User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
What happened to melanoma care during COVID-19 sequestration
Initial evidence suggests that the , Rebecca I. Hartman, MD, MPH, said at a virtual forum on cutaneous malignancies jointly presented by Postgraduate Institute for Medicine and Global Academy for Medication Education.
This is not what National Comprehensive Cancer Network officials expected when they issued short-term recommendations on how to manage cutaneous melanoma during the first wave of the COVID-19 pandemic. Those recommendations for restriction of care, which Dr. Hartman characterized as “pretty significant changes from how we typically practice melanoma care in the U.S.,” came at a time when there was justifiable concern that the first COVID-19 surge would strain the U.S. health care system beyond the breaking point.
The rationale given for the NCCN recommendations was that most time-to-treat studies have shown no adverse patient outcomes for 90-day delays in treatment, even for thicker melanomas. But those studies, all retrospective, have been called into question. And the first real-world data on the impact of care restrictions during the lockdown, reported by Italian dermatologists, highlights adverse effects with potentially far-reaching consequences, noted Dr. Hartman, director of melanoma epidemiology at Brigham and Women’s Hospital and a dermatologist, Harvard University, Boston.
Analysis of the impact of lockdown-induced delays in melanoma care is not merely an academic exercise, she added. While everyone hopes that the spring 2020 COVID-19 shelter-in-place was a once-in-a-lifetime event, there’s no guarantee that will be the case. Moreover, the lockdown provides a natural experiment addressing the possible consequences of melanoma care delays on patient outcomes, a topic that for ethical reasons could never be addressed in a randomized trial.
The short-term NCCN recommendations included the use of excisional biopsies for melanoma diagnosis whenever possible; and delay of up to 3 months for wide local excision of in situ melanoma, any invasive melanoma with negative margins, and even T1 melanomas with positive margins provided the bulk of the lesion had been excised. The guidance also suggested delaying sentinel lymph node biopsy (SLNB), along with increased use of neoadjuvant therapy in patients with clinically palpable regional lymph nodes in order to delay surgery for up to 8 weeks. Single-agent systemic therapy at the least-frequent dosing was advised in order to minimize toxicity and reduce the need for additional health care resources: for example, nivolumab (Opdivo) at 480 mg every 4 weeks instead of every 2 weeks, and pembrolizumab (Keytruda) at 400 mg every 6 weeks, rather than every 3 weeks.
So, that’s what the NCCN recommended. Here’s what actually happened during shelter-in-place as captured in Dr. Hartman’s survey of 18 U.S. members of the Melanoma Prevention Working Group, all practicing dermatology in centers particularly hard-hit in the first wave of the pandemic: In-person new melanoma patient visits plunged from an average of 4.83 per week per provider to 0.83 per week. Telemedicine visits with new melanoma patients went from zero prepandemic to 0.67 visits per week per provider, which doesn’t come close to making up for the drop in in-person visits. Interestingly, two respondents reported turning to gene-expression profile testing for patient prognostication because of delays in SLNB.
Wide local excision was delayed by an average of 6 weeks in roughly one-third of melanoma patients with early tumor stage disease, regardless of margin status. For patients with stage T1b disease, wide local excision was typically performed on time during shelter-in-place; however, SLNB was delayed by an average of 5 weeks in 22% of patients with positive margins and 28% of those with negative margins. In contrast, 80% of patients with more advanced T2-T4 melanoma underwent on-schedule definitive management with wide local excision and SLNB, Dr. Hartman reported.
Critics have taken issue with the NCCN’s conclusion that most time-to-treatment studies show no harm arising from 90-day treatment delays. A review of the relevant published literature by Dr. Hartman’s Harvard colleagues, published in July, found that the evidence is mixed. “There is insufficient evidence to definitively conclude that delayed wide resection after gross removal of the primary melanoma is without harm,” they concluded in the review.
Spanish dermatologists performed a modeling study in order to estimate the potential impact of COVID-19 lockdowns on 5- and 10-year survival of melanoma patients. Using the growth rate of a random sample of 1,000 melanomas to model estimates of tumor thickness after various delays, coupled with American Joint Committee on Cancer survival data for different T stages, they estimated that 5-year survival would be reduced from 94.2% to 92.3% with a 90-day delay in diagnosis, and that 10-year survival would drop from 90.0% to 87.6%.
But that’s merely modeling. Francesco Ricci, MD, PhD, and colleagues from the melanoma unit at the Istituto Dermopatico dell’Immacolata, Rome, have provided a first look at the real-world impact of the lockdown. In the prelockdown period of January through March 9th, 2020, the referral center averaged 2.3 new melanoma diagnoses per day. During the Rome lockdown, from March 10th through May 3rd, this figure dropped to a mean of 0.6 melanoma diagnoses per day. Postlockdown, from May 4th to June 6th, the average climbed to 1.3 per day. The rate of newly diagnosed nodular melanoma was 5.5-fold greater postlockdown, compared with prelockdown; the rate of ulcerated melanoma was 4.9-fold greater.
“We can hypothesize that this may have been due to delays in diagnosis and care,” Dr. Hartman commented. “This is important because we know that nodular melanoma as well as ulceration tend to have a worse prognosis in terms of mortality.”
The mean Breslow thickness of newly diagnosed melanomas was 0.88 mm prelockdown, 0.66 mm during lockdown, and 1.96 mm postlockdown. The investigators speculated that the reduced Breslow thickness of melanomas diagnosed during lockdown might be explained by a greater willingness of more health-conscious people to defy the shelter-in-place instructions because of their concern about a suspicious skin lesion. “Though it is way too early to gauge the consequences of such diagnostic delay, should this issue be neglected, dermatologists and their patients may pay a higher price later with increased morbidity, mortality, and financial burden,” according to the investigators.
Dr. Hartman observed that it will be important to learn whether similar experiences occurred elsewhere during lockdown.
Another speaker, John M. Kirkwood, MD, said he has seen several melanoma patients referred from outside centers who had delays of up to 3 months in sentinel lymph node management of T2 and T3 tumors during lockdown who now have widespread metastatic disease.
“Now, is that anecdotal? I don’t know, it’s just worrisome to me,” commented Dr. Kirkwood, professor of medicine, dermatology, and translational science at the University of Pittsburgh.
Merrick Ross, MD, professor of surgical oncology at M.D. Anderson Cancer Center, Houston, recalled, “There was a period of time [during the lockdown] when we weren’t allowed to do certain elective procedures, if you want to call cancer surgery elective.”
“It’s too soon to talk about outcomes because a lot of patients are still in the process of being treated after what I would consider a significant delay in diagnosis,” the surgeon added.
An audience member asked if there will be an opportunity to see data on the damage done by delaying melanoma management as compared to lives saved through the lockdown for COVID-19. Dr. Ross replied that M.D. Anderson is in the midst of an institution-wide study analyzing the delay in diagnosis of a range of cancers.
“In our melanoma center it is absolutely clear, although we’re still collecting data, that the median tumor thickness is much higher since the lockdown,” Dr. Ross commented.
Dr. Hartman said she and her coinvestigators in the Melanoma Prevention Working Group are attempting to tally up the damage done via the lockdown by delaying melanoma diagnosis and treatment. But she agreed with the questioner that the most important thing is overall net lives saved through shelter-in-place.
“I’m sure that, separately, nondermatologists – perhaps infectious disease doctors and internists – are looking at how many lives were saved by the lockdown policy. So I do think all that data will come out,” Dr. Hartman predicted.
She reported having no financial conflicts regarding her presentation.
Global Academy for Medical Education and this news organization are owned by the same company.
SOURCE: Hartman, R. Cutaneous malignancies forum.
Initial evidence suggests that the , Rebecca I. Hartman, MD, MPH, said at a virtual forum on cutaneous malignancies jointly presented by Postgraduate Institute for Medicine and Global Academy for Medication Education.
This is not what National Comprehensive Cancer Network officials expected when they issued short-term recommendations on how to manage cutaneous melanoma during the first wave of the COVID-19 pandemic. Those recommendations for restriction of care, which Dr. Hartman characterized as “pretty significant changes from how we typically practice melanoma care in the U.S.,” came at a time when there was justifiable concern that the first COVID-19 surge would strain the U.S. health care system beyond the breaking point.
The rationale given for the NCCN recommendations was that most time-to-treat studies have shown no adverse patient outcomes for 90-day delays in treatment, even for thicker melanomas. But those studies, all retrospective, have been called into question. And the first real-world data on the impact of care restrictions during the lockdown, reported by Italian dermatologists, highlights adverse effects with potentially far-reaching consequences, noted Dr. Hartman, director of melanoma epidemiology at Brigham and Women’s Hospital and a dermatologist, Harvard University, Boston.
Analysis of the impact of lockdown-induced delays in melanoma care is not merely an academic exercise, she added. While everyone hopes that the spring 2020 COVID-19 shelter-in-place was a once-in-a-lifetime event, there’s no guarantee that will be the case. Moreover, the lockdown provides a natural experiment addressing the possible consequences of melanoma care delays on patient outcomes, a topic that for ethical reasons could never be addressed in a randomized trial.
The short-term NCCN recommendations included the use of excisional biopsies for melanoma diagnosis whenever possible; and delay of up to 3 months for wide local excision of in situ melanoma, any invasive melanoma with negative margins, and even T1 melanomas with positive margins provided the bulk of the lesion had been excised. The guidance also suggested delaying sentinel lymph node biopsy (SLNB), along with increased use of neoadjuvant therapy in patients with clinically palpable regional lymph nodes in order to delay surgery for up to 8 weeks. Single-agent systemic therapy at the least-frequent dosing was advised in order to minimize toxicity and reduce the need for additional health care resources: for example, nivolumab (Opdivo) at 480 mg every 4 weeks instead of every 2 weeks, and pembrolizumab (Keytruda) at 400 mg every 6 weeks, rather than every 3 weeks.
So, that’s what the NCCN recommended. Here’s what actually happened during shelter-in-place as captured in Dr. Hartman’s survey of 18 U.S. members of the Melanoma Prevention Working Group, all practicing dermatology in centers particularly hard-hit in the first wave of the pandemic: In-person new melanoma patient visits plunged from an average of 4.83 per week per provider to 0.83 per week. Telemedicine visits with new melanoma patients went from zero prepandemic to 0.67 visits per week per provider, which doesn’t come close to making up for the drop in in-person visits. Interestingly, two respondents reported turning to gene-expression profile testing for patient prognostication because of delays in SLNB.
Wide local excision was delayed by an average of 6 weeks in roughly one-third of melanoma patients with early tumor stage disease, regardless of margin status. For patients with stage T1b disease, wide local excision was typically performed on time during shelter-in-place; however, SLNB was delayed by an average of 5 weeks in 22% of patients with positive margins and 28% of those with negative margins. In contrast, 80% of patients with more advanced T2-T4 melanoma underwent on-schedule definitive management with wide local excision and SLNB, Dr. Hartman reported.
Critics have taken issue with the NCCN’s conclusion that most time-to-treatment studies show no harm arising from 90-day treatment delays. A review of the relevant published literature by Dr. Hartman’s Harvard colleagues, published in July, found that the evidence is mixed. “There is insufficient evidence to definitively conclude that delayed wide resection after gross removal of the primary melanoma is without harm,” they concluded in the review.
Spanish dermatologists performed a modeling study in order to estimate the potential impact of COVID-19 lockdowns on 5- and 10-year survival of melanoma patients. Using the growth rate of a random sample of 1,000 melanomas to model estimates of tumor thickness after various delays, coupled with American Joint Committee on Cancer survival data for different T stages, they estimated that 5-year survival would be reduced from 94.2% to 92.3% with a 90-day delay in diagnosis, and that 10-year survival would drop from 90.0% to 87.6%.
But that’s merely modeling. Francesco Ricci, MD, PhD, and colleagues from the melanoma unit at the Istituto Dermopatico dell’Immacolata, Rome, have provided a first look at the real-world impact of the lockdown. In the prelockdown period of January through March 9th, 2020, the referral center averaged 2.3 new melanoma diagnoses per day. During the Rome lockdown, from March 10th through May 3rd, this figure dropped to a mean of 0.6 melanoma diagnoses per day. Postlockdown, from May 4th to June 6th, the average climbed to 1.3 per day. The rate of newly diagnosed nodular melanoma was 5.5-fold greater postlockdown, compared with prelockdown; the rate of ulcerated melanoma was 4.9-fold greater.
“We can hypothesize that this may have been due to delays in diagnosis and care,” Dr. Hartman commented. “This is important because we know that nodular melanoma as well as ulceration tend to have a worse prognosis in terms of mortality.”
The mean Breslow thickness of newly diagnosed melanomas was 0.88 mm prelockdown, 0.66 mm during lockdown, and 1.96 mm postlockdown. The investigators speculated that the reduced Breslow thickness of melanomas diagnosed during lockdown might be explained by a greater willingness of more health-conscious people to defy the shelter-in-place instructions because of their concern about a suspicious skin lesion. “Though it is way too early to gauge the consequences of such diagnostic delay, should this issue be neglected, dermatologists and their patients may pay a higher price later with increased morbidity, mortality, and financial burden,” according to the investigators.
Dr. Hartman observed that it will be important to learn whether similar experiences occurred elsewhere during lockdown.
Another speaker, John M. Kirkwood, MD, said he has seen several melanoma patients referred from outside centers who had delays of up to 3 months in sentinel lymph node management of T2 and T3 tumors during lockdown who now have widespread metastatic disease.
“Now, is that anecdotal? I don’t know, it’s just worrisome to me,” commented Dr. Kirkwood, professor of medicine, dermatology, and translational science at the University of Pittsburgh.
Merrick Ross, MD, professor of surgical oncology at M.D. Anderson Cancer Center, Houston, recalled, “There was a period of time [during the lockdown] when we weren’t allowed to do certain elective procedures, if you want to call cancer surgery elective.”
“It’s too soon to talk about outcomes because a lot of patients are still in the process of being treated after what I would consider a significant delay in diagnosis,” the surgeon added.
An audience member asked if there will be an opportunity to see data on the damage done by delaying melanoma management as compared to lives saved through the lockdown for COVID-19. Dr. Ross replied that M.D. Anderson is in the midst of an institution-wide study analyzing the delay in diagnosis of a range of cancers.
“In our melanoma center it is absolutely clear, although we’re still collecting data, that the median tumor thickness is much higher since the lockdown,” Dr. Ross commented.
Dr. Hartman said she and her coinvestigators in the Melanoma Prevention Working Group are attempting to tally up the damage done via the lockdown by delaying melanoma diagnosis and treatment. But she agreed with the questioner that the most important thing is overall net lives saved through shelter-in-place.
“I’m sure that, separately, nondermatologists – perhaps infectious disease doctors and internists – are looking at how many lives were saved by the lockdown policy. So I do think all that data will come out,” Dr. Hartman predicted.
She reported having no financial conflicts regarding her presentation.
Global Academy for Medical Education and this news organization are owned by the same company.
SOURCE: Hartman, R. Cutaneous malignancies forum.
Initial evidence suggests that the , Rebecca I. Hartman, MD, MPH, said at a virtual forum on cutaneous malignancies jointly presented by Postgraduate Institute for Medicine and Global Academy for Medication Education.
This is not what National Comprehensive Cancer Network officials expected when they issued short-term recommendations on how to manage cutaneous melanoma during the first wave of the COVID-19 pandemic. Those recommendations for restriction of care, which Dr. Hartman characterized as “pretty significant changes from how we typically practice melanoma care in the U.S.,” came at a time when there was justifiable concern that the first COVID-19 surge would strain the U.S. health care system beyond the breaking point.
The rationale given for the NCCN recommendations was that most time-to-treat studies have shown no adverse patient outcomes for 90-day delays in treatment, even for thicker melanomas. But those studies, all retrospective, have been called into question. And the first real-world data on the impact of care restrictions during the lockdown, reported by Italian dermatologists, highlights adverse effects with potentially far-reaching consequences, noted Dr. Hartman, director of melanoma epidemiology at Brigham and Women’s Hospital and a dermatologist, Harvard University, Boston.
Analysis of the impact of lockdown-induced delays in melanoma care is not merely an academic exercise, she added. While everyone hopes that the spring 2020 COVID-19 shelter-in-place was a once-in-a-lifetime event, there’s no guarantee that will be the case. Moreover, the lockdown provides a natural experiment addressing the possible consequences of melanoma care delays on patient outcomes, a topic that for ethical reasons could never be addressed in a randomized trial.
The short-term NCCN recommendations included the use of excisional biopsies for melanoma diagnosis whenever possible; and delay of up to 3 months for wide local excision of in situ melanoma, any invasive melanoma with negative margins, and even T1 melanomas with positive margins provided the bulk of the lesion had been excised. The guidance also suggested delaying sentinel lymph node biopsy (SLNB), along with increased use of neoadjuvant therapy in patients with clinically palpable regional lymph nodes in order to delay surgery for up to 8 weeks. Single-agent systemic therapy at the least-frequent dosing was advised in order to minimize toxicity and reduce the need for additional health care resources: for example, nivolumab (Opdivo) at 480 mg every 4 weeks instead of every 2 weeks, and pembrolizumab (Keytruda) at 400 mg every 6 weeks, rather than every 3 weeks.
So, that’s what the NCCN recommended. Here’s what actually happened during shelter-in-place as captured in Dr. Hartman’s survey of 18 U.S. members of the Melanoma Prevention Working Group, all practicing dermatology in centers particularly hard-hit in the first wave of the pandemic: In-person new melanoma patient visits plunged from an average of 4.83 per week per provider to 0.83 per week. Telemedicine visits with new melanoma patients went from zero prepandemic to 0.67 visits per week per provider, which doesn’t come close to making up for the drop in in-person visits. Interestingly, two respondents reported turning to gene-expression profile testing for patient prognostication because of delays in SLNB.
Wide local excision was delayed by an average of 6 weeks in roughly one-third of melanoma patients with early tumor stage disease, regardless of margin status. For patients with stage T1b disease, wide local excision was typically performed on time during shelter-in-place; however, SLNB was delayed by an average of 5 weeks in 22% of patients with positive margins and 28% of those with negative margins. In contrast, 80% of patients with more advanced T2-T4 melanoma underwent on-schedule definitive management with wide local excision and SLNB, Dr. Hartman reported.
Critics have taken issue with the NCCN’s conclusion that most time-to-treatment studies show no harm arising from 90-day treatment delays. A review of the relevant published literature by Dr. Hartman’s Harvard colleagues, published in July, found that the evidence is mixed. “There is insufficient evidence to definitively conclude that delayed wide resection after gross removal of the primary melanoma is without harm,” they concluded in the review.
Spanish dermatologists performed a modeling study in order to estimate the potential impact of COVID-19 lockdowns on 5- and 10-year survival of melanoma patients. Using the growth rate of a random sample of 1,000 melanomas to model estimates of tumor thickness after various delays, coupled with American Joint Committee on Cancer survival data for different T stages, they estimated that 5-year survival would be reduced from 94.2% to 92.3% with a 90-day delay in diagnosis, and that 10-year survival would drop from 90.0% to 87.6%.
But that’s merely modeling. Francesco Ricci, MD, PhD, and colleagues from the melanoma unit at the Istituto Dermopatico dell’Immacolata, Rome, have provided a first look at the real-world impact of the lockdown. In the prelockdown period of January through March 9th, 2020, the referral center averaged 2.3 new melanoma diagnoses per day. During the Rome lockdown, from March 10th through May 3rd, this figure dropped to a mean of 0.6 melanoma diagnoses per day. Postlockdown, from May 4th to June 6th, the average climbed to 1.3 per day. The rate of newly diagnosed nodular melanoma was 5.5-fold greater postlockdown, compared with prelockdown; the rate of ulcerated melanoma was 4.9-fold greater.
“We can hypothesize that this may have been due to delays in diagnosis and care,” Dr. Hartman commented. “This is important because we know that nodular melanoma as well as ulceration tend to have a worse prognosis in terms of mortality.”
The mean Breslow thickness of newly diagnosed melanomas was 0.88 mm prelockdown, 0.66 mm during lockdown, and 1.96 mm postlockdown. The investigators speculated that the reduced Breslow thickness of melanomas diagnosed during lockdown might be explained by a greater willingness of more health-conscious people to defy the shelter-in-place instructions because of their concern about a suspicious skin lesion. “Though it is way too early to gauge the consequences of such diagnostic delay, should this issue be neglected, dermatologists and their patients may pay a higher price later with increased morbidity, mortality, and financial burden,” according to the investigators.
