User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Clinical Updates on Osteoarthritis of the Hip
As primary care doctors, we diagnosis and treat many patients with osteoarthritis. In fact, according to World Health Organization statistics, approximately 528 million people around the world suffer from some form of this type of arthritis. With the aging of the population and the obesity epidemic, the rate of osteoarthritis has increased 113% since 1990 and is predicted to continue to rise.
While the knee is the most commonly affected joint, osteoarthritis also frequently affects the hands and hips. The American Academy of Orthopaedic Surgeons issued guidelines concerning the management of osteoarthritis of the hip. The clinical guidelines are aimed at orthopedists, but it is important for primary care doctors be aware of them as well since we are the physicians who usually diagnose the disease, manage it in its early stages, and follow the patients with and after the orthopedist has undertaken any procedures.
While the complete set of guidelines is 80 pages long, strong recommendations have been made that everyone should be aware of. The role of non-steroidal anti-inflammatory drugs has been reconfirmed as a modality to improve pain and function. A recommendation against using intra-articular hyaluronic acid in the hip was made as the evidence shows it did not improve pain or function better than placebo. Conversely, intra-articular corticosteroids were shown to improve pain and function in the short-term and many primary care doctors provide this treatment in their practice.
These guidelines do a great job covering the totality of management of osteoarthritis of the hip, from conservation management to surgical and post-surgical treatments. Patients often come to us with their questions so not only is it important to know the evidence for what we do in our practices, we need to know what our orthopedic colleagues are doing. We will be the ones asked to do the pre-operative evaluations on these patients, so we need to understand the procedure and its risks. We will also manage these patients post-operatively and need to be aware of what the evidence shows.
Opioid use is also covered in the guidelines: they recommend against the use of opioids to control pain in these patients. In the age of the opioid epidemic, it is a good reminder to be cautious with these meds. It is also a good time to stress smoking cessation with patients.
The guidelines discuss adverse outcomes in patients with diabetes and/or obesity. As primary care physicians, we need to be aware of those risks and be sure our patients are medically optimized before signing that pre-operative form.
A new feature of these guidelines is a discussion on social detriments to health. This is important for many diseases that we treat and we often don’t realize the impact they can have on a patient’s health and recovery. Even if we know a patient would benefit from physical therapy, it doesn’t help them if the patient has no way to get to the appointment. Some patients have copays for every physical therapy session and just can’t afford it. Knowing what the patient needs medically is not enough. We need to understand how they can access that care. Some patients have no one to help them after hip surgery and may avoid doing it for that reason. As primary care doctors, we should be helping our patients access the care they need.
We need to be able to say that a procedure needs to be delayed in the face of poorly controlled disease, such as diabetes. As the rates of osteoarthritis continue to rise, we need to understand that it is not an inevitable age-based occurrence in a patient’s life but rather an inflammatory disease that causes great pain and dysfunction. Utilizing these guidelines and working with our orthopedic colleagues can help patients decrease pain, improve functioning, and enjoy life again.
Dr. Girgis practices family medicine in South River, New Jersey, and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, New Jersey. She was paid by Pfizer as a consultant on Paxlovid, paid by GlaxoSmithKline as a consultant for the Shingrix vaccine, and is the editor in chief of Physician’s Weekly.
As primary care doctors, we diagnosis and treat many patients with osteoarthritis. In fact, according to World Health Organization statistics, approximately 528 million people around the world suffer from some form of this type of arthritis. With the aging of the population and the obesity epidemic, the rate of osteoarthritis has increased 113% since 1990 and is predicted to continue to rise.
While the knee is the most commonly affected joint, osteoarthritis also frequently affects the hands and hips. The American Academy of Orthopaedic Surgeons issued guidelines concerning the management of osteoarthritis of the hip. The clinical guidelines are aimed at orthopedists, but it is important for primary care doctors be aware of them as well since we are the physicians who usually diagnose the disease, manage it in its early stages, and follow the patients with and after the orthopedist has undertaken any procedures.
While the complete set of guidelines is 80 pages long, strong recommendations have been made that everyone should be aware of. The role of non-steroidal anti-inflammatory drugs has been reconfirmed as a modality to improve pain and function. A recommendation against using intra-articular hyaluronic acid in the hip was made as the evidence shows it did not improve pain or function better than placebo. Conversely, intra-articular corticosteroids were shown to improve pain and function in the short-term and many primary care doctors provide this treatment in their practice.
These guidelines do a great job covering the totality of management of osteoarthritis of the hip, from conservation management to surgical and post-surgical treatments. Patients often come to us with their questions so not only is it important to know the evidence for what we do in our practices, we need to know what our orthopedic colleagues are doing. We will be the ones asked to do the pre-operative evaluations on these patients, so we need to understand the procedure and its risks. We will also manage these patients post-operatively and need to be aware of what the evidence shows.
Opioid use is also covered in the guidelines: they recommend against the use of opioids to control pain in these patients. In the age of the opioid epidemic, it is a good reminder to be cautious with these meds. It is also a good time to stress smoking cessation with patients.
The guidelines discuss adverse outcomes in patients with diabetes and/or obesity. As primary care physicians, we need to be aware of those risks and be sure our patients are medically optimized before signing that pre-operative form.
A new feature of these guidelines is a discussion on social detriments to health. This is important for many diseases that we treat and we often don’t realize the impact they can have on a patient’s health and recovery. Even if we know a patient would benefit from physical therapy, it doesn’t help them if the patient has no way to get to the appointment. Some patients have copays for every physical therapy session and just can’t afford it. Knowing what the patient needs medically is not enough. We need to understand how they can access that care. Some patients have no one to help them after hip surgery and may avoid doing it for that reason. As primary care doctors, we should be helping our patients access the care they need.
We need to be able to say that a procedure needs to be delayed in the face of poorly controlled disease, such as diabetes. As the rates of osteoarthritis continue to rise, we need to understand that it is not an inevitable age-based occurrence in a patient’s life but rather an inflammatory disease that causes great pain and dysfunction. Utilizing these guidelines and working with our orthopedic colleagues can help patients decrease pain, improve functioning, and enjoy life again.
Dr. Girgis practices family medicine in South River, New Jersey, and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, New Jersey. She was paid by Pfizer as a consultant on Paxlovid, paid by GlaxoSmithKline as a consultant for the Shingrix vaccine, and is the editor in chief of Physician’s Weekly.
As primary care doctors, we diagnosis and treat many patients with osteoarthritis. In fact, according to World Health Organization statistics, approximately 528 million people around the world suffer from some form of this type of arthritis. With the aging of the population and the obesity epidemic, the rate of osteoarthritis has increased 113% since 1990 and is predicted to continue to rise.
While the knee is the most commonly affected joint, osteoarthritis also frequently affects the hands and hips. The American Academy of Orthopaedic Surgeons issued guidelines concerning the management of osteoarthritis of the hip. The clinical guidelines are aimed at orthopedists, but it is important for primary care doctors be aware of them as well since we are the physicians who usually diagnose the disease, manage it in its early stages, and follow the patients with and after the orthopedist has undertaken any procedures.
While the complete set of guidelines is 80 pages long, strong recommendations have been made that everyone should be aware of. The role of non-steroidal anti-inflammatory drugs has been reconfirmed as a modality to improve pain and function. A recommendation against using intra-articular hyaluronic acid in the hip was made as the evidence shows it did not improve pain or function better than placebo. Conversely, intra-articular corticosteroids were shown to improve pain and function in the short-term and many primary care doctors provide this treatment in their practice.
These guidelines do a great job covering the totality of management of osteoarthritis of the hip, from conservation management to surgical and post-surgical treatments. Patients often come to us with their questions so not only is it important to know the evidence for what we do in our practices, we need to know what our orthopedic colleagues are doing. We will be the ones asked to do the pre-operative evaluations on these patients, so we need to understand the procedure and its risks. We will also manage these patients post-operatively and need to be aware of what the evidence shows.
Opioid use is also covered in the guidelines: they recommend against the use of opioids to control pain in these patients. In the age of the opioid epidemic, it is a good reminder to be cautious with these meds. It is also a good time to stress smoking cessation with patients.
The guidelines discuss adverse outcomes in patients with diabetes and/or obesity. As primary care physicians, we need to be aware of those risks and be sure our patients are medically optimized before signing that pre-operative form.
A new feature of these guidelines is a discussion on social detriments to health. This is important for many diseases that we treat and we often don’t realize the impact they can have on a patient’s health and recovery. Even if we know a patient would benefit from physical therapy, it doesn’t help them if the patient has no way to get to the appointment. Some patients have copays for every physical therapy session and just can’t afford it. Knowing what the patient needs medically is not enough. We need to understand how they can access that care. Some patients have no one to help them after hip surgery and may avoid doing it for that reason. As primary care doctors, we should be helping our patients access the care they need.
We need to be able to say that a procedure needs to be delayed in the face of poorly controlled disease, such as diabetes. As the rates of osteoarthritis continue to rise, we need to understand that it is not an inevitable age-based occurrence in a patient’s life but rather an inflammatory disease that causes great pain and dysfunction. Utilizing these guidelines and working with our orthopedic colleagues can help patients decrease pain, improve functioning, and enjoy life again.
Dr. Girgis practices family medicine in South River, New Jersey, and is a clinical assistant professor of family medicine at Robert Wood Johnson Medical School, New Brunswick, New Jersey. She was paid by Pfizer as a consultant on Paxlovid, paid by GlaxoSmithKline as a consultant for the Shingrix vaccine, and is the editor in chief of Physician’s Weekly.
More Evidence Ties Semaglutide to Reduced Alzheimer’s Risk
Adults with type 2 diabetes who were prescribed the GLP-1 RA semaglutide had a significantly lower risk for Alzheimer’s disease compared with their peers who were prescribed any of seven other antidiabetic medications, including other types of GLP-1 receptor–targeting medications.
“These findings support further clinical trials to assess semaglutide’s potential in delaying or preventing Alzheimer’s disease,” wrote the investigators, led by Rong Xu, PhD, with Case Western Reserve School of Medicine, Cleveland, Ohio.
The study was published online on October 24 in Alzheimer’s & Dementia.
Real-World Data
Semaglutide has shown neuroprotective effects in animal models of neurodegenerative diseases, including Alzheimer’s disease and Parkinson’s disease. In animal models of Alzheimer’s disease, the drug reduced beta-amyloid deposition and improved spatial learning and memory, as well as glucose metabolism in the brain.
In a real-world analysis, Xu and colleagues used electronic health record data to identify 17,104 new users of semaglutide and 1,077,657 new users of seven other antidiabetic medications, including other GLP-1 RAs, insulin, metformin, dipeptidyl peptidase 4 inhibitors, sodium-glucose cotransporter 2 inhibitors, sulfonylurea, and thiazolidinedione.
Over 3 years, treatment with semaglutide was associated with significantly reduced risk of developing Alzheimer’s disease, most strongly compared with insulin (hazard ratio [HR], 0.33) and most weakly compared with other GLP-1 RAs (HR, 0.59).
Compared with the other medications, semaglutide was associated with a 40%-70% reduced risk for first-time diagnosis of Alzheimer’s disease in patients with type 2 diabetes, with similar reductions seen across obesity status and gender and age groups, the authors reported.
The findings align with recent evidence suggesting GLP-1 RAs may protect cognitive function.
For example, as previously reported, in the phase 2b ELAD clinical trial, adults with early-stage Alzheimer’s disease taking the GLP-1 RA liraglutide exhibited slower decline in memory and thinking and experienced less brain atrophy over 12 months compared with placebo.
Promising, but Preliminary
Reached for comment, Courtney Kloske, PhD, Alzheimer’s Association director of scientific engagement, noted that diabetes is a known risk factor for AD and managing diabetes with drugs such as semaglutide “could benefit brain health simply by managing diabetes.”
“However, we still need large clinical trials in representative populations to determine if semaglutide specifically lowers the risk of Alzheimer’s, so it is too early to recommend it for prevention,” Kloske said.
She noted that some research suggests that GLP-1 RAs “may help reduce inflammation and positively impact brain energy use. However, more research is needed to fully understand how these processes might contribute to preventing cognitive decline or Alzheimer’s,” Kloske cautioned.
The Alzheimer’s Association’s “Part the Cloud” initiative has invested more than $68 million to advance 65 clinical trials targeting a variety of compounds, including repurposed drugs that may address known and potential new aspects of the disease, Kloske said.
The study was supported by grants from the National Institute on Aging and the National Center for Advancing Translational Sciences. Xu and Kloske have no relevant conflicts.
A version of this article appeared on Medscape.com.
Adults with type 2 diabetes who were prescribed the GLP-1 RA semaglutide had a significantly lower risk for Alzheimer’s disease compared with their peers who were prescribed any of seven other antidiabetic medications, including other types of GLP-1 receptor–targeting medications.
