User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
New panic disorder model flags risk for recurrence, persistence
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.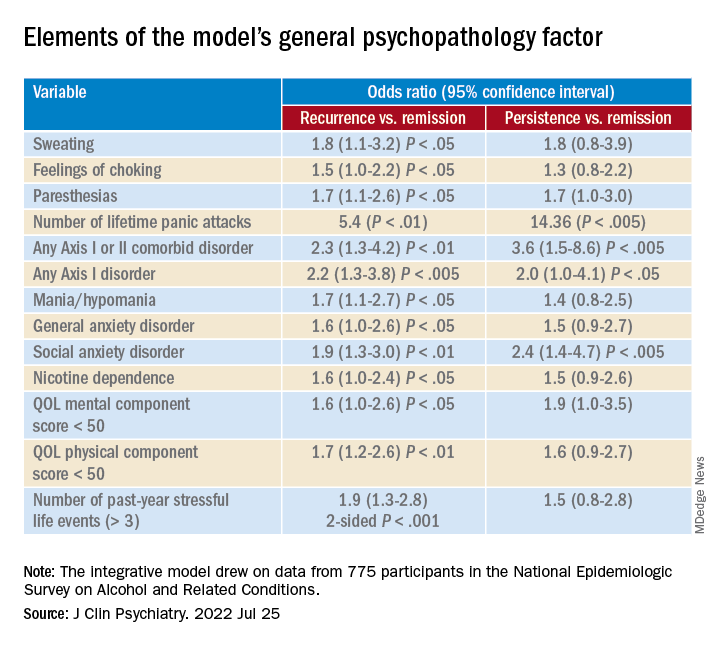
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.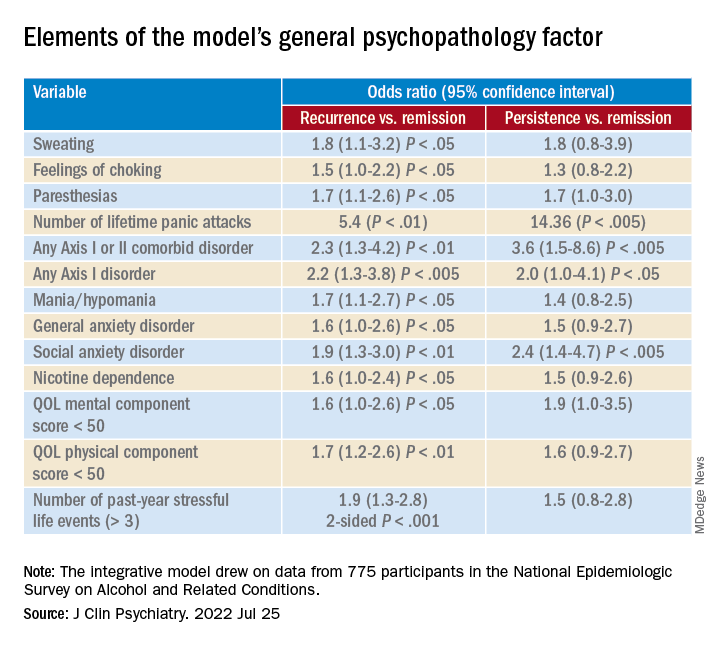
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
Investigators based in France and the United States analyzed data for almost 800 patients with DSM-IV–diagnosed PD.
Results showed that having a “general psychopathology factor,” defined as the shared effects of all comorbid conditions, or PD liability, significantly and independently predicted 3-year recurrence or persistence of PD symptoms.
Having a lower physical health-related quality of life (QOL), a greater number of stressful life events, and not seeking treatment at baseline were also significant and independent predictors.
“This integrative model could help clinicians to identify individuals at high risk of recurrence or persistence of panic disorder and provide content for future research,” Valentin Scheer, MD, MPH, a resident in psychiatry at AP-HP, Assistance Publique, Hôpitaux de Paris, and colleagues wrote.
The findings were published online in the Journal of Clinical Psychiatry.
Integration needed
PD is a disabling disorder with a “chronic course” – and a recurrence rate ranging from 25% to 50%, the investigators noted.
“Because of the heterogeneous course of PD, there is a need to develop a comprehensive predictive model of recurrence or persistence,” they wrote. This could “help practitioners adapt therapeutic strategies and develop prevention strategies in high-risk individuals.”
Most previous studies that have investigated risk factors for PD recurrence and persistence have relied on clinical samples, often with limited sample sizes.
Moreover, each risk factor, when considered individually, accounts for only a “small proportion” of the variance in risk, the researchers noted. The co-occurrence of these risk factors “suggests the need to combine them into a broad multivariable model.”
However, currently proposed integrative models do not identify independent predictors or mitigate the influence of confounding variables. To fill this gap, the investigators conducted a study using structural equation modeling “to take into account multiple correlations across predictors.”
They drew on data from 775 participants (mean age, 40 years) in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). For the current analysis, they examined two waves of NESARC (2001-2002 and 2004-2005) to “build a comprehensive model” of the 3-year recurrence or persistence of PD.
The researchers used a “latent variable approach” that simultaneously examined the effect of the following five groups of potential predictors of recurrence or persistence: PD severity, severity of comorbidity, family history of psychiatric disorders, sociodemographic characteristics, and treatment-seeking behavior.
They also distinguished between risk factors responsible for recurrence and those responsible for persistence.
Psychiatric diagnoses were determined on the basis of the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV. Participants also completed Version 2 of the Short Form 12-Item Health Survey, which assesses both mental and physical QOL over the previous 4 weeks.
Early treatment needed
Among participants with a 12-month diagnosis of PD at wave 1, 13% had persistent PD and 27.6% had recurrent PD during the 3-year period. The mean duration of illness was 9.5 years.
A greater number of lifetime panic attacks, the presence of any Axis I or II comorbid disorder, and any Axis I disorder, especially social anxiety disorder, were significantly associated with 3-year risk for recurrence and for persistence.
Sweating, choking, paresthesias, the comorbid disorders of mania/hypomania and general anxiety disorder, nicotine dependence, lower mental and physical QOL scores, and exposure to a greater number of stressful life events in the previous year were all significantly associated with 3-year risk for recurrence.
Only variables shown with a P value were statistically significant, “with the a priori fixed at .05,” the researchers noted.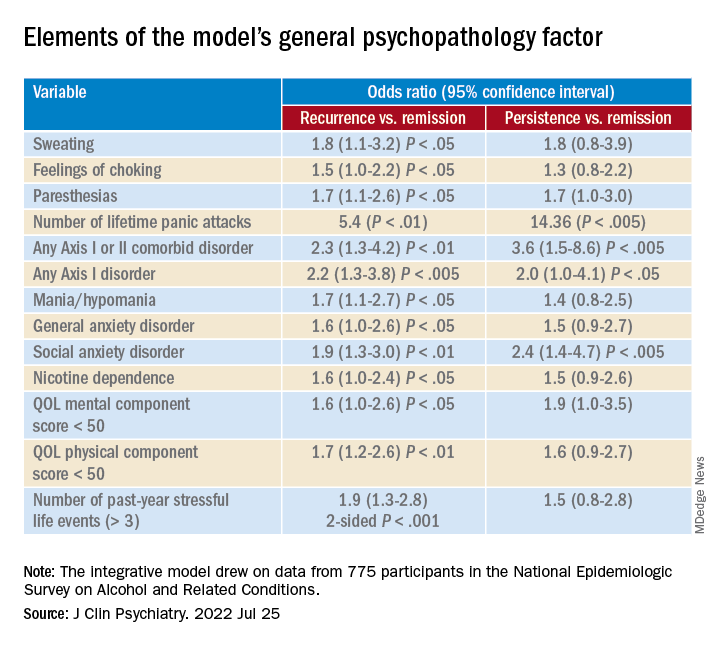
A combination of psychopathology factors, such as the shared effect of all comorbid psychiatric conditions, PD liability, lower physical health-related QOL, more life stressors during the past year, and not seeking treatment at baseline “significantly and independently” predicted recurrence or persistence of symptoms between the two waves (all Ps < .05), the investigators reported.
One study limitation cited was that several psychiatric disorders known to be associated with PD recurrence or persistence, such as borderline personality disorder, were not examined. Additionally, the study used a 3-year follow-up period – and the results might have differed for other follow-up time frames, the researchers noted.
Nevertheless, the findings constitute a “comprehensive model” to predict recurrence and persistence of PD, they wrote. Moreover, early treatment-seeking behavior “should be promoted, as it may reduce the risk of recurrence.”
Not much new?
Commenting on the study, Peter Roy-Byrne, MD, professor of psychiatry, University of Washington, Seattle, noted, “there is not much that is new here.”
Dr. Roy-Byrne, who was not involved with the study, said that a “general theme for years has been that more severe illness, whether you measure it by greater number of other Axis I disorders or symptom severity or a general psychopathology factor, usually predicts worse outcome – here codified as persistence and recurrence.”
Greater stress and reluctance to seek treatment may also predict worse outcomes, he noted.
In addition, the study “did not examine another very important factor: the degree of social connection/social support that someone has,” Dr. Roy-Byrne said. However, “perhaps some of this was contained in specific life events.”
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Siblings of children with chronic health conditions may have increased mental health risks
Siblings of children with chronic health conditions could be at an increased risk for depression, according to a new report.
In a systematic review of 34 studies, siblings of children with chronic health conditions had significantly higher scores on depressive rating scales than individuals without a sibling with a chronic health condition (standardized mean difference = 0.53; P < .001). Findings related to other clinical health outcomes, such as physical health conditions or mortality, were inconsistent.
“We’ve known for a long time that siblings of kids with chronic conditions undergo stress, and there have been conflicting data on how that stress is manifested in terms of their own health,” senior study author Eyal Cohen, MD, program head for child health evaluative sciences at the Hospital for Sick Children, Toronto, told this news organization.
“For some siblings, having the experience of being raised with a child with a chronic condition may be an asset and build resiliency, while other siblings may feel strong negative emotions, such as sadness, anger, and fear,” he said. “Although we know that this experience is stressful for many siblings, it is important to know whether it changes their health outcomes, so that appropriate support can be put in place for those who need it.”
The study was published online in the Journal of Pediatrics.
Risk for psychological challenges
About a quarter of children in the United States have a mental, emotional, developmental, or behavioral condition, and more than a third have at least one current or lifelong health condition, the study authors write. A childhood chronic health condition can affect family members through worse mental health outcomes, increased stress, and poorer health-related quality of life.
Dr. Cohen and colleagues conducted a systematic review and meta-analysis to assess the clinical mental and physical health outcomes of siblings of children with chronic health conditions in comparison with siblings of healthy children or normative data.
The research team included English-language studies that reported on clinically diagnosable mental or physical health outcomes among siblings of persons younger than 18 years who had a chronic health condition. They included a comparison group and used an experimental or observational design for their study. The researchers analyzed 34 studies, including 28 that reported on mental health, 3 that reported on physical health, and 3 that reported on mortality.
Overall, siblings of children with chronic health conditions had significantly higher scores on depression rating scales than their comparison groups. Siblings’ anxiety scores weren’t substantially higher, however (standard mean difference = 0.21; P = .07).
The effects for confirmed psychiatric diagnoses, physical health outcomes, and mortality could not be included in the meta-analysis, owing to the limited number of studies and the high level of heterogeneity among the studies.
Dr. Cohen noted that although the researchers weren’t surprised that siblings may be at increased risk of mental health challenges, they were surprised by the limited data regarding physical health.
“At a minimum, our findings support the importance of asking open-ended questions about how a family is doing during clinical encounters,” he said. “These siblings may also benefit from programs such as support groups or summer camps, which have been shown to improve mental health and behavioral outcomes in siblings of children with chronic health conditions, such as cancer and neurodevelopmental disabilities.”
Future studies should assess the specific risk factors for mental health problems in siblings of children with chronic health conditions, Dr. Cohen said. Additional research could also investigate the design and effectiveness of interventions that address these concerns.
Message of inclusiveness
“The message that resonates with me is about the interventions and resources needed to support siblings,” Linda Nguyen, a doctoral student in rehabilitation science and researcher with the CanChild Center for Childhood Disability Research at McMaster University in Hamilton, Ont., told this news organization.
Ms. Nguyen, who wasn’t involved with this study, has researched the resources available to siblings in Canada and has found a lack of support options, particularly when it comes to specific health care management roles.
“Consistently throughout my research, I’ve seen the need for resources that go beyond a focus on siblings’ well-being and instead support them in their different roles,” she said. “Some want to be friends, mentors, supporters, and caregivers for their siblings in the future.”
Siblings often adopt different roles as they form their own identity, Ms. Nguyen noted, which becomes a larger part of the health care conversation as children with chronic conditions make the transition from pediatric to adult health care. Siblings want to be asked how they’d like to be involved, she said. Some would like to be involved with health care appointments, the chronic condition community, research, and policy making.
“At the societal level and public level, there’s also a message of inclusiveness and making sure that we’re welcoming youth with disabilities and chronic conditions,” Jan Willem Gorter, MD, PhD, a professor of pediatrics and scientist for CanChild at McMaster University, told this news organization.
Dr. Gorter, who also was not involved with this study, noted that children with chronic conditions often feel left behind, which can influence the involvement of their siblings as well.
“There are a lot of places in the world where children with disabilities go to special schools, and they spend a lot of time in a different world, with different experiences than their siblings,” he said. “At the public health level, we want to advocate for an inclusive society and support the whole family, which benefits everybody.”
The study was funded by the Canadian Institutes of Health Research and the CHILD-BRIGHT Network summer studentship, which is supported by the Canadian Institute for Health Research Strategy for Patient-Oriented Research. Dr. Cohen, Ms. Nguyen, and Dr. Gorter have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Siblings of children with chronic health conditions could be at an increased risk for depression, according to a new report.
In a systematic review of 34 studies, siblings of children with chronic health conditions had significantly higher scores on depressive rating scales than individuals without a sibling with a chronic health condition (standardized mean difference = 0.53; P < .001). Findings related to other clinical health outcomes, such as physical health conditions or mortality, were inconsistent.
“We’ve known for a long time that siblings of kids with chronic conditions undergo stress, and there have been conflicting data on how that stress is manifested in terms of their own health,” senior study author Eyal Cohen, MD, program head for child health evaluative sciences at the Hospital for Sick Children, Toronto, told this news organization.
“For some siblings, having the experience of being raised with a child with a chronic condition may be an asset and build resiliency, while other siblings may feel strong negative emotions, such as sadness, anger, and fear,” he said. “Although we know that this experience is stressful for many siblings, it is important to know whether it changes their health outcomes, so that appropriate support can be put in place for those who need it.”
The study was published online in the Journal of Pediatrics.
Risk for psychological challenges
About a quarter of children in the United States have a mental, emotional, developmental, or behavioral condition, and more than a third have at least one current or lifelong health condition, the study authors write. A childhood chronic health condition can affect family members through worse mental health outcomes, increased stress, and poorer health-related quality of life.
Dr. Cohen and colleagues conducted a systematic review and meta-analysis to assess the clinical mental and physical health outcomes of siblings of children with chronic health conditions in comparison with siblings of healthy children or normative data.
The research team included English-language studies that reported on clinically diagnosable mental or physical health outcomes among siblings of persons younger than 18 years who had a chronic health condition. They included a comparison group and used an experimental or observational design for their study. The researchers analyzed 34 studies, including 28 that reported on mental health, 3 that reported on physical health, and 3 that reported on mortality.
Overall, siblings of children with chronic health conditions had significantly higher scores on depression rating scales than their comparison groups. Siblings’ anxiety scores weren’t substantially higher, however (standard mean difference = 0.21; P = .07).
The effects for confirmed psychiatric diagnoses, physical health outcomes, and mortality could not be included in the meta-analysis, owing to the limited number of studies and the high level of heterogeneity among the studies.
Dr. Cohen noted that although the researchers weren’t surprised that siblings may be at increased risk of mental health challenges, they were surprised by the limited data regarding physical health.
“At a minimum, our findings support the importance of asking open-ended questions about how a family is doing during clinical encounters,” he said. “These siblings may also benefit from programs such as support groups or summer camps, which have been shown to improve mental health and behavioral outcomes in siblings of children with chronic health conditions, such as cancer and neurodevelopmental disabilities.”
Future studies should assess the specific risk factors for mental health problems in siblings of children with chronic health conditions, Dr. Cohen said. Additional research could also investigate the design and effectiveness of interventions that address these concerns.
Message of inclusiveness
“The message that resonates with me is about the interventions and resources needed to support siblings,” Linda Nguyen, a doctoral student in rehabilitation science and researcher with the CanChild Center for Childhood Disability Research at McMaster University in Hamilton, Ont., told this news organization.
Ms. Nguyen, who wasn’t involved with this study, has researched the resources available to siblings in Canada and has found a lack of support options, particularly when it comes to specific health care management roles.
“Consistently throughout my research, I’ve seen the need for resources that go beyond a focus on siblings’ well-being and instead support them in their different roles,” she said. “Some want to be friends, mentors, supporters, and caregivers for their siblings in the future.”
Siblings often adopt different roles as they form their own identity, Ms. Nguyen noted, which becomes a larger part of the health care conversation as children with chronic conditions make the transition from pediatric to adult health care. Siblings want to be asked how they’d like to be involved, she said. Some would like to be involved with health care appointments, the chronic condition community, research, and policy making.
“At the societal level and public level, there’s also a message of inclusiveness and making sure that we’re welcoming youth with disabilities and chronic conditions,” Jan Willem Gorter, MD, PhD, a professor of pediatrics and scientist for CanChild at McMaster University, told this news organization.
Dr. Gorter, who also was not involved with this study, noted that children with chronic conditions often feel left behind, which can influence the involvement of their siblings as well.
“There are a lot of places in the world where children with disabilities go to special schools, and they spend a lot of time in a different world, with different experiences than their siblings,” he said. “At the public health level, we want to advocate for an inclusive society and support the whole family, which benefits everybody.”
The study was funded by the Canadian Institutes of Health Research and the CHILD-BRIGHT Network summer studentship, which is supported by the Canadian Institute for Health Research Strategy for Patient-Oriented Research. Dr. Cohen, Ms. Nguyen, and Dr. Gorter have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Siblings of children with chronic health conditions could be at an increased risk for depression, according to a new report.
In a systematic review of 34 studies, siblings of children with chronic health conditions had significantly higher scores on depressive rating scales than individuals without a sibling with a chronic health condition (standardized mean difference = 0.53; P < .001). Findings related to other clinical health outcomes, such as physical health conditions or mortality, were inconsistent.
“We’ve known for a long time that siblings of kids with chronic conditions undergo stress, and there have been conflicting data on how that stress is manifested in terms of their own health,” senior study author Eyal Cohen, MD, program head for child health evaluative sciences at the Hospital for Sick Children, Toronto, told this news organization.
