User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
PCOS common in adolescent girls with type 2 diabetes
Polycystic ovary syndrome is common in girls with type 2 diabetes, findings of a new study suggest, and authors say screening for PCOS is critical in this group.
In a systematic review and meta-analysis involving 470 girls (average age 12.9-16.1 years) with type 2 diabetes in six studies, the prevalence of PCOS was nearly 1 in 5 (19.58%; 95% confidence interval, 12.02%-27.14%; P = .002), substantially higher than that of PCOS in the general adolescent population.
PCOS, a complex endocrine disorder, occurs in 1.14%-11.04% of adolescent girls globally, according to the paper published online in JAMA Network Open.
The secondary outcome studied links to prevalence of PCOS with race and obesity.
Insulin resistance and compensatory hyperinsulinemia are present in 44%-70% of women with PCOS, suggesting that they are more likely to develop type 2 diabetes, according to the researchers led by Milena Cioana, BHSc, with the department of pediatrics, McMaster University, Hamilton, Ont.
Kelly A. Curran, MD, an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center in Oklahoma City, where she practices adolescent medicine, said in an interview that it has been known that women with PCOS have higher rates of diabetes and many in the field have suspected the relationship is bidirectional.
“In my clinical practice, I’ve seen a high percentage of women with type 2 diabetes present with irregular menses, some of whom have gone on to be diagnosed with PCOS,” said Dr. Curran, who was not involved with the study.
However, she said, she was surprised the prevalence of PCOS reported in this paper – nearly one in five – was so high. Early diagnosis is important for PCOS to prevent complications such as hypertension, hyperglycemia, and dyslipidemia.
Psychiatric conditions are also prevalent in patients with PCOS, including anxiety (18%), depression (16%), and ADHD (9%).
Dr. Curran agreed there is a need to screen for PCOS and to evaluate for other causes of irregular periods in patients with type 2 diabetes.
“Menstrual irregularities are often overlooked in young women without further work-up, especially in patients who have chronic illnesses,” she noted.
Results come with a caveat
However, the authors said, results should be viewed with caution because “studies including the larger numbers of girls did not report the criteria used to diagnose PCOS, which is a challenge during adolescence.”
Diagnostic criteria for PCOS during adolescence include the combination of menstrual irregularities according to time since their first period and clinical or biochemical hyperandrogenism after excluding other potential causes.
Dr. Curran explained that PCOS symptoms include irregular periods and acne which can overlap with normal changes in puberty. In her experience, PCOS is often diagnosed without patients meeting full criteria. She agreed further research with standardized criteria is urgently needed.
The European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine, the Pediatric Endocrine Society, and the International Consortium of Paediatric Endocrinology guidelines suggest that using ultrasound to check the size of ovaries could help diagnose PCOS, but other guidelines are more conservative, the authors noted.
They added that “there is a need for a consensus to establish the pediatric criteria for diagnosing PCOS in adolescents to ensure accurate diagnosis and lower the misclassification rates.”
Assessing links to obesity and race
Still unclear, the authors wrote, is whether and how obesity and race affect prevalence of PCOS among girls with type 2 diabetes.
The authors wrote: “Although earlier studies suggested that obesity-related insulin resistance and hyperinsulinemia can contribute to PCOS pathogenesis, insulin resistance in patients with PCOS may be present independently of [body mass index]. Obesity seems to increase the risk of PCOS only slightly and might represent a referral bias for PCOS.”
Few studies included in the meta-analysis had race-specific data, so the authors were limited in assessing associations between race and PCOS prevalence.
“However,” they wrote, “our data demonstrate that Indian girls had the highest prevalence, followed by White girls, and then Indigenous girls in Canada.”
Further studies are needed to help define at-risk subgroups and evaluate treatment strategies, the authors noted.
They reported having no relevant financial relationships. Dr. Curran had no conflicts of interest.
Polycystic ovary syndrome is common in girls with type 2 diabetes, findings of a new study suggest, and authors say screening for PCOS is critical in this group.
In a systematic review and meta-analysis involving 470 girls (average age 12.9-16.1 years) with type 2 diabetes in six studies, the prevalence of PCOS was nearly 1 in 5 (19.58%; 95% confidence interval, 12.02%-27.14%; P = .002), substantially higher than that of PCOS in the general adolescent population.
PCOS, a complex endocrine disorder, occurs in 1.14%-11.04% of adolescent girls globally, according to the paper published online in JAMA Network Open.
The secondary outcome studied links to prevalence of PCOS with race and obesity.
Insulin resistance and compensatory hyperinsulinemia are present in 44%-70% of women with PCOS, suggesting that they are more likely to develop type 2 diabetes, according to the researchers led by Milena Cioana, BHSc, with the department of pediatrics, McMaster University, Hamilton, Ont.
Kelly A. Curran, MD, an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center in Oklahoma City, where she practices adolescent medicine, said in an interview that it has been known that women with PCOS have higher rates of diabetes and many in the field have suspected the relationship is bidirectional.
“In my clinical practice, I’ve seen a high percentage of women with type 2 diabetes present with irregular menses, some of whom have gone on to be diagnosed with PCOS,” said Dr. Curran, who was not involved with the study.
However, she said, she was surprised the prevalence of PCOS reported in this paper – nearly one in five – was so high. Early diagnosis is important for PCOS to prevent complications such as hypertension, hyperglycemia, and dyslipidemia.
Psychiatric conditions are also prevalent in patients with PCOS, including anxiety (18%), depression (16%), and ADHD (9%).
Dr. Curran agreed there is a need to screen for PCOS and to evaluate for other causes of irregular periods in patients with type 2 diabetes.
“Menstrual irregularities are often overlooked in young women without further work-up, especially in patients who have chronic illnesses,” she noted.
Results come with a caveat
However, the authors said, results should be viewed with caution because “studies including the larger numbers of girls did not report the criteria used to diagnose PCOS, which is a challenge during adolescence.”
Diagnostic criteria for PCOS during adolescence include the combination of menstrual irregularities according to time since their first period and clinical or biochemical hyperandrogenism after excluding other potential causes.
Dr. Curran explained that PCOS symptoms include irregular periods and acne which can overlap with normal changes in puberty. In her experience, PCOS is often diagnosed without patients meeting full criteria. She agreed further research with standardized criteria is urgently needed.
The European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine, the Pediatric Endocrine Society, and the International Consortium of Paediatric Endocrinology guidelines suggest that using ultrasound to check the size of ovaries could help diagnose PCOS, but other guidelines are more conservative, the authors noted.
They added that “there is a need for a consensus to establish the pediatric criteria for diagnosing PCOS in adolescents to ensure accurate diagnosis and lower the misclassification rates.”
Assessing links to obesity and race
Still unclear, the authors wrote, is whether and how obesity and race affect prevalence of PCOS among girls with type 2 diabetes.
The authors wrote: “Although earlier studies suggested that obesity-related insulin resistance and hyperinsulinemia can contribute to PCOS pathogenesis, insulin resistance in patients with PCOS may be present independently of [body mass index]. Obesity seems to increase the risk of PCOS only slightly and might represent a referral bias for PCOS.”
Few studies included in the meta-analysis had race-specific data, so the authors were limited in assessing associations between race and PCOS prevalence.
“However,” they wrote, “our data demonstrate that Indian girls had the highest prevalence, followed by White girls, and then Indigenous girls in Canada.”
Further studies are needed to help define at-risk subgroups and evaluate treatment strategies, the authors noted.
They reported having no relevant financial relationships. Dr. Curran had no conflicts of interest.
Polycystic ovary syndrome is common in girls with type 2 diabetes, findings of a new study suggest, and authors say screening for PCOS is critical in this group.
In a systematic review and meta-analysis involving 470 girls (average age 12.9-16.1 years) with type 2 diabetes in six studies, the prevalence of PCOS was nearly 1 in 5 (19.58%; 95% confidence interval, 12.02%-27.14%; P = .002), substantially higher than that of PCOS in the general adolescent population.
PCOS, a complex endocrine disorder, occurs in 1.14%-11.04% of adolescent girls globally, according to the paper published online in JAMA Network Open.
The secondary outcome studied links to prevalence of PCOS with race and obesity.
Insulin resistance and compensatory hyperinsulinemia are present in 44%-70% of women with PCOS, suggesting that they are more likely to develop type 2 diabetes, according to the researchers led by Milena Cioana, BHSc, with the department of pediatrics, McMaster University, Hamilton, Ont.
Kelly A. Curran, MD, an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center in Oklahoma City, where she practices adolescent medicine, said in an interview that it has been known that women with PCOS have higher rates of diabetes and many in the field have suspected the relationship is bidirectional.
“In my clinical practice, I’ve seen a high percentage of women with type 2 diabetes present with irregular menses, some of whom have gone on to be diagnosed with PCOS,” said Dr. Curran, who was not involved with the study.
However, she said, she was surprised the prevalence of PCOS reported in this paper – nearly one in five – was so high. Early diagnosis is important for PCOS to prevent complications such as hypertension, hyperglycemia, and dyslipidemia.
Psychiatric conditions are also prevalent in patients with PCOS, including anxiety (18%), depression (16%), and ADHD (9%).
Dr. Curran agreed there is a need to screen for PCOS and to evaluate for other causes of irregular periods in patients with type 2 diabetes.
“Menstrual irregularities are often overlooked in young women without further work-up, especially in patients who have chronic illnesses,” she noted.
Results come with a caveat
However, the authors said, results should be viewed with caution because “studies including the larger numbers of girls did not report the criteria used to diagnose PCOS, which is a challenge during adolescence.”
Diagnostic criteria for PCOS during adolescence include the combination of menstrual irregularities according to time since their first period and clinical or biochemical hyperandrogenism after excluding other potential causes.
Dr. Curran explained that PCOS symptoms include irregular periods and acne which can overlap with normal changes in puberty. In her experience, PCOS is often diagnosed without patients meeting full criteria. She agreed further research with standardized criteria is urgently needed.
The European Society of Human Reproduction and Embryology/American Society of Reproductive Medicine, the Pediatric Endocrine Society, and the International Consortium of Paediatric Endocrinology guidelines suggest that using ultrasound to check the size of ovaries could help diagnose PCOS, but other guidelines are more conservative, the authors noted.
They added that “there is a need for a consensus to establish the pediatric criteria for diagnosing PCOS in adolescents to ensure accurate diagnosis and lower the misclassification rates.”
Assessing links to obesity and race
Still unclear, the authors wrote, is whether and how obesity and race affect prevalence of PCOS among girls with type 2 diabetes.
The authors wrote: “Although earlier studies suggested that obesity-related insulin resistance and hyperinsulinemia can contribute to PCOS pathogenesis, insulin resistance in patients with PCOS may be present independently of [body mass index]. Obesity seems to increase the risk of PCOS only slightly and might represent a referral bias for PCOS.”
Few studies included in the meta-analysis had race-specific data, so the authors were limited in assessing associations between race and PCOS prevalence.
“However,” they wrote, “our data demonstrate that Indian girls had the highest prevalence, followed by White girls, and then Indigenous girls in Canada.”
Further studies are needed to help define at-risk subgroups and evaluate treatment strategies, the authors noted.
They reported having no relevant financial relationships. Dr. Curran had no conflicts of interest.
FROM JAMA NETWORK OPEN
Assisting Surgeons with Management: Initial Presentation of Abnormal Bleeding and Diagnosing of Fibroids
As an Advanced Practice Provider, when and why might a patient with uterine fibroids be scheduled to visit with you?
Ms. Haibach: Typically, with the flow of how our practice runs, a patient would schedule with me as an initial visit to explore their abnormal or heavy bleeding. Oftentimes, a patient is unsure with what they have going on medically and will view APPs as a safe place to start. Other times, I will see a patient for a general wellness exam who will mention heavier menses over the years or just a change in their bleeding pattern-- longer flow, things like that.
It may stem from something that seems out of the ordinary for them or a symptom impacting their life. For example, if a patient says, “I have to run home and change my clothes,” or “I'm bleeding through my bed sheets.” Those statements prompt further evaluation. At times, patients who have already been diagnosed with fibroids, will come to see me if they have chosen medical management over surgical management of their fibroids. They continue to follow up with me to reevaluate the success of their treatment plan periodically. So, whether I start them on a plan, or a physician does, they can follow up with me to revisit their medical plan and ensure it remains appropriate.
You touched on this a bit, but can you dive deeper into exactly what you are looking for as part of that visit?
Ms. Haibach: Definitely. With an initial consult to me, the number one question that I would ask my patients first is, what is your most bothersome symptom? With this question, I'm looking to determine: is it pain that brought you to me? Is it heavy bleeding? Do you feel bulk and bloaty? Are you having issues getting pregnant? Do you have bowel or bladder issues?
The information I get from that one initial question, helps guide the remainder of my visit. If bleeding is the main concern, we would focus on getting that under control. So, we need to suppress the menses with medication options. If bulk and bloating is the main concern, for instance the patient feels like they have a pregnant-looking abdomen, typically surgical options are warranted. If the main complaint is infertility, we do have fertility specialists in our practice who remove fibroids to aid patients in achieving pregnancy.
The most important purpose of this visit is to really listen to the patient to find out how these symptoms are impacting their daily lives. From there, I can use that information to guide my treatment plan.
So, once it is determined that the patient is a good surgical candidate, what would be the next steps?
Ms. Haibach: If at the end of my visit, I determine that a patient is potentially a suitable surgical candidate, the first thing I would do is order appropriate imaging. For example, if the patient is interested in uterine preservation for future fertility, she is likely going to opt for a laparoscopic myomectomy, where fibroids would be removed, and her uterus would be left in place. In that case, she would require an MRI for fibroid mapping. If a woman has completed childbearing, then oftentimes a pelvic ultrasound would suffice, at least to start, since she'd likely elect hysterectomy if she has reached her fertility goals.
I would also perform an endometrial biopsy to rule out malignant process before going into surgery. To optimize a patient for our MIGS surgeons, I gather a thorough medical history to ensure their comorbidities are appropriately managed. For example, diabetes is under control, sleep apnea is being treated, no active infections. If there is anything else going on that needs to be addressed, I'd refer them to the appropriate provider first.
Once I have acceptable imaging, a negative endometrial biopsy and an adequate medical history, I would then assist the patient in scheduling with one of the surgeons on my team for a consult and physical exam to determine surgery planning. Once they see our physician, a surgery date is booked. The patient would come back to see me within 30 days of surgery, and we would do a preoperative education appointment. I see them again 2 weeks after surgery for a post-op visit. We’d perform the post-of visit virtually in our practice. We would see the patient sooner if there are any other concerns that arise post-operatively.
What if the patient is not a surgical candidate? How do you as an APP assist in ongoing medical management?
Ms. Haibach: The presence of fibroids alone, without symptoms, often does not require surgical intervention. There are occasions where a patient is, for example, seen in the emergency room for abdominal pain, whereas they’ll get a CT scan of the abdomen pelvis, and a fibroid is incidentally found. At that point, they are instructed to see gynecology for follow-up. If the patient was unaware of the fibroid, has no symptoms and there's no concerning imaging features, then management with ongoing surveillance (repeat imaging and office follow up) and instructions on when to return is usually appropriate.
Depending on the symptoms, medical management typically includes hormonal suppression of menses in the form of a birth control pill or an IUD. If bleeding is the main concern, it is my goal to at least slow her bleeding, if not try to stop it. Not all women are good candidates for hormone therapy, so there is a medication option that is non-hormonal. In my role, I would start a medication plan for a patient and initiate a new medication such as hormonal suppression in the form of birth control, IUD, non-hormonal medications etc.
Typically, when I do that, I'll have the patient follow up with me in about two to three months to reassess the medication’s effectiveness. The goal of the reassessment is to determine if it is working for her life, to be sure there are no major side-effects, and just to make sure she is amenable to the plan. As part of the medical management, sometimes it is necessary to monitor blood counts for anemia to be certain that medical management is still appropriate for her.
From your experience in practicing, are you more likely to be visited by one age bracket or ethnicity over another?
Ms. Haibach: Actually, data tells us that most fibroids occur in women of reproductive age. They are also diagnosed in African American women two to three times more frequently than in white women. Fibroids are infrequently seen in premenstrual women. A relief of symptoms of the fibroids often occurs at the time of menopause, when the menstrual cyclicity seizes and steroid hormone levels decrease. My demographic is consistent with the above statistics. I tend to see women within the ages of 20’s-50’s and more often African Americans.
Was there anything else that you'd like to mention?
Ms. Haibach: Abnormal bleeding can be very stressful for women. APPs are a great place to start an abnormal bleeding or fibroid work-up. Patients should rest assure that although we cannot perform surgery, APPs can help get them in the right direction for the best care possible.
US Department of Health and Human Services, Office on Women’s Health. Uterine fibroids. (https://www.womenshealth.gov/a-z-topics/uterine-fibroids) Accessed 1/26/2022.
The American College of Obstetricians and Gynecologists. Uterine Fibroids. (https://www.acog.org/patient-resources/faqs/gynecologic-problems/uterine-fibroids) Accessed 1/26/2022.
As an Advanced Practice Provider, when and why might a patient with uterine fibroids be scheduled to visit with you?
Ms. Haibach: Typically, with the flow of how our practice runs, a patient would schedule with me as an initial visit to explore their abnormal or heavy bleeding. Oftentimes, a patient is unsure with what they have going on medically and will view APPs as a safe place to start. Other times, I will see a patient for a general wellness exam who will mention heavier menses over the years or just a change in their bleeding pattern-- longer flow, things like that.
It may stem from something that seems out of the ordinary for them or a symptom impacting their life. For example, if a patient says, “I have to run home and change my clothes,” or “I'm bleeding through my bed sheets.” Those statements prompt further evaluation. At times, patients who have already been diagnosed with fibroids, will come to see me if they have chosen medical management over surgical management of their fibroids. They continue to follow up with me to reevaluate the success of their treatment plan periodically. So, whether I start them on a plan, or a physician does, they can follow up with me to revisit their medical plan and ensure it remains appropriate.
You touched on this a bit, but can you dive deeper into exactly what you are looking for as part of that visit?
Ms. Haibach: Definitely. With an initial consult to me, the number one question that I would ask my patients first is, what is your most bothersome symptom? With this question, I'm looking to determine: is it pain that brought you to me? Is it heavy bleeding? Do you feel bulk and bloaty? Are you having issues getting pregnant? Do you have bowel or bladder issues?
The information I get from that one initial question, helps guide the remainder of my visit. If bleeding is the main concern, we would focus on getting that under control. So, we need to suppress the menses with medication options. If bulk and bloating is the main concern, for instance the patient feels like they have a pregnant-looking abdomen, typically surgical options are warranted. If the main complaint is infertility, we do have fertility specialists in our practice who remove fibroids to aid patients in achieving pregnancy.
The most important purpose of this visit is to really listen to the patient to find out how these symptoms are impacting their daily lives. From there, I can use that information to guide my treatment plan.
So, once it is determined that the patient is a good surgical candidate, what would be the next steps?
Ms. Haibach: If at the end of my visit, I determine that a patient is potentially a suitable surgical candidate, the first thing I would do is order appropriate imaging. For example, if the patient is interested in uterine preservation for future fertility, she is likely going to opt for a laparoscopic myomectomy, where fibroids would be removed, and her uterus would be left in place. In that case, she would require an MRI for fibroid mapping. If a woman has completed childbearing, then oftentimes a pelvic ultrasound would suffice, at least to start, since she'd likely elect hysterectomy if she has reached her fertility goals.
