapies (typically delivered through part C interventions in the United States) are initiated to ameliorate the disability associated with ASD,” Dr. Constantino and associates said.
Approximately 42% reported seeing multiple professionals before receiving an ASD diagnosis (14% saw six or more), and 31% said that a lack of available professionals had contributed to the delay. Almost all families – 98% – reported having some type of health insurance at the time of their first concerns (49% private, 46% public, and 5% others).
The data also show that excess intellectual disability comorbidity seen in African American children cannot be explained by familial or sociodemographic factors that have traditionally been associated with variation in IQ in the general population. Nor can it be explained by overclassification of intellectual disability, the authors said.
they wrote.
The NIH-funded program involved parental completion of “Diagnostic Odyssey” interviews (characterizing service-seeking experiences and obstacles to diagnosis, treatment, and care) and several in-person cognitive assessments and measurements of adaptive functioning. “These were in-depth [highly validated] intellectual assessments based on IQ measures that were tailored to the level of functioning of the children and backed by extensive assessments of adaptive functioning,” Dr. Constantino said in an interview.
Historically, autism has been underdiagnosed among minority children. Now that this is no longer the case, as demonstrated in the CDC’s 2018 report from its Autism and Developmental Disabilities Monitoring Network, the thought that higher rates of intellectual disability comorbidity among minority children are due to ascertainment bias – to “our only diagnosing the most serious cases” – “is no longer true,” he said.
And now, with use of data from the largest-available repository of diagnostic and phenotypic information on African American children with ASD, “we’ve dispelled other misperceptions, other factors that might be used to dismiss or explain away why Black children might have a high rate of intellectual disability,” Dr. Constantino said in the interview, referring to the absence of association between the IQ scores of children with ASD and those of their first-degree relatives as well as the lack of significant associations between the IQ of children with ASD and factors such as family income (above versus below the median income of the cohort), the mother having or not having a college degree, and the estimated gestational age at birth (before versus after 37 weeks).
“This kind of complication of autism lasts for the life of a child and profoundly impairs their functioning,” he said. “If anyone thinks there isn’t an opportunity to improve the timing of diagnosis and to improve access to services and appropriate developmental therapies, that’s wrong. There is opportunity – parents are raising the alarm, and we are not coming to these children’s rescue.”
In an accompanying editorial, Sarabeth Broder-Fingert, MD, MPH, of Boston University and Boston Medical Center, and associates wrote that the “confluence of findings [in this study] are suggestive of structural racism leading to inequity.”
For example, they said, “although the causes of delays from first parental concern to ASD diagnosis are complex, they can result from a number of issues, including racial bias and discrimination experienced by families, a lack of diversity in health professionals (impacting patient-provider relationships), and/or concentration of specialists in geographic areas with fewer minority residents.” Each of these issues, they wrote, can be linked to racism, both structural and individual.
Combined with previous research on inequity in ASD, the new data “necessitate an immediate evaluation of how issues of structural racism have impacted ASD diagnosis and, more importantly, an action plan to address inequity,” they said.
Issues of workforce capacity for ASD diagnosis need to be addressed by evaluating Medicaid reimbursement rates for ASD diagnosis, for instance, and removing restrictions on who is qualified to make a diagnosis, increasing adherence to evidence-based practices, “increasing workforce cultural humility, and recruiting a workforce that reflects the diverse communities they serve,” Dr. Broder-Fingert and associates said.
Jeremiah Dickerson, MD, a child and adolescent psychiatrist at the University of Vermont, Burlington, said he is hopeful that the inequities and structural obstacles that he sees in his patients are “being informed more and more by science” and that “we’re taking steps in exploring our own cultural humility and focusing on problems ... that have been under the surface for decades.”
Years of diagnostic delay and missed intervention for ASD can lead to increasing lifelong functional difficulties, which in turn can be compounded by enduring inequities and stigma, he said when asked to comment on the study.
“Diagnosing and teasing apart ID [intellectual disability] versus ASD, and ID co-occurring with ASD, can be very complicated, particularly in young children with significant language impairments,” he added. “If indeed there is a higher proportion of African American children with co-occurring ASD and ID ... we have to do a much better job with identifying those children earlier and providing longitudinal follow-up/assessment that can help provide diagnostic clarity and inform recommendations.”
Understanding better why this occurs “without repeating the history of assigning cause based upon racist thinking” is also important, said Dr. Dickerson, who directs the autism assessment clinic at the university’s Vermont Center for Children, Youth & Families.
Dr. Constantino, who has been involved in the CDC’s 11-site ASD surveillance network, said it is unclear to what extent broad implementation of early and high-quality interventions can reduce the proportion of African American children with autism and comorbid intellectual disability. “We may be only half-successful in closing the gap, or there may be other factors involved that we don’t understand yet,” he said. “But we haven’t even attempted to close the gap [through] reasonable application of an intervention strategy that is available and that we know can improve cognitive outcomes.”
“Some primary care doctors are reluctant to make the diagnosis in the first place because they have nothing to offer the families,” Dr. Constantino noted.
Continued research on the interactions between genetic background and specific biological susceptibilities to autism is an ongoing objective of the Autism Genetic Resource Exchange.
The CDC recently published its latest report on the prevalence of ASD in children aged 8 years, concluding again that continued efforts are needed for “early and equitable identification of ASD and timely enrollment in services.
The study was supported by grants from the National Institutes of Health and from the Intellectual and Developmental Disabilities Research Center at Washington University. Dr. Constantino is author of the Social Responsiveness Scale-2, from which he receives royalties. A coauthor helped author the Vineland-3 and receives royalties, and this coauthor and another associate also have ties to pharmaceutical companies or other organizations; the remaining authors of the study said they had no relevant financial disclosures. Dr. Broder-Fingert and associates said they have no relevant financial relationships; the editorial was funded by the National Institutes of Health. Dr. Dickerson said he had no relevant financial disclosures.
SOURCE: Constantino JN et al. Pediatrics. 2020. doi: 10.1542/peds.2019-3629.
An analysis of a large cohort of African American children with autism spectrum disorder (ASD) reveals a more than 3-year time lag between parental recognition of a development delay and an ASD diagnosis, reported John N. Constantino, MD, of the department of psychiatry at Washington University, St. Louis, and coauthors.
The analysis also highlights the need to further understand – and act on – the disproportionate burden of intellectual disability comorbidity among these children, the investigators say.
Their analysis, published in Pediatrics, builds on national community surveillance data from the Centers for Disease Control and Prevention published in 2018 showing near-equal rates of identification of ASD among African American (and other minorities) and non-Hispanic white children, but greater delays in diagnosis for African American children as well as twice the rate of comorbid intellectual disability, compared with non-Hispanic white children (44% vs. 22%).
To explore potential drivers of both diagnostic delays and the intellectual disability disparity, the investigators tapped into a repository of data on 584 African American children with ASD and their first-degree relatives who were consecutively enrolled in the National Institutes of Health–funded Autism Genetic Resource Exchange across four academic sites. The program aims to improve the representation of families of self-reported African ancestry in ASD genetics research.
The mean age of diagnosis was 65 months, which came at an average of more than 3 years after parents reported having concerns about their child’s language, behavior or development – and “the period when early developmental therapies (typically delivered through part C interventions in the United States) are initiated to ameliorate the disability associated with ASD,” Dr. Constantino and associates said.
Approximately 42% reported seeing multiple professionals before receiving an ASD diagnosis (14% saw six or more), and 31% said that a lack of available professionals had contributed to the delay. Almost all families – 98% – reported having some type of health insurance at the time of their first concerns (49% private, 46% public, and 5% others).
The data also show that excess intellectual disability comorbidity seen in African American children cannot be explained by familial or sociodemographic factors that have traditionally been associated with variation in IQ in the general population. Nor can it be explained by overclassification of intellectual disability, the authors said.
they wrote.
The NIH-funded program involved parental completion of “Diagnostic Odyssey” interviews (characterizing service-seeking experiences and obstacles to diagnosis, treatment, and care) and several in-person cognitive assessments and measurements of adaptive functioning. “These were in-depth [highly validated] intellectual assessments based on IQ measures that were tailored to the level of functioning of the children and backed by extensive assessments of adaptive functioning,” Dr. Constantino said in an interview.
Historically, autism has been underdiagnosed among minority children. Now that this is no longer the case, as demonstrated in the CDC’s 2018 report from its Autism and Developmental Disabilities Monitoring Network, the thought that higher rates of intellectual disability comorbidity among minority children are due to ascertainment bias – to “our only diagnosing the most serious cases” – “is no longer true,” he said.
And now, with use of data from the largest-available repository of diagnostic and phenotypic information on African American children with ASD, “we’ve dispelled other misperceptions, other factors that might be used to dismiss or explain away why Black children might have a high rate of intellectual disability,” Dr. Constantino said in the interview, referring to the absence of association between the IQ scores of children with ASD and those of their first-degree relatives as well as the lack of significant associations between the IQ of children with ASD and factors such as family income (above versus below the median income of the cohort), the mother having or not having a college degree, and the estimated gestational age at birth (before versus after 37 weeks).
“This kind of complication of autism lasts for the life of a child and profoundly impairs their functioning,” he said. “If anyone thinks there isn’t an opportunity to improve the timing of diagnosis and to improve access to services and appropriate developmental therapies, that’s wrong. There is opportunity – parents are raising the alarm, and we are not coming to these children’s rescue.”
In an accompanying editorial, Sarabeth Broder-Fingert, MD, MPH, of Boston University and Boston Medical Center, and associates wrote that the “confluence of findings [in this study] are suggestive of structural racism leading to inequity.”
For example, they said, “although the causes of delays from first parental concern to ASD diagnosis are complex, they can result from a number of issues, including racial bias and discrimination experienced by families, a lack of diversity in health professionals (impacting patient-provider relationships), and/or concentration of specialists in geographic areas with fewer minority residents.” Each of these issues, they wrote, can be linked to racism, both structural and individual.
Combined with previous research on inequity in ASD, the new data “necessitate an immediate evaluation of how issues of structural racism have impacted ASD diagnosis and, more importantly, an action plan to address inequity,” they said.
Issues of workforce capacity for ASD diagnosis need to be addressed by evaluating Medicaid reimbursement rates for ASD diagnosis, for instance, and removing restrictions on who is qualified to make a diagnosis, increasing adherence to evidence-based practices, “increasing workforce cultural humility, and recruiting a workforce that reflects the diverse communities they serve,” Dr. Broder-Fingert and associates said.
Jeremiah Dickerson, MD, a child and adolescent psychiatrist at the University of Vermont, Burlington, said he is hopeful that the inequities and structural obstacles that he sees in his patients are “being informed more and more by science” and that “we’re taking steps in exploring our own cultural humility and focusing on problems ... that have been under the surface for decades.”
Years of diagnostic delay and missed intervention for ASD can lead to increasing lifelong functional difficulties, which in turn can be compounded by enduring inequities and stigma, he said when asked to comment on the study.
“Diagnosing and teasing apart ID [intellectual disability] versus ASD, and ID co-occurring with ASD, can be very complicated, particularly in young children with significant language impairments,” he added. “If indeed there is a higher proportion of African American children with co-occurring ASD and ID ... we have to do a much better job with identifying those children earlier and providing longitudinal follow-up/assessment that can help provide diagnostic clarity and inform recommendations.”
Understanding better why this occurs “without repeating the history of assigning cause based upon racist thinking” is also important, said Dr. Dickerson, who directs the autism assessment clinic at the university’s Vermont Center for Children, Youth & Families.
Dr. Constantino, who has been involved in the CDC’s 11-site ASD surveillance network, said it is unclear to what extent broad implementation of early and high-quality interventions can reduce the proportion of African American children with autism and comorbid intellectual disability. “We may be only half-successful in closing the gap, or there may be other factors involved that we don’t understand yet,” he said. “But we haven’t even attempted to close the gap [through] reasonable application of an intervention strategy that is available and that we know can improve cognitive outcomes.”
“Some primary care doctors are reluctant to make the diagnosis in the first place because they have nothing to offer the families,” Dr. Constantino noted.
Continued research on the interactions between genetic background and specific biological susceptibilities to autism is an ongoing objective of the Autism Genetic Resource Exchange.
The CDC recently published its latest report on the prevalence of ASD in children aged 8 years, concluding again that continued efforts are needed for “early and equitable identification of ASD and timely enrollment in services.
The study was supported by grants from the National Institutes of Health and from the Intellectual and Developmental Disabilities Research Center at Washington University. Dr. Constantino is author of the Social Responsiveness Scale-2, from which he receives royalties. A coauthor helped author the Vineland-3 and receives royalties, and this coauthor and another associate also have ties to pharmaceutical companies or other organizations; the remaining authors of the study said they had no relevant financial disclosures. Dr. Broder-Fingert and associates said they have no relevant financial relationships; the editorial was funded by the National Institutes of Health. Dr. Dickerson said he had no relevant financial disclosures.
SOURCE: Constantino JN et al. Pediatrics. 2020. doi: 10.1542/peds.2019-3629.
An analysis of a large cohort of African American children with autism spectrum disorder (ASD) reveals a more than 3-year time lag between parental recognition of a development delay and an ASD diagnosis, reported John N. Constantino, MD, of the department of psychiatry at Washington University, St. Louis, and coauthors.
The analysis also highlights the need to further understand – and act on – the disproportionate burden of intellectual disability comorbidity among these children, the investigators say.
Their analysis, published in Pediatrics, builds on national community surveillance data from the Centers for Disease Control and Prevention published in 2018 showing near-equal rates of identification of ASD among African American (and other minorities) and non-Hispanic white children, but greater delays in diagnosis for African American children as well as twice the rate of comorbid intellectual disability, compared with non-Hispanic white children (44% vs. 22%).
To explore potential drivers of both diagnostic delays and the intellectual disability disparity, the investigators tapped into a repository of data on 584 African American children with ASD and their first-degree relatives who were consecutively enrolled in the National Institutes of Health–funded Autism Genetic Resource Exchange across four academic sites. The program aims to improve the representation of families of self-reported African ancestry in ASD genetics research.
The mean age of diagnosis was 65 months, which came at an average of more than 3 years after parents reported having concerns about their child’s language, behavior or development – and “the period when early developmental therapies (typically delivered through part C interventions in the United States) are initiated to ameliorate the disability associated with ASD,” Dr. Constantino and associates said.
Approximately 42% reported seeing multiple professionals before receiving an ASD diagnosis (14% saw six or more), and 31% said that a lack of available professionals had contributed to the delay. Almost all families – 98% – reported having some type of health insurance at the time of their first concerns (49% private, 46% public, and 5% others).
The data also show that excess intellectual disability comorbidity seen in African American children cannot be explained by familial or sociodemographic factors that have traditionally been associated with variation in IQ in the general population. Nor can it be explained by overclassification of intellectual disability, the authors said.
they wrote.
The NIH-funded program involved parental completion of “Diagnostic Odyssey” interviews (characterizing service-seeking experiences and obstacles to diagnosis, treatment, and care) and several in-person cognitive assessments and measurements of adaptive functioning. “These were in-depth [highly validated] intellectual assessments based on IQ measures that were tailored to the level of functioning of the children and backed by extensive assessments of adaptive functioning,” Dr. Constantino said in an interview.
