User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
More doctors used digital tools in 2019
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
The use of digital tools among physicians has markedly risen since 2016, with telehealth visits and remote patient monitoring making the greatest strides in usage, an American Medical Association report shows.
In 2019, 28% of physicians used televisits/virtual visits, up from 14% in 2016, while remote monitoring and management for improved care rose to 22% in 2019, an increase from 13% in 2016, according to the AMA report, released in February 2020. The report, which surveyed 1,359 doctors, includes responses from 672 primary care physicians and 687 specialists.
Remote monitoring for efficiency, meanwhile, grew to 16% in 2019 from 12% in 2016. Remote monitoring for efficiency pertains to smart versions of common clinical devices such as thermometers, blood pressure cuffs, and scales that automatically enter readings in the record. Remote monitoring for improved care refers to mobile applications and devices used for daily measurement of vital signs such as weight, blood pressure, blood glucose.
Adoption of other digital tools by physicians have also grown, including clinical decision support, which climbed to 37% in 2019 from 28% in 2016 and patient engagement tools, which rose to 33% in 2019, up from 26% in 2016. Clinical decision support tools pertain to modules used in conjunction with the electronic health record (EHR), or mobile applications integrated with an EHR that can signify changes in patient data, such as weight gain/loss, or change in blood chemistry. Patient engagement tools, meanwhile, refer to solutions that promote patient wellness and active patient participation in their care.
Tools that encompass use of point of care/workflow enhancement increased to 47% in 2019, from 42% in 2016. This area includes communication and sharing of electronic clinical data to consult with specialists, make referrals and/or transitions of care. Tools that address consumer access to their clinical data, meanwhile, rose to 58% in 2019 from 53% in 2016, the highest adoption rate among the digital health tool categories.
Overall, more physicians see an advantage to digital health solutions than did 3 years ago. More primary care physicians and specialists in 2019 reported a “definite advantage” to digital tools enhancing care of patients than in 2016. Doctors who see no advantage to such tools are trending downward and are concentrated to those age 50 and older, according to the report.
Solo-practice physicians are slowly increasing their use of digital health tools. In 2016, solo physicians reported using an average of 1.5 digital tools, which in 2019 increased to an average of 2.2 digital tools. Small practices with between one and three doctors used an average of 1.4 tools in 2016, which rose to an average of 2.2 tools in 2019, the report found. PCPs used slightly more digital tools, compared with specialists, in both 2016 and 2019.
Female doctors are slightly ahead of their male counterparts when it comes to digital health tools. In 2019, female physicians used an average of 2.6 digital tools, up from 1.9 in 2016. Male doctors used an average of 2.4 tools in 2019, compared with 1.9 tools in 2016.
For the physicians surveyed, the most important factor associated with usage was that digital tools were covered by malpractice insurance, followed by the importance of data privacy/security ensured by the EHR vendor, and that the tools were well integrated with the EHR. Other important factors included that data security was ensured by the practice or hospital, that doctors were reimbursed for their time spent using digital tools, and that the tools were supported by the EHR vendor.
Regarding the top motivator for doctors to use digital tools, 51% of physicians in 2019 said improved efficiency was “very important,” up from 48% in 2016. Other top motivators included that digital tools increased safety, improved diagnostic ability, and addressed physician burnout.
In 2019, the demonstration of safety and efficacy in peer-reviewed publications as it relates to digital tools also grew in importance. Of the physicians surveyed, 36% reported that safety and efficacy demonstrated in peer-reviewed publications was “very important,” an increase from 32% in 2016. Other “very important” factors for physicians are that digital tools used are proven to be as good/superior to traditional care, that they are intuitive/require no special training, that they align with the standard of care, and that their safety and efficacy is validated by the Food and Drug Administration.
“The rise of the digital-native physician will have a profound impact on health care and patient outcomes, and will place digital health technologies under pressure to perform according to higher expectations,” AMA board chair Jesse M. Ehrenfeld, MD, PhD, said in a statement. “The AMA survey provides deep insight into the emerging requirements that physicians expect from digital technologies and sets an industry guidepost for understanding what a growing number of physicians require to adopt new technology.”
The survey was derived from the same physician panel used in 2016, provided by WebMD. For the 2019 survey, the basic 2016 survey was followed in wording and question order, with a few variations to remove some questions no longer relevant. The 2019 sample used careful quotas to ensure a sample composition similar to that of 2016, according to the report.
SOURCE: AMA Digital Health Research: Physicians’ motivations and requirements for adopting digital health – Adoption and attitudinal shifts from 2016 to 2019. American Medical Association. February 2020.
COVID-19 spurs telemedicine, furloughs, retirement
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
The broad use of telemedicine has been a bright spot in the COVID-19 response, but the pandemic is also creating significant disruption as some physicians are furloughed and others consider practice changes.
A recent survey of physicians conducted by Merritt Hawkins and The Physicians Foundation examined how physicians are being affected by and responding to the pandemic. The findings are based on completed surveys from 842 physicians. About one-third of respondents are primary care physicians, while two-thirds are surgical, medical, and diagnostic specialists and subspecialists.
The survey shines a light on the rapid adoption of telemedicine, with 48% of physicians respondents reporting that they are now treating patients through telemedicine.
“I think that is purely explainable on the situation that COVID has led to with the desire to see patients remotely, still take care of them, and the fact that at the federal level this was recognized and doctors are being compensated for seeing patients remotely,” Gary Price, MD, a plastic surgeon and president of The Physicians Foundation, said in an interview.
“The Foundation does a study of the nation’s physicians every other year and in 2018, when we asked the same question, only 18% of physicians were using some form of telemedicine,” he added.
And Dr. Price said he thinks the shift to telemedicine is here to stay.
“I think that will be a lasting effect of the pandemic,” he said. “More physicians and more patients will be using telemedicine approaches, I think, from here on out. We will see a shift that persists. I think that’s a good thing. Physicians like it. Patients like it. It won’t replace all in-person visits, certainly, but there are a number of health care visits that could be taken care of quite well with a virtual visit and it saves the patients travel time, time away from work, and I think it can make the physicians’ practice more efficient as well.”
The key to sustainability, he said, will be that private insurers and the Centers for Medicare & Medicaid Services continue to pay for it.
“I think we will have had a good demonstration, not only that it can work, but that it does work and that it can be accomplished without any diminishment in the quality of care that’s delivered,” he said.
But the recent survey also identified a number of employment issues that have arisen during the COVID-19 pandemic. Overall, 18% of respondents who were treating COVID-19 patients and 30% of those not treating COVID-19 patients reported that they had been furloughed or experienced a pay cut. Among respondents, just 38.5% reported that they are seeing COVID-19 patients.
“It is unprecedented to my knowledge in the physician employment sphere,” Dr. Price said. “That was the most surprising thing to me. I think you might be able to explain that by the increasing number of physicians who are employees now of larger health systems and the fact that a big portion of those health systems too, in normal times, involves care that right now no one is able to get to or even wants to be seen for because of the risk, of course, of COVID-19.”
The survey also revealed that some respondents had or were planning a change in practice because of COVID-19: 14% said they had or would seek a different practice, 6% reported they had or would find a job without patient care, 7% said they had or would close their practice temporarily, 5% reported that they had or would retire, and 4% said they had or would leave private practice and seek employment at a hospital.
“The survey represents how they are feeling at the time and it doesn’t mean they will necessarily do that, but if even a portion of doctors did that all at once, we would really aggravate an access problem and what we know is a worsening physician shortage in the country,” he said. “So we are very concerned about that.”
Dr. Price also predicted there would be increased consolidation within the health care system as more smaller, independent practices feel the financial stress of the pandemic.
“I hope that I am wrong about that,” he said. “I think smaller practices offer a very cost-effective solution for high-quality care, and their competition in the marketplace for health care is a good and healthy thing.”
Will COVID-19 finally trigger action on health disparities?
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Because of stark racial disparities in COVID-19 infection and mortality, the pandemic is being called a “sentinel” and “bellwether” event that should push the United States to finally come to grips with disparities in health care.
When it comes to COVID-19, the pattern is “irrefutable”: Blacks in the United States are being infected with SARS-CoV-2 and are dying of COVID-19 at higher rates than whites, Clyde W. Yancy, MD, Northwestern University, Chicago, wrote in a viewpoint article published online April 15 in JAMA.
According to one recent survey, he noted, the infection rate is threefold higher and the death rate is sixfold higher in predominantly black counties in the United States relative to predominantly white counties.
A sixfold increase in the rate of death for blacks due to a now ubiquitous virus should be deemed “unconscionable” and a moment of “ethical reckoning,” Dr. Yancy wrote.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
The COVID-19 pandemic may be the “bellwether” event that the United States has needed to fully address disparities in health care, Dr. Yancy said.
“Public health is complicated and social reengineering is complex, but change of this magnitude does not happen without a new resolve,” he concluded. “The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event. Certainly, within the broad and powerful economic and legislative engines of the U.S., there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain.”
The question is, he asks, will the nation finally “think differently, and, as has been done in response to other major diseases, declare that a civil society will no longer accept disproportionate suffering?”
Keith C. Ferdinand, MD, Tulane University, New Orleans, doesn’t think so.
In a related editorial published online April 17 in the Journal of the American College of Cardiology, he points out that the 1985 Heckler Report, from the Department of Health and Human Services, documented higher racial/ethnic mortality rates and the need to correct them. This was followed in 2002 by a report from the Institute of Medicine called Unequal Treatment that also underscored health disparities.
Despite some progress, the goal of reducing and eventually eliminating racial/ethnic disparities has not been realized, Dr. Ferdinand said. “I think baked into the consciousness of the American psyche is that there are some people who have and some who have not,” he said in an interview.
