User login
Self-expanding TAVR bests surgery based on 3-year stroke and death risks
Patients with severe aortic stenosis that puts them at increased risk for surgery continue to do better at 3 years after receiving a self-expanding transcatheter aortic valve replacement than do similar patients who have an open surgical valve replacement, according to new results from a randomized trial presented at the annual meeting of the American College of Cardiology.
Two-year follow-up results from the same trial cohort, the CoreValve U.S. Pivotal High Risk Trial, showed superior survival and stroke outcomes for TAVR compared with open surgery (J Am Coll Cardiol. 2015;66[2]:113-21). The difference in outcomes was thought to stem mainly from fewer postprocedural complications and faster recovery in the TAVR group.
The new study, presented at the meeting and simultaneously published online April 3 in the Journal of the American College of Cardiology (doi: 10.1016/j.jacc.2016.03.506) aimed to determine whether the previously seen benefits extended into the third year and whether these were accompanied by differences in valve hemodynamics.
Dr. G. Michael Deeb, Herbert Sloan Collegiate Professor of Cardiac Surgery at the University of Michigan, Ann Arbor, and his colleagues evaluated three-year clinical and echocardiographic outcomes from the 391 patients who underwent TAVR and 359 who had SAVR. At baseline all patients had severe aortic stenosis and were considered to be at increased risk for SAVR, with an estimated 30-day mortality risk 15% or greater and a combined 30-day surgical mortality and major morbidity risk less than 50%.
At 3 years follow-up in the treated groups, combined all-cause mortality or stroke was significantly lower at 37% in TAVR patients as compared to nearly 47% in SAVR patients. All-cause mortality was 33% with TAVR and 39% with SAVR, a difference that did not reach statistical significance. Stroke rates were nearly 13% with TAVR and 19% with SAVR; major adverse cardiovascular or cerebrovascular events were 40% with TAVR and 48% for SAVR. Both were significant differences.
While mean aortic valve gradient measures were more favorable – 7.62 ± 3.57 mm Hg with TAVR and 11.40 ± 6.81 mm Hg with SAVR – regurgitation was significantly higher at nearly 7% with TAVR and no regurgitation with SAVR. Valve thrombosis and valve structural deterioration were not observed in either group.
While the findings show sustained 3-year clinical benefit of self-expanding TAVR over SAVR in patients with aortic stenosis at increased risk for surgery, longer studies are needed to determine whether the crimping and re-crimping of the transcatheter valve would have an impact on long-term bioprosthesis durability.
The study was funded by the device manufacturer Medtronic, and 21 of its 28 authors disclosed financial relationships with Medtronic and/or other manufacturers; one is a Medtronic employee. Dr. Deeb disclosed serving as an unpaid advisor to Medtronic.
Patients with severe aortic stenosis that puts them at increased risk for surgery continue to do better at 3 years after receiving a self-expanding transcatheter aortic valve replacement than do similar patients who have an open surgical valve replacement, according to new results from a randomized trial presented at the annual meeting of the American College of Cardiology.
Two-year follow-up results from the same trial cohort, the CoreValve U.S. Pivotal High Risk Trial, showed superior survival and stroke outcomes for TAVR compared with open surgery (J Am Coll Cardiol. 2015;66[2]:113-21). The difference in outcomes was thought to stem mainly from fewer postprocedural complications and faster recovery in the TAVR group.
The new study, presented at the meeting and simultaneously published online April 3 in the Journal of the American College of Cardiology (doi: 10.1016/j.jacc.2016.03.506) aimed to determine whether the previously seen benefits extended into the third year and whether these were accompanied by differences in valve hemodynamics.
Dr. G. Michael Deeb, Herbert Sloan Collegiate Professor of Cardiac Surgery at the University of Michigan, Ann Arbor, and his colleagues evaluated three-year clinical and echocardiographic outcomes from the 391 patients who underwent TAVR and 359 who had SAVR. At baseline all patients had severe aortic stenosis and were considered to be at increased risk for SAVR, with an estimated 30-day mortality risk 15% or greater and a combined 30-day surgical mortality and major morbidity risk less than 50%.
At 3 years follow-up in the treated groups, combined all-cause mortality or stroke was significantly lower at 37% in TAVR patients as compared to nearly 47% in SAVR patients. All-cause mortality was 33% with TAVR and 39% with SAVR, a difference that did not reach statistical significance. Stroke rates were nearly 13% with TAVR and 19% with SAVR; major adverse cardiovascular or cerebrovascular events were 40% with TAVR and 48% for SAVR. Both were significant differences.
While mean aortic valve gradient measures were more favorable – 7.62 ± 3.57 mm Hg with TAVR and 11.40 ± 6.81 mm Hg with SAVR – regurgitation was significantly higher at nearly 7% with TAVR and no regurgitation with SAVR. Valve thrombosis and valve structural deterioration were not observed in either group.
While the findings show sustained 3-year clinical benefit of self-expanding TAVR over SAVR in patients with aortic stenosis at increased risk for surgery, longer studies are needed to determine whether the crimping and re-crimping of the transcatheter valve would have an impact on long-term bioprosthesis durability.
The study was funded by the device manufacturer Medtronic, and 21 of its 28 authors disclosed financial relationships with Medtronic and/or other manufacturers; one is a Medtronic employee. Dr. Deeb disclosed serving as an unpaid advisor to Medtronic.
Patients with severe aortic stenosis that puts them at increased risk for surgery continue to do better at 3 years after receiving a self-expanding transcatheter aortic valve replacement than do similar patients who have an open surgical valve replacement, according to new results from a randomized trial presented at the annual meeting of the American College of Cardiology.
Two-year follow-up results from the same trial cohort, the CoreValve U.S. Pivotal High Risk Trial, showed superior survival and stroke outcomes for TAVR compared with open surgery (J Am Coll Cardiol. 2015;66[2]:113-21). The difference in outcomes was thought to stem mainly from fewer postprocedural complications and faster recovery in the TAVR group.
The new study, presented at the meeting and simultaneously published online April 3 in the Journal of the American College of Cardiology (doi: 10.1016/j.jacc.2016.03.506) aimed to determine whether the previously seen benefits extended into the third year and whether these were accompanied by differences in valve hemodynamics.
Dr. G. Michael Deeb, Herbert Sloan Collegiate Professor of Cardiac Surgery at the University of Michigan, Ann Arbor, and his colleagues evaluated three-year clinical and echocardiographic outcomes from the 391 patients who underwent TAVR and 359 who had SAVR. At baseline all patients had severe aortic stenosis and were considered to be at increased risk for SAVR, with an estimated 30-day mortality risk 15% or greater and a combined 30-day surgical mortality and major morbidity risk less than 50%.
At 3 years follow-up in the treated groups, combined all-cause mortality or stroke was significantly lower at 37% in TAVR patients as compared to nearly 47% in SAVR patients. All-cause mortality was 33% with TAVR and 39% with SAVR, a difference that did not reach statistical significance. Stroke rates were nearly 13% with TAVR and 19% with SAVR; major adverse cardiovascular or cerebrovascular events were 40% with TAVR and 48% for SAVR. Both were significant differences.
While mean aortic valve gradient measures were more favorable – 7.62 ± 3.57 mm Hg with TAVR and 11.40 ± 6.81 mm Hg with SAVR – regurgitation was significantly higher at nearly 7% with TAVR and no regurgitation with SAVR. Valve thrombosis and valve structural deterioration were not observed in either group.
While the findings show sustained 3-year clinical benefit of self-expanding TAVR over SAVR in patients with aortic stenosis at increased risk for surgery, longer studies are needed to determine whether the crimping and re-crimping of the transcatheter valve would have an impact on long-term bioprosthesis durability.
The study was funded by the device manufacturer Medtronic, and 21 of its 28 authors disclosed financial relationships with Medtronic and/or other manufacturers; one is a Medtronic employee. Dr. Deeb disclosed serving as an unpaid advisor to Medtronic.
FROM ACC 2016
Key clinical point: Patients randomized to self-expanding TAVR or open surgical aortic valve replacement were less likely to have died or had a stroke at 3 years post-procedure
Major finding:. Three-year all-cause mortality and stroke rate was significantly lower in TAVR patients – 37% versus nearly 47% in SAVR patients.
Data source: A cohort of 750 patients deemed high risk who underwent open aortic valve replacement or TAVR after randomization; procedures performed at 45 sites
Disclosures: The study was sponsored by Medtronic, maker of the self-expanding transcatheter technology. Most study authors, though not the lead author, had direct financial involvement.
CDC urges states to prepare for Zika
As warmer weather raises the possibility of local Zika virus transmission in the continental United States, federal health officials are pushing state and local governments to devise plans aimed at protecting pregnant women from infection, to increase access to contraception, and to ensure better coordination by mosquito control districts.
On April 1, the U.S. Centers for Disease Prevention and Control hosted a day-long seminar on Zika attended by some 300 state and local public health professionals. Zika virus, which is increasingly linked to adverse fetal outcomes including microcephaly, is now spreading in Puerto Rico, the U.S. Virgin Islands, and American Samoa.
Though most of the U.S. response effort is currently concentrated in Puerto Rico, and no local transmission has yet been reported in the continental U.S., a CDC report issued concurrently with the conference highlighted the potential for Zika transmission within the U.S. The entire southern half of the continental U.S., and much of its east coast, is home to the Aedes aegypti mosquitoes that can carry Zika virus.
In the same report, CDC also stressed that pregnant women should avoid travel to areas where Zika is being rapidly transmitted, and avoid sexual contact or consistently use condoms with partners who “reside in or have traveled to areas with active Zika virus transmission.”
“The key here is to reduce the risk to pregnant women,” Dr. Tom Frieden, CDC director, said at a news conference during the meeting. “There is an urgent need for all of us to learn more and do more,” he noted, acknowledging that officials had concerns about securing sufficient federal funding, getting rapid screening tools commercially developed in the absence of such funding, and improving the capabilities of U.S. mosquito control districts in the states most likely to be affected.
As local clusters of dengue virus disease have occurred in Florida, Texas, and Hawaii, Dr. Frieden said these states need to be particularly responsive to the Zika threat. However, Zika transmission could follow a different pattern, he said.
While Dr. Frieden described some local mosquito control districts and their capabilities as robust, others are considerably less so. Many districts in vulnerable states are not contiguous, leading to potential gaps in vector control. Dr. Frieden noted that even where control is most intensive, such as in Puerto Rico, vector resistance to common pesticides is a problem.
Dr. Frieden also stressed the importance of widening local access to contraception. He clarified that the CDC was not advising couples to avoid or delay pregnancy, even in Puerto Rico. However, he said, “if a woman and her partner choose not to become pregnant [there should be] ready access to effective contraception,” particularly the long-term reversible methods likely to be most effective.
Amy Pope, deputy homeland security advisor in the Obama administration, underscored the concern about Zika-specific funding. In February, the administration requested some $1.9 billion from Congress to combat Zika, including by improving access to contraception, developing vaccines and diagnostics, and other efforts. This funding has yet to be approved, Ms. Pope noted, adding that some members of Congress proposed redirecting funding that had been earmarked to combat Ebola.
“Congress is asking the American people to choose which disease it wants the most protection from,” Ms. Pope said, and Dr. Frieden reminded the conference that the Ebola crisis was not over. A new case from Liberia was announced April 1, he noted, and an ongoing cluster of transmission is occurring in Guinea.
As warmer weather raises the possibility of local Zika virus transmission in the continental United States, federal health officials are pushing state and local governments to devise plans aimed at protecting pregnant women from infection, to increase access to contraception, and to ensure better coordination by mosquito control districts.
On April 1, the U.S. Centers for Disease Prevention and Control hosted a day-long seminar on Zika attended by some 300 state and local public health professionals. Zika virus, which is increasingly linked to adverse fetal outcomes including microcephaly, is now spreading in Puerto Rico, the U.S. Virgin Islands, and American Samoa.
Though most of the U.S. response effort is currently concentrated in Puerto Rico, and no local transmission has yet been reported in the continental U.S., a CDC report issued concurrently with the conference highlighted the potential for Zika transmission within the U.S. The entire southern half of the continental U.S., and much of its east coast, is home to the Aedes aegypti mosquitoes that can carry Zika virus.