Dr. Hartman observed that it will be important to learn whether similar experiences occurred elsewhere during lockdown.
Another speaker, John M. Kirkwood, MD, said he has seen several melanoma patients referred from outside centers who had delays of up to 3 months in sentinel lymph node management of T2 and T3 tumors during lockdown who now have widespread metastatic disease.
“Now, is that anecdotal? I don’t know, it’s just worrisome to me,” commented Dr. Kirkwood, professor of medicine, dermatology, and translational science at the University of Pittsburgh.
Merrick Ross, MD, professor of surgical oncology at M.D. Anderson Cancer Center, Houston, recalled, “There was a period of time [during the lockdown] when we weren’t allowed to do certain elective procedures, if you want to call cancer surgery elective.”
“It’s too soon to talk about outcomes because a lot of patients are still in the process of being treated after what I would consider a significant delay in diagnosis,” the surgeon added.
An audience member asked if there will be an opportunity to see data on the damage done by delaying melanoma management as compared to lives saved through the lockdown for COVID-19. Dr. Ross replied that M.D. Anderson is in the midst of an institution-wide study analyzing the delay in diagnosis of a range of cancers.
“In our melanoma center it is absolutely clear, although we’re still collecting data, that the median tumor thickness is much higher since the lockdown,” Dr. Ross commented.
Dr. Hartman said she and her coinvestigators in the Melanoma Prevention Working Group are attempting to tally up the damage done via the lockdown by delaying melanoma diagnosis and treatment. But she agreed with the questioner that the most important thing is overall net lives saved through shelter-in-place.
“I’m sure that, separately, nondermatologists – perhaps infectious disease doctors and internists – are looking at how many lives were saved by the lockdown policy. So I do think all that data will come out,” Dr. Hartman predicted.
She reported having no financial conflicts regarding her presentation.
Global Academy for Medical Education and this news organization are owned by the same company.
SOURCE: Hartman, R. Cutaneous malignancies forum.
REPORTING FROM THE CUTANEOUS MALIGNANCIES FORUM
Trump could clean house at health agencies
Others may soon depart voluntarily. Politico reported in late October that more than two dozen political appointees had already left the U.S. Department Health and Human Services (HHS) since the start of the COVID-19 pandemic in February and that potentially dozens of the more than 100 in the department would leave if Trump was not reelected.
Trump hasn’t conceded, he is challenging the election results, and he has already fired his Defense Secretary, Mark Esper.
Among those possibly in Trump’s sights: HHS Secretary Alex Azar, US Food and Drug Administration (FDA) Commissioner Stephen Hahn, MD, Centers for Disease Control and Prevention (CDC) Director Robert Redfield, MD, and White House Coronavirus Task Force member Anthony Fauci, MD, who is also the director of the National Institutes of Allergy and Infectious Diseases.
Seema Verma, the administrator of the Centers for Medicare & Medicaid Services (CMS), is likely safe. According to Politico, Verma is expected to leave on her own terms.
Azar has had a long run as a Trump appointee. He took office in January 2018 and has been a staunch loyalist. But he’s frequently been the butt of grousing by Trump for not doing enough to help lower drug prices and for his handling of the coronavirus pandemic. Azar was initially in charge of the Trump virus effort but was quickly replaced by Vice President Mike Pence.
It was widely reported in late April that Trump was considering firing Azar, but the president called that “fake news” in a tweet.
Azar has complained about Hahn, who was confirmed in December 2019. According to Politico, Azar was looking into how to remove Hahn as commissioner because of the FDA’s battle with the White House over standards for emergency use authorization of a coronavirus vaccine.
In addition, Trump was infuriated by the agency’s insistence that it stick to the highest bar for an emergency approval. “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd,” Trump tweeted at Hahn.
Fauci on the firing line?
Most of the president’s ire has been directed at Fauci. As far back as April, Trump retweeted a call for Fauci’s firing. Twitter removed the original tweet but kept Trump’s comments on the original tweet.
The president has frequently questioned Fauci’s advice, sidelined him from task force meetings, and infrequently met with him. Trump called Fauci a “disaster” during a call with supporters in October, and then, at a campaign rally in November, intimated that he would fire the scientist after the election, according to The Washington Post.
But such a firing cannot be easily done. Some have speculated that Trump could pressure Fauci’s boss, Francis Collins, MD, PhD — the director of the National Institutes of Health (NIH), who is a political appointee — to get rid of him. But Collins would have to come up with a reason to fire Fauci. Because he is not a political appointee, Fauci is afforded a raft of protections given to civil service employees of the federal government.
To demote or fire Fauci, Collins would have to give him 30 days’ notice unless there’s a belief that he committed a crime. Fauci would have at least a week to offer evidence and affidavits in support of his service.
He’d also be entitled to legal representation, a written decision, and the specific reasons for the action being taken quickly. He could also request a hearing, and he’d be able to appeal any action to the Merit Systems Protection Board. The process could take months, if not years.
In late October, Trump issued an executive order that would reclassify certain federal employees so that they wouldn’t have such protections. But agencies have until mid-January to come up with lists of such workers, according to Government Executive.
Collins has been with NIH since 1993, when he headed the Human Genome Project and the National Human Genome Research Institute. Politico has speculated that Collins, 70, might retire if Trump was reelected. It’s unclear what he’ll do now.
Redfield, who has taken heat for his leadership from many in public health — and was asked in October to stand up to Trump by former CDC Director William H. Foege, MD — has been openly contradicted by the president on more than one occasion, according to The New York Times.
In September, The Hill reported that Trump told reporters that he’d chastised Redfield by phone soon after Redfield had told a Senate committee that a coronavirus vaccine would not be available until mid-2021.
This article first appeared on Medscape.com.
Others may soon depart voluntarily. Politico reported in late October that more than two dozen political appointees had already left the U.S. Department Health and Human Services (HHS) since the start of the COVID-19 pandemic in February and that potentially dozens of the more than 100 in the department would leave if Trump was not reelected.
Trump hasn’t conceded, he is challenging the election results, and he has already fired his Defense Secretary, Mark Esper.
Among those possibly in Trump’s sights: HHS Secretary Alex Azar, US Food and Drug Administration (FDA) Commissioner Stephen Hahn, MD, Centers for Disease Control and Prevention (CDC) Director Robert Redfield, MD, and White House Coronavirus Task Force member Anthony Fauci, MD, who is also the director of the National Institutes of Allergy and Infectious Diseases.
Seema Verma, the administrator of the Centers for Medicare & Medicaid Services (CMS), is likely safe. According to Politico, Verma is expected to leave on her own terms.
Azar has had a long run as a Trump appointee. He took office in January 2018 and has been a staunch loyalist. But he’s frequently been the butt of grousing by Trump for not doing enough to help lower drug prices and for his handling of the coronavirus pandemic. Azar was initially in charge of the Trump virus effort but was quickly replaced by Vice President Mike Pence.
It was widely reported in late April that Trump was considering firing Azar, but the president called that “fake news” in a tweet.
Azar has complained about Hahn, who was confirmed in December 2019. According to Politico, Azar was looking into how to remove Hahn as commissioner because of the FDA’s battle with the White House over standards for emergency use authorization of a coronavirus vaccine.
In addition, Trump was infuriated by the agency’s insistence that it stick to the highest bar for an emergency approval. “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd,” Trump tweeted at Hahn.
Fauci on the firing line?
Most of the president’s ire has been directed at Fauci. As far back as April, Trump retweeted a call for Fauci’s firing. Twitter removed the original tweet but kept Trump’s comments on the original tweet.
The president has frequently questioned Fauci’s advice, sidelined him from task force meetings, and infrequently met with him. Trump called Fauci a “disaster” during a call with supporters in October, and then, at a campaign rally in November, intimated that he would fire the scientist after the election, according to The Washington Post.
But such a firing cannot be easily done. Some have speculated that Trump could pressure Fauci’s boss, Francis Collins, MD, PhD — the director of the National Institutes of Health (NIH), who is a political appointee — to get rid of him. But Collins would have to come up with a reason to fire Fauci. Because he is not a political appointee, Fauci is afforded a raft of protections given to civil service employees of the federal government.
To demote or fire Fauci, Collins would have to give him 30 days’ notice unless there’s a belief that he committed a crime. Fauci would have at least a week to offer evidence and affidavits in support of his service.
He’d also be entitled to legal representation, a written decision, and the specific reasons for the action being taken quickly. He could also request a hearing, and he’d be able to appeal any action to the Merit Systems Protection Board. The process could take months, if not years.
In late October, Trump issued an executive order that would reclassify certain federal employees so that they wouldn’t have such protections. But agencies have until mid-January to come up with lists of such workers, according to Government Executive.
Collins has been with NIH since 1993, when he headed the Human Genome Project and the National Human Genome Research Institute. Politico has speculated that Collins, 70, might retire if Trump was reelected. It’s unclear what he’ll do now.
Redfield, who has taken heat for his leadership from many in public health — and was asked in October to stand up to Trump by former CDC Director William H. Foege, MD — has been openly contradicted by the president on more than one occasion, according to The New York Times.
In September, The Hill reported that Trump told reporters that he’d chastised Redfield by phone soon after Redfield had told a Senate committee that a coronavirus vaccine would not be available until mid-2021.
This article first appeared on Medscape.com.
Others may soon depart voluntarily. Politico reported in late October that more than two dozen political appointees had already left the U.S. Department Health and Human Services (HHS) since the start of the COVID-19 pandemic in February and that potentially dozens of the more than 100 in the department would leave if Trump was not reelected.
Trump hasn’t conceded, he is challenging the election results, and he has already fired his Defense Secretary, Mark Esper.
Among those possibly in Trump’s sights: HHS Secretary Alex Azar, US Food and Drug Administration (FDA) Commissioner Stephen Hahn, MD, Centers for Disease Control and Prevention (CDC) Director Robert Redfield, MD, and White House Coronavirus Task Force member Anthony Fauci, MD, who is also the director of the National Institutes of Allergy and Infectious Diseases.
Seema Verma, the administrator of the Centers for Medicare & Medicaid Services (CMS), is likely safe. According to Politico, Verma is expected to leave on her own terms.
Azar has had a long run as a Trump appointee. He took office in January 2018 and has been a staunch loyalist. But he’s frequently been the butt of grousing by Trump for not doing enough to help lower drug prices and for his handling of the coronavirus pandemic. Azar was initially in charge of the Trump virus effort but was quickly replaced by Vice President Mike Pence.
It was widely reported in late April that Trump was considering firing Azar, but the president called that “fake news” in a tweet.
Azar has complained about Hahn, who was confirmed in December 2019. According to Politico, Azar was looking into how to remove Hahn as commissioner because of the FDA’s battle with the White House over standards for emergency use authorization of a coronavirus vaccine.
In addition, Trump was infuriated by the agency’s insistence that it stick to the highest bar for an emergency approval. “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd,” Trump tweeted at Hahn.
Fauci on the firing line?
Most of the president’s ire has been directed at Fauci. As far back as April, Trump retweeted a call for Fauci’s firing. Twitter removed the original tweet but kept Trump’s comments on the original tweet.
The president has frequently questioned Fauci’s advice, sidelined him from task force meetings, and infrequently met with him. Trump called Fauci a “disaster” during a call with supporters in October, and then, at a campaign rally in November, intimated that he would fire the scientist after the election, according to The Washington Post.
But such a firing cannot be easily done. Some have speculated that Trump could pressure Fauci’s boss, Francis Collins, MD, PhD — the director of the National Institutes of Health (NIH), who is a political appointee — to get rid of him. But Collins would have to come up with a reason to fire Fauci. Because he is not a political appointee, Fauci is afforded a raft of protections given to civil service employees of the federal government.
To demote or fire Fauci, Collins would have to give him 30 days’ notice unless there’s a belief that he committed a crime. Fauci would have at least a week to offer evidence and affidavits in support of his service.
He’d also be entitled to legal representation, a written decision, and the specific reasons for the action being taken quickly. He could also request a hearing, and he’d be able to appeal any action to the Merit Systems Protection Board. The process could take months, if not years.
In late October, Trump issued an executive order that would reclassify certain federal employees so that they wouldn’t have such protections. But agencies have until mid-January to come up with lists of such workers, according to Government Executive.
Collins has been with NIH since 1993, when he headed the Human Genome Project and the National Human Genome Research Institute. Politico has speculated that Collins, 70, might retire if Trump was reelected. It’s unclear what he’ll do now.
Redfield, who has taken heat for his leadership from many in public health — and was asked in October to stand up to Trump by former CDC Director William H. Foege, MD — has been openly contradicted by the president on more than one occasion, according to The New York Times.
In September, The Hill reported that Trump told reporters that he’d chastised Redfield by phone soon after Redfield had told a Senate committee that a coronavirus vaccine would not be available until mid-2021.
This article first appeared on Medscape.com.
Supreme Court Justices seem skeptical of case to overturn ACA
The Justices conducted arguments by telephone in the case, California v Texas (previously California v US), which was brought by 18 Republican state officials and two individual plaintiffs. The Trump administration joined the plaintiffs in June, arguing that the entire law should be overturned. The ACA is being defended by Democratic state officials from 16 states and Washington, D.C.
The Republican plaintiffs have essentially argued that the ACA cannot stand without the individual mandate requirement – that it is not possible to “sever” it from the rest of the Act. In 2017, Congress set the tax penalty to $0 if an individual did not buy insurance. The mandate to buy insurance was left in place, but there were no longer any consequences. The plaintiffs said that congressional act was equivalent to severing the mandate.
But many Justices appeared to take a dim view of that argument.
“It’s a very straightforward case for severability under our precedents,” said Justice Brett Kavanaugh. “Meaning that we would excise the mandate and leave the rest of the Act in play. Congress knows how to write an inseverability clause and that is not the language that they chose here,” he said.
Justice Elena Kagan also questioned how it would jibe with legal precedent to allow the severing of one part of a law when there was no clear instruction from Congress on the issue. She also raised the concern that it would open the door to all sorts of challenges.
“It would seem a big deal to say that, if you can point to injury with respect to one provision and you can concoct some kind of inseverability argument, that allows you to challenge anything else in the statute,” she said.
“Isn’t that something that really cuts against all of our doctrine?” asked Kagan.
“I think it’s hard for you to argue that Congress intended the entire Act to fall if the mandate was struck down when the same Congress that lowered the penalty to zero did not even try to repeal the rest of the act,” said Chief Justice John Roberts.
“I think, frankly, that they wanted the Court to do that but that’s not our job,” he added.
Proof of harm?
To have the standing to sue, the plaintiffs have to prove they have been harmed by the ACA. Texas Solicitor General Kyle Hawkins said that individuals feel compelled to buy insurance – even without a penalty hanging over their heads.
Justice Stephen Breyer argued that many laws include what he called “precatory” language – that is, they seek to compel citizens to do something. But most don’t penalize those who fail to act – just like the ACA currently.
If, as the Texas plaintiffs argued, it’s still unconstitutional to make such a request, “I think there will be an awful lot of language in an awful lot of statutes that will suddenly be the subject of court constitutional challenge,” he said.
Hawkins disagreed. He said the ACA’s mandate “is not some suggestion, not some hortatory statement. It is the law of the United States of America today that you have to purchase health insurance and not just any health insurance, but health insurance that the federal government has decided would be best for you.”
Hawkins said that, if just one additional person signed up for Medicaid, the state of Texas and the other plaintiff states would be harmed. He said people were continuing to enroll in the program because they believed the law required them to get health insurance.
Justice Sonia Sotomayor said that defied common sense. “The problem is that your theory assumes people that people are going to pay a tax and break the law by not buying insurance, but they wouldn’t do it when the tax is zero.”
What’s at stake
It’s unlikely the justices will issue a decision immediately. They have until the end of the term in June to rule.
Katie Keith, JD, MPH, a principal at Keith Policy Solutions, LLC, outlined the potential outcomes in Health Affairs .
“The most likely scenario is that the Court maintains the status quo,” she wrote. They could get there by deciding Texas et al. did not have standing to bring the case. Or they could decide that either the mandate is constitutional or that it is unconstitutional but can be severed from the rest of the ACA.
The Court could alternatively find that some or all of the law’s insurance provisions – such as protections for people with pre-existing conditions – can’t be severed from the mandate. Or the justices could strike down all of the insurance consumer protections, the health insurance marketplaces, premium tax credits, and other provisions, which would force states to come up with the money to help people buy insurance. And states are unlikely to be able to do so, especially with the pandemic stretching their budgets.
Finally, the Court could find that the mandate can’t be separated, which would essentially overturn the law.
If that happens, some 15 million people could lose Medicaid coverage, 11 million who buy on health insurance exchanges could lose coverage, and 2.3 million young adults would no longer be able to stay on parents’ policies, according to the Kaiser Family Foundation. Kaiser also estimates that 54 million people under age 65 who have pre-existing conditions would no longer be guaranteed coverage.
The Urban Institute estimates that 21 million people could lose insurance – 15 million through Medicaid and the Children’s Health Insurance Program (CHIP) and 7.6 million through private nongroup coverage.
Medical societies weigh in
Multiple physicians’ groups, patient advocates, and hospital organizations have filed briefs with the Court in favor of keeping the law intact.
Twenty patient groups representing millions with pre-existing conditions – including the American Cancer Society, American Diabetes Association, American Heart Association, National Alliance on Mental Illness, National Organization for Rare Disorders, and the Kennedy Forum – filed a court brief in May arguing that the law has expanded access to insurance and improved patient outcomes.
“The coronavirus pandemic has only served to underscore the necessity of meaningful coverage – especially for those who are at high risk of being severely affected by the virus – including countless Americans who have pre-existing, acute or chronic conditions like heart disease, cancer, diabetes, lung diseases and multiple sclerosis,” they said in a statement.
Jacqueline W. Fincher, MD, MACP, president of the American College of Physicians, which joined a court brief in support of the law with 19 other medical organizations, said the law has worked.
“The coverage, protections and benefits provided by the ACA are critical to the well-being of millions of Americans,” she said in a statement.
“If the ACA were to be thrown out at the same time that we face the pandemic, it would cause chaos for physicians and our patients, and for the entire health care system,” said Fincher, adding that millions of Americans who have been infected could lose insurance if protections for pre-existing conditions disappeared.
“The ACA has revolutionized access to care for tens of millions of women by helping them obtain meaningful health coverage, ensuring that essential care is covered by insurers, and protecting patients from unfair insurance practices,” said Maureen G. Phipps, MD, MPH, CEO of the American College of Obstetricians and Gynecologists (ACOG), in a statement.
Overturning the ACA “would be one of the most singularly disruptive acts to be committed during this public health crisis,” she said.
American Psychiatric Association President Jeffrey Geller, MD, MPH, also warned of disruptions to care, especially for those with mental health and substance use disorders. “We urge the Supreme Court to preserve the entire Act, including the individual mandate,” he said, in a statement.
“In the midst of COVID is no time to let down the millions who we serve as our patients,” said Chip Kahn, Federation of American Health Systems president and CEO, in a statement.
“As caregivers, the goal of hospitals for our patients is to see increased access to affordable coverage for all Americans – not new obstacles,” he said, adding that the ACA “can accomplish this goal. We hope the Supreme Court will see its way clear to allow it to go forward.”
For the defense
Many legal analysts on social media who listened in to today’s hearing agreed that the tenor of the proceedings seemed to lean toward survival of the ACA.
“At this point I would say it is *extremely* likely that the ACA will be upheld, but the mandate struck down and severed out,” tweeted Raffi Melkonian, an appellate lawyer in Houston, Texas. “A decision on standing (throwing out the case entirely) is also possible. The chance that the ACA is struck down v. low.”
“Both Kavanaugh and Roberts have suggested this morning that they may view the individual mandate as severable from the rest of the law. If those two justices join the court’s three liberals in finding that the mandate is severable, that would be five votes to save the ACA,” tweeted the analysts at SCOTUS Blog.
Sean Marotta, a lawyer with Hogan Lovells’ Supreme Court group, agreed. “Oral argument is always an imperfect measure, but the Act’s defenders should feel good today,” he tweeted.
This article first appeared on Medscape.com.