“These findings support further clinical trials to assess semaglutide’s potential in delaying or preventing Alzheimer’s disease,” wrote the investigators, led by Rong Xu, PhD, with Case Western Reserve School of Medicine, Cleveland, Ohio.
The study was published online on October 24 in Alzheimer’s & Dementia.
Real-World Data
Semaglutide has shown neuroprotective effects in animal models of neurodegenerative diseases, including Alzheimer’s disease and Parkinson’s disease. In animal models of Alzheimer’s disease, the drug reduced beta-amyloid deposition and improved spatial learning and memory, as well as glucose metabolism in the brain.
In a real-world analysis, Xu and colleagues used electronic health record data to identify 17,104 new users of semaglutide and 1,077,657 new users of seven other antidiabetic medications, including other GLP-1 RAs, insulin, metformin, dipeptidyl peptidase 4 inhibitors, sodium-glucose cotransporter 2 inhibitors, sulfonylurea, and thiazolidinedione.
Over 3 years, treatment with semaglutide was associated with significantly reduced risk of developing Alzheimer’s disease, most strongly compared with insulin (hazard ratio [HR], 0.33) and most weakly compared with other GLP-1 RAs (HR, 0.59).
Compared with the other medications, semaglutide was associated with a 40%-70% reduced risk for first-time diagnosis of Alzheimer’s disease in patients with type 2 diabetes, with similar reductions seen across obesity status and gender and age groups, the authors reported.
The findings align with recent evidence suggesting GLP-1 RAs may protect cognitive function.
For example, as previously reported, in the phase 2b ELAD clinical trial, adults with early-stage Alzheimer’s disease taking the GLP-1 RA liraglutide exhibited slower decline in memory and thinking and experienced less brain atrophy over 12 months compared with placebo.
Promising, but Preliminary
Reached for comment, Courtney Kloske, PhD, Alzheimer’s Association director of scientific engagement, noted that diabetes is a known risk factor for AD and managing diabetes with drugs such as semaglutide “could benefit brain health simply by managing diabetes.”
“However, we still need large clinical trials in representative populations to determine if semaglutide specifically lowers the risk of Alzheimer’s, so it is too early to recommend it for prevention,” Kloske said.
She noted that some research suggests that GLP-1 RAs “may help reduce inflammation and positively impact brain energy use. However, more research is needed to fully understand how these processes might contribute to preventing cognitive decline or Alzheimer’s,” Kloske cautioned.
The Alzheimer’s Association’s “Part the Cloud” initiative has invested more than $68 million to advance 65 clinical trials targeting a variety of compounds, including repurposed drugs that may address known and potential new aspects of the disease, Kloske said.
The study was supported by grants from the National Institute on Aging and the National Center for Advancing Translational Sciences. Xu and Kloske have no relevant conflicts.
A version of this article appeared on Medscape.com.
Adults with type 2 diabetes who were prescribed the GLP-1 RA semaglutide had a significantly lower risk for Alzheimer’s disease compared with their peers who were prescribed any of seven other antidiabetic medications, including other types of GLP-1 receptor–targeting medications.
“These findings support further clinical trials to assess semaglutide’s potential in delaying or preventing Alzheimer’s disease,” wrote the investigators, led by Rong Xu, PhD, with Case Western Reserve School of Medicine, Cleveland, Ohio.
The study was published online on October 24 in Alzheimer’s & Dementia.
Real-World Data
Semaglutide has shown neuroprotective effects in animal models of neurodegenerative diseases, including Alzheimer’s disease and Parkinson’s disease. In animal models of Alzheimer’s disease, the drug reduced beta-amyloid deposition and improved spatial learning and memory, as well as glucose metabolism in the brain.
In a real-world analysis, Xu and colleagues used electronic health record data to identify 17,104 new users of semaglutide and 1,077,657 new users of seven other antidiabetic medications, including other GLP-1 RAs, insulin, metformin, dipeptidyl peptidase 4 inhibitors, sodium-glucose cotransporter 2 inhibitors, sulfonylurea, and thiazolidinedione.
Over 3 years, treatment with semaglutide was associated with significantly reduced risk of developing Alzheimer’s disease, most strongly compared with insulin (hazard ratio [HR], 0.33) and most weakly compared with other GLP-1 RAs (HR, 0.59).
Compared with the other medications, semaglutide was associated with a 40%-70% reduced risk for first-time diagnosis of Alzheimer’s disease in patients with type 2 diabetes, with similar reductions seen across obesity status and gender and age groups, the authors reported.
The findings align with recent evidence suggesting GLP-1 RAs may protect cognitive function.
For example, as previously reported, in the phase 2b ELAD clinical trial, adults with early-stage Alzheimer’s disease taking the GLP-1 RA liraglutide exhibited slower decline in memory and thinking and experienced less brain atrophy over 12 months compared with placebo.
Promising, but Preliminary
Reached for comment, Courtney Kloske, PhD, Alzheimer’s Association director of scientific engagement, noted that diabetes is a known risk factor for AD and managing diabetes with drugs such as semaglutide “could benefit brain health simply by managing diabetes.”
“However, we still need large clinical trials in representative populations to determine if semaglutide specifically lowers the risk of Alzheimer’s, so it is too early to recommend it for prevention,” Kloske said.
She noted that some research suggests that GLP-1 RAs “may help reduce inflammation and positively impact brain energy use. However, more research is needed to fully understand how these processes might contribute to preventing cognitive decline or Alzheimer’s,” Kloske cautioned.
The Alzheimer’s Association’s “Part the Cloud” initiative has invested more than $68 million to advance 65 clinical trials targeting a variety of compounds, including repurposed drugs that may address known and potential new aspects of the disease, Kloske said.
The study was supported by grants from the National Institute on Aging and the National Center for Advancing Translational Sciences. Xu and Kloske have no relevant conflicts.
A version of this article appeared on Medscape.com.
FROM ALZHEIMER’S & DEMENTIA
How Old Are You? Stand on One Leg and I’ll Tell You
This transcript has been edited for clarity.
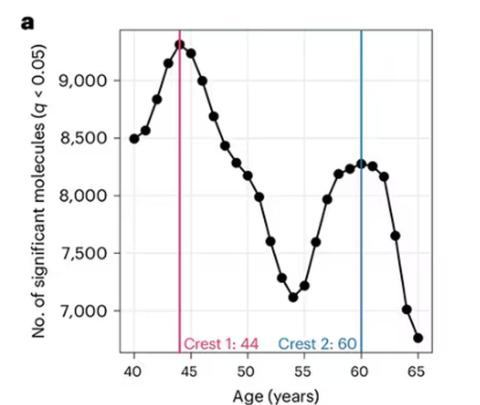
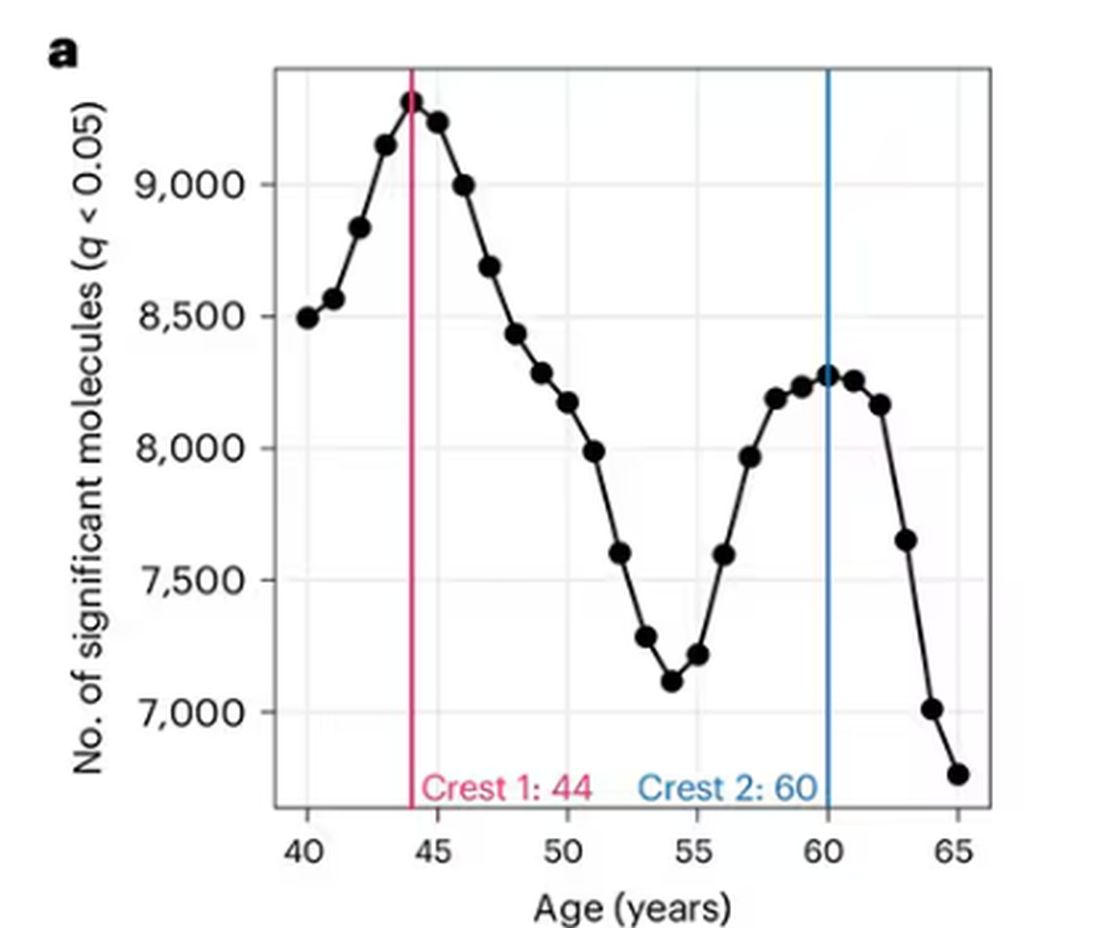
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
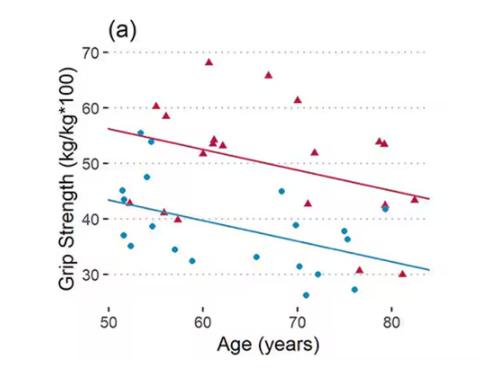
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
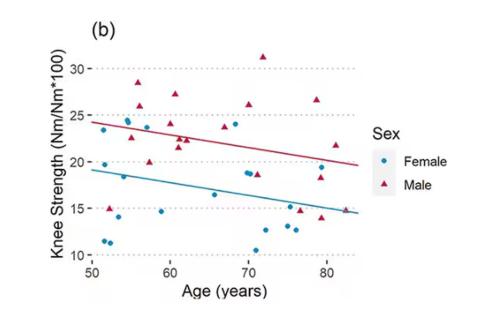
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Is CGM the New CBT?
Lauren is a 45-year-old corporate lawyer who managed to excel in every aspect of her life, including parenting her three children while working full-time as a corporate lawyer. A math major at Harvard, she loves data.
Suffice it to say, given that I was treating her for a thyroid condition rather than diabetes, I was a little surprised when she requested I prescribe her a FreeStyle Libre (Abbott) monitor. She explained she was struggling to lose 10 pounds, and she thought continuous glucose monitoring (CGM) would help her determine which foods were impeding her weight loss journey.
While I didn’t see much downside to acquiescing, I felt she had probably been spending too much time on Reddit. What information could CGM give someone without diabetes that couldn’t be gleaned from a food label? Nevertheless, Lauren filled the prescription and began her foray into this relatively uncharted world. When she returned for a follow-up visit several months later, I was shocked to see that she had lost her intended weight. With my tail between my legs, I decided to review the theories and science behind the use of CGM in patients without insulin resistance.
Although it’s not rocket science, CGM can help patients through a “carrot and stick” approach to dieting. Lean proteins, nonstarchy vegetables, and monounsaturated fats such as nuts and avocado all support weight loss and tend to keep blood glucose levels stable. In contrast, foods known to cause weight gain (eg, sugary foods, refined starches, and processed foods) cause sugar spikes in real time. Similarly, large portion sizes are more likely to result in sugar spikes, and pairing proteins with carbohydrates minimizes blood glucose excursions.
Though all of this is basic common sense, . And because blood glucose is influenced by myriad factors including stress, genetics and metabolism, CGM can also potentially help create personal guidance for food choices.