“To some extent, some societies at some point become immune. We would not like to think that America, with its sense of egalitarianism, would get to that point, but maybe we have,” said Dr. Ferdinand.
A ‘sentinel event’
He points out that black people are not genetically or biologically predisposed to COVID-19 but are socially prone to coronavirus exposure and are more likely to have comorbid conditions, such as hypertension, diabetes, obesity, and heart disease, that fuel complications.
The “tragic” higher COVID-19 mortality among African Americans and other racial/ethnic minorities confirms “inadequate” efforts on the part of society to eliminate disparities in cardiovascular disease (CVD) and is a “sentinel event,” Dr. Ferdinand wrote.
A sentinel event, as defined by the Joint Commission, is an unexpected occurrence that leads to death or serious physical or psychological injury or the risk thereof, he explained.
“Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate [African American] COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated,” Dr. Ferdinand concluded.
Dr. Yancy and Dr. Ferdinand have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Consensus recommendations on AMI management during COVID-19
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
A consensus statement from the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) outlines recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic.
The statement was published in the Journal of the American College of Cardiology.
During the COVID-19 pandemic, percutaneous coronary intervention (PCI) remains the standard of care for patients with ST-segment elevation MI (STEMI) at PCI-capable hospitals when it can be provided in a timely fashion in a dedicated cardiac catheterization laboratory with an expert care team wearing personal protection equipment (PPE), the writing group advised.
“A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option,” they said.
SCAI President Ehtisham Mahmud, MD, of the University of California, San Diego, and the writing group also said that clinicians should recognize that cardiovascular manifestations of COVID-19 are “complex” in patients presenting with AMI, myocarditis simulating a STEMI, stress cardiomyopathy, nonischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury.
A “broad differential diagnosis for ST elevations (including COVID-associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy,” they advised.
In the absence of hemodynamic instability or ongoing ischemic symptoms, non-STEMI patients with known or suspected COVID-19 are best managed with an initial medical stabilization strategy, the group said.
They also said it is “imperative that health care workers use appropriate PPE for all invasive procedures during this pandemic” and that new rapid COVID-19 testing be “expeditiously” disseminated to all hospitals that manage patients with AMI.
Major challenges are that the prevalence of the COVID-19 in the United States remains unknown and there is the risk for asymptomatic spread.
The writing group said it’s “critical” to “inform the public that we can minimize exposure to the coronavirus so they can continue to call the Emergency Medical System (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants.”
This research had no commercial funding. Dr. Mahmud reported receiving clinical trial research support from Corindus, Abbott Vascular, and CSI; consulting with Medtronic; and consulting and equity with Abiomed. A complete list of author disclosures is included with the original article.
A version of this article originally appeared on Medscape.com.
CMS suspends advance payment program to clinicians for COVID-19 relief
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
The Centers for Medicare & Medicaid Services will suspend its Medicare advance payment program for clinicians and is reevaluating how much to pay to hospitals going forward through particular COVID-19 relief initiatives. CMS announced the changes on April 26. Physicians and others who use the accelerated and advance Medicare payments program repay these advances, and they are typically given 1 year or less to repay the funding.
CMS said in a news release it will not accept new applications for the advanced Medicare payment, and it will be reevaluating all pending and new applications “in light of historical direct payments made available through the Department of Health & Human Services’ (HHS) Provider Relief Fund.”
The advance Medicare payment program predates COVID-19, although it previously was used on a much smaller scale. In the past 5 years, CMS approved about 100 total requests for advanced Medicare payment, with most being tied to natural disasters such as hurricanes.
CMS said it has approved, since March, more than 21,000 applications for advanced Medicare payment, totaling $59.6 billion, for hospitals and other organizations that bill its Part A program. In addition, CMS approved almost 24,000 applications for its Part B program, advancing $40.4 billion for physicians, other clinicians, and medical equipment suppliers.
CMS noted that Congress also has provided $175 billion in aid for the medical community that clinicians and medical organizations would not need to repay. The Coronavirus Aid, Relief, and Economic Security (CARES) Act enacted in March included $100 billion, and the Paycheck Protection Program and Health Care Enhancement Act, enacted March 24, includes another $75 billion.
A version of this article was originally published on Medscape.com.
Changing habits, sleep patterns, and home duties during the pandemic
Like you, I’m not sure when this weird Twilight Zone world of coronavirus will end. Even when it does, its effects will be with us for a long time to come.
But in some ways, they may be for the better. Hopefully some of these changes will stick. Like every new situation, I try to take away something of value from it.
As pithy as it sounds, I used to obsess (sort of) over the daily mail delivery. My secretary would check it mid-afternoon, and if it wasn’t there either she or I would run down again before we left. If it still wasn’t there I’d swing by the box when I came in early the next morning. On Saturdays, I’d sometimes drive in just to get the mail.
There certainly are things that come in that are important: payments, bills, medical records, legal cases to review ... but realistically a lot of mail is junk. Office-supply catalogs, CME or pharmaceutical ads, credit card promotions, and so on.
Now? I just don’t care. If I go several days without seeing patients at the office, the mail is at the back of my mind. It’s in a locked box and isn’t going anywhere. Why worry about it? Next time I’m there I can deal with it. It’s not worth thinking about, it’s just the mail. It’s not worth a special trip.
Sleep is another thing. For years my internal alarm has had me up around 4:00 a.m. (I don’t even bother to set one on my phone), and I get up and go in to get started on the day.
Now? I don’t think I’ve ever slept this much. If I have to go to my office, I’m much less rushed. Many days I don’t even have to do that. I walk down to my home office, call up my charts and the day’s video appointment schedule, and we’re off. Granted, once things return to speed, this will probably be back to normal.
My kids are all home from college, so I have the extra time at home to enjoy them and our dogs. My wife, an oncology infusion nurse, doesn’t get home until 6:00 each night, so for now I’ve become a stay-at-home dad. This is actually something I’ve always liked (in high school, I was voted “most likely to to be a house husband”). So I do the laundry and am in charge of dinner each night. I’m enjoying the last, as I get to pick things out, go through recipes, and cook. I won’t say I’m a great cook, but I’m learning and having fun. As strange as it sounds, being a house husband has always been something I wanted to do, so I’m appreciating the opportunity while it lasts.
I think all of us have come to accept this strange pause button that’s been pushed, and I’ll try to learn what I can from it and take that with me as I move forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Like you, I’m not sure when this weird Twilight Zone world of coronavirus will end. Even when it does, its effects will be with us for a long time to come.
But in some ways, they may be for the better. Hopefully some of these changes will stick. Like every new situation, I try to take away something of value from it.
As pithy as it sounds, I used to obsess (sort of) over the daily mail delivery. My secretary would check it mid-afternoon, and if it wasn’t there either she or I would run down again before we left. If it still wasn’t there I’d swing by the box when I came in early the next morning. On Saturdays, I’d sometimes drive in just to get the mail.
There certainly are things that come in that are important: payments, bills, medical records, legal cases to review ... but realistically a lot of mail is junk. Office-supply catalogs, CME or pharmaceutical ads, credit card promotions, and so on.
Now? I just don’t care. If I go several days without seeing patients at the office, the mail is at the back of my mind. It’s in a locked box and isn’t going anywhere. Why worry about it? Next time I’m there I can deal with it. It’s not worth thinking about, it’s just the mail. It’s not worth a special trip.
Sleep is another thing. For years my internal alarm has had me up around 4:00 a.m. (I don’t even bother to set one on my phone), and I get up and go in to get started on the day.
Now? I don’t think I’ve ever slept this much. If I have to go to my office, I’m much less rushed. Many days I don’t even have to do that. I walk down to my home office, call up my charts and the day’s video appointment schedule, and we’re off. Granted, once things return to speed, this will probably be back to normal.
My kids are all home from college, so I have the extra time at home to enjoy them and our dogs. My wife, an oncology infusion nurse, doesn’t get home until 6:00 each night, so for now I’ve become a stay-at-home dad. This is actually something I’ve always liked (in high school, I was voted “most likely to to be a house husband”). So I do the laundry and am in charge of dinner each night. I’m enjoying the last, as I get to pick things out, go through recipes, and cook. I won’t say I’m a great cook, but I’m learning and having fun. As strange as it sounds, being a house husband has always been something I wanted to do, so I’m appreciating the opportunity while it lasts.
I think all of us have come to accept this strange pause button that’s been pushed, and I’ll try to learn what I can from it and take that with me as I move forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Like you, I’m not sure when this weird Twilight Zone world of coronavirus will end. Even when it does, its effects will be with us for a long time to come.
But in some ways, they may be for the better. Hopefully some of these changes will stick. Like every new situation, I try to take away something of value from it.
As pithy as it sounds, I used to obsess (sort of) over the daily mail delivery. My secretary would check it mid-afternoon, and if it wasn’t there either she or I would run down again before we left. If it still wasn’t there I’d swing by the box when I came in early the next morning. On Saturdays, I’d sometimes drive in just to get the mail.
There certainly are things that come in that are important: payments, bills, medical records, legal cases to review ... but realistically a lot of mail is junk. Office-supply catalogs, CME or pharmaceutical ads, credit card promotions, and so on.
Now? I just don’t care. If I go several days without seeing patients at the office, the mail is at the back of my mind. It’s in a locked box and isn’t going anywhere. Why worry about it? Next time I’m there I can deal with it. It’s not worth thinking about, it’s just the mail. It’s not worth a special trip.
Sleep is another thing. For years my internal alarm has had me up around 4:00 a.m. (I don’t even bother to set one on my phone), and I get up and go in to get started on the day.
Now? I don’t think I’ve ever slept this much. If I have to go to my office, I’m much less rushed. Many days I don’t even have to do that. I walk down to my home office, call up my charts and the day’s video appointment schedule, and we’re off. Granted, once things return to speed, this will probably be back to normal.
