User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
U.S. mothers underestimate role breastfeeding plays in curbing breast cancer
The majority of women in the United States remain unaware of the benefits breastfeeding offers in reducing the risk of breast cancer, reported Adrienne Hoyt-Austin, DO, and colleagues at University of California, Davis.
Using nationally representative data collected from the 2015-2017 National Survey of Family Growth, Dr. Hoyt-Austin and colleagues analyzed responses to the question: “Do you think that breastfeeding decreases a woman’s chances of getting breast cancer a lot, a little, or not at all, no opinion, or don’t know?” A total of 5,554 female respondents aged 15-49 years participated. The response rate was 66.7%.
Multiparous status and education play a role in decreased awareness
Those who had given birth more than once, who had no more than a high school education, or who were U.S.-born Hispanic had the lowest level of awareness, believing that breastfeeding offers only “a little” protection. Of those who were aware of the link, 44% reported that breastfeeding provides “a lot” of protection, and foreign-born participants as well as those who breastfed for more than a year were more likely to conclude that breastfeeding offers “a lot” of protection. The researchers found that neither mammogram or personal family history of breast cancer had any bearing on awareness.
Although multiple studies have found breastfeeding to confer a lower rate of cancer risk, morbidity and mortality, with a 26% lower lifetime risk for those mothers who breastfeed for 12 months or longer, only 36% of women in the United States actually breastfeed.
Limited data indicate whether respondents were breastfed themselves
“Public health initiatives must consider the complex roots of disparities in breastfeeding,” noted Dr. Hoyt-Austin and colleagues. They acknowledged the subjectivity of perceptions of “a lot” versus “a little” and noted that the study was limited by a lack of data on whether participants were breastfed themselves.
Clinicians have an opportunity to play a key role in better educating families concerning the benefits of breastfeeding, both for mother and child, they advised. According to one recent study, just 5 minutes of counseling on the benefits of breastfeeding “significantly strengthened women’s intentions to breastfeed.
In a separate interview, Amy E. Cyr, MD, FACS, section of surgical oncology at Washington University, St. Louis, noted that “many breast cancer risk factors – age, sex, family history, and age of menopause – are nonmodifiable.” And while other risk factors, including alcohol use, diet, and exercise are controllable, “pregnancies and breastfeeding don’t always go as planned,” Dr. Cyr added.
“Although Dr. Hoyt-Austin et al. observed that many women aren’t aware that breastfeeding decreases breast cancer risk – or to what extent (they cite a 26% cancer risk reduction after 12 or more months of breastfeeding) – most studies haven’t shown that large a drop in breast cancer risk,“ she pointed out, adding that “I think it’s an overstatement to suggest that breastfeeding reduces cancer risk by ‘a lot,’ as one of the survey choices offered in the study suggests.”
Whether or not a woman breastfeeds depends not only on desire but on social and economic support and biology; for some, breastfeeding simply isn’t an option. “I agree that we should educate women about the benefits of breastfeeding so they can make an informed decision for themselves and their infants, but we also need to acknowledge the complexity of this issue,” she cautioned.
One coauthor reported a travel stipend by the Human Milk Banking Association of North America; Dr. Hoyt-Austin and the other authors had no conflicts of interest to report. Dr. Cyr had no conflicts of interest to report.
SOURCE: Hoyt-Austin A et al. Obstet Gynecol. 2020 Dec. doi: 10.1097/AOG.0000000000004162.
The majority of women in the United States remain unaware of the benefits breastfeeding offers in reducing the risk of breast cancer, reported Adrienne Hoyt-Austin, DO, and colleagues at University of California, Davis.
Using nationally representative data collected from the 2015-2017 National Survey of Family Growth, Dr. Hoyt-Austin and colleagues analyzed responses to the question: “Do you think that breastfeeding decreases a woman’s chances of getting breast cancer a lot, a little, or not at all, no opinion, or don’t know?” A total of 5,554 female respondents aged 15-49 years participated. The response rate was 66.7%.
Multiparous status and education play a role in decreased awareness
Those who had given birth more than once, who had no more than a high school education, or who were U.S.-born Hispanic had the lowest level of awareness, believing that breastfeeding offers only “a little” protection. Of those who were aware of the link, 44% reported that breastfeeding provides “a lot” of protection, and foreign-born participants as well as those who breastfed for more than a year were more likely to conclude that breastfeeding offers “a lot” of protection. The researchers found that neither mammogram or personal family history of breast cancer had any bearing on awareness.
Although multiple studies have found breastfeeding to confer a lower rate of cancer risk, morbidity and mortality, with a 26% lower lifetime risk for those mothers who breastfeed for 12 months or longer, only 36% of women in the United States actually breastfeed.
Limited data indicate whether respondents were breastfed themselves
“Public health initiatives must consider the complex roots of disparities in breastfeeding,” noted Dr. Hoyt-Austin and colleagues. They acknowledged the subjectivity of perceptions of “a lot” versus “a little” and noted that the study was limited by a lack of data on whether participants were breastfed themselves.
Clinicians have an opportunity to play a key role in better educating families concerning the benefits of breastfeeding, both for mother and child, they advised. According to one recent study, just 5 minutes of counseling on the benefits of breastfeeding “significantly strengthened women’s intentions to breastfeed.
In a separate interview, Amy E. Cyr, MD, FACS, section of surgical oncology at Washington University, St. Louis, noted that “many breast cancer risk factors – age, sex, family history, and age of menopause – are nonmodifiable.” And while other risk factors, including alcohol use, diet, and exercise are controllable, “pregnancies and breastfeeding don’t always go as planned,” Dr. Cyr added.
“Although Dr. Hoyt-Austin et al. observed that many women aren’t aware that breastfeeding decreases breast cancer risk – or to what extent (they cite a 26% cancer risk reduction after 12 or more months of breastfeeding) – most studies haven’t shown that large a drop in breast cancer risk,“ she pointed out, adding that “I think it’s an overstatement to suggest that breastfeeding reduces cancer risk by ‘a lot,’ as one of the survey choices offered in the study suggests.”
Whether or not a woman breastfeeds depends not only on desire but on social and economic support and biology; for some, breastfeeding simply isn’t an option. “I agree that we should educate women about the benefits of breastfeeding so they can make an informed decision for themselves and their infants, but we also need to acknowledge the complexity of this issue,” she cautioned.
One coauthor reported a travel stipend by the Human Milk Banking Association of North America; Dr. Hoyt-Austin and the other authors had no conflicts of interest to report. Dr. Cyr had no conflicts of interest to report.
SOURCE: Hoyt-Austin A et al. Obstet Gynecol. 2020 Dec. doi: 10.1097/AOG.0000000000004162.
The majority of women in the United States remain unaware of the benefits breastfeeding offers in reducing the risk of breast cancer, reported Adrienne Hoyt-Austin, DO, and colleagues at University of California, Davis.
Using nationally representative data collected from the 2015-2017 National Survey of Family Growth, Dr. Hoyt-Austin and colleagues analyzed responses to the question: “Do you think that breastfeeding decreases a woman’s chances of getting breast cancer a lot, a little, or not at all, no opinion, or don’t know?” A total of 5,554 female respondents aged 15-49 years participated. The response rate was 66.7%.
Multiparous status and education play a role in decreased awareness
Those who had given birth more than once, who had no more than a high school education, or who were U.S.-born Hispanic had the lowest level of awareness, believing that breastfeeding offers only “a little” protection. Of those who were aware of the link, 44% reported that breastfeeding provides “a lot” of protection, and foreign-born participants as well as those who breastfed for more than a year were more likely to conclude that breastfeeding offers “a lot” of protection. The researchers found that neither mammogram or personal family history of breast cancer had any bearing on awareness.
Although multiple studies have found breastfeeding to confer a lower rate of cancer risk, morbidity and mortality, with a 26% lower lifetime risk for those mothers who breastfeed for 12 months or longer, only 36% of women in the United States actually breastfeed.
Limited data indicate whether respondents were breastfed themselves
“Public health initiatives must consider the complex roots of disparities in breastfeeding,” noted Dr. Hoyt-Austin and colleagues. They acknowledged the subjectivity of perceptions of “a lot” versus “a little” and noted that the study was limited by a lack of data on whether participants were breastfed themselves.
Clinicians have an opportunity to play a key role in better educating families concerning the benefits of breastfeeding, both for mother and child, they advised. According to one recent study, just 5 minutes of counseling on the benefits of breastfeeding “significantly strengthened women’s intentions to breastfeed.
In a separate interview, Amy E. Cyr, MD, FACS, section of surgical oncology at Washington University, St. Louis, noted that “many breast cancer risk factors – age, sex, family history, and age of menopause – are nonmodifiable.” And while other risk factors, including alcohol use, diet, and exercise are controllable, “pregnancies and breastfeeding don’t always go as planned,” Dr. Cyr added.
“Although Dr. Hoyt-Austin et al. observed that many women aren’t aware that breastfeeding decreases breast cancer risk – or to what extent (they cite a 26% cancer risk reduction after 12 or more months of breastfeeding) – most studies haven’t shown that large a drop in breast cancer risk,“ she pointed out, adding that “I think it’s an overstatement to suggest that breastfeeding reduces cancer risk by ‘a lot,’ as one of the survey choices offered in the study suggests.”
Whether or not a woman breastfeeds depends not only on desire but on social and economic support and biology; for some, breastfeeding simply isn’t an option. “I agree that we should educate women about the benefits of breastfeeding so they can make an informed decision for themselves and their infants, but we also need to acknowledge the complexity of this issue,” she cautioned.
One coauthor reported a travel stipend by the Human Milk Banking Association of North America; Dr. Hoyt-Austin and the other authors had no conflicts of interest to report. Dr. Cyr had no conflicts of interest to report.
SOURCE: Hoyt-Austin A et al. Obstet Gynecol. 2020 Dec. doi: 10.1097/AOG.0000000000004162.
FROM OBSTETRICS & GYNECOLOGY
Ultraprocessed food again linked to increased CVD, death
Yet another study has linked the consumption of ultraprocessed, or “junk,” foods to bad health outcomes.
In a longitudinal analysis of more than 22,000 men and women from southern Italy, those who consumed the most ultraprocessed food (UPF) had the highest risk for cardiovascular disease (CVD) and all-cause mortality, likely mediated through a diet high in sugar, researchers said.
High consumption of UPF in this Mediterranean cohort was associated with a 58% increased risk for CVD mortality and 52% higher risk of dying from ischemic heart disease (IHD) and cerebrovascular causes, independently of known risk factors for CVD, even among individuals who otherwise adhered to the Mediterranean diet.
The findings “should serve as an incentive for limiting consumption of UPF and encouraging natural or minimally processed foods, as several national nutritional policies recommend,” Marialaura Bonaccio, PhD, department of epidemiology and prevention, IRCCS Neuromed, Pozzilli, Italy, and colleagues wrote. The results were published online Dec. 18 in the American Journal of Clinical Nutrition.
Earlier this year, as reported by this news organization, researchers found mounting evidence that the obesity epidemic and the increase in incidence of related chronic conditions corresponded with an increase in the intake of UPF.
A study that was conducted in a European cohort found that adults whose diet included more UPF and beverages, such as ice cream, soda, and hamburgers, were more likely to develop CVD or die sooner than others who had a more wholesome diet.
As reported previously by this news organization, among adults in France who had a 10% higher intake of UPF and beverages, the rate of CVD, coronary heart disease, and cerebrovascular disease was 11% to 13% higher over a period of about 5 years.
Similarly, university graduates in Spain who consumed more than four servings of UPF and beverages a day were 62% more likely to die of any cause over about a decade than those who consumed less than two servings per day.
Where’s the food?
There is very little actual food in UPF. “The NOVA classification provides 4 main classes of food and beverages, the last of which is represented by the ultraprocessed food group. This comprises products (e.g., snacks, drinks, and ready meals, ‘created mostly or entirely from substances extracted from foods or derived from food constituents with little, if any intact food, which often contain flavors, colors, and other additives that imitate or intensify the sensory qualities of foods or culinary preparations made from foods,’ ” Dr. Bonaccio and colleagues wrote.
Such foods are very convenient, tasty, inexpensive, and have a long shelf life. They are highly competitive with foods that are naturally ready to consume and freshly prepared dishes and meals, the authors add.
The researchers conducted a longitudinal analysis on 22,475 men and women (mean age, 55 years; range, 43-67 years) who were recruited from the Moli-sani Study, a population-based cohort of men and women aged 35 years and older in the Molise region of southern Italy, between 2005 and 2010. Participants were followed for 8.2 years.
Food intake was assessed with the Food Frequency Questionnaire; UPF was defined using the NOVA classification according to degree of processing.
UPF intakes were categorized as quartiles of the ratio of UPF to total food consumed.
Overall, study participants reported a median of 10% (interquartile range, 6.6%-14.6%) of dietary intake as UPF and a total of 181.5 g/d of UPF intake.
The foods that contributed most to total UPF consumed were processed meat, which accounted for 19.8% of UPF intake; pizza (16.8%); and cakes and pies (13.4%).
High consumers of UPF, defined as those for whom UPF constituted more than 14.6% of their total diet, were more likely to be women, to be younger, and to have a higher educational level. They also reported fewer risk factors and fewer baseline chronic diseases and health conditions than persons who consumed UPF less frequently.
In addition, high consumption of UPF was associated with lower adherence to the Mediterranean diet; higher intake of fat, sugar, dietary cholesterol, and sodium; and lower intake of fiber.
During a median follow-up of 8.2 years, 1,216 all-cause deaths occurred. Of these, 439 were attributed to CVD, 255 to IHD/cerebrovascular disease, 477 to cancer, and 300 to other causes.
The more UPF, the higher the risk for CVD, death
The researchers found a direct linear dose-response relation between a 5% increase in the proportion of UPF in the diet and risk for all-cause and CVD mortality.
Individuals who reported the highest intake of UPF (fourth quartile, 14.6% of total food) as opposed to the lowest (first quartile, UPF <6.6%) experienced increased risks for CVD mortality (hazard ratio, 1.58; 95% CI, 1.23-2.03), death from IHD/cerebrovascular disease (HR, 1.52, 95% CI, 1.10-2.09), and all-cause mortality (HR, 1.26; 95% CI, 1.09-1.46).
High sugar content accounted for 36.3% of the relation of UPF with IHD/cerebrovascular mortality. Other nutritional factors, such as saturated fats, were unlikely to play a role, the researchers wrote.
Biomarkers of renal function accounted for 20.1% of the association of UPF with all-cause mortality and 12.0% for that of UPF with CVD mortality.
Subgroup analyses indicated that the magnitude of the association between UPF and all-cause mortality risk was greater among high-risk individuals, such as those with a history of CVD or diabetes. UPF was also likely to be more strongly associated with CVD mortality among those high-risk groups.
The interesting finding that the association between UPF and CVD mortality was greater among individuals with good adherence to the Mediterranean diet, which is known to have health benefits, could be explained by the fact that people who may benefit from a Mediterranean diet are more susceptible to losing health advantages when they also include “detrimental dietary behavior,” whereas those who consume a poor-quality diet are less likely to be harmed by an additional unhealthy behavior such as eating UPF regularly, wrote Dr. Bonaccio and colleagues.
