User login
In diabetes, women far more likely to develop CHD than men
Women with diabetes have a 44% greater chance of developing coronary heart disease than do men with diabetes, a large review and meta-analysis has shown.
In a retrospective review of data from more than 850,000 people that included over 28,000 confirmed coronary heart disease (CHD) events across the globe between 1966 and 2011, women with diabetes had nearly three times the likelihood (relative risk, 2.82) of developing CHD than did women without diabetes. Meanwhile, men with diabetes were only twice as likely (RR, 2.16) to have CHD than men without the disease. After adjustment for sex differences in other CHD factors such as tobacco use, women with diabetes had a 44% increased risk of developing heart disease, compared with men with the disease (RR, 1.44).
Sex differences in diabetes-related risk for CHD remained consistent across subgroups defined by age and region, and were unchanged when factoring nonfatal CHD events.
The study, conducted by researchers from Europe and Australia, appears online in Diabetologia 2014 [doi:10.1007/s00125-014-3260-6]. The findings corroborate a previous meta-analysis that also showed clinically meaningful sex differences lead to a greater CHD risk in women with diabetes than in men with diabetes (BMJ 2006;332:73-8 [doi:10.1136/bmj.38678.389583.7C]. Dr. Rachel Huxley of the University of Queensland School of Population Health in Australia, was an investigator in both studies.
Reasons for the disparity cannot be attributed to pharmacotherapy alone, according to the authors of the current study. Data reviewed in the study showed that women with diabetes were undertreated for cardiovascular disease risk factors prior to 1986, but that despite current increased awareness of the cardiovascular risks posed to women with diabetes, they are still less likely to achieve treatment targets.
“We hypothesize that the excess risk in women is due to a combination of both a greater deterioration in cardiovascular risk factor levels and a chronically elevated cardiovascular risk profile in the prediabetic state, driven by greater levels of adiposity in women, compared with men,” the authors wrote.
The authors cited previous research indicating that men develop diabetes at a lower body mass index (BMI), compared with women. As an example, in the UK General Practice Research Database, the BMI of those diagnosed with diabetes was on average 1.8 kg/m2 higher in women than in men. (Diabetologia 2012;55:1556-7).
“Greater awareness of early symptoms of CHD in women and sex-specific therapeutic risk factor management, irrespective of the presence of diabetes, is optimal for improving clinical outcomes in both women and men,” the authors concluded.
[email protected]
On Twitter @whitneymcknight
Women with diabetes have a 44% greater chance of developing coronary heart disease than do men with diabetes, a large review and meta-analysis has shown.
In a retrospective review of data from more than 850,000 people that included over 28,000 confirmed coronary heart disease (CHD) events across the globe between 1966 and 2011, women with diabetes had nearly three times the likelihood (relative risk, 2.82) of developing CHD than did women without diabetes. Meanwhile, men with diabetes were only twice as likely (RR, 2.16) to have CHD than men without the disease. After adjustment for sex differences in other CHD factors such as tobacco use, women with diabetes had a 44% increased risk of developing heart disease, compared with men with the disease (RR, 1.44).
Sex differences in diabetes-related risk for CHD remained consistent across subgroups defined by age and region, and were unchanged when factoring nonfatal CHD events.
The study, conducted by researchers from Europe and Australia, appears online in Diabetologia 2014 [doi:10.1007/s00125-014-3260-6]. The findings corroborate a previous meta-analysis that also showed clinically meaningful sex differences lead to a greater CHD risk in women with diabetes than in men with diabetes (BMJ 2006;332:73-8 [doi:10.1136/bmj.38678.389583.7C]. Dr. Rachel Huxley of the University of Queensland School of Population Health in Australia, was an investigator in both studies.
Reasons for the disparity cannot be attributed to pharmacotherapy alone, according to the authors of the current study. Data reviewed in the study showed that women with diabetes were undertreated for cardiovascular disease risk factors prior to 1986, but that despite current increased awareness of the cardiovascular risks posed to women with diabetes, they are still less likely to achieve treatment targets.
“We hypothesize that the excess risk in women is due to a combination of both a greater deterioration in cardiovascular risk factor levels and a chronically elevated cardiovascular risk profile in the prediabetic state, driven by greater levels of adiposity in women, compared with men,” the authors wrote.
The authors cited previous research indicating that men develop diabetes at a lower body mass index (BMI), compared with women. As an example, in the UK General Practice Research Database, the BMI of those diagnosed with diabetes was on average 1.8 kg/m2 higher in women than in men. (Diabetologia 2012;55:1556-7).
“Greater awareness of early symptoms of CHD in women and sex-specific therapeutic risk factor management, irrespective of the presence of diabetes, is optimal for improving clinical outcomes in both women and men,” the authors concluded.
[email protected]
On Twitter @whitneymcknight
Women with diabetes have a 44% greater chance of developing coronary heart disease than do men with diabetes, a large review and meta-analysis has shown.
In a retrospective review of data from more than 850,000 people that included over 28,000 confirmed coronary heart disease (CHD) events across the globe between 1966 and 2011, women with diabetes had nearly three times the likelihood (relative risk, 2.82) of developing CHD than did women without diabetes. Meanwhile, men with diabetes were only twice as likely (RR, 2.16) to have CHD than men without the disease. After adjustment for sex differences in other CHD factors such as tobacco use, women with diabetes had a 44% increased risk of developing heart disease, compared with men with the disease (RR, 1.44).
Sex differences in diabetes-related risk for CHD remained consistent across subgroups defined by age and region, and were unchanged when factoring nonfatal CHD events.
The study, conducted by researchers from Europe and Australia, appears online in Diabetologia 2014 [doi:10.1007/s00125-014-3260-6]. The findings corroborate a previous meta-analysis that also showed clinically meaningful sex differences lead to a greater CHD risk in women with diabetes than in men with diabetes (BMJ 2006;332:73-8 [doi:10.1136/bmj.38678.389583.7C]. Dr. Rachel Huxley of the University of Queensland School of Population Health in Australia, was an investigator in both studies.
Reasons for the disparity cannot be attributed to pharmacotherapy alone, according to the authors of the current study. Data reviewed in the study showed that women with diabetes were undertreated for cardiovascular disease risk factors prior to 1986, but that despite current increased awareness of the cardiovascular risks posed to women with diabetes, they are still less likely to achieve treatment targets.
“We hypothesize that the excess risk in women is due to a combination of both a greater deterioration in cardiovascular risk factor levels and a chronically elevated cardiovascular risk profile in the prediabetic state, driven by greater levels of adiposity in women, compared with men,” the authors wrote.
The authors cited previous research indicating that men develop diabetes at a lower body mass index (BMI), compared with women. As an example, in the UK General Practice Research Database, the BMI of those diagnosed with diabetes was on average 1.8 kg/m2 higher in women than in men. (Diabetologia 2012;55:1556-7).
“Greater awareness of early symptoms of CHD in women and sex-specific therapeutic risk factor management, irrespective of the presence of diabetes, is optimal for improving clinical outcomes in both women and men,” the authors concluded.
[email protected]
On Twitter @whitneymcknight
FROM DIABETOLOGIA
Key clinical point: Consider screening asymptomatic women for diabetes and offering risk
factor management.
Major finding: Women with diabetes are 44% more
likely to develop CHD than men with diabetes.
Data source: Systematic review and meta-analysis of
more than 850,000 people and over 28,000 CHD events recorded in 64 studies
worldwide between 1966 and 2011.
Disclosures: The authors of this study declared
they had no relevant disclosures.
Dalfampridine’s effects on walking ability in MS extend to 24 weeks
PHILADELPHIA – Dalfampridine was shown to improve walking ability and balance in patients with progressive and relapsing-remitting multiple sclerosis, according to data presented at the annual meeting of the American Academy of Neurology.
For a more integrated assessment of dalfampridine’s effect on patients’ walking abilities over a longer period of time, Dr. Jan Lycke of the University of Gothenberg (Sweden) and his associates randomized 132 patients with MS and an Expanded Disability Status Scale score of 4-7 to 24 weeks of dalfampridine or placebo in the double-blind trial called MOBILE (Exploratory Study to Assess the Effect of Fampridine on Walking Ability and Balance in Patients With Multiple Sclerosis).
The study was conducted in Canada and European countries with prolonged-release fampridine (Fampyra), known as dalfampridine (Ampyra) in the United States. Dalfampridine was approved in the United States in 2010 as the first oral medication for MS based on its ability to improve walking speed, although it has since been associated with seizures in some patients in doses above the recommended 10 mg twice daily.
The 68 patients who took dalfampridine 10 mg twice daily and the 64 in the placebo group were assessed using the Multiple Sclerosis Walking Scale-12 (MSWS-12), the Multiple Sclerosis Impact Scale-29 (MSIS-29), the Timed Up and Go (TUG), and the Berg Balance Scale (BBS).
