User login
Terry Rudd has covered clinical news and health policy as a reporter and editor since 1994.
VIDEO: Postsurgical readmissions present pay-for-performance challenges
The causes of most hospital readmissions after surgery may complicate the use of performance-based reimbursement to reduce such returns.
“The reasons why patients come back after surgery are due to expected complications,” not the worsening of existing medical conditions, noted Dr. Karl Y. Bilimoria of Northwestern University, Chicago, and lead author of a new study on what drives 30-day hospital readmissions after surgery (JAMA 2015;313:483-95).
In a video interview, Dr. Bilimoria discussed the challenges that the timing and causes of postsurgical readmissions present for prevention programs and for pay-for-performance initiatives.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The causes of most hospital readmissions after surgery may complicate the use of performance-based reimbursement to reduce such returns.
“The reasons why patients come back after surgery are due to expected complications,” not the worsening of existing medical conditions, noted Dr. Karl Y. Bilimoria of Northwestern University, Chicago, and lead author of a new study on what drives 30-day hospital readmissions after surgery (JAMA 2015;313:483-95).
In a video interview, Dr. Bilimoria discussed the challenges that the timing and causes of postsurgical readmissions present for prevention programs and for pay-for-performance initiatives.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The causes of most hospital readmissions after surgery may complicate the use of performance-based reimbursement to reduce such returns.
“The reasons why patients come back after surgery are due to expected complications,” not the worsening of existing medical conditions, noted Dr. Karl Y. Bilimoria of Northwestern University, Chicago, and lead author of a new study on what drives 30-day hospital readmissions after surgery (JAMA 2015;313:483-95).
In a video interview, Dr. Bilimoria discussed the challenges that the timing and causes of postsurgical readmissions present for prevention programs and for pay-for-performance initiatives.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Will New HCV Drugs’ Costs Kill Health Care Budgets?
BOSTON – The estimated cost of treating all eligible U.S. hepatitis C patients with a new generation of high-priced medications may be breathtaking, but would the resulting savings over those cured patients’ lifetimes offset the initial financial blow?
A new analysis unveiled at the annual meeting of the American Association for the Study of Liver Diseases calculated the impact of the new drugs on treatment costs and compared the cost of treatment with new drugs to the old standard of care.
“We found that the cost of treatment is very high, as expected,” explained lead investigator Jagpreet Chhatwal, Ph.D., of MD Anderson Cancer Center, Houston. In fact, if everyone who was eligible for the new drugs were treated, the cost over the next 5 years would be $136 billion.
“This is clearly unsustainable for any payer,” he noted. “So the question is: How can we manage to treat people who need this treatment?”
In a video interview, Dr. Chhatwal outlined how the researchers calculated their cost estimates, what cost savings could be gained with the new drugs, and how patients and payers alike could manage the price of treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The estimated cost of treating all eligible U.S. hepatitis C patients with a new generation of high-priced medications may be breathtaking, but would the resulting savings over those cured patients’ lifetimes offset the initial financial blow?
A new analysis unveiled at the annual meeting of the American Association for the Study of Liver Diseases calculated the impact of the new drugs on treatment costs and compared the cost of treatment with new drugs to the old standard of care.
“We found that the cost of treatment is very high, as expected,” explained lead investigator Jagpreet Chhatwal, Ph.D., of MD Anderson Cancer Center, Houston. In fact, if everyone who was eligible for the new drugs were treated, the cost over the next 5 years would be $136 billion.
“This is clearly unsustainable for any payer,” he noted. “So the question is: How can we manage to treat people who need this treatment?”
In a video interview, Dr. Chhatwal outlined how the researchers calculated their cost estimates, what cost savings could be gained with the new drugs, and how patients and payers alike could manage the price of treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The estimated cost of treating all eligible U.S. hepatitis C patients with a new generation of high-priced medications may be breathtaking, but would the resulting savings over those cured patients’ lifetimes offset the initial financial blow?
A new analysis unveiled at the annual meeting of the American Association for the Study of Liver Diseases calculated the impact of the new drugs on treatment costs and compared the cost of treatment with new drugs to the old standard of care.