Historically, autism has been underdiagnosed among minority children. Now that this is no longer the case, as demonstrated in the CDC’s 2018 report from its Autism and Developmental Disabilities Monitoring Network, the thought that higher rates of intellectual disability comorbidity among minority children are due to ascertainment bias – to “our only diagnosing the most serious cases” – “is no longer true,” he said.
And now, with use of data from the largest-available repository of diagnostic and phenotypic information on African American children with ASD, “we’ve dispelled other misperceptions, other factors that might be used to dismiss or explain away why Black children might have a high rate of intellectual disability,” Dr. Constantino said in the interview, referring to the absence of association between the IQ scores of children with ASD and those of their first-degree relatives as well as the lack of significant associations between the IQ of children with ASD and factors such as family income (above versus below the median income of the cohort), the mother having or not having a college degree, and the estimated gestational age at birth (before versus after 37 weeks).
“This kind of complication of autism lasts for the life of a child and profoundly impairs their functioning,” he said. “If anyone thinks there isn’t an opportunity to improve the timing of diagnosis and to improve access to services and appropriate developmental therapies, that’s wrong. There is opportunity – parents are raising the alarm, and we are not coming to these children’s rescue.”
In an accompanying editorial, Sarabeth Broder-Fingert, MD, MPH, of Boston University and Boston Medical Center, and associates wrote that the “confluence of findings [in this study] are suggestive of structural racism leading to inequity.”
For example, they said, “although the causes of delays from first parental concern to ASD diagnosis are complex, they can result from a number of issues, including racial bias and discrimination experienced by families, a lack of diversity in health professionals (impacting patient-provider relationships), and/or concentration of specialists in geographic areas with fewer minority residents.” Each of these issues, they wrote, can be linked to racism, both structural and individual.
Combined with previous research on inequity in ASD, the new data “necessitate an immediate evaluation of how issues of structural racism have impacted ASD diagnosis and, more importantly, an action plan to address inequity,” they said.
Issues of workforce capacity for ASD diagnosis need to be addressed by evaluating Medicaid reimbursement rates for ASD diagnosis, for instance, and removing restrictions on who is qualified to make a diagnosis, increasing adherence to evidence-based practices, “increasing workforce cultural humility, and recruiting a workforce that reflects the diverse communities they serve,” Dr. Broder-Fingert and associates said.
Jeremiah Dickerson, MD, a child and adolescent psychiatrist at the University of Vermont, Burlington, said he is hopeful that the inequities and structural obstacles that he sees in his patients are “being informed more and more by science” and that “we’re taking steps in exploring our own cultural humility and focusing on problems ... that have been under the surface for decades.”
Years of diagnostic delay and missed intervention for ASD can lead to increasing lifelong functional difficulties, which in turn can be compounded by enduring inequities and stigma, he said when asked to comment on the study.
“Diagnosing and teasing apart ID [intellectual disability] versus ASD, and ID co-occurring with ASD, can be very complicated, particularly in young children with significant language impairments,” he added. “If indeed there is a higher proportion of African American children with co-occurring ASD and ID ... we have to do a much better job with identifying those children earlier and providing longitudinal follow-up/assessment that can help provide diagnostic clarity and inform recommendations.”
Understanding better why this occurs “without repeating the history of assigning cause based upon racist thinking” is also important, said Dr. Dickerson, who directs the autism assessment clinic at the university’s Vermont Center for Children, Youth & Families.
Dr. Constantino, who has been involved in the CDC’s 11-site ASD surveillance network, said it is unclear to what extent broad implementation of early and high-quality interventions can reduce the proportion of African American children with autism and comorbid intellectual disability. “We may be only half-successful in closing the gap, or there may be other factors involved that we don’t understand yet,” he said. “But we haven’t even attempted to close the gap [through] reasonable application of an intervention strategy that is available and that we know can improve cognitive outcomes.”
“Some primary care doctors are reluctant to make the diagnosis in the first place because they have nothing to offer the families,” Dr. Constantino noted.
Continued research on the interactions between genetic background and specific biological susceptibilities to autism is an ongoing objective of the Autism Genetic Resource Exchange.
The CDC recently published its latest report on the prevalence of ASD in children aged 8 years, concluding again that continued efforts are needed for “early and equitable identification of ASD and timely enrollment in services.
The study was supported by grants from the National Institutes of Health and from the Intellectual and Developmental Disabilities Research Center at Washington University. Dr. Constantino is author of the Social Responsiveness Scale-2, from which he receives royalties. A coauthor helped author the Vineland-3 and receives royalties, and this coauthor and another associate also have ties to pharmaceutical companies or other organizations; the remaining authors of the study said they had no relevant financial disclosures. Dr. Broder-Fingert and associates said they have no relevant financial relationships; the editorial was funded by the National Institutes of Health. Dr. Dickerson said he had no relevant financial disclosures.
SOURCE: Constantino JN et al. Pediatrics. 2020. doi: 10.1542/peds.2019-3629.
FROM PEDIATRICS
New uterine compression technique controls postpartum hemorrhage
A newly described uterine compression technique that uses simple supplies and does not require hysterotomy was successful in controlling postpartum hemorrhage in 16 of 18 (89%) women in two teaching hospitals in Nigeria, averting the need for hysterectomy in these women.
Each of the women had severe postpartum hemorrhage attributable to uterine atony and had undergone local protocols for medical management “to no avail,” Chidi Ochu Uzoma Esike, MD, who developed the technique, wrote in a report published in Obstetrics and Gynecology.
The technique involves placing six polyglactin (Vicryl) #2 or chromic #2 sutures in the lower uterine segment – three anteriorly and three posteriorly – and could be particularly useful in developing countries, where many women die from postpartum hemorrhage “because most of the medical officers who attend the majority of births in health facilities can perform cesarean delivery but cannot perform hysterectomy and find existing compression suture techniques too complex to perform,” Dr. Esike wrote in the case series report.
In addition, “specialized sutures and needles required for some of the known compression techniques are not readily available,” said Dr. Esike of the department of obstetrics and gynecology at Alex Ekwueme Federal University Hospital and Ebyonyi State University in Abakaliki, Nigeria.
Angela Martin, MD, a maternal-fetal medicine specialist at the University of Kansas Medical Center in Kansas City, said that “having a quick and effective surgical technique [for uncontrollable postpartum hemorrhage] is essential.”
“I love that Esike’s technique uses polyglactin (Vicryl) or chromic sutures. These are familiar to most surgeons, cheap, and typically available even in most resource-deficient settings,” said Dr. Martin, who was asked to comment on the report, adding that several of the known surgical techniques for uterine atony require a skilled operator and are indeed not universally feasible.
“If successful,” Dr. Martin said in an interview, “compression sutures can be lifesaving and fertility preserving.”
The technique involves tying the two middle sutures (one placed anteriorly and one posteriorly) at the fundus as an assistant slowly and continuously compresses the uterus. The more laterally placed sutures are tied similarly, with each pair tied at about 4 cm from the lateral edge of the uterus. “As the uterus is compressed, the slack should be taken up by the sutures before tying,” said Dr. Esike, whose report features both diagrammatic and photographic representations of suture insertion and tying.
For patients who delivered vaginally – nine in this case series – the technique involves performing a laparotomy and exteriorizing the uterus. The technique’s “suture placement,” Dr. Esike wrote, “took 11-25 minutes from the onset of laparotomy to completion.” There were no short or long-term complications in any of the 18 patients.
B-Lynch compression sutures are more complex to perform and require a larger curved needle, Dr. Esike wrote, and the Hayman technique similarly requires a longer needle that may not be available in resource-constrained countries. The hysterotomy required in the B-Lynch technique, Dr. Esike added, “leads to the uterus not contracting maximally until it is repaired,” which increases blood loss from the procedure.
Dr. Martin said the small size of the case series is not discouraging. “The B-Lynch suture was widely adopted after it was described in five cases in 1997,” she said. There are no randomized controlled trials to suggest that one method of uterine compression sutures is better than another. “Ultimately,” she said, “the technique chosen will depend on the surgeon’s training and available supplies.”
Dr. Esike had no relevant financial disclosures. Dr. Martin had no relevant financial disclosures.
SOURCE: Esike COU. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003947.
A newly described uterine compression technique that uses simple supplies and does not require hysterotomy was successful in controlling postpartum hemorrhage in 16 of 18 (89%) women in two teaching hospitals in Nigeria, averting the need for hysterectomy in these women.
Each of the women had severe postpartum hemorrhage attributable to uterine atony and had undergone local protocols for medical management “to no avail,” Chidi Ochu Uzoma Esike, MD, who developed the technique, wrote in a report published in Obstetrics and Gynecology.
The technique involves placing six polyglactin (Vicryl) #2 or chromic #2 sutures in the lower uterine segment – three anteriorly and three posteriorly – and could be particularly useful in developing countries, where many women die from postpartum hemorrhage “because most of the medical officers who attend the majority of births in health facilities can perform cesarean delivery but cannot perform hysterectomy and find existing compression suture techniques too complex to perform,” Dr. Esike wrote in the case series report.
In addition, “specialized sutures and needles required for some of the known compression techniques are not readily available,” said Dr. Esike of the department of obstetrics and gynecology at Alex Ekwueme Federal University Hospital and Ebyonyi State University in Abakaliki, Nigeria.
Angela Martin, MD, a maternal-fetal medicine specialist at the University of Kansas Medical Center in Kansas City, said that “having a quick and effective surgical technique [for uncontrollable postpartum hemorrhage] is essential.”
“I love that Esike’s technique uses polyglactin (Vicryl) or chromic sutures. These are familiar to most surgeons, cheap, and typically available even in most resource-deficient settings,” said Dr. Martin, who was asked to comment on the report, adding that several of the known surgical techniques for uterine atony require a skilled operator and are indeed not universally feasible.
“If successful,” Dr. Martin said in an interview, “compression sutures can be lifesaving and fertility preserving.”
The technique involves tying the two middle sutures (one placed anteriorly and one posteriorly) at the fundus as an assistant slowly and continuously compresses the uterus. The more laterally placed sutures are tied similarly, with each pair tied at about 4 cm from the lateral edge of the uterus. “As the uterus is compressed, the slack should be taken up by the sutures before tying,” said Dr. Esike, whose report features both diagrammatic and photographic representations of suture insertion and tying.
For patients who delivered vaginally – nine in this case series – the technique involves performing a laparotomy and exteriorizing the uterus. The technique’s “suture placement,” Dr. Esike wrote, “took 11-25 minutes from the onset of laparotomy to completion.” There were no short or long-term complications in any of the 18 patients.
B-Lynch compression sutures are more complex to perform and require a larger curved needle, Dr. Esike wrote, and the Hayman technique similarly requires a longer needle that may not be available in resource-constrained countries. The hysterotomy required in the B-Lynch technique, Dr. Esike added, “leads to the uterus not contracting maximally until it is repaired,” which increases blood loss from the procedure.
Dr. Martin said the small size of the case series is not discouraging. “The B-Lynch suture was widely adopted after it was described in five cases in 1997,” she said. There are no randomized controlled trials to suggest that one method of uterine compression sutures is better than another. “Ultimately,” she said, “the technique chosen will depend on the surgeon’s training and available supplies.”
Dr. Esike had no relevant financial disclosures. Dr. Martin had no relevant financial disclosures.
SOURCE: Esike COU. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003947.
A newly described uterine compression technique that uses simple supplies and does not require hysterotomy was successful in controlling postpartum hemorrhage in 16 of 18 (89%) women in two teaching hospitals in Nigeria, averting the need for hysterectomy in these women.
Each of the women had severe postpartum hemorrhage attributable to uterine atony and had undergone local protocols for medical management “to no avail,” Chidi Ochu Uzoma Esike, MD, who developed the technique, wrote in a report published in Obstetrics and Gynecology.
The technique involves placing six polyglactin (Vicryl) #2 or chromic #2 sutures in the lower uterine segment – three anteriorly and three posteriorly – and could be particularly useful in developing countries, where many women die from postpartum hemorrhage “because most of the medical officers who attend the majority of births in health facilities can perform cesarean delivery but cannot perform hysterectomy and find existing compression suture techniques too complex to perform,” Dr. Esike wrote in the case series report.
In addition, “specialized sutures and needles required for some of the known compression techniques are not readily available,” said Dr. Esike of the department of obstetrics and gynecology at Alex Ekwueme Federal University Hospital and Ebyonyi State University in Abakaliki, Nigeria.
Angela Martin, MD, a maternal-fetal medicine specialist at the University of Kansas Medical Center in Kansas City, said that “having a quick and effective surgical technique [for uncontrollable postpartum hemorrhage] is essential.”
“I love that Esike’s technique uses polyglactin (Vicryl) or chromic sutures. These are familiar to most surgeons, cheap, and typically available even in most resource-deficient settings,” said Dr. Martin, who was asked to comment on the report, adding that several of the known surgical techniques for uterine atony require a skilled operator and are indeed not universally feasible.
“If successful,” Dr. Martin said in an interview, “compression sutures can be lifesaving and fertility preserving.”
The technique involves tying the two middle sutures (one placed anteriorly and one posteriorly) at the fundus as an assistant slowly and continuously compresses the uterus. The more laterally placed sutures are tied similarly, with each pair tied at about 4 cm from the lateral edge of the uterus. “As the uterus is compressed, the slack should be taken up by the sutures before tying,” said Dr. Esike, whose report features both diagrammatic and photographic representations of suture insertion and tying.
For patients who delivered vaginally – nine in this case series – the technique involves performing a laparotomy and exteriorizing the uterus. The technique’s “suture placement,” Dr. Esike wrote, “took 11-25 minutes from the onset of laparotomy to completion.” There were no short or long-term complications in any of the 18 patients.
B-Lynch compression sutures are more complex to perform and require a larger curved needle, Dr. Esike wrote, and the Hayman technique similarly requires a longer needle that may not be available in resource-constrained countries. The hysterotomy required in the B-Lynch technique, Dr. Esike added, “leads to the uterus not contracting maximally until it is repaired,” which increases blood loss from the procedure.
Dr. Martin said the small size of the case series is not discouraging. “The B-Lynch suture was widely adopted after it was described in five cases in 1997,” she said. There are no randomized controlled trials to suggest that one method of uterine compression sutures is better than another. “Ultimately,” she said, “the technique chosen will depend on the surgeon’s training and available supplies.”
Dr. Esike had no relevant financial disclosures. Dr. Martin had no relevant financial disclosures.
SOURCE: Esike COU. Obstet Gynecol. 2020. doi: 10.1097/AOG.0000000000003947.
FROM OBSTETRICS & GYNECOLOGY
Screening criteria for diabetes in youth won’t capture all at high risk
and therefore “may miss high-risk youth who should be targeted for diabetes prevention,” according to the investigators of a cross-sectional analysis of youth in the 1999-2016 National Health and Nutrition Examination Survey (NHANES) database.
Regardless of whether or not youth meet screening eligibility, they say, hemoglobin A1c appears to be a “specific and useful test” for detecting high-risk youth.