“For some siblings, having the experience of being raised with a child with a chronic condition may be an asset and build resiliency, while other siblings may feel strong negative emotions, such as sadness, anger, and fear,” he said. “Although we know that this experience is stressful for many siblings, it is important to know whether it changes their health outcomes, so that appropriate support can be put in place for those who need it.”
The study was published online in the Journal of Pediatrics.
Risk for psychological challenges
About a quarter of children in the United States have a mental, emotional, developmental, or behavioral condition, and more than a third have at least one current or lifelong health condition, the study authors write. A childhood chronic health condition can affect family members through worse mental health outcomes, increased stress, and poorer health-related quality of life.
Dr. Cohen and colleagues conducted a systematic review and meta-analysis to assess the clinical mental and physical health outcomes of siblings of children with chronic health conditions in comparison with siblings of healthy children or normative data.
The research team included English-language studies that reported on clinically diagnosable mental or physical health outcomes among siblings of persons younger than 18 years who had a chronic health condition. They included a comparison group and used an experimental or observational design for their study. The researchers analyzed 34 studies, including 28 that reported on mental health, 3 that reported on physical health, and 3 that reported on mortality.
Overall, siblings of children with chronic health conditions had significantly higher scores on depression rating scales than their comparison groups. Siblings’ anxiety scores weren’t substantially higher, however (standard mean difference = 0.21; P = .07).
The effects for confirmed psychiatric diagnoses, physical health outcomes, and mortality could not be included in the meta-analysis, owing to the limited number of studies and the high level of heterogeneity among the studies.
Dr. Cohen noted that although the researchers weren’t surprised that siblings may be at increased risk of mental health challenges, they were surprised by the limited data regarding physical health.
“At a minimum, our findings support the importance of asking open-ended questions about how a family is doing during clinical encounters,” he said. “These siblings may also benefit from programs such as support groups or summer camps, which have been shown to improve mental health and behavioral outcomes in siblings of children with chronic health conditions, such as cancer and neurodevelopmental disabilities.”
Future studies should assess the specific risk factors for mental health problems in siblings of children with chronic health conditions, Dr. Cohen said. Additional research could also investigate the design and effectiveness of interventions that address these concerns.
Message of inclusiveness
“The message that resonates with me is about the interventions and resources needed to support siblings,” Linda Nguyen, a doctoral student in rehabilitation science and researcher with the CanChild Center for Childhood Disability Research at McMaster University in Hamilton, Ont., told this news organization.
Ms. Nguyen, who wasn’t involved with this study, has researched the resources available to siblings in Canada and has found a lack of support options, particularly when it comes to specific health care management roles.
“Consistently throughout my research, I’ve seen the need for resources that go beyond a focus on siblings’ well-being and instead support them in their different roles,” she said. “Some want to be friends, mentors, supporters, and caregivers for their siblings in the future.”
Siblings often adopt different roles as they form their own identity, Ms. Nguyen noted, which becomes a larger part of the health care conversation as children with chronic conditions make the transition from pediatric to adult health care. Siblings want to be asked how they’d like to be involved, she said. Some would like to be involved with health care appointments, the chronic condition community, research, and policy making.
“At the societal level and public level, there’s also a message of inclusiveness and making sure that we’re welcoming youth with disabilities and chronic conditions,” Jan Willem Gorter, MD, PhD, a professor of pediatrics and scientist for CanChild at McMaster University, told this news organization.
Dr. Gorter, who also was not involved with this study, noted that children with chronic conditions often feel left behind, which can influence the involvement of their siblings as well.
“There are a lot of places in the world where children with disabilities go to special schools, and they spend a lot of time in a different world, with different experiences than their siblings,” he said. “At the public health level, we want to advocate for an inclusive society and support the whole family, which benefits everybody.”
The study was funded by the Canadian Institutes of Health Research and the CHILD-BRIGHT Network summer studentship, which is supported by the Canadian Institute for Health Research Strategy for Patient-Oriented Research. Dr. Cohen, Ms. Nguyen, and Dr. Gorter have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF PEDIATRICS
Postpartum depression risk higher with family psych history
Mothers who have a family history of any psychiatric disorder have almost two times the risk of postpartum depression as do mothers without such history, according to a new study.
Mette-Marie Zacher Kjeldsen, MSc, with the National Centre for Register-based Research at Aarhus (Denmark) University, led the study, a meta-analysis that included 26 studies with information on 100,877 women.
Findings were published online in JAMA Psychiatry.
When mothers had a family history of psychiatric disorders, the odds ratio for PPD was 2.08 (95% confidence interval, 1.67-2.59). That corresponds to a risk ratio of 1.79 (95% CI, 1.52-2.09), assuming a 15% postpartum depression prevalence in the general population.
Not doomed to develop PPD
Polina Teslyar, MD, a perinatal psychiatrist at Brigham and Women’s Hospital in Boston told this news organization it’s important to point out that though the risk is higher, women with a family psychiatric history should not feel as though they are destined to develop PPD.
“You are still more likely to not have postpartum depression, but it is important to be aware of personal risk factors so that if a person is experiencing that, they ask for help quickly rather than suffering and not knowing something is amiss,” she emphasized. Dr. Teslyar says she does see the higher risk for PPD, which is preventable and treatable, in her own practice when women have had a family history of psychiatric disorders.
The association makes sense, but literature on why that is has been varied, she said, and likely involves both genetics and socioeconomic factors. It’s difficult to tease apart how big a part each plays.
In her perinatal practice she sees women even before they are pregnant to discuss risk factors for PPD so she does ask about family history of psychiatric disorders, specifically about history of PPD and anxiety.
The researchers suggest routine perinatal care should include an easy low-cost, two-part question about both personal and family history of psychiatric disorders.
“As the assessment is possible even prior to conception, this would leave time for planning preventive efforts, such as psychosocial and psychological interventions targeting these at-risk women,” the authors write.
Asking about family history a challenge
Dr. Teslyar noted though that one of the challenges in asking about family history is that families may not have openly shared psychiatric history details with offspring. Family members may also report conditions they suspect a family member had rather than having a documented diagnosis.
In places where there is universal health care, she noted, finding documented diagnoses is easier, but otherwise “you’re really taking a subjective interpretation.”
The researchers found that subgroup, sensitivity, and meta–regression analyses aligned with the primary findings. The overall certainty of evidence was graded as moderate.
This study was not able to make clear how the specific diagnoses of family members affect the risk of developing PPD because much of the data from the studies came from self-report and questions were not consistent across the studies.
For instance, only 7 studies asked specifically about first-degree family members and 10 asked about specific diagnoses. Diagnoses ranged from mild affective disorders to more intrusive disorders, such as schizophrenia.
And while this study doesn’t seek to determine why the family history and risk of PPD appear to be connected, the authors offer some possible explanations.
“Growing up in an environment with parents struggling with mental health problems potentially influences the social support received from these parents when going into motherhood,” the authors write. “This particular explanation is supported by umbrella reviews concluding that lack of social support is a significant PPD risk factor.”
Screening, extraction, and assessment of studies included was done independently by two reviewers, increasing validity, the authors note.
The authors state that approximately 10%-15% of new mothers experience PPD, but Dr. Teslyar points out the numbers in the United States are typically quoted at up to 20%-30%. PPD ranges from mild to severe episodes and includes symptoms like those for major depression outside the postpartum period.
Study authors received funding from The Lundbeck Foundation and the European Union’s Horizon 2020 Research and Innovation Programme. A coauthor, Vibe G. Frokjaer, MD, PhD, has served as consultant and lecturer for H. Lundbeck and Sage Therapeutics. No other disclosures were reported. Dr. Teslyar reports no relevant financial relationships.
Mothers who have a family history of any psychiatric disorder have almost two times the risk of postpartum depression as do mothers without such history, according to a new study.
Mette-Marie Zacher Kjeldsen, MSc, with the National Centre for Register-based Research at Aarhus (Denmark) University, led the study, a meta-analysis that included 26 studies with information on 100,877 women.
Findings were published online in JAMA Psychiatry.
When mothers had a family history of psychiatric disorders, the odds ratio for PPD was 2.08 (95% confidence interval, 1.67-2.59). That corresponds to a risk ratio of 1.79 (95% CI, 1.52-2.09), assuming a 15% postpartum depression prevalence in the general population.
Not doomed to develop PPD
Polina Teslyar, MD, a perinatal psychiatrist at Brigham and Women’s Hospital in Boston told this news organization it’s important to point out that though the risk is higher, women with a family psychiatric history should not feel as though they are destined to develop PPD.
“You are still more likely to not have postpartum depression, but it is important to be aware of personal risk factors so that if a person is experiencing that, they ask for help quickly rather than suffering and not knowing something is amiss,” she emphasized. Dr. Teslyar says she does see the higher risk for PPD, which is preventable and treatable, in her own practice when women have had a family history of psychiatric disorders.
The association makes sense, but literature on why that is has been varied, she said, and likely involves both genetics and socioeconomic factors. It’s difficult to tease apart how big a part each plays.
In her perinatal practice she sees women even before they are pregnant to discuss risk factors for PPD so she does ask about family history of psychiatric disorders, specifically about history of PPD and anxiety.
The researchers suggest routine perinatal care should include an easy low-cost, two-part question about both personal and family history of psychiatric disorders.
“As the assessment is possible even prior to conception, this would leave time for planning preventive efforts, such as psychosocial and psychological interventions targeting these at-risk women,” the authors write.
Asking about family history a challenge
Dr. Teslyar noted though that one of the challenges in asking about family history is that families may not have openly shared psychiatric history details with offspring. Family members may also report conditions they suspect a family member had rather than having a documented diagnosis.
In places where there is universal health care, she noted, finding documented diagnoses is easier, but otherwise “you’re really taking a subjective interpretation.”
The researchers found that subgroup, sensitivity, and meta–regression analyses aligned with the primary findings. The overall certainty of evidence was graded as moderate.
This study was not able to make clear how the specific diagnoses of family members affect the risk of developing PPD because much of the data from the studies came from self-report and questions were not consistent across the studies.
For instance, only 7 studies asked specifically about first-degree family members and 10 asked about specific diagnoses. Diagnoses ranged from mild affective disorders to more intrusive disorders, such as schizophrenia.
And while this study doesn’t seek to determine why the family history and risk of PPD appear to be connected, the authors offer some possible explanations.
“Growing up in an environment with parents struggling with mental health problems potentially influences the social support received from these parents when going into motherhood,” the authors write. “This particular explanation is supported by umbrella reviews concluding that lack of social support is a significant PPD risk factor.”
Screening, extraction, and assessment of studies included was done independently by two reviewers, increasing validity, the authors note.
The authors state that approximately 10%-15% of new mothers experience PPD, but Dr. Teslyar points out the numbers in the United States are typically quoted at up to 20%-30%. PPD ranges from mild to severe episodes and includes symptoms like those for major depression outside the postpartum period.
Study authors received funding from The Lundbeck Foundation and the European Union’s Horizon 2020 Research and Innovation Programme. A coauthor, Vibe G. Frokjaer, MD, PhD, has served as consultant and lecturer for H. Lundbeck and Sage Therapeutics. No other disclosures were reported. Dr. Teslyar reports no relevant financial relationships.
Mothers who have a family history of any psychiatric disorder have almost two times the risk of postpartum depression as do mothers without such history, according to a new study.
Mette-Marie Zacher Kjeldsen, MSc, with the National Centre for Register-based Research at Aarhus (Denmark) University, led the study, a meta-analysis that included 26 studies with information on 100,877 women.
Findings were published online in JAMA Psychiatry.
When mothers had a family history of psychiatric disorders, the odds ratio for PPD was 2.08 (95% confidence interval, 1.67-2.59). That corresponds to a risk ratio of 1.79 (95% CI, 1.52-2.09), assuming a 15% postpartum depression prevalence in the general population.
Not doomed to develop PPD
Polina Teslyar, MD, a perinatal psychiatrist at Brigham and Women’s Hospital in Boston told this news organization it’s important to point out that though the risk is higher, women with a family psychiatric history should not feel as though they are destined to develop PPD.
“You are still more likely to not have postpartum depression, but it is important to be aware of personal risk factors so that if a person is experiencing that, they ask for help quickly rather than suffering and not knowing something is amiss,” she emphasized. Dr. Teslyar says she does see the higher risk for PPD, which is preventable and treatable, in her own practice when women have had a family history of psychiatric disorders.
The association makes sense, but literature on why that is has been varied, she said, and likely involves both genetics and socioeconomic factors. It’s difficult to tease apart how big a part each plays.
In her perinatal practice she sees women even before they are pregnant to discuss risk factors for PPD so she does ask about family history of psychiatric disorders, specifically about history of PPD and anxiety.
The researchers suggest routine perinatal care should include an easy low-cost, two-part question about both personal and family history of psychiatric disorders.
“As the assessment is possible even prior to conception, this would leave time for planning preventive efforts, such as psychosocial and psychological interventions targeting these at-risk women,” the authors write.
Asking about family history a challenge
Dr. Teslyar noted though that one of the challenges in asking about family history is that families may not have openly shared psychiatric history details with offspring. Family members may also report conditions they suspect a family member had rather than having a documented diagnosis.
In places where there is universal health care, she noted, finding documented diagnoses is easier, but otherwise “you’re really taking a subjective interpretation.”
The researchers found that subgroup, sensitivity, and meta–regression analyses aligned with the primary findings. The overall certainty of evidence was graded as moderate.
This study was not able to make clear how the specific diagnoses of family members affect the risk of developing PPD because much of the data from the studies came from self-report and questions were not consistent across the studies.
For instance, only 7 studies asked specifically about first-degree family members and 10 asked about specific diagnoses. Diagnoses ranged from mild affective disorders to more intrusive disorders, such as schizophrenia.
And while this study doesn’t seek to determine why the family history and risk of PPD appear to be connected, the authors offer some possible explanations.
“Growing up in an environment with parents struggling with mental health problems potentially influences the social support received from these parents when going into motherhood,” the authors write. “This particular explanation is supported by umbrella reviews concluding that lack of social support is a significant PPD risk factor.”
Screening, extraction, and assessment of studies included was done independently by two reviewers, increasing validity, the authors note.
The authors state that approximately 10%-15% of new mothers experience PPD, but Dr. Teslyar points out the numbers in the United States are typically quoted at up to 20%-30%. PPD ranges from mild to severe episodes and includes symptoms like those for major depression outside the postpartum period.
Study authors received funding from The Lundbeck Foundation and the European Union’s Horizon 2020 Research and Innovation Programme. A coauthor, Vibe G. Frokjaer, MD, PhD, has served as consultant and lecturer for H. Lundbeck and Sage Therapeutics. No other disclosures were reported. Dr. Teslyar reports no relevant financial relationships.
FROM JAMA PSYCHIATRY
COVID-19 may trigger irritable bowel syndrome
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
Gastrointestinal symptoms are common with long COVID, also known as post-acute COVID-19 syndrome, according to Walter Chan, MD, MPH, and Madhusudan Grover, MBBS.
Dr. Chan, an assistant professor at Harvard Medical School, Boston, and Dr. Grover, an associate professor of medicine and physiology at Mayo Clinic, Rochester, Minn., conducted a review of the literature on COVID-19’s long-term gastrointestinal effects. Their review was published in Clinical Gastroenterology and Hepatology.
Estimates of the prevalence of gastrointestinal symptoms with COVID-19 have ranged as high as 60%, Dr. Chan and Dr. Grover report, and the symptoms may be present in patients with long COVID, a syndrome that continues 4 weeks or longer.
In one survey of 749 COVID-19 survivors, 29% reported at least one new chronic gastrointestinal symptom. The most common were heartburn, constipation, diarrhea, and abdominal pain. Of those with abdominal pain, 39% had symptoms that met Rome IV criteria for irritable bowel syndrome.
People who have gastrointestinal symptoms after their initial SARS-CoV-2 infection are more likely to have them with long COVID. Psychiatric diagnoses, hospitalization, and the loss of smell and taste are predictors of gastrointestinal symptoms.
Infectious gastroenteritis can increase the risk for disorders of gut-brain interaction, especially postinfection IBS, Dr. Chan and Dr. Grover write.
COVID-19 likely causes gastrointestinal symptoms through multiple mechanisms. It may suppress angiotensin-converting enzyme 2, which protects intestinal cells. It can alter the microbiome. It can cause or worsen weight gain and diabetes. It may disrupt the immune system and trigger an autoimmune reaction. It can cause depression and anxiety, and it can alter dietary habits.
No specific treatments for gastrointestinal symptoms associated with long COVID have emerged, so clinicians should make use of established therapies for disorders of gut-brain interaction, Dr. Chan and Dr. Grover recommend.
Beyond adequate sleep and exercise, these may include high-fiber, low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, low-carbohydrate, or elimination diets.
For diarrhea, they list loperamide, ondansetron, alosetron, eluxadoline, antispasmodics, rifaximin, and bile acid sequestrants.
For constipation, they mention fiber supplements, polyethylene glycol, linaclotide, plecanatide, lubiprostone, tenapanor, tegaserod, and prucalopride.
For modulating intestinal permeability, they recommend glutamine.
Neuromodulation may be achieved with tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, azaperones, and delta ligands, they write.
For psychological therapy, they recommend cognitive-behavioral therapy and gut-directed hypnotherapy.
A handful of studies have suggested benefits from Lactiplantibacillus plantarum and Pediococcus acidilactici as probiotic therapies. Additionally, one study showed positive results with a high-fiber formula, perhaps by nourishing short-chain fatty acid-producing bacteria, Dr. Chan and Dr. Grover write.
Dr. Chan reported financial relationships with Ironwood, Takeda, and Phathom Pharmaceuticals. Dr. Grover reported financial relationships with Takeda, Donga, Alexza Pharmaceuticals, and Alfasigma.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Early dementia but no specialists: Reinforcements needed?
Patients in rural areas are also less likely to see psychologists and undergo neuropsychological testing, according to the study, published in JAMA Network Open.
Patients who forgo such specialist visits and testing may be missing information about their condition that could help them prepare for changes in job responsibilities and future care decisions, said Wendy Yi Xu, PhD, of The Ohio State University, Columbus, who led the research.
“A lot of them are still in the workforce,” Dr. Xu said. Patients in the study were an average age of 56 years, well before the conventional age of retirement.
Location, location, location
To examine rural versus urban differences in the use of diagnostic tests and health care visits for early onset Alzheimer’s disease and related dementias, Dr. Xu and colleagues analyzed commercial claims data from 2012-2018. They identified more than 71,000 patients aged 40-64 years with those conditions and focused on health care use by 7,311 patients in urban areas and 1,119 in rural areas within 90 days of a new dementia diagnosis.