“We found that the cost of treatment is very high, as expected,” explained lead investigator Jagpreet Chhatwal, Ph.D., of MD Anderson Cancer Center, Houston. In fact, if everyone who was eligible for the new drugs were treated, the cost over the next 5 years would be $136 billion.
“This is clearly unsustainable for any payer,” he noted. “So the question is: How can we manage to treat people who need this treatment?”
In a video interview, Dr. Chhatwal outlined how the researchers calculated their cost estimates, what cost savings could be gained with the new drugs, and how patients and payers alike could manage the price of treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Will new HCV drugs’ costs kill health care budgets?
BOSTON – The estimated cost of treating all eligible U.S. hepatitis C patients with a new generation of high-priced medications may be breathtaking, but would the resulting savings over those cured patients’ lifetimes offset the initial financial blow?
A new analysis unveiled at the annual meeting of the American Association for the Study of Liver Diseases calculated the impact of the new drugs on treatment costs and compared the cost of treatment with new drugs to the old standard of care.
“We found that the cost of treatment is very high, as expected,” explained lead investigator Jagpreet Chhatwal, Ph.D., of MD Anderson Cancer Center, Houston. In fact, if everyone who was eligible for the new drugs were treated, the cost over the next 5 years would be $136 billion.
“This is clearly unsustainable for any payer,” he noted. “So the question is: How can we manage to treat people who need this treatment?”
In a video interview, Dr. Chhatwal outlined how the researchers calculated their cost estimates, what cost savings could be gained with the new drugs, and how patients and payers alike could manage the price of treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The estimated cost of treating all eligible U.S. hepatitis C patients with a new generation of high-priced medications may be breathtaking, but would the resulting savings over those cured patients’ lifetimes offset the initial financial blow?
A new analysis unveiled at the annual meeting of the American Association for the Study of Liver Diseases calculated the impact of the new drugs on treatment costs and compared the cost of treatment with new drugs to the old standard of care.
“We found that the cost of treatment is very high, as expected,” explained lead investigator Jagpreet Chhatwal, Ph.D., of MD Anderson Cancer Center, Houston. In fact, if everyone who was eligible for the new drugs were treated, the cost over the next 5 years would be $136 billion.
“This is clearly unsustainable for any payer,” he noted. “So the question is: How can we manage to treat people who need this treatment?”
In a video interview, Dr. Chhatwal outlined how the researchers calculated their cost estimates, what cost savings could be gained with the new drugs, and how patients and payers alike could manage the price of treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – The estimated cost of treating all eligible U.S. hepatitis C patients with a new generation of high-priced medications may be breathtaking, but would the resulting savings over those cured patients’ lifetimes offset the initial financial blow?
A new analysis unveiled at the annual meeting of the American Association for the Study of Liver Diseases calculated the impact of the new drugs on treatment costs and compared the cost of treatment with new drugs to the old standard of care.
“We found that the cost of treatment is very high, as expected,” explained lead investigator Jagpreet Chhatwal, Ph.D., of MD Anderson Cancer Center, Houston. In fact, if everyone who was eligible for the new drugs were treated, the cost over the next 5 years would be $136 billion.
“This is clearly unsustainable for any payer,” he noted. “So the question is: How can we manage to treat people who need this treatment?”
In a video interview, Dr. Chhatwal outlined how the researchers calculated their cost estimates, what cost savings could be gained with the new drugs, and how patients and payers alike could manage the price of treatment.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FROM THE LIVER MEETING 2014
VIDEO: How Clinicians Can Help Kids Make Smart Media Choices
SAN DIEGO – Digital technology and media are important components in children’s social and emotional development, and physicians can play a central role in ensuring kids make the right decisions when using those media.
“Because parents and kids trust them, pediatricians have an opportunity to educate parents across the country about the impact of media and digital technology on children,” explained James Steyer, founder of Common Sense Media in San Francisco.