The Justices conducted arguments by telephone in the case, California v Texas (previously California v US), which was brought by 18 Republican state officials and two individual plaintiffs. The Trump administration joined the plaintiffs in June, arguing that the entire law should be overturned. The ACA is being defended by Democratic state officials from 16 states and Washington, D.C.
The Republican plaintiffs have essentially argued that the ACA cannot stand without the individual mandate requirement – that it is not possible to “sever” it from the rest of the Act. In 2017, Congress set the tax penalty to $0 if an individual did not buy insurance. The mandate to buy insurance was left in place, but there were no longer any consequences. The plaintiffs said that congressional act was equivalent to severing the mandate.
But many Justices appeared to take a dim view of that argument.
“It’s a very straightforward case for severability under our precedents,” said Justice Brett Kavanaugh. “Meaning that we would excise the mandate and leave the rest of the Act in play. Congress knows how to write an inseverability clause and that is not the language that they chose here,” he said.
Justice Elena Kagan also questioned how it would jibe with legal precedent to allow the severing of one part of a law when there was no clear instruction from Congress on the issue. She also raised the concern that it would open the door to all sorts of challenges.
“It would seem a big deal to say that, if you can point to injury with respect to one provision and you can concoct some kind of inseverability argument, that allows you to challenge anything else in the statute,” she said.
“Isn’t that something that really cuts against all of our doctrine?” asked Kagan.
“I think it’s hard for you to argue that Congress intended the entire Act to fall if the mandate was struck down when the same Congress that lowered the penalty to zero did not even try to repeal the rest of the act,” said Chief Justice John Roberts.
“I think, frankly, that they wanted the Court to do that but that’s not our job,” he added.
Proof of harm?
To have the standing to sue, the plaintiffs have to prove they have been harmed by the ACA. Texas Solicitor General Kyle Hawkins said that individuals feel compelled to buy insurance – even without a penalty hanging over their heads.
Justice Stephen Breyer argued that many laws include what he called “precatory” language – that is, they seek to compel citizens to do something. But most don’t penalize those who fail to act – just like the ACA currently.
If, as the Texas plaintiffs argued, it’s still unconstitutional to make such a request, “I think there will be an awful lot of language in an awful lot of statutes that will suddenly be the subject of court constitutional challenge,” he said.
Hawkins disagreed. He said the ACA’s mandate “is not some suggestion, not some hortatory statement. It is the law of the United States of America today that you have to purchase health insurance and not just any health insurance, but health insurance that the federal government has decided would be best for you.”
Hawkins said that, if just one additional person signed up for Medicaid, the state of Texas and the other plaintiff states would be harmed. He said people were continuing to enroll in the program because they believed the law required them to get health insurance.
Justice Sonia Sotomayor said that defied common sense. “The problem is that your theory assumes people that people are going to pay a tax and break the law by not buying insurance, but they wouldn’t do it when the tax is zero.”
What’s at stake
It’s unlikely the justices will issue a decision immediately. They have until the end of the term in June to rule.
Katie Keith, JD, MPH, a principal at Keith Policy Solutions, LLC, outlined the potential outcomes in Health Affairs .
“The most likely scenario is that the Court maintains the status quo,” she wrote. They could get there by deciding Texas et al. did not have standing to bring the case. Or they could decide that either the mandate is constitutional or that it is unconstitutional but can be severed from the rest of the ACA.
The Court could alternatively find that some or all of the law’s insurance provisions – such as protections for people with pre-existing conditions – can’t be severed from the mandate. Or the justices could strike down all of the insurance consumer protections, the health insurance marketplaces, premium tax credits, and other provisions, which would force states to come up with the money to help people buy insurance. And states are unlikely to be able to do so, especially with the pandemic stretching their budgets.
Finally, the Court could find that the mandate can’t be separated, which would essentially overturn the law.
If that happens, some 15 million people could lose Medicaid coverage, 11 million who buy on health insurance exchanges could lose coverage, and 2.3 million young adults would no longer be able to stay on parents’ policies, according to the Kaiser Family Foundation. Kaiser also estimates that 54 million people under age 65 who have pre-existing conditions would no longer be guaranteed coverage.
The Urban Institute estimates that 21 million people could lose insurance – 15 million through Medicaid and the Children’s Health Insurance Program (CHIP) and 7.6 million through private nongroup coverage.
Medical societies weigh in
Multiple physicians’ groups, patient advocates, and hospital organizations have filed briefs with the Court in favor of keeping the law intact.
Twenty patient groups representing millions with pre-existing conditions – including the American Cancer Society, American Diabetes Association, American Heart Association, National Alliance on Mental Illness, National Organization for Rare Disorders, and the Kennedy Forum – filed a court brief in May arguing that the law has expanded access to insurance and improved patient outcomes.
“The coronavirus pandemic has only served to underscore the necessity of meaningful coverage – especially for those who are at high risk of being severely affected by the virus – including countless Americans who have pre-existing, acute or chronic conditions like heart disease, cancer, diabetes, lung diseases and multiple sclerosis,” they said in a statement.
Jacqueline W. Fincher, MD, MACP, president of the American College of Physicians, which joined a court brief in support of the law with 19 other medical organizations, said the law has worked.
“The coverage, protections and benefits provided by the ACA are critical to the well-being of millions of Americans,” she said in a statement.
“If the ACA were to be thrown out at the same time that we face the pandemic, it would cause chaos for physicians and our patients, and for the entire health care system,” said Fincher, adding that millions of Americans who have been infected could lose insurance if protections for pre-existing conditions disappeared.
“The ACA has revolutionized access to care for tens of millions of women by helping them obtain meaningful health coverage, ensuring that essential care is covered by insurers, and protecting patients from unfair insurance practices,” said Maureen G. Phipps, MD, MPH, CEO of the American College of Obstetricians and Gynecologists (ACOG), in a statement.
Overturning the ACA “would be one of the most singularly disruptive acts to be committed during this public health crisis,” she said.
American Psychiatric Association President Jeffrey Geller, MD, MPH, also warned of disruptions to care, especially for those with mental health and substance use disorders. “We urge the Supreme Court to preserve the entire Act, including the individual mandate,” he said, in a statement.
“In the midst of COVID is no time to let down the millions who we serve as our patients,” said Chip Kahn, Federation of American Health Systems president and CEO, in a statement.
“As caregivers, the goal of hospitals for our patients is to see increased access to affordable coverage for all Americans – not new obstacles,” he said, adding that the ACA “can accomplish this goal. We hope the Supreme Court will see its way clear to allow it to go forward.”
For the defense
Many legal analysts on social media who listened in to today’s hearing agreed that the tenor of the proceedings seemed to lean toward survival of the ACA.
“At this point I would say it is *extremely* likely that the ACA will be upheld, but the mandate struck down and severed out,” tweeted Raffi Melkonian, an appellate lawyer in Houston, Texas. “A decision on standing (throwing out the case entirely) is also possible. The chance that the ACA is struck down v. low.”
“Both Kavanaugh and Roberts have suggested this morning that they may view the individual mandate as severable from the rest of the law. If those two justices join the court’s three liberals in finding that the mandate is severable, that would be five votes to save the ACA,” tweeted the analysts at SCOTUS Blog.
Sean Marotta, a lawyer with Hogan Lovells’ Supreme Court group, agreed. “Oral argument is always an imperfect measure, but the Act’s defenders should feel good today,” he tweeted.
This article first appeared on Medscape.com.
The Justices conducted arguments by telephone in the case, California v Texas (previously California v US), which was brought by 18 Republican state officials and two individual plaintiffs. The Trump administration joined the plaintiffs in June, arguing that the entire law should be overturned. The ACA is being defended by Democratic state officials from 16 states and Washington, D.C.
The Republican plaintiffs have essentially argued that the ACA cannot stand without the individual mandate requirement – that it is not possible to “sever” it from the rest of the Act. In 2017, Congress set the tax penalty to $0 if an individual did not buy insurance. The mandate to buy insurance was left in place, but there were no longer any consequences. The plaintiffs said that congressional act was equivalent to severing the mandate.
But many Justices appeared to take a dim view of that argument.
“It’s a very straightforward case for severability under our precedents,” said Justice Brett Kavanaugh. “Meaning that we would excise the mandate and leave the rest of the Act in play. Congress knows how to write an inseverability clause and that is not the language that they chose here,” he said.
Justice Elena Kagan also questioned how it would jibe with legal precedent to allow the severing of one part of a law when there was no clear instruction from Congress on the issue. She also raised the concern that it would open the door to all sorts of challenges.
“It would seem a big deal to say that, if you can point to injury with respect to one provision and you can concoct some kind of inseverability argument, that allows you to challenge anything else in the statute,” she said.
“Isn’t that something that really cuts against all of our doctrine?” asked Kagan.
“I think it’s hard for you to argue that Congress intended the entire Act to fall if the mandate was struck down when the same Congress that lowered the penalty to zero did not even try to repeal the rest of the act,” said Chief Justice John Roberts.
“I think, frankly, that they wanted the Court to do that but that’s not our job,” he added.
Proof of harm?
To have the standing to sue, the plaintiffs have to prove they have been harmed by the ACA. Texas Solicitor General Kyle Hawkins said that individuals feel compelled to buy insurance – even without a penalty hanging over their heads.
Justice Stephen Breyer argued that many laws include what he called “precatory” language – that is, they seek to compel citizens to do something. But most don’t penalize those who fail to act – just like the ACA currently.
If, as the Texas plaintiffs argued, it’s still unconstitutional to make such a request, “I think there will be an awful lot of language in an awful lot of statutes that will suddenly be the subject of court constitutional challenge,” he said.
Hawkins disagreed. He said the ACA’s mandate “is not some suggestion, not some hortatory statement. It is the law of the United States of America today that you have to purchase health insurance and not just any health insurance, but health insurance that the federal government has decided would be best for you.”
Hawkins said that, if just one additional person signed up for Medicaid, the state of Texas and the other plaintiff states would be harmed. He said people were continuing to enroll in the program because they believed the law required them to get health insurance.
Justice Sonia Sotomayor said that defied common sense. “The problem is that your theory assumes people that people are going to pay a tax and break the law by not buying insurance, but they wouldn’t do it when the tax is zero.”
What’s at stake
It’s unlikely the justices will issue a decision immediately. They have until the end of the term in June to rule.
Katie Keith, JD, MPH, a principal at Keith Policy Solutions, LLC, outlined the potential outcomes in Health Affairs .
“The most likely scenario is that the Court maintains the status quo,” she wrote. They could get there by deciding Texas et al. did not have standing to bring the case. Or they could decide that either the mandate is constitutional or that it is unconstitutional but can be severed from the rest of the ACA.
The Court could alternatively find that some or all of the law’s insurance provisions – such as protections for people with pre-existing conditions – can’t be severed from the mandate. Or the justices could strike down all of the insurance consumer protections, the health insurance marketplaces, premium tax credits, and other provisions, which would force states to come up with the money to help people buy insurance. And states are unlikely to be able to do so, especially with the pandemic stretching their budgets.
Finally, the Court could find that the mandate can’t be separated, which would essentially overturn the law.
If that happens, some 15 million people could lose Medicaid coverage, 11 million who buy on health insurance exchanges could lose coverage, and 2.3 million young adults would no longer be able to stay on parents’ policies, according to the Kaiser Family Foundation. Kaiser also estimates that 54 million people under age 65 who have pre-existing conditions would no longer be guaranteed coverage.
The Urban Institute estimates that 21 million people could lose insurance – 15 million through Medicaid and the Children’s Health Insurance Program (CHIP) and 7.6 million through private nongroup coverage.
Medical societies weigh in
Multiple physicians’ groups, patient advocates, and hospital organizations have filed briefs with the Court in favor of keeping the law intact.
Twenty patient groups representing millions with pre-existing conditions – including the American Cancer Society, American Diabetes Association, American Heart Association, National Alliance on Mental Illness, National Organization for Rare Disorders, and the Kennedy Forum – filed a court brief in May arguing that the law has expanded access to insurance and improved patient outcomes.
“The coronavirus pandemic has only served to underscore the necessity of meaningful coverage – especially for those who are at high risk of being severely affected by the virus – including countless Americans who have pre-existing, acute or chronic conditions like heart disease, cancer, diabetes, lung diseases and multiple sclerosis,” they said in a statement.
Jacqueline W. Fincher, MD, MACP, president of the American College of Physicians, which joined a court brief in support of the law with 19 other medical organizations, said the law has worked.
“The coverage, protections and benefits provided by the ACA are critical to the well-being of millions of Americans,” she said in a statement.
“If the ACA were to be thrown out at the same time that we face the pandemic, it would cause chaos for physicians and our patients, and for the entire health care system,” said Fincher, adding that millions of Americans who have been infected could lose insurance if protections for pre-existing conditions disappeared.
“The ACA has revolutionized access to care for tens of millions of women by helping them obtain meaningful health coverage, ensuring that essential care is covered by insurers, and protecting patients from unfair insurance practices,” said Maureen G. Phipps, MD, MPH, CEO of the American College of Obstetricians and Gynecologists (ACOG), in a statement.
Overturning the ACA “would be one of the most singularly disruptive acts to be committed during this public health crisis,” she said.
American Psychiatric Association President Jeffrey Geller, MD, MPH, also warned of disruptions to care, especially for those with mental health and substance use disorders. “We urge the Supreme Court to preserve the entire Act, including the individual mandate,” he said, in a statement.
“In the midst of COVID is no time to let down the millions who we serve as our patients,” said Chip Kahn, Federation of American Health Systems president and CEO, in a statement.
“As caregivers, the goal of hospitals for our patients is to see increased access to affordable coverage for all Americans – not new obstacles,” he said, adding that the ACA “can accomplish this goal. We hope the Supreme Court will see its way clear to allow it to go forward.”
For the defense
Many legal analysts on social media who listened in to today’s hearing agreed that the tenor of the proceedings seemed to lean toward survival of the ACA.
“At this point I would say it is *extremely* likely that the ACA will be upheld, but the mandate struck down and severed out,” tweeted Raffi Melkonian, an appellate lawyer in Houston, Texas. “A decision on standing (throwing out the case entirely) is also possible. The chance that the ACA is struck down v. low.”
“Both Kavanaugh and Roberts have suggested this morning that they may view the individual mandate as severable from the rest of the law. If those two justices join the court’s three liberals in finding that the mandate is severable, that would be five votes to save the ACA,” tweeted the analysts at SCOTUS Blog.
Sean Marotta, a lawyer with Hogan Lovells’ Supreme Court group, agreed. “Oral argument is always an imperfect measure, but the Act’s defenders should feel good today,” he tweeted.
This article first appeared on Medscape.com.
FDA grants emergency use authorization to Lilly’s antibody COVID-19 therapy
The monoclonal antibody therapy has emergency authorization for treating patients who have tested positive for SARS-CoV-2 infection and who are considered to be at high risk for progression to severe COVID-19 or hospitalization. To be eligible for treatment with bamlanivimab, patients must be at least 12 years of age and weigh at least 40 kg (approximately 88 lb). The agency notes that this includes patients aged 65 years and older or people with certain chronic conditions.
Bamlanivimab is not authorized for use in patients who are hospitalized or who require oxygen therapy because of COVID-19. The FDA’s action comes less than 2 weeks after Eli Lilly halted the ACTIV-3 study of the therapy for severe, hospitalized COVID-19 patients after evidence showed that adding the antibody therapy to standard care did not improve outcomes over standard care alone for patients with advanced COVID-19.
The government contract with Eli Lilly involves the purchase of 300,000 doses through December, with the option to procure another 650,000 doses through June 2021.
Because of Operation Warp Speed, “we have supplies to distribute now. Product distribution will begin this week,” US Health & Human Services (HHS) Secretary Alex Azar said at a news conference today.
“We talked about building the bridge to safe and effective vaccines” for COVID-19, Azar added. “With this therapeutic, the bridge is taking shape.”
Bamlanivimab 700 mg will be administered as a 1-hour infusion followed by a 1-hour observation period for detecting any infusion-related side effects. The authorized dose is 700 mg, which was on the lower end of the dose range evaluated in studies.
During the press conference, a reporter asked whether the lower dose was chosen in order that more doses of the antibody could be made available. “The lower dose is a rational choice in this situation because we don’t want to give more of a drug than you need,” said Janet Woodcock, MD, the therapeutics lead for Operation Warp Speed. “I think we could probably go lower.”
Bamlanivimab works by attaching to the virus and blocking its entry into the cells and possibly by helping the patients’ immune system clear the virus, said Woodcock, who is also director of the FDA’s Center for Drug Evaluation and Research.
“The goal is to treat high-risk people as soon as possible after they show symptoms and are diagnosed,” she added.
Infusions an initial challenge?
There could be some logistic challenges at first because the antibody is administered via infusion. “We expect there will initially be a challenge in administering ... these infusions and setting up infusion centers,” Woodcock said.
Outpatient intravenous infusions are normally performed at infusion centers for patients with cancer and immune disorders, she noted. “You really don’t want them mixing with people who have COVID-19 disease, so we will need to set up separate sites.”
Bamlanivimab will be provided free of cost to patients, Azar said. Patients should be aware that coinsurance may be required for the infusion.
“Fair and equitable” distribution planned
During phase 1 of distribution, the agent will first be allocated to hospitals and hospital-affiliated locations only, John Redd, MD, MPH, chief medical officer, Office of the Assistant Secretary for Preparedness and Response at HHS, said at the press conference.
During phase 2, “there will be expanded distribution to outpatient sites,” he said. In an effort to keep the process transparent, a new website features the latest updates on the distribution of bamlanivimab.
Allocation will be based on two factors: the number of new cases reported in a state or territory in the prior 7 days, and rates of COVID-19 hospitalization during the same period.
Asked why the government would determine distribution of the antibody on the basis of the number of hospitalized patients when the indication includes prevention of admission, Woodcock replied that hospitalization is a surrogate measure that can reflect risk factors in a particular state population, such as obesity, diabetes, or the proportion of older people.
Furthermore, the confirmed cases are a “leading indicator,” she said, that can help identify a steep rise in COVID-19 cases that could indicate more hospitalizations are likely soon. “We don’t want to miss that.”
Data underlying the EUA decision
A decrease in hospitalizations or emergency department visits within 28 days of treatment in preclinical studies was “the most important evidence that bamlanivimab may be effective,” the agency noted in the press release announcing the EUA. Among patients at high risk for progression, 3% required such interventions, compared with 10% of placebo-treated patients.
Potential side effects of bamlanivimab include anaphylaxis, infusion-related reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting.
“As illustrated by today’s action, the FDA remains committed to expediting the development and availability of potential COVID-19 treatments and providing sick patients timely access to new therapies where appropriate,” FDA Commissioner Stephen M. Hahn, MD, said in the news release.
Healthcare providers can download a detailed FDA fact sheet on the EUA for bamlanivimab, which includes dosing instructions.
This article first appeared on Medscape.com.
The monoclonal antibody therapy has emergency authorization for treating patients who have tested positive for SARS-CoV-2 infection and who are considered to be at high risk for progression to severe COVID-19 or hospitalization. To be eligible for treatment with bamlanivimab, patients must be at least 12 years of age and weigh at least 40 kg (approximately 88 lb). The agency notes that this includes patients aged 65 years and older or people with certain chronic conditions.
Bamlanivimab is not authorized for use in patients who are hospitalized or who require oxygen therapy because of COVID-19. The FDA’s action comes less than 2 weeks after Eli Lilly halted the ACTIV-3 study of the therapy for severe, hospitalized COVID-19 patients after evidence showed that adding the antibody therapy to standard care did not improve outcomes over standard care alone for patients with advanced COVID-19.
The government contract with Eli Lilly involves the purchase of 300,000 doses through December, with the option to procure another 650,000 doses through June 2021.
Because of Operation Warp Speed, “we have supplies to distribute now. Product distribution will begin this week,” US Health & Human Services (HHS) Secretary Alex Azar said at a news conference today.
“We talked about building the bridge to safe and effective vaccines” for COVID-19, Azar added. “With this therapeutic, the bridge is taking shape.”
Bamlanivimab 700 mg will be administered as a 1-hour infusion followed by a 1-hour observation period for detecting any infusion-related side effects. The authorized dose is 700 mg, which was on the lower end of the dose range evaluated in studies.