The proportion who received neuropsychological testing was 19% among urban patients and 16% among rural patients. Psychological assessments, which are less specialized and detailed than neuropsychological testing, and brain imaging occurred at similar rates in both groups. Similar proportions of rural and urban patients visited neurologists (17.7% and 17.96%, respectively) and psychiatrists (6.02% and 6.47%).
But more urban patients than rural patients visited a psychologist, at 19% versus 15%, according to the researchers.
Approximately 18% of patients in rural areas saw a primary care provider without visiting other specialists, compared with 13% in urban areas.
The researchers found that rural patients were significantly less likely to undergo neuropsychological testing (odds ratio, 0.83; 95% confidence interval, 0.70-0.98) or see a psychologist (OR, 0.72; 95% CI, 0.60-0.85).
Similarly, rural patients had significantly higher odds of having only primary care providers involved in the diagnosis of dementia and symptom management (OR, 1.40; 95% CI, 1.19-1.66).
Addressing workforce deficiencies
More primary care training in dementia care and collaboration with specialist colleagues could help address differences in care, Dr. Xu’s group writes. Such efforts are already underway.
In 2018, the Alzheimer’s Association launched telementoring programs focused on dementia care using the Project ECHO (Extension for Community Healthcare Outcomes) model. Researchers originally developed Project ECHO at the University of New Mexico in 2003 to teach primary care clinicians in remote settings how to treat patients infected with the hepatitis C virus.
With the Alzheimer’s and Dementia Care ECHO Program for Clinicians, primary care clinicians can participate in interactive case-based video conferencing sessions to better understand dementia and how to provide high-quality care in community settings, according to the association.
The program covers guidelines for diagnosis, disclosure, and follow-up; the initiation of care planning; managing disease-related challenges; and resources for patients and caregivers.
Since 2018, nearly 100 primary care practices in the United States have completed training in dementia care using Project ECHO, said Morgan Daven, vice president of health systems for the Alzheimer’s Association. Many cases featured in the program are challenging, he added.
“With primary care being on the front lines, it is really important that primary care physicians are equipped to do what they can to detect or diagnose and know when to refer,” Mr. Daven said.
The association has compiled other resources for clinicians as well.
A 2020 report from the association examined the role that primary care physicians play in dementia care. One survey found that 82% of primary care physicians consider themselves on the front lines of providing care for patients with dementia.
Meanwhile, about half say medical professionals are not prepared to meet rising demands associated with Alzheimer’s disease and dementia care.
Mr. Daven said the geographic disparities Dr. Xu and colleagues found are unsurprising. More than half of primary care physicians who care for people with Alzheimer’s disease say dementia specialists in their communities cannot meet demand. The problem is more urgent in rural areas. Roughly half of nonmetropolitan counties in the United States lack a practicing psychologist, according to a 2018 study published in the American Journal of Preventive Medicine.
“We really need to approach this on both sides – build the capacity in primary care, but we also need to address the dementia care specialty shortages,” Mr. Daven said.
The lack of obvious differences in access to neurologists in the new study “was surprising, given the more than fourfold difference between urban and rural areas in the supply of neurologists,” the researchers note. Health plans may maintain more access to neurologists than psychologists because of relatively higher reimbursement for neurologists, they observed.
One of the study coauthors disclosed ties to Aveanna Healthcare, a company that delivers home health and hospice care.
A version of this article first appeared on Medscape.com.
Patients in rural areas are also less likely to see psychologists and undergo neuropsychological testing, according to the study, published in JAMA Network Open.
Patients who forgo such specialist visits and testing may be missing information about their condition that could help them prepare for changes in job responsibilities and future care decisions, said Wendy Yi Xu, PhD, of The Ohio State University, Columbus, who led the research.
“A lot of them are still in the workforce,” Dr. Xu said. Patients in the study were an average age of 56 years, well before the conventional age of retirement.
Location, location, location
To examine rural versus urban differences in the use of diagnostic tests and health care visits for early onset Alzheimer’s disease and related dementias, Dr. Xu and colleagues analyzed commercial claims data from 2012-2018. They identified more than 71,000 patients aged 40-64 years with those conditions and focused on health care use by 7,311 patients in urban areas and 1,119 in rural areas within 90 days of a new dementia diagnosis.
The proportion who received neuropsychological testing was 19% among urban patients and 16% among rural patients. Psychological assessments, which are less specialized and detailed than neuropsychological testing, and brain imaging occurred at similar rates in both groups. Similar proportions of rural and urban patients visited neurologists (17.7% and 17.96%, respectively) and psychiatrists (6.02% and 6.47%).
But more urban patients than rural patients visited a psychologist, at 19% versus 15%, according to the researchers.
Approximately 18% of patients in rural areas saw a primary care provider without visiting other specialists, compared with 13% in urban areas.
The researchers found that rural patients were significantly less likely to undergo neuropsychological testing (odds ratio, 0.83; 95% confidence interval, 0.70-0.98) or see a psychologist (OR, 0.72; 95% CI, 0.60-0.85).
Similarly, rural patients had significantly higher odds of having only primary care providers involved in the diagnosis of dementia and symptom management (OR, 1.40; 95% CI, 1.19-1.66).
Addressing workforce deficiencies
More primary care training in dementia care and collaboration with specialist colleagues could help address differences in care, Dr. Xu’s group writes. Such efforts are already underway.
In 2018, the Alzheimer’s Association launched telementoring programs focused on dementia care using the Project ECHO (Extension for Community Healthcare Outcomes) model. Researchers originally developed Project ECHO at the University of New Mexico in 2003 to teach primary care clinicians in remote settings how to treat patients infected with the hepatitis C virus.
With the Alzheimer’s and Dementia Care ECHO Program for Clinicians, primary care clinicians can participate in interactive case-based video conferencing sessions to better understand dementia and how to provide high-quality care in community settings, according to the association.
The program covers guidelines for diagnosis, disclosure, and follow-up; the initiation of care planning; managing disease-related challenges; and resources for patients and caregivers.
Since 2018, nearly 100 primary care practices in the United States have completed training in dementia care using Project ECHO, said Morgan Daven, vice president of health systems for the Alzheimer’s Association. Many cases featured in the program are challenging, he added.
“With primary care being on the front lines, it is really important that primary care physicians are equipped to do what they can to detect or diagnose and know when to refer,” Mr. Daven said.
The association has compiled other resources for clinicians as well.
A 2020 report from the association examined the role that primary care physicians play in dementia care. One survey found that 82% of primary care physicians consider themselves on the front lines of providing care for patients with dementia.
Meanwhile, about half say medical professionals are not prepared to meet rising demands associated with Alzheimer’s disease and dementia care.
Mr. Daven said the geographic disparities Dr. Xu and colleagues found are unsurprising. More than half of primary care physicians who care for people with Alzheimer’s disease say dementia specialists in their communities cannot meet demand. The problem is more urgent in rural areas. Roughly half of nonmetropolitan counties in the United States lack a practicing psychologist, according to a 2018 study published in the American Journal of Preventive Medicine.
“We really need to approach this on both sides – build the capacity in primary care, but we also need to address the dementia care specialty shortages,” Mr. Daven said.
The lack of obvious differences in access to neurologists in the new study “was surprising, given the more than fourfold difference between urban and rural areas in the supply of neurologists,” the researchers note. Health plans may maintain more access to neurologists than psychologists because of relatively higher reimbursement for neurologists, they observed.
One of the study coauthors disclosed ties to Aveanna Healthcare, a company that delivers home health and hospice care.
A version of this article first appeared on Medscape.com.
Patients in rural areas are also less likely to see psychologists and undergo neuropsychological testing, according to the study, published in JAMA Network Open.
Patients who forgo such specialist visits and testing may be missing information about their condition that could help them prepare for changes in job responsibilities and future care decisions, said Wendy Yi Xu, PhD, of The Ohio State University, Columbus, who led the research.
“A lot of them are still in the workforce,” Dr. Xu said. Patients in the study were an average age of 56 years, well before the conventional age of retirement.
Location, location, location
To examine rural versus urban differences in the use of diagnostic tests and health care visits for early onset Alzheimer’s disease and related dementias, Dr. Xu and colleagues analyzed commercial claims data from 2012-2018. They identified more than 71,000 patients aged 40-64 years with those conditions and focused on health care use by 7,311 patients in urban areas and 1,119 in rural areas within 90 days of a new dementia diagnosis.
The proportion who received neuropsychological testing was 19% among urban patients and 16% among rural patients. Psychological assessments, which are less specialized and detailed than neuropsychological testing, and brain imaging occurred at similar rates in both groups. Similar proportions of rural and urban patients visited neurologists (17.7% and 17.96%, respectively) and psychiatrists (6.02% and 6.47%).
But more urban patients than rural patients visited a psychologist, at 19% versus 15%, according to the researchers.
Approximately 18% of patients in rural areas saw a primary care provider without visiting other specialists, compared with 13% in urban areas.
The researchers found that rural patients were significantly less likely to undergo neuropsychological testing (odds ratio, 0.83; 95% confidence interval, 0.70-0.98) or see a psychologist (OR, 0.72; 95% CI, 0.60-0.85).
Similarly, rural patients had significantly higher odds of having only primary care providers involved in the diagnosis of dementia and symptom management (OR, 1.40; 95% CI, 1.19-1.66).
Addressing workforce deficiencies
More primary care training in dementia care and collaboration with specialist colleagues could help address differences in care, Dr. Xu’s group writes. Such efforts are already underway.
In 2018, the Alzheimer’s Association launched telementoring programs focused on dementia care using the Project ECHO (Extension for Community Healthcare Outcomes) model. Researchers originally developed Project ECHO at the University of New Mexico in 2003 to teach primary care clinicians in remote settings how to treat patients infected with the hepatitis C virus.
With the Alzheimer’s and Dementia Care ECHO Program for Clinicians, primary care clinicians can participate in interactive case-based video conferencing sessions to better understand dementia and how to provide high-quality care in community settings, according to the association.
The program covers guidelines for diagnosis, disclosure, and follow-up; the initiation of care planning; managing disease-related challenges; and resources for patients and caregivers.
Since 2018, nearly 100 primary care practices in the United States have completed training in dementia care using Project ECHO, said Morgan Daven, vice president of health systems for the Alzheimer’s Association. Many cases featured in the program are challenging, he added.
“With primary care being on the front lines, it is really important that primary care physicians are equipped to do what they can to detect or diagnose and know when to refer,” Mr. Daven said.
The association has compiled other resources for clinicians as well.
A 2020 report from the association examined the role that primary care physicians play in dementia care. One survey found that 82% of primary care physicians consider themselves on the front lines of providing care for patients with dementia.
Meanwhile, about half say medical professionals are not prepared to meet rising demands associated with Alzheimer’s disease and dementia care.
Mr. Daven said the geographic disparities Dr. Xu and colleagues found are unsurprising. More than half of primary care physicians who care for people with Alzheimer’s disease say dementia specialists in their communities cannot meet demand. The problem is more urgent in rural areas. Roughly half of nonmetropolitan counties in the United States lack a practicing psychologist, according to a 2018 study published in the American Journal of Preventive Medicine.
“We really need to approach this on both sides – build the capacity in primary care, but we also need to address the dementia care specialty shortages,” Mr. Daven said.
The lack of obvious differences in access to neurologists in the new study “was surprising, given the more than fourfold difference between urban and rural areas in the supply of neurologists,” the researchers note. Health plans may maintain more access to neurologists than psychologists because of relatively higher reimbursement for neurologists, they observed.
One of the study coauthors disclosed ties to Aveanna Healthcare, a company that delivers home health and hospice care.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Understanding the relationship between life satisfaction and cognitive decline
Every day, we depend on our working memory, spatial cognition, and processing speed abilities to optimize productivity, interpersonal interactions, and psychological wellbeing. These cognitive functioning indices relate closely with academic and work performance, managing emotions, physical fitness, and a sense of fulfillment in personal and work relationships. They are linked intimately to complex cognitive skills (van Dijk et al., 2020). It is thus imperative to identify modifiable predictors of cognitive functioning in the brain to protect against aging-related cognitive decline and maximize the quality of life.
A decline in life satisfaction can worsen cognitive functioning over long periods via lifestyle factors (e.g., suboptimal diet and nutrition, lack of exercise) (Ratigan et al., 2016). Inadequate engagement in these health-enhancing pursuits could build up inflammation in EF-linked brain areas, thus negatively impacting cognitive functioning in adulthood (Grant et al., 2009). Possible pathways include long-term wear and tear of the hypothalamic-pituitary axis and brain regions linked to executive functioning (Zainal and Newman, 2022a). These processes may deteriorate working memory, spatial cognition, and processing speed across time.
Similarly, it is plausible that a reduction in cognitive functioning may lead to a long-term decrease in life satisfaction. Working memory, processing speed, spatial cognition, and related capacities are essential to meaningful activities and feelings of gratification in personal and professional relationships and other spheres of health throughout life (Baumeister et al., 2007). These cognitive functioning markers safeguard against reduced life satisfaction by facilitating effective problem-solving, and choices (Swanson and Fung, 2016). For example, stronger working memory, processing speed, and related domains coincided with better tolerance for stress and trading off immediate rewards for long-term values and life goals (Hofmann et al., 2012). Therefore, reduction in cognitive functioning abilities could precede a future decline in life satisfaction.
Nonetheless, the literature on this topic has several limitations. Most of the studies have been cross-sectional (i.e., across a single time-point) and thus do not permit inferences between cause and effect (e.g., Toh et al., 2020). Also, most studies used statistical methods that did not differentiate between between-person (trait-like individual differences) and within-person (state-like) relations. Distinguishing within- and between-person relations is necessary because they may vary in magnitude and direction. The preceding theories emphasize change-to-future change relations within persons rather than between persons (Wright and Woods, 2020).
Clinical implications
Our recent work (Zainal and Newman, 2022b) added to the literature by using an advanced statistical method to determine the relations between change in life satisfaction and future change in cognitive functioning domains within persons. The choice of an advanced statistical technique minimizes biases due to the passage of time and assessment unreliability. It also adjusts for between-person effects (Klopack and Wickrama, 2020). Improving understanding of the within-person factors leading to the deterioration of cognitive functioning and life satisfaction is crucial given the rising rates of psychiatric and neurocognitive illnesses (Cui et al., 2020). Identifying these changeable risk factors can optimize prevention, early detection, and treatment approaches.
Specifically, we analyzed the publicly available Swedish Adoption/Twin Study of Aging (SATSA) dataset (Petkus et al., 2017). Their dataset comprised 520 middle- to older-aged twin adults without dementia. Participants provided data across 23 years with five time points. Each time lag ranged from 3 to 11 years. The analyses demonstrated that greater decreases in life satisfaction predicted larger future declines in processing speed, verbal working memory, and spatial cognition. Moreover, declines in verbal working memory and processing speed predicted a reduction in life satisfaction. However, change in spatial awareness did not predict change in life satisfaction.
Our study offers multiple theoretical perspectives. Scar theories propose that decreased life satisfaction and related mental health problems can compromise working memory, processing speed, and spatial cognition in the long term. This scarring process occurs through the buildup of allostatic load, such as increased biomarkers of chronic stress (e.g., cortisol) and inflammation (e.g., interleukin-6, C-reactive protein) (Fancourt and Steptoe, 2020; Zainal and Newman, 2021a). Also, findings suggest the importance of executive functioning domains to attain desired milestones and aspirations to enhance a sense of fulfillment (Baddeley, 2013; Toh and Yang, 2020). Reductions in these cognitive functioning capacities could, over time, adversely affect the ability to engage in daily living activities and manage negative moods.
Limitations of our study include the lack of a multiple-assessment approach to measuring diverse cognitive functioning domains. Also, the absence of cognitive self-reports is a shortcoming since perceived cognitive difficulties might not align with performance on cognitive tests. Relatedly, future studies should administer cognitive tests that parallel and transfer to everyday tasks. However, our study’s strengths include the robust findings across different intervals between study waves, advanced statistics, and the large sample size.
If future studies replicate a similar pattern of results, the clinical applications of this study merit attention. Mindfulness-based interventions can promote working memory, sustained awareness, and spatial cognition or protect against cognitive decline (Jha et al., 2019; Zainal and Newman, 2021b). Further, clinical science can profit from exploring cognitive-behavioral therapies to improve adults’ cognitive function or life satisfaction (Sok et al., 2021).
Dr. Zainal recently accepted a 2-year postdoctoral research associate position at Harvard Medical School, Boston, starting in summer 2022. She received her Ph.D. from Pennsylvania State University, University Park, and completed a predoctoral clinical fellowship at the HMS-affiliated Massachusetts General Hospital – Cognitive Behavioral Scientist Track. Her research interests focus on how executive functioning, social cognition, and cognitive-behavioral strategies link to the etiology, maintenance, and treatment of anxiety and depressive disorders. Dr. Newman is a professor of psychology and psychiatry, and the director of the Center for the Treatment of Anxiety and Depression, at Pennsylvania State University. She has conducted basic and applied research on anxiety disorders and depression and has published over 200 papers on these topics.
Sources
Baddeley A. Working memory and emotion: Ruminations on a theory of depression. Rev Gen Psychol. 2013;17(1):20-7. doi: 10.1037/a0030029.
Baumeister RF et al. “Self-regulation and the executive function: The self as controlling agent,” in Social Psychology: Handbook of Basic Principles, 2nd ed. (pp. 516-39). The Guilford Press: New York, 2007.
Cui L et al. Prevalence of alzheimer’s disease and parkinson’s disease in China: An updated systematical analysis. Front Aging Neurosci. 2020 Dec 21;12:603854. doi: 10.3389/fnagi.2020.603854.
Fancourt D and Steptoe A. The longitudinal relationship between changes in wellbeing and inflammatory markers: Are associations independent of depression? Brain Behav Immun. 2020 Jan;83:146-52. doi: 10.1016/j.bbi.2019.10.004.
Grant N et al. The relationship between life satisfaction and health behavior: A cross-cultural analysis of young adults. Int J Behav Med. 2009;16(3):259-68. doi: 10.1007/s12529-009-9032-x.
Hofmann W et al. Executive functions and self-regulation. Trends Cogn Sci. 2012 Mar;16(3):174-80. doi: 10.1016/j.tics.2012.01.006.
Jha AP et al. Bolstering cognitive resilience via train-the-trainer delivery of mindfulness training in applied high-demand settings. Mindfulness. 2019;11(3):683-97. doi: 10.1007/s12671-019-01284-7.
Klopack ET and Wickrama K. Modeling latent change score analysis and extensions in Mplus: A practical guide for researchers. Struct Equ Modeling. 2020;27(1):97-110. doi: 10.1080/10705511.2018.1562929.
