User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Electroacupuncture promising for depression-related insomnia
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).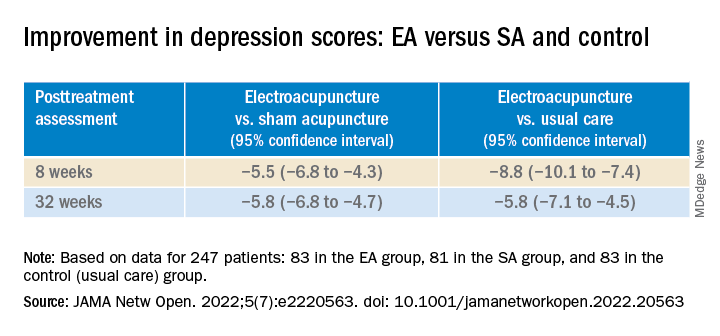
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).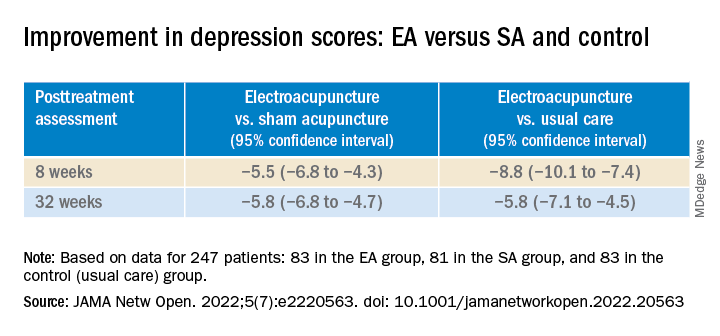
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).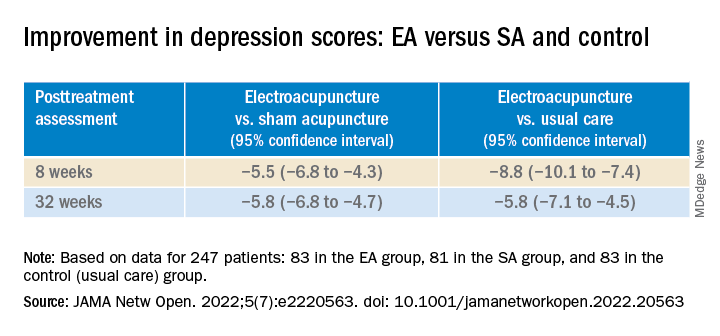
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Anxiety spreads from mother to daughter, father to son
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
The new findings suggest that children learn anxious behavior from their parents, study investigator Barbara Pavlova, PhD, clinical psychologist with Nova Scotia Health Authority, told this news organization.
“This means that transmission of anxiety from parents to children may be preventable,” said Dr. Pavlova, assistant professor, department of psychiatry, Dalhousie University, Halifax, Canada.
“Treating parents’ anxiety is not just important for their own health but also for the health of their children. This may be especially true if the child and the parent are the same sex,” Dr. Pavlova added.
The study was published online in JAMA Network Open.
Parental anxiety a disruptor
Anxiety disorders run in families. Both genes and environment are thought to be at play, but there are few data on sex-specific transmission from parent to child.
To investigate, the researchers conducted a cross-sectional study of 203 girls and 195 boys and their parents. The average age of the children was 11 years, and they had a familial risk for mood disorders.
Anxiety disorder in a same-sex parent was significantly associated with anxiety disorder in offspring (odds ratio, 2.85; 95% confidence interval, 1.52-5.34; P = .001) but not in an opposite-sex parent (OR, 1.51; 95% CI, 0.81-2.81; P = .20).
Living with a same-sex parent without anxiety was associated with lower rates of offspring anxiety (OR, 0.38; 95% CI, 0.22-0.67; P = .001).
Among all 398 children, 108 (27%) had been diagnosed with one or more anxiety disorders, including generalized anxiety disorder (7.8%), social anxiety disorder (6.3%), separation anxiety disorder (8.6%), specific phobia (8%), and anxiety disorder not otherwise specified (5%).
Rates of anxiety disorders in children increased with age, from 14% in those younger than 9 years to 52% in those older than 15 years. Anxiety disorders were similarly common among boys (24%) and girls (30%).
Rates of anxiety disorders were lowest (24%) in children of two parents without anxiety disorders and highest (41%) in cases in which both parents had anxiety disorders.
The findings point to the possible role of environmental factors, “such as modeling and vicarious learning,” in the transmission of anxiety from parents to their children, the researchers note.
“A child receives [a] similar amount of genetic information from each biological parent. A strong same-sex parent effect suggests children learn resilience by modeling the behavior of their same-sex parent. A parent’s anxiety disorder may disrupt this protective learning,” said Dr. Pavlova.
Early diagnosis, treatment essential
Reached for comment, Jill Emanuele, PhD, vice president of clinical training for the Child MIND Institute, New York, said that when it comes to anxiety, it’s important to assess and treat both the parent and the child.
“We know that both environment and genetics play a role in anxiety disorders. From a clinical perspective, if we see a parent with an anxiety disorder, we know that there is a chance that that is also going to affect the child – whether or not the child has an anxiety disorder,” Dr. Emanuele said in an interview.
“Anxiety disorders are the most common psychiatric disorders diagnosed. We also know that anxiety disorders emerge earlier than mood disorders and certainly can emerge in childhood. It’s important to address anxiety early because those same problems can continue into adulthood if left untreated,” Dr. Emanuele added.
The study was supported by the Canada Research Chairs Program, the Canadian Institutes of Health Research, the Brain & Behavior Research Foundation, the Nova Scotia Health Research Foundation, and the Dalhousie Medical Research Foundation. The authors have disclosed no relevant financial relationships. Dr. Emanuele is a board member with the Anxiety and Depression Association of America.
A version of this article first appeared on Medscape.com.
Americans’ biggest source of anxiety? Hint: It’s not COVID-19
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
, results from a new national report from the American Psychiatric Association show.
“The economy seems to have supplanted COVID as a major factor in Americans’ day-to-day anxiety,” APA President Rebecca W. Brendel, MD, JD, said in a news release.
“Knowing that so many Americans are concerned about finances is important because it can prepare clinicians to be ready to approach the subject, which is one that people are often reluctant or ashamed to raise on their own,” Dr. Brendel told this news organization.
What’s the best way to bring up the sensitive topic of money?
“In general, it’s best to start with open-ended questions to allow individuals in therapy to share what is on their minds, explore their concerns, and develop strategies to address these issues. Once a patient raises a concern, that is a good time to ask more about the issues they’ve raised and to explore other potential sources of anxiety or stress,” said Dr. Brendel.
The latest APA poll was conducted by Morning Consult, June 18-20, 2022, among a nationally representative sample of 2,210 adults.
In addition to an uptick in worry about inflation, the poll shows that more than half (51%) of adults are worried about a potential loss of income.
Hispanic adults (66%), mothers (65%), millennials (63%), and genZers (62%) are among the groups most likely to be concerned about income loss.
“Stress is not good for health, mental or physical. So, while it’s a reality that Americans are faced with finding ways of making ends meet, it’s more important than ever to make sure that we are all accessing the care that we need,” said Dr. Brendel.
“People should be aware that there may be low- or no-cost options such as community mental health centers or employer-sponsored resources to address mental health concerns,” she added.
Coping with traumatic events
The latest poll also shows that about one-third of adults are worried about gun violence (35% overall, 47% among genZers) or a natural disaster (29%) personally affecting them.
Climate change anxiety is also up slightly in June, compared with May (+4%).
The same goes for mid-term election-related anxiety (+3%) – particularly among Democrats (54% vs. 59%) compared with Republicans (48% vs. 48%).
The latest poll provides insight how Americans would cope after a traumatic event. More adults report they will turn to family and friends for support (60%) than practice self-care (42%), speak openly about their feelings (37%), or seek help from a professional (31%). Nearly one-third (30%) say they will move on from it and not dwell on their feelings.
GenZers are the least likely to say they will speak openly about their feelings (29%) and are less likely than millennials to say they would speak to a health professional (28% vs. 38%).
“While many people show resilience, it’s troubling that most Americans wouldn’t speak openly about their feelings after a traumatic event,” APA CEO and Medical Director Saul Levin, MD, said in the news release.
“In many ways, naming feelings is the most important step toward healing, and this reluctance to air our thoughts may indicate that mental health stigma is still a powerful force in our society,” Dr. Levin said.
After a traumatic current event, 41% of Americans say they consume more news and 30% say they take in more social media, but the majority say this does not impact their mental health, the poll shows.
Two in five adults (43%) say the news of a traumatic event makes them feel more informed, 32% say it makes them feel more anxious, and about one-quarter say it makes them feel overwhelmed (27%) or discouraged (24%).
Dr. Brendel noted that, after a traumatic event, “it’s expected that people may experience anxiety or other symptoms for brief periods of time. However, no two people experience things the same way. If symptoms don’t go away, are overwhelming, or get worse over time, for example, it’s critical to seek help right away.”
The June poll shows that 50% of Americans are anxious about the future of reproductive rights but the poll was conducted before the Dobbs ruling.
Anxiety around COVID-19 continues to ease, with about 47% of Americans saying they are concerned about the pandemic, down 2% among all Americans and 16% among Black Americans since May.
The APA’s Healthy Minds Monthly tracks timely mental health issues throughout the year. The APA also releases its annual Healthy Minds Poll each May in conjunction with Mental Health Awareness Month.
A version of this article first appeared on Medscape.com.
Red Flag: Suicide risk
How AI is helping prevent suicide in veterans

Medically reviewed by Jennifer Casarella, MD
Dan Miller has parked his Nissan Altima on the side of the road near a field outside Chicago and is holding a gun to his head.
Haunted for years by the compounded trauma of tours of duty in the Middle East and his work as a police officer in Chicago, at that moment, Dr. Miller saw no reason to live. And there were troubles at home with his wife and children, who had grown fearful of his behavior.
“My whole world was falling apart,” he says of that dark night in 2014. “It left a hole I didn’t know how to fill.”
He chose not to pull the trigger after a brochure on the passenger seat of his car gave him an unexpected perspective – and launched him on a path to help others in his situation.
Had Mr. Miller taken his life that night, he would have joined thousands of other veterans who died by suicide. About 17 U.S. veterans lose their lives this way each day, on average, according to the Department of Veterans Affairs. In 2019, the last year for which records are available, 6,261 veterans took their own lives – and the suicide rate for veterans was 52% higher than for nonveterans, the agency’s records show.
The problem has become so severe that
But that wasn’t available when Dan Miller’s life was unraveling.
In the years leading up to his near-suicide, his wife had pushed him to get help. “She said, ‘You’re not the same person you were when you left. The kids are scared of you. The pets are scared of you,” he recalls.
He resisted, even when his wife threatened divorce. Rising through the ranks of the Marines, Mr. Miller had become more emotionally isolated. He feared losing his job and the respect of others if he let anyone know what he was going through.
Finally, he gave the VHA a chance. He went in for an initial consultation in 2010 and didn’t find it helpful. He didn’t like being told what to do. So he stopped. He turned to obsessive exercise and excessive drinking.
That day in 2014, Mr. Miller’s wife told him she was taking the kids out for a playdate. After she left, he was served with divorce papers. Less than an hour later, he was parked in his car with his gun, ready to end his life.
But if it all had happened just a few years later, things might never have gotten to that point.
Scanning for suicide risk
In 2017, the VHA piloted its AI program, called REACH VET, that aims to help prevent veterans from dying by suicide.
Every month, a computer scans the electronic health records of all VHA patients who’ve had a health care visit for any reason in the last 2 years. It checks more than 140 variables and weights them to estimate someone’s overall suicide risk at that moment in time.
To build the risk algorithm, a computer combed through the medical records of 6,360 veterans confirmed to have died by suicide between 2009 and 2011. (The VHA continually updates the list of variables from the health records of VHA patients, including those who have died by suicide since then and others.)
Some variables are things you’d expect:
- A past suicide attempt.
- A diagnosis of depression or other mental illness.
- A diagnosis of a terminal illness.
Others are more surprising. For example, a diagnosis of arthritis or diabetes adds weight.
REACH VET flags the riskiest cases – the top 0.1% – for a mental health or primary care provider to review. They reach out to the patient to tell them how and why their record was flagged, discuss any recommended treatment changes, and ask them to come in for a visit.
“It’s an opportunity to talk about their risk factors, which is designed to lead to a conversation about safety planning,” says clinical psychologist Matthew Miller, PhD, national director of the U.S. Department of Veterans Affairs’ Suicide Prevention Program. He’s not related to Dan Miller.
Making a suicide safety plan
A safety plan is a document that outlines how a person can help prevent their own suicide in a crisis.
The plan may include:
- A list of personal triggers or warning signs.
- What’s helped them in the past.
- Names of people or organizations who can support them.
- Plans to remove means of suicide, such as guns, from their environment.
- Their reasons for living.
In people at risk for suicide, research shows that having a safety plan reduces suicidal thoughts and attempts, lowers rates of depression and hopelessness, and boosts veterans’ engagement with the health care system. It may also help people manage things that trigger their suicidal thoughts.
Getting the call
What if REACH VET had been around when Dan Miller was in crisis – and he’d gotten a call from the VHA?
“It absolutely, positively would have helped because one of the biggest things on that day when I got served was feeling completely alone and that I had no one to turn to,” Mr. Miller says. He’s now a speaker for the Wounded Warrior Project, a nonprofit that serves veterans and active-duty service people.