I would also perform an endometrial biopsy to rule out malignant process before going into surgery. To optimize a patient for our MIGS surgeons, I gather a thorough medical history to ensure their comorbidities are appropriately managed. For example, diabetes is under control, sleep apnea is being treated, no active infections. If there is anything else going on that needs to be addressed, I'd refer them to the appropriate provider first.
Once I have acceptable imaging, a negative endometrial biopsy and an adequate medical history, I would then assist the patient in scheduling with one of the surgeons on my team for a consult and physical exam to determine surgery planning. Once they see our physician, a surgery date is booked. The patient would come back to see me within 30 days of surgery, and we would do a preoperative education appointment. I see them again 2 weeks after surgery for a post-op visit. We’d perform the post-of visit virtually in our practice. We would see the patient sooner if there are any other concerns that arise post-operatively.
What if the patient is not a surgical candidate? How do you as an APP assist in ongoing medical management?
Ms. Haibach: The presence of fibroids alone, without symptoms, often does not require surgical intervention. There are occasions where a patient is, for example, seen in the emergency room for abdominal pain, whereas they’ll get a CT scan of the abdomen pelvis, and a fibroid is incidentally found. At that point, they are instructed to see gynecology for follow-up. If the patient was unaware of the fibroid, has no symptoms and there's no concerning imaging features, then management with ongoing surveillance (repeat imaging and office follow up) and instructions on when to return is usually appropriate.
Depending on the symptoms, medical management typically includes hormonal suppression of menses in the form of a birth control pill or an IUD. If bleeding is the main concern, it is my goal to at least slow her bleeding, if not try to stop it. Not all women are good candidates for hormone therapy, so there is a medication option that is non-hormonal. In my role, I would start a medication plan for a patient and initiate a new medication such as hormonal suppression in the form of birth control, IUD, non-hormonal medications etc.
Typically, when I do that, I'll have the patient follow up with me in about two to three months to reassess the medication’s effectiveness. The goal of the reassessment is to determine if it is working for her life, to be sure there are no major side-effects, and just to make sure she is amenable to the plan. As part of the medical management, sometimes it is necessary to monitor blood counts for anemia to be certain that medical management is still appropriate for her.
From your experience in practicing, are you more likely to be visited by one age bracket or ethnicity over another?
Ms. Haibach: Actually, data tells us that most fibroids occur in women of reproductive age. They are also diagnosed in African American women two to three times more frequently than in white women. Fibroids are infrequently seen in premenstrual women. A relief of symptoms of the fibroids often occurs at the time of menopause, when the menstrual cyclicity seizes and steroid hormone levels decrease. My demographic is consistent with the above statistics. I tend to see women within the ages of 20’s-50’s and more often African Americans.
Was there anything else that you'd like to mention?
Ms. Haibach: Abnormal bleeding can be very stressful for women. APPs are a great place to start an abnormal bleeding or fibroid work-up. Patients should rest assure that although we cannot perform surgery, APPs can help get them in the right direction for the best care possible.
As an Advanced Practice Provider, when and why might a patient with uterine fibroids be scheduled to visit with you?
Ms. Haibach: Typically, with the flow of how our practice runs, a patient would schedule with me as an initial visit to explore their abnormal or heavy bleeding. Oftentimes, a patient is unsure with what they have going on medically and will view APPs as a safe place to start. Other times, I will see a patient for a general wellness exam who will mention heavier menses over the years or just a change in their bleeding pattern-- longer flow, things like that.
It may stem from something that seems out of the ordinary for them or a symptom impacting their life. For example, if a patient says, “I have to run home and change my clothes,” or “I'm bleeding through my bed sheets.” Those statements prompt further evaluation. At times, patients who have already been diagnosed with fibroids, will come to see me if they have chosen medical management over surgical management of their fibroids. They continue to follow up with me to reevaluate the success of their treatment plan periodically. So, whether I start them on a plan, or a physician does, they can follow up with me to revisit their medical plan and ensure it remains appropriate.
You touched on this a bit, but can you dive deeper into exactly what you are looking for as part of that visit?
Ms. Haibach: Definitely. With an initial consult to me, the number one question that I would ask my patients first is, what is your most bothersome symptom? With this question, I'm looking to determine: is it pain that brought you to me? Is it heavy bleeding? Do you feel bulk and bloaty? Are you having issues getting pregnant? Do you have bowel or bladder issues?
The information I get from that one initial question, helps guide the remainder of my visit. If bleeding is the main concern, we would focus on getting that under control. So, we need to suppress the menses with medication options. If bulk and bloating is the main concern, for instance the patient feels like they have a pregnant-looking abdomen, typically surgical options are warranted. If the main complaint is infertility, we do have fertility specialists in our practice who remove fibroids to aid patients in achieving pregnancy.
The most important purpose of this visit is to really listen to the patient to find out how these symptoms are impacting their daily lives. From there, I can use that information to guide my treatment plan.
So, once it is determined that the patient is a good surgical candidate, what would be the next steps?
Ms. Haibach: If at the end of my visit, I determine that a patient is potentially a suitable surgical candidate, the first thing I would do is order appropriate imaging. For example, if the patient is interested in uterine preservation for future fertility, she is likely going to opt for a laparoscopic myomectomy, where fibroids would be removed, and her uterus would be left in place. In that case, she would require an MRI for fibroid mapping. If a woman has completed childbearing, then oftentimes a pelvic ultrasound would suffice, at least to start, since she'd likely elect hysterectomy if she has reached her fertility goals.
I would also perform an endometrial biopsy to rule out malignant process before going into surgery. To optimize a patient for our MIGS surgeons, I gather a thorough medical history to ensure their comorbidities are appropriately managed. For example, diabetes is under control, sleep apnea is being treated, no active infections. If there is anything else going on that needs to be addressed, I'd refer them to the appropriate provider first.
Once I have acceptable imaging, a negative endometrial biopsy and an adequate medical history, I would then assist the patient in scheduling with one of the surgeons on my team for a consult and physical exam to determine surgery planning. Once they see our physician, a surgery date is booked. The patient would come back to see me within 30 days of surgery, and we would do a preoperative education appointment. I see them again 2 weeks after surgery for a post-op visit. We’d perform the post-of visit virtually in our practice. We would see the patient sooner if there are any other concerns that arise post-operatively.
What if the patient is not a surgical candidate? How do you as an APP assist in ongoing medical management?
Ms. Haibach: The presence of fibroids alone, without symptoms, often does not require surgical intervention. There are occasions where a patient is, for example, seen in the emergency room for abdominal pain, whereas they’ll get a CT scan of the abdomen pelvis, and a fibroid is incidentally found. At that point, they are instructed to see gynecology for follow-up. If the patient was unaware of the fibroid, has no symptoms and there's no concerning imaging features, then management with ongoing surveillance (repeat imaging and office follow up) and instructions on when to return is usually appropriate.
Depending on the symptoms, medical management typically includes hormonal suppression of menses in the form of a birth control pill or an IUD. If bleeding is the main concern, it is my goal to at least slow her bleeding, if not try to stop it. Not all women are good candidates for hormone therapy, so there is a medication option that is non-hormonal. In my role, I would start a medication plan for a patient and initiate a new medication such as hormonal suppression in the form of birth control, IUD, non-hormonal medications etc.
Typically, when I do that, I'll have the patient follow up with me in about two to three months to reassess the medication’s effectiveness. The goal of the reassessment is to determine if it is working for her life, to be sure there are no major side-effects, and just to make sure she is amenable to the plan. As part of the medical management, sometimes it is necessary to monitor blood counts for anemia to be certain that medical management is still appropriate for her.
From your experience in practicing, are you more likely to be visited by one age bracket or ethnicity over another?
Ms. Haibach: Actually, data tells us that most fibroids occur in women of reproductive age. They are also diagnosed in African American women two to three times more frequently than in white women. Fibroids are infrequently seen in premenstrual women. A relief of symptoms of the fibroids often occurs at the time of menopause, when the menstrual cyclicity seizes and steroid hormone levels decrease. My demographic is consistent with the above statistics. I tend to see women within the ages of 20’s-50’s and more often African Americans.
Was there anything else that you'd like to mention?
Ms. Haibach: Abnormal bleeding can be very stressful for women. APPs are a great place to start an abnormal bleeding or fibroid work-up. Patients should rest assure that although we cannot perform surgery, APPs can help get them in the right direction for the best care possible.
US Department of Health and Human Services, Office on Women’s Health. Uterine fibroids. (https://www.womenshealth.gov/a-z-topics/uterine-fibroids) Accessed 1/26/2022.
The American College of Obstetricians and Gynecologists. Uterine Fibroids. (https://www.acog.org/patient-resources/faqs/gynecologic-problems/uterine-fibroids) Accessed 1/26/2022.
US Department of Health and Human Services, Office on Women’s Health. Uterine fibroids. (https://www.womenshealth.gov/a-z-topics/uterine-fibroids) Accessed 1/26/2022.
The American College of Obstetricians and Gynecologists. Uterine Fibroids. (https://www.acog.org/patient-resources/faqs/gynecologic-problems/uterine-fibroids) Accessed 1/26/2022.
Fewer diabetes complications with NOACs in patients with AFib
The new research, which was published in Annals of Internal Medicine, found that taking non–vitamin K oral anticoagulants was associated with reduced diabetes complications and lower mortality vs. taking warfarin in the group examined.
In their paper, the researchers present the outcomes of a retrospective cohort study involving 30,209 patients with atrial fibrillation and diabetes. Of these, 19,909 were treated with non–vitamin K oral anticoagulants (NOACs) – dabigatran, rivaroxaban, apixaban, or edoxaban – and 10,300 were treated with warfarin.
Dr. Huei-Kai Huang from the Hualien (Taiwan) Tzu Chi Hospital and coauthors wrote that, while diabetes mellitus is an important risk factor for stroke, there’s not yet a good understanding of the effect of different oral anticoagulants on the risk for diabetes-related complications in patients with atrial fibrillation and diabetes.
“Recent evidence has suggested that NOAC and warfarin may have different effects on glycemic control through the vitamin K–related mechanisms,” coauthor Yu-Kang Tu, PhD, from the College of Public Health at the National Taiwan University in Taipei said in an interview. “It was therefore natural to further evaluate whether NOAC could help decrease various diabetes-related complications, compared with warfarin.”
Hazards with NOACS vs. warfarin
The researchers found that patients treated with NOACs had a 16% lower hazard of macrovascular complications – a composite of coronary artery disease, stroke, and peripheral vascular disease (95% confidence interval, 0.78-0.91; P < .001) – and a 21% lower hazard of microvascular complications including dialysis and lower-extremity amputations (95% CI, 0.73-0.85; P < .001).
NOAC therapy was also associated a 22% lower hazard of death (95% CI, 0.75-0.82; P < .001) and a 9% lower hazard for glycemic emergency (95% CI, 0.83-0.99; P = .043), which the authors defined as a composite of diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
In particular, patients treated with NOACs showed significantly lower hazards for coronary artery disease, stroke, dialysis, amputation of lower extremities, and death from cardiovascular and noncardiovascular causes, compared with warfarin users.
The study also found that patients on higher volumes of NOAC medication had greater reductions in mortality and diabetes complications.
“Although our main findings can be explained by the potential differences in underlying mechanisms of action between NOAC and warfarin, we were still surprised with the significantly lower risks of retinopathy, neuropathy, and hypoglycemia in patients taking NOAC with high medication possession ratio,” Dr. Tu said.
Study provides more diabetes-specific outcomes data
Commenting on the findings, Dr. Peter Rossing, head of complications research at the Steno Diabetes Center in Copenhagen said there has long been discussion about whether the newer and more expensive NOACs offer greater benefits to patient with diabetes – beyond stroke prevention – compared with the older and cheaper warfarin. As such, this study was important in providing more diabetes-specific outcomes data and in a large population.
“The effect size they find is certainly meaningful and relevant and should support decision-making,” Dr. Rossing noted in an interview. The finding of reduced risk of amputation and mortality “fits in line with theory that maybe if you block vitamin K, you get calcification, you get vascular damage that leads to failure of the kidney and leads to limb amputations, and that is potentially prevented or not developed when you give the NOACs.”
Dr. John Camm, professor of clinical cardiology at St George’s University of London, said the findings of the benefits of NOACs in this patient group ,were confirmation of earlier, smaller studies, and were important not just for patients with atrial fibrillation and diabetes, but also those prone to diabetes.
“We know from previous studies from the same database, and also from Korea, [for example], that patients who are treated with NOACs as opposed to warfarin develop less diabetes,” he explained.
Dr. Camm said many guidelines around the world now suggest NOACs, and, in some cases, even advise against using vitamin K antagonists as a first option, except in certain situations, such as when patients have rheumatic heart disease, mild to moderate mitral stenosis in rheumatic disease, or prosthetic heart valves.
The researchers applied two methods to account for covariates that may have influenced whether patients received one class of treatment or the other. These achieved ‘appropriate balance’ of baseline characteristics such as comorbidities and baseline medication use for diabetes and other conditions, Dr. Tu and colleagues wrote.
The benefits of NOACs were less evident in younger patients, and the reductions in mortality and diabetes complications associated with NOACs did not reach statistical significance in those aged under 65 years. Regarding this, Dr. Camm noted that there was a debate as to whether patients under 65 years with atrial fibrillation and diabetes should be put on an anticoagulant.
The study was funded by Hualien Tzu Chi Hospital. No conflicts of interest were declared.
The new research, which was published in Annals of Internal Medicine, found that taking non–vitamin K oral anticoagulants was associated with reduced diabetes complications and lower mortality vs. taking warfarin in the group examined.
In their paper, the researchers present the outcomes of a retrospective cohort study involving 30,209 patients with atrial fibrillation and diabetes. Of these, 19,909 were treated with non–vitamin K oral anticoagulants (NOACs) – dabigatran, rivaroxaban, apixaban, or edoxaban – and 10,300 were treated with warfarin.
Dr. Huei-Kai Huang from the Hualien (Taiwan) Tzu Chi Hospital and coauthors wrote that, while diabetes mellitus is an important risk factor for stroke, there’s not yet a good understanding of the effect of different oral anticoagulants on the risk for diabetes-related complications in patients with atrial fibrillation and diabetes.
“Recent evidence has suggested that NOAC and warfarin may have different effects on glycemic control through the vitamin K–related mechanisms,” coauthor Yu-Kang Tu, PhD, from the College of Public Health at the National Taiwan University in Taipei said in an interview. “It was therefore natural to further evaluate whether NOAC could help decrease various diabetes-related complications, compared with warfarin.”
Hazards with NOACS vs. warfarin
The researchers found that patients treated with NOACs had a 16% lower hazard of macrovascular complications – a composite of coronary artery disease, stroke, and peripheral vascular disease (95% confidence interval, 0.78-0.91; P < .001) – and a 21% lower hazard of microvascular complications including dialysis and lower-extremity amputations (95% CI, 0.73-0.85; P < .001).
NOAC therapy was also associated a 22% lower hazard of death (95% CI, 0.75-0.82; P < .001) and a 9% lower hazard for glycemic emergency (95% CI, 0.83-0.99; P = .043), which the authors defined as a composite of diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
In particular, patients treated with NOACs showed significantly lower hazards for coronary artery disease, stroke, dialysis, amputation of lower extremities, and death from cardiovascular and noncardiovascular causes, compared with warfarin users.
The study also found that patients on higher volumes of NOAC medication had greater reductions in mortality and diabetes complications.
“Although our main findings can be explained by the potential differences in underlying mechanisms of action between NOAC and warfarin, we were still surprised with the significantly lower risks of retinopathy, neuropathy, and hypoglycemia in patients taking NOAC with high medication possession ratio,” Dr. Tu said.
Study provides more diabetes-specific outcomes data
Commenting on the findings, Dr. Peter Rossing, head of complications research at the Steno Diabetes Center in Copenhagen said there has long been discussion about whether the newer and more expensive NOACs offer greater benefits to patient with diabetes – beyond stroke prevention – compared with the older and cheaper warfarin. As such, this study was important in providing more diabetes-specific outcomes data and in a large population.
“The effect size they find is certainly meaningful and relevant and should support decision-making,” Dr. Rossing noted in an interview. The finding of reduced risk of amputation and mortality “fits in line with theory that maybe if you block vitamin K, you get calcification, you get vascular damage that leads to failure of the kidney and leads to limb amputations, and that is potentially prevented or not developed when you give the NOACs.”
Dr. John Camm, professor of clinical cardiology at St George’s University of London, said the findings of the benefits of NOACs in this patient group ,were confirmation of earlier, smaller studies, and were important not just for patients with atrial fibrillation and diabetes, but also those prone to diabetes.
“We know from previous studies from the same database, and also from Korea, [for example], that patients who are treated with NOACs as opposed to warfarin develop less diabetes,” he explained.
Dr. Camm said many guidelines around the world now suggest NOACs, and, in some cases, even advise against using vitamin K antagonists as a first option, except in certain situations, such as when patients have rheumatic heart disease, mild to moderate mitral stenosis in rheumatic disease, or prosthetic heart valves.
The researchers applied two methods to account for covariates that may have influenced whether patients received one class of treatment or the other. These achieved ‘appropriate balance’ of baseline characteristics such as comorbidities and baseline medication use for diabetes and other conditions, Dr. Tu and colleagues wrote.
The benefits of NOACs were less evident in younger patients, and the reductions in mortality and diabetes complications associated with NOACs did not reach statistical significance in those aged under 65 years. Regarding this, Dr. Camm noted that there was a debate as to whether patients under 65 years with atrial fibrillation and diabetes should be put on an anticoagulant.
The study was funded by Hualien Tzu Chi Hospital. No conflicts of interest were declared.
The new research, which was published in Annals of Internal Medicine, found that taking non–vitamin K oral anticoagulants was associated with reduced diabetes complications and lower mortality vs. taking warfarin in the group examined.
In their paper, the researchers present the outcomes of a retrospective cohort study involving 30,209 patients with atrial fibrillation and diabetes. Of these, 19,909 were treated with non–vitamin K oral anticoagulants (NOACs) – dabigatran, rivaroxaban, apixaban, or edoxaban – and 10,300 were treated with warfarin.
Dr. Huei-Kai Huang from the Hualien (Taiwan) Tzu Chi Hospital and coauthors wrote that, while diabetes mellitus is an important risk factor for stroke, there’s not yet a good understanding of the effect of different oral anticoagulants on the risk for diabetes-related complications in patients with atrial fibrillation and diabetes.
“Recent evidence has suggested that NOAC and warfarin may have different effects on glycemic control through the vitamin K–related mechanisms,” coauthor Yu-Kang Tu, PhD, from the College of Public Health at the National Taiwan University in Taipei said in an interview. “It was therefore natural to further evaluate whether NOAC could help decrease various diabetes-related complications, compared with warfarin.”
Hazards with NOACS vs. warfarin
The researchers found that patients treated with NOACs had a 16% lower hazard of macrovascular complications – a composite of coronary artery disease, stroke, and peripheral vascular disease (95% confidence interval, 0.78-0.91; P < .001) – and a 21% lower hazard of microvascular complications including dialysis and lower-extremity amputations (95% CI, 0.73-0.85; P < .001).