In addition, CGM can reveal the effect of poor sleep and stress on blood glucose levels, thereby encouraging healthier lifestyle choices. The data collected also may provide information on how different modalities of physical activity affect blood glucose levels. A recent study compared the effect of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postmeal blood glucose in overweight individuals without diabetes. CGM revealed that HIIT is more advantageous for preventing postmeal spikes.
Although CGM appears to be a sophisticated form of cognitive-behavioral therapy, I do worry that the incessant stream of information can lead to worsening anxiety, obsessive compulsive behaviors, or restrictive eating tendencies. Still, thanks to Lauren, I now believe that real-time CGM may lead to behavior modification in food selection and physical activity.
Dr. Messer, Clinical Assistant Professor, Mount Sinai School of Medicine; Associate Professor, Hofstra School of Medicine, New York, NY, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Lauren is a 45-year-old corporate lawyer who managed to excel in every aspect of her life, including parenting her three children while working full-time as a corporate lawyer. A math major at Harvard, she loves data.
Suffice it to say, given that I was treating her for a thyroid condition rather than diabetes, I was a little surprised when she requested I prescribe her a FreeStyle Libre (Abbott) monitor. She explained she was struggling to lose 10 pounds, and she thought continuous glucose monitoring (CGM) would help her determine which foods were impeding her weight loss journey.
While I didn’t see much downside to acquiescing, I felt she had probably been spending too much time on Reddit. What information could CGM give someone without diabetes that couldn’t be gleaned from a food label? Nevertheless, Lauren filled the prescription and began her foray into this relatively uncharted world. When she returned for a follow-up visit several months later, I was shocked to see that she had lost her intended weight. With my tail between my legs, I decided to review the theories and science behind the use of CGM in patients without insulin resistance.
Although it’s not rocket science, CGM can help patients through a “carrot and stick” approach to dieting. Lean proteins, nonstarchy vegetables, and monounsaturated fats such as nuts and avocado all support weight loss and tend to keep blood glucose levels stable. In contrast, foods known to cause weight gain (eg, sugary foods, refined starches, and processed foods) cause sugar spikes in real time. Similarly, large portion sizes are more likely to result in sugar spikes, and pairing proteins with carbohydrates minimizes blood glucose excursions.
Though all of this is basic common sense, . And because blood glucose is influenced by myriad factors including stress, genetics and metabolism, CGM can also potentially help create personal guidance for food choices.
In addition, CGM can reveal the effect of poor sleep and stress on blood glucose levels, thereby encouraging healthier lifestyle choices. The data collected also may provide information on how different modalities of physical activity affect blood glucose levels. A recent study compared the effect of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postmeal blood glucose in overweight individuals without diabetes. CGM revealed that HIIT is more advantageous for preventing postmeal spikes.
Although CGM appears to be a sophisticated form of cognitive-behavioral therapy, I do worry that the incessant stream of information can lead to worsening anxiety, obsessive compulsive behaviors, or restrictive eating tendencies. Still, thanks to Lauren, I now believe that real-time CGM may lead to behavior modification in food selection and physical activity.
Dr. Messer, Clinical Assistant Professor, Mount Sinai School of Medicine; Associate Professor, Hofstra School of Medicine, New York, NY, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Lauren is a 45-year-old corporate lawyer who managed to excel in every aspect of her life, including parenting her three children while working full-time as a corporate lawyer. A math major at Harvard, she loves data.
Suffice it to say, given that I was treating her for a thyroid condition rather than diabetes, I was a little surprised when she requested I prescribe her a FreeStyle Libre (Abbott) monitor. She explained she was struggling to lose 10 pounds, and she thought continuous glucose monitoring (CGM) would help her determine which foods were impeding her weight loss journey.
While I didn’t see much downside to acquiescing, I felt she had probably been spending too much time on Reddit. What information could CGM give someone without diabetes that couldn’t be gleaned from a food label? Nevertheless, Lauren filled the prescription and began her foray into this relatively uncharted world. When she returned for a follow-up visit several months later, I was shocked to see that she had lost her intended weight. With my tail between my legs, I decided to review the theories and science behind the use of CGM in patients without insulin resistance.
Although it’s not rocket science, CGM can help patients through a “carrot and stick” approach to dieting. Lean proteins, nonstarchy vegetables, and monounsaturated fats such as nuts and avocado all support weight loss and tend to keep blood glucose levels stable. In contrast, foods known to cause weight gain (eg, sugary foods, refined starches, and processed foods) cause sugar spikes in real time. Similarly, large portion sizes are more likely to result in sugar spikes, and pairing proteins with carbohydrates minimizes blood glucose excursions.
Though all of this is basic common sense, . And because blood glucose is influenced by myriad factors including stress, genetics and metabolism, CGM can also potentially help create personal guidance for food choices.
In addition, CGM can reveal the effect of poor sleep and stress on blood glucose levels, thereby encouraging healthier lifestyle choices. The data collected also may provide information on how different modalities of physical activity affect blood glucose levels. A recent study compared the effect of high-intensity interval training (HIIT) and continuous moderate-intensity exercise on postmeal blood glucose in overweight individuals without diabetes. CGM revealed that HIIT is more advantageous for preventing postmeal spikes.
Although CGM appears to be a sophisticated form of cognitive-behavioral therapy, I do worry that the incessant stream of information can lead to worsening anxiety, obsessive compulsive behaviors, or restrictive eating tendencies. Still, thanks to Lauren, I now believe that real-time CGM may lead to behavior modification in food selection and physical activity.
Dr. Messer, Clinical Assistant Professor, Mount Sinai School of Medicine; Associate Professor, Hofstra School of Medicine, New York, NY, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
How Much Does Long COVID Cost Society? New Data Shed Light
Long COVID, a major public health crisis, is also becoming a significant economic crisis. A new study in Nature reports that the global annual economic impact of long COVID has hit $1 trillion — or about 1% of the global economy.
Long COVID is estimated to affect 6%-7% of adults. Those afflicted are often unable to work for extended periods, and some simply stop working altogether.
Besides damaging individual lives, long COVID is having wide-ranging impacts on health systems and economies worldwide, as those who suffer from it have large absences from work, leading to lower productivity. Even those who return to work after weeks, months, or even up to a year out of work may come back with worse productivity and some functional impairment — as a few of the condition’s common symptoms include fatigue and brain fog.
Experts say more is needed not only in terms of scientific research into new treatments for long COVID but also from a public policy perspective.
Long COVID’s impact on the labor force is already having ripple effects throughout the economy of the United States and other countries. Earlier this year, the US Government Accountability Office stated long COVID potentially affects up to 23 million Americans, with as many as a million people out of work. The healthcare industry is particularly hard hit.
The latest survey from the National Center for Health Statistics estimated 17.3%-18.6% of adults have experienced long COVID. This isn’t the same as those who have it now, only a broad indicator of people who’ve ever experienced symptoms.
Public health experts, economists, researchers, and physicians say they are only beginning to focus on ways to reduce long COVID’s impact.
They suggest a range of potential solutions to address the public health crisis and the economic impacts — including implementing a more thorough surveillance system to track long COVID cases, building better ventilation systems in hospitals and buildings to reduce the spread of the virus, increasing vaccination efforts as new viral strains continuously emerge, and more funding for long COVID research to better quantify and qualify the disease’s impact.
Shaky Statistics, Inconsistent Surveillance
David Smith, MD, an infectious disease specialist at the University of California, San Diego, said more needs to be done to survey, quantify, and qualify the impacts of long COVID on the economy before practical solutions can be identified.
“Our surveillance system sucks,” Smith said. “I can see how many people test positive for COVID, but how many of those people have long COVID?”
Long COVID also doesn’t have a true definition or standard diagnosis, which complicates surveillance efforts. It includes a spectrum of symptoms such as shortness of breath, chronic fatigue, and brain fog that linger for 2-3 months after an acute infection. But there’s no “concrete case definition,” Smith said. “And not everybody’s long COVID is exactly the same as everybody else’s.”
As a result, epidemiologists can’t effectively characterize the disease, and health economists can’t measure its exact economic impact.
Few countries have established comprehensive surveillance systems to estimate the burden of long COVID at the population level.
The United States currently tracks new cases by measuring wastewater levels, which isn’t as comprehensive as the tracking that was done during the pandemic. But positive wastewater samples can’t tell us who is infected in an area, nor can it distinguish whether a visitor/tourist or resident is mostly contributing to the wastewater analysis — an important distinction in public health studies.
Wastewater surveillance is an excellent complement to traditional disease surveillance with advantages and disadvantages, but it shouldn’t be the sole way to measure disease.
What Research Best Informs the Debate?
A study by Economist Impact — a think tank that partners with corporations, foundations, NGOs, and governments to help drive policy — estimated between a 0.5% and 2.3% gross domestic product (GDP) loss across eight separate countries in 2024. The study included the United Kingdom and United States.
Meanwhile, Australian researchers recently detailed how long COVID-related reductions in labor supply affected its productivity and GDP from 2022 to 2024. The study found that long COVID could be costing the Australian economy about 0.5% of its GDP, which researchers deemed a conservative estimate.
Public health researchers in New Zealand used the estimate of GDP loss in Australia to measure their own potential losses and advocated for strengthening occupational support across all sectors to protect health.
But these studies can’t quite compare with what would have to be done for the United States economy.
“New Zealand is small ... and has an excellent public health system with good delivery of vaccines and treatments…so how do we compare that to us?” Smith said. “They do better in all of their public health metrics than we do.”
Measuring the Economic Impact
Gopi Shah Goda, PhD, a health economist and senior fellow in economic studies at the Brookings Institution, co-authored a 2023 study that found COVID-19 reduced the US labor force by about 500,000 people.
Plus, workers who missed a full week due to COVID-19 absences became 7% less likely to return to the labor force a year later compared with workers who didn’t miss work for health reasons. That amounts to 0.2% of the labor force, a significant number.
“Even a small percent of the labor force is a big number…it’s like an extra year of populating aging,” Goda said.
“Some people who get long COVID might have dropped out of the labor force anyway,” Goda added.
The study concluded that average individual earnings lost from long COVID were $9000, and the total lost labor supply amounted to $62 billion annually — about half the estimated productivity losses from cancer or diabetes.
But research into long COVID research continues to be underfunded compared with other health conditions, experts noted.
Cancer and diabetes both receive billions of research dollars annually from the National Institutes of Health. Long COVID research gets only a few million, according to Goda.
Informing Public Health Policy
When it comes to caring for patients with long COVID, the big issue facing every nation’s public policy leaders is how best to allocate limited health resources.
“Public health never has enough money ... Do they buy more vaccines? Do they do educational programs? Who do they target the most?” Smith said.
Though Smith thinks the best preventative measure is increased vaccination, vaccination rates remain low in the United States.
“Unfortunately, as last fall demonstrated, there’s a lot of vaccine indifference and skepticism,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University School of Medicine, Nashville, Tennessee.
Over the past year, only 14% of eligible children and 22% of adults received the 2023-2024 COVID vaccine boosters.
Schaffner said public health experts wrestle with ways to assure the public vaccines are safe and effective.
“They’re trying to provide a level of comfort that [getting vaccinated] is the socially appropriate thing to do,” which remains a significant challenge, Schaffner said.
Some people don’t have access to vaccines and comprehensive medical services because they lack insurance, Medicaid, and Medicare. And the United States still doesn’t distribute vaccines as well as other countries, Schaffner added.
“In other countries, every doctor’s office gets vaccines for free ... here, we have a large commercial enterprise that basically runs it…there are still populations who aren’t reached,” he said.
Long COVID clinics that have opened around the country have offered help to some patients with long COVID. A year and a half ago, Yale University, New Haven, Connecticut, established its Long COVID Care Center. Stanford University, Stanford, California, opened its Long COVID Clinic back in 2021. Vanderbilt University now has its own, as well — the Adult Post-COVID Clinic.
But these clinics have faced declining federal resources, forcing some to close and others to face questions about whether they will be able to continue to operate without more aggressive federal direction and policy planning.
“With some central direction, we could provide better supportive care for the many patients with long COVID out there,” Schaffner said.
For countries with universal healthcare systems, services such as occupational health, extended sick leave, extended time for disability, and workers’ compensation benefits are readily available.
But in the United States, it’s often left to the physicians and their patients to figure out a plan.
“I think we could make physicians more aware of options for their patients…for example, regularly check eligibility for workers compensation,” Schaffner said.
A version of this article first appeared on Medscape.com.
Long COVID, a major public health crisis, is also becoming a significant economic crisis. A new study in Nature reports that the global annual economic impact of long COVID has hit $1 trillion — or about 1% of the global economy.
Long COVID is estimated to affect 6%-7% of adults. Those afflicted are often unable to work for extended periods, and some simply stop working altogether.