“This is an interesting study confirming that consumption of highly processed foods such as pizza, processed meats, and soda are associated with greater risks of cardiovascular disease,” Walter Willett, MD, professor of epidemiology and nutrition, Harvard School of Public Health, Boston, said in an interview.
“These higher risks appear to be mediated in part by high intakes of saturated fat and sugar, but lower intakes of health-promoting aspects of diet also likely contribute to the findings,” Dr. Willett said.
“Some processing of food can be useful for preservation and control of infectious agents, but in general, a diet emphasizing minimally processed fruits and vegetables, whole grains, nuts, legumes, and plant sources of fat will be best for long-term well-being,” he said.
The study was supported in part by the Italian Ministry of Health and the HYPERCAN Study Italian Association for Cancer Research. Dr. Bonaccio and Dr. Willett reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Yet another study has linked the consumption of ultraprocessed, or “junk,” foods to bad health outcomes.
In a longitudinal analysis of more than 22,000 men and women from southern Italy, those who consumed the most ultraprocessed food (UPF) had the highest risk for cardiovascular disease (CVD) and all-cause mortality, likely mediated through a diet high in sugar, researchers said.
High consumption of UPF in this Mediterranean cohort was associated with a 58% increased risk for CVD mortality and 52% higher risk of dying from ischemic heart disease (IHD) and cerebrovascular causes, independently of known risk factors for CVD, even among individuals who otherwise adhered to the Mediterranean diet.
The findings “should serve as an incentive for limiting consumption of UPF and encouraging natural or minimally processed foods, as several national nutritional policies recommend,” Marialaura Bonaccio, PhD, department of epidemiology and prevention, IRCCS Neuromed, Pozzilli, Italy, and colleagues wrote. The results were published online Dec. 18 in the American Journal of Clinical Nutrition.
Earlier this year, as reported by this news organization, researchers found mounting evidence that the obesity epidemic and the increase in incidence of related chronic conditions corresponded with an increase in the intake of UPF.
A study that was conducted in a European cohort found that adults whose diet included more UPF and beverages, such as ice cream, soda, and hamburgers, were more likely to develop CVD or die sooner than others who had a more wholesome diet.
As reported previously by this news organization, among adults in France who had a 10% higher intake of UPF and beverages, the rate of CVD, coronary heart disease, and cerebrovascular disease was 11% to 13% higher over a period of about 5 years.
Similarly, university graduates in Spain who consumed more than four servings of UPF and beverages a day were 62% more likely to die of any cause over about a decade than those who consumed less than two servings per day.
Where’s the food?
There is very little actual food in UPF. “The NOVA classification provides 4 main classes of food and beverages, the last of which is represented by the ultraprocessed food group. This comprises products (e.g., snacks, drinks, and ready meals, ‘created mostly or entirely from substances extracted from foods or derived from food constituents with little, if any intact food, which often contain flavors, colors, and other additives that imitate or intensify the sensory qualities of foods or culinary preparations made from foods,’ ” Dr. Bonaccio and colleagues wrote.
Such foods are very convenient, tasty, inexpensive, and have a long shelf life. They are highly competitive with foods that are naturally ready to consume and freshly prepared dishes and meals, the authors add.
The researchers conducted a longitudinal analysis on 22,475 men and women (mean age, 55 years; range, 43-67 years) who were recruited from the Moli-sani Study, a population-based cohort of men and women aged 35 years and older in the Molise region of southern Italy, between 2005 and 2010. Participants were followed for 8.2 years.
Food intake was assessed with the Food Frequency Questionnaire; UPF was defined using the NOVA classification according to degree of processing.
UPF intakes were categorized as quartiles of the ratio of UPF to total food consumed.
Overall, study participants reported a median of 10% (interquartile range, 6.6%-14.6%) of dietary intake as UPF and a total of 181.5 g/d of UPF intake.
The foods that contributed most to total UPF consumed were processed meat, which accounted for 19.8% of UPF intake; pizza (16.8%); and cakes and pies (13.4%).
High consumers of UPF, defined as those for whom UPF constituted more than 14.6% of their total diet, were more likely to be women, to be younger, and to have a higher educational level. They also reported fewer risk factors and fewer baseline chronic diseases and health conditions than persons who consumed UPF less frequently.
In addition, high consumption of UPF was associated with lower adherence to the Mediterranean diet; higher intake of fat, sugar, dietary cholesterol, and sodium; and lower intake of fiber.
During a median follow-up of 8.2 years, 1,216 all-cause deaths occurred. Of these, 439 were attributed to CVD, 255 to IHD/cerebrovascular disease, 477 to cancer, and 300 to other causes.
The more UPF, the higher the risk for CVD, death
The researchers found a direct linear dose-response relation between a 5% increase in the proportion of UPF in the diet and risk for all-cause and CVD mortality.
Individuals who reported the highest intake of UPF (fourth quartile, 14.6% of total food) as opposed to the lowest (first quartile, UPF <6.6%) experienced increased risks for CVD mortality (hazard ratio, 1.58; 95% CI, 1.23-2.03), death from IHD/cerebrovascular disease (HR, 1.52, 95% CI, 1.10-2.09), and all-cause mortality (HR, 1.26; 95% CI, 1.09-1.46).
High sugar content accounted for 36.3% of the relation of UPF with IHD/cerebrovascular mortality. Other nutritional factors, such as saturated fats, were unlikely to play a role, the researchers wrote.
Biomarkers of renal function accounted for 20.1% of the association of UPF with all-cause mortality and 12.0% for that of UPF with CVD mortality.
Subgroup analyses indicated that the magnitude of the association between UPF and all-cause mortality risk was greater among high-risk individuals, such as those with a history of CVD or diabetes. UPF was also likely to be more strongly associated with CVD mortality among those high-risk groups.
The interesting finding that the association between UPF and CVD mortality was greater among individuals with good adherence to the Mediterranean diet, which is known to have health benefits, could be explained by the fact that people who may benefit from a Mediterranean diet are more susceptible to losing health advantages when they also include “detrimental dietary behavior,” whereas those who consume a poor-quality diet are less likely to be harmed by an additional unhealthy behavior such as eating UPF regularly, wrote Dr. Bonaccio and colleagues.
“This is an interesting study confirming that consumption of highly processed foods such as pizza, processed meats, and soda are associated with greater risks of cardiovascular disease,” Walter Willett, MD, professor of epidemiology and nutrition, Harvard School of Public Health, Boston, said in an interview.
“These higher risks appear to be mediated in part by high intakes of saturated fat and sugar, but lower intakes of health-promoting aspects of diet also likely contribute to the findings,” Dr. Willett said.
“Some processing of food can be useful for preservation and control of infectious agents, but in general, a diet emphasizing minimally processed fruits and vegetables, whole grains, nuts, legumes, and plant sources of fat will be best for long-term well-being,” he said.
The study was supported in part by the Italian Ministry of Health and the HYPERCAN Study Italian Association for Cancer Research. Dr. Bonaccio and Dr. Willett reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Yet another study has linked the consumption of ultraprocessed, or “junk,” foods to bad health outcomes.
In a longitudinal analysis of more than 22,000 men and women from southern Italy, those who consumed the most ultraprocessed food (UPF) had the highest risk for cardiovascular disease (CVD) and all-cause mortality, likely mediated through a diet high in sugar, researchers said.
High consumption of UPF in this Mediterranean cohort was associated with a 58% increased risk for CVD mortality and 52% higher risk of dying from ischemic heart disease (IHD) and cerebrovascular causes, independently of known risk factors for CVD, even among individuals who otherwise adhered to the Mediterranean diet.
The findings “should serve as an incentive for limiting consumption of UPF and encouraging natural or minimally processed foods, as several national nutritional policies recommend,” Marialaura Bonaccio, PhD, department of epidemiology and prevention, IRCCS Neuromed, Pozzilli, Italy, and colleagues wrote. The results were published online Dec. 18 in the American Journal of Clinical Nutrition.
Earlier this year, as reported by this news organization, researchers found mounting evidence that the obesity epidemic and the increase in incidence of related chronic conditions corresponded with an increase in the intake of UPF.
A study that was conducted in a European cohort found that adults whose diet included more UPF and beverages, such as ice cream, soda, and hamburgers, were more likely to develop CVD or die sooner than others who had a more wholesome diet.
As reported previously by this news organization, among adults in France who had a 10% higher intake of UPF and beverages, the rate of CVD, coronary heart disease, and cerebrovascular disease was 11% to 13% higher over a period of about 5 years.
Similarly, university graduates in Spain who consumed more than four servings of UPF and beverages a day were 62% more likely to die of any cause over about a decade than those who consumed less than two servings per day.
Where’s the food?
There is very little actual food in UPF. “The NOVA classification provides 4 main classes of food and beverages, the last of which is represented by the ultraprocessed food group. This comprises products (e.g., snacks, drinks, and ready meals, ‘created mostly or entirely from substances extracted from foods or derived from food constituents with little, if any intact food, which often contain flavors, colors, and other additives that imitate or intensify the sensory qualities of foods or culinary preparations made from foods,’ ” Dr. Bonaccio and colleagues wrote.
Such foods are very convenient, tasty, inexpensive, and have a long shelf life. They are highly competitive with foods that are naturally ready to consume and freshly prepared dishes and meals, the authors add.
The researchers conducted a longitudinal analysis on 22,475 men and women (mean age, 55 years; range, 43-67 years) who were recruited from the Moli-sani Study, a population-based cohort of men and women aged 35 years and older in the Molise region of southern Italy, between 2005 and 2010. Participants were followed for 8.2 years.
Food intake was assessed with the Food Frequency Questionnaire; UPF was defined using the NOVA classification according to degree of processing.
UPF intakes were categorized as quartiles of the ratio of UPF to total food consumed.
Overall, study participants reported a median of 10% (interquartile range, 6.6%-14.6%) of dietary intake as UPF and a total of 181.5 g/d of UPF intake.
The foods that contributed most to total UPF consumed were processed meat, which accounted for 19.8% of UPF intake; pizza (16.8%); and cakes and pies (13.4%).
High consumers of UPF, defined as those for whom UPF constituted more than 14.6% of their total diet, were more likely to be women, to be younger, and to have a higher educational level. They also reported fewer risk factors and fewer baseline chronic diseases and health conditions than persons who consumed UPF less frequently.
In addition, high consumption of UPF was associated with lower adherence to the Mediterranean diet; higher intake of fat, sugar, dietary cholesterol, and sodium; and lower intake of fiber.
During a median follow-up of 8.2 years, 1,216 all-cause deaths occurred. Of these, 439 were attributed to CVD, 255 to IHD/cerebrovascular disease, 477 to cancer, and 300 to other causes.
The more UPF, the higher the risk for CVD, death
The researchers found a direct linear dose-response relation between a 5% increase in the proportion of UPF in the diet and risk for all-cause and CVD mortality.
Individuals who reported the highest intake of UPF (fourth quartile, 14.6% of total food) as opposed to the lowest (first quartile, UPF <6.6%) experienced increased risks for CVD mortality (hazard ratio, 1.58; 95% CI, 1.23-2.03), death from IHD/cerebrovascular disease (HR, 1.52, 95% CI, 1.10-2.09), and all-cause mortality (HR, 1.26; 95% CI, 1.09-1.46).
High sugar content accounted for 36.3% of the relation of UPF with IHD/cerebrovascular mortality. Other nutritional factors, such as saturated fats, were unlikely to play a role, the researchers wrote.
Biomarkers of renal function accounted for 20.1% of the association of UPF with all-cause mortality and 12.0% for that of UPF with CVD mortality.
Subgroup analyses indicated that the magnitude of the association between UPF and all-cause mortality risk was greater among high-risk individuals, such as those with a history of CVD or diabetes. UPF was also likely to be more strongly associated with CVD mortality among those high-risk groups.
The interesting finding that the association between UPF and CVD mortality was greater among individuals with good adherence to the Mediterranean diet, which is known to have health benefits, could be explained by the fact that people who may benefit from a Mediterranean diet are more susceptible to losing health advantages when they also include “detrimental dietary behavior,” whereas those who consume a poor-quality diet are less likely to be harmed by an additional unhealthy behavior such as eating UPF regularly, wrote Dr. Bonaccio and colleagues.
“This is an interesting study confirming that consumption of highly processed foods such as pizza, processed meats, and soda are associated with greater risks of cardiovascular disease,” Walter Willett, MD, professor of epidemiology and nutrition, Harvard School of Public Health, Boston, said in an interview.
“These higher risks appear to be mediated in part by high intakes of saturated fat and sugar, but lower intakes of health-promoting aspects of diet also likely contribute to the findings,” Dr. Willett said.
“Some processing of food can be useful for preservation and control of infectious agents, but in general, a diet emphasizing minimally processed fruits and vegetables, whole grains, nuts, legumes, and plant sources of fat will be best for long-term well-being,” he said.
The study was supported in part by the Italian Ministry of Health and the HYPERCAN Study Italian Association for Cancer Research. Dr. Bonaccio and Dr. Willett reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AGA Clinical Practice Update: How diet and exercise can help manage NAFLD
Exercise and a hypocaloric, Mediterranean-style diet remain first-line interventions that can benefit all patients with nonalcoholic fatty liver disease (NAFLD), according to a clinical practice update from the American Gastroenterological Association.
“[W]eight loss is associated with a reduction in liver fat, which provides a potential for reversal of disease progression,” wrote Zobair M. Younossi, MD, MPH, of Inova Fairfax Medical Campus in Falls Church, Va., with his associates. Lifestyle modifications remain “the cornerstone for management” because, even though NAFLD affects approximately 25% of individuals worldwide according to one meta-analytic assessment, interventions such as medications, bariatric endoscopy, and surgery are usually reserved for the subset of patients with severe obesity, comorbid diabetes, or nonalcoholic steatohepatitis (NASH) with at least stage 2 fibrosis, the experts wrote in Gastroenterology.
They note that clinically significant weight loss typically requires a hypocaloric diet of 1,200-1,500 kilocalories/day or a decrease of 500-1,000 kilocalories/day from baseline. A Mediterranean diet of fresh vegetables, fruits, legumes, minimally processed whole grains, fish, olive oil, nuts, and seeds is recommended because its antioxidant, anti-inflammatory effects may slow NAFLD progression. This diet minimizes or eliminates sweets, refined grains, and red and processed meats. Fructose from fruit is not associated with NAFLD, but patients should consume little or no commercially prepared fructose, which has been linked to visceral adiposity, insulin resistance, hepatic inflammation, and fibrosis progression. Other hypocaloric diets have not been studied enough to support their routine use in NAFLD treatment, according to the clinical practice update.