Nearly half of patients in the treatment arm (49% vs. 28.1% on placebo; P = .015) reached or exceeded the clinically meaningful threshold of at least an 8-point improvement on the MSWS-12, beginning in weeks 2-4 and then sustained throughout the study period, Dr. Lycke said.
"There was a median improvement change in the [TUG] measurement of at least 10%-15% [47.1% vs. 30.2% placebo; P = .026], which was sustained throughout the treatment period," he told the audience. A 15% or greater improvement of the TUG score was considered clinically meaningful. This cohort had similar improvement rates over baseline for BBS scores, he said.
Dalfampridine treatment led to greater median treatment differences from baseline to week 24, compared with placebo, on the MSWS-12 (–3.27; 95% confidence interval, –7.59-1.19), TUG speed (9.64%; 95% CI, 2.05%-16.48%), BBS score (1.50; 95% CI, 0.00-2.93), and MSIS-29 physical subscale (–3.30; 95% CI, –7.68-0.98). After treatment discontinuation at week 24, the measurements returned to baseline levels.
No seizures were recorded during the trial, Dr. Lycke said.
The trial was sponsored by Biogen Idec, which holds a licensing agreement with Acorda Therapeutics to market prolonged-released fampridine outside of the United States. Dr. Lycke had numerous disclosures, including Biogen Idec, Genzyme, Novartis, and Teva.
On Twitter @whitneymcknight
PHILADELPHIA – Dalfampridine was shown to improve walking ability and balance in patients with progressive and relapsing-remitting multiple sclerosis, according to data presented at the annual meeting of the American Academy of Neurology.
For a more integrated assessment of dalfampridine’s effect on patients’ walking abilities over a longer period of time, Dr. Jan Lycke of the University of Gothenberg (Sweden) and his associates randomized 132 patients with MS and an Expanded Disability Status Scale score of 4-7 to 24 weeks of dalfampridine or placebo in the double-blind trial called MOBILE (Exploratory Study to Assess the Effect of Fampridine on Walking Ability and Balance in Patients With Multiple Sclerosis).
The study was conducted in Canada and European countries with prolonged-release fampridine (Fampyra), known as dalfampridine (Ampyra) in the United States. Dalfampridine was approved in the United States in 2010 as the first oral medication for MS based on its ability to improve walking speed, although it has since been associated with seizures in some patients in doses above the recommended 10 mg twice daily.
The 68 patients who took dalfampridine 10 mg twice daily and the 64 in the placebo group were assessed using the Multiple Sclerosis Walking Scale-12 (MSWS-12), the Multiple Sclerosis Impact Scale-29 (MSIS-29), the Timed Up and Go (TUG), and the Berg Balance Scale (BBS).
Nearly half of patients in the treatment arm (49% vs. 28.1% on placebo; P = .015) reached or exceeded the clinically meaningful threshold of at least an 8-point improvement on the MSWS-12, beginning in weeks 2-4 and then sustained throughout the study period, Dr. Lycke said.
"There was a median improvement change in the [TUG] measurement of at least 10%-15% [47.1% vs. 30.2% placebo; P = .026], which was sustained throughout the treatment period," he told the audience. A 15% or greater improvement of the TUG score was considered clinically meaningful. This cohort had similar improvement rates over baseline for BBS scores, he said.
Dalfampridine treatment led to greater median treatment differences from baseline to week 24, compared with placebo, on the MSWS-12 (–3.27; 95% confidence interval, –7.59-1.19), TUG speed (9.64%; 95% CI, 2.05%-16.48%), BBS score (1.50; 95% CI, 0.00-2.93), and MSIS-29 physical subscale (–3.30; 95% CI, –7.68-0.98). After treatment discontinuation at week 24, the measurements returned to baseline levels.
No seizures were recorded during the trial, Dr. Lycke said.
The trial was sponsored by Biogen Idec, which holds a licensing agreement with Acorda Therapeutics to market prolonged-released fampridine outside of the United States. Dr. Lycke had numerous disclosures, including Biogen Idec, Genzyme, Novartis, and Teva.
On Twitter @whitneymcknight
PHILADELPHIA – Dalfampridine was shown to improve walking ability and balance in patients with progressive and relapsing-remitting multiple sclerosis, according to data presented at the annual meeting of the American Academy of Neurology.
For a more integrated assessment of dalfampridine’s effect on patients’ walking abilities over a longer period of time, Dr. Jan Lycke of the University of Gothenberg (Sweden) and his associates randomized 132 patients with MS and an Expanded Disability Status Scale score of 4-7 to 24 weeks of dalfampridine or placebo in the double-blind trial called MOBILE (Exploratory Study to Assess the Effect of Fampridine on Walking Ability and Balance in Patients With Multiple Sclerosis).
The study was conducted in Canada and European countries with prolonged-release fampridine (Fampyra), known as dalfampridine (Ampyra) in the United States. Dalfampridine was approved in the United States in 2010 as the first oral medication for MS based on its ability to improve walking speed, although it has since been associated with seizures in some patients in doses above the recommended 10 mg twice daily.
The 68 patients who took dalfampridine 10 mg twice daily and the 64 in the placebo group were assessed using the Multiple Sclerosis Walking Scale-12 (MSWS-12), the Multiple Sclerosis Impact Scale-29 (MSIS-29), the Timed Up and Go (TUG), and the Berg Balance Scale (BBS).
Nearly half of patients in the treatment arm (49% vs. 28.1% on placebo; P = .015) reached or exceeded the clinically meaningful threshold of at least an 8-point improvement on the MSWS-12, beginning in weeks 2-4 and then sustained throughout the study period, Dr. Lycke said.
"There was a median improvement change in the [TUG] measurement of at least 10%-15% [47.1% vs. 30.2% placebo; P = .026], which was sustained throughout the treatment period," he told the audience. A 15% or greater improvement of the TUG score was considered clinically meaningful. This cohort had similar improvement rates over baseline for BBS scores, he said.
Dalfampridine treatment led to greater median treatment differences from baseline to week 24, compared with placebo, on the MSWS-12 (–3.27; 95% confidence interval, –7.59-1.19), TUG speed (9.64%; 95% CI, 2.05%-16.48%), BBS score (1.50; 95% CI, 0.00-2.93), and MSIS-29 physical subscale (–3.30; 95% CI, –7.68-0.98). After treatment discontinuation at week 24, the measurements returned to baseline levels.
No seizures were recorded during the trial, Dr. Lycke said.
The trial was sponsored by Biogen Idec, which holds a licensing agreement with Acorda Therapeutics to market prolonged-released fampridine outside of the United States. Dr. Lycke had numerous disclosures, including Biogen Idec, Genzyme, Novartis, and Teva.
On Twitter @whitneymcknight
AT THE AAN 2014 ANNUAL MEETING
Key clinical point: The improvements in walking ability that are observed with dalfampridine extend to at least 24 weeks.
Major finding: Nearly half of dalfampridine-treated patients improved at least 8 or more points on the MSWS-12 scale and saw a 15% or greater improvement in their TUG speed, compared with only a third of the placebo arm.
Data source: A 24-week, double-blind, placebo-controlled, randomized study of 132 patients with MS.
Disclosures: The trial was sponsored by Biogen Idec. Dr. Lycke had numerous disclosures, including Biogen Idec, Genzyme, Novartis, and Teva.
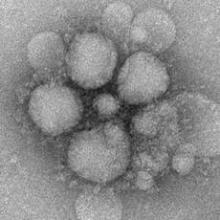
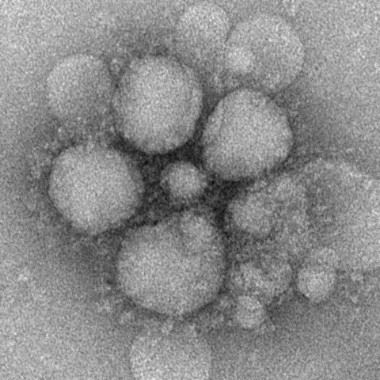
Illinois man tests positive for MERS CoV after contact with infected patient
An Illinois citizen who came in contact with the first Middle Eastern Respiratory Syndrome Coronavirus patient detected in the United States has tested positive for the virus, according to a statement from the Centers for Disease Control and Prevention on May 17.
"This latest development does not change CDC’s current recommendations to prevent the spread of MERS," Dr. David Swerdlow, who is heading the CDC’s response to the virus, said in the statement. "It’s possible that as the investigation continues others may also test positive for MERS-CoV infection but not get sick. Along with state and local health experts, CDC will investigate those initial cases and if new information is learned that requires us to change our prevention recommendations, we can do so," said Dr. Swerdlow.