Besides damaging individual lives, long COVID is having wide-ranging impacts on health systems and economies worldwide, as those who suffer from it have large absences from work, leading to lower productivity. Even those who return to work after weeks, months, or even up to a year out of work may come back with worse productivity and some functional impairment — as a few of the condition’s common symptoms include fatigue and brain fog.
Experts say more is needed not only in terms of scientific research into new treatments for long COVID but also from a public policy perspective.
Long COVID’s impact on the labor force is already having ripple effects throughout the economy of the United States and other countries. Earlier this year, the US Government Accountability Office stated long COVID potentially affects up to 23 million Americans, with as many as a million people out of work. The healthcare industry is particularly hard hit.
The latest survey from the National Center for Health Statistics estimated 17.3%-18.6% of adults have experienced long COVID. This isn’t the same as those who have it now, only a broad indicator of people who’ve ever experienced symptoms.
Public health experts, economists, researchers, and physicians say they are only beginning to focus on ways to reduce long COVID’s impact.
They suggest a range of potential solutions to address the public health crisis and the economic impacts — including implementing a more thorough surveillance system to track long COVID cases, building better ventilation systems in hospitals and buildings to reduce the spread of the virus, increasing vaccination efforts as new viral strains continuously emerge, and more funding for long COVID research to better quantify and qualify the disease’s impact.
Shaky Statistics, Inconsistent Surveillance
David Smith, MD, an infectious disease specialist at the University of California, San Diego, said more needs to be done to survey, quantify, and qualify the impacts of long COVID on the economy before practical solutions can be identified.
“Our surveillance system sucks,” Smith said. “I can see how many people test positive for COVID, but how many of those people have long COVID?”
Long COVID also doesn’t have a true definition or standard diagnosis, which complicates surveillance efforts. It includes a spectrum of symptoms such as shortness of breath, chronic fatigue, and brain fog that linger for 2-3 months after an acute infection. But there’s no “concrete case definition,” Smith said. “And not everybody’s long COVID is exactly the same as everybody else’s.”
As a result, epidemiologists can’t effectively characterize the disease, and health economists can’t measure its exact economic impact.
Few countries have established comprehensive surveillance systems to estimate the burden of long COVID at the population level.
The United States currently tracks new cases by measuring wastewater levels, which isn’t as comprehensive as the tracking that was done during the pandemic. But positive wastewater samples can’t tell us who is infected in an area, nor can it distinguish whether a visitor/tourist or resident is mostly contributing to the wastewater analysis — an important distinction in public health studies.
Wastewater surveillance is an excellent complement to traditional disease surveillance with advantages and disadvantages, but it shouldn’t be the sole way to measure disease.
What Research Best Informs the Debate?
A study by Economist Impact — a think tank that partners with corporations, foundations, NGOs, and governments to help drive policy — estimated between a 0.5% and 2.3% gross domestic product (GDP) loss across eight separate countries in 2024. The study included the United Kingdom and United States.
Meanwhile, Australian researchers recently detailed how long COVID-related reductions in labor supply affected its productivity and GDP from 2022 to 2024. The study found that long COVID could be costing the Australian economy about 0.5% of its GDP, which researchers deemed a conservative estimate.
Public health researchers in New Zealand used the estimate of GDP loss in Australia to measure their own potential losses and advocated for strengthening occupational support across all sectors to protect health.
But these studies can’t quite compare with what would have to be done for the United States economy.
“New Zealand is small ... and has an excellent public health system with good delivery of vaccines and treatments…so how do we compare that to us?” Smith said. “They do better in all of their public health metrics than we do.”
Measuring the Economic Impact
Gopi Shah Goda, PhD, a health economist and senior fellow in economic studies at the Brookings Institution, co-authored a 2023 study that found COVID-19 reduced the US labor force by about 500,000 people.
Plus, workers who missed a full week due to COVID-19 absences became 7% less likely to return to the labor force a year later compared with workers who didn’t miss work for health reasons. That amounts to 0.2% of the labor force, a significant number.
“Even a small percent of the labor force is a big number…it’s like an extra year of populating aging,” Goda said.
“Some people who get long COVID might have dropped out of the labor force anyway,” Goda added.
The study concluded that average individual earnings lost from long COVID were $9000, and the total lost labor supply amounted to $62 billion annually — about half the estimated productivity losses from cancer or diabetes.
But research into long COVID research continues to be underfunded compared with other health conditions, experts noted.
Cancer and diabetes both receive billions of research dollars annually from the National Institutes of Health. Long COVID research gets only a few million, according to Goda.
Informing Public Health Policy
When it comes to caring for patients with long COVID, the big issue facing every nation’s public policy leaders is how best to allocate limited health resources.
“Public health never has enough money ... Do they buy more vaccines? Do they do educational programs? Who do they target the most?” Smith said.
Though Smith thinks the best preventative measure is increased vaccination, vaccination rates remain low in the United States.
“Unfortunately, as last fall demonstrated, there’s a lot of vaccine indifference and skepticism,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University School of Medicine, Nashville, Tennessee.
Over the past year, only 14% of eligible children and 22% of adults received the 2023-2024 COVID vaccine boosters.
Schaffner said public health experts wrestle with ways to assure the public vaccines are safe and effective.
“They’re trying to provide a level of comfort that [getting vaccinated] is the socially appropriate thing to do,” which remains a significant challenge, Schaffner said.
Some people don’t have access to vaccines and comprehensive medical services because they lack insurance, Medicaid, and Medicare. And the United States still doesn’t distribute vaccines as well as other countries, Schaffner added.
“In other countries, every doctor’s office gets vaccines for free ... here, we have a large commercial enterprise that basically runs it…there are still populations who aren’t reached,” he said.
Long COVID clinics that have opened around the country have offered help to some patients with long COVID. A year and a half ago, Yale University, New Haven, Connecticut, established its Long COVID Care Center. Stanford University, Stanford, California, opened its Long COVID Clinic back in 2021. Vanderbilt University now has its own, as well — the Adult Post-COVID Clinic.
But these clinics have faced declining federal resources, forcing some to close and others to face questions about whether they will be able to continue to operate without more aggressive federal direction and policy planning.
“With some central direction, we could provide better supportive care for the many patients with long COVID out there,” Schaffner said.
For countries with universal healthcare systems, services such as occupational health, extended sick leave, extended time for disability, and workers’ compensation benefits are readily available.
But in the United States, it’s often left to the physicians and their patients to figure out a plan.
“I think we could make physicians more aware of options for their patients…for example, regularly check eligibility for workers compensation,” Schaffner said.
A version of this article first appeared on Medscape.com.
Long COVID, a major public health crisis, is also becoming a significant economic crisis. A new study in Nature reports that the global annual economic impact of long COVID has hit $1 trillion — or about 1% of the global economy.
Long COVID is estimated to affect 6%-7% of adults. Those afflicted are often unable to work for extended periods, and some simply stop working altogether.
Besides damaging individual lives, long COVID is having wide-ranging impacts on health systems and economies worldwide, as those who suffer from it have large absences from work, leading to lower productivity. Even those who return to work after weeks, months, or even up to a year out of work may come back with worse productivity and some functional impairment — as a few of the condition’s common symptoms include fatigue and brain fog.
Experts say more is needed not only in terms of scientific research into new treatments for long COVID but also from a public policy perspective.
Long COVID’s impact on the labor force is already having ripple effects throughout the economy of the United States and other countries. Earlier this year, the US Government Accountability Office stated long COVID potentially affects up to 23 million Americans, with as many as a million people out of work. The healthcare industry is particularly hard hit.
The latest survey from the National Center for Health Statistics estimated 17.3%-18.6% of adults have experienced long COVID. This isn’t the same as those who have it now, only a broad indicator of people who’ve ever experienced symptoms.
Public health experts, economists, researchers, and physicians say they are only beginning to focus on ways to reduce long COVID’s impact.
They suggest a range of potential solutions to address the public health crisis and the economic impacts — including implementing a more thorough surveillance system to track long COVID cases, building better ventilation systems in hospitals and buildings to reduce the spread of the virus, increasing vaccination efforts as new viral strains continuously emerge, and more funding for long COVID research to better quantify and qualify the disease’s impact.
Shaky Statistics, Inconsistent Surveillance
David Smith, MD, an infectious disease specialist at the University of California, San Diego, said more needs to be done to survey, quantify, and qualify the impacts of long COVID on the economy before practical solutions can be identified.
“Our surveillance system sucks,” Smith said. “I can see how many people test positive for COVID, but how many of those people have long COVID?”
Long COVID also doesn’t have a true definition or standard diagnosis, which complicates surveillance efforts. It includes a spectrum of symptoms such as shortness of breath, chronic fatigue, and brain fog that linger for 2-3 months after an acute infection. But there’s no “concrete case definition,” Smith said. “And not everybody’s long COVID is exactly the same as everybody else’s.”
As a result, epidemiologists can’t effectively characterize the disease, and health economists can’t measure its exact economic impact.
Few countries have established comprehensive surveillance systems to estimate the burden of long COVID at the population level.
The United States currently tracks new cases by measuring wastewater levels, which isn’t as comprehensive as the tracking that was done during the pandemic. But positive wastewater samples can’t tell us who is infected in an area, nor can it distinguish whether a visitor/tourist or resident is mostly contributing to the wastewater analysis — an important distinction in public health studies.
Wastewater surveillance is an excellent complement to traditional disease surveillance with advantages and disadvantages, but it shouldn’t be the sole way to measure disease.
What Research Best Informs the Debate?
A study by Economist Impact — a think tank that partners with corporations, foundations, NGOs, and governments to help drive policy — estimated between a 0.5% and 2.3% gross domestic product (GDP) loss across eight separate countries in 2024. The study included the United Kingdom and United States.
Meanwhile, Australian researchers recently detailed how long COVID-related reductions in labor supply affected its productivity and GDP from 2022 to 2024. The study found that long COVID could be costing the Australian economy about 0.5% of its GDP, which researchers deemed a conservative estimate.
Public health researchers in New Zealand used the estimate of GDP loss in Australia to measure their own potential losses and advocated for strengthening occupational support across all sectors to protect health.
But these studies can’t quite compare with what would have to be done for the United States economy.
“New Zealand is small ... and has an excellent public health system with good delivery of vaccines and treatments…so how do we compare that to us?” Smith said. “They do better in all of their public health metrics than we do.”
Measuring the Economic Impact
Gopi Shah Goda, PhD, a health economist and senior fellow in economic studies at the Brookings Institution, co-authored a 2023 study that found COVID-19 reduced the US labor force by about 500,000 people.
Plus, workers who missed a full week due to COVID-19 absences became 7% less likely to return to the labor force a year later compared with workers who didn’t miss work for health reasons. That amounts to 0.2% of the labor force, a significant number.
“Even a small percent of the labor force is a big number…it’s like an extra year of populating aging,” Goda said.
“Some people who get long COVID might have dropped out of the labor force anyway,” Goda added.
The study concluded that average individual earnings lost from long COVID were $9000, and the total lost labor supply amounted to $62 billion annually — about half the estimated productivity losses from cancer or diabetes.
But research into long COVID research continues to be underfunded compared with other health conditions, experts noted.
Cancer and diabetes both receive billions of research dollars annually from the National Institutes of Health. Long COVID research gets only a few million, according to Goda.
Informing Public Health Policy
When it comes to caring for patients with long COVID, the big issue facing every nation’s public policy leaders is how best to allocate limited health resources.
“Public health never has enough money ... Do they buy more vaccines? Do they do educational programs? Who do they target the most?” Smith said.
Though Smith thinks the best preventative measure is increased vaccination, vaccination rates remain low in the United States.
“Unfortunately, as last fall demonstrated, there’s a lot of vaccine indifference and skepticism,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University School of Medicine, Nashville, Tennessee.
Over the past year, only 14% of eligible children and 22% of adults received the 2023-2024 COVID vaccine boosters.
Schaffner said public health experts wrestle with ways to assure the public vaccines are safe and effective.
“They’re trying to provide a level of comfort that [getting vaccinated] is the socially appropriate thing to do,” which remains a significant challenge, Schaffner said.
Some people don’t have access to vaccines and comprehensive medical services because they lack insurance, Medicaid, and Medicare. And the United States still doesn’t distribute vaccines as well as other countries, Schaffner added.
“In other countries, every doctor’s office gets vaccines for free ... here, we have a large commercial enterprise that basically runs it…there are still populations who aren’t reached,” he said.
Long COVID clinics that have opened around the country have offered help to some patients with long COVID. A year and a half ago, Yale University, New Haven, Connecticut, established its Long COVID Care Center. Stanford University, Stanford, California, opened its Long COVID Clinic back in 2021. Vanderbilt University now has its own, as well — the Adult Post-COVID Clinic.
But these clinics have faced declining federal resources, forcing some to close and others to face questions about whether they will be able to continue to operate without more aggressive federal direction and policy planning.