In a video interview at the annual meeting of the American Academy of Pediatrics, Mr. Steyer talks about research on how media and digital technology affect children’s brain development, and how physicians can shape their young patients’ choices with techniques such as “media diets.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Digital technology and media are important components in children’s social and emotional development, and physicians can play a central role in ensuring kids make the right decisions when using those media.
“Because parents and kids trust them, pediatricians have an opportunity to educate parents across the country about the impact of media and digital technology on children,” explained James Steyer, founder of Common Sense Media in San Francisco.
In a video interview at the annual meeting of the American Academy of Pediatrics, Mr. Steyer talks about research on how media and digital technology affect children’s brain development, and how physicians can shape their young patients’ choices with techniques such as “media diets.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Digital technology and media are important components in children’s social and emotional development, and physicians can play a central role in ensuring kids make the right decisions when using those media.
“Because parents and kids trust them, pediatricians have an opportunity to educate parents across the country about the impact of media and digital technology on children,” explained James Steyer, founder of Common Sense Media in San Francisco.
In a video interview at the annual meeting of the American Academy of Pediatrics, Mr. Steyer talks about research on how media and digital technology affect children’s brain development, and how physicians can shape their young patients’ choices with techniques such as “media diets.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAP NATIONAL CONFERENCE
VIDEO: How physicians can help kids make smart media choices
SAN DIEGO – Digital technology and media are important components in children’s social and emotional development, and physicians can play a central role in ensuring kids make the right decisions when using those media.
“Because parents and kids trust them, pediatricians have an opportunity to educate parents across the country about the impact of media and digital technology on children,” explained James Steyer, founder of Common Sense Media in San Francisco.
In a video interview at the annual meeting of the American Academy of Pediatrics, Mr. Steyer talks about research on how media and digital technology affect children’s brain development, and how physicians can shape their young patients’ choices with techniques such as “media diets.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Digital technology and media are important components in children’s social and emotional development, and physicians can play a central role in ensuring kids make the right decisions when using those media.
“Because parents and kids trust them, pediatricians have an opportunity to educate parents across the country about the impact of media and digital technology on children,” explained James Steyer, founder of Common Sense Media in San Francisco.
In a video interview at the annual meeting of the American Academy of Pediatrics, Mr. Steyer talks about research on how media and digital technology affect children’s brain development, and how physicians can shape their young patients’ choices with techniques such as “media diets.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Digital technology and media are important components in children’s social and emotional development, and physicians can play a central role in ensuring kids make the right decisions when using those media.
“Because parents and kids trust them, pediatricians have an opportunity to educate parents across the country about the impact of media and digital technology on children,” explained James Steyer, founder of Common Sense Media in San Francisco.
In a video interview at the annual meeting of the American Academy of Pediatrics, Mr. Steyer talks about research on how media and digital technology affect children’s brain development, and how physicians can shape their young patients’ choices with techniques such as “media diets.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAP NATIONAL CONFERENCE
VIDEO: Pharmacogenomics can sharpen treatment choices in children
SAN DIEGO – Why do some children respond differently to medications than others? Pharmacogenomics is giving physicians a better understanding of differential responses and how to tailor treatment choices to individual patients’ genetic makeup.
Pharmacogenomics’ goal is to move away from the waste and potential dangers inherent in the typical empiric approach to medications, explained Dr. Marc Williams, director of the Geisinger Genomic Medicine Institute in Scranton, Pa. Instead, “our sort-of mantra is ‘the rights’: the right person with the right medication at the right time for the right reasons.”
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Williams talks about the promise of pharmacogenomics and the challenges faced in bringing genomic knowledge into pediatric clinical practice.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Why do some children respond differently to medications than others? Pharmacogenomics is giving physicians a better understanding of differential responses and how to tailor treatment choices to individual patients’ genetic makeup.
Pharmacogenomics’ goal is to move away from the waste and potential dangers inherent in the typical empiric approach to medications, explained Dr. Marc Williams, director of the Geisinger Genomic Medicine Institute in Scranton, Pa. Instead, “our sort-of mantra is ‘the rights’: the right person with the right medication at the right time for the right reasons.”