During the press conference, a reporter asked whether the lower dose was chosen in order that more doses of the antibody could be made available. “The lower dose is a rational choice in this situation because we don’t want to give more of a drug than you need,” said Janet Woodcock, MD, the therapeutics lead for Operation Warp Speed. “I think we could probably go lower.”
Bamlanivimab works by attaching to the virus and blocking its entry into the cells and possibly by helping the patients’ immune system clear the virus, said Woodcock, who is also director of the FDA’s Center for Drug Evaluation and Research.
“The goal is to treat high-risk people as soon as possible after they show symptoms and are diagnosed,” she added.
Infusions an initial challenge?
There could be some logistic challenges at first because the antibody is administered via infusion. “We expect there will initially be a challenge in administering ... these infusions and setting up infusion centers,” Woodcock said.
Outpatient intravenous infusions are normally performed at infusion centers for patients with cancer and immune disorders, she noted. “You really don’t want them mixing with people who have COVID-19 disease, so we will need to set up separate sites.”
Bamlanivimab will be provided free of cost to patients, Azar said. Patients should be aware that coinsurance may be required for the infusion.
“Fair and equitable” distribution planned
During phase 1 of distribution, the agent will first be allocated to hospitals and hospital-affiliated locations only, John Redd, MD, MPH, chief medical officer, Office of the Assistant Secretary for Preparedness and Response at HHS, said at the press conference.
During phase 2, “there will be expanded distribution to outpatient sites,” he said. In an effort to keep the process transparent, a new website features the latest updates on the distribution of bamlanivimab.
Allocation will be based on two factors: the number of new cases reported in a state or territory in the prior 7 days, and rates of COVID-19 hospitalization during the same period.
Asked why the government would determine distribution of the antibody on the basis of the number of hospitalized patients when the indication includes prevention of admission, Woodcock replied that hospitalization is a surrogate measure that can reflect risk factors in a particular state population, such as obesity, diabetes, or the proportion of older people.
Furthermore, the confirmed cases are a “leading indicator,” she said, that can help identify a steep rise in COVID-19 cases that could indicate more hospitalizations are likely soon. “We don’t want to miss that.”
Data underlying the EUA decision
A decrease in hospitalizations or emergency department visits within 28 days of treatment in preclinical studies was “the most important evidence that bamlanivimab may be effective,” the agency noted in the press release announcing the EUA. Among patients at high risk for progression, 3% required such interventions, compared with 10% of placebo-treated patients.
Potential side effects of bamlanivimab include anaphylaxis, infusion-related reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting.
“As illustrated by today’s action, the FDA remains committed to expediting the development and availability of potential COVID-19 treatments and providing sick patients timely access to new therapies where appropriate,” FDA Commissioner Stephen M. Hahn, MD, said in the news release.
Healthcare providers can download a detailed FDA fact sheet on the EUA for bamlanivimab, which includes dosing instructions.
This article first appeared on Medscape.com.
The monoclonal antibody therapy has emergency authorization for treating patients who have tested positive for SARS-CoV-2 infection and who are considered to be at high risk for progression to severe COVID-19 or hospitalization. To be eligible for treatment with bamlanivimab, patients must be at least 12 years of age and weigh at least 40 kg (approximately 88 lb). The agency notes that this includes patients aged 65 years and older or people with certain chronic conditions.
Bamlanivimab is not authorized for use in patients who are hospitalized or who require oxygen therapy because of COVID-19. The FDA’s action comes less than 2 weeks after Eli Lilly halted the ACTIV-3 study of the therapy for severe, hospitalized COVID-19 patients after evidence showed that adding the antibody therapy to standard care did not improve outcomes over standard care alone for patients with advanced COVID-19.
The government contract with Eli Lilly involves the purchase of 300,000 doses through December, with the option to procure another 650,000 doses through June 2021.
Because of Operation Warp Speed, “we have supplies to distribute now. Product distribution will begin this week,” US Health & Human Services (HHS) Secretary Alex Azar said at a news conference today.
“We talked about building the bridge to safe and effective vaccines” for COVID-19, Azar added. “With this therapeutic, the bridge is taking shape.”
Bamlanivimab 700 mg will be administered as a 1-hour infusion followed by a 1-hour observation period for detecting any infusion-related side effects. The authorized dose is 700 mg, which was on the lower end of the dose range evaluated in studies.
During the press conference, a reporter asked whether the lower dose was chosen in order that more doses of the antibody could be made available. “The lower dose is a rational choice in this situation because we don’t want to give more of a drug than you need,” said Janet Woodcock, MD, the therapeutics lead for Operation Warp Speed. “I think we could probably go lower.”
Bamlanivimab works by attaching to the virus and blocking its entry into the cells and possibly by helping the patients’ immune system clear the virus, said Woodcock, who is also director of the FDA’s Center for Drug Evaluation and Research.
“The goal is to treat high-risk people as soon as possible after they show symptoms and are diagnosed,” she added.
Infusions an initial challenge?
There could be some logistic challenges at first because the antibody is administered via infusion. “We expect there will initially be a challenge in administering ... these infusions and setting up infusion centers,” Woodcock said.
Outpatient intravenous infusions are normally performed at infusion centers for patients with cancer and immune disorders, she noted. “You really don’t want them mixing with people who have COVID-19 disease, so we will need to set up separate sites.”
Bamlanivimab will be provided free of cost to patients, Azar said. Patients should be aware that coinsurance may be required for the infusion.
“Fair and equitable” distribution planned
During phase 1 of distribution, the agent will first be allocated to hospitals and hospital-affiliated locations only, John Redd, MD, MPH, chief medical officer, Office of the Assistant Secretary for Preparedness and Response at HHS, said at the press conference.
During phase 2, “there will be expanded distribution to outpatient sites,” he said. In an effort to keep the process transparent, a new website features the latest updates on the distribution of bamlanivimab.
Allocation will be based on two factors: the number of new cases reported in a state or territory in the prior 7 days, and rates of COVID-19 hospitalization during the same period.
Asked why the government would determine distribution of the antibody on the basis of the number of hospitalized patients when the indication includes prevention of admission, Woodcock replied that hospitalization is a surrogate measure that can reflect risk factors in a particular state population, such as obesity, diabetes, or the proportion of older people.
Furthermore, the confirmed cases are a “leading indicator,” she said, that can help identify a steep rise in COVID-19 cases that could indicate more hospitalizations are likely soon. “We don’t want to miss that.”
Data underlying the EUA decision
A decrease in hospitalizations or emergency department visits within 28 days of treatment in preclinical studies was “the most important evidence that bamlanivimab may be effective,” the agency noted in the press release announcing the EUA. Among patients at high risk for progression, 3% required such interventions, compared with 10% of placebo-treated patients.
Potential side effects of bamlanivimab include anaphylaxis, infusion-related reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting.
“As illustrated by today’s action, the FDA remains committed to expediting the development and availability of potential COVID-19 treatments and providing sick patients timely access to new therapies where appropriate,” FDA Commissioner Stephen M. Hahn, MD, said in the news release.
Healthcare providers can download a detailed FDA fact sheet on the EUA for bamlanivimab, which includes dosing instructions.
This article first appeared on Medscape.com.
FAST trial clears febuxostat of increased mortality in gout
Febuxostat (Uloric) emerged as noninferior to allopurinol regarding risk of cardiovascular death among people 60 years and older with gout and at least one additional cardiovascular risk factor, results of the Febuxostat versus Allopurinol Streamlined Trial (FAST) suggest.
This primary outcome of the FAST trial stands in contrast to results of the CARES trial in 2018. The CARES researchers previously reported a 4.3% increased risk of cardiovascular death associated with febuxostat, compared with a 3.2% rate with allopurinol, a statistically significant 34% increase in the relative risk.
“In contrast to previous studies, there was no evidence of increased mortality with febuxostat, and we believe the regulators should review febuxostat licensing restrictions,” senior author Thomas MacDonald, MD, of the University of Dundee (Scotland), said during a late-breaking abstract session at the virtual annual meeting of the American College of Rheumatology.
The results of the FAST trial were simultaneously published online in The Lancet.
Both febuxostat and allopurinol treat gout by lowering urate levels. Concerns about the cardiovascular safety of febuxostat led to two post-licensing studies: the Cardiovascular Safety of Febuxostat and Allopurinol in Participants with Gout and Cardiovascular Comorbidities (CARES) study, mandated by the U.S. Food and Drug Administration, and FAST, requested by the European Medicines Agency. In February 2019, the FDA added a warning about elevated cardiovascular death and death risk associated with febuxostat.
“When CARES was published, it was somewhat of a threat to our study,” Dr. MacDonald said. “After hearing from our data-monitoring committee, we were told we could continue the trial.”
Some switched from allopurinol to febuxostat
So Dr. MacDonald, lead author Isla Mackenzie, MBChB, and their colleagues enrolled 6,128 people with gout in the United Kingdom, Sweden, and Denmark between December 2011 and January 2018. They followed patients for a median of 4 years. Participants had a mean age of 71 years, 85% were men, and 33% had a history of cardiovascular disease. The investigators excluded anyone with a stroke or myocardial infarction in the previous 6 months.
All participants were being treated with allopurinol. The investigators titrated those not at target up to an ideal dose that achieved a serum urate concentration of less than 0.357 mmol/L (< 6 mg/dL). Next, they randomly assigned 3,065 people to continue allopurinol and another 3,063 to switch to 80-120 mg of febuxostat.
The primary outcome of the multicenter, prospective, randomized, open-label FAST trial was a composite of hospitalization for nonfatal MI or biomarker positive for acute coronary syndrome, nonfatal stroke, or cardiovascular death.
Key findings
“There was definitely a noninferior primary outcome,” Dr. MacDonald said. In the on-treatment analysis, 172 patients in the febuxostat group reached the composite endpoint versus 241 patients in the allopurinol group. There were 1.72 events per 100 patient-years in the febuxostat group versus 2.05 events in the allopurinol group (adjusted hazard ratio, 0.85; 95% confidence interval, 0.70-1.03). An intent-to-treat analysis also found that febuxostat was noninferior to allopurinol on this measure.
Urate levels were approximately 80 micromoles lower in the febuxostat group versus the allopurinol group each year of the study, Dr. MacDonald said.
At least one gout flare was experienced by 1,017 patients in the febuxostat group and by 1,044 participants in the allopurinol group. “However, there was no placebo group, so we don’t know the effectiveness of either of these agents at preventing flares” based on this research, he said.
Both the on-treatment and intention-to-treat (ITT) secondary analyses demonstrated the noninferiority of febuxostat, compared with allopurinol, for all-cause death, each individual component of the composite primary outcome – cardiovascular death, hospitalization for heart failure, and hospitalization for new, unstable, or worsening angina.
In contrast, the ITT analysis revealed a “nominally significant increase” in hospitalization for arrhythmia with no evidence of ischemia in the febuxostat group. The 0.583 events per 100 patient-years in this group versus 0.385 events in the allopurinol cohort generated an adjusted HR of 1.51 (95% CI, 1.05-2.17).
In terms of all-cause mortality, 222 participants (7.2%) in the febuxostat group died, compared with 263 people (8.6%) in the allopurinol group.
Adverse events and withdrawals
A total 1,720 participants (57.3%) in the febuxostat group experienced at least one serious adverse event, as did 1,812 participants (59.4%) in the allopurinol group. Less than 1% of serious adverse events in each group were considered treatment-related.
Dr. MacDonald said that 6.2% of the febuxostat patients and 5.5% of the allopurinol group withdrew from the study. “We had pretty good follow-up [94%],” Dr. MacDonald said. “I don’t want to criticize CARES, but 47% did drop out of that study, and they could not follow them anymore.”
Limitations of FAST include its open-label design and lack of a placebo group, although Dr. MacDonald pointed out that a placebo group would have been unethical. Strengths included its large randomized trial design and good external validity, he added. “This is what will happen in clinical practice if you switch people from allopurinol to febuxostat.”
When asked how he would treat people with gout now given the FAST findings, Dr. MacDonald said, “I’m not a rheumatologist, I’m a cardiovascular physician. But I would say from the evidence from the FAST trial, it appears to be safe to give patients febuxostat whether or not they have cardiovascular risk factors or prior cardiovascular disease.”
“The FAST study indicates that febuxostat is similar to allopurinol in terms of cardiovascular events during the treatment period. The strengths of this study are its large sample size, excellent follow-up rate, and the relatively long follow-up time,” session moderator Shervin Assassi, MD, said when asked for comment. Dr. Assassi, director of the division of rheumatology at the University of Texas Health Science Center at Houston, was not involved in the research.
Menarini, Ipsen, and Teijin Pharma funded the study. The University of Dundee receives research funds from Menarini. Dr. MacDonald disclosed that he received speaker or consultant fees from Menarini. Dr. Assassi had no relevant disclosures.
SOURCE: MacDonald T et al. Arthritis Rheumatol. 2020;72(suppl 10). ACR 2020, Abstract L08.
Febuxostat (Uloric) emerged as noninferior to allopurinol regarding risk of cardiovascular death among people 60 years and older with gout and at least one additional cardiovascular risk factor, results of the Febuxostat versus Allopurinol Streamlined Trial (FAST) suggest.
This primary outcome of the FAST trial stands in contrast to results of the CARES trial in 2018. The CARES researchers previously reported a 4.3% increased risk of cardiovascular death associated with febuxostat, compared with a 3.2% rate with allopurinol, a statistically significant 34% increase in the relative risk.
“In contrast to previous studies, there was no evidence of increased mortality with febuxostat, and we believe the regulators should review febuxostat licensing restrictions,” senior author Thomas MacDonald, MD, of the University of Dundee (Scotland), said during a late-breaking abstract session at the virtual annual meeting of the American College of Rheumatology.
The results of the FAST trial were simultaneously published online in The Lancet.
Both febuxostat and allopurinol treat gout by lowering urate levels. Concerns about the cardiovascular safety of febuxostat led to two post-licensing studies: the Cardiovascular Safety of Febuxostat and Allopurinol in Participants with Gout and Cardiovascular Comorbidities (CARES) study, mandated by the U.S. Food and Drug Administration, and FAST, requested by the European Medicines Agency. In February 2019, the FDA added a warning about elevated cardiovascular death and death risk associated with febuxostat.
“When CARES was published, it was somewhat of a threat to our study,” Dr. MacDonald said. “After hearing from our data-monitoring committee, we were told we could continue the trial.”
Some switched from allopurinol to febuxostat
So Dr. MacDonald, lead author Isla Mackenzie, MBChB, and their colleagues enrolled 6,128 people with gout in the United Kingdom, Sweden, and Denmark between December 2011 and January 2018. They followed patients for a median of 4 years. Participants had a mean age of 71 years, 85% were men, and 33% had a history of cardiovascular disease. The investigators excluded anyone with a stroke or myocardial infarction in the previous 6 months.
All participants were being treated with allopurinol. The investigators titrated those not at target up to an ideal dose that achieved a serum urate concentration of less than 0.357 mmol/L (< 6 mg/dL). Next, they randomly assigned 3,065 people to continue allopurinol and another 3,063 to switch to 80-120 mg of febuxostat.
The primary outcome of the multicenter, prospective, randomized, open-label FAST trial was a composite of hospitalization for nonfatal MI or biomarker positive for acute coronary syndrome, nonfatal stroke, or cardiovascular death.
Key findings
“There was definitely a noninferior primary outcome,” Dr. MacDonald said. In the on-treatment analysis, 172 patients in the febuxostat group reached the composite endpoint versus 241 patients in the allopurinol group. There were 1.72 events per 100 patient-years in the febuxostat group versus 2.05 events in the allopurinol group (adjusted hazard ratio, 0.85; 95% confidence interval, 0.70-1.03). An intent-to-treat analysis also found that febuxostat was noninferior to allopurinol on this measure.
Urate levels were approximately 80 micromoles lower in the febuxostat group versus the allopurinol group each year of the study, Dr. MacDonald said.
At least one gout flare was experienced by 1,017 patients in the febuxostat group and by 1,044 participants in the allopurinol group. “However, there was no placebo group, so we don’t know the effectiveness of either of these agents at preventing flares” based on this research, he said.
Both the on-treatment and intention-to-treat (ITT) secondary analyses demonstrated the noninferiority of febuxostat, compared with allopurinol, for all-cause death, each individual component of the composite primary outcome – cardiovascular death, hospitalization for heart failure, and hospitalization for new, unstable, or worsening angina.
In contrast, the ITT analysis revealed a “nominally significant increase” in hospitalization for arrhythmia with no evidence of ischemia in the febuxostat group. The 0.583 events per 100 patient-years in this group versus 0.385 events in the allopurinol cohort generated an adjusted HR of 1.51 (95% CI, 1.05-2.17).
In terms of all-cause mortality, 222 participants (7.2%) in the febuxostat group died, compared with 263 people (8.6%) in the allopurinol group.
Adverse events and withdrawals
A total 1,720 participants (57.3%) in the febuxostat group experienced at least one serious adverse event, as did 1,812 participants (59.4%) in the allopurinol group. Less than 1% of serious adverse events in each group were considered treatment-related.
Dr. MacDonald said that 6.2% of the febuxostat patients and 5.5% of the allopurinol group withdrew from the study. “We had pretty good follow-up [94%],” Dr. MacDonald said. “I don’t want to criticize CARES, but 47% did drop out of that study, and they could not follow them anymore.”
Limitations of FAST include its open-label design and lack of a placebo group, although Dr. MacDonald pointed out that a placebo group would have been unethical. Strengths included its large randomized trial design and good external validity, he added. “This is what will happen in clinical practice if you switch people from allopurinol to febuxostat.”
When asked how he would treat people with gout now given the FAST findings, Dr. MacDonald said, “I’m not a rheumatologist, I’m a cardiovascular physician. But I would say from the evidence from the FAST trial, it appears to be safe to give patients febuxostat whether or not they have cardiovascular risk factors or prior cardiovascular disease.”
“The FAST study indicates that febuxostat is similar to allopurinol in terms of cardiovascular events during the treatment period. The strengths of this study are its large sample size, excellent follow-up rate, and the relatively long follow-up time,” session moderator Shervin Assassi, MD, said when asked for comment. Dr. Assassi, director of the division of rheumatology at the University of Texas Health Science Center at Houston, was not involved in the research.
Menarini, Ipsen, and Teijin Pharma funded the study. The University of Dundee receives research funds from Menarini. Dr. MacDonald disclosed that he received speaker or consultant fees from Menarini. Dr. Assassi had no relevant disclosures.
SOURCE: MacDonald T et al. Arthritis Rheumatol. 2020;72(suppl 10). ACR 2020, Abstract L08.
Febuxostat (Uloric) emerged as noninferior to allopurinol regarding risk of cardiovascular death among people 60 years and older with gout and at least one additional cardiovascular risk factor, results of the Febuxostat versus Allopurinol Streamlined Trial (FAST) suggest.
This primary outcome of the FAST trial stands in contrast to results of the CARES trial in 2018. The CARES researchers previously reported a 4.3% increased risk of cardiovascular death associated with febuxostat, compared with a 3.2% rate with allopurinol, a statistically significant 34% increase in the relative risk.
“In contrast to previous studies, there was no evidence of increased mortality with febuxostat, and we believe the regulators should review febuxostat licensing restrictions,” senior author Thomas MacDonald, MD, of the University of Dundee (Scotland), said during a late-breaking abstract session at the virtual annual meeting of the American College of Rheumatology.
The results of the FAST trial were simultaneously published online in The Lancet.
Both febuxostat and allopurinol treat gout by lowering urate levels. Concerns about the cardiovascular safety of febuxostat led to two post-licensing studies: the Cardiovascular Safety of Febuxostat and Allopurinol in Participants with Gout and Cardiovascular Comorbidities (CARES) study, mandated by the U.S. Food and Drug Administration, and FAST, requested by the European Medicines Agency. In February 2019, the FDA added a warning about elevated cardiovascular death and death risk associated with febuxostat.
“When CARES was published, it was somewhat of a threat to our study,” Dr. MacDonald said. “After hearing from our data-monitoring committee, we were told we could continue the trial.”
Some switched from allopurinol to febuxostat
So Dr. MacDonald, lead author Isla Mackenzie, MBChB, and their colleagues enrolled 6,128 people with gout in the United Kingdom, Sweden, and Denmark between December 2011 and January 2018. They followed patients for a median of 4 years. Participants had a mean age of 71 years, 85% were men, and 33% had a history of cardiovascular disease. The investigators excluded anyone with a stroke or myocardial infarction in the previous 6 months.