Vets’ reactions to the unexpected VHA phone call, psychologist Dr. Miller says, “run the gamut from ‘Thank you for contacting me. Let’s talk,’ to ‘What are you talking about? Leave me alone!’ ”
Nothing stops all suicides. But REACH VET is having an impact. In a clinical trial, vets contacted through REACH VET had more doctor visits, were more likely to have a written suicide prevention safety plan, and had fewer hospital admissions for mental health, ER visits, and suicide attempts.
An assist from AI
Even simple outreach can make a big difference. And there’s research to prove it.
One study included 4,730 veterans recently discharged from psychiatric care at the VHA, a group considered at high risk for suicide.
Half of them got 13 caring emails from hospital staff in the weeks after leaving the hospital. The emails mentioned personal things the patient had shared, like a love of hiking, and wished them well. The other veterans got routine follow-up but no emails.
Two years later, those who got the caring emails were less likely to have died by suicide than the other vets. The study was published in 2014 in Contemporary Clinical Trials.
Researchers have done studies like this many times: with handwritten notes from the primary care doctor, postcards from the ER, and so forth. The results never vary: The notes reduce suicide risk.
“If we could use AI to identify people to receive notes or phone calls, it would be a very effective and inexpensive way to guide follow-up care,” says Rebecca Bernert, PhD, director and founder of the Suicide Prevention Research Laboratory at Stanford (Calif.) University.
AI doesn’t replace clinical judgment.
“AI can capture data that we miss due to the limits of our humanity,” psychologist Dr. Miller says. “There’s suicide prevention processes founded on big data and AI, and there are processes founded in clinical intuition and acumen.”
AI is only as good as the data it’s based on. If that data lacks diversity, it may miss things. And variables that apply to veterans may differ in civilians.
Stopping suicidal thoughts
Google is putting AI to work against suicide, too. Its MUM (Multitask Unified Model) technology seeks to understand the intent behind what we google.
MUM powers Google Search. It can often tell the difference between a search for information about suicide for someone writing a research paper on the topic and a search for information on how or where to carry out a suicide.
When Google Search detects that someone in the United States might be in crisis and at risk of suicide, the first search results that person gets are the number for the National Suicide Prevention Lifeline and other resources for people in crisis.
Google Home Assistant works in the same way. When a user makes a query that signals a suicide-related crisis, the gadget serves up resources that offer help.
MUM is working to understand the nuances of crisis language in 75 languages so that Google Search can provide people in crisis with hotlines or other resources in many countries.
“We want to find partners that are accessible to users in terms of hours of operation. We have a strong preference for finding partners that promise confidentiality and privacy to the extent that those are permitted [in that country],” says Anne Merritt, MD, a product manager at Google Search.
Other companies are working on apps that use AI to spot suicide risk in other ways, including voice technology that may notice subtle changes in the voice of someone who’s depressed and may be thinking of suicide. Those are still in development but show promise. Keep in mind that apps do not require government approval, so if you try one, be sure to let your health care provider know.
Changing the channel
Seeing a hotline number on your phone or computer screen can help, Dan Miller says. “If I happened to be online, searching maybe for a bridge to jump off of ... and suddenly that pops up on the screen, it’s like it changes the channel.”
It may not work for everyone, he says, but that search result could interrupt someone’s suicidal train of thought.
That’s crucial, psychologist Dr. Miller says, because most suicide attempts escalate from first thought to potentially fatal action in just 1 hour. That’s how fast it happened for Dan Miller in 2014.
“When you’re able to put time and space between the suicidal thought and the access to the method to act on that thought, you save lives,” Dr. Bernert says.
Making a different choice
An interruption in Mr. Miller’s thinking is what had saved his life.
Holding the gun to his head, Mr. Miller looked over at the passenger seat at a brochure from Wounded Warrior Project, which he had just learned about. Mr. Miller noticed a photo of a man in a wheelchair, a veteran like him, who had no legs. He thought that the man looked worse off than him but hadn’t given up.
Mr. Miller put down his gun and decided to get help.
Recovering from a near suicide attempt, he says, is a journey. It doesn’t happen overnight. Now, 8 years later, Mr. Miller is planning a brief break from the speaker circuit. He plans to spend 2 weeks in an outpatient counseling program for posttraumatic stress disorder and traumatic brain injury.
“Telling my story to strangers – part of it is healing me in a way, but I’m learning that repeating the story over and over again is also keeping me from letting it go. And I’m still healing.”
A version of this article first appeared on WebMD.com.
How AI is helping prevent suicide in veterans
How AI is helping prevent suicide in veterans

Medically reviewed by Jennifer Casarella, MD
Dan Miller has parked his Nissan Altima on the side of the road near a field outside Chicago and is holding a gun to his head.
Haunted for years by the compounded trauma of tours of duty in the Middle East and his work as a police officer in Chicago, at that moment, Dr. Miller saw no reason to live. And there were troubles at home with his wife and children, who had grown fearful of his behavior.
“My whole world was falling apart,” he says of that dark night in 2014. “It left a hole I didn’t know how to fill.”
He chose not to pull the trigger after a brochure on the passenger seat of his car gave him an unexpected perspective – and launched him on a path to help others in his situation.
Had Mr. Miller taken his life that night, he would have joined thousands of other veterans who died by suicide. About 17 U.S. veterans lose their lives this way each day, on average, according to the Department of Veterans Affairs. In 2019, the last year for which records are available, 6,261 veterans took their own lives – and the suicide rate for veterans was 52% higher than for nonveterans, the agency’s records show.
The problem has become so severe that
But that wasn’t available when Dan Miller’s life was unraveling.
In the years leading up to his near-suicide, his wife had pushed him to get help. “She said, ‘You’re not the same person you were when you left. The kids are scared of you. The pets are scared of you,” he recalls.
He resisted, even when his wife threatened divorce. Rising through the ranks of the Marines, Mr. Miller had become more emotionally isolated. He feared losing his job and the respect of others if he let anyone know what he was going through.
Finally, he gave the VHA a chance. He went in for an initial consultation in 2010 and didn’t find it helpful. He didn’t like being told what to do. So he stopped. He turned to obsessive exercise and excessive drinking.
That day in 2014, Mr. Miller’s wife told him she was taking the kids out for a playdate. After she left, he was served with divorce papers. Less than an hour later, he was parked in his car with his gun, ready to end his life.
But if it all had happened just a few years later, things might never have gotten to that point.
Scanning for suicide risk
In 2017, the VHA piloted its AI program, called REACH VET, that aims to help prevent veterans from dying by suicide.
Every month, a computer scans the electronic health records of all VHA patients who’ve had a health care visit for any reason in the last 2 years. It checks more than 140 variables and weights them to estimate someone’s overall suicide risk at that moment in time.
To build the risk algorithm, a computer combed through the medical records of 6,360 veterans confirmed to have died by suicide between 2009 and 2011. (The VHA continually updates the list of variables from the health records of VHA patients, including those who have died by suicide since then and others.)
Some variables are things you’d expect:
- A past suicide attempt.
- A diagnosis of depression or other mental illness.
- A diagnosis of a terminal illness.
Others are more surprising. For example, a diagnosis of arthritis or diabetes adds weight.
REACH VET flags the riskiest cases – the top 0.1% – for a mental health or primary care provider to review. They reach out to the patient to tell them how and why their record was flagged, discuss any recommended treatment changes, and ask them to come in for a visit.
“It’s an opportunity to talk about their risk factors, which is designed to lead to a conversation about safety planning,” says clinical psychologist Matthew Miller, PhD, national director of the U.S. Department of Veterans Affairs’ Suicide Prevention Program. He’s not related to Dan Miller.
Making a suicide safety plan
A safety plan is a document that outlines how a person can help prevent their own suicide in a crisis.
The plan may include:
- A list of personal triggers or warning signs.
- What’s helped them in the past.
- Names of people or organizations who can support them.
- Plans to remove means of suicide, such as guns, from their environment.
- Their reasons for living.
In people at risk for suicide, research shows that having a safety plan reduces suicidal thoughts and attempts, lowers rates of depression and hopelessness, and boosts veterans’ engagement with the health care system. It may also help people manage things that trigger their suicidal thoughts.
Getting the call
What if REACH VET had been around when Dan Miller was in crisis – and he’d gotten a call from the VHA?
“It absolutely, positively would have helped because one of the biggest things on that day when I got served was feeling completely alone and that I had no one to turn to,” Mr. Miller says. He’s now a speaker for the Wounded Warrior Project, a nonprofit that serves veterans and active-duty service people.
Vets’ reactions to the unexpected VHA phone call, psychologist Dr. Miller says, “run the gamut from ‘Thank you for contacting me. Let’s talk,’ to ‘What are you talking about? Leave me alone!’ ”
Nothing stops all suicides. But REACH VET is having an impact. In a clinical trial, vets contacted through REACH VET had more doctor visits, were more likely to have a written suicide prevention safety plan, and had fewer hospital admissions for mental health, ER visits, and suicide attempts.
An assist from AI
Even simple outreach can make a big difference. And there’s research to prove it.
One study included 4,730 veterans recently discharged from psychiatric care at the VHA, a group considered at high risk for suicide.
Half of them got 13 caring emails from hospital staff in the weeks after leaving the hospital. The emails mentioned personal things the patient had shared, like a love of hiking, and wished them well. The other veterans got routine follow-up but no emails.
Two years later, those who got the caring emails were less likely to have died by suicide than the other vets. The study was published in 2014 in Contemporary Clinical Trials.
Researchers have done studies like this many times: with handwritten notes from the primary care doctor, postcards from the ER, and so forth. The results never vary: The notes reduce suicide risk.
“If we could use AI to identify people to receive notes or phone calls, it would be a very effective and inexpensive way to guide follow-up care,” says Rebecca Bernert, PhD, director and founder of the Suicide Prevention Research Laboratory at Stanford (Calif.) University.
AI doesn’t replace clinical judgment.
“AI can capture data that we miss due to the limits of our humanity,” psychologist Dr. Miller says. “There’s suicide prevention processes founded on big data and AI, and there are processes founded in clinical intuition and acumen.”
AI is only as good as the data it’s based on. If that data lacks diversity, it may miss things. And variables that apply to veterans may differ in civilians.
Stopping suicidal thoughts
Google is putting AI to work against suicide, too. Its MUM (Multitask Unified Model) technology seeks to understand the intent behind what we google.
MUM powers Google Search. It can often tell the difference between a search for information about suicide for someone writing a research paper on the topic and a search for information on how or where to carry out a suicide.
When Google Search detects that someone in the United States might be in crisis and at risk of suicide, the first search results that person gets are the number for the National Suicide Prevention Lifeline and other resources for people in crisis.
Google Home Assistant works in the same way. When a user makes a query that signals a suicide-related crisis, the gadget serves up resources that offer help.
MUM is working to understand the nuances of crisis language in 75 languages so that Google Search can provide people in crisis with hotlines or other resources in many countries.
“We want to find partners that are accessible to users in terms of hours of operation. We have a strong preference for finding partners that promise confidentiality and privacy to the extent that those are permitted [in that country],” says Anne Merritt, MD, a product manager at Google Search.
Other companies are working on apps that use AI to spot suicide risk in other ways, including voice technology that may notice subtle changes in the voice of someone who’s depressed and may be thinking of suicide. Those are still in development but show promise. Keep in mind that apps do not require government approval, so if you try one, be sure to let your health care provider know.
Changing the channel
Seeing a hotline number on your phone or computer screen can help, Dan Miller says. “If I happened to be online, searching maybe for a bridge to jump off of ... and suddenly that pops up on the screen, it’s like it changes the channel.”
It may not work for everyone, he says, but that search result could interrupt someone’s suicidal train of thought.
That’s crucial, psychologist Dr. Miller says, because most suicide attempts escalate from first thought to potentially fatal action in just 1 hour. That’s how fast it happened for Dan Miller in 2014.
“When you’re able to put time and space between the suicidal thought and the access to the method to act on that thought, you save lives,” Dr. Bernert says.
Making a different choice
An interruption in Mr. Miller’s thinking is what had saved his life.
Holding the gun to his head, Mr. Miller looked over at the passenger seat at a brochure from Wounded Warrior Project, which he had just learned about. Mr. Miller noticed a photo of a man in a wheelchair, a veteran like him, who had no legs. He thought that the man looked worse off than him but hadn’t given up.
Mr. Miller put down his gun and decided to get help.
Recovering from a near suicide attempt, he says, is a journey. It doesn’t happen overnight. Now, 8 years later, Mr. Miller is planning a brief break from the speaker circuit. He plans to spend 2 weeks in an outpatient counseling program for posttraumatic stress disorder and traumatic brain injury.
“Telling my story to strangers – part of it is healing me in a way, but I’m learning that repeating the story over and over again is also keeping me from letting it go. And I’m still healing.”
A version of this article first appeared on WebMD.com.

Medically reviewed by Jennifer Casarella, MD
Dan Miller has parked his Nissan Altima on the side of the road near a field outside Chicago and is holding a gun to his head.
Haunted for years by the compounded trauma of tours of duty in the Middle East and his work as a police officer in Chicago, at that moment, Dr. Miller saw no reason to live. And there were troubles at home with his wife and children, who had grown fearful of his behavior.
“My whole world was falling apart,” he says of that dark night in 2014. “It left a hole I didn’t know how to fill.”
He chose not to pull the trigger after a brochure on the passenger seat of his car gave him an unexpected perspective – and launched him on a path to help others in his situation.