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Williams talks about the promise of pharmacogenomics and the challenges faced in bringing genomic knowledge into pediatric clinical practice.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Why do some children respond differently to medications than others? Pharmacogenomics is giving physicians a better understanding of differential responses and how to tailor treatment choices to individual patients’ genetic makeup.
Pharmacogenomics’ goal is to move away from the waste and potential dangers inherent in the typical empiric approach to medications, explained Dr. Marc Williams, director of the Geisinger Genomic Medicine Institute in Scranton, Pa. Instead, “our sort-of mantra is ‘the rights’: the right person with the right medication at the right time for the right reasons.”
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Williams talks about the promise of pharmacogenomics and the challenges faced in bringing genomic knowledge into pediatric clinical practice.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAP NATIONAL CONFERENCE
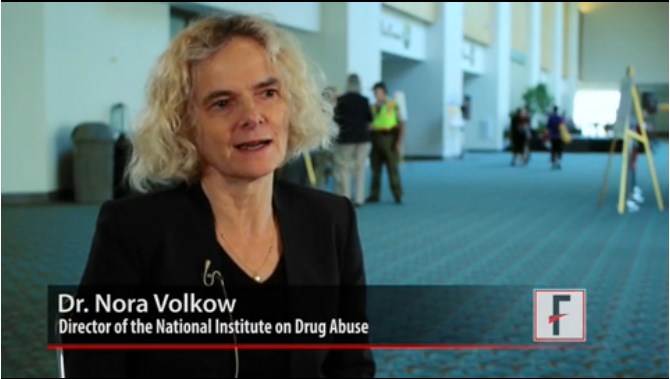
VIDEO: How physicians can reduce risks of adolescent drug addiction
SAN DIEGO – Children and adolescents are at great risk for experimentation with drugs, and they’re also more vulnerable than adults to addiction, warned Dr. Nora Volkow, director of the National Institute on Drug Abuse, Rockville, Md.
The adolescent brain is particularly malleable, she cautioned, which is why it changes faster than an adult’s brain when teenagers take drugs.
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Volkow discusses drug experimentation’s impact on teens’ decision-making, the long-term effects of addiction in adolescents, and the interventions that pediatricians can take to reduce the risk of teen drug use.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Children and adolescents are at great risk for experimentation with drugs, and they’re also more vulnerable than adults to addiction, warned Dr. Nora Volkow, director of the National Institute on Drug Abuse, Rockville, Md.
The adolescent brain is particularly malleable, she cautioned, which is why it changes faster than an adult’s brain when teenagers take drugs.
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Volkow discusses drug experimentation’s impact on teens’ decision-making, the long-term effects of addiction in adolescents, and the interventions that pediatricians can take to reduce the risk of teen drug use.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Children and adolescents are at great risk for experimentation with drugs, and they’re also more vulnerable than adults to addiction, warned Dr. Nora Volkow, director of the National Institute on Drug Abuse, Rockville, Md.
The adolescent brain is particularly malleable, she cautioned, which is why it changes faster than an adult’s brain when teenagers take drugs.
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Volkow discusses drug experimentation’s impact on teens’ decision-making, the long-term effects of addiction in adolescents, and the interventions that pediatricians can take to reduce the risk of teen drug use.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAP NATIONAL CONFERENCE
VIDEO: Telepsychiatry can reach children in underserved communities
SAN DIEGO – Telemedicine services can reach children with mental health needs in underserved rural and urban communities, but physicians must know how to find those services.
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Jane Oski of Tuba City (Ariz.) Regional Health Care explains how Medicaid reimbursement for such services varies by state, and where physicians treating children in underserved areas should start in their search for telepsychiatry services and resources.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Telemedicine services can reach children with mental health needs in underserved rural and urban communities, but physicians must know how to find those services.
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Jane Oski of Tuba City (Ariz.) Regional Health Care explains how Medicaid reimbursement for such services varies by state, and where physicians treating children in underserved areas should start in their search for telepsychiatry services and resources.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Telemedicine services can reach children with mental health needs in underserved rural and urban communities, but physicians must know how to find those services.