For patients with NASH, which is the more severe form of NAFLD and is associated with significant morbidity and mortality caused by complications from cirrhosis, hepatic decompensation, and hepatocellular carcinoma, weight loss also has a big impact: Losing at least 5% of total body weight can decrease hepatic steatosis, losing at least 7% can resolve NASH, and losing at least 10% can lessen or stabilize hepatic fibrosis, according to level 1 evidence cited by the update. Weight loss “can significantly impact all aspects of NAFLD histology including fibrosis, but a goal of 10% total body weight loss should be considered for patients with overweight or obese NAFLD,” the authors wrote. Fat loss also improves liver histology in patients with lean NAFLD (body mass index, 26 kg/m2 in non-Asian patients or 24 in Asians), for whom a hypocaloric diet targeting a more modest 3%-5% total body weight loss is recommended.
Because aerobic exercise reduces hepatic fat levels independently of hypocaloric diet, patients with NAFLD should consider a weekly regimen of 150-300 minutes of moderate-intensity exercise or 75-150 minutes of vigorous activity. Resistance training can complement aerobic exercise “but [is] not a replacement,” the authors noted. In addition, patients with NAFLD should restrict alcohol consumption to reduce the risk for liver-related events, and those with advanced hepatic fibrosis should “avoid alcohol entirely.” These recommendations reflect the findings of a large prospective study in which the consumption of even low amounts of alcohol led to worse liver-related outcomes among patients with NAFLD.
Clinicians should screen for and “aggressively” manage common NAFLD comorbidities, including diabetes mellitus, hypertension, and obstructive sleep apnea, according to the clinical practice update. Patients with coexisting metabolic conditions should be risk-stratified for cardiovascular disease and treated based on guidelines from the American College of Cardiology and the American Heart Association.
It is believed that sarcopenia affects patients with NASH cirrhosis because their livers cannot effectively store, metabolize, or mobilize carbohydrates, which leads to a catabolic state in which protein and fat are used as energy sources, according to the update. To avoid exacerbations, these patients may need to optimize their protein intake – a minimum of 1.2-1.5 g/kg of body weight is recommended – from sources of branched-chain amino acids, such as chicken, fish, eggs, nuts, lentils, or soy. Patients with sarcopenic NAFLD also should consume small, frequent meals spaced no more than 4-6 hours apart. When possible, they should consult with a specialized nutritionist. Moderate-intensity exercise may also benefit patients experiencing sarcopenia.
The researchers disclosed ties to Gilead Sciences, Intercept, Bristol Myers Squibb, Novo Nordisk, and several other companies. The review was commissioned and approved by the AGA Institute’s Clinical Practice Updates Committee and the AGA Governing Board.
SOURCE: Younossi ZM et al. Gastroenterology. 2020 Dec 8. doi: 10.1053/j.gastro.2020.11.051.
This article was updated Feb. 10, 2021.
Exercise and a hypocaloric, Mediterranean-style diet remain first-line interventions that can benefit all patients with nonalcoholic fatty liver disease (NAFLD), according to a clinical practice update from the American Gastroenterological Association.
“[W]eight loss is associated with a reduction in liver fat, which provides a potential for reversal of disease progression,” wrote Zobair M. Younossi, MD, MPH, of Inova Fairfax Medical Campus in Falls Church, Va., with his associates. Lifestyle modifications remain “the cornerstone for management” because, even though NAFLD affects approximately 25% of individuals worldwide according to one meta-analytic assessment, interventions such as medications, bariatric endoscopy, and surgery are usually reserved for the subset of patients with severe obesity, comorbid diabetes, or nonalcoholic steatohepatitis (NASH) with at least stage 2 fibrosis, the experts wrote in Gastroenterology.
They note that clinically significant weight loss typically requires a hypocaloric diet of 1,200-1,500 kilocalories/day or a decrease of 500-1,000 kilocalories/day from baseline. A Mediterranean diet of fresh vegetables, fruits, legumes, minimally processed whole grains, fish, olive oil, nuts, and seeds is recommended because its antioxidant, anti-inflammatory effects may slow NAFLD progression. This diet minimizes or eliminates sweets, refined grains, and red and processed meats. Fructose from fruit is not associated with NAFLD, but patients should consume little or no commercially prepared fructose, which has been linked to visceral adiposity, insulin resistance, hepatic inflammation, and fibrosis progression. Other hypocaloric diets have not been studied enough to support their routine use in NAFLD treatment, according to the clinical practice update.
For patients with NASH, which is the more severe form of NAFLD and is associated with significant morbidity and mortality caused by complications from cirrhosis, hepatic decompensation, and hepatocellular carcinoma, weight loss also has a big impact: Losing at least 5% of total body weight can decrease hepatic steatosis, losing at least 7% can resolve NASH, and losing at least 10% can lessen or stabilize hepatic fibrosis, according to level 1 evidence cited by the update. Weight loss “can significantly impact all aspects of NAFLD histology including fibrosis, but a goal of 10% total body weight loss should be considered for patients with overweight or obese NAFLD,” the authors wrote. Fat loss also improves liver histology in patients with lean NAFLD (body mass index, 26 kg/m2 in non-Asian patients or 24 in Asians), for whom a hypocaloric diet targeting a more modest 3%-5% total body weight loss is recommended.
Because aerobic exercise reduces hepatic fat levels independently of hypocaloric diet, patients with NAFLD should consider a weekly regimen of 150-300 minutes of moderate-intensity exercise or 75-150 minutes of vigorous activity. Resistance training can complement aerobic exercise “but [is] not a replacement,” the authors noted. In addition, patients with NAFLD should restrict alcohol consumption to reduce the risk for liver-related events, and those with advanced hepatic fibrosis should “avoid alcohol entirely.” These recommendations reflect the findings of a large prospective study in which the consumption of even low amounts of alcohol led to worse liver-related outcomes among patients with NAFLD.
Clinicians should screen for and “aggressively” manage common NAFLD comorbidities, including diabetes mellitus, hypertension, and obstructive sleep apnea, according to the clinical practice update. Patients with coexisting metabolic conditions should be risk-stratified for cardiovascular disease and treated based on guidelines from the American College of Cardiology and the American Heart Association.
It is believed that sarcopenia affects patients with NASH cirrhosis because their livers cannot effectively store, metabolize, or mobilize carbohydrates, which leads to a catabolic state in which protein and fat are used as energy sources, according to the update. To avoid exacerbations, these patients may need to optimize their protein intake – a minimum of 1.2-1.5 g/kg of body weight is recommended – from sources of branched-chain amino acids, such as chicken, fish, eggs, nuts, lentils, or soy. Patients with sarcopenic NAFLD also should consume small, frequent meals spaced no more than 4-6 hours apart. When possible, they should consult with a specialized nutritionist. Moderate-intensity exercise may also benefit patients experiencing sarcopenia.
The researchers disclosed ties to Gilead Sciences, Intercept, Bristol Myers Squibb, Novo Nordisk, and several other companies. The review was commissioned and approved by the AGA Institute’s Clinical Practice Updates Committee and the AGA Governing Board.
SOURCE: Younossi ZM et al. Gastroenterology. 2020 Dec 8. doi: 10.1053/j.gastro.2020.11.051.
This article was updated Feb. 10, 2021.
Exercise and a hypocaloric, Mediterranean-style diet remain first-line interventions that can benefit all patients with nonalcoholic fatty liver disease (NAFLD), according to a clinical practice update from the American Gastroenterological Association.
“[W]eight loss is associated with a reduction in liver fat, which provides a potential for reversal of disease progression,” wrote Zobair M. Younossi, MD, MPH, of Inova Fairfax Medical Campus in Falls Church, Va., with his associates. Lifestyle modifications remain “the cornerstone for management” because, even though NAFLD affects approximately 25% of individuals worldwide according to one meta-analytic assessment, interventions such as medications, bariatric endoscopy, and surgery are usually reserved for the subset of patients with severe obesity, comorbid diabetes, or nonalcoholic steatohepatitis (NASH) with at least stage 2 fibrosis, the experts wrote in Gastroenterology.
They note that clinically significant weight loss typically requires a hypocaloric diet of 1,200-1,500 kilocalories/day or a decrease of 500-1,000 kilocalories/day from baseline. A Mediterranean diet of fresh vegetables, fruits, legumes, minimally processed whole grains, fish, olive oil, nuts, and seeds is recommended because its antioxidant, anti-inflammatory effects may slow NAFLD progression. This diet minimizes or eliminates sweets, refined grains, and red and processed meats. Fructose from fruit is not associated with NAFLD, but patients should consume little or no commercially prepared fructose, which has been linked to visceral adiposity, insulin resistance, hepatic inflammation, and fibrosis progression. Other hypocaloric diets have not been studied enough to support their routine use in NAFLD treatment, according to the clinical practice update.
For patients with NASH, which is the more severe form of NAFLD and is associated with significant morbidity and mortality caused by complications from cirrhosis, hepatic decompensation, and hepatocellular carcinoma, weight loss also has a big impact: Losing at least 5% of total body weight can decrease hepatic steatosis, losing at least 7% can resolve NASH, and losing at least 10% can lessen or stabilize hepatic fibrosis, according to level 1 evidence cited by the update. Weight loss “can significantly impact all aspects of NAFLD histology including fibrosis, but a goal of 10% total body weight loss should be considered for patients with overweight or obese NAFLD,” the authors wrote. Fat loss also improves liver histology in patients with lean NAFLD (body mass index, 26 kg/m2 in non-Asian patients or 24 in Asians), for whom a hypocaloric diet targeting a more modest 3%-5% total body weight loss is recommended.
Because aerobic exercise reduces hepatic fat levels independently of hypocaloric diet, patients with NAFLD should consider a weekly regimen of 150-300 minutes of moderate-intensity exercise or 75-150 minutes of vigorous activity. Resistance training can complement aerobic exercise “but [is] not a replacement,” the authors noted. In addition, patients with NAFLD should restrict alcohol consumption to reduce the risk for liver-related events, and those with advanced hepatic fibrosis should “avoid alcohol entirely.” These recommendations reflect the findings of a large prospective study in which the consumption of even low amounts of alcohol led to worse liver-related outcomes among patients with NAFLD.
Clinicians should screen for and “aggressively” manage common NAFLD comorbidities, including diabetes mellitus, hypertension, and obstructive sleep apnea, according to the clinical practice update. Patients with coexisting metabolic conditions should be risk-stratified for cardiovascular disease and treated based on guidelines from the American College of Cardiology and the American Heart Association.
It is believed that sarcopenia affects patients with NASH cirrhosis because their livers cannot effectively store, metabolize, or mobilize carbohydrates, which leads to a catabolic state in which protein and fat are used as energy sources, according to the update. To avoid exacerbations, these patients may need to optimize their protein intake – a minimum of 1.2-1.5 g/kg of body weight is recommended – from sources of branched-chain amino acids, such as chicken, fish, eggs, nuts, lentils, or soy. Patients with sarcopenic NAFLD also should consume small, frequent meals spaced no more than 4-6 hours apart. When possible, they should consult with a specialized nutritionist. Moderate-intensity exercise may also benefit patients experiencing sarcopenia.
The researchers disclosed ties to Gilead Sciences, Intercept, Bristol Myers Squibb, Novo Nordisk, and several other companies. The review was commissioned and approved by the AGA Institute’s Clinical Practice Updates Committee and the AGA Governing Board.
SOURCE: Younossi ZM et al. Gastroenterology. 2020 Dec 8. doi: 10.1053/j.gastro.2020.11.051.
This article was updated Feb. 10, 2021.
FROM GASTROENTEROLOGY
Far too few with treatment-resistant hypertension get hormone test
despite guidelines that call for such an approach, according to findings from the first reported large-scale, multicenter study of PA testing practices.
Researchers ran a retrospective review of PA testing among 269,010 patients who met the definition as having treatment-resistant hypertension and were managed at any one of 130 Veterans Health Administration (VHA) medical centers from 2000 to 2017.
The results showed that, despite the fact that primary aldosteronism is highly prevalent among patients with treatment-resistant hypertension, only 4,277 (1.6%) underwent assessment for PA during a median of 3.3 years’ follow-up after they first met the defining criteria, Jordana B. Cohen, MD, and her associates reported in a study published in Annals of Internal Medicine on December 28.
“Testing rates also did not change meaningfully over nearly 2 decades ... despite an increasing number of guidelines recommending testing for primary aldosteronism in this population,” including the most recent recommendations from the Endocrine Society, issued in 2016, noted Dr. Cohen, a nephrologist and hypertension researcher at the University of Pennsylvania in Philadelphia, and colleagues.
Most patients in the study (almost 90%) were seen by a primary care practitioner (PCP).
The small percentage of patients seen by a nephrologist or endocrinologist were more than twice as likely to be tested for PA than those seen by a PCP or cardiologist.
Those clinicians who did order a test for PA were much more likely to treat patients with the appropriate medication, a mineralocorticoid receptor antagonist (MRA). In addition, therapy was started sooner, the researchers found.
“Our results corroborate” earlier reports from smaller health systems and suggest that dramatic underuse of PA assessment “is an issue across the US,” Dr. Cohen said in an interview.
The VHA experience “is very representative of what we think goes on across U.S. practice” and contrasts with the VHA’s reputation for “doing a pretty good job managing hypertension” in general, she noted.
Missed diagnosis, missed treatment
Dr. Cohen believes a number of factors likely help drive the abysmally low rate of PA testing they observed in the VHA system. She believes rates of PA testing are low elsewhere as well.
First, optimal hypertension management “is often taken for granted” but is challenging in busy primary care practices, so many of patients likely fall through the cracks, she said.
Dr. Cohen cited efforts at her institution, as well as by the VHA system, to better employ electronic health records to flag patients with treatment-resistant hypertension – defined as patients whose systolic or diastolic blood pressure remains at or above 140/90 mm Hg on at least two successive measurements at least a month apart while the patient is undergoing treatment with three conventional antihypertensive drugs – and to guide clinicians to order the right tests and treatments for these patients.
Many care providers mistakenly “see treatment-resistant hypertension as a disease of noncompliance,” although it is much more often the result of a missed diagnosis and inadequate intervention, she explained.
Physicians in denial; side effects of MRAs may deter prescribing
A second big cause of low PA testing rates is that doctors make the mistake of thinking a PA test result won’t change how they manage these patients.
The established treatment for most patients with treatment-resistant hypertension as well as PA is adding an MRA, either spironolactone or eplerenone (Inspra).
Many providers cling to the belief that they will start an MRA in these patients without first determining their PA status, says Dr. Cohen, but the data she and her colleagues collected show the opposite.
Overall, about 13% of all patients in the study began treatment with an MRA during follow-up. The likelihood of starting treatment with this drug class was fourfold higher among the patients tested for PA compared with those who were not tested.
PA testing also hastened the start of MRA use by more than a year, compared with untested patients.
“Providers think they prescribe an MRA” to treatment-resistant patients, “but it’s part of their denial. They are not using the evidence-based treatments [spironolactone or eplerenone], perhaps because of concerns about MRA side effects, although those have been pretty well overcome during the past 20 years,” she observed.
Dr. Cohen says gynecomastia is one adverse effect that gives pause to VHA clinicians who see a heavily male patient population. “It’s probably the biggest concern and why PA testing and MRA use is low” in the VHA system, she said.
“You can use a lower dosage of spironolactone, and the incidence is less common with eplerenone,” although using eplerenone does not completely eliminate all gynecomastia cases, she noted.
