User login
‘Cancer Doesn’t Wait’: How Prior Authorization Harms Care
Fantine Giap, MD, sat across from a 21-year-old with a rare sarcoma at the base of her skull.
Despite the large tumor, nestled in a sensitive area, the Boston-based radiation oncologist could envision a bright future for her patient.
She and the other members of the patient’s care team had an impressive cancer-fighting arsenal at her fingertips. The team had recommended surgery, followed by proton therapy — a sophisticated tool able to deliver concentrated, razor-focused radiation to the once apple-sized growth, while sparing the fragile brain stem, optic nerve, and spinal cord.
Surgery went as planned. But as the days and weeks wore on and insurance prior authorization for the proton therapy never came, the tumor roared back, leading to more surgeries and more complications. Ultimately, the young woman needed a tracheostomy and a feeding tube.
By the time insurance said yes, more than 1 year from her initial visit, the future the team had envisioned seemed out of reach.
“Unfortunately for this patient, it went from a potentially curable situation to a likely not curable situation,” recalled Dr. Giap, a clinician at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. “I wanted to cry every day that she waited.’’
While a stark example, such insurance delays are not uncommon, according to new research published in JAMA Network Open.
Other studies have found that number to be even higher, with more than 86% of prior authorization requests ultimately approved with few changes.
‘’It gives you the idea that this entire process might be a little futile — that it’s just wasting people’s time,’’ said Fumiko Chino, MD, coauthor on the JAMA study and now an assistant professor in radiation oncology at MD Anderson Cancer Center in Houston. ‘’The problem is cancer doesn’t wait for bureaucracy.’’
Barriers at Every Step
As Dr. Chino and her study coauthors explained, advancements like intensity-modulated radiation therapy and stereotactic radiosurgery have allowed a new generation of specialists to treat previously untreatable cancers in ways that maximize tumor-killing power while minimizing collateral damage. But these tools require sophisticated planning, imaging, simulations and execution — all of which are subject to increased insurance scrutiny.
‘’We face barriers pretty much every step of the way for every patient,’’ said Dr. Chino.
To investigate how such barriers impact care, Dr. Chino and colleagues at Memorial Sloan Kettering Cancer Center — where she worked until July — looked at 206 cases in which payers denied prior authorization for radiation therapy from November 1, 2021 to December 8, 2022.
The team found that 62% were ultimately approved without any change to technique or dose, while 28% were authorized, but with lower doses or less sophisticated techniques. Four people, however, never got authorization at all — three abandoned treatment altogether, and one sought treatment at another institution.
Treatment delays ranged from 1 day to 49 days. Eighty-three patients died.
Would some of them have lived if it weren’t for prior authorization?
Dr. Chino cannot say for sure, but did note that certain cancers, like cervical cancer, can grow so quickly that every day of delayed treatment makes them harder to control.
Patients with metastatic or late-stage cancers are often denied more aggressive treatments by insurers who, in essence, “assume that they are going to die from their disease anyway,” Dr. Chino said.
She views this as tragically shortsighted.
‘’There’s actually a strong body of evidence to show that if you treat even metastatic stage IV diseases aggressively, you can prolong not just quality of life but also quantity,’’ she said.
In cases where the cancer is more localized and insurance mandates lower doses or cheaper techniques, the consequences can be equally heartbreaking.
‘’It’s like saying instead of taking an extra-strength Tylenol you can only have a baby aspirin,’’ she said. ‘’Their pain is less likely to be controlled, their disease is less likely to be controlled, and they are more likely to need retreatment.’’
Prior authorization delays can also significantly stress patients at the most vulnerable point of their lives.
In another recent study, Dr. Chino found that 69% of patients with cancer reported prior authorization-related delays in care, with one-third waiting a month or longer. One in five never got the care their doctors recommended, and 20% reported spending more than 11 hours on the phone haggling with their insurance companies.
Most patients rated the process as ‘’bad’’ or ‘’horrible,’’ and said it fueled anxiety.
Such delays can be hard on clinicians and the healthcare system too.
One 2022 study found that a typical academic radiation oncology practice spent about a half-million dollars per year seeking insurance preauthorization. Nationally, that number exceeds $40 million.
Then there is the burnout factor.
Dr. Giap, an early-career physician who specializes in rare, aggressive sarcomas, works at an institution that helped pioneer proton therapy. She says it pains her to tell a desperate patient, like the 21-year-old, who has traveled to her from out of state that they have to wait.
‘’Knowing that the majority of the cases are ultimately approved and that this wait is often unnecessary makes it even tougher,’’ she said.
Dr. Chino, a breast cancer specialist, has taken to warning patients before the alarming insurance letter arrives in the mail that their insurance may delay authorizing their care. But she tells patients that she will do everything she can to fight for them and develops a back-up plan to pivot to quickly, if needed.
‘’No one goes into medicine to spend their time talking to insurance companies,’’ said Dr. Chino.
The national trade group, America’s Health Insurance Plans (AHIP), did not return repeated requests for an interview for this story. But their official position, as stated on their website, is that “prior authorization is one of many tools health insurance providers use to promote safe, timely, evidence-based, affordable, and efficient care.”
Both Dr. Giap and Dr. Chino believe that prior authorization was developed with good intentions: to save healthcare costs and rein in treatments that don’t necessarily benefit patients.
But, in their specialty, the burden has proliferated to a point that Dr. Chino characterizes as ‘’unconscionable.’’
She believes that policy changes like the proposed Improving Seniors’ Timely Access to Care Act — which would require real-time decisions for procedures that are routinely approved — could go a long way in improving patient care.
Meanwhile, Dr. Giap said, more research and professional guidelines are necessary to bolster insurance company confidence in newer technologies, particularly for rare cancers.
Her patient ultimately got her proton therapy and is ‘’doing relatively well, all things considered.’’
But not all the stories end like this.
Dr. Chino will never forget a patient with a cancer growing so rapidly she could see it protruding through her chest wall. She called for an urgent PET scan to see where else in the body the cancer might be brewing and rushed the planning process for radiation therapy, both of which faced prior authorization barriers. That scan — which ultimately showed the cancer had spread — was delayed for months.*
If the team had had those imaging results upfront, she said, they would have recommended a completely different course of treatment.
And her patient might be alive today.
‘’Unfortunately,” Dr. Chino said, “the people with the very worst prior authorization stories aren’t here anymore to tell you about them.”
*Correction, 10/4/24: An earlier version of this article erroneously stated that Dr. Chino called for surgery for her patient. She actually called for a PET scan and an urgent radiation start.
A version of this article first appeared on Medscape.com.
Fantine Giap, MD, sat across from a 21-year-old with a rare sarcoma at the base of her skull.
Despite the large tumor, nestled in a sensitive area, the Boston-based radiation oncologist could envision a bright future for her patient.
She and the other members of the patient’s care team had an impressive cancer-fighting arsenal at her fingertips. The team had recommended surgery, followed by proton therapy — a sophisticated tool able to deliver concentrated, razor-focused radiation to the once apple-sized growth, while sparing the fragile brain stem, optic nerve, and spinal cord.
Surgery went as planned. But as the days and weeks wore on and insurance prior authorization for the proton therapy never came, the tumor roared back, leading to more surgeries and more complications. Ultimately, the young woman needed a tracheostomy and a feeding tube.
By the time insurance said yes, more than 1 year from her initial visit, the future the team had envisioned seemed out of reach.
“Unfortunately for this patient, it went from a potentially curable situation to a likely not curable situation,” recalled Dr. Giap, a clinician at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. “I wanted to cry every day that she waited.’’
While a stark example, such insurance delays are not uncommon, according to new research published in JAMA Network Open.
Other studies have found that number to be even higher, with more than 86% of prior authorization requests ultimately approved with few changes.
‘’It gives you the idea that this entire process might be a little futile — that it’s just wasting people’s time,’’ said Fumiko Chino, MD, coauthor on the JAMA study and now an assistant professor in radiation oncology at MD Anderson Cancer Center in Houston. ‘’The problem is cancer doesn’t wait for bureaucracy.’’
Barriers at Every Step
As Dr. Chino and her study coauthors explained, advancements like intensity-modulated radiation therapy and stereotactic radiosurgery have allowed a new generation of specialists to treat previously untreatable cancers in ways that maximize tumor-killing power while minimizing collateral damage. But these tools require sophisticated planning, imaging, simulations and execution — all of which are subject to increased insurance scrutiny.
‘’We face barriers pretty much every step of the way for every patient,’’ said Dr. Chino.
To investigate how such barriers impact care, Dr. Chino and colleagues at Memorial Sloan Kettering Cancer Center — where she worked until July — looked at 206 cases in which payers denied prior authorization for radiation therapy from November 1, 2021 to December 8, 2022.
The team found that 62% were ultimately approved without any change to technique or dose, while 28% were authorized, but with lower doses or less sophisticated techniques. Four people, however, never got authorization at all — three abandoned treatment altogether, and one sought treatment at another institution.
Treatment delays ranged from 1 day to 49 days. Eighty-three patients died.
Would some of them have lived if it weren’t for prior authorization?
Dr. Chino cannot say for sure, but did note that certain cancers, like cervical cancer, can grow so quickly that every day of delayed treatment makes them harder to control.
Patients with metastatic or late-stage cancers are often denied more aggressive treatments by insurers who, in essence, “assume that they are going to die from their disease anyway,” Dr. Chino said.
She views this as tragically shortsighted.
‘’There’s actually a strong body of evidence to show that if you treat even metastatic stage IV diseases aggressively, you can prolong not just quality of life but also quantity,’’ she said.
In cases where the cancer is more localized and insurance mandates lower doses or cheaper techniques, the consequences can be equally heartbreaking.
‘’It’s like saying instead of taking an extra-strength Tylenol you can only have a baby aspirin,’’ she said. ‘’Their pain is less likely to be controlled, their disease is less likely to be controlled, and they are more likely to need retreatment.’’
Prior authorization delays can also significantly stress patients at the most vulnerable point of their lives.
In another recent study, Dr. Chino found that 69% of patients with cancer reported prior authorization-related delays in care, with one-third waiting a month or longer. One in five never got the care their doctors recommended, and 20% reported spending more than 11 hours on the phone haggling with their insurance companies.
Most patients rated the process as ‘’bad’’ or ‘’horrible,’’ and said it fueled anxiety.
Such delays can be hard on clinicians and the healthcare system too.
One 2022 study found that a typical academic radiation oncology practice spent about a half-million dollars per year seeking insurance preauthorization. Nationally, that number exceeds $40 million.
Then there is the burnout factor.
Dr. Giap, an early-career physician who specializes in rare, aggressive sarcomas, works at an institution that helped pioneer proton therapy. She says it pains her to tell a desperate patient, like the 21-year-old, who has traveled to her from out of state that they have to wait.
‘’Knowing that the majority of the cases are ultimately approved and that this wait is often unnecessary makes it even tougher,’’ she said.
Dr. Chino, a breast cancer specialist, has taken to warning patients before the alarming insurance letter arrives in the mail that their insurance may delay authorizing their care. But she tells patients that she will do everything she can to fight for them and develops a back-up plan to pivot to quickly, if needed.
‘’No one goes into medicine to spend their time talking to insurance companies,’’ said Dr. Chino.
The national trade group, America’s Health Insurance Plans (AHIP), did not return repeated requests for an interview for this story. But their official position, as stated on their website, is that “prior authorization is one of many tools health insurance providers use to promote safe, timely, evidence-based, affordable, and efficient care.”
Both Dr. Giap and Dr. Chino believe that prior authorization was developed with good intentions: to save healthcare costs and rein in treatments that don’t necessarily benefit patients.
But, in their specialty, the burden has proliferated to a point that Dr. Chino characterizes as ‘’unconscionable.’’
She believes that policy changes like the proposed Improving Seniors’ Timely Access to Care Act — which would require real-time decisions for procedures that are routinely approved — could go a long way in improving patient care.
Meanwhile, Dr. Giap said, more research and professional guidelines are necessary to bolster insurance company confidence in newer technologies, particularly for rare cancers.
Her patient ultimately got her proton therapy and is ‘’doing relatively well, all things considered.’’
But not all the stories end like this.
Dr. Chino will never forget a patient with a cancer growing so rapidly she could see it protruding through her chest wall. She called for an urgent PET scan to see where else in the body the cancer might be brewing and rushed the planning process for radiation therapy, both of which faced prior authorization barriers. That scan — which ultimately showed the cancer had spread — was delayed for months.*
If the team had had those imaging results upfront, she said, they would have recommended a completely different course of treatment.
And her patient might be alive today.
‘’Unfortunately,” Dr. Chino said, “the people with the very worst prior authorization stories aren’t here anymore to tell you about them.”
*Correction, 10/4/24: An earlier version of this article erroneously stated that Dr. Chino called for surgery for her patient. She actually called for a PET scan and an urgent radiation start.
A version of this article first appeared on Medscape.com.
Fantine Giap, MD, sat across from a 21-year-old with a rare sarcoma at the base of her skull.
Despite the large tumor, nestled in a sensitive area, the Boston-based radiation oncologist could envision a bright future for her patient.
She and the other members of the patient’s care team had an impressive cancer-fighting arsenal at her fingertips. The team had recommended surgery, followed by proton therapy — a sophisticated tool able to deliver concentrated, razor-focused radiation to the once apple-sized growth, while sparing the fragile brain stem, optic nerve, and spinal cord.
Surgery went as planned. But as the days and weeks wore on and insurance prior authorization for the proton therapy never came, the tumor roared back, leading to more surgeries and more complications. Ultimately, the young woman needed a tracheostomy and a feeding tube.
By the time insurance said yes, more than 1 year from her initial visit, the future the team had envisioned seemed out of reach.
“Unfortunately for this patient, it went from a potentially curable situation to a likely not curable situation,” recalled Dr. Giap, a clinician at Massachusetts General Hospital and instructor at Harvard Medical School, Boston. “I wanted to cry every day that she waited.’’
While a stark example, such insurance delays are not uncommon, according to new research published in JAMA Network Open.
Other studies have found that number to be even higher, with more than 86% of prior authorization requests ultimately approved with few changes.
‘’It gives you the idea that this entire process might be a little futile — that it’s just wasting people’s time,’’ said Fumiko Chino, MD, coauthor on the JAMA study and now an assistant professor in radiation oncology at MD Anderson Cancer Center in Houston. ‘’The problem is cancer doesn’t wait for bureaucracy.’’
Barriers at Every Step
As Dr. Chino and her study coauthors explained, advancements like intensity-modulated radiation therapy and stereotactic radiosurgery have allowed a new generation of specialists to treat previously untreatable cancers in ways that maximize tumor-killing power while minimizing collateral damage. But these tools require sophisticated planning, imaging, simulations and execution — all of which are subject to increased insurance scrutiny.
‘’We face barriers pretty much every step of the way for every patient,’’ said Dr. Chino.
To investigate how such barriers impact care, Dr. Chino and colleagues at Memorial Sloan Kettering Cancer Center — where she worked until July — looked at 206 cases in which payers denied prior authorization for radiation therapy from November 1, 2021 to December 8, 2022.
The team found that 62% were ultimately approved without any change to technique or dose, while 28% were authorized, but with lower doses or less sophisticated techniques. Four people, however, never got authorization at all — three abandoned treatment altogether, and one sought treatment at another institution.
Treatment delays ranged from 1 day to 49 days. Eighty-three patients died.
Would some of them have lived if it weren’t for prior authorization?
Dr. Chino cannot say for sure, but did note that certain cancers, like cervical cancer, can grow so quickly that every day of delayed treatment makes them harder to control.
Patients with metastatic or late-stage cancers are often denied more aggressive treatments by insurers who, in essence, “assume that they are going to die from their disease anyway,” Dr. Chino said.
She views this as tragically shortsighted.
‘’There’s actually a strong body of evidence to show that if you treat even metastatic stage IV diseases aggressively, you can prolong not just quality of life but also quantity,’’ she said.
In cases where the cancer is more localized and insurance mandates lower doses or cheaper techniques, the consequences can be equally heartbreaking.
‘’It’s like saying instead of taking an extra-strength Tylenol you can only have a baby aspirin,’’ she said. ‘’Their pain is less likely to be controlled, their disease is less likely to be controlled, and they are more likely to need retreatment.’’
Prior authorization delays can also significantly stress patients at the most vulnerable point of their lives.
In another recent study, Dr. Chino found that 69% of patients with cancer reported prior authorization-related delays in care, with one-third waiting a month or longer. One in five never got the care their doctors recommended, and 20% reported spending more than 11 hours on the phone haggling with their insurance companies.
Most patients rated the process as ‘’bad’’ or ‘’horrible,’’ and said it fueled anxiety.
Such delays can be hard on clinicians and the healthcare system too.
One 2022 study found that a typical academic radiation oncology practice spent about a half-million dollars per year seeking insurance preauthorization. Nationally, that number exceeds $40 million.
Then there is the burnout factor.
Dr. Giap, an early-career physician who specializes in rare, aggressive sarcomas, works at an institution that helped pioneer proton therapy. She says it pains her to tell a desperate patient, like the 21-year-old, who has traveled to her from out of state that they have to wait.
‘’Knowing that the majority of the cases are ultimately approved and that this wait is often unnecessary makes it even tougher,’’ she said.
Dr. Chino, a breast cancer specialist, has taken to warning patients before the alarming insurance letter arrives in the mail that their insurance may delay authorizing their care. But she tells patients that she will do everything she can to fight for them and develops a back-up plan to pivot to quickly, if needed.
‘’No one goes into medicine to spend their time talking to insurance companies,’’ said Dr. Chino.
The national trade group, America’s Health Insurance Plans (AHIP), did not return repeated requests for an interview for this story. But their official position, as stated on their website, is that “prior authorization is one of many tools health insurance providers use to promote safe, timely, evidence-based, affordable, and efficient care.”
Both Dr. Giap and Dr. Chino believe that prior authorization was developed with good intentions: to save healthcare costs and rein in treatments that don’t necessarily benefit patients.
But, in their specialty, the burden has proliferated to a point that Dr. Chino characterizes as ‘’unconscionable.’’
She believes that policy changes like the proposed Improving Seniors’ Timely Access to Care Act — which would require real-time decisions for procedures that are routinely approved — could go a long way in improving patient care.
Meanwhile, Dr. Giap said, more research and professional guidelines are necessary to bolster insurance company confidence in newer technologies, particularly for rare cancers.
Her patient ultimately got her proton therapy and is ‘’doing relatively well, all things considered.’’
But not all the stories end like this.
Dr. Chino will never forget a patient with a cancer growing so rapidly she could see it protruding through her chest wall. She called for an urgent PET scan to see where else in the body the cancer might be brewing and rushed the planning process for radiation therapy, both of which faced prior authorization barriers. That scan — which ultimately showed the cancer had spread — was delayed for months.*
If the team had had those imaging results upfront, she said, they would have recommended a completely different course of treatment.
And her patient might be alive today.
‘’Unfortunately,” Dr. Chino said, “the people with the very worst prior authorization stories aren’t here anymore to tell you about them.”
*Correction, 10/4/24: An earlier version of this article erroneously stated that Dr. Chino called for surgery for her patient. She actually called for a PET scan and an urgent radiation start.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
‘Chemoresistance Can Be Reversed’: Toughest Cancers Targeted
In the war against cancer, doctors and patients have long reached for three main weapons to target diseased cells: chemotherapy, radiation, and surgery.
But new research published this month in the journal Nature Materials suggests that manipulating the tissue around those cells — a strategy known as
“Our study shows the importance of the tumor microenvironment and its properties in dictating how cancer progresses and responds to drug treatment,” said first author Bauer LeSavage, PhD, who conducted the study as a postdoctoral researcher in the Bioengineering Department at Stanford University, Stanford, California. “It also demonstrates that chemoresistance can be reversed.”
Each year, about 66,000 people are diagnosed with pancreatic cancer, and 52,000 die from it. It is a particularly lethal type of cancer, with 5-year survival rates hovering around 7% — a rate that has not improved much since 1996 when the first-line chemotherapy drug gemcitabine was approved.