In the same report, CDC also stressed that pregnant women should avoid travel to areas where Zika is being rapidly transmitted, and avoid sexual contact or consistently use condoms with partners who “reside in or have traveled to areas with active Zika virus transmission.”
“The key here is to reduce the risk to pregnant women,” Dr. Tom Frieden, CDC director, said at a news conference during the meeting. “There is an urgent need for all of us to learn more and do more,” he noted, acknowledging that officials had concerns about securing sufficient federal funding, getting rapid screening tools commercially developed in the absence of such funding, and improving the capabilities of U.S. mosquito control districts in the states most likely to be affected.
As local clusters of dengue virus disease have occurred in Florida, Texas, and Hawaii, Dr. Frieden said these states need to be particularly responsive to the Zika threat. However, Zika transmission could follow a different pattern, he said.
While Dr. Frieden described some local mosquito control districts and their capabilities as robust, others are considerably less so. Many districts in vulnerable states are not contiguous, leading to potential gaps in vector control. Dr. Frieden noted that even where control is most intensive, such as in Puerto Rico, vector resistance to common pesticides is a problem.
Dr. Frieden also stressed the importance of widening local access to contraception. He clarified that the CDC was not advising couples to avoid or delay pregnancy, even in Puerto Rico. However, he said, “if a woman and her partner choose not to become pregnant [there should be] ready access to effective contraception,” particularly the long-term reversible methods likely to be most effective.
Amy Pope, deputy homeland security advisor in the Obama administration, underscored the concern about Zika-specific funding. In February, the administration requested some $1.9 billion from Congress to combat Zika, including by improving access to contraception, developing vaccines and diagnostics, and other efforts. This funding has yet to be approved, Ms. Pope noted, adding that some members of Congress proposed redirecting funding that had been earmarked to combat Ebola.
“Congress is asking the American people to choose which disease it wants the most protection from,” Ms. Pope said, and Dr. Frieden reminded the conference that the Ebola crisis was not over. A new case from Liberia was announced April 1, he noted, and an ongoing cluster of transmission is occurring in Guinea.
As warmer weather raises the possibility of local Zika virus transmission in the continental United States, federal health officials are pushing state and local governments to devise plans aimed at protecting pregnant women from infection, to increase access to contraception, and to ensure better coordination by mosquito control districts.
On April 1, the U.S. Centers for Disease Prevention and Control hosted a day-long seminar on Zika attended by some 300 state and local public health professionals. Zika virus, which is increasingly linked to adverse fetal outcomes including microcephaly, is now spreading in Puerto Rico, the U.S. Virgin Islands, and American Samoa.
Though most of the U.S. response effort is currently concentrated in Puerto Rico, and no local transmission has yet been reported in the continental U.S., a CDC report issued concurrently with the conference highlighted the potential for Zika transmission within the U.S. The entire southern half of the continental U.S., and much of its east coast, is home to the Aedes aegypti mosquitoes that can carry Zika virus.
In the same report, CDC also stressed that pregnant women should avoid travel to areas where Zika is being rapidly transmitted, and avoid sexual contact or consistently use condoms with partners who “reside in or have traveled to areas with active Zika virus transmission.”
“The key here is to reduce the risk to pregnant women,” Dr. Tom Frieden, CDC director, said at a news conference during the meeting. “There is an urgent need for all of us to learn more and do more,” he noted, acknowledging that officials had concerns about securing sufficient federal funding, getting rapid screening tools commercially developed in the absence of such funding, and improving the capabilities of U.S. mosquito control districts in the states most likely to be affected.
As local clusters of dengue virus disease have occurred in Florida, Texas, and Hawaii, Dr. Frieden said these states need to be particularly responsive to the Zika threat. However, Zika transmission could follow a different pattern, he said.
While Dr. Frieden described some local mosquito control districts and their capabilities as robust, others are considerably less so. Many districts in vulnerable states are not contiguous, leading to potential gaps in vector control. Dr. Frieden noted that even where control is most intensive, such as in Puerto Rico, vector resistance to common pesticides is a problem.
Dr. Frieden also stressed the importance of widening local access to contraception. He clarified that the CDC was not advising couples to avoid or delay pregnancy, even in Puerto Rico. However, he said, “if a woman and her partner choose not to become pregnant [there should be] ready access to effective contraception,” particularly the long-term reversible methods likely to be most effective.
Amy Pope, deputy homeland security advisor in the Obama administration, underscored the concern about Zika-specific funding. In February, the administration requested some $1.9 billion from Congress to combat Zika, including by improving access to contraception, developing vaccines and diagnostics, and other efforts. This funding has yet to be approved, Ms. Pope noted, adding that some members of Congress proposed redirecting funding that had been earmarked to combat Ebola.
“Congress is asking the American people to choose which disease it wants the most protection from,” Ms. Pope said, and Dr. Frieden reminded the conference that the Ebola crisis was not over. A new case from Liberia was announced April 1, he noted, and an ongoing cluster of transmission is occurring in Guinea.
Aiming to reduce biopsies with high-tech photoacoustics and a low-tech sponge
BOSTON – Two award-winning researchers have received funding from the AGA Research Foundation to support their research into less invasive diagnostic techniques for GI patient care. The researchers shared updates on their findings at the 2016 AGA Tech Summit, which is sponsored by the AGA Center for GI Innovation and Technology.
Update on AGA-Boston Scientific Career Development Technology & Innovation Award
Guan Xu, Ph.D., of the University of Michigan, Ann Arbor, received the 2015 AGA–Boston Scientific award to support his investigation of an experimental, optically induced ultrasonic imaging technique called photoacoustic imaging, or PAI, in Crohn’s disease.
PAI uses pulsed laser light to penetrate tissues at different depths, allowing researchers to distinguish the absorption spectra indicative of the different chemical compositions seen in inflammatory and fibrous intestinal strictures.
Though a number of experimental modalities are being investigated to characterize intestinal strictures less invasively, tissue biopsy is still considered the only reliable way to determine whether strictures are inflammatory or fibrous. Inflammatory strictures can be treated medically, while collagen-based fibrotic strictures must be removed surgically or treated with endoscopic dilation.
Dr. Xu joined Michigan’s radiology department as a postdoctoral research fellow in 2012 and is now a research investigator there. He previously helped develop a photoacoustic ultrasound imaging system for finger arthritis, designed for use in a clinical setting.
Dr. Xu and colleagues in the radiology, pathology, engineering and internal medicine departments at the University of Michigan are now investigating in animal models whether PAI is as accurate as tissue biopsy in distinguishing the two types of intestinal strictures seen in Crohn’s. They are also designing a capsule PAI device that can be fitted to an endoscope.
The PAI technology builds on and extends the ultrasound technology that is currently the standard of care, explained Dr. Xu, saying “We are standing on the shoulders of giants.”
At the Tech Summit, Dr. Xu presented an update of his research. Preliminary results have revealed significant differences in photoacoustic signal intensity among normal, inflammatory, and fibrotic bowel tissues in rats, and also strong correlations between photoacoustic images and histology in human stricture tissues. A prototype capsule PAI probe has been developed and it will soon be tested on mouse and rabbit models.
In an interview, Dr. Xu expressed “sincere gratitude to the AGA Research Foundation and Boston Scientific for the support of our preliminary study. We will work toward translation of our system to clinics.”
If Dr. Xu and his colleagues’ work is successful, clinicians may one day be able to distinguish between inflammatory and fibrotic intestinal strictures in Crohn’s disease patients without needing to perform endoscopic biopsy. The team’s findings may also prove useful in the preclinical investigation of antifibrotic medical therapies.
Update on AGA-Covidien Research & Development Pilot Award in Technology
Dr. David A. Katzka received the 2015 AGA–Covidien (now Medtronic) award, for his ongoing research into a simple, inexpensive technology as a possible alternative to repeat endoscopy and biopsy to monitor therapeutic response in people with eosinophilic esophagitis (EoE).
EoE is thought to result from exposure to food antigens, leading to inflammation and stricture formation. Current treatment recommendations include topical steroids and elimination diets, both of which are effective. However, response to withdrawal or reintroduction of problem foods often needs to be reassessed with repeat endoscopy and biopsy, which is both costly and time consuming.
Dr. Katzka, head of the Esophageal Interest Group at the Mayo Clinic in Rochester, Minn., has been developing the Cytosponge, an easily swallowed encapsulated mesh that expands in the stomach. Upon retrieval (by means of an attached string), the sponge provides a sample of esophageal mucosa. The technology was originally developed as a screening modality for esophageal cancer and Barrett’s esophagus. Unlike with endoscopy, no sedation is required.
A preliminary feasibility study in 20 patients with EoE who underwent both Cytosponge and endoscopic biopsy found good correlation of eosinophils between the two technologies, and a high sensitivity (84%) in diagnosing EoE. Genetic analysis of patient specimens obtained with Cytosponge showed consistency with previous transcriptome data seen on biopsy specimens. Importantly, patients favored the Cytosponge as faster and easier to tolerate than endoscopy.
Dr. Katzka’s research team is now studying a larger patient group to compare the Cytosponge with endoscopic biopsy as a reliable and independent means of monitoring disease activity and response to therapy. Genomic analysis is also being performed on specimens so that as molecular predictors of response to therapy are further developed and become available, these tests may be also be performed – with the idea of limiting or eliminating the need for endoscopy.
Dr. Katzka reported recruitment of 79 EoE patients in addition to the 20 patients from the pilot study. Thirty-five of these patients had active EoE and 44 were in remission. The accuracy of the Cytosponge in comparison to biopsy remained high, with 81% sensitivity and 79% specificity.
Furthermore, five patients were diagnosed with active disease with the Cytosponge who were not diagnosed by biopsy. The endoscopic abrasion scores were all 0 or 1. The procedure was well tolerated, with near universal preference for undergoing the Cytosponge procedure rather than sedated endoscopy. A trial to use the sponge for monitoring diet therapy is underway, with 35 patients currently being recruited.
The study has also expanded to become multicenter, starting with Dr. Evan Dellon at the University of North Carolina, where 15 patients have undergone the procedure with central processing of pathology at the Mayo Clinic.
Announcement of 2016 AGA-Medtronic Research & Development Pilot Award in Technology
The 2016 AGA-Medtronic award winner is Wa Xian, Ph.D., assistant professor at the University of Texas Health Science Center, Houston. In naming Dr. Xian as the awardee, Dr. Michael L. Kochman said that her work proposes to test the hypothesis that inflammatory bowel disease is caused by genetic defects in the intestines’ epithelial barriers to gut microbes. Dr. Xian will build on her previous work of cloning colonic stem cells to test the genetic defect hypothesis, said Dr. Kochman, professor of medicine at Penn Medicine.
Kari Oakes contributed to this report.
BOSTON – Two award-winning researchers have received funding from the AGA Research Foundation to support their research into less invasive diagnostic techniques for GI patient care. The researchers shared updates on their findings at the 2016 AGA Tech Summit, which is sponsored by the AGA Center for GI Innovation and Technology.
Update on AGA-Boston Scientific Career Development Technology & Innovation Award
Guan Xu, Ph.D., of the University of Michigan, Ann Arbor, received the 2015 AGA–Boston Scientific award to support his investigation of an experimental, optically induced ultrasonic imaging technique called photoacoustic imaging, or PAI, in Crohn’s disease.
PAI uses pulsed laser light to penetrate tissues at different depths, allowing researchers to distinguish the absorption spectra indicative of the different chemical compositions seen in inflammatory and fibrous intestinal strictures.
Though a number of experimental modalities are being investigated to characterize intestinal strictures less invasively, tissue biopsy is still considered the only reliable way to determine whether strictures are inflammatory or fibrous. Inflammatory strictures can be treated medically, while collagen-based fibrotic strictures must be removed surgically or treated with endoscopic dilation.
Dr. Xu joined Michigan’s radiology department as a postdoctoral research fellow in 2012 and is now a research investigator there. He previously helped develop a photoacoustic ultrasound imaging system for finger arthritis, designed for use in a clinical setting.
Dr. Xu and colleagues in the radiology, pathology, engineering and internal medicine departments at the University of Michigan are now investigating in animal models whether PAI is as accurate as tissue biopsy in distinguishing the two types of intestinal strictures seen in Crohn’s. They are also designing a capsule PAI device that can be fitted to an endoscope.