My kids are all home from college, so I have the extra time at home to enjoy them and our dogs. My wife, an oncology infusion nurse, doesn’t get home until 6:00 each night, so for now I’ve become a stay-at-home dad. This is actually something I’ve always liked (in high school, I was voted “most likely to to be a house husband”). So I do the laundry and am in charge of dinner each night. I’m enjoying the last, as I get to pick things out, go through recipes, and cook. I won’t say I’m a great cook, but I’m learning and having fun. As strange as it sounds, being a house husband has always been something I wanted to do, so I’m appreciating the opportunity while it lasts.
I think all of us have come to accept this strange pause button that’s been pushed, and I’ll try to learn what I can from it and take that with me as I move forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Rural ICU capacity could be strained by COVID-19
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
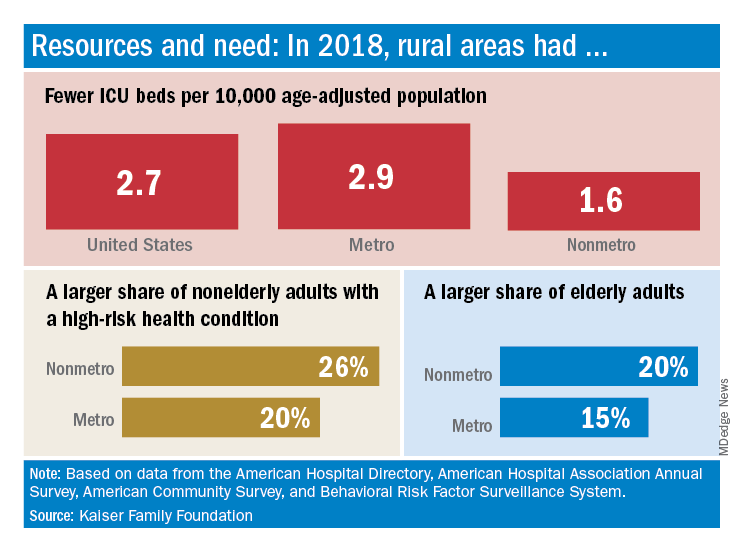
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
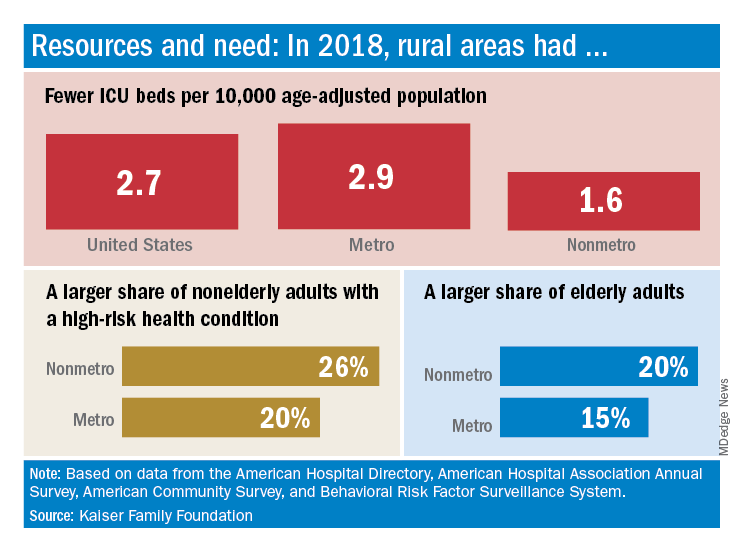
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
The nonmetropolitan, largely rural, areas of the United States have fewer ICU beds than do urban areas, but their populations may be at higher risk for COVID-19 complications, according to the Kaiser Family Foundation.
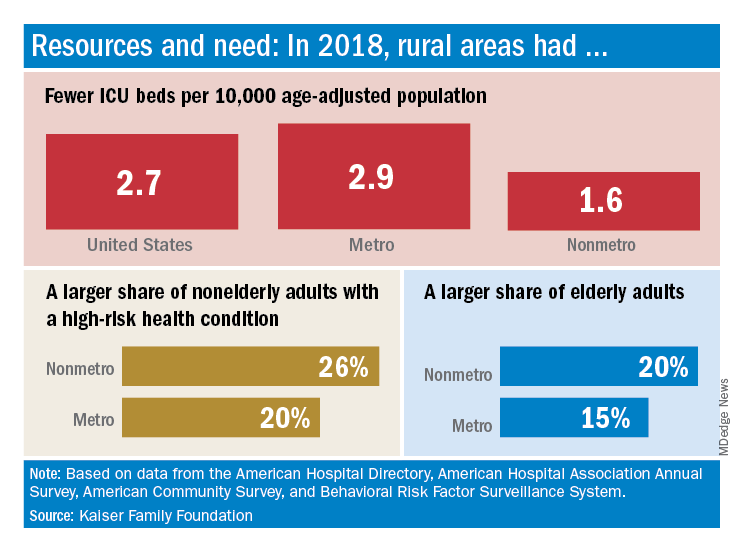
In 2018, the United States had 2.7 ICU beds per 10,000 age-adjusted population, but that number drops to 1.6 beds per 10,000 in nonmetro America and rises to 2.9 per 10,000 in metro areas. Counts for all hospital beds were much closer: 21.6 per 10,000 (rural) and 23.9 per 10,000 (urban), Kaiser investigators reported.
“The novel coronavirus was slower to spread to rural areas in the U.S., but that appears to be changing, with new outbreaks becoming evident in less densely populated parts of the country,” Kendal Orgera and associates said in a recent analysis.
Those rural areas have COVID-19 issues beyond ICU bed counts. Populations in nonmetro areas are less healthy – 26% of adults under age 65 years had a preexisting medical condition in 2018, compared with 20% in metro areas – and older – 20% of people are 65 and older, versus 15% in metro areas, they said.
“If coronavirus continues to spread in rural communities across the U.S., it is possible many [nonmetro] areas will face shortages of ICU beds with limited options to adapt. Patients in rural areas experiencing more severe illnesses may be transferred to hospitals with greater capacity, but if nearby urban areas are also overwhelmed, transfer may not be an option,” Ms. Orgera and associates wrote.
They defined nonmetro counties as those with rural towns of fewer than 2,500 people and/or “urban areas with populations ranging from 2,500 to 49,999 that are not part of larger labor market areas.” The Kaiser analysis involved 2018 data from the American Hospital Association, American Hospital Directory, American Community Survey, and the Behavioral Risk Factor Surveillance System.
Seniors with COVID-19 show unusual symptoms, doctors say
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
complicating efforts to ensure they get timely and appropriate treatment, according to physicians.
COVID-19 is typically signaled by three symptoms: a fever, an insistent cough, and shortness of breath. But older adults – the age group most at risk of severe complications or death from this condition – may have none of these characteristics.
Instead, seniors may seem “off” – not acting like themselves – early on after being infected by the coronavirus. They may sleep more than usual or stop eating. They may seem unusually apathetic or confused, losing orientation to their surroundings. They may become dizzy and fall. Sometimes, seniors stop speaking or simply collapse.
“With a lot of conditions, older adults don’t present in a typical way, and we’re seeing that with COVID-19 as well,” said Camille Vaughan, MD, section chief of geriatrics and gerontology at Emory University, Atlanta.
The reason has to do with how older bodies respond to illness and infection.
At advanced ages, “someone’s immune response may be blunted and their ability to regulate temperature may be altered,” said Dr. Joseph Ouslander, a professor of geriatric medicine at Florida Atlantic University in Boca Raton.
“Underlying chronic illnesses can mask or interfere with signs of infection,” he said. “Some older people, whether from age-related changes or previous neurologic issues such as a stroke, may have altered cough reflexes. Others with cognitive impairment may not be able to communicate their symptoms.”
Recognizing danger signs is important: If early signs of COVID-19 are missed, seniors may deteriorate before getting needed care. And people may go in and out of their homes without adequate protective measures, risking the spread of infection.
Quratulain Syed, MD, an Atlanta geriatrician, describes a man in his 80s whom she treated in mid-March. Over a period of days, this patient, who had heart disease, diabetes and moderate cognitive impairment, stopped walking and became incontinent and profoundly lethargic. But he didn’t have a fever or a cough. His only respiratory symptom: sneezing off and on.
The man’s elderly spouse called 911 twice. Both times, paramedics checked his vital signs and declared he was OK. After another worried call from the overwhelmed spouse, Dr. Syed insisted the patient be taken to the hospital, where he tested positive for COVID-19.
“I was quite concerned about the paramedics and health aides who’d been in the house and who hadn’t used PPE [personal protective equipment],” Dr. Syed said.
Dr. Sam Torbati, medical director of the emergency department at Cedars-Sinai Medical Center, Los Angeles, describes treating seniors who initially appear to be trauma patients but are found to have COVID-19.
“They get weak and dehydrated,” he said, “and when they stand to walk, they collapse and injure themselves badly.”
Dr. Torbati has seen older adults who are profoundly disoriented and unable to speak and who appear at first to have suffered strokes.
“When we test them, we discover that what’s producing these changes is a central nervous system effect of coronavirus,” he said.
Laura Perry, MD, of the University of California, San Francisco, saw a patient like this several weeks ago. The woman, in her 80s, had what seemed to be a cold before becoming very confused. In the hospital, she couldn’t identify where she was or stay awake during an examination. Dr. Perry diagnosed hypoactive delirium, an altered mental state in which people become inactive and drowsy. The patient tested positive for coronavirus and is still in the ICU.