The laboratory test results are "preliminary and suggest that the Illinois resident probably got the virus from the Indiana patient and the person’s body developed antibodies to fight the virus," according to the CDC statement.
The previously reported Indiana MERS patient recently had returned from Saudi Arabia when he met with a business associate in Illinois. Shortly after the meeting, the Indiana man was identified as having MERS. The business associate in Illinois, whom the CDC said has no history of travel to the Arabian Peninsula, was tested soon after. Initial results of the Illinois man’s test performed on May 5 were negative, but on May 16, he was found to have antibodies to MERS-CoV.
"At this time he’s reported to have had mild cold-like symptoms, but he did not seek or require medical care since exposure to the Indiana MERS patient. He is currently reported to be feeling well," Dr. Swerdlow told reporters during a CDC telebriefing. "Public health officials have advised him to remain in self-isolation until further tests are completed."
The investigation into the Indiana case is ongoing. "We don’t know exactly when people transmit [the virus]. We do know that the Indiana patient was having symptoms at the time of the interaction [with the Illinois man]", said Dr. Swerdlow.
To date, there have been two confirmed imported cases of MERS in the United States: The first in Indiana on May 2; the second in Florida on May 11.
MERS was first detected in Saudi Arabia in 2012, and has since spread through out the Arabian Peninsula. MERS typically presents in most patients as severe acute respiratory illness with symptoms of fever, cough, and shortness of breath. In some instances, the virus has spread from person to person through close contact. However, at this time, the CDC is not reporting evidence of sustained spread of MERS-CoV in community settings.
On Twitter @whitneymcknight
An Illinois citizen who came in contact with the first Middle Eastern Respiratory Syndrome Coronavirus patient detected in the United States has tested positive for the virus, according to a statement from the Centers for Disease Control and Prevention on May 17.
"This latest development does not change CDC’s current recommendations to prevent the spread of MERS," Dr. David Swerdlow, who is heading the CDC’s response to the virus, said in the statement. "It’s possible that as the investigation continues others may also test positive for MERS-CoV infection but not get sick. Along with state and local health experts, CDC will investigate those initial cases and if new information is learned that requires us to change our prevention recommendations, we can do so," said Dr. Swerdlow.
The laboratory test results are "preliminary and suggest that the Illinois resident probably got the virus from the Indiana patient and the person’s body developed antibodies to fight the virus," according to the CDC statement.
The previously reported Indiana MERS patient recently had returned from Saudi Arabia when he met with a business associate in Illinois. Shortly after the meeting, the Indiana man was identified as having MERS. The business associate in Illinois, whom the CDC said has no history of travel to the Arabian Peninsula, was tested soon after. Initial results of the Illinois man’s test performed on May 5 were negative, but on May 16, he was found to have antibodies to MERS-CoV.
"At this time he’s reported to have had mild cold-like symptoms, but he did not seek or require medical care since exposure to the Indiana MERS patient. He is currently reported to be feeling well," Dr. Swerdlow told reporters during a CDC telebriefing. "Public health officials have advised him to remain in self-isolation until further tests are completed."
The investigation into the Indiana case is ongoing. "We don’t know exactly when people transmit [the virus]. We do know that the Indiana patient was having symptoms at the time of the interaction [with the Illinois man]", said Dr. Swerdlow.
To date, there have been two confirmed imported cases of MERS in the United States: The first in Indiana on May 2; the second in Florida on May 11.
MERS was first detected in Saudi Arabia in 2012, and has since spread through out the Arabian Peninsula. MERS typically presents in most patients as severe acute respiratory illness with symptoms of fever, cough, and shortness of breath. In some instances, the virus has spread from person to person through close contact. However, at this time, the CDC is not reporting evidence of sustained spread of MERS-CoV in community settings.
On Twitter @whitneymcknight
An Illinois citizen who came in contact with the first Middle Eastern Respiratory Syndrome Coronavirus patient detected in the United States has tested positive for the virus, according to a statement from the Centers for Disease Control and Prevention on May 17.
"This latest development does not change CDC’s current recommendations to prevent the spread of MERS," Dr. David Swerdlow, who is heading the CDC’s response to the virus, said in the statement. "It’s possible that as the investigation continues others may also test positive for MERS-CoV infection but not get sick. Along with state and local health experts, CDC will investigate those initial cases and if new information is learned that requires us to change our prevention recommendations, we can do so," said Dr. Swerdlow.
The laboratory test results are "preliminary and suggest that the Illinois resident probably got the virus from the Indiana patient and the person’s body developed antibodies to fight the virus," according to the CDC statement.
The previously reported Indiana MERS patient recently had returned from Saudi Arabia when he met with a business associate in Illinois. Shortly after the meeting, the Indiana man was identified as having MERS. The business associate in Illinois, whom the CDC said has no history of travel to the Arabian Peninsula, was tested soon after. Initial results of the Illinois man’s test performed on May 5 were negative, but on May 16, he was found to have antibodies to MERS-CoV.
"At this time he’s reported to have had mild cold-like symptoms, but he did not seek or require medical care since exposure to the Indiana MERS patient. He is currently reported to be feeling well," Dr. Swerdlow told reporters during a CDC telebriefing. "Public health officials have advised him to remain in self-isolation until further tests are completed."
The investigation into the Indiana case is ongoing. "We don’t know exactly when people transmit [the virus]. We do know that the Indiana patient was having symptoms at the time of the interaction [with the Illinois man]", said Dr. Swerdlow.
To date, there have been two confirmed imported cases of MERS in the United States: The first in Indiana on May 2; the second in Florida on May 11.
MERS was first detected in Saudi Arabia in 2012, and has since spread through out the Arabian Peninsula. MERS typically presents in most patients as severe acute respiratory illness with symptoms of fever, cough, and shortness of breath. In some instances, the virus has spread from person to person through close contact. However, at this time, the CDC is not reporting evidence of sustained spread of MERS-CoV in community settings.
On Twitter @whitneymcknight
Magnetic foreign body injury rate on the rise
Magnetic foreign body–related injuries increased significantly between 2002 and 2012, particularly those involving multiple magnet ingestion, according to a retrospective study.
"With the advent of stronger neodymium-iron-boron magnets and their inclusion as part of children’s toys, jewelry, and desk toys, there has been a documented increased in the number of cases resulting in serious morbidity and in rare cases, mortality," Dr. Matt Strickland of the Hospital for Sick Children, Toronto, and his associates, said in a report published online in the Journal of Pediatrics.
In a chart review of electronic emergency department (ED) records from a single urban tertiary site between April 1, 2002 and December 31, 2012, of 2,722 patients aged 18 years or younger, 94 were admitted for suspicion of magnet ingestion. In 75 (3%) patients, magnet ingestion was confirmed after removal or by a combination of history and imaging.
In 2010, shortly after smaller, more powerful magnets, often sold in multiples, were introduced to the marketplace, the incidence rate ratio (IRR) of magnet-related injuries increased by a factor of 2.94 (95% confidence interval, 1.84-4.70). Injuries involving multiple magnets increased by a factor of 8.40 (95% CI, 3.44-20.56). Of the confirmed ingestions, 65% were male, with a median age of 4.6 years. The volume of the magnets decreased from 878.6 mm3 to 259.8 mm3 during the years studied, as measured by radiography (P = .04), they reported (J. Pediatr. 2014 May 8 [doi:10.1016/j.jpeds.2014.04.002]).
Dr. Strickland and his associates noted that multiple magnets "pose the unique danger of being able to attract each other through different loops of bowel, arresting their movement, and potentially causing mural pressure necrosis." Six of the cases recorded in the study required the surgical removal of magnets because of intraabdominal sepsis or suspected imminent bowel perforation. Ten cases required endoscopic removal of magnets. Multiple magnet ingestion also can result in fistulas, volvulus, obstruction, and even death, although no deaths were recorded in this study.
Study limitations of note include the possibility that, after 2010, media attention and recalls of products with the magnets might have heightened public sensitivity to the dangers of magnet ingestion, driving up the number of patients admitted to the ED in the latter years of the study period.
The authors of this study did not declare any conflicts of interest.
On Twitter @whitneymcknight
Magnetic foreign body–related injuries increased significantly between 2002 and 2012, particularly those involving multiple magnet ingestion, according to a retrospective study.
"With the advent of stronger neodymium-iron-boron magnets and their inclusion as part of children’s toys, jewelry, and desk toys, there has been a documented increased in the number of cases resulting in serious morbidity and in rare cases, mortality," Dr. Matt Strickland of the Hospital for Sick Children, Toronto, and his associates, said in a report published online in the Journal of Pediatrics.