Had Mr. Miller taken his life that night, he would have joined thousands of other veterans who died by suicide. About 17 U.S. veterans lose their lives this way each day, on average, according to the Department of Veterans Affairs. In 2019, the last year for which records are available, 6,261 veterans took their own lives – and the suicide rate for veterans was 52% higher than for nonveterans, the agency’s records show.
The problem has become so severe that
But that wasn’t available when Dan Miller’s life was unraveling.
In the years leading up to his near-suicide, his wife had pushed him to get help. “She said, ‘You’re not the same person you were when you left. The kids are scared of you. The pets are scared of you,” he recalls.
He resisted, even when his wife threatened divorce. Rising through the ranks of the Marines, Mr. Miller had become more emotionally isolated. He feared losing his job and the respect of others if he let anyone know what he was going through.
Finally, he gave the VHA a chance. He went in for an initial consultation in 2010 and didn’t find it helpful. He didn’t like being told what to do. So he stopped. He turned to obsessive exercise and excessive drinking.
That day in 2014, Mr. Miller’s wife told him she was taking the kids out for a playdate. After she left, he was served with divorce papers. Less than an hour later, he was parked in his car with his gun, ready to end his life.
But if it all had happened just a few years later, things might never have gotten to that point.
Scanning for suicide risk
In 2017, the VHA piloted its AI program, called REACH VET, that aims to help prevent veterans from dying by suicide.
Every month, a computer scans the electronic health records of all VHA patients who’ve had a health care visit for any reason in the last 2 years. It checks more than 140 variables and weights them to estimate someone’s overall suicide risk at that moment in time.
To build the risk algorithm, a computer combed through the medical records of 6,360 veterans confirmed to have died by suicide between 2009 and 2011. (The VHA continually updates the list of variables from the health records of VHA patients, including those who have died by suicide since then and others.)
Some variables are things you’d expect:
- A past suicide attempt.
- A diagnosis of depression or other mental illness.
- A diagnosis of a terminal illness.
Others are more surprising. For example, a diagnosis of arthritis or diabetes adds weight.
REACH VET flags the riskiest cases – the top 0.1% – for a mental health or primary care provider to review. They reach out to the patient to tell them how and why their record was flagged, discuss any recommended treatment changes, and ask them to come in for a visit.
“It’s an opportunity to talk about their risk factors, which is designed to lead to a conversation about safety planning,” says clinical psychologist Matthew Miller, PhD, national director of the U.S. Department of Veterans Affairs’ Suicide Prevention Program. He’s not related to Dan Miller.
Making a suicide safety plan
A safety plan is a document that outlines how a person can help prevent their own suicide in a crisis.
The plan may include:
- A list of personal triggers or warning signs.
- What’s helped them in the past.
- Names of people or organizations who can support them.
- Plans to remove means of suicide, such as guns, from their environment.
- Their reasons for living.
In people at risk for suicide, research shows that having a safety plan reduces suicidal thoughts and attempts, lowers rates of depression and hopelessness, and boosts veterans’ engagement with the health care system. It may also help people manage things that trigger their suicidal thoughts.
Getting the call
What if REACH VET had been around when Dan Miller was in crisis – and he’d gotten a call from the VHA?
“It absolutely, positively would have helped because one of the biggest things on that day when I got served was feeling completely alone and that I had no one to turn to,” Mr. Miller says. He’s now a speaker for the Wounded Warrior Project, a nonprofit that serves veterans and active-duty service people.
Vets’ reactions to the unexpected VHA phone call, psychologist Dr. Miller says, “run the gamut from ‘Thank you for contacting me. Let’s talk,’ to ‘What are you talking about? Leave me alone!’ ”
Nothing stops all suicides. But REACH VET is having an impact. In a clinical trial, vets contacted through REACH VET had more doctor visits, were more likely to have a written suicide prevention safety plan, and had fewer hospital admissions for mental health, ER visits, and suicide attempts.
An assist from AI
Even simple outreach can make a big difference. And there’s research to prove it.
One study included 4,730 veterans recently discharged from psychiatric care at the VHA, a group considered at high risk for suicide.
Half of them got 13 caring emails from hospital staff in the weeks after leaving the hospital. The emails mentioned personal things the patient had shared, like a love of hiking, and wished them well. The other veterans got routine follow-up but no emails.
Two years later, those who got the caring emails were less likely to have died by suicide than the other vets. The study was published in 2014 in Contemporary Clinical Trials.
Researchers have done studies like this many times: with handwritten notes from the primary care doctor, postcards from the ER, and so forth. The results never vary: The notes reduce suicide risk.
“If we could use AI to identify people to receive notes or phone calls, it would be a very effective and inexpensive way to guide follow-up care,” says Rebecca Bernert, PhD, director and founder of the Suicide Prevention Research Laboratory at Stanford (Calif.) University.
AI doesn’t replace clinical judgment.
“AI can capture data that we miss due to the limits of our humanity,” psychologist Dr. Miller says. “There’s suicide prevention processes founded on big data and AI, and there are processes founded in clinical intuition and acumen.”
AI is only as good as the data it’s based on. If that data lacks diversity, it may miss things. And variables that apply to veterans may differ in civilians.
Stopping suicidal thoughts
Google is putting AI to work against suicide, too. Its MUM (Multitask Unified Model) technology seeks to understand the intent behind what we google.
MUM powers Google Search. It can often tell the difference between a search for information about suicide for someone writing a research paper on the topic and a search for information on how or where to carry out a suicide.
When Google Search detects that someone in the United States might be in crisis and at risk of suicide, the first search results that person gets are the number for the National Suicide Prevention Lifeline and other resources for people in crisis.
Google Home Assistant works in the same way. When a user makes a query that signals a suicide-related crisis, the gadget serves up resources that offer help.
MUM is working to understand the nuances of crisis language in 75 languages so that Google Search can provide people in crisis with hotlines or other resources in many countries.
“We want to find partners that are accessible to users in terms of hours of operation. We have a strong preference for finding partners that promise confidentiality and privacy to the extent that those are permitted [in that country],” says Anne Merritt, MD, a product manager at Google Search.
Other companies are working on apps that use AI to spot suicide risk in other ways, including voice technology that may notice subtle changes in the voice of someone who’s depressed and may be thinking of suicide. Those are still in development but show promise. Keep in mind that apps do not require government approval, so if you try one, be sure to let your health care provider know.
Changing the channel
Seeing a hotline number on your phone or computer screen can help, Dan Miller says. “If I happened to be online, searching maybe for a bridge to jump off of ... and suddenly that pops up on the screen, it’s like it changes the channel.”
It may not work for everyone, he says, but that search result could interrupt someone’s suicidal train of thought.
That’s crucial, psychologist Dr. Miller says, because most suicide attempts escalate from first thought to potentially fatal action in just 1 hour. That’s how fast it happened for Dan Miller in 2014.
“When you’re able to put time and space between the suicidal thought and the access to the method to act on that thought, you save lives,” Dr. Bernert says.
Making a different choice
An interruption in Mr. Miller’s thinking is what had saved his life.
Holding the gun to his head, Mr. Miller looked over at the passenger seat at a brochure from Wounded Warrior Project, which he had just learned about. Mr. Miller noticed a photo of a man in a wheelchair, a veteran like him, who had no legs. He thought that the man looked worse off than him but hadn’t given up.
Mr. Miller put down his gun and decided to get help.
Recovering from a near suicide attempt, he says, is a journey. It doesn’t happen overnight. Now, 8 years later, Mr. Miller is planning a brief break from the speaker circuit. He plans to spend 2 weeks in an outpatient counseling program for posttraumatic stress disorder and traumatic brain injury.
“Telling my story to strangers – part of it is healing me in a way, but I’m learning that repeating the story over and over again is also keeping me from letting it go. And I’m still healing.”
A version of this article first appeared on WebMD.com.
Alcohol’s detrimental impact on the brain explained?
Results of a large observational study suggest brain iron accumulation is a “plausible pathway” through which alcohol negatively affects cognition, study Anya Topiwala, MD, PhD, senior clinical researcher, Nuffield Department of Population Health, University of Oxford, England, said in an interview.
Study participants who drank 56 grams of alcohol a week had higher brain iron levels. The U.K. guideline for “low risk” alcohol consumption is less than 14 units weekly, or 112 grams.
“We are finding harmful associations with iron within those low-risk alcohol intake guidelines,” said Dr. Topiwala.
The study was published online in PLOS Medicine.
Early intervention opportunity?
Previous research suggests higher brain iron may be involved in the pathophysiology of Alzheimer’s and Parkinson’s diseases. However, it’s unclear whether deposition plays a role in alcohol’s effect on the brain and if it does, whether this could present an opportunity for early intervention with, for example, chelating agents.
The study included 20,729 participants in the UK Biobank study, which recruited volunteers from 2006 to 2010. Participants had a mean age of 54.8 years, and 48.6% were female.
Participants self-identified as current, never, or previous alcohol consumers. For current drinkers, researchers calculated the total weekly number of U.K. units of alcohol consumed. One unit is 8 grams. A standard drink in the United States is 14 grams. They categorized weekly consumption into quintiles and used the lowest quintile as the reference category.
Participants underwent MRI to determine brain iron levels. Areas of interest were deep brain structures in the basal ganglia.
Mean weekly alcohol consumption was 17.7 units, which is higher than U.K. guidelines for low-risk consumption. “Half of the sample were drinking above what is recommended,” said Dr. Topiwala.
Alcohol consumption was associated with markers of higher iron in the bilateral putamen (beta, 0.08 standard deviation; 95% confidence interval, 0.06-0.09; P < .001), caudate (beta, 0.05; 95% CI, 0.04-0.07; P < .001), and substantia nigra (beta, 0.03; 95% CI; 0.02-0.05; P < .001).
Poorer performance
Drinking more than 7 units (56 grams) weekly was associated with higher susceptibility for all brain regions, except the thalamus.
Controlling for menopause status did not alter associations between alcohol and susceptibility for any brain region. This was also the case when excluding blood pressure and cholesterol as covariates.
There were significant interactions with age in the bilateral putamen and caudate but not with sex, smoking, or Townsend Deprivation Index, which includes such factors as unemployment and living conditions.
To gather data on liver iron levels, participants underwent abdominal imaging at the same time as brain imaging. Dr. Topiwala explained that the liver is a primary storage center for iron, so it was used as “a kind of surrogate marker” of iron in the body.
The researchers showed an indirect effect of alcohol through systemic iron. A 1 SD increase in weekly alcohol consumption was associated with a 0.05 mg/g (95% CI, 0.02-0.07; P < .001) increase in liver iron. In addition, a 1 mg/g increase in liver iron was associated with a 0.44 (95% CI, 0.35-0.52; P < .001) SD increase in left putamen susceptibility.
In this sample, 32% (95% CI, 22-49; P < .001) of alcohol’s total effect on left putamen susceptibility was mediated via higher systemic iron levels.
To minimize the impact of other factors influencing the association between alcohol consumption and brain iron – and the possibility that people with more brain iron drink more – researchers used Mendelian randomization that considers genetically predicted alcohol intake. This analysis supported findings of associations between alcohol consumption and brain iron.
Participants completed a cognitive battery, which included trail-making tests that reflect executive function, puzzle tests that assess fluid intelligence or logic and reasoning, and task-based tests using the “Snap” card game to measure reaction time.
Investigators found the more iron that was present in certain brain regions, the poorer participants’ cognitive performance.
Patients should know about the risks of moderate alcohol intake so they can make decisions about drinking, said Dr. Topiwala. “They should be aware that 14 units of alcohol per week is not a zero risk.”
Novel research
Commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, noted the study’s large size as a strength of the research.
She noted previous research has shown an association between higher iron levels and alcohol dependence and worse cognitive function, but the potential connection of brain iron levels, moderate alcohol consumption, and cognition has not been studied to date.
“This paper aims to look at whether there is a potential biological link between moderate alcohol consumption and cognition through iron-related pathways.”
The authors suggest more work is needed to understand whether alcohol consumption impacts iron-related biologies to affect downstream cognition, said Dr. Snyder. “Although this study does not answer that question, it does highlight some important questions.”
Study authors received funding from Wellcome Trust, UK Medical Research Council, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, BHF Centre of Research Excellence, British Heart Foundation, NIHR Cambridge Biomedical Research Centre, U.S. Department of Veterans Affairs, China Scholarship Council, and Li Ka Shing Centre for Health Information and Discovery. Dr. Topiwala has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large observational study suggest brain iron accumulation is a “plausible pathway” through which alcohol negatively affects cognition, study Anya Topiwala, MD, PhD, senior clinical researcher, Nuffield Department of Population Health, University of Oxford, England, said in an interview.
Study participants who drank 56 grams of alcohol a week had higher brain iron levels. The U.K. guideline for “low risk” alcohol consumption is less than 14 units weekly, or 112 grams.
“We are finding harmful associations with iron within those low-risk alcohol intake guidelines,” said Dr. Topiwala.
The study was published online in PLOS Medicine.
Early intervention opportunity?
Previous research suggests higher brain iron may be involved in the pathophysiology of Alzheimer’s and Parkinson’s diseases. However, it’s unclear whether deposition plays a role in alcohol’s effect on the brain and if it does, whether this could present an opportunity for early intervention with, for example, chelating agents.
The study included 20,729 participants in the UK Biobank study, which recruited volunteers from 2006 to 2010. Participants had a mean age of 54.8 years, and 48.6% were female.
Participants self-identified as current, never, or previous alcohol consumers. For current drinkers, researchers calculated the total weekly number of U.K. units of alcohol consumed. One unit is 8 grams. A standard drink in the United States is 14 grams. They categorized weekly consumption into quintiles and used the lowest quintile as the reference category.