Anthony Perry, MD, of the department of geriatric medicine at Rush University Medical Center in Chicago, tells of an 81-year-old woman with nausea, vomiting, and diarrhea who tested positive for COVID-19 in the emergency room. After receiving intravenous fluids, oxygen, and medication for her intestinal upset, she returned home after 2 days and is doing well.
Another 80-year-old Rush patient with similar symptoms – nausea and vomiting, but no cough, fever, or shortness of breath – is in intensive care after getting a positive COVID-19 test and due to be put on a ventilator. The difference? This patient is frail with “a lot of cardiovascular disease,” Dr. Perry said. Other than that, it’s not yet clear why some older patients do well while others do not.
So far, reports of cases like these have been anecdotal. But a few physicians are trying to gather more systematic information.
In Switzerland, Sylvain Nguyen, MD, a geriatrician at the University of Lausanne Hospital Center, put together a list of typical and atypical symptoms in older COVID-19 patients for a paper to be published in the Revue Médicale Suisse. Included on the atypical list are changes in a patient’s usual status, delirium, falls, fatigue, lethargy, low blood pressure, painful swallowing, fainting, diarrhea, nausea, vomiting, abdominal pain, and the loss of smell and taste.
Data come from hospitals and nursing homes in Switzerland, Italy, and France, Dr. Nguyen said in an email.
On the front lines, physicians need to make sure they carefully assess an older patient’s symptoms.
“While we have to have a high suspicion of COVID-19 because it’s so dangerous in the older population, there are many other things to consider,” said Kathleen Unroe, MD, a geriatrician at Indiana University, Indianapolis.
Seniors may also do poorly because their routines have changed. In nursing homes and most assisted living centers, activities have stopped and “residents are going to get weaker and more deconditioned because they’re not walking to and from the dining hall,” she said.
At home, isolated seniors may not be getting as much help with medication management or other essential needs from family members who are keeping their distance, other experts suggested. Or they may have become apathetic or depressed.
“I’d want to know ‘What’s the potential this person has had an exposure [to the coronavirus], especially in the last 2 weeks?’ ” said Dr. Vaughan of Emory. “Do they have home health personnel coming in? Have they gotten together with other family members? Are chronic conditions being controlled? Is there another diagnosis that seems more likely?”
“Someone may be just having a bad day. But if they’re not themselves for a couple of days, absolutely reach out to a primary care doctor or a local health system hotline to see if they meet the threshold for [coronavirus] testing,” Dr. Vaughan advised. “Be persistent. If you get a ‘no’ the first time and things aren’t improving, call back and ask again.”
Kaiser Health News (khn.org) is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Undeterred during COVID-19, hospital chaplains transform delivery of spiritual care
The first time that the Rev. Michael Mercier, BCC (a board-certified chaplain), provided spiritual care for a patient hospitalized with COVID-19 in March, he found himself engaged in a bit of soul-searching. Even though he donned a mask, gloves, and gown, he could get no closer than the hospital room doorway to interact with the patient because of infection-control measures.

“It went against all my natural instincts and my experience as a chaplain,” said Rev. Mercier, who serves as director of spiritual care for Rhode Island Hospital, Hasbro Children’s Hospital, Miriam Hospital, and Newport Hospital, which are operated by Lifespan, Rhode Island’s largest health system. “The first instinct is to be physically present in the room with the person who’s dying, to have the family gathered around the bedside.”
Prior to standing in the doorway that day, he’d been on the phone with family members, “just listening to their fear and their anxiety that they could not be with their loved one when their loved one was dying,” he said. “I validated their feelings. I also urged them to work with me and the nurse to bring a phone into the room, hold it to the patient’s ear, and they were able to say their goodbyes and how much they loved the person.”
The patient was a devout Roman Catholic, he added, and the family requested that the Prayer of Commendation and the Apostolic Pardon be performed. Rev. Mercier arranged for a Catholic priest to carry out this request. “The nurse told the patient what was going on, and the priest offered the prayers and the rituals from the doorway,” Rev. Mercier said. “It was a surreal experience. For me, it was almost entirely phone based, and it was mostly with the family because the patient couldn’t talk too much.”
To add to the sense of detachment in a situation like that, doctors, nurses, and chaplains caring for COVID-19 patients are wearing masks and face shields, and sometimes the sickest patients are intubated, which can complicate efforts to communicate. “I’m surprised at how we find the mask as somewhat of a barrier,” said Carolanne B. Hauck, BCC, director of chaplaincy care & education and volunteer services at Lancaster (Pa.) General Hospital, which is part of the Penn Medicine system. “By that I mean, often for us, sitting at the bedside and really being able to see someone’s face and have them see our face – with our masks, that’s just not happening. We’re also having briefer visits when we’re visiting with COVID patients.”
COVID-19 may have quarantined some traditional ways of providing spiritual care, but hospital chaplains are relying on technology more than ever in their efforts to meet the needs of patients and their families, including the use of iPads, FaceTime, and video conferencing programs like Zoom and BlueJeans.
“We’ve used Zoom to talk with family members that live out of state,” Rev. Mercier said. “Most of the time, I get an invitation to join a Zoom meeting, but now I need to become proficient in utilizing Zoom to set up those end-of-life family meetings. There’s a lot of learning on the fly, how to use these technologies in a way that’s helpful for everybody. That’s the biggest thing I’m learning: Connection is connection during this time of high stress and anxiety, and we just have to get creative.”
Despite the “disembodied” nature of technology, patients and their families have expressed gratitude to chaplains for their efforts to facilitate connections between loved ones and to be “a guide on the side,” as Mary Wetsch-Johnson, BCC, put it. She recalled one phone conversation with the daughter of a man with COVID-19 who was placed on comfort measures. “She said her dad was like the dad on the TV series Father Knows Best, just a kind-hearted, loving, wonderful man,” said Ms. Wetsch-Johnson, a chaplain at CHI Franciscan Health, which operates 10 acute-care hospitals in the Puget Sound region of Washington state. “She was able to describe him in a way that I felt like I knew him. She talked about the discord they had in their family and how they’re processing through that, and about her own personal journey with grief and loss. She then asked me for information about funeral homes, and I provided her with information. At the end of it, she said, ‘I did not know that I needed you today, but you are exactly what I needed.’ ”
Hospital chaplains may be using smartphones and other gadgets to communicate with patients and their families more than they did in the pre-COVID-19 world, but their basic job has not changed, said Rabbi Neal J. Loevinger, BCC, director of spiritual care services at Vassar Brothers Medical Center in Poughkeepsie, N.Y., part of a seven-hospital system operated by Nuvance Health. “We offer the hope of a caring presence,” said Rabbi Loevinger, who is also a member of the board of directors for Neshama: Association of Jewish Chaplains. “If someone is in a hole, our job is to climb down into the hole with them and say, ‘We’re going to get out of this hole together.’ We can’t promise that someone’s going to get better. We can’t promise that everything’s going to be all right. What we can promise is that we will not abandon you. We can promise that there will be someone accompanying you in any way we can through this crisis.”
Ms. Hauck remembered a phone conversation with the granddaughter of a patient hospitalized with COVID-19 who was nearing the end of her life. The granddaughter told her a story about how her grandmother and her best friend made a pact with each other that, when one was dying, the other would come to her side and pray the Rosary with her. “The granddaughter got tearful and said, ‘That can’t happen now,’ ” said Ms. Hauck, who oversees a staff of 9 chaplains and 10 per diem chaplains. “I made a promise that I would do my best to be at the bedside and pray the Rosary with her grandmother.”
The nurses were aware of the request, and about a day later, Ms. Hauck received a call at 1 a.m., indicating that the patient was close to dying. She drove to Lancaster General, put on her personal protective equipment, made it to the patient’s bedside, and began to pray the Rosary with her, with a nurse in the room. “The nurse said to me, ‘Carolanne, all of her stats are going up,’ and the patient actually became a little more alert,” she recalled. “We talked a little bit, and I asked, ‘Would you like to pray the Rosary now?’ She shook her head yes, and said, ‘Hail Mary, full of grace ...’ and those were the last words that she spoke. I finished the prayers for her, and then she died. It was very meaningful knowing that I could honor that wish for her, but more importantly, that I could do that for the family, who otherwise would have been at her side saying the Rosary with her. We have a recognition of how hard it is to leave someone at the hospital and not be at their bedside.”

Hospital chaplains are also supporting interdisciplinary teams of physicians, nurses, and other staff, as they navigate the provision of care in the wake of a pandemic. “They are under a great deal of stress – not only from being at work but with all the role changes that have happened in their home life,” Ms. Wetsch-Johnson said. “Some of them now are being the teacher at home and having to care for children. They have a lot that they come in with. My job is to help them so that they can go do their job. Regularly what I do is check in with the units and ask, ‘How are you doing today? What’s going on for you?’ Because people need to know that someone’s there to be with them and walk with them and listen to them.”
In the spirit of being present for their staff, she and her colleagues established “respite rooms” at CHI Franciscan hospitals, where workers can decompress and get recentered before returning to work. “We usually have water and snacks in there for them, and some type of soothing music,” Ms. Wetsch-Johnson said. “There is also literature on breathing exercises and stretching exercises. We’re also inviting people to write little notes of hope and gratitude, and they’re putting those up for each other. It’s important that we keep supporting them as they support the patients. Personally, I also round with our physicians, because they carry a lot with them, just as much as any other staff. I check in with dietary and environmental services. Everybody’s giving in their own unique way; that helps this whole health care system keep going.”
On any given day, it’s not uncommon for hospital staff members to spontaneously pull aside chaplains to vent, pray, or just to talk. “They process their own fears and anxieties about working in this kind of environment,” Rev. Mercier said. “They’re scared for themselves. They think, ‘Could I get the virus? Could I spread the virus to my family?’ Or, they may express the care and concern they have for their patients. Oftentimes, it’s a mixture of both. Those spontaneous conversations are often the most powerful.”