Those with prediabetic levels of A1c or fasting plasma glucose (FPG) – A1c especially – had a high burden of other cardiometabolic risk factors that could benefit from lifestyle interventions to prevent diabetes and cardiovascular risk in adulthood, wrote Amelia S. Wallace and coinvestigators at the Johns Hopkins Bloomberg School of Public Health, Baltimore. The report is in Pediatrics.Their epidemiologic study had two aims: To assess the performance of the American Diabetes Association guidelines for screening in youth, and to evaluate how well various clinical definitions of diabetes and prediabetes identify U.S. youth at high cardiometabolic risk.
The 2018 ADA guidelines recommend screening for type 2 diabetes and prediabetes in all asymptomatic youth ages 10 years and older who are overweight or obese and who have at least one risk factor for diabetes: nonwhite race, family history of type 2 diabetes, maternal gestational diabetes, or signs of insulin resistance or conditions associated with insulin resistance (Diabetes Care. 2018:41[suppl 1:S13-S37]).
Approximately one-quarter of U.S. youth were found to be eligible for screening under the current ADA criteria, but there were few cases of confirmed diabetes (A1c greater than or equal to 6.5% and fasting plasma glucose greater than or equal to 126 mg/dL) that had gone undiagnosed (less than 0.5%), said Ms. Wallace and her associates.
Considering all hyperglycemia (undiagnosed diabetes or prediabetes) in the NHANES youth population, the sensitivity and specificity of the ADA criteria for detecting A1c-defined hyperglycemia (greater than or equal to 5.7%) were 56% and 76%, respectively, and the sensitivity and specificity for detecting FBG-defined hyperglycemia (greater than or equal to 100 mg/dL) were 36% and 77%.
The prevalence of any hyperglycemia was higher in youth who met ADA screening criteria than in those who didn’t, but there were also “a substantial number of youth with hyperglycemia in the non–screening eligible population,” they wrote. “In fact, the absolute number of youth with elevated FPG was larger in the non–screening eligible population, and the majority (88.5%) of these youth were of normal weight.”
Across all youth (irrespective of screening eligibility), both FPG and A1c-defined hyperglycemia effectively identified children and adolescents who had a high burden of cardiometabolic risk (obesity, metabolic syndrome, and hypercholesterolemia). Using a confirmatory definition of elevations in both FPG and A1c “provided the highest discrimination for cardiometabolic risk,” Ms. Wallace and her associates said.
But in comparing the single tests, risk factor associations with hyperglycemia were consistently stronger with A1c-defined hyperglycemia (odds ratios of 2.6-4.1) than FBG-defined hyperglycemia (ORs of 1.5-3.0). A1c-defined hyperglycemia “identifies a smaller, but higher-risk, population than FPG-defined hyperglycemia,” they said.
In an accompanying commentary, Tamara S. Hannon, MD, MS, of the division of pediatric endocrinology and diabetology at Indiana University in Indianapolis, said that more effective algorithms to determine who should have laboratory testing “could be useful.” Still, “for youth with obesity and multiple risk factors for developing type 2 diabetes, the principal challenge is how to effectively prevent or delay this disease for them and future generations.”
Pediatricians, she said, should screen for prediabetes and type 2 diabetes “according to professional recommendations with simple clinical tests, such as A1c. Screening and education about prediabetes alone can lead to better rates of follow-up for obesity,” she noted (Pediatrics. August 2020. doi: 10.1542/peds.2020-010272).
Sheela N. Magge, MD, MSCE, who directs the division of pediatric endocrinology and diabetes at John Hopkins University, Baltimore, and was asked to comment on the study, similarly said that the findings should not discourage use of the ADA guidelines.
While the guidelines may not have optimal sensitivity and specificity, “neither HbA1c nor fasting glucose are perfect screening tools for prediabetes and likely give us different mechanistic information,” she said. (The ADA guidelines also allow the use of a 2-hour oral glucose tolerance test, but this is not often used by pediatricians, she noted.)
The measurements are “only tools used to identify children who have prediabetes and are therefore at increased risk for type 2 diabetes,” said Dr. Magge, the Lawson Wilkins Endowed Chair of Pediatric Endocrinology at the university. “These children then need to be managed and followed to try to prevent worsening glycemia.”
Both she and Dr. Hannon stressed that youth with type 2 diabetes have more rapidly progressive disease compared with adults.
Microvascular complications are seen even at diagnosis, Dr. Magge said, and “youth may face serious complications such as cardiovascular disease decades earlier than previous generations.”
Dr. Hannon also noted in her commentary that oral diabetes medications often fail in youth with type 2 diabetes, leading to insulin therapy early on.
The prevalence of youth-onset type 2 diabetes has increased because of rising rates of pediatric overweight and obesity, Dr. Magge emphasized. In her experience, the diabetes risk factors that guide the ADA’s screening approach “are so common in overweight and obese youth that they all have at least one.”
The NHANES data did not contain information on all the variables that make up the current diabetes screening criteria in youth; there was no explicit information on history of maternal gestational diabetes and family history of type 2 diabetes, for instance, or the presence of acanthosis nigricans or polycystic ovarian syndrome – conditions associated with insulin resistance. The investigators said it’s likely, therefore, that the study underestimated the number of U.S. youth who would be eligible for diabetes screening.
And, as Dr. Magge said, “it is difficult to determine which risk factors [in the ADA guidelines] were less predictive.”
The NHANES analysis covered 14,119 youth in the 1999-2016 NHANES surveys, which consisted of interviews and standardized physical exams, including laboratory tests, in home and at a mobile examination center. Analyses involving any fasting lab tests were limited to a random subsample of participants aged 12-19 years without diagnosed diabetes who were asked to fast the night before; 6,225 youth properly followed instructions and were included in this subsample.
The surveys are conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. The study authors and the editorial author indicated that they have no relevant financial disclosures or conflicts of interest. Dr. Magge also said she has no relevant disclosures.
SOURCE: Wallace AS et al. Pediatrics. August 2020. doi: 10.1542/peds.2020-0265.
and therefore “may miss high-risk youth who should be targeted for diabetes prevention,” according to the investigators of a cross-sectional analysis of youth in the 1999-2016 National Health and Nutrition Examination Survey (NHANES) database.
Regardless of whether or not youth meet screening eligibility, they say, hemoglobin A1c appears to be a “specific and useful test” for detecting high-risk youth.
Those with prediabetic levels of A1c or fasting plasma glucose (FPG) – A1c especially – had a high burden of other cardiometabolic risk factors that could benefit from lifestyle interventions to prevent diabetes and cardiovascular risk in adulthood, wrote Amelia S. Wallace and coinvestigators at the Johns Hopkins Bloomberg School of Public Health, Baltimore. The report is in Pediatrics.Their epidemiologic study had two aims: To assess the performance of the American Diabetes Association guidelines for screening in youth, and to evaluate how well various clinical definitions of diabetes and prediabetes identify U.S. youth at high cardiometabolic risk.
The 2018 ADA guidelines recommend screening for type 2 diabetes and prediabetes in all asymptomatic youth ages 10 years and older who are overweight or obese and who have at least one risk factor for diabetes: nonwhite race, family history of type 2 diabetes, maternal gestational diabetes, or signs of insulin resistance or conditions associated with insulin resistance (Diabetes Care. 2018:41[suppl 1:S13-S37]).
Approximately one-quarter of U.S. youth were found to be eligible for screening under the current ADA criteria, but there were few cases of confirmed diabetes (A1c greater than or equal to 6.5% and fasting plasma glucose greater than or equal to 126 mg/dL) that had gone undiagnosed (less than 0.5%), said Ms. Wallace and her associates.
Considering all hyperglycemia (undiagnosed diabetes or prediabetes) in the NHANES youth population, the sensitivity and specificity of the ADA criteria for detecting A1c-defined hyperglycemia (greater than or equal to 5.7%) were 56% and 76%, respectively, and the sensitivity and specificity for detecting FBG-defined hyperglycemia (greater than or equal to 100 mg/dL) were 36% and 77%.
The prevalence of any hyperglycemia was higher in youth who met ADA screening criteria than in those who didn’t, but there were also “a substantial number of youth with hyperglycemia in the non–screening eligible population,” they wrote. “In fact, the absolute number of youth with elevated FPG was larger in the non–screening eligible population, and the majority (88.5%) of these youth were of normal weight.”
Across all youth (irrespective of screening eligibility), both FPG and A1c-defined hyperglycemia effectively identified children and adolescents who had a high burden of cardiometabolic risk (obesity, metabolic syndrome, and hypercholesterolemia). Using a confirmatory definition of elevations in both FPG and A1c “provided the highest discrimination for cardiometabolic risk,” Ms. Wallace and her associates said.
But in comparing the single tests, risk factor associations with hyperglycemia were consistently stronger with A1c-defined hyperglycemia (odds ratios of 2.6-4.1) than FBG-defined hyperglycemia (ORs of 1.5-3.0). A1c-defined hyperglycemia “identifies a smaller, but higher-risk, population than FPG-defined hyperglycemia,” they said.
In an accompanying commentary, Tamara S. Hannon, MD, MS, of the division of pediatric endocrinology and diabetology at Indiana University in Indianapolis, said that more effective algorithms to determine who should have laboratory testing “could be useful.” Still, “for youth with obesity and multiple risk factors for developing type 2 diabetes, the principal challenge is how to effectively prevent or delay this disease for them and future generations.”
Pediatricians, she said, should screen for prediabetes and type 2 diabetes “according to professional recommendations with simple clinical tests, such as A1c. Screening and education about prediabetes alone can lead to better rates of follow-up for obesity,” she noted (Pediatrics. August 2020. doi: 10.1542/peds.2020-010272).
Sheela N. Magge, MD, MSCE, who directs the division of pediatric endocrinology and diabetes at John Hopkins University, Baltimore, and was asked to comment on the study, similarly said that the findings should not discourage use of the ADA guidelines.
While the guidelines may not have optimal sensitivity and specificity, “neither HbA1c nor fasting glucose are perfect screening tools for prediabetes and likely give us different mechanistic information,” she said. (The ADA guidelines also allow the use of a 2-hour oral glucose tolerance test, but this is not often used by pediatricians, she noted.)
The measurements are “only tools used to identify children who have prediabetes and are therefore at increased risk for type 2 diabetes,” said Dr. Magge, the Lawson Wilkins Endowed Chair of Pediatric Endocrinology at the university. “These children then need to be managed and followed to try to prevent worsening glycemia.”
Both she and Dr. Hannon stressed that youth with type 2 diabetes have more rapidly progressive disease compared with adults.
Microvascular complications are seen even at diagnosis, Dr. Magge said, and “youth may face serious complications such as cardiovascular disease decades earlier than previous generations.”
Dr. Hannon also noted in her commentary that oral diabetes medications often fail in youth with type 2 diabetes, leading to insulin therapy early on.
The prevalence of youth-onset type 2 diabetes has increased because of rising rates of pediatric overweight and obesity, Dr. Magge emphasized. In her experience, the diabetes risk factors that guide the ADA’s screening approach “are so common in overweight and obese youth that they all have at least one.”
The NHANES data did not contain information on all the variables that make up the current diabetes screening criteria in youth; there was no explicit information on history of maternal gestational diabetes and family history of type 2 diabetes, for instance, or the presence of acanthosis nigricans or polycystic ovarian syndrome – conditions associated with insulin resistance. The investigators said it’s likely, therefore, that the study underestimated the number of U.S. youth who would be eligible for diabetes screening.
And, as Dr. Magge said, “it is difficult to determine which risk factors [in the ADA guidelines] were less predictive.”
The NHANES analysis covered 14,119 youth in the 1999-2016 NHANES surveys, which consisted of interviews and standardized physical exams, including laboratory tests, in home and at a mobile examination center. Analyses involving any fasting lab tests were limited to a random subsample of participants aged 12-19 years without diagnosed diabetes who were asked to fast the night before; 6,225 youth properly followed instructions and were included in this subsample.
The surveys are conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. The study authors and the editorial author indicated that they have no relevant financial disclosures or conflicts of interest. Dr. Magge also said she has no relevant disclosures.
SOURCE: Wallace AS et al. Pediatrics. August 2020. doi: 10.1542/peds.2020-0265.
and therefore “may miss high-risk youth who should be targeted for diabetes prevention,” according to the investigators of a cross-sectional analysis of youth in the 1999-2016 National Health and Nutrition Examination Survey (NHANES) database.
Regardless of whether or not youth meet screening eligibility, they say, hemoglobin A1c appears to be a “specific and useful test” for detecting high-risk youth.
Those with prediabetic levels of A1c or fasting plasma glucose (FPG) – A1c especially – had a high burden of other cardiometabolic risk factors that could benefit from lifestyle interventions to prevent diabetes and cardiovascular risk in adulthood, wrote Amelia S. Wallace and coinvestigators at the Johns Hopkins Bloomberg School of Public Health, Baltimore. The report is in Pediatrics.Their epidemiologic study had two aims: To assess the performance of the American Diabetes Association guidelines for screening in youth, and to evaluate how well various clinical definitions of diabetes and prediabetes identify U.S. youth at high cardiometabolic risk.
The 2018 ADA guidelines recommend screening for type 2 diabetes and prediabetes in all asymptomatic youth ages 10 years and older who are overweight or obese and who have at least one risk factor for diabetes: nonwhite race, family history of type 2 diabetes, maternal gestational diabetes, or signs of insulin resistance or conditions associated with insulin resistance (Diabetes Care. 2018:41[suppl 1:S13-S37]).
Approximately one-quarter of U.S. youth were found to be eligible for screening under the current ADA criteria, but there were few cases of confirmed diabetes (A1c greater than or equal to 6.5% and fasting plasma glucose greater than or equal to 126 mg/dL) that had gone undiagnosed (less than 0.5%), said Ms. Wallace and her associates.
Considering all hyperglycemia (undiagnosed diabetes or prediabetes) in the NHANES youth population, the sensitivity and specificity of the ADA criteria for detecting A1c-defined hyperglycemia (greater than or equal to 5.7%) were 56% and 76%, respectively, and the sensitivity and specificity for detecting FBG-defined hyperglycemia (greater than or equal to 100 mg/dL) were 36% and 77%.
The prevalence of any hyperglycemia was higher in youth who met ADA screening criteria than in those who didn’t, but there were also “a substantial number of youth with hyperglycemia in the non–screening eligible population,” they wrote. “In fact, the absolute number of youth with elevated FPG was larger in the non–screening eligible population, and the majority (88.5%) of these youth were of normal weight.”
Across all youth (irrespective of screening eligibility), both FPG and A1c-defined hyperglycemia effectively identified children and adolescents who had a high burden of cardiometabolic risk (obesity, metabolic syndrome, and hypercholesterolemia). Using a confirmatory definition of elevations in both FPG and A1c “provided the highest discrimination for cardiometabolic risk,” Ms. Wallace and her associates said.