Participants underwent MRI to determine brain iron levels. Areas of interest were deep brain structures in the basal ganglia.
Mean weekly alcohol consumption was 17.7 units, which is higher than U.K. guidelines for low-risk consumption. “Half of the sample were drinking above what is recommended,” said Dr. Topiwala.
Alcohol consumption was associated with markers of higher iron in the bilateral putamen (beta, 0.08 standard deviation; 95% confidence interval, 0.06-0.09; P < .001), caudate (beta, 0.05; 95% CI, 0.04-0.07; P < .001), and substantia nigra (beta, 0.03; 95% CI; 0.02-0.05; P < .001).
Poorer performance
Drinking more than 7 units (56 grams) weekly was associated with higher susceptibility for all brain regions, except the thalamus.
Controlling for menopause status did not alter associations between alcohol and susceptibility for any brain region. This was also the case when excluding blood pressure and cholesterol as covariates.
There were significant interactions with age in the bilateral putamen and caudate but not with sex, smoking, or Townsend Deprivation Index, which includes such factors as unemployment and living conditions.
To gather data on liver iron levels, participants underwent abdominal imaging at the same time as brain imaging. Dr. Topiwala explained that the liver is a primary storage center for iron, so it was used as “a kind of surrogate marker” of iron in the body.
The researchers showed an indirect effect of alcohol through systemic iron. A 1 SD increase in weekly alcohol consumption was associated with a 0.05 mg/g (95% CI, 0.02-0.07; P < .001) increase in liver iron. In addition, a 1 mg/g increase in liver iron was associated with a 0.44 (95% CI, 0.35-0.52; P < .001) SD increase in left putamen susceptibility.
In this sample, 32% (95% CI, 22-49; P < .001) of alcohol’s total effect on left putamen susceptibility was mediated via higher systemic iron levels.
To minimize the impact of other factors influencing the association between alcohol consumption and brain iron – and the possibility that people with more brain iron drink more – researchers used Mendelian randomization that considers genetically predicted alcohol intake. This analysis supported findings of associations between alcohol consumption and brain iron.
Participants completed a cognitive battery, which included trail-making tests that reflect executive function, puzzle tests that assess fluid intelligence or logic and reasoning, and task-based tests using the “Snap” card game to measure reaction time.
Investigators found the more iron that was present in certain brain regions, the poorer participants’ cognitive performance.
Patients should know about the risks of moderate alcohol intake so they can make decisions about drinking, said Dr. Topiwala. “They should be aware that 14 units of alcohol per week is not a zero risk.”
Novel research
Commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, noted the study’s large size as a strength of the research.
She noted previous research has shown an association between higher iron levels and alcohol dependence and worse cognitive function, but the potential connection of brain iron levels, moderate alcohol consumption, and cognition has not been studied to date.
“This paper aims to look at whether there is a potential biological link between moderate alcohol consumption and cognition through iron-related pathways.”
The authors suggest more work is needed to understand whether alcohol consumption impacts iron-related biologies to affect downstream cognition, said Dr. Snyder. “Although this study does not answer that question, it does highlight some important questions.”
Study authors received funding from Wellcome Trust, UK Medical Research Council, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, BHF Centre of Research Excellence, British Heart Foundation, NIHR Cambridge Biomedical Research Centre, U.S. Department of Veterans Affairs, China Scholarship Council, and Li Ka Shing Centre for Health Information and Discovery. Dr. Topiwala has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large observational study suggest brain iron accumulation is a “plausible pathway” through which alcohol negatively affects cognition, study Anya Topiwala, MD, PhD, senior clinical researcher, Nuffield Department of Population Health, University of Oxford, England, said in an interview.
Study participants who drank 56 grams of alcohol a week had higher brain iron levels. The U.K. guideline for “low risk” alcohol consumption is less than 14 units weekly, or 112 grams.
“We are finding harmful associations with iron within those low-risk alcohol intake guidelines,” said Dr. Topiwala.
The study was published online in PLOS Medicine.
Early intervention opportunity?
Previous research suggests higher brain iron may be involved in the pathophysiology of Alzheimer’s and Parkinson’s diseases. However, it’s unclear whether deposition plays a role in alcohol’s effect on the brain and if it does, whether this could present an opportunity for early intervention with, for example, chelating agents.
The study included 20,729 participants in the UK Biobank study, which recruited volunteers from 2006 to 2010. Participants had a mean age of 54.8 years, and 48.6% were female.
Participants self-identified as current, never, or previous alcohol consumers. For current drinkers, researchers calculated the total weekly number of U.K. units of alcohol consumed. One unit is 8 grams. A standard drink in the United States is 14 grams. They categorized weekly consumption into quintiles and used the lowest quintile as the reference category.
Participants underwent MRI to determine brain iron levels. Areas of interest were deep brain structures in the basal ganglia.
Mean weekly alcohol consumption was 17.7 units, which is higher than U.K. guidelines for low-risk consumption. “Half of the sample were drinking above what is recommended,” said Dr. Topiwala.
Alcohol consumption was associated with markers of higher iron in the bilateral putamen (beta, 0.08 standard deviation; 95% confidence interval, 0.06-0.09; P < .001), caudate (beta, 0.05; 95% CI, 0.04-0.07; P < .001), and substantia nigra (beta, 0.03; 95% CI; 0.02-0.05; P < .001).
Poorer performance
Drinking more than 7 units (56 grams) weekly was associated with higher susceptibility for all brain regions, except the thalamus.
Controlling for menopause status did not alter associations between alcohol and susceptibility for any brain region. This was also the case when excluding blood pressure and cholesterol as covariates.
There were significant interactions with age in the bilateral putamen and caudate but not with sex, smoking, or Townsend Deprivation Index, which includes such factors as unemployment and living conditions.
To gather data on liver iron levels, participants underwent abdominal imaging at the same time as brain imaging. Dr. Topiwala explained that the liver is a primary storage center for iron, so it was used as “a kind of surrogate marker” of iron in the body.
The researchers showed an indirect effect of alcohol through systemic iron. A 1 SD increase in weekly alcohol consumption was associated with a 0.05 mg/g (95% CI, 0.02-0.07; P < .001) increase in liver iron. In addition, a 1 mg/g increase in liver iron was associated with a 0.44 (95% CI, 0.35-0.52; P < .001) SD increase in left putamen susceptibility.
In this sample, 32% (95% CI, 22-49; P < .001) of alcohol’s total effect on left putamen susceptibility was mediated via higher systemic iron levels.
To minimize the impact of other factors influencing the association between alcohol consumption and brain iron – and the possibility that people with more brain iron drink more – researchers used Mendelian randomization that considers genetically predicted alcohol intake. This analysis supported findings of associations between alcohol consumption and brain iron.
Participants completed a cognitive battery, which included trail-making tests that reflect executive function, puzzle tests that assess fluid intelligence or logic and reasoning, and task-based tests using the “Snap” card game to measure reaction time.
Investigators found the more iron that was present in certain brain regions, the poorer participants’ cognitive performance.
Patients should know about the risks of moderate alcohol intake so they can make decisions about drinking, said Dr. Topiwala. “They should be aware that 14 units of alcohol per week is not a zero risk.”
Novel research
Commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations, Alzheimer’s Association, noted the study’s large size as a strength of the research.
She noted previous research has shown an association between higher iron levels and alcohol dependence and worse cognitive function, but the potential connection of brain iron levels, moderate alcohol consumption, and cognition has not been studied to date.
“This paper aims to look at whether there is a potential biological link between moderate alcohol consumption and cognition through iron-related pathways.”
The authors suggest more work is needed to understand whether alcohol consumption impacts iron-related biologies to affect downstream cognition, said Dr. Snyder. “Although this study does not answer that question, it does highlight some important questions.”
Study authors received funding from Wellcome Trust, UK Medical Research Council, National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, BHF Centre of Research Excellence, British Heart Foundation, NIHR Cambridge Biomedical Research Centre, U.S. Department of Veterans Affairs, China Scholarship Council, and Li Ka Shing Centre for Health Information and Discovery. Dr. Topiwala has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE
Best meds for insomnia identified?
In a comprehensive comparative-effectiveness analysis, lemborexant and eszopiclone showed the best efficacy, acceptability, and tolerability for acute and long-term insomnia treatment.
However, eszopiclone may cause substantial side effects – and safety data on lemborexant were inconclusive, the researchers note.
Not surprisingly, short-acting, intermediate-acting, and long-acting benzodiazepines were effective in the acute treatment of insomnia, but they have unfavorable tolerability and safety profiles, and there are no long-term data on these issues.
For many insomnia medications, there is a “striking” and “appalling” lack of long-term data, study investigator Andrea Cipriani, MD, PhD, professor of psychiatry, University of Oxford, United Kingdom, noted during a press briefing.
“This is a call for regulators to raise the bar and ask for long-term data when companies submit an application for licensing insomnia drugs,” Dr. Cipriani said.
The findings were published online in The Lancet.
Prevalent, debilitating
Insomnia is highly prevalent, affecting up to 1 in 5 adults, and can have a profound impact on health, well-being, and productivity.
Sleep hygiene and cognitive-behavioral therapy for insomnia (CBT-I) are recommended first-line treatments, but they are often unavailable, which often leads patients and clinicians to turn to medications.
However, “insomnia drugs are not all created equal. Even within the same drug class there are differences,” Dr. Cipriani said.
In a large-scale systematic review and network meta-analysis, the researchers analyzed data from 154 double-blind, randomized controlled trials of medications (licensed or not) used for acute and long-term treatment of insomnia in 44,089 adults (mean age, 51.7 years; 63% women).
Results showed, for the acute treatment of insomnia, benzodiazepines, doxylamine, eszopiclone, lemborexant, seltorexant, zolpidem, and zopiclone were more effective than placebo (standardized mean difference range, 0.36-0.83; high-to-moderate certainty of evidence).
In addition, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more effective than melatonin, ramelteon, and zaleplon (SMD, 0.27-0.71; moderate-to-very low certainty of evidence).
“Our results show that the melatonergic drugs melatonin and ramelteon are not really effective. The data do not support the regular use of these drugs,” co-investigator Phil Cowen, PhD, professor of psychopharmacology, University of Oxford, said at the briefing.
Best available evidence
What little long-term data is available suggest eszopiclone and lemborexant are more effective than placebo. Plus, eszopiclone is more effective than ramelteon and zolpidem but with “very low” certainty of evidence, the researchers report.
“There was insufficient evidence to support the prescription of benzodiazepines and zolpidem in long-term treatment,” they write.
Another problem was lack of data on other important outcomes, they add.
“We wanted to look at hangover effects, daytime sleepiness, [and] rebound effect, but often there was no data reported in trials. We need to collect data about these outcomes because they matter to clinicians and patients,” Dr. Cipriani said.
Summing up, the researchers note the current findings represent the “best available evidence base to guide the choice about pharmacological treatment for insomnia disorder in adults and will assist in shared decisionmaking between patients, carers, and their clinicians, as well as policy makers.”
They caution, however, that all statements comparing the merits of one drug with another “should be tempered by the potential limitations of the current analysis, the quality of the available evidence, the characteristics of the patient populations, and the uncertainties that might result from choice of dose or treatment setting.”
In addition, it is important to also consider nonpharmacologic treatments for insomnia disorder, as they are supported by “high-quality evidence and recommended as first-line treatment by guidelines,” the investigator write.
Shared decisionmaking
In an accompanying editorial, Myrto Samara, MD, University of Thessaly, Larissa, Greece, agrees with the researchers that discussion with patients is key.
“For insomnia treatment, patient-physician shared decisionmaking is crucial to decide when a pharmacological intervention is deemed necessary and which drug [is] to be given by considering the trade-offs for efficacy and side effects,” Dr. Samara writes.
The study was funded by the UK National Institute for Health Research (NIHR) Oxford Health Biomedical Research Center. Dr. Cipriani has received research and consultancy fees from the Italian Network for Pediatric Trials, CARIPLO Foundation, and Angelini Pharma, and is the chief and principal investigator of two trials of seltorexant in depression that are sponsored by Janssen. Dr. Samara has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a comprehensive comparative-effectiveness analysis, lemborexant and eszopiclone showed the best efficacy, acceptability, and tolerability for acute and long-term insomnia treatment.
However, eszopiclone may cause substantial side effects – and safety data on lemborexant were inconclusive, the researchers note.
Not surprisingly, short-acting, intermediate-acting, and long-acting benzodiazepines were effective in the acute treatment of insomnia, but they have unfavorable tolerability and safety profiles, and there are no long-term data on these issues.
For many insomnia medications, there is a “striking” and “appalling” lack of long-term data, study investigator Andrea Cipriani, MD, PhD, professor of psychiatry, University of Oxford, United Kingdom, noted during a press briefing.
“This is a call for regulators to raise the bar and ask for long-term data when companies submit an application for licensing insomnia drugs,” Dr. Cipriani said.
The findings were published online in The Lancet.
Prevalent, debilitating
Insomnia is highly prevalent, affecting up to 1 in 5 adults, and can have a profound impact on health, well-being, and productivity.
Sleep hygiene and cognitive-behavioral therapy for insomnia (CBT-I) are recommended first-line treatments, but they are often unavailable, which often leads patients and clinicians to turn to medications.
However, “insomnia drugs are not all created equal. Even within the same drug class there are differences,” Dr. Cipriani said.