NOAC therapy was also associated a 22% lower hazard of death (95% CI, 0.75-0.82; P < .001) and a 9% lower hazard for glycemic emergency (95% CI, 0.83-0.99; P = .043), which the authors defined as a composite of diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia.
In particular, patients treated with NOACs showed significantly lower hazards for coronary artery disease, stroke, dialysis, amputation of lower extremities, and death from cardiovascular and noncardiovascular causes, compared with warfarin users.
The study also found that patients on higher volumes of NOAC medication had greater reductions in mortality and diabetes complications.
“Although our main findings can be explained by the potential differences in underlying mechanisms of action between NOAC and warfarin, we were still surprised with the significantly lower risks of retinopathy, neuropathy, and hypoglycemia in patients taking NOAC with high medication possession ratio,” Dr. Tu said.
Study provides more diabetes-specific outcomes data
Commenting on the findings, Dr. Peter Rossing, head of complications research at the Steno Diabetes Center in Copenhagen said there has long been discussion about whether the newer and more expensive NOACs offer greater benefits to patient with diabetes – beyond stroke prevention – compared with the older and cheaper warfarin. As such, this study was important in providing more diabetes-specific outcomes data and in a large population.
“The effect size they find is certainly meaningful and relevant and should support decision-making,” Dr. Rossing noted in an interview. The finding of reduced risk of amputation and mortality “fits in line with theory that maybe if you block vitamin K, you get calcification, you get vascular damage that leads to failure of the kidney and leads to limb amputations, and that is potentially prevented or not developed when you give the NOACs.”
Dr. John Camm, professor of clinical cardiology at St George’s University of London, said the findings of the benefits of NOACs in this patient group ,were confirmation of earlier, smaller studies, and were important not just for patients with atrial fibrillation and diabetes, but also those prone to diabetes.
“We know from previous studies from the same database, and also from Korea, [for example], that patients who are treated with NOACs as opposed to warfarin develop less diabetes,” he explained.
Dr. Camm said many guidelines around the world now suggest NOACs, and, in some cases, even advise against using vitamin K antagonists as a first option, except in certain situations, such as when patients have rheumatic heart disease, mild to moderate mitral stenosis in rheumatic disease, or prosthetic heart valves.
The researchers applied two methods to account for covariates that may have influenced whether patients received one class of treatment or the other. These achieved ‘appropriate balance’ of baseline characteristics such as comorbidities and baseline medication use for diabetes and other conditions, Dr. Tu and colleagues wrote.
The benefits of NOACs were less evident in younger patients, and the reductions in mortality and diabetes complications associated with NOACs did not reach statistical significance in those aged under 65 years. Regarding this, Dr. Camm noted that there was a debate as to whether patients under 65 years with atrial fibrillation and diabetes should be put on an anticoagulant.
The study was funded by Hualien Tzu Chi Hospital. No conflicts of interest were declared.
FROM ANNALS OF INTERNAL MEDICINE
Organ transplantation: Unvaccinated need not apply
I agree with most advice given by the affable TV character Ted Lasso. “Every choice is a chance,” he said. Pandemic-era physicians must now consider whether a politically motivated choice to decline COVID-19 vaccination should negatively affect the chance to receive an organ donation.
And in confronting these choices, we have a chance to educate the public on the complexities of the organ allocation process.
A well-informed patient’s personal choice should be honored, even if clinicians disagree, if it does not affect the well-being of others. For example, I once had a patient in acute leukemic crisis who declined blood products because she was a Jehovah’s Witness. She died. Her choice affected her longevity only.
Compare that decision with awarding an organ to an individual who has declined readily available protection of that organ. Weigh that choice against the fact that said protection is against an infectious disease that has killed over 5.5 million worldwide.
Some institutions stand strong, others hedge their bets
Admirably, Loyola University Health System understands that difference. They published a firm stand on transplant candidacy and COVID-19 vaccination status in the Journal of Heart and Lung Transplant. Daniel Dilling, MD, medical director of the lung transplantation program , and Mark Kuczewski, PhD, a professor of medical ethics at Loyola University Chicago, Maywood, Ill., wrote that: “We believe that requiring vaccination against COVID-19 should not be controversial when we focus strictly on established frameworks and practices surrounding eligibility for wait-listing to receive a solid organ transplant.”
The Cleveland Clinic apparently agrees. In October 2021, they denied a liver transplant to Michelle Vitullo of Ohio, whose daughter had been deemed “a perfect match.” Her daughter, also unvaccinated, stated: “Being denied for a nonmedical reason for someone’s beliefs that are different to yours, I mean that’s not how that should be.”
But vaccination status is a medical reason, given well-established data regarding increased mortality among the immunosuppressed. Ms. Vitullo then said: “We are trying to get to UPMC [University of Pittsburgh Medical Center] as they don’t require a vaccination.”
The public information page on transplant candidacy from UPMC reads (my italics): It is recommended that all transplant candidates, transplant recipients, and their household members receive COVID-19 vaccination when the vaccine is available to them. It is preferred that transplant candidates are vaccinated more than 2 weeks before transplantation.
I reached out to UPMC for clarification and was told by email that “we do not have a policy regarding COVID-19 vaccination requirement for current transplant candidates.” Houston Methodist shares the same agnostic stance.
Compare these opinions with Brigham and Women’s Hospital, where the requirements are resolute: “Like most other transplant programs across the country, the COVID-19 vaccine is one of several vaccines and lifestyle behaviors that are required for patients awaiting solid organ transplant.”
They add that “transplant candidates must also receive the seasonal influenza and hepatitis B vaccines, follow other healthy behaviors, and demonstrate they can commit to taking the required medications following transplant.”
In January 2022, Brigham and Women’s Hospital declared 31-year-old D.J. Ferguson ineligible for a heart transplant because he declined to be vaccinated against COVID-19. According to the New York Post and ABC News, his physicians resorted to left ventricular assist device support. His mother, Tracy Ferguson, is quoted as saying: “He’s not an antivaxxer. He has all of his vaccines.” I’ll just leave that right there.
Unfortunately, Michelle Vitullo’s obituary was published in December 2021. Regardless of whether she received her liver transplant, the outcome is tragic, and whatever you think of this family’s battle playing out in the glare of the national spotlight, their loss is no less devastating.
The directed-donation aspect of this case poses an interesting question. A news anchor asked the mother and daughter: “If you both accept the risks, why doesn’t the hospital just let you try?” The answers are obvious to us clinicians. Performing a transplantation in an unvaccinated patient could lead to their early death if they became infected because of their immunocompromised state, would open the door for transplantation of any patient who is unvaccinated for anything, including influenza and hepatitis B, which could result in the preventable waste of organs, and puts other vulnerable hospitalized patients at risk during the initial transplant stay and follow-up.
That’s not to mention the potential legal suit. Never has a consent form dissuaded any party from lodging an accusation of wrongful death or medical malpractice. In the face of strong data on higher mortality in unvaccinated, immunocompromised patients, a good lawyer could charge that the institution and transplant surgeons should have known better, regardless of the donor and recipient’s willingness to accept the risks.
The Vitullo and Ferguson cases are among many similar dilemmas surrounding transplant candidacy across the United States.
University of Virginia Health in Charlottesville denied 42-year-old Shamgar Connors a kidney transplant because he is unvaccinated, despite a previous COVID-19 infection. In October 2021, Leilani Lutali of Colorado was denied a kidney by UCHealth because she declined vaccination.
As Ted Lasso says: “There’s a bunch of crazy stuff on Twitter.”
Predictably, social media is full of public outcry. “Some cold-hearted people on here” tweeted one. “What if it was one of your loved ones who needed a transplant?” Another tweeted the Hippocratic oath with the comment that “They all swore under this noble ‘oat’, but I guess it’s been forgotten.” (This was followed with a photo of a box of Quaker Oats in a failed attempt at humor.) These discussions among the Twitterati highlight the depths of misunderstanding on organ transplantation.
To be fair, unless you have been personally involved in the decision-making process for transplant candidacy, there is little opportunity to be educated. I explain to my anxious patients and their families that a donor organ is like a fumbled football. There may be well over 100 patients at all levels of transplant status in many geographic locations diving for that same organ.
The transplant team is tasked with finding the best match, determining who is the sickest, assessing time for transport of that organ, and, above all, who will be the best steward of that organ.
Take heart transplantation, for instance. Approximately 3,500 patients in the United States are awaiting one each year. Instead of facing an almost certain death within 5 years, a transplant recipient has a chance at a median survival of 12-13 years. The cost of a heart transplant is approximately $1.38 million, according to Milliman, a consulting firm. This is “an incredibly resource intensive procedure,” including expenditures for transportation, antirejection medication, office visits, physician fees, ICU stays, rejection surveillance, and acute rejection therapies.
Transplant denial is nothing new
People get turned down for organ transplants all the time. My patient with end-stage dilated cardiomyopathy was denied a heart transplant when it was discovered that he had scores of outstanding parking tickets. This was seen as a surrogate for an inability to afford his antirejection medication.
Another patient swore that her positive cotinine levels were caused by endless hours at the bingo hall where second-hand smoke swirled. She was also denied. Many potential candidates who are in acute decline hold precariously to newfound sobriety. They are denied. A patient’s boyfriend told the transplant team that he couldn’t be relied upon to drive her to her appointments. She was denied.
Many people who engage in antisocial behaviors have no idea that these actions may result in the denial of an organ transplant should their future selves need one. These are hard lines, but everyone should agree that the odds of survival are heavily in favor of the consistently adherent.
We should take this opportunity to educate the public on how complicated obtaining an organ transplant can be. More than 6,000 people die each year waiting for an organ because of the supply-and-demand disparities in the transplantation arena. I’m willing to bet that many of the loudest protesters in favor of unvaccinated transplant recipients have not signed the organ donor box on the back of their driver’s license. This conversation is an opportunity to change that and remind people that organ donation may be their only opportunity to save a fellow human’s life.
Again, to quote Ted Lasso: “If you care about someone and you got a little love in your heart, there ain’t nothing you can’t get through together.” That philosophy should apply to the tasks of selecting the best organ donors as well as the best organ recipients.
And every organ should go to the one who will honor their donor and their donor’s family by taking the best care of that ultimate gift of life, including being vaccinated against COVID-19.
Dr. Walton-Shirley is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
I agree with most advice given by the affable TV character Ted Lasso. “Every choice is a chance,” he said. Pandemic-era physicians must now consider whether a politically motivated choice to decline COVID-19 vaccination should negatively affect the chance to receive an organ donation.
And in confronting these choices, we have a chance to educate the public on the complexities of the organ allocation process.
A well-informed patient’s personal choice should be honored, even if clinicians disagree, if it does not affect the well-being of others. For example, I once had a patient in acute leukemic crisis who declined blood products because she was a Jehovah’s Witness. She died. Her choice affected her longevity only.
Compare that decision with awarding an organ to an individual who has declined readily available protection of that organ. Weigh that choice against the fact that said protection is against an infectious disease that has killed over 5.5 million worldwide.
Some institutions stand strong, others hedge their bets
Admirably, Loyola University Health System understands that difference. They published a firm stand on transplant candidacy and COVID-19 vaccination status in the Journal of Heart and Lung Transplant. Daniel Dilling, MD, medical director of the lung transplantation program , and Mark Kuczewski, PhD, a professor of medical ethics at Loyola University Chicago, Maywood, Ill., wrote that: “We believe that requiring vaccination against COVID-19 should not be controversial when we focus strictly on established frameworks and practices surrounding eligibility for wait-listing to receive a solid organ transplant.”
The Cleveland Clinic apparently agrees. In October 2021, they denied a liver transplant to Michelle Vitullo of Ohio, whose daughter had been deemed “a perfect match.” Her daughter, also unvaccinated, stated: “Being denied for a nonmedical reason for someone’s beliefs that are different to yours, I mean that’s not how that should be.”
But vaccination status is a medical reason, given well-established data regarding increased mortality among the immunosuppressed. Ms. Vitullo then said: “We are trying to get to UPMC [University of Pittsburgh Medical Center] as they don’t require a vaccination.”
The public information page on transplant candidacy from UPMC reads (my italics): It is recommended that all transplant candidates, transplant recipients, and their household members receive COVID-19 vaccination when the vaccine is available to them. It is preferred that transplant candidates are vaccinated more than 2 weeks before transplantation.
I reached out to UPMC for clarification and was told by email that “we do not have a policy regarding COVID-19 vaccination requirement for current transplant candidates.” Houston Methodist shares the same agnostic stance.
Compare these opinions with Brigham and Women’s Hospital, where the requirements are resolute: “Like most other transplant programs across the country, the COVID-19 vaccine is one of several vaccines and lifestyle behaviors that are required for patients awaiting solid organ transplant.”
They add that “transplant candidates must also receive the seasonal influenza and hepatitis B vaccines, follow other healthy behaviors, and demonstrate they can commit to taking the required medications following transplant.”
In January 2022, Brigham and Women’s Hospital declared 31-year-old D.J. Ferguson ineligible for a heart transplant because he declined to be vaccinated against COVID-19. According to the New York Post and ABC News, his physicians resorted to left ventricular assist device support. His mother, Tracy Ferguson, is quoted as saying: “He’s not an antivaxxer. He has all of his vaccines.” I’ll just leave that right there.
Unfortunately, Michelle Vitullo’s obituary was published in December 2021. Regardless of whether she received her liver transplant, the outcome is tragic, and whatever you think of this family’s battle playing out in the glare of the national spotlight, their loss is no less devastating.
The directed-donation aspect of this case poses an interesting question. A news anchor asked the mother and daughter: “If you both accept the risks, why doesn’t the hospital just let you try?” The answers are obvious to us clinicians. Performing a transplantation in an unvaccinated patient could lead to their early death if they became infected because of their immunocompromised state, would open the door for transplantation of any patient who is unvaccinated for anything, including influenza and hepatitis B, which could result in the preventable waste of organs, and puts other vulnerable hospitalized patients at risk during the initial transplant stay and follow-up.
That’s not to mention the potential legal suit. Never has a consent form dissuaded any party from lodging an accusation of wrongful death or medical malpractice. In the face of strong data on higher mortality in unvaccinated, immunocompromised patients, a good lawyer could charge that the institution and transplant surgeons should have known better, regardless of the donor and recipient’s willingness to accept the risks.
The Vitullo and Ferguson cases are among many similar dilemmas surrounding transplant candidacy across the United States.
University of Virginia Health in Charlottesville denied 42-year-old Shamgar Connors a kidney transplant because he is unvaccinated, despite a previous COVID-19 infection. In October 2021, Leilani Lutali of Colorado was denied a kidney by UCHealth because she declined vaccination.
As Ted Lasso says: “There’s a bunch of crazy stuff on Twitter.”
Predictably, social media is full of public outcry. “Some cold-hearted people on here” tweeted one. “What if it was one of your loved ones who needed a transplant?” Another tweeted the Hippocratic oath with the comment that “They all swore under this noble ‘oat’, but I guess it’s been forgotten.” (This was followed with a photo of a box of Quaker Oats in a failed attempt at humor.) These discussions among the Twitterati highlight the depths of misunderstanding on organ transplantation.
To be fair, unless you have been personally involved in the decision-making process for transplant candidacy, there is little opportunity to be educated. I explain to my anxious patients and their families that a donor organ is like a fumbled football. There may be well over 100 patients at all levels of transplant status in many geographic locations diving for that same organ.
The transplant team is tasked with finding the best match, determining who is the sickest, assessing time for transport of that organ, and, above all, who will be the best steward of that organ.
Take heart transplantation, for instance. Approximately 3,500 patients in the United States are awaiting one each year. Instead of facing an almost certain death within 5 years, a transplant recipient has a chance at a median survival of 12-13 years. The cost of a heart transplant is approximately $1.38 million, according to Milliman, a consulting firm. This is “an incredibly resource intensive procedure,” including expenditures for transportation, antirejection medication, office visits, physician fees, ICU stays, rejection surveillance, and acute rejection therapies.
Transplant denial is nothing new
People get turned down for organ transplants all the time. My patient with end-stage dilated cardiomyopathy was denied a heart transplant when it was discovered that he had scores of outstanding parking tickets. This was seen as a surrogate for an inability to afford his antirejection medication.
Another patient swore that her positive cotinine levels were caused by endless hours at the bingo hall where second-hand smoke swirled. She was also denied. Many potential candidates who are in acute decline hold precariously to newfound sobriety. They are denied. A patient’s boyfriend told the transplant team that he couldn’t be relied upon to drive her to her appointments. She was denied.
Many people who engage in antisocial behaviors have no idea that these actions may result in the denial of an organ transplant should their future selves need one. These are hard lines, but everyone should agree that the odds of survival are heavily in favor of the consistently adherent.
We should take this opportunity to educate the public on how complicated obtaining an organ transplant can be. More than 6,000 people die each year waiting for an organ because of the supply-and-demand disparities in the transplantation arena. I’m willing to bet that many of the loudest protesters in favor of unvaccinated transplant recipients have not signed the organ donor box on the back of their driver’s license. This conversation is an opportunity to change that and remind people that organ donation may be their only opportunity to save a fellow human’s life.
Again, to quote Ted Lasso: “If you care about someone and you got a little love in your heart, there ain’t nothing you can’t get through together.” That philosophy should apply to the tasks of selecting the best organ donors as well as the best organ recipients.
And every organ should go to the one who will honor their donor and their donor’s family by taking the best care of that ultimate gift of life, including being vaccinated against COVID-19.
Dr. Walton-Shirley is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
I agree with most advice given by the affable TV character Ted Lasso. “Every choice is a chance,” he said. Pandemic-era physicians must now consider whether a politically motivated choice to decline COVID-19 vaccination should negatively affect the chance to receive an organ donation.
And in confronting these choices, we have a chance to educate the public on the complexities of the organ allocation process.
A well-informed patient’s personal choice should be honored, even if clinicians disagree, if it does not affect the well-being of others. For example, I once had a patient in acute leukemic crisis who declined blood products because she was a Jehovah’s Witness. She died. Her choice affected her longevity only.
Compare that decision with awarding an organ to an individual who has declined readily available protection of that organ. Weigh that choice against the fact that said protection is against an infectious disease that has killed over 5.5 million worldwide.
Some institutions stand strong, others hedge their bets
Admirably, Loyola University Health System understands that difference. They published a firm stand on transplant candidacy and COVID-19 vaccination status in the Journal of Heart and Lung Transplant. Daniel Dilling, MD, medical director of the lung transplantation program , and Mark Kuczewski, PhD, a professor of medical ethics at Loyola University Chicago, Maywood, Ill., wrote that: “We believe that requiring vaccination against COVID-19 should not be controversial when we focus strictly on established frameworks and practices surrounding eligibility for wait-listing to receive a solid organ transplant.”
The Cleveland Clinic apparently agrees. In October 2021, they denied a liver transplant to Michelle Vitullo of Ohio, whose daughter had been deemed “a perfect match.” Her daughter, also unvaccinated, stated: “Being denied for a nonmedical reason for someone’s beliefs that are different to yours, I mean that’s not how that should be.”
But vaccination status is a medical reason, given well-established data regarding increased mortality among the immunosuppressed. Ms. Vitullo then said: “We are trying to get to UPMC [University of Pittsburgh Medical Center] as they don’t require a vaccination.”