“With some central direction, we could provide better supportive care for the many patients with long COVID out there,” Schaffner said.
For countries with universal healthcare systems, services such as occupational health, extended sick leave, extended time for disability, and workers’ compensation benefits are readily available.
But in the United States, it’s often left to the physicians and their patients to figure out a plan.
“I think we could make physicians more aware of options for their patients…for example, regularly check eligibility for workers compensation,” Schaffner said.
A version of this article first appeared on Medscape.com.
FROM NATURE
Dry Eye Linked to Increased Risk for Mental Health Disorders
TOPLINE:
Patients with dry eye disease are more than three times as likely to have mental health conditions, such as depression and anxiety, as those without the condition.
METHODOLOGY:
- Researchers used a database from the National Institutes of Health to investigate the association between dry eye disease and mental health disorders in a large and diverse nationwide population of American adults.
- They identified 18,257 patients (mean age, 64.9 years; 67% women) with dry eye disease who were propensity score–matched with 54,765 participants without the condition.
- The cases of dry eye disease were identified using Systematized Nomenclature of Medicine codes for dry eyes, meibomian gland dysfunction, and tear film insufficiency.
- The outcome measures for mental health conditions were clinical diagnoses of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders.
TAKEAWAY:
- Patients with dry eye disease had more than triple the risk for mental health conditions than participants without the condition (adjusted odds ratio [aOR], 3.21; P < .001).
- Patients with dry eye disease had a higher risk for a depressive disorder (aOR, 3.47), anxiety-related disorder (aOR, 2.74), bipolar disorder (aOR, 2.23), and schizophrenia spectrum disorder (aOR, 2.48; P < .001 for all) than participants without the condition.
- The associations between dry eye disease and mental health conditions were significantly stronger among Black individuals than among White individuals, except for bipolar disorder.
- Dry eye disease was associated with two- to threefold higher odds of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders even in participants who never used medications for mental health (P < .001 for all).
IN PRACTICE:
“Greater efforts should be undertaken to screen patients with DED [dry eye disease] for mental health conditions, particularly in historically medically underserved populations,” the authors of the study wrote.
SOURCE:
This study was led by Aaron T. Zhao, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and was published online on October 15, 2024, in the American Journal of Ophthalmology.
LIMITATIONS:
This study relied on electronic health record data, which may have led to the inclusion of participants with undiagnosed dry eye disease as control participants. Moreover, the study did not evaluate the severity of dry eye disease or the severity and duration of mental health conditions, which may have affected the results. The database analyzed in this study may not have fully captured the complete demographic profile of the nationwide population, which may have affected the generalizability of the findings.
DISCLOSURES:
This study was supported by funding from the National Institutes of Health and Research to Prevent Blindness. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Patients with dry eye disease are more than three times as likely to have mental health conditions, such as depression and anxiety, as those without the condition.
METHODOLOGY:
- Researchers used a database from the National Institutes of Health to investigate the association between dry eye disease and mental health disorders in a large and diverse nationwide population of American adults.
- They identified 18,257 patients (mean age, 64.9 years; 67% women) with dry eye disease who were propensity score–matched with 54,765 participants without the condition.
- The cases of dry eye disease were identified using Systematized Nomenclature of Medicine codes for dry eyes, meibomian gland dysfunction, and tear film insufficiency.
- The outcome measures for mental health conditions were clinical diagnoses of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders.
TAKEAWAY:
- Patients with dry eye disease had more than triple the risk for mental health conditions than participants without the condition (adjusted odds ratio [aOR], 3.21; P < .001).
- Patients with dry eye disease had a higher risk for a depressive disorder (aOR, 3.47), anxiety-related disorder (aOR, 2.74), bipolar disorder (aOR, 2.23), and schizophrenia spectrum disorder (aOR, 2.48; P < .001 for all) than participants without the condition.
- The associations between dry eye disease and mental health conditions were significantly stronger among Black individuals than among White individuals, except for bipolar disorder.
- Dry eye disease was associated with two- to threefold higher odds of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders even in participants who never used medications for mental health (P < .001 for all).
IN PRACTICE:
“Greater efforts should be undertaken to screen patients with DED [dry eye disease] for mental health conditions, particularly in historically medically underserved populations,” the authors of the study wrote.
SOURCE:
This study was led by Aaron T. Zhao, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and was published online on October 15, 2024, in the American Journal of Ophthalmology.
LIMITATIONS:
This study relied on electronic health record data, which may have led to the inclusion of participants with undiagnosed dry eye disease as control participants. Moreover, the study did not evaluate the severity of dry eye disease or the severity and duration of mental health conditions, which may have affected the results. The database analyzed in this study may not have fully captured the complete demographic profile of the nationwide population, which may have affected the generalizability of the findings.
DISCLOSURES:
This study was supported by funding from the National Institutes of Health and Research to Prevent Blindness. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Patients with dry eye disease are more than three times as likely to have mental health conditions, such as depression and anxiety, as those without the condition.
METHODOLOGY:
- Researchers used a database from the National Institutes of Health to investigate the association between dry eye disease and mental health disorders in a large and diverse nationwide population of American adults.
- They identified 18,257 patients (mean age, 64.9 years; 67% women) with dry eye disease who were propensity score–matched with 54,765 participants without the condition.
- The cases of dry eye disease were identified using Systematized Nomenclature of Medicine codes for dry eyes, meibomian gland dysfunction, and tear film insufficiency.
- The outcome measures for mental health conditions were clinical diagnoses of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders.
TAKEAWAY:
- Patients with dry eye disease had more than triple the risk for mental health conditions than participants without the condition (adjusted odds ratio [aOR], 3.21; P < .001).
- Patients with dry eye disease had a higher risk for a depressive disorder (aOR, 3.47), anxiety-related disorder (aOR, 2.74), bipolar disorder (aOR, 2.23), and schizophrenia spectrum disorder (aOR, 2.48; P < .001 for all) than participants without the condition.
- The associations between dry eye disease and mental health conditions were significantly stronger among Black individuals than among White individuals, except for bipolar disorder.
- Dry eye disease was associated with two- to threefold higher odds of depressive disorders, anxiety-related disorders, bipolar disorder, and schizophrenia spectrum disorders even in participants who never used medications for mental health (P < .001 for all).
IN PRACTICE:
“Greater efforts should be undertaken to screen patients with DED [dry eye disease] for mental health conditions, particularly in historically medically underserved populations,” the authors of the study wrote.
SOURCE:
This study was led by Aaron T. Zhao, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and was published online on October 15, 2024, in the American Journal of Ophthalmology.
LIMITATIONS:
This study relied on electronic health record data, which may have led to the inclusion of participants with undiagnosed dry eye disease as control participants. Moreover, the study did not evaluate the severity of dry eye disease or the severity and duration of mental health conditions, which may have affected the results. The database analyzed in this study may not have fully captured the complete demographic profile of the nationwide population, which may have affected the generalizability of the findings.
DISCLOSURES:
This study was supported by funding from the National Institutes of Health and Research to Prevent Blindness. The authors declared having no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Can Weight Loss Drugs Also Treat Addiction?
A new study provides more evidence that glucagon-like peptide 1 receptor agonists (GLP-1 RAs) used to treat diabetes and obesity could be repurposed for opioid use disorder (OUD) and alcohol use disorder (AUD).
Researchers found that patients with OUD or AUD who were taking semaglutide (Ozempic, Novo Nordisk) or similar medications for diabetes or weight-related conditions had a 40% lower rate of opioid overdose and a 50% lower rate of alcohol intoxication than their peers with OUD or AUD who were not taking these medications.
Their real-world study of more than 1 million adults with a history of OUD or AUD provide “foundational” estimates of the association between glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA prescriptions and opioid overdose/alcohol intoxication “and introduce the idea that GLP-1 RA and other related drugs should be investigated as a novel pharmacotherapy treatment option for individuals with OUD or AUD,” wrote the investigators, led by Fares Qeadan, PhD, Parkinson School of Health Sciences and Public Health, Loyola University Chicago, Maywood, Illinois.
The study was published online in the journal Addiction.
Protective Effect?
As previously reported by Medscape Medical News, earlier studies have pointed to a link between weight loss drugs and reduced overdose risk in people with OUD and decreased alcohol intake in people with AUD.
Until now, most studies on GLP-1 RAs and GIP agonists like tirzepatide (Mounjaro) to treat substance use disorders consisted of animal studies and small-scale clinical trials, investigators noted.
This new retrospective cohort study analyzed de-identified electronic health record data from the Oracle Health Real-World Data.
Participants, all aged 18 years or older, included 503,747 patients with a history of OUD, of whom 8103 had a GLP-1 RA or GIP prescription, and 817,309 patients with a history of AUD, of whom 5621 had a GLP-1 RA or GIP prescription.
Patients with OUD who were prescribed GLP-1 RAs had a 40% lower rate of opioid overdose than those without such prescriptions (adjusted incidence rate ratio [aIRR], 0.60; 95% CI, 0.43-0.83), the study team found.
In addition, patients with AUD and a GLP-1 RA prescription exhibited a 50% lower rate of alcohol intoxication (aIRR, 0.50; 95% CI, 0.40-0.63).
The protective effect of GLP-1 RA on opioid overdose and alcohol intoxication was maintained across patients with comorbid conditions, such as type 2 diabetes and obesity.
“Future research should focus on prospective clinical trials to validate these findings, explore the underlying mechanisms, and determine the long-term efficacy and safety of GIP/GLP-1 RA medications in diverse populations,” Qeadan and colleagues concluded.
“Additionally, the study highlights the importance of interdisciplinary research in understanding the neurobiological links between metabolic disorders and problematic substance use, potentially leading to more effective treatment strategies within healthcare systems,” they added.
Questions Remain
In a statement from the UK nonprofit Science Media Centre, Matt Field, DPhil, professor of psychology, The University of Sheffield, in England, noted that the findings “add to those from other studies, particularly animal research, which suggest that this and similar drugs might one day be prescribed to help people with addiction.”
However, “a note of caution is that the outcomes are very extreme instances of substance intoxication,” added Field, who wasn’t involved in the study.
“Those outcomes are very different from the outcomes used when researchers test new treatments for addiction, in which case we might look at whether the treatment helps people to stop taking the substance altogether (complete abstinence), or if it helps people to reduce the amount of substance they consume, or how often they consume it. Those things could not be measured in this study,” he continued.
“This leaves open the possibility that while Ozempic may — for reasons currently unknown — prevent people from taking so much alcohol or heroin that they overdose and end up in hospital, it may not actually help them to reduce their substance use, or to abstain altogether,” Field said.
The study had no specific funding. The study authors and Field declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A new study provides more evidence that glucagon-like peptide 1 receptor agonists (GLP-1 RAs) used to treat diabetes and obesity could be repurposed for opioid use disorder (OUD) and alcohol use disorder (AUD).
Researchers found that patients with OUD or AUD who were taking semaglutide (Ozempic, Novo Nordisk) or similar medications for diabetes or weight-related conditions had a 40% lower rate of opioid overdose and a 50% lower rate of alcohol intoxication than their peers with OUD or AUD who were not taking these medications.
Their real-world study of more than 1 million adults with a history of OUD or AUD provide “foundational” estimates of the association between glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA prescriptions and opioid overdose/alcohol intoxication “and introduce the idea that GLP-1 RA and other related drugs should be investigated as a novel pharmacotherapy treatment option for individuals with OUD or AUD,” wrote the investigators, led by Fares Qeadan, PhD, Parkinson School of Health Sciences and Public Health, Loyola University Chicago, Maywood, Illinois.
The study was published online in the journal Addiction.
Protective Effect?
As previously reported by Medscape Medical News, earlier studies have pointed to a link between weight loss drugs and reduced overdose risk in people with OUD and decreased alcohol intake in people with AUD.
Until now, most studies on GLP-1 RAs and GIP agonists like tirzepatide (Mounjaro) to treat substance use disorders consisted of animal studies and small-scale clinical trials, investigators noted.
This new retrospective cohort study analyzed de-identified electronic health record data from the Oracle Health Real-World Data.
Participants, all aged 18 years or older, included 503,747 patients with a history of OUD, of whom 8103 had a GLP-1 RA or GIP prescription, and 817,309 patients with a history of AUD, of whom 5621 had a GLP-1 RA or GIP prescription.
Patients with OUD who were prescribed GLP-1 RAs had a 40% lower rate of opioid overdose than those without such prescriptions (adjusted incidence rate ratio [aIRR], 0.60; 95% CI, 0.43-0.83), the study team found.
In addition, patients with AUD and a GLP-1 RA prescription exhibited a 50% lower rate of alcohol intoxication (aIRR, 0.50; 95% CI, 0.40-0.63).