Ms. Hauck noted that some nurses and clinicians at Lancaster General Hospital “are doing work they may have not done before,” she said. “Some of them are experiencing death for the first time, so we help them to navigate that. One of the best things we can do is hear the anxiety they have or the sadness they have when a patient dies. Also, maybe the frustration that they couldn’t do more in some cases and helping them to see that sometimes their best is good enough.”
She recalled one younger patient with COVID-19 who fell seriously ill. “It was really affecting a lot of people on the unit because of the patient’s age,” she said. “When we saw that the patient was getting better and would be discharged, there was such a sense of relief. I’m not sure that patient will ever understand how that helped us. It was comforting to us to know that people are getting better. It is something we celebrate.”
As chaplains adjust to their “new normal,” carving out time for self-care is key. Ms. Hauck and her staff periodically meet on Zoom with a psychotherapist “who understands what we do, asks us really good questions, and reminds us to take care of ourselves,” she said. “Personally, I’m making sure I get my exercise in, I pack a healthy lunch. We do check in with each other. Part of our handoff at every shift provides for an opportunity to debrief about how your day was.”
Rev. Mercier’s self check-in includes deep-breathing meditation and reciting certain prayers throughout the day. “The deep breathing helps me center and refocus with my body, while the prayers remind me of my connection to the Divine,” he said. “It also reminds me that in the midst of the fear and the anxiety, I fear for myself. It’s hard not to be concerned that I could be infected. I have a family at home and could spread this to them. The prayer practices are a reminder to me that it’s okay to feel those fears and anxieties. Sometimes the spiritual practice helps me find that place of acceptance. That enables me to keep moving forward.”
Ms. Wetsch-Johnson described the sense of upendedness caused by the COVID-19 pandemic as a “ripple in the water that’s going to have long-lasting effects on the delivery of health care. People are taking the time to listen to one another. I’ve seen people in all departments be more compassionate with one another. I’ve seen managers go out of their way to make sure their staff are deeply cared for. I think that will have a ripple effect. That’s my hope, that we will continue to be more compassionate, more loving, and more understanding.”
Rabbi Loevinger hopes that even the most reticent physicians remember that chaplains serve as their advocate, too, especially during times of crisis. “This has been a time of unprecedented ethical wrestling in our hospitals, where there’s been a real concern that doctors, nurses, and respiratory therapists are going to be faced with morally distressing situations regarding insufficient PPE, or insufficient ventilator or dialysis machine supply to support everybody that needs to be supported,” he said. “Chaplains are a key part of the process of making ethical decisions, but also supporting physicians who are in distress over [being in] situations they never had imagined. Physicians don’t like to talk about the fact that a lot of the decisions they make are really heartbreaking. But if chaplains understand anything, it’s that being brokenhearted is part of the human condition, and that we can be part of the answer for keeping physicians morally and spiritually grounded in their work. We always invite that conversation.”
For Rev. Mercier, serving in a time of crisis reminds him of the importance of providing care as a team, “not just for patients and families, but for one another,” he said. “One of the lessons we can learn is, how can we build that connection with one another, to support and care for one another? How can we make sure that no one feels alone while working in the hospital?”
He draws inspiration from a saying credited to St. John of the Cross, which reads, “I saw the river through which every soul must pass, and the name of that river is suffering. I saw the boat that carries each soul across that river, and the name of that boat is love.”
“It’s that image that’s sticking with me, not just for myself as a chaplain but for all of my colleagues in the hospital,” said Rev. Mercier, who also pastors Tabernacle Baptist Church in Hope, R.I. “We’re in that river with the patients right now, suffering, and we’re doing our best to help them get to the other side – whatever the other side may look like.”
Correction, 4/30/20: An earlier version of the caption for the photo with Mary Wetsch-Johnson misstated the location. The photo was taken outside St. Elizabeth Hospital in Enumclaw, Wash.
The first time that the Rev. Michael Mercier, BCC (a board-certified chaplain), provided spiritual care for a patient hospitalized with COVID-19 in March, he found himself engaged in a bit of soul-searching. Even though he donned a mask, gloves, and gown, he could get no closer than the hospital room doorway to interact with the patient because of infection-control measures.

“It went against all my natural instincts and my experience as a chaplain,” said Rev. Mercier, who serves as director of spiritual care for Rhode Island Hospital, Hasbro Children’s Hospital, Miriam Hospital, and Newport Hospital, which are operated by Lifespan, Rhode Island’s largest health system. “The first instinct is to be physically present in the room with the person who’s dying, to have the family gathered around the bedside.”
Prior to standing in the doorway that day, he’d been on the phone with family members, “just listening to their fear and their anxiety that they could not be with their loved one when their loved one was dying,” he said. “I validated their feelings. I also urged them to work with me and the nurse to bring a phone into the room, hold it to the patient’s ear, and they were able to say their goodbyes and how much they loved the person.”
The patient was a devout Roman Catholic, he added, and the family requested that the Prayer of Commendation and the Apostolic Pardon be performed. Rev. Mercier arranged for a Catholic priest to carry out this request. “The nurse told the patient what was going on, and the priest offered the prayers and the rituals from the doorway,” Rev. Mercier said. “It was a surreal experience. For me, it was almost entirely phone based, and it was mostly with the family because the patient couldn’t talk too much.”
To add to the sense of detachment in a situation like that, doctors, nurses, and chaplains caring for COVID-19 patients are wearing masks and face shields, and sometimes the sickest patients are intubated, which can complicate efforts to communicate. “I’m surprised at how we find the mask as somewhat of a barrier,” said Carolanne B. Hauck, BCC, director of chaplaincy care & education and volunteer services at Lancaster (Pa.) General Hospital, which is part of the Penn Medicine system. “By that I mean, often for us, sitting at the bedside and really being able to see someone’s face and have them see our face – with our masks, that’s just not happening. We’re also having briefer visits when we’re visiting with COVID patients.”
COVID-19 may have quarantined some traditional ways of providing spiritual care, but hospital chaplains are relying on technology more than ever in their efforts to meet the needs of patients and their families, including the use of iPads, FaceTime, and video conferencing programs like Zoom and BlueJeans.
“We’ve used Zoom to talk with family members that live out of state,” Rev. Mercier said. “Most of the time, I get an invitation to join a Zoom meeting, but now I need to become proficient in utilizing Zoom to set up those end-of-life family meetings. There’s a lot of learning on the fly, how to use these technologies in a way that’s helpful for everybody. That’s the biggest thing I’m learning: Connection is connection during this time of high stress and anxiety, and we just have to get creative.”
Despite the “disembodied” nature of technology, patients and their families have expressed gratitude to chaplains for their efforts to facilitate connections between loved ones and to be “a guide on the side,” as Mary Wetsch-Johnson, BCC, put it. She recalled one phone conversation with the daughter of a man with COVID-19 who was placed on comfort measures. “She said her dad was like the dad on the TV series Father Knows Best, just a kind-hearted, loving, wonderful man,” said Ms. Wetsch-Johnson, a chaplain at CHI Franciscan Health, which operates 10 acute-care hospitals in the Puget Sound region of Washington state. “She was able to describe him in a way that I felt like I knew him. She talked about the discord they had in their family and how they’re processing through that, and about her own personal journey with grief and loss. She then asked me for information about funeral homes, and I provided her with information. At the end of it, she said, ‘I did not know that I needed you today, but you are exactly what I needed.’ ”
Hospital chaplains may be using smartphones and other gadgets to communicate with patients and their families more than they did in the pre-COVID-19 world, but their basic job has not changed, said Rabbi Neal J. Loevinger, BCC, director of spiritual care services at Vassar Brothers Medical Center in Poughkeepsie, N.Y., part of a seven-hospital system operated by Nuvance Health. “We offer the hope of a caring presence,” said Rabbi Loevinger, who is also a member of the board of directors for Neshama: Association of Jewish Chaplains. “If someone is in a hole, our job is to climb down into the hole with them and say, ‘We’re going to get out of this hole together.’ We can’t promise that someone’s going to get better. We can’t promise that everything’s going to be all right. What we can promise is that we will not abandon you. We can promise that there will be someone accompanying you in any way we can through this crisis.”
Ms. Hauck remembered a phone conversation with the granddaughter of a patient hospitalized with COVID-19 who was nearing the end of her life. The granddaughter told her a story about how her grandmother and her best friend made a pact with each other that, when one was dying, the other would come to her side and pray the Rosary with her. “The granddaughter got tearful and said, ‘That can’t happen now,’ ” said Ms. Hauck, who oversees a staff of 9 chaplains and 10 per diem chaplains. “I made a promise that I would do my best to be at the bedside and pray the Rosary with her grandmother.”
The nurses were aware of the request, and about a day later, Ms. Hauck received a call at 1 a.m., indicating that the patient was close to dying. She drove to Lancaster General, put on her personal protective equipment, made it to the patient’s bedside, and began to pray the Rosary with her, with a nurse in the room. “The nurse said to me, ‘Carolanne, all of her stats are going up,’ and the patient actually became a little more alert,” she recalled. “We talked a little bit, and I asked, ‘Would you like to pray the Rosary now?’ She shook her head yes, and said, ‘Hail Mary, full of grace ...’ and those were the last words that she spoke. I finished the prayers for her, and then she died. It was very meaningful knowing that I could honor that wish for her, but more importantly, that I could do that for the family, who otherwise would have been at her side saying the Rosary with her. We have a recognition of how hard it is to leave someone at the hospital and not be at their bedside.”