In a chart review of electronic emergency department (ED) records from a single urban tertiary site between April 1, 2002 and December 31, 2012, of 2,722 patients aged 18 years or younger, 94 were admitted for suspicion of magnet ingestion. In 75 (3%) patients, magnet ingestion was confirmed after removal or by a combination of history and imaging.
In 2010, shortly after smaller, more powerful magnets, often sold in multiples, were introduced to the marketplace, the incidence rate ratio (IRR) of magnet-related injuries increased by a factor of 2.94 (95% confidence interval, 1.84-4.70). Injuries involving multiple magnets increased by a factor of 8.40 (95% CI, 3.44-20.56). Of the confirmed ingestions, 65% were male, with a median age of 4.6 years. The volume of the magnets decreased from 878.6 mm3 to 259.8 mm3 during the years studied, as measured by radiography (P = .04), they reported (J. Pediatr. 2014 May 8 [doi:10.1016/j.jpeds.2014.04.002]).
Dr. Strickland and his associates noted that multiple magnets "pose the unique danger of being able to attract each other through different loops of bowel, arresting their movement, and potentially causing mural pressure necrosis." Six of the cases recorded in the study required the surgical removal of magnets because of intraabdominal sepsis or suspected imminent bowel perforation. Ten cases required endoscopic removal of magnets. Multiple magnet ingestion also can result in fistulas, volvulus, obstruction, and even death, although no deaths were recorded in this study.
Study limitations of note include the possibility that, after 2010, media attention and recalls of products with the magnets might have heightened public sensitivity to the dangers of magnet ingestion, driving up the number of patients admitted to the ED in the latter years of the study period.
The authors of this study did not declare any conflicts of interest.
On Twitter @whitneymcknight
Magnetic foreign body–related injuries increased significantly between 2002 and 2012, particularly those involving multiple magnet ingestion, according to a retrospective study.
"With the advent of stronger neodymium-iron-boron magnets and their inclusion as part of children’s toys, jewelry, and desk toys, there has been a documented increased in the number of cases resulting in serious morbidity and in rare cases, mortality," Dr. Matt Strickland of the Hospital for Sick Children, Toronto, and his associates, said in a report published online in the Journal of Pediatrics.
In a chart review of electronic emergency department (ED) records from a single urban tertiary site between April 1, 2002 and December 31, 2012, of 2,722 patients aged 18 years or younger, 94 were admitted for suspicion of magnet ingestion. In 75 (3%) patients, magnet ingestion was confirmed after removal or by a combination of history and imaging.
In 2010, shortly after smaller, more powerful magnets, often sold in multiples, were introduced to the marketplace, the incidence rate ratio (IRR) of magnet-related injuries increased by a factor of 2.94 (95% confidence interval, 1.84-4.70). Injuries involving multiple magnets increased by a factor of 8.40 (95% CI, 3.44-20.56). Of the confirmed ingestions, 65% were male, with a median age of 4.6 years. The volume of the magnets decreased from 878.6 mm3 to 259.8 mm3 during the years studied, as measured by radiography (P = .04), they reported (J. Pediatr. 2014 May 8 [doi:10.1016/j.jpeds.2014.04.002]).
Dr. Strickland and his associates noted that multiple magnets "pose the unique danger of being able to attract each other through different loops of bowel, arresting their movement, and potentially causing mural pressure necrosis." Six of the cases recorded in the study required the surgical removal of magnets because of intraabdominal sepsis or suspected imminent bowel perforation. Ten cases required endoscopic removal of magnets. Multiple magnet ingestion also can result in fistulas, volvulus, obstruction, and even death, although no deaths were recorded in this study.
Study limitations of note include the possibility that, after 2010, media attention and recalls of products with the magnets might have heightened public sensitivity to the dangers of magnet ingestion, driving up the number of patients admitted to the ED in the latter years of the study period.
The authors of this study did not declare any conflicts of interest.
On Twitter @whitneymcknight
FROM THE JOURNAL OF PEDIATRICS
Key clinical point: Parents and providers should be aware of dangers posed by today’s smaller, stronger magnets, especially if ingested in multiples.
Major finding: ED visits for magnet ingestion increased by a factor of 2.94 between the periods 2002-2009 and 2010-2012; ED visits for multiple magnet ingestion over the same time span increased by a factor of 8.40.
Data source: Chart review of patients 18 years of age and younger admitted to ED with magnetic foreign body ingestion at a single urban tertiary site between 2002 and 2012.
Disclosures: The authors of this study did not declare any conflicts of interest.
Vertical incision at C-section in morbidly obese women led to lower infection rates
NEW ORLEANS – Vertical incisions in morbidly obese women undergoing a primary cesarean delivery are associated with fewer wound complications, compared with transverse incisions.
The findings were "contrary to expectations," presenter Dr. Caroline C. Marrs told an audience at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The registry study of morbidly obese women who had had a primary C-section showed that those with a vertical incision were found to have higher rates of all adverse maternal outcomes, except for transfusions, but had lower incision-to-delivery times (9.2 plus or minus 5.5 vs. 11.1 plus or minus 6.1, P less than .001). "However, there was significant confounder bias, because after adjusting for significant baseline and clinical characteristics such as race, smoking status, and body mass index, vertical incisions were not associated with higher rates of composite maternal morbidity," said Dr. Marrs of the University of Texas Health Science Center in Houston.
Using data collected between 1999 and 2002 for the cesarean registry of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network from 19 academic medical centers, Dr. Marrs and her colleagues identified 3,200 women with a body mass index of 40 kg/m2 at the time of their delivery by primary C-section whose incision type was known
The transverse skin incision cohort numbered 2,603 (81%), and the vertical incision group was 597 (19%).
An analysis of patient characteristics indicated the type of incision a woman had positively correlated with her race, smoking status, and insurance type, as well as whether the woman had gestational diabetes, chorioamnionitis, non–lower-segment hysterotomy, and an emergency C-section.
Logistical regression showed that vertical skin incisions were associated with parity (1.16, adjusted odds ratio 1.09-1.25); black race (1.24, AOR 1.03-1.51), maternal body mass index (1.06, AOR 1.04-1.08), low transverse hysterotomy (4.46, AOR 3.21-6.20), and nonemergent cesarean delivery (0.49, AOR 0.39-0.62).
A univariate analysis of composite wound complications such as seroma or hematoma indicated that vertical wounds were more associated with higher complication rates (4.2% of the vertical group vs. 1.7% of the transverse group, P less than .001).
Multivariate progression analysis indicated that the adjusted odds ratio for a vertical incision being a risk factor for wound complications was 0.32 (0.17-62). Other risk factors noted were: nonwhite race (0.48, AOR 0.25 to 0.94), maternal BMI (1.05, AOR 1.00 to 1.09), and ASA score (2.10, AOR 1.21-3.65).
"We suspect selection bias played a role," said Dr. Marrs. "Given the differences in baseline clinical characteristics of women who had vertical incisions, surgeons may have chosen this route based on selected factors such as BMI or need for emergency delivery."
Dr. Marrs did not have any relevant disclosures.
NEW ORLEANS – Vertical incisions in morbidly obese women undergoing a primary cesarean delivery are associated with fewer wound complications, compared with transverse incisions.
The findings were "contrary to expectations," presenter Dr. Caroline C. Marrs told an audience at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The registry study of morbidly obese women who had had a primary C-section showed that those with a vertical incision were found to have higher rates of all adverse maternal outcomes, except for transfusions, but had lower incision-to-delivery times (9.2 plus or minus 5.5 vs. 11.1 plus or minus 6.1, P less than .001). "However, there was significant confounder bias, because after adjusting for significant baseline and clinical characteristics such as race, smoking status, and body mass index, vertical incisions were not associated with higher rates of composite maternal morbidity," said Dr. Marrs of the University of Texas Health Science Center in Houston.
Using data collected between 1999 and 2002 for the cesarean registry of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network from 19 academic medical centers, Dr. Marrs and her colleagues identified 3,200 women with a body mass index of 40 kg/m2 at the time of their delivery by primary C-section whose incision type was known
The transverse skin incision cohort numbered 2,603 (81%), and the vertical incision group was 597 (19%).
An analysis of patient characteristics indicated the type of incision a woman had positively correlated with her race, smoking status, and insurance type, as well as whether the woman had gestational diabetes, chorioamnionitis, non–lower-segment hysterotomy, and an emergency C-section.
Logistical regression showed that vertical skin incisions were associated with parity (1.16, adjusted odds ratio 1.09-1.25); black race (1.24, AOR 1.03-1.51), maternal body mass index (1.06, AOR 1.04-1.08), low transverse hysterotomy (4.46, AOR 3.21-6.20), and nonemergent cesarean delivery (0.49, AOR 0.39-0.62).