The public information page on transplant candidacy from UPMC reads (my italics): It is recommended that all transplant candidates, transplant recipients, and their household members receive COVID-19 vaccination when the vaccine is available to them. It is preferred that transplant candidates are vaccinated more than 2 weeks before transplantation.
I reached out to UPMC for clarification and was told by email that “we do not have a policy regarding COVID-19 vaccination requirement for current transplant candidates.” Houston Methodist shares the same agnostic stance.
Compare these opinions with Brigham and Women’s Hospital, where the requirements are resolute: “Like most other transplant programs across the country, the COVID-19 vaccine is one of several vaccines and lifestyle behaviors that are required for patients awaiting solid organ transplant.”
They add that “transplant candidates must also receive the seasonal influenza and hepatitis B vaccines, follow other healthy behaviors, and demonstrate they can commit to taking the required medications following transplant.”
In January 2022, Brigham and Women’s Hospital declared 31-year-old D.J. Ferguson ineligible for a heart transplant because he declined to be vaccinated against COVID-19. According to the New York Post and ABC News, his physicians resorted to left ventricular assist device support. His mother, Tracy Ferguson, is quoted as saying: “He’s not an antivaxxer. He has all of his vaccines.” I’ll just leave that right there.
Unfortunately, Michelle Vitullo’s obituary was published in December 2021. Regardless of whether she received her liver transplant, the outcome is tragic, and whatever you think of this family’s battle playing out in the glare of the national spotlight, their loss is no less devastating.
The directed-donation aspect of this case poses an interesting question. A news anchor asked the mother and daughter: “If you both accept the risks, why doesn’t the hospital just let you try?” The answers are obvious to us clinicians. Performing a transplantation in an unvaccinated patient could lead to their early death if they became infected because of their immunocompromised state, would open the door for transplantation of any patient who is unvaccinated for anything, including influenza and hepatitis B, which could result in the preventable waste of organs, and puts other vulnerable hospitalized patients at risk during the initial transplant stay and follow-up.
That’s not to mention the potential legal suit. Never has a consent form dissuaded any party from lodging an accusation of wrongful death or medical malpractice. In the face of strong data on higher mortality in unvaccinated, immunocompromised patients, a good lawyer could charge that the institution and transplant surgeons should have known better, regardless of the donor and recipient’s willingness to accept the risks.
The Vitullo and Ferguson cases are among many similar dilemmas surrounding transplant candidacy across the United States.
University of Virginia Health in Charlottesville denied 42-year-old Shamgar Connors a kidney transplant because he is unvaccinated, despite a previous COVID-19 infection. In October 2021, Leilani Lutali of Colorado was denied a kidney by UCHealth because she declined vaccination.
As Ted Lasso says: “There’s a bunch of crazy stuff on Twitter.”
Predictably, social media is full of public outcry. “Some cold-hearted people on here” tweeted one. “What if it was one of your loved ones who needed a transplant?” Another tweeted the Hippocratic oath with the comment that “They all swore under this noble ‘oat’, but I guess it’s been forgotten.” (This was followed with a photo of a box of Quaker Oats in a failed attempt at humor.) These discussions among the Twitterati highlight the depths of misunderstanding on organ transplantation.
To be fair, unless you have been personally involved in the decision-making process for transplant candidacy, there is little opportunity to be educated. I explain to my anxious patients and their families that a donor organ is like a fumbled football. There may be well over 100 patients at all levels of transplant status in many geographic locations diving for that same organ.
The transplant team is tasked with finding the best match, determining who is the sickest, assessing time for transport of that organ, and, above all, who will be the best steward of that organ.
Take heart transplantation, for instance. Approximately 3,500 patients in the United States are awaiting one each year. Instead of facing an almost certain death within 5 years, a transplant recipient has a chance at a median survival of 12-13 years. The cost of a heart transplant is approximately $1.38 million, according to Milliman, a consulting firm. This is “an incredibly resource intensive procedure,” including expenditures for transportation, antirejection medication, office visits, physician fees, ICU stays, rejection surveillance, and acute rejection therapies.
Transplant denial is nothing new
People get turned down for organ transplants all the time. My patient with end-stage dilated cardiomyopathy was denied a heart transplant when it was discovered that he had scores of outstanding parking tickets. This was seen as a surrogate for an inability to afford his antirejection medication.
Another patient swore that her positive cotinine levels were caused by endless hours at the bingo hall where second-hand smoke swirled. She was also denied. Many potential candidates who are in acute decline hold precariously to newfound sobriety. They are denied. A patient’s boyfriend told the transplant team that he couldn’t be relied upon to drive her to her appointments. She was denied.
Many people who engage in antisocial behaviors have no idea that these actions may result in the denial of an organ transplant should their future selves need one. These are hard lines, but everyone should agree that the odds of survival are heavily in favor of the consistently adherent.
We should take this opportunity to educate the public on how complicated obtaining an organ transplant can be. More than 6,000 people die each year waiting for an organ because of the supply-and-demand disparities in the transplantation arena. I’m willing to bet that many of the loudest protesters in favor of unvaccinated transplant recipients have not signed the organ donor box on the back of their driver’s license. This conversation is an opportunity to change that and remind people that organ donation may be their only opportunity to save a fellow human’s life.
Again, to quote Ted Lasso: “If you care about someone and you got a little love in your heart, there ain’t nothing you can’t get through together.” That philosophy should apply to the tasks of selecting the best organ donors as well as the best organ recipients.
And every organ should go to the one who will honor their donor and their donor’s family by taking the best care of that ultimate gift of life, including being vaccinated against COVID-19.
Dr. Walton-Shirley is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. She disclosed no relevant conflicts of interest. A version of this article first appeared on Medscape.com.
Fungating Mass on the Abdominal Wall
The Diagnosis: Basal Cell Carcinoma
Histopathology was consistent with fungating basal cell carcinoma (BCC). The nodules were comprised of syncytial basaloid cells with high nuclear to cytoplasmic ratios, numerous mitotic figures, fibromyxoid stroma, and peripheral nuclear palisading (Figure). Fortunately, no perineural or lymphovascular invasion was identified, and the margins of the specimen were negative. Despite the high-risk nature of giant BCC, the mass was solitary without notable local invasion, leaving it amendable to surgery. On follow-up, the patient has remained recurrence free, and her hemoglobin level has since stabilized.
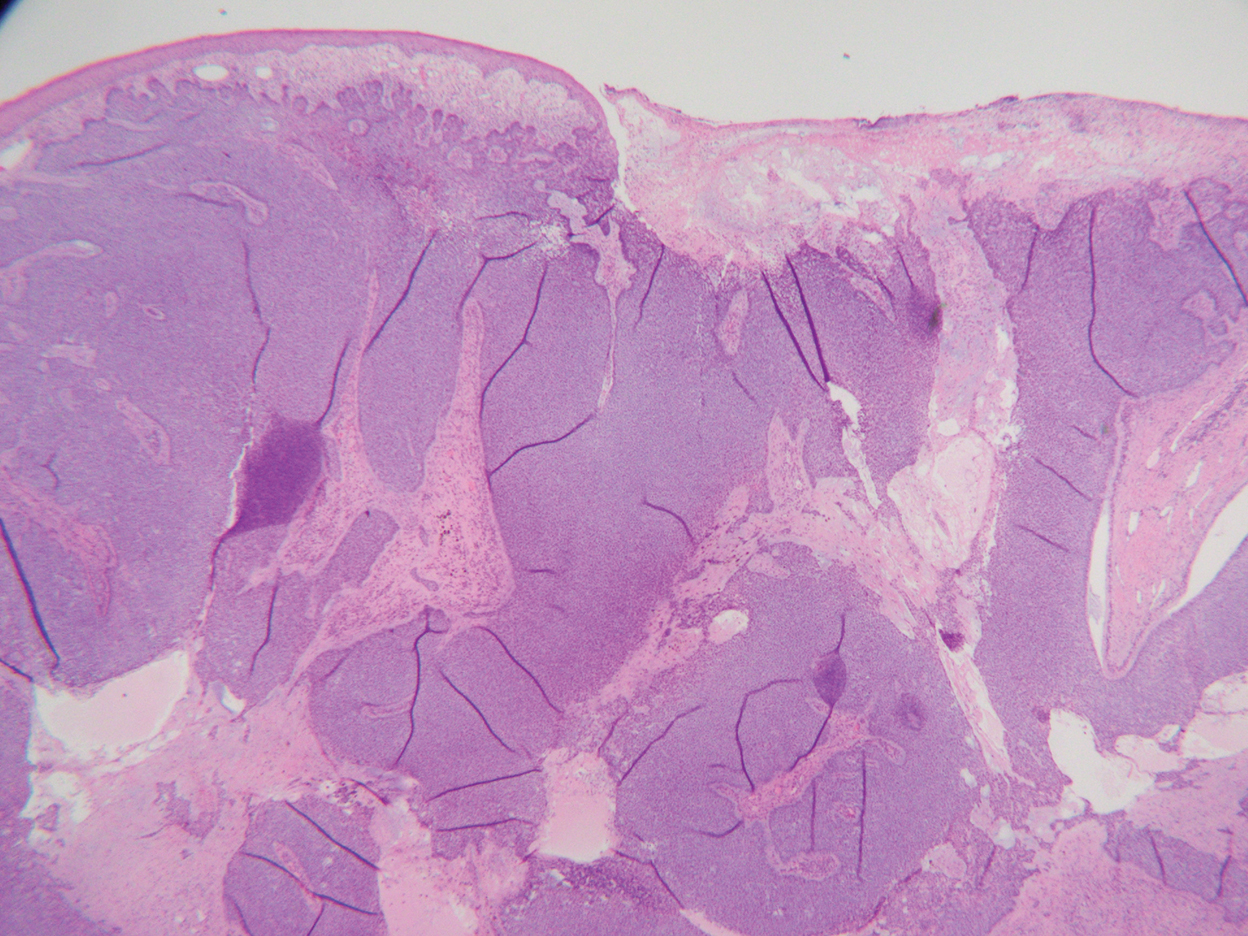
Skin cancer is the most common malignancy worldwide, and BCC accounts for more than 80% of nonmelanoma skin cancers in the United States. The incidence is on the rise due to the aging population and increasing cumulative skin exposure.1 Risk factors include both individual physical characteristics and environmental exposures. Individuals with lighter skin tones, red and blonde hair, and blue and green eyes are at an increased risk.2 UV radiation exposure is the most important cause of BCC.3 Chronic immunosuppression and exposure to arsenic, ionizing radiation, and psoralen plus UVA radiation also have been linked to the development of BCC.4-6 Basal cell carcinomas most commonly arise on sun-exposed areas such as the face, though more than 10% of cases appear on the trunk.7 Lesions characteristically remain localized, and growth rate is variable; however, when left untreated, BCCs have the potential to become locally destructive and difficult to treat.
Advanced BCCs are tumors that penetrate deeply into the skin. They often are not amenable to traditional therapy and/ or metastasize. Those that grow to a diameter greater than 5 cm, as in our patient, are known as giant BCCs. Only 0.5% to 1% of BCCs are giant BCCs8 ; they typically are more aggressive in nature with higher rates of local recurrence and metastasis. Individuals who develop giant BCCs either have had a delay in access to medical care or a history of BCC that was inadequately managed.9,10 During the COVID-19 pandemic, patient access to health care was substantially impacted during lockdowns. As in our patient, skin neoplasms and other medical conditions may present in later stages due to medical neglect.11,12 Metastasis is rare, even in advanced BCCs. A review of the literature from 1984 estimated that the incidence of metastasis of BCCs is 1 in 1000 to 35,000. Metastasis portends a poor prognosis with a median overall survival of 8 to 14 months.13 An updated review in 2013 found similar outcomes.14
The choice of management for BCCs depends on the risk for recurrence as well as individual patient factors. Characteristics such as tumor size, location, histology, whether it is a primary or recurrent lesion, and the presence of chronic skin disease determine the recurrence rate.15 The management of advanced BCCs often requires a multidisciplinary approach, as these neoplasms may not be amenable to local therapy without causing substantial morbidity. Mohs micrographic surgery is the treatment of choice for BCCs at high risk for recurrence.16 Standard surgical excision with postoperative margin assessment is acceptable when Mohs micrographic surgery is not available.17 Radiation therapy is an alternative for patients who are not candidates for surgery.18
Recently, improved understanding of the molecular pathogenesis of BCCs has led to the development of novel systemic therapies. The Hedgehog signaling pathway has been found to play a critical role in the development of most BCCs.19 Vismodegib and sonidegib are small-molecule inhibitors of the Hedgehog signaling pathway approved for the treatment of locally advanced and metastatic BCCs that are not amenable to surgery or radiation. Approximately 50% of advanced BCCs respond to these therapies; however, long-term treatment may be limited by intolerable side effects and the development of resistance.20 Basal cell carcinomas that spread to lymph nodes or distant sites are treated with traditional systemic therapy. Historically, conventional cytotoxic chemotherapies, such as platinum-containing regimens, were employed with limited benefit and notable morbidity.21
The differential diagnosis for our patient included several other cutaneous neoplasms. Squamous cell carcinoma is the second most common type of skin cancer. Similar to BCC, it can reach a substantial size if left untreated. Risk factors include chronic inflammation, exposure to radiation or chemical carcinogens, burns, human papillomavirus, and other chronic infections. Giant squamous cell carcinomas have high malignant potential and require imaging to assess the extent of invasion and for metastasis. Surgery typically is necessary for both staging and treatment. Adjuvant therapy also may be necessary.22,23
Internal malignant neoplasms rarely present as cutaneous metastases. Breast cancer, melanoma, and cancers of the upper respiratory tract most frequently metastasize to the skin. Although colorectal cancer (CRC) rarely metastasizes to the skin, it is an important cause of cutaneous metastasis due to its high incidence in the general population. When it does spread to the skin, CRC preferentially affects the abdominal wall. Lesions typically resemble the primary tumor but may appear anaplastic. The occurrence of cutaneous metastasis suggests latestage disease and carries a poor prognosis.24
Merkel cell carcinoma and melanoma are aggressive skin cancers with high mortality rates. The former is rarer but more lethal. Merkel cell carcinomas typically occur in elderly white men on sun-exposed areas of the skin. Tumors present as asymptomatic, rapidly expanding, blue-red, firm nodules. Immunosuppression and UV light exposure are notable risk factors.25 Of the 4 major subtypes of cutaneous melanoma, superficial spreading is the most common, followed by nodular, lentigo maligna, and acral lentiginous.26 Superficial spreading melanoma characteristically presents as an expanding asymmetric macule or thin plaque with irregular borders and variation in size and color (black, brown, or red). Nodular melanoma usually presents as symmetric in shape and color (amelanotic, black, or brown). Early recognition by both the patient and clinician is essential in preventing tumor growth and progression.27
Our patient’s presentation was highly concerning for cutaneous metastasis given her history of CRC. Furthermore, the finding of severe anemia was atypical for skin cancer and more characteristic of the prior malignancy. Imaging revealed a locally confined mass with no evidence of extension, lymph node involvement, or additional lesions. The diagnosis was clinched with histopathologic examination.
- Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283-287.
- Lear JT, Tan BB, Smith AG, et al. Risk factors for basal cell carcinoma in the UK: case-control study in 806 patients. J R Soc Med. 1997; 90:371-374.
- Gallagher RP, Hill GB, Bajdik CD, et al. Sunlight exposure, pigmentary factors, and risk of nonmelanocytic skin cancer: I. basal cell carcinoma. Arch Dermatol. 1995;131:157-163.
- Guo HR, Yu HS, Hu H, et al. Arsenic in drinking water and skin cancers: cell-type specificity (Taiwan, ROC). Cancer Causes Control. 2001;12:909-916.
- Lichter MD, Karagas MR, Mott LA, et al; The New Hampshire Skin Cancer Study Group. Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. Arch Dermatol. 2000;136:1007-1011.
- Nijsten TEC, Stern RS. The increased risk of skin cancer is persistent after discontinuation of psoralen plus ultraviolet A: a cohort study. J Invest Dermatol. 2003;121:252-258.
- Scrivener Y, Grosshans E, Cribier B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br J Dermatol. 2002;147:41-47.
- Gualdi G, Monari P, Calzavara‐Pinton P, et al. When basal cell carcinomas became giant: an Italian multicenter study. Int J Dermatol. 2020;59:377-382.
- Randle HW, Roenigk RK, Brodland DG. Giant basal cell carcinoma (T3). who is at risk? Cancer. 1993;72:1624-1630.
- Archontaki M, Stavrianos SD, Korkolis DP, et al. Giant basal cell carcinoma: clinicopathological analysis of 51 cases and review of the literature. Anticancer Res. 2009;29:2655-2663.
- Shifat Ahmed SAK, Ajisola M, Azeem K, et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown ssstakeholder engagements. BMJ Glob Health. 2020;5:E003042.
- Gomolin T, Cline A, Handler MZ. The danger of neglecting melanoma during the COVID-19 pandemic. J Dermatolog Treat. 2020;31:444-445.
- von Domarus H, Stevens PJ. Metastatic basal cell carcinoma. report of five cases and review of 170 cases in the literature. J Am Acad Dermatol. 1984;10:1043-1060.
- Wysong A, Aasi SZ, Tang JY. Update on metastatic basal cell carcinoma: a summary of published cases from 1981 through 2011. JAMA Dermatol. 2013;149:615-616.
- Bøgelund FS, Philipsen PA, Gniadecki R. Factors affecting the recurrence rate of basal cell carcinoma. Acta Derm Venereol. 2007;87:330-334.
- Mosterd K, Krekels GAM, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149-1156.
- Wetzig T, Woitek M, Eichhorn K, et al. Surgical excision of basal cell carcinoma with complete margin control: outcome at 5-year follow-up. Dermatology. 2010;220:363-369.
- Silverman MK, Kopf AW, Gladstein AH, et al. Recurrence rates of treated basal cell carcinomas. part 4: X-ray therapy. J Dermatol Surg Oncol. 1992;18:549-554.
- Tanese K, Emoto K, Kubota N, et al. Immunohistochemical visualization of the signature of activated Hedgehog signaling pathway in cutaneous epithelial tumors. J Dermatol. 2018;45:1181-1186.
- Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
- Carneiro BA, Watkin WG, Mehta UK, et al. Metastatic basal cell carcinoma: complete response to chemotherapy and associated pure red cell aplasia. Cancer Invest. 2006;24:396-400.
- Misiakos EP, Damaskou V, Koumarianou A, et al. A giant squamous cell carcinoma of the skin of the thoracic wall: a case report and review of the literature. J Med Case Rep. 2017;11:136.
- Wollina U, Bayyoud Y, Krönert C, et al. Giant epithelial malignancies (basal cell carcinoma, squamous cell carcinoma): a series of 20 tumors from a single center. J Cutan Aesthet Surg. 2012;5:12-19.
- Bittencourt MJS, Imbiriba AA, Oliveira OA, et al. Cutaneous metastasis of colorectal cancer. An Bras Dermatol. 2018;93:884-886.
- Heath M, Jaimes N, Lemos B, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58:375-381.
- Buettner PG, Leiter U, Eigentler TK, et al. Development of prognostic factors and survival in cutaneous melanoma over 25 years: an analysis of the Central Malignant Melanoma Registry of the German Dermatological Society. Cancer. 2005;103:616-624.