Petkus AJ et al. Temporal dynamics of cognitive performance and anxiety across older adulthood. Psychol Aging. 2017 May;32(3):278-92. doi: 10.1037/pag0000164.
Ratigan A et al. Sex differences in the association of physical function and cognitive function with life satisfaction in older age: The Rancho Bernardo Study. Maturitas. 2016 Jul;89:29-35. doi: 10.1016/j.maturitas.2016.04.007.
Sok S et al. Effects of cognitive/exercise dual-task program on the cognitive function, health status, depression, and life satisfaction of the elderly living in the community. Int J Environ Res Public Health. 2021 Jul 24;18(15):7848. doi: 10.3390/ijerph18157848.
Swanson HL and Fung W. Working memory components and problem-solving accuracy: Are there multiple pathways? J Educ Psychol. 2016;108(8):1153-77. doi: 10.1037/edu0000116.
Toh WX and Yang H. Executive function moderates the effect of reappraisal on life satisfaction: A latent variable analysis. Emotion. 2020;22(3):554-71. doi: 10.1037/emo0000907.
Toh WX et al. Executive function and subjective wellbeing in middle and late adulthood. J Gerontol B Psychol Sci Soc Sci. 2020 Jun 2;75(6):e69-e77. doi: 10.1093/geronb/gbz006.
van Dijk DM, et al. Cognitive functioning, sleep quality, and work performance in non-clinical burnout: The role of working memory. PLoS One. 2020 Apr 23;15(4):e0231906. doi: 10.1371/journal.pone.0231906.
Wright AGC and Woods WC. Personalized models of psychopathology. Annu Rev Clin Psychol. 2020 May 7;16:49-74. doi: 10.1146/annurev-clinpsy-102419-125032.
Zainal NH and Newman MG. (2021a). Depression and worry symptoms predict future executive functioning impairment via inflammation. Psychol Med. 2021 Mar 3;1-11. doi: 10.1017/S0033291721000398.
Zainal NH and Newman MG. (2021b). Mindfulness enhances cognitive functioning: A meta-analysis of 111 randomized controlled trials. PsyArXiv Preprints. 2021 May 11. doi: 10.31234/osf.io/vzxw7.
Zainal NH and Newman MG. (2022a). Inflammation mediates depression and generalized anxiety symptoms predicting executive function impairment after 18 years. J Affect Disord. 2022 Jan 1;296:465-75. doi: 10.1016/j.jad.2021.08.077.
Zainal NH and Newman MG. (2022b). Life satisfaction prevents decline in working memory, spatial cognition, and processing speed: Latent change score analyses across 23 years. Eur Psychiatry. 2022 Apr 19;65(1):1-55. doi: 10.1192/j.eurpsy.2022.19.
Every day, we depend on our working memory, spatial cognition, and processing speed abilities to optimize productivity, interpersonal interactions, and psychological wellbeing. These cognitive functioning indices relate closely with academic and work performance, managing emotions, physical fitness, and a sense of fulfillment in personal and work relationships. They are linked intimately to complex cognitive skills (van Dijk et al., 2020). It is thus imperative to identify modifiable predictors of cognitive functioning in the brain to protect against aging-related cognitive decline and maximize the quality of life.
A decline in life satisfaction can worsen cognitive functioning over long periods via lifestyle factors (e.g., suboptimal diet and nutrition, lack of exercise) (Ratigan et al., 2016). Inadequate engagement in these health-enhancing pursuits could build up inflammation in EF-linked brain areas, thus negatively impacting cognitive functioning in adulthood (Grant et al., 2009). Possible pathways include long-term wear and tear of the hypothalamic-pituitary axis and brain regions linked to executive functioning (Zainal and Newman, 2022a). These processes may deteriorate working memory, spatial cognition, and processing speed across time.
Similarly, it is plausible that a reduction in cognitive functioning may lead to a long-term decrease in life satisfaction. Working memory, processing speed, spatial cognition, and related capacities are essential to meaningful activities and feelings of gratification in personal and professional relationships and other spheres of health throughout life (Baumeister et al., 2007). These cognitive functioning markers safeguard against reduced life satisfaction by facilitating effective problem-solving, and choices (Swanson and Fung, 2016). For example, stronger working memory, processing speed, and related domains coincided with better tolerance for stress and trading off immediate rewards for long-term values and life goals (Hofmann et al., 2012). Therefore, reduction in cognitive functioning abilities could precede a future decline in life satisfaction.
Nonetheless, the literature on this topic has several limitations. Most of the studies have been cross-sectional (i.e., across a single time-point) and thus do not permit inferences between cause and effect (e.g., Toh et al., 2020). Also, most studies used statistical methods that did not differentiate between between-person (trait-like individual differences) and within-person (state-like) relations. Distinguishing within- and between-person relations is necessary because they may vary in magnitude and direction. The preceding theories emphasize change-to-future change relations within persons rather than between persons (Wright and Woods, 2020).
Clinical implications
Our recent work (Zainal and Newman, 2022b) added to the literature by using an advanced statistical method to determine the relations between change in life satisfaction and future change in cognitive functioning domains within persons. The choice of an advanced statistical technique minimizes biases due to the passage of time and assessment unreliability. It also adjusts for between-person effects (Klopack and Wickrama, 2020). Improving understanding of the within-person factors leading to the deterioration of cognitive functioning and life satisfaction is crucial given the rising rates of psychiatric and neurocognitive illnesses (Cui et al., 2020). Identifying these changeable risk factors can optimize prevention, early detection, and treatment approaches.
Specifically, we analyzed the publicly available Swedish Adoption/Twin Study of Aging (SATSA) dataset (Petkus et al., 2017). Their dataset comprised 520 middle- to older-aged twin adults without dementia. Participants provided data across 23 years with five time points. Each time lag ranged from 3 to 11 years. The analyses demonstrated that greater decreases in life satisfaction predicted larger future declines in processing speed, verbal working memory, and spatial cognition. Moreover, declines in verbal working memory and processing speed predicted a reduction in life satisfaction. However, change in spatial awareness did not predict change in life satisfaction.
Our study offers multiple theoretical perspectives. Scar theories propose that decreased life satisfaction and related mental health problems can compromise working memory, processing speed, and spatial cognition in the long term. This scarring process occurs through the buildup of allostatic load, such as increased biomarkers of chronic stress (e.g., cortisol) and inflammation (e.g., interleukin-6, C-reactive protein) (Fancourt and Steptoe, 2020; Zainal and Newman, 2021a). Also, findings suggest the importance of executive functioning domains to attain desired milestones and aspirations to enhance a sense of fulfillment (Baddeley, 2013; Toh and Yang, 2020). Reductions in these cognitive functioning capacities could, over time, adversely affect the ability to engage in daily living activities and manage negative moods.
Limitations of our study include the lack of a multiple-assessment approach to measuring diverse cognitive functioning domains. Also, the absence of cognitive self-reports is a shortcoming since perceived cognitive difficulties might not align with performance on cognitive tests. Relatedly, future studies should administer cognitive tests that parallel and transfer to everyday tasks. However, our study’s strengths include the robust findings across different intervals between study waves, advanced statistics, and the large sample size.
If future studies replicate a similar pattern of results, the clinical applications of this study merit attention. Mindfulness-based interventions can promote working memory, sustained awareness, and spatial cognition or protect against cognitive decline (Jha et al., 2019; Zainal and Newman, 2021b). Further, clinical science can profit from exploring cognitive-behavioral therapies to improve adults’ cognitive function or life satisfaction (Sok et al., 2021).
Dr. Zainal recently accepted a 2-year postdoctoral research associate position at Harvard Medical School, Boston, starting in summer 2022. She received her Ph.D. from Pennsylvania State University, University Park, and completed a predoctoral clinical fellowship at the HMS-affiliated Massachusetts General Hospital – Cognitive Behavioral Scientist Track. Her research interests focus on how executive functioning, social cognition, and cognitive-behavioral strategies link to the etiology, maintenance, and treatment of anxiety and depressive disorders. Dr. Newman is a professor of psychology and psychiatry, and the director of the Center for the Treatment of Anxiety and Depression, at Pennsylvania State University. She has conducted basic and applied research on anxiety disorders and depression and has published over 200 papers on these topics.
Sources
Baddeley A. Working memory and emotion: Ruminations on a theory of depression. Rev Gen Psychol. 2013;17(1):20-7. doi: 10.1037/a0030029.
Baumeister RF et al. “Self-regulation and the executive function: The self as controlling agent,” in Social Psychology: Handbook of Basic Principles, 2nd ed. (pp. 516-39). The Guilford Press: New York, 2007.
Cui L et al. Prevalence of alzheimer’s disease and parkinson’s disease in China: An updated systematical analysis. Front Aging Neurosci. 2020 Dec 21;12:603854. doi: 10.3389/fnagi.2020.603854.
Fancourt D and Steptoe A. The longitudinal relationship between changes in wellbeing and inflammatory markers: Are associations independent of depression? Brain Behav Immun. 2020 Jan;83:146-52. doi: 10.1016/j.bbi.2019.10.004.
Grant N et al. The relationship between life satisfaction and health behavior: A cross-cultural analysis of young adults. Int J Behav Med. 2009;16(3):259-68. doi: 10.1007/s12529-009-9032-x.
Hofmann W et al. Executive functions and self-regulation. Trends Cogn Sci. 2012 Mar;16(3):174-80. doi: 10.1016/j.tics.2012.01.006.
Jha AP et al. Bolstering cognitive resilience via train-the-trainer delivery of mindfulness training in applied high-demand settings. Mindfulness. 2019;11(3):683-97. doi: 10.1007/s12671-019-01284-7.
Klopack ET and Wickrama K. Modeling latent change score analysis and extensions in Mplus: A practical guide for researchers. Struct Equ Modeling. 2020;27(1):97-110. doi: 10.1080/10705511.2018.1562929.
Petkus AJ et al. Temporal dynamics of cognitive performance and anxiety across older adulthood. Psychol Aging. 2017 May;32(3):278-92. doi: 10.1037/pag0000164.
Ratigan A et al. Sex differences in the association of physical function and cognitive function with life satisfaction in older age: The Rancho Bernardo Study. Maturitas. 2016 Jul;89:29-35. doi: 10.1016/j.maturitas.2016.04.007.
Sok S et al. Effects of cognitive/exercise dual-task program on the cognitive function, health status, depression, and life satisfaction of the elderly living in the community. Int J Environ Res Public Health. 2021 Jul 24;18(15):7848. doi: 10.3390/ijerph18157848.
Swanson HL and Fung W. Working memory components and problem-solving accuracy: Are there multiple pathways? J Educ Psychol. 2016;108(8):1153-77. doi: 10.1037/edu0000116.
Toh WX and Yang H. Executive function moderates the effect of reappraisal on life satisfaction: A latent variable analysis. Emotion. 2020;22(3):554-71. doi: 10.1037/emo0000907.
Toh WX et al. Executive function and subjective wellbeing in middle and late adulthood. J Gerontol B Psychol Sci Soc Sci. 2020 Jun 2;75(6):e69-e77. doi: 10.1093/geronb/gbz006.
van Dijk DM, et al. Cognitive functioning, sleep quality, and work performance in non-clinical burnout: The role of working memory. PLoS One. 2020 Apr 23;15(4):e0231906. doi: 10.1371/journal.pone.0231906.
Wright AGC and Woods WC. Personalized models of psychopathology. Annu Rev Clin Psychol. 2020 May 7;16:49-74. doi: 10.1146/annurev-clinpsy-102419-125032.
Zainal NH and Newman MG. (2021a). Depression and worry symptoms predict future executive functioning impairment via inflammation. Psychol Med. 2021 Mar 3;1-11. doi: 10.1017/S0033291721000398.
Zainal NH and Newman MG. (2021b). Mindfulness enhances cognitive functioning: A meta-analysis of 111 randomized controlled trials. PsyArXiv Preprints. 2021 May 11. doi: 10.31234/osf.io/vzxw7.
Zainal NH and Newman MG. (2022a). Inflammation mediates depression and generalized anxiety symptoms predicting executive function impairment after 18 years. J Affect Disord. 2022 Jan 1;296:465-75. doi: 10.1016/j.jad.2021.08.077.
Zainal NH and Newman MG. (2022b). Life satisfaction prevents decline in working memory, spatial cognition, and processing speed: Latent change score analyses across 23 years. Eur Psychiatry. 2022 Apr 19;65(1):1-55. doi: 10.1192/j.eurpsy.2022.19.
Every day, we depend on our working memory, spatial cognition, and processing speed abilities to optimize productivity, interpersonal interactions, and psychological wellbeing. These cognitive functioning indices relate closely with academic and work performance, managing emotions, physical fitness, and a sense of fulfillment in personal and work relationships. They are linked intimately to complex cognitive skills (van Dijk et al., 2020). It is thus imperative to identify modifiable predictors of cognitive functioning in the brain to protect against aging-related cognitive decline and maximize the quality of life.
A decline in life satisfaction can worsen cognitive functioning over long periods via lifestyle factors (e.g., suboptimal diet and nutrition, lack of exercise) (Ratigan et al., 2016). Inadequate engagement in these health-enhancing pursuits could build up inflammation in EF-linked brain areas, thus negatively impacting cognitive functioning in adulthood (Grant et al., 2009). Possible pathways include long-term wear and tear of the hypothalamic-pituitary axis and brain regions linked to executive functioning (Zainal and Newman, 2022a). These processes may deteriorate working memory, spatial cognition, and processing speed across time.
Similarly, it is plausible that a reduction in cognitive functioning may lead to a long-term decrease in life satisfaction. Working memory, processing speed, spatial cognition, and related capacities are essential to meaningful activities and feelings of gratification in personal and professional relationships and other spheres of health throughout life (Baumeister et al., 2007). These cognitive functioning markers safeguard against reduced life satisfaction by facilitating effective problem-solving, and choices (Swanson and Fung, 2016). For example, stronger working memory, processing speed, and related domains coincided with better tolerance for stress and trading off immediate rewards for long-term values and life goals (Hofmann et al., 2012). Therefore, reduction in cognitive functioning abilities could precede a future decline in life satisfaction.
Nonetheless, the literature on this topic has several limitations. Most of the studies have been cross-sectional (i.e., across a single time-point) and thus do not permit inferences between cause and effect (e.g., Toh et al., 2020). Also, most studies used statistical methods that did not differentiate between between-person (trait-like individual differences) and within-person (state-like) relations. Distinguishing within- and between-person relations is necessary because they may vary in magnitude and direction. The preceding theories emphasize change-to-future change relations within persons rather than between persons (Wright and Woods, 2020).
Clinical implications
Our recent work (Zainal and Newman, 2022b) added to the literature by using an advanced statistical method to determine the relations between change in life satisfaction and future change in cognitive functioning domains within persons. The choice of an advanced statistical technique minimizes biases due to the passage of time and assessment unreliability. It also adjusts for between-person effects (Klopack and Wickrama, 2020). Improving understanding of the within-person factors leading to the deterioration of cognitive functioning and life satisfaction is crucial given the rising rates of psychiatric and neurocognitive illnesses (Cui et al., 2020). Identifying these changeable risk factors can optimize prevention, early detection, and treatment approaches.
Specifically, we analyzed the publicly available Swedish Adoption/Twin Study of Aging (SATSA) dataset (Petkus et al., 2017). Their dataset comprised 520 middle- to older-aged twin adults without dementia. Participants provided data across 23 years with five time points. Each time lag ranged from 3 to 11 years. The analyses demonstrated that greater decreases in life satisfaction predicted larger future declines in processing speed, verbal working memory, and spatial cognition. Moreover, declines in verbal working memory and processing speed predicted a reduction in life satisfaction. However, change in spatial awareness did not predict change in life satisfaction.
Our study offers multiple theoretical perspectives. Scar theories propose that decreased life satisfaction and related mental health problems can compromise working memory, processing speed, and spatial cognition in the long term. This scarring process occurs through the buildup of allostatic load, such as increased biomarkers of chronic stress (e.g., cortisol) and inflammation (e.g., interleukin-6, C-reactive protein) (Fancourt and Steptoe, 2020; Zainal and Newman, 2021a). Also, findings suggest the importance of executive functioning domains to attain desired milestones and aspirations to enhance a sense of fulfillment (Baddeley, 2013; Toh and Yang, 2020). Reductions in these cognitive functioning capacities could, over time, adversely affect the ability to engage in daily living activities and manage negative moods.
Limitations of our study include the lack of a multiple-assessment approach to measuring diverse cognitive functioning domains. Also, the absence of cognitive self-reports is a shortcoming since perceived cognitive difficulties might not align with performance on cognitive tests. Relatedly, future studies should administer cognitive tests that parallel and transfer to everyday tasks. However, our study’s strengths include the robust findings across different intervals between study waves, advanced statistics, and the large sample size.
If future studies replicate a similar pattern of results, the clinical applications of this study merit attention. Mindfulness-based interventions can promote working memory, sustained awareness, and spatial cognition or protect against cognitive decline (Jha et al., 2019; Zainal and Newman, 2021b). Further, clinical science can profit from exploring cognitive-behavioral therapies to improve adults’ cognitive function or life satisfaction (Sok et al., 2021).
Dr. Zainal recently accepted a 2-year postdoctoral research associate position at Harvard Medical School, Boston, starting in summer 2022. She received her Ph.D. from Pennsylvania State University, University Park, and completed a predoctoral clinical fellowship at the HMS-affiliated Massachusetts General Hospital – Cognitive Behavioral Scientist Track. Her research interests focus on how executive functioning, social cognition, and cognitive-behavioral strategies link to the etiology, maintenance, and treatment of anxiety and depressive disorders. Dr. Newman is a professor of psychology and psychiatry, and the director of the Center for the Treatment of Anxiety and Depression, at Pennsylvania State University. She has conducted basic and applied research on anxiety disorders and depression and has published over 200 papers on these topics.
Sources
Baddeley A. Working memory and emotion: Ruminations on a theory of depression. Rev Gen Psychol. 2013;17(1):20-7. doi: 10.1037/a0030029.
Baumeister RF et al. “Self-regulation and the executive function: The self as controlling agent,” in Social Psychology: Handbook of Basic Principles, 2nd ed. (pp. 516-39). The Guilford Press: New York, 2007.
Cui L et al. Prevalence of alzheimer’s disease and parkinson’s disease in China: An updated systematical analysis. Front Aging Neurosci. 2020 Dec 21;12:603854. doi: 10.3389/fnagi.2020.603854.
Fancourt D and Steptoe A. The longitudinal relationship between changes in wellbeing and inflammatory markers: Are associations independent of depression? Brain Behav Immun. 2020 Jan;83:146-52. doi: 10.1016/j.bbi.2019.10.004.