A univariate analysis of composite wound complications such as seroma or hematoma indicated that vertical wounds were more associated with higher complication rates (4.2% of the vertical group vs. 1.7% of the transverse group, P less than .001).
Multivariate progression analysis indicated that the adjusted odds ratio for a vertical incision being a risk factor for wound complications was 0.32 (0.17-62). Other risk factors noted were: nonwhite race (0.48, AOR 0.25 to 0.94), maternal BMI (1.05, AOR 1.00 to 1.09), and ASA score (2.10, AOR 1.21-3.65).
"We suspect selection bias played a role," said Dr. Marrs. "Given the differences in baseline clinical characteristics of women who had vertical incisions, surgeons may have chosen this route based on selected factors such as BMI or need for emergency delivery."
Dr. Marrs did not have any relevant disclosures.
NEW ORLEANS – Vertical incisions in morbidly obese women undergoing a primary cesarean delivery are associated with fewer wound complications, compared with transverse incisions.
The findings were "contrary to expectations," presenter Dr. Caroline C. Marrs told an audience at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The registry study of morbidly obese women who had had a primary C-section showed that those with a vertical incision were found to have higher rates of all adverse maternal outcomes, except for transfusions, but had lower incision-to-delivery times (9.2 plus or minus 5.5 vs. 11.1 plus or minus 6.1, P less than .001). "However, there was significant confounder bias, because after adjusting for significant baseline and clinical characteristics such as race, smoking status, and body mass index, vertical incisions were not associated with higher rates of composite maternal morbidity," said Dr. Marrs of the University of Texas Health Science Center in Houston.
Using data collected between 1999 and 2002 for the cesarean registry of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network from 19 academic medical centers, Dr. Marrs and her colleagues identified 3,200 women with a body mass index of 40 kg/m2 at the time of their delivery by primary C-section whose incision type was known
The transverse skin incision cohort numbered 2,603 (81%), and the vertical incision group was 597 (19%).
An analysis of patient characteristics indicated the type of incision a woman had positively correlated with her race, smoking status, and insurance type, as well as whether the woman had gestational diabetes, chorioamnionitis, non–lower-segment hysterotomy, and an emergency C-section.
Logistical regression showed that vertical skin incisions were associated with parity (1.16, adjusted odds ratio 1.09-1.25); black race (1.24, AOR 1.03-1.51), maternal body mass index (1.06, AOR 1.04-1.08), low transverse hysterotomy (4.46, AOR 3.21-6.20), and nonemergent cesarean delivery (0.49, AOR 0.39-0.62).
A univariate analysis of composite wound complications such as seroma or hematoma indicated that vertical wounds were more associated with higher complication rates (4.2% of the vertical group vs. 1.7% of the transverse group, P less than .001).
Multivariate progression analysis indicated that the adjusted odds ratio for a vertical incision being a risk factor for wound complications was 0.32 (0.17-62). Other risk factors noted were: nonwhite race (0.48, AOR 0.25 to 0.94), maternal BMI (1.05, AOR 1.00 to 1.09), and ASA score (2.10, AOR 1.21-3.65).
"We suspect selection bias played a role," said Dr. Marrs. "Given the differences in baseline clinical characteristics of women who had vertical incisions, surgeons may have chosen this route based on selected factors such as BMI or need for emergency delivery."
Dr. Marrs did not have any relevant disclosures.
AT THE PREGNANCY MEETING
Key clinical point: Vertical incisions at primary C-section appear to be a better choice for morbidly obese women, at least in terms of infection rate.
Major finding: Vertical incisions are associated with lower wound complication rates compared with transverse incisions in morbidly obese pregnant women.
Data source: Registry cohort study with multivariate analysis of 3,200 morbidly obese women who underwent primary cesarean delivery: 2,603 with a transverse incision and 597 with a vertical one.
Disclosures: Dr. Marrs did not have any relevant disclosures.
Parents, teens misunderstand parameters of confidential interviews
PHILADELPHIA – Despite an overall agreement on its merit, both parents and their adolescent daughters are leery of the confidential interview in the gynecologic setting, in part because each cohort believes that it is tantamount to parents being excluded in the teen’s health care decision-making process.
"The majority of parents felt that this was inappropriate for their teen because this was a specialized setting," Dr. Gylynthia E. Trotman, a second-year fellow at Medstar Washington Hospital Center, Children’s National Medical Center, said in an interview.
"The adolescent felt that way, too, which came as a shock to us," Dr. Trotman said during the poster session at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology. "They wanted parents to be a part of their decision making."
The data, derived from a survey of 62 pairs of parents and 62 of their collective adolescent daughters between the ages of 11 and 17 years, showed that while 85% of teens and 78% of parents thought the confidential interview was beneficial, 31% and 40% respectively thought it limited the parents’ role in addressing their child’s health concern. In addition, only half of parents surveyed fully knew and understood the confidentiality policy at their daughter’s clinic.
Only half the parents in the study understood that they would only be informed of the details of the interview if their child assented, or if their child was at serious risk. A third thought they would be informed of what their child revealed, regardless of what the teen wanted. Nearly 20% said they were unsure of the clinic’s policy on confidentiality.
The findings led Dr. Trotman and her colleagues to conclude that gynecologic specialists could do more to educate patients and their families about the confidential interview and improve the efficacy of its delivery.
Meanwhile, despite a third of parents stating that the most appropriate age for confidential interviews to begin was age 17 years, the study also found that the adolescents were engaging in an array of risky behaviors, including but not limited to those to do with sex, as early as age 11 years.
There was parity between what the parents perceived were their daughters’ sexual activity and the percentage of teens who reported being sexually active (12% vs. 15%); however, Dr. Trotman said that while "parents are definitely speaking to their teens more about sex and about drinking alcohol," they were essentially unaware of the extent to which their children were reportedly bullied and/or engaging in self-harm, eating disorders, and other deleterious behaviors.
"At all ages, there was a significant difference between the parents’ perception of their own teen’s [behavior] and what behavior the adolescents [reported]," said Dr. Trotman (P less than or equal to .0001).
"This is the message we try to get across: that the confidential interview is for more than talking about sexual behaviors," said Dr. Trotman.
Dr. Trotman reported no relevant disclosures.
On Twitter @whitneymcknight
PHILADELPHIA – Despite an overall agreement on its merit, both parents and their adolescent daughters are leery of the confidential interview in the gynecologic setting, in part because each cohort believes that it is tantamount to parents being excluded in the teen’s health care decision-making process.
"The majority of parents felt that this was inappropriate for their teen because this was a specialized setting," Dr. Gylynthia E. Trotman, a second-year fellow at Medstar Washington Hospital Center, Children’s National Medical Center, said in an interview.
"The adolescent felt that way, too, which came as a shock to us," Dr. Trotman said during the poster session at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology. "They wanted parents to be a part of their decision making."
The data, derived from a survey of 62 pairs of parents and 62 of their collective adolescent daughters between the ages of 11 and 17 years, showed that while 85% of teens and 78% of parents thought the confidential interview was beneficial, 31% and 40% respectively thought it limited the parents’ role in addressing their child’s health concern. In addition, only half of parents surveyed fully knew and understood the confidentiality policy at their daughter’s clinic.
Only half the parents in the study understood that they would only be informed of the details of the interview if their child assented, or if their child was at serious risk. A third thought they would be informed of what their child revealed, regardless of what the teen wanted. Nearly 20% said they were unsure of the clinic’s policy on confidentiality.
The findings led Dr. Trotman and her colleagues to conclude that gynecologic specialists could do more to educate patients and their families about the confidential interview and improve the efficacy of its delivery.
Meanwhile, despite a third of parents stating that the most appropriate age for confidential interviews to begin was age 17 years, the study also found that the adolescents were engaging in an array of risky behaviors, including but not limited to those to do with sex, as early as age 11 years.
There was parity between what the parents perceived were their daughters’ sexual activity and the percentage of teens who reported being sexually active (12% vs. 15%); however, Dr. Trotman said that while "parents are definitely speaking to their teens more about sex and about drinking alcohol," they were essentially unaware of the extent to which their children were reportedly bullied and/or engaging in self-harm, eating disorders, and other deleterious behaviors.
"At all ages, there was a significant difference between the parents’ perception of their own teen’s [behavior] and what behavior the adolescents [reported]," said Dr. Trotman (P less than or equal to .0001).
"This is the message we try to get across: that the confidential interview is for more than talking about sexual behaviors," said Dr. Trotman.
Dr. Trotman reported no relevant disclosures.
On Twitter @whitneymcknight
PHILADELPHIA – Despite an overall agreement on its merit, both parents and their adolescent daughters are leery of the confidential interview in the gynecologic setting, in part because each cohort believes that it is tantamount to parents being excluded in the teen’s health care decision-making process.