The protective effect of GLP-1 RA on opioid overdose and alcohol intoxication was maintained across patients with comorbid conditions, such as type 2 diabetes and obesity.
“Future research should focus on prospective clinical trials to validate these findings, explore the underlying mechanisms, and determine the long-term efficacy and safety of GIP/GLP-1 RA medications in diverse populations,” Qeadan and colleagues concluded.
“Additionally, the study highlights the importance of interdisciplinary research in understanding the neurobiological links between metabolic disorders and problematic substance use, potentially leading to more effective treatment strategies within healthcare systems,” they added.
Questions Remain
In a statement from the UK nonprofit Science Media Centre, Matt Field, DPhil, professor of psychology, The University of Sheffield, in England, noted that the findings “add to those from other studies, particularly animal research, which suggest that this and similar drugs might one day be prescribed to help people with addiction.”
However, “a note of caution is that the outcomes are very extreme instances of substance intoxication,” added Field, who wasn’t involved in the study.
“Those outcomes are very different from the outcomes used when researchers test new treatments for addiction, in which case we might look at whether the treatment helps people to stop taking the substance altogether (complete abstinence), or if it helps people to reduce the amount of substance they consume, or how often they consume it. Those things could not be measured in this study,” he continued.
“This leaves open the possibility that while Ozempic may — for reasons currently unknown — prevent people from taking so much alcohol or heroin that they overdose and end up in hospital, it may not actually help them to reduce their substance use, or to abstain altogether,” Field said.
The study had no specific funding. The study authors and Field declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
A new study provides more evidence that glucagon-like peptide 1 receptor agonists (GLP-1 RAs) used to treat diabetes and obesity could be repurposed for opioid use disorder (OUD) and alcohol use disorder (AUD).
Researchers found that patients with OUD or AUD who were taking semaglutide (Ozempic, Novo Nordisk) or similar medications for diabetes or weight-related conditions had a 40% lower rate of opioid overdose and a 50% lower rate of alcohol intoxication than their peers with OUD or AUD who were not taking these medications.
Their real-world study of more than 1 million adults with a history of OUD or AUD provide “foundational” estimates of the association between glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA prescriptions and opioid overdose/alcohol intoxication “and introduce the idea that GLP-1 RA and other related drugs should be investigated as a novel pharmacotherapy treatment option for individuals with OUD or AUD,” wrote the investigators, led by Fares Qeadan, PhD, Parkinson School of Health Sciences and Public Health, Loyola University Chicago, Maywood, Illinois.
The study was published online in the journal Addiction.
Protective Effect?
As previously reported by Medscape Medical News, earlier studies have pointed to a link between weight loss drugs and reduced overdose risk in people with OUD and decreased alcohol intake in people with AUD.
Until now, most studies on GLP-1 RAs and GIP agonists like tirzepatide (Mounjaro) to treat substance use disorders consisted of animal studies and small-scale clinical trials, investigators noted.
This new retrospective cohort study analyzed de-identified electronic health record data from the Oracle Health Real-World Data.
Participants, all aged 18 years or older, included 503,747 patients with a history of OUD, of whom 8103 had a GLP-1 RA or GIP prescription, and 817,309 patients with a history of AUD, of whom 5621 had a GLP-1 RA or GIP prescription.
Patients with OUD who were prescribed GLP-1 RAs had a 40% lower rate of opioid overdose than those without such prescriptions (adjusted incidence rate ratio [aIRR], 0.60; 95% CI, 0.43-0.83), the study team found.
In addition, patients with AUD and a GLP-1 RA prescription exhibited a 50% lower rate of alcohol intoxication (aIRR, 0.50; 95% CI, 0.40-0.63).
The protective effect of GLP-1 RA on opioid overdose and alcohol intoxication was maintained across patients with comorbid conditions, such as type 2 diabetes and obesity.
“Future research should focus on prospective clinical trials to validate these findings, explore the underlying mechanisms, and determine the long-term efficacy and safety of GIP/GLP-1 RA medications in diverse populations,” Qeadan and colleagues concluded.
“Additionally, the study highlights the importance of interdisciplinary research in understanding the neurobiological links between metabolic disorders and problematic substance use, potentially leading to more effective treatment strategies within healthcare systems,” they added.
Questions Remain
In a statement from the UK nonprofit Science Media Centre, Matt Field, DPhil, professor of psychology, The University of Sheffield, in England, noted that the findings “add to those from other studies, particularly animal research, which suggest that this and similar drugs might one day be prescribed to help people with addiction.”
However, “a note of caution is that the outcomes are very extreme instances of substance intoxication,” added Field, who wasn’t involved in the study.
“Those outcomes are very different from the outcomes used when researchers test new treatments for addiction, in which case we might look at whether the treatment helps people to stop taking the substance altogether (complete abstinence), or if it helps people to reduce the amount of substance they consume, or how often they consume it. Those things could not be measured in this study,” he continued.
“This leaves open the possibility that while Ozempic may — for reasons currently unknown — prevent people from taking so much alcohol or heroin that they overdose and end up in hospital, it may not actually help them to reduce their substance use, or to abstain altogether,” Field said.
The study had no specific funding. The study authors and Field declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM ADDICTION
A Single Jog Can Improve Glucose Metabolism in Young Adults
TOPLINE:
In healthy young adults, a single 30-minute bout of outdoor aerobic exercise significantly reduces fasting and 1-hour glucose levels during an oral glucose tolerance test (OGTT) the next day and improves insulin sensitivity.
METHODOLOGY:
- Recent studies have identified 1-hour post-load glucose concentration during an OGTT as a specific and early predictor of diabetes, and exercise has long been known for its metabolic benefits in people with and without diabetes.
- The researchers investigated the effect of a single bout of aerobic exercise on 1-hour post-load glucose levels during an OGTT in 32 young, healthy, normal-weight or marginally overweight individuals (mean age, 35 years; 14 women and 18 men) with a sedentary or moderately active lifestyle.
- The participants underwent an initial OGTT after at least 4 days of physical inactivity, followed by a second OGTT the day after a single 30-minute bout of aerobic exercise.
- The exercise session consisted of a light jog for 30 minutes, monitored using a metabolic holter to quantify energy expenditure and exercise intensity. The participants did not undertake any exercise outside the lab sessions.
- Blood glucose levels were measured, and insulin sensitivity and secretion were estimated using surrogate indices derived from OGTT glucose and insulin assays, including the Matsuda index, oral glucose insulin sensitivity (OGIS) index, and quantitative insulin sensitivity check index, as well as the homeostasis model assessment (HOMA) of insulin resistance and of beta-cell function (HOMA-B).
TAKEAWAY:
- Postexercise insulin levels also were significantly lower 1 hour after glucose load, decreasing from 57.4 IU/mL at baseline to 43.5 IU/mL the day after exercise (P = .01).
- Insulin sensitivity improved significantly after exercise, as indicated by increases in the Matsuda index (P = .02) and OGIS index (P = .04), along with a reduction in insulin resistance (P = .04).
- The study found a trend toward increased beta-cell function the day after an exercise bout, as indicated by a nonsignificant increase in HOMA-B from 144.7 at baseline to 167.1 after exercise.
IN PRACTICE:
“Improvement in 1-hour post-load plasma glucose following a single session of aerobic physical activity suggests that exercise could have a direct effect on T2D [type 2 diabetes] risk and cardiovascular risk,” the authors wrote.
SOURCE:
The study was led by Simona Moffa, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, and Gian Pio Sorice, Università Degli Studi di Bari “Aldo Moro,” Bari, Italy. It was published online in the Journal of Endocrinological Investigation.
LIMITATIONS:
The study had a limited sample size, which may affect the generalizability of the findings. C-peptide levels, which could have provided additional insights into insulin secretion, were not assessed in the study.
DISCLOSURES:
The study was supported by grants from Università Cattolica del Sacro Cuore. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
In healthy young adults, a single 30-minute bout of outdoor aerobic exercise significantly reduces fasting and 1-hour glucose levels during an oral glucose tolerance test (OGTT) the next day and improves insulin sensitivity.
METHODOLOGY:
- Recent studies have identified 1-hour post-load glucose concentration during an OGTT as a specific and early predictor of diabetes, and exercise has long been known for its metabolic benefits in people with and without diabetes.
- The researchers investigated the effect of a single bout of aerobic exercise on 1-hour post-load glucose levels during an OGTT in 32 young, healthy, normal-weight or marginally overweight individuals (mean age, 35 years; 14 women and 18 men) with a sedentary or moderately active lifestyle.
- The participants underwent an initial OGTT after at least 4 days of physical inactivity, followed by a second OGTT the day after a single 30-minute bout of aerobic exercise.
- The exercise session consisted of a light jog for 30 minutes, monitored using a metabolic holter to quantify energy expenditure and exercise intensity. The participants did not undertake any exercise outside the lab sessions.
- Blood glucose levels were measured, and insulin sensitivity and secretion were estimated using surrogate indices derived from OGTT glucose and insulin assays, including the Matsuda index, oral glucose insulin sensitivity (OGIS) index, and quantitative insulin sensitivity check index, as well as the homeostasis model assessment (HOMA) of insulin resistance and of beta-cell function (HOMA-B).
TAKEAWAY:
- Postexercise insulin levels also were significantly lower 1 hour after glucose load, decreasing from 57.4 IU/mL at baseline to 43.5 IU/mL the day after exercise (P = .01).
- Insulin sensitivity improved significantly after exercise, as indicated by increases in the Matsuda index (P = .02) and OGIS index (P = .04), along with a reduction in insulin resistance (P = .04).
- The study found a trend toward increased beta-cell function the day after an exercise bout, as indicated by a nonsignificant increase in HOMA-B from 144.7 at baseline to 167.1 after exercise.
IN PRACTICE:
“Improvement in 1-hour post-load plasma glucose following a single session of aerobic physical activity suggests that exercise could have a direct effect on T2D [type 2 diabetes] risk and cardiovascular risk,” the authors wrote.
SOURCE:
The study was led by Simona Moffa, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, and Gian Pio Sorice, Università Degli Studi di Bari “Aldo Moro,” Bari, Italy. It was published online in the Journal of Endocrinological Investigation.
LIMITATIONS:
The study had a limited sample size, which may affect the generalizability of the findings. C-peptide levels, which could have provided additional insights into insulin secretion, were not assessed in the study.
DISCLOSURES:
The study was supported by grants from Università Cattolica del Sacro Cuore. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
In healthy young adults, a single 30-minute bout of outdoor aerobic exercise significantly reduces fasting and 1-hour glucose levels during an oral glucose tolerance test (OGTT) the next day and improves insulin sensitivity.
METHODOLOGY:
- Recent studies have identified 1-hour post-load glucose concentration during an OGTT as a specific and early predictor of diabetes, and exercise has long been known for its metabolic benefits in people with and without diabetes.
- The researchers investigated the effect of a single bout of aerobic exercise on 1-hour post-load glucose levels during an OGTT in 32 young, healthy, normal-weight or marginally overweight individuals (mean age, 35 years; 14 women and 18 men) with a sedentary or moderately active lifestyle.
- The participants underwent an initial OGTT after at least 4 days of physical inactivity, followed by a second OGTT the day after a single 30-minute bout of aerobic exercise.
- The exercise session consisted of a light jog for 30 minutes, monitored using a metabolic holter to quantify energy expenditure and exercise intensity. The participants did not undertake any exercise outside the lab sessions.
- Blood glucose levels were measured, and insulin sensitivity and secretion were estimated using surrogate indices derived from OGTT glucose and insulin assays, including the Matsuda index, oral glucose insulin sensitivity (OGIS) index, and quantitative insulin sensitivity check index, as well as the homeostasis model assessment (HOMA) of insulin resistance and of beta-cell function (HOMA-B).
TAKEAWAY:
- Postexercise insulin levels also were significantly lower 1 hour after glucose load, decreasing from 57.4 IU/mL at baseline to 43.5 IU/mL the day after exercise (P = .01).
- Insulin sensitivity improved significantly after exercise, as indicated by increases in the Matsuda index (P = .02) and OGIS index (P = .04), along with a reduction in insulin resistance (P = .04).
- The study found a trend toward increased beta-cell function the day after an exercise bout, as indicated by a nonsignificant increase in HOMA-B from 144.7 at baseline to 167.1 after exercise.
IN PRACTICE:
“Improvement in 1-hour post-load plasma glucose following a single session of aerobic physical activity suggests that exercise could have a direct effect on T2D [type 2 diabetes] risk and cardiovascular risk,” the authors wrote.
SOURCE:
The study was led by Simona Moffa, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, and Gian Pio Sorice, Università Degli Studi di Bari “Aldo Moro,” Bari, Italy. It was published online in the Journal of Endocrinological Investigation.
LIMITATIONS:
The study had a limited sample size, which may affect the generalizability of the findings. C-peptide levels, which could have provided additional insights into insulin secretion, were not assessed in the study.