It looks different from many cancers, said Lynn Matrisian, PhD, chief science officer for the nonprofit Pancreatic Cancer Action Network. Instead of a tumorous mass, it is made of islands of cancer cells surrounded by unusually dense fibrous tissue known as the extracellular matrix, which can collapse blood vessels and prevent drugs from reaching the tumor.
For the study, Dr. LeSavage and his team engineered synthetic but lifelike three-dimensional pancreas tissue with varying degrees of stiffness and different biochemical properties. Then they inserted bits of real tumors from patients with pancreatic cancer, watched them grow, and tried to kill them with drugs.
They found that cells growing in a stiff matrix were more resistant to chemotherapy than those growing in a softer matrix. But the story didn’t end there.
They also found that high amounts of the tissue-strengthening protein hyaluronic acid in stiff tissue seemed to signal the cancer cells to develop tiny pumps on their surface which shuttled out the drugs before they could take effect.
When the researchers moved the cancer cells into either a softer matrix or a stiff matrix in which the hyaluronic acid receptor, called CD44, was blocked, the chemotherapy drugs started working again.
“This suggests that if we can disrupt the stiffness signaling that’s happening through the CD44 receptor, we could make patients’ pancreatic cancer treatable again by normal chemotherapy,” said senior study author Sarah Heilshorn, PhD, a professor of materials science and engineering at Stanford. “These results suggest an exciting new direction for new drug development.”
Targeting Nearby Tissue: A Novel Approach to Fighting Chemoresistance
The study is not the first to suggest that chemically targeting the microenvironment surrounding a tumor can influence how patients respond to treatment.
In one recent clinical trial, patients with metastatic pancreatic cancer were given an experimental drug to inhibit a protein called connective tissue growth factor, reduce fibrous tissue, and make pancreatic tumors easier to surgically remove. Results have not been published yet.
Other research suggests that the generic blood pressure drug losartan, when given in combination with chemotherapy and radiation, can boost survival in patients with advanced pancreatic cancer by, in part, improving the health of blood vessels that carry drugs to the tumor.
But other studies of such mechanotherapeutics have yielded inconclusive results, said Dr. Matrisian.
“This paper points to another reason why we should not give up on this approach,” she said.
Ning Wang, PhD, director of the new Institute for Mechanobiology at Northeastern University College of Engineering, Boston, said there is no question that the composition of a tumor’s environment can influence how cancer progresses or responds to drugs. The new paper, he said, adds an important new chapter to the evolving story.
“But it’s very complicated. It’s not as simple as saying make it softer or stiffer and you can change the outcome for the patient,” Dr. Wang said.
In fact, some research has shown that tissue becomes stiffer when cancer arises so it can contain it from spreading.
In one animal study of pancreatic cancer that had spread to the liver, administering drugs to soften the surrounding tissue, or stroma, actually had the opposite effect — accelerating tumor growth and reducing survival rates.
Dr. Wang also noted that any drug designed to influence the extracellular matrix would need to be extremely localized, to prevent damage to other tissues, like bone or heart muscle.
Dr. LeSavage said he sees the paper as a case study in how important the extracellular matrix is and an example of how artificially grown organs or tissues can play a key role in testing how drugs work or don’t work.
He imagines a day when doctors could personalize treatments by taking a bit of a patient’s tumor, growing it in artificial tissue, and seeing how different tissue-altering drugs affect different therapies.
“This isn’t something that is just unique to pancreatic cancer,” he said, noting that the extracellular matrix throughout the body interacts with different cancers. “If we could take someone who has a chemoresistant tumor and convert it into something that is sensitive to existing therapies again, we could give them a second chance.”
A version of this article appeared on Medscape.com.
In the war against cancer, doctors and patients have long reached for three main weapons to target diseased cells: chemotherapy, radiation, and surgery.
But new research published this month in the journal Nature Materials suggests that manipulating the tissue around those cells — a strategy known as
“Our study shows the importance of the tumor microenvironment and its properties in dictating how cancer progresses and responds to drug treatment,” said first author Bauer LeSavage, PhD, who conducted the study as a postdoctoral researcher in the Bioengineering Department at Stanford University, Stanford, California. “It also demonstrates that chemoresistance can be reversed.”
Each year, about 66,000 people are diagnosed with pancreatic cancer, and 52,000 die from it. It is a particularly lethal type of cancer, with 5-year survival rates hovering around 7% — a rate that has not improved much since 1996 when the first-line chemotherapy drug gemcitabine was approved.
It looks different from many cancers, said Lynn Matrisian, PhD, chief science officer for the nonprofit Pancreatic Cancer Action Network. Instead of a tumorous mass, it is made of islands of cancer cells surrounded by unusually dense fibrous tissue known as the extracellular matrix, which can collapse blood vessels and prevent drugs from reaching the tumor.
For the study, Dr. LeSavage and his team engineered synthetic but lifelike three-dimensional pancreas tissue with varying degrees of stiffness and different biochemical properties. Then they inserted bits of real tumors from patients with pancreatic cancer, watched them grow, and tried to kill them with drugs.
They found that cells growing in a stiff matrix were more resistant to chemotherapy than those growing in a softer matrix. But the story didn’t end there.
They also found that high amounts of the tissue-strengthening protein hyaluronic acid in stiff tissue seemed to signal the cancer cells to develop tiny pumps on their surface which shuttled out the drugs before they could take effect.
When the researchers moved the cancer cells into either a softer matrix or a stiff matrix in which the hyaluronic acid receptor, called CD44, was blocked, the chemotherapy drugs started working again.
“This suggests that if we can disrupt the stiffness signaling that’s happening through the CD44 receptor, we could make patients’ pancreatic cancer treatable again by normal chemotherapy,” said senior study author Sarah Heilshorn, PhD, a professor of materials science and engineering at Stanford. “These results suggest an exciting new direction for new drug development.”
Targeting Nearby Tissue: A Novel Approach to Fighting Chemoresistance
The study is not the first to suggest that chemically targeting the microenvironment surrounding a tumor can influence how patients respond to treatment.
In one recent clinical trial, patients with metastatic pancreatic cancer were given an experimental drug to inhibit a protein called connective tissue growth factor, reduce fibrous tissue, and make pancreatic tumors easier to surgically remove. Results have not been published yet.
Other research suggests that the generic blood pressure drug losartan, when given in combination with chemotherapy and radiation, can boost survival in patients with advanced pancreatic cancer by, in part, improving the health of blood vessels that carry drugs to the tumor.
But other studies of such mechanotherapeutics have yielded inconclusive results, said Dr. Matrisian.
“This paper points to another reason why we should not give up on this approach,” she said.
Ning Wang, PhD, director of the new Institute for Mechanobiology at Northeastern University College of Engineering, Boston, said there is no question that the composition of a tumor’s environment can influence how cancer progresses or responds to drugs. The new paper, he said, adds an important new chapter to the evolving story.
“But it’s very complicated. It’s not as simple as saying make it softer or stiffer and you can change the outcome for the patient,” Dr. Wang said.
In fact, some research has shown that tissue becomes stiffer when cancer arises so it can contain it from spreading.
In one animal study of pancreatic cancer that had spread to the liver, administering drugs to soften the surrounding tissue, or stroma, actually had the opposite effect — accelerating tumor growth and reducing survival rates.
Dr. Wang also noted that any drug designed to influence the extracellular matrix would need to be extremely localized, to prevent damage to other tissues, like bone or heart muscle.
Dr. LeSavage said he sees the paper as a case study in how important the extracellular matrix is and an example of how artificially grown organs or tissues can play a key role in testing how drugs work or don’t work.
He imagines a day when doctors could personalize treatments by taking a bit of a patient’s tumor, growing it in artificial tissue, and seeing how different tissue-altering drugs affect different therapies.
“This isn’t something that is just unique to pancreatic cancer,” he said, noting that the extracellular matrix throughout the body interacts with different cancers. “If we could take someone who has a chemoresistant tumor and convert it into something that is sensitive to existing therapies again, we could give them a second chance.”
A version of this article appeared on Medscape.com.
In the war against cancer, doctors and patients have long reached for three main weapons to target diseased cells: chemotherapy, radiation, and surgery.
But new research published this month in the journal Nature Materials suggests that manipulating the tissue around those cells — a strategy known as
“Our study shows the importance of the tumor microenvironment and its properties in dictating how cancer progresses and responds to drug treatment,” said first author Bauer LeSavage, PhD, who conducted the study as a postdoctoral researcher in the Bioengineering Department at Stanford University, Stanford, California. “It also demonstrates that chemoresistance can be reversed.”
Each year, about 66,000 people are diagnosed with pancreatic cancer, and 52,000 die from it. It is a particularly lethal type of cancer, with 5-year survival rates hovering around 7% — a rate that has not improved much since 1996 when the first-line chemotherapy drug gemcitabine was approved.
It looks different from many cancers, said Lynn Matrisian, PhD, chief science officer for the nonprofit Pancreatic Cancer Action Network. Instead of a tumorous mass, it is made of islands of cancer cells surrounded by unusually dense fibrous tissue known as the extracellular matrix, which can collapse blood vessels and prevent drugs from reaching the tumor.
For the study, Dr. LeSavage and his team engineered synthetic but lifelike three-dimensional pancreas tissue with varying degrees of stiffness and different biochemical properties. Then they inserted bits of real tumors from patients with pancreatic cancer, watched them grow, and tried to kill them with drugs.
They found that cells growing in a stiff matrix were more resistant to chemotherapy than those growing in a softer matrix. But the story didn’t end there.
They also found that high amounts of the tissue-strengthening protein hyaluronic acid in stiff tissue seemed to signal the cancer cells to develop tiny pumps on their surface which shuttled out the drugs before they could take effect.
When the researchers moved the cancer cells into either a softer matrix or a stiff matrix in which the hyaluronic acid receptor, called CD44, was blocked, the chemotherapy drugs started working again.
“This suggests that if we can disrupt the stiffness signaling that’s happening through the CD44 receptor, we could make patients’ pancreatic cancer treatable again by normal chemotherapy,” said senior study author Sarah Heilshorn, PhD, a professor of materials science and engineering at Stanford. “These results suggest an exciting new direction for new drug development.”
Targeting Nearby Tissue: A Novel Approach to Fighting Chemoresistance
The study is not the first to suggest that chemically targeting the microenvironment surrounding a tumor can influence how patients respond to treatment.
In one recent clinical trial, patients with metastatic pancreatic cancer were given an experimental drug to inhibit a protein called connective tissue growth factor, reduce fibrous tissue, and make pancreatic tumors easier to surgically remove. Results have not been published yet.
Other research suggests that the generic blood pressure drug losartan, when given in combination with chemotherapy and radiation, can boost survival in patients with advanced pancreatic cancer by, in part, improving the health of blood vessels that carry drugs to the tumor.
But other studies of such mechanotherapeutics have yielded inconclusive results, said Dr. Matrisian.
“This paper points to another reason why we should not give up on this approach,” she said.
Ning Wang, PhD, director of the new Institute for Mechanobiology at Northeastern University College of Engineering, Boston, said there is no question that the composition of a tumor’s environment can influence how cancer progresses or responds to drugs. The new paper, he said, adds an important new chapter to the evolving story.
“But it’s very complicated. It’s not as simple as saying make it softer or stiffer and you can change the outcome for the patient,” Dr. Wang said.
In fact, some research has shown that tissue becomes stiffer when cancer arises so it can contain it from spreading.
In one animal study of pancreatic cancer that had spread to the liver, administering drugs to soften the surrounding tissue, or stroma, actually had the opposite effect — accelerating tumor growth and reducing survival rates.
Dr. Wang also noted that any drug designed to influence the extracellular matrix would need to be extremely localized, to prevent damage to other tissues, like bone or heart muscle.
Dr. LeSavage said he sees the paper as a case study in how important the extracellular matrix is and an example of how artificially grown organs or tissues can play a key role in testing how drugs work or don’t work.
He imagines a day when doctors could personalize treatments by taking a bit of a patient’s tumor, growing it in artificial tissue, and seeing how different tissue-altering drugs affect different therapies.
“This isn’t something that is just unique to pancreatic cancer,” he said, noting that the extracellular matrix throughout the body interacts with different cancers. “If we could take someone who has a chemoresistant tumor and convert it into something that is sensitive to existing therapies again, we could give them a second chance.”
A version of this article appeared on Medscape.com.
Solving Restless Legs: Largest Genetic Study to Date May Help
For decades, scientists have been trying to unravel the mysteries of restless legs syndrome (RLS), a poorly understood and underdiagnosed neurological disorder causing itching, crawling, and aching sensations in the limbs that can only be relieved with movement.
A sweeping new genetic study, coauthored by an international team of 70 — including the world’s leading RLS experts — marks a significant advance in that pursuit. Published in Nature Genetics, it is the largest genetic study of the disease to date.
“It’s a huge step forward for patients as well as the scientific community,” said lead author Juliane Winkelmann, MD, a neurologist and geneticist with the Technical University of Munich, Munich, Germany, who’s been studying and treating patients with RLS for 30 years. “We believe it will allow us to better predict the likelihood of developing RLS and investigate new ways to prevent and modify it.”
The common condition, affecting about 1 in 10 adults, was first described centuries ago — by English physician Thomas Willis in the late 1600s. And while we know a lot more about it today — it’s familial in about half of all patients and has been linked to iron deficiency, among other conditions — its exact cause remains unknown.
With preferred drugs long prescribed to quell symptoms shown in recent years to actually worsen the disorder over time, doctors and patients are hungry for alternatives to treat or prevent the sleep-sabotaging condition.
“The main treatments that everybody continues to use are actually making people worse,” said Andrew Berkowski, MD, a Michigan-based neurologist and RLS specialist not involved in the study. These drugs — dopamine agonists such as levodopa and pramipexole — can also potentially cause drug dependence, Dr. Berkowski said.
How This Could Lead to New Treatments
In the new study, the group analyzed three genome-wide association studies, collectively including genetic information from 116,647 patients with RLS and more than 1.5 million people without it.
They identified 161 gene regions believed to contribute to RLS, about a dozen of which are already targets for existing drugs for other conditions. Previously, scientists knew of only 22 associated genes.
“It’s useful in that it identifies new genes we haven’t looked at yet and reinforces the science behind some of the older genes,” said Dr. Berkowski. “It’s given us some ideas for different things we should look into more closely.”
Among the top candidates are genes that influence glutamate — a key chemical messenger that helps move signals between nerve cells in the brain.
Several anticonvulsant and antiseizure drugs, including perampanel, lamotrigine, and gabapentin, target glutamate receptors. And at least one small study has shown perampanel prescribed off-label can improve RLS symptoms.
“Compared to starting at the beginning and developing an entirely new chemical entity, we could run clinical trials using these alternatives in RLS patients,” said the study’s first author, Steven Bell, PhD, an epidemiologist with the University of Cambridge, Cambridge, England.
The study also confirmed the MIES1 gene, which is related to dopamine expression and iron homeostasis, as a key genetic contributor to RLS risk. Low levels of iron in the blood have long been thought to trigger RLS.
The Role of Gene-Environment Interactions
Through additional data analysis, the team confirmed that many of the genes associated with RLS play a role in development of the central nervous system.
“This strongly supports the hypothesis that restless legs syndrome is a neurodevelopmental disorder that develops during the embryo stage but doesn’t clinically manifest until later in life,” said Dr. Winkelmann.
About half of people with RLS report some family history of it.
But not all with a genetic predisposition will develop symptoms.
For instance, the study found that while the same gene regions seem to be associated with risk in both men and women, in practice, RLS is twice as common among women. This suggests that something about women’s lives — menstruation, childbirth, metabolism — may switch a preexisting risk into a reality.
“We know that genetic factors play an important role in making people susceptible to the disease,” said Dr. Winkelmann, “but in the end, it is the interaction between genetic and environmental factors that may lead to its manifestation.”
The study also found associations between RLS and depression and suggests that RLS may increase the risk for type 2 diabetes.
Improving RLS Care
A potentially useful tool coming out of the study was a “polygenic risk score,” which the researchers developed based on the genes identified. When they tested how accurately the score could predict whether someone would develop RLS within the next 5 years, the model got it right about 90% of the time.
Dr. Winkelmann imagines a day when someone could use such a polygenic risk score to flag the high risk for RLS early enough to take action to try to prevent it. More research is necessary to determine precisely what that action would be.
As for treatments, Dr. Berkowski thinks it’s unlikely that doctors will suddenly begin using existing, glutamate-targeting drugs off-label to treat RLS, as many are prohibitively expensive and wouldn’t be covered by insurance. But he’s optimistic that the study can spawn new research that could ultimately help fill the treatment gap.
Shalini Paruthi, MD, an adjunct professor at Saint Louis University, St. Louis, Missouri, and chair of the Restless Legs Syndrome Foundation’s board of directors, sees another benefit.
“The associations found in this study between RLS and other medical disorders may help patients and their physicians take RLS more seriously,” Dr. Paruthi said, “as treating RLS can lead to multiple other downstream improvements in their health.”
A version of this article appeared on Medscape.com.
For decades, scientists have been trying to unravel the mysteries of restless legs syndrome (RLS), a poorly understood and underdiagnosed neurological disorder causing itching, crawling, and aching sensations in the limbs that can only be relieved with movement.
A sweeping new genetic study, coauthored by an international team of 70 — including the world’s leading RLS experts — marks a significant advance in that pursuit. Published in Nature Genetics, it is the largest genetic study of the disease to date.
“It’s a huge step forward for patients as well as the scientific community,” said lead author Juliane Winkelmann, MD, a neurologist and geneticist with the Technical University of Munich, Munich, Germany, who’s been studying and treating patients with RLS for 30 years. “We believe it will allow us to better predict the likelihood of developing RLS and investigate new ways to prevent and modify it.”
The common condition, affecting about 1 in 10 adults, was first described centuries ago — by English physician Thomas Willis in the late 1600s. And while we know a lot more about it today — it’s familial in about half of all patients and has been linked to iron deficiency, among other conditions — its exact cause remains unknown.
With preferred drugs long prescribed to quell symptoms shown in recent years to actually worsen the disorder over time, doctors and patients are hungry for alternatives to treat or prevent the sleep-sabotaging condition.
“The main treatments that everybody continues to use are actually making people worse,” said Andrew Berkowski, MD, a Michigan-based neurologist and RLS specialist not involved in the study. These drugs — dopamine agonists such as levodopa and pramipexole — can also potentially cause drug dependence, Dr. Berkowski said.
How This Could Lead to New Treatments
In the new study, the group analyzed three genome-wide association studies, collectively including genetic information from 116,647 patients with RLS and more than 1.5 million people without it.
They identified 161 gene regions believed to contribute to RLS, about a dozen of which are already targets for existing drugs for other conditions. Previously, scientists knew of only 22 associated genes.
“It’s useful in that it identifies new genes we haven’t looked at yet and reinforces the science behind some of the older genes,” said Dr. Berkowski. “It’s given us some ideas for different things we should look into more closely.”
Among the top candidates are genes that influence glutamate — a key chemical messenger that helps move signals between nerve cells in the brain.
Several anticonvulsant and antiseizure drugs, including perampanel, lamotrigine, and gabapentin, target glutamate receptors. And at least one small study has shown perampanel prescribed off-label can improve RLS symptoms.
“Compared to starting at the beginning and developing an entirely new chemical entity, we could run clinical trials using these alternatives in RLS patients,” said the study’s first author, Steven Bell, PhD, an epidemiologist with the University of Cambridge, Cambridge, England.
The study also confirmed the MIES1 gene, which is related to dopamine expression and iron homeostasis, as a key genetic contributor to RLS risk. Low levels of iron in the blood have long been thought to trigger RLS.
The Role of Gene-Environment Interactions
Through additional data analysis, the team confirmed that many of the genes associated with RLS play a role in development of the central nervous system.