But in comparing the single tests, risk factor associations with hyperglycemia were consistently stronger with A1c-defined hyperglycemia (odds ratios of 2.6-4.1) than FBG-defined hyperglycemia (ORs of 1.5-3.0). A1c-defined hyperglycemia “identifies a smaller, but higher-risk, population than FPG-defined hyperglycemia,” they said.
In an accompanying commentary, Tamara S. Hannon, MD, MS, of the division of pediatric endocrinology and diabetology at Indiana University in Indianapolis, said that more effective algorithms to determine who should have laboratory testing “could be useful.” Still, “for youth with obesity and multiple risk factors for developing type 2 diabetes, the principal challenge is how to effectively prevent or delay this disease for them and future generations.”
Pediatricians, she said, should screen for prediabetes and type 2 diabetes “according to professional recommendations with simple clinical tests, such as A1c. Screening and education about prediabetes alone can lead to better rates of follow-up for obesity,” she noted (Pediatrics. August 2020. doi: 10.1542/peds.2020-010272).
Sheela N. Magge, MD, MSCE, who directs the division of pediatric endocrinology and diabetes at John Hopkins University, Baltimore, and was asked to comment on the study, similarly said that the findings should not discourage use of the ADA guidelines.
While the guidelines may not have optimal sensitivity and specificity, “neither HbA1c nor fasting glucose are perfect screening tools for prediabetes and likely give us different mechanistic information,” she said. (The ADA guidelines also allow the use of a 2-hour oral glucose tolerance test, but this is not often used by pediatricians, she noted.)
The measurements are “only tools used to identify children who have prediabetes and are therefore at increased risk for type 2 diabetes,” said Dr. Magge, the Lawson Wilkins Endowed Chair of Pediatric Endocrinology at the university. “These children then need to be managed and followed to try to prevent worsening glycemia.”
Both she and Dr. Hannon stressed that youth with type 2 diabetes have more rapidly progressive disease compared with adults.
Microvascular complications are seen even at diagnosis, Dr. Magge said, and “youth may face serious complications such as cardiovascular disease decades earlier than previous generations.”
Dr. Hannon also noted in her commentary that oral diabetes medications often fail in youth with type 2 diabetes, leading to insulin therapy early on.
The prevalence of youth-onset type 2 diabetes has increased because of rising rates of pediatric overweight and obesity, Dr. Magge emphasized. In her experience, the diabetes risk factors that guide the ADA’s screening approach “are so common in overweight and obese youth that they all have at least one.”
The NHANES data did not contain information on all the variables that make up the current diabetes screening criteria in youth; there was no explicit information on history of maternal gestational diabetes and family history of type 2 diabetes, for instance, or the presence of acanthosis nigricans or polycystic ovarian syndrome – conditions associated with insulin resistance. The investigators said it’s likely, therefore, that the study underestimated the number of U.S. youth who would be eligible for diabetes screening.
And, as Dr. Magge said, “it is difficult to determine which risk factors [in the ADA guidelines] were less predictive.”
The NHANES analysis covered 14,119 youth in the 1999-2016 NHANES surveys, which consisted of interviews and standardized physical exams, including laboratory tests, in home and at a mobile examination center. Analyses involving any fasting lab tests were limited to a random subsample of participants aged 12-19 years without diagnosed diabetes who were asked to fast the night before; 6,225 youth properly followed instructions and were included in this subsample.
The surveys are conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. The study authors and the editorial author indicated that they have no relevant financial disclosures or conflicts of interest. Dr. Magge also said she has no relevant disclosures.
SOURCE: Wallace AS et al. Pediatrics. August 2020. doi: 10.1542/peds.2020-0265.
FROM PEDIATRICS
How three cardiac procedures changed in the COVID era
When Virginia’s governor directed the postponement of all elective surgeries in late March, Wayne Batchelor, MD and his colleagues at the Inova Heart and Vascular Institute in Falls Church, Va., canceled about two-thirds of their transcatheter aortic valve replacement (TAVR) procedures.
They then categorized patients by tiers to gauge which procedures could safely be postponed and to guide triaging. And while they did not deviate from the practice of having both an interventional cardiologist and a cardiothoracic surgeon present for TAVR, they slimmed down preprocedural testing when feasible and delayed some 30-day post-TAVR echocardiographic assessments. “It was a delicate dance, very difficult dance. But luckily, we were able to navigate the challenges effectively,” said Dr. Batchelor, the institute’s director of interventional cardiology and interventional cardiology research.
A “system capacity dashboard” that merged bed and staffing data from interventional cardiology spaces with cardiovascular and noncardiovascular ICU beds, operating rooms, and other resources – and daily cross-department meetings – enabled them to proceed with the most urgent TAVR procedures while “keeping a buffer of ICU beds to accommodate an anticipated surge of COVID-19,” he explained.
Such adaptations in cardiac procedures and processes are occurring in hospitals across the country as efforts are made to minimize the risk of COVID-19 exposure for patients and staff. Dr. Batchelor is one of four cardiologists who shared their experiences and advice on common cardiac procedures across three locales: TAVR in Virginia, percutaneous coronary intervention (PCI) in New York City, and atrial fibrillation (AFib) ablation in Kentucky.
More on TAVR in Virginia
Inova’s framework for triaging structural heart disease interventions (largely TAVR and/or percutaneous mitral valve repair) comprised three tiers. Tier 1 captured “emergent cases that had to be done, no questions asked,” Dr. Batchelor said. For TAVR, these were inpatients with severe to critical symptomatic aortic stenosis and advanced congestive heart failure who could not safely be discharged, as well as other patients “with refractory symptoms of heart failure that were compelling.” Many had associated left ventricular systolic dysfunction.
Those who could delay 14-30 days were placed in tier 2, and patients who “we felt were fairly stable and could wait at least 30 days” were placed in tier 3. “For TAVR, a tier 3 patient might be the one … who has severe aortic stenosis but is walking around and doing well at home with only stable exertional symptoms,” he said.
Patients whose procedures were delayed were contacted weekly by the valve clinic’s advanced practice practitioners through video visits or telephone calls, and tier categorization was reevaluated if symptoms worsened. “We had to keep in close contact with them,” Dr. Batchelor said. “These patients can deteriorate quite rapidly and sometimes without much warning.”
Virtual video visits were often used for 30-day postprocedural follow-ups, taking the place of in-person visits during which post-TAVR echocardiographic assessments would normally be performed. “For follow-up, we’d often just do a quick visit to check the vascular access site within 7-10 days, and then, if they were doing okay we’d delay the 30-day echo to a later time frame,” he said.
Preprocedural testing was streamlined to minimize the number of patient-provider interactions, with pulmonary function testing and pre-TAVR catheterization omitted unless absolutely necessary. “A TAVR CT angiogram [performed within the prior year] is the only test you really absolutely need,” Dr. Batchelor said. “We were much less likely to order a heart catheterization unless the patient was having angina and high risk or suspicion for significant coronary artery disease.”
This approach was not associated with any compromise in postprocedural outcomes, he noted. Prior to the pandemic, Inova routinely employed a minimalist approach to TAVR with moderate conscious sedation and avoiding transesophageal echocardiography – steps that were recommended for structural heart procedures in the COVID-19 era in a published review by the heart team at New York-Presbyterian Hospital/Columbia University Irving Medical Center.
The New York review is useful for cardiologists in areas with rising case burdens of COVID-19, Dr. Batchelor said, as is a position statement he coauthored from the American College of Cardiology and the Society for Cardiology and Angiography Interventions (SCAI) on triage considerations for structural heart disease interventions during the pandemic.
TAVR’s resource-heavy nature made the “system capacity dashboard” and daily meetings critical, Dr. Batchelor explained. At one point during the hold on elective procedures, the Falls Church INOVA facility had approximately 300 patients with COVID-19, a significant proportion of whom were in cardiac ICU beds.
“Everyone has to be flexible and learn,” he said. “We trained our cardiologists on managing ventilators in case some of the [critical care] staff got ill or were overwhelmed by the surge.”
More than 2 months after the surge eased and the ban on elective surgery was lifted, Dr. Batchelor and his colleagues are still using the dashboard and continue to meet daily to discuss COVID-19 prevalence in the hospital and the community as they work through the backlog of delayed procedures. They also routinely review the status of COVID-19 testing for inpatients and outpatients and the donning and doffing of personal protective equipment.
“You have to communicate early and often across the whole system of care because you’re competing for the same resources,” he advised. “And you have to be flexible and reassess. A policy that works at the beginning of the pandemic might have to change.”
PCI in New York
Before the pandemic, the cardiac catheterization laboratory at Mount Sinai Morningside Hospital in New York handled a monthly average of 140-150 PCIs, including 6-10 primary PCIs for ST-segment elevation myocardial infarction.
When electives were halted by the hospital in March and the City became the global epicenter for COVID-19, the cath lab went quiet. “Even though we were still able to do urgent cases or emergent cases, the case volume dropped tremendously,” said Jacqueline E. Tamis-Holland, MD, associate director of the cardiac catheterization laboratory and director of the interventional cardiology fellowship. “There weren’t many outpatients in our hospital … and by late March and through April, there wasn’t a single acute infarction.”
She and Tak W. Kwan, MD, director of the cardiac catheterization laboratory and professor of medicine at Icahn School of Medicine at Mount Sinai, New York, were prepared to move true STEMI patients into the cath lab for primary PCI without delay unless the staff or system were overrun.
That primary PCI should remain the first-line treatment for STEMI even in cases of confirmed or suspected COVID-19 was recommended by SCAI guidance issued in March and by a consensus statement released by the SCAI, ACC, and American College of Emergency Physicians in April – and “we were very much of the same frame of mind,” Dr. Tamis-Holland said.
Deciding which elective cases could not be delayed required a completely individualized approach, the cardiologists emphasized. Dr. Tamis-Holland had a few patients scheduled for elective PCI when the hold began, and “we spoke every few days or once a week in the beginning, then transitioned to once every 2 weeks,” she said. “With medical therapy and given that they were relatively sedentary, my patients did okay [with the delays].”
For subsequent patients, she considered their symptoms or stress test results. “If it’s someone who I’d [normally] wait until next week to schedule the cath, then we would wait 2 or 3 more weeks, or a month more with careful monitoring,” she said. “Certainly, there was a decrease in the number of abnormal stress tests that I referred to the cath lab during [the surge period].”
Dr. Kwan described one patient who had new-onset congestive heart failure in late March “with a markedly positive nuclear stress test.” The patient was monitored with twice-weekly telemedicine visits and office visits, and a cardiac catheterization was performed in early May as an urgent elective case. “He had severe three-vessel and left main disease,” he said. “Subsequently, [coronary artery bypass surgery] was done.”
There were no changes in the PCI procedure itself in terms of hospital stay (most elective cases at Mt. Sinai are same-day procedures) or in staffing, other than a ban on visiting students or residents. The most important changes during the surge – in addition to stocking enough personal protective equipment – concerned testing. Patients undergoing elective PCI are tested for the novel coronavirus 72 hours before the procedure, and rapid testing is performed in the emergency room for STEMI patients to determine patient disposition after the procedure.
“Until we have the results back we should treat all patients as if they are a patient under investigation or have COVID,” said Dr. Tamis-Holland, who helped develop emergency guidance on STEMI systems of care during the pandemic for the American Heart Association.
In early May, the hospital freed up additional space for cardiac care, allowing more “urgent-elective” PCIs to be done. Some patients were reluctant to proceed, the cardiologists said, because of a no-visitor policy. In mid-June, the hold on elective procedures was lifted, and around the same time, the hospital shifted to a one-visitor policy. Still, some patients opted to continue longer with medical therapy.
Patients need to feel comfortable, and “there is a lag time from the time everything opens up and when patients get their stress tests and their evaluations, and then arrive for PCI,” said Dr. Tamis-Holland.
By mid-July, the cardiologists were anticipating an increase in complications from infarctions among patients who “waited them out at home” – heart failure or mitral valve regurgitation, for instance – but, in their hospital at least, “we haven’t really seen that,” she added.
AFib ablation in Kentucky
As New York experienced its surge, John Mandrola, MD, and other electrophysiologists across the Baptist Health system in Kentucky reached a consensus on how to categorize their procedures. Electrophysiology interventions were classified urgent, emergent, and truly elective in the event that the state’s relatively low case burden of COVID-19 were to significantly worsen.
There was no doubt where AFib ablation sat. “It’s one of the most elective procedures there is” in terms of scheduling under normal circumstances, and it almost always requires an overnight stay and general anesthesia – factors that upped the ante on an elective classification, said Dr. Mandrola.
All AF ablations were deemed elective unless the patient required immediate hospitalization. For 8-10 weeks during the state’s shutdown of elective care, Dr. Mandrola and his partner successfully monitored patients with phone calls. “To be honest,” he said, “most patients did not want to have their AFib ablation anyway until the pandemic slowed and they knew it was safe.”
In some cases, patients reported that their symptoms were improving: “There are so many things to speculate about. ... Was it that everyone took their foot off the accelerator?” Dr. Mandrola thinks that postpandemic outcomes analyses may drive more scrutiny of the necessity of some AFib ablations and other procedures and tests. AFib ablation “has its place but is probably overused,” he said.
During the pause on electives, “the vast majority of procedures we did were pacemaker procedures,” he said. “We also did some atrial flutter ablations, and ablations for ventricular tachycardia and supraventricular tachycardia.” In mid-July, as the COVID-19 case burden in Kentucky remained relatively low, Dr. Mandrola was “up to 120%” of his pre-COVID electrophysiology volume – but ready to scale back again if needed.
Dr. Batchelor reported consulting fees from Boston Scientific, Abbott Medical, Medtronic, and V-wave. Dr. Kwan, Dr. Mandrola, and Dr. Tamis-Holland reported no relevant financial disclosures.
This article is a collaboration between Medscape and MDedge. A version of it originally appeared on Medscape.com.
When Virginia’s governor directed the postponement of all elective surgeries in late March, Wayne Batchelor, MD and his colleagues at the Inova Heart and Vascular Institute in Falls Church, Va., canceled about two-thirds of their transcatheter aortic valve replacement (TAVR) procedures.
They then categorized patients by tiers to gauge which procedures could safely be postponed and to guide triaging. And while they did not deviate from the practice of having both an interventional cardiologist and a cardiothoracic surgeon present for TAVR, they slimmed down preprocedural testing when feasible and delayed some 30-day post-TAVR echocardiographic assessments. “It was a delicate dance, very difficult dance. But luckily, we were able to navigate the challenges effectively,” said Dr. Batchelor, the institute’s director of interventional cardiology and interventional cardiology research.
A “system capacity dashboard” that merged bed and staffing data from interventional cardiology spaces with cardiovascular and noncardiovascular ICU beds, operating rooms, and other resources – and daily cross-department meetings – enabled them to proceed with the most urgent TAVR procedures while “keeping a buffer of ICU beds to accommodate an anticipated surge of COVID-19,” he explained.
Such adaptations in cardiac procedures and processes are occurring in hospitals across the country as efforts are made to minimize the risk of COVID-19 exposure for patients and staff. Dr. Batchelor is one of four cardiologists who shared their experiences and advice on common cardiac procedures across three locales: TAVR in Virginia, percutaneous coronary intervention (PCI) in New York City, and atrial fibrillation (AFib) ablation in Kentucky.