The PAI technology builds on and extends the ultrasound technology that is currently the standard of care, explained Dr. Xu, saying “We are standing on the shoulders of giants.”
At the Tech Summit, Dr. Xu presented an update of his research. Preliminary results have revealed significant differences in photoacoustic signal intensity among normal, inflammatory, and fibrotic bowel tissues in rats, and also strong correlations between photoacoustic images and histology in human stricture tissues. A prototype capsule PAI probe has been developed and it will soon be tested on mouse and rabbit models.
In an interview, Dr. Xu expressed “sincere gratitude to the AGA Research Foundation and Boston Scientific for the support of our preliminary study. We will work toward translation of our system to clinics.”
If Dr. Xu and his colleagues’ work is successful, clinicians may one day be able to distinguish between inflammatory and fibrotic intestinal strictures in Crohn’s disease patients without needing to perform endoscopic biopsy. The team’s findings may also prove useful in the preclinical investigation of antifibrotic medical therapies.
Update on AGA-Covidien Research & Development Pilot Award in Technology
Dr. David A. Katzka received the 2015 AGA–Covidien (now Medtronic) award, for his ongoing research into a simple, inexpensive technology as a possible alternative to repeat endoscopy and biopsy to monitor therapeutic response in people with eosinophilic esophagitis (EoE).
EoE is thought to result from exposure to food antigens, leading to inflammation and stricture formation. Current treatment recommendations include topical steroids and elimination diets, both of which are effective. However, response to withdrawal or reintroduction of problem foods often needs to be reassessed with repeat endoscopy and biopsy, which is both costly and time consuming.
Dr. Katzka, head of the Esophageal Interest Group at the Mayo Clinic in Rochester, Minn., has been developing the Cytosponge, an easily swallowed encapsulated mesh that expands in the stomach. Upon retrieval (by means of an attached string), the sponge provides a sample of esophageal mucosa. The technology was originally developed as a screening modality for esophageal cancer and Barrett’s esophagus. Unlike with endoscopy, no sedation is required.
A preliminary feasibility study in 20 patients with EoE who underwent both Cytosponge and endoscopic biopsy found good correlation of eosinophils between the two technologies, and a high sensitivity (84%) in diagnosing EoE. Genetic analysis of patient specimens obtained with Cytosponge showed consistency with previous transcriptome data seen on biopsy specimens. Importantly, patients favored the Cytosponge as faster and easier to tolerate than endoscopy.
Dr. Katzka’s research team is now studying a larger patient group to compare the Cytosponge with endoscopic biopsy as a reliable and independent means of monitoring disease activity and response to therapy. Genomic analysis is also being performed on specimens so that as molecular predictors of response to therapy are further developed and become available, these tests may be also be performed – with the idea of limiting or eliminating the need for endoscopy.
Dr. Katzka reported recruitment of 79 EoE patients in addition to the 20 patients from the pilot study. Thirty-five of these patients had active EoE and 44 were in remission. The accuracy of the Cytosponge in comparison to biopsy remained high, with 81% sensitivity and 79% specificity.
Furthermore, five patients were diagnosed with active disease with the Cytosponge who were not diagnosed by biopsy. The endoscopic abrasion scores were all 0 or 1. The procedure was well tolerated, with near universal preference for undergoing the Cytosponge procedure rather than sedated endoscopy. A trial to use the sponge for monitoring diet therapy is underway, with 35 patients currently being recruited.
The study has also expanded to become multicenter, starting with Dr. Evan Dellon at the University of North Carolina, where 15 patients have undergone the procedure with central processing of pathology at the Mayo Clinic.
Announcement of 2016 AGA-Medtronic Research & Development Pilot Award in Technology
The 2016 AGA-Medtronic award winner is Wa Xian, Ph.D., assistant professor at the University of Texas Health Science Center, Houston. In naming Dr. Xian as the awardee, Dr. Michael L. Kochman said that her work proposes to test the hypothesis that inflammatory bowel disease is caused by genetic defects in the intestines’ epithelial barriers to gut microbes. Dr. Xian will build on her previous work of cloning colonic stem cells to test the genetic defect hypothesis, said Dr. Kochman, professor of medicine at Penn Medicine.
Kari Oakes contributed to this report.
BOSTON – Two award-winning researchers have received funding from the AGA Research Foundation to support their research into less invasive diagnostic techniques for GI patient care. The researchers shared updates on their findings at the 2016 AGA Tech Summit, which is sponsored by the AGA Center for GI Innovation and Technology.
Update on AGA-Boston Scientific Career Development Technology & Innovation Award
Guan Xu, Ph.D., of the University of Michigan, Ann Arbor, received the 2015 AGA–Boston Scientific award to support his investigation of an experimental, optically induced ultrasonic imaging technique called photoacoustic imaging, or PAI, in Crohn’s disease.
PAI uses pulsed laser light to penetrate tissues at different depths, allowing researchers to distinguish the absorption spectra indicative of the different chemical compositions seen in inflammatory and fibrous intestinal strictures.
Though a number of experimental modalities are being investigated to characterize intestinal strictures less invasively, tissue biopsy is still considered the only reliable way to determine whether strictures are inflammatory or fibrous. Inflammatory strictures can be treated medically, while collagen-based fibrotic strictures must be removed surgically or treated with endoscopic dilation.
Dr. Xu joined Michigan’s radiology department as a postdoctoral research fellow in 2012 and is now a research investigator there. He previously helped develop a photoacoustic ultrasound imaging system for finger arthritis, designed for use in a clinical setting.
Dr. Xu and colleagues in the radiology, pathology, engineering and internal medicine departments at the University of Michigan are now investigating in animal models whether PAI is as accurate as tissue biopsy in distinguishing the two types of intestinal strictures seen in Crohn’s. They are also designing a capsule PAI device that can be fitted to an endoscope.
The PAI technology builds on and extends the ultrasound technology that is currently the standard of care, explained Dr. Xu, saying “We are standing on the shoulders of giants.”
At the Tech Summit, Dr. Xu presented an update of his research. Preliminary results have revealed significant differences in photoacoustic signal intensity among normal, inflammatory, and fibrotic bowel tissues in rats, and also strong correlations between photoacoustic images and histology in human stricture tissues. A prototype capsule PAI probe has been developed and it will soon be tested on mouse and rabbit models.
In an interview, Dr. Xu expressed “sincere gratitude to the AGA Research Foundation and Boston Scientific for the support of our preliminary study. We will work toward translation of our system to clinics.”
If Dr. Xu and his colleagues’ work is successful, clinicians may one day be able to distinguish between inflammatory and fibrotic intestinal strictures in Crohn’s disease patients without needing to perform endoscopic biopsy. The team’s findings may also prove useful in the preclinical investigation of antifibrotic medical therapies.
Update on AGA-Covidien Research & Development Pilot Award in Technology
Dr. David A. Katzka received the 2015 AGA–Covidien (now Medtronic) award, for his ongoing research into a simple, inexpensive technology as a possible alternative to repeat endoscopy and biopsy to monitor therapeutic response in people with eosinophilic esophagitis (EoE).
EoE is thought to result from exposure to food antigens, leading to inflammation and stricture formation. Current treatment recommendations include topical steroids and elimination diets, both of which are effective. However, response to withdrawal or reintroduction of problem foods often needs to be reassessed with repeat endoscopy and biopsy, which is both costly and time consuming.
Dr. Katzka, head of the Esophageal Interest Group at the Mayo Clinic in Rochester, Minn., has been developing the Cytosponge, an easily swallowed encapsulated mesh that expands in the stomach. Upon retrieval (by means of an attached string), the sponge provides a sample of esophageal mucosa. The technology was originally developed as a screening modality for esophageal cancer and Barrett’s esophagus. Unlike with endoscopy, no sedation is required.
A preliminary feasibility study in 20 patients with EoE who underwent both Cytosponge and endoscopic biopsy found good correlation of eosinophils between the two technologies, and a high sensitivity (84%) in diagnosing EoE. Genetic analysis of patient specimens obtained with Cytosponge showed consistency with previous transcriptome data seen on biopsy specimens. Importantly, patients favored the Cytosponge as faster and easier to tolerate than endoscopy.
Dr. Katzka’s research team is now studying a larger patient group to compare the Cytosponge with endoscopic biopsy as a reliable and independent means of monitoring disease activity and response to therapy. Genomic analysis is also being performed on specimens so that as molecular predictors of response to therapy are further developed and become available, these tests may be also be performed – with the idea of limiting or eliminating the need for endoscopy.
Dr. Katzka reported recruitment of 79 EoE patients in addition to the 20 patients from the pilot study. Thirty-five of these patients had active EoE and 44 were in remission. The accuracy of the Cytosponge in comparison to biopsy remained high, with 81% sensitivity and 79% specificity.
Furthermore, five patients were diagnosed with active disease with the Cytosponge who were not diagnosed by biopsy. The endoscopic abrasion scores were all 0 or 1. The procedure was well tolerated, with near universal preference for undergoing the Cytosponge procedure rather than sedated endoscopy. A trial to use the sponge for monitoring diet therapy is underway, with 35 patients currently being recruited.
The study has also expanded to become multicenter, starting with Dr. Evan Dellon at the University of North Carolina, where 15 patients have undergone the procedure with central processing of pathology at the Mayo Clinic.
Announcement of 2016 AGA-Medtronic Research & Development Pilot Award in Technology
The 2016 AGA-Medtronic award winner is Wa Xian, Ph.D., assistant professor at the University of Texas Health Science Center, Houston. In naming Dr. Xian as the awardee, Dr. Michael L. Kochman said that her work proposes to test the hypothesis that inflammatory bowel disease is caused by genetic defects in the intestines’ epithelial barriers to gut microbes. Dr. Xian will build on her previous work of cloning colonic stem cells to test the genetic defect hypothesis, said Dr. Kochman, professor of medicine at Penn Medicine.
Kari Oakes contributed to this report.
FROM THE AGA 2016 TECH SUMMIT
No increase in ASD prevalence seen between 2010 and 2012
The prevalence of autism spectrum disorder (ASD) in 8-year-old children in 2012 was estimated to be 14.6 per 1,000, or one in 68, according to the Centers for Disease Control and Prevention.
The estimate, published online March 31 in CDC’s Morbidity and Mortality Weekly Report (Surveill Summ. 2016. Apr 1;65[3]:1-23) is similar to that seen in CDC’s 2010 survey of 8-year-old children, where 14.7 of 1,000 were estimated affected. In CDC surveys prior to 2010, prevalence was usually seen increasing over time, from 6.6 children per 1,000 in 2002 to 9 in 2006 and 11.3 in 2008.
However, the investigators led by Deborah L. Christensen, Ph.D., of the CDC’s National Center on Birth Defects and Disabilities, Atlanta, cautioned that it was premature to conclude that overall prevalence of ASD was stabilizing, in part because of significant variation seen among the 11 study sites and because of potential underevaluation or delayed evaluation among some ethnic and racial subgroups. Also, prevalence was significantly higher at surveillance sites where both education and health records were reviewed (17.1 per 1,000), compared with sites where investigators reviewed health records only (10.7 per 1,000).
The CDC’s Autism and Developmental Disabilities Monitoring Network screens children in 11 states (Arkansas, Arizona, Colorado, Georgia, Maryland, Missouri, New Jersey, North Carolina, South Carolina, Utah, and Wisconsin) using health care and education sources to determine rates of ASD. The network surveillance area covered about 350,000 8-year-old children (53% white, 21% black, 20% Hispanic, 5% Asian, and 1% American Indian/Alaska Native) in 2012. Prevalence was markedly higher among boys (23.6 per 1,000, or 1 in 42) than among girls (5.3 per 1,000, or 1 in 189), a difference largely unchanged from previous studies.
ASD prevalence by ethnic or racial subgroup also did not change significantly over prior surveys, the investigators reported. However, lower estimates among black and Hispanic children could reflect “differences in awareness of ASD or access to specialty diagnostic services,” they wrote. Fewer black and Hispanic children in the survey had a comprehensive developmental evaluation by age 36 months (40% and 39%, respectively), compared with non-Hispanic white children (45%), which investigators called worrisome, as “early treatment might maximize the ability of children to function and participate in their community.”