In a large-scale systematic review and network meta-analysis, the researchers analyzed data from 154 double-blind, randomized controlled trials of medications (licensed or not) used for acute and long-term treatment of insomnia in 44,089 adults (mean age, 51.7 years; 63% women).
Results showed, for the acute treatment of insomnia, benzodiazepines, doxylamine, eszopiclone, lemborexant, seltorexant, zolpidem, and zopiclone were more effective than placebo (standardized mean difference range, 0.36-0.83; high-to-moderate certainty of evidence).
In addition, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more effective than melatonin, ramelteon, and zaleplon (SMD, 0.27-0.71; moderate-to-very low certainty of evidence).
“Our results show that the melatonergic drugs melatonin and ramelteon are not really effective. The data do not support the regular use of these drugs,” co-investigator Phil Cowen, PhD, professor of psychopharmacology, University of Oxford, said at the briefing.
Best available evidence
What little long-term data is available suggest eszopiclone and lemborexant are more effective than placebo. Plus, eszopiclone is more effective than ramelteon and zolpidem but with “very low” certainty of evidence, the researchers report.
“There was insufficient evidence to support the prescription of benzodiazepines and zolpidem in long-term treatment,” they write.
Another problem was lack of data on other important outcomes, they add.
“We wanted to look at hangover effects, daytime sleepiness, [and] rebound effect, but often there was no data reported in trials. We need to collect data about these outcomes because they matter to clinicians and patients,” Dr. Cipriani said.
Summing up, the researchers note the current findings represent the “best available evidence base to guide the choice about pharmacological treatment for insomnia disorder in adults and will assist in shared decisionmaking between patients, carers, and their clinicians, as well as policy makers.”
They caution, however, that all statements comparing the merits of one drug with another “should be tempered by the potential limitations of the current analysis, the quality of the available evidence, the characteristics of the patient populations, and the uncertainties that might result from choice of dose or treatment setting.”
In addition, it is important to also consider nonpharmacologic treatments for insomnia disorder, as they are supported by “high-quality evidence and recommended as first-line treatment by guidelines,” the investigator write.
Shared decisionmaking
In an accompanying editorial, Myrto Samara, MD, University of Thessaly, Larissa, Greece, agrees with the researchers that discussion with patients is key.
“For insomnia treatment, patient-physician shared decisionmaking is crucial to decide when a pharmacological intervention is deemed necessary and which drug [is] to be given by considering the trade-offs for efficacy and side effects,” Dr. Samara writes.
The study was funded by the UK National Institute for Health Research (NIHR) Oxford Health Biomedical Research Center. Dr. Cipriani has received research and consultancy fees from the Italian Network for Pediatric Trials, CARIPLO Foundation, and Angelini Pharma, and is the chief and principal investigator of two trials of seltorexant in depression that are sponsored by Janssen. Dr. Samara has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a comprehensive comparative-effectiveness analysis, lemborexant and eszopiclone showed the best efficacy, acceptability, and tolerability for acute and long-term insomnia treatment.
However, eszopiclone may cause substantial side effects – and safety data on lemborexant were inconclusive, the researchers note.
Not surprisingly, short-acting, intermediate-acting, and long-acting benzodiazepines were effective in the acute treatment of insomnia, but they have unfavorable tolerability and safety profiles, and there are no long-term data on these issues.
For many insomnia medications, there is a “striking” and “appalling” lack of long-term data, study investigator Andrea Cipriani, MD, PhD, professor of psychiatry, University of Oxford, United Kingdom, noted during a press briefing.
“This is a call for regulators to raise the bar and ask for long-term data when companies submit an application for licensing insomnia drugs,” Dr. Cipriani said.
The findings were published online in The Lancet.
Prevalent, debilitating
Insomnia is highly prevalent, affecting up to 1 in 5 adults, and can have a profound impact on health, well-being, and productivity.
Sleep hygiene and cognitive-behavioral therapy for insomnia (CBT-I) are recommended first-line treatments, but they are often unavailable, which often leads patients and clinicians to turn to medications.
However, “insomnia drugs are not all created equal. Even within the same drug class there are differences,” Dr. Cipriani said.
In a large-scale systematic review and network meta-analysis, the researchers analyzed data from 154 double-blind, randomized controlled trials of medications (licensed or not) used for acute and long-term treatment of insomnia in 44,089 adults (mean age, 51.7 years; 63% women).
Results showed, for the acute treatment of insomnia, benzodiazepines, doxylamine, eszopiclone, lemborexant, seltorexant, zolpidem, and zopiclone were more effective than placebo (standardized mean difference range, 0.36-0.83; high-to-moderate certainty of evidence).
In addition, benzodiazepines, eszopiclone, zolpidem, and zopiclone were more effective than melatonin, ramelteon, and zaleplon (SMD, 0.27-0.71; moderate-to-very low certainty of evidence).
“Our results show that the melatonergic drugs melatonin and ramelteon are not really effective. The data do not support the regular use of these drugs,” co-investigator Phil Cowen, PhD, professor of psychopharmacology, University of Oxford, said at the briefing.
Best available evidence
What little long-term data is available suggest eszopiclone and lemborexant are more effective than placebo. Plus, eszopiclone is more effective than ramelteon and zolpidem but with “very low” certainty of evidence, the researchers report.
“There was insufficient evidence to support the prescription of benzodiazepines and zolpidem in long-term treatment,” they write.
Another problem was lack of data on other important outcomes, they add.
“We wanted to look at hangover effects, daytime sleepiness, [and] rebound effect, but often there was no data reported in trials. We need to collect data about these outcomes because they matter to clinicians and patients,” Dr. Cipriani said.
Summing up, the researchers note the current findings represent the “best available evidence base to guide the choice about pharmacological treatment for insomnia disorder in adults and will assist in shared decisionmaking between patients, carers, and their clinicians, as well as policy makers.”
They caution, however, that all statements comparing the merits of one drug with another “should be tempered by the potential limitations of the current analysis, the quality of the available evidence, the characteristics of the patient populations, and the uncertainties that might result from choice of dose or treatment setting.”
In addition, it is important to also consider nonpharmacologic treatments for insomnia disorder, as they are supported by “high-quality evidence and recommended as first-line treatment by guidelines,” the investigator write.
Shared decisionmaking
In an accompanying editorial, Myrto Samara, MD, University of Thessaly, Larissa, Greece, agrees with the researchers that discussion with patients is key.
“For insomnia treatment, patient-physician shared decisionmaking is crucial to decide when a pharmacological intervention is deemed necessary and which drug [is] to be given by considering the trade-offs for efficacy and side effects,” Dr. Samara writes.
The study was funded by the UK National Institute for Health Research (NIHR) Oxford Health Biomedical Research Center. Dr. Cipriani has received research and consultancy fees from the Italian Network for Pediatric Trials, CARIPLO Foundation, and Angelini Pharma, and is the chief and principal investigator of two trials of seltorexant in depression that are sponsored by Janssen. Dr. Samara has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Violent patient throws scalding oil on MD; other patient dangers
Ralph Newman, MD, got a taste of how dangerous medicine could be at age 10, when he witnessed a physician being shot by a patient.
“I was visiting a friend whose father was a psychiatrist,” Dr. Newman recalled. “We were playing in the living room when the doorbell rang. My friend went to the door and opened it. Then I heard a shot. I ran to the front hall and saw my friend’s father slumped at the bottom of the stairs. He had come down the stairs to see who was there. It was a patient armed with a shotgun.”
As a result of the shooting, a large portion of the psychiatrist’s intestines was removed. In spite of this traumatic incident, Dr. Newman went on to become a psychiatrist – who treated many violent prisoners. “I knew it was dangerous,” he said, “but I rationalized that I wouldn’t be attacked because I would be nicer.”
That attitude seemed to work until 2002, when a prisoner threw boiling oil on him. Dr. Newman was working at the Federal Medical Center Butner, a facility for prisoners in North Carolina. “A prisoner I had been treating was denied parole, based on my recommendation,” he said. “From then on, he was looking for a way to exact revenge.”
“One day I was sitting in the nursing station, typing up notes,” Dr. Newman said. “Two new nurses, who were also there, had forgotten to lock the door, and the prisoner noticed that. He heated up some baby oil in a microwave, which was available to prisoners at the time. Then he walked into the office, threw the oil on my back, and came at me with a sharp pencil.”
Dr. Newman said the nurses fled to an adjoining office, locked the door, and wouldn’t let him in. He went into another office and collapsed in exhaustion. He was saved by an inmate who came on the scene, fended off the attacker, and called for help.
“I was taken to the burn unit,” Dr. Newman recalled. “I had second- and third-degree burns on 9% of my body. It was extremely painful. It took me 45 days to recover enough to get back to work.” The two nurses were fired.
Doctors take threats by patients more seriously now
When orthopedic surgeon Preston Phillips, MD, was killed by a patient in Tulsa, Okla., on June 1, Jennifer M. Weiss, MD, recognized the potential danger to physicians.
“The news left me feeling very shaken,” said Dr. Weiss, a pediatric orthopedic surgeon at Southern California Permanente Medical Group, Los Angeles. “Every orthopedic surgeon I talked to about it felt shaken.”
Dr. Weiss said the impact of that event prompted her to take a patient’s abuse more seriously than she might have previously. “Before the killing, my colleagues and I might have swept the incident under the rug, but we reported it to the authorities,” she said.
“What happened was I told a parent of a school-aged child that the child wasn’t ready to go back to sports,” Dr. Weiss says. “This parent was incredibly triggered – screaming and making verbal threats. The parent was standing between me and the door, so I couldn’t get out.”
Coworkers down the hall heard the yelling and helped Dr. Weiss get out of the room. “The parent was escorted out of the building, and the incident was reported to our risk management team,” she said.
Shooters/killers vs. agitated patients
Patients who shoot to kill are very different from agitated patients seen by many doctors on a regular basis – particularly in emergency departments (EDs), psychiatric units, and pain clinics, said Scott Zeller, MD, a psychiatrist who is vice president of Acute Psychiatric Medicine at Vituity, a multistate physician partnership based in Emeryville, California.
“Agitated patients have trouble communicating their needs and can become physically and verbally aggressive,” Dr. Zeller said. He reports that there are 1.7 million such incidents a year in this country, but most of the incidents of verbal aggression can be kept from exploding into physical violence.
Shooters, however, are very hard to stop because they usually plan the action in advance, Dr. Zeller said. He recalled the 2017 murder of Todd Graham, MD, a friend from medical school. Dr. Graham, an orthopedic surgeon in South Bend, Ind., was gunned down by the husband of one of his patients after Dr. Graham declined to prescribe opioids for her.
Playing down the risk of violence
Doctors may play down the risk of violence, even after they have experienced it personally. “Patients can get angry and may make threatening comments,” Dr. Weiss said. “A lot of doctors just brush it off.”
Simple remarks can set off violence-prone patients, as happened to James P. Phillips, MD, director of disaster and operational medicine at George Washington University, Washington. He recalled asking a prisoner who was visiting his hospital to “lower the volume,” and the man exploded. “Even though he was handcuffed to the bed, he heaved an oxygen tank into a window,” Dr. Phillips said. “He said he would be coming back to kill me.”
Sometimes threats or other types of verbal abuse can be as destructive as physical violence. Diann Krywko, MD, an emergency physician at the Medical University of South Carolina (MUSC) Health, Charleston, has had some tough assignments. She worked in EDs in Detroit and Flint, Mich., for a decade before coming to MUSC, where she serves as director of wellness, health, and resilience. One of the incidents that has bothered her the most involved a threat.
It happened when Dr. Krywko denied a patient’s request for narcotics. “She was very angry and said she’d come to my home and cut my children’s heads off,” Dr. Krywko said. “To this day, what she said horrifies me. I still see her smile as she said that.”
Dr. Krywko considered filing for a restraining order against the patient but didn’t because the patient could have learned her address. Dr. Phillips said fear of retaliation is one reason many doctors don’t report threats from patients. “The patient you report knows where you work and may come there to take revenge,” he said. “Also, you may have to continue caring for the person who punched you.”
Online threats also may cause a great deal of angst. Dr. Phillips said he received many online threats when was a medical analyst for CNN in 2020. “Someone sent my address to his Twitter followers, and they shared it with others, so now the whole world knows where I live,” he said. “I had to upgrade security at my home.”
How to deal with volatile patients
Being nice may not always work, but in many cases, it can keep a volatile situation from exploding, according to Dr. Krywko.
“When patients begin to show signs of agitation or are already there, we always try to verbally deescalate the situation, which involves listening,” Dr. Krywko said. “They want someone to hear them out.”
Doctors speak to patients from a position of authority, but Dr. Krywko advises that they should not be too blunt. “Don’t tell patients they’re wrong,” she said. “Even if they may be incorrect, they feel their viewpoint is valid. Encourage a dialogue with words like, ‘Tell me more,’ ” Dr. Krywko said.
Defending yourself
Doctors may have little warning of an impending attack because a patient’s mood can change quickly. This happened several years ago to Jennifer Casaletto, MD, an emergency physician in Charlotte, N.C.
“A man was brought into my ED by ambulance,” she said. “He seemed very calm for a long while, but then he became completely unhinged. A male nurse placed himself between the patient and others and was attacked. He got hurt but was able to continue working.”
Dr. Zeller said health care teams sometimes overreact when patients lash out. “The old-fashioned way to deal with an agitated patient is to call in the cavalry – everyone does a group takedown,” he said. “The patient is put in restraints and heavily sedated. This is not good for anybody. Not only is it likely to injure and traumatize the patient, it can also injure the care team.”