All participants were being treated with allopurinol. The investigators titrated those not at target up to an ideal dose that achieved a serum urate concentration of less than 0.357 mmol/L (< 6 mg/dL). Next, they randomly assigned 3,065 people to continue allopurinol and another 3,063 to switch to 80-120 mg of febuxostat.
The primary outcome of the multicenter, prospective, randomized, open-label FAST trial was a composite of hospitalization for nonfatal MI or biomarker positive for acute coronary syndrome, nonfatal stroke, or cardiovascular death.
Key findings
“There was definitely a noninferior primary outcome,” Dr. MacDonald said. In the on-treatment analysis, 172 patients in the febuxostat group reached the composite endpoint versus 241 patients in the allopurinol group. There were 1.72 events per 100 patient-years in the febuxostat group versus 2.05 events in the allopurinol group (adjusted hazard ratio, 0.85; 95% confidence interval, 0.70-1.03). An intent-to-treat analysis also found that febuxostat was noninferior to allopurinol on this measure.
Urate levels were approximately 80 micromoles lower in the febuxostat group versus the allopurinol group each year of the study, Dr. MacDonald said.
At least one gout flare was experienced by 1,017 patients in the febuxostat group and by 1,044 participants in the allopurinol group. “However, there was no placebo group, so we don’t know the effectiveness of either of these agents at preventing flares” based on this research, he said.
Both the on-treatment and intention-to-treat (ITT) secondary analyses demonstrated the noninferiority of febuxostat, compared with allopurinol, for all-cause death, each individual component of the composite primary outcome – cardiovascular death, hospitalization for heart failure, and hospitalization for new, unstable, or worsening angina.
In contrast, the ITT analysis revealed a “nominally significant increase” in hospitalization for arrhythmia with no evidence of ischemia in the febuxostat group. The 0.583 events per 100 patient-years in this group versus 0.385 events in the allopurinol cohort generated an adjusted HR of 1.51 (95% CI, 1.05-2.17).
In terms of all-cause mortality, 222 participants (7.2%) in the febuxostat group died, compared with 263 people (8.6%) in the allopurinol group.
Adverse events and withdrawals
A total 1,720 participants (57.3%) in the febuxostat group experienced at least one serious adverse event, as did 1,812 participants (59.4%) in the allopurinol group. Less than 1% of serious adverse events in each group were considered treatment-related.
Dr. MacDonald said that 6.2% of the febuxostat patients and 5.5% of the allopurinol group withdrew from the study. “We had pretty good follow-up [94%],” Dr. MacDonald said. “I don’t want to criticize CARES, but 47% did drop out of that study, and they could not follow them anymore.”
Limitations of FAST include its open-label design and lack of a placebo group, although Dr. MacDonald pointed out that a placebo group would have been unethical. Strengths included its large randomized trial design and good external validity, he added. “This is what will happen in clinical practice if you switch people from allopurinol to febuxostat.”
When asked how he would treat people with gout now given the FAST findings, Dr. MacDonald said, “I’m not a rheumatologist, I’m a cardiovascular physician. But I would say from the evidence from the FAST trial, it appears to be safe to give patients febuxostat whether or not they have cardiovascular risk factors or prior cardiovascular disease.”
“The FAST study indicates that febuxostat is similar to allopurinol in terms of cardiovascular events during the treatment period. The strengths of this study are its large sample size, excellent follow-up rate, and the relatively long follow-up time,” session moderator Shervin Assassi, MD, said when asked for comment. Dr. Assassi, director of the division of rheumatology at the University of Texas Health Science Center at Houston, was not involved in the research.
Menarini, Ipsen, and Teijin Pharma funded the study. The University of Dundee receives research funds from Menarini. Dr. MacDonald disclosed that he received speaker or consultant fees from Menarini. Dr. Assassi had no relevant disclosures.
SOURCE: MacDonald T et al. Arthritis Rheumatol. 2020;72(suppl 10). ACR 2020, Abstract L08.
FROM ACR 2020
Great Barrington coauthor backs off strict reliance on herd immunity
A coauthor of the Great Barrington Declaration says that he and colleagues have never argued against using mitigation strategies to keep COVID-19 from spreading, and that critics have mischaracterized the document as a “let it rip” strategy.
Jay Bhattacharya, MD, PhD, a professor and public health policy expert in infectious diseases at Stanford University in California, spoke on a JAMA Livestream debate on November 6. Marc Lipsitch, MD, an epidemiology professor at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, represented the 6900 signatories of the John Snow Memorandum, a rebuttal to the Great Barrington document.
The Great Barrington approach of “Focused Protection” advocates isolation and protection of people who are most vulnerable to COVID-19 while avoiding what they characterize as lockdowns. “The most compassionate approach that balances the risks and benefits of reaching herd immunity, is to allow those who are at minimal risk of death to live their lives normally to build up immunity to the virus through natural infection, while better protecting those who are at highest risk,” the document reads.
The Infectious Diseases Society of America (IDSA) and its HIV Medicine Association denounced the declaration, as reported by Medscape Medical News, and the World Health Organization (WHO) Director General Tedros Adhanom Ghebreyesus called the proposal “unethical.” But the idea has gained some traction at the White House, where Coronavirus Task Force Member and Stanford professor Scott Atlas, MD, has been advising President Donald J. Trump.
On the JAMA debate, Bhattacharya said, “I think all of the mitigation measures are really important,” listing social distancing, hand washing, and masks when distancing is not possible as chief among those strategies for the less vulnerable. “I don’t want to create infections intentionally, but I want us to allow people to go back to their lives as best they can, understanding of the risks they are taking when they do it,” he said, claiming that 99.95% of the population will survive infection.
“The harmful lockdowns are worse for many, many people,” Bhattacharya said.
“I think Jay is moving towards a middle ground which is not really what the Great Barrington Declaration seems to promote,” countered Lipsitch. The declaration does not say use masks or social distance, he said. “It just says we need to go back to a normal life.”
Bhattacharya’s statements to JAMA mean that “maybe we are approaching some common ground,” Lipsitch said.
Definition of a lockdown
Both men were asked to give their definition of a “lockdown.” To Lipsitch, it means people are not allowed out except for essential services and that most businesses are closed, with exceptions for those deemed essential.
Bhattacharya, however, said he views that as a quarantine. Lockdowns “are what we’re currently doing,” he said. Schools, churches, businesses, and arts and culture organizations are shuttered, and “almost every aspect of society is restricted in some way,” Bhattacharya said.
He blamed these lockdowns for most of the excess deaths over and above the COVID-19 deaths and said they had failed to control the pandemic.
Lipsitch said that “it feels to me that Jay is describing as lockdown everything that causes harm, even when it’s not locked down.” He noted that the country was truly closed down for 2 months or so in the spring.
“All of these harms I agree are real,” said Lipsitch. “But they are because the normal life of our society is being interfered with by viral transmission and by people’s inability to live their normal lives.”
Closures and lockdowns are essential to delaying cases and deaths, said Lipsitch. “A case today is worse than a case tomorrow and a lot worse than a case 6 months from now,” he said, noting that a vaccine or improved therapeutics could evolve.
“Delay is not nothing,” Lipsitch added. “It’s actually the goal as I see it, and as the John Snow memo says, we want to keep the virus under control in such a way as that the vulnerable people are not at risk.”
He predicted that cases will continue to grow exponentially because the nation is “not even close to herd immunity.” And, if intensive care units fill up, “there will be a responsive lockdown,” he said, adding that he did not endorse that as a general matter or favor it as a default position.
Bhattacharya claimed that Sweden has tallied only 1800 excess deaths since the pandemic began. “That’s lockdown harm avoided,” he said, advocating a similar strategy for the United States. But, infections have been on the rise in Sweden, and the nation has a higher COVID-19 death rate — with 6000 deaths — than other Nordic countries.
“If we keep this policy of lockdown we will have the same kind of outcomes we’ve already had — high excess deaths and sort of indifferent control of COVID,” Bhattacharya said.
“We’re still going to have misery and death going forward until we reach a point where there’s sufficient immunity either though a vaccine or through natural infection,” he said.
This article first appeared on Medscape.com.
A coauthor of the Great Barrington Declaration says that he and colleagues have never argued against using mitigation strategies to keep COVID-19 from spreading, and that critics have mischaracterized the document as a “let it rip” strategy.
Jay Bhattacharya, MD, PhD, a professor and public health policy expert in infectious diseases at Stanford University in California, spoke on a JAMA Livestream debate on November 6. Marc Lipsitch, MD, an epidemiology professor at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, represented the 6900 signatories of the John Snow Memorandum, a rebuttal to the Great Barrington document.
The Great Barrington approach of “Focused Protection” advocates isolation and protection of people who are most vulnerable to COVID-19 while avoiding what they characterize as lockdowns. “The most compassionate approach that balances the risks and benefits of reaching herd immunity, is to allow those who are at minimal risk of death to live their lives normally to build up immunity to the virus through natural infection, while better protecting those who are at highest risk,” the document reads.
The Infectious Diseases Society of America (IDSA) and its HIV Medicine Association denounced the declaration, as reported by Medscape Medical News, and the World Health Organization (WHO) Director General Tedros Adhanom Ghebreyesus called the proposal “unethical.” But the idea has gained some traction at the White House, where Coronavirus Task Force Member and Stanford professor Scott Atlas, MD, has been advising President Donald J. Trump.
On the JAMA debate, Bhattacharya said, “I think all of the mitigation measures are really important,” listing social distancing, hand washing, and masks when distancing is not possible as chief among those strategies for the less vulnerable. “I don’t want to create infections intentionally, but I want us to allow people to go back to their lives as best they can, understanding of the risks they are taking when they do it,” he said, claiming that 99.95% of the population will survive infection.
“The harmful lockdowns are worse for many, many people,” Bhattacharya said.
“I think Jay is moving towards a middle ground which is not really what the Great Barrington Declaration seems to promote,” countered Lipsitch. The declaration does not say use masks or social distance, he said. “It just says we need to go back to a normal life.”
Bhattacharya’s statements to JAMA mean that “maybe we are approaching some common ground,” Lipsitch said.
Definition of a lockdown
Both men were asked to give their definition of a “lockdown.” To Lipsitch, it means people are not allowed out except for essential services and that most businesses are closed, with exceptions for those deemed essential.
Bhattacharya, however, said he views that as a quarantine. Lockdowns “are what we’re currently doing,” he said. Schools, churches, businesses, and arts and culture organizations are shuttered, and “almost every aspect of society is restricted in some way,” Bhattacharya said.
He blamed these lockdowns for most of the excess deaths over and above the COVID-19 deaths and said they had failed to control the pandemic.
Lipsitch said that “it feels to me that Jay is describing as lockdown everything that causes harm, even when it’s not locked down.” He noted that the country was truly closed down for 2 months or so in the spring.
“All of these harms I agree are real,” said Lipsitch. “But they are because the normal life of our society is being interfered with by viral transmission and by people’s inability to live their normal lives.”
Closures and lockdowns are essential to delaying cases and deaths, said Lipsitch. “A case today is worse than a case tomorrow and a lot worse than a case 6 months from now,” he said, noting that a vaccine or improved therapeutics could evolve.
“Delay is not nothing,” Lipsitch added. “It’s actually the goal as I see it, and as the John Snow memo says, we want to keep the virus under control in such a way as that the vulnerable people are not at risk.”
He predicted that cases will continue to grow exponentially because the nation is “not even close to herd immunity.” And, if intensive care units fill up, “there will be a responsive lockdown,” he said, adding that he did not endorse that as a general matter or favor it as a default position.
Bhattacharya claimed that Sweden has tallied only 1800 excess deaths since the pandemic began. “That’s lockdown harm avoided,” he said, advocating a similar strategy for the United States. But, infections have been on the rise in Sweden, and the nation has a higher COVID-19 death rate — with 6000 deaths — than other Nordic countries.
“If we keep this policy of lockdown we will have the same kind of outcomes we’ve already had — high excess deaths and sort of indifferent control of COVID,” Bhattacharya said.
“We’re still going to have misery and death going forward until we reach a point where there’s sufficient immunity either though a vaccine or through natural infection,” he said.
This article first appeared on Medscape.com.
A coauthor of the Great Barrington Declaration says that he and colleagues have never argued against using mitigation strategies to keep COVID-19 from spreading, and that critics have mischaracterized the document as a “let it rip” strategy.
Jay Bhattacharya, MD, PhD, a professor and public health policy expert in infectious diseases at Stanford University in California, spoke on a JAMA Livestream debate on November 6. Marc Lipsitch, MD, an epidemiology professor at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, represented the 6900 signatories of the John Snow Memorandum, a rebuttal to the Great Barrington document.
The Great Barrington approach of “Focused Protection” advocates isolation and protection of people who are most vulnerable to COVID-19 while avoiding what they characterize as lockdowns. “The most compassionate approach that balances the risks and benefits of reaching herd immunity, is to allow those who are at minimal risk of death to live their lives normally to build up immunity to the virus through natural infection, while better protecting those who are at highest risk,” the document reads.
The Infectious Diseases Society of America (IDSA) and its HIV Medicine Association denounced the declaration, as reported by Medscape Medical News, and the World Health Organization (WHO) Director General Tedros Adhanom Ghebreyesus called the proposal “unethical.” But the idea has gained some traction at the White House, where Coronavirus Task Force Member and Stanford professor Scott Atlas, MD, has been advising President Donald J. Trump.
On the JAMA debate, Bhattacharya said, “I think all of the mitigation measures are really important,” listing social distancing, hand washing, and masks when distancing is not possible as chief among those strategies for the less vulnerable. “I don’t want to create infections intentionally, but I want us to allow people to go back to their lives as best they can, understanding of the risks they are taking when they do it,” he said, claiming that 99.95% of the population will survive infection.
“The harmful lockdowns are worse for many, many people,” Bhattacharya said.
“I think Jay is moving towards a middle ground which is not really what the Great Barrington Declaration seems to promote,” countered Lipsitch. The declaration does not say use masks or social distance, he said. “It just says we need to go back to a normal life.”
Bhattacharya’s statements to JAMA mean that “maybe we are approaching some common ground,” Lipsitch said.
Definition of a lockdown
Both men were asked to give their definition of a “lockdown.” To Lipsitch, it means people are not allowed out except for essential services and that most businesses are closed, with exceptions for those deemed essential.
Bhattacharya, however, said he views that as a quarantine. Lockdowns “are what we’re currently doing,” he said. Schools, churches, businesses, and arts and culture organizations are shuttered, and “almost every aspect of society is restricted in some way,” Bhattacharya said.
He blamed these lockdowns for most of the excess deaths over and above the COVID-19 deaths and said they had failed to control the pandemic.
Lipsitch said that “it feels to me that Jay is describing as lockdown everything that causes harm, even when it’s not locked down.” He noted that the country was truly closed down for 2 months or so in the spring.
“All of these harms I agree are real,” said Lipsitch. “But they are because the normal life of our society is being interfered with by viral transmission and by people’s inability to live their normal lives.”
Closures and lockdowns are essential to delaying cases and deaths, said Lipsitch. “A case today is worse than a case tomorrow and a lot worse than a case 6 months from now,” he said, noting that a vaccine or improved therapeutics could evolve.
“Delay is not nothing,” Lipsitch added. “It’s actually the goal as I see it, and as the John Snow memo says, we want to keep the virus under control in such a way as that the vulnerable people are not at risk.”
He predicted that cases will continue to grow exponentially because the nation is “not even close to herd immunity.” And, if intensive care units fill up, “there will be a responsive lockdown,” he said, adding that he did not endorse that as a general matter or favor it as a default position.
Bhattacharya claimed that Sweden has tallied only 1800 excess deaths since the pandemic began. “That’s lockdown harm avoided,” he said, advocating a similar strategy for the United States. But, infections have been on the rise in Sweden, and the nation has a higher COVID-19 death rate — with 6000 deaths — than other Nordic countries.
“If we keep this policy of lockdown we will have the same kind of outcomes we’ve already had — high excess deaths and sort of indifferent control of COVID,” Bhattacharya said.
“We’re still going to have misery and death going forward until we reach a point where there’s sufficient immunity either though a vaccine or through natural infection,” he said.
This article first appeared on Medscape.com.
Hospitals poised to launch first COVID-19 vaccines in clinicians
At first, when news spread of a 28-year-old doctor on the COVID-19 front lines in Brazil who died after receiving an experimental vaccine, doubts arose about the safety of one of the most promising coronavirus vaccine candidates. But then the story flipped. Although the vaccine maker wouldn’t confirm it, the doctor appeared to have been in the control group and had received a dose of an established meningitis vaccine. The danger came from exposure to the coronavirus itself.
That tragedy underscores the ongoing risk of COVID-19 to healthcare workers, who have been designated by US advisory panels as part of phase 1A – the first to receive doses of any approved vaccine. The Centers for Disease Control and Prevention (CDC) recently reported that 6% of adults hospitalized with COVID from March to May were healthcare workers. The report was based on surveillance data from 13 states. The average age of the patients was 49 years. The agency set a November 15 vaccination “readiness date” for jurisdictions, such as state health departments, even though a vaccine isn’t likely to be authorized by then.
As hospitals scramble to prepare, their watchword is flexibility. They don’t yet know how many initial doses they will get, of which vaccine, or in what time frame. They have a sophisticated infrastructure to deliver flu vaccines each fall, but that framework doesn’t align with the likely scenarios of limited supply, additional reporting requirements, two-dose regimens, and differing storage needs.
“Healthcare organizations have consistently risen to the challenge. I wholeheartedly believe in their potential to do this,” Anna Legreid Dopp, PharmD, senior director of quality improvement and guidelines for the American Society of Health-System Pharmacists, told Medscape Medical News.
Healthcare workers won’t face a vaccine mandate
Even after months of caring for COVID patients, most clinicians remain vulnerable to infection – at work and in their communities. That was what occupational medicine physician Kevin Smith, MD, realized when his health system, Toledo, Ohio–based ProMedica, offered antibody testing to all its 50,000 employees. About 2% of the 6933 tests given came back positive, he says.
Yet many physicians, nurses, and other healthcare workers share the public’s skepticism about the safety and effectiveness of a vaccine that receives swift US Food and Drug Administration (FDA) approval for emergency use. About half of nurses (47%) and almost 1 in 3 physicians (30%) say that they don’t want to get the vaccine when it first becomes available or that they’re unsure about vaccination, according to a Medscape survey.
Because vaccination of healthcare workers will set the stage for public acceptance of the vaccine, hospital epidemiologists are concerned. “We know that there will be some hesitancy in the healthcare workforce, just as there will be in the broader public,” said Marci Drees, MD, chief infection prevention officer and hospital epidemiologist for ChristianaCare in Newark, Delaware, and liaison from the Society for Healthcare Epidemiology of America to the CDC’s Advisory Committee on Immunization Practices.* “I do not think we can expect anyone to be vaccinated if we’re not willing to vaccinate ourselves.”
Healthcare workers are typically required to receive a range of vaccines, including measles, mumps, and rubella (MMR) and pertussis shots. Each year, close to half of US healthcare workers receive a flu vaccine under a workplace mandate. But COVID-19 will be different. The FDA requires anyone given products under an emergency use authorization (EUA) to receive information about risks and benefits and to have the option to decline. Hospitals instead will rely on education as they offer a novel vaccine (or more than one) that will have a minimum effectiveness of 50%.
ProMedica doesn’t require employees to be vaccinated against flu, but employees who decline must get a note from a doctor indicating that they have talked about the risks and benefits of the vaccine. A similar approach may be used with a COVID-19 vaccine, in which employees may be required to learn about the vaccine before they decline, Smith says. “I do believe some people will say they don’t want to get it,” he added.
Like colleagues across the country, Smith is identifying healthcare workers who are involved in direct care of COVID-19 patients and are at highest risk for exposure. Even within the top tier, those performing the riskiest tasks, such as respiratory therapists who provide breathing treatments that spread aerosols and droplets, will be tagged as a priority group, he says. Healthcare workers who spend the most time in proximity to COVID patients, such as nurses in a COVID unit, also are likely to get the first doses, he says.