At the University of Pennsylvania hospitals, men often start on spironolactone first because it retains a significant price advantage, even though eplerenone is now generic, but “if there is a hint of gynecomastia, we quickly switch to eplerenone, which is usually well tolerated,” she explained.
And while eplerenone has a reputation of being less effective than spironolactone, “I’ve prescribed a lot of eplerenone and have had good results,” Dr. Cohen said. “Even if the blood pressure lowering is not as great compared with spironolactone, it still blunts the toxic effects of aldosterone on target organs.”
Hyperkalemia is the other big concern about spironolactone and eplerenone. Both agents cause it at roughly the same rate, although the rate is lower in patients without chronic kidney disease.
A new, nonsteroidal MRA, finerenone, caused substantially less hyperkalemia in a recent phase 3 trial, FIDELIO-DKD, and as a nonsteroidal MRA, it does not cause gynecomastia. Finerenone has promise as a potentially safer option for treating PA and treatment-resistant hypertension, noted Cohen, but so far, no advanced clinical trials have been launched to examine its efficacy for these indications.
PA testing allows a surgical option
A third reason to test patients with treatment-resistant hypertension for PA is that jumping straight to MRA treatment denies the patient assessment for a unilateral adrenal adenoma as the cause of excess aldosterone.
When unilateral adenomas exist, patients are candidates for adrenalectomy. Despite the potential advantage this gives patients to eliminate the cause of their PA without the need for additional drug treatment, some clinicians don’t see this as a compelling rationale to test for PA because they have a bias against surgery or have seen too many cases in which surgery failed to produce full hypertension resolution.
“It’s all about setting expectations appropriately” for the impact of this surgery, Dr. Cohen said.
“Adrenalectomy is not a cure; it just gets rid of the source of excess aldosterone.” But in patients with long-standing PA and hypertension, this is often not enough to completely resolve entrenched cardiovascular pathology.
PCPs, cardiologists in rural locations least likely to order PA testing
Of the 269,010 patients analyzed by Dr. Cohen and her coauthors, the average age was 65 years; 96% were men; half were obese; and 40% had diabetes. The researchers excluded patients who had already been tested for PA, as well as those who were already receiving treatment with an MRA.
For 88% of the patients, the main physician overseeing care was a PCP. A cardiologist was the main physician for 10%; a nephrologist, for 1%; and an endocrinologist, for fewer than 1%.
The rate of testing for PA varied across the 130 VHA centers that contributed data, ranging from 0% to 6%. The testing data showed that endocrinologists were most likely to order PA testing, doing it 2.48-fold more often than PCPs. Nephrologists were roughly twice as likely to order PA testing than PCPs, and cardiologists ordered testing at about the same rate as PCPs.
Patients managed at VHA centers in rural locations were nearly half as likely to undergo testing as patients managed at nonrural centers. The number of patients with treatment-resistant hypertension seen by a physician or at a center had no significant relationship to PA testing frequency.
The study received no commercial funding. Dr. Cohen has disclosed no relevant financial relationships.
A version of this story first appeared on Medscape.com.
despite guidelines that call for such an approach, according to findings from the first reported large-scale, multicenter study of PA testing practices.
Researchers ran a retrospective review of PA testing among 269,010 patients who met the definition as having treatment-resistant hypertension and were managed at any one of 130 Veterans Health Administration (VHA) medical centers from 2000 to 2017.
The results showed that, despite the fact that primary aldosteronism is highly prevalent among patients with treatment-resistant hypertension, only 4,277 (1.6%) underwent assessment for PA during a median of 3.3 years’ follow-up after they first met the defining criteria, Jordana B. Cohen, MD, and her associates reported in a study published in Annals of Internal Medicine on December 28.
“Testing rates also did not change meaningfully over nearly 2 decades ... despite an increasing number of guidelines recommending testing for primary aldosteronism in this population,” including the most recent recommendations from the Endocrine Society, issued in 2016, noted Dr. Cohen, a nephrologist and hypertension researcher at the University of Pennsylvania in Philadelphia, and colleagues.
Most patients in the study (almost 90%) were seen by a primary care practitioner (PCP).
The small percentage of patients seen by a nephrologist or endocrinologist were more than twice as likely to be tested for PA than those seen by a PCP or cardiologist.
Those clinicians who did order a test for PA were much more likely to treat patients with the appropriate medication, a mineralocorticoid receptor antagonist (MRA). In addition, therapy was started sooner, the researchers found.
“Our results corroborate” earlier reports from smaller health systems and suggest that dramatic underuse of PA assessment “is an issue across the US,” Dr. Cohen said in an interview.
The VHA experience “is very representative of what we think goes on across U.S. practice” and contrasts with the VHA’s reputation for “doing a pretty good job managing hypertension” in general, she noted.
Missed diagnosis, missed treatment
Dr. Cohen believes a number of factors likely help drive the abysmally low rate of PA testing they observed in the VHA system. She believes rates of PA testing are low elsewhere as well.
First, optimal hypertension management “is often taken for granted” but is challenging in busy primary care practices, so many of patients likely fall through the cracks, she said.
Dr. Cohen cited efforts at her institution, as well as by the VHA system, to better employ electronic health records to flag patients with treatment-resistant hypertension – defined as patients whose systolic or diastolic blood pressure remains at or above 140/90 mm Hg on at least two successive measurements at least a month apart while the patient is undergoing treatment with three conventional antihypertensive drugs – and to guide clinicians to order the right tests and treatments for these patients.
Many care providers mistakenly “see treatment-resistant hypertension as a disease of noncompliance,” although it is much more often the result of a missed diagnosis and inadequate intervention, she explained.
Physicians in denial; side effects of MRAs may deter prescribing
A second big cause of low PA testing rates is that doctors make the mistake of thinking a PA test result won’t change how they manage these patients.
The established treatment for most patients with treatment-resistant hypertension as well as PA is adding an MRA, either spironolactone or eplerenone (Inspra).
Many providers cling to the belief that they will start an MRA in these patients without first determining their PA status, says Dr. Cohen, but the data she and her colleagues collected show the opposite.
Overall, about 13% of all patients in the study began treatment with an MRA during follow-up. The likelihood of starting treatment with this drug class was fourfold higher among the patients tested for PA compared with those who were not tested.
PA testing also hastened the start of MRA use by more than a year, compared with untested patients.
“Providers think they prescribe an MRA” to treatment-resistant patients, “but it’s part of their denial. They are not using the evidence-based treatments [spironolactone or eplerenone], perhaps because of concerns about MRA side effects, although those have been pretty well overcome during the past 20 years,” she observed.
Dr. Cohen says gynecomastia is one adverse effect that gives pause to VHA clinicians who see a heavily male patient population. “It’s probably the biggest concern and why PA testing and MRA use is low” in the VHA system, she said.
“You can use a lower dosage of spironolactone, and the incidence is less common with eplerenone,” although using eplerenone does not completely eliminate all gynecomastia cases, she noted.
At the University of Pennsylvania hospitals, men often start on spironolactone first because it retains a significant price advantage, even though eplerenone is now generic, but “if there is a hint of gynecomastia, we quickly switch to eplerenone, which is usually well tolerated,” she explained.
And while eplerenone has a reputation of being less effective than spironolactone, “I’ve prescribed a lot of eplerenone and have had good results,” Dr. Cohen said. “Even if the blood pressure lowering is not as great compared with spironolactone, it still blunts the toxic effects of aldosterone on target organs.”
Hyperkalemia is the other big concern about spironolactone and eplerenone. Both agents cause it at roughly the same rate, although the rate is lower in patients without chronic kidney disease.
A new, nonsteroidal MRA, finerenone, caused substantially less hyperkalemia in a recent phase 3 trial, FIDELIO-DKD, and as a nonsteroidal MRA, it does not cause gynecomastia. Finerenone has promise as a potentially safer option for treating PA and treatment-resistant hypertension, noted Cohen, but so far, no advanced clinical trials have been launched to examine its efficacy for these indications.
PA testing allows a surgical option
A third reason to test patients with treatment-resistant hypertension for PA is that jumping straight to MRA treatment denies the patient assessment for a unilateral adrenal adenoma as the cause of excess aldosterone.
When unilateral adenomas exist, patients are candidates for adrenalectomy. Despite the potential advantage this gives patients to eliminate the cause of their PA without the need for additional drug treatment, some clinicians don’t see this as a compelling rationale to test for PA because they have a bias against surgery or have seen too many cases in which surgery failed to produce full hypertension resolution.
“It’s all about setting expectations appropriately” for the impact of this surgery, Dr. Cohen said.
“Adrenalectomy is not a cure; it just gets rid of the source of excess aldosterone.” But in patients with long-standing PA and hypertension, this is often not enough to completely resolve entrenched cardiovascular pathology.
PCPs, cardiologists in rural locations least likely to order PA testing
Of the 269,010 patients analyzed by Dr. Cohen and her coauthors, the average age was 65 years; 96% were men; half were obese; and 40% had diabetes. The researchers excluded patients who had already been tested for PA, as well as those who were already receiving treatment with an MRA.
For 88% of the patients, the main physician overseeing care was a PCP. A cardiologist was the main physician for 10%; a nephrologist, for 1%; and an endocrinologist, for fewer than 1%.
The rate of testing for PA varied across the 130 VHA centers that contributed data, ranging from 0% to 6%. The testing data showed that endocrinologists were most likely to order PA testing, doing it 2.48-fold more often than PCPs. Nephrologists were roughly twice as likely to order PA testing than PCPs, and cardiologists ordered testing at about the same rate as PCPs.
Patients managed at VHA centers in rural locations were nearly half as likely to undergo testing as patients managed at nonrural centers. The number of patients with treatment-resistant hypertension seen by a physician or at a center had no significant relationship to PA testing frequency.
The study received no commercial funding. Dr. Cohen has disclosed no relevant financial relationships.
A version of this story first appeared on Medscape.com.
despite guidelines that call for such an approach, according to findings from the first reported large-scale, multicenter study of PA testing practices.
Researchers ran a retrospective review of PA testing among 269,010 patients who met the definition as having treatment-resistant hypertension and were managed at any one of 130 Veterans Health Administration (VHA) medical centers from 2000 to 2017.
The results showed that, despite the fact that primary aldosteronism is highly prevalent among patients with treatment-resistant hypertension, only 4,277 (1.6%) underwent assessment for PA during a median of 3.3 years’ follow-up after they first met the defining criteria, Jordana B. Cohen, MD, and her associates reported in a study published in Annals of Internal Medicine on December 28.
“Testing rates also did not change meaningfully over nearly 2 decades ... despite an increasing number of guidelines recommending testing for primary aldosteronism in this population,” including the most recent recommendations from the Endocrine Society, issued in 2016, noted Dr. Cohen, a nephrologist and hypertension researcher at the University of Pennsylvania in Philadelphia, and colleagues.
Most patients in the study (almost 90%) were seen by a primary care practitioner (PCP).
The small percentage of patients seen by a nephrologist or endocrinologist were more than twice as likely to be tested for PA than those seen by a PCP or cardiologist.
Those clinicians who did order a test for PA were much more likely to treat patients with the appropriate medication, a mineralocorticoid receptor antagonist (MRA). In addition, therapy was started sooner, the researchers found.
“Our results corroborate” earlier reports from smaller health systems and suggest that dramatic underuse of PA assessment “is an issue across the US,” Dr. Cohen said in an interview.
The VHA experience “is very representative of what we think goes on across U.S. practice” and contrasts with the VHA’s reputation for “doing a pretty good job managing hypertension” in general, she noted.
Missed diagnosis, missed treatment
Dr. Cohen believes a number of factors likely help drive the abysmally low rate of PA testing they observed in the VHA system. She believes rates of PA testing are low elsewhere as well.
First, optimal hypertension management “is often taken for granted” but is challenging in busy primary care practices, so many of patients likely fall through the cracks, she said.
Dr. Cohen cited efforts at her institution, as well as by the VHA system, to better employ electronic health records to flag patients with treatment-resistant hypertension – defined as patients whose systolic or diastolic blood pressure remains at or above 140/90 mm Hg on at least two successive measurements at least a month apart while the patient is undergoing treatment with three conventional antihypertensive drugs – and to guide clinicians to order the right tests and treatments for these patients.
Many care providers mistakenly “see treatment-resistant hypertension as a disease of noncompliance,” although it is much more often the result of a missed diagnosis and inadequate intervention, she explained.
Physicians in denial; side effects of MRAs may deter prescribing
A second big cause of low PA testing rates is that doctors make the mistake of thinking a PA test result won’t change how they manage these patients.
The established treatment for most patients with treatment-resistant hypertension as well as PA is adding an MRA, either spironolactone or eplerenone (Inspra).
Many providers cling to the belief that they will start an MRA in these patients without first determining their PA status, says Dr. Cohen, but the data she and her colleagues collected show the opposite.
Overall, about 13% of all patients in the study began treatment with an MRA during follow-up. The likelihood of starting treatment with this drug class was fourfold higher among the patients tested for PA compared with those who were not tested.
PA testing also hastened the start of MRA use by more than a year, compared with untested patients.
“Providers think they prescribe an MRA” to treatment-resistant patients, “but it’s part of their denial. They are not using the evidence-based treatments [spironolactone or eplerenone], perhaps because of concerns about MRA side effects, although those have been pretty well overcome during the past 20 years,” she observed.
Dr. Cohen says gynecomastia is one adverse effect that gives pause to VHA clinicians who see a heavily male patient population. “It’s probably the biggest concern and why PA testing and MRA use is low” in the VHA system, she said.
“You can use a lower dosage of spironolactone, and the incidence is less common with eplerenone,” although using eplerenone does not completely eliminate all gynecomastia cases, she noted.
At the University of Pennsylvania hospitals, men often start on spironolactone first because it retains a significant price advantage, even though eplerenone is now generic, but “if there is a hint of gynecomastia, we quickly switch to eplerenone, which is usually well tolerated,” she explained.
And while eplerenone has a reputation of being less effective than spironolactone, “I’ve prescribed a lot of eplerenone and have had good results,” Dr. Cohen said. “Even if the blood pressure lowering is not as great compared with spironolactone, it still blunts the toxic effects of aldosterone on target organs.”
Hyperkalemia is the other big concern about spironolactone and eplerenone. Both agents cause it at roughly the same rate, although the rate is lower in patients without chronic kidney disease.
A new, nonsteroidal MRA, finerenone, caused substantially less hyperkalemia in a recent phase 3 trial, FIDELIO-DKD, and as a nonsteroidal MRA, it does not cause gynecomastia. Finerenone has promise as a potentially safer option for treating PA and treatment-resistant hypertension, noted Cohen, but so far, no advanced clinical trials have been launched to examine its efficacy for these indications.
PA testing allows a surgical option
A third reason to test patients with treatment-resistant hypertension for PA is that jumping straight to MRA treatment denies the patient assessment for a unilateral adrenal adenoma as the cause of excess aldosterone.
When unilateral adenomas exist, patients are candidates for adrenalectomy. Despite the potential advantage this gives patients to eliminate the cause of their PA without the need for additional drug treatment, some clinicians don’t see this as a compelling rationale to test for PA because they have a bias against surgery or have seen too many cases in which surgery failed to produce full hypertension resolution.