Moreover, prevalence was seen increasing significantly over the previous survey in two states (New Jersey and Wisconsin), and decreasing significantly in one state (Missouri). Investigators suspected that variation in local health care systems’ ability to obtain comprehensive developmental evaluations might be a factor.
The wide range of ASD prevalence estimates, the investigators wrote, demands “caution in interpreting the similarity of overall estimated ASD prevalence between 2010 and 2012.”
The CDC funded the study and investigators disclosed no conflicts of interest.
The prevalence of autism spectrum disorder (ASD) in 8-year-old children in 2012 was estimated to be 14.6 per 1,000, or one in 68, according to the Centers for Disease Control and Prevention.
The estimate, published online March 31 in CDC’s Morbidity and Mortality Weekly Report (Surveill Summ. 2016. Apr 1;65[3]:1-23) is similar to that seen in CDC’s 2010 survey of 8-year-old children, where 14.7 of 1,000 were estimated affected. In CDC surveys prior to 2010, prevalence was usually seen increasing over time, from 6.6 children per 1,000 in 2002 to 9 in 2006 and 11.3 in 2008.
However, the investigators led by Deborah L. Christensen, Ph.D., of the CDC’s National Center on Birth Defects and Disabilities, Atlanta, cautioned that it was premature to conclude that overall prevalence of ASD was stabilizing, in part because of significant variation seen among the 11 study sites and because of potential underevaluation or delayed evaluation among some ethnic and racial subgroups. Also, prevalence was significantly higher at surveillance sites where both education and health records were reviewed (17.1 per 1,000), compared with sites where investigators reviewed health records only (10.7 per 1,000).
The CDC’s Autism and Developmental Disabilities Monitoring Network screens children in 11 states (Arkansas, Arizona, Colorado, Georgia, Maryland, Missouri, New Jersey, North Carolina, South Carolina, Utah, and Wisconsin) using health care and education sources to determine rates of ASD. The network surveillance area covered about 350,000 8-year-old children (53% white, 21% black, 20% Hispanic, 5% Asian, and 1% American Indian/Alaska Native) in 2012. Prevalence was markedly higher among boys (23.6 per 1,000, or 1 in 42) than among girls (5.3 per 1,000, or 1 in 189), a difference largely unchanged from previous studies.
ASD prevalence by ethnic or racial subgroup also did not change significantly over prior surveys, the investigators reported. However, lower estimates among black and Hispanic children could reflect “differences in awareness of ASD or access to specialty diagnostic services,” they wrote. Fewer black and Hispanic children in the survey had a comprehensive developmental evaluation by age 36 months (40% and 39%, respectively), compared with non-Hispanic white children (45%), which investigators called worrisome, as “early treatment might maximize the ability of children to function and participate in their community.”
Moreover, prevalence was seen increasing significantly over the previous survey in two states (New Jersey and Wisconsin), and decreasing significantly in one state (Missouri). Investigators suspected that variation in local health care systems’ ability to obtain comprehensive developmental evaluations might be a factor.
The wide range of ASD prevalence estimates, the investigators wrote, demands “caution in interpreting the similarity of overall estimated ASD prevalence between 2010 and 2012.”
The CDC funded the study and investigators disclosed no conflicts of interest.
The prevalence of autism spectrum disorder (ASD) in 8-year-old children in 2012 was estimated to be 14.6 per 1,000, or one in 68, according to the Centers for Disease Control and Prevention.
The estimate, published online March 31 in CDC’s Morbidity and Mortality Weekly Report (Surveill Summ. 2016. Apr 1;65[3]:1-23) is similar to that seen in CDC’s 2010 survey of 8-year-old children, where 14.7 of 1,000 were estimated affected. In CDC surveys prior to 2010, prevalence was usually seen increasing over time, from 6.6 children per 1,000 in 2002 to 9 in 2006 and 11.3 in 2008.
However, the investigators led by Deborah L. Christensen, Ph.D., of the CDC’s National Center on Birth Defects and Disabilities, Atlanta, cautioned that it was premature to conclude that overall prevalence of ASD was stabilizing, in part because of significant variation seen among the 11 study sites and because of potential underevaluation or delayed evaluation among some ethnic and racial subgroups. Also, prevalence was significantly higher at surveillance sites where both education and health records were reviewed (17.1 per 1,000), compared with sites where investigators reviewed health records only (10.7 per 1,000).
The CDC’s Autism and Developmental Disabilities Monitoring Network screens children in 11 states (Arkansas, Arizona, Colorado, Georgia, Maryland, Missouri, New Jersey, North Carolina, South Carolina, Utah, and Wisconsin) using health care and education sources to determine rates of ASD. The network surveillance area covered about 350,000 8-year-old children (53% white, 21% black, 20% Hispanic, 5% Asian, and 1% American Indian/Alaska Native) in 2012. Prevalence was markedly higher among boys (23.6 per 1,000, or 1 in 42) than among girls (5.3 per 1,000, or 1 in 189), a difference largely unchanged from previous studies.
ASD prevalence by ethnic or racial subgroup also did not change significantly over prior surveys, the investigators reported. However, lower estimates among black and Hispanic children could reflect “differences in awareness of ASD or access to specialty diagnostic services,” they wrote. Fewer black and Hispanic children in the survey had a comprehensive developmental evaluation by age 36 months (40% and 39%, respectively), compared with non-Hispanic white children (45%), which investigators called worrisome, as “early treatment might maximize the ability of children to function and participate in their community.”
Moreover, prevalence was seen increasing significantly over the previous survey in two states (New Jersey and Wisconsin), and decreasing significantly in one state (Missouri). Investigators suspected that variation in local health care systems’ ability to obtain comprehensive developmental evaluations might be a factor.
The wide range of ASD prevalence estimates, the investigators wrote, demands “caution in interpreting the similarity of overall estimated ASD prevalence between 2010 and 2012.”
The CDC funded the study and investigators disclosed no conflicts of interest.
FROM MMWR
Key clinical point: Rates of autism spectrum disorder in school-age children did not rise between 2010 and 2012, but investigators saw significant differences by region and evaluative approach, meaning it’s too early to say trends are stable.
Major finding: The prevalence of autism spectrum disorder in 8-year-old children in 2012 was 14.6 per 1,000 vs. 14.7 in 2010.
Data source: An ongoing CDC survey network covering about 350,000 8-year-old children in 11 states. Investigators reviewed developmental evaluations to determine eligibility for special education services and/or clinical developmental evaluations to determine prevalence of ASD in this population in 2012.
Disclosures: The CDC funded the study and investigators disclosed no conflicts of interest.
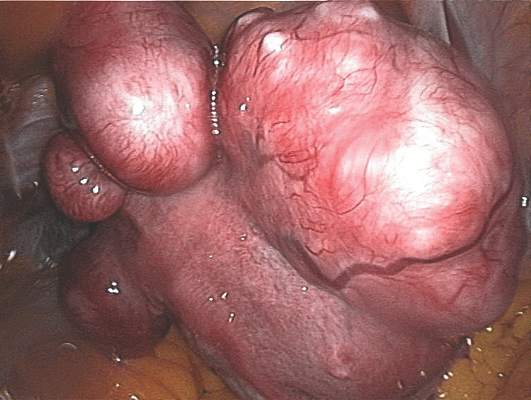
Fibroids, endometriosis linked to chemical exposures cost Europe $1.5 billion a year
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
The cost burden of uterine fibroids and endometriosis related to two types of endocrine-disrupting chemicals (EDCs) in Europe is about 1.4 billion euros a year, or more than $1.5 billion, according to an analysis published online March 22 in the Journal of Clinical Endocrinology & Metabolism.
Diphenyldichloroethene, or DDE, is an agricultural pesticide that has been linked to fibroids, while phthalates, used to soften plastics or deliver scent, are ubiquitous in consumer products and have been linked to endometriosis.
The true burden of female reproductive disorders linked to endocrine-disrupting chemicals is likely considerably higher than the study’s estimate reflects, says Dr. Leonardo Trasande of New York University Langone Medical Center, the lead investigator.
While Dr. Trasande and his colleagues limited the scope of their study to two reproductive tract abnormalities, others, including polycystic ovarian syndrome and fertility disorders, have increasingly been linked to EDCs. The investigators also limited their focus to the two chemicals for which the evidence was strong and for which the European Union is seeking guidance on regulating.
“We see this as a first step toward a more comprehensive investigation of the role of environmental chemicals and their impact on diseases that unfortunately are all too common in women,” Dr. Trasande said in an interview.
The investigators looked at levels of DDE exposures from cohorts of mothers from whom cord blood was drawn, while phthalate exposures were measured in urine from women who took part in a pan-European biomonitoring survey of mothers and children.
Incidence of fibroids (in women aged 15-54 years) and endometriosis (in women aged 20-44 years) was derived from large national cohorts. Per-patient treatment and lost-work costs were also drawn from national databases, based on 2010 figures. Excess risk of either disease per level of exposure was calculated based on previous findings. The investigators found that fibroids or endometriosis caused by chemical exposure accounted for between 20% and 39% of cases (J Clin Endocrinol Metab. 2016 Mar 22. doi: 10.1210/jc.2015-2873).
The European national health care systems offered the researchers the advantage of large, stable cohorts from which to draw data; a similar study would have been harder to carry out in the United States, Dr. Trasande noted.
Nonetheless, he said, the implications of the study apply broadly. “The greatest takeaway here is prevention related. The findings speak to the substantial health and economic burden of these chemicals both in Europe and other parts of the world.” Exposures are comparable between the United States and Europe, he said, meaning related disease burden and costs may be proportionally consistent. In the developing world, exposures are lower but increasing.
All the chemical exposures measured in Dr. Trasande and his colleagues’ study were of adult women, though much concern over EDCs relates to in utero or early-life exposures affecting adult outcomes.
“Without the data to compare exposure in early life and conditions that occur many years later, we had to rely upon associations that were closer in time,” he said. What’s needed now is “substantial and further investment in studies that leverage banked [early-life] specimens and can be associated with patients with a particular condition.”
The National Institutes of Health’s National Children’s Study was designed to do just this, measuring prenatal environmental exposures and conducting long-term follow-up in some 100,000 subjects. However, it was canceled in late 2014 due to recruitment concerns.
The planned ECHO (Environmental Influences on Child Health Outcomes) study, also under NIH, will attempt to measure long-term outcomes related to prenatal and early postnatal exposures, including through tissue banking. It will rely on existing birth cohorts instead.
Dr. Trasande and his colleagues’ study was funded by the Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation. Its authors disclosed no conflicts of interest.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Key clinical point: Between 20% and 39% of uterine fibroids and endometriosis cases in Europe are linked to two chemical exposures, and the associated costs exceed $1.5 billion annually.
Major finding: DDE-attributable fibroids and phthalate-attributable endometriosis cases were about 56,700 and 145,000, respectively, in 2010, with total combined economic and health care costs of about $1.5 billion.
Data source: Cohort biomarker data were used to assess European women’s exposures, and disease burden estimated from national health care databases.
Disclosures: The Endocrine Society, the John Merck Fund, the Broad Reach Foundation, and the Oak Foundation sponsored the study, whose authors disclosed no conflicts.
Acetaminophen ineffective against osteoarthritis pain
The widely used painkiller acetaminophen has little effect on osteoarthritic pain even at high doses, according to results from a new meta-analysis, while several other agents, including diclofenac, improve pain more robustly.
The study, published online March 17 in The Lancet (doi: 10.1016/S0140-6736(16)30002-2), reviewed results from 74 randomized trials enrolling nearly 60,000 patients with knee or hip osteoarthritis.
Patients were assigned different single-agent treatment regimens, comprising various dosages of seven nonsteroidal anti-inflammatory drugs (rofecoxib, lumiracoxib, etoricoxib, diclofenac, celecoxib, naproxen, and ibuprofen) or acetaminophen; in the included trials some treatments were compared head to head, and others to placebo.
First author Bruno R. da Costa, Ph.D., of the University of Bern (Switzerland) and his colleagues found to their surprise that acetaminophen had a nearly null effect on pain symptoms at doses ranging from under 2,000 mg a day to as much as 4,000 mg.
The study’s preestablished cutoff for clinically important pain reduction was an effect size of –0.37. While the most effective regimens in the study had effect sizes approaching –0.6, compared with placebo, acetaminophen’s effect size was only –0.17 across the doses studied.