Swirl, don’t shake, the vaccine
Hospitals are adept at ramping up vaccination campaigns. For example, last year, Vanderbilt University Medical Center, in Nashville, Tennessee, vaccinated nearly 16,000 employees against influenza in their 1-day “Flulapalooza” event. The medical center even earned a Guinness world record in 2011 at the first Flulapalooza for giving the most vaccinations ever within 8 hours.
The 10th anniversary of the event was canceled this year because of COVID restrictions. Instead, nurses, pharmacists, and other clinicians pitched in to vaccinate their coworkers against influenza. Now, plans for COVID-19 vaccination move forward amid uncertainty.
Instead of holding a mass event, “the delivery mechanisms will need to be more targeted and focused,” said Lori Rolando, MD, MPH, director of the Vanderbilt Occupational Health Clinic. In the CDC’s most recent version of its vaccination program “playbook,” the agency recommends giving the vaccines in an area that allows people to remain 6 feet apart and for them to wait for 15 minutes after receiving the shot to make sure they don’t faint, a potential risk common to almost all vaccines.
That’s the easy part. Planning becomes more complex, given the uncertainty as to which vaccines will receive approval and which one a hospital will receive.
If the Pfizer/BioNTech vaccine receives EUA in 2020, about 10 to 20 million doses could be available in November and 20 to 30 million doses in December. The ultracold containers used to ship the vaccines have to be replenished with dry ice within 24 hours of receipt and every 5 days thereafter. Hospitals will need temperature probes to monitor storage in the containers. The five-dose vials can be refrigerated before administering, but only for 5 days. The product must be diluted, and it then must be used within 6 hours.
The Moderna vaccine will be somewhat less plentiful at first. About 10 million doses are expected in November and 15 million doses by the end of December. The 10-dose vials are stored in a freezer. Once they are placed in a refrigerator to thaw, they have to be used within 7 days, and once they’re removed from the refrigerator, they have to be used within 12 hours. The pharmacist or other vaccinator must swirl – but not shake! – the vial before delivering a dose, according to the CDC playbook.
As more information emerges about the vaccines, instructions may change, and Smith is steeled for shifting scenarios. “These are all draft plans. We’re going to modify as we go along,” he says.
The Pfizer vaccine requires a second dose at 21 days, and the Moderna vaccine targets the second dose at 28 days. In addition to using information systems to track vaccinations and any adverse effects, hospitals will give employees a card indicating what vaccine they received, the date it was administered, and the date on which they need to return. (At this point, the time frame for the second dose doesn’t appear to be flexible.)
Regardless of the vaccine, one message stays the same: COVID precautions must continue. That means mask wearing, social distancing, and hand washing – practices that also must be followed by healthcare workers who test positive for naturally acquired antibodies.
“I don’t think anyone expects the COVID vaccine to be 100% effective at preventing COVID,” says Rolando. “So all of the other tools in our toolbox are going to need to be continued to be used as well.”
*Correction, 11/12/20: An earlier version of this article misstated the name of Dr. Drees' institution.
This article first appeared on Medscape.com.
At first, when news spread of a 28-year-old doctor on the COVID-19 front lines in Brazil who died after receiving an experimental vaccine, doubts arose about the safety of one of the most promising coronavirus vaccine candidates. But then the story flipped. Although the vaccine maker wouldn’t confirm it, the doctor appeared to have been in the control group and had received a dose of an established meningitis vaccine. The danger came from exposure to the coronavirus itself.
That tragedy underscores the ongoing risk of COVID-19 to healthcare workers, who have been designated by US advisory panels as part of phase 1A – the first to receive doses of any approved vaccine. The Centers for Disease Control and Prevention (CDC) recently reported that 6% of adults hospitalized with COVID from March to May were healthcare workers. The report was based on surveillance data from 13 states. The average age of the patients was 49 years. The agency set a November 15 vaccination “readiness date” for jurisdictions, such as state health departments, even though a vaccine isn’t likely to be authorized by then.
As hospitals scramble to prepare, their watchword is flexibility. They don’t yet know how many initial doses they will get, of which vaccine, or in what time frame. They have a sophisticated infrastructure to deliver flu vaccines each fall, but that framework doesn’t align with the likely scenarios of limited supply, additional reporting requirements, two-dose regimens, and differing storage needs.
“Healthcare organizations have consistently risen to the challenge. I wholeheartedly believe in their potential to do this,” Anna Legreid Dopp, PharmD, senior director of quality improvement and guidelines for the American Society of Health-System Pharmacists, told Medscape Medical News.
Healthcare workers won’t face a vaccine mandate
Even after months of caring for COVID patients, most clinicians remain vulnerable to infection – at work and in their communities. That was what occupational medicine physician Kevin Smith, MD, realized when his health system, Toledo, Ohio–based ProMedica, offered antibody testing to all its 50,000 employees. About 2% of the 6933 tests given came back positive, he says.
Yet many physicians, nurses, and other healthcare workers share the public’s skepticism about the safety and effectiveness of a vaccine that receives swift US Food and Drug Administration (FDA) approval for emergency use. About half of nurses (47%) and almost 1 in 3 physicians (30%) say that they don’t want to get the vaccine when it first becomes available or that they’re unsure about vaccination, according to a Medscape survey.
Because vaccination of healthcare workers will set the stage for public acceptance of the vaccine, hospital epidemiologists are concerned. “We know that there will be some hesitancy in the healthcare workforce, just as there will be in the broader public,” said Marci Drees, MD, chief infection prevention officer and hospital epidemiologist for ChristianaCare in Newark, Delaware, and liaison from the Society for Healthcare Epidemiology of America to the CDC’s Advisory Committee on Immunization Practices.* “I do not think we can expect anyone to be vaccinated if we’re not willing to vaccinate ourselves.”
Healthcare workers are typically required to receive a range of vaccines, including measles, mumps, and rubella (MMR) and pertussis shots. Each year, close to half of US healthcare workers receive a flu vaccine under a workplace mandate. But COVID-19 will be different. The FDA requires anyone given products under an emergency use authorization (EUA) to receive information about risks and benefits and to have the option to decline. Hospitals instead will rely on education as they offer a novel vaccine (or more than one) that will have a minimum effectiveness of 50%.
ProMedica doesn’t require employees to be vaccinated against flu, but employees who decline must get a note from a doctor indicating that they have talked about the risks and benefits of the vaccine. A similar approach may be used with a COVID-19 vaccine, in which employees may be required to learn about the vaccine before they decline, Smith says. “I do believe some people will say they don’t want to get it,” he added.
Like colleagues across the country, Smith is identifying healthcare workers who are involved in direct care of COVID-19 patients and are at highest risk for exposure. Even within the top tier, those performing the riskiest tasks, such as respiratory therapists who provide breathing treatments that spread aerosols and droplets, will be tagged as a priority group, he says. Healthcare workers who spend the most time in proximity to COVID patients, such as nurses in a COVID unit, also are likely to get the first doses, he says.
Swirl, don’t shake, the vaccine
Hospitals are adept at ramping up vaccination campaigns. For example, last year, Vanderbilt University Medical Center, in Nashville, Tennessee, vaccinated nearly 16,000 employees against influenza in their 1-day “Flulapalooza” event. The medical center even earned a Guinness world record in 2011 at the first Flulapalooza for giving the most vaccinations ever within 8 hours.
The 10th anniversary of the event was canceled this year because of COVID restrictions. Instead, nurses, pharmacists, and other clinicians pitched in to vaccinate their coworkers against influenza. Now, plans for COVID-19 vaccination move forward amid uncertainty.
Instead of holding a mass event, “the delivery mechanisms will need to be more targeted and focused,” said Lori Rolando, MD, MPH, director of the Vanderbilt Occupational Health Clinic. In the CDC’s most recent version of its vaccination program “playbook,” the agency recommends giving the vaccines in an area that allows people to remain 6 feet apart and for them to wait for 15 minutes after receiving the shot to make sure they don’t faint, a potential risk common to almost all vaccines.
That’s the easy part. Planning becomes more complex, given the uncertainty as to which vaccines will receive approval and which one a hospital will receive.
If the Pfizer/BioNTech vaccine receives EUA in 2020, about 10 to 20 million doses could be available in November and 20 to 30 million doses in December. The ultracold containers used to ship the vaccines have to be replenished with dry ice within 24 hours of receipt and every 5 days thereafter. Hospitals will need temperature probes to monitor storage in the containers. The five-dose vials can be refrigerated before administering, but only for 5 days. The product must be diluted, and it then must be used within 6 hours.
The Moderna vaccine will be somewhat less plentiful at first. About 10 million doses are expected in November and 15 million doses by the end of December. The 10-dose vials are stored in a freezer. Once they are placed in a refrigerator to thaw, they have to be used within 7 days, and once they’re removed from the refrigerator, they have to be used within 12 hours. The pharmacist or other vaccinator must swirl – but not shake! – the vial before delivering a dose, according to the CDC playbook.
As more information emerges about the vaccines, instructions may change, and Smith is steeled for shifting scenarios. “These are all draft plans. We’re going to modify as we go along,” he says.
The Pfizer vaccine requires a second dose at 21 days, and the Moderna vaccine targets the second dose at 28 days. In addition to using information systems to track vaccinations and any adverse effects, hospitals will give employees a card indicating what vaccine they received, the date it was administered, and the date on which they need to return. (At this point, the time frame for the second dose doesn’t appear to be flexible.)
Regardless of the vaccine, one message stays the same: COVID precautions must continue. That means mask wearing, social distancing, and hand washing – practices that also must be followed by healthcare workers who test positive for naturally acquired antibodies.
“I don’t think anyone expects the COVID vaccine to be 100% effective at preventing COVID,” says Rolando. “So all of the other tools in our toolbox are going to need to be continued to be used as well.”
*Correction, 11/12/20: An earlier version of this article misstated the name of Dr. Drees' institution.
This article first appeared on Medscape.com.
At first, when news spread of a 28-year-old doctor on the COVID-19 front lines in Brazil who died after receiving an experimental vaccine, doubts arose about the safety of one of the most promising coronavirus vaccine candidates. But then the story flipped. Although the vaccine maker wouldn’t confirm it, the doctor appeared to have been in the control group and had received a dose of an established meningitis vaccine. The danger came from exposure to the coronavirus itself.
That tragedy underscores the ongoing risk of COVID-19 to healthcare workers, who have been designated by US advisory panels as part of phase 1A – the first to receive doses of any approved vaccine. The Centers for Disease Control and Prevention (CDC) recently reported that 6% of adults hospitalized with COVID from March to May were healthcare workers. The report was based on surveillance data from 13 states. The average age of the patients was 49 years. The agency set a November 15 vaccination “readiness date” for jurisdictions, such as state health departments, even though a vaccine isn’t likely to be authorized by then.
As hospitals scramble to prepare, their watchword is flexibility. They don’t yet know how many initial doses they will get, of which vaccine, or in what time frame. They have a sophisticated infrastructure to deliver flu vaccines each fall, but that framework doesn’t align with the likely scenarios of limited supply, additional reporting requirements, two-dose regimens, and differing storage needs.
“Healthcare organizations have consistently risen to the challenge. I wholeheartedly believe in their potential to do this,” Anna Legreid Dopp, PharmD, senior director of quality improvement and guidelines for the American Society of Health-System Pharmacists, told Medscape Medical News.
Healthcare workers won’t face a vaccine mandate
Even after months of caring for COVID patients, most clinicians remain vulnerable to infection – at work and in their communities. That was what occupational medicine physician Kevin Smith, MD, realized when his health system, Toledo, Ohio–based ProMedica, offered antibody testing to all its 50,000 employees. About 2% of the 6933 tests given came back positive, he says.
Yet many physicians, nurses, and other healthcare workers share the public’s skepticism about the safety and effectiveness of a vaccine that receives swift US Food and Drug Administration (FDA) approval for emergency use. About half of nurses (47%) and almost 1 in 3 physicians (30%) say that they don’t want to get the vaccine when it first becomes available or that they’re unsure about vaccination, according to a Medscape survey.
Because vaccination of healthcare workers will set the stage for public acceptance of the vaccine, hospital epidemiologists are concerned. “We know that there will be some hesitancy in the healthcare workforce, just as there will be in the broader public,” said Marci Drees, MD, chief infection prevention officer and hospital epidemiologist for ChristianaCare in Newark, Delaware, and liaison from the Society for Healthcare Epidemiology of America to the CDC’s Advisory Committee on Immunization Practices.* “I do not think we can expect anyone to be vaccinated if we’re not willing to vaccinate ourselves.”
Healthcare workers are typically required to receive a range of vaccines, including measles, mumps, and rubella (MMR) and pertussis shots. Each year, close to half of US healthcare workers receive a flu vaccine under a workplace mandate. But COVID-19 will be different. The FDA requires anyone given products under an emergency use authorization (EUA) to receive information about risks and benefits and to have the option to decline. Hospitals instead will rely on education as they offer a novel vaccine (or more than one) that will have a minimum effectiveness of 50%.
ProMedica doesn’t require employees to be vaccinated against flu, but employees who decline must get a note from a doctor indicating that they have talked about the risks and benefits of the vaccine. A similar approach may be used with a COVID-19 vaccine, in which employees may be required to learn about the vaccine before they decline, Smith says. “I do believe some people will say they don’t want to get it,” he added.
Like colleagues across the country, Smith is identifying healthcare workers who are involved in direct care of COVID-19 patients and are at highest risk for exposure. Even within the top tier, those performing the riskiest tasks, such as respiratory therapists who provide breathing treatments that spread aerosols and droplets, will be tagged as a priority group, he says. Healthcare workers who spend the most time in proximity to COVID patients, such as nurses in a COVID unit, also are likely to get the first doses, he says.
Swirl, don’t shake, the vaccine
Hospitals are adept at ramping up vaccination campaigns. For example, last year, Vanderbilt University Medical Center, in Nashville, Tennessee, vaccinated nearly 16,000 employees against influenza in their 1-day “Flulapalooza” event. The medical center even earned a Guinness world record in 2011 at the first Flulapalooza for giving the most vaccinations ever within 8 hours.
The 10th anniversary of the event was canceled this year because of COVID restrictions. Instead, nurses, pharmacists, and other clinicians pitched in to vaccinate their coworkers against influenza. Now, plans for COVID-19 vaccination move forward amid uncertainty.
Instead of holding a mass event, “the delivery mechanisms will need to be more targeted and focused,” said Lori Rolando, MD, MPH, director of the Vanderbilt Occupational Health Clinic. In the CDC’s most recent version of its vaccination program “playbook,” the agency recommends giving the vaccines in an area that allows people to remain 6 feet apart and for them to wait for 15 minutes after receiving the shot to make sure they don’t faint, a potential risk common to almost all vaccines.
That’s the easy part. Planning becomes more complex, given the uncertainty as to which vaccines will receive approval and which one a hospital will receive.
If the Pfizer/BioNTech vaccine receives EUA in 2020, about 10 to 20 million doses could be available in November and 20 to 30 million doses in December. The ultracold containers used to ship the vaccines have to be replenished with dry ice within 24 hours of receipt and every 5 days thereafter. Hospitals will need temperature probes to monitor storage in the containers. The five-dose vials can be refrigerated before administering, but only for 5 days. The product must be diluted, and it then must be used within 6 hours.
The Moderna vaccine will be somewhat less plentiful at first. About 10 million doses are expected in November and 15 million doses by the end of December. The 10-dose vials are stored in a freezer. Once they are placed in a refrigerator to thaw, they have to be used within 7 days, and once they’re removed from the refrigerator, they have to be used within 12 hours. The pharmacist or other vaccinator must swirl – but not shake! – the vial before delivering a dose, according to the CDC playbook.
As more information emerges about the vaccines, instructions may change, and Smith is steeled for shifting scenarios. “These are all draft plans. We’re going to modify as we go along,” he says.
The Pfizer vaccine requires a second dose at 21 days, and the Moderna vaccine targets the second dose at 28 days. In addition to using information systems to track vaccinations and any adverse effects, hospitals will give employees a card indicating what vaccine they received, the date it was administered, and the date on which they need to return. (At this point, the time frame for the second dose doesn’t appear to be flexible.)
Regardless of the vaccine, one message stays the same: COVID precautions must continue. That means mask wearing, social distancing, and hand washing – practices that also must be followed by healthcare workers who test positive for naturally acquired antibodies.
“I don’t think anyone expects the COVID vaccine to be 100% effective at preventing COVID,” says Rolando. “So all of the other tools in our toolbox are going to need to be continued to be used as well.”
*Correction, 11/12/20: An earlier version of this article misstated the name of Dr. Drees' institution.
This article first appeared on Medscape.com.
United States adds nearly 74,000 more children with COVID-19
The new weekly high for COVID-19 cases in children announced last week has been surpassed already, as the United States experienced almost 74,000 new pediatric cases for the week ending Nov. 5, according to the American Academy of Pediatrics and the Children’s Hospital Association.
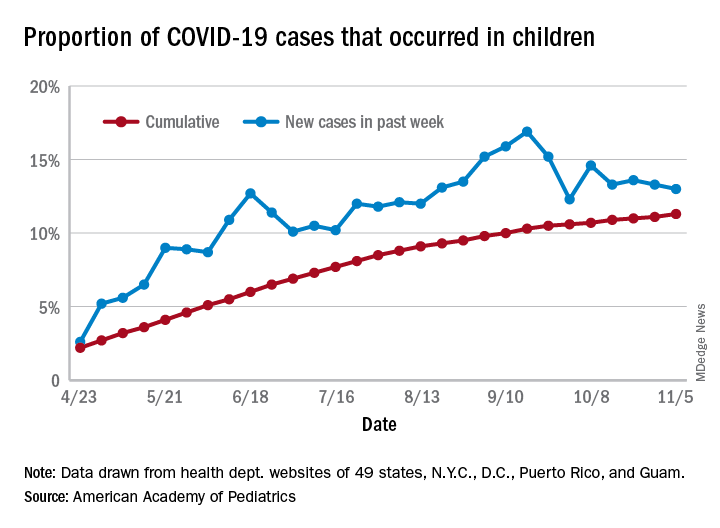
The total number of COVID-19 cases in children is now 927,518 in 49 states, the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly report.
Cumulatively, children represent 11.3% of all COVID-19 cases in those jurisdictions, up from 11.1% a week ago. For just the past week, those 73,883 children represent 13.0% of the 567,672 new cases reported among all ages. That proportion peaked at 16.9% in mid-September, the AAP/CHA data show.
Dropping down to the state level, cumulative proportions as of Nov. 5 range from 5.2% in New Jersey to 23.3% in Wyoming, with 11 other states over 15%. California has had more cases, 100,856, than any other state, and Vermont the fewest at 329, the AAP and CHA said.
The national rate per 100,000 children is now 1,232, up from 1,134 the previous week and more than doubled since mid-August (582.2 per 100,000 on Aug. 20). North Dakota’s rate of 3,990 per 100,000 children is the highest of any state (South Dakota is next at 2,779), while Vermont is again the lowest at 245 per 100,000, based on data collected from state health department websites.
Two COVID-19–related deaths in children were reported during the week ending Nov. 5, bringing the total to 123 but leaving the overall proportion of deaths in children unchanged at 0.06% of all deaths. Texas has reported the most COVID-19 deaths in children with 29, while 15 states have recorded no deaths so far (mortality data in children reported by 42 states and New York City), the AAP and CHA said.
The new weekly high for COVID-19 cases in children announced last week has been surpassed already, as the United States experienced almost 74,000 new pediatric cases for the week ending Nov. 5, according to the American Academy of Pediatrics and the Children’s Hospital Association.
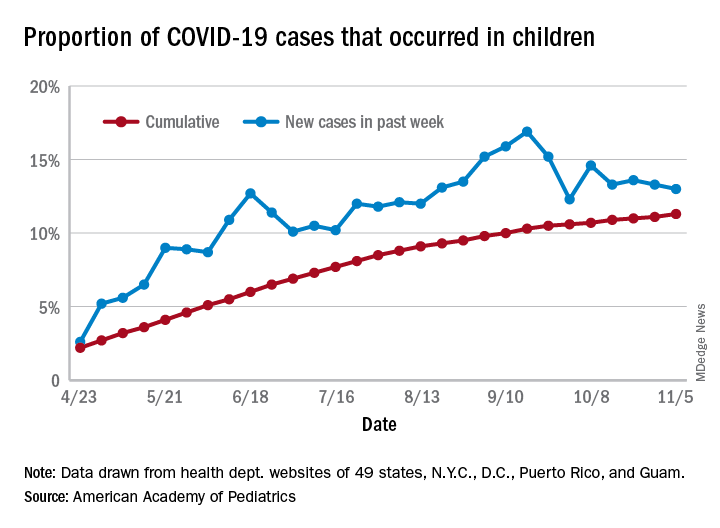
The total number of COVID-19 cases in children is now 927,518 in 49 states, the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly report.