Grant N et al. The relationship between life satisfaction and health behavior: A cross-cultural analysis of young adults. Int J Behav Med. 2009;16(3):259-68. doi: 10.1007/s12529-009-9032-x.
Hofmann W et al. Executive functions and self-regulation. Trends Cogn Sci. 2012 Mar;16(3):174-80. doi: 10.1016/j.tics.2012.01.006.
Jha AP et al. Bolstering cognitive resilience via train-the-trainer delivery of mindfulness training in applied high-demand settings. Mindfulness. 2019;11(3):683-97. doi: 10.1007/s12671-019-01284-7.
Klopack ET and Wickrama K. Modeling latent change score analysis and extensions in Mplus: A practical guide for researchers. Struct Equ Modeling. 2020;27(1):97-110. doi: 10.1080/10705511.2018.1562929.
Petkus AJ et al. Temporal dynamics of cognitive performance and anxiety across older adulthood. Psychol Aging. 2017 May;32(3):278-92. doi: 10.1037/pag0000164.
Ratigan A et al. Sex differences in the association of physical function and cognitive function with life satisfaction in older age: The Rancho Bernardo Study. Maturitas. 2016 Jul;89:29-35. doi: 10.1016/j.maturitas.2016.04.007.
Sok S et al. Effects of cognitive/exercise dual-task program on the cognitive function, health status, depression, and life satisfaction of the elderly living in the community. Int J Environ Res Public Health. 2021 Jul 24;18(15):7848. doi: 10.3390/ijerph18157848.
Swanson HL and Fung W. Working memory components and problem-solving accuracy: Are there multiple pathways? J Educ Psychol. 2016;108(8):1153-77. doi: 10.1037/edu0000116.
Toh WX and Yang H. Executive function moderates the effect of reappraisal on life satisfaction: A latent variable analysis. Emotion. 2020;22(3):554-71. doi: 10.1037/emo0000907.
Toh WX et al. Executive function and subjective wellbeing in middle and late adulthood. J Gerontol B Psychol Sci Soc Sci. 2020 Jun 2;75(6):e69-e77. doi: 10.1093/geronb/gbz006.
van Dijk DM, et al. Cognitive functioning, sleep quality, and work performance in non-clinical burnout: The role of working memory. PLoS One. 2020 Apr 23;15(4):e0231906. doi: 10.1371/journal.pone.0231906.
Wright AGC and Woods WC. Personalized models of psychopathology. Annu Rev Clin Psychol. 2020 May 7;16:49-74. doi: 10.1146/annurev-clinpsy-102419-125032.
Zainal NH and Newman MG. (2021a). Depression and worry symptoms predict future executive functioning impairment via inflammation. Psychol Med. 2021 Mar 3;1-11. doi: 10.1017/S0033291721000398.
Zainal NH and Newman MG. (2021b). Mindfulness enhances cognitive functioning: A meta-analysis of 111 randomized controlled trials. PsyArXiv Preprints. 2021 May 11. doi: 10.31234/osf.io/vzxw7.
Zainal NH and Newman MG. (2022a). Inflammation mediates depression and generalized anxiety symptoms predicting executive function impairment after 18 years. J Affect Disord. 2022 Jan 1;296:465-75. doi: 10.1016/j.jad.2021.08.077.
Zainal NH and Newman MG. (2022b). Life satisfaction prevents decline in working memory, spatial cognition, and processing speed: Latent change score analyses across 23 years. Eur Psychiatry. 2022 Apr 19;65(1):1-55. doi: 10.1192/j.eurpsy.2022.19.
Primary care now offering physicians the 26.7-hour day
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
Taking ‘not enough hours in the day’ to new heights
It’s no secret that there’s a big doctor shortage in the United States. Going through medical school is long, expensive, and stressful, and it’s not like those long, stressful hours stop once you finally do get that degree. There is, however, an excellent reason to take that dive into doctorhood: You’ll gain mastery over time itself.
A study from the University of Chicago, Johns Hopkins University, and Imperial College London has revealed the truth. By using data pulled from the National Health and Nutrition Examination Survey, the researchers found that primary care physicians who see an average number of patients and follow all the current national guidelines for preventive care, chronic disease care, and acute care – plus administrative tasks – must work 26.7 hours a day. That works out to 14.1 hours of preventive care, 7.2 hours of chronic disease care, 2.2 hours of acute care, and 3.2 hours of documentation and inbox management.
Astute readers may note that this is a bit more than the traditional 8-hour workday. It is, in fact, more hours than there actually are in a day. As it turns out, Doctor Strange is more of a documentary than …
Hang on, we’re receiving word that doctors are not in fact wizards who can bend time and space to their will, nor are they sitting on a stash of Time-Turners they saved from the Ministry of Magic before Voldemort destroyed them all. They are, according to the study, overworked and overburdened with too many things and too little time. This is why outcomes haven’t improved despite technological advances and why burnout is so common. We’d be burned out too, having to work temporally impossible hours.
The study authors suggested a team-based approach to medicine that would spread the workload out to nurses, physician assistants, dietitians, etc., estimating that about two-thirds of what a primary care physician does can be handled by someone else. A team-based approach would reduce the physician’s required hours down to 9.3 hours a day, which is at least physically possible. It’s either that or we make the day longer, which sounds like the plot of an episode of Futurama. Swap overwork for global warming and a longer day for a longer year and it is actually the plot of an episode of Futurama.
After a hard day of thinking, brains need their rest
Do you ever feel like you have no more capacity to think or make any more decisions after a long day at work? Do you need a few extra cups of coffee to even make it through the day, even though you’re mostly just sitting around talking and typing? Have we got the research for you: Mental exhaustion is an actual thing. Imagine that double whammy of having a job that’s physically and mentally demanding.
A recent study in Current Biology explained why we feel so exhausted after doing something mentally demanding for several hours. Over that time, glutamate builds up in synapses of the prefrontal cortex, which affects our decision making and leads to cognitive lethargy. Your brain eventually becomes more interested in tasks that are less mentally fatiguing, and that’s probably why you’re reading this LOTME right now instead of getting back to work.
“Our findings show that cognitive work results in a true functional alteration – accumulation of noxious substances – so fatigue would indeed be a signal that makes us stop working but for a different purpose: to preserve the integrity of brain functioning,” senior author Mathias Pessiglione of Pitié-Salpêtrière University, Paris, said in a written statement.
The group of researchers conducted studies by using magnetic resonance spectroscopy to look at two groups of people over the course of a workday: One group had mentally tasking jobs and one didn’t. Those who had to think harder for their jobs had more signs of fatigue, such as reduced pupil dilation and glutamate in synapses of the prefrontal cortex. They also looked for more rewards that required less thinking.
For those whose mentally exhausting jobs probably won’t get better or change, the researchers suggest getting as much rest as possible. Those who don’t have that option will have to continue drinking those 7 cups of coffee a day. ... and reading LOTME.
Hmm, might be a new tagline for us in there somewhere. LOTME: Tired brains love us? When you’re too tired to think, think of LOTME? You can’t spell mental exhaustion without L-O-T-M-E?
Testosterone shows its warm and fuzzy side
Stereotypically, men are loud, knuckle-dragging Neanderthals. The hair coming out of our faces is kind of a dead giveaway, right? We grunt, we scratch, we start wars, we watch sports on TV. But why? It’s the testosterone. Everyone knows that. Testosterone makes men aggressive … or does it?
Since this sort of research generally isn’t done with actual men, investigators at Emory University used Mongolian gerbils. The advantage being that males exhibit cuddling behavior after females become pregnant and they don’t watch a lot of sports on TV. They introduced a male and female gerbil, who then formed a pair bond and the female became pregnant. When the male started displaying cuddling behaviors, the researchers injected him with testosterone, expecting to see his antisocial side.
“Instead, we were surprised that a male gerbil became even more cuddly and prosocial with his partner. He became like ‘super partner,’ ” lead author Aubrey Kelly, PhD, said in a written statement from the university.
For the next experiment, the female was removed and another male was introduced to a male who had already received a testosterone injection. That male was surprisingly unaggressive toward the intruder, at least initially. Then he received a second injection of testosterone. “It was like they suddenly woke up and realized they weren’t supposed to be friendly in that context,” Dr. Kelly said.
The testosterone seemed to influence the activity of oxytocin, the so-called “love hormone,” the investigators suggested. “It’s surprising because normally we think of testosterone as increasing sexual behaviors and aggression. But we’ve shown that it can have more nuanced effects, depending on the social context.”
The researchers were not as surprised when their use of the phrase “super partner” led to a bidding war between DC and Marvel. Then came the contact from the Department of Defense, wondering about weaponized testosterone: Would it be possible for some sort of bomb to turn Vlad “the Impaler” Putin into Vlad “the Cuddler” Putin?
Are instruments spreading the sounds of COVID?
COVID restrictions are practically a thing of the past now. With more people laxed on being in close proximity to each other and the CDC not even recommending social distancing anymore, live concerts and events are back in full swing. But with new variants on the rise and people being a little more cautious, should we be worried about musical instruments spreading COVID?
Yes and no.
A study published in Physics of Fluids looked at wind instruments specifically and how much aerosol is produced and dispersed when playing them. For the study, the investigators measured fog particles with a laser and aerosol concentration with a particle counter to see how fast these particles decay in the air from the distance of the instrument.
Musicians in an orchestra typically would sit close together to produce the best sound, but with COVID that became an issue, senior author Paulo Arratia of the University of Pennsylvania, Philadelphia, noted in a separate written statement. By looking at the distance traveled by the particles coming from a single instrument and how quickly they decayed, they could determine if sitting in close proximity is an actual threat.
Well, the threat was no greater than talking to someone face to face. Particle exit speeds were lower than for a cough or a sneeze, and the maximum decay length was 2 meters from the instrument’s opening.
But that’s just one instrument: What kind of impact does a whole orchestra have on a space? The researchers are looking into that too, but for now they suggest that musicians continue to stay 6 feet away from each other.
So, yeah, there is a threat, but it’s probably safer for you to see that orchestra than have someone sneeze on you.
Music to our ears.
What ketamine and psilocybin can and cannot do in depression
Recent studies with hallucinogens have raised hopes for an effective drug-based therapy to treat chronic depression. At the German Congress of Psychosomatic Medicine and Psychotherapy, Torsten Passie, MD, PhD, professor of psychiatry and psychotherapy at the Hannover (Germay) Medical School, gave a presentation on the current state of psilocybin and ketamine/esketamine research.
Dr. Passie, who also is head physician of the specialist unit for addiction and addiction prevention at the Diakonisches Werk in Hannover, has been investigating hallucinogenic substances and their application in psychotherapy for decades.
New therapies sought
In depression, gloom extends beyond the patient’s mood. For some time there has been little cause for joy with regard to chronic depression therapy. Established drug therapies hardly perform any better than placebo in meta-analyses, as a study recently confirmed. The pharmaceutical industry pulled out of psycho-pharmaceutical development more than 10 years ago. What’s more, the number of cases is rising, especially among young people, and there are long waiting times for psychotherapy appointments.
It is no wonder that some are welcoming new drug-based approaches with lysergic acid diethylamide (LSD)–like hallucinogens. In 2016, a study on psilocybin was published in The Lancet Psychiatry, although the study was unblinded and included only 24 patients.
Evoking emotions
A range of substances can be classed as hallucinogens, including psilocybin, mescaline, LSD, 3,4-methylenedioxy-methamphetamine (MDMA, also known as ecstasy), and ketamine.
Taking hallucinogens can cause a release of serotonin and dopamine, an increase in activity levels in the brain, a shift in stimulus filtering, an increase in the production of internal stimuli (inner experiences), and a change in sensory integration (for example, synesthesia).
Besides falling into a dreamlike state, patients can achieve an expansion or narrowing of consciousness if they focus on an inner experience. Internal perception increases. Perceptual routines are broken apart. Thought processes become more image-based and are more associative than normal.
Patients therefore are more capable of making new and unusual connections between different biographical or current situations. Previously unconscious ideas can become conscious. At higher doses, ego loss can occur, which can be associated with a mystical feeling of connectedness.
Hallucinogens mainly evoke and heighten emotions. Those effects may be experienced strongly as internal visions or in physical manifestations (for example, crying or laughing). In contrast, conventional antidepressants work by suppressing emotions (that is, emotional blunting).
These different mechanisms result in two contrasting management strategies. For example, SSRI antidepressants cause a patient to perceive workplace bullying as less severe and to do nothing to change the situation; the patient remains passive.
In contrast, a therapeutically guided, emotionally activating experience on hallucinogens can help the patient to try more actively to change the stressful situation.
Ketamine has a special place among hallucinogens. Unlike other hallucinogens, ketamine causes a strong clouding of consciousness, a reduction in physical sensory perception, and significant disruption in thinking and memory. It is therefore only suitable as a short-term intervention and is therapeutically impractical over the long term.
Ketamine’s effects
Ketamine, a racemic mixture of the enantiomers S-ketamine and R-ketamine, was originally used only as an analgesic and anesthetic. Owing to its rapid antidepressant effect, it has since also been used as an emergency medication for severe depression, sometimes in combination with SSRIs or serotonin noradrenaline reuptake inhibitors.
Approximately 60% of patients respond to the treatment. Whereas with conventional antidepressants, onset of action requires 10-14 days, ketamine is effective within a few hours. However, relapse always occurs, usually very quickly. After 2-3 days, the effect is usually approximately that of a placebo. An administration interval of about 2 days is optimal. However, “resistance” to the effect often develops after some time: the drug’s antidepressant effect diminishes.
Ketamine also has some unpleasant side effects, such as depersonalization, dissociation, impaired thinking, nystagmus, and psychotomimetic effects. Nausea and vomiting also occur. Interestingly, the latter does not bother the patient much, owing to the drug’s psychological effects, and it does not lead to treatment discontinuation, said Dr. Passie, who described his clinical experiences with ketamine.
Since ketamine causes a considerable clouding of consciousness, sensory disorders, and significant memory problems, it is not suitable for psychedelic-assisted psychotherapy, unlike LSD or psilocybin, he emphasized.
Ketamine 2.0?
Esketamine, the pure S-enantiomer of ketamine, has been on the market since 2019 in the form of a nasal spray (Spravato). Esketamine has been approved in combination with oral antidepressant therapy for adults with a moderate to severe episode of major depression for acute treatment of a psychiatric emergency.
A meta-analysis from 2022 concluded that the original racemic ketamine is better than the new esketamine in reducing symptoms of depression.
In his own comprehensive study, Dr. Passie concluded that the mental impairments that occur during therapy did not differ significantly between substances. The patients even felt that the side effects from esketamine therapy were much more mentally unpleasant, said Dr. Passie. He concluded that the R-enantiomer may have a kind of protective effect against some of the psychopathological effects of the S-enantiomer (esketamine).
In addition, preclinical studies have indicated that the antidepressant effects of R-enantiomer, which is not contained in esketamine, are longer lasting and stronger.
Another problem is absorption, which can be inconsistent with a nasal spray. It may differ, for example, depending on the ambient humidity or whether the patient has recently had a cold. In addition, the spray is far more expensive than the ketamine injection, said Dr. Passie. Patients must also use the nasal spray under supervision at a medical practice (as with the intravenous application) and must receive follow-up care there. It therefore offers no advantage over the ketamine injection.
According to the Institute for Quality and Efficiency in Healthcare, no additional benefit has been proven for esketamine over standard therapies for adults who have experienced a moderate to severe depressive episode when used as short-term treatment for the rapid reduction of depressive symptoms in a psychiatric emergency. The German Medical Association agreed with this evaluation in October 2021.
In the United Kingdom, the medication was never approved, owing to the fact that it was too expensive and that no studies comparing it with psychotherapy were available.
Add-on psilocybin?
What was experienced under the influence of psilocybin can also be subsequently processed and used in psychotherapy.
The acute effect of psilocybin begins after approximately 40 minutes and lasts for 4-6 hours. The antidepressant effect, if it occurs at all, is of immediate onset. Unlike ketamine/esketamine, psilocybin hardly has any physical side effects.
The neurologic mechanism of action has been investigated recently using fMRI and PET techniques. According to the investigations, the substance causes individual networks of activity in the patient’s brain to interconnect more strongly, said Dr. Passie. The thalamus, the filter station for sensory information, as well as the limbic and paralimbic structures, which generate emotions, and the cortex are all activated more strongly.
Two therapeutic settings
Psilocybin, at least in the context of studies, is used in two settings: psycholytic therapy and psychedelic therapy. Both settings originated in the 1950s and were also used with LSD as the active substance.
Psycholytic therapy with psilocybin entails multiple administrations at low doses (for example, 10-18 mg), incorporated into a longer, mostly psychodynamic therapy of around 50-100 hours (often on an inpatient basis at the beginning). It results in what is described as an extended encounter with oneself. The focus is on psychodynamic experiences, such as memories and internal conflicts. In addition, novel experiences with oneself and self-recognition are important.
Psychedelic therapy generally entails one or two sessions with a high dose (for example, 25-35 mg psilocybin). The preparation and follow-up are limited to a few sessions. These methods refer to so-called transpersonal psychology, which addresses extraordinary states of consciousness in line with religious experiences. It often leads to an intense self-confrontation as well as to new evaluations of self and world. The central element to this therapy is the experience of a mystical ego loss and the concomitant feeling of connectedness, which should help to expand one’s perspective.
Euphoria and disillusionment
The first promising studies with a few patients suffering from depression were followed by others in which the euphoria was allowed to fade away somewhat. In the first direct comparison in a methodically high-grade double-blind study, psilocybin was inferior to the SSRI antidepressant escitalopram.
“There is a great variation in response from person to person,” said Dr. Passie. “The better the study is methodically controlled, the worse the results,” he hypothesized.
“Since the method is up to 50 times more expensive in practice, compared to SSRI therapy over 6-12 weeks, the question clearly must be asked as to whether it really has any great future.”
Outlook for psilocybin
Nevertheless, Dr. Passie still sees potential in psilocybin. He considers an approach in which psilocybin therapy is more firmly incorporated into psychotherapy, with between four and 10 therapy sessions before and after administration of a lower therapeutic dose of the substance, to be more promising.
“With this kind of intensive preparation and follow-up, as well as the repeated psilocybin sessions, the patient can benefit much more than is possible with one or two high-dose sessions,” said Dr. Passie, who also is chair of the International Society for Substance-Assisted Psychotherapy. “The constant ‘in-depth work on the ego’ required for drastic therapeutic changes can be more effective and lead to permanent improvements. I have no doubt about this.”
In Dr. Passie’s opinion, the best approach would involve a dignified inpatient setting with a longer period of follow-up care and consistent posttreatment care, including group therapy. The shape of future psilocybin therapy depends on whether the rather abrupt change seen with high-dose psychedelic therapy is permanent. The answer to this question will be decisive for the method and manner of its future clinical use.