More on TAVR in Virginia
Inova’s framework for triaging structural heart disease interventions (largely TAVR and/or percutaneous mitral valve repair) comprised three tiers. Tier 1 captured “emergent cases that had to be done, no questions asked,” Dr. Batchelor said. For TAVR, these were inpatients with severe to critical symptomatic aortic stenosis and advanced congestive heart failure who could not safely be discharged, as well as other patients “with refractory symptoms of heart failure that were compelling.” Many had associated left ventricular systolic dysfunction.
Those who could delay 14-30 days were placed in tier 2, and patients who “we felt were fairly stable and could wait at least 30 days” were placed in tier 3. “For TAVR, a tier 3 patient might be the one … who has severe aortic stenosis but is walking around and doing well at home with only stable exertional symptoms,” he said.
Patients whose procedures were delayed were contacted weekly by the valve clinic’s advanced practice practitioners through video visits or telephone calls, and tier categorization was reevaluated if symptoms worsened. “We had to keep in close contact with them,” Dr. Batchelor said. “These patients can deteriorate quite rapidly and sometimes without much warning.”
Virtual video visits were often used for 30-day postprocedural follow-ups, taking the place of in-person visits during which post-TAVR echocardiographic assessments would normally be performed. “For follow-up, we’d often just do a quick visit to check the vascular access site within 7-10 days, and then, if they were doing okay we’d delay the 30-day echo to a later time frame,” he said.
Preprocedural testing was streamlined to minimize the number of patient-provider interactions, with pulmonary function testing and pre-TAVR catheterization omitted unless absolutely necessary. “A TAVR CT angiogram [performed within the prior year] is the only test you really absolutely need,” Dr. Batchelor said. “We were much less likely to order a heart catheterization unless the patient was having angina and high risk or suspicion for significant coronary artery disease.”
This approach was not associated with any compromise in postprocedural outcomes, he noted. Prior to the pandemic, Inova routinely employed a minimalist approach to TAVR with moderate conscious sedation and avoiding transesophageal echocardiography – steps that were recommended for structural heart procedures in the COVID-19 era in a published review by the heart team at New York-Presbyterian Hospital/Columbia University Irving Medical Center.
The New York review is useful for cardiologists in areas with rising case burdens of COVID-19, Dr. Batchelor said, as is a position statement he coauthored from the American College of Cardiology and the Society for Cardiology and Angiography Interventions (SCAI) on triage considerations for structural heart disease interventions during the pandemic.
TAVR’s resource-heavy nature made the “system capacity dashboard” and daily meetings critical, Dr. Batchelor explained. At one point during the hold on elective procedures, the Falls Church INOVA facility had approximately 300 patients with COVID-19, a significant proportion of whom were in cardiac ICU beds.
“Everyone has to be flexible and learn,” he said. “We trained our cardiologists on managing ventilators in case some of the [critical care] staff got ill or were overwhelmed by the surge.”
More than 2 months after the surge eased and the ban on elective surgery was lifted, Dr. Batchelor and his colleagues are still using the dashboard and continue to meet daily to discuss COVID-19 prevalence in the hospital and the community as they work through the backlog of delayed procedures. They also routinely review the status of COVID-19 testing for inpatients and outpatients and the donning and doffing of personal protective equipment.
“You have to communicate early and often across the whole system of care because you’re competing for the same resources,” he advised. “And you have to be flexible and reassess. A policy that works at the beginning of the pandemic might have to change.”
PCI in New York
Before the pandemic, the cardiac catheterization laboratory at Mount Sinai Morningside Hospital in New York handled a monthly average of 140-150 PCIs, including 6-10 primary PCIs for ST-segment elevation myocardial infarction.
When electives were halted by the hospital in March and the City became the global epicenter for COVID-19, the cath lab went quiet. “Even though we were still able to do urgent cases or emergent cases, the case volume dropped tremendously,” said Jacqueline E. Tamis-Holland, MD, associate director of the cardiac catheterization laboratory and director of the interventional cardiology fellowship. “There weren’t many outpatients in our hospital … and by late March and through April, there wasn’t a single acute infarction.”
She and Tak W. Kwan, MD, director of the cardiac catheterization laboratory and professor of medicine at Icahn School of Medicine at Mount Sinai, New York, were prepared to move true STEMI patients into the cath lab for primary PCI without delay unless the staff or system were overrun.
That primary PCI should remain the first-line treatment for STEMI even in cases of confirmed or suspected COVID-19 was recommended by SCAI guidance issued in March and by a consensus statement released by the SCAI, ACC, and American College of Emergency Physicians in April – and “we were very much of the same frame of mind,” Dr. Tamis-Holland said.
Deciding which elective cases could not be delayed required a completely individualized approach, the cardiologists emphasized. Dr. Tamis-Holland had a few patients scheduled for elective PCI when the hold began, and “we spoke every few days or once a week in the beginning, then transitioned to once every 2 weeks,” she said. “With medical therapy and given that they were relatively sedentary, my patients did okay [with the delays].”
For subsequent patients, she considered their symptoms or stress test results. “If it’s someone who I’d [normally] wait until next week to schedule the cath, then we would wait 2 or 3 more weeks, or a month more with careful monitoring,” she said. “Certainly, there was a decrease in the number of abnormal stress tests that I referred to the cath lab during [the surge period].”
Dr. Kwan described one patient who had new-onset congestive heart failure in late March “with a markedly positive nuclear stress test.” The patient was monitored with twice-weekly telemedicine visits and office visits, and a cardiac catheterization was performed in early May as an urgent elective case. “He had severe three-vessel and left main disease,” he said. “Subsequently, [coronary artery bypass surgery] was done.”
There were no changes in the PCI procedure itself in terms of hospital stay (most elective cases at Mt. Sinai are same-day procedures) or in staffing, other than a ban on visiting students or residents. The most important changes during the surge – in addition to stocking enough personal protective equipment – concerned testing. Patients undergoing elective PCI are tested for the novel coronavirus 72 hours before the procedure, and rapid testing is performed in the emergency room for STEMI patients to determine patient disposition after the procedure.
“Until we have the results back we should treat all patients as if they are a patient under investigation or have COVID,” said Dr. Tamis-Holland, who helped develop emergency guidance on STEMI systems of care during the pandemic for the American Heart Association.
In early May, the hospital freed up additional space for cardiac care, allowing more “urgent-elective” PCIs to be done. Some patients were reluctant to proceed, the cardiologists said, because of a no-visitor policy. In mid-June, the hold on elective procedures was lifted, and around the same time, the hospital shifted to a one-visitor policy. Still, some patients opted to continue longer with medical therapy.
Patients need to feel comfortable, and “there is a lag time from the time everything opens up and when patients get their stress tests and their evaluations, and then arrive for PCI,” said Dr. Tamis-Holland.
By mid-July, the cardiologists were anticipating an increase in complications from infarctions among patients who “waited them out at home” – heart failure or mitral valve regurgitation, for instance – but, in their hospital at least, “we haven’t really seen that,” she added.
AFib ablation in Kentucky
As New York experienced its surge, John Mandrola, MD, and other electrophysiologists across the Baptist Health system in Kentucky reached a consensus on how to categorize their procedures. Electrophysiology interventions were classified urgent, emergent, and truly elective in the event that the state’s relatively low case burden of COVID-19 were to significantly worsen.
There was no doubt where AFib ablation sat. “It’s one of the most elective procedures there is” in terms of scheduling under normal circumstances, and it almost always requires an overnight stay and general anesthesia – factors that upped the ante on an elective classification, said Dr. Mandrola.
All AF ablations were deemed elective unless the patient required immediate hospitalization. For 8-10 weeks during the state’s shutdown of elective care, Dr. Mandrola and his partner successfully monitored patients with phone calls. “To be honest,” he said, “most patients did not want to have their AFib ablation anyway until the pandemic slowed and they knew it was safe.”
In some cases, patients reported that their symptoms were improving: “There are so many things to speculate about. ... Was it that everyone took their foot off the accelerator?” Dr. Mandrola thinks that postpandemic outcomes analyses may drive more scrutiny of the necessity of some AFib ablations and other procedures and tests. AFib ablation “has its place but is probably overused,” he said.
During the pause on electives, “the vast majority of procedures we did were pacemaker procedures,” he said. “We also did some atrial flutter ablations, and ablations for ventricular tachycardia and supraventricular tachycardia.” In mid-July, as the COVID-19 case burden in Kentucky remained relatively low, Dr. Mandrola was “up to 120%” of his pre-COVID electrophysiology volume – but ready to scale back again if needed.
Dr. Batchelor reported consulting fees from Boston Scientific, Abbott Medical, Medtronic, and V-wave. Dr. Kwan, Dr. Mandrola, and Dr. Tamis-Holland reported no relevant financial disclosures.
This article is a collaboration between Medscape and MDedge. A version of it originally appeared on Medscape.com.
When Virginia’s governor directed the postponement of all elective surgeries in late March, Wayne Batchelor, MD and his colleagues at the Inova Heart and Vascular Institute in Falls Church, Va., canceled about two-thirds of their transcatheter aortic valve replacement (TAVR) procedures.
They then categorized patients by tiers to gauge which procedures could safely be postponed and to guide triaging. And while they did not deviate from the practice of having both an interventional cardiologist and a cardiothoracic surgeon present for TAVR, they slimmed down preprocedural testing when feasible and delayed some 30-day post-TAVR echocardiographic assessments. “It was a delicate dance, very difficult dance. But luckily, we were able to navigate the challenges effectively,” said Dr. Batchelor, the institute’s director of interventional cardiology and interventional cardiology research.
A “system capacity dashboard” that merged bed and staffing data from interventional cardiology spaces with cardiovascular and noncardiovascular ICU beds, operating rooms, and other resources – and daily cross-department meetings – enabled them to proceed with the most urgent TAVR procedures while “keeping a buffer of ICU beds to accommodate an anticipated surge of COVID-19,” he explained.
Such adaptations in cardiac procedures and processes are occurring in hospitals across the country as efforts are made to minimize the risk of COVID-19 exposure for patients and staff. Dr. Batchelor is one of four cardiologists who shared their experiences and advice on common cardiac procedures across three locales: TAVR in Virginia, percutaneous coronary intervention (PCI) in New York City, and atrial fibrillation (AFib) ablation in Kentucky.
More on TAVR in Virginia
Inova’s framework for triaging structural heart disease interventions (largely TAVR and/or percutaneous mitral valve repair) comprised three tiers. Tier 1 captured “emergent cases that had to be done, no questions asked,” Dr. Batchelor said. For TAVR, these were inpatients with severe to critical symptomatic aortic stenosis and advanced congestive heart failure who could not safely be discharged, as well as other patients “with refractory symptoms of heart failure that were compelling.” Many had associated left ventricular systolic dysfunction.
Those who could delay 14-30 days were placed in tier 2, and patients who “we felt were fairly stable and could wait at least 30 days” were placed in tier 3. “For TAVR, a tier 3 patient might be the one … who has severe aortic stenosis but is walking around and doing well at home with only stable exertional symptoms,” he said.
Patients whose procedures were delayed were contacted weekly by the valve clinic’s advanced practice practitioners through video visits or telephone calls, and tier categorization was reevaluated if symptoms worsened. “We had to keep in close contact with them,” Dr. Batchelor said. “These patients can deteriorate quite rapidly and sometimes without much warning.”
Virtual video visits were often used for 30-day postprocedural follow-ups, taking the place of in-person visits during which post-TAVR echocardiographic assessments would normally be performed. “For follow-up, we’d often just do a quick visit to check the vascular access site within 7-10 days, and then, if they were doing okay we’d delay the 30-day echo to a later time frame,” he said.
Preprocedural testing was streamlined to minimize the number of patient-provider interactions, with pulmonary function testing and pre-TAVR catheterization omitted unless absolutely necessary. “A TAVR CT angiogram [performed within the prior year] is the only test you really absolutely need,” Dr. Batchelor said. “We were much less likely to order a heart catheterization unless the patient was having angina and high risk or suspicion for significant coronary artery disease.”
This approach was not associated with any compromise in postprocedural outcomes, he noted. Prior to the pandemic, Inova routinely employed a minimalist approach to TAVR with moderate conscious sedation and avoiding transesophageal echocardiography – steps that were recommended for structural heart procedures in the COVID-19 era in a published review by the heart team at New York-Presbyterian Hospital/Columbia University Irving Medical Center.
The New York review is useful for cardiologists in areas with rising case burdens of COVID-19, Dr. Batchelor said, as is a position statement he coauthored from the American College of Cardiology and the Society for Cardiology and Angiography Interventions (SCAI) on triage considerations for structural heart disease interventions during the pandemic.
TAVR’s resource-heavy nature made the “system capacity dashboard” and daily meetings critical, Dr. Batchelor explained. At one point during the hold on elective procedures, the Falls Church INOVA facility had approximately 300 patients with COVID-19, a significant proportion of whom were in cardiac ICU beds.
“Everyone has to be flexible and learn,” he said. “We trained our cardiologists on managing ventilators in case some of the [critical care] staff got ill or were overwhelmed by the surge.”
More than 2 months after the surge eased and the ban on elective surgery was lifted, Dr. Batchelor and his colleagues are still using the dashboard and continue to meet daily to discuss COVID-19 prevalence in the hospital and the community as they work through the backlog of delayed procedures. They also routinely review the status of COVID-19 testing for inpatients and outpatients and the donning and doffing of personal protective equipment.
“You have to communicate early and often across the whole system of care because you’re competing for the same resources,” he advised. “And you have to be flexible and reassess. A policy that works at the beginning of the pandemic might have to change.”
PCI in New York
Before the pandemic, the cardiac catheterization laboratory at Mount Sinai Morningside Hospital in New York handled a monthly average of 140-150 PCIs, including 6-10 primary PCIs for ST-segment elevation myocardial infarction.
When electives were halted by the hospital in March and the City became the global epicenter for COVID-19, the cath lab went quiet. “Even though we were still able to do urgent cases or emergent cases, the case volume dropped tremendously,” said Jacqueline E. Tamis-Holland, MD, associate director of the cardiac catheterization laboratory and director of the interventional cardiology fellowship. “There weren’t many outpatients in our hospital … and by late March and through April, there wasn’t a single acute infarction.”
She and Tak W. Kwan, MD, director of the cardiac catheterization laboratory and professor of medicine at Icahn School of Medicine at Mount Sinai, New York, were prepared to move true STEMI patients into the cath lab for primary PCI without delay unless the staff or system were overrun.
That primary PCI should remain the first-line treatment for STEMI even in cases of confirmed or suspected COVID-19 was recommended by SCAI guidance issued in March and by a consensus statement released by the SCAI, ACC, and American College of Emergency Physicians in April – and “we were very much of the same frame of mind,” Dr. Tamis-Holland said.
Deciding which elective cases could not be delayed required a completely individualized approach, the cardiologists emphasized. Dr. Tamis-Holland had a few patients scheduled for elective PCI when the hold began, and “we spoke every few days or once a week in the beginning, then transitioned to once every 2 weeks,” she said. “With medical therapy and given that they were relatively sedentary, my patients did okay [with the delays].”