Many hospital EDs have security guards. “I feel safer when a hospital has armed security guards, but they need to be well trained,” Dr. Casaletto said. “Many small hospitals and freestanding EDs do not have security officers at all, or the guards are undertrained or told not to touch anybody.”
In many electronic health record systems, doctors can flag violent patients so future caregivers can be forewarned. However, Dr. Zeller advises against writing about patients’ violence or rudeness in the medical record, because patients can have access to it and might take revenge.
Rising violence from patients
“It feels like it has become much more dangerous to work in the ED,” said Hasan Gokal, MD, an emergency physician working in EDs at the Texas Medical Center. “Just last week, a woman pulled out a gun and fired it in an ED near Houston.”
The statistics back up Dr. Gokal’s assessment. Injuries caused by violent attacks against medical professionals grew by 67% from 2011 to 2018, according to the U.S. Bureau of Labor Statistics. Those levels rose even more during the COVID-19 pandemic – the assault rate in hospitals rose 23% just in 2020.
Dr. Krywko said she had “a patient who said she wanted to hurt the next person who irritated her, and that happened to me. She jumped out of her bed swinging and punching, and I wasn’t ready for it. I yelled for help and the care team came.”
“The rise in violence has to do with a decline in respect for authority,” Dr. Phillips said. “Some people now believe doctors are lying to them about the need for COVID precautions because they are taking money from the vaccine companies. The pandemic has exacerbated violence in every way.”
Dr. Phillips said that a growing lack of resources had led to more anger among patients. “There are fewer nurses and reduced physician coverage,” he said. “That means longer wait times for patients, which increases patients’ frustrations.”
Dr. Weiss said patients have higher expectations. “In sports medicine, the expectations are incredible,” she said. “Parents want their kids to get back to playing as soon as possible.”
“Hospitals in particular are soft targets for violence,” Dr. Phillips said. “People know you can’t assault a flight attendant, because it’s a federal offense, but there is no such federal offense for violence against health care personnel.”
A version of this article first appeared on Medscape.com.
Ralph Newman, MD, got a taste of how dangerous medicine could be at age 10, when he witnessed a physician being shot by a patient.
“I was visiting a friend whose father was a psychiatrist,” Dr. Newman recalled. “We were playing in the living room when the doorbell rang. My friend went to the door and opened it. Then I heard a shot. I ran to the front hall and saw my friend’s father slumped at the bottom of the stairs. He had come down the stairs to see who was there. It was a patient armed with a shotgun.”
As a result of the shooting, a large portion of the psychiatrist’s intestines was removed. In spite of this traumatic incident, Dr. Newman went on to become a psychiatrist – who treated many violent prisoners. “I knew it was dangerous,” he said, “but I rationalized that I wouldn’t be attacked because I would be nicer.”
That attitude seemed to work until 2002, when a prisoner threw boiling oil on him. Dr. Newman was working at the Federal Medical Center Butner, a facility for prisoners in North Carolina. “A prisoner I had been treating was denied parole, based on my recommendation,” he said. “From then on, he was looking for a way to exact revenge.”
“One day I was sitting in the nursing station, typing up notes,” Dr. Newman said. “Two new nurses, who were also there, had forgotten to lock the door, and the prisoner noticed that. He heated up some baby oil in a microwave, which was available to prisoners at the time. Then he walked into the office, threw the oil on my back, and came at me with a sharp pencil.”
Dr. Newman said the nurses fled to an adjoining office, locked the door, and wouldn’t let him in. He went into another office and collapsed in exhaustion. He was saved by an inmate who came on the scene, fended off the attacker, and called for help.
“I was taken to the burn unit,” Dr. Newman recalled. “I had second- and third-degree burns on 9% of my body. It was extremely painful. It took me 45 days to recover enough to get back to work.” The two nurses were fired.
Doctors take threats by patients more seriously now
When orthopedic surgeon Preston Phillips, MD, was killed by a patient in Tulsa, Okla., on June 1, Jennifer M. Weiss, MD, recognized the potential danger to physicians.
“The news left me feeling very shaken,” said Dr. Weiss, a pediatric orthopedic surgeon at Southern California Permanente Medical Group, Los Angeles. “Every orthopedic surgeon I talked to about it felt shaken.”
Dr. Weiss said the impact of that event prompted her to take a patient’s abuse more seriously than she might have previously. “Before the killing, my colleagues and I might have swept the incident under the rug, but we reported it to the authorities,” she said.
“What happened was I told a parent of a school-aged child that the child wasn’t ready to go back to sports,” Dr. Weiss says. “This parent was incredibly triggered – screaming and making verbal threats. The parent was standing between me and the door, so I couldn’t get out.”
Coworkers down the hall heard the yelling and helped Dr. Weiss get out of the room. “The parent was escorted out of the building, and the incident was reported to our risk management team,” she said.
Shooters/killers vs. agitated patients
Patients who shoot to kill are very different from agitated patients seen by many doctors on a regular basis – particularly in emergency departments (EDs), psychiatric units, and pain clinics, said Scott Zeller, MD, a psychiatrist who is vice president of Acute Psychiatric Medicine at Vituity, a multistate physician partnership based in Emeryville, California.
“Agitated patients have trouble communicating their needs and can become physically and verbally aggressive,” Dr. Zeller said. He reports that there are 1.7 million such incidents a year in this country, but most of the incidents of verbal aggression can be kept from exploding into physical violence.
Shooters, however, are very hard to stop because they usually plan the action in advance, Dr. Zeller said. He recalled the 2017 murder of Todd Graham, MD, a friend from medical school. Dr. Graham, an orthopedic surgeon in South Bend, Ind., was gunned down by the husband of one of his patients after Dr. Graham declined to prescribe opioids for her.
Playing down the risk of violence
Doctors may play down the risk of violence, even after they have experienced it personally. “Patients can get angry and may make threatening comments,” Dr. Weiss said. “A lot of doctors just brush it off.”
Simple remarks can set off violence-prone patients, as happened to James P. Phillips, MD, director of disaster and operational medicine at George Washington University, Washington. He recalled asking a prisoner who was visiting his hospital to “lower the volume,” and the man exploded. “Even though he was handcuffed to the bed, he heaved an oxygen tank into a window,” Dr. Phillips said. “He said he would be coming back to kill me.”
Sometimes threats or other types of verbal abuse can be as destructive as physical violence. Diann Krywko, MD, an emergency physician at the Medical University of South Carolina (MUSC) Health, Charleston, has had some tough assignments. She worked in EDs in Detroit and Flint, Mich., for a decade before coming to MUSC, where she serves as director of wellness, health, and resilience. One of the incidents that has bothered her the most involved a threat.
It happened when Dr. Krywko denied a patient’s request for narcotics. “She was very angry and said she’d come to my home and cut my children’s heads off,” Dr. Krywko said. “To this day, what she said horrifies me. I still see her smile as she said that.”
Dr. Krywko considered filing for a restraining order against the patient but didn’t because the patient could have learned her address. Dr. Phillips said fear of retaliation is one reason many doctors don’t report threats from patients. “The patient you report knows where you work and may come there to take revenge,” he said. “Also, you may have to continue caring for the person who punched you.”
Online threats also may cause a great deal of angst. Dr. Phillips said he received many online threats when was a medical analyst for CNN in 2020. “Someone sent my address to his Twitter followers, and they shared it with others, so now the whole world knows where I live,” he said. “I had to upgrade security at my home.”
How to deal with volatile patients
Being nice may not always work, but in many cases, it can keep a volatile situation from exploding, according to Dr. Krywko.
“When patients begin to show signs of agitation or are already there, we always try to verbally deescalate the situation, which involves listening,” Dr. Krywko said. “They want someone to hear them out.”
Doctors speak to patients from a position of authority, but Dr. Krywko advises that they should not be too blunt. “Don’t tell patients they’re wrong,” she said. “Even if they may be incorrect, they feel their viewpoint is valid. Encourage a dialogue with words like, ‘Tell me more,’ ” Dr. Krywko said.
Defending yourself
Doctors may have little warning of an impending attack because a patient’s mood can change quickly. This happened several years ago to Jennifer Casaletto, MD, an emergency physician in Charlotte, N.C.
“A man was brought into my ED by ambulance,” she said. “He seemed very calm for a long while, but then he became completely unhinged. A male nurse placed himself between the patient and others and was attacked. He got hurt but was able to continue working.”
Dr. Zeller said health care teams sometimes overreact when patients lash out. “The old-fashioned way to deal with an agitated patient is to call in the cavalry – everyone does a group takedown,” he said. “The patient is put in restraints and heavily sedated. This is not good for anybody. Not only is it likely to injure and traumatize the patient, it can also injure the care team.”
Many hospital EDs have security guards. “I feel safer when a hospital has armed security guards, but they need to be well trained,” Dr. Casaletto said. “Many small hospitals and freestanding EDs do not have security officers at all, or the guards are undertrained or told not to touch anybody.”
In many electronic health record systems, doctors can flag violent patients so future caregivers can be forewarned. However, Dr. Zeller advises against writing about patients’ violence or rudeness in the medical record, because patients can have access to it and might take revenge.
Rising violence from patients
“It feels like it has become much more dangerous to work in the ED,” said Hasan Gokal, MD, an emergency physician working in EDs at the Texas Medical Center. “Just last week, a woman pulled out a gun and fired it in an ED near Houston.”
The statistics back up Dr. Gokal’s assessment. Injuries caused by violent attacks against medical professionals grew by 67% from 2011 to 2018, according to the U.S. Bureau of Labor Statistics. Those levels rose even more during the COVID-19 pandemic – the assault rate in hospitals rose 23% just in 2020.
Dr. Krywko said she had “a patient who said she wanted to hurt the next person who irritated her, and that happened to me. She jumped out of her bed swinging and punching, and I wasn’t ready for it. I yelled for help and the care team came.”
“The rise in violence has to do with a decline in respect for authority,” Dr. Phillips said. “Some people now believe doctors are lying to them about the need for COVID precautions because they are taking money from the vaccine companies. The pandemic has exacerbated violence in every way.”
Dr. Phillips said that a growing lack of resources had led to more anger among patients. “There are fewer nurses and reduced physician coverage,” he said. “That means longer wait times for patients, which increases patients’ frustrations.”
Dr. Weiss said patients have higher expectations. “In sports medicine, the expectations are incredible,” she said. “Parents want their kids to get back to playing as soon as possible.”
“Hospitals in particular are soft targets for violence,” Dr. Phillips said. “People know you can’t assault a flight attendant, because it’s a federal offense, but there is no such federal offense for violence against health care personnel.”
A version of this article first appeared on Medscape.com.
Ralph Newman, MD, got a taste of how dangerous medicine could be at age 10, when he witnessed a physician being shot by a patient.
“I was visiting a friend whose father was a psychiatrist,” Dr. Newman recalled. “We were playing in the living room when the doorbell rang. My friend went to the door and opened it. Then I heard a shot. I ran to the front hall and saw my friend’s father slumped at the bottom of the stairs. He had come down the stairs to see who was there. It was a patient armed with a shotgun.”
As a result of the shooting, a large portion of the psychiatrist’s intestines was removed. In spite of this traumatic incident, Dr. Newman went on to become a psychiatrist – who treated many violent prisoners. “I knew it was dangerous,” he said, “but I rationalized that I wouldn’t be attacked because I would be nicer.”
That attitude seemed to work until 2002, when a prisoner threw boiling oil on him. Dr. Newman was working at the Federal Medical Center Butner, a facility for prisoners in North Carolina. “A prisoner I had been treating was denied parole, based on my recommendation,” he said. “From then on, he was looking for a way to exact revenge.”
“One day I was sitting in the nursing station, typing up notes,” Dr. Newman said. “Two new nurses, who were also there, had forgotten to lock the door, and the prisoner noticed that. He heated up some baby oil in a microwave, which was available to prisoners at the time. Then he walked into the office, threw the oil on my back, and came at me with a sharp pencil.”
Dr. Newman said the nurses fled to an adjoining office, locked the door, and wouldn’t let him in. He went into another office and collapsed in exhaustion. He was saved by an inmate who came on the scene, fended off the attacker, and called for help.
“I was taken to the burn unit,” Dr. Newman recalled. “I had second- and third-degree burns on 9% of my body. It was extremely painful. It took me 45 days to recover enough to get back to work.” The two nurses were fired.
Doctors take threats by patients more seriously now
When orthopedic surgeon Preston Phillips, MD, was killed by a patient in Tulsa, Okla., on June 1, Jennifer M. Weiss, MD, recognized the potential danger to physicians.
“The news left me feeling very shaken,” said Dr. Weiss, a pediatric orthopedic surgeon at Southern California Permanente Medical Group, Los Angeles. “Every orthopedic surgeon I talked to about it felt shaken.”
Dr. Weiss said the impact of that event prompted her to take a patient’s abuse more seriously than she might have previously. “Before the killing, my colleagues and I might have swept the incident under the rug, but we reported it to the authorities,” she said.
“What happened was I told a parent of a school-aged child that the child wasn’t ready to go back to sports,” Dr. Weiss says. “This parent was incredibly triggered – screaming and making verbal threats. The parent was standing between me and the door, so I couldn’t get out.”
Coworkers down the hall heard the yelling and helped Dr. Weiss get out of the room. “The parent was escorted out of the building, and the incident was reported to our risk management team,” she said.
Shooters/killers vs. agitated patients
Patients who shoot to kill are very different from agitated patients seen by many doctors on a regular basis – particularly in emergency departments (EDs), psychiatric units, and pain clinics, said Scott Zeller, MD, a psychiatrist who is vice president of Acute Psychiatric Medicine at Vituity, a multistate physician partnership based in Emeryville, California.