Because of the somewhat negative study results, however, the initial investors are pulling out. Dr. Passie is therefore skeptical about whether the necessary larger studies will take place and whether psilocybin will make it onto the market.
In Switzerland, which is not subject to EU restrictions, more than 30 physicians have been authorized to use psilocybin, LSD, and MDMA in psychotherapy sessions. Still, in some respects this is a special case that cannot be transferred easily to other countries, said Dr. Passie.
Possible psilocybin improvement?
Various chemical derivatives of psychoactive substances have been researched, including a psilocybin variant with the label CYB003. With CYB003, the length of the acute psychedelic experience is reduced from around 6 hours (such as with psilocybin) to 1 hour. The plasma concentration of the substance is less variable between different patients. It is assumed that its effects will also differ less from person to person.
In July, researchers began a study of the use of CYB003 in the treatment of major depression. In the randomized, double-blind, placebo-controlled study with 40 patients, multiple doses of the substance will be administered.
When asked, Dr. Passie was rather skeptical about the study. He considers the approaches with psilocybin derivatives to be the consequences of a “gold-rush atmosphere” and expects there will be no real additional benefit, especially not a reduction in the period of action.
A version of this article first appeared on Medscape.com.
Recent studies with hallucinogens have raised hopes for an effective drug-based therapy to treat chronic depression. At the German Congress of Psychosomatic Medicine and Psychotherapy, Torsten Passie, MD, PhD, professor of psychiatry and psychotherapy at the Hannover (Germay) Medical School, gave a presentation on the current state of psilocybin and ketamine/esketamine research.
Dr. Passie, who also is head physician of the specialist unit for addiction and addiction prevention at the Diakonisches Werk in Hannover, has been investigating hallucinogenic substances and their application in psychotherapy for decades.
New therapies sought
In depression, gloom extends beyond the patient’s mood. For some time there has been little cause for joy with regard to chronic depression therapy. Established drug therapies hardly perform any better than placebo in meta-analyses, as a study recently confirmed. The pharmaceutical industry pulled out of psycho-pharmaceutical development more than 10 years ago. What’s more, the number of cases is rising, especially among young people, and there are long waiting times for psychotherapy appointments.
It is no wonder that some are welcoming new drug-based approaches with lysergic acid diethylamide (LSD)–like hallucinogens. In 2016, a study on psilocybin was published in The Lancet Psychiatry, although the study was unblinded and included only 24 patients.
Evoking emotions
A range of substances can be classed as hallucinogens, including psilocybin, mescaline, LSD, 3,4-methylenedioxy-methamphetamine (MDMA, also known as ecstasy), and ketamine.
Taking hallucinogens can cause a release of serotonin and dopamine, an increase in activity levels in the brain, a shift in stimulus filtering, an increase in the production of internal stimuli (inner experiences), and a change in sensory integration (for example, synesthesia).
Besides falling into a dreamlike state, patients can achieve an expansion or narrowing of consciousness if they focus on an inner experience. Internal perception increases. Perceptual routines are broken apart. Thought processes become more image-based and are more associative than normal.
Patients therefore are more capable of making new and unusual connections between different biographical or current situations. Previously unconscious ideas can become conscious. At higher doses, ego loss can occur, which can be associated with a mystical feeling of connectedness.
Hallucinogens mainly evoke and heighten emotions. Those effects may be experienced strongly as internal visions or in physical manifestations (for example, crying or laughing). In contrast, conventional antidepressants work by suppressing emotions (that is, emotional blunting).
These different mechanisms result in two contrasting management strategies. For example, SSRI antidepressants cause a patient to perceive workplace bullying as less severe and to do nothing to change the situation; the patient remains passive.
In contrast, a therapeutically guided, emotionally activating experience on hallucinogens can help the patient to try more actively to change the stressful situation.
Ketamine has a special place among hallucinogens. Unlike other hallucinogens, ketamine causes a strong clouding of consciousness, a reduction in physical sensory perception, and significant disruption in thinking and memory. It is therefore only suitable as a short-term intervention and is therapeutically impractical over the long term.
Ketamine’s effects
Ketamine, a racemic mixture of the enantiomers S-ketamine and R-ketamine, was originally used only as an analgesic and anesthetic. Owing to its rapid antidepressant effect, it has since also been used as an emergency medication for severe depression, sometimes in combination with SSRIs or serotonin noradrenaline reuptake inhibitors.
Approximately 60% of patients respond to the treatment. Whereas with conventional antidepressants, onset of action requires 10-14 days, ketamine is effective within a few hours. However, relapse always occurs, usually very quickly. After 2-3 days, the effect is usually approximately that of a placebo. An administration interval of about 2 days is optimal. However, “resistance” to the effect often develops after some time: the drug’s antidepressant effect diminishes.
Ketamine also has some unpleasant side effects, such as depersonalization, dissociation, impaired thinking, nystagmus, and psychotomimetic effects. Nausea and vomiting also occur. Interestingly, the latter does not bother the patient much, owing to the drug’s psychological effects, and it does not lead to treatment discontinuation, said Dr. Passie, who described his clinical experiences with ketamine.
Since ketamine causes a considerable clouding of consciousness, sensory disorders, and significant memory problems, it is not suitable for psychedelic-assisted psychotherapy, unlike LSD or psilocybin, he emphasized.
Ketamine 2.0?
Esketamine, the pure S-enantiomer of ketamine, has been on the market since 2019 in the form of a nasal spray (Spravato). Esketamine has been approved in combination with oral antidepressant therapy for adults with a moderate to severe episode of major depression for acute treatment of a psychiatric emergency.
A meta-analysis from 2022 concluded that the original racemic ketamine is better than the new esketamine in reducing symptoms of depression.
In his own comprehensive study, Dr. Passie concluded that the mental impairments that occur during therapy did not differ significantly between substances. The patients even felt that the side effects from esketamine therapy were much more mentally unpleasant, said Dr. Passie. He concluded that the R-enantiomer may have a kind of protective effect against some of the psychopathological effects of the S-enantiomer (esketamine).
In addition, preclinical studies have indicated that the antidepressant effects of R-enantiomer, which is not contained in esketamine, are longer lasting and stronger.
Another problem is absorption, which can be inconsistent with a nasal spray. It may differ, for example, depending on the ambient humidity or whether the patient has recently had a cold. In addition, the spray is far more expensive than the ketamine injection, said Dr. Passie. Patients must also use the nasal spray under supervision at a medical practice (as with the intravenous application) and must receive follow-up care there. It therefore offers no advantage over the ketamine injection.
According to the Institute for Quality and Efficiency in Healthcare, no additional benefit has been proven for esketamine over standard therapies for adults who have experienced a moderate to severe depressive episode when used as short-term treatment for the rapid reduction of depressive symptoms in a psychiatric emergency. The German Medical Association agreed with this evaluation in October 2021.
In the United Kingdom, the medication was never approved, owing to the fact that it was too expensive and that no studies comparing it with psychotherapy were available.
Add-on psilocybin?
What was experienced under the influence of psilocybin can also be subsequently processed and used in psychotherapy.
The acute effect of psilocybin begins after approximately 40 minutes and lasts for 4-6 hours. The antidepressant effect, if it occurs at all, is of immediate onset. Unlike ketamine/esketamine, psilocybin hardly has any physical side effects.
The neurologic mechanism of action has been investigated recently using fMRI and PET techniques. According to the investigations, the substance causes individual networks of activity in the patient’s brain to interconnect more strongly, said Dr. Passie. The thalamus, the filter station for sensory information, as well as the limbic and paralimbic structures, which generate emotions, and the cortex are all activated more strongly.
Two therapeutic settings
Psilocybin, at least in the context of studies, is used in two settings: psycholytic therapy and psychedelic therapy. Both settings originated in the 1950s and were also used with LSD as the active substance.
Psycholytic therapy with psilocybin entails multiple administrations at low doses (for example, 10-18 mg), incorporated into a longer, mostly psychodynamic therapy of around 50-100 hours (often on an inpatient basis at the beginning). It results in what is described as an extended encounter with oneself. The focus is on psychodynamic experiences, such as memories and internal conflicts. In addition, novel experiences with oneself and self-recognition are important.
Psychedelic therapy generally entails one or two sessions with a high dose (for example, 25-35 mg psilocybin). The preparation and follow-up are limited to a few sessions. These methods refer to so-called transpersonal psychology, which addresses extraordinary states of consciousness in line with religious experiences. It often leads to an intense self-confrontation as well as to new evaluations of self and world. The central element to this therapy is the experience of a mystical ego loss and the concomitant feeling of connectedness, which should help to expand one’s perspective.
Euphoria and disillusionment
The first promising studies with a few patients suffering from depression were followed by others in which the euphoria was allowed to fade away somewhat. In the first direct comparison in a methodically high-grade double-blind study, psilocybin was inferior to the SSRI antidepressant escitalopram.
“There is a great variation in response from person to person,” said Dr. Passie. “The better the study is methodically controlled, the worse the results,” he hypothesized.
“Since the method is up to 50 times more expensive in practice, compared to SSRI therapy over 6-12 weeks, the question clearly must be asked as to whether it really has any great future.”
Outlook for psilocybin
Nevertheless, Dr. Passie still sees potential in psilocybin. He considers an approach in which psilocybin therapy is more firmly incorporated into psychotherapy, with between four and 10 therapy sessions before and after administration of a lower therapeutic dose of the substance, to be more promising.
“With this kind of intensive preparation and follow-up, as well as the repeated psilocybin sessions, the patient can benefit much more than is possible with one or two high-dose sessions,” said Dr. Passie, who also is chair of the International Society for Substance-Assisted Psychotherapy. “The constant ‘in-depth work on the ego’ required for drastic therapeutic changes can be more effective and lead to permanent improvements. I have no doubt about this.”
In Dr. Passie’s opinion, the best approach would involve a dignified inpatient setting with a longer period of follow-up care and consistent posttreatment care, including group therapy. The shape of future psilocybin therapy depends on whether the rather abrupt change seen with high-dose psychedelic therapy is permanent. The answer to this question will be decisive for the method and manner of its future clinical use.
Because of the somewhat negative study results, however, the initial investors are pulling out. Dr. Passie is therefore skeptical about whether the necessary larger studies will take place and whether psilocybin will make it onto the market.
In Switzerland, which is not subject to EU restrictions, more than 30 physicians have been authorized to use psilocybin, LSD, and MDMA in psychotherapy sessions. Still, in some respects this is a special case that cannot be transferred easily to other countries, said Dr. Passie.
Possible psilocybin improvement?
Various chemical derivatives of psychoactive substances have been researched, including a psilocybin variant with the label CYB003. With CYB003, the length of the acute psychedelic experience is reduced from around 6 hours (such as with psilocybin) to 1 hour. The plasma concentration of the substance is less variable between different patients. It is assumed that its effects will also differ less from person to person.
In July, researchers began a study of the use of CYB003 in the treatment of major depression. In the randomized, double-blind, placebo-controlled study with 40 patients, multiple doses of the substance will be administered.
When asked, Dr. Passie was rather skeptical about the study. He considers the approaches with psilocybin derivatives to be the consequences of a “gold-rush atmosphere” and expects there will be no real additional benefit, especially not a reduction in the period of action.
A version of this article first appeared on Medscape.com.
Recent studies with hallucinogens have raised hopes for an effective drug-based therapy to treat chronic depression. At the German Congress of Psychosomatic Medicine and Psychotherapy, Torsten Passie, MD, PhD, professor of psychiatry and psychotherapy at the Hannover (Germay) Medical School, gave a presentation on the current state of psilocybin and ketamine/esketamine research.
Dr. Passie, who also is head physician of the specialist unit for addiction and addiction prevention at the Diakonisches Werk in Hannover, has been investigating hallucinogenic substances and their application in psychotherapy for decades.
New therapies sought
In depression, gloom extends beyond the patient’s mood. For some time there has been little cause for joy with regard to chronic depression therapy. Established drug therapies hardly perform any better than placebo in meta-analyses, as a study recently confirmed. The pharmaceutical industry pulled out of psycho-pharmaceutical development more than 10 years ago. What’s more, the number of cases is rising, especially among young people, and there are long waiting times for psychotherapy appointments.
It is no wonder that some are welcoming new drug-based approaches with lysergic acid diethylamide (LSD)–like hallucinogens. In 2016, a study on psilocybin was published in The Lancet Psychiatry, although the study was unblinded and included only 24 patients.
Evoking emotions
A range of substances can be classed as hallucinogens, including psilocybin, mescaline, LSD, 3,4-methylenedioxy-methamphetamine (MDMA, also known as ecstasy), and ketamine.
Taking hallucinogens can cause a release of serotonin and dopamine, an increase in activity levels in the brain, a shift in stimulus filtering, an increase in the production of internal stimuli (inner experiences), and a change in sensory integration (for example, synesthesia).
Besides falling into a dreamlike state, patients can achieve an expansion or narrowing of consciousness if they focus on an inner experience. Internal perception increases. Perceptual routines are broken apart. Thought processes become more image-based and are more associative than normal.
Patients therefore are more capable of making new and unusual connections between different biographical or current situations. Previously unconscious ideas can become conscious. At higher doses, ego loss can occur, which can be associated with a mystical feeling of connectedness.
Hallucinogens mainly evoke and heighten emotions. Those effects may be experienced strongly as internal visions or in physical manifestations (for example, crying or laughing). In contrast, conventional antidepressants work by suppressing emotions (that is, emotional blunting).
These different mechanisms result in two contrasting management strategies. For example, SSRI antidepressants cause a patient to perceive workplace bullying as less severe and to do nothing to change the situation; the patient remains passive.
In contrast, a therapeutically guided, emotionally activating experience on hallucinogens can help the patient to try more actively to change the stressful situation.
Ketamine has a special place among hallucinogens. Unlike other hallucinogens, ketamine causes a strong clouding of consciousness, a reduction in physical sensory perception, and significant disruption in thinking and memory. It is therefore only suitable as a short-term intervention and is therapeutically impractical over the long term.
Ketamine’s effects
Ketamine, a racemic mixture of the enantiomers S-ketamine and R-ketamine, was originally used only as an analgesic and anesthetic. Owing to its rapid antidepressant effect, it has since also been used as an emergency medication for severe depression, sometimes in combination with SSRIs or serotonin noradrenaline reuptake inhibitors.
Approximately 60% of patients respond to the treatment. Whereas with conventional antidepressants, onset of action requires 10-14 days, ketamine is effective within a few hours. However, relapse always occurs, usually very quickly. After 2-3 days, the effect is usually approximately that of a placebo. An administration interval of about 2 days is optimal. However, “resistance” to the effect often develops after some time: the drug’s antidepressant effect diminishes.
Ketamine also has some unpleasant side effects, such as depersonalization, dissociation, impaired thinking, nystagmus, and psychotomimetic effects. Nausea and vomiting also occur. Interestingly, the latter does not bother the patient much, owing to the drug’s psychological effects, and it does not lead to treatment discontinuation, said Dr. Passie, who described his clinical experiences with ketamine.
Since ketamine causes a considerable clouding of consciousness, sensory disorders, and significant memory problems, it is not suitable for psychedelic-assisted psychotherapy, unlike LSD or psilocybin, he emphasized.
Ketamine 2.0?
Esketamine, the pure S-enantiomer of ketamine, has been on the market since 2019 in the form of a nasal spray (Spravato). Esketamine has been approved in combination with oral antidepressant therapy for adults with a moderate to severe episode of major depression for acute treatment of a psychiatric emergency.
A meta-analysis from 2022 concluded that the original racemic ketamine is better than the new esketamine in reducing symptoms of depression.
In his own comprehensive study, Dr. Passie concluded that the mental impairments that occur during therapy did not differ significantly between substances. The patients even felt that the side effects from esketamine therapy were much more mentally unpleasant, said Dr. Passie. He concluded that the R-enantiomer may have a kind of protective effect against some of the psychopathological effects of the S-enantiomer (esketamine).
In addition, preclinical studies have indicated that the antidepressant effects of R-enantiomer, which is not contained in esketamine, are longer lasting and stronger.
Another problem is absorption, which can be inconsistent with a nasal spray. It may differ, for example, depending on the ambient humidity or whether the patient has recently had a cold. In addition, the spray is far more expensive than the ketamine injection, said Dr. Passie. Patients must also use the nasal spray under supervision at a medical practice (as with the intravenous application) and must receive follow-up care there. It therefore offers no advantage over the ketamine injection.
According to the Institute for Quality and Efficiency in Healthcare, no additional benefit has been proven for esketamine over standard therapies for adults who have experienced a moderate to severe depressive episode when used as short-term treatment for the rapid reduction of depressive symptoms in a psychiatric emergency. The German Medical Association agreed with this evaluation in October 2021.
In the United Kingdom, the medication was never approved, owing to the fact that it was too expensive and that no studies comparing it with psychotherapy were available.
Add-on psilocybin?
What was experienced under the influence of psilocybin can also be subsequently processed and used in psychotherapy.
The acute effect of psilocybin begins after approximately 40 minutes and lasts for 4-6 hours. The antidepressant effect, if it occurs at all, is of immediate onset. Unlike ketamine/esketamine, psilocybin hardly has any physical side effects.
The neurologic mechanism of action has been investigated recently using fMRI and PET techniques. According to the investigations, the substance causes individual networks of activity in the patient’s brain to interconnect more strongly, said Dr. Passie. The thalamus, the filter station for sensory information, as well as the limbic and paralimbic structures, which generate emotions, and the cortex are all activated more strongly.
Two therapeutic settings
Psilocybin, at least in the context of studies, is used in two settings: psycholytic therapy and psychedelic therapy. Both settings originated in the 1950s and were also used with LSD as the active substance.
Psycholytic therapy with psilocybin entails multiple administrations at low doses (for example, 10-18 mg), incorporated into a longer, mostly psychodynamic therapy of around 50-100 hours (often on an inpatient basis at the beginning). It results in what is described as an extended encounter with oneself. The focus is on psychodynamic experiences, such as memories and internal conflicts. In addition, novel experiences with oneself and self-recognition are important.
Psychedelic therapy generally entails one or two sessions with a high dose (for example, 25-35 mg psilocybin). The preparation and follow-up are limited to a few sessions. These methods refer to so-called transpersonal psychology, which addresses extraordinary states of consciousness in line with religious experiences. It often leads to an intense self-confrontation as well as to new evaluations of self and world. The central element to this therapy is the experience of a mystical ego loss and the concomitant feeling of connectedness, which should help to expand one’s perspective.
Euphoria and disillusionment
The first promising studies with a few patients suffering from depression were followed by others in which the euphoria was allowed to fade away somewhat. In the first direct comparison in a methodically high-grade double-blind study, psilocybin was inferior to the SSRI antidepressant escitalopram.