"The majority of parents felt that this was inappropriate for their teen because this was a specialized setting," Dr. Gylynthia E. Trotman, a second-year fellow at Medstar Washington Hospital Center, Children’s National Medical Center, said in an interview.
"The adolescent felt that way, too, which came as a shock to us," Dr. Trotman said during the poster session at the annual meeting of the North American Society for Pediatric and Adolescent Gynecology. "They wanted parents to be a part of their decision making."
The data, derived from a survey of 62 pairs of parents and 62 of their collective adolescent daughters between the ages of 11 and 17 years, showed that while 85% of teens and 78% of parents thought the confidential interview was beneficial, 31% and 40% respectively thought it limited the parents’ role in addressing their child’s health concern. In addition, only half of parents surveyed fully knew and understood the confidentiality policy at their daughter’s clinic.
Only half the parents in the study understood that they would only be informed of the details of the interview if their child assented, or if their child was at serious risk. A third thought they would be informed of what their child revealed, regardless of what the teen wanted. Nearly 20% said they were unsure of the clinic’s policy on confidentiality.
The findings led Dr. Trotman and her colleagues to conclude that gynecologic specialists could do more to educate patients and their families about the confidential interview and improve the efficacy of its delivery.
Meanwhile, despite a third of parents stating that the most appropriate age for confidential interviews to begin was age 17 years, the study also found that the adolescents were engaging in an array of risky behaviors, including but not limited to those to do with sex, as early as age 11 years.
There was parity between what the parents perceived were their daughters’ sexual activity and the percentage of teens who reported being sexually active (12% vs. 15%); however, Dr. Trotman said that while "parents are definitely speaking to their teens more about sex and about drinking alcohol," they were essentially unaware of the extent to which their children were reportedly bullied and/or engaging in self-harm, eating disorders, and other deleterious behaviors.
"At all ages, there was a significant difference between the parents’ perception of their own teen’s [behavior] and what behavior the adolescents [reported]," said Dr. Trotman (P less than or equal to .0001).
"This is the message we try to get across: that the confidential interview is for more than talking about sexual behaviors," said Dr. Trotman.
Dr. Trotman reported no relevant disclosures.
On Twitter @whitneymcknight
AT THE NASPAG ANNUAL MEETING
Major finding: Half the parents of adolescent girls knew and understood confidential gynecologic interview policy.
Data source: Survey of 62 pairs of parents with adolescent girls who underwent specialty gynecologic treatment at a single site.
Disclosures: Dr. Trotman reported no relevant disclosures.
AUDIO: CBT better for comorbid depression, anxiety in migraine
PHILADELPHIA – Which comes first, the migraine or the anxiety and depression? At the annual meeting of the American Academy of Neurology, Dr. Deborah Friedman, professor of neurology at the University of Texas Southwestern Medical Center, Dallas, suggests that patients can use cognitive-behavioral therapy rather than medication to best address the migraine-related anxiety and depression, possibly improving their ability to cope with their migraine by allowing them better insight into its impact.
On Twitter @whitneymcknight
PHILADELPHIA – Which comes first, the migraine or the anxiety and depression? At the annual meeting of the American Academy of Neurology, Dr. Deborah Friedman, professor of neurology at the University of Texas Southwestern Medical Center, Dallas, suggests that patients can use cognitive-behavioral therapy rather than medication to best address the migraine-related anxiety and depression, possibly improving their ability to cope with their migraine by allowing them better insight into its impact.
On Twitter @whitneymcknight
PHILADELPHIA – Which comes first, the migraine or the anxiety and depression? At the annual meeting of the American Academy of Neurology, Dr. Deborah Friedman, professor of neurology at the University of Texas Southwestern Medical Center, Dallas, suggests that patients can use cognitive-behavioral therapy rather than medication to best address the migraine-related anxiety and depression, possibly improving their ability to cope with their migraine by allowing them better insight into its impact.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE AAN 2014 ANNUAL MEETING
Emergency thrombolysis by presumed consent preferred in majority of older adults
PHILADELPHIA – Presumed consent for emergency thrombolysis is ethical and practical, according to the results of a population-based survey.
In an online survey of 1,100 adults aged 50 years or older, 76.9% said they would want intravenous tissue plasminogen activator for stroke. Of those surveyed, 76.0% also said they would want cardiopulmonary resuscitation for cardiac arrest. If they were unable to give informed consent in either situation, the desire for emergency thrombolysis remained essentially unchanged at 78.1%, while even more (83.6%) respondents said they would want CPR, Dr. Winston Chiong reported at the annual meeting of the American Academy of Neurology. The findings also appear in the April 23 issue of JAMA (2014;311:1689-91).
"The presumption is that ‘reasonable people’ in the middle of [an acute ischemic stroke] cascade would want thrombolytic treatment," Dr. Chiong told the platform science session blitz audience. "But this presumption has been controversial because thrombolysis has no short-term mortality benefit, unlike CPR."
In 2011, the AAN endorsed emergency thrombolysis under presumption of consent; in 2013, the American Heart Association and the American Stroke Association followed suit.
Dr. Chiong, whose interest lies in decision making and how it is affected by aging and neurodegenerative disease, said the findings provide empirical data that this presumption is justified.
He and his colleagues at the University of California, San Francisco, Memory and Aging Center randomly assigned survey participants to read one of two hypothetical scenarios. In the first, they saw themselves being brought to a hospital after having a severe acute ischemic stroke. In the second, they saw themselves have an out-of-hospital cardiac arrest that was treated by paramedics.
The stroke group was given a graphical depiction of the potential risks and benefits of treatment with thrombolysis, while the cardiac arrest group was told of the potential outcomes after paramedic-initiated CPR.
Each group was then asked whether they would want the respective treatment for their imagined scenario.
In the stroke group, 419 of 545 participants (76.9%) wanted thrombolysis, while 422 of 555 respondents (76.0%) wanted CPR for sudden cardiac arrest. Female sex, being divorced, and having less education were associated with refusing thrombolysis; poorer physical health, previous stroke, and possession of a health care advance directive was associated with refusal of CPR.
"In a clinical scenario involving an incapacitated patient where the treatment preferences are unknown and no surrogate decision maker can be found within the treatment window, we found equally strong ethical grounds for presuming thrombolysis of stroke as for presumed consent of CPR in cardiac arrest," Dr. Chiong said.
However, he underscored that despite there being a "pragmatic ethical and legal" basis for presumed consent, it is important to remember there are still a quarter of older adults who would not want the treatment if unable to consent.
"I spend a lot of time thinking about these things," he said, "The presumption of consent should not be taken to fully replace informed consent," particularly if there is some existing evidence of the patient’s wishes or if there is some question about the effectiveness of the intervention.
This study was supported in part by the American Brain Foundation Clinical Research Training Fellowship Program and grants from the National Science Foundation, the National Institute on Aging, and the National Center for Advancing Translational Sciences.
On Twitter @whitneymcknight
PHILADELPHIA – Presumed consent for emergency thrombolysis is ethical and practical, according to the results of a population-based survey.
In an online survey of 1,100 adults aged 50 years or older, 76.9% said they would want intravenous tissue plasminogen activator for stroke. Of those surveyed, 76.0% also said they would want cardiopulmonary resuscitation for cardiac arrest. If they were unable to give informed consent in either situation, the desire for emergency thrombolysis remained essentially unchanged at 78.1%, while even more (83.6%) respondents said they would want CPR, Dr. Winston Chiong reported at the annual meeting of the American Academy of Neurology. The findings also appear in the April 23 issue of JAMA (2014;311:1689-91).
"The presumption is that ‘reasonable people’ in the middle of [an acute ischemic stroke] cascade would want thrombolytic treatment," Dr. Chiong told the platform science session blitz audience. "But this presumption has been controversial because thrombolysis has no short-term mortality benefit, unlike CPR."
In 2011, the AAN endorsed emergency thrombolysis under presumption of consent; in 2013, the American Heart Association and the American Stroke Association followed suit.
Dr. Chiong, whose interest lies in decision making and how it is affected by aging and neurodegenerative disease, said the findings provide empirical data that this presumption is justified.
He and his colleagues at the University of California, San Francisco, Memory and Aging Center randomly assigned survey participants to read one of two hypothetical scenarios. In the first, they saw themselves being brought to a hospital after having a severe acute ischemic stroke. In the second, they saw themselves have an out-of-hospital cardiac arrest that was treated by paramedics.
The stroke group was given a graphical depiction of the potential risks and benefits of treatment with thrombolysis, while the cardiac arrest group was told of the potential outcomes after paramedic-initiated CPR.
Each group was then asked whether they would want the respective treatment for their imagined scenario.