Hospital chaplains are also supporting interdisciplinary teams of physicians, nurses, and other staff, as they navigate the provision of care in the wake of a pandemic. “They are under a great deal of stress – not only from being at work but with all the role changes that have happened in their home life,” Ms. Wetsch-Johnson said. “Some of them now are being the teacher at home and having to care for children. They have a lot that they come in with. My job is to help them so that they can go do their job. Regularly what I do is check in with the units and ask, ‘How are you doing today? What’s going on for you?’ Because people need to know that someone’s there to be with them and walk with them and listen to them.”
In the spirit of being present for their staff, she and her colleagues established “respite rooms” at CHI Franciscan hospitals, where workers can decompress and get recentered before returning to work. “We usually have water and snacks in there for them, and some type of soothing music,” Ms. Wetsch-Johnson said. “There is also literature on breathing exercises and stretching exercises. We’re also inviting people to write little notes of hope and gratitude, and they’re putting those up for each other. It’s important that we keep supporting them as they support the patients. Personally, I also round with our physicians, because they carry a lot with them, just as much as any other staff. I check in with dietary and environmental services. Everybody’s giving in their own unique way; that helps this whole health care system keep going.”
On any given day, it’s not uncommon for hospital staff members to spontaneously pull aside chaplains to vent, pray, or just to talk. “They process their own fears and anxieties about working in this kind of environment,” Rev. Mercier said. “They’re scared for themselves. They think, ‘Could I get the virus? Could I spread the virus to my family?’ Or, they may express the care and concern they have for their patients. Oftentimes, it’s a mixture of both. Those spontaneous conversations are often the most powerful.”
Ms. Hauck noted that some nurses and clinicians at Lancaster General Hospital “are doing work they may have not done before,” she said. “Some of them are experiencing death for the first time, so we help them to navigate that. One of the best things we can do is hear the anxiety they have or the sadness they have when a patient dies. Also, maybe the frustration that they couldn’t do more in some cases and helping them to see that sometimes their best is good enough.”
She recalled one younger patient with COVID-19 who fell seriously ill. “It was really affecting a lot of people on the unit because of the patient’s age,” she said. “When we saw that the patient was getting better and would be discharged, there was such a sense of relief. I’m not sure that patient will ever understand how that helped us. It was comforting to us to know that people are getting better. It is something we celebrate.”
As chaplains adjust to their “new normal,” carving out time for self-care is key. Ms. Hauck and her staff periodically meet on Zoom with a psychotherapist “who understands what we do, asks us really good questions, and reminds us to take care of ourselves,” she said. “Personally, I’m making sure I get my exercise in, I pack a healthy lunch. We do check in with each other. Part of our handoff at every shift provides for an opportunity to debrief about how your day was.”
Rev. Mercier’s self check-in includes deep-breathing meditation and reciting certain prayers throughout the day. “The deep breathing helps me center and refocus with my body, while the prayers remind me of my connection to the Divine,” he said. “It also reminds me that in the midst of the fear and the anxiety, I fear for myself. It’s hard not to be concerned that I could be infected. I have a family at home and could spread this to them. The prayer practices are a reminder to me that it’s okay to feel those fears and anxieties. Sometimes the spiritual practice helps me find that place of acceptance. That enables me to keep moving forward.”
Ms. Wetsch-Johnson described the sense of upendedness caused by the COVID-19 pandemic as a “ripple in the water that’s going to have long-lasting effects on the delivery of health care. People are taking the time to listen to one another. I’ve seen people in all departments be more compassionate with one another. I’ve seen managers go out of their way to make sure their staff are deeply cared for. I think that will have a ripple effect. That’s my hope, that we will continue to be more compassionate, more loving, and more understanding.”
Rabbi Loevinger hopes that even the most reticent physicians remember that chaplains serve as their advocate, too, especially during times of crisis. “This has been a time of unprecedented ethical wrestling in our hospitals, where there’s been a real concern that doctors, nurses, and respiratory therapists are going to be faced with morally distressing situations regarding insufficient PPE, or insufficient ventilator or dialysis machine supply to support everybody that needs to be supported,” he said. “Chaplains are a key part of the process of making ethical decisions, but also supporting physicians who are in distress over [being in] situations they never had imagined. Physicians don’t like to talk about the fact that a lot of the decisions they make are really heartbreaking. But if chaplains understand anything, it’s that being brokenhearted is part of the human condition, and that we can be part of the answer for keeping physicians morally and spiritually grounded in their work. We always invite that conversation.”
For Rev. Mercier, serving in a time of crisis reminds him of the importance of providing care as a team, “not just for patients and families, but for one another,” he said. “One of the lessons we can learn is, how can we build that connection with one another, to support and care for one another? How can we make sure that no one feels alone while working in the hospital?”
He draws inspiration from a saying credited to St. John of the Cross, which reads, “I saw the river through which every soul must pass, and the name of that river is suffering. I saw the boat that carries each soul across that river, and the name of that boat is love.”
“It’s that image that’s sticking with me, not just for myself as a chaplain but for all of my colleagues in the hospital,” said Rev. Mercier, who also pastors Tabernacle Baptist Church in Hope, R.I. “We’re in that river with the patients right now, suffering, and we’re doing our best to help them get to the other side – whatever the other side may look like.”
Correction, 4/30/20: An earlier version of the caption for the photo with Mary Wetsch-Johnson misstated the location. The photo was taken outside St. Elizabeth Hospital in Enumclaw, Wash.
The first time that the Rev. Michael Mercier, BCC (a board-certified chaplain), provided spiritual care for a patient hospitalized with COVID-19 in March, he found himself engaged in a bit of soul-searching. Even though he donned a mask, gloves, and gown, he could get no closer than the hospital room doorway to interact with the patient because of infection-control measures.

“It went against all my natural instincts and my experience as a chaplain,” said Rev. Mercier, who serves as director of spiritual care for Rhode Island Hospital, Hasbro Children’s Hospital, Miriam Hospital, and Newport Hospital, which are operated by Lifespan, Rhode Island’s largest health system. “The first instinct is to be physically present in the room with the person who’s dying, to have the family gathered around the bedside.”
Prior to standing in the doorway that day, he’d been on the phone with family members, “just listening to their fear and their anxiety that they could not be with their loved one when their loved one was dying,” he said. “I validated their feelings. I also urged them to work with me and the nurse to bring a phone into the room, hold it to the patient’s ear, and they were able to say their goodbyes and how much they loved the person.”
The patient was a devout Roman Catholic, he added, and the family requested that the Prayer of Commendation and the Apostolic Pardon be performed. Rev. Mercier arranged for a Catholic priest to carry out this request. “The nurse told the patient what was going on, and the priest offered the prayers and the rituals from the doorway,” Rev. Mercier said. “It was a surreal experience. For me, it was almost entirely phone based, and it was mostly with the family because the patient couldn’t talk too much.”
To add to the sense of detachment in a situation like that, doctors, nurses, and chaplains caring for COVID-19 patients are wearing masks and face shields, and sometimes the sickest patients are intubated, which can complicate efforts to communicate. “I’m surprised at how we find the mask as somewhat of a barrier,” said Carolanne B. Hauck, BCC, director of chaplaincy care & education and volunteer services at Lancaster (Pa.) General Hospital, which is part of the Penn Medicine system. “By that I mean, often for us, sitting at the bedside and really being able to see someone’s face and have them see our face – with our masks, that’s just not happening. We’re also having briefer visits when we’re visiting with COVID patients.”
COVID-19 may have quarantined some traditional ways of providing spiritual care, but hospital chaplains are relying on technology more than ever in their efforts to meet the needs of patients and their families, including the use of iPads, FaceTime, and video conferencing programs like Zoom and BlueJeans.
“We’ve used Zoom to talk with family members that live out of state,” Rev. Mercier said. “Most of the time, I get an invitation to join a Zoom meeting, but now I need to become proficient in utilizing Zoom to set up those end-of-life family meetings. There’s a lot of learning on the fly, how to use these technologies in a way that’s helpful for everybody. That’s the biggest thing I’m learning: Connection is connection during this time of high stress and anxiety, and we just have to get creative.”
Despite the “disembodied” nature of technology, patients and their families have expressed gratitude to chaplains for their efforts to facilitate connections between loved ones and to be “a guide on the side,” as Mary Wetsch-Johnson, BCC, put it. She recalled one phone conversation with the daughter of a man with COVID-19 who was placed on comfort measures. “She said her dad was like the dad on the TV series Father Knows Best, just a kind-hearted, loving, wonderful man,” said Ms. Wetsch-Johnson, a chaplain at CHI Franciscan Health, which operates 10 acute-care hospitals in the Puget Sound region of Washington state. “She was able to describe him in a way that I felt like I knew him. She talked about the discord they had in their family and how they’re processing through that, and about her own personal journey with grief and loss. She then asked me for information about funeral homes, and I provided her with information. At the end of it, she said, ‘I did not know that I needed you today, but you are exactly what I needed.’ ”
Hospital chaplains may be using smartphones and other gadgets to communicate with patients and their families more than they did in the pre-COVID-19 world, but their basic job has not changed, said Rabbi Neal J. Loevinger, BCC, director of spiritual care services at Vassar Brothers Medical Center in Poughkeepsie, N.Y., part of a seven-hospital system operated by Nuvance Health. “We offer the hope of a caring presence,” said Rabbi Loevinger, who is also a member of the board of directors for Neshama: Association of Jewish Chaplains. “If someone is in a hole, our job is to climb down into the hole with them and say, ‘We’re going to get out of this hole together.’ We can’t promise that someone’s going to get better. We can’t promise that everything’s going to be all right. What we can promise is that we will not abandon you. We can promise that there will be someone accompanying you in any way we can through this crisis.”