“Agitated patients have trouble communicating their needs and can become physically and verbally aggressive,” Dr. Zeller said. He reports that there are 1.7 million such incidents a year in this country, but most of the incidents of verbal aggression can be kept from exploding into physical violence.
Shooters, however, are very hard to stop because they usually plan the action in advance, Dr. Zeller said. He recalled the 2017 murder of Todd Graham, MD, a friend from medical school. Dr. Graham, an orthopedic surgeon in South Bend, Ind., was gunned down by the husband of one of his patients after Dr. Graham declined to prescribe opioids for her.
Playing down the risk of violence
Doctors may play down the risk of violence, even after they have experienced it personally. “Patients can get angry and may make threatening comments,” Dr. Weiss said. “A lot of doctors just brush it off.”
Simple remarks can set off violence-prone patients, as happened to James P. Phillips, MD, director of disaster and operational medicine at George Washington University, Washington. He recalled asking a prisoner who was visiting his hospital to “lower the volume,” and the man exploded. “Even though he was handcuffed to the bed, he heaved an oxygen tank into a window,” Dr. Phillips said. “He said he would be coming back to kill me.”
Sometimes threats or other types of verbal abuse can be as destructive as physical violence. Diann Krywko, MD, an emergency physician at the Medical University of South Carolina (MUSC) Health, Charleston, has had some tough assignments. She worked in EDs in Detroit and Flint, Mich., for a decade before coming to MUSC, where she serves as director of wellness, health, and resilience. One of the incidents that has bothered her the most involved a threat.
It happened when Dr. Krywko denied a patient’s request for narcotics. “She was very angry and said she’d come to my home and cut my children’s heads off,” Dr. Krywko said. “To this day, what she said horrifies me. I still see her smile as she said that.”
Dr. Krywko considered filing for a restraining order against the patient but didn’t because the patient could have learned her address. Dr. Phillips said fear of retaliation is one reason many doctors don’t report threats from patients. “The patient you report knows where you work and may come there to take revenge,” he said. “Also, you may have to continue caring for the person who punched you.”
Online threats also may cause a great deal of angst. Dr. Phillips said he received many online threats when was a medical analyst for CNN in 2020. “Someone sent my address to his Twitter followers, and they shared it with others, so now the whole world knows where I live,” he said. “I had to upgrade security at my home.”
How to deal with volatile patients
Being nice may not always work, but in many cases, it can keep a volatile situation from exploding, according to Dr. Krywko.
“When patients begin to show signs of agitation or are already there, we always try to verbally deescalate the situation, which involves listening,” Dr. Krywko said. “They want someone to hear them out.”
Doctors speak to patients from a position of authority, but Dr. Krywko advises that they should not be too blunt. “Don’t tell patients they’re wrong,” she said. “Even if they may be incorrect, they feel their viewpoint is valid. Encourage a dialogue with words like, ‘Tell me more,’ ” Dr. Krywko said.
Defending yourself
Doctors may have little warning of an impending attack because a patient’s mood can change quickly. This happened several years ago to Jennifer Casaletto, MD, an emergency physician in Charlotte, N.C.
“A man was brought into my ED by ambulance,” she said. “He seemed very calm for a long while, but then he became completely unhinged. A male nurse placed himself between the patient and others and was attacked. He got hurt but was able to continue working.”
Dr. Zeller said health care teams sometimes overreact when patients lash out. “The old-fashioned way to deal with an agitated patient is to call in the cavalry – everyone does a group takedown,” he said. “The patient is put in restraints and heavily sedated. This is not good for anybody. Not only is it likely to injure and traumatize the patient, it can also injure the care team.”
Many hospital EDs have security guards. “I feel safer when a hospital has armed security guards, but they need to be well trained,” Dr. Casaletto said. “Many small hospitals and freestanding EDs do not have security officers at all, or the guards are undertrained or told not to touch anybody.”
In many electronic health record systems, doctors can flag violent patients so future caregivers can be forewarned. However, Dr. Zeller advises against writing about patients’ violence or rudeness in the medical record, because patients can have access to it and might take revenge.
Rising violence from patients
“It feels like it has become much more dangerous to work in the ED,” said Hasan Gokal, MD, an emergency physician working in EDs at the Texas Medical Center. “Just last week, a woman pulled out a gun and fired it in an ED near Houston.”
The statistics back up Dr. Gokal’s assessment. Injuries caused by violent attacks against medical professionals grew by 67% from 2011 to 2018, according to the U.S. Bureau of Labor Statistics. Those levels rose even more during the COVID-19 pandemic – the assault rate in hospitals rose 23% just in 2020.
Dr. Krywko said she had “a patient who said she wanted to hurt the next person who irritated her, and that happened to me. She jumped out of her bed swinging and punching, and I wasn’t ready for it. I yelled for help and the care team came.”
“The rise in violence has to do with a decline in respect for authority,” Dr. Phillips said. “Some people now believe doctors are lying to them about the need for COVID precautions because they are taking money from the vaccine companies. The pandemic has exacerbated violence in every way.”
Dr. Phillips said that a growing lack of resources had led to more anger among patients. “There are fewer nurses and reduced physician coverage,” he said. “That means longer wait times for patients, which increases patients’ frustrations.”
Dr. Weiss said patients have higher expectations. “In sports medicine, the expectations are incredible,” she said. “Parents want their kids to get back to playing as soon as possible.”
“Hospitals in particular are soft targets for violence,” Dr. Phillips said. “People know you can’t assault a flight attendant, because it’s a federal offense, but there is no such federal offense for violence against health care personnel.”
A version of this article first appeared on Medscape.com.
Ten steps for clinicians to avoid being racist: The Francis commitment
As a Black man who grew up in this country, I can tell you first-hand what it does to you. The scars never go away, and your status is always in question, no matter your title or uniforms of respect. Eventually it wears you down.
I was born into poverty and the segregation of southwest Louisiana. I experienced the dehumanization intended for me: separate drinking fountains and poor foundational education. I was lucky to attend a historically Black college or university (Southern University, Baton Rouge, La.), that gave me my bearings. I then went to some of the very best, predominantly White institutions.
When I looked for a job after training, there were few integrated medical groups, so I started my own. It included practitioners who were White, Black, Jewish, Asian, Middle Eastern, Muslim, Christian, etc. We cross covered and treated patients from every corner of the globe.
In medicine, we treat human beings with disease. The disease should be the only difference that sets us apart. There is absolutely no place for racism.
It is difficult to be called a racist, and I have met only a handful of people in health care whom I would label as such. But racism is structural and institutionalized so that it is often hidden.
One way to overcome this is to make every effort possible to get to know people as individuals. Only then can we see that there are few real differences between us. I would often seek out a colleague from a different culture or race to have lunch with so I could learn more about them.
We all strive for the same things – validation, happiness, love, family, and a future. We all grieve over the same things.
What some caregivers may not realize is that, just as clinicians have been trained to recognize subtle signs and symptoms of disease, minorities can recognize racism immediately during a medical encounter. Our past experiences make us skilled at picking up a lack of eye contact or body language and tone of voice that are dismissive and disrespectful.
A patient who has felt racism may still return for care because of insurance coverage limitations, location, or a lack of alternatives. But trust and loyalty will never develop on the part of this patient, and empathy will be absent on the part of their caregiver.
To counter this in my own practice, I developed the Francis Commitment to avoid any hint of racism or bias toward my patients.
I commit to the following:
1. I see you.
2. I hear you.
3. I accept who you are.
4. I will try to understand how you must feel (empathy).
5. Treating you is very important to me.
6. I would like to gain your trust that I will do my very best to make you better.
7. I value you as a human being and will treat you as if you are family.
8. I care about what happens to you.
9. I want us to work together to fight this disease.
10. I am grateful that you chose me as your caregiver.
The INOVA health care system where I work has undertaken an initiative called What Matters Most to better understand the needs of every patient. We are currently working on a strategy of patient personalization to not only learn about their medical needs but also to discover who they are as a person. We incorporate Social Determinants of Health in our dealings with patients. We also have participated in a program called “A Long Talk”, where we learned that those of us who remain silent when we see or hear racism are responsible for its persistence and growth.
But we must do more. Racism will propagate if we live in silos surrounded by people whose ideas reflect our own. As long as we have nondiversified board rooms, departments, and staff, the problem will persist.
A lot of the biases that we unconsciously carry in our heads and hearts have no basis in reality and were placed there without our permission by parents, society, and friends. But we can replace these divisive thoughts and impulses.
What’s in your heart can only be known and controlled by you. How tolerant we are of racism is up to us: Do you call out racism; do you challenge any inkling of racism from friends or acquaintances; do you put pressure on institutions where you work to diversify in recruiting and hiring?
Think of all the advances in medicine that were achieved by people from different cultures and races. Racism has no place in what we have all devoted our lives to do – take care of our fellow humans.
A version of this article first appeared on Medscape.com.
As a Black man who grew up in this country, I can tell you first-hand what it does to you. The scars never go away, and your status is always in question, no matter your title or uniforms of respect. Eventually it wears you down.
I was born into poverty and the segregation of southwest Louisiana. I experienced the dehumanization intended for me: separate drinking fountains and poor foundational education. I was lucky to attend a historically Black college or university (Southern University, Baton Rouge, La.), that gave me my bearings. I then went to some of the very best, predominantly White institutions.
When I looked for a job after training, there were few integrated medical groups, so I started my own. It included practitioners who were White, Black, Jewish, Asian, Middle Eastern, Muslim, Christian, etc. We cross covered and treated patients from every corner of the globe.
In medicine, we treat human beings with disease. The disease should be the only difference that sets us apart. There is absolutely no place for racism.
It is difficult to be called a racist, and I have met only a handful of people in health care whom I would label as such. But racism is structural and institutionalized so that it is often hidden.
One way to overcome this is to make every effort possible to get to know people as individuals. Only then can we see that there are few real differences between us. I would often seek out a colleague from a different culture or race to have lunch with so I could learn more about them.
We all strive for the same things – validation, happiness, love, family, and a future. We all grieve over the same things.
What some caregivers may not realize is that, just as clinicians have been trained to recognize subtle signs and symptoms of disease, minorities can recognize racism immediately during a medical encounter. Our past experiences make us skilled at picking up a lack of eye contact or body language and tone of voice that are dismissive and disrespectful.
A patient who has felt racism may still return for care because of insurance coverage limitations, location, or a lack of alternatives. But trust and loyalty will never develop on the part of this patient, and empathy will be absent on the part of their caregiver.
To counter this in my own practice, I developed the Francis Commitment to avoid any hint of racism or bias toward my patients.
I commit to the following:
1. I see you.
2. I hear you.
3. I accept who you are.
4. I will try to understand how you must feel (empathy).
5. Treating you is very important to me.
6. I would like to gain your trust that I will do my very best to make you better.
7. I value you as a human being and will treat you as if you are family.
8. I care about what happens to you.
9. I want us to work together to fight this disease.
10. I am grateful that you chose me as your caregiver.
The INOVA health care system where I work has undertaken an initiative called What Matters Most to better understand the needs of every patient. We are currently working on a strategy of patient personalization to not only learn about their medical needs but also to discover who they are as a person. We incorporate Social Determinants of Health in our dealings with patients. We also have participated in a program called “A Long Talk”, where we learned that those of us who remain silent when we see or hear racism are responsible for its persistence and growth.
But we must do more. Racism will propagate if we live in silos surrounded by people whose ideas reflect our own. As long as we have nondiversified board rooms, departments, and staff, the problem will persist.
A lot of the biases that we unconsciously carry in our heads and hearts have no basis in reality and were placed there without our permission by parents, society, and friends. But we can replace these divisive thoughts and impulses.
What’s in your heart can only be known and controlled by you. How tolerant we are of racism is up to us: Do you call out racism; do you challenge any inkling of racism from friends or acquaintances; do you put pressure on institutions where you work to diversify in recruiting and hiring?
Think of all the advances in medicine that were achieved by people from different cultures and races. Racism has no place in what we have all devoted our lives to do – take care of our fellow humans.
A version of this article first appeared on Medscape.com.
As a Black man who grew up in this country, I can tell you first-hand what it does to you. The scars never go away, and your status is always in question, no matter your title or uniforms of respect. Eventually it wears you down.
I was born into poverty and the segregation of southwest Louisiana. I experienced the dehumanization intended for me: separate drinking fountains and poor foundational education. I was lucky to attend a historically Black college or university (Southern University, Baton Rouge, La.), that gave me my bearings. I then went to some of the very best, predominantly White institutions.
When I looked for a job after training, there were few integrated medical groups, so I started my own. It included practitioners who were White, Black, Jewish, Asian, Middle Eastern, Muslim, Christian, etc. We cross covered and treated patients from every corner of the globe.
In medicine, we treat human beings with disease. The disease should be the only difference that sets us apart. There is absolutely no place for racism.
It is difficult to be called a racist, and I have met only a handful of people in health care whom I would label as such. But racism is structural and institutionalized so that it is often hidden.
One way to overcome this is to make every effort possible to get to know people as individuals. Only then can we see that there are few real differences between us. I would often seek out a colleague from a different culture or race to have lunch with so I could learn more about them.
We all strive for the same things – validation, happiness, love, family, and a future. We all grieve over the same things.
What some caregivers may not realize is that, just as clinicians have been trained to recognize subtle signs and symptoms of disease, minorities can recognize racism immediately during a medical encounter. Our past experiences make us skilled at picking up a lack of eye contact or body language and tone of voice that are dismissive and disrespectful.