Cumulatively, children represent 11.3% of all COVID-19 cases in those jurisdictions, up from 11.1% a week ago. For just the past week, those 73,883 children represent 13.0% of the 567,672 new cases reported among all ages. That proportion peaked at 16.9% in mid-September, the AAP/CHA data show.
Dropping down to the state level, cumulative proportions as of Nov. 5 range from 5.2% in New Jersey to 23.3% in Wyoming, with 11 other states over 15%. California has had more cases, 100,856, than any other state, and Vermont the fewest at 329, the AAP and CHA said.
The national rate per 100,000 children is now 1,232, up from 1,134 the previous week and more than doubled since mid-August (582.2 per 100,000 on Aug. 20). North Dakota’s rate of 3,990 per 100,000 children is the highest of any state (South Dakota is next at 2,779), while Vermont is again the lowest at 245 per 100,000, based on data collected from state health department websites.
Two COVID-19–related deaths in children were reported during the week ending Nov. 5, bringing the total to 123 but leaving the overall proportion of deaths in children unchanged at 0.06% of all deaths. Texas has reported the most COVID-19 deaths in children with 29, while 15 states have recorded no deaths so far (mortality data in children reported by 42 states and New York City), the AAP and CHA said.
The new weekly high for COVID-19 cases in children announced last week has been surpassed already, as the United States experienced almost 74,000 new pediatric cases for the week ending Nov. 5, according to the American Academy of Pediatrics and the Children’s Hospital Association.
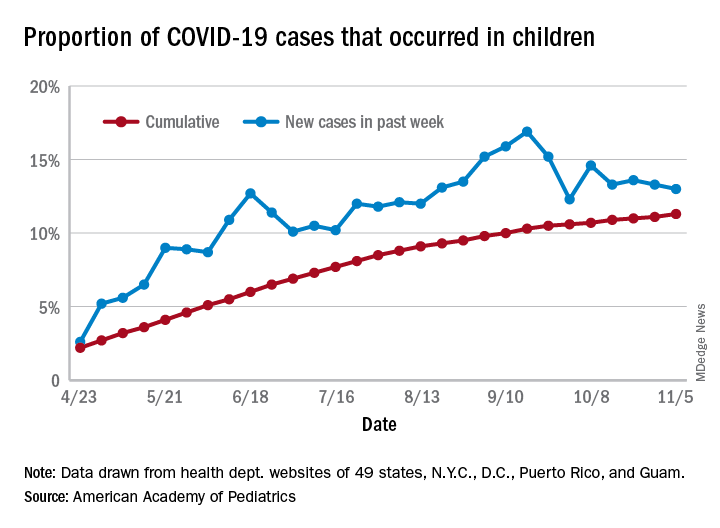
The total number of COVID-19 cases in children is now 927,518 in 49 states, the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly report.
Cumulatively, children represent 11.3% of all COVID-19 cases in those jurisdictions, up from 11.1% a week ago. For just the past week, those 73,883 children represent 13.0% of the 567,672 new cases reported among all ages. That proportion peaked at 16.9% in mid-September, the AAP/CHA data show.
Dropping down to the state level, cumulative proportions as of Nov. 5 range from 5.2% in New Jersey to 23.3% in Wyoming, with 11 other states over 15%. California has had more cases, 100,856, than any other state, and Vermont the fewest at 329, the AAP and CHA said.
The national rate per 100,000 children is now 1,232, up from 1,134 the previous week and more than doubled since mid-August (582.2 per 100,000 on Aug. 20). North Dakota’s rate of 3,990 per 100,000 children is the highest of any state (South Dakota is next at 2,779), while Vermont is again the lowest at 245 per 100,000, based on data collected from state health department websites.
Two COVID-19–related deaths in children were reported during the week ending Nov. 5, bringing the total to 123 but leaving the overall proportion of deaths in children unchanged at 0.06% of all deaths. Texas has reported the most COVID-19 deaths in children with 29, while 15 states have recorded no deaths so far (mortality data in children reported by 42 states and New York City), the AAP and CHA said.
Food insecurity called urgent issue you must address
and advocate on behalf of those experiencing or at risk of food insecurity, according to Kofi Essel, MD, MPH, a pediatrician at Children’s National Hospital in Washington.
More than one in four adults are dealing with food access hardships during the pandemic, Dr. Essel said at the virtual annual meeting of the American Academy of Pediatrics. Food insecurity is often interchangeable with hunger and refers to limited or uncertain availability of foods that are nutritious and safe.
“Food insecurity is as much about the threat of deprivation as it is about deprivation itself: A food-insecure life means a life lived in fear of hunger, and the psychological toll that takes,” according to a 2020 New York Times photo feature on food insecurity by Brenda Ann Kenneally that Dr. Essel quoted.
The lived experience of food insecure households includes food anxiety, a preoccupation with being able to get enough food that takes up cognitive bandwidth and prevents people from being able to focus on other important things. Another feature of food-insecure homes is a monotony of diet, which often involves an increase in caloric density and decrease in nutritional quality. As food insecurity grows more dire, adults’ food intake decreases, and then children’s intake decreases as adults seek out any way to get food, including “socially unacceptable” ways, which can include food pantries and bartering for food.
Food insecurity is associated with a wide range of negative outcomes even after accounting for other confounders, including decreased overall health, mental health, and educational outcomes. It’s also associated with an increase in developmental delays, hospitalizations, iron deficiency, asthma, and birth defects, among other problems. Somewhat paradoxically, it’s associated with both an increase and a decrease in obesity in the research.
Megan J. Gray, MD, MPH, assistant professor of pediatrics and population health at Dell Medical School at the The University of Texas at Austin, attended Dr. Essel’s session because food insecurity during COVID-19 now affects about half her patients, according to screening research she’s conducted.
“I wanted to learn more about the nuances of screening and using language and talking points that are helpful with families and with staff in building a culture of discussing food insecurity in our clinics,” Dr. Gray said in an interview. “What I’ve learned in my clinic is that if we don’t ask about it, families aren’t telling us – food insecurity is hiding in plain sight.”
She particularly appreciated Dr. Essel’s slides on the progression of food insecurity and how they acknowledged the mental health burden of food insecurity among parents.
“Right now during COVID-19, I see more patients I would call ‘socially complex’ rather than ‘medically complex,’ ” she said. “We all need to get a crash course in social work and Dr. Essel’s presentation is a great starting place.”
Screening for food insecurity
Beginning in 2015, an AAP policy statement charged pediatricians to “screen and intervene” with regard to food insecurity and their patients, Dr. Essel said. The statement also called for pediatricians to advocate for programs and policies that end childhood food insecurity.
The policy statement recommended a validated two-question screening tool called the Hunger Vital Sign:
1. “Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
2. “Within the past 12 months, the food that we bought just didn’t last and we didn’t have money to get more.”
But in screening, you need to be conscious of how dignity intersects with food insecurity concerns, Dr. Essel said.
“We need to create dignity for our families,” he said. “We need to create a safe environment for our families and use appropriate tools when necessary to be able to identify families that are struggling with food insecurity.”
That need is seen in research on food screening. The Hunger Vital Signs questions can be asked with a dichotomous variable, as a yes/no question, or on a Likert scale, though the latter is a more complex way to ask.
A 2017 study found, however, that asking with “yes/no” answers missed more than a quarter of at-risk families. In the AAP survey using “yes/no” answers, 31% of families screened positive for being at risk of food insecurity, compared with 46% when the same question was asked on a Likert scale. It seems the ability to answer with “sometimes” feels “safer” than answering “yes,” Dr. Essel said.
Another factor that potentially affects answers is how doctors ask. In a March 2020 study at a single primary care practice, 16% of families screened positive with yes/no responses to a food insecurity screen when the questions were written, compared with 10% of positive screens with verbal responses (P < .001).
Epidemiology of food insecurity
The most updated United States Department of Agriculture report on food insecurity released in September shows the United States finally reached prerecession levels in 2019, with 11% of families designated as “food insecure.” But 2019 data cannot show what has occurred since the pandemic.
Further, the numbers are higher in households with children: Fourteen percent, or one in seven households with children, are experiencing food insecurity. Racial and ethnic disparities in food insecurity have remained consistent over the past 2 decades, with about twice as many Black and Hispanic homes experiencing food insecurity as White homes.
More recent research using Census Household Pulse Surveys has found a tremendous increase in food insecurity for children in 2020. One in three Black children and one in four Hispanic children are food insecure, according to these surveys. The rates are one in six for Asian households and one in ten for White households.
“The disparity is consistent,” Dr. Essel said. “We see what COVID has done. We once may have described it as a great equalizer – everyone is touched in the same way – but the reality is, this is actually a great magnifier. It’s revealing to us and magnifying disparities that have existed for far too long and has really allowed us to see it in a new way.”
A big part of disparities in food insecurity is disparities in wealth, “the safety net or cushion for families when things go wrong,” Dr. Essel said. The median wealth of White Americans in 2016 was $171,000, compared to $20,700 among Latinx Americans and $17,600 among Black Americans, according to the Federal Reserve Board Survey of Consumer Finances.
Food insecurity interventions
Federal nutrition programs – such as Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and school meal programs – are key to addressing food insecurity, Dr. Essel said.
“They have a long track record of rescuing families out of poverty, of rescuing families from food security and improving overall health of families,” he said.
But emergency food relief programs are important as well. Four in 10 families currently coming into food pantries are new recipients, and these resources have seen a 60% increase in clients, he said.
“This is utterly unreasonable for them to be able to manage,” he said. “Food pantries are essential but inadequate to compensate for large numbers of families,” even while they also may be the only option for families unable or unwilling to access federal programs. For example, for every one meal that food banks can provide, SNAP can provide nine meals, Dr. Essel said. Further, during times of economic downtown, every SNAP $1 spent generates $1.50 to $2 in economic activity.
Currently, the Pandemic Electronic Benefit Transfer (P-EBT) program provides benefits to families for school breakfast and lunch and has been extended through December 2021. Another federal pandemic response was to increase SNAP to the maximum household benefit for families, about $646 for a family of four, although 40% of households were already receiving the maximum benefit.
Food insecurity advocacy
You can advocate for any one of multiple pillars when it comes to food insecurity, Dr. Essel said. “Food cannot solve food insecurity by itself,” he said. “We have to think about root causes – systemic causes – and think about unemployment, livable wage, systemic racism, oppression, an inequitable food system. All of these things are pillars that any of you can advocate for when recognizing a family that is struggling with food insecurity.”
He offered several suggestions for advocacy:
- Join your local AAP chapter and prioritize food insecurity.
- Join a local antihunger task force.
- Make your clinical environment as safe as possible for families to respond to questions about food insecurity.
- Know what’s happening in your community immigrant populations.
- Provide up-to-date information to families about eligibility for federal programs.
- Share stories through op-eds and letters to the editor, and by contacting congressional representatives and providing expert testimony to school boards and city councils.
- Educate others about food insecurity through the above channels and on social media.
Jessica Lazerov, MD, a general pediatrician at Children’s National Anacostia and assistant professor of pediatrics at George Washington University, Washington, said the session was fantastic.
“Dr. Essel went beyond the basics of food insecurity, delving into the root causes, potential solutions, and important considerations when screening for food insecurity in practice,” Dr. Lazerov said in an interview. “I enjoyed his focus on advocacy, as well as the fact that he spent a bit of time reviewing how the COVID pandemic has affected food insecurity. I truly felt empowered to take my advocacy efforts a step further as Dr. Essel laid out concrete, actionable next steps, as well as a review of the most relevant and current information about food insecurity.”
Dr. Essel, Dr. Lazerov, and Dr. Gray have no relevant financial disclosures.
and advocate on behalf of those experiencing or at risk of food insecurity, according to Kofi Essel, MD, MPH, a pediatrician at Children’s National Hospital in Washington.
More than one in four adults are dealing with food access hardships during the pandemic, Dr. Essel said at the virtual annual meeting of the American Academy of Pediatrics. Food insecurity is often interchangeable with hunger and refers to limited or uncertain availability of foods that are nutritious and safe.
“Food insecurity is as much about the threat of deprivation as it is about deprivation itself: A food-insecure life means a life lived in fear of hunger, and the psychological toll that takes,” according to a 2020 New York Times photo feature on food insecurity by Brenda Ann Kenneally that Dr. Essel quoted.
The lived experience of food insecure households includes food anxiety, a preoccupation with being able to get enough food that takes up cognitive bandwidth and prevents people from being able to focus on other important things. Another feature of food-insecure homes is a monotony of diet, which often involves an increase in caloric density and decrease in nutritional quality. As food insecurity grows more dire, adults’ food intake decreases, and then children’s intake decreases as adults seek out any way to get food, including “socially unacceptable” ways, which can include food pantries and bartering for food.
Food insecurity is associated with a wide range of negative outcomes even after accounting for other confounders, including decreased overall health, mental health, and educational outcomes. It’s also associated with an increase in developmental delays, hospitalizations, iron deficiency, asthma, and birth defects, among other problems. Somewhat paradoxically, it’s associated with both an increase and a decrease in obesity in the research.
Megan J. Gray, MD, MPH, assistant professor of pediatrics and population health at Dell Medical School at the The University of Texas at Austin, attended Dr. Essel’s session because food insecurity during COVID-19 now affects about half her patients, according to screening research she’s conducted.
“I wanted to learn more about the nuances of screening and using language and talking points that are helpful with families and with staff in building a culture of discussing food insecurity in our clinics,” Dr. Gray said in an interview. “What I’ve learned in my clinic is that if we don’t ask about it, families aren’t telling us – food insecurity is hiding in plain sight.”
She particularly appreciated Dr. Essel’s slides on the progression of food insecurity and how they acknowledged the mental health burden of food insecurity among parents.
“Right now during COVID-19, I see more patients I would call ‘socially complex’ rather than ‘medically complex,’ ” she said. “We all need to get a crash course in social work and Dr. Essel’s presentation is a great starting place.”
Screening for food insecurity
Beginning in 2015, an AAP policy statement charged pediatricians to “screen and intervene” with regard to food insecurity and their patients, Dr. Essel said. The statement also called for pediatricians to advocate for programs and policies that end childhood food insecurity.
The policy statement recommended a validated two-question screening tool called the Hunger Vital Sign:
1. “Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
2. “Within the past 12 months, the food that we bought just didn’t last and we didn’t have money to get more.”
But in screening, you need to be conscious of how dignity intersects with food insecurity concerns, Dr. Essel said.
“We need to create dignity for our families,” he said. “We need to create a safe environment for our families and use appropriate tools when necessary to be able to identify families that are struggling with food insecurity.”
That need is seen in research on food screening. The Hunger Vital Signs questions can be asked with a dichotomous variable, as a yes/no question, or on a Likert scale, though the latter is a more complex way to ask.
A 2017 study found, however, that asking with “yes/no” answers missed more than a quarter of at-risk families. In the AAP survey using “yes/no” answers, 31% of families screened positive for being at risk of food insecurity, compared with 46% when the same question was asked on a Likert scale. It seems the ability to answer with “sometimes” feels “safer” than answering “yes,” Dr. Essel said.
Another factor that potentially affects answers is how doctors ask. In a March 2020 study at a single primary care practice, 16% of families screened positive with yes/no responses to a food insecurity screen when the questions were written, compared with 10% of positive screens with verbal responses (P < .001).
Epidemiology of food insecurity
The most updated United States Department of Agriculture report on food insecurity released in September shows the United States finally reached prerecession levels in 2019, with 11% of families designated as “food insecure.” But 2019 data cannot show what has occurred since the pandemic.
Further, the numbers are higher in households with children: Fourteen percent, or one in seven households with children, are experiencing food insecurity. Racial and ethnic disparities in food insecurity have remained consistent over the past 2 decades, with about twice as many Black and Hispanic homes experiencing food insecurity as White homes.
More recent research using Census Household Pulse Surveys has found a tremendous increase in food insecurity for children in 2020. One in three Black children and one in four Hispanic children are food insecure, according to these surveys. The rates are one in six for Asian households and one in ten for White households.
“The disparity is consistent,” Dr. Essel said. “We see what COVID has done. We once may have described it as a great equalizer – everyone is touched in the same way – but the reality is, this is actually a great magnifier. It’s revealing to us and magnifying disparities that have existed for far too long and has really allowed us to see it in a new way.”
A big part of disparities in food insecurity is disparities in wealth, “the safety net or cushion for families when things go wrong,” Dr. Essel said. The median wealth of White Americans in 2016 was $171,000, compared to $20,700 among Latinx Americans and $17,600 among Black Americans, according to the Federal Reserve Board Survey of Consumer Finances.
Food insecurity interventions
Federal nutrition programs – such as Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and school meal programs – are key to addressing food insecurity, Dr. Essel said.
“They have a long track record of rescuing families out of poverty, of rescuing families from food security and improving overall health of families,” he said.
But emergency food relief programs are important as well. Four in 10 families currently coming into food pantries are new recipients, and these resources have seen a 60% increase in clients, he said.
“This is utterly unreasonable for them to be able to manage,” he said. “Food pantries are essential but inadequate to compensate for large numbers of families,” even while they also may be the only option for families unable or unwilling to access federal programs. For example, for every one meal that food banks can provide, SNAP can provide nine meals, Dr. Essel said. Further, during times of economic downtown, every SNAP $1 spent generates $1.50 to $2 in economic activity.
Currently, the Pandemic Electronic Benefit Transfer (P-EBT) program provides benefits to families for school breakfast and lunch and has been extended through December 2021. Another federal pandemic response was to increase SNAP to the maximum household benefit for families, about $646 for a family of four, although 40% of households were already receiving the maximum benefit.
Food insecurity advocacy
You can advocate for any one of multiple pillars when it comes to food insecurity, Dr. Essel said. “Food cannot solve food insecurity by itself,” he said. “We have to think about root causes – systemic causes – and think about unemployment, livable wage, systemic racism, oppression, an inequitable food system. All of these things are pillars that any of you can advocate for when recognizing a family that is struggling with food insecurity.”
He offered several suggestions for advocacy:
- Join your local AAP chapter and prioritize food insecurity.
- Join a local antihunger task force.
- Make your clinical environment as safe as possible for families to respond to questions about food insecurity.
- Know what’s happening in your community immigrant populations.
- Provide up-to-date information to families about eligibility for federal programs.
- Share stories through op-eds and letters to the editor, and by contacting congressional representatives and providing expert testimony to school boards and city councils.
- Educate others about food insecurity through the above channels and on social media.
Jessica Lazerov, MD, a general pediatrician at Children’s National Anacostia and assistant professor of pediatrics at George Washington University, Washington, said the session was fantastic.
“Dr. Essel went beyond the basics of food insecurity, delving into the root causes, potential solutions, and important considerations when screening for food insecurity in practice,” Dr. Lazerov said in an interview. “I enjoyed his focus on advocacy, as well as the fact that he spent a bit of time reviewing how the COVID pandemic has affected food insecurity. I truly felt empowered to take my advocacy efforts a step further as Dr. Essel laid out concrete, actionable next steps, as well as a review of the most relevant and current information about food insecurity.”
Dr. Essel, Dr. Lazerov, and Dr. Gray have no relevant financial disclosures.
and advocate on behalf of those experiencing or at risk of food insecurity, according to Kofi Essel, MD, MPH, a pediatrician at Children’s National Hospital in Washington.
More than one in four adults are dealing with food access hardships during the pandemic, Dr. Essel said at the virtual annual meeting of the American Academy of Pediatrics. Food insecurity is often interchangeable with hunger and refers to limited or uncertain availability of foods that are nutritious and safe.
“Food insecurity is as much about the threat of deprivation as it is about deprivation itself: A food-insecure life means a life lived in fear of hunger, and the psychological toll that takes,” according to a 2020 New York Times photo feature on food insecurity by Brenda Ann Kenneally that Dr. Essel quoted.
The lived experience of food insecure households includes food anxiety, a preoccupation with being able to get enough food that takes up cognitive bandwidth and prevents people from being able to focus on other important things. Another feature of food-insecure homes is a monotony of diet, which often involves an increase in caloric density and decrease in nutritional quality. As food insecurity grows more dire, adults’ food intake decreases, and then children’s intake decreases as adults seek out any way to get food, including “socially unacceptable” ways, which can include food pantries and bartering for food.
Food insecurity is associated with a wide range of negative outcomes even after accounting for other confounders, including decreased overall health, mental health, and educational outcomes. It’s also associated with an increase in developmental delays, hospitalizations, iron deficiency, asthma, and birth defects, among other problems. Somewhat paradoxically, it’s associated with both an increase and a decrease in obesity in the research.
Megan J. Gray, MD, MPH, assistant professor of pediatrics and population health at Dell Medical School at the The University of Texas at Austin, attended Dr. Essel’s session because food insecurity during COVID-19 now affects about half her patients, according to screening research she’s conducted.
“I wanted to learn more about the nuances of screening and using language and talking points that are helpful with families and with staff in building a culture of discussing food insecurity in our clinics,” Dr. Gray said in an interview. “What I’ve learned in my clinic is that if we don’t ask about it, families aren’t telling us – food insecurity is hiding in plain sight.”
She particularly appreciated Dr. Essel’s slides on the progression of food insecurity and how they acknowledged the mental health burden of food insecurity among parents.
“Right now during COVID-19, I see more patients I would call ‘socially complex’ rather than ‘medically complex,’ ” she said. “We all need to get a crash course in social work and Dr. Essel’s presentation is a great starting place.”
Screening for food insecurity
Beginning in 2015, an AAP policy statement charged pediatricians to “screen and intervene” with regard to food insecurity and their patients, Dr. Essel said. The statement also called for pediatricians to advocate for programs and policies that end childhood food insecurity.
The policy statement recommended a validated two-question screening tool called the Hunger Vital Sign:
1. “Within the past 12 months, we worried whether our food would run out before we got money to buy more.”
2. “Within the past 12 months, the food that we bought just didn’t last and we didn’t have money to get more.”
But in screening, you need to be conscious of how dignity intersects with food insecurity concerns, Dr. Essel said.
“We need to create dignity for our families,” he said. “We need to create a safe environment for our families and use appropriate tools when necessary to be able to identify families that are struggling with food insecurity.”
That need is seen in research on food screening. The Hunger Vital Signs questions can be asked with a dichotomous variable, as a yes/no question, or on a Likert scale, though the latter is a more complex way to ask.
A 2017 study found, however, that asking with “yes/no” answers missed more than a quarter of at-risk families. In the AAP survey using “yes/no” answers, 31% of families screened positive for being at risk of food insecurity, compared with 46% when the same question was asked on a Likert scale. It seems the ability to answer with “sometimes” feels “safer” than answering “yes,” Dr. Essel said.
Another factor that potentially affects answers is how doctors ask. In a March 2020 study at a single primary care practice, 16% of families screened positive with yes/no responses to a food insecurity screen when the questions were written, compared with 10% of positive screens with verbal responses (P < .001).
Epidemiology of food insecurity
The most updated United States Department of Agriculture report on food insecurity released in September shows the United States finally reached prerecession levels in 2019, with 11% of families designated as “food insecure.” But 2019 data cannot show what has occurred since the pandemic.
Further, the numbers are higher in households with children: Fourteen percent, or one in seven households with children, are experiencing food insecurity. Racial and ethnic disparities in food insecurity have remained consistent over the past 2 decades, with about twice as many Black and Hispanic homes experiencing food insecurity as White homes.
More recent research using Census Household Pulse Surveys has found a tremendous increase in food insecurity for children in 2020. One in three Black children and one in four Hispanic children are food insecure, according to these surveys. The rates are one in six for Asian households and one in ten for White households.
“The disparity is consistent,” Dr. Essel said. “We see what COVID has done. We once may have described it as a great equalizer – everyone is touched in the same way – but the reality is, this is actually a great magnifier. It’s revealing to us and magnifying disparities that have existed for far too long and has really allowed us to see it in a new way.”
A big part of disparities in food insecurity is disparities in wealth, “the safety net or cushion for families when things go wrong,” Dr. Essel said. The median wealth of White Americans in 2016 was $171,000, compared to $20,700 among Latinx Americans and $17,600 among Black Americans, according to the Federal Reserve Board Survey of Consumer Finances.
Food insecurity interventions
Federal nutrition programs – such as Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and school meal programs – are key to addressing food insecurity, Dr. Essel said.
“They have a long track record of rescuing families out of poverty, of rescuing families from food security and improving overall health of families,” he said.
But emergency food relief programs are important as well. Four in 10 families currently coming into food pantries are new recipients, and these resources have seen a 60% increase in clients, he said.
“This is utterly unreasonable for them to be able to manage,” he said. “Food pantries are essential but inadequate to compensate for large numbers of families,” even while they also may be the only option for families unable or unwilling to access federal programs. For example, for every one meal that food banks can provide, SNAP can provide nine meals, Dr. Essel said. Further, during times of economic downtown, every SNAP $1 spent generates $1.50 to $2 in economic activity.
Currently, the Pandemic Electronic Benefit Transfer (P-EBT) program provides benefits to families for school breakfast and lunch and has been extended through December 2021. Another federal pandemic response was to increase SNAP to the maximum household benefit for families, about $646 for a family of four, although 40% of households were already receiving the maximum benefit.
Food insecurity advocacy
You can advocate for any one of multiple pillars when it comes to food insecurity, Dr. Essel said. “Food cannot solve food insecurity by itself,” he said. “We have to think about root causes – systemic causes – and think about unemployment, livable wage, systemic racism, oppression, an inequitable food system. All of these things are pillars that any of you can advocate for when recognizing a family that is struggling with food insecurity.”
He offered several suggestions for advocacy:
- Join your local AAP chapter and prioritize food insecurity.
- Join a local antihunger task force.
- Make your clinical environment as safe as possible for families to respond to questions about food insecurity.
- Know what’s happening in your community immigrant populations.
- Provide up-to-date information to families about eligibility for federal programs.
- Share stories through op-eds and letters to the editor, and by contacting congressional representatives and providing expert testimony to school boards and city councils.
- Educate others about food insecurity through the above channels and on social media.
Jessica Lazerov, MD, a general pediatrician at Children’s National Anacostia and assistant professor of pediatrics at George Washington University, Washington, said the session was fantastic.
“Dr. Essel went beyond the basics of food insecurity, delving into the root causes, potential solutions, and important considerations when screening for food insecurity in practice,” Dr. Lazerov said in an interview. “I enjoyed his focus on advocacy, as well as the fact that he spent a bit of time reviewing how the COVID pandemic has affected food insecurity. I truly felt empowered to take my advocacy efforts a step further as Dr. Essel laid out concrete, actionable next steps, as well as a review of the most relevant and current information about food insecurity.”
Dr. Essel, Dr. Lazerov, and Dr. Gray have no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 2020
Proinflammatory dietary pattern linked to higher CV risk
Dietary patterns with higher inflammatory potential were significantly associated with a higher incidence of cardiovascular disease (CVD) and stroke in a new pooled analysis of three prospective cohort studies.
The analysis included 210,145 U.S. women and men followed for up to 32 years in the Nurses’ Health Studies I and II and the Health Professionals Follow-up Study.
After adjustment for use of anti-inflammatory medications and CVD risk factors, those whose dietary pattern ranked in the highest quintile of inflammatory potential had a 38% higher risk of CVD (hazard ratio comparing highest with lowest quintiles, 1.38), a 46% higher risk of coronary heart disease (HR, 1.46), and a 28% higher risk of stroke (HR, 1.28) (all P for trend < .001).
Jun Li, MD, PhD, and colleagues at Harvard School of Public Health and Harvard Medical School, Boston, published the findings of their study in the Nov. 10 issue of the Journal of the American College of Cardiology.
The inflammatory potential of a diet was assessed using a food-based, dietary index called the “empirical dietary inflammatory pattern” or EDIP.
In an interview, Dr. Li explained that the EDIP was developed 4 years ago by many of the same authors involved with this study, including nutrition heavyweights Walter C. Willett, MD, DrPH, and Frank B. Hu, MD, PhD, both from Harvard.
“We summarized all the foods people eat into 39 defined food groups and did a reduced-rank regression analysis that looked at these 39 food groups and three inflammatory markers – interleukin-6, C-reactive protein, and tumor necrosis factor–alpha receptor 2. We found 18 food groups that are most predictive of these biomarkers, and the EDIP was calculated as the weighted sum of these 18 food groups.”
Individuals who had higher intakes of green-leafy vegetables (kale, spinach, arugula), dark-yellow vegetables (pumpkin, yellow peppers, carrots), whole grains, fruits, tea, coffee and wine had lower long-term CVD risk than those with higher intakes of red meat, processed meat, organ meat, refined carbohydrates, and sweetened beverages.
The associations were consistent across cohorts and between sexes and remained significant in multiple sensitivity analysis that adjusted for alcohol consumption, smoking pack-years, use of lipid-lowering and antihypertensive medications, sodium intake, and blood pressure.
In a secondary analysis, diets with higher inflammatory potential were also associated with significantly higher biomarker levels indicative of more systemic, vascular, and metabolic inflammation, as well as less favorable lipid profiles.
“We wanted to be able to provide guidance on dietary patterns and food combinations,” said Dr. Li. “If you tell people to eat more polyunsaturated fats instead of saturated fat or trans fat, most people don’t know what foods are higher and lower in those nutrients. Also, many foods have different nutrients – some of which are good and some of which are bad – so we wanted to help people find the foods with the higher proportion of healthy nutrients rather than point out specific nutrients to avoid.”
Researchers used prospectively gathered data from the Nurses’ Health Studies I and II starting from 1984 and from the Health Professionals Follow-up Study. After excluding participants with missing diet information or previously diagnosed heart disease, stroke or cancer, over 210,000 participants were included in the analysis. Participants completed a survey every 4 years to ascertain dietary intake.
Prevention, not treatment
In an editorial comment, Ramon Estruch, MD, PhD, from the Hospital Clinic in Barcelona, and colleagues suggested that it might be time for better dietary guidelines.
“A better knowledge of health protection provided by different foods and dietary patterns, mainly their anti-inflammatory properties, should provide the basis for designing even healthier dietary patterns to protect against heart disease,” the editorialists wrote.
They added extra-virgin olive oil, fatty fish, and tomatoes to the list of foods with “established anti-inflammatory activity.”
In a comment, Dr. Estruch said the findings of this new study are confirmatory of the PREDIMED trial, which showed a reduction in risk of major CV events in individuals at high cardiovascular risk assigned to an anti-inflammatory Mediterranean diet pattern supplemented with extra-virgin olive oil or nuts as compared with those assigned to a reduced-fat diet.
“The study of Jun Li et al. confirms that an anti-inflammatory diet is useful to prevent cardiovascular events and, more important, that healthy dietary patterns may be even healthier if subjects increase consumption of foods with the highest anti-inflammatory potential,” he said, adding that “mechanistic explanations add plausibility to the results of observational studies.”
Dr. Estruch was the principal investigator of PREDIMED. This trial was originally published in 2013 and then retracted and republished in 2018, with some required corrections, but the results had not materially changed.
Dr. Li is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases and Boston Nutrition Obesity Research Center. Dr. Estruch disclosed no financial relationships relevant to the contents of this article.
A version of this article originally appeared on Medscape.com.
Dietary patterns with higher inflammatory potential were significantly associated with a higher incidence of cardiovascular disease (CVD) and stroke in a new pooled analysis of three prospective cohort studies.
The analysis included 210,145 U.S. women and men followed for up to 32 years in the Nurses’ Health Studies I and II and the Health Professionals Follow-up Study.
After adjustment for use of anti-inflammatory medications and CVD risk factors, those whose dietary pattern ranked in the highest quintile of inflammatory potential had a 38% higher risk of CVD (hazard ratio comparing highest with lowest quintiles, 1.38), a 46% higher risk of coronary heart disease (HR, 1.46), and a 28% higher risk of stroke (HR, 1.28) (all P for trend < .001).
Jun Li, MD, PhD, and colleagues at Harvard School of Public Health and Harvard Medical School, Boston, published the findings of their study in the Nov. 10 issue of the Journal of the American College of Cardiology.
The inflammatory potential of a diet was assessed using a food-based, dietary index called the “empirical dietary inflammatory pattern” or EDIP.
In an interview, Dr. Li explained that the EDIP was developed 4 years ago by many of the same authors involved with this study, including nutrition heavyweights Walter C. Willett, MD, DrPH, and Frank B. Hu, MD, PhD, both from Harvard.
“We summarized all the foods people eat into 39 defined food groups and did a reduced-rank regression analysis that looked at these 39 food groups and three inflammatory markers – interleukin-6, C-reactive protein, and tumor necrosis factor–alpha receptor 2. We found 18 food groups that are most predictive of these biomarkers, and the EDIP was calculated as the weighted sum of these 18 food groups.”
Individuals who had higher intakes of green-leafy vegetables (kale, spinach, arugula), dark-yellow vegetables (pumpkin, yellow peppers, carrots), whole grains, fruits, tea, coffee and wine had lower long-term CVD risk than those with higher intakes of red meat, processed meat, organ meat, refined carbohydrates, and sweetened beverages.
The associations were consistent across cohorts and between sexes and remained significant in multiple sensitivity analysis that adjusted for alcohol consumption, smoking pack-years, use of lipid-lowering and antihypertensive medications, sodium intake, and blood pressure.
In a secondary analysis, diets with higher inflammatory potential were also associated with significantly higher biomarker levels indicative of more systemic, vascular, and metabolic inflammation, as well as less favorable lipid profiles.
“We wanted to be able to provide guidance on dietary patterns and food combinations,” said Dr. Li. “If you tell people to eat more polyunsaturated fats instead of saturated fat or trans fat, most people don’t know what foods are higher and lower in those nutrients. Also, many foods have different nutrients – some of which are good and some of which are bad – so we wanted to help people find the foods with the higher proportion of healthy nutrients rather than point out specific nutrients to avoid.”
Researchers used prospectively gathered data from the Nurses’ Health Studies I and II starting from 1984 and from the Health Professionals Follow-up Study. After excluding participants with missing diet information or previously diagnosed heart disease, stroke or cancer, over 210,000 participants were included in the analysis. Participants completed a survey every 4 years to ascertain dietary intake.
Prevention, not treatment
In an editorial comment, Ramon Estruch, MD, PhD, from the Hospital Clinic in Barcelona, and colleagues suggested that it might be time for better dietary guidelines.
“A better knowledge of health protection provided by different foods and dietary patterns, mainly their anti-inflammatory properties, should provide the basis for designing even healthier dietary patterns to protect against heart disease,” the editorialists wrote.
They added extra-virgin olive oil, fatty fish, and tomatoes to the list of foods with “established anti-inflammatory activity.”
In a comment, Dr. Estruch said the findings of this new study are confirmatory of the PREDIMED trial, which showed a reduction in risk of major CV events in individuals at high cardiovascular risk assigned to an anti-inflammatory Mediterranean diet pattern supplemented with extra-virgin olive oil or nuts as compared with those assigned to a reduced-fat diet.
“The study of Jun Li et al. confirms that an anti-inflammatory diet is useful to prevent cardiovascular events and, more important, that healthy dietary patterns may be even healthier if subjects increase consumption of foods with the highest anti-inflammatory potential,” he said, adding that “mechanistic explanations add plausibility to the results of observational studies.”
Dr. Estruch was the principal investigator of PREDIMED. This trial was originally published in 2013 and then retracted and republished in 2018, with some required corrections, but the results had not materially changed.
Dr. Li is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases and Boston Nutrition Obesity Research Center. Dr. Estruch disclosed no financial relationships relevant to the contents of this article.
A version of this article originally appeared on Medscape.com.
Dietary patterns with higher inflammatory potential were significantly associated with a higher incidence of cardiovascular disease (CVD) and stroke in a new pooled analysis of three prospective cohort studies.
The analysis included 210,145 U.S. women and men followed for up to 32 years in the Nurses’ Health Studies I and II and the Health Professionals Follow-up Study.
After adjustment for use of anti-inflammatory medications and CVD risk factors, those whose dietary pattern ranked in the highest quintile of inflammatory potential had a 38% higher risk of CVD (hazard ratio comparing highest with lowest quintiles, 1.38), a 46% higher risk of coronary heart disease (HR, 1.46), and a 28% higher risk of stroke (HR, 1.28) (all P for trend < .001).
Jun Li, MD, PhD, and colleagues at Harvard School of Public Health and Harvard Medical School, Boston, published the findings of their study in the Nov. 10 issue of the Journal of the American College of Cardiology.
The inflammatory potential of a diet was assessed using a food-based, dietary index called the “empirical dietary inflammatory pattern” or EDIP.
In an interview, Dr. Li explained that the EDIP was developed 4 years ago by many of the same authors involved with this study, including nutrition heavyweights Walter C. Willett, MD, DrPH, and Frank B. Hu, MD, PhD, both from Harvard.
“We summarized all the foods people eat into 39 defined food groups and did a reduced-rank regression analysis that looked at these 39 food groups and three inflammatory markers – interleukin-6, C-reactive protein, and tumor necrosis factor–alpha receptor 2. We found 18 food groups that are most predictive of these biomarkers, and the EDIP was calculated as the weighted sum of these 18 food groups.”
Individuals who had higher intakes of green-leafy vegetables (kale, spinach, arugula), dark-yellow vegetables (pumpkin, yellow peppers, carrots), whole grains, fruits, tea, coffee and wine had lower long-term CVD risk than those with higher intakes of red meat, processed meat, organ meat, refined carbohydrates, and sweetened beverages.
The associations were consistent across cohorts and between sexes and remained significant in multiple sensitivity analysis that adjusted for alcohol consumption, smoking pack-years, use of lipid-lowering and antihypertensive medications, sodium intake, and blood pressure.
In a secondary analysis, diets with higher inflammatory potential were also associated with significantly higher biomarker levels indicative of more systemic, vascular, and metabolic inflammation, as well as less favorable lipid profiles.
“We wanted to be able to provide guidance on dietary patterns and food combinations,” said Dr. Li. “If you tell people to eat more polyunsaturated fats instead of saturated fat or trans fat, most people don’t know what foods are higher and lower in those nutrients. Also, many foods have different nutrients – some of which are good and some of which are bad – so we wanted to help people find the foods with the higher proportion of healthy nutrients rather than point out specific nutrients to avoid.”
Researchers used prospectively gathered data from the Nurses’ Health Studies I and II starting from 1984 and from the Health Professionals Follow-up Study. After excluding participants with missing diet information or previously diagnosed heart disease, stroke or cancer, over 210,000 participants were included in the analysis. Participants completed a survey every 4 years to ascertain dietary intake.
Prevention, not treatment
In an editorial comment, Ramon Estruch, MD, PhD, from the Hospital Clinic in Barcelona, and colleagues suggested that it might be time for better dietary guidelines.
“A better knowledge of health protection provided by different foods and dietary patterns, mainly their anti-inflammatory properties, should provide the basis for designing even healthier dietary patterns to protect against heart disease,” the editorialists wrote.
They added extra-virgin olive oil, fatty fish, and tomatoes to the list of foods with “established anti-inflammatory activity.”
In a comment, Dr. Estruch said the findings of this new study are confirmatory of the PREDIMED trial, which showed a reduction in risk of major CV events in individuals at high cardiovascular risk assigned to an anti-inflammatory Mediterranean diet pattern supplemented with extra-virgin olive oil or nuts as compared with those assigned to a reduced-fat diet.
“The study of Jun Li et al. confirms that an anti-inflammatory diet is useful to prevent cardiovascular events and, more important, that healthy dietary patterns may be even healthier if subjects increase consumption of foods with the highest anti-inflammatory potential,” he said, adding that “mechanistic explanations add plausibility to the results of observational studies.”
Dr. Estruch was the principal investigator of PREDIMED. This trial was originally published in 2013 and then retracted and republished in 2018, with some required corrections, but the results had not materially changed.
Dr. Li is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases and Boston Nutrition Obesity Research Center. Dr. Estruch disclosed no financial relationships relevant to the contents of this article.
A version of this article originally appeared on Medscape.com.