“It’s all about setting expectations appropriately” for the impact of this surgery, Dr. Cohen said.
“Adrenalectomy is not a cure; it just gets rid of the source of excess aldosterone.” But in patients with long-standing PA and hypertension, this is often not enough to completely resolve entrenched cardiovascular pathology.
PCPs, cardiologists in rural locations least likely to order PA testing
Of the 269,010 patients analyzed by Dr. Cohen and her coauthors, the average age was 65 years; 96% were men; half were obese; and 40% had diabetes. The researchers excluded patients who had already been tested for PA, as well as those who were already receiving treatment with an MRA.
For 88% of the patients, the main physician overseeing care was a PCP. A cardiologist was the main physician for 10%; a nephrologist, for 1%; and an endocrinologist, for fewer than 1%.
The rate of testing for PA varied across the 130 VHA centers that contributed data, ranging from 0% to 6%. The testing data showed that endocrinologists were most likely to order PA testing, doing it 2.48-fold more often than PCPs. Nephrologists were roughly twice as likely to order PA testing than PCPs, and cardiologists ordered testing at about the same rate as PCPs.
Patients managed at VHA centers in rural locations were nearly half as likely to undergo testing as patients managed at nonrural centers. The number of patients with treatment-resistant hypertension seen by a physician or at a center had no significant relationship to PA testing frequency.
The study received no commercial funding. Dr. Cohen has disclosed no relevant financial relationships.
A version of this story first appeared on Medscape.com.
Bariatric surgery might reduce severity of COVID-19 infection
and the disease was less severe than among COVID patients with obesity who had not undergone the surgery, a new retrospective analysis shows.
The research was published in Surgery for Obesity and Related Diseases.
Because obesity is a well-known risk factor for poor COVID-19 outcomes, Ali Aminian, MD, Bariatric and Metabolic Institute, Cleveland Clinic, and colleagues decided to study whether weight-loss surgery had a bearing on outcomes of patients with COVID-19.
They matched 33 COVID-19 patients who had undergone metabolic surgery with 330 control patients with obesity who were infected with the virus during the first wave of the pandemic.
Surgery was associated with a 69% reduction in the risk of being hospitalized as a result of COVID-19. None of the surgery patients required intensive care, mechanical ventilation, or dialysis, and none died.
“Patients after bariatric surgery become significantly healthier and can fight the virus better,” said Dr. Aminian in a statement from his institution. “If confirmed by future studies, this can be added to the long list of health benefits of bariatric surgery.”
COVID-19 is a wake-up call for the consequences of obesity
Dr. Aminian said in an interview that COVID-19 is a “wake-up call to show the public and health care professionals that obesity is a major health problem and has multiple health consequences.”
More than 300 articles in the literature show that obesity is a major risk factor for poor outcomes following COVID-19 infection. Dr. Aminian said the pandemic has “improved public awareness about the consequences of obesity.”
Compared with last year at his institution, the intake of new patients “who would like to join a program to have surgery or have some tools to help them to lose weight is almost double,” he noted.
Furthermore, referrals to their unit from primary care physicians, as well as from endocrinologists and cardiologists, for bariatric surgery nearly doubled in recent months.
Although the unit had to stop all bariatric surgeries for around 6 weeks in April because of COVID-19, it has performed the same number of procedures this year as in 2019 and 2018.
Because of the recent surge in COVID cases in Ohio, bariatric procedures are once again on hold. “Elective operations that require hospital beds after surgery have been paused to provide beds for patients who have COVID-19,” he explained.
Small sample size, study should be repeated
For their study, Dr. Aminian and colleagues examined the records of 4,365 patients at the Cleveland Clinic Health System who tested positive for the virus between March 8 and July 22, 2020.
Of these, 1,003 had a body mass index of at least 35 mg/kg2; 482 had a BMI of at least 40. The team identified 33 patients who had previously undergone metabolic surgery, comprising 20 sleeve gastrectomies and 13 Roux-en-Y gastric bypasses.
The surgical patients were propensity matched in a 1:10 ratio with nonsurgical control patients with a BMI of at least 40. The patients were matched on the basis of age, sex, ethnicity, location, smoking status, and history of chronic obstructive pulmonary disease.
The mean BMI of surgical patients was 49.1 before their procedure. It fell to 37.2 by the time they tested positive for COVID-19. This compares with an average of 46.7 in the control group at the time they tested positive for the virus.
The team found that 18.2% of metabolic surgery patients were admitted to hospital versus 42.1% of control patients (P = .013).
Moreover, metabolic surgery patients did not require admission to the intensive care unit, nor did they require mechanical ventilation or dialysis, and none died. This compares with 13.0% (P = .021), 6.7% (P = .24), 1.5%, and 2.4%, respectively, of patients in the control group.
Multivariate analysis indicated that prior metabolic surgery was associated with lower hospital admission, at an odds ratio of 0.31 (P = .028), in comparison with control patients with obesity.
Acknowledging the limited sample size of their study, the team wrote: “As this study reflects findings early in the course of the pandemic, it will be of interest to repeat this study with larger data sets and later in the course of the pandemic.”
Continue as many aspects of obesity management as possible during pandemic
Dr. Aminian underlined that, for him, the take-home message from the study is that health care professionals should “ideally” continue all aspects of obesity management during the pandemic, including “medical management, behavioral therapy, lifestyle changes, and access to bariatric surgery.”
This is despite the fact that insurance coverage for bariatric surgery has “always been a challenge for many patients, since many insurance plans do not cover” bariatric procedures, he noted.
In July, the American Society for Metabolic and Bariatric Surgery issued a statement declaring that obesity surgery should not be considered an elective procedure and should be resumed as soon as it’s safe to do so during any resurgence of the COVID-19 pandemic.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and the disease was less severe than among COVID patients with obesity who had not undergone the surgery, a new retrospective analysis shows.
The research was published in Surgery for Obesity and Related Diseases.
Because obesity is a well-known risk factor for poor COVID-19 outcomes, Ali Aminian, MD, Bariatric and Metabolic Institute, Cleveland Clinic, and colleagues decided to study whether weight-loss surgery had a bearing on outcomes of patients with COVID-19.
They matched 33 COVID-19 patients who had undergone metabolic surgery with 330 control patients with obesity who were infected with the virus during the first wave of the pandemic.
Surgery was associated with a 69% reduction in the risk of being hospitalized as a result of COVID-19. None of the surgery patients required intensive care, mechanical ventilation, or dialysis, and none died.
“Patients after bariatric surgery become significantly healthier and can fight the virus better,” said Dr. Aminian in a statement from his institution. “If confirmed by future studies, this can be added to the long list of health benefits of bariatric surgery.”
COVID-19 is a wake-up call for the consequences of obesity
Dr. Aminian said in an interview that COVID-19 is a “wake-up call to show the public and health care professionals that obesity is a major health problem and has multiple health consequences.”
More than 300 articles in the literature show that obesity is a major risk factor for poor outcomes following COVID-19 infection. Dr. Aminian said the pandemic has “improved public awareness about the consequences of obesity.”
Compared with last year at his institution, the intake of new patients “who would like to join a program to have surgery or have some tools to help them to lose weight is almost double,” he noted.
Furthermore, referrals to their unit from primary care physicians, as well as from endocrinologists and cardiologists, for bariatric surgery nearly doubled in recent months.
Although the unit had to stop all bariatric surgeries for around 6 weeks in April because of COVID-19, it has performed the same number of procedures this year as in 2019 and 2018.
Because of the recent surge in COVID cases in Ohio, bariatric procedures are once again on hold. “Elective operations that require hospital beds after surgery have been paused to provide beds for patients who have COVID-19,” he explained.
Small sample size, study should be repeated
For their study, Dr. Aminian and colleagues examined the records of 4,365 patients at the Cleveland Clinic Health System who tested positive for the virus between March 8 and July 22, 2020.
Of these, 1,003 had a body mass index of at least 35 mg/kg2; 482 had a BMI of at least 40. The team identified 33 patients who had previously undergone metabolic surgery, comprising 20 sleeve gastrectomies and 13 Roux-en-Y gastric bypasses.
The surgical patients were propensity matched in a 1:10 ratio with nonsurgical control patients with a BMI of at least 40. The patients were matched on the basis of age, sex, ethnicity, location, smoking status, and history of chronic obstructive pulmonary disease.
The mean BMI of surgical patients was 49.1 before their procedure. It fell to 37.2 by the time they tested positive for COVID-19. This compares with an average of 46.7 in the control group at the time they tested positive for the virus.
The team found that 18.2% of metabolic surgery patients were admitted to hospital versus 42.1% of control patients (P = .013).
Moreover, metabolic surgery patients did not require admission to the intensive care unit, nor did they require mechanical ventilation or dialysis, and none died. This compares with 13.0% (P = .021), 6.7% (P = .24), 1.5%, and 2.4%, respectively, of patients in the control group.
Multivariate analysis indicated that prior metabolic surgery was associated with lower hospital admission, at an odds ratio of 0.31 (P = .028), in comparison with control patients with obesity.
Acknowledging the limited sample size of their study, the team wrote: “As this study reflects findings early in the course of the pandemic, it will be of interest to repeat this study with larger data sets and later in the course of the pandemic.”
Continue as many aspects of obesity management as possible during pandemic
Dr. Aminian underlined that, for him, the take-home message from the study is that health care professionals should “ideally” continue all aspects of obesity management during the pandemic, including “medical management, behavioral therapy, lifestyle changes, and access to bariatric surgery.”
This is despite the fact that insurance coverage for bariatric surgery has “always been a challenge for many patients, since many insurance plans do not cover” bariatric procedures, he noted.
In July, the American Society for Metabolic and Bariatric Surgery issued a statement declaring that obesity surgery should not be considered an elective procedure and should be resumed as soon as it’s safe to do so during any resurgence of the COVID-19 pandemic.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and the disease was less severe than among COVID patients with obesity who had not undergone the surgery, a new retrospective analysis shows.
The research was published in Surgery for Obesity and Related Diseases.
Because obesity is a well-known risk factor for poor COVID-19 outcomes, Ali Aminian, MD, Bariatric and Metabolic Institute, Cleveland Clinic, and colleagues decided to study whether weight-loss surgery had a bearing on outcomes of patients with COVID-19.
They matched 33 COVID-19 patients who had undergone metabolic surgery with 330 control patients with obesity who were infected with the virus during the first wave of the pandemic.
Surgery was associated with a 69% reduction in the risk of being hospitalized as a result of COVID-19. None of the surgery patients required intensive care, mechanical ventilation, or dialysis, and none died.
“Patients after bariatric surgery become significantly healthier and can fight the virus better,” said Dr. Aminian in a statement from his institution. “If confirmed by future studies, this can be added to the long list of health benefits of bariatric surgery.”
COVID-19 is a wake-up call for the consequences of obesity
Dr. Aminian said in an interview that COVID-19 is a “wake-up call to show the public and health care professionals that obesity is a major health problem and has multiple health consequences.”
More than 300 articles in the literature show that obesity is a major risk factor for poor outcomes following COVID-19 infection. Dr. Aminian said the pandemic has “improved public awareness about the consequences of obesity.”
Compared with last year at his institution, the intake of new patients “who would like to join a program to have surgery or have some tools to help them to lose weight is almost double,” he noted.
Furthermore, referrals to their unit from primary care physicians, as well as from endocrinologists and cardiologists, for bariatric surgery nearly doubled in recent months.
Although the unit had to stop all bariatric surgeries for around 6 weeks in April because of COVID-19, it has performed the same number of procedures this year as in 2019 and 2018.
Because of the recent surge in COVID cases in Ohio, bariatric procedures are once again on hold. “Elective operations that require hospital beds after surgery have been paused to provide beds for patients who have COVID-19,” he explained.
Small sample size, study should be repeated
For their study, Dr. Aminian and colleagues examined the records of 4,365 patients at the Cleveland Clinic Health System who tested positive for the virus between March 8 and July 22, 2020.
Of these, 1,003 had a body mass index of at least 35 mg/kg2; 482 had a BMI of at least 40. The team identified 33 patients who had previously undergone metabolic surgery, comprising 20 sleeve gastrectomies and 13 Roux-en-Y gastric bypasses.
The surgical patients were propensity matched in a 1:10 ratio with nonsurgical control patients with a BMI of at least 40. The patients were matched on the basis of age, sex, ethnicity, location, smoking status, and history of chronic obstructive pulmonary disease.
The mean BMI of surgical patients was 49.1 before their procedure. It fell to 37.2 by the time they tested positive for COVID-19. This compares with an average of 46.7 in the control group at the time they tested positive for the virus.
The team found that 18.2% of metabolic surgery patients were admitted to hospital versus 42.1% of control patients (P = .013).
Moreover, metabolic surgery patients did not require admission to the intensive care unit, nor did they require mechanical ventilation or dialysis, and none died. This compares with 13.0% (P = .021), 6.7% (P = .24), 1.5%, and 2.4%, respectively, of patients in the control group.
Multivariate analysis indicated that prior metabolic surgery was associated with lower hospital admission, at an odds ratio of 0.31 (P = .028), in comparison with control patients with obesity.
Acknowledging the limited sample size of their study, the team wrote: “As this study reflects findings early in the course of the pandemic, it will be of interest to repeat this study with larger data sets and later in the course of the pandemic.”
Continue as many aspects of obesity management as possible during pandemic
Dr. Aminian underlined that, for him, the take-home message from the study is that health care professionals should “ideally” continue all aspects of obesity management during the pandemic, including “medical management, behavioral therapy, lifestyle changes, and access to bariatric surgery.”
This is despite the fact that insurance coverage for bariatric surgery has “always been a challenge for many patients, since many insurance plans do not cover” bariatric procedures, he noted.
In July, the American Society for Metabolic and Bariatric Surgery issued a statement declaring that obesity surgery should not be considered an elective procedure and should be resumed as soon as it’s safe to do so during any resurgence of the COVID-19 pandemic.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Hidden’ danger of type 2 diabetes diagnosis at early age
Those who are found to have type 2 diabetes at a younger age face “hidden” dangers. The issue is becoming more and more important, “since new diagnoses in this younger age group continue to rise,” said the authors of a new study, led by Natalie Nanayakkara, MD.
They believe clinical approaches should be based on age at diagnosis. The results of their new meta-analysis, published online in Diabetologia, reveal the extent of the problem.
Believed to be the first systematic review of its kind, the study showed that the younger the age at diagnosis of type 2 diabetes, the greater the risks of dying and of having either microvascular or macrovascular complications each subsequent year (adjusted for current age).
“This difference in risk between younger and older people in terms of absolute versus lifetime risks of type 2 diabetes complications should perhaps be recognized in diabetes management guidelines,” wrote Dr. Nanayakkara, an endocrinologist at Monash University, Melbourne, and colleagues.
Those diagnosed at younger ages are more likely to develop complications that cause greater disability and lead to loss of productivity compared with people diagnosed at an older age, they stressed.
Hence, they suggested “a greater emphasis on preventive measures for younger people with type 2 diabetes,” with “early intensive multifactorial risk factor intervention ... sustained long term to minimize risks over time.”