A patient who has felt racism may still return for care because of insurance coverage limitations, location, or a lack of alternatives. But trust and loyalty will never develop on the part of this patient, and empathy will be absent on the part of their caregiver.
To counter this in my own practice, I developed the Francis Commitment to avoid any hint of racism or bias toward my patients.
I commit to the following:
1. I see you.
2. I hear you.
3. I accept who you are.
4. I will try to understand how you must feel (empathy).
5. Treating you is very important to me.
6. I would like to gain your trust that I will do my very best to make you better.
7. I value you as a human being and will treat you as if you are family.
8. I care about what happens to you.
9. I want us to work together to fight this disease.
10. I am grateful that you chose me as your caregiver.
The INOVA health care system where I work has undertaken an initiative called What Matters Most to better understand the needs of every patient. We are currently working on a strategy of patient personalization to not only learn about their medical needs but also to discover who they are as a person. We incorporate Social Determinants of Health in our dealings with patients. We also have participated in a program called “A Long Talk”, where we learned that those of us who remain silent when we see or hear racism are responsible for its persistence and growth.
But we must do more. Racism will propagate if we live in silos surrounded by people whose ideas reflect our own. As long as we have nondiversified board rooms, departments, and staff, the problem will persist.
A lot of the biases that we unconsciously carry in our heads and hearts have no basis in reality and were placed there without our permission by parents, society, and friends. But we can replace these divisive thoughts and impulses.
What’s in your heart can only be known and controlled by you. How tolerant we are of racism is up to us: Do you call out racism; do you challenge any inkling of racism from friends or acquaintances; do you put pressure on institutions where you work to diversify in recruiting and hiring?
Think of all the advances in medicine that were achieved by people from different cultures and races. Racism has no place in what we have all devoted our lives to do – take care of our fellow humans.
A version of this article first appeared on Medscape.com.
Antidepressants may curb opioid overdose
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.

“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.

“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.

“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PSYCHIATRIC SERVICES
People really can get ‘hangry’ when hungry
The notion that people get ‘hangry’ – irritable and short-tempered when they’re hungry – is such an established part of modern folklore that the word has even been added to the Oxford English Dictionary. Although experimental studies in the past have shown that low blood glucose levels increase impulsivity, anger, and aggression, there has been little solid evidence that this translates to real-life settings.
Now new research has confirmed that the phenomenon does really exist in everyday life. The study, published in the journal PLOS ONE, is the first to investigate how hunger affects people’s emotions on a day-to-day level. Lead author Viren Swami, professor of social psychology at Anglia Ruskin University, Cambridge, England, said: “Many of us are aware that being hungry can influence our emotions, but surprisingly little scientific research has focused on being ‘hangry’.”
He and coauthors from Karl Landsteiner University of Health Sciences in Krems an der Donau, Austria, recruited 64 participants from Central Europe who completed a 21-day experience sampling phase, in which they were prompted to report their feelings on a smartphone app five times a day. At each prompt, they reported their levels of hunger, anger, irritability, pleasure, and arousal on a visual analog scale.
Participants were on average 29.9 years old (range = 18-60), predominantly (81.3%) women, and had a mean body mass index of 23.8 kg/m2 (range 15.8-36.5 kg/m2).
Anger was rated on a 5-point scale but the team explained that the effects of hunger are unlikely to be unique to anger per se, so they also asked about experiences of irritability and, in order to obtain a more holistic view of emotionality, also about pleasure and arousal, as indexed using Russell’s affect grid.
They also asked about eating behaviors over the previous 3 weeks, including frequency of main meals, snacking behavior, healthy eating, feeling hungry, and sense of satiety, and about dietary behaviors including restrictive eating, emotionally induced eating, and externally determined eating behavior.
Analysis of the resulting total of 9,142 responses showed that higher levels of self-reported hunger were associated with greater feelings of anger and irritability, and with lower levels of pleasure. These findings remained significant after accounting for participants’ sex, age, body mass index, dietary behaviors, and trait anger. However, associations with arousal were not significant.
The authors commented that the use of the app allowed data collection to take place in subjects’ everyday environments, such as their workplace and at home. “These results provide evidence that everyday levels of hunger are associated with negative emotionality and supports the notion of being ‘hangry.’ ”
‘Substantial’ effects
“The effects were substantial,” the team said, “even after taking into account demographic factors” such as age and sex, body mass index, dietary behavior, and individual personality traits. Hunger was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants.
The research also showed that the negative emotions – irritability, anger, and unpleasantness – were caused by both day-to-day fluctuations in hunger and residual levels of hunger measured by averages over the 3-week period.
The authors said their findings “suggest that the experience of being hangry is real, insofar as hunger was associated with greater anger and irritability, and lower pleasure, in our sample over a period of 3 weeks.
“These results may have important implications for understanding everyday experiences of emotions, and may also assist practitioners to more effectively ensure productive individual behaviors and interpersonal relationships (for example, by ensuring that no one goes hungry).”
Although the majority of participants (55%) said they paid attention to hunger pangs, only 23% said that they knew when they were full and then stopped eating, whereas 63% said they could tell when they were full but sometimes continued to eat. Few (4.7%) people said they could not tell when they were full and therefore oriented their eating based on the size of the meal, but 9% described frequent overeating because of not feeling satiated, and 13% stated they ate when they were stressed, upset, angry, or bored.
Professor Swami said: “Ours is the first study to examine being ‘hangry’ outside of a lab. By following people in their day-to-day lives, we found that hunger was related to levels of anger, irritability, and pleasure.
“Although our study doesn’t present ways to mitigate negative hunger-induced emotions, research suggests that being able to label an emotion can help people to regulate it, such as by recognizing that we feel angry simply because we are hungry. Therefore, greater awareness of being ‘hangry’ could reduce the likelihood that hunger results in negative emotions and behaviors in individuals.”
A version of this article first appeared on Medscape UK.
The notion that people get ‘hangry’ – irritable and short-tempered when they’re hungry – is such an established part of modern folklore that the word has even been added to the Oxford English Dictionary. Although experimental studies in the past have shown that low blood glucose levels increase impulsivity, anger, and aggression, there has been little solid evidence that this translates to real-life settings.
Now new research has confirmed that the phenomenon does really exist in everyday life. The study, published in the journal PLOS ONE, is the first to investigate how hunger affects people’s emotions on a day-to-day level. Lead author Viren Swami, professor of social psychology at Anglia Ruskin University, Cambridge, England, said: “Many of us are aware that being hungry can influence our emotions, but surprisingly little scientific research has focused on being ‘hangry’.”
He and coauthors from Karl Landsteiner University of Health Sciences in Krems an der Donau, Austria, recruited 64 participants from Central Europe who completed a 21-day experience sampling phase, in which they were prompted to report their feelings on a smartphone app five times a day. At each prompt, they reported their levels of hunger, anger, irritability, pleasure, and arousal on a visual analog scale.
Participants were on average 29.9 years old (range = 18-60), predominantly (81.3%) women, and had a mean body mass index of 23.8 kg/m2 (range 15.8-36.5 kg/m2).
Anger was rated on a 5-point scale but the team explained that the effects of hunger are unlikely to be unique to anger per se, so they also asked about experiences of irritability and, in order to obtain a more holistic view of emotionality, also about pleasure and arousal, as indexed using Russell’s affect grid.
They also asked about eating behaviors over the previous 3 weeks, including frequency of main meals, snacking behavior, healthy eating, feeling hungry, and sense of satiety, and about dietary behaviors including restrictive eating, emotionally induced eating, and externally determined eating behavior.
Analysis of the resulting total of 9,142 responses showed that higher levels of self-reported hunger were associated with greater feelings of anger and irritability, and with lower levels of pleasure. These findings remained significant after accounting for participants’ sex, age, body mass index, dietary behaviors, and trait anger. However, associations with arousal were not significant.
The authors commented that the use of the app allowed data collection to take place in subjects’ everyday environments, such as their workplace and at home. “These results provide evidence that everyday levels of hunger are associated with negative emotionality and supports the notion of being ‘hangry.’ ”
‘Substantial’ effects
“The effects were substantial,” the team said, “even after taking into account demographic factors” such as age and sex, body mass index, dietary behavior, and individual personality traits. Hunger was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants.
The research also showed that the negative emotions – irritability, anger, and unpleasantness – were caused by both day-to-day fluctuations in hunger and residual levels of hunger measured by averages over the 3-week period.
The authors said their findings “suggest that the experience of being hangry is real, insofar as hunger was associated with greater anger and irritability, and lower pleasure, in our sample over a period of 3 weeks.
“These results may have important implications for understanding everyday experiences of emotions, and may also assist practitioners to more effectively ensure productive individual behaviors and interpersonal relationships (for example, by ensuring that no one goes hungry).”
Although the majority of participants (55%) said they paid attention to hunger pangs, only 23% said that they knew when they were full and then stopped eating, whereas 63% said they could tell when they were full but sometimes continued to eat. Few (4.7%) people said they could not tell when they were full and therefore oriented their eating based on the size of the meal, but 9% described frequent overeating because of not feeling satiated, and 13% stated they ate when they were stressed, upset, angry, or bored.
Professor Swami said: “Ours is the first study to examine being ‘hangry’ outside of a lab. By following people in their day-to-day lives, we found that hunger was related to levels of anger, irritability, and pleasure.
“Although our study doesn’t present ways to mitigate negative hunger-induced emotions, research suggests that being able to label an emotion can help people to regulate it, such as by recognizing that we feel angry simply because we are hungry. Therefore, greater awareness of being ‘hangry’ could reduce the likelihood that hunger results in negative emotions and behaviors in individuals.”
A version of this article first appeared on Medscape UK.
The notion that people get ‘hangry’ – irritable and short-tempered when they’re hungry – is such an established part of modern folklore that the word has even been added to the Oxford English Dictionary. Although experimental studies in the past have shown that low blood glucose levels increase impulsivity, anger, and aggression, there has been little solid evidence that this translates to real-life settings.
Now new research has confirmed that the phenomenon does really exist in everyday life. The study, published in the journal PLOS ONE, is the first to investigate how hunger affects people’s emotions on a day-to-day level. Lead author Viren Swami, professor of social psychology at Anglia Ruskin University, Cambridge, England, said: “Many of us are aware that being hungry can influence our emotions, but surprisingly little scientific research has focused on being ‘hangry’.”
He and coauthors from Karl Landsteiner University of Health Sciences in Krems an der Donau, Austria, recruited 64 participants from Central Europe who completed a 21-day experience sampling phase, in which they were prompted to report their feelings on a smartphone app five times a day. At each prompt, they reported their levels of hunger, anger, irritability, pleasure, and arousal on a visual analog scale.
Participants were on average 29.9 years old (range = 18-60), predominantly (81.3%) women, and had a mean body mass index of 23.8 kg/m2 (range 15.8-36.5 kg/m2).
Anger was rated on a 5-point scale but the team explained that the effects of hunger are unlikely to be unique to anger per se, so they also asked about experiences of irritability and, in order to obtain a more holistic view of emotionality, also about pleasure and arousal, as indexed using Russell’s affect grid.
They also asked about eating behaviors over the previous 3 weeks, including frequency of main meals, snacking behavior, healthy eating, feeling hungry, and sense of satiety, and about dietary behaviors including restrictive eating, emotionally induced eating, and externally determined eating behavior.
Analysis of the resulting total of 9,142 responses showed that higher levels of self-reported hunger were associated with greater feelings of anger and irritability, and with lower levels of pleasure. These findings remained significant after accounting for participants’ sex, age, body mass index, dietary behaviors, and trait anger. However, associations with arousal were not significant.
The authors commented that the use of the app allowed data collection to take place in subjects’ everyday environments, such as their workplace and at home. “These results provide evidence that everyday levels of hunger are associated with negative emotionality and supports the notion of being ‘hangry.’ ”
‘Substantial’ effects
“The effects were substantial,” the team said, “even after taking into account demographic factors” such as age and sex, body mass index, dietary behavior, and individual personality traits. Hunger was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants.
The research also showed that the negative emotions – irritability, anger, and unpleasantness – were caused by both day-to-day fluctuations in hunger and residual levels of hunger measured by averages over the 3-week period.
The authors said their findings “suggest that the experience of being hangry is real, insofar as hunger was associated with greater anger and irritability, and lower pleasure, in our sample over a period of 3 weeks.
“These results may have important implications for understanding everyday experiences of emotions, and may also assist practitioners to more effectively ensure productive individual behaviors and interpersonal relationships (for example, by ensuring that no one goes hungry).”
Although the majority of participants (55%) said they paid attention to hunger pangs, only 23% said that they knew when they were full and then stopped eating, whereas 63% said they could tell when they were full but sometimes continued to eat. Few (4.7%) people said they could not tell when they were full and therefore oriented their eating based on the size of the meal, but 9% described frequent overeating because of not feeling satiated, and 13% stated they ate when they were stressed, upset, angry, or bored.
Professor Swami said: “Ours is the first study to examine being ‘hangry’ outside of a lab. By following people in their day-to-day lives, we found that hunger was related to levels of anger, irritability, and pleasure.
“Although our study doesn’t present ways to mitigate negative hunger-induced emotions, research suggests that being able to label an emotion can help people to regulate it, such as by recognizing that we feel angry simply because we are hungry. Therefore, greater awareness of being ‘hangry’ could reduce the likelihood that hunger results in negative emotions and behaviors in individuals.”
A version of this article first appeared on Medscape UK.
FROM PLOS ONE