- Klebanov N, Gunasekera N, Lin WM, et al. The clinical spectrum of cutaneous melanoma morphology. J Am Acad Dermatol. 2019; 80:178-188.e3.
The Diagnosis: Basal Cell Carcinoma
Histopathology was consistent with fungating basal cell carcinoma (BCC). The nodules were comprised of syncytial basaloid cells with high nuclear to cytoplasmic ratios, numerous mitotic figures, fibromyxoid stroma, and peripheral nuclear palisading (Figure). Fortunately, no perineural or lymphovascular invasion was identified, and the margins of the specimen were negative. Despite the high-risk nature of giant BCC, the mass was solitary without notable local invasion, leaving it amendable to surgery. On follow-up, the patient has remained recurrence free, and her hemoglobin level has since stabilized.
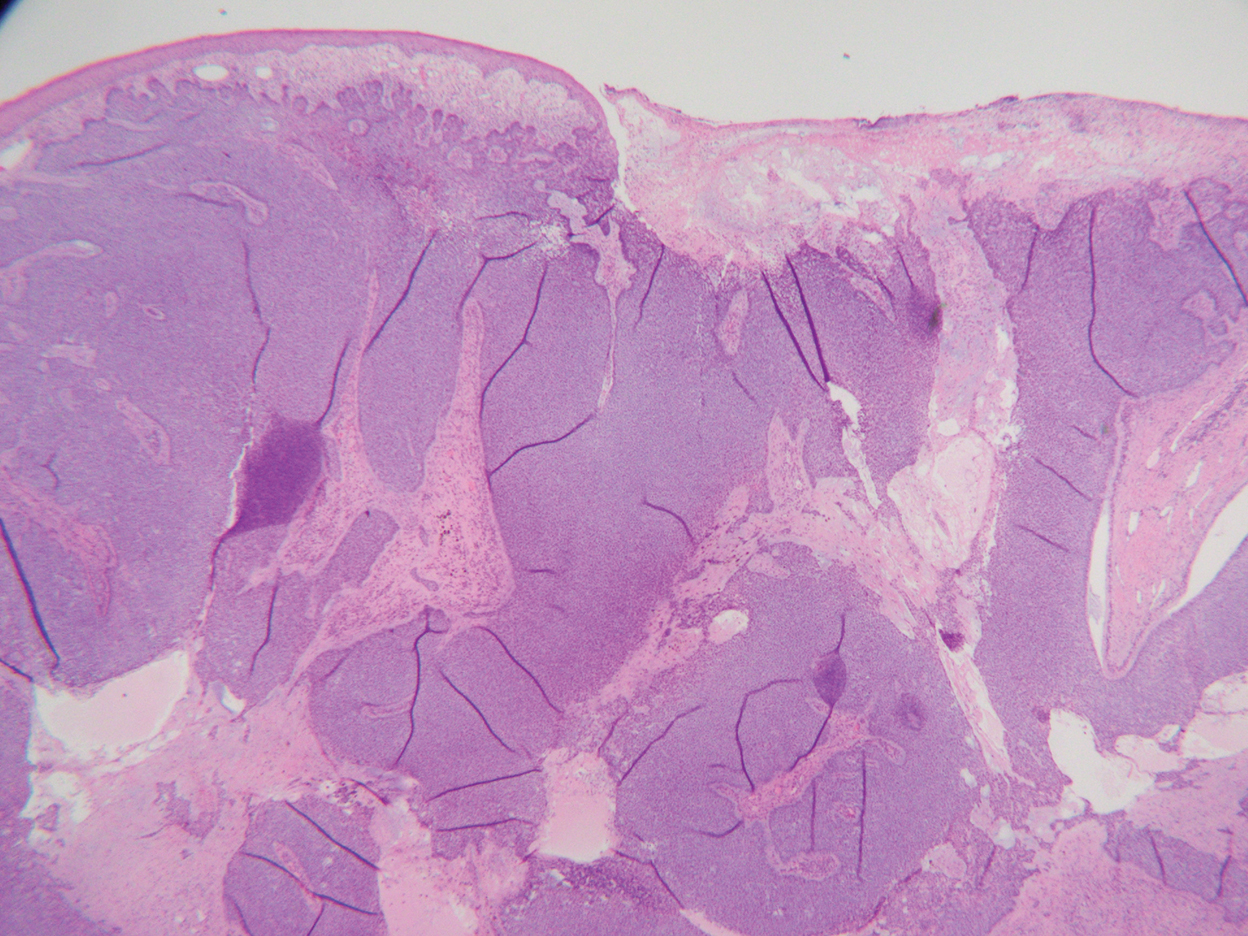
Skin cancer is the most common malignancy worldwide, and BCC accounts for more than 80% of nonmelanoma skin cancers in the United States. The incidence is on the rise due to the aging population and increasing cumulative skin exposure.1 Risk factors include both individual physical characteristics and environmental exposures. Individuals with lighter skin tones, red and blonde hair, and blue and green eyes are at an increased risk.2 UV radiation exposure is the most important cause of BCC.3 Chronic immunosuppression and exposure to arsenic, ionizing radiation, and psoralen plus UVA radiation also have been linked to the development of BCC.4-6 Basal cell carcinomas most commonly arise on sun-exposed areas such as the face, though more than 10% of cases appear on the trunk.7 Lesions characteristically remain localized, and growth rate is variable; however, when left untreated, BCCs have the potential to become locally destructive and difficult to treat.
Advanced BCCs are tumors that penetrate deeply into the skin. They often are not amenable to traditional therapy and/ or metastasize. Those that grow to a diameter greater than 5 cm, as in our patient, are known as giant BCCs. Only 0.5% to 1% of BCCs are giant BCCs8 ; they typically are more aggressive in nature with higher rates of local recurrence and metastasis. Individuals who develop giant BCCs either have had a delay in access to medical care or a history of BCC that was inadequately managed.9,10 During the COVID-19 pandemic, patient access to health care was substantially impacted during lockdowns. As in our patient, skin neoplasms and other medical conditions may present in later stages due to medical neglect.11,12 Metastasis is rare, even in advanced BCCs. A review of the literature from 1984 estimated that the incidence of metastasis of BCCs is 1 in 1000 to 35,000. Metastasis portends a poor prognosis with a median overall survival of 8 to 14 months.13 An updated review in 2013 found similar outcomes.14
The choice of management for BCCs depends on the risk for recurrence as well as individual patient factors. Characteristics such as tumor size, location, histology, whether it is a primary or recurrent lesion, and the presence of chronic skin disease determine the recurrence rate.15 The management of advanced BCCs often requires a multidisciplinary approach, as these neoplasms may not be amenable to local therapy without causing substantial morbidity. Mohs micrographic surgery is the treatment of choice for BCCs at high risk for recurrence.16 Standard surgical excision with postoperative margin assessment is acceptable when Mohs micrographic surgery is not available.17 Radiation therapy is an alternative for patients who are not candidates for surgery.18
Recently, improved understanding of the molecular pathogenesis of BCCs has led to the development of novel systemic therapies. The Hedgehog signaling pathway has been found to play a critical role in the development of most BCCs.19 Vismodegib and sonidegib are small-molecule inhibitors of the Hedgehog signaling pathway approved for the treatment of locally advanced and metastatic BCCs that are not amenable to surgery or radiation. Approximately 50% of advanced BCCs respond to these therapies; however, long-term treatment may be limited by intolerable side effects and the development of resistance.20 Basal cell carcinomas that spread to lymph nodes or distant sites are treated with traditional systemic therapy. Historically, conventional cytotoxic chemotherapies, such as platinum-containing regimens, were employed with limited benefit and notable morbidity.21
The differential diagnosis for our patient included several other cutaneous neoplasms. Squamous cell carcinoma is the second most common type of skin cancer. Similar to BCC, it can reach a substantial size if left untreated. Risk factors include chronic inflammation, exposure to radiation or chemical carcinogens, burns, human papillomavirus, and other chronic infections. Giant squamous cell carcinomas have high malignant potential and require imaging to assess the extent of invasion and for metastasis. Surgery typically is necessary for both staging and treatment. Adjuvant therapy also may be necessary.22,23
Internal malignant neoplasms rarely present as cutaneous metastases. Breast cancer, melanoma, and cancers of the upper respiratory tract most frequently metastasize to the skin. Although colorectal cancer (CRC) rarely metastasizes to the skin, it is an important cause of cutaneous metastasis due to its high incidence in the general population. When it does spread to the skin, CRC preferentially affects the abdominal wall. Lesions typically resemble the primary tumor but may appear anaplastic. The occurrence of cutaneous metastasis suggests latestage disease and carries a poor prognosis.24
Merkel cell carcinoma and melanoma are aggressive skin cancers with high mortality rates. The former is rarer but more lethal. Merkel cell carcinomas typically occur in elderly white men on sun-exposed areas of the skin. Tumors present as asymptomatic, rapidly expanding, blue-red, firm nodules. Immunosuppression and UV light exposure are notable risk factors.25 Of the 4 major subtypes of cutaneous melanoma, superficial spreading is the most common, followed by nodular, lentigo maligna, and acral lentiginous.26 Superficial spreading melanoma characteristically presents as an expanding asymmetric macule or thin plaque with irregular borders and variation in size and color (black, brown, or red). Nodular melanoma usually presents as symmetric in shape and color (amelanotic, black, or brown). Early recognition by both the patient and clinician is essential in preventing tumor growth and progression.27
Our patient’s presentation was highly concerning for cutaneous metastasis given her history of CRC. Furthermore, the finding of severe anemia was atypical for skin cancer and more characteristic of the prior malignancy. Imaging revealed a locally confined mass with no evidence of extension, lymph node involvement, or additional lesions. The diagnosis was clinched with histopathologic examination.
The Diagnosis: Basal Cell Carcinoma
Histopathology was consistent with fungating basal cell carcinoma (BCC). The nodules were comprised of syncytial basaloid cells with high nuclear to cytoplasmic ratios, numerous mitotic figures, fibromyxoid stroma, and peripheral nuclear palisading (Figure). Fortunately, no perineural or lymphovascular invasion was identified, and the margins of the specimen were negative. Despite the high-risk nature of giant BCC, the mass was solitary without notable local invasion, leaving it amendable to surgery. On follow-up, the patient has remained recurrence free, and her hemoglobin level has since stabilized.
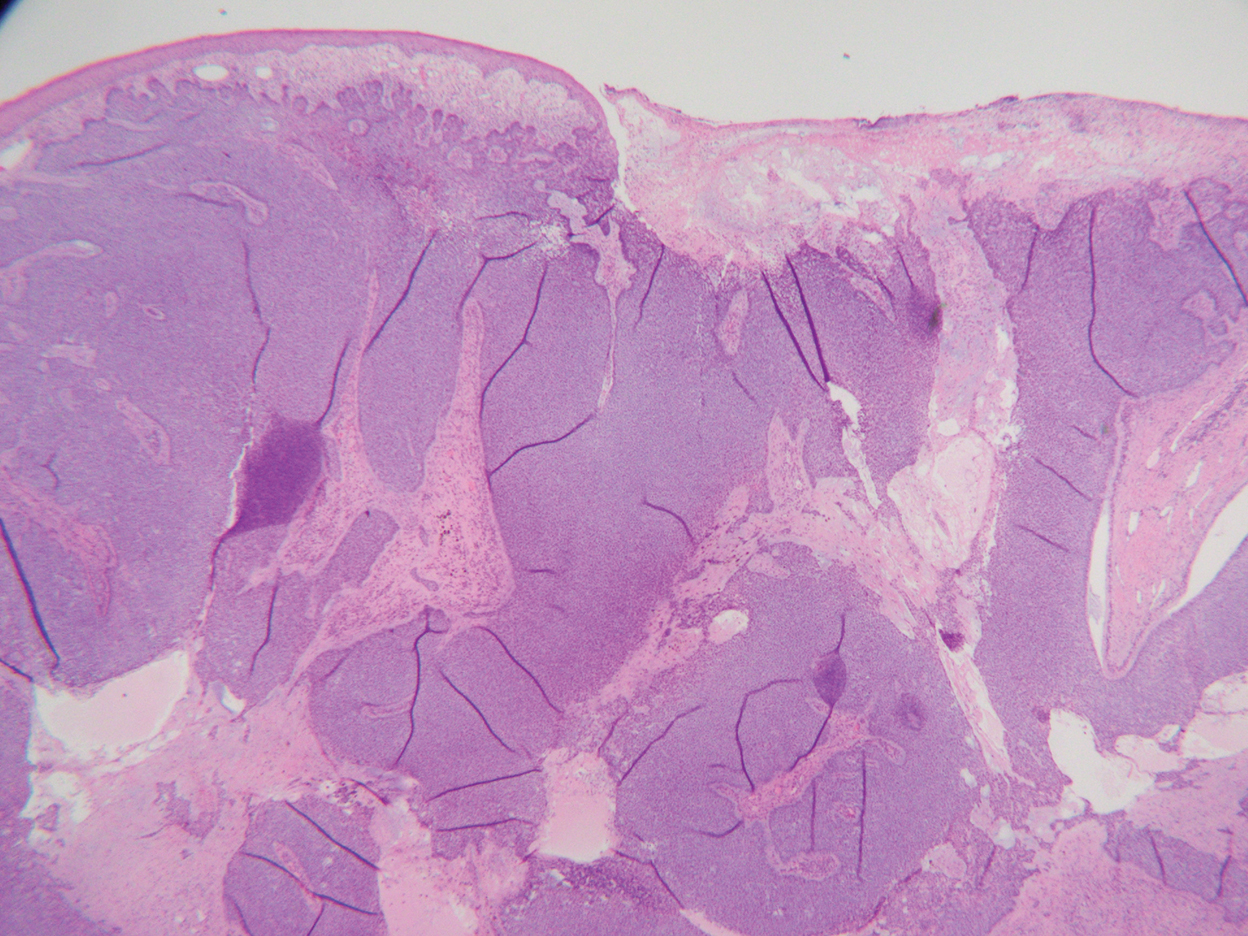
Skin cancer is the most common malignancy worldwide, and BCC accounts for more than 80% of nonmelanoma skin cancers in the United States. The incidence is on the rise due to the aging population and increasing cumulative skin exposure.1 Risk factors include both individual physical characteristics and environmental exposures. Individuals with lighter skin tones, red and blonde hair, and blue and green eyes are at an increased risk.2 UV radiation exposure is the most important cause of BCC.3 Chronic immunosuppression and exposure to arsenic, ionizing radiation, and psoralen plus UVA radiation also have been linked to the development of BCC.4-6 Basal cell carcinomas most commonly arise on sun-exposed areas such as the face, though more than 10% of cases appear on the trunk.7 Lesions characteristically remain localized, and growth rate is variable; however, when left untreated, BCCs have the potential to become locally destructive and difficult to treat.
Advanced BCCs are tumors that penetrate deeply into the skin. They often are not amenable to traditional therapy and/ or metastasize. Those that grow to a diameter greater than 5 cm, as in our patient, are known as giant BCCs. Only 0.5% to 1% of BCCs are giant BCCs8 ; they typically are more aggressive in nature with higher rates of local recurrence and metastasis. Individuals who develop giant BCCs either have had a delay in access to medical care or a history of BCC that was inadequately managed.9,10 During the COVID-19 pandemic, patient access to health care was substantially impacted during lockdowns. As in our patient, skin neoplasms and other medical conditions may present in later stages due to medical neglect.11,12 Metastasis is rare, even in advanced BCCs. A review of the literature from 1984 estimated that the incidence of metastasis of BCCs is 1 in 1000 to 35,000. Metastasis portends a poor prognosis with a median overall survival of 8 to 14 months.13 An updated review in 2013 found similar outcomes.14
The choice of management for BCCs depends on the risk for recurrence as well as individual patient factors. Characteristics such as tumor size, location, histology, whether it is a primary or recurrent lesion, and the presence of chronic skin disease determine the recurrence rate.15 The management of advanced BCCs often requires a multidisciplinary approach, as these neoplasms may not be amenable to local therapy without causing substantial morbidity. Mohs micrographic surgery is the treatment of choice for BCCs at high risk for recurrence.16 Standard surgical excision with postoperative margin assessment is acceptable when Mohs micrographic surgery is not available.17 Radiation therapy is an alternative for patients who are not candidates for surgery.18
Recently, improved understanding of the molecular pathogenesis of BCCs has led to the development of novel systemic therapies. The Hedgehog signaling pathway has been found to play a critical role in the development of most BCCs.19 Vismodegib and sonidegib are small-molecule inhibitors of the Hedgehog signaling pathway approved for the treatment of locally advanced and metastatic BCCs that are not amenable to surgery or radiation. Approximately 50% of advanced BCCs respond to these therapies; however, long-term treatment may be limited by intolerable side effects and the development of resistance.20 Basal cell carcinomas that spread to lymph nodes or distant sites are treated with traditional systemic therapy. Historically, conventional cytotoxic chemotherapies, such as platinum-containing regimens, were employed with limited benefit and notable morbidity.21
The differential diagnosis for our patient included several other cutaneous neoplasms. Squamous cell carcinoma is the second most common type of skin cancer. Similar to BCC, it can reach a substantial size if left untreated. Risk factors include chronic inflammation, exposure to radiation or chemical carcinogens, burns, human papillomavirus, and other chronic infections. Giant squamous cell carcinomas have high malignant potential and require imaging to assess the extent of invasion and for metastasis. Surgery typically is necessary for both staging and treatment. Adjuvant therapy also may be necessary.22,23
Internal malignant neoplasms rarely present as cutaneous metastases. Breast cancer, melanoma, and cancers of the upper respiratory tract most frequently metastasize to the skin. Although colorectal cancer (CRC) rarely metastasizes to the skin, it is an important cause of cutaneous metastasis due to its high incidence in the general population. When it does spread to the skin, CRC preferentially affects the abdominal wall. Lesions typically resemble the primary tumor but may appear anaplastic. The occurrence of cutaneous metastasis suggests latestage disease and carries a poor prognosis.24
Merkel cell carcinoma and melanoma are aggressive skin cancers with high mortality rates. The former is rarer but more lethal. Merkel cell carcinomas typically occur in elderly white men on sun-exposed areas of the skin. Tumors present as asymptomatic, rapidly expanding, blue-red, firm nodules. Immunosuppression and UV light exposure are notable risk factors.25 Of the 4 major subtypes of cutaneous melanoma, superficial spreading is the most common, followed by nodular, lentigo maligna, and acral lentiginous.26 Superficial spreading melanoma characteristically presents as an expanding asymmetric macule or thin plaque with irregular borders and variation in size and color (black, brown, or red). Nodular melanoma usually presents as symmetric in shape and color (amelanotic, black, or brown). Early recognition by both the patient and clinician is essential in preventing tumor growth and progression.27
Our patient’s presentation was highly concerning for cutaneous metastasis given her history of CRC. Furthermore, the finding of severe anemia was atypical for skin cancer and more characteristic of the prior malignancy. Imaging revealed a locally confined mass with no evidence of extension, lymph node involvement, or additional lesions. The diagnosis was clinched with histopathologic examination.
- Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283-287.
- Lear JT, Tan BB, Smith AG, et al. Risk factors for basal cell carcinoma in the UK: case-control study in 806 patients. J R Soc Med. 1997; 90:371-374.