DISCLOSURES:
The study was supported by grants from Università Cattolica del Sacro Cuore. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
These Patients May Be Less Adherent to nAMD Treatment
TOPLINE:
BARCELONA, SPAIN — Patients who receive a diagnosis of neovascular age-related macular degeneration (nAMD) from their primary care clinician may be less likely to adhere to treatment than those who receive the diagnosis from a specialist who provides anti–vascular endothelial growth factor (anti-VEGF) therapy, according to global survey results presented at the European Society of Retina Specialists (EURETINA) 2024. Likewise, patients who self-pay for the medication or who have bilateral nAMD may be less adherent to therapy, researchers found.
METHODOLOGY:
- Researchers analyzed data from 4558 patients with nAMD who participated in the Barometer Global Survey, which involved 77 clinics in 24 countries, including Canada, Mexico, Brazil, Germany, and France.
- The survey included multiple-choice questions on personal characteristics, disease awareness, experiences with treatment, and logistical challenges with getting to appointments.
- An exploratory statistical analysis identified 19 variables that influenced patient adherence to anti-VEGF therapy.
- The researchers classified 670 patients who missed two or more appointments during a 12-month period as nonadherent.
TAKEAWAY:
- Patients with nAMD diagnosed by their family doctor or general practitioner had a threefold higher risk for nonadherence than those diagnosed by the physician treating their nAMD.
- Self-pay was associated with more than twice the odds of nonadherence compared with having insurance coverage (odds ratio [OR], 2.5).
- Compared with unilateral nAMD, bilateral nAMD was associated with higher odds of multiple missed appointments (OR, 1.7).
- Nonadherence increased with the number of anti-VEGF injections, which may show that “longer treatment durations could permit more opportunities for absenteeism,” the investigators noted.
IN PRACTICE:
“Identifying patient characteristics and challenges that may be associated with nonadherence allows clinicians to recognize patients at risk for nonadherence and provide further support before these patients begin to miss appointments,” the study authors wrote.
SOURCE:
This study was led by Laurent Kodjikian, MD, PhD, with Croix-Rousse University Hospital and the University of Lyon in France. The findings were presented in a poster at EURETINA 2024 (September 19-22).
LIMITATIONS:
The survey relied on participant responses using Likert scales and single-choice questions. Patients from the United States were not included in the study.
DISCLOSURES:
The survey and medical writing support for the study were funded by Bayer Consumer Care. Kodjikian and co-authors disclosed consulting work for Bayer and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
BARCELONA, SPAIN — Patients who receive a diagnosis of neovascular age-related macular degeneration (nAMD) from their primary care clinician may be less likely to adhere to treatment than those who receive the diagnosis from a specialist who provides anti–vascular endothelial growth factor (anti-VEGF) therapy, according to global survey results presented at the European Society of Retina Specialists (EURETINA) 2024. Likewise, patients who self-pay for the medication or who have bilateral nAMD may be less adherent to therapy, researchers found.
METHODOLOGY:
- Researchers analyzed data from 4558 patients with nAMD who participated in the Barometer Global Survey, which involved 77 clinics in 24 countries, including Canada, Mexico, Brazil, Germany, and France.
- The survey included multiple-choice questions on personal characteristics, disease awareness, experiences with treatment, and logistical challenges with getting to appointments.
- An exploratory statistical analysis identified 19 variables that influenced patient adherence to anti-VEGF therapy.
- The researchers classified 670 patients who missed two or more appointments during a 12-month period as nonadherent.
TAKEAWAY:
- Patients with nAMD diagnosed by their family doctor or general practitioner had a threefold higher risk for nonadherence than those diagnosed by the physician treating their nAMD.
- Self-pay was associated with more than twice the odds of nonadherence compared with having insurance coverage (odds ratio [OR], 2.5).
- Compared with unilateral nAMD, bilateral nAMD was associated with higher odds of multiple missed appointments (OR, 1.7).
- Nonadherence increased with the number of anti-VEGF injections, which may show that “longer treatment durations could permit more opportunities for absenteeism,” the investigators noted.
IN PRACTICE:
“Identifying patient characteristics and challenges that may be associated with nonadherence allows clinicians to recognize patients at risk for nonadherence and provide further support before these patients begin to miss appointments,” the study authors wrote.
SOURCE:
This study was led by Laurent Kodjikian, MD, PhD, with Croix-Rousse University Hospital and the University of Lyon in France. The findings were presented in a poster at EURETINA 2024 (September 19-22).
LIMITATIONS:
The survey relied on participant responses using Likert scales and single-choice questions. Patients from the United States were not included in the study.
DISCLOSURES:
The survey and medical writing support for the study were funded by Bayer Consumer Care. Kodjikian and co-authors disclosed consulting work for Bayer and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
BARCELONA, SPAIN — Patients who receive a diagnosis of neovascular age-related macular degeneration (nAMD) from their primary care clinician may be less likely to adhere to treatment than those who receive the diagnosis from a specialist who provides anti–vascular endothelial growth factor (anti-VEGF) therapy, according to global survey results presented at the European Society of Retina Specialists (EURETINA) 2024. Likewise, patients who self-pay for the medication or who have bilateral nAMD may be less adherent to therapy, researchers found.
METHODOLOGY:
- Researchers analyzed data from 4558 patients with nAMD who participated in the Barometer Global Survey, which involved 77 clinics in 24 countries, including Canada, Mexico, Brazil, Germany, and France.
- The survey included multiple-choice questions on personal characteristics, disease awareness, experiences with treatment, and logistical challenges with getting to appointments.
- An exploratory statistical analysis identified 19 variables that influenced patient adherence to anti-VEGF therapy.
- The researchers classified 670 patients who missed two or more appointments during a 12-month period as nonadherent.
TAKEAWAY:
- Patients with nAMD diagnosed by their family doctor or general practitioner had a threefold higher risk for nonadherence than those diagnosed by the physician treating their nAMD.
- Self-pay was associated with more than twice the odds of nonadherence compared with having insurance coverage (odds ratio [OR], 2.5).
- Compared with unilateral nAMD, bilateral nAMD was associated with higher odds of multiple missed appointments (OR, 1.7).
- Nonadherence increased with the number of anti-VEGF injections, which may show that “longer treatment durations could permit more opportunities for absenteeism,” the investigators noted.
IN PRACTICE:
“Identifying patient characteristics and challenges that may be associated with nonadherence allows clinicians to recognize patients at risk for nonadherence and provide further support before these patients begin to miss appointments,” the study authors wrote.
SOURCE:
This study was led by Laurent Kodjikian, MD, PhD, with Croix-Rousse University Hospital and the University of Lyon in France. The findings were presented in a poster at EURETINA 2024 (September 19-22).
LIMITATIONS:
The survey relied on participant responses using Likert scales and single-choice questions. Patients from the United States were not included in the study.
DISCLOSURES:
The survey and medical writing support for the study were funded by Bayer Consumer Care. Kodjikian and co-authors disclosed consulting work for Bayer and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Postoperative Chronic Pain: Experts Urge Better Recognition
Postoperative chronic pain (POCP) is common and is expected to become increasingly prevalent. This type of pain, however, which specifically arises following surgery, independent of any infection or surgical failure, remains poorly understood. Facilities dedicated to treating it are nearly nonexistent.
At the 2024 congress of the French Society of Anesthesia and Resuscitation, anesthesiologists specializing in pain management advocated for improved management of POCP. They put themselves forward as essential interlocutors and actors in this effort. The anesthesiologists also called for better recognition of postoperative pain by patients, general practitioners, and surgeons to enable early intervention and reduce the risk for chronicity.
Underrecognized, Poorly Managed
POCP is defined as persistent pain lasting more than 3 months after surgery, unrelated to preoperative pain, and not associated with surgical complications. It can manifest in various forms, but the most typical scenario involves a patient complaining of persistent pain that developed following a surgical procedure. Normal radiological and biologic assessments rule out infectious complications. The persistence of pain long after surgery contrasts with what is often considered a successful surgical outcome by the surgeon.
“Of the 10 million patients operated on each year in France, it is estimated that about 10% will develop POCP, equating to 1.2 million patients,” explained Cyril Quémeneur, a specialist in anesthesiology and pain management at Pitié-Salpêtrière Hospital in Paris, France.
Because of the increasing number of surgical interventions in recent years, POCP has become a major concern. “Currently, there are 275 facilities dedicated to chronic pain across the country, capable of accommodating between 300,000 and 400,000 patients. Given that knee replacement surgery — the incidence of which is rising sharply — results in postoperative pain for 20%-30% of operated patients, the question of managing this type of pain will become even more pressing in the future,” said Quémeneur.
Moreover, specialized facilities for transitional pain management are not widespread in France, unlike in Canada, which has been developing them for about a decade, he noted.
France’s pain treatment centers “are overwhelmed,” said Gilles Lebuffe, a specialist in anesthesiology and pain management at Lille University Hospital in Lille, France. “Thus, the time between when the patient is operated on and when we discuss chronic pain allows the painful condition to establish itself, leading to central sensitization at the neurological level.” Once established, this pain is difficult to treat. “The later a patient arrives at a pain center, the more challenging the situation is to manage,” said Lebuffe.
Risk Factors
It is therefore crucial to identify patients at higher risk for postoperative pain during the anesthesia consultation, thus allowing for monitoring during the postoperative period. These pains can be highly debilitating because of their intensity, chronicity, and impact on quality of life.
To target these patients, it is essential to understand which surgeries and patient types constitute risk factors, as well as the characteristics of the pain experienced.
While all surgeries can lead to POCP, certain procedures are more likely to result in chronic pain. They include breast surgery with mastectomy, thoracic and spinal surgery, amputations, and knee replacement surgery. Notably, surgical repair of inguinal hernias, considered routine surgery, is emblematic of the risk for POCP. Its incidence after this procedure is 10% or more in the literature.
In addition, POCP often has neuropathic characteristics. Patients frequently describe their pain using terms like “burning” or “electric shock.” These pains are often associated with strange sensations such as tingling, prickling, itching, or numbness. “This describes neuropathic pain, which increases the risk of chronicity,” said Lebuffe.
Preoperative Opioid Use
Another warning sign for healthcare professionals is that patients with chronic pain may have factors associated with vulnerability. Women, who have a higher incidence of chronic pain syndrome, are at greater risk of developing postoperative chronic pain than men.
It has also been shown that preoperative opioid use leads to higher postoperative pain intensities for several days. This is a factor to consider, even though opioid consumption rates in France are far lower than those in the United States, where as much as 35% of patients use opioids preoperatively, said Frédéric Aubrun, head of the Anesthesia and Intensive Care Department and a pain management specialist at the Hospices Civils de Lyon in Lyon, France. Finally, significant literature indicates that psychological fragility is a risk factor for more intense acute pain and for POCP. “Patients with chronic pain frequently have depressive symptoms and anxiety,” said Lebuffe.
Involving General Practitioners
Because one responsibility of general practitioners is to identify patients with abnormal postoperative pain trajectories, the anesthesiologists at the press conference advocated for greater patient awareness and increased involvement of general practitioners in this identification process.
“If there is an expected duration of postoperative pain at varying intensities, since it all depends on the patient’s journey (the number of reoperations, history of opioid use, etc.), it is necessary to make patients aware that it is not normal to suffer long after a surgical intervention,” said Aubrun. In addition, it is important to “connect with primary care” and mobilize general practitioners to “detect patients sliding toward opioid overconsumption” and refer them to the appropriate care structure, he said.
Although dedicated facilities for this type of pain — like transitional pain clinics in Canada or northern Europe — do not exist in France, some hospitals, like Lille University Hospital, have established “intermediate consultations targeting patients with specific pain or chronicity characteristics. In these consultations, patients are systematically reviewed 4-6 weeks after surgery by the surgeon, who has been trained to identify neuropathic pain,” said Lebuffe. When a patient with such pain is identified, he or she is referred to an intermediate consultation and seen by a fellow anesthesiologist. The advantage of this consultation is that it is linked to a chronic pain structure. Consequently, frequent exchanges occur with the pain specialists involved in this structure, thus allowing for immediate optimization of pain treatments. The goal is to halt the process of central sensitization.
“We strongly believe in this type of transitional structure, even though it requires significant human resources,” said Lebuffe. He also called for a “societal reflection” on this issue because patients with chronic pain represent a significant cost to society, in terms of medications and work stoppages. Moreover, patients who are forced to stop working see their lives disrupted.