Ms. Hauck remembered a phone conversation with the granddaughter of a patient hospitalized with COVID-19 who was nearing the end of her life. The granddaughter told her a story about how her grandmother and her best friend made a pact with each other that, when one was dying, the other would come to her side and pray the Rosary with her. “The granddaughter got tearful and said, ‘That can’t happen now,’ ” said Ms. Hauck, who oversees a staff of 9 chaplains and 10 per diem chaplains. “I made a promise that I would do my best to be at the bedside and pray the Rosary with her grandmother.”
The nurses were aware of the request, and about a day later, Ms. Hauck received a call at 1 a.m., indicating that the patient was close to dying. She drove to Lancaster General, put on her personal protective equipment, made it to the patient’s bedside, and began to pray the Rosary with her, with a nurse in the room. “The nurse said to me, ‘Carolanne, all of her stats are going up,’ and the patient actually became a little more alert,” she recalled. “We talked a little bit, and I asked, ‘Would you like to pray the Rosary now?’ She shook her head yes, and said, ‘Hail Mary, full of grace ...’ and those were the last words that she spoke. I finished the prayers for her, and then she died. It was very meaningful knowing that I could honor that wish for her, but more importantly, that I could do that for the family, who otherwise would have been at her side saying the Rosary with her. We have a recognition of how hard it is to leave someone at the hospital and not be at their bedside.”

Hospital chaplains are also supporting interdisciplinary teams of physicians, nurses, and other staff, as they navigate the provision of care in the wake of a pandemic. “They are under a great deal of stress – not only from being at work but with all the role changes that have happened in their home life,” Ms. Wetsch-Johnson said. “Some of them now are being the teacher at home and having to care for children. They have a lot that they come in with. My job is to help them so that they can go do their job. Regularly what I do is check in with the units and ask, ‘How are you doing today? What’s going on for you?’ Because people need to know that someone’s there to be with them and walk with them and listen to them.”
In the spirit of being present for their staff, she and her colleagues established “respite rooms” at CHI Franciscan hospitals, where workers can decompress and get recentered before returning to work. “We usually have water and snacks in there for them, and some type of soothing music,” Ms. Wetsch-Johnson said. “There is also literature on breathing exercises and stretching exercises. We’re also inviting people to write little notes of hope and gratitude, and they’re putting those up for each other. It’s important that we keep supporting them as they support the patients. Personally, I also round with our physicians, because they carry a lot with them, just as much as any other staff. I check in with dietary and environmental services. Everybody’s giving in their own unique way; that helps this whole health care system keep going.”
On any given day, it’s not uncommon for hospital staff members to spontaneously pull aside chaplains to vent, pray, or just to talk. “They process their own fears and anxieties about working in this kind of environment,” Rev. Mercier said. “They’re scared for themselves. They think, ‘Could I get the virus? Could I spread the virus to my family?’ Or, they may express the care and concern they have for their patients. Oftentimes, it’s a mixture of both. Those spontaneous conversations are often the most powerful.”
Ms. Hauck noted that some nurses and clinicians at Lancaster General Hospital “are doing work they may have not done before,” she said. “Some of them are experiencing death for the first time, so we help them to navigate that. One of the best things we can do is hear the anxiety they have or the sadness they have when a patient dies. Also, maybe the frustration that they couldn’t do more in some cases and helping them to see that sometimes their best is good enough.”
She recalled one younger patient with COVID-19 who fell seriously ill. “It was really affecting a lot of people on the unit because of the patient’s age,” she said. “When we saw that the patient was getting better and would be discharged, there was such a sense of relief. I’m not sure that patient will ever understand how that helped us. It was comforting to us to know that people are getting better. It is something we celebrate.”
As chaplains adjust to their “new normal,” carving out time for self-care is key. Ms. Hauck and her staff periodically meet on Zoom with a psychotherapist “who understands what we do, asks us really good questions, and reminds us to take care of ourselves,” she said. “Personally, I’m making sure I get my exercise in, I pack a healthy lunch. We do check in with each other. Part of our handoff at every shift provides for an opportunity to debrief about how your day was.”
Rev. Mercier’s self check-in includes deep-breathing meditation and reciting certain prayers throughout the day. “The deep breathing helps me center and refocus with my body, while the prayers remind me of my connection to the Divine,” he said. “It also reminds me that in the midst of the fear and the anxiety, I fear for myself. It’s hard not to be concerned that I could be infected. I have a family at home and could spread this to them. The prayer practices are a reminder to me that it’s okay to feel those fears and anxieties. Sometimes the spiritual practice helps me find that place of acceptance. That enables me to keep moving forward.”
Ms. Wetsch-Johnson described the sense of upendedness caused by the COVID-19 pandemic as a “ripple in the water that’s going to have long-lasting effects on the delivery of health care. People are taking the time to listen to one another. I’ve seen people in all departments be more compassionate with one another. I’ve seen managers go out of their way to make sure their staff are deeply cared for. I think that will have a ripple effect. That’s my hope, that we will continue to be more compassionate, more loving, and more understanding.”
Rabbi Loevinger hopes that even the most reticent physicians remember that chaplains serve as their advocate, too, especially during times of crisis. “This has been a time of unprecedented ethical wrestling in our hospitals, where there’s been a real concern that doctors, nurses, and respiratory therapists are going to be faced with morally distressing situations regarding insufficient PPE, or insufficient ventilator or dialysis machine supply to support everybody that needs to be supported,” he said. “Chaplains are a key part of the process of making ethical decisions, but also supporting physicians who are in distress over [being in] situations they never had imagined. Physicians don’t like to talk about the fact that a lot of the decisions they make are really heartbreaking. But if chaplains understand anything, it’s that being brokenhearted is part of the human condition, and that we can be part of the answer for keeping physicians morally and spiritually grounded in their work. We always invite that conversation.”
For Rev. Mercier, serving in a time of crisis reminds him of the importance of providing care as a team, “not just for patients and families, but for one another,” he said. “One of the lessons we can learn is, how can we build that connection with one another, to support and care for one another? How can we make sure that no one feels alone while working in the hospital?”
He draws inspiration from a saying credited to St. John of the Cross, which reads, “I saw the river through which every soul must pass, and the name of that river is suffering. I saw the boat that carries each soul across that river, and the name of that boat is love.”
“It’s that image that’s sticking with me, not just for myself as a chaplain but for all of my colleagues in the hospital,” said Rev. Mercier, who also pastors Tabernacle Baptist Church in Hope, R.I. “We’re in that river with the patients right now, suffering, and we’re doing our best to help them get to the other side – whatever the other side may look like.”
Correction, 4/30/20: An earlier version of the caption for the photo with Mary Wetsch-Johnson misstated the location. The photo was taken outside St. Elizabeth Hospital in Enumclaw, Wash.
Visa worries besiege immigrant physicians fighting COVID-19
Physicians and their sponsoring health care facilities shouldn’t have to worry about visa technicalities as they work on the front lines during the COVID-19 pandemic, said health care leaders and immigration reform advocates.
In a press call hosted by the National Immigration Forum, speakers highlighted the need for fast and flexible solutions to enable health care workers, including physicians, to contribute to efforts to combat the pandemic.
Nationwide, over one in five physicians are immigrants, according to data from the Forum. That figure is over one in three in New York, New Jersey, and California, three states hard-hit by COVID-19 cases.
Many physicians stand willing and able to serve where they’re needed, but visa restrictions often block the ability of immigrant physicians to meet COVID-19 surges across the country, said Amit Vashist, MD, senior vice president and chief clinical officer for Ballad Health, Johnson City, Tenn., and a member of the public policy committee of the Society of Hospital Medicine. Ballad Health is an integrated health care system that serves 29 counties in the rural Southeast.
“This pandemic is a war with an invisible enemy, and immigrant physicians have been absolutely critical to providing quality care, especially on the front lines – but current visa restrictions have limited the ability to deploy these physicians in communities with the greatest need,” said Dr. Vashist during the press conference.
Visa requirements currently tie a non-US citizen resident physician to a particular institution and facility, limiting the ability to meet demand flexibly. “Federal agencies and Congress should provide additional flexibility in visa processing to allow for automatic renewals and expediting processing so immigrant medical workers can focus on treating the sick and not on their visa requirements,” said Dr. Vashist.
Dr. Vashist noted that, when he speaks with the many Ballad Health hospitalists who are waiting on permanent residency or citizenship, many of them also cite worries about the fate of their families should they themselves fall ill. Depending on the physician’s visa status, the family may face deportation without recourse if the physician should die.
“Tens of thousands of our physicians continue to endure years, even decades of waiting to obtain a permanent residency in the United States and at the same time, relentlessly and fearlessly serve their communities including in this COVID-19 pandemic,” said Dr. Vashist. “It’s time we take care of them and their long-term immigration needs, and give them the peace of mind that they so desperately deserve,” he added.
Frank Trinity, chief legal officer for the Association of American Medical Colleges, also participated in the call. “For decades,” he said, the United States “has relied on physicians from other countries, especially in rural and underserved areas.”
One of these physicians, Mihir Patel, MD, FHM, a hospitalist at Ballad Health, came to the United States in 2005, but 15 years later is still waiting for the green card that signifies U.S. permanent residency status. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the health system’s COVID-10 Strike Team.
“During the COVID crisis, these restrictions can cause significant negative impact for small rural hospitals,” Dr. Patel said. “There are physicians on a visa who cannot legally work outside their primary facilities – even though they are willing to do so.”
Regarding the pandemic, Mr. Trinity expressed concerns about whether the surge of patients would “outstrip our workforce.” He noted that, with an unprecedented number of desperately ill patients needing emergency care all across the country, “now is the time for our government to take every possible action to ensure that these highly qualified and courageous health professionals are available in the fight against the coronavirus.”