- Gallagher RP, Hill GB, Bajdik CD, et al. Sunlight exposure, pigmentary factors, and risk of nonmelanocytic skin cancer: I. basal cell carcinoma. Arch Dermatol. 1995;131:157-163.
- Guo HR, Yu HS, Hu H, et al. Arsenic in drinking water and skin cancers: cell-type specificity (Taiwan, ROC). Cancer Causes Control. 2001;12:909-916.
- Lichter MD, Karagas MR, Mott LA, et al; The New Hampshire Skin Cancer Study Group. Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. Arch Dermatol. 2000;136:1007-1011.
- Nijsten TEC, Stern RS. The increased risk of skin cancer is persistent after discontinuation of psoralen plus ultraviolet A: a cohort study. J Invest Dermatol. 2003;121:252-258.
- Scrivener Y, Grosshans E, Cribier B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br J Dermatol. 2002;147:41-47.
- Gualdi G, Monari P, Calzavara‐Pinton P, et al. When basal cell carcinomas became giant: an Italian multicenter study. Int J Dermatol. 2020;59:377-382.
- Randle HW, Roenigk RK, Brodland DG. Giant basal cell carcinoma (T3). who is at risk? Cancer. 1993;72:1624-1630.
- Archontaki M, Stavrianos SD, Korkolis DP, et al. Giant basal cell carcinoma: clinicopathological analysis of 51 cases and review of the literature. Anticancer Res. 2009;29:2655-2663.
- Shifat Ahmed SAK, Ajisola M, Azeem K, et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown ssstakeholder engagements. BMJ Glob Health. 2020;5:E003042.
- Gomolin T, Cline A, Handler MZ. The danger of neglecting melanoma during the COVID-19 pandemic. J Dermatolog Treat. 2020;31:444-445.
- von Domarus H, Stevens PJ. Metastatic basal cell carcinoma. report of five cases and review of 170 cases in the literature. J Am Acad Dermatol. 1984;10:1043-1060.
- Wysong A, Aasi SZ, Tang JY. Update on metastatic basal cell carcinoma: a summary of published cases from 1981 through 2011. JAMA Dermatol. 2013;149:615-616.
- Bøgelund FS, Philipsen PA, Gniadecki R. Factors affecting the recurrence rate of basal cell carcinoma. Acta Derm Venereol. 2007;87:330-334.
- Mosterd K, Krekels GAM, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149-1156.
- Wetzig T, Woitek M, Eichhorn K, et al. Surgical excision of basal cell carcinoma with complete margin control: outcome at 5-year follow-up. Dermatology. 2010;220:363-369.
- Silverman MK, Kopf AW, Gladstein AH, et al. Recurrence rates of treated basal cell carcinomas. part 4: X-ray therapy. J Dermatol Surg Oncol. 1992;18:549-554.
- Tanese K, Emoto K, Kubota N, et al. Immunohistochemical visualization of the signature of activated Hedgehog signaling pathway in cutaneous epithelial tumors. J Dermatol. 2018;45:1181-1186.
- Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
- Carneiro BA, Watkin WG, Mehta UK, et al. Metastatic basal cell carcinoma: complete response to chemotherapy and associated pure red cell aplasia. Cancer Invest. 2006;24:396-400.
- Misiakos EP, Damaskou V, Koumarianou A, et al. A giant squamous cell carcinoma of the skin of the thoracic wall: a case report and review of the literature. J Med Case Rep. 2017;11:136.
- Wollina U, Bayyoud Y, Krönert C, et al. Giant epithelial malignancies (basal cell carcinoma, squamous cell carcinoma): a series of 20 tumors from a single center. J Cutan Aesthet Surg. 2012;5:12-19.
- Bittencourt MJS, Imbiriba AA, Oliveira OA, et al. Cutaneous metastasis of colorectal cancer. An Bras Dermatol. 2018;93:884-886.
- Heath M, Jaimes N, Lemos B, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58:375-381.
- Buettner PG, Leiter U, Eigentler TK, et al. Development of prognostic factors and survival in cutaneous melanoma over 25 years: an analysis of the Central Malignant Melanoma Registry of the German Dermatological Society. Cancer. 2005;103:616-624.
- Klebanov N, Gunasekera N, Lin WM, et al. The clinical spectrum of cutaneous melanoma morphology. J Am Acad Dermatol. 2019; 80:178-188.e3.
- Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283-287.
- Lear JT, Tan BB, Smith AG, et al. Risk factors for basal cell carcinoma in the UK: case-control study in 806 patients. J R Soc Med. 1997; 90:371-374.
- Gallagher RP, Hill GB, Bajdik CD, et al. Sunlight exposure, pigmentary factors, and risk of nonmelanocytic skin cancer: I. basal cell carcinoma. Arch Dermatol. 1995;131:157-163.
- Guo HR, Yu HS, Hu H, et al. Arsenic in drinking water and skin cancers: cell-type specificity (Taiwan, ROC). Cancer Causes Control. 2001;12:909-916.
- Lichter MD, Karagas MR, Mott LA, et al; The New Hampshire Skin Cancer Study Group. Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. Arch Dermatol. 2000;136:1007-1011.
- Nijsten TEC, Stern RS. The increased risk of skin cancer is persistent after discontinuation of psoralen plus ultraviolet A: a cohort study. J Invest Dermatol. 2003;121:252-258.
- Scrivener Y, Grosshans E, Cribier B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br J Dermatol. 2002;147:41-47.
- Gualdi G, Monari P, Calzavara‐Pinton P, et al. When basal cell carcinomas became giant: an Italian multicenter study. Int J Dermatol. 2020;59:377-382.
- Randle HW, Roenigk RK, Brodland DG. Giant basal cell carcinoma (T3). who is at risk? Cancer. 1993;72:1624-1630.
- Archontaki M, Stavrianos SD, Korkolis DP, et al. Giant basal cell carcinoma: clinicopathological analysis of 51 cases and review of the literature. Anticancer Res. 2009;29:2655-2663.
- Shifat Ahmed SAK, Ajisola M, Azeem K, et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown ssstakeholder engagements. BMJ Glob Health. 2020;5:E003042.
- Gomolin T, Cline A, Handler MZ. The danger of neglecting melanoma during the COVID-19 pandemic. J Dermatolog Treat. 2020;31:444-445.
- von Domarus H, Stevens PJ. Metastatic basal cell carcinoma. report of five cases and review of 170 cases in the literature. J Am Acad Dermatol. 1984;10:1043-1060.
- Wysong A, Aasi SZ, Tang JY. Update on metastatic basal cell carcinoma: a summary of published cases from 1981 through 2011. JAMA Dermatol. 2013;149:615-616.
- Bøgelund FS, Philipsen PA, Gniadecki R. Factors affecting the recurrence rate of basal cell carcinoma. Acta Derm Venereol. 2007;87:330-334.
- Mosterd K, Krekels GAM, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149-1156.
- Wetzig T, Woitek M, Eichhorn K, et al. Surgical excision of basal cell carcinoma with complete margin control: outcome at 5-year follow-up. Dermatology. 2010;220:363-369.
- Silverman MK, Kopf AW, Gladstein AH, et al. Recurrence rates of treated basal cell carcinomas. part 4: X-ray therapy. J Dermatol Surg Oncol. 1992;18:549-554.
- Tanese K, Emoto K, Kubota N, et al. Immunohistochemical visualization of the signature of activated Hedgehog signaling pathway in cutaneous epithelial tumors. J Dermatol. 2018;45:1181-1186.
- Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
- Carneiro BA, Watkin WG, Mehta UK, et al. Metastatic basal cell carcinoma: complete response to chemotherapy and associated pure red cell aplasia. Cancer Invest. 2006;24:396-400.
- Misiakos EP, Damaskou V, Koumarianou A, et al. A giant squamous cell carcinoma of the skin of the thoracic wall: a case report and review of the literature. J Med Case Rep. 2017;11:136.
- Wollina U, Bayyoud Y, Krönert C, et al. Giant epithelial malignancies (basal cell carcinoma, squamous cell carcinoma): a series of 20 tumors from a single center. J Cutan Aesthet Surg. 2012;5:12-19.
- Bittencourt MJS, Imbiriba AA, Oliveira OA, et al. Cutaneous metastasis of colorectal cancer. An Bras Dermatol. 2018;93:884-886.
- Heath M, Jaimes N, Lemos B, et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58:375-381.
- Buettner PG, Leiter U, Eigentler TK, et al. Development of prognostic factors and survival in cutaneous melanoma over 25 years: an analysis of the Central Malignant Melanoma Registry of the German Dermatological Society. Cancer. 2005;103:616-624.
- Klebanov N, Gunasekera N, Lin WM, et al. The clinical spectrum of cutaneous melanoma morphology. J Am Acad Dermatol. 2019; 80:178-188.e3.
A 77-year-old woman was admitted to the hospital with anemia (hemoglobin, 5.2 g/dL [reference range, 12.0–15.5 g/dL]) and a rapidly growing abdominal wall mass. She had a history of stage IIA colon cancer (T3N0M0) that was treated 5 years prior with a partial colon resection and adjuvant chemotherapy. She initially noticed a red scaly lesion developing around a scar from a prior surgery that had been stable for years. Over the last 2 months, the lesion rapidly expanded and would intermittently bleed. Physical examination revealed a 13×10×4.5-cm, pink-red, nodular, firm mass over the patient’s right upper quadrant. Computed tomography revealed a mass limited to the skin and superficial tissue. General surgery was consulted for excision of the mass.

Sports experts on T2D: Boost activity, cut sedentary time
The American College of Sports Medicine (ACSM) has issued new recommendations for exercise/physical activity in people with type 2 diabetes, which update a 2010 joint ACSM/American Diabetes Association position statement.
The guidance has been published in the February issue of Medicine & Science in Sports & Exercise.
“This consensus statement provides a brief summary of the current evidence and extends and updates the prior recommendations,” the authors explain.
In the past decade, there has been a “considerable amount” of research about exercise in people with type 2 diabetes, they add, while the prevalence of diabetes has steadily increased.
The updated recommendations have been “expanded to include physical activity – a broader, more comprehensive definition of human movement than planned exercise – and reducing sedentary time,” the authors note.
“The latest guidelines are applicable to most individuals with diabetes, including youth, with a few exceptions and modifications,” lead author Jill A. Kanaley, PhD, said in a press release from the ACSM.
The key takeaway is that “all individuals [with type 2 diabetes] should engage in regular physical activity, reduce sedentary time, and break up sitting time with frequent activity breaks,” said Dr. Kanaley, a professor in the department of nutrition and exercise physiology, University of Missouri, Columbia.
“Exercise can play an important role in managing type 2 diabetes, and workouts can be modified to fit the abilities of most people,” she stressed.
And those with type 2 diabetes who want to lose weight “should consider workouts of moderately high volume for 4 to 5 days per week,” she added.
Six key tips for physical activity in adults with type 2 diabetes
The consensus statement gives six key tips for physical activity in adults with type 2 diabetes, as follows.
- Regular aerobic exercise improves glycemic management; meta-analyses have reported fewer daily hyperglycemic episodes and reductions in A1c of 0.5%-0.7%.
- High-intensity resistance exercise, when performed safely, is better than low-to-moderate intensity resistance exercise for glucose management and attenuation of insulin levels. Resistance exercise typically results in improvements of 10% to 15% in strength, bone mineral density, blood pressure, lipid profile, skeletal muscle mass, and insulin sensitivity.
- Exercise after meals, such as taking a walk after dinner at one’s own pace, takes advantage of the blood glucose-stabilizing effects of exercise.
- Reduce sedentary time by taking regular breaks for small “doses” of physical activity, which can modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
- To prevent hypoglycemia during or after exercise, people taking insulin or insulin secretagogues should increase carbohydrate intake, or if possible, reduce insulin.
- People who are taking beta blockers should not rely on a heart monitor to measure workout intensity. They could ask a certified exercise professional about using ratings of perceived exertion to track how a workout feels.
Other recommendations
The consensus statement also summarizes precautions that people with complications of type 2 diabetes (such as neuropathy, retinopathy, kidney disease, and hypertension) should take.
Low impact exercises for flexibility can help introduce sedentary people to physical activity, the consensus group writes. Balance exercises can be helpful for older adults.
Weight loss greater than 5% can benefit A1c, blood lipid, and blood pressure levels. Moderate exercise 4 to 5 days a week can reduce visceral fat.
In studies of youth with type 2 diabetes, intensive lifestyle interventions plus metformin were not superior to metformin alone for managing glycemia. Physical activity goals are the same for youth with or without diabetes.
Pregnant women with diabetes should participate in at least 20 to 30 minutes of moderate-intensity exercise most days of the week.
Participating in an exercise program before and after bariatric surgery may enhance surgical outcomes.
Dr. Kanaley has reported receiving a grant from the National Institutes of Health. Disclosures for the other authors are listed in the article.
A version of this article first appeared on Medscape.com.
The American College of Sports Medicine (ACSM) has issued new recommendations for exercise/physical activity in people with type 2 diabetes, which update a 2010 joint ACSM/American Diabetes Association position statement.
The guidance has been published in the February issue of Medicine & Science in Sports & Exercise.
“This consensus statement provides a brief summary of the current evidence and extends and updates the prior recommendations,” the authors explain.
In the past decade, there has been a “considerable amount” of research about exercise in people with type 2 diabetes, they add, while the prevalence of diabetes has steadily increased.
The updated recommendations have been “expanded to include physical activity – a broader, more comprehensive definition of human movement than planned exercise – and reducing sedentary time,” the authors note.
“The latest guidelines are applicable to most individuals with diabetes, including youth, with a few exceptions and modifications,” lead author Jill A. Kanaley, PhD, said in a press release from the ACSM.
The key takeaway is that “all individuals [with type 2 diabetes] should engage in regular physical activity, reduce sedentary time, and break up sitting time with frequent activity breaks,” said Dr. Kanaley, a professor in the department of nutrition and exercise physiology, University of Missouri, Columbia.
“Exercise can play an important role in managing type 2 diabetes, and workouts can be modified to fit the abilities of most people,” she stressed.
And those with type 2 diabetes who want to lose weight “should consider workouts of moderately high volume for 4 to 5 days per week,” she added.
Six key tips for physical activity in adults with type 2 diabetes
The consensus statement gives six key tips for physical activity in adults with type 2 diabetes, as follows.
- Regular aerobic exercise improves glycemic management; meta-analyses have reported fewer daily hyperglycemic episodes and reductions in A1c of 0.5%-0.7%.
- High-intensity resistance exercise, when performed safely, is better than low-to-moderate intensity resistance exercise for glucose management and attenuation of insulin levels. Resistance exercise typically results in improvements of 10% to 15% in strength, bone mineral density, blood pressure, lipid profile, skeletal muscle mass, and insulin sensitivity.
- Exercise after meals, such as taking a walk after dinner at one’s own pace, takes advantage of the blood glucose-stabilizing effects of exercise.
- Reduce sedentary time by taking regular breaks for small “doses” of physical activity, which can modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
- To prevent hypoglycemia during or after exercise, people taking insulin or insulin secretagogues should increase carbohydrate intake, or if possible, reduce insulin.
- People who are taking beta blockers should not rely on a heart monitor to measure workout intensity. They could ask a certified exercise professional about using ratings of perceived exertion to track how a workout feels.
Other recommendations
The consensus statement also summarizes precautions that people with complications of type 2 diabetes (such as neuropathy, retinopathy, kidney disease, and hypertension) should take.
Low impact exercises for flexibility can help introduce sedentary people to physical activity, the consensus group writes. Balance exercises can be helpful for older adults.
Weight loss greater than 5% can benefit A1c, blood lipid, and blood pressure levels. Moderate exercise 4 to 5 days a week can reduce visceral fat.
In studies of youth with type 2 diabetes, intensive lifestyle interventions plus metformin were not superior to metformin alone for managing glycemia. Physical activity goals are the same for youth with or without diabetes.
Pregnant women with diabetes should participate in at least 20 to 30 minutes of moderate-intensity exercise most days of the week.
Participating in an exercise program before and after bariatric surgery may enhance surgical outcomes.
Dr. Kanaley has reported receiving a grant from the National Institutes of Health. Disclosures for the other authors are listed in the article.
A version of this article first appeared on Medscape.com.
The American College of Sports Medicine (ACSM) has issued new recommendations for exercise/physical activity in people with type 2 diabetes, which update a 2010 joint ACSM/American Diabetes Association position statement.
The guidance has been published in the February issue of Medicine & Science in Sports & Exercise.
“This consensus statement provides a brief summary of the current evidence and extends and updates the prior recommendations,” the authors explain.
In the past decade, there has been a “considerable amount” of research about exercise in people with type 2 diabetes, they add, while the prevalence of diabetes has steadily increased.
The updated recommendations have been “expanded to include physical activity – a broader, more comprehensive definition of human movement than planned exercise – and reducing sedentary time,” the authors note.
“The latest guidelines are applicable to most individuals with diabetes, including youth, with a few exceptions and modifications,” lead author Jill A. Kanaley, PhD, said in a press release from the ACSM.
The key takeaway is that “all individuals [with type 2 diabetes] should engage in regular physical activity, reduce sedentary time, and break up sitting time with frequent activity breaks,” said Dr. Kanaley, a professor in the department of nutrition and exercise physiology, University of Missouri, Columbia.
“Exercise can play an important role in managing type 2 diabetes, and workouts can be modified to fit the abilities of most people,” she stressed.
And those with type 2 diabetes who want to lose weight “should consider workouts of moderately high volume for 4 to 5 days per week,” she added.
Six key tips for physical activity in adults with type 2 diabetes
The consensus statement gives six key tips for physical activity in adults with type 2 diabetes, as follows.
- Regular aerobic exercise improves glycemic management; meta-analyses have reported fewer daily hyperglycemic episodes and reductions in A1c of 0.5%-0.7%.
- High-intensity resistance exercise, when performed safely, is better than low-to-moderate intensity resistance exercise for glucose management and attenuation of insulin levels. Resistance exercise typically results in improvements of 10% to 15% in strength, bone mineral density, blood pressure, lipid profile, skeletal muscle mass, and insulin sensitivity.
- Exercise after meals, such as taking a walk after dinner at one’s own pace, takes advantage of the blood glucose-stabilizing effects of exercise.
- Reduce sedentary time by taking regular breaks for small “doses” of physical activity, which can modestly attenuate postprandial glucose and insulin levels, particularly in individuals with insulin resistance and a higher body mass index.
- To prevent hypoglycemia during or after exercise, people taking insulin or insulin secretagogues should increase carbohydrate intake, or if possible, reduce insulin.
- People who are taking beta blockers should not rely on a heart monitor to measure workout intensity. They could ask a certified exercise professional about using ratings of perceived exertion to track how a workout feels.
Other recommendations
The consensus statement also summarizes precautions that people with complications of type 2 diabetes (such as neuropathy, retinopathy, kidney disease, and hypertension) should take.
Low impact exercises for flexibility can help introduce sedentary people to physical activity, the consensus group writes. Balance exercises can be helpful for older adults.
Weight loss greater than 5% can benefit A1c, blood lipid, and blood pressure levels. Moderate exercise 4 to 5 days a week can reduce visceral fat.
In studies of youth with type 2 diabetes, intensive lifestyle interventions plus metformin were not superior to metformin alone for managing glycemia. Physical activity goals are the same for youth with or without diabetes.