Large dataset: Use age at diagnosis to risk stratify patients
Rates of type 2 diabetes have increased in all age groups and virtually all countries over the past 3 decades. Particularly worrying is a trend toward increased rates among adults aged 20-44 years. The increases are associated with higher rates of overweight and obesity, poor diet, and decreasing levels of physical activity, numerous studies have shown.
But few studies have examined the association between age at diagnosis and subsequent complications from type 2 diabetes, the authors noted.
Their review included 26 observational studies involving more than one million individuals from 30 countries in the Asia Pacific, Europe, and North America. The investigators found that each 1-year increase in age at diabetes diagnosis was significantly associated with a 4%, 3%, and 5% decreased risk for all-cause mortality, macrovascular disease, and microvascular disease, respectively, adjusted for current age (all P < .001).
Similar decreases in risk per 1-year increase in age at diabetes diagnosis were seen for coronary heart disease (2%), cerebrovascular disease (2%), peripheral vascular disease (3%), retinopathy (8%), nephropathy (6%), and neuropathy (5%); all associations were significant (P < .001).
Dr. Nanayakkara and colleagues noted that current treatment guidelines are limited in that they’re related to the management of patients with suboptimal blood glucose control, and there is no way to predict which people require intensified treatment.
Therefore, they said, “refined stratification using age at diagnosis may provide a method of identifying, at diagnosis, those at greatest risk of complications who would most benefit from targeted, individualized treatment regimens.”
Awareness of this “hidden” danger to younger adults with type 2 diabetes is becoming more and more important, because such cases continue to rise, they reiterated.
They also advised that “public health measures to delay and/or prevent the onset of type 2 diabetes until older age may yield benefits by reducing the duration of diabetes and the burden of complications.”
Dr. Nanayakkara disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Those who are found to have type 2 diabetes at a younger age face “hidden” dangers. The issue is becoming more and more important, “since new diagnoses in this younger age group continue to rise,” said the authors of a new study, led by Natalie Nanayakkara, MD.
They believe clinical approaches should be based on age at diagnosis. The results of their new meta-analysis, published online in Diabetologia, reveal the extent of the problem.
Believed to be the first systematic review of its kind, the study showed that the younger the age at diagnosis of type 2 diabetes, the greater the risks of dying and of having either microvascular or macrovascular complications each subsequent year (adjusted for current age).
“This difference in risk between younger and older people in terms of absolute versus lifetime risks of type 2 diabetes complications should perhaps be recognized in diabetes management guidelines,” wrote Dr. Nanayakkara, an endocrinologist at Monash University, Melbourne, and colleagues.
Those diagnosed at younger ages are more likely to develop complications that cause greater disability and lead to loss of productivity compared with people diagnosed at an older age, they stressed.
Hence, they suggested “a greater emphasis on preventive measures for younger people with type 2 diabetes,” with “early intensive multifactorial risk factor intervention ... sustained long term to minimize risks over time.”
Large dataset: Use age at diagnosis to risk stratify patients
Rates of type 2 diabetes have increased in all age groups and virtually all countries over the past 3 decades. Particularly worrying is a trend toward increased rates among adults aged 20-44 years. The increases are associated with higher rates of overweight and obesity, poor diet, and decreasing levels of physical activity, numerous studies have shown.
But few studies have examined the association between age at diagnosis and subsequent complications from type 2 diabetes, the authors noted.
Their review included 26 observational studies involving more than one million individuals from 30 countries in the Asia Pacific, Europe, and North America. The investigators found that each 1-year increase in age at diabetes diagnosis was significantly associated with a 4%, 3%, and 5% decreased risk for all-cause mortality, macrovascular disease, and microvascular disease, respectively, adjusted for current age (all P < .001).
Similar decreases in risk per 1-year increase in age at diabetes diagnosis were seen for coronary heart disease (2%), cerebrovascular disease (2%), peripheral vascular disease (3%), retinopathy (8%), nephropathy (6%), and neuropathy (5%); all associations were significant (P < .001).
Dr. Nanayakkara and colleagues noted that current treatment guidelines are limited in that they’re related to the management of patients with suboptimal blood glucose control, and there is no way to predict which people require intensified treatment.
Therefore, they said, “refined stratification using age at diagnosis may provide a method of identifying, at diagnosis, those at greatest risk of complications who would most benefit from targeted, individualized treatment regimens.”
Awareness of this “hidden” danger to younger adults with type 2 diabetes is becoming more and more important, because such cases continue to rise, they reiterated.
They also advised that “public health measures to delay and/or prevent the onset of type 2 diabetes until older age may yield benefits by reducing the duration of diabetes and the burden of complications.”
Dr. Nanayakkara disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Those who are found to have type 2 diabetes at a younger age face “hidden” dangers. The issue is becoming more and more important, “since new diagnoses in this younger age group continue to rise,” said the authors of a new study, led by Natalie Nanayakkara, MD.
They believe clinical approaches should be based on age at diagnosis. The results of their new meta-analysis, published online in Diabetologia, reveal the extent of the problem.
Believed to be the first systematic review of its kind, the study showed that the younger the age at diagnosis of type 2 diabetes, the greater the risks of dying and of having either microvascular or macrovascular complications each subsequent year (adjusted for current age).
“This difference in risk between younger and older people in terms of absolute versus lifetime risks of type 2 diabetes complications should perhaps be recognized in diabetes management guidelines,” wrote Dr. Nanayakkara, an endocrinologist at Monash University, Melbourne, and colleagues.
Those diagnosed at younger ages are more likely to develop complications that cause greater disability and lead to loss of productivity compared with people diagnosed at an older age, they stressed.
Hence, they suggested “a greater emphasis on preventive measures for younger people with type 2 diabetes,” with “early intensive multifactorial risk factor intervention ... sustained long term to minimize risks over time.”
Large dataset: Use age at diagnosis to risk stratify patients
Rates of type 2 diabetes have increased in all age groups and virtually all countries over the past 3 decades. Particularly worrying is a trend toward increased rates among adults aged 20-44 years. The increases are associated with higher rates of overweight and obesity, poor diet, and decreasing levels of physical activity, numerous studies have shown.
But few studies have examined the association between age at diagnosis and subsequent complications from type 2 diabetes, the authors noted.
Their review included 26 observational studies involving more than one million individuals from 30 countries in the Asia Pacific, Europe, and North America. The investigators found that each 1-year increase in age at diabetes diagnosis was significantly associated with a 4%, 3%, and 5% decreased risk for all-cause mortality, macrovascular disease, and microvascular disease, respectively, adjusted for current age (all P < .001).
Similar decreases in risk per 1-year increase in age at diabetes diagnosis were seen for coronary heart disease (2%), cerebrovascular disease (2%), peripheral vascular disease (3%), retinopathy (8%), nephropathy (6%), and neuropathy (5%); all associations were significant (P < .001).
Dr. Nanayakkara and colleagues noted that current treatment guidelines are limited in that they’re related to the management of patients with suboptimal blood glucose control, and there is no way to predict which people require intensified treatment.
Therefore, they said, “refined stratification using age at diagnosis may provide a method of identifying, at diagnosis, those at greatest risk of complications who would most benefit from targeted, individualized treatment regimens.”
Awareness of this “hidden” danger to younger adults with type 2 diabetes is becoming more and more important, because such cases continue to rise, they reiterated.
They also advised that “public health measures to delay and/or prevent the onset of type 2 diabetes until older age may yield benefits by reducing the duration of diabetes and the burden of complications.”
Dr. Nanayakkara disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Anorexia and diarrhea top list of GI symptoms in COVID-19 patients
Patients with severe COVID-19 were significantly more likely than those with milder cases to have GI symptoms of anorexia and diarrhea, as well as abnormal liver function, based on data from a meta-analysis of more than 4,500 patients.
Previous studies have shown that liver damage “was more likely to be observed in severe patients during the process of disease,” and other studies have shown varying degrees of liver insufficiency in COVID-19 patients, but gastrointestinal symptoms have not been well studied, wrote Zi-yuan Dong, MD, of China Medical University, Shenyang City, and colleagues.
In a study published in the Journal of Clinical Gastroenterology, the researchers identified 31 studies including 4,682 COVID-19 patients. Case collection was from Dec. 11, 2019, to Feb. 28, 2020. Median age among studies ranged from 36 to 62 years, and 55% of patients were male.
A total of 26 studies were analyzed for the prevalence of GI symptoms, specifically nausea, vomiting, diarrhea, abdominal pain, and anorexia. Of these, anorexia and diarrhea were significantly more common in COVID-19 patients, with prevalence of 17% and 8% respectively, (P < .0001 for both).
In addition, 14 of the studies included in the analysis assessed the prevalence of abnormal liver function based on increased levels of aspartate aminotransferase, alanine aminotransferase, and total bilirubin. Of these, increased alanine aminotransferase was the most common, occurring in 25% of patients, compared with increased AST (in 24%) and total bilirubin (in 13%).
When assessed by disease severity, patients with severe disease and those in the ICU were significantly more likely than general/non-ICU patients to have anorexia (odds ratio, 2.19), diarrhea (OR, 1.65), and abdominal pain (OR, 6.38). The severely ill patients were significantly more likely to have increased AST and ALT (OR, 2.98 and 2.66, respectively).
“However, there were no significant differences between severe/ICU group and general/non-ICU group for the prevalence of nausea and vomiting and liver disease,” the researchers said.
The study findings were limited by several factors including the unclear classification of digestive system disease and liver disease in many of the studies, the small sample sizes, and the lack of data on pathology of the liver or colon in COVID-19 patients, the researchers noted.
More research is needed, but the findings suggest that COVID-19 could contribute to liver damage because the most significant abnormal liver function was increased ALT, they said.
Check liver function in cases with GI symptoms
“COVID patients can present asymptomatically or with nonspecific symptoms, including GI symptoms,” said Ziad F. Gellad, MD, of Duke University Medical Center, Durham, N.C., in an interview. “While the focus of management naturally is directed to the pulmonary consequences of the disease, it is important to evaluate the patient holistically,” he said.
“I do not think these findings have profound clinical implications because they identify relatively nonspecific symptoms that are commonly seen in patients in a number of other conditions,” noted Dr. Gellad. “The management of COVID should not change, with the exception of perhaps making sure to check for abnormal liver function tests in patients that present with more typical COVID symptoms,” he said.
“Additional research is needed to understand the biologic mechanism by which COVID impacts systems outside of the lungs,” Dr. Gellad emphasized. “For example, there has been some very interesting work understanding the impact of COVID on the pancreas and risk for pancreatitis. That work is similarly needed to understand how COVID, outside of causing a general illness, specifically impacts the rest of the GI tract,” he said.
The study was supported by the Liaoning Science and Technology Foundation. The researchers had no financial conflicts to disclose. Dr. Gellad had no financial conflicts to disclose.
SOURCE: Dong Z-Y et al. J Clin Gastroenterol. 2021 Jan. doi: 10.1097/MCG.0000000000001424.
Patients with severe COVID-19 were significantly more likely than those with milder cases to have GI symptoms of anorexia and diarrhea, as well as abnormal liver function, based on data from a meta-analysis of more than 4,500 patients.
Previous studies have shown that liver damage “was more likely to be observed in severe patients during the process of disease,” and other studies have shown varying degrees of liver insufficiency in COVID-19 patients, but gastrointestinal symptoms have not been well studied, wrote Zi-yuan Dong, MD, of China Medical University, Shenyang City, and colleagues.
In a study published in the Journal of Clinical Gastroenterology, the researchers identified 31 studies including 4,682 COVID-19 patients. Case collection was from Dec. 11, 2019, to Feb. 28, 2020. Median age among studies ranged from 36 to 62 years, and 55% of patients were male.
A total of 26 studies were analyzed for the prevalence of GI symptoms, specifically nausea, vomiting, diarrhea, abdominal pain, and anorexia. Of these, anorexia and diarrhea were significantly more common in COVID-19 patients, with prevalence of 17% and 8% respectively, (P < .0001 for both).
In addition, 14 of the studies included in the analysis assessed the prevalence of abnormal liver function based on increased levels of aspartate aminotransferase, alanine aminotransferase, and total bilirubin. Of these, increased alanine aminotransferase was the most common, occurring in 25% of patients, compared with increased AST (in 24%) and total bilirubin (in 13%).
When assessed by disease severity, patients with severe disease and those in the ICU were significantly more likely than general/non-ICU patients to have anorexia (odds ratio, 2.19), diarrhea (OR, 1.65), and abdominal pain (OR, 6.38). The severely ill patients were significantly more likely to have increased AST and ALT (OR, 2.98 and 2.66, respectively).
“However, there were no significant differences between severe/ICU group and general/non-ICU group for the prevalence of nausea and vomiting and liver disease,” the researchers said.
The study findings were limited by several factors including the unclear classification of digestive system disease and liver disease in many of the studies, the small sample sizes, and the lack of data on pathology of the liver or colon in COVID-19 patients, the researchers noted.
More research is needed, but the findings suggest that COVID-19 could contribute to liver damage because the most significant abnormal liver function was increased ALT, they said.
Check liver function in cases with GI symptoms
“COVID patients can present asymptomatically or with nonspecific symptoms, including GI symptoms,” said Ziad F. Gellad, MD, of Duke University Medical Center, Durham, N.C., in an interview. “While the focus of management naturally is directed to the pulmonary consequences of the disease, it is important to evaluate the patient holistically,” he said.
“I do not think these findings have profound clinical implications because they identify relatively nonspecific symptoms that are commonly seen in patients in a number of other conditions,” noted Dr. Gellad. “The management of COVID should not change, with the exception of perhaps making sure to check for abnormal liver function tests in patients that present with more typical COVID symptoms,” he said.
“Additional research is needed to understand the biologic mechanism by which COVID impacts systems outside of the lungs,” Dr. Gellad emphasized. “For example, there has been some very interesting work understanding the impact of COVID on the pancreas and risk for pancreatitis. That work is similarly needed to understand how COVID, outside of causing a general illness, specifically impacts the rest of the GI tract,” he said.
The study was supported by the Liaoning Science and Technology Foundation. The researchers had no financial conflicts to disclose. Dr. Gellad had no financial conflicts to disclose.
SOURCE: Dong Z-Y et al. J Clin Gastroenterol. 2021 Jan. doi: 10.1097/MCG.0000000000001424.
Patients with severe COVID-19 were significantly more likely than those with milder cases to have GI symptoms of anorexia and diarrhea, as well as abnormal liver function, based on data from a meta-analysis of more than 4,500 patients.
Previous studies have shown that liver damage “was more likely to be observed in severe patients during the process of disease,” and other studies have shown varying degrees of liver insufficiency in COVID-19 patients, but gastrointestinal symptoms have not been well studied, wrote Zi-yuan Dong, MD, of China Medical University, Shenyang City, and colleagues.
In a study published in the Journal of Clinical Gastroenterology, the researchers identified 31 studies including 4,682 COVID-19 patients. Case collection was from Dec. 11, 2019, to Feb. 28, 2020. Median age among studies ranged from 36 to 62 years, and 55% of patients were male.