For subsequent patients, she considered their symptoms or stress test results. “If it’s someone who I’d [normally] wait until next week to schedule the cath, then we would wait 2 or 3 more weeks, or a month more with careful monitoring,” she said. “Certainly, there was a decrease in the number of abnormal stress tests that I referred to the cath lab during [the surge period].”
Dr. Kwan described one patient who had new-onset congestive heart failure in late March “with a markedly positive nuclear stress test.” The patient was monitored with twice-weekly telemedicine visits and office visits, and a cardiac catheterization was performed in early May as an urgent elective case. “He had severe three-vessel and left main disease,” he said. “Subsequently, [coronary artery bypass surgery] was done.”
There were no changes in the PCI procedure itself in terms of hospital stay (most elective cases at Mt. Sinai are same-day procedures) or in staffing, other than a ban on visiting students or residents. The most important changes during the surge – in addition to stocking enough personal protective equipment – concerned testing. Patients undergoing elective PCI are tested for the novel coronavirus 72 hours before the procedure, and rapid testing is performed in the emergency room for STEMI patients to determine patient disposition after the procedure.
“Until we have the results back we should treat all patients as if they are a patient under investigation or have COVID,” said Dr. Tamis-Holland, who helped develop emergency guidance on STEMI systems of care during the pandemic for the American Heart Association.
In early May, the hospital freed up additional space for cardiac care, allowing more “urgent-elective” PCIs to be done. Some patients were reluctant to proceed, the cardiologists said, because of a no-visitor policy. In mid-June, the hold on elective procedures was lifted, and around the same time, the hospital shifted to a one-visitor policy. Still, some patients opted to continue longer with medical therapy.
Patients need to feel comfortable, and “there is a lag time from the time everything opens up and when patients get their stress tests and their evaluations, and then arrive for PCI,” said Dr. Tamis-Holland.
By mid-July, the cardiologists were anticipating an increase in complications from infarctions among patients who “waited them out at home” – heart failure or mitral valve regurgitation, for instance – but, in their hospital at least, “we haven’t really seen that,” she added.
AFib ablation in Kentucky
As New York experienced its surge, John Mandrola, MD, and other electrophysiologists across the Baptist Health system in Kentucky reached a consensus on how to categorize their procedures. Electrophysiology interventions were classified urgent, emergent, and truly elective in the event that the state’s relatively low case burden of COVID-19 were to significantly worsen.
There was no doubt where AFib ablation sat. “It’s one of the most elective procedures there is” in terms of scheduling under normal circumstances, and it almost always requires an overnight stay and general anesthesia – factors that upped the ante on an elective classification, said Dr. Mandrola.
All AF ablations were deemed elective unless the patient required immediate hospitalization. For 8-10 weeks during the state’s shutdown of elective care, Dr. Mandrola and his partner successfully monitored patients with phone calls. “To be honest,” he said, “most patients did not want to have their AFib ablation anyway until the pandemic slowed and they knew it was safe.”
In some cases, patients reported that their symptoms were improving: “There are so many things to speculate about. ... Was it that everyone took their foot off the accelerator?” Dr. Mandrola thinks that postpandemic outcomes analyses may drive more scrutiny of the necessity of some AFib ablations and other procedures and tests. AFib ablation “has its place but is probably overused,” he said.
During the pause on electives, “the vast majority of procedures we did were pacemaker procedures,” he said. “We also did some atrial flutter ablations, and ablations for ventricular tachycardia and supraventricular tachycardia.” In mid-July, as the COVID-19 case burden in Kentucky remained relatively low, Dr. Mandrola was “up to 120%” of his pre-COVID electrophysiology volume – but ready to scale back again if needed.
Dr. Batchelor reported consulting fees from Boston Scientific, Abbott Medical, Medtronic, and V-wave. Dr. Kwan, Dr. Mandrola, and Dr. Tamis-Holland reported no relevant financial disclosures.
This article is a collaboration between Medscape and MDedge. A version of it originally appeared on Medscape.com.
Marked improvements seen for women in dermatology since the 1970s
Wilma F. Bergfeld, MD, one of only five women in her medical school class of 1964 and the third female in her dermatology residency program, had recently been appointed as a junior clinical dermatologist and head of dermatopathology at the Cleveland Clinic when she was told by a superior that she would not be promoted or invited to serve on any committee or decision-making group.
“I was told I should go home at night and take care of my husband and two children,” she recalled of that moment in the 1970s. The comment made her feel “outraged,” and it drove her, calmly and steadily, to work harder and to “challenge the system.”
Dr. Bergfeld not only was elected to the Cleveland Clinic’s board of governors and board of trustees and served as president of the Clinic’s staff in 1990, she also became the first woman president of the American Academy of Dermatology (1992) and led numerous other dermatologic organizations. Much earlier on, in 1973, to help fulfill her vision of “women helping women,” she had also founded the Women’s Dermatologic Society (WDS). Three years earlier, in 1970, 6.9% of the approximately 4,000 dermatologists in the United States were women, according to the American Medical Association.
Today, when she goes to work as the long-time director of the Clinic’s dermatopathology fellowship and professor of dermatology and pathology at the Cleveland Clinic Educational Foundation, she sees a transformed staff and, more broadly, a national physician workforce in which women made up almost 50% of active dermatologists in 2017 and almost 60% of dermatology residents in 2018, according to data from the American Association of Medical Colleges.
It’s a different and better world, she and other women dermatologists said, but one in which women must continue to mentor other women and continue to challenge the system. Achieving work-life balance, fairer compensation, and a greater proportion of women in the higher ranks of academia are all on their work list.
Women’s impact on the specialty
Dr. Bergfeld and Molly Hinshaw, MD, the current president of the WDS, said they believe women are drawn to dermatology for its visual nature, the growth in diagnostic tests and therapies, and the opportunity to diagnose early and prevent progression of disease in patients of all ages. “It’s a small but mighty specialty,” said Dr. Hinshaw, associate professor of dermatology and section chief of dermatopathology at the University of Wisconsin–Madison.
It’s also a versatile specialty with a variety of subspecialties and niches to pursue – and women have been stepping in to fill unmet needs, Dr. Hinshaw said. “Women dermatologists are directing vulvar specialty clinics across the country, for example. There aren’t that many, but they’re filling an important niche. We have one at [our university] and it is packed.”
Women have also been drawn to the in-demand subspecialty of pediatric dermatology, she noted. They now make up more than two-thirds of all pediatric dermatologists, and many in practice have trained the old-fashioned way, completing two residencies. “That’s [involved] self-selection into an additional year of years training and a commitment to caring for special populations that, quite honestly, takes more time,” said Dr. Hinshaw, who, as part of her dermatology practice, runs a nail clinic at UW Health in Madison.
Amy S. Paller, MD, who chairs the department of dermatology at Northwestern University, Chicago, where she is professor of dermatology and pediatrics and directs the Skin Biology & Diseases Resource-Based Center, is one of these women. She took a long and determined journey into the subspecialty, encountering bias and discouragement while actively seeking out mentors who helped her advance.
While in medical school at Stanford (Calif.) University in the late 1970s in a class “very progressively” made up of about one-third women, Dr. Paller met Alvin Jacobs, MD, who, in 1975, had founded the Society for Pediatric Dermatology. “There wasn’t much pediatric dermatology in the world at the time, and it was Al who helped [me realize] that it combined my love of genetic research with my [desire] to work with children,” she recalled.
Per Dr. Jacob’s advice, she went to Northwestern to train in both pediatrics and dermatology under Nancy Esterly, MD, who “is considered by many to be the mother of pediatric dermatology.” And knowing that she wanted to do research, Dr. Paller also worked with Ruth Freinkel, MD, who “was the strongest bench researcher” at Northwestern. (Dr. Freinkel had been one of the first female dermatology residents at Harvard and was the first full-time faculty member in dermatology at Northwestern).
After completing postdoctoral research at the University of North Carolina at Chapel Hill, Dr. Paller returned to Chicago and assumed Dr. Esterly’s position as chief of dermatology at the Children’s National Hospital of Chicago. It was there that “someone in a leadership position questioned me about how I could possibly be a scientist, a strong clinician, and a good mother to my three children – and suggested that I drop research,” Dr. Paller recalled.
“I think this person was trying to be helpful to me, but I was shocked,” she said. Just as Dr. Bergfeld had done, Dr. Paller channeled her frustration into new pursuits.
“It made me go home and think, how could I strengthen myself? What else could I do?” she said. “Soon after, with a highly supportive husband, I did a ‘pseudosabbatical,’ basically spending every ounce of spare time I had working with one of the premier female scientists in the country, Elaine Fuchs, and learning molecular biology” in her lab at the University of Chicago.
“I think we’ve all had discrimination along the way. Sometimes there’s implicit bias and sometimes there’s overt bias,” said Dr. Paller, who in 2004 led the society which her mentor Dr. Jacobs had founded several decades earlier. “I just jumped right in, and that’s enabled me to find good role models.”
Across dermatology broadly, the often holistic nature of the specialty – of the ability to peer into the body and its internal health – is another quality that women have been drawn to and advanced, Dr. Hinshaw said. “One of the reasons why I chose dermatology is because it’s a window to total patient health. Patients often see their dermatologists as physicians who help them identify next steps in their health care, who can help them address issues related to their overall health and well-being, including their mental health.”
In a WDS membership survey conducted in 2018, most respondents reported that they frequently or occasionally detect and diagnose systemic/internal diseases and conditions in their female patients, and that they consult and collaborate with different kinds of physicians (Int J Womens Dermatol. 2018 Nov 15;4[4]:189-92).
And in a March 2019 “Dialogues in Dermatology” podcast episode on the history and advancement of women in dermatology produced by the American Academy of Dermatology, Pearl Grimes, MD, a clinical professor of dermatology of the University of California, Los Angeles, and then-president of the WDS, described why “total women’s health” had become an additional focus for the society.
“We’re already gatekeepers” in many respects, Dr. Grimes said. “In addition to my addressing specific skin issues, my patients query me on hormone issues, on nutrition, on stress-related issues….and on [what other physicians they should see].”
Phoebe Rich, MD, who owns a small all-woman practice and a research center in Portland, Oregon, said that, in general, many women also communicate and practice in a way that facilitates holistic care. “These qualities aren’t exclusive to women, but women are very caring. We take time and are interested in [patients’] lives in general, not just their disease.”
Disparities in academia
Dermatology departments in academic medicine have burgeoned in size in the past 50 years, and women are well represented overall. In 2018, women comprised 51.2% of dermatology department faculty – up from 10.8% in 1970 – a current proportion that ranks fifth among specialties for the proportion of female faculty, according to a cross-sectional study of faculty diversity trends using data from the AAMC faculty roster (JAMA Dermatol. 2020 Jan 8;156[3]:280-7).
The AAMC data show the share of women dermatology faculty declining at each subsequent rank, however – a finding that suggests that women are not promoted as quickly or to the same levels of leadership as men, the report’s authors noted. (Dermatology isn’t alone: The AAMC issued a call to action on gender equity in medicine this year, citing this inverse association.)
Another recently published study of gender trends in academic dermatology – this one looking at a smaller sample of data from 15 institutions – similarly found that women dermatologists made up a majority of faculty (53.6%) and were well represented as assistant professors (60.7%) but underrepresented as full professors (17%).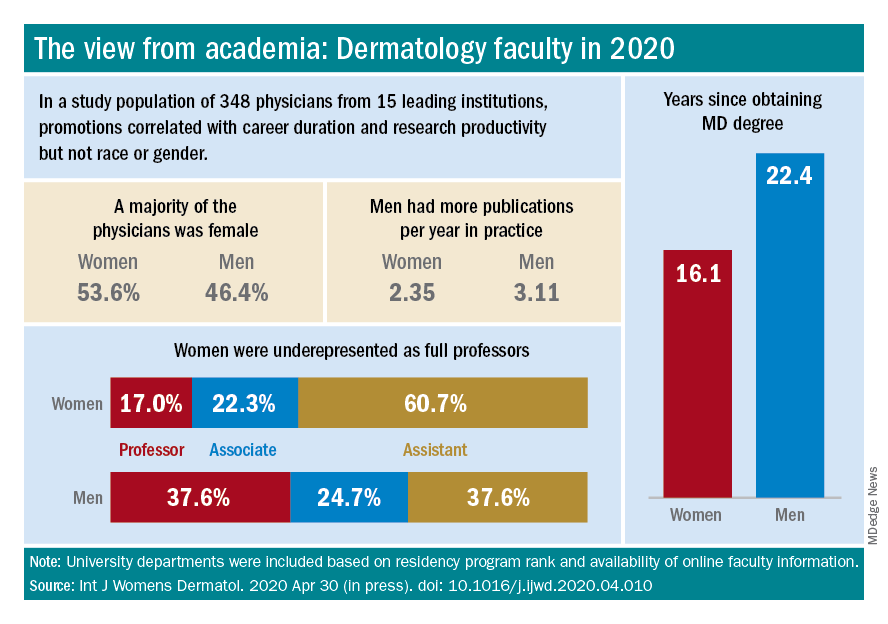
This study differed from the larger AAMC study, however, in that it controlled for “achievement indicators” – career duration, publications per year, and National Institutes of Health research funding – and found that gender alone was not associated with higher rank. Instead, promotions were correlated most significantly with NIH research funding and also with career duration and publications per year.
“If research achievement is to be used as a benchmark for academic promotion, increased efforts are needed to support the research activities of women,” the authors wrote, adding that recognition should be given to other factors as well.
Dr. Paller and Dr. Hinshaw both described the situation as complex and multifaceted. Some research on promotion in academia in general – but not all – has suggested that women do need to publish more than men in order to be promoted. But “the promotion process also has within it the ability to use judgment [about] the impact and merits of work,” said Dr. Hinshaw. “Not all publications [and levels of authorship] may be considered equal, for instance.”
Dr. Hinshaw said she is also concerned by data showing that women still perform the majority of household duties, “even in households in which both partners work outside the home equivalently.” As long as this is the case, women may be “inherently disadvantaged” in their ability to have adequate research time and to advance.
From where she sits, Dr. Paller sees several factors at play: “The pipeline, achievement during the pipeline, and decision-making about advancement” on the part of women themselves. Having served on search committees for top leadership in specialties in which women are well represented, she said, “I’ve seen fewer women who’ve come forward and been interested in rising into a chair or a dean position.”
And “having talked to so many women,” Dr. Paller added, “I think there’s a phenomenon where it’s harder for women to accept positions [that require] a significant change.”
Women “are nurturers, which makes them extremely good [leaders] and chairs, but it also makes it harder to make life changes that affect the people they love,” she said, noting that becoming a department chair or a dean often involves moving. “I also think that women in general are happier and committed to what they’re [currently] doing.”
Dr. Paller is optimistic that, with the support of department chairs and continued attention to role modeling and mentoring, the portrait of women in academic dermatology will continue to improve. Currently, 34 chairs of dermatology departments are female, she noted. “That number was 11 less 15 years ago.”