Acetaminophen “is clinically ineffective and should not be recommended for the symptomatic treatment of osteoarthritis, irrespective of the dose,” the researchers concluded.
Diclofenac, meanwhile, had one of the greatest effect sizes at the maximum dose of 150 mg per day (–0.57), and etoricoxib 60 mg and rofecoxib 25 mg were comparably effective. All three agents at these maximum daily doses had 100% probability to reach the minimum clinically important difference established in the study when used to reduce osteoarthritic pain.
By comparison, maximum daily doses of ibuprofen (2,400 mg) and naproxen (1,000 mg) had 83% and 78% probability, respectively, of achieving clinically important reductions. Treatment effects increased with dosage, but reached statistical significance only for celecoxib, diclofenac, and naproxen.
“Although our findings suggest that some NSAIDs have a clinically relevant treatment effect on osteoarthritis pain,” the investigators wrote, their benefit has to be weighed against their potential harmful effects, which include cardiovascular risk associated with diclofenac and gastrointestinal complications linked to naproxen.
“Appropriate drug selection is a major challenge in patients with osteoarthritis, who are often elderly with polypharmacy. Our study will help to put the available safety data into perspective,” they wrote.
The agents were used short-term, reflecting real-life practice, with average follow-up in the study less than 3 months. However, trials with longer-term follow-up may be needed to compare effectiveness of regimens “on a continuous fixed-dose versus NSAIDs on an as-needed basis,” the researchers acknowledged.
The Swiss National Science Foundation and the Arco Foundation of Switzerland sponsored the study. One investigator disclosed institutional research support from AstraZeneca, Biotronik, Biosensors International, Eli Lilly, and the Medicines Company, while another is currently employed by Novartis and holds shares in Cogitars.
In this network meta-analysis, the most remarkable result is that acetaminophen does not seem to confer any demonstrable effect or benefit in osteoarthritis, at any dose. This finding is not entirely unexpected. It has been on the market for as long as most of us remember. Its efficacy has never been properly established or quantified in chronic diseases, and is probably not as great as many would believe. Its safety is also questioned, not just in overdose. Is recommending it as the universal first-line analgesic in osteoarthritis still tenable? Many patients could be suffering needlessly because of perceived NSAIDs risks and acetaminophen benefits (which might not be real). Perhaps researchers need to reassess both these perceptions (or misconceptions) and the use of other analgesic options that have been discarded over time.
These comments are taken from an editorial by Dr. Nicholas Moore and associates from the department of pharmacology at the University of Bordeaux (France) that accompanied the report by Dr. da Costa and colleagues (Lancet. 2016 Mar 17. doi: 10.1016/S0140-6736(15)01170-8). Dr. Moore disclosed past research support from Boots, Reckitt-Benckiser, Novartis, Pfizer, Roche, Rhone Poulenc, Sanofi, and Helsinn.
In this network meta-analysis, the most remarkable result is that acetaminophen does not seem to confer any demonstrable effect or benefit in osteoarthritis, at any dose. This finding is not entirely unexpected. It has been on the market for as long as most of us remember. Its efficacy has never been properly established or quantified in chronic diseases, and is probably not as great as many would believe. Its safety is also questioned, not just in overdose. Is recommending it as the universal first-line analgesic in osteoarthritis still tenable? Many patients could be suffering needlessly because of perceived NSAIDs risks and acetaminophen benefits (which might not be real). Perhaps researchers need to reassess both these perceptions (or misconceptions) and the use of other analgesic options that have been discarded over time.
These comments are taken from an editorial by Dr. Nicholas Moore and associates from the department of pharmacology at the University of Bordeaux (France) that accompanied the report by Dr. da Costa and colleagues (Lancet. 2016 Mar 17. doi: 10.1016/S0140-6736(15)01170-8). Dr. Moore disclosed past research support from Boots, Reckitt-Benckiser, Novartis, Pfizer, Roche, Rhone Poulenc, Sanofi, and Helsinn.
In this network meta-analysis, the most remarkable result is that acetaminophen does not seem to confer any demonstrable effect or benefit in osteoarthritis, at any dose. This finding is not entirely unexpected. It has been on the market for as long as most of us remember. Its efficacy has never been properly established or quantified in chronic diseases, and is probably not as great as many would believe. Its safety is also questioned, not just in overdose. Is recommending it as the universal first-line analgesic in osteoarthritis still tenable? Many patients could be suffering needlessly because of perceived NSAIDs risks and acetaminophen benefits (which might not be real). Perhaps researchers need to reassess both these perceptions (or misconceptions) and the use of other analgesic options that have been discarded over time.
These comments are taken from an editorial by Dr. Nicholas Moore and associates from the department of pharmacology at the University of Bordeaux (France) that accompanied the report by Dr. da Costa and colleagues (Lancet. 2016 Mar 17. doi: 10.1016/S0140-6736(15)01170-8). Dr. Moore disclosed past research support from Boots, Reckitt-Benckiser, Novartis, Pfizer, Roche, Rhone Poulenc, Sanofi, and Helsinn.
The widely used painkiller acetaminophen has little effect on osteoarthritic pain even at high doses, according to results from a new meta-analysis, while several other agents, including diclofenac, improve pain more robustly.
The study, published online March 17 in The Lancet (doi: 10.1016/S0140-6736(16)30002-2), reviewed results from 74 randomized trials enrolling nearly 60,000 patients with knee or hip osteoarthritis.
Patients were assigned different single-agent treatment regimens, comprising various dosages of seven nonsteroidal anti-inflammatory drugs (rofecoxib, lumiracoxib, etoricoxib, diclofenac, celecoxib, naproxen, and ibuprofen) or acetaminophen; in the included trials some treatments were compared head to head, and others to placebo.
First author Bruno R. da Costa, Ph.D., of the University of Bern (Switzerland) and his colleagues found to their surprise that acetaminophen had a nearly null effect on pain symptoms at doses ranging from under 2,000 mg a day to as much as 4,000 mg.
The study’s preestablished cutoff for clinically important pain reduction was an effect size of –0.37. While the most effective regimens in the study had effect sizes approaching –0.6, compared with placebo, acetaminophen’s effect size was only –0.17 across the doses studied.
Acetaminophen “is clinically ineffective and should not be recommended for the symptomatic treatment of osteoarthritis, irrespective of the dose,” the researchers concluded.
Diclofenac, meanwhile, had one of the greatest effect sizes at the maximum dose of 150 mg per day (–0.57), and etoricoxib 60 mg and rofecoxib 25 mg were comparably effective. All three agents at these maximum daily doses had 100% probability to reach the minimum clinically important difference established in the study when used to reduce osteoarthritic pain.
By comparison, maximum daily doses of ibuprofen (2,400 mg) and naproxen (1,000 mg) had 83% and 78% probability, respectively, of achieving clinically important reductions. Treatment effects increased with dosage, but reached statistical significance only for celecoxib, diclofenac, and naproxen.
“Although our findings suggest that some NSAIDs have a clinically relevant treatment effect on osteoarthritis pain,” the investigators wrote, their benefit has to be weighed against their potential harmful effects, which include cardiovascular risk associated with diclofenac and gastrointestinal complications linked to naproxen.
“Appropriate drug selection is a major challenge in patients with osteoarthritis, who are often elderly with polypharmacy. Our study will help to put the available safety data into perspective,” they wrote.
The agents were used short-term, reflecting real-life practice, with average follow-up in the study less than 3 months. However, trials with longer-term follow-up may be needed to compare effectiveness of regimens “on a continuous fixed-dose versus NSAIDs on an as-needed basis,” the researchers acknowledged.
The Swiss National Science Foundation and the Arco Foundation of Switzerland sponsored the study. One investigator disclosed institutional research support from AstraZeneca, Biotronik, Biosensors International, Eli Lilly, and the Medicines Company, while another is currently employed by Novartis and holds shares in Cogitars.
The widely used painkiller acetaminophen has little effect on osteoarthritic pain even at high doses, according to results from a new meta-analysis, while several other agents, including diclofenac, improve pain more robustly.
The study, published online March 17 in The Lancet (doi: 10.1016/S0140-6736(16)30002-2), reviewed results from 74 randomized trials enrolling nearly 60,000 patients with knee or hip osteoarthritis.
Patients were assigned different single-agent treatment regimens, comprising various dosages of seven nonsteroidal anti-inflammatory drugs (rofecoxib, lumiracoxib, etoricoxib, diclofenac, celecoxib, naproxen, and ibuprofen) or acetaminophen; in the included trials some treatments were compared head to head, and others to placebo.
First author Bruno R. da Costa, Ph.D., of the University of Bern (Switzerland) and his colleagues found to their surprise that acetaminophen had a nearly null effect on pain symptoms at doses ranging from under 2,000 mg a day to as much as 4,000 mg.
The study’s preestablished cutoff for clinically important pain reduction was an effect size of –0.37. While the most effective regimens in the study had effect sizes approaching –0.6, compared with placebo, acetaminophen’s effect size was only –0.17 across the doses studied.
Acetaminophen “is clinically ineffective and should not be recommended for the symptomatic treatment of osteoarthritis, irrespective of the dose,” the researchers concluded.
Diclofenac, meanwhile, had one of the greatest effect sizes at the maximum dose of 150 mg per day (–0.57), and etoricoxib 60 mg and rofecoxib 25 mg were comparably effective. All three agents at these maximum daily doses had 100% probability to reach the minimum clinically important difference established in the study when used to reduce osteoarthritic pain.
By comparison, maximum daily doses of ibuprofen (2,400 mg) and naproxen (1,000 mg) had 83% and 78% probability, respectively, of achieving clinically important reductions. Treatment effects increased with dosage, but reached statistical significance only for celecoxib, diclofenac, and naproxen.
“Although our findings suggest that some NSAIDs have a clinically relevant treatment effect on osteoarthritis pain,” the investigators wrote, their benefit has to be weighed against their potential harmful effects, which include cardiovascular risk associated with diclofenac and gastrointestinal complications linked to naproxen.
“Appropriate drug selection is a major challenge in patients with osteoarthritis, who are often elderly with polypharmacy. Our study will help to put the available safety data into perspective,” they wrote.
The agents were used short-term, reflecting real-life practice, with average follow-up in the study less than 3 months. However, trials with longer-term follow-up may be needed to compare effectiveness of regimens “on a continuous fixed-dose versus NSAIDs on an as-needed basis,” the researchers acknowledged.
The Swiss National Science Foundation and the Arco Foundation of Switzerland sponsored the study. One investigator disclosed institutional research support from AstraZeneca, Biotronik, Biosensors International, Eli Lilly, and the Medicines Company, while another is currently employed by Novartis and holds shares in Cogitars.
FROM THE LANCET
Key clinical point:Acetaminophen, even at high doses, is largely ineffective at reducing pain in knee or hip osteoarthritis.
Major finding: Effect size for acetaminophen was –0.17 vs. placebo (not reaching clinical threshold of –0.37), compared with –0.57 for the maximum dose of diclofenac.
Data source: A meta-analysis of 74 randomized trials evaluating 23 treatment regimens including seven NSAIDS and acetaminophen in 58,566 patients
Disclosures: The Swiss National Science Foundation and the Arco Foundation of Switzerland sponsored the study. Two investigators disclosed industry relationships.
Antenatal steroids help neonates born before 24 weeks
A course of antenatal corticosteroids can reduce mortality by about half in neonates born before 24 weeks, according to findings from a recent meta-analysis.
Previous studies have established that antenatal corticosteroids, used to hasten development of the lungs and therefore improve chances of survival, are helpful when given to women at high risk of preterm delivery between 24 and 34 weeks of gestation. However, little evidence has been available to recommend their use when risk of preterm delivery became evident before 24 weeks.
In the current meta-analysis, Christina Park, of McMaster University in Hamilton, Ontario, and her colleagues, reviewed data from observational studies published between 2002 and 2011 that included more than 3,600 neonates born before 24 weeks (Obstet Gynecol. 2016 Mar 7;127:715-25).
The researchers found that the odds of in-hospital mortality – the primary outcome of the study – were 52% less in those neonates that had been treated with antenatal corticosteroids (58.1% compared with 71.8%; adjusted odds ratio, 0.48), a difference that reached statistical significance. They graded the evidence in these studies as being of “moderate” quality.