A total of 26 studies were analyzed for the prevalence of GI symptoms, specifically nausea, vomiting, diarrhea, abdominal pain, and anorexia. Of these, anorexia and diarrhea were significantly more common in COVID-19 patients, with prevalence of 17% and 8% respectively, (P < .0001 for both).
In addition, 14 of the studies included in the analysis assessed the prevalence of abnormal liver function based on increased levels of aspartate aminotransferase, alanine aminotransferase, and total bilirubin. Of these, increased alanine aminotransferase was the most common, occurring in 25% of patients, compared with increased AST (in 24%) and total bilirubin (in 13%).
When assessed by disease severity, patients with severe disease and those in the ICU were significantly more likely than general/non-ICU patients to have anorexia (odds ratio, 2.19), diarrhea (OR, 1.65), and abdominal pain (OR, 6.38). The severely ill patients were significantly more likely to have increased AST and ALT (OR, 2.98 and 2.66, respectively).
“However, there were no significant differences between severe/ICU group and general/non-ICU group for the prevalence of nausea and vomiting and liver disease,” the researchers said.
The study findings were limited by several factors including the unclear classification of digestive system disease and liver disease in many of the studies, the small sample sizes, and the lack of data on pathology of the liver or colon in COVID-19 patients, the researchers noted.
More research is needed, but the findings suggest that COVID-19 could contribute to liver damage because the most significant abnormal liver function was increased ALT, they said.
Check liver function in cases with GI symptoms
“COVID patients can present asymptomatically or with nonspecific symptoms, including GI symptoms,” said Ziad F. Gellad, MD, of Duke University Medical Center, Durham, N.C., in an interview. “While the focus of management naturally is directed to the pulmonary consequences of the disease, it is important to evaluate the patient holistically,” he said.
“I do not think these findings have profound clinical implications because they identify relatively nonspecific symptoms that are commonly seen in patients in a number of other conditions,” noted Dr. Gellad. “The management of COVID should not change, with the exception of perhaps making sure to check for abnormal liver function tests in patients that present with more typical COVID symptoms,” he said.
“Additional research is needed to understand the biologic mechanism by which COVID impacts systems outside of the lungs,” Dr. Gellad emphasized. “For example, there has been some very interesting work understanding the impact of COVID on the pancreas and risk for pancreatitis. That work is similarly needed to understand how COVID, outside of causing a general illness, specifically impacts the rest of the GI tract,” he said.
The study was supported by the Liaoning Science and Technology Foundation. The researchers had no financial conflicts to disclose. Dr. Gellad had no financial conflicts to disclose.
SOURCE: Dong Z-Y et al. J Clin Gastroenterol. 2021 Jan. doi: 10.1097/MCG.0000000000001424.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
FDA okays first generic injected glucagon for hypoglycemia
The FDA determined that Amphastar’s Glucagon for Injection Emergency Kit, 1 mg, a synthetic peptide product, is bioequivalent and therapeutically equivalent to Eli Lilly’s recombinant DNA Glucagon Emergency Kit for Low Blood Sugar.
Both require a multistep mixing process that means they are complicated to use.
In 2019, FDA approved two branded, easier-to-use formulations of glucagon – one nasally administered (Baqsimi, Eli Lilly & Co) and the other a prefilled pen or syringe (Gvoke HypoPen and Gvoke PFS, respectively, Xeris Pharmaceuticals).
The new generic will have the advantage of lower cost, Amphastar spokesman Dan Dischner said in an interview.
“Our generic glucagon will be priced as a generic product so that patients will benefit from a lower price. As we are just at the beginning of the commercialization of the product, we are unable to discuss our specific product price,” he wrote.
As with the branded Lilly injectable glucagon, the new generic is also indicated as a diagnostic aid in gastrointestinal radiologic imaging, as glucagon slows gastric motility.
According to an FDA statement, glucagon is a “complex product” that has been difficult to manufacture generically despite the lifting of patent protection. This approval was the result of the FDA’s efforts to encourage the development and submission of applications for such drugs.
Amphastar specializes in “developing, manufacturing, marketing, and selling technically-challenging generic and proprietary injectable, inhalation, and intranasal products,” the company website says.
Mr. Dischner said, “Glucagon is a complex product that requires R&D and manufacturing capabilities to develop a highly purified synthetic peptide product bioequivalent and therapeutically equivalent to the recombinant DNA origin Glucagon. Given that this product has been through various review cycles, its complexity, and the technological capabilities required to manufacture, it is no surprise that there hasn’t been a generic of glucagon until now.”
Side effects of injected glucagon include nausea, vomiting, transient increase in heart rate, and redness/swelling of the injection site.
Mr. Dischner added, “We are confident that our generic to Lilly’s time-tested glucagon will provide a favorable option, at a reasonable price, to patients who rely on this product.”
A version of this article first appeared on Medscape.com.
The FDA determined that Amphastar’s Glucagon for Injection Emergency Kit, 1 mg, a synthetic peptide product, is bioequivalent and therapeutically equivalent to Eli Lilly’s recombinant DNA Glucagon Emergency Kit for Low Blood Sugar.
Both require a multistep mixing process that means they are complicated to use.
In 2019, FDA approved two branded, easier-to-use formulations of glucagon – one nasally administered (Baqsimi, Eli Lilly & Co) and the other a prefilled pen or syringe (Gvoke HypoPen and Gvoke PFS, respectively, Xeris Pharmaceuticals).
The new generic will have the advantage of lower cost, Amphastar spokesman Dan Dischner said in an interview.
“Our generic glucagon will be priced as a generic product so that patients will benefit from a lower price. As we are just at the beginning of the commercialization of the product, we are unable to discuss our specific product price,” he wrote.
As with the branded Lilly injectable glucagon, the new generic is also indicated as a diagnostic aid in gastrointestinal radiologic imaging, as glucagon slows gastric motility.
According to an FDA statement, glucagon is a “complex product” that has been difficult to manufacture generically despite the lifting of patent protection. This approval was the result of the FDA’s efforts to encourage the development and submission of applications for such drugs.
Amphastar specializes in “developing, manufacturing, marketing, and selling technically-challenging generic and proprietary injectable, inhalation, and intranasal products,” the company website says.
Mr. Dischner said, “Glucagon is a complex product that requires R&D and manufacturing capabilities to develop a highly purified synthetic peptide product bioequivalent and therapeutically equivalent to the recombinant DNA origin Glucagon. Given that this product has been through various review cycles, its complexity, and the technological capabilities required to manufacture, it is no surprise that there hasn’t been a generic of glucagon until now.”
Side effects of injected glucagon include nausea, vomiting, transient increase in heart rate, and redness/swelling of the injection site.
Mr. Dischner added, “We are confident that our generic to Lilly’s time-tested glucagon will provide a favorable option, at a reasonable price, to patients who rely on this product.”
A version of this article first appeared on Medscape.com.
The FDA determined that Amphastar’s Glucagon for Injection Emergency Kit, 1 mg, a synthetic peptide product, is bioequivalent and therapeutically equivalent to Eli Lilly’s recombinant DNA Glucagon Emergency Kit for Low Blood Sugar.
Both require a multistep mixing process that means they are complicated to use.
In 2019, FDA approved two branded, easier-to-use formulations of glucagon – one nasally administered (Baqsimi, Eli Lilly & Co) and the other a prefilled pen or syringe (Gvoke HypoPen and Gvoke PFS, respectively, Xeris Pharmaceuticals).
The new generic will have the advantage of lower cost, Amphastar spokesman Dan Dischner said in an interview.
“Our generic glucagon will be priced as a generic product so that patients will benefit from a lower price. As we are just at the beginning of the commercialization of the product, we are unable to discuss our specific product price,” he wrote.
As with the branded Lilly injectable glucagon, the new generic is also indicated as a diagnostic aid in gastrointestinal radiologic imaging, as glucagon slows gastric motility.
According to an FDA statement, glucagon is a “complex product” that has been difficult to manufacture generically despite the lifting of patent protection. This approval was the result of the FDA’s efforts to encourage the development and submission of applications for such drugs.
Amphastar specializes in “developing, manufacturing, marketing, and selling technically-challenging generic and proprietary injectable, inhalation, and intranasal products,” the company website says.
Mr. Dischner said, “Glucagon is a complex product that requires R&D and manufacturing capabilities to develop a highly purified synthetic peptide product bioequivalent and therapeutically equivalent to the recombinant DNA origin Glucagon. Given that this product has been through various review cycles, its complexity, and the technological capabilities required to manufacture, it is no surprise that there hasn’t been a generic of glucagon until now.”
Side effects of injected glucagon include nausea, vomiting, transient increase in heart rate, and redness/swelling of the injection site.
Mr. Dischner added, “We are confident that our generic to Lilly’s time-tested glucagon will provide a favorable option, at a reasonable price, to patients who rely on this product.”
A version of this article first appeared on Medscape.com.
New pediatric cases down as U.S. tops 2 million children with COVID-19
The United States exceeded 2 million reported cases of COVID-19 in children just 6 weeks after recording its 1 millionth case, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
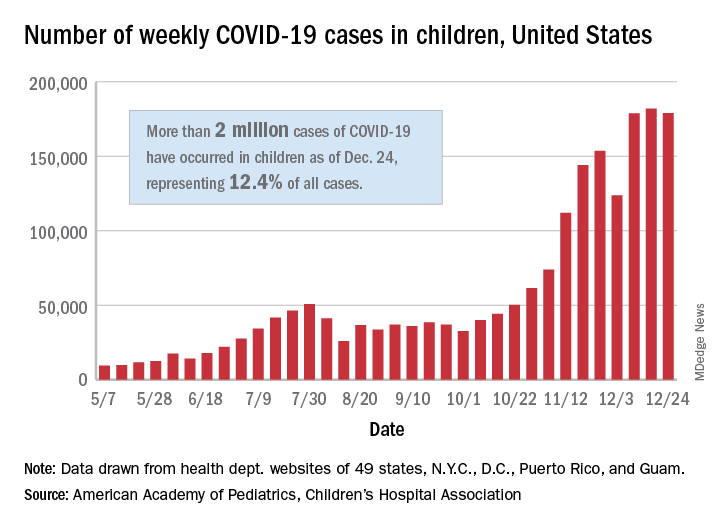
The total number of cases in children was 2,000,681 as of Dec. 24, which represents 12.4% of all cases reported by the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA stated Dec. 29.
The case count for just the latest week, 178,935, was actually down 1.7% from the 182,018 reported the week before, marking the second drop since the beginning of December. The first came during the week ending Dec. 3, when the number of cases dropped more than 19% from the previous week, based on data from the AAP/CHA report.
The cumulative national rate of coronavirus infection is now 2,658 cases per 100,000 children, and “13 states have reported more than 4,000 cases per 100,000,” the two groups said.
The highest rate for any state can be found in North Dakota, which has had 7,722 cases of COVID-19 per 100,000 children. Wyoming has the highest proportion of cases in children at 20.5%, and California has reported the most cases overall, 234,174, the report shows.
Data on testing, hospitalization, and mortality were not included in the Dec. 29 report because of the holiday but will be available in the next edition, scheduled for release on Jan. 5, 2021.
The United States exceeded 2 million reported cases of COVID-19 in children just 6 weeks after recording its 1 millionth case, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
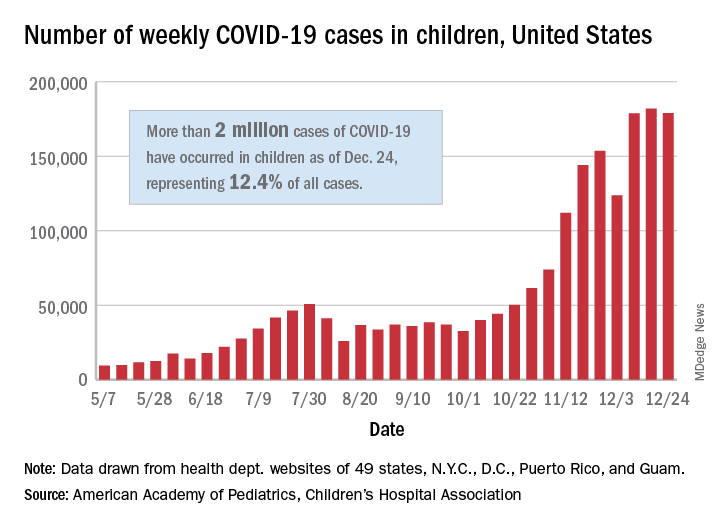
The total number of cases in children was 2,000,681 as of Dec. 24, which represents 12.4% of all cases reported by the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA stated Dec. 29.
The case count for just the latest week, 178,935, was actually down 1.7% from the 182,018 reported the week before, marking the second drop since the beginning of December. The first came during the week ending Dec. 3, when the number of cases dropped more than 19% from the previous week, based on data from the AAP/CHA report.
The cumulative national rate of coronavirus infection is now 2,658 cases per 100,000 children, and “13 states have reported more than 4,000 cases per 100,000,” the two groups said.
The highest rate for any state can be found in North Dakota, which has had 7,722 cases of COVID-19 per 100,000 children. Wyoming has the highest proportion of cases in children at 20.5%, and California has reported the most cases overall, 234,174, the report shows.
Data on testing, hospitalization, and mortality were not included in the Dec. 29 report because of the holiday but will be available in the next edition, scheduled for release on Jan. 5, 2021.
The United States exceeded 2 million reported cases of COVID-19 in children just 6 weeks after recording its 1 millionth case, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
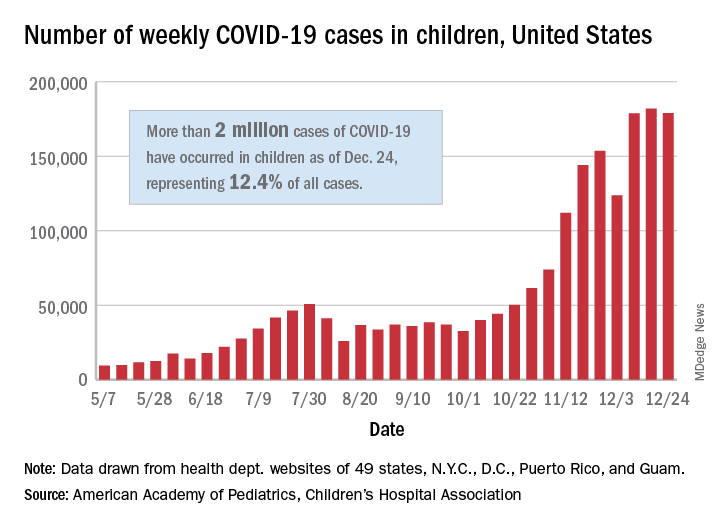
The total number of cases in children was 2,000,681 as of Dec. 24, which represents 12.4% of all cases reported by the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA stated Dec. 29.
The case count for just the latest week, 178,935, was actually down 1.7% from the 182,018 reported the week before, marking the second drop since the beginning of December. The first came during the week ending Dec. 3, when the number of cases dropped more than 19% from the previous week, based on data from the AAP/CHA report.