In a video interview at the annual meeting of the American Academy of Pediatrics, Dr. Jane Oski of Tuba City (Ariz.) Regional Health Care explains how Medicaid reimbursement for such services varies by state, and where physicians treating children in underserved areas should start in their search for telepsychiatry services and resources.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAP NATIONAL CONFERENCE
VIDEO: Ebola's U.S. threat low, but delivers infectious disease ‘wake-up call’
PHILADELPHIA – Despite the relatively limited threat Ebola poses to the United States, the disease’s arrival here “is a great wake-up message for us,” noted infectious disease expert Bruce Ribner.
“We have to be sensitive to the fact that ... people travel to areas where there are serious communicable diseases that are endemic,” noted Dr. Ribner, medical director of Emory University Hospital’s serious communicable diseases unit in Atlanta.
In an interview at IDWeek 2014, Dr. Ribner assessed Ebola’s low threat to the U.S. population, the resources available to contain that threat, and screening tactics to help contain the risks of infectious diseases beyond Ebola.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Despite the relatively limited threat Ebola poses to the United States, the disease’s arrival here “is a great wake-up message for us,” noted infectious disease expert Bruce Ribner.
“We have to be sensitive to the fact that ... people travel to areas where there are serious communicable diseases that are endemic,” noted Dr. Ribner, medical director of Emory University Hospital’s serious communicable diseases unit in Atlanta.
In an interview at IDWeek 2014, Dr. Ribner assessed Ebola’s low threat to the U.S. population, the resources available to contain that threat, and screening tactics to help contain the risks of infectious diseases beyond Ebola.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Despite the relatively limited threat Ebola poses to the United States, the disease’s arrival here “is a great wake-up message for us,” noted infectious disease expert Bruce Ribner.
“We have to be sensitive to the fact that ... people travel to areas where there are serious communicable diseases that are endemic,” noted Dr. Ribner, medical director of Emory University Hospital’s serious communicable diseases unit in Atlanta.
In an interview at IDWeek 2014, Dr. Ribner assessed Ebola’s low threat to the U.S. population, the resources available to contain that threat, and screening tactics to help contain the risks of infectious diseases beyond Ebola.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT IDWEEK 2014
VIDEO: How to diagnose multiple sclerosis in childhood and adolescence
PHILADELPHIA – Correctly identifying the onset of multiple sclerosis in childhood and adolescence can pose a difficult diagnostic challenge, but predictive factors including older age, female gender, and the presence of persistent lesions on MRI are more likely to point to a first attack of MS.
In an interview at the annual meeting of the American Academy of Neurology, Dr. Brenda Banwell of the University of Pennsylvania, Philadelphia, talked with Dr. Timothy Vartanian of New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, about the diagnostic keys to differentiating monophasic illnesses such as acute disseminated encephalomyelitis from the onset of multiple sclerosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Correctly identifying the onset of multiple sclerosis in childhood and adolescence can pose a difficult diagnostic challenge, but predictive factors including older age, female gender, and the presence of persistent lesions on MRI are more likely to point to a first attack of MS.
In an interview at the annual meeting of the American Academy of Neurology, Dr. Brenda Banwell of the University of Pennsylvania, Philadelphia, talked with Dr. Timothy Vartanian of New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, about the diagnostic keys to differentiating monophasic illnesses such as acute disseminated encephalomyelitis from the onset of multiple sclerosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHILADELPHIA – Correctly identifying the onset of multiple sclerosis in childhood and adolescence can pose a difficult diagnostic challenge, but predictive factors including older age, female gender, and the presence of persistent lesions on MRI are more likely to point to a first attack of MS.
In an interview at the annual meeting of the American Academy of Neurology, Dr. Brenda Banwell of the University of Pennsylvania, Philadelphia, talked with Dr. Timothy Vartanian of New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, about the diagnostic keys to differentiating monophasic illnesses such as acute disseminated encephalomyelitis from the onset of multiple sclerosis.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AAN 2014 ANNUAL MEETING