A subgroup analysis comparing outcomes for neonates at 22 and 23 weeks of gestation found no difference in terms of in-hospital mortality.
Secondary outcomes such as respiratory distress syndrome and other diseases associated with preterm birth did not reach statistical significance. This finding was surprising, the researchers noted, because they had expected a reduction in morbidities would accompany lowered mortality. However, a misdiagnosis of respiratory distress syndrome may have occurred in the included studies, they wrote.
Antenatal corticosteroids may help reduce mortality in neonates delivered before 24 weeks and clinicians should consider them for women at this gestational point who would choose postnatal resuscitation. “Family counseling and planning of services are essential for these births,” they wrote, “because advances in care have opened the possibility of survival at progressively early gestations.”
Two of the researchers reported receiving grants from the Canadian Institutes of Health. They reported having no other financial disclosures.
A course of antenatal corticosteroids can reduce mortality by about half in neonates born before 24 weeks, according to findings from a recent meta-analysis.
Previous studies have established that antenatal corticosteroids, used to hasten development of the lungs and therefore improve chances of survival, are helpful when given to women at high risk of preterm delivery between 24 and 34 weeks of gestation. However, little evidence has been available to recommend their use when risk of preterm delivery became evident before 24 weeks.
In the current meta-analysis, Christina Park, of McMaster University in Hamilton, Ontario, and her colleagues, reviewed data from observational studies published between 2002 and 2011 that included more than 3,600 neonates born before 24 weeks (Obstet Gynecol. 2016 Mar 7;127:715-25).
The researchers found that the odds of in-hospital mortality – the primary outcome of the study – were 52% less in those neonates that had been treated with antenatal corticosteroids (58.1% compared with 71.8%; adjusted odds ratio, 0.48), a difference that reached statistical significance. They graded the evidence in these studies as being of “moderate” quality.
A subgroup analysis comparing outcomes for neonates at 22 and 23 weeks of gestation found no difference in terms of in-hospital mortality.
Secondary outcomes such as respiratory distress syndrome and other diseases associated with preterm birth did not reach statistical significance. This finding was surprising, the researchers noted, because they had expected a reduction in morbidities would accompany lowered mortality. However, a misdiagnosis of respiratory distress syndrome may have occurred in the included studies, they wrote.
Antenatal corticosteroids may help reduce mortality in neonates delivered before 24 weeks and clinicians should consider them for women at this gestational point who would choose postnatal resuscitation. “Family counseling and planning of services are essential for these births,” they wrote, “because advances in care have opened the possibility of survival at progressively early gestations.”
Two of the researchers reported receiving grants from the Canadian Institutes of Health. They reported having no other financial disclosures.
A course of antenatal corticosteroids can reduce mortality by about half in neonates born before 24 weeks, according to findings from a recent meta-analysis.
Previous studies have established that antenatal corticosteroids, used to hasten development of the lungs and therefore improve chances of survival, are helpful when given to women at high risk of preterm delivery between 24 and 34 weeks of gestation. However, little evidence has been available to recommend their use when risk of preterm delivery became evident before 24 weeks.
In the current meta-analysis, Christina Park, of McMaster University in Hamilton, Ontario, and her colleagues, reviewed data from observational studies published between 2002 and 2011 that included more than 3,600 neonates born before 24 weeks (Obstet Gynecol. 2016 Mar 7;127:715-25).
The researchers found that the odds of in-hospital mortality – the primary outcome of the study – were 52% less in those neonates that had been treated with antenatal corticosteroids (58.1% compared with 71.8%; adjusted odds ratio, 0.48), a difference that reached statistical significance. They graded the evidence in these studies as being of “moderate” quality.
A subgroup analysis comparing outcomes for neonates at 22 and 23 weeks of gestation found no difference in terms of in-hospital mortality.
Secondary outcomes such as respiratory distress syndrome and other diseases associated with preterm birth did not reach statistical significance. This finding was surprising, the researchers noted, because they had expected a reduction in morbidities would accompany lowered mortality. However, a misdiagnosis of respiratory distress syndrome may have occurred in the included studies, they wrote.
Antenatal corticosteroids may help reduce mortality in neonates delivered before 24 weeks and clinicians should consider them for women at this gestational point who would choose postnatal resuscitation. “Family counseling and planning of services are essential for these births,” they wrote, “because advances in care have opened the possibility of survival at progressively early gestations.”
Two of the researchers reported receiving grants from the Canadian Institutes of Health. They reported having no other financial disclosures.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Antenatal corticosteroid treatment may improve survival odds for neonates born before 24 weeks.
Major finding: In-hospital mortality was reduced by 52% among neonates delivered before 24 weeks who received antenatal steroids and active intense treatment.
Data source: A meta-analysis of observational studies that included more than 3,600 infants born before 24 weeks with and without antenatal steroids.
Disclosures: Two of the researchers reported receiving grants from the Canadian Institutes of Health. They reported having no other financial disclosures.
Enlarged uterus helps predict morcellation in vaginal hysterectomy
Women undergoing vaginal hysterectomy are more likely to receive cold-knife morcellation if they have an enlarged uterus, leiomyoma, or no prolapse, according to new research.
Electromechanical morcellation, a technique used during laparoscopic hysterectomy to cut the uterus into small pieces for removal, has come under heavy scrutiny in recent years due to risk of disseminating undiagnosed uterine cancers. However, morcellation can also be performed manually during a vaginal hysterectomy. While current recommendations stress caution for all types of morcellation, the risks and prognostic factors for cold-knife morcellation are poorly understood.
In a retrospective cohort study, Dr. Megan Wasson, of the Mayo Clinic Arizona in Phoenix, and her colleagues examined a cohort of 743 women who underwent hysterectomy with either intact uterine removal (383 women) or with cold-knife morcellation (360 women).
Dr. Wasson and her colleagues found that women were significantly more likely to undergo morcellation, compared with intact uterine removal if they had larger uterine weight (adjusted odds ratio, 7.25; P less than .001), lack of prolapse (aOR, 3.87; P less than .001), or the presence of leiomyoma (aOR, 2.77, P = .035).
Women with prior vaginal delivery were significantly less likely to receive morcellation (aOR, 0.79, P = .005).
Younger age, lower parity, and nonwhite race were also associated with a higher likelihood of undergoing morcellation (Obstet Gynecol. 2016;127:752–7).
“This study identified prognostic factors associated with an increased likelihood of morcellation required at the time of vaginal hysterectomy,” Dr. Wasson and her colleagues wrote, stressing that higher uterine weight was the strongest predictor. “The ability to preoperatively predict uterine weight and size is essential for surgical planning given that a large uterus is most predictive of needing morcellation at the time of vaginal hysterectomy.”
The findings, they wrote, may help clinicians identify those patients who need additional counseling about the potential risks of morcellation, as well as patients who may need to avoid vaginal hysterectomy to negate the risks of morcellation.
The investigators identified limitations to their study, including that the majority of the women (88%) were white, and that candidates for vaginal hysterectomy were carefully chosen by expert surgeons, leading to likely selection bias.
The investigators reported having no financial disclosures.
Women undergoing vaginal hysterectomy are more likely to receive cold-knife morcellation if they have an enlarged uterus, leiomyoma, or no prolapse, according to new research.
Electromechanical morcellation, a technique used during laparoscopic hysterectomy to cut the uterus into small pieces for removal, has come under heavy scrutiny in recent years due to risk of disseminating undiagnosed uterine cancers. However, morcellation can also be performed manually during a vaginal hysterectomy. While current recommendations stress caution for all types of morcellation, the risks and prognostic factors for cold-knife morcellation are poorly understood.
In a retrospective cohort study, Dr. Megan Wasson, of the Mayo Clinic Arizona in Phoenix, and her colleagues examined a cohort of 743 women who underwent hysterectomy with either intact uterine removal (383 women) or with cold-knife morcellation (360 women).
Dr. Wasson and her colleagues found that women were significantly more likely to undergo morcellation, compared with intact uterine removal if they had larger uterine weight (adjusted odds ratio, 7.25; P less than .001), lack of prolapse (aOR, 3.87; P less than .001), or the presence of leiomyoma (aOR, 2.77, P = .035).
Women with prior vaginal delivery were significantly less likely to receive morcellation (aOR, 0.79, P = .005).
Younger age, lower parity, and nonwhite race were also associated with a higher likelihood of undergoing morcellation (Obstet Gynecol. 2016;127:752–7).
“This study identified prognostic factors associated with an increased likelihood of morcellation required at the time of vaginal hysterectomy,” Dr. Wasson and her colleagues wrote, stressing that higher uterine weight was the strongest predictor. “The ability to preoperatively predict uterine weight and size is essential for surgical planning given that a large uterus is most predictive of needing morcellation at the time of vaginal hysterectomy.”
The findings, they wrote, may help clinicians identify those patients who need additional counseling about the potential risks of morcellation, as well as patients who may need to avoid vaginal hysterectomy to negate the risks of morcellation.
The investigators identified limitations to their study, including that the majority of the women (88%) were white, and that candidates for vaginal hysterectomy were carefully chosen by expert surgeons, leading to likely selection bias.
The investigators reported having no financial disclosures.
Women undergoing vaginal hysterectomy are more likely to receive cold-knife morcellation if they have an enlarged uterus, leiomyoma, or no prolapse, according to new research.
Electromechanical morcellation, a technique used during laparoscopic hysterectomy to cut the uterus into small pieces for removal, has come under heavy scrutiny in recent years due to risk of disseminating undiagnosed uterine cancers. However, morcellation can also be performed manually during a vaginal hysterectomy. While current recommendations stress caution for all types of morcellation, the risks and prognostic factors for cold-knife morcellation are poorly understood.
In a retrospective cohort study, Dr. Megan Wasson, of the Mayo Clinic Arizona in Phoenix, and her colleagues examined a cohort of 743 women who underwent hysterectomy with either intact uterine removal (383 women) or with cold-knife morcellation (360 women).
Dr. Wasson and her colleagues found that women were significantly more likely to undergo morcellation, compared with intact uterine removal if they had larger uterine weight (adjusted odds ratio, 7.25; P less than .001), lack of prolapse (aOR, 3.87; P less than .001), or the presence of leiomyoma (aOR, 2.77, P = .035).
Women with prior vaginal delivery were significantly less likely to receive morcellation (aOR, 0.79, P = .005).
Younger age, lower parity, and nonwhite race were also associated with a higher likelihood of undergoing morcellation (Obstet Gynecol. 2016;127:752–7).
“This study identified prognostic factors associated with an increased likelihood of morcellation required at the time of vaginal hysterectomy,” Dr. Wasson and her colleagues wrote, stressing that higher uterine weight was the strongest predictor. “The ability to preoperatively predict uterine weight and size is essential for surgical planning given that a large uterus is most predictive of needing morcellation at the time of vaginal hysterectomy.”
The findings, they wrote, may help clinicians identify those patients who need additional counseling about the potential risks of morcellation, as well as patients who may need to avoid vaginal hysterectomy to negate the risks of morcellation.
The investigators identified limitations to their study, including that the majority of the women (88%) were white, and that candidates for vaginal hysterectomy were carefully chosen by expert surgeons, leading to likely selection bias.
The investigators reported having no financial disclosures.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Women with a larger-than-normal uterus are likelier to undergo cold-knife morcellation versus intact uterine removal during a vaginal hysterectomy.
Major finding: Larger-than-normal uterine weight was associated with increased odds of morcellation (aOR, 7.25; P less than .001).
Data source: A retrospective cohort study of 743 women selected for vaginal hysterectomy.
Disclosures: The investigators reported having no financial disclosures.
‘Vaginal seeding’ practice comes with risks
Newborns delivered by cesarean section have different microbial colonization patterns than babies delivered vaginally, and several studies have suggested that their immunologic and metabolic development may be disadvantaged as a result.
Preliminary results from a recent proof-of concept study in 18 babies, published online in Nature Medicine, showed that transferring vaginal fluid to newborns shortly after delivery by C-section resulted in microbiome profiles resembling those of babies delivered vaginally (doi: 10.1038/nm.4039).
But it is still unknown whether promoting colonization in this way approximates the microbial transfer that occurs during labor, or whether it affects later health outcomes in these infants. The researchers, led by Maria G. Dominguez-Bello, Ph.D., of New York University in New York City, stressed in their study that considerably more time and research are needed to answer these questions.
Still, as the practice gains more attention in the press and in parenting blogs, patients are asking clinicians to perform vaginal fluid transfer or “vaginal seeding” following C-sections.
BMJ highlights concerns
A Feb. 23 editorial in the BMJ stressed that clinicians not recommend vaginal seeding, because of insufficient evidence and because of the potential for unrecognized infections to be transmitted from mother to newborn (BMJ. 2016;352:i227. doi: 10.1136/bmj.i227).
“It might seem reasonable to perform this simple and cheap procedure, even without clear evidence of benefit, but only if we can be sure that it is safe,” wrote a group of clinicians led by Dr. Aubrey J. Cunnington of Imperial College London. For now, they wrote, breastfeeding and avoidance of unnecessary antibiotics should be stressed to promote early microbiome development.
But even if clinicians and hospitals refuse to perform seeding – which can be done by placing gauze in the vagina prior to delivery and then using it to swab the newborn – “mothers can easily do it themselves,” Dr. Cunnington and colleagues said in their editorial.
The potential demand for vaginal seeding raises a host of issues, according to three U.S.-based ob.gyns., all of whom said they agree with the caution expressed in the BMJ editorial, but have varying approaches to how to advise their patients.
“From a clinician’s point of view, I think it’s really important to not wait for a woman to say, ‘Should I do this?’ but instead for doctors to proactively say, ‘You may have read about this and we don’t recommend it,’ ” Dr. Lauren Streicher,of Northwestern University, Chicago, said in an interview.
“The real concern is that since you don’t need a doctor to do it, mothers are going to take it upon themselves,” Dr. Streicher said, particularly as the practice gains more attention in the lay press, or if vaginal seeding gets endorsed or promoted by someone famous, something she said is all but inevitable.
Patients need to be aware that there are risks inherent in either mode of delivery, Dr. Streicher noted, and vaginal delivery comes with the risk of transmitting undiagnosed group B streptococcus, chlamydia, gonorrhea, or herpes viruses.
Dr. Layne Kumetz, an ob.gyn. in Beverly Hills, Calif., said in an interview that her patients tend to be educated and “early adopters” when it comes to medical trends. She said she has already received patient queries about vaginal seeding and counseled patients on the potential risks. As a mother herself, she has also noticed active discussion about vaginal seeding on parenting blogs.
But Dr. Kumetz said that pending much more study, “routine practicing of the procedure is simply not appropriate.”
She added, “The long term implications about whether this will alter the health of newborns have not been determined, whether this is a safe procedure has not been determined, [and] what the proper protocol should be in terms of women wishing to have this procedure performed has not been determined.”
The women in the pilot study who had used vaginal seeding, Dr. Kumetz noted, had been carefully selected and screened, had been treated with antibiotics prior to their C-sections, and were group B strep negative. In the general population, meanwhile, nearly a third of patients are group B positive, she said.
Dr. Kumetz said she would not bring up the seeding with patients who don’t ask, nor was it something that the hospitals she’s working with are willing to perform.
Emphasize alternatives
Dr. Eliza Bennett of the University of Wisconsin–Madison said that requests for vaginal seeding had become more frequent, even months before the pilot study was published. The procedure is allowed at her hospital, but is available only by request.
Dr. Bennett stressed that she, like Dr. Kumetz, does not discuss the practice with patients unless they bring it up themselves. For women who do request it, nurses have been trained in the practice, she said, and “we have established really strict exclusion criteria,” including repeat screening for group B strep, HIV, genital herpes, and sexually transmitted infections during pregnancy.
Dr. Bennett said she would much rather emphasize the safer, evidence-based practices already in place at her hospital to promote microbiome development in C-section newborns. These include delaying the first bath until after 12 hours, placing babies directly on mothers’ skin in the operating room in the first minutes post delivery, and “offering the ability for moms to breastfeed right in the OR,” she said.
Like Dr. Streicher and Dr. Kumetz, Dr. Bennett said she’s not expecting to see data resolving the questions about the risks and benefits of vaginal seeding anytime soon.
“Instead of focusing on vaginal seeding, we should continue to focus our efforts on decreasing cesarean delivery rates and ensuring and encouraging appropriate candidates to have the opportunity to have a trial of labor after cesarean delivery,” she said.
Avoiding C-section, she added, “confers multiple maternal and fetal benefits beyond the microbiome.”
Newborns delivered by cesarean section have different microbial colonization patterns than babies delivered vaginally, and several studies have suggested that their immunologic and metabolic development may be disadvantaged as a result.
Preliminary results from a recent proof-of concept study in 18 babies, published online in Nature Medicine, showed that transferring vaginal fluid to newborns shortly after delivery by C-section resulted in microbiome profiles resembling those of babies delivered vaginally (doi: 10.1038/nm.4039).
But it is still unknown whether promoting colonization in this way approximates the microbial transfer that occurs during labor, or whether it affects later health outcomes in these infants. The researchers, led by Maria G. Dominguez-Bello, Ph.D., of New York University in New York City, stressed in their study that considerably more time and research are needed to answer these questions.
Still, as the practice gains more attention in the press and in parenting blogs, patients are asking clinicians to perform vaginal fluid transfer or “vaginal seeding” following C-sections.
BMJ highlights concerns
A Feb. 23 editorial in the BMJ stressed that clinicians not recommend vaginal seeding, because of insufficient evidence and because of the potential for unrecognized infections to be transmitted from mother to newborn (BMJ. 2016;352:i227. doi: 10.1136/bmj.i227).
“It might seem reasonable to perform this simple and cheap procedure, even without clear evidence of benefit, but only if we can be sure that it is safe,” wrote a group of clinicians led by Dr. Aubrey J. Cunnington of Imperial College London. For now, they wrote, breastfeeding and avoidance of unnecessary antibiotics should be stressed to promote early microbiome development.
But even if clinicians and hospitals refuse to perform seeding – which can be done by placing gauze in the vagina prior to delivery and then using it to swab the newborn – “mothers can easily do it themselves,” Dr. Cunnington and colleagues said in their editorial.
The potential demand for vaginal seeding raises a host of issues, according to three U.S.-based ob.gyns., all of whom said they agree with the caution expressed in the BMJ editorial, but have varying approaches to how to advise their patients.
“From a clinician’s point of view, I think it’s really important to not wait for a woman to say, ‘Should I do this?’ but instead for doctors to proactively say, ‘You may have read about this and we don’t recommend it,’ ” Dr. Lauren Streicher,of Northwestern University, Chicago, said in an interview.
“The real concern is that since you don’t need a doctor to do it, mothers are going to take it upon themselves,” Dr. Streicher said, particularly as the practice gains more attention in the lay press, or if vaginal seeding gets endorsed or promoted by someone famous, something she said is all but inevitable.
Patients need to be aware that there are risks inherent in either mode of delivery, Dr. Streicher noted, and vaginal delivery comes with the risk of transmitting undiagnosed group B streptococcus, chlamydia, gonorrhea, or herpes viruses.
Dr. Layne Kumetz, an ob.gyn. in Beverly Hills, Calif., said in an interview that her patients tend to be educated and “early adopters” when it comes to medical trends. She said she has already received patient queries about vaginal seeding and counseled patients on the potential risks. As a mother herself, she has also noticed active discussion about vaginal seeding on parenting blogs.
But Dr. Kumetz said that pending much more study, “routine practicing of the procedure is simply not appropriate.”
She added, “The long term implications about whether this will alter the health of newborns have not been determined, whether this is a safe procedure has not been determined, [and] what the proper protocol should be in terms of women wishing to have this procedure performed has not been determined.”
The women in the pilot study who had used vaginal seeding, Dr. Kumetz noted, had been carefully selected and screened, had been treated with antibiotics prior to their C-sections, and were group B strep negative. In the general population, meanwhile, nearly a third of patients are group B positive, she said.
Dr. Kumetz said she would not bring up the seeding with patients who don’t ask, nor was it something that the hospitals she’s working with are willing to perform.
Emphasize alternatives
Dr. Eliza Bennett of the University of Wisconsin–Madison said that requests for vaginal seeding had become more frequent, even months before the pilot study was published. The procedure is allowed at her hospital, but is available only by request.
Dr. Bennett stressed that she, like Dr. Kumetz, does not discuss the practice with patients unless they bring it up themselves. For women who do request it, nurses have been trained in the practice, she said, and “we have established really strict exclusion criteria,” including repeat screening for group B strep, HIV, genital herpes, and sexually transmitted infections during pregnancy.
Dr. Bennett said she would much rather emphasize the safer, evidence-based practices already in place at her hospital to promote microbiome development in C-section newborns. These include delaying the first bath until after 12 hours, placing babies directly on mothers’ skin in the operating room in the first minutes post delivery, and “offering the ability for moms to breastfeed right in the OR,” she said.
Like Dr. Streicher and Dr. Kumetz, Dr. Bennett said she’s not expecting to see data resolving the questions about the risks and benefits of vaginal seeding anytime soon.
“Instead of focusing on vaginal seeding, we should continue to focus our efforts on decreasing cesarean delivery rates and ensuring and encouraging appropriate candidates to have the opportunity to have a trial of labor after cesarean delivery,” she said.
Avoiding C-section, she added, “confers multiple maternal and fetal benefits beyond the microbiome.”
Newborns delivered by cesarean section have different microbial colonization patterns than babies delivered vaginally, and several studies have suggested that their immunologic and metabolic development may be disadvantaged as a result.
Preliminary results from a recent proof-of concept study in 18 babies, published online in Nature Medicine, showed that transferring vaginal fluid to newborns shortly after delivery by C-section resulted in microbiome profiles resembling those of babies delivered vaginally (doi: 10.1038/nm.4039).
But it is still unknown whether promoting colonization in this way approximates the microbial transfer that occurs during labor, or whether it affects later health outcomes in these infants. The researchers, led by Maria G. Dominguez-Bello, Ph.D., of New York University in New York City, stressed in their study that considerably more time and research are needed to answer these questions.
Still, as the practice gains more attention in the press and in parenting blogs, patients are asking clinicians to perform vaginal fluid transfer or “vaginal seeding” following C-sections.
BMJ highlights concerns
A Feb. 23 editorial in the BMJ stressed that clinicians not recommend vaginal seeding, because of insufficient evidence and because of the potential for unrecognized infections to be transmitted from mother to newborn (BMJ. 2016;352:i227. doi: 10.1136/bmj.i227).
“It might seem reasonable to perform this simple and cheap procedure, even without clear evidence of benefit, but only if we can be sure that it is safe,” wrote a group of clinicians led by Dr. Aubrey J. Cunnington of Imperial College London. For now, they wrote, breastfeeding and avoidance of unnecessary antibiotics should be stressed to promote early microbiome development.
But even if clinicians and hospitals refuse to perform seeding – which can be done by placing gauze in the vagina prior to delivery and then using it to swab the newborn – “mothers can easily do it themselves,” Dr. Cunnington and colleagues said in their editorial.
The potential demand for vaginal seeding raises a host of issues, according to three U.S.-based ob.gyns., all of whom said they agree with the caution expressed in the BMJ editorial, but have varying approaches to how to advise their patients.
“From a clinician’s point of view, I think it’s really important to not wait for a woman to say, ‘Should I do this?’ but instead for doctors to proactively say, ‘You may have read about this and we don’t recommend it,’ ” Dr. Lauren Streicher,of Northwestern University, Chicago, said in an interview.
“The real concern is that since you don’t need a doctor to do it, mothers are going to take it upon themselves,” Dr. Streicher said, particularly as the practice gains more attention in the lay press, or if vaginal seeding gets endorsed or promoted by someone famous, something she said is all but inevitable.
Patients need to be aware that there are risks inherent in either mode of delivery, Dr. Streicher noted, and vaginal delivery comes with the risk of transmitting undiagnosed group B streptococcus, chlamydia, gonorrhea, or herpes viruses.
Dr. Layne Kumetz, an ob.gyn. in Beverly Hills, Calif., said in an interview that her patients tend to be educated and “early adopters” when it comes to medical trends. She said she has already received patient queries about vaginal seeding and counseled patients on the potential risks. As a mother herself, she has also noticed active discussion about vaginal seeding on parenting blogs.
But Dr. Kumetz said that pending much more study, “routine practicing of the procedure is simply not appropriate.”
She added, “The long term implications about whether this will alter the health of newborns have not been determined, whether this is a safe procedure has not been determined, [and] what the proper protocol should be in terms of women wishing to have this procedure performed has not been determined.”
The women in the pilot study who had used vaginal seeding, Dr. Kumetz noted, had been carefully selected and screened, had been treated with antibiotics prior to their C-sections, and were group B strep negative. In the general population, meanwhile, nearly a third of patients are group B positive, she said.
Dr. Kumetz said she would not bring up the seeding with patients who don’t ask, nor was it something that the hospitals she’s working with are willing to perform.
Emphasize alternatives
Dr. Eliza Bennett of the University of Wisconsin–Madison said that requests for vaginal seeding had become more frequent, even months before the pilot study was published. The procedure is allowed at her hospital, but is available only by request.
Dr. Bennett stressed that she, like Dr. Kumetz, does not discuss the practice with patients unless they bring it up themselves. For women who do request it, nurses have been trained in the practice, she said, and “we have established really strict exclusion criteria,” including repeat screening for group B strep, HIV, genital herpes, and sexually transmitted infections during pregnancy.
Dr. Bennett said she would much rather emphasize the safer, evidence-based practices already in place at her hospital to promote microbiome development in C-section newborns. These include delaying the first bath until after 12 hours, placing babies directly on mothers’ skin in the operating room in the first minutes post delivery, and “offering the ability for moms to breastfeed right in the OR,” she said.
Like Dr. Streicher and Dr. Kumetz, Dr. Bennett said she’s not expecting to see data resolving the questions about the risks and benefits of vaginal seeding anytime soon.
“Instead of focusing on vaginal seeding, we should continue to focus our efforts on decreasing cesarean delivery rates and ensuring and encouraging appropriate candidates to have the opportunity to have a trial of labor after cesarean delivery,” she said.
Avoiding C-section, she added, “confers multiple maternal and fetal benefits beyond the microbiome.”
Stronger Evidence Links Zika to Guillain-Barré Syndrome
Serological evidence from French Polynesia links an outbreak of Zika virus to a spike in cases of Guillain-Barré syndrome seen there in 2013-2014.
The research, published online Feb. 29 in The Lancet, is the first to use a case-control design to demonstrate that Zika, a mosquito-borne flavivirus, is associated with Guillain-Barré syndrome (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
Guillain-Barré syndrome (GBS) is an immune-mediated flaccid paralysis that can follow viral or bacterial infections. Most patients with GBS recover with intensive care in hospitals, although the syndrome can be permanently debilitating or, in rare cases, fatal.
As a large outbreak of Zika continues in Central and South America, hospitals should be prepared for excess GBS cases, the authors of the study say, and assure adequate intensive-care capacity to treat them. Based on the 66% attack rate of Zika during the French Polynesia outbreak, investigators estimated the incidence of GBS at 0.24 per 1,000 Zika infections, but noted that it could be different in the current outbreak.
Dr. Van-Mai Cao-Lormeau of the Unit of Emerging Infectious Diseases at Institut Louis Malardé in Papeete, French Polynesia, alongside colleagues in France and French Polynesia, used a case-control design to compare serological samples from 42 patients (74% male) diagnosed at a Tahiti hospital with GBS with samples from age-and sex-matched patients who presented at the same hospital, also during the time of the outbreak, with a nonfebrile illness (n = 98) or with acute Zika disease without neurological symptoms (n = 70).
The investigators found that all but one patient with GBS had Zika virus antibodies, and all of them had neutralizing antibodies to Zika virus. By comparison, only 56% (n = 54) of the control group admitted with nonfebrile illness had neutralizing antibodies (P less than .0001).
Also, 93% of the GBS patients had Zika virus immunoglobulin M (IgM) and 88% reported symptoms consistent with Zika infection a mean of 6 days before onset of neurological symptoms. Acute Zika infection is usually characterized by rash, fever, and conjunctivitis.
Past dengue virus infection, which had been considered a possible risk factor for Zika-mediated GBS, did not differ significantly between patients in the control groups and those with GBS.
The investigators were also able to subtype the clinical characteristics of the GBS cases as consistent with acute motor axonal neuropathy, or AMAN, phenotype. However, the antibodies typically seen associated with AMAN were not seen in these patients, leading investigators to suspect that a different biological pathway was responsible.
More than a third of the GBS patients in the study required intensive care, most of these also with respiratory support, though none died.
The government of France, the European Union, and the Wellcome Trust funded the study. The researchers declared that they had no competing interests.
Zika virus can be added to our list of viruses that can cause Guillain-Barré syndrome, and investigation of these cases should include tests for Zika when there is a possibility of infection by that virus. Whether Zika will be proven to pose a greater threat in causing Guillain-Barré syndrome than its various flavivirus cousins remains to be determined. A little caution should be taken because the data are still scarce and we do not know whether the current Zika virus is identical to that in previous outbreaks, whether it will behave exactly the same in a different population with a different genetic and immunity background, or whether a cofactor or co-infection is responsible. Reassuringly, the investigators did not find any evidence that previous dengue infection enhanced the severity of the disease, which could substantially have increased the threat in areas of regular activity.
Dr. David W. Smith is a clinical professor of pathology and laboratory medicine at the University of Western Australia in Perth. John Mackenzie, Ph.D., is a professor of tropical and infectious diseases at Curtin University in Bentley, Australia. They had no competing interests to disclose.
Zika virus can be added to our list of viruses that can cause Guillain-Barré syndrome, and investigation of these cases should include tests for Zika when there is a possibility of infection by that virus. Whether Zika will be proven to pose a greater threat in causing Guillain-Barré syndrome than its various flavivirus cousins remains to be determined. A little caution should be taken because the data are still scarce and we do not know whether the current Zika virus is identical to that in previous outbreaks, whether it will behave exactly the same in a different population with a different genetic and immunity background, or whether a cofactor or co-infection is responsible. Reassuringly, the investigators did not find any evidence that previous dengue infection enhanced the severity of the disease, which could substantially have increased the threat in areas of regular activity.
Dr. David W. Smith is a clinical professor of pathology and laboratory medicine at the University of Western Australia in Perth. John Mackenzie, Ph.D., is a professor of tropical and infectious diseases at Curtin University in Bentley, Australia. They had no competing interests to disclose.
Zika virus can be added to our list of viruses that can cause Guillain-Barré syndrome, and investigation of these cases should include tests for Zika when there is a possibility of infection by that virus. Whether Zika will be proven to pose a greater threat in causing Guillain-Barré syndrome than its various flavivirus cousins remains to be determined. A little caution should be taken because the data are still scarce and we do not know whether the current Zika virus is identical to that in previous outbreaks, whether it will behave exactly the same in a different population with a different genetic and immunity background, or whether a cofactor or co-infection is responsible. Reassuringly, the investigators did not find any evidence that previous dengue infection enhanced the severity of the disease, which could substantially have increased the threat in areas of regular activity.
Dr. David W. Smith is a clinical professor of pathology and laboratory medicine at the University of Western Australia in Perth. John Mackenzie, Ph.D., is a professor of tropical and infectious diseases at Curtin University in Bentley, Australia. They had no competing interests to disclose.
Serological evidence from French Polynesia links an outbreak of Zika virus to a spike in cases of Guillain-Barré syndrome seen there in 2013-2014.
The research, published online Feb. 29 in The Lancet, is the first to use a case-control design to demonstrate that Zika, a mosquito-borne flavivirus, is associated with Guillain-Barré syndrome (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
Guillain-Barré syndrome (GBS) is an immune-mediated flaccid paralysis that can follow viral or bacterial infections. Most patients with GBS recover with intensive care in hospitals, although the syndrome can be permanently debilitating or, in rare cases, fatal.
As a large outbreak of Zika continues in Central and South America, hospitals should be prepared for excess GBS cases, the authors of the study say, and assure adequate intensive-care capacity to treat them. Based on the 66% attack rate of Zika during the French Polynesia outbreak, investigators estimated the incidence of GBS at 0.24 per 1,000 Zika infections, but noted that it could be different in the current outbreak.
Dr. Van-Mai Cao-Lormeau of the Unit of Emerging Infectious Diseases at Institut Louis Malardé in Papeete, French Polynesia, alongside colleagues in France and French Polynesia, used a case-control design to compare serological samples from 42 patients (74% male) diagnosed at a Tahiti hospital with GBS with samples from age-and sex-matched patients who presented at the same hospital, also during the time of the outbreak, with a nonfebrile illness (n = 98) or with acute Zika disease without neurological symptoms (n = 70).
The investigators found that all but one patient with GBS had Zika virus antibodies, and all of them had neutralizing antibodies to Zika virus. By comparison, only 56% (n = 54) of the control group admitted with nonfebrile illness had neutralizing antibodies (P less than .0001).
Also, 93% of the GBS patients had Zika virus immunoglobulin M (IgM) and 88% reported symptoms consistent with Zika infection a mean of 6 days before onset of neurological symptoms. Acute Zika infection is usually characterized by rash, fever, and conjunctivitis.
Past dengue virus infection, which had been considered a possible risk factor for Zika-mediated GBS, did not differ significantly between patients in the control groups and those with GBS.
The investigators were also able to subtype the clinical characteristics of the GBS cases as consistent with acute motor axonal neuropathy, or AMAN, phenotype. However, the antibodies typically seen associated with AMAN were not seen in these patients, leading investigators to suspect that a different biological pathway was responsible.
More than a third of the GBS patients in the study required intensive care, most of these also with respiratory support, though none died.
The government of France, the European Union, and the Wellcome Trust funded the study. The researchers declared that they had no competing interests.
Serological evidence from French Polynesia links an outbreak of Zika virus to a spike in cases of Guillain-Barré syndrome seen there in 2013-2014.
The research, published online Feb. 29 in The Lancet, is the first to use a case-control design to demonstrate that Zika, a mosquito-borne flavivirus, is associated with Guillain-Barré syndrome (Lancet. 2016 Feb 29. doi: 10.1016/S0140-6736(16)00562-6).
Guillain-Barré syndrome (GBS) is an immune-mediated flaccid paralysis that can follow viral or bacterial infections. Most patients with GBS recover with intensive care in hospitals, although the syndrome can be permanently debilitating or, in rare cases, fatal.
As a large outbreak of Zika continues in Central and South America, hospitals should be prepared for excess GBS cases, the authors of the study say, and assure adequate intensive-care capacity to treat them. Based on the 66% attack rate of Zika during the French Polynesia outbreak, investigators estimated the incidence of GBS at 0.24 per 1,000 Zika infections, but noted that it could be different in the current outbreak.
Dr. Van-Mai Cao-Lormeau of the Unit of Emerging Infectious Diseases at Institut Louis Malardé in Papeete, French Polynesia, alongside colleagues in France and French Polynesia, used a case-control design to compare serological samples from 42 patients (74% male) diagnosed at a Tahiti hospital with GBS with samples from age-and sex-matched patients who presented at the same hospital, also during the time of the outbreak, with a nonfebrile illness (n = 98) or with acute Zika disease without neurological symptoms (n = 70).
The investigators found that all but one patient with GBS had Zika virus antibodies, and all of them had neutralizing antibodies to Zika virus. By comparison, only 56% (n = 54) of the control group admitted with nonfebrile illness had neutralizing antibodies (P less than .0001).
Also, 93% of the GBS patients had Zika virus immunoglobulin M (IgM) and 88% reported symptoms consistent with Zika infection a mean of 6 days before onset of neurological symptoms. Acute Zika infection is usually characterized by rash, fever, and conjunctivitis.
Past dengue virus infection, which had been considered a possible risk factor for Zika-mediated GBS, did not differ significantly between patients in the control groups and those with GBS.
The investigators were also able to subtype the clinical characteristics of the GBS cases as consistent with acute motor axonal neuropathy, or AMAN, phenotype. However, the antibodies typically seen associated with AMAN were not seen in these patients, leading investigators to suspect that a different biological pathway was responsible.
More than a third of the GBS patients in the study required intensive care, most of these also with respiratory support, though none died.
The government of France, the European Union, and the Wellcome Trust funded the study. The researchers declared that they had no competing interests.
FROM THE LANCET