In the meantime, researchers are increasingly documenting trends in women’s editorships of journals as well as leadership and speaking opportunities at professional conferences.
The authors of one study published this year, for instance, reviewed the editorial boards of dermatology journals and found that women occupied 18% of editor in chief roles, 36% of deputy editor positions, and 22% of overall editorial board roles (Int J Womens Dermatol. 2019 Sep 12;6[1]:20-4). Other research shows women comprising 43% of all authorships across 23 dermatologic journals from 2008 to May 2017, 50.2% of first authorships, and 33.1% of last authorships (BMJ Open. 2018 Apr 13;8[4]:e020089).
Both in academic medicine and in practice, a gender pay gap still affects women physicians across the board. Medscape’s 2020 dermatologist compensation report shows male dermatologists earning about 12% more than their female peers (average, $435,000 vs. $387,000, respectively), while the average number of hours per week spent seeing patients is similar (36.2 vs. 35.6 hours, respectively).
And in its 2020 statement on gender equity, the AAMC said that women in academic medicine are offered less in starting salary, negotiated pay, and other forms of compensation than men “despite equal effort, rank, training, and experience.”
It’s complicated to tease apart all the factors that may be involved – but important to keep challenging the system, said Dr. Bergfeld, who was a long-time board adviser for Dermatology News. “I was underpaid,” she noted, and “this was only rectified in the last 10 years.”
Work-life balance
In the AAD podcast on women in dermatology, Dr. Grimes said that achieving a healthy and balanced work life remains one of the greatest challenges for women dermatologists – and it may be even greater than in the past given the growing numbers of group practices. “When women enter the realm of group practice, they have less flexibility in controlling their time and their own schedules.”
If Anna Hare, MD, is any indication, younger dermatologists may buck this trend. The daughter of Dr. Rich in Portland, Dr. Hare joined her mother’s dermatology practice and research center knowing that she’d have “the respect and flexibility for deciding how I want to practice.”
Younger dermatologists, she said, place “more of an emphasis on work-life balance and quality of life.”
Fortunately, said Dr. Bergfeld, women have advanced enough in the ranks of dermatology that, in networking, in mentorship, and in workplace settings, attention can be paid more fully to discussions about work-life management – “how to manage your life when you’re working with family and kids and parents.”
In the 1970s, at the Cleveland Clinic, “there were only five women on staff and we were fighting for [basic] rights,” she said. “We wanted equality – we were [perceived as] little worker bees….We needed to climb as the men did to positions of leadership and address the problems of women.”
In pursuing their goals and making further progress, women dermatologists today should be “steady and calm,” she advised. Formally acquiring leadership skills and communication skills is a timeless need. And when there are biases or conflicts, “you cannot have righteous indignation, you cannot have revenge. You have to calm yourself and move forward.”
Wilma F. Bergfeld, MD, one of only five women in her medical school class of 1964 and the third female in her dermatology residency program, had recently been appointed as a junior clinical dermatologist and head of dermatopathology at the Cleveland Clinic when she was told by a superior that she would not be promoted or invited to serve on any committee or decision-making group.
“I was told I should go home at night and take care of my husband and two children,” she recalled of that moment in the 1970s. The comment made her feel “outraged,” and it drove her, calmly and steadily, to work harder and to “challenge the system.”
Dr. Bergfeld not only was elected to the Cleveland Clinic’s board of governors and board of trustees and served as president of the Clinic’s staff in 1990, she also became the first woman president of the American Academy of Dermatology (1992) and led numerous other dermatologic organizations. Much earlier on, in 1973, to help fulfill her vision of “women helping women,” she had also founded the Women’s Dermatologic Society (WDS). Three years earlier, in 1970, 6.9% of the approximately 4,000 dermatologists in the United States were women, according to the American Medical Association.
Today, when she goes to work as the long-time director of the Clinic’s dermatopathology fellowship and professor of dermatology and pathology at the Cleveland Clinic Educational Foundation, she sees a transformed staff and, more broadly, a national physician workforce in which women made up almost 50% of active dermatologists in 2017 and almost 60% of dermatology residents in 2018, according to data from the American Association of Medical Colleges.
It’s a different and better world, she and other women dermatologists said, but one in which women must continue to mentor other women and continue to challenge the system. Achieving work-life balance, fairer compensation, and a greater proportion of women in the higher ranks of academia are all on their work list.
Women’s impact on the specialty
Dr. Bergfeld and Molly Hinshaw, MD, the current president of the WDS, said they believe women are drawn to dermatology for its visual nature, the growth in diagnostic tests and therapies, and the opportunity to diagnose early and prevent progression of disease in patients of all ages. “It’s a small but mighty specialty,” said Dr. Hinshaw, associate professor of dermatology and section chief of dermatopathology at the University of Wisconsin–Madison.
It’s also a versatile specialty with a variety of subspecialties and niches to pursue – and women have been stepping in to fill unmet needs, Dr. Hinshaw said. “Women dermatologists are directing vulvar specialty clinics across the country, for example. There aren’t that many, but they’re filling an important niche. We have one at [our university] and it is packed.”
Women have also been drawn to the in-demand subspecialty of pediatric dermatology, she noted. They now make up more than two-thirds of all pediatric dermatologists, and many in practice have trained the old-fashioned way, completing two residencies. “That’s [involved] self-selection into an additional year of years training and a commitment to caring for special populations that, quite honestly, takes more time,” said Dr. Hinshaw, who, as part of her dermatology practice, runs a nail clinic at UW Health in Madison.
Amy S. Paller, MD, who chairs the department of dermatology at Northwestern University, Chicago, where she is professor of dermatology and pediatrics and directs the Skin Biology & Diseases Resource-Based Center, is one of these women. She took a long and determined journey into the subspecialty, encountering bias and discouragement while actively seeking out mentors who helped her advance.
While in medical school at Stanford (Calif.) University in the late 1970s in a class “very progressively” made up of about one-third women, Dr. Paller met Alvin Jacobs, MD, who, in 1975, had founded the Society for Pediatric Dermatology. “There wasn’t much pediatric dermatology in the world at the time, and it was Al who helped [me realize] that it combined my love of genetic research with my [desire] to work with children,” she recalled.
Per Dr. Jacob’s advice, she went to Northwestern to train in both pediatrics and dermatology under Nancy Esterly, MD, who “is considered by many to be the mother of pediatric dermatology.” And knowing that she wanted to do research, Dr. Paller also worked with Ruth Freinkel, MD, who “was the strongest bench researcher” at Northwestern. (Dr. Freinkel had been one of the first female dermatology residents at Harvard and was the first full-time faculty member in dermatology at Northwestern).
After completing postdoctoral research at the University of North Carolina at Chapel Hill, Dr. Paller returned to Chicago and assumed Dr. Esterly’s position as chief of dermatology at the Children’s National Hospital of Chicago. It was there that “someone in a leadership position questioned me about how I could possibly be a scientist, a strong clinician, and a good mother to my three children – and suggested that I drop research,” Dr. Paller recalled.
“I think this person was trying to be helpful to me, but I was shocked,” she said. Just as Dr. Bergfeld had done, Dr. Paller channeled her frustration into new pursuits.
“It made me go home and think, how could I strengthen myself? What else could I do?” she said. “Soon after, with a highly supportive husband, I did a ‘pseudosabbatical,’ basically spending every ounce of spare time I had working with one of the premier female scientists in the country, Elaine Fuchs, and learning molecular biology” in her lab at the University of Chicago.
“I think we’ve all had discrimination along the way. Sometimes there’s implicit bias and sometimes there’s overt bias,” said Dr. Paller, who in 2004 led the society which her mentor Dr. Jacobs had founded several decades earlier. “I just jumped right in, and that’s enabled me to find good role models.”
Across dermatology broadly, the often holistic nature of the specialty – of the ability to peer into the body and its internal health – is another quality that women have been drawn to and advanced, Dr. Hinshaw said. “One of the reasons why I chose dermatology is because it’s a window to total patient health. Patients often see their dermatologists as physicians who help them identify next steps in their health care, who can help them address issues related to their overall health and well-being, including their mental health.”
In a WDS membership survey conducted in 2018, most respondents reported that they frequently or occasionally detect and diagnose systemic/internal diseases and conditions in their female patients, and that they consult and collaborate with different kinds of physicians (Int J Womens Dermatol. 2018 Nov 15;4[4]:189-92).
And in a March 2019 “Dialogues in Dermatology” podcast episode on the history and advancement of women in dermatology produced by the American Academy of Dermatology, Pearl Grimes, MD, a clinical professor of dermatology of the University of California, Los Angeles, and then-president of the WDS, described why “total women’s health” had become an additional focus for the society.
“We’re already gatekeepers” in many respects, Dr. Grimes said. “In addition to my addressing specific skin issues, my patients query me on hormone issues, on nutrition, on stress-related issues….and on [what other physicians they should see].”
Phoebe Rich, MD, who owns a small all-woman practice and a research center in Portland, Oregon, said that, in general, many women also communicate and practice in a way that facilitates holistic care. “These qualities aren’t exclusive to women, but women are very caring. We take time and are interested in [patients’] lives in general, not just their disease.”
Disparities in academia
Dermatology departments in academic medicine have burgeoned in size in the past 50 years, and women are well represented overall. In 2018, women comprised 51.2% of dermatology department faculty – up from 10.8% in 1970 – a current proportion that ranks fifth among specialties for the proportion of female faculty, according to a cross-sectional study of faculty diversity trends using data from the AAMC faculty roster (JAMA Dermatol. 2020 Jan 8;156[3]:280-7).
The AAMC data show the share of women dermatology faculty declining at each subsequent rank, however – a finding that suggests that women are not promoted as quickly or to the same levels of leadership as men, the report’s authors noted. (Dermatology isn’t alone: The AAMC issued a call to action on gender equity in medicine this year, citing this inverse association.)
Another recently published study of gender trends in academic dermatology – this one looking at a smaller sample of data from 15 institutions – similarly found that women dermatologists made up a majority of faculty (53.6%) and were well represented as assistant professors (60.7%) but underrepresented as full professors (17%).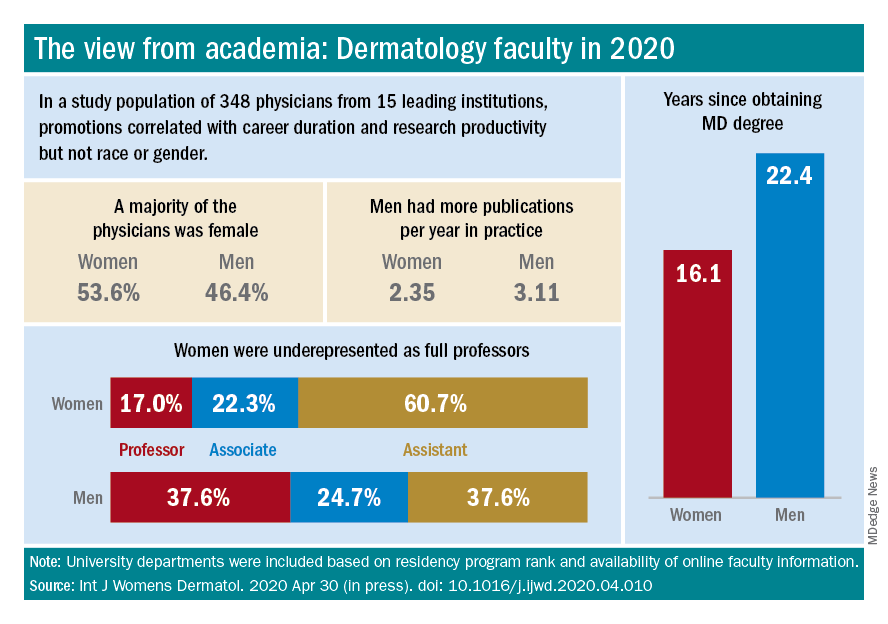
This study differed from the larger AAMC study, however, in that it controlled for “achievement indicators” – career duration, publications per year, and National Institutes of Health research funding – and found that gender alone was not associated with higher rank. Instead, promotions were correlated most significantly with NIH research funding and also with career duration and publications per year.
“If research achievement is to be used as a benchmark for academic promotion, increased efforts are needed to support the research activities of women,” the authors wrote, adding that recognition should be given to other factors as well.
Dr. Paller and Dr. Hinshaw both described the situation as complex and multifaceted. Some research on promotion in academia in general – but not all – has suggested that women do need to publish more than men in order to be promoted. But “the promotion process also has within it the ability to use judgment [about] the impact and merits of work,” said Dr. Hinshaw. “Not all publications [and levels of authorship] may be considered equal, for instance.”
Dr. Hinshaw said she is also concerned by data showing that women still perform the majority of household duties, “even in households in which both partners work outside the home equivalently.” As long as this is the case, women may be “inherently disadvantaged” in their ability to have adequate research time and to advance.
From where she sits, Dr. Paller sees several factors at play: “The pipeline, achievement during the pipeline, and decision-making about advancement” on the part of women themselves. Having served on search committees for top leadership in specialties in which women are well represented, she said, “I’ve seen fewer women who’ve come forward and been interested in rising into a chair or a dean position.”
And “having talked to so many women,” Dr. Paller added, “I think there’s a phenomenon where it’s harder for women to accept positions [that require] a significant change.”
Women “are nurturers, which makes them extremely good [leaders] and chairs, but it also makes it harder to make life changes that affect the people they love,” she said, noting that becoming a department chair or a dean often involves moving. “I also think that women in general are happier and committed to what they’re [currently] doing.”
Dr. Paller is optimistic that, with the support of department chairs and continued attention to role modeling and mentoring, the portrait of women in academic dermatology will continue to improve. Currently, 34 chairs of dermatology departments are female, she noted. “That number was 11 less 15 years ago.”
In the meantime, researchers are increasingly documenting trends in women’s editorships of journals as well as leadership and speaking opportunities at professional conferences.
The authors of one study published this year, for instance, reviewed the editorial boards of dermatology journals and found that women occupied 18% of editor in chief roles, 36% of deputy editor positions, and 22% of overall editorial board roles (Int J Womens Dermatol. 2019 Sep 12;6[1]:20-4). Other research shows women comprising 43% of all authorships across 23 dermatologic journals from 2008 to May 2017, 50.2% of first authorships, and 33.1% of last authorships (BMJ Open. 2018 Apr 13;8[4]:e020089).
Both in academic medicine and in practice, a gender pay gap still affects women physicians across the board. Medscape’s 2020 dermatologist compensation report shows male dermatologists earning about 12% more than their female peers (average, $435,000 vs. $387,000, respectively), while the average number of hours per week spent seeing patients is similar (36.2 vs. 35.6 hours, respectively).
And in its 2020 statement on gender equity, the AAMC said that women in academic medicine are offered less in starting salary, negotiated pay, and other forms of compensation than men “despite equal effort, rank, training, and experience.”
It’s complicated to tease apart all the factors that may be involved – but important to keep challenging the system, said Dr. Bergfeld, who was a long-time board adviser for Dermatology News. “I was underpaid,” she noted, and “this was only rectified in the last 10 years.”