Managing POCP
When POCP with neuropathic characteristics has been diagnosed, specific treatments and techniques for chronic pain can be prescribed earlier than they currently are. “Systemic drug treatments for neuropathic POCP rely on various therapeutic classes (opioids, antidepressants, antiepileptics), which are not without side effects for the patient,” said Violaine D’ans, an anesthesiologist and pain management specialist at Polyclinique du Parc in Caen, France. Hence, the idea is to prescribe a minimal dose while providing the patient with techniques available to anesthesiologists. “We have a good range of management options that we use in perioperative pain management, and we have a role to play in radio- or CT-guided perinerve infiltrations, with continuous peripheral nerve blocks and possibly later with electrostimulation to help restore movement and avoid kinesiophobia.”
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Postoperative chronic pain (POCP) is common and is expected to become increasingly prevalent. This type of pain, however, which specifically arises following surgery, independent of any infection or surgical failure, remains poorly understood. Facilities dedicated to treating it are nearly nonexistent.
At the 2024 congress of the French Society of Anesthesia and Resuscitation, anesthesiologists specializing in pain management advocated for improved management of POCP. They put themselves forward as essential interlocutors and actors in this effort. The anesthesiologists also called for better recognition of postoperative pain by patients, general practitioners, and surgeons to enable early intervention and reduce the risk for chronicity.
Underrecognized, Poorly Managed
POCP is defined as persistent pain lasting more than 3 months after surgery, unrelated to preoperative pain, and not associated with surgical complications. It can manifest in various forms, but the most typical scenario involves a patient complaining of persistent pain that developed following a surgical procedure. Normal radiological and biologic assessments rule out infectious complications. The persistence of pain long after surgery contrasts with what is often considered a successful surgical outcome by the surgeon.
“Of the 10 million patients operated on each year in France, it is estimated that about 10% will develop POCP, equating to 1.2 million patients,” explained Cyril Quémeneur, a specialist in anesthesiology and pain management at Pitié-Salpêtrière Hospital in Paris, France.
Because of the increasing number of surgical interventions in recent years, POCP has become a major concern. “Currently, there are 275 facilities dedicated to chronic pain across the country, capable of accommodating between 300,000 and 400,000 patients. Given that knee replacement surgery — the incidence of which is rising sharply — results in postoperative pain for 20%-30% of operated patients, the question of managing this type of pain will become even more pressing in the future,” said Quémeneur.
Moreover, specialized facilities for transitional pain management are not widespread in France, unlike in Canada, which has been developing them for about a decade, he noted.
France’s pain treatment centers “are overwhelmed,” said Gilles Lebuffe, a specialist in anesthesiology and pain management at Lille University Hospital in Lille, France. “Thus, the time between when the patient is operated on and when we discuss chronic pain allows the painful condition to establish itself, leading to central sensitization at the neurological level.” Once established, this pain is difficult to treat. “The later a patient arrives at a pain center, the more challenging the situation is to manage,” said Lebuffe.
Risk Factors
It is therefore crucial to identify patients at higher risk for postoperative pain during the anesthesia consultation, thus allowing for monitoring during the postoperative period. These pains can be highly debilitating because of their intensity, chronicity, and impact on quality of life.
To target these patients, it is essential to understand which surgeries and patient types constitute risk factors, as well as the characteristics of the pain experienced.
While all surgeries can lead to POCP, certain procedures are more likely to result in chronic pain. They include breast surgery with mastectomy, thoracic and spinal surgery, amputations, and knee replacement surgery. Notably, surgical repair of inguinal hernias, considered routine surgery, is emblematic of the risk for POCP. Its incidence after this procedure is 10% or more in the literature.
In addition, POCP often has neuropathic characteristics. Patients frequently describe their pain using terms like “burning” or “electric shock.” These pains are often associated with strange sensations such as tingling, prickling, itching, or numbness. “This describes neuropathic pain, which increases the risk of chronicity,” said Lebuffe.
Preoperative Opioid Use
Another warning sign for healthcare professionals is that patients with chronic pain may have factors associated with vulnerability. Women, who have a higher incidence of chronic pain syndrome, are at greater risk of developing postoperative chronic pain than men.
It has also been shown that preoperative opioid use leads to higher postoperative pain intensities for several days. This is a factor to consider, even though opioid consumption rates in France are far lower than those in the United States, where as much as 35% of patients use opioids preoperatively, said Frédéric Aubrun, head of the Anesthesia and Intensive Care Department and a pain management specialist at the Hospices Civils de Lyon in Lyon, France. Finally, significant literature indicates that psychological fragility is a risk factor for more intense acute pain and for POCP. “Patients with chronic pain frequently have depressive symptoms and anxiety,” said Lebuffe.
Involving General Practitioners
Because one responsibility of general practitioners is to identify patients with abnormal postoperative pain trajectories, the anesthesiologists at the press conference advocated for greater patient awareness and increased involvement of general practitioners in this identification process.
“If there is an expected duration of postoperative pain at varying intensities, since it all depends on the patient’s journey (the number of reoperations, history of opioid use, etc.), it is necessary to make patients aware that it is not normal to suffer long after a surgical intervention,” said Aubrun. In addition, it is important to “connect with primary care” and mobilize general practitioners to “detect patients sliding toward opioid overconsumption” and refer them to the appropriate care structure, he said.
Although dedicated facilities for this type of pain — like transitional pain clinics in Canada or northern Europe — do not exist in France, some hospitals, like Lille University Hospital, have established “intermediate consultations targeting patients with specific pain or chronicity characteristics. In these consultations, patients are systematically reviewed 4-6 weeks after surgery by the surgeon, who has been trained to identify neuropathic pain,” said Lebuffe. When a patient with such pain is identified, he or she is referred to an intermediate consultation and seen by a fellow anesthesiologist. The advantage of this consultation is that it is linked to a chronic pain structure. Consequently, frequent exchanges occur with the pain specialists involved in this structure, thus allowing for immediate optimization of pain treatments. The goal is to halt the process of central sensitization.
“We strongly believe in this type of transitional structure, even though it requires significant human resources,” said Lebuffe. He also called for a “societal reflection” on this issue because patients with chronic pain represent a significant cost to society, in terms of medications and work stoppages. Moreover, patients who are forced to stop working see their lives disrupted.
Managing POCP
When POCP with neuropathic characteristics has been diagnosed, specific treatments and techniques for chronic pain can be prescribed earlier than they currently are. “Systemic drug treatments for neuropathic POCP rely on various therapeutic classes (opioids, antidepressants, antiepileptics), which are not without side effects for the patient,” said Violaine D’ans, an anesthesiologist and pain management specialist at Polyclinique du Parc in Caen, France. Hence, the idea is to prescribe a minimal dose while providing the patient with techniques available to anesthesiologists. “We have a good range of management options that we use in perioperative pain management, and we have a role to play in radio- or CT-guided perinerve infiltrations, with continuous peripheral nerve blocks and possibly later with electrostimulation to help restore movement and avoid kinesiophobia.”
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Postoperative chronic pain (POCP) is common and is expected to become increasingly prevalent. This type of pain, however, which specifically arises following surgery, independent of any infection or surgical failure, remains poorly understood. Facilities dedicated to treating it are nearly nonexistent.
At the 2024 congress of the French Society of Anesthesia and Resuscitation, anesthesiologists specializing in pain management advocated for improved management of POCP. They put themselves forward as essential interlocutors and actors in this effort. The anesthesiologists also called for better recognition of postoperative pain by patients, general practitioners, and surgeons to enable early intervention and reduce the risk for chronicity.
Underrecognized, Poorly Managed
POCP is defined as persistent pain lasting more than 3 months after surgery, unrelated to preoperative pain, and not associated with surgical complications. It can manifest in various forms, but the most typical scenario involves a patient complaining of persistent pain that developed following a surgical procedure. Normal radiological and biologic assessments rule out infectious complications. The persistence of pain long after surgery contrasts with what is often considered a successful surgical outcome by the surgeon.
“Of the 10 million patients operated on each year in France, it is estimated that about 10% will develop POCP, equating to 1.2 million patients,” explained Cyril Quémeneur, a specialist in anesthesiology and pain management at Pitié-Salpêtrière Hospital in Paris, France.
Because of the increasing number of surgical interventions in recent years, POCP has become a major concern. “Currently, there are 275 facilities dedicated to chronic pain across the country, capable of accommodating between 300,000 and 400,000 patients. Given that knee replacement surgery — the incidence of which is rising sharply — results in postoperative pain for 20%-30% of operated patients, the question of managing this type of pain will become even more pressing in the future,” said Quémeneur.
Moreover, specialized facilities for transitional pain management are not widespread in France, unlike in Canada, which has been developing them for about a decade, he noted.
France’s pain treatment centers “are overwhelmed,” said Gilles Lebuffe, a specialist in anesthesiology and pain management at Lille University Hospital in Lille, France. “Thus, the time between when the patient is operated on and when we discuss chronic pain allows the painful condition to establish itself, leading to central sensitization at the neurological level.” Once established, this pain is difficult to treat. “The later a patient arrives at a pain center, the more challenging the situation is to manage,” said Lebuffe.
Risk Factors
It is therefore crucial to identify patients at higher risk for postoperative pain during the anesthesia consultation, thus allowing for monitoring during the postoperative period. These pains can be highly debilitating because of their intensity, chronicity, and impact on quality of life.
To target these patients, it is essential to understand which surgeries and patient types constitute risk factors, as well as the characteristics of the pain experienced.
While all surgeries can lead to POCP, certain procedures are more likely to result in chronic pain. They include breast surgery with mastectomy, thoracic and spinal surgery, amputations, and knee replacement surgery. Notably, surgical repair of inguinal hernias, considered routine surgery, is emblematic of the risk for POCP. Its incidence after this procedure is 10% or more in the literature.
In addition, POCP often has neuropathic characteristics. Patients frequently describe their pain using terms like “burning” or “electric shock.” These pains are often associated with strange sensations such as tingling, prickling, itching, or numbness. “This describes neuropathic pain, which increases the risk of chronicity,” said Lebuffe.
Preoperative Opioid Use
Another warning sign for healthcare professionals is that patients with chronic pain may have factors associated with vulnerability. Women, who have a higher incidence of chronic pain syndrome, are at greater risk of developing postoperative chronic pain than men.
It has also been shown that preoperative opioid use leads to higher postoperative pain intensities for several days. This is a factor to consider, even though opioid consumption rates in France are far lower than those in the United States, where as much as 35% of patients use opioids preoperatively, said Frédéric Aubrun, head of the Anesthesia and Intensive Care Department and a pain management specialist at the Hospices Civils de Lyon in Lyon, France. Finally, significant literature indicates that psychological fragility is a risk factor for more intense acute pain and for POCP. “Patients with chronic pain frequently have depressive symptoms and anxiety,” said Lebuffe.
Involving General Practitioners
Because one responsibility of general practitioners is to identify patients with abnormal postoperative pain trajectories, the anesthesiologists at the press conference advocated for greater patient awareness and increased involvement of general practitioners in this identification process.
“If there is an expected duration of postoperative pain at varying intensities, since it all depends on the patient’s journey (the number of reoperations, history of opioid use, etc.), it is necessary to make patients aware that it is not normal to suffer long after a surgical intervention,” said Aubrun. In addition, it is important to “connect with primary care” and mobilize general practitioners to “detect patients sliding toward opioid overconsumption” and refer them to the appropriate care structure, he said.
Although dedicated facilities for this type of pain — like transitional pain clinics in Canada or northern Europe — do not exist in France, some hospitals, like Lille University Hospital, have established “intermediate consultations targeting patients with specific pain or chronicity characteristics. In these consultations, patients are systematically reviewed 4-6 weeks after surgery by the surgeon, who has been trained to identify neuropathic pain,” said Lebuffe. When a patient with such pain is identified, he or she is referred to an intermediate consultation and seen by a fellow anesthesiologist. The advantage of this consultation is that it is linked to a chronic pain structure. Consequently, frequent exchanges occur with the pain specialists involved in this structure, thus allowing for immediate optimization of pain treatments. The goal is to halt the process of central sensitization.
“We strongly believe in this type of transitional structure, even though it requires significant human resources,” said Lebuffe. He also called for a “societal reflection” on this issue because patients with chronic pain represent a significant cost to society, in terms of medications and work stoppages. Moreover, patients who are forced to stop working see their lives disrupted.
Managing POCP
When POCP with neuropathic characteristics has been diagnosed, specific treatments and techniques for chronic pain can be prescribed earlier than they currently are. “Systemic drug treatments for neuropathic POCP rely on various therapeutic classes (opioids, antidepressants, antiepileptics), which are not without side effects for the patient,” said Violaine D’ans, an anesthesiologist and pain management specialist at Polyclinique du Parc in Caen, France. Hence, the idea is to prescribe a minimal dose while providing the patient with techniques available to anesthesiologists. “We have a good range of management options that we use in perioperative pain management, and we have a role to play in radio- or CT-guided perinerve infiltrations, with continuous peripheral nerve blocks and possibly later with electrostimulation to help restore movement and avoid kinesiophobia.”
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.