In the stroke group, 419 of 545 participants (76.9%) wanted thrombolysis, while 422 of 555 respondents (76.0%) wanted CPR for sudden cardiac arrest. Female sex, being divorced, and having less education were associated with refusing thrombolysis; poorer physical health, previous stroke, and possession of a health care advance directive was associated with refusal of CPR.
"In a clinical scenario involving an incapacitated patient where the treatment preferences are unknown and no surrogate decision maker can be found within the treatment window, we found equally strong ethical grounds for presuming thrombolysis of stroke as for presumed consent of CPR in cardiac arrest," Dr. Chiong said.
However, he underscored that despite there being a "pragmatic ethical and legal" basis for presumed consent, it is important to remember there are still a quarter of older adults who would not want the treatment if unable to consent.
"I spend a lot of time thinking about these things," he said, "The presumption of consent should not be taken to fully replace informed consent," particularly if there is some existing evidence of the patient’s wishes or if there is some question about the effectiveness of the intervention.
This study was supported in part by the American Brain Foundation Clinical Research Training Fellowship Program and grants from the National Science Foundation, the National Institute on Aging, and the National Center for Advancing Translational Sciences.
On Twitter @whitneymcknight
PHILADELPHIA – Presumed consent for emergency thrombolysis is ethical and practical, according to the results of a population-based survey.
In an online survey of 1,100 adults aged 50 years or older, 76.9% said they would want intravenous tissue plasminogen activator for stroke. Of those surveyed, 76.0% also said they would want cardiopulmonary resuscitation for cardiac arrest. If they were unable to give informed consent in either situation, the desire for emergency thrombolysis remained essentially unchanged at 78.1%, while even more (83.6%) respondents said they would want CPR, Dr. Winston Chiong reported at the annual meeting of the American Academy of Neurology. The findings also appear in the April 23 issue of JAMA (2014;311:1689-91).
"The presumption is that ‘reasonable people’ in the middle of [an acute ischemic stroke] cascade would want thrombolytic treatment," Dr. Chiong told the platform science session blitz audience. "But this presumption has been controversial because thrombolysis has no short-term mortality benefit, unlike CPR."
In 2011, the AAN endorsed emergency thrombolysis under presumption of consent; in 2013, the American Heart Association and the American Stroke Association followed suit.
Dr. Chiong, whose interest lies in decision making and how it is affected by aging and neurodegenerative disease, said the findings provide empirical data that this presumption is justified.
He and his colleagues at the University of California, San Francisco, Memory and Aging Center randomly assigned survey participants to read one of two hypothetical scenarios. In the first, they saw themselves being brought to a hospital after having a severe acute ischemic stroke. In the second, they saw themselves have an out-of-hospital cardiac arrest that was treated by paramedics.
The stroke group was given a graphical depiction of the potential risks and benefits of treatment with thrombolysis, while the cardiac arrest group was told of the potential outcomes after paramedic-initiated CPR.
Each group was then asked whether they would want the respective treatment for their imagined scenario.
In the stroke group, 419 of 545 participants (76.9%) wanted thrombolysis, while 422 of 555 respondents (76.0%) wanted CPR for sudden cardiac arrest. Female sex, being divorced, and having less education were associated with refusing thrombolysis; poorer physical health, previous stroke, and possession of a health care advance directive was associated with refusal of CPR.
"In a clinical scenario involving an incapacitated patient where the treatment preferences are unknown and no surrogate decision maker can be found within the treatment window, we found equally strong ethical grounds for presuming thrombolysis of stroke as for presumed consent of CPR in cardiac arrest," Dr. Chiong said.
However, he underscored that despite there being a "pragmatic ethical and legal" basis for presumed consent, it is important to remember there are still a quarter of older adults who would not want the treatment if unable to consent.
"I spend a lot of time thinking about these things," he said, "The presumption of consent should not be taken to fully replace informed consent," particularly if there is some existing evidence of the patient’s wishes or if there is some question about the effectiveness of the intervention.
This study was supported in part by the American Brain Foundation Clinical Research Training Fellowship Program and grants from the National Science Foundation, the National Institute on Aging, and the National Center for Advancing Translational Sciences.
On Twitter @whitneymcknight
AT THE AAN 2014 ANNUAL MEETING
Key clinical point: Presumption of consent during a stroke is a "pragmatic ethical and legal" convention.
Major finding: 78.1% of older adults would want emergency thrombolysis for stroke without informed consent.
Data source: A population-based survey of 1,100 adults aged 50 years or older.
Disclosures: This study was supported in part by the American Brain Foundation Clinical Research Training Fellowship Program and grants from the National Science Foundation, the National Institute on Aging, and the National Center for Advancing Translational Sciences.
VIDEO: New meds, remyelination therapies move ahead in multiple sclerosis
PHILADELPHIA – From biomarkers for better diagnosis to new biologic agents for more effective treatment, multiple sclerosis patients may soon enjoy a wave of promising advances.
In an interview at the annual meeting of the American Academy of Neurology, Dr. Emmanuelle Waubant, professor of neurology at the University of California, San Francisco, talked about progress being made with remyelination therapies and discussed three investigational drugs that could reach the market soon.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – From biomarkers for better diagnosis to new biologic agents for more effective treatment, multiple sclerosis patients may soon enjoy a wave of promising advances.
In an interview at the annual meeting of the American Academy of Neurology, Dr. Emmanuelle Waubant, professor of neurology at the University of California, San Francisco, talked about progress being made with remyelination therapies and discussed three investigational drugs that could reach the market soon.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
PHILADELPHIA – From biomarkers for better diagnosis to new biologic agents for more effective treatment, multiple sclerosis patients may soon enjoy a wave of promising advances.
In an interview at the annual meeting of the American Academy of Neurology, Dr. Emmanuelle Waubant, professor of neurology at the University of California, San Francisco, talked about progress being made with remyelination therapies and discussed three investigational drugs that could reach the market soon.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM THE AAN 2014 ANNUAL MEETING
Rasagiline’s failure as active control halts phase III preladenant trial
PHILADELPHIA – Results of the phase III clinical trial to evaluate preladenant as monotherapy for Parkinson’s disease are difficult to interpret because the lack of observed efficacy of rasagiline as an active control indicates that the study didn’t work.
"There was not a significantly greater benefit in any of the arms, compared with placebo, including all the preladenant arms, and the rasagiline arm, our active-control medication with known efficacy," Dr. Robert A. Hauser revealed to a giggling crowd, some of whom applauded, at the annual meeting of the American Academy of Neurology.
"Interestingly enough, placebo was statistically superior to the lowest dose of preladenant," said Dr. Hauser, director of the Parkinson’s Disease and Movement Disorder Center at the University of South Florida, Tampa.
The randomized, double-blind, placebo- and active-controlled, parallel-group trial was designed to cover two 26-week time periods for a total of 52 weeks, and it was conducted at multiple centers in multiple countries. More than half (58%) of the 1,022 participants were men. The average age was 63 years, and the mean baseline score on the Unified Parkinson’s Disease Rating Scale (UPDRS) parts 2 and 3 was 28.5. The study participants had been diagnosed with Parkinson’s disease within the previous 5 years, and had not yet received any levodopa or dopamine agonists.
The efficacy parameter was based on a change from baseline (CFB) in patient UPDRS scores. There was a dose-ordered response, although the patients in the preladenant 2 mg twice daily arm actually worsened, showing a significant CFB of 0.30 and a 2.60 difference when compared with placebo (P = .0033; 95% confidence interval, 0.86-4.30).
The preladenant 5 mg twice-daily group improved, showing a –1.00 CFB and a 1.30 difference from placebo (P = .1382; 95% CI, –0.41-2.94). The preladenant 10 mg twice-daily arm also improved, showing a CFB of –1.80 with a difference of 0.40 from placebo (P = .6378; 95% CI, –1.29-2.11).
Patients in the 1 mg once-daily rasagiline group improved, but not significantly, with a CFB of -1.90 when compared with placebo (P = .6923; 95% CI, –1.35-2.03), however, the placebo arm had the best results overall with a CFB of –2.20.
"I should point out that rasagiline was our active comparator, and it was included to make sure that the trial worked," said Dr. Hauser. "The fact that [the rasagiline group] did not separate from placebo indicates that this was a failed trial."
Rasagiline is a monoamine oxidase type-B inhibitor, with Food and Drug Administration approval as both monotherapy in early Parkinson’s disease an as an adjunctive treatment in moderate to advanced Parkinson’s disease.
A post hoc analyses revealed that, across the sites, the strongest rasagiline response vs. placebo (when looking at the CFB on the UPDRS parts 2 and 3) occurred in the European Union (–2.4) and North America (–1.5). In Eastern Europe, placebo performed 4 points better than did rasagiline. In Latin America, the rasagiline and placebo arms showed parity. Dr. Hauser speculated that regional differences might reflect experience and expertise of sites in those regions that participated in the trial.