Work-life balance
In the AAD podcast on women in dermatology, Dr. Grimes said that achieving a healthy and balanced work life remains one of the greatest challenges for women dermatologists – and it may be even greater than in the past given the growing numbers of group practices. “When women enter the realm of group practice, they have less flexibility in controlling their time and their own schedules.”
If Anna Hare, MD, is any indication, younger dermatologists may buck this trend. The daughter of Dr. Rich in Portland, Dr. Hare joined her mother’s dermatology practice and research center knowing that she’d have “the respect and flexibility for deciding how I want to practice.”
Younger dermatologists, she said, place “more of an emphasis on work-life balance and quality of life.”
Fortunately, said Dr. Bergfeld, women have advanced enough in the ranks of dermatology that, in networking, in mentorship, and in workplace settings, attention can be paid more fully to discussions about work-life management – “how to manage your life when you’re working with family and kids and parents.”
In the 1970s, at the Cleveland Clinic, “there were only five women on staff and we were fighting for [basic] rights,” she said. “We wanted equality – we were [perceived as] little worker bees….We needed to climb as the men did to positions of leadership and address the problems of women.”
In pursuing their goals and making further progress, women dermatologists today should be “steady and calm,” she advised. Formally acquiring leadership skills and communication skills is a timeless need. And when there are biases or conflicts, “you cannot have righteous indignation, you cannot have revenge. You have to calm yourself and move forward.”
Wilma F. Bergfeld, MD, one of only five women in her medical school class of 1964 and the third female in her dermatology residency program, had recently been appointed as a junior clinical dermatologist and head of dermatopathology at the Cleveland Clinic when she was told by a superior that she would not be promoted or invited to serve on any committee or decision-making group.
“I was told I should go home at night and take care of my husband and two children,” she recalled of that moment in the 1970s. The comment made her feel “outraged,” and it drove her, calmly and steadily, to work harder and to “challenge the system.”
Dr. Bergfeld not only was elected to the Cleveland Clinic’s board of governors and board of trustees and served as president of the Clinic’s staff in 1990, she also became the first woman president of the American Academy of Dermatology (1992) and led numerous other dermatologic organizations. Much earlier on, in 1973, to help fulfill her vision of “women helping women,” she had also founded the Women’s Dermatologic Society (WDS). Three years earlier, in 1970, 6.9% of the approximately 4,000 dermatologists in the United States were women, according to the American Medical Association.
Today, when she goes to work as the long-time director of the Clinic’s dermatopathology fellowship and professor of dermatology and pathology at the Cleveland Clinic Educational Foundation, she sees a transformed staff and, more broadly, a national physician workforce in which women made up almost 50% of active dermatologists in 2017 and almost 60% of dermatology residents in 2018, according to data from the American Association of Medical Colleges.
It’s a different and better world, she and other women dermatologists said, but one in which women must continue to mentor other women and continue to challenge the system. Achieving work-life balance, fairer compensation, and a greater proportion of women in the higher ranks of academia are all on their work list.
Women’s impact on the specialty
Dr. Bergfeld and Molly Hinshaw, MD, the current president of the WDS, said they believe women are drawn to dermatology for its visual nature, the growth in diagnostic tests and therapies, and the opportunity to diagnose early and prevent progression of disease in patients of all ages. “It’s a small but mighty specialty,” said Dr. Hinshaw, associate professor of dermatology and section chief of dermatopathology at the University of Wisconsin–Madison.
It’s also a versatile specialty with a variety of subspecialties and niches to pursue – and women have been stepping in to fill unmet needs, Dr. Hinshaw said. “Women dermatologists are directing vulvar specialty clinics across the country, for example. There aren’t that many, but they’re filling an important niche. We have one at [our university] and it is packed.”
Women have also been drawn to the in-demand subspecialty of pediatric dermatology, she noted. They now make up more than two-thirds of all pediatric dermatologists, and many in practice have trained the old-fashioned way, completing two residencies. “That’s [involved] self-selection into an additional year of years training and a commitment to caring for special populations that, quite honestly, takes more time,” said Dr. Hinshaw, who, as part of her dermatology practice, runs a nail clinic at UW Health in Madison.
Amy S. Paller, MD, who chairs the department of dermatology at Northwestern University, Chicago, where she is professor of dermatology and pediatrics and directs the Skin Biology & Diseases Resource-Based Center, is one of these women. She took a long and determined journey into the subspecialty, encountering bias and discouragement while actively seeking out mentors who helped her advance.
While in medical school at Stanford (Calif.) University in the late 1970s in a class “very progressively” made up of about one-third women, Dr. Paller met Alvin Jacobs, MD, who, in 1975, had founded the Society for Pediatric Dermatology. “There wasn’t much pediatric dermatology in the world at the time, and it was Al who helped [me realize] that it combined my love of genetic research with my [desire] to work with children,” she recalled.
Per Dr. Jacob’s advice, she went to Northwestern to train in both pediatrics and dermatology under Nancy Esterly, MD, who “is considered by many to be the mother of pediatric dermatology.” And knowing that she wanted to do research, Dr. Paller also worked with Ruth Freinkel, MD, who “was the strongest bench researcher” at Northwestern. (Dr. Freinkel had been one of the first female dermatology residents at Harvard and was the first full-time faculty member in dermatology at Northwestern).
After completing postdoctoral research at the University of North Carolina at Chapel Hill, Dr. Paller returned to Chicago and assumed Dr. Esterly’s position as chief of dermatology at the Children’s National Hospital of Chicago. It was there that “someone in a leadership position questioned me about how I could possibly be a scientist, a strong clinician, and a good mother to my three children – and suggested that I drop research,” Dr. Paller recalled.
“I think this person was trying to be helpful to me, but I was shocked,” she said. Just as Dr. Bergfeld had done, Dr. Paller channeled her frustration into new pursuits.
“It made me go home and think, how could I strengthen myself? What else could I do?” she said. “Soon after, with a highly supportive husband, I did a ‘pseudosabbatical,’ basically spending every ounce of spare time I had working with one of the premier female scientists in the country, Elaine Fuchs, and learning molecular biology” in her lab at the University of Chicago.
“I think we’ve all had discrimination along the way. Sometimes there’s implicit bias and sometimes there’s overt bias,” said Dr. Paller, who in 2004 led the society which her mentor Dr. Jacobs had founded several decades earlier. “I just jumped right in, and that’s enabled me to find good role models.”
Across dermatology broadly, the often holistic nature of the specialty – of the ability to peer into the body and its internal health – is another quality that women have been drawn to and advanced, Dr. Hinshaw said. “One of the reasons why I chose dermatology is because it’s a window to total patient health. Patients often see their dermatologists as physicians who help them identify next steps in their health care, who can help them address issues related to their overall health and well-being, including their mental health.”
In a WDS membership survey conducted in 2018, most respondents reported that they frequently or occasionally detect and diagnose systemic/internal diseases and conditions in their female patients, and that they consult and collaborate with different kinds of physicians (Int J Womens Dermatol. 2018 Nov 15;4[4]:189-92).
And in a March 2019 “Dialogues in Dermatology” podcast episode on the history and advancement of women in dermatology produced by the American Academy of Dermatology, Pearl Grimes, MD, a clinical professor of dermatology of the University of California, Los Angeles, and then-president of the WDS, described why “total women’s health” had become an additional focus for the society.
“We’re already gatekeepers” in many respects, Dr. Grimes said. “In addition to my addressing specific skin issues, my patients query me on hormone issues, on nutrition, on stress-related issues….and on [what other physicians they should see].”
Phoebe Rich, MD, who owns a small all-woman practice and a research center in Portland, Oregon, said that, in general, many women also communicate and practice in a way that facilitates holistic care. “These qualities aren’t exclusive to women, but women are very caring. We take time and are interested in [patients’] lives in general, not just their disease.”
Disparities in academia
Dermatology departments in academic medicine have burgeoned in size in the past 50 years, and women are well represented overall. In 2018, women comprised 51.2% of dermatology department faculty – up from 10.8% in 1970 – a current proportion that ranks fifth among specialties for the proportion of female faculty, according to a cross-sectional study of faculty diversity trends using data from the AAMC faculty roster (JAMA Dermatol. 2020 Jan 8;156[3]:280-7).
The AAMC data show the share of women dermatology faculty declining at each subsequent rank, however – a finding that suggests that women are not promoted as quickly or to the same levels of leadership as men, the report’s authors noted. (Dermatology isn’t alone: The AAMC issued a call to action on gender equity in medicine this year, citing this inverse association.)
Another recently published study of gender trends in academic dermatology – this one looking at a smaller sample of data from 15 institutions – similarly found that women dermatologists made up a majority of faculty (53.6%) and were well represented as assistant professors (60.7%) but underrepresented as full professors (17%).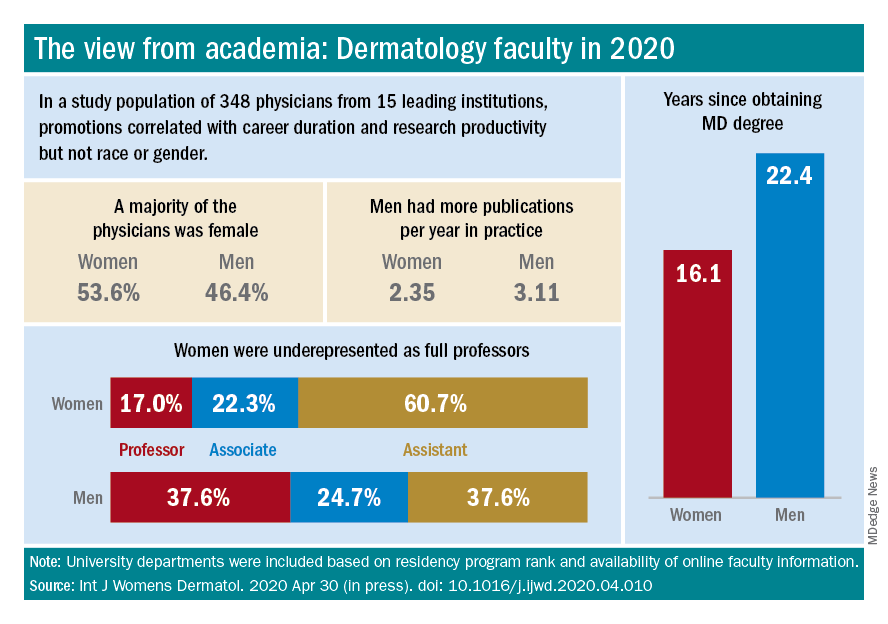
This study differed from the larger AAMC study, however, in that it controlled for “achievement indicators” – career duration, publications per year, and National Institutes of Health research funding – and found that gender alone was not associated with higher rank. Instead, promotions were correlated most significantly with NIH research funding and also with career duration and publications per year.
“If research achievement is to be used as a benchmark for academic promotion, increased efforts are needed to support the research activities of women,” the authors wrote, adding that recognition should be given to other factors as well.
Dr. Paller and Dr. Hinshaw both described the situation as complex and multifaceted. Some research on promotion in academia in general – but not all – has suggested that women do need to publish more than men in order to be promoted. But “the promotion process also has within it the ability to use judgment [about] the impact and merits of work,” said Dr. Hinshaw. “Not all publications [and levels of authorship] may be considered equal, for instance.”
Dr. Hinshaw said she is also concerned by data showing that women still perform the majority of household duties, “even in households in which both partners work outside the home equivalently.” As long as this is the case, women may be “inherently disadvantaged” in their ability to have adequate research time and to advance.
From where she sits, Dr. Paller sees several factors at play: “The pipeline, achievement during the pipeline, and decision-making about advancement” on the part of women themselves. Having served on search committees for top leadership in specialties in which women are well represented, she said, “I’ve seen fewer women who’ve come forward and been interested in rising into a chair or a dean position.”
And “having talked to so many women,” Dr. Paller added, “I think there’s a phenomenon where it’s harder for women to accept positions [that require] a significant change.”
Women “are nurturers, which makes them extremely good [leaders] and chairs, but it also makes it harder to make life changes that affect the people they love,” she said, noting that becoming a department chair or a dean often involves moving. “I also think that women in general are happier and committed to what they’re [currently] doing.”
Dr. Paller is optimistic that, with the support of department chairs and continued attention to role modeling and mentoring, the portrait of women in academic dermatology will continue to improve. Currently, 34 chairs of dermatology departments are female, she noted. “That number was 11 less 15 years ago.”
In the meantime, researchers are increasingly documenting trends in women’s editorships of journals as well as leadership and speaking opportunities at professional conferences.
The authors of one study published this year, for instance, reviewed the editorial boards of dermatology journals and found that women occupied 18% of editor in chief roles, 36% of deputy editor positions, and 22% of overall editorial board roles (Int J Womens Dermatol. 2019 Sep 12;6[1]:20-4). Other research shows women comprising 43% of all authorships across 23 dermatologic journals from 2008 to May 2017, 50.2% of first authorships, and 33.1% of last authorships (BMJ Open. 2018 Apr 13;8[4]:e020089).
Both in academic medicine and in practice, a gender pay gap still affects women physicians across the board. Medscape’s 2020 dermatologist compensation report shows male dermatologists earning about 12% more than their female peers (average, $435,000 vs. $387,000, respectively), while the average number of hours per week spent seeing patients is similar (36.2 vs. 35.6 hours, respectively).
And in its 2020 statement on gender equity, the AAMC said that women in academic medicine are offered less in starting salary, negotiated pay, and other forms of compensation than men “despite equal effort, rank, training, and experience.”
It’s complicated to tease apart all the factors that may be involved – but important to keep challenging the system, said Dr. Bergfeld, who was a long-time board adviser for Dermatology News. “I was underpaid,” she noted, and “this was only rectified in the last 10 years.”
Work-life balance
In the AAD podcast on women in dermatology, Dr. Grimes said that achieving a healthy and balanced work life remains one of the greatest challenges for women dermatologists – and it may be even greater than in the past given the growing numbers of group practices. “When women enter the realm of group practice, they have less flexibility in controlling their time and their own schedules.”
If Anna Hare, MD, is any indication, younger dermatologists may buck this trend. The daughter of Dr. Rich in Portland, Dr. Hare joined her mother’s dermatology practice and research center knowing that she’d have “the respect and flexibility for deciding how I want to practice.”
Younger dermatologists, she said, place “more of an emphasis on work-life balance and quality of life.”
Fortunately, said Dr. Bergfeld, women have advanced enough in the ranks of dermatology that, in networking, in mentorship, and in workplace settings, attention can be paid more fully to discussions about work-life management – “how to manage your life when you’re working with family and kids and parents.”
In the 1970s, at the Cleveland Clinic, “there were only five women on staff and we were fighting for [basic] rights,” she said. “We wanted equality – we were [perceived as] little worker bees….We needed to climb as the men did to positions of leadership and address the problems of women.”
In pursuing their goals and making further progress, women dermatologists today should be “steady and calm,” she advised. Formally acquiring leadership skills and communication skills is a timeless need. And when there are biases or conflicts, “you cannot have righteous indignation, you cannot have revenge. You have to calm yourself and move forward.”