The cumulative national rate of coronavirus infection is now 2,658 cases per 100,000 children, and “13 states have reported more than 4,000 cases per 100,000,” the two groups said.
The highest rate for any state can be found in North Dakota, which has had 7,722 cases of COVID-19 per 100,000 children. Wyoming has the highest proportion of cases in children at 20.5%, and California has reported the most cases overall, 234,174, the report shows.
Data on testing, hospitalization, and mortality were not included in the Dec. 29 report because of the holiday but will be available in the next edition, scheduled for release on Jan. 5, 2021.
New dietary guidelines omit recommended cuts to sugar, alcohol intake
Although the new guidelines were informed by an advisory committee’s scientific report, officials omitted certain recommendations that would have reduced allowances for added sugars and alcohol intake.
The 2020-2025 Dietary Guidelines for Americans “carried forward the committee’s emphasis on limiting these dietary components, but did not include changes to quantitative recommendations, as there was not a preponderance of evidence in the material the committee reviewed to support specific changes, as required by law,” the agencies said in a news release.
The guidelines encourage Americans to “Make Every Bite Count” through four overarching suggestions:
- Follow a healthy dietary pattern at every life stage.
- Customize nutrient-dense food and beverage choices to reflect preferences, cultural traditions, and budgets.
- Focus on meeting dietary needs from five food groups – vegetables, fruits, grains, dairy and fortified soy alternatives, and proteins – and stay within calorie limits.
- Limit foods and beverages that are higher in added sugars, saturated fat, and sodium, and limit alcoholic beverages.
The guidance “can help all Americans lead healthier lives by making every bite count,” Secretary of Agriculture Sonny Perdue said.
Proposed cutoffs rejected
The guidelines omit a recommendation from the advisory committee’s scientific report to reduce intake of added sugars from less than 10% of calories to less than 6% of calories.
It also omits a recommendation that men and women who drink alcohol limit themselves to one drink per day. It maintains guidance from the 2015-2020 edition that allows two drinks per day for men.
The agencies published a document explaining why they omitted the advisory committee›s conclusions.
The American Heart Association in July had praised the suggestion to reduce added sugars. The proposed change would have helped “steer the public toward a more heart-healthy path in their daily diets,” Mitchell S.V. Elkind, MD, president of the AHA, said at the time. The association would “strongly oppose any efforts to weaken these recommendations,” he added.
In its response to the new guidelines, Dr. Elkind praised the emphasis on a healthy diet “at every life stage” but called out a missed opportunity.
“We are disappointed that USDA and HHS did not accept all of the Dietary Guidelines Advisory Committee’s science-based recommendations in the final guidelines for 2020, including the recommendation to lower added sugars consumption to less than 6% of calories,” he said in a prepared statement.
Guidance for infants and toddlers
The guidelines advise that for about the first 6 months of life, infants should exclusively receive breast milk. Infants should continue to receive breast milk through at least the first year of life, and longer if desired. Infants should be fed iron-fortified infant formula during the first year of life when breast milk is unavailable, and infants should receive supplemental vitamin D soon after birth, the guidelines advise.
At about 6 months, infants should be introduced to a variety of nutrient-dense complementary foods, including potentially allergenic foods. Infants should eat foods that are rich in iron and zinc, particularly if they are fed breast milk.
The guidelines also include dietary and caloric advice for pregnant and lactating women with daily or weekly amounts of food from different groups and subgroups.
Dr. Elkind highlighted the significance of these additions.
“We are pleased that for the first time, the guidelines provide recommendations for pregnant and breastfeeding women as well as infants and toddlers, underscoring the importance of maternal health and proper nutrition across the lifespan,” he said.
For all ages
From 12 months through older adulthood, people should follow a healthy dietary pattern to meet nutrient needs, help achieve a healthy body weight, and reduce the risk of chronic disease.
According to the guidelines, core elements of a healthy diet include:
- Vegetables of all types (dark green; red and orange; beans, peas, and lentils; starchy; and other types).
- Fruits (especially whole fruit).
- Grains, at least half of which are whole grain.
- Dairy, including fat-free or low-fat milk, yogurt, and cheese, and lactose-free versions; and fortified soy beverages and yogurt as alternatives.
- Protein foods, including lean meats, poultry, and eggs; seafood; beans, peas, and lentils; and nuts, seeds, and soy products.
- Oils, including vegetable oils and oils in food, such as seafood and nuts.
The guidelines spell out limits to added sugars, sodium, saturated fat, and alcohol. The recommendation to limit added sugars to less than 10% of calories per day starts at age 2 years. Before age 2, foods and beverages with added sugars should be avoided.
Saturated fat should be limited to less than 10% of calories per day starting at age 2. And sodium intake should be limited to 2,300 mg/day for those age 14 and older, but just 1,200 mg/day for toddlers, 1,500 mg/day for children aged 4-8, and 1,800 mg/day for children 9-13.
“Adults of legal drinking age can choose not to drink or to drink in moderation by limiting intake to 2 drinks or less in a day for men and 1 drink or less in a day for women, when alcohol is consumed,” the agencies said. “Drinking less is better for health than drinking more. There are some adults who should not drink alcohol, such as women who are pregnant.”
An appendix includes estimated calorie needs based on a person’s age, sex, height, weight, and level of physical activity. A need to lose, maintain, or gain weight are among the factors that influence how many calories should be consumed, the guidelines note.
The guidelines are designed for use by health care professionals and policymakers. The USDA has launched a new MyPlate website to help consumers incorporate the dietary guidance.
A version of this article first appeared on Medscape.com.
Although the new guidelines were informed by an advisory committee’s scientific report, officials omitted certain recommendations that would have reduced allowances for added sugars and alcohol intake.
The 2020-2025 Dietary Guidelines for Americans “carried forward the committee’s emphasis on limiting these dietary components, but did not include changes to quantitative recommendations, as there was not a preponderance of evidence in the material the committee reviewed to support specific changes, as required by law,” the agencies said in a news release.
The guidelines encourage Americans to “Make Every Bite Count” through four overarching suggestions:
- Follow a healthy dietary pattern at every life stage.
- Customize nutrient-dense food and beverage choices to reflect preferences, cultural traditions, and budgets.
- Focus on meeting dietary needs from five food groups – vegetables, fruits, grains, dairy and fortified soy alternatives, and proteins – and stay within calorie limits.
- Limit foods and beverages that are higher in added sugars, saturated fat, and sodium, and limit alcoholic beverages.
The guidance “can help all Americans lead healthier lives by making every bite count,” Secretary of Agriculture Sonny Perdue said.
Proposed cutoffs rejected
The guidelines omit a recommendation from the advisory committee’s scientific report to reduce intake of added sugars from less than 10% of calories to less than 6% of calories.
It also omits a recommendation that men and women who drink alcohol limit themselves to one drink per day. It maintains guidance from the 2015-2020 edition that allows two drinks per day for men.
The agencies published a document explaining why they omitted the advisory committee›s conclusions.
The American Heart Association in July had praised the suggestion to reduce added sugars. The proposed change would have helped “steer the public toward a more heart-healthy path in their daily diets,” Mitchell S.V. Elkind, MD, president of the AHA, said at the time. The association would “strongly oppose any efforts to weaken these recommendations,” he added.
In its response to the new guidelines, Dr. Elkind praised the emphasis on a healthy diet “at every life stage” but called out a missed opportunity.
“We are disappointed that USDA and HHS did not accept all of the Dietary Guidelines Advisory Committee’s science-based recommendations in the final guidelines for 2020, including the recommendation to lower added sugars consumption to less than 6% of calories,” he said in a prepared statement.
Guidance for infants and toddlers
The guidelines advise that for about the first 6 months of life, infants should exclusively receive breast milk. Infants should continue to receive breast milk through at least the first year of life, and longer if desired. Infants should be fed iron-fortified infant formula during the first year of life when breast milk is unavailable, and infants should receive supplemental vitamin D soon after birth, the guidelines advise.
At about 6 months, infants should be introduced to a variety of nutrient-dense complementary foods, including potentially allergenic foods. Infants should eat foods that are rich in iron and zinc, particularly if they are fed breast milk.
The guidelines also include dietary and caloric advice for pregnant and lactating women with daily or weekly amounts of food from different groups and subgroups.
Dr. Elkind highlighted the significance of these additions.
“We are pleased that for the first time, the guidelines provide recommendations for pregnant and breastfeeding women as well as infants and toddlers, underscoring the importance of maternal health and proper nutrition across the lifespan,” he said.
For all ages
From 12 months through older adulthood, people should follow a healthy dietary pattern to meet nutrient needs, help achieve a healthy body weight, and reduce the risk of chronic disease.
According to the guidelines, core elements of a healthy diet include:
- Vegetables of all types (dark green; red and orange; beans, peas, and lentils; starchy; and other types).
- Fruits (especially whole fruit).
- Grains, at least half of which are whole grain.
- Dairy, including fat-free or low-fat milk, yogurt, and cheese, and lactose-free versions; and fortified soy beverages and yogurt as alternatives.
- Protein foods, including lean meats, poultry, and eggs; seafood; beans, peas, and lentils; and nuts, seeds, and soy products.
- Oils, including vegetable oils and oils in food, such as seafood and nuts.
The guidelines spell out limits to added sugars, sodium, saturated fat, and alcohol. The recommendation to limit added sugars to less than 10% of calories per day starts at age 2 years. Before age 2, foods and beverages with added sugars should be avoided.
Saturated fat should be limited to less than 10% of calories per day starting at age 2. And sodium intake should be limited to 2,300 mg/day for those age 14 and older, but just 1,200 mg/day for toddlers, 1,500 mg/day for children aged 4-8, and 1,800 mg/day for children 9-13.
“Adults of legal drinking age can choose not to drink or to drink in moderation by limiting intake to 2 drinks or less in a day for men and 1 drink or less in a day for women, when alcohol is consumed,” the agencies said. “Drinking less is better for health than drinking more. There are some adults who should not drink alcohol, such as women who are pregnant.”
An appendix includes estimated calorie needs based on a person’s age, sex, height, weight, and level of physical activity. A need to lose, maintain, or gain weight are among the factors that influence how many calories should be consumed, the guidelines note.
The guidelines are designed for use by health care professionals and policymakers. The USDA has launched a new MyPlate website to help consumers incorporate the dietary guidance.
A version of this article first appeared on Medscape.com.
Although the new guidelines were informed by an advisory committee’s scientific report, officials omitted certain recommendations that would have reduced allowances for added sugars and alcohol intake.
The 2020-2025 Dietary Guidelines for Americans “carried forward the committee’s emphasis on limiting these dietary components, but did not include changes to quantitative recommendations, as there was not a preponderance of evidence in the material the committee reviewed to support specific changes, as required by law,” the agencies said in a news release.
The guidelines encourage Americans to “Make Every Bite Count” through four overarching suggestions:
- Follow a healthy dietary pattern at every life stage.
- Customize nutrient-dense food and beverage choices to reflect preferences, cultural traditions, and budgets.
- Focus on meeting dietary needs from five food groups – vegetables, fruits, grains, dairy and fortified soy alternatives, and proteins – and stay within calorie limits.
- Limit foods and beverages that are higher in added sugars, saturated fat, and sodium, and limit alcoholic beverages.
The guidance “can help all Americans lead healthier lives by making every bite count,” Secretary of Agriculture Sonny Perdue said.
Proposed cutoffs rejected
The guidelines omit a recommendation from the advisory committee’s scientific report to reduce intake of added sugars from less than 10% of calories to less than 6% of calories.
It also omits a recommendation that men and women who drink alcohol limit themselves to one drink per day. It maintains guidance from the 2015-2020 edition that allows two drinks per day for men.
The agencies published a document explaining why they omitted the advisory committee›s conclusions.
The American Heart Association in July had praised the suggestion to reduce added sugars. The proposed change would have helped “steer the public toward a more heart-healthy path in their daily diets,” Mitchell S.V. Elkind, MD, president of the AHA, said at the time. The association would “strongly oppose any efforts to weaken these recommendations,” he added.
In its response to the new guidelines, Dr. Elkind praised the emphasis on a healthy diet “at every life stage” but called out a missed opportunity.
“We are disappointed that USDA and HHS did not accept all of the Dietary Guidelines Advisory Committee’s science-based recommendations in the final guidelines for 2020, including the recommendation to lower added sugars consumption to less than 6% of calories,” he said in a prepared statement.
Guidance for infants and toddlers
The guidelines advise that for about the first 6 months of life, infants should exclusively receive breast milk. Infants should continue to receive breast milk through at least the first year of life, and longer if desired. Infants should be fed iron-fortified infant formula during the first year of life when breast milk is unavailable, and infants should receive supplemental vitamin D soon after birth, the guidelines advise.
At about 6 months, infants should be introduced to a variety of nutrient-dense complementary foods, including potentially allergenic foods. Infants should eat foods that are rich in iron and zinc, particularly if they are fed breast milk.
The guidelines also include dietary and caloric advice for pregnant and lactating women with daily or weekly amounts of food from different groups and subgroups.
Dr. Elkind highlighted the significance of these additions.
“We are pleased that for the first time, the guidelines provide recommendations for pregnant and breastfeeding women as well as infants and toddlers, underscoring the importance of maternal health and proper nutrition across the lifespan,” he said.
For all ages
From 12 months through older adulthood, people should follow a healthy dietary pattern to meet nutrient needs, help achieve a healthy body weight, and reduce the risk of chronic disease.
According to the guidelines, core elements of a healthy diet include:
- Vegetables of all types (dark green; red and orange; beans, peas, and lentils; starchy; and other types).
- Fruits (especially whole fruit).
- Grains, at least half of which are whole grain.
- Dairy, including fat-free or low-fat milk, yogurt, and cheese, and lactose-free versions; and fortified soy beverages and yogurt as alternatives.
- Protein foods, including lean meats, poultry, and eggs; seafood; beans, peas, and lentils; and nuts, seeds, and soy products.
- Oils, including vegetable oils and oils in food, such as seafood and nuts.
The guidelines spell out limits to added sugars, sodium, saturated fat, and alcohol. The recommendation to limit added sugars to less than 10% of calories per day starts at age 2 years. Before age 2, foods and beverages with added sugars should be avoided.
Saturated fat should be limited to less than 10% of calories per day starting at age 2. And sodium intake should be limited to 2,300 mg/day for those age 14 and older, but just 1,200 mg/day for toddlers, 1,500 mg/day for children aged 4-8, and 1,800 mg/day for children 9-13.
“Adults of legal drinking age can choose not to drink or to drink in moderation by limiting intake to 2 drinks or less in a day for men and 1 drink or less in a day for women, when alcohol is consumed,” the agencies said. “Drinking less is better for health than drinking more. There are some adults who should not drink alcohol, such as women who are pregnant.”
An appendix includes estimated calorie needs based on a person’s age, sex, height, weight, and level of physical activity. A need to lose, maintain, or gain weight are among the factors that influence how many calories should be consumed, the guidelines note.
The guidelines are designed for use by health care professionals and policymakers. The USDA has launched a new MyPlate website to help consumers incorporate the dietary guidance.
A version of this article first appeared on Medscape.com.