“This strongly supports the hypothesis that restless legs syndrome is a neurodevelopmental disorder that develops during the embryo stage but doesn’t clinically manifest until later in life,” said Dr. Winkelmann.
About half of people with RLS report some family history of it.
But not all with a genetic predisposition will develop symptoms.
For instance, the study found that while the same gene regions seem to be associated with risk in both men and women, in practice, RLS is twice as common among women. This suggests that something about women’s lives — menstruation, childbirth, metabolism — may switch a preexisting risk into a reality.
“We know that genetic factors play an important role in making people susceptible to the disease,” said Dr. Winkelmann, “but in the end, it is the interaction between genetic and environmental factors that may lead to its manifestation.”
The study also found associations between RLS and depression and suggests that RLS may increase the risk for type 2 diabetes.
Improving RLS Care
A potentially useful tool coming out of the study was a “polygenic risk score,” which the researchers developed based on the genes identified. When they tested how accurately the score could predict whether someone would develop RLS within the next 5 years, the model got it right about 90% of the time.
Dr. Winkelmann imagines a day when someone could use such a polygenic risk score to flag the high risk for RLS early enough to take action to try to prevent it. More research is necessary to determine precisely what that action would be.
As for treatments, Dr. Berkowski thinks it’s unlikely that doctors will suddenly begin using existing, glutamate-targeting drugs off-label to treat RLS, as many are prohibitively expensive and wouldn’t be covered by insurance. But he’s optimistic that the study can spawn new research that could ultimately help fill the treatment gap.
Shalini Paruthi, MD, an adjunct professor at Saint Louis University, St. Louis, Missouri, and chair of the Restless Legs Syndrome Foundation’s board of directors, sees another benefit.
“The associations found in this study between RLS and other medical disorders may help patients and their physicians take RLS more seriously,” Dr. Paruthi said, “as treating RLS can lead to multiple other downstream improvements in their health.”
A version of this article appeared on Medscape.com.
For decades, scientists have been trying to unravel the mysteries of restless legs syndrome (RLS), a poorly understood and underdiagnosed neurological disorder causing itching, crawling, and aching sensations in the limbs that can only be relieved with movement.
A sweeping new genetic study, coauthored by an international team of 70 — including the world’s leading RLS experts — marks a significant advance in that pursuit. Published in Nature Genetics, it is the largest genetic study of the disease to date.
“It’s a huge step forward for patients as well as the scientific community,” said lead author Juliane Winkelmann, MD, a neurologist and geneticist with the Technical University of Munich, Munich, Germany, who’s been studying and treating patients with RLS for 30 years. “We believe it will allow us to better predict the likelihood of developing RLS and investigate new ways to prevent and modify it.”
The common condition, affecting about 1 in 10 adults, was first described centuries ago — by English physician Thomas Willis in the late 1600s. And while we know a lot more about it today — it’s familial in about half of all patients and has been linked to iron deficiency, among other conditions — its exact cause remains unknown.
With preferred drugs long prescribed to quell symptoms shown in recent years to actually worsen the disorder over time, doctors and patients are hungry for alternatives to treat or prevent the sleep-sabotaging condition.
“The main treatments that everybody continues to use are actually making people worse,” said Andrew Berkowski, MD, a Michigan-based neurologist and RLS specialist not involved in the study. These drugs — dopamine agonists such as levodopa and pramipexole — can also potentially cause drug dependence, Dr. Berkowski said.
How This Could Lead to New Treatments
In the new study, the group analyzed three genome-wide association studies, collectively including genetic information from 116,647 patients with RLS and more than 1.5 million people without it.
They identified 161 gene regions believed to contribute to RLS, about a dozen of which are already targets for existing drugs for other conditions. Previously, scientists knew of only 22 associated genes.
“It’s useful in that it identifies new genes we haven’t looked at yet and reinforces the science behind some of the older genes,” said Dr. Berkowski. “It’s given us some ideas for different things we should look into more closely.”
Among the top candidates are genes that influence glutamate — a key chemical messenger that helps move signals between nerve cells in the brain.
Several anticonvulsant and antiseizure drugs, including perampanel, lamotrigine, and gabapentin, target glutamate receptors. And at least one small study has shown perampanel prescribed off-label can improve RLS symptoms.
“Compared to starting at the beginning and developing an entirely new chemical entity, we could run clinical trials using these alternatives in RLS patients,” said the study’s first author, Steven Bell, PhD, an epidemiologist with the University of Cambridge, Cambridge, England.
The study also confirmed the MIES1 gene, which is related to dopamine expression and iron homeostasis, as a key genetic contributor to RLS risk. Low levels of iron in the blood have long been thought to trigger RLS.
The Role of Gene-Environment Interactions
Through additional data analysis, the team confirmed that many of the genes associated with RLS play a role in development of the central nervous system.
“This strongly supports the hypothesis that restless legs syndrome is a neurodevelopmental disorder that develops during the embryo stage but doesn’t clinically manifest until later in life,” said Dr. Winkelmann.
About half of people with RLS report some family history of it.
But not all with a genetic predisposition will develop symptoms.
For instance, the study found that while the same gene regions seem to be associated with risk in both men and women, in practice, RLS is twice as common among women. This suggests that something about women’s lives — menstruation, childbirth, metabolism — may switch a preexisting risk into a reality.
“We know that genetic factors play an important role in making people susceptible to the disease,” said Dr. Winkelmann, “but in the end, it is the interaction between genetic and environmental factors that may lead to its manifestation.”
The study also found associations between RLS and depression and suggests that RLS may increase the risk for type 2 diabetes.
Improving RLS Care
A potentially useful tool coming out of the study was a “polygenic risk score,” which the researchers developed based on the genes identified. When they tested how accurately the score could predict whether someone would develop RLS within the next 5 years, the model got it right about 90% of the time.
Dr. Winkelmann imagines a day when someone could use such a polygenic risk score to flag the high risk for RLS early enough to take action to try to prevent it. More research is necessary to determine precisely what that action would be.
As for treatments, Dr. Berkowski thinks it’s unlikely that doctors will suddenly begin using existing, glutamate-targeting drugs off-label to treat RLS, as many are prohibitively expensive and wouldn’t be covered by insurance. But he’s optimistic that the study can spawn new research that could ultimately help fill the treatment gap.
Shalini Paruthi, MD, an adjunct professor at Saint Louis University, St. Louis, Missouri, and chair of the Restless Legs Syndrome Foundation’s board of directors, sees another benefit.
“The associations found in this study between RLS and other medical disorders may help patients and their physicians take RLS more seriously,” Dr. Paruthi said, “as treating RLS can lead to multiple other downstream improvements in their health.”
A version of this article appeared on Medscape.com.
New Transparent AI Predicts Breast Cancer 5 Years Out
A new way of using artificial intelligence (AI) can predict breast cancer 5 years in advance with impressive accuracy — and unlike previous AI models, we know how this one works.
The new AI system, called AsymMirai, simplifies previous models by solely comparing differences between right and left breasts to predict risk. It could potentially save lives, prevent unnecessary testing, and save the healthcare system money, its creators say.
“With traditional AI, you ask it a question and it spits out an answer, but no one really knows how it makes its decisions. It’s a black box,” said Jon Donnelly, a PhD student in the department of computer science at Duke University, Durham, North Carolina, and first author on a new paper in Radiology describing the model.
“With our approach, people know how the algorithm comes up with its output so they can fact-check it and trust it,” he said.
One in eight women will develop invasive breast cancer, and 1 in 39 will die from it. Mammograms miss about 20% of breast cancers. (The shortcomings of genetic screening and mammograms received extra attention recently when actress Olivia Munn disclosed that she’d been treated for an aggressive form of breast cancer despite a normal mammogram and a negative genetic test.)
The model could help doctors bring the often-abstract idea of AI to the bedside in a meaningful way, said radiologist Vivianne Freitas, MD, assistant professor of medical imaging at the University of Toronto.
“This marks a new chapter in the field of AI,” said Dr. Freitas, who authored an editorial lauding the new paper. “It makes AI more tangible and understandable, thereby improving its potential for acceptance.”
AI as a Second Set of Eyes
Mr. Donnelly described AsymMirai as a simpler, more transparent, and easier-to-use version of Mirai, a breakthrough AI model which made headlines in 2021 with its promise to determine with unprecedented accuracy whether a patient is likely to get breast cancer within the next 5 years.
Mirai identified up to twice as many future cancer diagnoses as the conventional risk calculator Tyrer-Cuzick. It also maintained accuracy across a diverse set of patients — a notable plus for two fields (AI and healthcare) notorious for delivering poorer results for minorities.
Tyrer-Cuzick and other lower-tech risk calculators use personal and family history to statistically calculate risk. Mirai, on the other hand, analyzes countless bits of raw data embedded in a mammogram to decipher patterns a radiologist’s eyes may not catch. Four images, including two angles from each breast, are fed into the model, which produces a score between 0 and 1 to indicate the person’s risk of getting breast cancer in 1, 3, or 5 years.
But even Mirai’s creators have conceded they didn’t know exactly how it arrives at that score — a fact that has fueled hesitancy among clinicians.
Study coauthor Fides Schwartz, MD, a radiologist at Brigham and Women’s Hospital, Boston, said researchers were able to crack the code on Mirai’s “black box,” finding that its scores were largely determined by assessing subtle differences between right breast tissue and left breast tissue.
Knowing this, the research team simplified the model to predict risk based solely on “local bilateral dissimilarity.” AsymMirai was born.
The team then used AsymMirai to look back at > 200,000 mammograms from nearly 82,000 patients. They found it worked nearly as well as its predecessor, assigning a higher risk to those who would go on to develop cancer 66% of the time (vs Mirai’s 71%). In patients where it noticed the same asymmetry multiple years in a row it worked even better, with an 88% chance of giving people who would develop cancer later a higher score than those who would not.
“We found that we can, with surprisingly high accuracy, predict whether a woman will develop cancer in the next 1-5 years based solely on localized differences between her left and right breast tissue,” said Mr. Donnelly.
Dr. Schwartz imagines a day when radiologists could use the model to help develop personalized screening strategies for patients. Doctors might advise those with higher scores to get screened more often than guidelines suggest, supplement mammograms with an MRI , and keep a close watch on trouble spots identified by AI.
“For people with really low risk, on the other hand, maybe we can save them an annual exam that’s not super pleasant and might not be necessary,” said Dr. Schwartz.
Cautious Optimism
Robert Smith, PhD, senior vice president of early cancer detection science at the American Cancer Society, noted that AI has been used for decades to try to reduce radiologists’ workload and improve diagnoses.
“But AI just never really lived up to its fullest potential,” Dr. Smith said, “quite often because it was being used as a crutch by inexperienced radiologists who, instead of interpreting the mammogram and then seeing what AI had to say ended up letting AI do most of the work which, frankly, just wasn’t that accurate.”
He’s hopeful that newer, more sophisticated iterations of AI medical imaging platforms (roughly 18-20 models are in development) can ultimately save women’s lives, particularly in areas where radiologists are in short supply.
But he believes it will be a long time before doctors, or their patients, are willing to risk postponing a mammogram based on an algorithm.
A version of this article appeared on Medscape.com.
A new way of using artificial intelligence (AI) can predict breast cancer 5 years in advance with impressive accuracy — and unlike previous AI models, we know how this one works.
The new AI system, called AsymMirai, simplifies previous models by solely comparing differences between right and left breasts to predict risk. It could potentially save lives, prevent unnecessary testing, and save the healthcare system money, its creators say.
“With traditional AI, you ask it a question and it spits out an answer, but no one really knows how it makes its decisions. It’s a black box,” said Jon Donnelly, a PhD student in the department of computer science at Duke University, Durham, North Carolina, and first author on a new paper in Radiology describing the model.
“With our approach, people know how the algorithm comes up with its output so they can fact-check it and trust it,” he said.
One in eight women will develop invasive breast cancer, and 1 in 39 will die from it. Mammograms miss about 20% of breast cancers. (The shortcomings of genetic screening and mammograms received extra attention recently when actress Olivia Munn disclosed that she’d been treated for an aggressive form of breast cancer despite a normal mammogram and a negative genetic test.)
The model could help doctors bring the often-abstract idea of AI to the bedside in a meaningful way, said radiologist Vivianne Freitas, MD, assistant professor of medical imaging at the University of Toronto.
“This marks a new chapter in the field of AI,” said Dr. Freitas, who authored an editorial lauding the new paper. “It makes AI more tangible and understandable, thereby improving its potential for acceptance.”
AI as a Second Set of Eyes
Mr. Donnelly described AsymMirai as a simpler, more transparent, and easier-to-use version of Mirai, a breakthrough AI model which made headlines in 2021 with its promise to determine with unprecedented accuracy whether a patient is likely to get breast cancer within the next 5 years.
Mirai identified up to twice as many future cancer diagnoses as the conventional risk calculator Tyrer-Cuzick. It also maintained accuracy across a diverse set of patients — a notable plus for two fields (AI and healthcare) notorious for delivering poorer results for minorities.
Tyrer-Cuzick and other lower-tech risk calculators use personal and family history to statistically calculate risk. Mirai, on the other hand, analyzes countless bits of raw data embedded in a mammogram to decipher patterns a radiologist’s eyes may not catch. Four images, including two angles from each breast, are fed into the model, which produces a score between 0 and 1 to indicate the person’s risk of getting breast cancer in 1, 3, or 5 years.
But even Mirai’s creators have conceded they didn’t know exactly how it arrives at that score — a fact that has fueled hesitancy among clinicians.
Study coauthor Fides Schwartz, MD, a radiologist at Brigham and Women’s Hospital, Boston, said researchers were able to crack the code on Mirai’s “black box,” finding that its scores were largely determined by assessing subtle differences between right breast tissue and left breast tissue.
Knowing this, the research team simplified the model to predict risk based solely on “local bilateral dissimilarity.” AsymMirai was born.
The team then used AsymMirai to look back at > 200,000 mammograms from nearly 82,000 patients. They found it worked nearly as well as its predecessor, assigning a higher risk to those who would go on to develop cancer 66% of the time (vs Mirai’s 71%). In patients where it noticed the same asymmetry multiple years in a row it worked even better, with an 88% chance of giving people who would develop cancer later a higher score than those who would not.
“We found that we can, with surprisingly high accuracy, predict whether a woman will develop cancer in the next 1-5 years based solely on localized differences between her left and right breast tissue,” said Mr. Donnelly.
Dr. Schwartz imagines a day when radiologists could use the model to help develop personalized screening strategies for patients. Doctors might advise those with higher scores to get screened more often than guidelines suggest, supplement mammograms with an MRI , and keep a close watch on trouble spots identified by AI.
“For people with really low risk, on the other hand, maybe we can save them an annual exam that’s not super pleasant and might not be necessary,” said Dr. Schwartz.
Cautious Optimism
Robert Smith, PhD, senior vice president of early cancer detection science at the American Cancer Society, noted that AI has been used for decades to try to reduce radiologists’ workload and improve diagnoses.
“But AI just never really lived up to its fullest potential,” Dr. Smith said, “quite often because it was being used as a crutch by inexperienced radiologists who, instead of interpreting the mammogram and then seeing what AI had to say ended up letting AI do most of the work which, frankly, just wasn’t that accurate.”
He’s hopeful that newer, more sophisticated iterations of AI medical imaging platforms (roughly 18-20 models are in development) can ultimately save women’s lives, particularly in areas where radiologists are in short supply.
But he believes it will be a long time before doctors, or their patients, are willing to risk postponing a mammogram based on an algorithm.
A version of this article appeared on Medscape.com.
A new way of using artificial intelligence (AI) can predict breast cancer 5 years in advance with impressive accuracy — and unlike previous AI models, we know how this one works.
The new AI system, called AsymMirai, simplifies previous models by solely comparing differences between right and left breasts to predict risk. It could potentially save lives, prevent unnecessary testing, and save the healthcare system money, its creators say.
“With traditional AI, you ask it a question and it spits out an answer, but no one really knows how it makes its decisions. It’s a black box,” said Jon Donnelly, a PhD student in the department of computer science at Duke University, Durham, North Carolina, and first author on a new paper in Radiology describing the model.
“With our approach, people know how the algorithm comes up with its output so they can fact-check it and trust it,” he said.
One in eight women will develop invasive breast cancer, and 1 in 39 will die from it. Mammograms miss about 20% of breast cancers. (The shortcomings of genetic screening and mammograms received extra attention recently when actress Olivia Munn disclosed that she’d been treated for an aggressive form of breast cancer despite a normal mammogram and a negative genetic test.)
The model could help doctors bring the often-abstract idea of AI to the bedside in a meaningful way, said radiologist Vivianne Freitas, MD, assistant professor of medical imaging at the University of Toronto.
“This marks a new chapter in the field of AI,” said Dr. Freitas, who authored an editorial lauding the new paper. “It makes AI more tangible and understandable, thereby improving its potential for acceptance.”
AI as a Second Set of Eyes
Mr. Donnelly described AsymMirai as a simpler, more transparent, and easier-to-use version of Mirai, a breakthrough AI model which made headlines in 2021 with its promise to determine with unprecedented accuracy whether a patient is likely to get breast cancer within the next 5 years.
Mirai identified up to twice as many future cancer diagnoses as the conventional risk calculator Tyrer-Cuzick. It also maintained accuracy across a diverse set of patients — a notable plus for two fields (AI and healthcare) notorious for delivering poorer results for minorities.
Tyrer-Cuzick and other lower-tech risk calculators use personal and family history to statistically calculate risk. Mirai, on the other hand, analyzes countless bits of raw data embedded in a mammogram to decipher patterns a radiologist’s eyes may not catch. Four images, including two angles from each breast, are fed into the model, which produces a score between 0 and 1 to indicate the person’s risk of getting breast cancer in 1, 3, or 5 years.
But even Mirai’s creators have conceded they didn’t know exactly how it arrives at that score — a fact that has fueled hesitancy among clinicians.
Study coauthor Fides Schwartz, MD, a radiologist at Brigham and Women’s Hospital, Boston, said researchers were able to crack the code on Mirai’s “black box,” finding that its scores were largely determined by assessing subtle differences between right breast tissue and left breast tissue.
Knowing this, the research team simplified the model to predict risk based solely on “local bilateral dissimilarity.” AsymMirai was born.
The team then used AsymMirai to look back at > 200,000 mammograms from nearly 82,000 patients. They found it worked nearly as well as its predecessor, assigning a higher risk to those who would go on to develop cancer 66% of the time (vs Mirai’s 71%). In patients where it noticed the same asymmetry multiple years in a row it worked even better, with an 88% chance of giving people who would develop cancer later a higher score than those who would not.
“We found that we can, with surprisingly high accuracy, predict whether a woman will develop cancer in the next 1-5 years based solely on localized differences between her left and right breast tissue,” said Mr. Donnelly.
Dr. Schwartz imagines a day when radiologists could use the model to help develop personalized screening strategies for patients. Doctors might advise those with higher scores to get screened more often than guidelines suggest, supplement mammograms with an MRI , and keep a close watch on trouble spots identified by AI.
“For people with really low risk, on the other hand, maybe we can save them an annual exam that’s not super pleasant and might not be necessary,” said Dr. Schwartz.
Cautious Optimism
Robert Smith, PhD, senior vice president of early cancer detection science at the American Cancer Society, noted that AI has been used for decades to try to reduce radiologists’ workload and improve diagnoses.
“But AI just never really lived up to its fullest potential,” Dr. Smith said, “quite often because it was being used as a crutch by inexperienced radiologists who, instead of interpreting the mammogram and then seeing what AI had to say ended up letting AI do most of the work which, frankly, just wasn’t that accurate.”
He’s hopeful that newer, more sophisticated iterations of AI medical imaging platforms (roughly 18-20 models are in development) can ultimately save women’s lives, particularly in areas where radiologists are in short supply.
But he believes it will be a long time before doctors, or their patients, are willing to risk postponing a mammogram based on an algorithm.
A version of this article appeared on Medscape.com.
Next Gen Smart Pills Could Transform Personalized Care
On a November morning in 2022, James Messenger opened wide and swallowed a capsule like no other.
Messenger was no stranger to taking pills.
He’d first experimented with prescription opioids as a teenager in Morgantown, West Virginia, battled addiction on-and-off since, and known more than 70 people who had fatally overdosed. So, when asked to test a new “smart pill” that could detect an overdose in progress and call for help, he didn’t hesitate to join the study.
“I’ve lost pretty much every good friend I’ve ever had to this,” said Mr. Messenger. “This pill could save a lot of lives.”
The new Vitals Monitoring capsule he tested is just one example in a growing effort to radically rethink what the humble pill is capable of.
As far back as 1965, scientists introduced the Heidelberg capsule, an electronic pill that measured acidity from within the gut. In 1994, the University of Buffalo coined the term “smart pill” with a device promising to ferry medicine to a precise spot in the intestine, “like the tiny ship in the film Fantastic Voyage.” And in 2001, the US Food and Drug Administration (FDA) approved the first video capsule endoscope, a miniature-camera-toting pill that enabled noninvasive imaging of the small intestine.
But now, nearly 300 iterations are in various stages of development, according to a 2022 analysis. Advances in materials, imaging, and artificial intelligence (AI) are helping address everything from sleep apnea to HIV/AIDS to gut disorders via real-time tracking and real-time help.
“These technologies could enable us to shift the paradigm from ‘Let’s wait until the patient comes to us and find out what happened’ to ‘Let’s see how things are changing in real time, intervene now, and personalize that intervention,’ ” said Peter Chai, MD, associate professor of emergency medicine and health technology researcher at Brigham and Women’s Hospital in Boston.
Tracking Vitals From the Inside Out
Already, overdose-reversal agents like naloxone are saving lives. But more than 60% of overdoses occur when no one is around to administer them.
“While we need to focus on treatment, we also need to come up with more acute ways to save individuals when treatment doesn’t work or relapse occurs,” said James J. Mahoney III, PhD, director of addictions research at the Rockefeller Neuroscience Institute at West Virginia University (WVU), Morgantown.
Enter Celero Systems, a Massachusetts-based digital health company that has developed a vitamin-sized capsule packed with tiny sensors, microprocessors, and a radio antenna. It can measure breathing, heart rate, and core temperature — all from deep within the gut.
Respiratory distress is a hallmark early sign of an overdose. But it can be hard to monitor from a distance, especially in populations without access to a charged smartwatch.
Dr. Mahoney imagines a day when patients at risk could be given a weekly pill like Celero’s. If their respiratory rate drops below a dangerous level, it could alert loved ones or, better yet, release an overdose-reversal drug.
“It’s early days,” stressed Dr. Mahoney, whose team has been conducting pilot tests of the pill. “But initial data look promising.”
For one study, published in the journal Device in November 2023, the research team administered an overdose of fentanyl to anesthetized pigs with the pill in their stomachs. The capsule was able to detect respiratory depression within a minute and alert researchers via their laptop in time to step in.
When they gave the pill to 10 volunteers undergoing sleep studies at WVU, they found it could detect respiration rate with an accuracy of 93% compared with external monitoring devices — a feature that could also help diagnose sleep apnea or chronic obstructive pulmonary disease without expensive, intrusive tests.
Accuracy for heart rate was nearly 97%.
In another yet-to-be published trial, Dr. Mahoney tested the device with 10 volunteers in a residential treatment center to determine how well it could be tolerated.
Among the participants was Mr. Messenger, who said the thought of being tracked didn’t bother him.
“It was simple — just like taking a multivitamin,” said Mr. Messenger, now 34, sober, and working as a peer recovery support specialist at a hospital in his hometown. “It could be a great way to keep people alive long enough for them to get their head wrapped around the idea of treatment.”
Boosting Medication Adherence
At Brigham and Women’s Hospital, Dr. Chai is experimenting with a different smart pill — one he believes could help curb the ongoing HIV/AIDS epidemic.
Developed by Florida-based etectRx, the ID-Cap consists of a gelatin capsule embedded with a tiny radiofrequency transmitter, similar to the kind in retail antitheft devices. The capsule can be filled with a variety of medications. When swallowed, stomach acid dissolves the gel and activates the transmitter, which sends a signal to a receiver on a smartwatch, smartphone, or wall-mounted reader to confirm the medication was taken. If it isn’t, the patient’s smartphone or smart speaker might nudge them with a reminder or a family member might be notified.
In recent trials of men at a high risk for HIV, the system improved adherence to the once-daily prevention regimen pre-exposure prophylaxis (PrEP) by double digits.
“PrEP is almost 99% effective in preventing HIV, but you have to take it,” said Dr. Chai, who led the trials. “That seems like such a simple thing, but anyone who is chronically on medication can tell you just how difficult it can be.”
The pill is not the first designed to improve adherence. In 2017, the FDA approved the first digital ingestion tracking system, Abilify MyCite, for the treatment of schizophrenia and bipolar disorder. But its maker, Proteus Digital Health, filed for bankruptcy in 2020 after struggling to recruit patients willing to be tracked. (Some expressed privacy concerns. Others disliked the uncomfortable patch that received and forwarded the signal.)
More recent designs have been streamlined to ditch the patch, said etectRx senior vice president of operations Chris Carnes, PhD. And the cost of making a pill this kind of “smart” has come down to about a dollar.
So far, said Dr. Chai, in the patients he’s worked with, perceived benefits generally outweigh privacy concerns.
Studies are now underway in patients with heart disease and tuberculosis, and the company hopes to move into the aging and memory care space where medication-adherence is a serious problem.
“For us, or any company in this space, to succeed, you have to have a strong business case,” said Dr. Carnes. “If family members can keep their loved ones at home a little longer at an additional cost of $30 a month, that’s a no-brainer.”
Pillcams 2.0
Twenty-three years ago, the first video capsule endoscopy made it possible to image the small intestine via a tiny camera you swallow.
Such “pillcams” offered a more patient-friendly way to diagnose small bowel disorders, such as gastrointestinal bleeding and Crohn’s disease. Rather than undergoing sedation or anesthesia, as required during tube-based endoscopy, patients can go about their day as the pill painlessly passes through their gastrointestinal (GI) tract, capturing and recording data and images.
But the pills have their downsides.
Because they move passively, driven by movement in the intestine, they can miss trouble spots. Their ability to image the esophagus, stomach, and colon has proven limited. And unlike other procedures, like colonoscopy, they can’t intervene with therapy, like removing polyps.
The pillcam “had so much promise, to sort of revolutionize endoscopy, but it never really got the adoption that it seemed like it might,” said Andrew Meltzer, MD, professor of emergency medicine at the GW School of Medicine and Health Sciences in Washington.
That could soon change, he said, thanks to advances in locomotion and AI.
In a recent study of 40 patients, Dr. Meltzer tested a new magnetically controlled capsule endoscopy. Standing at a patient’s side, he could use a joystick to steer the pill around the stomach, capturing images in real time.
The pilot study, published in June 2023, found that the pill clearly identified six key stomach landmarks accurately 95% of the time and didn’t miss any lesions caught with traditional endoscopy. Notably, 80% of the patients preferred the pillcam over the tube.
“They are awake. They can go to work as soon as they leave. And it’s easy for them to tolerate,” Dr. Meltzer said.
More research is necessary, but Dr. Meltzer believes the technology could be particularly useful in the emergency department, allowing doctors to rule out high-risk bleeds in the stomach on the spot without admitting patients unnecessarily or making them return for a traditional scope.
“It has the potential to increase screening and provide more cost-effective care in emergencies,” he said.
It could also be useful in the telemedicine space, allowing a doctor to “drive” the pill from afar to diagnose a distant patient.
Someday, AI could enable the capsule to drive itself, so a doctor could merely press a button and wait. Or it could be adapted to treat what it finds, like administering a drug or cauterizing a bleed.
“If we can come up with a Mars rover which can explore other planets, we should be able to have something that can explore the stomach remotely,” Dr. Meltzer said.
Swallowing the Future
At the California Institute of Technology, researchers have developed a “location-aware” smart pill that uses magnetic fields to help pinpoint its location in the twists and turns of intestines. This could be useful for monitoring food in the GI tract to determine why things aren’t moving.
Other researchers are using AI models to enhance the transmission of video from inside the body and reduce the time it takes to interpret images.
One group at the Massachusetts Institute of Technology has developed a vibrating weight loss capsule designed to stimulate receptors in the gut to signal the brain that the person is full.
Not everyone is a fan of the smart-pill revolution. Some critics have raised concerns about privacy. Others fear that doctors risk yielding too much power to technology. Even those who are excited about the pills’ possibilities temper their optimism with caution.
None of these smart pills have gone mainstream yet in clinical practice, said Vivek Kaul, MD, professor of medicine at the University of Rochester Medical Center, Rochester, New York, and secretary general of the World Gastroenterology Organization.
Clinical validation, accessibility, and insurance coverage “will be critical in shaping their role,” he said. “But overall, it would be fair to state that this technology has come of age and the future is bright.”
A version of this article appeared on Medscape.com.
On a November morning in 2022, James Messenger opened wide and swallowed a capsule like no other.
Messenger was no stranger to taking pills.
He’d first experimented with prescription opioids as a teenager in Morgantown, West Virginia, battled addiction on-and-off since, and known more than 70 people who had fatally overdosed. So, when asked to test a new “smart pill” that could detect an overdose in progress and call for help, he didn’t hesitate to join the study.
“I’ve lost pretty much every good friend I’ve ever had to this,” said Mr. Messenger. “This pill could save a lot of lives.”
The new Vitals Monitoring capsule he tested is just one example in a growing effort to radically rethink what the humble pill is capable of.
As far back as 1965, scientists introduced the Heidelberg capsule, an electronic pill that measured acidity from within the gut. In 1994, the University of Buffalo coined the term “smart pill” with a device promising to ferry medicine to a precise spot in the intestine, “like the tiny ship in the film Fantastic Voyage.” And in 2001, the US Food and Drug Administration (FDA) approved the first video capsule endoscope, a miniature-camera-toting pill that enabled noninvasive imaging of the small intestine.
But now, nearly 300 iterations are in various stages of development, according to a 2022 analysis. Advances in materials, imaging, and artificial intelligence (AI) are helping address everything from sleep apnea to HIV/AIDS to gut disorders via real-time tracking and real-time help.
“These technologies could enable us to shift the paradigm from ‘Let’s wait until the patient comes to us and find out what happened’ to ‘Let’s see how things are changing in real time, intervene now, and personalize that intervention,’ ” said Peter Chai, MD, associate professor of emergency medicine and health technology researcher at Brigham and Women’s Hospital in Boston.
Tracking Vitals From the Inside Out
Already, overdose-reversal agents like naloxone are saving lives. But more than 60% of overdoses occur when no one is around to administer them.
“While we need to focus on treatment, we also need to come up with more acute ways to save individuals when treatment doesn’t work or relapse occurs,” said James J. Mahoney III, PhD, director of addictions research at the Rockefeller Neuroscience Institute at West Virginia University (WVU), Morgantown.
Enter Celero Systems, a Massachusetts-based digital health company that has developed a vitamin-sized capsule packed with tiny sensors, microprocessors, and a radio antenna. It can measure breathing, heart rate, and core temperature — all from deep within the gut.
Respiratory distress is a hallmark early sign of an overdose. But it can be hard to monitor from a distance, especially in populations without access to a charged smartwatch.
Dr. Mahoney imagines a day when patients at risk could be given a weekly pill like Celero’s. If their respiratory rate drops below a dangerous level, it could alert loved ones or, better yet, release an overdose-reversal drug.
“It’s early days,” stressed Dr. Mahoney, whose team has been conducting pilot tests of the pill. “But initial data look promising.”
For one study, published in the journal Device in November 2023, the research team administered an overdose of fentanyl to anesthetized pigs with the pill in their stomachs. The capsule was able to detect respiratory depression within a minute and alert researchers via their laptop in time to step in.
When they gave the pill to 10 volunteers undergoing sleep studies at WVU, they found it could detect respiration rate with an accuracy of 93% compared with external monitoring devices — a feature that could also help diagnose sleep apnea or chronic obstructive pulmonary disease without expensive, intrusive tests.
Accuracy for heart rate was nearly 97%.
In another yet-to-be published trial, Dr. Mahoney tested the device with 10 volunteers in a residential treatment center to determine how well it could be tolerated.
Among the participants was Mr. Messenger, who said the thought of being tracked didn’t bother him.
“It was simple — just like taking a multivitamin,” said Mr. Messenger, now 34, sober, and working as a peer recovery support specialist at a hospital in his hometown. “It could be a great way to keep people alive long enough for them to get their head wrapped around the idea of treatment.”
Boosting Medication Adherence
At Brigham and Women’s Hospital, Dr. Chai is experimenting with a different smart pill — one he believes could help curb the ongoing HIV/AIDS epidemic.
Developed by Florida-based etectRx, the ID-Cap consists of a gelatin capsule embedded with a tiny radiofrequency transmitter, similar to the kind in retail antitheft devices. The capsule can be filled with a variety of medications. When swallowed, stomach acid dissolves the gel and activates the transmitter, which sends a signal to a receiver on a smartwatch, smartphone, or wall-mounted reader to confirm the medication was taken. If it isn’t, the patient’s smartphone or smart speaker might nudge them with a reminder or a family member might be notified.
In recent trials of men at a high risk for HIV, the system improved adherence to the once-daily prevention regimen pre-exposure prophylaxis (PrEP) by double digits.
“PrEP is almost 99% effective in preventing HIV, but you have to take it,” said Dr. Chai, who led the trials. “That seems like such a simple thing, but anyone who is chronically on medication can tell you just how difficult it can be.”
The pill is not the first designed to improve adherence. In 2017, the FDA approved the first digital ingestion tracking system, Abilify MyCite, for the treatment of schizophrenia and bipolar disorder. But its maker, Proteus Digital Health, filed for bankruptcy in 2020 after struggling to recruit patients willing to be tracked. (Some expressed privacy concerns. Others disliked the uncomfortable patch that received and forwarded the signal.)
More recent designs have been streamlined to ditch the patch, said etectRx senior vice president of operations Chris Carnes, PhD. And the cost of making a pill this kind of “smart” has come down to about a dollar.
So far, said Dr. Chai, in the patients he’s worked with, perceived benefits generally outweigh privacy concerns.
Studies are now underway in patients with heart disease and tuberculosis, and the company hopes to move into the aging and memory care space where medication-adherence is a serious problem.
“For us, or any company in this space, to succeed, you have to have a strong business case,” said Dr. Carnes. “If family members can keep their loved ones at home a little longer at an additional cost of $30 a month, that’s a no-brainer.”
Pillcams 2.0
Twenty-three years ago, the first video capsule endoscopy made it possible to image the small intestine via a tiny camera you swallow.
Such “pillcams” offered a more patient-friendly way to diagnose small bowel disorders, such as gastrointestinal bleeding and Crohn’s disease. Rather than undergoing sedation or anesthesia, as required during tube-based endoscopy, patients can go about their day as the pill painlessly passes through their gastrointestinal (GI) tract, capturing and recording data and images.
But the pills have their downsides.
Because they move passively, driven by movement in the intestine, they can miss trouble spots. Their ability to image the esophagus, stomach, and colon has proven limited. And unlike other procedures, like colonoscopy, they can’t intervene with therapy, like removing polyps.
The pillcam “had so much promise, to sort of revolutionize endoscopy, but it never really got the adoption that it seemed like it might,” said Andrew Meltzer, MD, professor of emergency medicine at the GW School of Medicine and Health Sciences in Washington.
That could soon change, he said, thanks to advances in locomotion and AI.
In a recent study of 40 patients, Dr. Meltzer tested a new magnetically controlled capsule endoscopy. Standing at a patient’s side, he could use a joystick to steer the pill around the stomach, capturing images in real time.
The pilot study, published in June 2023, found that the pill clearly identified six key stomach landmarks accurately 95% of the time and didn’t miss any lesions caught with traditional endoscopy. Notably, 80% of the patients preferred the pillcam over the tube.
“They are awake. They can go to work as soon as they leave. And it’s easy for them to tolerate,” Dr. Meltzer said.
More research is necessary, but Dr. Meltzer believes the technology could be particularly useful in the emergency department, allowing doctors to rule out high-risk bleeds in the stomach on the spot without admitting patients unnecessarily or making them return for a traditional scope.
“It has the potential to increase screening and provide more cost-effective care in emergencies,” he said.
It could also be useful in the telemedicine space, allowing a doctor to “drive” the pill from afar to diagnose a distant patient.
Someday, AI could enable the capsule to drive itself, so a doctor could merely press a button and wait. Or it could be adapted to treat what it finds, like administering a drug or cauterizing a bleed.
“If we can come up with a Mars rover which can explore other planets, we should be able to have something that can explore the stomach remotely,” Dr. Meltzer said.
Swallowing the Future
At the California Institute of Technology, researchers have developed a “location-aware” smart pill that uses magnetic fields to help pinpoint its location in the twists and turns of intestines. This could be useful for monitoring food in the GI tract to determine why things aren’t moving.
Other researchers are using AI models to enhance the transmission of video from inside the body and reduce the time it takes to interpret images.
One group at the Massachusetts Institute of Technology has developed a vibrating weight loss capsule designed to stimulate receptors in the gut to signal the brain that the person is full.
Not everyone is a fan of the smart-pill revolution. Some critics have raised concerns about privacy. Others fear that doctors risk yielding too much power to technology. Even those who are excited about the pills’ possibilities temper their optimism with caution.
None of these smart pills have gone mainstream yet in clinical practice, said Vivek Kaul, MD, professor of medicine at the University of Rochester Medical Center, Rochester, New York, and secretary general of the World Gastroenterology Organization.
Clinical validation, accessibility, and insurance coverage “will be critical in shaping their role,” he said. “But overall, it would be fair to state that this technology has come of age and the future is bright.”
A version of this article appeared on Medscape.com.
On a November morning in 2022, James Messenger opened wide and swallowed a capsule like no other.
Messenger was no stranger to taking pills.
He’d first experimented with prescription opioids as a teenager in Morgantown, West Virginia, battled addiction on-and-off since, and known more than 70 people who had fatally overdosed. So, when asked to test a new “smart pill” that could detect an overdose in progress and call for help, he didn’t hesitate to join the study.
“I’ve lost pretty much every good friend I’ve ever had to this,” said Mr. Messenger. “This pill could save a lot of lives.”
The new Vitals Monitoring capsule he tested is just one example in a growing effort to radically rethink what the humble pill is capable of.
As far back as 1965, scientists introduced the Heidelberg capsule, an electronic pill that measured acidity from within the gut. In 1994, the University of Buffalo coined the term “smart pill” with a device promising to ferry medicine to a precise spot in the intestine, “like the tiny ship in the film Fantastic Voyage.” And in 2001, the US Food and Drug Administration (FDA) approved the first video capsule endoscope, a miniature-camera-toting pill that enabled noninvasive imaging of the small intestine.
But now, nearly 300 iterations are in various stages of development, according to a 2022 analysis. Advances in materials, imaging, and artificial intelligence (AI) are helping address everything from sleep apnea to HIV/AIDS to gut disorders via real-time tracking and real-time help.
“These technologies could enable us to shift the paradigm from ‘Let’s wait until the patient comes to us and find out what happened’ to ‘Let’s see how things are changing in real time, intervene now, and personalize that intervention,’ ” said Peter Chai, MD, associate professor of emergency medicine and health technology researcher at Brigham and Women’s Hospital in Boston.
Tracking Vitals From the Inside Out
Already, overdose-reversal agents like naloxone are saving lives. But more than 60% of overdoses occur when no one is around to administer them.
“While we need to focus on treatment, we also need to come up with more acute ways to save individuals when treatment doesn’t work or relapse occurs,” said James J. Mahoney III, PhD, director of addictions research at the Rockefeller Neuroscience Institute at West Virginia University (WVU), Morgantown.
Enter Celero Systems, a Massachusetts-based digital health company that has developed a vitamin-sized capsule packed with tiny sensors, microprocessors, and a radio antenna. It can measure breathing, heart rate, and core temperature — all from deep within the gut.
Respiratory distress is a hallmark early sign of an overdose. But it can be hard to monitor from a distance, especially in populations without access to a charged smartwatch.
Dr. Mahoney imagines a day when patients at risk could be given a weekly pill like Celero’s. If their respiratory rate drops below a dangerous level, it could alert loved ones or, better yet, release an overdose-reversal drug.
“It’s early days,” stressed Dr. Mahoney, whose team has been conducting pilot tests of the pill. “But initial data look promising.”
For one study, published in the journal Device in November 2023, the research team administered an overdose of fentanyl to anesthetized pigs with the pill in their stomachs. The capsule was able to detect respiratory depression within a minute and alert researchers via their laptop in time to step in.
When they gave the pill to 10 volunteers undergoing sleep studies at WVU, they found it could detect respiration rate with an accuracy of 93% compared with external monitoring devices — a feature that could also help diagnose sleep apnea or chronic obstructive pulmonary disease without expensive, intrusive tests.
Accuracy for heart rate was nearly 97%.
In another yet-to-be published trial, Dr. Mahoney tested the device with 10 volunteers in a residential treatment center to determine how well it could be tolerated.
Among the participants was Mr. Messenger, who said the thought of being tracked didn’t bother him.
“It was simple — just like taking a multivitamin,” said Mr. Messenger, now 34, sober, and working as a peer recovery support specialist at a hospital in his hometown. “It could be a great way to keep people alive long enough for them to get their head wrapped around the idea of treatment.”
Boosting Medication Adherence
At Brigham and Women’s Hospital, Dr. Chai is experimenting with a different smart pill — one he believes could help curb the ongoing HIV/AIDS epidemic.
Developed by Florida-based etectRx, the ID-Cap consists of a gelatin capsule embedded with a tiny radiofrequency transmitter, similar to the kind in retail antitheft devices. The capsule can be filled with a variety of medications. When swallowed, stomach acid dissolves the gel and activates the transmitter, which sends a signal to a receiver on a smartwatch, smartphone, or wall-mounted reader to confirm the medication was taken. If it isn’t, the patient’s smartphone or smart speaker might nudge them with a reminder or a family member might be notified.
In recent trials of men at a high risk for HIV, the system improved adherence to the once-daily prevention regimen pre-exposure prophylaxis (PrEP) by double digits.
“PrEP is almost 99% effective in preventing HIV, but you have to take it,” said Dr. Chai, who led the trials. “That seems like such a simple thing, but anyone who is chronically on medication can tell you just how difficult it can be.”
The pill is not the first designed to improve adherence. In 2017, the FDA approved the first digital ingestion tracking system, Abilify MyCite, for the treatment of schizophrenia and bipolar disorder. But its maker, Proteus Digital Health, filed for bankruptcy in 2020 after struggling to recruit patients willing to be tracked. (Some expressed privacy concerns. Others disliked the uncomfortable patch that received and forwarded the signal.)
More recent designs have been streamlined to ditch the patch, said etectRx senior vice president of operations Chris Carnes, PhD. And the cost of making a pill this kind of “smart” has come down to about a dollar.
So far, said Dr. Chai, in the patients he’s worked with, perceived benefits generally outweigh privacy concerns.
Studies are now underway in patients with heart disease and tuberculosis, and the company hopes to move into the aging and memory care space where medication-adherence is a serious problem.
“For us, or any company in this space, to succeed, you have to have a strong business case,” said Dr. Carnes. “If family members can keep their loved ones at home a little longer at an additional cost of $30 a month, that’s a no-brainer.”
Pillcams 2.0
Twenty-three years ago, the first video capsule endoscopy made it possible to image the small intestine via a tiny camera you swallow.
Such “pillcams” offered a more patient-friendly way to diagnose small bowel disorders, such as gastrointestinal bleeding and Crohn’s disease. Rather than undergoing sedation or anesthesia, as required during tube-based endoscopy, patients can go about their day as the pill painlessly passes through their gastrointestinal (GI) tract, capturing and recording data and images.
But the pills have their downsides.
Because they move passively, driven by movement in the intestine, they can miss trouble spots. Their ability to image the esophagus, stomach, and colon has proven limited. And unlike other procedures, like colonoscopy, they can’t intervene with therapy, like removing polyps.
The pillcam “had so much promise, to sort of revolutionize endoscopy, but it never really got the adoption that it seemed like it might,” said Andrew Meltzer, MD, professor of emergency medicine at the GW School of Medicine and Health Sciences in Washington.
That could soon change, he said, thanks to advances in locomotion and AI.
In a recent study of 40 patients, Dr. Meltzer tested a new magnetically controlled capsule endoscopy. Standing at a patient’s side, he could use a joystick to steer the pill around the stomach, capturing images in real time.
The pilot study, published in June 2023, found that the pill clearly identified six key stomach landmarks accurately 95% of the time and didn’t miss any lesions caught with traditional endoscopy. Notably, 80% of the patients preferred the pillcam over the tube.
“They are awake. They can go to work as soon as they leave. And it’s easy for them to tolerate,” Dr. Meltzer said.
More research is necessary, but Dr. Meltzer believes the technology could be particularly useful in the emergency department, allowing doctors to rule out high-risk bleeds in the stomach on the spot without admitting patients unnecessarily or making them return for a traditional scope.
“It has the potential to increase screening and provide more cost-effective care in emergencies,” he said.
It could also be useful in the telemedicine space, allowing a doctor to “drive” the pill from afar to diagnose a distant patient.
Someday, AI could enable the capsule to drive itself, so a doctor could merely press a button and wait. Or it could be adapted to treat what it finds, like administering a drug or cauterizing a bleed.
“If we can come up with a Mars rover which can explore other planets, we should be able to have something that can explore the stomach remotely,” Dr. Meltzer said.
Swallowing the Future
At the California Institute of Technology, researchers have developed a “location-aware” smart pill that uses magnetic fields to help pinpoint its location in the twists and turns of intestines. This could be useful for monitoring food in the GI tract to determine why things aren’t moving.
Other researchers are using AI models to enhance the transmission of video from inside the body and reduce the time it takes to interpret images.
One group at the Massachusetts Institute of Technology has developed a vibrating weight loss capsule designed to stimulate receptors in the gut to signal the brain that the person is full.
Not everyone is a fan of the smart-pill revolution. Some critics have raised concerns about privacy. Others fear that doctors risk yielding too much power to technology. Even those who are excited about the pills’ possibilities temper their optimism with caution.
None of these smart pills have gone mainstream yet in clinical practice, said Vivek Kaul, MD, professor of medicine at the University of Rochester Medical Center, Rochester, New York, and secretary general of the World Gastroenterology Organization.
Clinical validation, accessibility, and insurance coverage “will be critical in shaping their role,” he said. “But overall, it would be fair to state that this technology has come of age and the future is bright.”
A version of this article appeared on Medscape.com.
What causes obesity? More science points to the brain
For much of his life, 32-year-old Michael Smith had a war going on in his head.
After a big meal, he knew he should be full. But an inexplicable hunger would drive him to pick up the fork again.
Cravings for fried chicken or gummy bears overwhelmed him, fueling late-night DoorDash orders that — despite their bounty of fat and sugar — never satisfied him.
He recalls waking up on the couch, half-eaten takeout in his lap, feeling sluggish and out of control.
“It was like I was food drunk,” recalls Smith, who lives in Boston. “I had a moment I looked at myself in the mirror. I was around 380 pounds, and I said, ‘OK, something has got to give.’ “
Smith is among the 42% of U.S. adults living with obesity, a misunderstood and stubbornly hard-to-manage condition that doctors have only recently begun to call a disease. Its root causes have been debated for decades, with studies suggesting everything from genes to lifestyle to a shifting food supply loaded with carbohydrates and ultra-processed foods. Solutions have long targeted self-discipline and a simple “eat less, move more” strategy with remarkably grim results.
Those who successfully slim down tend to gain back 50% of that weight within 2 years, and 80% within 5 years. Meanwhile, the obesity epidemic marches on.
But a new frontier of brain-based therapies — from GLP-1 agonist drugs thought to act on reward and appetite centers to deep brain stimulation aimed at resetting neural circuits — has kindled hope among patients like Smith and the doctors who treat them. The treatments, and theories behind them, are not without controversy. They’re expensive, have side effects, and, critics contend, pull focus from diet and exercise.
But most agree that in the battle against obesity, one crucial organ has been overlooked.
“Obesity, in almost all circumstances, is most likely a disorder of the brain,” said Casey Halpern, MD, associate professor of neurosurgery at the University of Pennsylvania. “What these individuals need is not simply more willpower, but the therapeutic equivalent of an electrician that can make right these connections inside their brain.”
A Break in the Machine
Throughout the day, the machine that is our brain is constantly humming in the background, taking in subtle signals from our gut, hormones, and environment to determine when we’re hungry, how food makes us feel, and whether we are taking in enough energy, or expending too much, to survive.
said Kevin Hall, PhD, an obesity researcher with the National Institute of Diabetes and Digestive and Kidney Diseases. “I liken it to holding your breath. I can do that for a period of time, and I have some conscious control. But eventually, physiology wins out.”
Mounting evidence suggests that in people with obesity, something in the machine is broken.
One seminal 2001 study in The Lancet suggested that, like people addicted to cocaine or alcohol, they lack receptors to the feel-good brain chemical dopamine and overeat in pursuit of the pleasure they lack.
A recent study, not yet published, from Dr. Hall’s lab drew a slightly different conclusion, suggesting that people with obesity actually have too much dopamine, filling up those receptors so the pleasure spike from eating doesn’t feel like much.
“It’s kind of like trying to shout in a noisy room. You’re going to have to shout louder to have the same effect,” said Dr. Hall.
Gut-brain pathways that tell us we’re full may also be impaired.
In another study, Yale researchers tube-fed 500 calories of sugar or fat directly into the stomachs of 28 lean people and 30 people with obesity. Then they observed brain activity using functional magnetic resonance imaging (fMRI).
In lean people, about 30 regions of the brain quieted after the meal, including parts of the striatum (associated with cravings).
In those with obesity, the brain barely responded at all.
“In my clinic, patients will often say ‘I just finished my dinner, but it doesn’t feel like it,’” said senior author Mireille Serlie, MD, PhD, an obesity researcher at the Yale School of Medicine. “It may be that this nutrient-sensing interaction between the gut and the brain is less pronounced or comes too late for them after the meal.”
Dr. Halpern recently identified a brain circuit linking a memory center (hippocampus) to an appetite control region (hypothalamus). In people with obesity and binge eating disorder, the circuit appears jammed. This may cause them to, in a sense, forget they just ate.
“Some of their eating episodes are almost dissociative — they’re not realizing how much they are eating and can’t keep track of it,” he said.
Another brain system works to maintain longer-term homeostasis — or weight stability. Like a set thermostat, it kicks on to trigger hunger and fatigue when it senses we’re low on fat.
The hormone leptin, found in fat cells, sends signals to the hypothalamus to let it know how much energy we have on board.
“If leptin levels go up, it signals the brain that you have too much fat and you should eat less to return to the starting point,” said Rockefeller University geneticist Jeffrey Friedman, MD, PhD, who discovered the hormone in 1994. “If you have too little fat and leptin is low, that will stimulate appetite to return you to the starting point.”
In people with obesity, he said, the thermostat — or set point the body seeks to maintain — is too high.
All this raises a crucial question: How do these circuits and pathways malfunction in the first place?
What Breaks the Brain?
Genes, scientists agree, play a role.
Studies show that genetics underlie as much as 75% of people’s differences in body mass index (BMI), with certain gene combinations raising obesity risk in particular environments.
While hundreds of genes are believed to have a small effect, about a dozen single genes are thought to have a large effect. (Notably, most influence brain function.) For instance, about 6% of people with severe obesity since childhood have mutations in a gene called MC4R (melanocortin 4 receptor), which influences leptin signaling.
Still, genetics alone cannot account for the explosion in obesity in the U.S. over the last 50 years, says epidemiologist Deirdre Tobias, ScD, assistant professor of medicine at Harvard Medical School.
At the population level, “our genes don’t change that much in less than a generation,” she said.
But our food supply has.
Ultra-processed foods — those containing hydrogenated oils, high-fructose corn syrup, flavoring agents, emulsifiers, and other manufactured ingredients — now make up about 60% of the food supply.
“The evidence is fairly consistent indicating that there’s something about these foods that is possibly causing obesity,” said Tobias.
In one telling 2019 study, Dr. Hall and his colleagues brought 20 men and women into a study center to live for a month and tightly controlled their food intake and activity. One group was provided with meals with 80% of calories from ultra-processed food. The other was given meals with no processed food.
The three daily meals provided had the same calories, sugars, fats, fiber, and carbohydrates, and people were told to eat as much as they wanted.
Those on the ultra-processed diet ate about 500 calories more per day, ate faster, and gained weight. Those on the unprocessed diet lost weight.
“This is a stark example of how, when you can change the food environment, you cause really remarkable changes in food intake without people even being aware that they are overeating,” said Dr. Hall.
Just what it is about these relatively novel foods that may trigger overeating is unclear. It could be the crunch, the lack of water content, the engineered balance of sugar/salt/fat, their easy-to-devour texture, or something else.
Some research suggests that the foods may interfere with gut-brain signaling that tells the brain you’re full.
“Evidence is amassing that the nutritional content of processed foods is not accurately conveyed to the brain,” Dana M. Small, PhD, a neuroscientist at Yale, wrote in a recent perspective paper in Science.
Even more concerning: Some animal studies suggest processed foods reprogram the brain to dislike healthy foods.
And once these brain changes are made, they are hard to reverse.
“The problem is, our brain is not wired for this,” said Dr. Halpern. “We are not evolved to eat the food we are eating, so our brain adapts, but it adapts in a negative way that puts us at risk.”
That’s why changing the food environment via public policy must be part of the solution in combating obesity, Dr. Tobias said.
A New Era of Brain-Based Solutions
In the spring of 2021, after years of trying and failing to lose weight via the “move more, eat less” model, Michael Smith began to take a medication called Vyvanse. The drug was approved in 2008 for attention deficit hyperactivity disorder, but since it also influences levels of the hormones dopamine and norepinephrine to reduce cravings, it is now frequently prescribed for binge eating disorder.
“That was pretty much how I got rid of my first 60 to 70 pounds,” Smith said.
A few months later, after he hit a plateau, he had surgery to shrink the size of his stomach — a decision he now second-guesses.
While it kept him from overeating for a time, the fried chicken and gummy bear cravings returned a few months later.
His doctor, Fatima Cody Stanford, MD, put him on a second medication: semaglutide, or Wegovy, the weekly shot approved for weight loss in 2021. It works, in part, by mimicking glucagon-like peptide-1 (GLP-1), a key gut hormone that lets your brain know you are full.
The weight began to fall off again.
Smith’s success story is just one of many that Dr. Stanford, an obesity medicine doctor-scientist at Harvard, has heard in her office in recent years.
“I do not believe these drugs are a panacea,” she said. “There are nonresponders, and those are the patients I take off the medication. But for the high-responders, and there are many of them, they are telling me, ‘Oh my gosh. For the first time in my life, I am not constantly thinking about eating. My life has changed.’”
A Multi-Pronged Approach
Dr. Halpern, at Penn, has also been hearing success stories.
In recent years, he has placed permanent electrodes in the brains of three people with grade III, or severe, obesity and binge eating disorder.
All had tried exercise, dieting, support groups, medication, and weight loss surgery to no avail.
The electrodes modulate an area in the center of the brain called the nucleus accumbens, which in mice studies has been shown to reduce cravings when stimulated.
Thus far, all three are seeing promising results.
“It’s not like I don’t think about food at all,” one of them, Robyn Baldwin, told The New York Times. “But I’m no longer a craving person.”
Dr. Halpern is now extending the trial to more patients and hopes to ultimately include other areas of the brain, including those that involve memory.
He imagines a day when people with severe obesity, who have failed conventional treatments, can walk into a clinic and have their brain circuits assessed to see which ones may be misfiring.
Many might find relief with noninvasive brain stimulation, like transcranial magnetic stimulation (already in use for depression). Others might need a more extreme approach, like the deep brain stimulation, or DBS, therapy Dr. Halpern used.
“Obviously, DBS is hard to scale, so it would have to be reserved for the most severe patients,” he said.
Still, not everyone believes brain-based drugs and surgeries are the answer.
David Ludwig, MD, PhD, a professor of nutrition at the Harvard School of Public Health, played a key role in the discovery of GLP-1 and acknowledges that “of course” the brain influences body composition. But to him, explaining obesity as a disease of the brain oversimplifies it, discounting metabolic factors such as a tendency to store too much fat.
He noted that it’s hard to get drug companies, or any agencies, to fund large clinical trials on simple things like low-carbohydrate diets or exercise programs.
“We need all the tools we can get in the battle against the obesity epidemic, and new technologies are worth exploring,” he said. “However, the success of these drugs should not lead us to deprioritize diet and lifestyle interventions.”
Dr. Stanford, who has received consulting fees from Wegovy, believes the future of treatment lies in a multi-pronged approach, with surgery, medication, and lifestyle changes coalescing in a lasting, but fragile, remission.
“Unfortunately, there is no cure for obesity,” said Dr. Stanford, whose patients often have setbacks and must try new strategies. “There are treatments that work for a while, but they are constantly pushing up against this origin in the brain.”
Smith says understanding this has been a big part of his success.
He is now a leaner and healthier 5-foot-6 and 204 pounds. In addition to taking his medication, he walks to work, goes to the gym twice a week, limits his portions, and tries to reframe the way he thinks about food, viewing it as fuel rather than an indulgence.
Sometimes, when he looks in the mirror, he is reminded of his 380-pound self, and it scares him. He doesn’t want to go back there. He’s confident now that he won’t have to.
“There is this misconception out there that you just need to put the fork down, but I’m learning it’s more complicated than that,” he said. “I intend to treat this as the illness that it is and do what I need to combat it so I’m able to keep this new reality I have built for myself.”
A version of this article appeared on WebMD.com .
For much of his life, 32-year-old Michael Smith had a war going on in his head.
After a big meal, he knew he should be full. But an inexplicable hunger would drive him to pick up the fork again.
Cravings for fried chicken or gummy bears overwhelmed him, fueling late-night DoorDash orders that — despite their bounty of fat and sugar — never satisfied him.
He recalls waking up on the couch, half-eaten takeout in his lap, feeling sluggish and out of control.
“It was like I was food drunk,” recalls Smith, who lives in Boston. “I had a moment I looked at myself in the mirror. I was around 380 pounds, and I said, ‘OK, something has got to give.’ “
Smith is among the 42% of U.S. adults living with obesity, a misunderstood and stubbornly hard-to-manage condition that doctors have only recently begun to call a disease. Its root causes have been debated for decades, with studies suggesting everything from genes to lifestyle to a shifting food supply loaded with carbohydrates and ultra-processed foods. Solutions have long targeted self-discipline and a simple “eat less, move more” strategy with remarkably grim results.
Those who successfully slim down tend to gain back 50% of that weight within 2 years, and 80% within 5 years. Meanwhile, the obesity epidemic marches on.
But a new frontier of brain-based therapies — from GLP-1 agonist drugs thought to act on reward and appetite centers to deep brain stimulation aimed at resetting neural circuits — has kindled hope among patients like Smith and the doctors who treat them. The treatments, and theories behind them, are not without controversy. They’re expensive, have side effects, and, critics contend, pull focus from diet and exercise.
But most agree that in the battle against obesity, one crucial organ has been overlooked.
“Obesity, in almost all circumstances, is most likely a disorder of the brain,” said Casey Halpern, MD, associate professor of neurosurgery at the University of Pennsylvania. “What these individuals need is not simply more willpower, but the therapeutic equivalent of an electrician that can make right these connections inside their brain.”
A Break in the Machine
Throughout the day, the machine that is our brain is constantly humming in the background, taking in subtle signals from our gut, hormones, and environment to determine when we’re hungry, how food makes us feel, and whether we are taking in enough energy, or expending too much, to survive.
said Kevin Hall, PhD, an obesity researcher with the National Institute of Diabetes and Digestive and Kidney Diseases. “I liken it to holding your breath. I can do that for a period of time, and I have some conscious control. But eventually, physiology wins out.”
Mounting evidence suggests that in people with obesity, something in the machine is broken.
One seminal 2001 study in The Lancet suggested that, like people addicted to cocaine or alcohol, they lack receptors to the feel-good brain chemical dopamine and overeat in pursuit of the pleasure they lack.
A recent study, not yet published, from Dr. Hall’s lab drew a slightly different conclusion, suggesting that people with obesity actually have too much dopamine, filling up those receptors so the pleasure spike from eating doesn’t feel like much.
“It’s kind of like trying to shout in a noisy room. You’re going to have to shout louder to have the same effect,” said Dr. Hall.
Gut-brain pathways that tell us we’re full may also be impaired.
In another study, Yale researchers tube-fed 500 calories of sugar or fat directly into the stomachs of 28 lean people and 30 people with obesity. Then they observed brain activity using functional magnetic resonance imaging (fMRI).
In lean people, about 30 regions of the brain quieted after the meal, including parts of the striatum (associated with cravings).
In those with obesity, the brain barely responded at all.
“In my clinic, patients will often say ‘I just finished my dinner, but it doesn’t feel like it,’” said senior author Mireille Serlie, MD, PhD, an obesity researcher at the Yale School of Medicine. “It may be that this nutrient-sensing interaction between the gut and the brain is less pronounced or comes too late for them after the meal.”
Dr. Halpern recently identified a brain circuit linking a memory center (hippocampus) to an appetite control region (hypothalamus). In people with obesity and binge eating disorder, the circuit appears jammed. This may cause them to, in a sense, forget they just ate.
“Some of their eating episodes are almost dissociative — they’re not realizing how much they are eating and can’t keep track of it,” he said.
Another brain system works to maintain longer-term homeostasis — or weight stability. Like a set thermostat, it kicks on to trigger hunger and fatigue when it senses we’re low on fat.
The hormone leptin, found in fat cells, sends signals to the hypothalamus to let it know how much energy we have on board.
“If leptin levels go up, it signals the brain that you have too much fat and you should eat less to return to the starting point,” said Rockefeller University geneticist Jeffrey Friedman, MD, PhD, who discovered the hormone in 1994. “If you have too little fat and leptin is low, that will stimulate appetite to return you to the starting point.”
In people with obesity, he said, the thermostat — or set point the body seeks to maintain — is too high.
All this raises a crucial question: How do these circuits and pathways malfunction in the first place?
What Breaks the Brain?
Genes, scientists agree, play a role.
Studies show that genetics underlie as much as 75% of people’s differences in body mass index (BMI), with certain gene combinations raising obesity risk in particular environments.
While hundreds of genes are believed to have a small effect, about a dozen single genes are thought to have a large effect. (Notably, most influence brain function.) For instance, about 6% of people with severe obesity since childhood have mutations in a gene called MC4R (melanocortin 4 receptor), which influences leptin signaling.
Still, genetics alone cannot account for the explosion in obesity in the U.S. over the last 50 years, says epidemiologist Deirdre Tobias, ScD, assistant professor of medicine at Harvard Medical School.
At the population level, “our genes don’t change that much in less than a generation,” she said.
But our food supply has.
Ultra-processed foods — those containing hydrogenated oils, high-fructose corn syrup, flavoring agents, emulsifiers, and other manufactured ingredients — now make up about 60% of the food supply.
“The evidence is fairly consistent indicating that there’s something about these foods that is possibly causing obesity,” said Tobias.
In one telling 2019 study, Dr. Hall and his colleagues brought 20 men and women into a study center to live for a month and tightly controlled their food intake and activity. One group was provided with meals with 80% of calories from ultra-processed food. The other was given meals with no processed food.
The three daily meals provided had the same calories, sugars, fats, fiber, and carbohydrates, and people were told to eat as much as they wanted.
Those on the ultra-processed diet ate about 500 calories more per day, ate faster, and gained weight. Those on the unprocessed diet lost weight.
“This is a stark example of how, when you can change the food environment, you cause really remarkable changes in food intake without people even being aware that they are overeating,” said Dr. Hall.
Just what it is about these relatively novel foods that may trigger overeating is unclear. It could be the crunch, the lack of water content, the engineered balance of sugar/salt/fat, their easy-to-devour texture, or something else.
Some research suggests that the foods may interfere with gut-brain signaling that tells the brain you’re full.
“Evidence is amassing that the nutritional content of processed foods is not accurately conveyed to the brain,” Dana M. Small, PhD, a neuroscientist at Yale, wrote in a recent perspective paper in Science.
Even more concerning: Some animal studies suggest processed foods reprogram the brain to dislike healthy foods.
And once these brain changes are made, they are hard to reverse.
“The problem is, our brain is not wired for this,” said Dr. Halpern. “We are not evolved to eat the food we are eating, so our brain adapts, but it adapts in a negative way that puts us at risk.”
That’s why changing the food environment via public policy must be part of the solution in combating obesity, Dr. Tobias said.
A New Era of Brain-Based Solutions
In the spring of 2021, after years of trying and failing to lose weight via the “move more, eat less” model, Michael Smith began to take a medication called Vyvanse. The drug was approved in 2008 for attention deficit hyperactivity disorder, but since it also influences levels of the hormones dopamine and norepinephrine to reduce cravings, it is now frequently prescribed for binge eating disorder.
“That was pretty much how I got rid of my first 60 to 70 pounds,” Smith said.
A few months later, after he hit a plateau, he had surgery to shrink the size of his stomach — a decision he now second-guesses.
While it kept him from overeating for a time, the fried chicken and gummy bear cravings returned a few months later.
His doctor, Fatima Cody Stanford, MD, put him on a second medication: semaglutide, or Wegovy, the weekly shot approved for weight loss in 2021. It works, in part, by mimicking glucagon-like peptide-1 (GLP-1), a key gut hormone that lets your brain know you are full.
The weight began to fall off again.
Smith’s success story is just one of many that Dr. Stanford, an obesity medicine doctor-scientist at Harvard, has heard in her office in recent years.
“I do not believe these drugs are a panacea,” she said. “There are nonresponders, and those are the patients I take off the medication. But for the high-responders, and there are many of them, they are telling me, ‘Oh my gosh. For the first time in my life, I am not constantly thinking about eating. My life has changed.’”
A Multi-Pronged Approach
Dr. Halpern, at Penn, has also been hearing success stories.
In recent years, he has placed permanent electrodes in the brains of three people with grade III, or severe, obesity and binge eating disorder.
All had tried exercise, dieting, support groups, medication, and weight loss surgery to no avail.
The electrodes modulate an area in the center of the brain called the nucleus accumbens, which in mice studies has been shown to reduce cravings when stimulated.
Thus far, all three are seeing promising results.
“It’s not like I don’t think about food at all,” one of them, Robyn Baldwin, told The New York Times. “But I’m no longer a craving person.”
Dr. Halpern is now extending the trial to more patients and hopes to ultimately include other areas of the brain, including those that involve memory.
He imagines a day when people with severe obesity, who have failed conventional treatments, can walk into a clinic and have their brain circuits assessed to see which ones may be misfiring.
Many might find relief with noninvasive brain stimulation, like transcranial magnetic stimulation (already in use for depression). Others might need a more extreme approach, like the deep brain stimulation, or DBS, therapy Dr. Halpern used.
“Obviously, DBS is hard to scale, so it would have to be reserved for the most severe patients,” he said.
Still, not everyone believes brain-based drugs and surgeries are the answer.
David Ludwig, MD, PhD, a professor of nutrition at the Harvard School of Public Health, played a key role in the discovery of GLP-1 and acknowledges that “of course” the brain influences body composition. But to him, explaining obesity as a disease of the brain oversimplifies it, discounting metabolic factors such as a tendency to store too much fat.
He noted that it’s hard to get drug companies, or any agencies, to fund large clinical trials on simple things like low-carbohydrate diets or exercise programs.
“We need all the tools we can get in the battle against the obesity epidemic, and new technologies are worth exploring,” he said. “However, the success of these drugs should not lead us to deprioritize diet and lifestyle interventions.”
Dr. Stanford, who has received consulting fees from Wegovy, believes the future of treatment lies in a multi-pronged approach, with surgery, medication, and lifestyle changes coalescing in a lasting, but fragile, remission.
“Unfortunately, there is no cure for obesity,” said Dr. Stanford, whose patients often have setbacks and must try new strategies. “There are treatments that work for a while, but they are constantly pushing up against this origin in the brain.”
Smith says understanding this has been a big part of his success.
He is now a leaner and healthier 5-foot-6 and 204 pounds. In addition to taking his medication, he walks to work, goes to the gym twice a week, limits his portions, and tries to reframe the way he thinks about food, viewing it as fuel rather than an indulgence.
Sometimes, when he looks in the mirror, he is reminded of his 380-pound self, and it scares him. He doesn’t want to go back there. He’s confident now that he won’t have to.
“There is this misconception out there that you just need to put the fork down, but I’m learning it’s more complicated than that,” he said. “I intend to treat this as the illness that it is and do what I need to combat it so I’m able to keep this new reality I have built for myself.”
A version of this article appeared on WebMD.com .
For much of his life, 32-year-old Michael Smith had a war going on in his head.
After a big meal, he knew he should be full. But an inexplicable hunger would drive him to pick up the fork again.
Cravings for fried chicken or gummy bears overwhelmed him, fueling late-night DoorDash orders that — despite their bounty of fat and sugar — never satisfied him.
He recalls waking up on the couch, half-eaten takeout in his lap, feeling sluggish and out of control.
“It was like I was food drunk,” recalls Smith, who lives in Boston. “I had a moment I looked at myself in the mirror. I was around 380 pounds, and I said, ‘OK, something has got to give.’ “
Smith is among the 42% of U.S. adults living with obesity, a misunderstood and stubbornly hard-to-manage condition that doctors have only recently begun to call a disease. Its root causes have been debated for decades, with studies suggesting everything from genes to lifestyle to a shifting food supply loaded with carbohydrates and ultra-processed foods. Solutions have long targeted self-discipline and a simple “eat less, move more” strategy with remarkably grim results.
Those who successfully slim down tend to gain back 50% of that weight within 2 years, and 80% within 5 years. Meanwhile, the obesity epidemic marches on.
But a new frontier of brain-based therapies — from GLP-1 agonist drugs thought to act on reward and appetite centers to deep brain stimulation aimed at resetting neural circuits — has kindled hope among patients like Smith and the doctors who treat them. The treatments, and theories behind them, are not without controversy. They’re expensive, have side effects, and, critics contend, pull focus from diet and exercise.
But most agree that in the battle against obesity, one crucial organ has been overlooked.
“Obesity, in almost all circumstances, is most likely a disorder of the brain,” said Casey Halpern, MD, associate professor of neurosurgery at the University of Pennsylvania. “What these individuals need is not simply more willpower, but the therapeutic equivalent of an electrician that can make right these connections inside their brain.”
A Break in the Machine
Throughout the day, the machine that is our brain is constantly humming in the background, taking in subtle signals from our gut, hormones, and environment to determine when we’re hungry, how food makes us feel, and whether we are taking in enough energy, or expending too much, to survive.
said Kevin Hall, PhD, an obesity researcher with the National Institute of Diabetes and Digestive and Kidney Diseases. “I liken it to holding your breath. I can do that for a period of time, and I have some conscious control. But eventually, physiology wins out.”
Mounting evidence suggests that in people with obesity, something in the machine is broken.
One seminal 2001 study in The Lancet suggested that, like people addicted to cocaine or alcohol, they lack receptors to the feel-good brain chemical dopamine and overeat in pursuit of the pleasure they lack.
A recent study, not yet published, from Dr. Hall’s lab drew a slightly different conclusion, suggesting that people with obesity actually have too much dopamine, filling up those receptors so the pleasure spike from eating doesn’t feel like much.
“It’s kind of like trying to shout in a noisy room. You’re going to have to shout louder to have the same effect,” said Dr. Hall.
Gut-brain pathways that tell us we’re full may also be impaired.
In another study, Yale researchers tube-fed 500 calories of sugar or fat directly into the stomachs of 28 lean people and 30 people with obesity. Then they observed brain activity using functional magnetic resonance imaging (fMRI).
In lean people, about 30 regions of the brain quieted after the meal, including parts of the striatum (associated with cravings).
In those with obesity, the brain barely responded at all.
“In my clinic, patients will often say ‘I just finished my dinner, but it doesn’t feel like it,’” said senior author Mireille Serlie, MD, PhD, an obesity researcher at the Yale School of Medicine. “It may be that this nutrient-sensing interaction between the gut and the brain is less pronounced or comes too late for them after the meal.”
Dr. Halpern recently identified a brain circuit linking a memory center (hippocampus) to an appetite control region (hypothalamus). In people with obesity and binge eating disorder, the circuit appears jammed. This may cause them to, in a sense, forget they just ate.
“Some of their eating episodes are almost dissociative — they’re not realizing how much they are eating and can’t keep track of it,” he said.
Another brain system works to maintain longer-term homeostasis — or weight stability. Like a set thermostat, it kicks on to trigger hunger and fatigue when it senses we’re low on fat.
The hormone leptin, found in fat cells, sends signals to the hypothalamus to let it know how much energy we have on board.
“If leptin levels go up, it signals the brain that you have too much fat and you should eat less to return to the starting point,” said Rockefeller University geneticist Jeffrey Friedman, MD, PhD, who discovered the hormone in 1994. “If you have too little fat and leptin is low, that will stimulate appetite to return you to the starting point.”
In people with obesity, he said, the thermostat — or set point the body seeks to maintain — is too high.
All this raises a crucial question: How do these circuits and pathways malfunction in the first place?
What Breaks the Brain?
Genes, scientists agree, play a role.
Studies show that genetics underlie as much as 75% of people’s differences in body mass index (BMI), with certain gene combinations raising obesity risk in particular environments.
While hundreds of genes are believed to have a small effect, about a dozen single genes are thought to have a large effect. (Notably, most influence brain function.) For instance, about 6% of people with severe obesity since childhood have mutations in a gene called MC4R (melanocortin 4 receptor), which influences leptin signaling.
Still, genetics alone cannot account for the explosion in obesity in the U.S. over the last 50 years, says epidemiologist Deirdre Tobias, ScD, assistant professor of medicine at Harvard Medical School.
At the population level, “our genes don’t change that much in less than a generation,” she said.
But our food supply has.
Ultra-processed foods — those containing hydrogenated oils, high-fructose corn syrup, flavoring agents, emulsifiers, and other manufactured ingredients — now make up about 60% of the food supply.
“The evidence is fairly consistent indicating that there’s something about these foods that is possibly causing obesity,” said Tobias.
In one telling 2019 study, Dr. Hall and his colleagues brought 20 men and women into a study center to live for a month and tightly controlled their food intake and activity. One group was provided with meals with 80% of calories from ultra-processed food. The other was given meals with no processed food.
The three daily meals provided had the same calories, sugars, fats, fiber, and carbohydrates, and people were told to eat as much as they wanted.
Those on the ultra-processed diet ate about 500 calories more per day, ate faster, and gained weight. Those on the unprocessed diet lost weight.
“This is a stark example of how, when you can change the food environment, you cause really remarkable changes in food intake without people even being aware that they are overeating,” said Dr. Hall.
Just what it is about these relatively novel foods that may trigger overeating is unclear. It could be the crunch, the lack of water content, the engineered balance of sugar/salt/fat, their easy-to-devour texture, or something else.
Some research suggests that the foods may interfere with gut-brain signaling that tells the brain you’re full.
“Evidence is amassing that the nutritional content of processed foods is not accurately conveyed to the brain,” Dana M. Small, PhD, a neuroscientist at Yale, wrote in a recent perspective paper in Science.
Even more concerning: Some animal studies suggest processed foods reprogram the brain to dislike healthy foods.
And once these brain changes are made, they are hard to reverse.
“The problem is, our brain is not wired for this,” said Dr. Halpern. “We are not evolved to eat the food we are eating, so our brain adapts, but it adapts in a negative way that puts us at risk.”
That’s why changing the food environment via public policy must be part of the solution in combating obesity, Dr. Tobias said.
A New Era of Brain-Based Solutions
In the spring of 2021, after years of trying and failing to lose weight via the “move more, eat less” model, Michael Smith began to take a medication called Vyvanse. The drug was approved in 2008 for attention deficit hyperactivity disorder, but since it also influences levels of the hormones dopamine and norepinephrine to reduce cravings, it is now frequently prescribed for binge eating disorder.
“That was pretty much how I got rid of my first 60 to 70 pounds,” Smith said.
A few months later, after he hit a plateau, he had surgery to shrink the size of his stomach — a decision he now second-guesses.
While it kept him from overeating for a time, the fried chicken and gummy bear cravings returned a few months later.
His doctor, Fatima Cody Stanford, MD, put him on a second medication: semaglutide, or Wegovy, the weekly shot approved for weight loss in 2021. It works, in part, by mimicking glucagon-like peptide-1 (GLP-1), a key gut hormone that lets your brain know you are full.
The weight began to fall off again.
Smith’s success story is just one of many that Dr. Stanford, an obesity medicine doctor-scientist at Harvard, has heard in her office in recent years.
“I do not believe these drugs are a panacea,” she said. “There are nonresponders, and those are the patients I take off the medication. But for the high-responders, and there are many of them, they are telling me, ‘Oh my gosh. For the first time in my life, I am not constantly thinking about eating. My life has changed.’”
A Multi-Pronged Approach
Dr. Halpern, at Penn, has also been hearing success stories.
In recent years, he has placed permanent electrodes in the brains of three people with grade III, or severe, obesity and binge eating disorder.
All had tried exercise, dieting, support groups, medication, and weight loss surgery to no avail.
The electrodes modulate an area in the center of the brain called the nucleus accumbens, which in mice studies has been shown to reduce cravings when stimulated.
Thus far, all three are seeing promising results.
“It’s not like I don’t think about food at all,” one of them, Robyn Baldwin, told The New York Times. “But I’m no longer a craving person.”
Dr. Halpern is now extending the trial to more patients and hopes to ultimately include other areas of the brain, including those that involve memory.
He imagines a day when people with severe obesity, who have failed conventional treatments, can walk into a clinic and have their brain circuits assessed to see which ones may be misfiring.
Many might find relief with noninvasive brain stimulation, like transcranial magnetic stimulation (already in use for depression). Others might need a more extreme approach, like the deep brain stimulation, or DBS, therapy Dr. Halpern used.
“Obviously, DBS is hard to scale, so it would have to be reserved for the most severe patients,” he said.
Still, not everyone believes brain-based drugs and surgeries are the answer.
David Ludwig, MD, PhD, a professor of nutrition at the Harvard School of Public Health, played a key role in the discovery of GLP-1 and acknowledges that “of course” the brain influences body composition. But to him, explaining obesity as a disease of the brain oversimplifies it, discounting metabolic factors such as a tendency to store too much fat.
He noted that it’s hard to get drug companies, or any agencies, to fund large clinical trials on simple things like low-carbohydrate diets or exercise programs.
“We need all the tools we can get in the battle against the obesity epidemic, and new technologies are worth exploring,” he said. “However, the success of these drugs should not lead us to deprioritize diet and lifestyle interventions.”
Dr. Stanford, who has received consulting fees from Wegovy, believes the future of treatment lies in a multi-pronged approach, with surgery, medication, and lifestyle changes coalescing in a lasting, but fragile, remission.
“Unfortunately, there is no cure for obesity,” said Dr. Stanford, whose patients often have setbacks and must try new strategies. “There are treatments that work for a while, but they are constantly pushing up against this origin in the brain.”
Smith says understanding this has been a big part of his success.
He is now a leaner and healthier 5-foot-6 and 204 pounds. In addition to taking his medication, he walks to work, goes to the gym twice a week, limits his portions, and tries to reframe the way he thinks about food, viewing it as fuel rather than an indulgence.
Sometimes, when he looks in the mirror, he is reminded of his 380-pound self, and it scares him. He doesn’t want to go back there. He’s confident now that he won’t have to.
“There is this misconception out there that you just need to put the fork down, but I’m learning it’s more complicated than that,” he said. “I intend to treat this as the illness that it is and do what I need to combat it so I’m able to keep this new reality I have built for myself.”
A version of this article appeared on WebMD.com .
New AI-enhanced bandages poised to transform wound treatment
You cut yourself. You put on a bandage. In a week or so, your wound heals.
Most people take this routine for granted. But for the more than 8.2 million Americans who have chronic wounds, it’s not so simple.
Traumatic injuries, post-surgical complications, advanced age, and chronic illnesses like diabetes and vascular disease can all disrupt the delicate healing process, leading to wounds that last months or years.
Left untreated, about 30% led to amputation. And recent studies show the risk of dying from a chronic wound complication within 5 years rivals that of most cancers.
Yet until recently, medical technology had not kept up with what experts say is a snowballing threat to public health.
“Wound care – even with all of the billions of products that are sold – still exists on kind of a medieval level,” said Geoffrey Gurtner, MD, chair of the department of surgery and professor of biomedical engineering at the University of Arizona College of Medicine. “We’re still putting on poultices and salves ... and when it comes to diagnosing infection, it’s really an art. I think we can do better.”
Old-school bandage meets AI
Dr. Gurtner is among dozens of clinicians and researchers reimagining the humble bandage, combining cutting-edge materials science with artificial intelligence and patient data to develop “smart bandages” that do far more than shield a wound.
Someday soon, these paper-thin bandages embedded with miniaturized electronics could monitor the healing process in real time, alerting the patient – or a doctor – when things go wrong. With the press of a smartphone button, that bandage could deliver medicine to fight an infection or an electrical pulse to stimulate healing.
Some “closed-loop” designs need no prompting, instead monitoring the wound and automatically giving it what it needs.
Others in development could halt a battlefield wound from hemorrhaging or kick-start healing in a blast wound, preventing longer-term disability.
The same technologies could – if the price is right – speed up healing and reduce scarring in minor cuts and scrapes, too, said Dr. Gurtner.
And unlike many cutting-edge medical innovations, these next-generation bandages could be made relatively cheaply and benefit some of the most vulnerable populations, including older adults, people with low incomes, and those in developing countries.
They could also save the health care system money, as the U.S. spends more than $28 billion annually treating chronic wounds.
“This is a condition that many patients find shameful and embarrassing, so there hasn’t been a lot of advocacy,” said Dr. Gurtner, outgoing board president of the Wound Healing Society. “It’s a relatively ignored problem afflicting an underserved population that has a huge cost. It’s a perfect storm.”
How wounds heal, or don’t
Wound healing is one of the most complex processes of the human body.
First platelets rush to the injury, prompting blood to clot. Then immune cells emit compounds called inflammatory cytokines, helping to fight off pathogens and keep infection at bay. Other compounds, including nitric oxide, spark the growth of new blood vessels and collagen to rebuild skin and connective tissue. As inflammation slows and stops, the flesh continues to reform.
But some conditions can stall the process, often in the inflammatory stage.
In people with diabetes, high glucose levels and poor circulation tend to sabotage the process. And people with nerve damage from spinal cord injuries, diabetes, or other ailments may not be able to feel it when a wound is getting worse or reinjured.
“We end up with patients going months with open wounds that are festering and infected,” said Roslyn Rivkah Isseroff, MD, professor of dermatology at the University of California Davis and head of the VA Northern California Health Care System’s wound healing clinic. “The patients are upset with the smell. These open ulcers put the patient at risk for systemic infection, like sepsis.” It can impact mental health, draining the patient’s ability to care for their wound.
“We see them once a week and send them home and say change your dressing every day, and they say, ‘I can barely move. I can’t do this,’ ” said Dr. Isseroff.
Checking for infection means removing bandages and culturing the wound. That can be painful, and results take time.
A lot can happen to a wound in a week.
“Sometimes, they come back and it’s a disaster, and they have to be admitted to the ER or even get an amputation,” Dr. Gurtner said.
People who are housing insecure or lack access to health care are even more vulnerable to complications.
“If you had the ability to say ‘there is something bad happening,’ you could do a lot to prevent this cascade and downward spiral.”
Bandages 2.0
In 2019, the Defense Advanced Research Projects Agency, the research arm of the Department of Defense, launched the Bioelectronics for Tissue Regeneration program to encourage scientists to develop a “closed-loop” bandage capable of both monitoring and hastening healing.
Tens of millions in funding has kick-started a flood of innovation since.
“It’s kind of a race to the finish,” said Marco Rolandi, PhD, associate professor of electrical and computer engineering at the University of California Santa Cruz and the principal investigator for a team including engineers, medical doctors, and computer scientists from UC Santa Cruz, UC Davis, and Tufts. “I’ve been amazed and impressed at all the work coming out.”
His team’s goal is to cut healing time in half by using (a) real-time monitoring of how a wound is healing – using indicators like temperature, pH level, oxygen, moisture, glucose, electrical activity, and certain proteins, and (b) appropriate stimulation.
“Every wound is different, so there is no one solution,” said Dr. Isseroff, the team’s clinical lead. “The idea is that it will be able to sense different parameters unique to the wound, use AI to figure out what stage it is in, and provide the right stimulus to kick it out of that stalled stage.”
The team has developed a proof-of-concept prototype: a bandage embedded with a tiny camera that takes pictures and transmits them to a computer algorithm to assess the wound’s progress. Miniaturized battery-powered actuators, or motors, automatically deliver medication.
Phase I trials in rodents went well, Dr. Rolandi said. The team is now testing the bandage on pigs.
Across the globe, other promising developments are underway.
In a scientific paper published in May, researchers at the University of Glasgow described a new “low-cost, environmentally friendly” bandage embedded with light-emitting diodes that use ultraviolet light to kill bacteria – no antibiotics needed. The fabric is stitched with a slim, flexible coil that powers the lights without a battery using wireless power transfer. In lab studies, it eradicated gram-negative bacteria (some of the nastiest bugs) in 6 hours.
Also in May, in the journal Bioactive Materials, a Penn State team detailed a bandage with medicine-injecting microneedles that can halt bleeding immediately after injury. In lab and animal tests, it reduced clotting time from 11.5 minutes to 1.3 minutes and bleeding by 90%.
“With hemorrhaging injuries, it is often the loss of blood – not the injury itself – that causes death,” said study author Amir Sheikhi, PhD, assistant professor of chemical and biomedical engineering at Penn State. “Those 10 minutes could be the difference between life and death.”
Another smart bandage, developed at Northwestern University, Chicago, harmlessly dissolves – electrodes and all – into the body after it is no longer needed, eliminating what can be a painful removal.
Guillermo Ameer, DSc, a study author reporting on the technology in Science Advances, hopes it could be made cheaply and used in developing countries.
“We’d like to create something that you could use in your home, even in a very remote village,” said Dr. Ameer, professor of biomedical engineering at Northwestern.
Timeline for clinical use
These are early days for the smart bandage, scientists say. Most studies have been in rodents and more work is needed to develop human-scale bandages, reduce cost, solve long-term data storage, and ensure material adheres well without irritating the skin.
But Dr. Gurtner is hopeful that some iteration could be used in clinical practice within a few years.
In May, he and colleagues at Stanford (Calif.) University published a paper in Nature Biotechnology describing their smart bandage. It includes a microcontroller unit, a radio antenna, biosensors, and an electrical stimulator all affixed to a rubbery, skin-like polymer (or hydrogel) about the thickness of a single coat of latex paint.
The bandage senses changes in temperature and electrical conductivity as the wound heals, and it gives electrical stimulation to accelerate that healing.
Animals treated with the bandage healed 25% faster, with 50% less scarring.
Electrical currents are already used for wound healing in clinical practice, Dr. Gurtner said. Because the stimulus is already approved and the cost to make the bandage could be low (as little as $10 to $50), he believes it could be ushered through the approval processes relatively quickly.
“Is this the ultimate embodiment of all the bells and whistles that are possible in a smart bandage? No. Not yet,” he said. “But we think it will help people. And right now, that’s good enough.”
A version of this article appeared on WebMD.com.
You cut yourself. You put on a bandage. In a week or so, your wound heals.
Most people take this routine for granted. But for the more than 8.2 million Americans who have chronic wounds, it’s not so simple.
Traumatic injuries, post-surgical complications, advanced age, and chronic illnesses like diabetes and vascular disease can all disrupt the delicate healing process, leading to wounds that last months or years.
Left untreated, about 30% led to amputation. And recent studies show the risk of dying from a chronic wound complication within 5 years rivals that of most cancers.
Yet until recently, medical technology had not kept up with what experts say is a snowballing threat to public health.
“Wound care – even with all of the billions of products that are sold – still exists on kind of a medieval level,” said Geoffrey Gurtner, MD, chair of the department of surgery and professor of biomedical engineering at the University of Arizona College of Medicine. “We’re still putting on poultices and salves ... and when it comes to diagnosing infection, it’s really an art. I think we can do better.”
Old-school bandage meets AI
Dr. Gurtner is among dozens of clinicians and researchers reimagining the humble bandage, combining cutting-edge materials science with artificial intelligence and patient data to develop “smart bandages” that do far more than shield a wound.
Someday soon, these paper-thin bandages embedded with miniaturized electronics could monitor the healing process in real time, alerting the patient – or a doctor – when things go wrong. With the press of a smartphone button, that bandage could deliver medicine to fight an infection or an electrical pulse to stimulate healing.
Some “closed-loop” designs need no prompting, instead monitoring the wound and automatically giving it what it needs.
Others in development could halt a battlefield wound from hemorrhaging or kick-start healing in a blast wound, preventing longer-term disability.
The same technologies could – if the price is right – speed up healing and reduce scarring in minor cuts and scrapes, too, said Dr. Gurtner.
And unlike many cutting-edge medical innovations, these next-generation bandages could be made relatively cheaply and benefit some of the most vulnerable populations, including older adults, people with low incomes, and those in developing countries.
They could also save the health care system money, as the U.S. spends more than $28 billion annually treating chronic wounds.
“This is a condition that many patients find shameful and embarrassing, so there hasn’t been a lot of advocacy,” said Dr. Gurtner, outgoing board president of the Wound Healing Society. “It’s a relatively ignored problem afflicting an underserved population that has a huge cost. It’s a perfect storm.”
How wounds heal, or don’t
Wound healing is one of the most complex processes of the human body.
First platelets rush to the injury, prompting blood to clot. Then immune cells emit compounds called inflammatory cytokines, helping to fight off pathogens and keep infection at bay. Other compounds, including nitric oxide, spark the growth of new blood vessels and collagen to rebuild skin and connective tissue. As inflammation slows and stops, the flesh continues to reform.
But some conditions can stall the process, often in the inflammatory stage.
In people with diabetes, high glucose levels and poor circulation tend to sabotage the process. And people with nerve damage from spinal cord injuries, diabetes, or other ailments may not be able to feel it when a wound is getting worse or reinjured.
“We end up with patients going months with open wounds that are festering and infected,” said Roslyn Rivkah Isseroff, MD, professor of dermatology at the University of California Davis and head of the VA Northern California Health Care System’s wound healing clinic. “The patients are upset with the smell. These open ulcers put the patient at risk for systemic infection, like sepsis.” It can impact mental health, draining the patient’s ability to care for their wound.
“We see them once a week and send them home and say change your dressing every day, and they say, ‘I can barely move. I can’t do this,’ ” said Dr. Isseroff.
Checking for infection means removing bandages and culturing the wound. That can be painful, and results take time.
A lot can happen to a wound in a week.
“Sometimes, they come back and it’s a disaster, and they have to be admitted to the ER or even get an amputation,” Dr. Gurtner said.
People who are housing insecure or lack access to health care are even more vulnerable to complications.
“If you had the ability to say ‘there is something bad happening,’ you could do a lot to prevent this cascade and downward spiral.”
Bandages 2.0
In 2019, the Defense Advanced Research Projects Agency, the research arm of the Department of Defense, launched the Bioelectronics for Tissue Regeneration program to encourage scientists to develop a “closed-loop” bandage capable of both monitoring and hastening healing.
Tens of millions in funding has kick-started a flood of innovation since.
“It’s kind of a race to the finish,” said Marco Rolandi, PhD, associate professor of electrical and computer engineering at the University of California Santa Cruz and the principal investigator for a team including engineers, medical doctors, and computer scientists from UC Santa Cruz, UC Davis, and Tufts. “I’ve been amazed and impressed at all the work coming out.”
His team’s goal is to cut healing time in half by using (a) real-time monitoring of how a wound is healing – using indicators like temperature, pH level, oxygen, moisture, glucose, electrical activity, and certain proteins, and (b) appropriate stimulation.
“Every wound is different, so there is no one solution,” said Dr. Isseroff, the team’s clinical lead. “The idea is that it will be able to sense different parameters unique to the wound, use AI to figure out what stage it is in, and provide the right stimulus to kick it out of that stalled stage.”
The team has developed a proof-of-concept prototype: a bandage embedded with a tiny camera that takes pictures and transmits them to a computer algorithm to assess the wound’s progress. Miniaturized battery-powered actuators, or motors, automatically deliver medication.
Phase I trials in rodents went well, Dr. Rolandi said. The team is now testing the bandage on pigs.
Across the globe, other promising developments are underway.
In a scientific paper published in May, researchers at the University of Glasgow described a new “low-cost, environmentally friendly” bandage embedded with light-emitting diodes that use ultraviolet light to kill bacteria – no antibiotics needed. The fabric is stitched with a slim, flexible coil that powers the lights without a battery using wireless power transfer. In lab studies, it eradicated gram-negative bacteria (some of the nastiest bugs) in 6 hours.
Also in May, in the journal Bioactive Materials, a Penn State team detailed a bandage with medicine-injecting microneedles that can halt bleeding immediately after injury. In lab and animal tests, it reduced clotting time from 11.5 minutes to 1.3 minutes and bleeding by 90%.
“With hemorrhaging injuries, it is often the loss of blood – not the injury itself – that causes death,” said study author Amir Sheikhi, PhD, assistant professor of chemical and biomedical engineering at Penn State. “Those 10 minutes could be the difference between life and death.”
Another smart bandage, developed at Northwestern University, Chicago, harmlessly dissolves – electrodes and all – into the body after it is no longer needed, eliminating what can be a painful removal.
Guillermo Ameer, DSc, a study author reporting on the technology in Science Advances, hopes it could be made cheaply and used in developing countries.
“We’d like to create something that you could use in your home, even in a very remote village,” said Dr. Ameer, professor of biomedical engineering at Northwestern.
Timeline for clinical use
These are early days for the smart bandage, scientists say. Most studies have been in rodents and more work is needed to develop human-scale bandages, reduce cost, solve long-term data storage, and ensure material adheres well without irritating the skin.
But Dr. Gurtner is hopeful that some iteration could be used in clinical practice within a few years.
In May, he and colleagues at Stanford (Calif.) University published a paper in Nature Biotechnology describing their smart bandage. It includes a microcontroller unit, a radio antenna, biosensors, and an electrical stimulator all affixed to a rubbery, skin-like polymer (or hydrogel) about the thickness of a single coat of latex paint.
The bandage senses changes in temperature and electrical conductivity as the wound heals, and it gives electrical stimulation to accelerate that healing.
Animals treated with the bandage healed 25% faster, with 50% less scarring.
Electrical currents are already used for wound healing in clinical practice, Dr. Gurtner said. Because the stimulus is already approved and the cost to make the bandage could be low (as little as $10 to $50), he believes it could be ushered through the approval processes relatively quickly.
“Is this the ultimate embodiment of all the bells and whistles that are possible in a smart bandage? No. Not yet,” he said. “But we think it will help people. And right now, that’s good enough.”
A version of this article appeared on WebMD.com.
You cut yourself. You put on a bandage. In a week or so, your wound heals.
Most people take this routine for granted. But for the more than 8.2 million Americans who have chronic wounds, it’s not so simple.
Traumatic injuries, post-surgical complications, advanced age, and chronic illnesses like diabetes and vascular disease can all disrupt the delicate healing process, leading to wounds that last months or years.
Left untreated, about 30% led to amputation. And recent studies show the risk of dying from a chronic wound complication within 5 years rivals that of most cancers.
Yet until recently, medical technology had not kept up with what experts say is a snowballing threat to public health.
“Wound care – even with all of the billions of products that are sold – still exists on kind of a medieval level,” said Geoffrey Gurtner, MD, chair of the department of surgery and professor of biomedical engineering at the University of Arizona College of Medicine. “We’re still putting on poultices and salves ... and when it comes to diagnosing infection, it’s really an art. I think we can do better.”
Old-school bandage meets AI
Dr. Gurtner is among dozens of clinicians and researchers reimagining the humble bandage, combining cutting-edge materials science with artificial intelligence and patient data to develop “smart bandages” that do far more than shield a wound.
Someday soon, these paper-thin bandages embedded with miniaturized electronics could monitor the healing process in real time, alerting the patient – or a doctor – when things go wrong. With the press of a smartphone button, that bandage could deliver medicine to fight an infection or an electrical pulse to stimulate healing.
Some “closed-loop” designs need no prompting, instead monitoring the wound and automatically giving it what it needs.
Others in development could halt a battlefield wound from hemorrhaging or kick-start healing in a blast wound, preventing longer-term disability.
The same technologies could – if the price is right – speed up healing and reduce scarring in minor cuts and scrapes, too, said Dr. Gurtner.
And unlike many cutting-edge medical innovations, these next-generation bandages could be made relatively cheaply and benefit some of the most vulnerable populations, including older adults, people with low incomes, and those in developing countries.
They could also save the health care system money, as the U.S. spends more than $28 billion annually treating chronic wounds.
“This is a condition that many patients find shameful and embarrassing, so there hasn’t been a lot of advocacy,” said Dr. Gurtner, outgoing board president of the Wound Healing Society. “It’s a relatively ignored problem afflicting an underserved population that has a huge cost. It’s a perfect storm.”
How wounds heal, or don’t
Wound healing is one of the most complex processes of the human body.
First platelets rush to the injury, prompting blood to clot. Then immune cells emit compounds called inflammatory cytokines, helping to fight off pathogens and keep infection at bay. Other compounds, including nitric oxide, spark the growth of new blood vessels and collagen to rebuild skin and connective tissue. As inflammation slows and stops, the flesh continues to reform.
But some conditions can stall the process, often in the inflammatory stage.
In people with diabetes, high glucose levels and poor circulation tend to sabotage the process. And people with nerve damage from spinal cord injuries, diabetes, or other ailments may not be able to feel it when a wound is getting worse or reinjured.
“We end up with patients going months with open wounds that are festering and infected,” said Roslyn Rivkah Isseroff, MD, professor of dermatology at the University of California Davis and head of the VA Northern California Health Care System’s wound healing clinic. “The patients are upset with the smell. These open ulcers put the patient at risk for systemic infection, like sepsis.” It can impact mental health, draining the patient’s ability to care for their wound.
“We see them once a week and send them home and say change your dressing every day, and they say, ‘I can barely move. I can’t do this,’ ” said Dr. Isseroff.
Checking for infection means removing bandages and culturing the wound. That can be painful, and results take time.
A lot can happen to a wound in a week.
“Sometimes, they come back and it’s a disaster, and they have to be admitted to the ER or even get an amputation,” Dr. Gurtner said.
People who are housing insecure or lack access to health care are even more vulnerable to complications.
“If you had the ability to say ‘there is something bad happening,’ you could do a lot to prevent this cascade and downward spiral.”
Bandages 2.0
In 2019, the Defense Advanced Research Projects Agency, the research arm of the Department of Defense, launched the Bioelectronics for Tissue Regeneration program to encourage scientists to develop a “closed-loop” bandage capable of both monitoring and hastening healing.
Tens of millions in funding has kick-started a flood of innovation since.
“It’s kind of a race to the finish,” said Marco Rolandi, PhD, associate professor of electrical and computer engineering at the University of California Santa Cruz and the principal investigator for a team including engineers, medical doctors, and computer scientists from UC Santa Cruz, UC Davis, and Tufts. “I’ve been amazed and impressed at all the work coming out.”
His team’s goal is to cut healing time in half by using (a) real-time monitoring of how a wound is healing – using indicators like temperature, pH level, oxygen, moisture, glucose, electrical activity, and certain proteins, and (b) appropriate stimulation.
“Every wound is different, so there is no one solution,” said Dr. Isseroff, the team’s clinical lead. “The idea is that it will be able to sense different parameters unique to the wound, use AI to figure out what stage it is in, and provide the right stimulus to kick it out of that stalled stage.”
The team has developed a proof-of-concept prototype: a bandage embedded with a tiny camera that takes pictures and transmits them to a computer algorithm to assess the wound’s progress. Miniaturized battery-powered actuators, or motors, automatically deliver medication.
Phase I trials in rodents went well, Dr. Rolandi said. The team is now testing the bandage on pigs.
Across the globe, other promising developments are underway.
In a scientific paper published in May, researchers at the University of Glasgow described a new “low-cost, environmentally friendly” bandage embedded with light-emitting diodes that use ultraviolet light to kill bacteria – no antibiotics needed. The fabric is stitched with a slim, flexible coil that powers the lights without a battery using wireless power transfer. In lab studies, it eradicated gram-negative bacteria (some of the nastiest bugs) in 6 hours.
Also in May, in the journal Bioactive Materials, a Penn State team detailed a bandage with medicine-injecting microneedles that can halt bleeding immediately after injury. In lab and animal tests, it reduced clotting time from 11.5 minutes to 1.3 minutes and bleeding by 90%.
“With hemorrhaging injuries, it is often the loss of blood – not the injury itself – that causes death,” said study author Amir Sheikhi, PhD, assistant professor of chemical and biomedical engineering at Penn State. “Those 10 minutes could be the difference between life and death.”
Another smart bandage, developed at Northwestern University, Chicago, harmlessly dissolves – electrodes and all – into the body after it is no longer needed, eliminating what can be a painful removal.
Guillermo Ameer, DSc, a study author reporting on the technology in Science Advances, hopes it could be made cheaply and used in developing countries.
“We’d like to create something that you could use in your home, even in a very remote village,” said Dr. Ameer, professor of biomedical engineering at Northwestern.
Timeline for clinical use
These are early days for the smart bandage, scientists say. Most studies have been in rodents and more work is needed to develop human-scale bandages, reduce cost, solve long-term data storage, and ensure material adheres well without irritating the skin.
But Dr. Gurtner is hopeful that some iteration could be used in clinical practice within a few years.
In May, he and colleagues at Stanford (Calif.) University published a paper in Nature Biotechnology describing their smart bandage. It includes a microcontroller unit, a radio antenna, biosensors, and an electrical stimulator all affixed to a rubbery, skin-like polymer (or hydrogel) about the thickness of a single coat of latex paint.
The bandage senses changes in temperature and electrical conductivity as the wound heals, and it gives electrical stimulation to accelerate that healing.
Animals treated with the bandage healed 25% faster, with 50% less scarring.
Electrical currents are already used for wound healing in clinical practice, Dr. Gurtner said. Because the stimulus is already approved and the cost to make the bandage could be low (as little as $10 to $50), he believes it could be ushered through the approval processes relatively quickly.
“Is this the ultimate embodiment of all the bells and whistles that are possible in a smart bandage? No. Not yet,” he said. “But we think it will help people. And right now, that’s good enough.”
A version of this article appeared on WebMD.com.
The weird world of hydrogels: How they’ll change health care
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.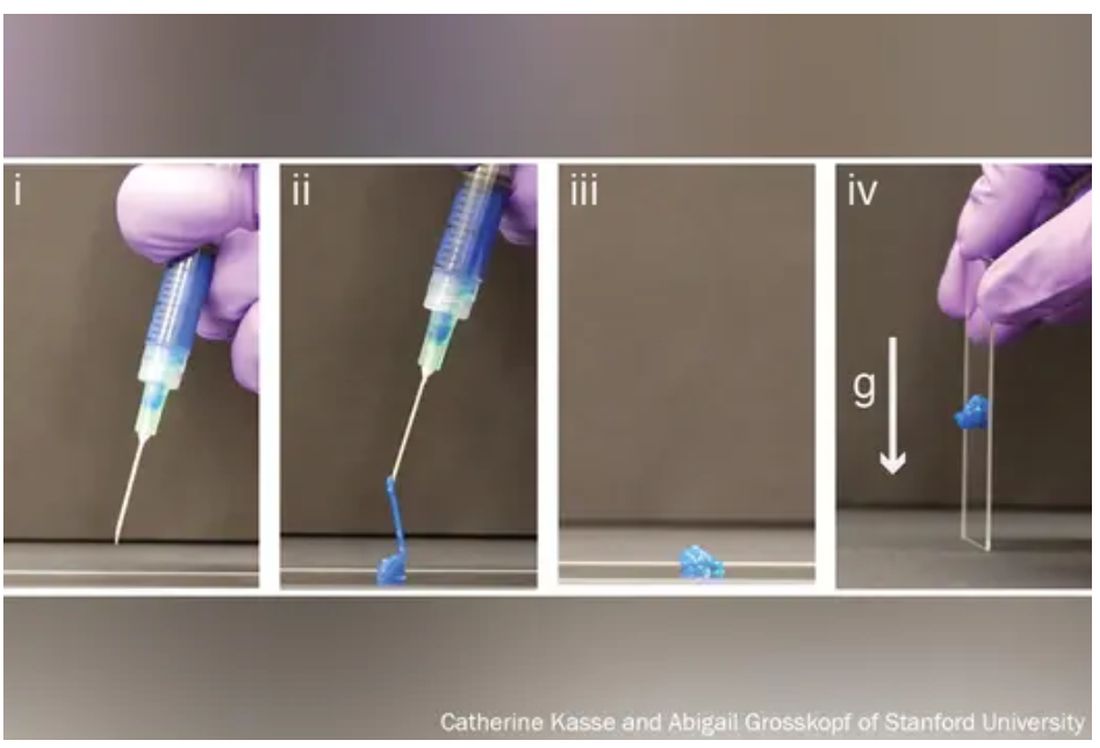
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.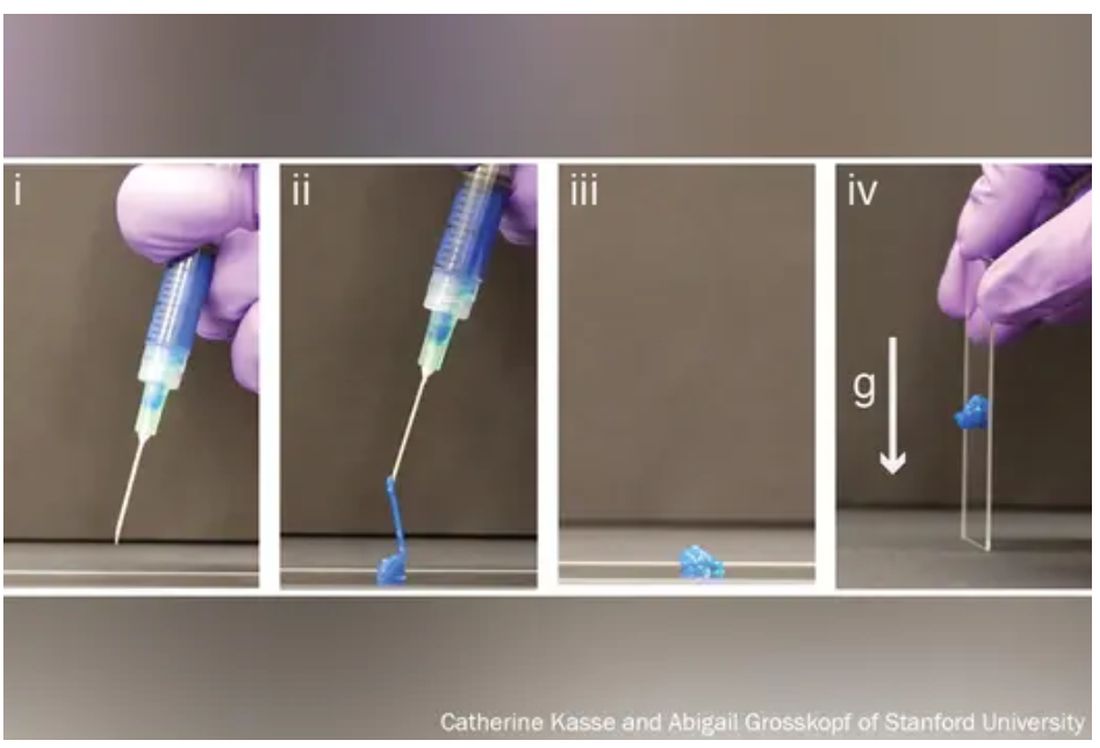
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
Imagine a day when a simple injection prompts a broken bone to heal. When tiny, ingestible devices linger in the body, unnoticed, tracking our health or delivering life-saving medications. When brain and heart implants mesh with flesh so seamlessly that the body thinks they’ve been there all along.
These are the dreams of materials scientists who have toiled for decades to mimic the complex architecture of the human body in hopes of replacing broken parts or treating disease.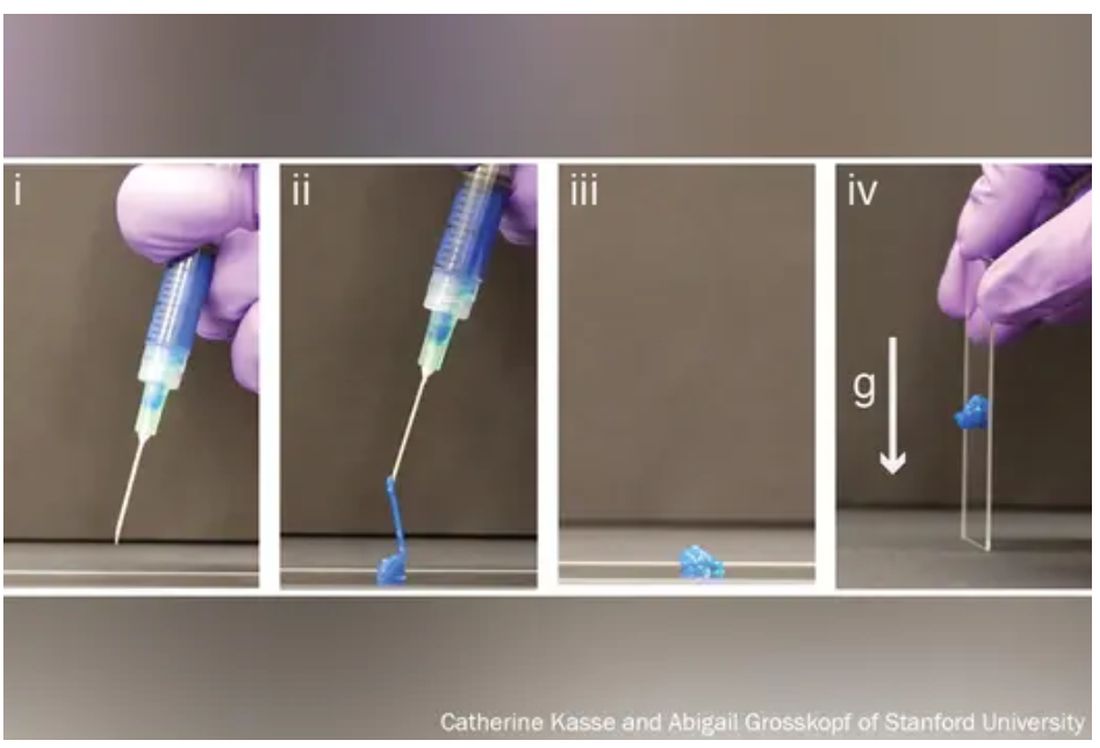
The problem, say bioengineers, is that most replacement and corrective parts – from prosthetics to pacemakers – are made of hard, dry, lifeless materials, like metal or plastic, while biological tissue is soft, wet, and living.
The body knows the difference and tends to reject imitations.
Enter hydrogels, three-dimensional networks of molecules swollen with – by definition – water.
First described in 1960 by creators of soft contact lenses, these weird, shape-shifting substances are able to morph from liquid to solid to a squishy in-between. (Early, simple uses include hair gel or Jell-O.). Slow to gain attention, growing to just 1,000 studies published by 1982, they’ve become the subject of intense study recently, with 100,000 papers published by 2020, and 3,800 already this year alone.
As chemists, biologists, and engineers begin to work more with one another and with medical doctors,
“We are, essentially, hydrogels,” said Benjamin Wiley, PhD, a chemistry professor at Duke University in Durham, N.C. “As people develop new hydrogels that more closely match the tissues in our body, we’ll be able to treat a whole host of ailments we couldn’t treat before.”
From contact lenses to brain implants
Put simply, a hydrogel is like a mesh bag of water.
The mesh is made of polymers, or spaghetti-like strands of molecules, stitched together in a repeating pattern and swollen with H2O, much like the way 3D matrixes in our body surround, support, and give structure to our cells and tissues.
“Imagine a soccer net, with all of these long fibers woven together to create the net,” said Eric Appel, PhD, associate professor of materials science and engineering at Stanford (Calif.) University.
While the broader category of “gels” could be filled with anything, including chemical solvents, water is the key ingredient that sets hydrogels apart, making them ideal for, as some scientists put it, “merging humans and machines.”
Human bones are about 25% water, while muscles hover around 70% and the brain is 85%. The precious liquid plays a host of critical roles, from shuttling nutrients in and waste out to helping cells talk to each other.
Lab-made hydrogels can be loaded with cargo (like a ball in the net), including cells or drugs that help mimic some of those functions.
Hydrogels are soft and pliable like flesh. So, if used in implants, they may be less likely to damage surrounding tissue.
“Think about a metal spoon in your bowl of pudding. As you’re shaking the bowl, the spoon doesn’t stay in place, and you get scarring around the spoon,” said Christina Tringides, PhD, a materials scientist who studies neural engineering. That, she says, is exactly what happens to brain implants when patients breathe or move. “It’s a mechanical mismatch. But with hydrogels, you could get perfect mechanical matching.”
Hydrogels also tend to be nontoxic, so the immune system may be less likely to attack them as foreign bodies.
All this has made hydrogels the new darling of the bioengineering world.
“There has been an absolute explosion of interest in these materials,” Dr. Appel said.
Smarter drug delivery and ingestible electronics
Early versions of hydrogels were thick and gooey, making it hard to get them inside the body.
“Think of a block of Jell-O. You couldn’t inject something like that,” Dr. Appel said.
But Dr. Appel, whose lab develops new drug delivery systems, has been tinkering with gel formulas for years in hopes that these high-tech globs could someday ferry timed-release drugs to just the right spot in the body.
His new hydrogels start as fully formed gels (which help preserve the drug contents) inside a syringe. But once the plunger is pushed, they magically shape-shift to a liquid thin enough to flow easily through a standard needle. Upon exit, they immediately reform into gels, protecting the inherent cargo from degrading.
This could be a game changer at a time when many cutting-edge drugs – think Humira for arthritis or Ozempic for type 2 diabetes – are made of quickly degrading proteins too large and complex to simply jam into a pill. Instead, they must be injected, often frequently.
“Because the gel takes months to dissolve, it slowly delivers the drug over time,” Dr. Appel said. “You could conceivably go from a shot once a week to once every 4 months.”
Such slow-release hydrogels could make vaccines last longer, in turn teaching the body to better resist emerging virus variants, and deliver tumor-busting therapies more precisely, said Dr. Appel, who has formed a startup and hopes to fast-track the first hydrogel drug delivery system to clinical trials within a few years.
Meanwhile, another team at the Massachusetts Institute of Technology has taken a different approach, developing a standard-sized ingestible hydrogel pill that swells up like a puffer fish in the stomach, lasting a month and slowly releasing drugs all the while. To remove the pill, a patient simply drinks a salt-based solution that shrivels the ping-pong ball–sized device so it can be passed out of the body.
In a paper in Nature Communications, the scientists showed the puffer fish pill could also be loaded with tiny cameras or monitors to track conditions like ulcers or cancer.
“The dream is to have a Jell-O-like smart pill that, once swallowed, stays in the stomach and monitors the patient’s health,” said Xuanhe Zhao, PhD, a researcher on the project and associate professor of mechanical engineering at MIT.
Building joints and regrowing bones
Since the 1970s, researchers have mulled using hydrogels to replace human cartilage, a remarkably strong and flexible tissue made of about 90% water but able to withstand the weight of a car on an area about the size of a coin.
Until recently, those efforts have largely failed. Meaning when knee cartilage wears down, things like cartilage transplants, drilling holes to stimulate new growth, or total joint replacements – all of which require lengthy rehab – are the only options.
But that may be about to change.
Dr. Wiley and his colleagues at Duke recently reported that they’d developed the first gel-based cartilage substitute even stronger and more durable than the real thing.
By attaching their hydrogel to a titanium backing to help stick it in place, they hope to repair damaged cartilage “much like a dentist fills a cavity” long before surgery is necessary.
They too have partnered with industry to bring their hydrogel to market – starting with knees.
“Ultimately, the goal is to do any joint – hips, ankles, fingers, and toes,” Dr. Wiley said.
At the University of Toronto, chemist Karina Carneiro, PhD, and dentist Christopher McCulloch, DDS, are also thinking big.
In a recent paper in Proceedings of the National Academy of Sciences, they describe a hydrogel, designed by Dr. Carneiro and made of DNA, that can be injected, migrate to a defect in bone – an irreparable break, hole from surgery, or jawbone withered by age – and fill in the gap like putty. But not only does it patch the hole, it prompts the bone to regenerate.
In rats with holes in their skulls due to surgery, they found that the treatment did not work as well as the existing gold standard for repairing holes in bone – grafting bone from elsewhere in the body. But it did work.
“These are very early days for DNA hydrogels,” cautioned Dr. McCulloch, a study coauthor and professor in the Faculty of Dentistry, noting that it will likely be a decade or more before such technology could be available to patients. “But there is the potential that DNA hydrogel could someday grow bone without having to have highly invasive surgical procedures. That’s a significant advancement.”
A sci-fi future
Perhaps the wildest, and weirdest, potential applications of hydrogels come in the realm of human-machine interaction.
Numerous companies are already dabbling in neural prosthetic or brain computer interfaces that might someday, for instance, let someone who is paralyzed and can’t speak write on a laptop using their thoughts.
The spoon-in-the-Jell-O problem has been a major stumbling block.
But Dr. Tringides, who recently earned her PhD in biophysics from Harvard, is working on it.
She and her team have developed a seaweed-based hydrogel loaded with tiny flecks of nanomaterials that can not only meld nicely into squishy brain tissue but also conduct electricity.
Within a decade, she says, this could replace the clunky platinum metal discs used for electrocorticography – recording electrical activity in the brain to identify where seizures start or doing precise brain surgery.
In 30 to 50 years? Let your imagination run wild.
“I’m a skeptic. I like to take research step by step,” she said. “But things are definitely progressing in an interesting direction.”
A version of this article first appeared on WebMD.com.