Mr. Trinity outlined five governmental actions AAMC is proposing to allow immigrant physicians to participate fully in the battle against COVID-19. The first would be to approve a blanket extension of visa deadlines. The second would be to expedite processing of visa extension applications, including reinstating expedited processing of physicians currently holding H-1B visa status.
The third action proposed by AAMC is to provide flexibility to visa sponsors during the emergency so that an individual whose visa is currently limited to a particular program can provide care at another location or by means of telehealth.
Fourth, AAMC proposes streamlined entry for the 4,200 physicians who are matched into residency programs so that they may begin their residencies on time or early.
Finally, Mr. Trinity said that AAMC is proposing that work authorizations be maintained for the 29,000 physicians who are currently not U.S. citizens and actively participating in the health care workforce.
Jacinta Ma, the Forum’s vice president of policy and advocacy, said immigrants are a critical component of the U.S. health care workforce as a whole.
“With immigrants accounting for 17% of health care workers amid the COVID-19 pandemic, it’s clear that they are vital to our communities,” she said. “Congress and the Trump administration both have an opportunity to advance solutions that protect immigrants, and remove immigration-related barriers for immigrant medical professionals by ensuring that immigrant doctors, nurses, home health care workers, researchers, and others can continue their vital work during this pandemic while being afforded adequate protection from COVID-19.”
Physicians and their sponsoring health care facilities shouldn’t have to worry about visa technicalities as they work on the front lines during the COVID-19 pandemic, said health care leaders and immigration reform advocates.
In a press call hosted by the National Immigration Forum, speakers highlighted the need for fast and flexible solutions to enable health care workers, including physicians, to contribute to efforts to combat the pandemic.
Nationwide, over one in five physicians are immigrants, according to data from the Forum. That figure is over one in three in New York, New Jersey, and California, three states hard-hit by COVID-19 cases.
Many physicians stand willing and able to serve where they’re needed, but visa restrictions often block the ability of immigrant physicians to meet COVID-19 surges across the country, said Amit Vashist, MD, senior vice president and chief clinical officer for Ballad Health, Johnson City, Tenn., and a member of the public policy committee of the Society of Hospital Medicine. Ballad Health is an integrated health care system that serves 29 counties in the rural Southeast.
“This pandemic is a war with an invisible enemy, and immigrant physicians have been absolutely critical to providing quality care, especially on the front lines – but current visa restrictions have limited the ability to deploy these physicians in communities with the greatest need,” said Dr. Vashist during the press conference.
Visa requirements currently tie a non-US citizen resident physician to a particular institution and facility, limiting the ability to meet demand flexibly. “Federal agencies and Congress should provide additional flexibility in visa processing to allow for automatic renewals and expediting processing so immigrant medical workers can focus on treating the sick and not on their visa requirements,” said Dr. Vashist.
Dr. Vashist noted that, when he speaks with the many Ballad Health hospitalists who are waiting on permanent residency or citizenship, many of them also cite worries about the fate of their families should they themselves fall ill. Depending on the physician’s visa status, the family may face deportation without recourse if the physician should die.
“Tens of thousands of our physicians continue to endure years, even decades of waiting to obtain a permanent residency in the United States and at the same time, relentlessly and fearlessly serve their communities including in this COVID-19 pandemic,” said Dr. Vashist. “It’s time we take care of them and their long-term immigration needs, and give them the peace of mind that they so desperately deserve,” he added.
Frank Trinity, chief legal officer for the Association of American Medical Colleges, also participated in the call. “For decades,” he said, the United States “has relied on physicians from other countries, especially in rural and underserved areas.”
One of these physicians, Mihir Patel, MD, FHM, a hospitalist at Ballad Health, came to the United States in 2005, but 15 years later is still waiting for the green card that signifies U.S. permanent residency status. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the health system’s COVID-10 Strike Team.
“During the COVID crisis, these restrictions can cause significant negative impact for small rural hospitals,” Dr. Patel said. “There are physicians on a visa who cannot legally work outside their primary facilities – even though they are willing to do so.”
Regarding the pandemic, Mr. Trinity expressed concerns about whether the surge of patients would “outstrip our workforce.” He noted that, with an unprecedented number of desperately ill patients needing emergency care all across the country, “now is the time for our government to take every possible action to ensure that these highly qualified and courageous health professionals are available in the fight against the coronavirus.”
Mr. Trinity outlined five governmental actions AAMC is proposing to allow immigrant physicians to participate fully in the battle against COVID-19. The first would be to approve a blanket extension of visa deadlines. The second would be to expedite processing of visa extension applications, including reinstating expedited processing of physicians currently holding H-1B visa status.
The third action proposed by AAMC is to provide flexibility to visa sponsors during the emergency so that an individual whose visa is currently limited to a particular program can provide care at another location or by means of telehealth.
Fourth, AAMC proposes streamlined entry for the 4,200 physicians who are matched into residency programs so that they may begin their residencies on time or early.
Finally, Mr. Trinity said that AAMC is proposing that work authorizations be maintained for the 29,000 physicians who are currently not U.S. citizens and actively participating in the health care workforce.
Jacinta Ma, the Forum’s vice president of policy and advocacy, said immigrants are a critical component of the U.S. health care workforce as a whole.
“With immigrants accounting for 17% of health care workers amid the COVID-19 pandemic, it’s clear that they are vital to our communities,” she said. “Congress and the Trump administration both have an opportunity to advance solutions that protect immigrants, and remove immigration-related barriers for immigrant medical professionals by ensuring that immigrant doctors, nurses, home health care workers, researchers, and others can continue their vital work during this pandemic while being afforded adequate protection from COVID-19.”
Physicians and their sponsoring health care facilities shouldn’t have to worry about visa technicalities as they work on the front lines during the COVID-19 pandemic, said health care leaders and immigration reform advocates.
In a press call hosted by the National Immigration Forum, speakers highlighted the need for fast and flexible solutions to enable health care workers, including physicians, to contribute to efforts to combat the pandemic.
Nationwide, over one in five physicians are immigrants, according to data from the Forum. That figure is over one in three in New York, New Jersey, and California, three states hard-hit by COVID-19 cases.
Many physicians stand willing and able to serve where they’re needed, but visa restrictions often block the ability of immigrant physicians to meet COVID-19 surges across the country, said Amit Vashist, MD, senior vice president and chief clinical officer for Ballad Health, Johnson City, Tenn., and a member of the public policy committee of the Society of Hospital Medicine. Ballad Health is an integrated health care system that serves 29 counties in the rural Southeast.
“This pandemic is a war with an invisible enemy, and immigrant physicians have been absolutely critical to providing quality care, especially on the front lines – but current visa restrictions have limited the ability to deploy these physicians in communities with the greatest need,” said Dr. Vashist during the press conference.
Visa requirements currently tie a non-US citizen resident physician to a particular institution and facility, limiting the ability to meet demand flexibly. “Federal agencies and Congress should provide additional flexibility in visa processing to allow for automatic renewals and expediting processing so immigrant medical workers can focus on treating the sick and not on their visa requirements,” said Dr. Vashist.
Dr. Vashist noted that, when he speaks with the many Ballad Health hospitalists who are waiting on permanent residency or citizenship, many of them also cite worries about the fate of their families should they themselves fall ill. Depending on the physician’s visa status, the family may face deportation without recourse if the physician should die.
“Tens of thousands of our physicians continue to endure years, even decades of waiting to obtain a permanent residency in the United States and at the same time, relentlessly and fearlessly serve their communities including in this COVID-19 pandemic,” said Dr. Vashist. “It’s time we take care of them and their long-term immigration needs, and give them the peace of mind that they so desperately deserve,” he added.
Frank Trinity, chief legal officer for the Association of American Medical Colleges, also participated in the call. “For decades,” he said, the United States “has relied on physicians from other countries, especially in rural and underserved areas.”
One of these physicians, Mihir Patel, MD, FHM, a hospitalist at Ballad Health, came to the United States in 2005, but 15 years later is still waiting for the green card that signifies U.S. permanent residency status. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the health system’s COVID-10 Strike Team.
“During the COVID crisis, these restrictions can cause significant negative impact for small rural hospitals,” Dr. Patel said. “There are physicians on a visa who cannot legally work outside their primary facilities – even though they are willing to do so.”
Regarding the pandemic, Mr. Trinity expressed concerns about whether the surge of patients would “outstrip our workforce.” He noted that, with an unprecedented number of desperately ill patients needing emergency care all across the country, “now is the time for our government to take every possible action to ensure that these highly qualified and courageous health professionals are available in the fight against the coronavirus.”
Mr. Trinity outlined five governmental actions AAMC is proposing to allow immigrant physicians to participate fully in the battle against COVID-19. The first would be to approve a blanket extension of visa deadlines. The second would be to expedite processing of visa extension applications, including reinstating expedited processing of physicians currently holding H-1B visa status.
The third action proposed by AAMC is to provide flexibility to visa sponsors during the emergency so that an individual whose visa is currently limited to a particular program can provide care at another location or by means of telehealth.
Fourth, AAMC proposes streamlined entry for the 4,200 physicians who are matched into residency programs so that they may begin their residencies on time or early.
Finally, Mr. Trinity said that AAMC is proposing that work authorizations be maintained for the 29,000 physicians who are currently not U.S. citizens and actively participating in the health care workforce.
Jacinta Ma, the Forum’s vice president of policy and advocacy, said immigrants are a critical component of the U.S. health care workforce as a whole.
“With immigrants accounting for 17% of health care workers amid the COVID-19 pandemic, it’s clear that they are vital to our communities,” she said. “Congress and the Trump administration both have an opportunity to advance solutions that protect immigrants, and remove immigration-related barriers for immigrant medical professionals by ensuring that immigrant doctors, nurses, home health care workers, researchers, and others can continue their vital work during this pandemic while being afforded adequate protection from COVID-19.”