Pregnant women with diabetes should participate in at least 20 to 30 minutes of moderate-intensity exercise most days of the week.
Participating in an exercise program before and after bariatric surgery may enhance surgical outcomes.
Dr. Kanaley has reported receiving a grant from the National Institutes of Health. Disclosures for the other authors are listed in the article.
A version of this article first appeared on Medscape.com.
Small group of higher-volume antibiotic prescribers identified
“Higher-volume prescribers prescribed antibiotics to a larger share of their patient panel and their prescribing rate was 60% higher than that of lower-volume prescribers, indicating that their prescribing practices might be independent of the number of beneficiaries under their care,” Katryna A. Gouin, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
In 2019, 41% of all Part D antibiotics – that’s 24.4 million prescriptions – were prescribed by 69,835 higher-volume prescribers. The other 59% of all antibiotics were prescribed by the 627,000 lower-volume health care providers included in the analysis (those who prescribed fewer than 11 antibiotics were excluded), Ms. Gouin of Chenega in Anchorage, Alaska, and associates noted.
The analysis involved the Medicare Part D Prescribers by Provider data set and defined the highest-volume prescribers “as those in the highest 10th percentile of prescriber-level antibiotic volume (number of antibiotic prescriptions filled) across all Medicare providers nationwide,” the investigators explained.
The antibiotic-prescribing rate for the higher-volume prescribers was 680 prescriptions per 1,000 beneficiaries, which was 60% higher than the 426 prescriptions per 1,000 among the lower 90% of prescribers. Another way to look at it: The top 10% of health care providers “wrote a median of 284 antibiotic prescriptions, compared with a median of 41 among lower-volume prescribers,” the investigators said.
Physicians in internal medicine and family practice, the two largest medical specialties, were the most likely to be 10-percenters, accounting for 24.6% and 27.5%, respectively, of the higher-volume group. They were followed by nurse practitioners (14.1%) and physician assistants (7.4%), who were classified as specialists for the purposes of the study, Ms. Gouin and associates said.
The only other group of physicians among the top six specialties were urologists, who represented 6.8% of high-volume prescribers but only 1% of all prescribers, they noted.
The highest antibiotic prescription rate in the six largest groups of providers occurred among dentists, whose highest-prescribing practitioners wrote 1,271 prescriptions per 1,000 beneficiaries. Even the lower-prescribing 90% of dentists prescribed more antibiotics (1,068 per 1,000) than did the higher-prescribing family physicians (611 per 1,000) and internists (590 per 1,000), the researchers said.
The prescribing rates for all the other specialties that were not included separately also were higher than the family physicians’ and internists’. These rates were 850 per 1,000 beneficiaries for the higher-prescribers and 360 per 1,000 for the lower-prescribers, the researchers wrote.
The considerable differences in prescribing practices between specialties and even among those of the same specialty present “opportunities for improved prescribing through antibiotic stewardship activities focusing on these higher-volume prescribers, independent of specialty,” Ms. Gouin and associates wrote.
“Higher-volume prescribers prescribed antibiotics to a larger share of their patient panel and their prescribing rate was 60% higher than that of lower-volume prescribers, indicating that their prescribing practices might be independent of the number of beneficiaries under their care,” Katryna A. Gouin, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
In 2019, 41% of all Part D antibiotics – that’s 24.4 million prescriptions – were prescribed by 69,835 higher-volume prescribers. The other 59% of all antibiotics were prescribed by the 627,000 lower-volume health care providers included in the analysis (those who prescribed fewer than 11 antibiotics were excluded), Ms. Gouin of Chenega in Anchorage, Alaska, and associates noted.
The analysis involved the Medicare Part D Prescribers by Provider data set and defined the highest-volume prescribers “as those in the highest 10th percentile of prescriber-level antibiotic volume (number of antibiotic prescriptions filled) across all Medicare providers nationwide,” the investigators explained.
The antibiotic-prescribing rate for the higher-volume prescribers was 680 prescriptions per 1,000 beneficiaries, which was 60% higher than the 426 prescriptions per 1,000 among the lower 90% of prescribers. Another way to look at it: The top 10% of health care providers “wrote a median of 284 antibiotic prescriptions, compared with a median of 41 among lower-volume prescribers,” the investigators said.
Physicians in internal medicine and family practice, the two largest medical specialties, were the most likely to be 10-percenters, accounting for 24.6% and 27.5%, respectively, of the higher-volume group. They were followed by nurse practitioners (14.1%) and physician assistants (7.4%), who were classified as specialists for the purposes of the study, Ms. Gouin and associates said.
The only other group of physicians among the top six specialties were urologists, who represented 6.8% of high-volume prescribers but only 1% of all prescribers, they noted.
The highest antibiotic prescription rate in the six largest groups of providers occurred among dentists, whose highest-prescribing practitioners wrote 1,271 prescriptions per 1,000 beneficiaries. Even the lower-prescribing 90% of dentists prescribed more antibiotics (1,068 per 1,000) than did the higher-prescribing family physicians (611 per 1,000) and internists (590 per 1,000), the researchers said.
The prescribing rates for all the other specialties that were not included separately also were higher than the family physicians’ and internists’. These rates were 850 per 1,000 beneficiaries for the higher-prescribers and 360 per 1,000 for the lower-prescribers, the researchers wrote.
The considerable differences in prescribing practices between specialties and even among those of the same specialty present “opportunities for improved prescribing through antibiotic stewardship activities focusing on these higher-volume prescribers, independent of specialty,” Ms. Gouin and associates wrote.
“Higher-volume prescribers prescribed antibiotics to a larger share of their patient panel and their prescribing rate was 60% higher than that of lower-volume prescribers, indicating that their prescribing practices might be independent of the number of beneficiaries under their care,” Katryna A. Gouin, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
In 2019, 41% of all Part D antibiotics – that’s 24.4 million prescriptions – were prescribed by 69,835 higher-volume prescribers. The other 59% of all antibiotics were prescribed by the 627,000 lower-volume health care providers included in the analysis (those who prescribed fewer than 11 antibiotics were excluded), Ms. Gouin of Chenega in Anchorage, Alaska, and associates noted.
The analysis involved the Medicare Part D Prescribers by Provider data set and defined the highest-volume prescribers “as those in the highest 10th percentile of prescriber-level antibiotic volume (number of antibiotic prescriptions filled) across all Medicare providers nationwide,” the investigators explained.
The antibiotic-prescribing rate for the higher-volume prescribers was 680 prescriptions per 1,000 beneficiaries, which was 60% higher than the 426 prescriptions per 1,000 among the lower 90% of prescribers. Another way to look at it: The top 10% of health care providers “wrote a median of 284 antibiotic prescriptions, compared with a median of 41 among lower-volume prescribers,” the investigators said.
Physicians in internal medicine and family practice, the two largest medical specialties, were the most likely to be 10-percenters, accounting for 24.6% and 27.5%, respectively, of the higher-volume group. They were followed by nurse practitioners (14.1%) and physician assistants (7.4%), who were classified as specialists for the purposes of the study, Ms. Gouin and associates said.
The only other group of physicians among the top six specialties were urologists, who represented 6.8% of high-volume prescribers but only 1% of all prescribers, they noted.
The highest antibiotic prescription rate in the six largest groups of providers occurred among dentists, whose highest-prescribing practitioners wrote 1,271 prescriptions per 1,000 beneficiaries. Even the lower-prescribing 90% of dentists prescribed more antibiotics (1,068 per 1,000) than did the higher-prescribing family physicians (611 per 1,000) and internists (590 per 1,000), the researchers said.
The prescribing rates for all the other specialties that were not included separately also were higher than the family physicians’ and internists’. These rates were 850 per 1,000 beneficiaries for the higher-prescribers and 360 per 1,000 for the lower-prescribers, the researchers wrote.
The considerable differences in prescribing practices between specialties and even among those of the same specialty present “opportunities for improved prescribing through antibiotic stewardship activities focusing on these higher-volume prescribers, independent of specialty,” Ms. Gouin and associates wrote.
FROM THE MMWR
FDA okays 6-month implanted Eversense CGM for diabetes
The U.S. Food and Drug Administration has approved a new second-generation version of the implanted continuous glucose monitoring (CGM) system Eversense (Senseonics) that lasts for 6 months.
The Eversense E3 CGM system doubles the wear time from 3 months with the previous Eversense device approved in the United States in 2018. As before, the new system is approved for adults with diabetes aged 18 years and older.
This means that it will be the longest lasting CGM system available in the United States, with essentially two sensor insertion and removal procedures per year, the company said.
Data from the pivotal PROMISE trial of the 6-month version were presented at the American Diabetes Association Scientific Sessions in 2021, as reported by this news organization.
An older 6-month wear time version (Eversense XL) has been available in Europe since 2017. The new second-generation 6-month system is currently under regulatory review there.
The PROMISE trial included 181 participants with diabetes, about two-thirds with type 1 and one-third with type 2 diabetes, at eight clinical research sites.
“We repeatedly hear from our patients with diabetes that what they desire is a long-lasting sensor that is also highly accurate ... The next generation Eversense E3 System delivers on both,” said PROMISE study principal investigator Satish Garg, MD, professor of medicine and director of the adult diabetes program at the Barbara Davis Center, University of Colorado, Aurora, in a company press release.
The Eversense E3 consists of a fluorescence-based sensor, a transmitter, and a smartphone app that displays glucose values, trends, and alerts. The sensor is inserted subcutaneously into the upper arm by a certified health care professional in a brief office procedure. The transmitter is placed on the skin on top of the sensor. Glucose data are sent to the app automatically every 5 minutes.
The system includes an on-body vibratory alert as well as alerts on the app for high and low blood glucose values. Eversense readings may be used for treatment decisions, but users still must perform fingerstick glucose checks for calibration.
The regulatory review for the Eversense E3 was delayed for a year due to the COVID-19 pandemic. It will be distributed in the United States through a partnership with Ascensia Diabetes Care beginning in the second quarter of 2022, according to a Senseonics statement.
In addition, “the company expects the majority of its expenses for 2022 to be for research and development for ongoing feasibility and pivotal clinical trials for additional products in its product pipeline, including the start of its 365-day pivotal trial.”
Health care providers who want to offer the Eversense CGM System to their patients can sign up here or call 844-SENSE4U (844-736-7348).
Patients interested in getting started on Eversense can sign up here and will be among the first to know when Eversense E3 is commercially available.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a new second-generation version of the implanted continuous glucose monitoring (CGM) system Eversense (Senseonics) that lasts for 6 months.
The Eversense E3 CGM system doubles the wear time from 3 months with the previous Eversense device approved in the United States in 2018. As before, the new system is approved for adults with diabetes aged 18 years and older.
This means that it will be the longest lasting CGM system available in the United States, with essentially two sensor insertion and removal procedures per year, the company said.
Data from the pivotal PROMISE trial of the 6-month version were presented at the American Diabetes Association Scientific Sessions in 2021, as reported by this news organization.
An older 6-month wear time version (Eversense XL) has been available in Europe since 2017. The new second-generation 6-month system is currently under regulatory review there.
The PROMISE trial included 181 participants with diabetes, about two-thirds with type 1 and one-third with type 2 diabetes, at eight clinical research sites.
“We repeatedly hear from our patients with diabetes that what they desire is a long-lasting sensor that is also highly accurate ... The next generation Eversense E3 System delivers on both,” said PROMISE study principal investigator Satish Garg, MD, professor of medicine and director of the adult diabetes program at the Barbara Davis Center, University of Colorado, Aurora, in a company press release.
The Eversense E3 consists of a fluorescence-based sensor, a transmitter, and a smartphone app that displays glucose values, trends, and alerts. The sensor is inserted subcutaneously into the upper arm by a certified health care professional in a brief office procedure. The transmitter is placed on the skin on top of the sensor. Glucose data are sent to the app automatically every 5 minutes.
The system includes an on-body vibratory alert as well as alerts on the app for high and low blood glucose values. Eversense readings may be used for treatment decisions, but users still must perform fingerstick glucose checks for calibration.
The regulatory review for the Eversense E3 was delayed for a year due to the COVID-19 pandemic. It will be distributed in the United States through a partnership with Ascensia Diabetes Care beginning in the second quarter of 2022, according to a Senseonics statement.
In addition, “the company expects the majority of its expenses for 2022 to be for research and development for ongoing feasibility and pivotal clinical trials for additional products in its product pipeline, including the start of its 365-day pivotal trial.”
Health care providers who want to offer the Eversense CGM System to their patients can sign up here or call 844-SENSE4U (844-736-7348).
Patients interested in getting started on Eversense can sign up here and will be among the first to know when Eversense E3 is commercially available.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a new second-generation version of the implanted continuous glucose monitoring (CGM) system Eversense (Senseonics) that lasts for 6 months.
The Eversense E3 CGM system doubles the wear time from 3 months with the previous Eversense device approved in the United States in 2018. As before, the new system is approved for adults with diabetes aged 18 years and older.
This means that it will be the longest lasting CGM system available in the United States, with essentially two sensor insertion and removal procedures per year, the company said.
Data from the pivotal PROMISE trial of the 6-month version were presented at the American Diabetes Association Scientific Sessions in 2021, as reported by this news organization.
An older 6-month wear time version (Eversense XL) has been available in Europe since 2017. The new second-generation 6-month system is currently under regulatory review there.
The PROMISE trial included 181 participants with diabetes, about two-thirds with type 1 and one-third with type 2 diabetes, at eight clinical research sites.
“We repeatedly hear from our patients with diabetes that what they desire is a long-lasting sensor that is also highly accurate ... The next generation Eversense E3 System delivers on both,” said PROMISE study principal investigator Satish Garg, MD, professor of medicine and director of the adult diabetes program at the Barbara Davis Center, University of Colorado, Aurora, in a company press release.
The Eversense E3 consists of a fluorescence-based sensor, a transmitter, and a smartphone app that displays glucose values, trends, and alerts. The sensor is inserted subcutaneously into the upper arm by a certified health care professional in a brief office procedure. The transmitter is placed on the skin on top of the sensor. Glucose data are sent to the app automatically every 5 minutes.
The system includes an on-body vibratory alert as well as alerts on the app for high and low blood glucose values. Eversense readings may be used for treatment decisions, but users still must perform fingerstick glucose checks for calibration.
The regulatory review for the Eversense E3 was delayed for a year due to the COVID-19 pandemic. It will be distributed in the United States through a partnership with Ascensia Diabetes Care beginning in the second quarter of 2022, according to a Senseonics statement.
In addition, “the company expects the majority of its expenses for 2022 to be for research and development for ongoing feasibility and pivotal clinical trials for additional products in its product pipeline, including the start of its 365-day pivotal trial.”
Health care providers who want to offer the Eversense CGM System to their patients can sign up here or call 844-SENSE4U (844-736-7348).
Patients interested in getting started on Eversense can sign up here and will be among the first to know when Eversense E3 is commercially available.
A version of this article first appeared on Medscape.com.
Study questions need for repeat Lp(a) testing
Repeat testing of lipoprotein(a) to assess a patient’s cardiovascular risk doesn’t seem to yield any additional helpful information, and a one-time baseline measure of Lp(a) molar concentration could be sufficient to help define lifetime risk, suggests a large analysis of a national database in the United Kingdom.
The study examined the correlation between baseline and first follow-up measures of Lp(a) molar concentration and incident coronary artery disease among 16,017 individuals in a cohort of the UK Biobank, a prospective observational study of about 500,000 middle-aged people recruited between 2006 and 2010 with ongoing follow-up.
Results showed found little change in Lp(a) molar concentration measures from baseline to an average of 4.4 years afterward, but did find an association between statin usage and significant increases in Lp(a) in people with high baseline levels. The study was published online on Feb. 14 in the Journal of the American College of Cardiology.
The baseline and follow-up Lp(a) molar concentration measures “are highly correlated with 85% of the repeat values being within 25 nmol/L of each other,” senior author Pradeep Natarajan, MD, MMSc, of Massachusetts General Hospital, Boston, said in an interview. “When predicting events, the follow-up Lp(a) concentration did not yield additional information beyond the baseline Lp(a).”
Additionally, the study found that statin therapy didn’t lead to meaningful changes in Lp(a) molar concentration levels. Patients on statins who had baseline Lp(a) above 70 nmol/L “had modest follow-up concentrations, but this did not appreciably change atherosclerotic cardiovascular disease risks,” Dr. Natarajan said. “For patients without clinical cardiovascular disease who are not on medicines that markedly change Lp(a), additional Lp(a) assessments are unlikely to provide additional prognostic information beyond the baseline Lp(a) measurement.”
Added lead author Mark Trinder, MSc: “These findings suggest that, in the absence of therapies substantially altering Lp(a), a single accurate measurement of Lp(a) molar concentration is an efficient method to inform atherosclerotic cardiovascular disease risk.” Mr. Trinder is an MD/PhD candidate at the Centre for Heart Lung Innovation at the University of British Columbia, Vancouver, and a visiting scholar in medical and population genetics and the Cardiovascular Disease Initiative at the Broad Institute of MIT and Harvard in Cambridge, Mass.
This study claims to be unique for two reasons: It reported on repeat Lp(a) measurements among the general population rather than a clinical trial, and it assessed the influence of statins on Lp(a) molar concentration rather than Lp(a) mass.
“Lp(a) molar concentration aims to mitigate challenges with mass assays, which are influenced by assay size,” Dr. Natarajan said. However, he noted that major clinical trials of investigative drugs for lowering Lp(a), specifically the ongoing HORIZON trial (NCT04023552), are using Lp(a) mass rather than molar concentration.
“There is an imperfect correlation between the two,” Dr. Natarajan said. “Depending on the results of this trial and others, and evaluation of both mass and molar concentration assays, we will then be able to better understand the path forward. These issues and the multiple assays have been challenging for both the clinical and scientific community.”
Santica Marcovina, ScD, PhD, coauthor of the invited commentary (J Am Coll Cardiol. 2022 Feb 14. doi: 10.1016/j.jacc.2021.11.053), said in an interview that the study’s major contribution to the literature is the finding that the molar concentration of Lp(a) appears to be stable regardless of statin use. “This important finding provides evidence that no longitudinal measurements of Lp(a) are needed in the primary prevention of atherosclerotic CVD and that once-in-a-lifetime measurement may reliably allow clinicians to assess whether or not Lp(a)-related risk is present in their patients,” she said. Dr. Marcovina is senior director of clinical laboratory sciences at Medpace Reference Laboratories, Cincinnati.
She noted that this study provides an actionable strategy for cardiologists. “Considering the clinical benefits, the relative low cost for measuring Lp(a), the fact that measurements need to be performed only once in the vast majority of individuals, all point to the implementation of Lp(a) general screening as soon as possible.”
Dr. Natarajan has financial relationships with Amgen, Apple, AstraZeneca, Boston Scientific, Blackstone Life Sciences, Genentech and Novartis. Dr. Marcovina has provided consulting for Roche, Denka, and Novartis, and has received research support from Amgen through Medpace.
Repeat testing of lipoprotein(a) to assess a patient’s cardiovascular risk doesn’t seem to yield any additional helpful information, and a one-time baseline measure of Lp(a) molar concentration could be sufficient to help define lifetime risk, suggests a large analysis of a national database in the United Kingdom.