“There is a great variation in response from person to person,” said Dr. Passie. “The better the study is methodically controlled, the worse the results,” he hypothesized.
“Since the method is up to 50 times more expensive in practice, compared to SSRI therapy over 6-12 weeks, the question clearly must be asked as to whether it really has any great future.”
Outlook for psilocybin
Nevertheless, Dr. Passie still sees potential in psilocybin. He considers an approach in which psilocybin therapy is more firmly incorporated into psychotherapy, with between four and 10 therapy sessions before and after administration of a lower therapeutic dose of the substance, to be more promising.
“With this kind of intensive preparation and follow-up, as well as the repeated psilocybin sessions, the patient can benefit much more than is possible with one or two high-dose sessions,” said Dr. Passie, who also is chair of the International Society for Substance-Assisted Psychotherapy. “The constant ‘in-depth work on the ego’ required for drastic therapeutic changes can be more effective and lead to permanent improvements. I have no doubt about this.”
In Dr. Passie’s opinion, the best approach would involve a dignified inpatient setting with a longer period of follow-up care and consistent posttreatment care, including group therapy. The shape of future psilocybin therapy depends on whether the rather abrupt change seen with high-dose psychedelic therapy is permanent. The answer to this question will be decisive for the method and manner of its future clinical use.
Because of the somewhat negative study results, however, the initial investors are pulling out. Dr. Passie is therefore skeptical about whether the necessary larger studies will take place and whether psilocybin will make it onto the market.
In Switzerland, which is not subject to EU restrictions, more than 30 physicians have been authorized to use psilocybin, LSD, and MDMA in psychotherapy sessions. Still, in some respects this is a special case that cannot be transferred easily to other countries, said Dr. Passie.
Possible psilocybin improvement?
Various chemical derivatives of psychoactive substances have been researched, including a psilocybin variant with the label CYB003. With CYB003, the length of the acute psychedelic experience is reduced from around 6 hours (such as with psilocybin) to 1 hour. The plasma concentration of the substance is less variable between different patients. It is assumed that its effects will also differ less from person to person.
In July, researchers began a study of the use of CYB003 in the treatment of major depression. In the randomized, double-blind, placebo-controlled study with 40 patients, multiple doses of the substance will be administered.
When asked, Dr. Passie was rather skeptical about the study. He considers the approaches with psilocybin derivatives to be the consequences of a “gold-rush atmosphere” and expects there will be no real additional benefit, especially not a reduction in the period of action.
A version of this article first appeared on Medscape.com.
Doctors using fake positive reviews to boost business
Five years ago, Kay Dean relied upon Yelp! and Google reviews in her search for a doctor in her area. After finding a physician with fairly high reviews, Ms. Dean was shocked when her personal experience was significantly worse than patients on the review platforms.
Following her experience, Ms. Dean, a former federal government investigator, became skeptical and used her skills to investigate the practice on all review platforms. She uncovered that the practice had a review from an individual who was involved in a review trading group on Facebook, where organizations openly barter their services in exchange for positive reviews fraud.
“I discovered that the online review world was just saturated with fake reviews, much more so than I think most people are aware ... and law enforcement regulators aren’t doing anything to address the problem,” said Ms. Dean. “In this online space, it’s the Wild West; cheating is rewarded.”
Ms. Dean decided to take matters into her own hands. She created a YouTube channel called Fake Review Watch, where she exposes real businesses and their attempts to dupe potential consumers with fake positive reviews.
For example, one video analyzes an orthopedic surgeon in Manhattan with an abundance of five-star reviews. Through her detailed analysis, Ms. Dean created a spreadsheet of the 26 alleged patients of the orthopedic surgeon that had submitted glowing reviews. She looked into other businesses that the individuals had left reviews for and found a significant amount of overlap.
According to the video, 19 of the doctor’s reviewers had left high reviews for the same moving company in Las Vegas, and 18 of them reviewed the same locksmith in Texas. Overall, eight of the patients reviewed the same mover, locksmith, and hotel in New Zealand.
A matter of trust
Ms. Dean expressed the gravity of this phenomenon, especially in health care, as patients often head online first when searching for care options. Based on a survey by Software Advice, about 84% of patients use online reviews to assess a physician, and 77% use review sites as the first step in finding a doctor.
Patient trust has continued to diminish in recent years, particularly following the pandemic. In a 2021 global ranking of trust levels towards health care by country, the U.S. health care system ranked 19th, far below those of several developing countries.
Owing to the rise of fake patient reviews and their inscrutable nature, Ms. Dean advises staying away from online review platforms. Instead, she suggests sticking to the old-fashioned method of getting recommendations from friends and relatives, not virtual people.
Ms. Dean explained a few indicators that she looks for when trying to identify a fake review.
“The business has all five-star reviews, negative reviews are followed by five-star reviews, or the business has an abnormal number of positive reviews in a short period of time,” she noted. “Some businesses try to bury legitimate negative reviews by obtaining more recent, fake, positive ones. The recent reviews will contradict the specific criticisms in the negative review.”
She warned that consumers should not give credibility to reviews simply because the reviewer is dubbed “Elite” or a Google Local Guide, because she has seen plenty of these individuals posting fake reviews.
Unfortunately, review platforms haven’t been doing much self-policing. Google and Healthgrades have a series of policies against fake engagement, impersonation, misinformation, and misrepresentation, according to their websites. However, the only consequence of these violations is review removal.
Both Yelp! and Google say they have automated software that distinguishes real versus fake reviews. When Yelp! uncovers users engaging in compensation review activity, it removes their reviews, closes their account, and blocks those users from creating future Yelp! accounts.
Physicians’ basis
Moreover,
“I think there’s an erosion of business ethics because cheating is rewarded. You can’t compete in an environment where your competition is allowed to accumulate numerous fake reviews while you’re still trying to fill chairs in your business,” said Ms. Dean. “Your competition is then getting the business because the tech companies are allowing this fraud.”
Family physician and practice owner Mike Woo-Ming, MD, MPH, provides career coaching for physicians, including maintaining a good reputation – in-person and online. He has seen physicians bumping up their own five-star reviews personally as well as posting negative reviews for their competition.
“I’ve seen where they’re going to lose business, as many practices were affected through COVID,” he said. “Business owners can become desperate and may decide to start posting or buying reviews because they know people will choose certain services these days based upon reviews.”
Dr. Woo-Ming expressed his frustration with fellow physicians who give in to purchasing fake reviews, because the patients have no idea whether reviews are genuine or not.
To encourage genuine positive reviews, Dr. Woo-Ming’s practice uses a third-party app system that sends patients a follow-up email or text asking about their experience with a link to review sites.
“Honest reviews are a reflection of what I can do to improve my business. At the end of the day, if you’re truly providing great service and you’re helping people by providing great medical care, those are going to win out,” he said. “I would rather, as a responsible practice owner, improve the experience and outcome for the patient.”
A version of this article first appeared on Medscape.com.
Five years ago, Kay Dean relied upon Yelp! and Google reviews in her search for a doctor in her area. After finding a physician with fairly high reviews, Ms. Dean was shocked when her personal experience was significantly worse than patients on the review platforms.
Following her experience, Ms. Dean, a former federal government investigator, became skeptical and used her skills to investigate the practice on all review platforms. She uncovered that the practice had a review from an individual who was involved in a review trading group on Facebook, where organizations openly barter their services in exchange for positive reviews fraud.
“I discovered that the online review world was just saturated with fake reviews, much more so than I think most people are aware ... and law enforcement regulators aren’t doing anything to address the problem,” said Ms. Dean. “In this online space, it’s the Wild West; cheating is rewarded.”
Ms. Dean decided to take matters into her own hands. She created a YouTube channel called Fake Review Watch, where she exposes real businesses and their attempts to dupe potential consumers with fake positive reviews.
For example, one video analyzes an orthopedic surgeon in Manhattan with an abundance of five-star reviews. Through her detailed analysis, Ms. Dean created a spreadsheet of the 26 alleged patients of the orthopedic surgeon that had submitted glowing reviews. She looked into other businesses that the individuals had left reviews for and found a significant amount of overlap.
According to the video, 19 of the doctor’s reviewers had left high reviews for the same moving company in Las Vegas, and 18 of them reviewed the same locksmith in Texas. Overall, eight of the patients reviewed the same mover, locksmith, and hotel in New Zealand.
A matter of trust
Ms. Dean expressed the gravity of this phenomenon, especially in health care, as patients often head online first when searching for care options. Based on a survey by Software Advice, about 84% of patients use online reviews to assess a physician, and 77% use review sites as the first step in finding a doctor.
Patient trust has continued to diminish in recent years, particularly following the pandemic. In a 2021 global ranking of trust levels towards health care by country, the U.S. health care system ranked 19th, far below those of several developing countries.
Owing to the rise of fake patient reviews and their inscrutable nature, Ms. Dean advises staying away from online review platforms. Instead, she suggests sticking to the old-fashioned method of getting recommendations from friends and relatives, not virtual people.
Ms. Dean explained a few indicators that she looks for when trying to identify a fake review.
“The business has all five-star reviews, negative reviews are followed by five-star reviews, or the business has an abnormal number of positive reviews in a short period of time,” she noted. “Some businesses try to bury legitimate negative reviews by obtaining more recent, fake, positive ones. The recent reviews will contradict the specific criticisms in the negative review.”
She warned that consumers should not give credibility to reviews simply because the reviewer is dubbed “Elite” or a Google Local Guide, because she has seen plenty of these individuals posting fake reviews.
Unfortunately, review platforms haven’t been doing much self-policing. Google and Healthgrades have a series of policies against fake engagement, impersonation, misinformation, and misrepresentation, according to their websites. However, the only consequence of these violations is review removal.
Both Yelp! and Google say they have automated software that distinguishes real versus fake reviews. When Yelp! uncovers users engaging in compensation review activity, it removes their reviews, closes their account, and blocks those users from creating future Yelp! accounts.
Physicians’ basis
Moreover,
“I think there’s an erosion of business ethics because cheating is rewarded. You can’t compete in an environment where your competition is allowed to accumulate numerous fake reviews while you’re still trying to fill chairs in your business,” said Ms. Dean. “Your competition is then getting the business because the tech companies are allowing this fraud.”
Family physician and practice owner Mike Woo-Ming, MD, MPH, provides career coaching for physicians, including maintaining a good reputation – in-person and online. He has seen physicians bumping up their own five-star reviews personally as well as posting negative reviews for their competition.
“I’ve seen where they’re going to lose business, as many practices were affected through COVID,” he said. “Business owners can become desperate and may decide to start posting or buying reviews because they know people will choose certain services these days based upon reviews.”
Dr. Woo-Ming expressed his frustration with fellow physicians who give in to purchasing fake reviews, because the patients have no idea whether reviews are genuine or not.
To encourage genuine positive reviews, Dr. Woo-Ming’s practice uses a third-party app system that sends patients a follow-up email or text asking about their experience with a link to review sites.
“Honest reviews are a reflection of what I can do to improve my business. At the end of the day, if you’re truly providing great service and you’re helping people by providing great medical care, those are going to win out,” he said. “I would rather, as a responsible practice owner, improve the experience and outcome for the patient.”
A version of this article first appeared on Medscape.com.
Five years ago, Kay Dean relied upon Yelp! and Google reviews in her search for a doctor in her area. After finding a physician with fairly high reviews, Ms. Dean was shocked when her personal experience was significantly worse than patients on the review platforms.
Following her experience, Ms. Dean, a former federal government investigator, became skeptical and used her skills to investigate the practice on all review platforms. She uncovered that the practice had a review from an individual who was involved in a review trading group on Facebook, where organizations openly barter their services in exchange for positive reviews fraud.
“I discovered that the online review world was just saturated with fake reviews, much more so than I think most people are aware ... and law enforcement regulators aren’t doing anything to address the problem,” said Ms. Dean. “In this online space, it’s the Wild West; cheating is rewarded.”
Ms. Dean decided to take matters into her own hands. She created a YouTube channel called Fake Review Watch, where she exposes real businesses and their attempts to dupe potential consumers with fake positive reviews.
For example, one video analyzes an orthopedic surgeon in Manhattan with an abundance of five-star reviews. Through her detailed analysis, Ms. Dean created a spreadsheet of the 26 alleged patients of the orthopedic surgeon that had submitted glowing reviews. She looked into other businesses that the individuals had left reviews for and found a significant amount of overlap.
According to the video, 19 of the doctor’s reviewers had left high reviews for the same moving company in Las Vegas, and 18 of them reviewed the same locksmith in Texas. Overall, eight of the patients reviewed the same mover, locksmith, and hotel in New Zealand.
A matter of trust
Ms. Dean expressed the gravity of this phenomenon, especially in health care, as patients often head online first when searching for care options. Based on a survey by Software Advice, about 84% of patients use online reviews to assess a physician, and 77% use review sites as the first step in finding a doctor.
Patient trust has continued to diminish in recent years, particularly following the pandemic. In a 2021 global ranking of trust levels towards health care by country, the U.S. health care system ranked 19th, far below those of several developing countries.
Owing to the rise of fake patient reviews and their inscrutable nature, Ms. Dean advises staying away from online review platforms. Instead, she suggests sticking to the old-fashioned method of getting recommendations from friends and relatives, not virtual people.
Ms. Dean explained a few indicators that she looks for when trying to identify a fake review.
“The business has all five-star reviews, negative reviews are followed by five-star reviews, or the business has an abnormal number of positive reviews in a short period of time,” she noted. “Some businesses try to bury legitimate negative reviews by obtaining more recent, fake, positive ones. The recent reviews will contradict the specific criticisms in the negative review.”
She warned that consumers should not give credibility to reviews simply because the reviewer is dubbed “Elite” or a Google Local Guide, because she has seen plenty of these individuals posting fake reviews.
Unfortunately, review platforms haven’t been doing much self-policing. Google and Healthgrades have a series of policies against fake engagement, impersonation, misinformation, and misrepresentation, according to their websites. However, the only consequence of these violations is review removal.
Both Yelp! and Google say they have automated software that distinguishes real versus fake reviews. When Yelp! uncovers users engaging in compensation review activity, it removes their reviews, closes their account, and blocks those users from creating future Yelp! accounts.
Physicians’ basis
Moreover,
“I think there’s an erosion of business ethics because cheating is rewarded. You can’t compete in an environment where your competition is allowed to accumulate numerous fake reviews while you’re still trying to fill chairs in your business,” said Ms. Dean. “Your competition is then getting the business because the tech companies are allowing this fraud.”
Family physician and practice owner Mike Woo-Ming, MD, MPH, provides career coaching for physicians, including maintaining a good reputation – in-person and online. He has seen physicians bumping up their own five-star reviews personally as well as posting negative reviews for their competition.
“I’ve seen where they’re going to lose business, as many practices were affected through COVID,” he said. “Business owners can become desperate and may decide to start posting or buying reviews because they know people will choose certain services these days based upon reviews.”
Dr. Woo-Ming expressed his frustration with fellow physicians who give in to purchasing fake reviews, because the patients have no idea whether reviews are genuine or not.
To encourage genuine positive reviews, Dr. Woo-Ming’s practice uses a third-party app system that sends patients a follow-up email or text asking about their experience with a link to review sites.
“Honest reviews are a reflection of what I can do to improve my business. At the end of the day, if you’re truly providing great service and you’re helping people by providing great medical care, those are going to win out,” he said. “I would rather, as a responsible practice owner, improve the experience and outcome for the patient.”
A version of this article first appeared on Medscape.com.
Why our brains wear out at the end of the day
The transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Once again, we’re doing an informal journal club to talk about a really interesting study, “A Neuro-metabolic Account of Why Daylong Cognitive Work Alters the Control of Economic Decisions,” that just came out. It tries to answer the question of why our brains wear out. I’m going to put myself in the corner here. Let’s walk through this study, which appears in Current Biology, by lead author Antonius Wiehler from Paris.
The big question is what’s going on with cognitive fatigue. If you look at chess players who are exerting a lot of cognitive effort, it’s well documented that over hours of play, they get worse and make more mistakes. It takes them longer to make decisions. The question is, why?
Why does your brain get tired?
To date, it’s been a little bit hard to tease that out. Now, there is some suggestion of what is responsible for this. The cognitive control center of the brain is probably somewhere in the left lateral prefrontal cortex (LLPC).
The prefrontal cortex is responsible for higher-level thinking. It’s what causes you to be inhibited. It gets shut off by alcohol and leads to impulsive behaviors. The LLPC, according to functional MRI studies, has reduced activity as people become more and more cognitively fatigued. The LLPC helps you think through choices. As you become more fatigued, this area of the brain isn’t working as well. But why would it not work as well? What is going on in that particular part of the brain? It doesn’t seem to be something simple, like glucose levels; that’s been investigated and glucose levels are pretty constant throughout the brain, regardless of cognitive task. This paper seeks to tease out what is actually going on in the LLPC when you are becoming cognitively tired.
They did an experiment where they induced cognitive fatigue, and it sounds like a painful experiment. For more than 6 hours, volunteers completed sessions during which they had to perform cognitive switching tasks. Investigators showed participants a letter, in either red or green, and the participant would respond with whether it was a vowel or a consonant or whether it was a capital or lowercase letter, based on the color. If it’s red, say whether it’s a consonant or vowel. If it’s green, say whether it’s upper- or lowercase.
It’s hard, and doing it for 6 hours is likely to induce a lot of cognitive fatigue. They had a control group as well, which is really important here. The control group also did a task like this for 6 hours, but for them, investigators didn’t change the color as often – perhaps only once per session. For the study group, they were switching colors back and forth quite a lot. They also incorporated a memory challenge that worked in a similar way.
So, what are the readouts of this study? They had a group who went through the hard cognitive challenge and a group who went through the easy cognitive challenge. They looked at a variety of metrics. I’ll describe a few.
The first is performance decrement. Did they get it wrong? What percentage of the time did the participant say “consonant” when they should have said “lowercase?”
You can see here that the hard group did a little bit worse overall. It was harder, so they don’t do as well. That makes sense. But both groups kind of waned over time a little bit. It’s not as though the hard group declines much more. The slopes of those lines are pretty similar. So, not very robust findings there.
What about subjective fatigue? They asked the participants how exhausted they were from doing the tasks.
Both groups were worn out. It was a long day. There was a suggestion that the hard group became worn out a little bit sooner, but I don’t think this achieves statistical significance. Everyone was getting tired by hour 6 here.
What about response time? How quickly could the participant say “consonant,” “vowel,” “lowercase,” or “uppercase?”
The hard group took longer to respond because it was a harder task. But over time, the response times were pretty flat.
So far there isn’t a robust readout that would make us say, oh, yeah, that is a good marker of cognitive fatigue. That’s how you measure cognitive fatigue. It’s not what people say. It’s not how quick they are. It’s not even how accurate they are.
But then the investigators got a little bit clever. Participants were asked to play a “would you rather” game, a reward game. Here are two examples.
Would you rather:
- Have a 25% chance of earning $50 OR a 95% chance of earning $17.30?
- Earn $50, but your next task session will be hard or earn $40 and your next task session will be easy?
Participants had to figure out the better odds – what should they be choosing here? They had to tease out whether they preferred lower cost lower-risk choices – when they are cognitively fatigued, which has been shown in prior studies.
This showed a pretty dramatic difference between the groups in terms of the low-cost bias – how much more likely they were to pick the low-cost, easier choice as they became more and more cognitively fatigued. The hard group participants were more likely to pick the easy thing rather than the potentially more lucrative thing, which is really interesting when we think about how our own cognitive fatigue happens at the end of a difficult workday, how you may just be likely to go with the flow and do something easy because you just don’t have that much decision-making power left.
It would be nice to have some objective physiologic measurements for this, and they do. This is pupil dilation.
When you’re paying attention to something, your pupils dilate a little bit. They were able to show that as the hard group became more and more fatigued, pupil dilation sort of went away. In fact, if anything, their pupils constricted a little bit. But basically there was a significant difference here. The easy group’s pupils were still fine; they were still dilating. The hard group’s pupils got more sluggish. This is a physiologic correlate of what’s going on.
But again, these are all downstream of whatever is happening in the LLPC. So the real meat of this study is a functional MRI analysis, and the way they did this is pretty clever. They were looking for metabolites in the various parts of the brain using a labeled hydrogen MRI, which is even fancier than a functional MRI. It’s like MRI spectroscopy, and it can measure the levels of certain chemicals in the brain. They hypothesized that if there is a chemical that builds up when you are tired, it should build up preferentially in the LLPC.
Whereas in the rest of the brain, there shouldn’t be that much difference because we know the action is happening in the LLPC. The control part of the brain is a section called V1. They looked at a variety of metabolites, but the only one that behaved the way they expected was glutamate and glutamic acid (glutamate metabolites). In the hard group, the glutamate is building up over time, so there is a higher concentration of glutamate in the LLPC but not the rest of the brain. There is also a greater diffusion of glutamate from the intracellular to the extracellular space, which suggests that it’s kind of leaking out of the cells.
So the signal here is that the thing that’s impacting that part of the brain is this buildup of glutamate. To tie this together, they showed in the scatterplot the relationship between the increase in glutamate and the low-cost bias from the decision fatigue example.
It’s not the strongest correlation, but it is statistically significant that the more glutamate in your LLPC, the more likely you are to just take the easy decision as opposed to really thinking things through. That is pretty powerful. It’s telling us that your brain making you fatigued, and making you less likely to continue to use your LLPC, may be a self-defense mechanism against a buildup of glutamate, which may be neurotoxic. And that’s a fascinating bit of homeostasis.
Of course, it makes you wonder how we might adjust glutamate levels in the brain, although maybe we should let the brain be tired if the brain wants to be tired. It reminds me of that old Far Side cartoon where the guy is raising his hand and asking: “Can I be excused? My brain is full.” That is essentially what’s happening. This part of your brain is becoming taxed and building up glutamate. There’s some kind of negative feedback loop. The authors don’t know what the receptor pathway is that down-regulates that part of the brain based on the glutamate buildup, but some kind of negative feedback loop is saying, okay, give this part of the brain a rest. Things have gone on too far here.
It’s a fascinating study, although it’s not clear what we can do with this information. It’s not clear whether we can manipulate glutamate levels in this particular part of the brain or not. But it’s nice to see some biologic correlates of a psychological phenomenon that is incredibly well described – the phenomenon of decision fatigue. I think we all feel it at the end of a hard workday. If you’ve been doing a lot of cognitively intensive tasks, you just don’t have it in you anymore. And maybe the act of a good night’s sleep is clearing out some of that glutamate in the LLPC, which lets you start over and make some good decisions again. So I hope you all make some good decisions and keep your glutamate levels low. And I’ll see you next time.
For Medscape, I’m Perry Wilson.
Dr. Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Once again, we’re doing an informal journal club to talk about a really interesting study, “A Neuro-metabolic Account of Why Daylong Cognitive Work Alters the Control of Economic Decisions,” that just came out. It tries to answer the question of why our brains wear out. I’m going to put myself in the corner here. Let’s walk through this study, which appears in Current Biology, by lead author Antonius Wiehler from Paris.
The big question is what’s going on with cognitive fatigue. If you look at chess players who are exerting a lot of cognitive effort, it’s well documented that over hours of play, they get worse and make more mistakes. It takes them longer to make decisions. The question is, why?
Why does your brain get tired?
To date, it’s been a little bit hard to tease that out. Now, there is some suggestion of what is responsible for this. The cognitive control center of the brain is probably somewhere in the left lateral prefrontal cortex (LLPC).
The prefrontal cortex is responsible for higher-level thinking. It’s what causes you to be inhibited. It gets shut off by alcohol and leads to impulsive behaviors. The LLPC, according to functional MRI studies, has reduced activity as people become more and more cognitively fatigued. The LLPC helps you think through choices. As you become more fatigued, this area of the brain isn’t working as well. But why would it not work as well? What is going on in that particular part of the brain? It doesn’t seem to be something simple, like glucose levels; that’s been investigated and glucose levels are pretty constant throughout the brain, regardless of cognitive task. This paper seeks to tease out what is actually going on in the LLPC when you are becoming cognitively tired.
They did an experiment where they induced cognitive fatigue, and it sounds like a painful experiment. For more than 6 hours, volunteers completed sessions during which they had to perform cognitive switching tasks. Investigators showed participants a letter, in either red or green, and the participant would respond with whether it was a vowel or a consonant or whether it was a capital or lowercase letter, based on the color. If it’s red, say whether it’s a consonant or vowel. If it’s green, say whether it’s upper- or lowercase.
It’s hard, and doing it for 6 hours is likely to induce a lot of cognitive fatigue. They had a control group as well, which is really important here. The control group also did a task like this for 6 hours, but for them, investigators didn’t change the color as often – perhaps only once per session. For the study group, they were switching colors back and forth quite a lot. They also incorporated a memory challenge that worked in a similar way.
So, what are the readouts of this study? They had a group who went through the hard cognitive challenge and a group who went through the easy cognitive challenge. They looked at a variety of metrics. I’ll describe a few.
The first is performance decrement. Did they get it wrong? What percentage of the time did the participant say “consonant” when they should have said “lowercase?”
You can see here that the hard group did a little bit worse overall. It was harder, so they don’t do as well. That makes sense. But both groups kind of waned over time a little bit. It’s not as though the hard group declines much more. The slopes of those lines are pretty similar. So, not very robust findings there.
What about subjective fatigue? They asked the participants how exhausted they were from doing the tasks.
Both groups were worn out. It was a long day. There was a suggestion that the hard group became worn out a little bit sooner, but I don’t think this achieves statistical significance. Everyone was getting tired by hour 6 here.
What about response time? How quickly could the participant say “consonant,” “vowel,” “lowercase,” or “uppercase?”
The hard group took longer to respond because it was a harder task. But over time, the response times were pretty flat.
So far there isn’t a robust readout that would make us say, oh, yeah, that is a good marker of cognitive fatigue. That’s how you measure cognitive fatigue. It’s not what people say. It’s not how quick they are. It’s not even how accurate they are.
But then the investigators got a little bit clever. Participants were asked to play a “would you rather” game, a reward game. Here are two examples.
Would you rather:
- Have a 25% chance of earning $50 OR a 95% chance of earning $17.30?
- Earn $50, but your next task session will be hard or earn $40 and your next task session will be easy?
Participants had to figure out the better odds – what should they be choosing here? They had to tease out whether they preferred lower cost lower-risk choices – when they are cognitively fatigued, which has been shown in prior studies.
This showed a pretty dramatic difference between the groups in terms of the low-cost bias – how much more likely they were to pick the low-cost, easier choice as they became more and more cognitively fatigued. The hard group participants were more likely to pick the easy thing rather than the potentially more lucrative thing, which is really interesting when we think about how our own cognitive fatigue happens at the end of a difficult workday, how you may just be likely to go with the flow and do something easy because you just don’t have that much decision-making power left.
It would be nice to have some objective physiologic measurements for this, and they do. This is pupil dilation.
When you’re paying attention to something, your pupils dilate a little bit. They were able to show that as the hard group became more and more fatigued, pupil dilation sort of went away. In fact, if anything, their pupils constricted a little bit. But basically there was a significant difference here. The easy group’s pupils were still fine; they were still dilating. The hard group’s pupils got more sluggish. This is a physiologic correlate of what’s going on.
But again, these are all downstream of whatever is happening in the LLPC. So the real meat of this study is a functional MRI analysis, and the way they did this is pretty clever. They were looking for metabolites in the various parts of the brain using a labeled hydrogen MRI, which is even fancier than a functional MRI. It’s like MRI spectroscopy, and it can measure the levels of certain chemicals in the brain. They hypothesized that if there is a chemical that builds up when you are tired, it should build up preferentially in the LLPC.
Whereas in the rest of the brain, there shouldn’t be that much difference because we know the action is happening in the LLPC. The control part of the brain is a section called V1. They looked at a variety of metabolites, but the only one that behaved the way they expected was glutamate and glutamic acid (glutamate metabolites). In the hard group, the glutamate is building up over time, so there is a higher concentration of glutamate in the LLPC but not the rest of the brain. There is also a greater diffusion of glutamate from the intracellular to the extracellular space, which suggests that it’s kind of leaking out of the cells.
So the signal here is that the thing that’s impacting that part of the brain is this buildup of glutamate. To tie this together, they showed in the scatterplot the relationship between the increase in glutamate and the low-cost bias from the decision fatigue example.
It’s not the strongest correlation, but it is statistically significant that the more glutamate in your LLPC, the more likely you are to just take the easy decision as opposed to really thinking things through. That is pretty powerful. It’s telling us that your brain making you fatigued, and making you less likely to continue to use your LLPC, may be a self-defense mechanism against a buildup of glutamate, which may be neurotoxic. And that’s a fascinating bit of homeostasis.
Of course, it makes you wonder how we might adjust glutamate levels in the brain, although maybe we should let the brain be tired if the brain wants to be tired. It reminds me of that old Far Side cartoon where the guy is raising his hand and asking: “Can I be excused? My brain is full.” That is essentially what’s happening. This part of your brain is becoming taxed and building up glutamate. There’s some kind of negative feedback loop. The authors don’t know what the receptor pathway is that down-regulates that part of the brain based on the glutamate buildup, but some kind of negative feedback loop is saying, okay, give this part of the brain a rest. Things have gone on too far here.
It’s a fascinating study, although it’s not clear what we can do with this information. It’s not clear whether we can manipulate glutamate levels in this particular part of the brain or not. But it’s nice to see some biologic correlates of a psychological phenomenon that is incredibly well described – the phenomenon of decision fatigue. I think we all feel it at the end of a hard workday. If you’ve been doing a lot of cognitively intensive tasks, you just don’t have it in you anymore. And maybe the act of a good night’s sleep is clearing out some of that glutamate in the LLPC, which lets you start over and make some good decisions again. So I hope you all make some good decisions and keep your glutamate levels low. And I’ll see you next time.
For Medscape, I’m Perry Wilson.
Dr. Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Once again, we’re doing an informal journal club to talk about a really interesting study, “A Neuro-metabolic Account of Why Daylong Cognitive Work Alters the Control of Economic Decisions,” that just came out. It tries to answer the question of why our brains wear out. I’m going to put myself in the corner here. Let’s walk through this study, which appears in Current Biology, by lead author Antonius Wiehler from Paris.
The big question is what’s going on with cognitive fatigue. If you look at chess players who are exerting a lot of cognitive effort, it’s well documented that over hours of play, they get worse and make more mistakes. It takes them longer to make decisions. The question is, why?
Why does your brain get tired?
To date, it’s been a little bit hard to tease that out. Now, there is some suggestion of what is responsible for this. The cognitive control center of the brain is probably somewhere in the left lateral prefrontal cortex (LLPC).
The prefrontal cortex is responsible for higher-level thinking. It’s what causes you to be inhibited. It gets shut off by alcohol and leads to impulsive behaviors. The LLPC, according to functional MRI studies, has reduced activity as people become more and more cognitively fatigued. The LLPC helps you think through choices. As you become more fatigued, this area of the brain isn’t working as well. But why would it not work as well? What is going on in that particular part of the brain? It doesn’t seem to be something simple, like glucose levels; that’s been investigated and glucose levels are pretty constant throughout the brain, regardless of cognitive task. This paper seeks to tease out what is actually going on in the LLPC when you are becoming cognitively tired.
They did an experiment where they induced cognitive fatigue, and it sounds like a painful experiment. For more than 6 hours, volunteers completed sessions during which they had to perform cognitive switching tasks. Investigators showed participants a letter, in either red or green, and the participant would respond with whether it was a vowel or a consonant or whether it was a capital or lowercase letter, based on the color. If it’s red, say whether it’s a consonant or vowel. If it’s green, say whether it’s upper- or lowercase.
It’s hard, and doing it for 6 hours is likely to induce a lot of cognitive fatigue. They had a control group as well, which is really important here. The control group also did a task like this for 6 hours, but for them, investigators didn’t change the color as often – perhaps only once per session. For the study group, they were switching colors back and forth quite a lot. They also incorporated a memory challenge that worked in a similar way.
So, what are the readouts of this study? They had a group who went through the hard cognitive challenge and a group who went through the easy cognitive challenge. They looked at a variety of metrics. I’ll describe a few.
The first is performance decrement. Did they get it wrong? What percentage of the time did the participant say “consonant” when they should have said “lowercase?”
You can see here that the hard group did a little bit worse overall. It was harder, so they don’t do as well. That makes sense. But both groups kind of waned over time a little bit. It’s not as though the hard group declines much more. The slopes of those lines are pretty similar. So, not very robust findings there.
What about subjective fatigue? They asked the participants how exhausted they were from doing the tasks.
Both groups were worn out. It was a long day. There was a suggestion that the hard group became worn out a little bit sooner, but I don’t think this achieves statistical significance. Everyone was getting tired by hour 6 here.
What about response time? How quickly could the participant say “consonant,” “vowel,” “lowercase,” or “uppercase?”
The hard group took longer to respond because it was a harder task. But over time, the response times were pretty flat.
So far there isn’t a robust readout that would make us say, oh, yeah, that is a good marker of cognitive fatigue. That’s how you measure cognitive fatigue. It’s not what people say. It’s not how quick they are. It’s not even how accurate they are.
But then the investigators got a little bit clever. Participants were asked to play a “would you rather” game, a reward game. Here are two examples.
Would you rather:
- Have a 25% chance of earning $50 OR a 95% chance of earning $17.30?
- Earn $50, but your next task session will be hard or earn $40 and your next task session will be easy?
Participants had to figure out the better odds – what should they be choosing here? They had to tease out whether they preferred lower cost lower-risk choices – when they are cognitively fatigued, which has been shown in prior studies.
This showed a pretty dramatic difference between the groups in terms of the low-cost bias – how much more likely they were to pick the low-cost, easier choice as they became more and more cognitively fatigued. The hard group participants were more likely to pick the easy thing rather than the potentially more lucrative thing, which is really interesting when we think about how our own cognitive fatigue happens at the end of a difficult workday, how you may just be likely to go with the flow and do something easy because you just don’t have that much decision-making power left.
It would be nice to have some objective physiologic measurements for this, and they do. This is pupil dilation.
When you’re paying attention to something, your pupils dilate a little bit. They were able to show that as the hard group became more and more fatigued, pupil dilation sort of went away. In fact, if anything, their pupils constricted a little bit. But basically there was a significant difference here. The easy group’s pupils were still fine; they were still dilating. The hard group’s pupils got more sluggish. This is a physiologic correlate of what’s going on.
But again, these are all downstream of whatever is happening in the LLPC. So the real meat of this study is a functional MRI analysis, and the way they did this is pretty clever. They were looking for metabolites in the various parts of the brain using a labeled hydrogen MRI, which is even fancier than a functional MRI. It’s like MRI spectroscopy, and it can measure the levels of certain chemicals in the brain. They hypothesized that if there is a chemical that builds up when you are tired, it should build up preferentially in the LLPC.
Whereas in the rest of the brain, there shouldn’t be that much difference because we know the action is happening in the LLPC. The control part of the brain is a section called V1. They looked at a variety of metabolites, but the only one that behaved the way they expected was glutamate and glutamic acid (glutamate metabolites). In the hard group, the glutamate is building up over time, so there is a higher concentration of glutamate in the LLPC but not the rest of the brain. There is also a greater diffusion of glutamate from the intracellular to the extracellular space, which suggests that it’s kind of leaking out of the cells.
So the signal here is that the thing that’s impacting that part of the brain is this buildup of glutamate. To tie this together, they showed in the scatterplot the relationship between the increase in glutamate and the low-cost bias from the decision fatigue example.
It’s not the strongest correlation, but it is statistically significant that the more glutamate in your LLPC, the more likely you are to just take the easy decision as opposed to really thinking things through. That is pretty powerful. It’s telling us that your brain making you fatigued, and making you less likely to continue to use your LLPC, may be a self-defense mechanism against a buildup of glutamate, which may be neurotoxic. And that’s a fascinating bit of homeostasis.
Of course, it makes you wonder how we might adjust glutamate levels in the brain, although maybe we should let the brain be tired if the brain wants to be tired. It reminds me of that old Far Side cartoon where the guy is raising his hand and asking: “Can I be excused? My brain is full.” That is essentially what’s happening. This part of your brain is becoming taxed and building up glutamate. There’s some kind of negative feedback loop. The authors don’t know what the receptor pathway is that down-regulates that part of the brain based on the glutamate buildup, but some kind of negative feedback loop is saying, okay, give this part of the brain a rest. Things have gone on too far here.
It’s a fascinating study, although it’s not clear what we can do with this information. It’s not clear whether we can manipulate glutamate levels in this particular part of the brain or not. But it’s nice to see some biologic correlates of a psychological phenomenon that is incredibly well described – the phenomenon of decision fatigue. I think we all feel it at the end of a hard workday. If you’ve been doing a lot of cognitively intensive tasks, you just don’t have it in you anymore. And maybe the act of a good night’s sleep is clearing out some of that glutamate in the LLPC, which lets you start over and make some good decisions again. So I hope you all make some good decisions and keep your glutamate levels low. And I’ll see you next time.
For Medscape, I’m Perry Wilson.
Dr. Wilson is an associate professor of medicine and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.