Preladenant previously had been found effective as an adjunct to levodopa when dosed at either 5 mg or 10 mg twice per day.
While it is not possible to draw definitive conclusions about preladenant’s efficacy as a monotherapy for Parkinson’s disease based on this trial, Dr. Hauser stated, "One of things I think this trial demonstrates is the value of having an active-control medication known to have efficacy in a situation when you are testing a new medication."
Dr. Hauser disclosed that he and his associates had many industry relationships, including his own with Abbott Laboratories, Allergan, AstraZeneca, Biotie Therapies, Ceregene, Chelsea Therapeutics, and GE Healthcare. This trial was underwritten by Merck.
On Twitter @whitneymcknight
PHILADELPHIA – Results of the phase III clinical trial to evaluate preladenant as monotherapy for Parkinson’s disease are difficult to interpret because the lack of observed efficacy of rasagiline as an active control indicates that the study didn’t work.
"There was not a significantly greater benefit in any of the arms, compared with placebo, including all the preladenant arms, and the rasagiline arm, our active-control medication with known efficacy," Dr. Robert A. Hauser revealed to a giggling crowd, some of whom applauded, at the annual meeting of the American Academy of Neurology.
"Interestingly enough, placebo was statistically superior to the lowest dose of preladenant," said Dr. Hauser, director of the Parkinson’s Disease and Movement Disorder Center at the University of South Florida, Tampa.
The randomized, double-blind, placebo- and active-controlled, parallel-group trial was designed to cover two 26-week time periods for a total of 52 weeks, and it was conducted at multiple centers in multiple countries. More than half (58%) of the 1,022 participants were men. The average age was 63 years, and the mean baseline score on the Unified Parkinson’s Disease Rating Scale (UPDRS) parts 2 and 3 was 28.5. The study participants had been diagnosed with Parkinson’s disease within the previous 5 years, and had not yet received any levodopa or dopamine agonists.
The efficacy parameter was based on a change from baseline (CFB) in patient UPDRS scores. There was a dose-ordered response, although the patients in the preladenant 2 mg twice daily arm actually worsened, showing a significant CFB of 0.30 and a 2.60 difference when compared with placebo (P = .0033; 95% confidence interval, 0.86-4.30).
The preladenant 5 mg twice-daily group improved, showing a –1.00 CFB and a 1.30 difference from placebo (P = .1382; 95% CI, –0.41-2.94). The preladenant 10 mg twice-daily arm also improved, showing a CFB of –1.80 with a difference of 0.40 from placebo (P = .6378; 95% CI, –1.29-2.11).
Patients in the 1 mg once-daily rasagiline group improved, but not significantly, with a CFB of -1.90 when compared with placebo (P = .6923; 95% CI, –1.35-2.03), however, the placebo arm had the best results overall with a CFB of –2.20.
"I should point out that rasagiline was our active comparator, and it was included to make sure that the trial worked," said Dr. Hauser. "The fact that [the rasagiline group] did not separate from placebo indicates that this was a failed trial."
Rasagiline is a monoamine oxidase type-B inhibitor, with Food and Drug Administration approval as both monotherapy in early Parkinson’s disease an as an adjunctive treatment in moderate to advanced Parkinson’s disease.
A post hoc analyses revealed that, across the sites, the strongest rasagiline response vs. placebo (when looking at the CFB on the UPDRS parts 2 and 3) occurred in the European Union (–2.4) and North America (–1.5). In Eastern Europe, placebo performed 4 points better than did rasagiline. In Latin America, the rasagiline and placebo arms showed parity. Dr. Hauser speculated that regional differences might reflect experience and expertise of sites in those regions that participated in the trial.
Preladenant previously had been found effective as an adjunct to levodopa when dosed at either 5 mg or 10 mg twice per day.
While it is not possible to draw definitive conclusions about preladenant’s efficacy as a monotherapy for Parkinson’s disease based on this trial, Dr. Hauser stated, "One of things I think this trial demonstrates is the value of having an active-control medication known to have efficacy in a situation when you are testing a new medication."
Dr. Hauser disclosed that he and his associates had many industry relationships, including his own with Abbott Laboratories, Allergan, AstraZeneca, Biotie Therapies, Ceregene, Chelsea Therapeutics, and GE Healthcare. This trial was underwritten by Merck.
On Twitter @whitneymcknight
PHILADELPHIA – Results of the phase III clinical trial to evaluate preladenant as monotherapy for Parkinson’s disease are difficult to interpret because the lack of observed efficacy of rasagiline as an active control indicates that the study didn’t work.
"There was not a significantly greater benefit in any of the arms, compared with placebo, including all the preladenant arms, and the rasagiline arm, our active-control medication with known efficacy," Dr. Robert A. Hauser revealed to a giggling crowd, some of whom applauded, at the annual meeting of the American Academy of Neurology.
"Interestingly enough, placebo was statistically superior to the lowest dose of preladenant," said Dr. Hauser, director of the Parkinson’s Disease and Movement Disorder Center at the University of South Florida, Tampa.
The randomized, double-blind, placebo- and active-controlled, parallel-group trial was designed to cover two 26-week time periods for a total of 52 weeks, and it was conducted at multiple centers in multiple countries. More than half (58%) of the 1,022 participants were men. The average age was 63 years, and the mean baseline score on the Unified Parkinson’s Disease Rating Scale (UPDRS) parts 2 and 3 was 28.5. The study participants had been diagnosed with Parkinson’s disease within the previous 5 years, and had not yet received any levodopa or dopamine agonists.
The efficacy parameter was based on a change from baseline (CFB) in patient UPDRS scores. There was a dose-ordered response, although the patients in the preladenant 2 mg twice daily arm actually worsened, showing a significant CFB of 0.30 and a 2.60 difference when compared with placebo (P = .0033; 95% confidence interval, 0.86-4.30).
The preladenant 5 mg twice-daily group improved, showing a –1.00 CFB and a 1.30 difference from placebo (P = .1382; 95% CI, –0.41-2.94). The preladenant 10 mg twice-daily arm also improved, showing a CFB of –1.80 with a difference of 0.40 from placebo (P = .6378; 95% CI, –1.29-2.11).
Patients in the 1 mg once-daily rasagiline group improved, but not significantly, with a CFB of -1.90 when compared with placebo (P = .6923; 95% CI, –1.35-2.03), however, the placebo arm had the best results overall with a CFB of –2.20.
"I should point out that rasagiline was our active comparator, and it was included to make sure that the trial worked," said Dr. Hauser. "The fact that [the rasagiline group] did not separate from placebo indicates that this was a failed trial."
Rasagiline is a monoamine oxidase type-B inhibitor, with Food and Drug Administration approval as both monotherapy in early Parkinson’s disease an as an adjunctive treatment in moderate to advanced Parkinson’s disease.
A post hoc analyses revealed that, across the sites, the strongest rasagiline response vs. placebo (when looking at the CFB on the UPDRS parts 2 and 3) occurred in the European Union (–2.4) and North America (–1.5). In Eastern Europe, placebo performed 4 points better than did rasagiline. In Latin America, the rasagiline and placebo arms showed parity. Dr. Hauser speculated that regional differences might reflect experience and expertise of sites in those regions that participated in the trial.
Preladenant previously had been found effective as an adjunct to levodopa when dosed at either 5 mg or 10 mg twice per day.
While it is not possible to draw definitive conclusions about preladenant’s efficacy as a monotherapy for Parkinson’s disease based on this trial, Dr. Hauser stated, "One of things I think this trial demonstrates is the value of having an active-control medication known to have efficacy in a situation when you are testing a new medication."
Dr. Hauser disclosed that he and his associates had many industry relationships, including his own with Abbott Laboratories, Allergan, AstraZeneca, Biotie Therapies, Ceregene, Chelsea Therapeutics, and GE Healthcare. This trial was underwritten by Merck.
On Twitter @whitneymcknight
AT THE AAN 2014 ANNUAL MEETING
Key clinical point: An active-control medication with known efficacy is a valuable tool when testing a new medication.
Major finding: Neither preladenant nor rasagiline bested placebo for Parkinson’s disease monotherapy by week 26 of a 1-year, phase III clinical trial.
Data source: Multicenter, double-blind randomized study of 1,022 persons diagnosed with Parkinson’s disease within 5 years, who were not receiving levodopa or dopamine agonists.
Disclosures: Dr. Hauser disclosed that he and his associates had many industry relationships, including his own with Abbott Laboratories, Allergan, AstraZeneca, Biotie Therapies, Ceregene, Chelsea Therapeutics, and GE Healthcare. This trial was underwritten by Merck.