The study examined the correlation between baseline and first follow-up measures of Lp(a) molar concentration and incident coronary artery disease among 16,017 individuals in a cohort of the UK Biobank, a prospective observational study of about 500,000 middle-aged people recruited between 2006 and 2010 with ongoing follow-up.
Results showed found little change in Lp(a) molar concentration measures from baseline to an average of 4.4 years afterward, but did find an association between statin usage and significant increases in Lp(a) in people with high baseline levels. The study was published online on Feb. 14 in the Journal of the American College of Cardiology.
The baseline and follow-up Lp(a) molar concentration measures “are highly correlated with 85% of the repeat values being within 25 nmol/L of each other,” senior author Pradeep Natarajan, MD, MMSc, of Massachusetts General Hospital, Boston, said in an interview. “When predicting events, the follow-up Lp(a) concentration did not yield additional information beyond the baseline Lp(a).”
Additionally, the study found that statin therapy didn’t lead to meaningful changes in Lp(a) molar concentration levels. Patients on statins who had baseline Lp(a) above 70 nmol/L “had modest follow-up concentrations, but this did not appreciably change atherosclerotic cardiovascular disease risks,” Dr. Natarajan said. “For patients without clinical cardiovascular disease who are not on medicines that markedly change Lp(a), additional Lp(a) assessments are unlikely to provide additional prognostic information beyond the baseline Lp(a) measurement.”
Added lead author Mark Trinder, MSc: “These findings suggest that, in the absence of therapies substantially altering Lp(a), a single accurate measurement of Lp(a) molar concentration is an efficient method to inform atherosclerotic cardiovascular disease risk.” Mr. Trinder is an MD/PhD candidate at the Centre for Heart Lung Innovation at the University of British Columbia, Vancouver, and a visiting scholar in medical and population genetics and the Cardiovascular Disease Initiative at the Broad Institute of MIT and Harvard in Cambridge, Mass.
This study claims to be unique for two reasons: It reported on repeat Lp(a) measurements among the general population rather than a clinical trial, and it assessed the influence of statins on Lp(a) molar concentration rather than Lp(a) mass.
“Lp(a) molar concentration aims to mitigate challenges with mass assays, which are influenced by assay size,” Dr. Natarajan said. However, he noted that major clinical trials of investigative drugs for lowering Lp(a), specifically the ongoing HORIZON trial (NCT04023552), are using Lp(a) mass rather than molar concentration.
“There is an imperfect correlation between the two,” Dr. Natarajan said. “Depending on the results of this trial and others, and evaluation of both mass and molar concentration assays, we will then be able to better understand the path forward. These issues and the multiple assays have been challenging for both the clinical and scientific community.”
Santica Marcovina, ScD, PhD, coauthor of the invited commentary (J Am Coll Cardiol. 2022 Feb 14. doi: 10.1016/j.jacc.2021.11.053), said in an interview that the study’s major contribution to the literature is the finding that the molar concentration of Lp(a) appears to be stable regardless of statin use. “This important finding provides evidence that no longitudinal measurements of Lp(a) are needed in the primary prevention of atherosclerotic CVD and that once-in-a-lifetime measurement may reliably allow clinicians to assess whether or not Lp(a)-related risk is present in their patients,” she said. Dr. Marcovina is senior director of clinical laboratory sciences at Medpace Reference Laboratories, Cincinnati.
She noted that this study provides an actionable strategy for cardiologists. “Considering the clinical benefits, the relative low cost for measuring Lp(a), the fact that measurements need to be performed only once in the vast majority of individuals, all point to the implementation of Lp(a) general screening as soon as possible.”
Dr. Natarajan has financial relationships with Amgen, Apple, AstraZeneca, Boston Scientific, Blackstone Life Sciences, Genentech and Novartis. Dr. Marcovina has provided consulting for Roche, Denka, and Novartis, and has received research support from Amgen through Medpace.
Repeat testing of lipoprotein(a) to assess a patient’s cardiovascular risk doesn’t seem to yield any additional helpful information, and a one-time baseline measure of Lp(a) molar concentration could be sufficient to help define lifetime risk, suggests a large analysis of a national database in the United Kingdom.
The study examined the correlation between baseline and first follow-up measures of Lp(a) molar concentration and incident coronary artery disease among 16,017 individuals in a cohort of the UK Biobank, a prospective observational study of about 500,000 middle-aged people recruited between 2006 and 2010 with ongoing follow-up.
Results showed found little change in Lp(a) molar concentration measures from baseline to an average of 4.4 years afterward, but did find an association between statin usage and significant increases in Lp(a) in people with high baseline levels. The study was published online on Feb. 14 in the Journal of the American College of Cardiology.
The baseline and follow-up Lp(a) molar concentration measures “are highly correlated with 85% of the repeat values being within 25 nmol/L of each other,” senior author Pradeep Natarajan, MD, MMSc, of Massachusetts General Hospital, Boston, said in an interview. “When predicting events, the follow-up Lp(a) concentration did not yield additional information beyond the baseline Lp(a).”
Additionally, the study found that statin therapy didn’t lead to meaningful changes in Lp(a) molar concentration levels. Patients on statins who had baseline Lp(a) above 70 nmol/L “had modest follow-up concentrations, but this did not appreciably change atherosclerotic cardiovascular disease risks,” Dr. Natarajan said. “For patients without clinical cardiovascular disease who are not on medicines that markedly change Lp(a), additional Lp(a) assessments are unlikely to provide additional prognostic information beyond the baseline Lp(a) measurement.”
Added lead author Mark Trinder, MSc: “These findings suggest that, in the absence of therapies substantially altering Lp(a), a single accurate measurement of Lp(a) molar concentration is an efficient method to inform atherosclerotic cardiovascular disease risk.” Mr. Trinder is an MD/PhD candidate at the Centre for Heart Lung Innovation at the University of British Columbia, Vancouver, and a visiting scholar in medical and population genetics and the Cardiovascular Disease Initiative at the Broad Institute of MIT and Harvard in Cambridge, Mass.
This study claims to be unique for two reasons: It reported on repeat Lp(a) measurements among the general population rather than a clinical trial, and it assessed the influence of statins on Lp(a) molar concentration rather than Lp(a) mass.
“Lp(a) molar concentration aims to mitigate challenges with mass assays, which are influenced by assay size,” Dr. Natarajan said. However, he noted that major clinical trials of investigative drugs for lowering Lp(a), specifically the ongoing HORIZON trial (NCT04023552), are using Lp(a) mass rather than molar concentration.
“There is an imperfect correlation between the two,” Dr. Natarajan said. “Depending on the results of this trial and others, and evaluation of both mass and molar concentration assays, we will then be able to better understand the path forward. These issues and the multiple assays have been challenging for both the clinical and scientific community.”
Santica Marcovina, ScD, PhD, coauthor of the invited commentary (J Am Coll Cardiol. 2022 Feb 14. doi: 10.1016/j.jacc.2021.11.053), said in an interview that the study’s major contribution to the literature is the finding that the molar concentration of Lp(a) appears to be stable regardless of statin use. “This important finding provides evidence that no longitudinal measurements of Lp(a) are needed in the primary prevention of atherosclerotic CVD and that once-in-a-lifetime measurement may reliably allow clinicians to assess whether or not Lp(a)-related risk is present in their patients,” she said. Dr. Marcovina is senior director of clinical laboratory sciences at Medpace Reference Laboratories, Cincinnati.
She noted that this study provides an actionable strategy for cardiologists. “Considering the clinical benefits, the relative low cost for measuring Lp(a), the fact that measurements need to be performed only once in the vast majority of individuals, all point to the implementation of Lp(a) general screening as soon as possible.”
Dr. Natarajan has financial relationships with Amgen, Apple, AstraZeneca, Boston Scientific, Blackstone Life Sciences, Genentech and Novartis. Dr. Marcovina has provided consulting for Roche, Denka, and Novartis, and has received research support from Amgen through Medpace.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Body fat linked to lower bone density, particularly in men
an analysis of data from a large, nationally representative sample has found.
Much previous research has suggested that obesity protects against fractures and loss of BMD for a variety of reasons, including the beneficial effects of weight-bearing on the skeleton and hormonal factors linked to body fat. But the new findings should prompt a reconsideration of the relationship between obesity and fracture risk, according to the investigators, whose study appears in the Journal of Clinical Endocrinology & Metabolism.
“While higher BMI [body mass index] is generally associated with higher bone density, our study demonstrates that lean and fat mass affect bone density differently and that obesity is not a guarantee against osteoporosis,” Rajesh K. Jain, MD, of the University of Chicago said in an interview.
Dr. Jain and a colleague, Tamara Vokes, MD, used multivariant modeling to examine the relationship between BMD and body composition of 10,814 men and women aged 20-59 years from the National Health and Nutrition Examination Survey (NHANES) 2011-2018. All underwent total body dual-energy x-ray absorptiometry scans.
Participants were stratified into sex-specific quartiles based on lean mass index (LMI; lean mass divided by height squared) and fat mass index (FMI; fat mass divided by height squared). Lean mass had a strong positive association with bone density, whereas fat mass had a moderate negative effect, the researchers found.
An additional kg/m2 of FMI was associated with a 0.10 lower T score, the number of standard deviations from the expected bone density of a young adult (P < .001). The negative effect was greater in men, who had a 0.13 lower T score per additional 1 kg/m2 of FMI, compared with 0.08 lower in women (P < .001). The effect was most pronounced in people in the highest FMI quartile.
Body composition is not a routine clinical measurement, Dr. Jain and Dr. Vokes noted. Prior studies of the effect of body composition on bone density have been limited by small patient numbers, referral bias, lack of racial or ethnic diversity, and the use of estimates rather than true measures of fat and lean tissue. NHANES is designed to mirror the U.S. population.
The researchers say when it comes to patients with obesity, the findings “should not dissuade clinicians from assessing bone density, particularly if other risk factors are present.”
Useful clinical proxies for body composition
Clinicians have no routine way to measure body composition in an office setting. As a result, Dr. Jain advised clinicians to look at factors that correlate with high body fat, such as the presence of diabetes, or with low lean mass, such as poor performance on physical activity measures like grip strength, when deciding whether to consider osteoporosis screening. Patients with obesity should undergo recommended bone density screening, especially if they have other risk factors such as older age, previous fracture, steroid use, or a family history of fracture.
Although some extra weight may have a beneficial loading effect, too much extra weight can lead to metabolic problems and restrict movement, according to Rodrigo J. Valderrábano, MD, medical director of clinical research for the Research Program in Men’s Health: Aging and Metabolism, Brigham and Women’s Hospital in Boston. “There’s a general sense that the extra weight is only good for your bones if you can carry it around,” said Dr. Valderrábano, who was not involved in the study.
More research is needed to understand why fat affects men and women differently, Dr. Jain noted. The researchers found that testosterone and estradiol values did not fully explain the variation.
Adipokines released by fat cells may be important in driving bone loss but were not measured in the study, Peter R. Ebeling, MD, president of the American Society of Bone and Mineral Research, said in an interview. Distribution of fractures in obesity suggests that a high FMI may preferentially affect cortical bone instead of trabecular bone, but further studies using high-resolution peripheral quantitative CT are required to confirm the difference.
Dr. Ebeling, who was not involved in the new study, agreed that the positive relationship between BMI and BMD has led to false reassurance that people with obesity may be protected from fragility fractures. “The take-home message for clinicians is that we should not neglect bone health in our patients with obesity, both male and female.”
Dr. Jain has reported receiving grant support from the Amgen Foundation and being a consultant for Radius Health. Dr. Vokes has reported being an investigator, consultant, and speaker for Radius Health, investigator and consultant for Takeda Pharmaceutical, and investigator for Ascendis Pharma. Dr. Valderrábano and Dr. Ebeling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
an analysis of data from a large, nationally representative sample has found.
Much previous research has suggested that obesity protects against fractures and loss of BMD for a variety of reasons, including the beneficial effects of weight-bearing on the skeleton and hormonal factors linked to body fat. But the new findings should prompt a reconsideration of the relationship between obesity and fracture risk, according to the investigators, whose study appears in the Journal of Clinical Endocrinology & Metabolism.
“While higher BMI [body mass index] is generally associated with higher bone density, our study demonstrates that lean and fat mass affect bone density differently and that obesity is not a guarantee against osteoporosis,” Rajesh K. Jain, MD, of the University of Chicago said in an interview.
Dr. Jain and a colleague, Tamara Vokes, MD, used multivariant modeling to examine the relationship between BMD and body composition of 10,814 men and women aged 20-59 years from the National Health and Nutrition Examination Survey (NHANES) 2011-2018. All underwent total body dual-energy x-ray absorptiometry scans.
Participants were stratified into sex-specific quartiles based on lean mass index (LMI; lean mass divided by height squared) and fat mass index (FMI; fat mass divided by height squared). Lean mass had a strong positive association with bone density, whereas fat mass had a moderate negative effect, the researchers found.
An additional kg/m2 of FMI was associated with a 0.10 lower T score, the number of standard deviations from the expected bone density of a young adult (P < .001). The negative effect was greater in men, who had a 0.13 lower T score per additional 1 kg/m2 of FMI, compared with 0.08 lower in women (P < .001). The effect was most pronounced in people in the highest FMI quartile.
Body composition is not a routine clinical measurement, Dr. Jain and Dr. Vokes noted. Prior studies of the effect of body composition on bone density have been limited by small patient numbers, referral bias, lack of racial or ethnic diversity, and the use of estimates rather than true measures of fat and lean tissue. NHANES is designed to mirror the U.S. population.
The researchers say when it comes to patients with obesity, the findings “should not dissuade clinicians from assessing bone density, particularly if other risk factors are present.”
Useful clinical proxies for body composition
Clinicians have no routine way to measure body composition in an office setting. As a result, Dr. Jain advised clinicians to look at factors that correlate with high body fat, such as the presence of diabetes, or with low lean mass, such as poor performance on physical activity measures like grip strength, when deciding whether to consider osteoporosis screening. Patients with obesity should undergo recommended bone density screening, especially if they have other risk factors such as older age, previous fracture, steroid use, or a family history of fracture.
Although some extra weight may have a beneficial loading effect, too much extra weight can lead to metabolic problems and restrict movement, according to Rodrigo J. Valderrábano, MD, medical director of clinical research for the Research Program in Men’s Health: Aging and Metabolism, Brigham and Women’s Hospital in Boston. “There’s a general sense that the extra weight is only good for your bones if you can carry it around,” said Dr. Valderrábano, who was not involved in the study.
More research is needed to understand why fat affects men and women differently, Dr. Jain noted. The researchers found that testosterone and estradiol values did not fully explain the variation.
Adipokines released by fat cells may be important in driving bone loss but were not measured in the study, Peter R. Ebeling, MD, president of the American Society of Bone and Mineral Research, said in an interview. Distribution of fractures in obesity suggests that a high FMI may preferentially affect cortical bone instead of trabecular bone, but further studies using high-resolution peripheral quantitative CT are required to confirm the difference.
Dr. Ebeling, who was not involved in the new study, agreed that the positive relationship between BMI and BMD has led to false reassurance that people with obesity may be protected from fragility fractures. “The take-home message for clinicians is that we should not neglect bone health in our patients with obesity, both male and female.”
Dr. Jain has reported receiving grant support from the Amgen Foundation and being a consultant for Radius Health. Dr. Vokes has reported being an investigator, consultant, and speaker for Radius Health, investigator and consultant for Takeda Pharmaceutical, and investigator for Ascendis Pharma. Dr. Valderrábano and Dr. Ebeling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
an analysis of data from a large, nationally representative sample has found.
Much previous research has suggested that obesity protects against fractures and loss of BMD for a variety of reasons, including the beneficial effects of weight-bearing on the skeleton and hormonal factors linked to body fat. But the new findings should prompt a reconsideration of the relationship between obesity and fracture risk, according to the investigators, whose study appears in the Journal of Clinical Endocrinology & Metabolism.
“While higher BMI [body mass index] is generally associated with higher bone density, our study demonstrates that lean and fat mass affect bone density differently and that obesity is not a guarantee against osteoporosis,” Rajesh K. Jain, MD, of the University of Chicago said in an interview.
Dr. Jain and a colleague, Tamara Vokes, MD, used multivariant modeling to examine the relationship between BMD and body composition of 10,814 men and women aged 20-59 years from the National Health and Nutrition Examination Survey (NHANES) 2011-2018. All underwent total body dual-energy x-ray absorptiometry scans.
Participants were stratified into sex-specific quartiles based on lean mass index (LMI; lean mass divided by height squared) and fat mass index (FMI; fat mass divided by height squared). Lean mass had a strong positive association with bone density, whereas fat mass had a moderate negative effect, the researchers found.
An additional kg/m2 of FMI was associated with a 0.10 lower T score, the number of standard deviations from the expected bone density of a young adult (P < .001). The negative effect was greater in men, who had a 0.13 lower T score per additional 1 kg/m2 of FMI, compared with 0.08 lower in women (P < .001). The effect was most pronounced in people in the highest FMI quartile.
Body composition is not a routine clinical measurement, Dr. Jain and Dr. Vokes noted. Prior studies of the effect of body composition on bone density have been limited by small patient numbers, referral bias, lack of racial or ethnic diversity, and the use of estimates rather than true measures of fat and lean tissue. NHANES is designed to mirror the U.S. population.
The researchers say when it comes to patients with obesity, the findings “should not dissuade clinicians from assessing bone density, particularly if other risk factors are present.”
Useful clinical proxies for body composition
Clinicians have no routine way to measure body composition in an office setting. As a result, Dr. Jain advised clinicians to look at factors that correlate with high body fat, such as the presence of diabetes, or with low lean mass, such as poor performance on physical activity measures like grip strength, when deciding whether to consider osteoporosis screening. Patients with obesity should undergo recommended bone density screening, especially if they have other risk factors such as older age, previous fracture, steroid use, or a family history of fracture.
Although some extra weight may have a beneficial loading effect, too much extra weight can lead to metabolic problems and restrict movement, according to Rodrigo J. Valderrábano, MD, medical director of clinical research for the Research Program in Men’s Health: Aging and Metabolism, Brigham and Women’s Hospital in Boston. “There’s a general sense that the extra weight is only good for your bones if you can carry it around,” said Dr. Valderrábano, who was not involved in the study.
More research is needed to understand why fat affects men and women differently, Dr. Jain noted. The researchers found that testosterone and estradiol values did not fully explain the variation.
Adipokines released by fat cells may be important in driving bone loss but were not measured in the study, Peter R. Ebeling, MD, president of the American Society of Bone and Mineral Research, said in an interview. Distribution of fractures in obesity suggests that a high FMI may preferentially affect cortical bone instead of trabecular bone, but further studies using high-resolution peripheral quantitative CT are required to confirm the difference.
Dr. Ebeling, who was not involved in the new study, agreed that the positive relationship between BMI and BMD has led to false reassurance that people with obesity may be protected from fragility fractures. “The take-home message for clinicians is that we should not neglect bone health in our patients with obesity, both male and female.”
Dr. Jain has reported receiving grant support from the Amgen Foundation and being a consultant for Radius Health. Dr. Vokes has reported being an investigator, consultant, and speaker for Radius Health, investigator and consultant for Takeda Pharmaceutical, and investigator for Ascendis Pharma. Dr. Valderrábano and Dr. Ebeling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM












