User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Murder of physician raises the stress level for all clinicians
As if it weren’t enough that doctors work in a profession where it’s almost more a question of when they’ll be sued than if they’ll be sued – where COVID, staff shortages, long hours, and patients frustrated over canceled procedures have caused unrelenting fatigue and stress – they now have to worry that an unhappy patient is going to buy a gun, walk into their office, and kill them.
That’s exactly what happened in Tulsa, Okla., where a patient complaining of pain after back surgery murdered his doctor and several others who happened to be in the wrong place at the wrong time.
The temptation in the aftermath of such tragedies is to think about preventive measures: Make medical facilities “hardened” targets, like schools have become, with armed guards, metal detectors, automatically locking doors, physical barriers within, security cameras, and buzzers for entry – although hardening a large medical center where members of the community routinely come and go would be challenging.
What about the enormous stress on doctors, nurses, and others in the medical workplace? Physicians who have been sued for malpractice often describe how it changes the way they interact with patients: They now size patients up and make judgments about their potential litigiousness. Will the physicians now look over their patients’ shoulders at the video feed from a security camera when they’re taking a history? Will medical professionals be forced to make snap judgments about patients’ psychological state before deciding whether to treat them?
Remember, there was a time when school shootings were unimaginable. Once one person crosses that line, others inevitably follow.
It could be a drug-seeking patient complaining of ongoing pain, angry because he can’t get a new prescription. It could be a patient whose unpaid bill was turned over to a collection agency, angry because he’s now getting calls from collectors. It could be someone who blames a physician for the loss of a loved one. It could be someone who would otherwise have filed a lawsuit, who now thinks he has a more effective option for exacting retribution.
Most of us would find it unbearable to live and work under the kind of stress faced by medical professionals today. And unfortunately, there is no short-term, systemic relief on the horizon. But there are methods of relieving at least some of the psychological burden being carried by these dedicated individuals.
For starters, the government should provide funds to improve safety and security at medical facilities. It’s sad but it’s a fact of life. The physical structure of schools, along with emergency procedures, have been changed since Columbine and Sandy Hook, and our children and their teachers undergo active shooter drills. Health care facilities will need to adopt similar strategies.
But if we don’t also support the individuals who work in health care, we’ll no longer have even partially staffed health care facilities. Hospitals and medical groups need to be conscious of the effects stress may have on them. Medical staff and administrators need to recognize changes in their colleagues’ behavior and refer those cohorts to professional stress coaches who can get them back on track.
Medical personnel should be picking up on warning signs, like irritability, depression, sudden weight gain or loss, lack of motivation and job satisfaction, obsessiveness, unusual levels of fatigue, alcohol or drug use, and, of course, avoidable medical errors.
In addition, colleagues in the medical workplace need to know each other well. They are usually the first ones to notice if something is off and may be in the best position to refer coworkers for help. Also, medical malpractice insurance carriers should consider encouraging and covering coaching sessions, because helping physicians cope with this heightened stress will prevent medical errors and the lawsuits that inevitably accompany mistakes.
This needn’t be a long-term process like ongoing psychotherapy; a few sessions with a well-trained coach may help psychologically challenged peers restore their focus and perspective. It won’t eliminate the threat any more than litigation stress coaching eliminates the threat of being sued, but it can prevent that stress from leading to avoidable errors. It also can prevent physicians’ personal lives and relationships from going off the rails and driving them out of the medical profession.
None of us can afford to ignore the impacts that these new stressors are having and simply act as if it’s business as usual. The people in the trenches need our help.
Ms. Fiore is President of Winning Focus in Murrysville, Pa. She has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As if it weren’t enough that doctors work in a profession where it’s almost more a question of when they’ll be sued than if they’ll be sued – where COVID, staff shortages, long hours, and patients frustrated over canceled procedures have caused unrelenting fatigue and stress – they now have to worry that an unhappy patient is going to buy a gun, walk into their office, and kill them.
That’s exactly what happened in Tulsa, Okla., where a patient complaining of pain after back surgery murdered his doctor and several others who happened to be in the wrong place at the wrong time.
The temptation in the aftermath of such tragedies is to think about preventive measures: Make medical facilities “hardened” targets, like schools have become, with armed guards, metal detectors, automatically locking doors, physical barriers within, security cameras, and buzzers for entry – although hardening a large medical center where members of the community routinely come and go would be challenging.
What about the enormous stress on doctors, nurses, and others in the medical workplace? Physicians who have been sued for malpractice often describe how it changes the way they interact with patients: They now size patients up and make judgments about their potential litigiousness. Will the physicians now look over their patients’ shoulders at the video feed from a security camera when they’re taking a history? Will medical professionals be forced to make snap judgments about patients’ psychological state before deciding whether to treat them?
Remember, there was a time when school shootings were unimaginable. Once one person crosses that line, others inevitably follow.
It could be a drug-seeking patient complaining of ongoing pain, angry because he can’t get a new prescription. It could be a patient whose unpaid bill was turned over to a collection agency, angry because he’s now getting calls from collectors. It could be someone who blames a physician for the loss of a loved one. It could be someone who would otherwise have filed a lawsuit, who now thinks he has a more effective option for exacting retribution.
Most of us would find it unbearable to live and work under the kind of stress faced by medical professionals today. And unfortunately, there is no short-term, systemic relief on the horizon. But there are methods of relieving at least some of the psychological burden being carried by these dedicated individuals.
For starters, the government should provide funds to improve safety and security at medical facilities. It’s sad but it’s a fact of life. The physical structure of schools, along with emergency procedures, have been changed since Columbine and Sandy Hook, and our children and their teachers undergo active shooter drills. Health care facilities will need to adopt similar strategies.
But if we don’t also support the individuals who work in health care, we’ll no longer have even partially staffed health care facilities. Hospitals and medical groups need to be conscious of the effects stress may have on them. Medical staff and administrators need to recognize changes in their colleagues’ behavior and refer those cohorts to professional stress coaches who can get them back on track.
Medical personnel should be picking up on warning signs, like irritability, depression, sudden weight gain or loss, lack of motivation and job satisfaction, obsessiveness, unusual levels of fatigue, alcohol or drug use, and, of course, avoidable medical errors.
In addition, colleagues in the medical workplace need to know each other well. They are usually the first ones to notice if something is off and may be in the best position to refer coworkers for help. Also, medical malpractice insurance carriers should consider encouraging and covering coaching sessions, because helping physicians cope with this heightened stress will prevent medical errors and the lawsuits that inevitably accompany mistakes.
This needn’t be a long-term process like ongoing psychotherapy; a few sessions with a well-trained coach may help psychologically challenged peers restore their focus and perspective. It won’t eliminate the threat any more than litigation stress coaching eliminates the threat of being sued, but it can prevent that stress from leading to avoidable errors. It also can prevent physicians’ personal lives and relationships from going off the rails and driving them out of the medical profession.
None of us can afford to ignore the impacts that these new stressors are having and simply act as if it’s business as usual. The people in the trenches need our help.
Ms. Fiore is President of Winning Focus in Murrysville, Pa. She has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As if it weren’t enough that doctors work in a profession where it’s almost more a question of when they’ll be sued than if they’ll be sued – where COVID, staff shortages, long hours, and patients frustrated over canceled procedures have caused unrelenting fatigue and stress – they now have to worry that an unhappy patient is going to buy a gun, walk into their office, and kill them.
That’s exactly what happened in Tulsa, Okla., where a patient complaining of pain after back surgery murdered his doctor and several others who happened to be in the wrong place at the wrong time.
The temptation in the aftermath of such tragedies is to think about preventive measures: Make medical facilities “hardened” targets, like schools have become, with armed guards, metal detectors, automatically locking doors, physical barriers within, security cameras, and buzzers for entry – although hardening a large medical center where members of the community routinely come and go would be challenging.
What about the enormous stress on doctors, nurses, and others in the medical workplace? Physicians who have been sued for malpractice often describe how it changes the way they interact with patients: They now size patients up and make judgments about their potential litigiousness. Will the physicians now look over their patients’ shoulders at the video feed from a security camera when they’re taking a history? Will medical professionals be forced to make snap judgments about patients’ psychological state before deciding whether to treat them?
Remember, there was a time when school shootings were unimaginable. Once one person crosses that line, others inevitably follow.
It could be a drug-seeking patient complaining of ongoing pain, angry because he can’t get a new prescription. It could be a patient whose unpaid bill was turned over to a collection agency, angry because he’s now getting calls from collectors. It could be someone who blames a physician for the loss of a loved one. It could be someone who would otherwise have filed a lawsuit, who now thinks he has a more effective option for exacting retribution.
Most of us would find it unbearable to live and work under the kind of stress faced by medical professionals today. And unfortunately, there is no short-term, systemic relief on the horizon. But there are methods of relieving at least some of the psychological burden being carried by these dedicated individuals.
For starters, the government should provide funds to improve safety and security at medical facilities. It’s sad but it’s a fact of life. The physical structure of schools, along with emergency procedures, have been changed since Columbine and Sandy Hook, and our children and their teachers undergo active shooter drills. Health care facilities will need to adopt similar strategies.
But if we don’t also support the individuals who work in health care, we’ll no longer have even partially staffed health care facilities. Hospitals and medical groups need to be conscious of the effects stress may have on them. Medical staff and administrators need to recognize changes in their colleagues’ behavior and refer those cohorts to professional stress coaches who can get them back on track.
Medical personnel should be picking up on warning signs, like irritability, depression, sudden weight gain or loss, lack of motivation and job satisfaction, obsessiveness, unusual levels of fatigue, alcohol or drug use, and, of course, avoidable medical errors.
In addition, colleagues in the medical workplace need to know each other well. They are usually the first ones to notice if something is off and may be in the best position to refer coworkers for help. Also, medical malpractice insurance carriers should consider encouraging and covering coaching sessions, because helping physicians cope with this heightened stress will prevent medical errors and the lawsuits that inevitably accompany mistakes.
This needn’t be a long-term process like ongoing psychotherapy; a few sessions with a well-trained coach may help psychologically challenged peers restore their focus and perspective. It won’t eliminate the threat any more than litigation stress coaching eliminates the threat of being sued, but it can prevent that stress from leading to avoidable errors. It also can prevent physicians’ personal lives and relationships from going off the rails and driving them out of the medical profession.
None of us can afford to ignore the impacts that these new stressors are having and simply act as if it’s business as usual. The people in the trenches need our help.
Ms. Fiore is President of Winning Focus in Murrysville, Pa. She has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alabama cites Roe decision in call to ban transgender health care
Alabama urged a federal court on June 28 to drop its block on the state’s ban on gender-affirming care for transgender youth, citing the Supreme Court’s recent decision to overturn Roe v. Wade.
Alabama Attorney General Steve Marshall said the high court ruled that abortion isn’t protected under the 14th Amendment because it’s not “deeply rooted” in the nation’s history, which he noted could be said about access to gender-affirming care as well, according to Axios.
“No one – adult or child – has a right to transitioning treatments that is deeply rooted in our Nation’s history and tradition,” he wrote in a court document.
“The State can thus regulate or prohibit those interventions for children, even if an adult wants the drugs for his child,” he wrote.
In May, a federal judge blocked part of Alabama’s Senate Bill 184, which makes it a felony for someone to “engage in or cause” certain types of medical care for transgender youths. The law, which was put in place in April, allows for criminal prosecution against doctors, parents, guardians, and anyone else who provides care to a minor. The penalties could result in up to 10 years in prison and up to $15,000 in fines.
At that time, U.S. District Judge Liles Burke issued an injunction to stop Alabama from enforcing the law and allow challenges, including one filed by the Department of Justice. Mr. Burke said the state provided “no credible evidence to show that transitioning medications are ‘experimental.’ ”
“While Defendants offer some evidence that transitioning medications pose certain risks, the uncontradicted record evidence is that at least twenty-two major medical associations in the United States endorse transitioning medications as well-established, evidence-based treatments for gender dysphoria in minors,” he wrote in the ruling.
Medical organizations such as the American Academy of Pediatrics, American Psychological Association, and American Medical Association have urged governors to oppose legislation this year that would restrict gender-affirming medical care, saying that such laws could have negative effects on the mental health of transgender youths.
But on June 28, Mr. Marshall focused on the Constitution and what he believes the recent overturn of Roe implies.
“Just as the parental relationship does not unlock a Due Process right allowing parents to obtain medical marijuana or abortions for their children, neither does it unlock a right to transitioning treatments,” he wrote.
“The Constitution reserves to the State – not courts or medical interest groups – the authority to determine that these sterilizing interventions are too dangerous for minors,” he said.
Since the Supreme Court overturned Roe, people have expressed concerns that lawsuits could now target several rights that are protected under the 14th Amendment, including same-sex relationships, marriage equality, and access to contraceptives.
Justice Clarence Thomas, who wrote a concurring opinion to the majority decision, said the Supreme Court, “in future cases” should reconsider “substantive due process precedents” under previous landmark cases such as Griswold v. Connecticut, Lawrence v. Texas, and Obergefell v. Hodges.
At the same time, Justice Brett Kavanaugh, who also wrote a concurring opinion, said the decision to overturn Roe was only focused on abortion, saying it “does not mean the overruling of those precedents, and does not threaten or cast doubt on those precedents.”
A version of this article first appeared on WebMD.com.
Alabama urged a federal court on June 28 to drop its block on the state’s ban on gender-affirming care for transgender youth, citing the Supreme Court’s recent decision to overturn Roe v. Wade.
Alabama Attorney General Steve Marshall said the high court ruled that abortion isn’t protected under the 14th Amendment because it’s not “deeply rooted” in the nation’s history, which he noted could be said about access to gender-affirming care as well, according to Axios.
“No one – adult or child – has a right to transitioning treatments that is deeply rooted in our Nation’s history and tradition,” he wrote in a court document.
“The State can thus regulate or prohibit those interventions for children, even if an adult wants the drugs for his child,” he wrote.
In May, a federal judge blocked part of Alabama’s Senate Bill 184, which makes it a felony for someone to “engage in or cause” certain types of medical care for transgender youths. The law, which was put in place in April, allows for criminal prosecution against doctors, parents, guardians, and anyone else who provides care to a minor. The penalties could result in up to 10 years in prison and up to $15,000 in fines.
At that time, U.S. District Judge Liles Burke issued an injunction to stop Alabama from enforcing the law and allow challenges, including one filed by the Department of Justice. Mr. Burke said the state provided “no credible evidence to show that transitioning medications are ‘experimental.’ ”
“While Defendants offer some evidence that transitioning medications pose certain risks, the uncontradicted record evidence is that at least twenty-two major medical associations in the United States endorse transitioning medications as well-established, evidence-based treatments for gender dysphoria in minors,” he wrote in the ruling.
Medical organizations such as the American Academy of Pediatrics, American Psychological Association, and American Medical Association have urged governors to oppose legislation this year that would restrict gender-affirming medical care, saying that such laws could have negative effects on the mental health of transgender youths.
But on June 28, Mr. Marshall focused on the Constitution and what he believes the recent overturn of Roe implies.
“Just as the parental relationship does not unlock a Due Process right allowing parents to obtain medical marijuana or abortions for their children, neither does it unlock a right to transitioning treatments,” he wrote.
“The Constitution reserves to the State – not courts or medical interest groups – the authority to determine that these sterilizing interventions are too dangerous for minors,” he said.
Since the Supreme Court overturned Roe, people have expressed concerns that lawsuits could now target several rights that are protected under the 14th Amendment, including same-sex relationships, marriage equality, and access to contraceptives.
Justice Clarence Thomas, who wrote a concurring opinion to the majority decision, said the Supreme Court, “in future cases” should reconsider “substantive due process precedents” under previous landmark cases such as Griswold v. Connecticut, Lawrence v. Texas, and Obergefell v. Hodges.
At the same time, Justice Brett Kavanaugh, who also wrote a concurring opinion, said the decision to overturn Roe was only focused on abortion, saying it “does not mean the overruling of those precedents, and does not threaten or cast doubt on those precedents.”
A version of this article first appeared on WebMD.com.
Alabama urged a federal court on June 28 to drop its block on the state’s ban on gender-affirming care for transgender youth, citing the Supreme Court’s recent decision to overturn Roe v. Wade.
Alabama Attorney General Steve Marshall said the high court ruled that abortion isn’t protected under the 14th Amendment because it’s not “deeply rooted” in the nation’s history, which he noted could be said about access to gender-affirming care as well, according to Axios.
“No one – adult or child – has a right to transitioning treatments that is deeply rooted in our Nation’s history and tradition,” he wrote in a court document.
“The State can thus regulate or prohibit those interventions for children, even if an adult wants the drugs for his child,” he wrote.
In May, a federal judge blocked part of Alabama’s Senate Bill 184, which makes it a felony for someone to “engage in or cause” certain types of medical care for transgender youths. The law, which was put in place in April, allows for criminal prosecution against doctors, parents, guardians, and anyone else who provides care to a minor. The penalties could result in up to 10 years in prison and up to $15,000 in fines.
At that time, U.S. District Judge Liles Burke issued an injunction to stop Alabama from enforcing the law and allow challenges, including one filed by the Department of Justice. Mr. Burke said the state provided “no credible evidence to show that transitioning medications are ‘experimental.’ ”
“While Defendants offer some evidence that transitioning medications pose certain risks, the uncontradicted record evidence is that at least twenty-two major medical associations in the United States endorse transitioning medications as well-established, evidence-based treatments for gender dysphoria in minors,” he wrote in the ruling.
Medical organizations such as the American Academy of Pediatrics, American Psychological Association, and American Medical Association have urged governors to oppose legislation this year that would restrict gender-affirming medical care, saying that such laws could have negative effects on the mental health of transgender youths.
But on June 28, Mr. Marshall focused on the Constitution and what he believes the recent overturn of Roe implies.
“Just as the parental relationship does not unlock a Due Process right allowing parents to obtain medical marijuana or abortions for their children, neither does it unlock a right to transitioning treatments,” he wrote.
“The Constitution reserves to the State – not courts or medical interest groups – the authority to determine that these sterilizing interventions are too dangerous for minors,” he said.
Since the Supreme Court overturned Roe, people have expressed concerns that lawsuits could now target several rights that are protected under the 14th Amendment, including same-sex relationships, marriage equality, and access to contraceptives.
Justice Clarence Thomas, who wrote a concurring opinion to the majority decision, said the Supreme Court, “in future cases” should reconsider “substantive due process precedents” under previous landmark cases such as Griswold v. Connecticut, Lawrence v. Texas, and Obergefell v. Hodges.
At the same time, Justice Brett Kavanaugh, who also wrote a concurring opinion, said the decision to overturn Roe was only focused on abortion, saying it “does not mean the overruling of those precedents, and does not threaten or cast doubt on those precedents.”
A version of this article first appeared on WebMD.com.
In the Grand Canyon, norovirus gives new meaning to ‘leave no trace’
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Prioritizing Mental Health in Residency
The World Health Organization declared COVID-19 a pandemic on March 11, 2020, just 4 months before the start of a new residency cycle. Referred to as “COVID interns,” PGY-1 residents transitioning out of medical school in 2020 faced an unprecedented challenge of doctoring within a confused and ill-prepared health care system, while senior residents scrambled to adjust to their rapidly changing training programs. Each subsequent week brought more sobering news of increasing hospitalizations, intensive care unit admissions, and deaths; hospitals across the country resorted to the redeployment of residents across all specialties to buffer the growing need within their internal medicine and critical care units.1 And while the news and social media blurred into a collage of ventilator shortages, politicization of science, and “#healthcareheroes,” one study showed53.7% of medical interns (N=108) were struggling with mild to extremely severe depression, while 63.9% reported mild to severe anxiety.2
Many shortcomings of our health care system—ill preparedness, racial disparity, health illiteracy—were highlighted during the COVID-19 pandemic, and providers’ mental health was no exception.3 Classic psychosocial risk factors, such as high demands, lack of control, lack of institutional support, and absence of reward defined the workplace, leading Theorell4 to call it “a randomized trial for maximal worsening of the work environment.” Stress and burnout during residency are not novel concepts. A 2002 survey including 415 medical residency programs with a response from more than 4000 residents found depressive symptoms in 35% of respondents, paired with feelings of increased cynicism and decreased humanism despite major curricular reforms and duty hour limitations.5 Unfortunately, the statistics in the coming years hardly budged and, in the wake of the pandemic, culminated to more than 50% to 76% of physicians worldwide reporting burnout in 2020.6-8
As a COVID intern at Brigham and Women’s Hospital (Boston, Massachusetts), I also experienced the demanding workload and witnessed the struggle of my colleagues firsthand. Brigham and Women’s Hospital, similar to many of its peer institutions, implemented frequent mental health check-ins within its curriculum. Known as the Intern Humanistic Curriculum, these check-ins essentially were an echo chamber to unload the psychological burdens of our workdays, and we eagerly shared what made us angry, sad, hopeful, and hopeless. During one such session, I learned about moral injury, a term originating in the military defined as the psychological stress resulting from actions—or the lack of actions—that violates one’s moral or ethical code.9 With the onslaught of patient deaths for which most of us felt unprepared, we had all endured varying degrees of moral injury. Greenberg et al9 described 2 potential outcomes after moral injury: (1) the development of mental health disorders such as depression and posttraumatic stress disorder, or (2) posttraumatic growth, which is the bolstering of psychological resilience. Notably, the outcome is based on the way someone is supported before, during, and after the challenging incident.9
With the aim of psychological growth and developing resilience, residents should prioritize mental health throughout their training. To this end, several resources are readily available, many of which I actively use or frequently revisit, which are reviewed here.
Mindfulness Meditation App
Calm (https://www.calm.com/) is one of several popular mobile applications (apps) that delivers mindfulness mediation—the practice of attending to experiences, thoughts, and emotions without bias or judgment. With more than 100 million downloads, Calm includes meditation tutorials, breathing exercises, nature scenes and sounds, and audio programs taught by mindfulness experts for $69.99 a year or $14.99 a month. Systemic reviews have demonstrated reduced sleep disturbance, decreased ruminative thoughts and emotional reactivity, and increased awareness and acceptance in those practicing mindfulness meditation. Calm users have reported these benefits, with many able to forego the time- and cost-intensive cognitive behavioral therapy that requires highly trained therapists.10-12
Exercise to Relieve Stress
Both aerobic and anaerobic exercises are antidepressive and anxiolytic and also lower one’s overall sensitivity to stress. Whether it is governed by neurotransmitters such as the activation of the opioid systems or the release of endogenous endorphins or time spent focusing on a different task at hand, the benefits of exercise against mental stressors have been extensively studied and established.13 Consider obtaining a new gym membership at the start of residency or joining an intramural team. Both have the added benefit of expanding your social circle.
Socialize With Others
Social isolation and perceived loneliness are key stressors linked to neuroendocrine disturbances that underlie depression, anxiety, and even schizophrenia.14,15 Throughout residency there will be several social events and opportunities to gather with colleagues—inside or outside of the work environment—and residents should attend as time allows. Even virtual social interactions were found to reduce stress and help in the treatment of social anxiety disorder.14
Communicate About Stressors
Open up to your co-residents, friends, and family about any struggles that may be invisible on the outside. Even attendings can empathize with the struggles of residency, and the mentors in place are actively trained to prioritize resident wellness. If verbal communication is not your strength, try journaling. Writing helps to untangle and better define underlying stressors and is itself meditative.16,17 However, ensure that your journaling is focused on positive emotional responses and aims to determine the positive benefits within any stressful event; those solely expressing negative emotions were found to have higher levels of stress and anxiety afterward than they had before.17
Seek a Mental Health Specialist
As with all other human ailments, severe mental health disorders require specialists and proper medication. Unfortunately, substantial stigma accompanying mental health continues to permeate medicine, creating considerable barriers for residents in need of care.18 A 2016 survey of more than 2000 physicians found that those with mental illnesses did not seek treatment due to limited time, fear of being reported to a medical licensing board, concern over obtaining licensure, and shame or embarrassment at the diagnosis.19 Besides urging residents to seek care, more effort should be invested in addressing the stigma and ensuring confidentiality. In 2021, the internal medicine and medicine-pediatrics residency at the University of Colorado Anschutz Medical Campus (Aurora, Colorado) developed a confidential opt-out, rather than opt-in, mental health program, and appointments were made for all 80 interns in advance. In doing so, they found increased participation and self-reported wellness at a relatively low cost and simple implementation.20 For trainees without such access, online or mobile therapy platforms offering electronic mental health treatment or telepsychiatry also have been employed.21,22 The onus ultimately is still on the individual to seek the care they need. Although only an anecdotal piece of evidence, I have found the prevalence of physicians taking selective serotonin reuptake inhibitors such as escitalopram, sertraline, or fluoxetine to be strikingly common and quite beneficial.
Final Thoughts
Residency remains rife with financial, emotional, and physical stressors; even as the dust settles on the COVID-19 pandemic, the light shed on the importance of trainee mental health must remain illuminated. For the aforementioned resources to have an impact, residents need to be empowered to openly discuss mental health issues and to seek help if necessary. Finally, in 2018, the Journal of Graduate Medical Education published a 10-year prospective cohort study that found that emotional distress during residency persists in professional practice even 10 years after residency and is associated with future burnout.23 Trainees should consider prioritizing their mental health to not only improve their quality of life in the present but also as an investment for their future.
- Spiegelman J, Praiss A, Syeda S, et al. Preparation and redeployment of house staff during a pandemic. Semin Perinatol. 2020;44:151297.
- Debnath PR, Islam MS, Karmakar PK, et al. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary care hospital in Bangladesh. Int J Ment Health Addict. 2021:1-21. doi:10.1007/s11469-021-00690-0
- O’Reilly-Shah VN, Gentry KR, Van Cleve W, et al. The COVID-19 pandemic highlights shortcomings in US health care informatics infrastructure: a call to action. Anesth Analg. 2020;131:340-344.
- Theorell T. COVID-19 and working conditions in health care. Psychother Psychosom. 2020;89:193-194.
- Collier VU, McCue JD, Markus A, et al. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136:384-390.
- AbuDujain NM, Almuhaideb QA, Alrumaihi NA, et al. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13:E19250.
- Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020;8:421.
- Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80-90.
- Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211.
- Gal E, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;279:131-142.
- Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:E14273.
- Huberty J, Puzia ME, Larkey L, et al. Can a meditation app help my sleep? a cross-sectional survey of Calm users. PLoS One. 2021;16:E0257518.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61.
- Kampmann IL, Emmelkamp PM, Hartanto D, et al. Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav Res Ther. 2016;77:147-156.
- Mumtaz F, Khan MI, Zubair M, et al. Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother. 2018;105:1205-1222.
- Khanna P, Singh K. Stress management training and gratitude journaling in the classroom: an initial investigation in Indian context. Curr Psychol. 2021;40:5737-5748.
- Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med. 2002;24:244-250.
- Outhoff K. Depression in doctors: a bitter pill to swallow. S Afr Fam Pract. 2019;61(suppl 1):S11-S14.
- Gold KJ, Andrew LB, Goldman EB, et al. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51-57.
- Major A, Williams JG, McGuire WC, et al. Removing barriers: a confidential opt-out mental health pilot program for internal medicine interns. Acad Med. 2021;96:686-689.
- Greenhalgh T, Wherton J. Telepsychiatry: learning from the pandemic. Br J Psychiatry. 2022;220:1-5.
- Timakum T, Xie Q, Song M. Analysis of E-mental health research: mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 2022;22:57.
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10:524-531.
The World Health Organization declared COVID-19 a pandemic on March 11, 2020, just 4 months before the start of a new residency cycle. Referred to as “COVID interns,” PGY-1 residents transitioning out of medical school in 2020 faced an unprecedented challenge of doctoring within a confused and ill-prepared health care system, while senior residents scrambled to adjust to their rapidly changing training programs. Each subsequent week brought more sobering news of increasing hospitalizations, intensive care unit admissions, and deaths; hospitals across the country resorted to the redeployment of residents across all specialties to buffer the growing need within their internal medicine and critical care units.1 And while the news and social media blurred into a collage of ventilator shortages, politicization of science, and “#healthcareheroes,” one study showed53.7% of medical interns (N=108) were struggling with mild to extremely severe depression, while 63.9% reported mild to severe anxiety.2
Many shortcomings of our health care system—ill preparedness, racial disparity, health illiteracy—were highlighted during the COVID-19 pandemic, and providers’ mental health was no exception.3 Classic psychosocial risk factors, such as high demands, lack of control, lack of institutional support, and absence of reward defined the workplace, leading Theorell4 to call it “a randomized trial for maximal worsening of the work environment.” Stress and burnout during residency are not novel concepts. A 2002 survey including 415 medical residency programs with a response from more than 4000 residents found depressive symptoms in 35% of respondents, paired with feelings of increased cynicism and decreased humanism despite major curricular reforms and duty hour limitations.5 Unfortunately, the statistics in the coming years hardly budged and, in the wake of the pandemic, culminated to more than 50% to 76% of physicians worldwide reporting burnout in 2020.6-8
As a COVID intern at Brigham and Women’s Hospital (Boston, Massachusetts), I also experienced the demanding workload and witnessed the struggle of my colleagues firsthand. Brigham and Women’s Hospital, similar to many of its peer institutions, implemented frequent mental health check-ins within its curriculum. Known as the Intern Humanistic Curriculum, these check-ins essentially were an echo chamber to unload the psychological burdens of our workdays, and we eagerly shared what made us angry, sad, hopeful, and hopeless. During one such session, I learned about moral injury, a term originating in the military defined as the psychological stress resulting from actions—or the lack of actions—that violates one’s moral or ethical code.9 With the onslaught of patient deaths for which most of us felt unprepared, we had all endured varying degrees of moral injury. Greenberg et al9 described 2 potential outcomes after moral injury: (1) the development of mental health disorders such as depression and posttraumatic stress disorder, or (2) posttraumatic growth, which is the bolstering of psychological resilience. Notably, the outcome is based on the way someone is supported before, during, and after the challenging incident.9
With the aim of psychological growth and developing resilience, residents should prioritize mental health throughout their training. To this end, several resources are readily available, many of which I actively use or frequently revisit, which are reviewed here.
Mindfulness Meditation App
Calm (https://www.calm.com/) is one of several popular mobile applications (apps) that delivers mindfulness mediation—the practice of attending to experiences, thoughts, and emotions without bias or judgment. With more than 100 million downloads, Calm includes meditation tutorials, breathing exercises, nature scenes and sounds, and audio programs taught by mindfulness experts for $69.99 a year or $14.99 a month. Systemic reviews have demonstrated reduced sleep disturbance, decreased ruminative thoughts and emotional reactivity, and increased awareness and acceptance in those practicing mindfulness meditation. Calm users have reported these benefits, with many able to forego the time- and cost-intensive cognitive behavioral therapy that requires highly trained therapists.10-12
Exercise to Relieve Stress
Both aerobic and anaerobic exercises are antidepressive and anxiolytic and also lower one’s overall sensitivity to stress. Whether it is governed by neurotransmitters such as the activation of the opioid systems or the release of endogenous endorphins or time spent focusing on a different task at hand, the benefits of exercise against mental stressors have been extensively studied and established.13 Consider obtaining a new gym membership at the start of residency or joining an intramural team. Both have the added benefit of expanding your social circle.
Socialize With Others
Social isolation and perceived loneliness are key stressors linked to neuroendocrine disturbances that underlie depression, anxiety, and even schizophrenia.14,15 Throughout residency there will be several social events and opportunities to gather with colleagues—inside or outside of the work environment—and residents should attend as time allows. Even virtual social interactions were found to reduce stress and help in the treatment of social anxiety disorder.14
Communicate About Stressors
Open up to your co-residents, friends, and family about any struggles that may be invisible on the outside. Even attendings can empathize with the struggles of residency, and the mentors in place are actively trained to prioritize resident wellness. If verbal communication is not your strength, try journaling. Writing helps to untangle and better define underlying stressors and is itself meditative.16,17 However, ensure that your journaling is focused on positive emotional responses and aims to determine the positive benefits within any stressful event; those solely expressing negative emotions were found to have higher levels of stress and anxiety afterward than they had before.17
Seek a Mental Health Specialist
As with all other human ailments, severe mental health disorders require specialists and proper medication. Unfortunately, substantial stigma accompanying mental health continues to permeate medicine, creating considerable barriers for residents in need of care.18 A 2016 survey of more than 2000 physicians found that those with mental illnesses did not seek treatment due to limited time, fear of being reported to a medical licensing board, concern over obtaining licensure, and shame or embarrassment at the diagnosis.19 Besides urging residents to seek care, more effort should be invested in addressing the stigma and ensuring confidentiality. In 2021, the internal medicine and medicine-pediatrics residency at the University of Colorado Anschutz Medical Campus (Aurora, Colorado) developed a confidential opt-out, rather than opt-in, mental health program, and appointments were made for all 80 interns in advance. In doing so, they found increased participation and self-reported wellness at a relatively low cost and simple implementation.20 For trainees without such access, online or mobile therapy platforms offering electronic mental health treatment or telepsychiatry also have been employed.21,22 The onus ultimately is still on the individual to seek the care they need. Although only an anecdotal piece of evidence, I have found the prevalence of physicians taking selective serotonin reuptake inhibitors such as escitalopram, sertraline, or fluoxetine to be strikingly common and quite beneficial.
Final Thoughts
Residency remains rife with financial, emotional, and physical stressors; even as the dust settles on the COVID-19 pandemic, the light shed on the importance of trainee mental health must remain illuminated. For the aforementioned resources to have an impact, residents need to be empowered to openly discuss mental health issues and to seek help if necessary. Finally, in 2018, the Journal of Graduate Medical Education published a 10-year prospective cohort study that found that emotional distress during residency persists in professional practice even 10 years after residency and is associated with future burnout.23 Trainees should consider prioritizing their mental health to not only improve their quality of life in the present but also as an investment for their future.
The World Health Organization declared COVID-19 a pandemic on March 11, 2020, just 4 months before the start of a new residency cycle. Referred to as “COVID interns,” PGY-1 residents transitioning out of medical school in 2020 faced an unprecedented challenge of doctoring within a confused and ill-prepared health care system, while senior residents scrambled to adjust to their rapidly changing training programs. Each subsequent week brought more sobering news of increasing hospitalizations, intensive care unit admissions, and deaths; hospitals across the country resorted to the redeployment of residents across all specialties to buffer the growing need within their internal medicine and critical care units.1 And while the news and social media blurred into a collage of ventilator shortages, politicization of science, and “#healthcareheroes,” one study showed53.7% of medical interns (N=108) were struggling with mild to extremely severe depression, while 63.9% reported mild to severe anxiety.2
Many shortcomings of our health care system—ill preparedness, racial disparity, health illiteracy—were highlighted during the COVID-19 pandemic, and providers’ mental health was no exception.3 Classic psychosocial risk factors, such as high demands, lack of control, lack of institutional support, and absence of reward defined the workplace, leading Theorell4 to call it “a randomized trial for maximal worsening of the work environment.” Stress and burnout during residency are not novel concepts. A 2002 survey including 415 medical residency programs with a response from more than 4000 residents found depressive symptoms in 35% of respondents, paired with feelings of increased cynicism and decreased humanism despite major curricular reforms and duty hour limitations.5 Unfortunately, the statistics in the coming years hardly budged and, in the wake of the pandemic, culminated to more than 50% to 76% of physicians worldwide reporting burnout in 2020.6-8
As a COVID intern at Brigham and Women’s Hospital (Boston, Massachusetts), I also experienced the demanding workload and witnessed the struggle of my colleagues firsthand. Brigham and Women’s Hospital, similar to many of its peer institutions, implemented frequent mental health check-ins within its curriculum. Known as the Intern Humanistic Curriculum, these check-ins essentially were an echo chamber to unload the psychological burdens of our workdays, and we eagerly shared what made us angry, sad, hopeful, and hopeless. During one such session, I learned about moral injury, a term originating in the military defined as the psychological stress resulting from actions—or the lack of actions—that violates one’s moral or ethical code.9 With the onslaught of patient deaths for which most of us felt unprepared, we had all endured varying degrees of moral injury. Greenberg et al9 described 2 potential outcomes after moral injury: (1) the development of mental health disorders such as depression and posttraumatic stress disorder, or (2) posttraumatic growth, which is the bolstering of psychological resilience. Notably, the outcome is based on the way someone is supported before, during, and after the challenging incident.9
With the aim of psychological growth and developing resilience, residents should prioritize mental health throughout their training. To this end, several resources are readily available, many of which I actively use or frequently revisit, which are reviewed here.
Mindfulness Meditation App
Calm (https://www.calm.com/) is one of several popular mobile applications (apps) that delivers mindfulness mediation—the practice of attending to experiences, thoughts, and emotions without bias or judgment. With more than 100 million downloads, Calm includes meditation tutorials, breathing exercises, nature scenes and sounds, and audio programs taught by mindfulness experts for $69.99 a year or $14.99 a month. Systemic reviews have demonstrated reduced sleep disturbance, decreased ruminative thoughts and emotional reactivity, and increased awareness and acceptance in those practicing mindfulness meditation. Calm users have reported these benefits, with many able to forego the time- and cost-intensive cognitive behavioral therapy that requires highly trained therapists.10-12
Exercise to Relieve Stress
Both aerobic and anaerobic exercises are antidepressive and anxiolytic and also lower one’s overall sensitivity to stress. Whether it is governed by neurotransmitters such as the activation of the opioid systems or the release of endogenous endorphins or time spent focusing on a different task at hand, the benefits of exercise against mental stressors have been extensively studied and established.13 Consider obtaining a new gym membership at the start of residency or joining an intramural team. Both have the added benefit of expanding your social circle.
Socialize With Others
Social isolation and perceived loneliness are key stressors linked to neuroendocrine disturbances that underlie depression, anxiety, and even schizophrenia.14,15 Throughout residency there will be several social events and opportunities to gather with colleagues—inside or outside of the work environment—and residents should attend as time allows. Even virtual social interactions were found to reduce stress and help in the treatment of social anxiety disorder.14
Communicate About Stressors
Open up to your co-residents, friends, and family about any struggles that may be invisible on the outside. Even attendings can empathize with the struggles of residency, and the mentors in place are actively trained to prioritize resident wellness. If verbal communication is not your strength, try journaling. Writing helps to untangle and better define underlying stressors and is itself meditative.16,17 However, ensure that your journaling is focused on positive emotional responses and aims to determine the positive benefits within any stressful event; those solely expressing negative emotions were found to have higher levels of stress and anxiety afterward than they had before.17
Seek a Mental Health Specialist
As with all other human ailments, severe mental health disorders require specialists and proper medication. Unfortunately, substantial stigma accompanying mental health continues to permeate medicine, creating considerable barriers for residents in need of care.18 A 2016 survey of more than 2000 physicians found that those with mental illnesses did not seek treatment due to limited time, fear of being reported to a medical licensing board, concern over obtaining licensure, and shame or embarrassment at the diagnosis.19 Besides urging residents to seek care, more effort should be invested in addressing the stigma and ensuring confidentiality. In 2021, the internal medicine and medicine-pediatrics residency at the University of Colorado Anschutz Medical Campus (Aurora, Colorado) developed a confidential opt-out, rather than opt-in, mental health program, and appointments were made for all 80 interns in advance. In doing so, they found increased participation and self-reported wellness at a relatively low cost and simple implementation.20 For trainees without such access, online or mobile therapy platforms offering electronic mental health treatment or telepsychiatry also have been employed.21,22 The onus ultimately is still on the individual to seek the care they need. Although only an anecdotal piece of evidence, I have found the prevalence of physicians taking selective serotonin reuptake inhibitors such as escitalopram, sertraline, or fluoxetine to be strikingly common and quite beneficial.
Final Thoughts
Residency remains rife with financial, emotional, and physical stressors; even as the dust settles on the COVID-19 pandemic, the light shed on the importance of trainee mental health must remain illuminated. For the aforementioned resources to have an impact, residents need to be empowered to openly discuss mental health issues and to seek help if necessary. Finally, in 2018, the Journal of Graduate Medical Education published a 10-year prospective cohort study that found that emotional distress during residency persists in professional practice even 10 years after residency and is associated with future burnout.23 Trainees should consider prioritizing their mental health to not only improve their quality of life in the present but also as an investment for their future.
- Spiegelman J, Praiss A, Syeda S, et al. Preparation and redeployment of house staff during a pandemic. Semin Perinatol. 2020;44:151297.
- Debnath PR, Islam MS, Karmakar PK, et al. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary care hospital in Bangladesh. Int J Ment Health Addict. 2021:1-21. doi:10.1007/s11469-021-00690-0
- O’Reilly-Shah VN, Gentry KR, Van Cleve W, et al. The COVID-19 pandemic highlights shortcomings in US health care informatics infrastructure: a call to action. Anesth Analg. 2020;131:340-344.
- Theorell T. COVID-19 and working conditions in health care. Psychother Psychosom. 2020;89:193-194.
- Collier VU, McCue JD, Markus A, et al. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136:384-390.
- AbuDujain NM, Almuhaideb QA, Alrumaihi NA, et al. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13:E19250.
- Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020;8:421.
- Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80-90.
- Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211.
- Gal E, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;279:131-142.
- Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:E14273.
- Huberty J, Puzia ME, Larkey L, et al. Can a meditation app help my sleep? a cross-sectional survey of Calm users. PLoS One. 2021;16:E0257518.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61.
- Kampmann IL, Emmelkamp PM, Hartanto D, et al. Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav Res Ther. 2016;77:147-156.
- Mumtaz F, Khan MI, Zubair M, et al. Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother. 2018;105:1205-1222.
- Khanna P, Singh K. Stress management training and gratitude journaling in the classroom: an initial investigation in Indian context. Curr Psychol. 2021;40:5737-5748.
- Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med. 2002;24:244-250.
- Outhoff K. Depression in doctors: a bitter pill to swallow. S Afr Fam Pract. 2019;61(suppl 1):S11-S14.
- Gold KJ, Andrew LB, Goldman EB, et al. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51-57.
- Major A, Williams JG, McGuire WC, et al. Removing barriers: a confidential opt-out mental health pilot program for internal medicine interns. Acad Med. 2021;96:686-689.
- Greenhalgh T, Wherton J. Telepsychiatry: learning from the pandemic. Br J Psychiatry. 2022;220:1-5.
- Timakum T, Xie Q, Song M. Analysis of E-mental health research: mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 2022;22:57.
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10:524-531.
- Spiegelman J, Praiss A, Syeda S, et al. Preparation and redeployment of house staff during a pandemic. Semin Perinatol. 2020;44:151297.
- Debnath PR, Islam MS, Karmakar PK, et al. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary care hospital in Bangladesh. Int J Ment Health Addict. 2021:1-21. doi:10.1007/s11469-021-00690-0
- O’Reilly-Shah VN, Gentry KR, Van Cleve W, et al. The COVID-19 pandemic highlights shortcomings in US health care informatics infrastructure: a call to action. Anesth Analg. 2020;131:340-344.
- Theorell T. COVID-19 and working conditions in health care. Psychother Psychosom. 2020;89:193-194.
- Collier VU, McCue JD, Markus A, et al. Stress in medical residency: status quo after a decade of reform? Ann Intern Med. 2002;136:384-390.
- AbuDujain NM, Almuhaideb QA, Alrumaihi NA, et al. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13:E19250.
- Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020;8:421.
- Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80-90.
- Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211.
- Gal E, Stefan S, Cristea IA. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;279:131-142.
- Huberty J, Green J, Glissmann C, et al. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:E14273.
- Huberty J, Puzia ME, Larkey L, et al. Can a meditation app help my sleep? a cross-sectional survey of Calm users. PLoS One. 2021;16:E0257518.
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61.
- Kampmann IL, Emmelkamp PM, Hartanto D, et al. Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav Res Ther. 2016;77:147-156.
- Mumtaz F, Khan MI, Zubair M, et al. Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother. 2018;105:1205-1222.
- Khanna P, Singh K. Stress management training and gratitude journaling in the classroom: an initial investigation in Indian context. Curr Psychol. 2021;40:5737-5748.
- Ullrich PM, Lutgendorf SK. Journaling about stressful events: effects of cognitive processing and emotional expression. Ann Behav Med. 2002;24:244-250.
- Outhoff K. Depression in doctors: a bitter pill to swallow. S Afr Fam Pract. 2019;61(suppl 1):S11-S14.
- Gold KJ, Andrew LB, Goldman EB, et al. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. 2016;43:51-57.
- Major A, Williams JG, McGuire WC, et al. Removing barriers: a confidential opt-out mental health pilot program for internal medicine interns. Acad Med. 2021;96:686-689.
- Greenhalgh T, Wherton J. Telepsychiatry: learning from the pandemic. Br J Psychiatry. 2022;220:1-5.
- Timakum T, Xie Q, Song M. Analysis of E-mental health research: mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 2022;22:57.
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: a 10-year prospective cohort study. J Grad Med Educ. 2018;10:524-531.
Resident Pearl
- Although institution-sponsored wellness programs exist to promote the mental health of trainees, rates of anxiety and depression remain high among residents, which was further highlighted during the COVID-19 pandemic. Instead of passively engaging with wellness messages, residents must actively prioritize their own mental health to avoid stress and burnout.
Systemic Targeted Treatments for Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most common keratinocyte carcinoma and affects more than 3 million individuals per year in the United States.1 Approximately 40% of patients diagnosed with BCC will develop another BCC within 5 years of the initial diagnosis.2 Most cases are successfully treated with surgical excision and occasionally topical therapy or radiotherapy. Despite the high cure rate with conventional treatments, BCC can recur and can cause substantial destruction of the surrounding tissue if left untreated.3-5 In some instances, BCC can even metastasize and lead to death.6 For patients who are poor candidates for surgical or topical treatment modalities because of locally advanced BCC (laBCC) or metastatic BCC (mBCC), systemic treatment may be indicated. Vismodegib, sonidegib, and cemiplimab are the only systemic medications approved by the US Food and Drug Administration (FDA) for the treatment of laBCC and/or mBCC. Vismodegib and sonidegib target the sonic hedgehog (SHH) signaling pathway that is abnormally activated in more than 90% of BCCs.7 Cemiplimab is an immune checkpoint inhibitor (ICI) that targets the programmed cell death protein 1 (PD-1) receptor.8 Herein, we review the clinical utility of these medications and their evolving roles in the treatment of BCC.
SHH Pathway Inhibitors
The SHH pathway is a key regulator of cell proliferation and differentiation during embryogenesis.7 During adulthood, SHH signaling decreases but still plays an important role in stem cell activation and in regulation of the hair follicle growth cycle.9,10 However, de novo mutations in the genes that comprise the SHH pathway can result in aberrant constitutive activation, leading to unrestricted cell proliferation. Genetic mutations resulting in activation of Smoothened (SMO), a G-protein–coupled receptor involved in the signal transduction and propagation of the SHH pathway, have been implicated in the pathogenesis of BCC. Inactivating mutations also are commonly observed in patched homolog 1, an upstream cell-surface protein that inhibits SMO.7 The mechanism by which vismodegib and sonidegib, 2 of the FDA-approved oral medications for the treatment of advanced BCC, block the SHH pathway is through the selective inhibition of SMO.7,11
Vismodegib first received FDA approval in 2012 for the treatment of laBCC and mBCC after initial results from the pivotal ERIVANCE phase 2 trial demonstrated an objective response rate (ORR) of 43% (27/63) and 30% (10/33) in patients with locally advanced and metastatic disease, respectively. In this single-arm study, all enrolled patients (63 with laBCC and 33 with mBCC) received 150 mg of oral vismodegib daily.12 Updated results at 39 months demonstrated improved ORRs of 60% (38/63) and 48% (16/33) for the laBCC and mBCC groups, respectively. A complete response (CR) and partial response (PR) were observed in 32% (n=20) and 29% (n=18) of patients with laBCC, respectively.13 These results have been confirmed in subsequent studies, including the large international open-label trial known as STEVIE, with ORRs of 68.5% for 1119 cases of laBCC and 37% for 96 cases of mBCC.14-17 The CR and PR rates were 33% and 35%, respectively, for the laBCC group. The CR and PR rates for the mBCC group were 5% and 32%, respectively.14
The FDA approval of sonidegib for laBCC—but not mBCC—occurred in 2015 after the pivotal BOLT randomized phase 2 trial demonstrated an initial ORR of 43% (18/42) for laBCC and 15% (2/13) for mBCC after administration of 200 mg of sonidegib daily.18 A final follow-up analysis at 42 months resulted in ORRs of 56% (37/66) and 8% (1/13) for the laBCC and mBCC groups, respectively.19 Additionally, improved efficacy was not observed in the 151 patients who were randomized to receive treatment with the higher 800-mg dose; however, they did experience a higher incidence of adverse events.18,19
Currently, the true clinical differences between vismodegib and sonidegib remain uncertain, as no head-to-head trials have been conducted. Moreover, direct comparison of the data from the ERIVANCE and BOLT trials is challenging owing to fundamental differences in methodologic design, including the criteria used to assess BCC severity. The ERIVANCE trial utilized the conventional Response Evaluation Criteria in Solid Tumors (RECIST), while BOLT used the rigorous modified RECIST. However, an expert consensus study attempted to compare the 2 trials by modifying the outcomes from BOLT with the former RECIST criteria. The expert group found that the 2 SHH inhibitors had comparable efficacy and adverse event profiles.20 Nevertheless, a recent meta-analysis found that although ORRs for laBCC were similar between the 2 drugs, the CR rate for vismodegib was 31% compared with 3% for sonidegib. Additionally, for mBCC, they reported the ORR of vismodegib to be 2.7 times higher than that of sonidegib (39% vs 15%).21
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors have successfully been utilized in the treatment of cutaneous squamous cell carcinoma (cSCC); however, their use for treating BCC has been limited until recently.22-25 In February 2021, cemiplimab became the first and only ICI approved for the treatment of laBCC and mBCC in patients who did not respond to or were intolerant to prior SHH inhibitor therapy.26 Cemiplimab—a human monoclonal antibody against the PD-1 receptor expressed on T cells—blocks its interaction with programmed cell death ligand 1 and programmed cell death ligand 2 present on tumor cells. The blockade of the PD-1 pathway releases the inhibition of the antitumor immune response and enables appropriate cytotoxic T-cell activity to occur.8
The FDA approval of cemiplimab for the treatment of advanced BCC was based on an open-label, multicenter, single-arm phase 2 trial (NCT03132636) evaluating 84 patients with laBCC refractory or intolerant to SHH inhibitor therapy.26 Patients received an intravenous infusion of cemiplimab 350 mg every 3 weeks for up to 93 weeks or until disease progression or unacceptable toxicity. An ORR of 31% (26/84) was observed with a CR and PR of 6% (5/84) and 25% (21/84), respectively. The median duration of follow-up was 15 months.26 Given the clinically meaningful results of this trial, investigating the efficacy of other PD-1 inhibitors, such as pembrolizumab and nivolumab, for treatment of advanced BCC may prove worthwhile.
Adverse Effects of Systemic Treatments
The 2 approved SHH inhibitors—vismodegib and sonidegib—appear to have similar side-effect profiles, with the most common adverse effects being muscle spasms, dysgeusia, alopecia, nausea, vomiting, diarrhea, weight loss, and fatigue.20,21,27 These side effects occur at high frequencies (>40%) for both SHH inhibitors and often lead to discontinuation of the medication.21 Rates of treatment discontinuation range from 15% to 50% on average.12-14,18 Fortunately, the majority of these adverse effects do not appear to increase in severity or frequency with prolonged use of these medications.14,16,28
Various conservative and pharmacologic measures can be implemented to help manage side effects. For muscle spasms, which are the most commonly reported adverse effect, supplementation with magnesium, transcutaneous electrical nerve stimulation, acupuncture, massages, stretching, and thermal compresses can potentially be beneficial.29 Calcium channel blockers also may be effective, as one small prospective cohort study reported a reduction in the frequency of muscle cramps with amlodipine 10 mg daily.30 For alopecia, which typically is reversible and caused by SHH inhibition of the normal hair cycle, minoxidil theoretically can help, as it reduces telogen arrest and extends the anagen growth phase.31,32 Although usually mild and self-limiting, management of dysgeusia, weight loss, and gastrointestinal upset often can be managed with dietary changes, such as smaller, more frequent meals.33,34 Finally, alternative dosing strategies and drug holidays have been employed to mitigate these side effects and increase drug tolerability.35,36 These are discussed in the Alternative Dosing section.
Given the essential role of the SHH pathway in embryologic development, SHH inhibitors carry a black box warning of embryofetal teratogenicity and are contraindicated in females who are pregnant or breastfeeding. For females of reproductive potential, verification of pregnancy status should be performed prior to initiating treatment with an SHH inhibitor. These patients should be counseled on the use of contraception during treatment and for at least 24 months and 20 months after cessation of vismodegib and sonidegib, respectively.27,37,38 Male patients, even after a vasectomy, should use barrier contraception during treatment and for at least 3 months and 8 months after the final dose of vismodegib and sonidegib, respectively.37,38
Laboratory abnormalities commonly associated with SHH inhibitors include elevated hepatic enzymes, particularly with vismodegib, and elevated creatine kinase levels, particularly with sonidegib.28,39 Other laboratory abnormalities that can occur include hypercholesterolemia, hypercreatininemia, hyperglycemia, and increased serum lipase levels.19,28 Although these laboratory abnormalities usually are asymptomatic and self-limiting, regular monitoring should be performed.
There also is concern that SHH inhibitors may induce the development of cSCC. A case-control study of 55 cases and 125 control patients found an increased risk for cSCC in those previously treated with vismodegib, with a hazard ratio of 8.12.40 However, a subsequent retrospective cohort study of 1675 patients with BCC failed to find any association with cSCC among those treated with vismodegib compared to those who received standard surgical therapy.41 Clinical data for sonidegib are lacking, but the BOLT trial found that cSCC occurred in 3 patients receiving treatment with the SHH inhibitor.18 Thus, further studies are needed to more thoroughly assess this concern. Close monitoring for cSCC may be warranted in patients prescribed SHH inhibitors at this time.
Cemiplimab has demonstrated an acceptable safety profile and is generally well tolerated. In the phase 2 trial of cemiplimab for cSCC, approximately 5% of patients discontinued treatment because of adverse effects. The most commonly reported side effects of cemiplimab were diarrhea (27%), fatigue (24%), nausea (17%), constipation (15%), and rash (15%).23 In the phase 2 trial for laBCC, grade 3 or 4 adverse events occurred in 48% of patients, with hypertension (5%) being the most common.26 Although rare, immune-mediated adverse reactions also can occur, given the mechanism of action of ICIs. These side effects, ranging in severity from mild to fatal, include pneumonitis, colitis, hepatitis, nephritis, myocarditis, and hypophysitis. Therefore, close monitoring for these immune-mediated reactions is critical, but most can be managed with corticosteroids or treatment interruption if they occur.42,43
No absolute contraindications exist for cemiplimab; however, extreme caution should be taken in immunosuppressed individuals, such as solid organ transplant recipients and those with chronic lymphocytic leukemia (CLL), as safety data are limited in these patients.44,45 Although small retrospective studies have reported reasonable tolerability in solid organ transplant recipients treated with ICIs, an allograft rejection rate of 41% was found in a meta-analysis of 64 patients.46-48 In CLL patients with keratinocyte carcinomas, ICIs have been safely used and have even demonstrated efficacy for CLL in some cases.49-52
Alternative Dosing
The side effects of SHH inhibitors have led to alternative dosing strategies to prevent medication discontinuation and improve adherence. In patients with basal cell nevus syndrome, multimonth drug holidays have been shown to increase drug tolerability without compromising efficacy.35,36 Weekly intermittent dosing regimens of vismodegib ranging from 1 week on followed by 1 to 3 weeks off demonstrated efficacy in a retrospective study of 7 patients with advanced BCC.53 All 7 patients experienced improvement in their BCCs, with 3 patients experiencing CR. Importantly, treatment-related adverse effects were mild and well tolerated, with no patients terminating the medication.53 Two other retrospective case series of patients with advanced BCC treated with vismodegib reported similar findings for those placed on an intermittent dosing schedule ranging from once every other day to once per week.54,55
In the large phase 2 randomized trial known as MIKIE, 2 different intermittent dosing regimens of 150 mg vismodegib daily for patients with multiple BCCs were found to have good activity and tolerability.56 The first group (n=116) received vismodegib for 12 weeks, then 3 rounds of 8 weeks of placebo, followed by 12 weeks of vismodegib; there was a 63% reduction in clinically evident BCCs after 73 weeks. The second group (n=113) received the medication for 24 weeks, then 3 rounds of 8 weeks of placebo, followed by 8 weeks of vismodegib; there was a 54% reduction at the end of 73 weeks.56 Subsequent analyses found improvements in health-related quality-of-life outcomes that were similar for both groups.57
Consequently, alternative dosing schedules appear to be a viable option for patients at risk of discontinuing treatment because of adverse effects, and current data support the recently approved recommendations of dose interruptions of up to 8 weeks to manage adverse effects in patients with laBCC or mBCC.58 Nevertheless, further clinical studies are required to determine the optimal intermittent dosing regimen for patients treated with SHH inhibitors.
Neoadjuvant Administration
Recently, vismodegib has been studied as a neoadjuvant therapy for BCC with promising results. Several small retrospective studies and case reports have documented successful treatment of both operable and inoperable periocular laBCC, with preservation of the eye in all patients.59-61 An open-label trial of 15 patients with advanced BCC who received neoadjuvant vismodegib for 3 to 6 months prior to surgical excision reported a mean reduction of 35% in the final surgical defect size, with no recurrence at 22 months.62,63 The latest and largest study performed was a phase 2 open-label trial known as VISMONEO, where 44 of 55 laBCC patients (80%) receiving neoadjuvant vismodegib for a mean duration of 6 months (range, 4–10 months) achieved the primary end point of tumor surgical downstaging.64 Of the 44 patients who had tumor downstaging, 27 (61%) experienced histologically proven CRs. Additionally, a 66% reduction in the average target lesion size was reported in this group compared to29% in the 11 patients who did not have tumor downstaging (P=.0002).64 Thus, SHH inhibitors may hold an important neoadjuvant role in the treatment of BCC by decreasing surgical defect size and allowing for surgical management of previously inoperable cases.
Synergism With Radiation
Preliminary data suggest SHH inhibitors may help potentiate the effects of radiation therapy for the treatment of BCC. Currently, the evidence primarily is limited to case studies, with several reports describing complete remission in patients with advanced BCCs who were considered unsuitable candidates for surgery. In these cases, vismodegib was administered either prior to or concurrently with radiation treatment.65-69 An in vitro study also documented the radiation-sensitizing effects of vismodegib in a BCC cell line.70 Recently, a phase 2 trial (ClinicalTrials.gov identifier NCT01835626) evaluating the concurrent use of vismodegib and radiotherapy for patients with advanced BCC was completed, but data has yet to be published.
Synergism With and Benefit of Antifungal Therapy
The antifungal drug itraconazole is a potent inhibitor of the SHH pathway and may have an adjunctive role in the treatment of BCC. Similar to vismodegib and sonidegib, itraconazole acts as a direct antagonist of SMO. However, it is thought to bind to a distinct site on SMO.71,72 An open-label, exploratory phase 2 trial of 19 patients with BCC found that oral itraconazole 200 to 400 mg daily decreased tumor proliferative index by 45% (P=.04), as measured by Ki-67; SHH activity by 65% (P=.03), as measured by GLI1 messenger RNA; and mean tumor area by 24%.73 In a case series of 5 patients with mBCC refractory to conventional SHH inhibitor therapy, combined treatment with itraconazole and arsenic trioxide resulted in stable disease and a 75% reduction in SHH activity (P<.001).74 One case report documented tumor regression leading to stable disease for 15 months in a patient with laBCC treated with itraconazole monotherapy due to being unable to afford vismodegib or sonidegib. However, within 2 months of treatment discontinuation, the lesion progressed considerably.75 The efficacy of a topical formulation of itraconazole also has been tested in an open-label, placebo-controlled phase 2 trial, but no benefit was observed.76
Posaconazole is a second-generation antifungal agent that may serve as a potential alternative to itraconazole.77 Although clinical data are lacking, a basic science study found that posaconazole could inhibit the growth of SHH-dependent BCC in vivo (in mice).78 Furthermore, posaconazole has demonstrated a better safety profile with fewer and more mild side effects than itraconazole and does not require dose adjustment for those with hepatic or renal failure.79,80 Thus, posaconazole may be a safer alternative to itraconazole for the treatment of BCC. Further clinical studies are needed to elucidate the potential synergistic effects of these antifungal agents with the 2 currently approved SHH inhibitors for the treatment of advanced BCC.
Drug Resistance
Treatment resistance to SHH inhibitors, though uncommon, is a growing concern. Acquired mutations in the SMO binding site or downstream mediators of the SHH pathway have been shown to confer resistance to vismodegib and sonidegib.72,81-83 In addition, it appears that there may be shared resistance among the drugs in this class. One study assessing the efficacy of sonidegib in 9 patients with laBCC resistant to vismodegib found that these patients also did not respond to sonidegib.84 Interestingly, 1 case report documented tumor regression of an intracranial BCC in a patient treated with sonidegib and itraconazole after failure with vismodegib.85 An in vitro study also found that itraconazole maintained SHH inhibitory activity for all drug-resistant SMO mutations that have been reported.72 Therefore, itraconazole monotherapy or combination therapy with a canonical SHH inhibitor may be considered for patients with recalcitrant BCC and warrants further investigation.
Taladegib is a newly developed SMO inhibitor that may serve as another promising alternative for patients who develop resistance to vismodegib or sonidegib. A phase 1 trial of taladegib for advanced BCC found an ORR of 69% (11/16) in the SHH inhibitor–naïve group and an ORR of 36% (11/32) in the group previously treated with a SHH inhibitor.86 Additionally, the safety profile and frequency of adverse effects appear to be similar to those associated with vismodegib and sonidegib.86,87 Unfortunately, no clinical trials evaluating taladegib for BCC are ongoing or in development at this time.
Recurrence
There appears to be a relatively high rate of recurrence for BCC patients who achieve a CR to SHH inhibitors. In a retrospective study of 116 laBCC patients who experienced a CR after vismodegib therapy, 54 patients (47%) relapsed at 36 months. Among the 54 patients that relapsed, 27 were re-treated with vismodegib, which resulted in an ORR of 85% (23/27), a CR rate of 37% (10/27), and a PR rate of 48% (13/27).88 Another retrospective study of 35 laBCC patients who relapsed after vismodegib treatment reported a 31% (11/35) clinical recurrence rate at 6-month follow-up.89 An observational retrospective study also assessed the efficacy of SHH inhibitor maintenance therapy for advanced BCC patients who achieved a CR.90 In the study, 27 (64%) patients received a maintenance dose of 150 mg vismodegib once per week for 1 year, while 15 (36%) patients decided not to take a maintenance dose following CR of their BCC. All patients who took the maintenance therapy did not experience clinical recurrence at 1-year follow-up, whereas 26% of patients not on the maintenance dose relapsed.90 Consequently, these results indicate that BCC recurrence is frequent after SHH inhibitor therapy and highlights the importance of close surveillance after CR is attained. Nevertheless, most patients still respond to treatment with SHH inhibitors after relapsing, and intermittent maintenance doses may be an effective means to reduce risk of recurrence.
Conclusion
Vismodegib and sonidegib are SHH inhibitors approved for the treatment of laBCC and mBCC. Cemiplimab is now also approved for patients who do not respond to SHH inhibitors or for whom SHH inhibitors are not tolerable. Although these systemic targeted therapies can lead to notable tumor shrinkage and even complete regression in some patients, recurrence is common, and adverse effects may limit their use. Drug resistance is an emerging issue that requires additional examination. Further clinical studies are needed to determine which patients are likely to respond to these targeted treatments.
Various intermittent and maintenance drug regimens should be evaluated for their potential to mitigate adverse effects and reduce risk of recurrence, respectively. The synergistic effects of these medications with other therapies as well as their neoadjuvant and adjuvant roles should be further investigated. For example, administration of an SHH inhibitor prior to surgical excision of a BCC may allow for a smaller surgical defect size, thereby improving cosmetic and functional outcomes. Moreover, these systemic targeted medications may allow for previously inoperable tumors to become amenable to surgical treatment.
Although SHH inhibitors and PD-1 inhibitors represent a major advancement in the field of oncodermatology, real-world efficacy and safety data in the upcoming years will be important for elucidating their true benefit for patients with BCC.
- Rogers HW, Weinstock MA, Feldman SR, et al. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. population, 2012. JAMA Dermatol. 2015;151:1081-1086.
- Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80:303-317.
- Rees JR, Zens MS, Celaya MO, et al. Survival after squamous cell and basal cell carcinoma of the skin: a retrospective cohort analysis. Int J Cancer. 2015;137:878-884.
- Kasumagic-Halilovic E, Hasic M, Ovcina-Kurtovic N. A clinical study of basal cell carcinoma. Med Arch. 2019;73:394-398.
- Goldenberg G, Karagiannis T, Palmer JB, et al. Incidence and prevalence of basal cell carcinoma (BCC) and locally advanced BCC (LABCC) in a large commercially insured population in the United States: a retrospective cohort study. J Am Acad Dermatol. 2016;75:957.e952-966.e952.
- Laga AC, Schaefer IM, Sholl LM, et al. Metastatic basal cell carcinoma. Am J Clin Pathol. 2019;152:706-717.
- Rimkus TK, Carpenter RL, Qasem S, et al. Targeting the sonic hedgehog signaling pathway: review of smoothened and GLI inhibitors. Cancers (Basel). 2016;8:22.
- Burova E, Hermann A, Waite J, et al. Characterization of the anti–PD-1 antibody REGN2810 and its antitumor activity in human PD-1 knock-in mice. Mol Cancer Ther. 2017;16:861-870.
- Bhardwaj G, Murdoch B, Wu D, et al. Sonic hedgehog induces the proliferation of primitive human hematopoietic cells via BMP regulation. Nat Immunol. 2001;2:172-180.
- Paladini RD, Saleh J, Qian C, et al. Modulation of hair growth with small molecule agonists of the hedgehog signaling pathway. J Invest Dermatol. 2005;125:638-646.
- Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164-1172.
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-2179.
- Sekulic A, Migden MR, Basset-Seguin N, et al. Long-term safety and efficacy of vismodegib in patients with advanced basal cell carcinoma: final update of the pivotal ERIVANCE BCC study. BMC Cancer. 2017;17:332.
- Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
- Cozzani R, Del Aguila R, Carrizo M, et al. Efficacy and safety profile of vismodegib in a real-world setting cohort of patients with advanced basal cell carcinoma in Argentina. Int J Dermatol. 2020;59:627-632.
- Spallone G, Sollena P, Ventura A, et al. Efficacy and safety of vismodegib treatment in patients with advanced basal cell carcinoma and multiple comorbidities. Dermatol Ther. 2019;32:E13108.
- Fosko SW, Chu MB, Armbrecht E, et al. Efficacy, rate of tumor response, and safety of a short course (12-24 weeks) of oral vismodegib in various histologic subtypes (infiltrative, nodular, and superficial) of high-risk or locally advanced basal cell carcinoma, in an open-label, prospective case series clinical trial. J Am Acad Dermatol. 2020;82:946-954.
- Migden MR, Guminski A, Gutzmer R, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): a multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16:716-728.
- Dummer R, Guminksi A, Gutzmer R, et al. Long-term efficacy and safety of sonidegib in patients with advanced basal cell carcinoma: 42-month analysis of the phase II randomized, double-blind BOLT study. Br J Dermatol. 2020;182:1369-1378.
- Dummer R, Ascierto PA, Basset-Seguin N, et al. Sonidegib and vismodegib in the treatment of patients with locally advanced basal cell carcinoma: a joint expert opinion. J Eur Acad Dermatol Venereol. 2020;34:1944-1956.
- Xie P, Lefrançois P. Efficacy, safety, and comparison of sonic hedgehog inhibitors in basal cell carcinomas: a systematic review and meta-analysis. J Am Acad Dermatol. 2018;79:1089-1100.e1017.
- Gentzler R, Hall R, Kunk PR, et al. Beyond melanoma: inhibiting the PD-1/PD-L1 pathway in solid tumors. Immunotherapy. 2016;8:583-600.
- Guminski AD, Lim AML, Khushalani NI, et al. Phase 2 study of cemiplimab, a human monoclonal anti-PD-1, in patients (pts) with metastatic cutaneous squamous cell carcinoma (mCSCC; group 1): 12-month follow-up [abstract]. J Clin Oncol. 2019;37(15 suppl):9526.
- Grob JJ, Gonzalez Mendoza R, Basset-Seguin N, et al. Pembrolizumab for recurrent/metastatic cutaneous squamous cell carcinoma (cSCC): efficacy and safety results from the phase II KEYNOTE-629 study [abstract]. Ann Oncol. 2019;30 (suppl 5):v908.
- Maubec E, Boubaya M, Petrow P, et al. Pembrolizumab as first-line therapy in patients with unresectable cutaneous squamous cell carcinoma (cSCC): phase 2 results from CARSKIN [abstract]. J Clin Oncol. 2019;37(15 suppl):9547.
- Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22:848-857.
- Carpenter RL, Ray H. Safety and tolerability of sonic hedgehog pathway inhibitors in cancer. Drug Saf. 2019;42:263-279.
- Villani A, Fabbrocini G, Costa C, et al. Sonidegib: safety and efficacy in treatment of advanced basal cell carcinoma. Dermatol Ther (Heidelb). 2020;10:401-412.
- Wright A, Sluka KA. Nonpharmacological treatments for musculoskeletal pain. Clin J Pain. 2001;17:33-46.
- Ally MS, Tang JY, Lindgren J, et al. Effect of calcium channel blockade on vismodegib-induced muscle cramps. JAMA Dermatol. 2015;151:1132-1134.
- Yang X, Thai K-E. Treatment of permanent chemotherapy-induced alopecia with low dose oral minoxidil. Australas J Dermatol. 2016;57:e130-e132.
- Ferguson JS, Hannam S, Toholka R, et al. Hair loss and hedgehog inhibitors: a class effect? Br J Dermatol. 2015;173:262-264.
- Kumbargere Nagraj S, George RP, Shetty N, et al. Interventions for managing taste disturbances. Cochrane Database Syst Rev. 2017;12:CD010470.
- Jacobsen AA, Kydd AR, Strasswimmer J. Practical management of the adverse effects of hedgehog pathway inhibitor therapy for basal cell carcinoma. J Am Acad Dermatol. 2017;76:767-768.
- Ally MS, Tang JY, Joseph T, et al. The use of vismodegib to shrink keratocystic odontogenic tumors in patients with basal cell nevus syndrome. JAMA Dermatol. 2014;150:542-545.
- Yang X, Dinehart SM. Intermittent vismodegib therapy in basal cell nevus syndrome. JAMA Dermatol. 2016;152:223-224.
- Erivedge. Prescribing information. Genentech; 2015.
- Odomzo. Prescribing information. Novartis; 2015.
- Ventarola DJ, Silverstein DI. Vismodegib-associated hepatotoxicity: a potential side effect detected in postmarketing surveillance. J Am Acad Dermatol. 2014;71:397-398.
- Mohan SV, Chang J, Li S, et al. Increased risk of cutaneous squamous cell carcinoma after vismodegib therapy for basal cell carcinoma. JAMA Dermatol. 2016;152:527-532.
- Bhutani T, Abrouk M, Sima CS, et al. Risk of cutaneous squamous cell carcinoma after treatment of basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2017;77:713-718.
- Morgado M, Plácido A, Morgado S, et al. Management of the adverse effects of immune checkpoint inhibitors. Vaccines (Basel). 2020;8:575.
- Martins F, Sofiya L, Sykiotis GP, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16:563-580.
- Ntsethe A, Dludla PV, Nyambuya TM, et al. The impact of immune checkpoint inhibitors in patients with chronic lymphocytic leukemia (CLL): a protocol for a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99:E21167.
- Johnson DB, Sullivan RJ, Menzies AM. Immune checkpoint inhibitors in challenging populations. Cancer. 2017;123:1904-1911.
- Tsung I, Worden FP, Fontana RJ. Safety and efficacy of checkpoint inhibitors in solid organ transplant recipients with cutaneous squamous cell carcinoma [abstract]. J Clin Oncol. 2020;38(15 suppl):E22014.
- Owoyemi I, Vaughan LE, Costello CM, et al. Clinical outcomes of solid organ transplant recipients with metastatic cancers who are treated with immune checkpoint inhibitors: a single-center analysis. Cancer. 2020;126:4780-4787.
- Kumar V, Shinagare AB, Rennke HG, et al. The safety and efficacy of checkpoint inhibitors in transplant recipients: a case series and systematic review of literature. Oncologist. 2020;25:505-514.
- Arenbergerova M, Fialova A, Arenberger P, et al. Killing two birds with one stone: response to pembrolizumab in a patient with metastatic melanoma and B-cell chronic lymphocytic leukaemia. J Eur Acad Dermatol Venereol. 2018;32:E72-E74.
- Archibald WJ, Meacham PJ, Williams AM, et al. Management of melanoma in patients with chronic lymphocytic leukemia. Leuk Res. 2018;71:43-46.
- Ding W, LaPlant BR, Call TG, et al. Pembrolizumab in patients with CLL and Richter transformation or with relapsed CLL. Blood. 2017;129:3419-3427.
- Leiter U, Loquai C, Reinhardt L, et al. Immune checkpoint inhibition therapy for advanced skin cancer in patients with concomitant hematological malignancy: a retrospective multicenter DeCOG study of 84 patients. J Immunother Cancer. 2020;8:E000897.
- Becker LR, Aakhus AE, Reich HC, et al. A novel alternate dosing of vismodegib for treatment of patients with advanced basal cell carcinomas. JAMA Dermatol. 2017;153:321-322.
- Woltsche N, Pichler N, Wolf I, et al. Managing adverse effects by dose reduction during routine treatment of locally advanced basal cell carcinoma with the hedgehog inhibitor vismodegib: a single centre experience. J Eur Acad Dermatol Venereol. 2019;33:E144-E145.
- Wong C, Poblete-Lopez C, Vidimos A. Comparison of daily dosing versus Monday through Friday dosing of vismodegib for locally advanced basal cell carcinoma and basal cell nevus syndrome: a retrospective case series. J Am Acad Dermatol. 2020;82:1539-1542.
- Dréno B, Kunstfeld R, Hauschild A, et al. Two intermittent vismodegib dosing regimens in patients with multiple basal-cell carcinomas (MIKIE): a randomised, regimen-controlled, double-blind, phase 2 trial. Lancet Oncol. 2017;18:404-412.
- Schadendorf D, Hauschild A, Fosko S, et al. Quality-of-life analysis with intermittent vismodegib regimens in patients with multiple basal cell carcinomas: patient-reported outcomes from the MIKIE study. J Eur Acad Dermatol Venereol. 2020;34:E526-E529.
- Chanu P, Musib L, Wang X, et al. Vismodegib efficacy in advanced basal cell carcinoma maintained with 8-week dose interruptions: a model-based evaluation. J Invest Dermatol. 2021;141:930-933.
- Su MG, Potts LB, Tsai JH. Treatment of periocular basal cell carcinoma with neoadjuvant vismodegib. Am J Ophthalmol Case Rep. 2020;19:100755.
- González AR, Etchichury D, Gil ME, et al. Neoadjuvant vismodegib and Mohs micrographic surgery for locally advanced periocular basal cell carcinoma. Ophthalmic Plast Reconstr Surg. 2019;35:56-61.
- Sagiv O, Nagarajan P, Ferrarotto R, et al. Ocular preservation with neoadjuvant vismodegib in patients with locally advanced periocular basal cell carcinoma. Br J Ophthalmol. 2019;103:775-780.
- Ally MS, Aasi S, Wysong A, et al. An investigator-initiated open-label clinical trial of vismodegib as a neoadjuvant to surgery for high-risk basal cell carcinoma. J Am Acad Dermatol. 2014;71:904-911.e1.
- Kwon GP, Ally MS, Bailey-Healy I, et al. Update to an open-label clinical trial of vismodegib as neoadjuvant before surgery for high-risk basal cell carcinoma (BCC). J Am Acad Dermatol. 2016;75:213-215.
- Mortier L, Bertrand N, Basset-Seguin N, et al. Vismodegib in neoadjuvant treatment of locally advanced basal cell carcinoma: first results of a multicenter, open-label, phase 2 trial (VISMONEO study) [abstract]. J Clin Oncol. 2018;36(15 suppl):9509.
- Strasswimmer JM. Potential synergy of radiation therapy with vismodegib for basal cell carcinoma. JAMA Dermatol. 2015;151:925-926.
- Gathings RM, Orscheln CS, Huang WW. Compassionate use of vismodegib and adjuvant radiotherapy in the treatment of multiple locally advanced and inoperable basal cell carcinomas and squamous cell carcinomas of the skin. J Am Acad Dermatol. 2014;70:E88-E89.
- Franco AI, Eastwick G, Farah R, et al. Upfront radiotherapy with concurrent and adjuvant vismodegib is effective and well-tolerated in a patient with advanced, multifocal basal cell carcinoma. Case Rep Dermatol Med. 2018;2018:2354146.
- Pollom EL, Bui TT, Chang AL, et al. Concurrent vismodegib and radiotherapy for recurrent, advanced basal cell carcinoma. JAMA Dermatol. 2015;151:998-1001.
- Janela-Lapert R, Dubray B, Duval-Modeste A, et al. Treatment of advanced basal cell carcinoma with vismodegib followed by radiotherapy [in French]. Ann Dermatol Venereol. 2020;147:780-782.
- Hehlgans S, Booms P, Güllülü Ö, et al. Radiation sensitization of basal cell and head and neck squamous cell carcinoma by the hedgehog pathway inhibitor vismodegib. Int J Mol Sci. 2018;19:2485.
- Kim J, Tang JY, Gong R, et al. Itraconazole, a commonly used antifungal that inhibits hedgehog pathway activity and cancer growth. Cancer Cell. 2010;17:388-399.
- Kim J, Aftab BT, Tang JY, et al. Itraconazole and arsenic trioxide inhibit hedgehog pathway activation and tumor growth associated with acquired resistance to smoothened antagonists. Cancer Cell. 2013;23:23-34.
- Kim DJ, Kim J, Spaunhurst K, et al. Open-label, exploratory phase II trial of oral itraconazole for the treatment of basal cell carcinoma. J Clin Oncol. 2014;32:745-751.
- Ally MS, Ransohoff K, Sarin K, et al. Effects of combined treatment with arsenic trioxide and itraconazole in patients with refractory metastatic basal cell carcinoma. JAMA Dermatol. 2016;152:452-456.
- Cia˛z˙yn´yska M, Narbutt J, Skibin´ska M, et al. Itraconazole—a new player in the therapy of advanced basal cell carcinoma: a case report. JCO Oncol Pract. 2020;16:837-838.
- Sohn GK, Kwon GP, Bailey-Healy I, et al. Topical itraconazole for the treatment of basal cell carcinoma in patients with basal cell nevus syndrome or high-frequency basal cell carcinomas: a phase 2, open-label, placebo-controlled trial. JAMA Dermatol. 2019;155:1078-1080.
- Lass-Flörl C. Triazole antifungal agents in invasive fungal infections: a comparative review. Drugs. 2011;71:2405-2419.
- Chen B, Trang V, Lee A, et al. Posaconazole, a second-generation triazole antifungal drug, inhibits the hedgehog signaling pathway and progression of basal cell carcinoma. Mol Cancer Ther. 2016;15:866-876.
- Katragkou A, Tsikopoulou F, Roilides E, et al. Posaconazole: when and how? the clinician’s view. Mycoses. 2012;55:110-122.
- Raad II, Graybill JR, Bustamante AB, et al. Safety of long-term oral posaconazole use in the treatment of refractory invasive fungal infections. Clin Infect Dis. 2006;42:1726-1734.
- Atwood SX, Sarin KY, Whitson RJ, et al. Smoothened variants explain the majority of drug resistance in basal cell carcinoma. Cancer Cell. 2015;27:342-353.
- Sun Q, Atzmony L, Zaki T, et al. Clues to primary vismodegib resistance lie in histology and genetics. J Clin Pathol. 2020;73:678-680.
- Verkouteren BJA, Wakkee M, van Geel M, et al. Molecular testing in metastatic basal cell carcinoma. J Am Acad Dermatol. 2021;85:1135-1142.
- Danial C, Sarin KY, Oro AE, et al. An investigator-initiated open-label trial of sonidegib in advanced basal cell carcinoma patients resistant to vismodegib. Clin Cancer Res. 2016;22:1325-1329.
- Yoon J, Apicelli AJ 3rd, Pavlopoulos TV. Intracranial regression of an advanced basal cell carcinoma using sonidegib and itraconazole after failure with vismodegib. JAAD Case Rep. 2017;4:10-12.
- Bendell J, Andre V, Ho A, et al. Phase I study of LY2940680, a Smo antagonist, in patients with advanced cancer including treatment-naïve and previously treated basal cell carcinoma. Clin Cancer Res. 2018;24:2082-2091.
- Ueno H, Kondo S, Yoshikawa S, et al. A phase I and pharmacokinetic study of taladegib, a Smoothened inhibitor, in Japanese patients with advanced solid tumors. Invest New Drugs. 2018;36:647-656.
- Herms F, Lambert J, Grob JJ, et al. Follow-up of patients with complete remission of locally advanced basal cell carcinoma after vismodegib discontinuation: a multicenter French study of 116 patients. J Clin Oncol. 2019;37:3275-3282.
- Villani A, Megna M, Fabbrocini G, et al. Long-term efficacy of vismodegib after its withdrawal and patients’ health-related quality of life using the Dermatology Life Quality Index (DLQI). Dermatol Ther (Heidelb). 2019;9:719-724.
- Scalvenzi M, Cappello M, Costa C, et al. Low-dose vismodegib as maintenance therapy after locally advanced basal cell carcinoma complete remission: high efficacy with minimal toxicity. Dermatol Ther (Heidelb). 2020;10:465-468.
Basal cell carcinoma (BCC) is the most common keratinocyte carcinoma and affects more than 3 million individuals per year in the United States.1 Approximately 40% of patients diagnosed with BCC will develop another BCC within 5 years of the initial diagnosis.2 Most cases are successfully treated with surgical excision and occasionally topical therapy or radiotherapy. Despite the high cure rate with conventional treatments, BCC can recur and can cause substantial destruction of the surrounding tissue if left untreated.3-5 In some instances, BCC can even metastasize and lead to death.6 For patients who are poor candidates for surgical or topical treatment modalities because of locally advanced BCC (laBCC) or metastatic BCC (mBCC), systemic treatment may be indicated. Vismodegib, sonidegib, and cemiplimab are the only systemic medications approved by the US Food and Drug Administration (FDA) for the treatment of laBCC and/or mBCC. Vismodegib and sonidegib target the sonic hedgehog (SHH) signaling pathway that is abnormally activated in more than 90% of BCCs.7 Cemiplimab is an immune checkpoint inhibitor (ICI) that targets the programmed cell death protein 1 (PD-1) receptor.8 Herein, we review the clinical utility of these medications and their evolving roles in the treatment of BCC.
SHH Pathway Inhibitors
The SHH pathway is a key regulator of cell proliferation and differentiation during embryogenesis.7 During adulthood, SHH signaling decreases but still plays an important role in stem cell activation and in regulation of the hair follicle growth cycle.9,10 However, de novo mutations in the genes that comprise the SHH pathway can result in aberrant constitutive activation, leading to unrestricted cell proliferation. Genetic mutations resulting in activation of Smoothened (SMO), a G-protein–coupled receptor involved in the signal transduction and propagation of the SHH pathway, have been implicated in the pathogenesis of BCC. Inactivating mutations also are commonly observed in patched homolog 1, an upstream cell-surface protein that inhibits SMO.7 The mechanism by which vismodegib and sonidegib, 2 of the FDA-approved oral medications for the treatment of advanced BCC, block the SHH pathway is through the selective inhibition of SMO.7,11
Vismodegib first received FDA approval in 2012 for the treatment of laBCC and mBCC after initial results from the pivotal ERIVANCE phase 2 trial demonstrated an objective response rate (ORR) of 43% (27/63) and 30% (10/33) in patients with locally advanced and metastatic disease, respectively. In this single-arm study, all enrolled patients (63 with laBCC and 33 with mBCC) received 150 mg of oral vismodegib daily.12 Updated results at 39 months demonstrated improved ORRs of 60% (38/63) and 48% (16/33) for the laBCC and mBCC groups, respectively. A complete response (CR) and partial response (PR) were observed in 32% (n=20) and 29% (n=18) of patients with laBCC, respectively.13 These results have been confirmed in subsequent studies, including the large international open-label trial known as STEVIE, with ORRs of 68.5% for 1119 cases of laBCC and 37% for 96 cases of mBCC.14-17 The CR and PR rates were 33% and 35%, respectively, for the laBCC group. The CR and PR rates for the mBCC group were 5% and 32%, respectively.14
The FDA approval of sonidegib for laBCC—but not mBCC—occurred in 2015 after the pivotal BOLT randomized phase 2 trial demonstrated an initial ORR of 43% (18/42) for laBCC and 15% (2/13) for mBCC after administration of 200 mg of sonidegib daily.18 A final follow-up analysis at 42 months resulted in ORRs of 56% (37/66) and 8% (1/13) for the laBCC and mBCC groups, respectively.19 Additionally, improved efficacy was not observed in the 151 patients who were randomized to receive treatment with the higher 800-mg dose; however, they did experience a higher incidence of adverse events.18,19
Currently, the true clinical differences between vismodegib and sonidegib remain uncertain, as no head-to-head trials have been conducted. Moreover, direct comparison of the data from the ERIVANCE and BOLT trials is challenging owing to fundamental differences in methodologic design, including the criteria used to assess BCC severity. The ERIVANCE trial utilized the conventional Response Evaluation Criteria in Solid Tumors (RECIST), while BOLT used the rigorous modified RECIST. However, an expert consensus study attempted to compare the 2 trials by modifying the outcomes from BOLT with the former RECIST criteria. The expert group found that the 2 SHH inhibitors had comparable efficacy and adverse event profiles.20 Nevertheless, a recent meta-analysis found that although ORRs for laBCC were similar between the 2 drugs, the CR rate for vismodegib was 31% compared with 3% for sonidegib. Additionally, for mBCC, they reported the ORR of vismodegib to be 2.7 times higher than that of sonidegib (39% vs 15%).21
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors have successfully been utilized in the treatment of cutaneous squamous cell carcinoma (cSCC); however, their use for treating BCC has been limited until recently.22-25 In February 2021, cemiplimab became the first and only ICI approved for the treatment of laBCC and mBCC in patients who did not respond to or were intolerant to prior SHH inhibitor therapy.26 Cemiplimab—a human monoclonal antibody against the PD-1 receptor expressed on T cells—blocks its interaction with programmed cell death ligand 1 and programmed cell death ligand 2 present on tumor cells. The blockade of the PD-1 pathway releases the inhibition of the antitumor immune response and enables appropriate cytotoxic T-cell activity to occur.8
The FDA approval of cemiplimab for the treatment of advanced BCC was based on an open-label, multicenter, single-arm phase 2 trial (NCT03132636) evaluating 84 patients with laBCC refractory or intolerant to SHH inhibitor therapy.26 Patients received an intravenous infusion of cemiplimab 350 mg every 3 weeks for up to 93 weeks or until disease progression or unacceptable toxicity. An ORR of 31% (26/84) was observed with a CR and PR of 6% (5/84) and 25% (21/84), respectively. The median duration of follow-up was 15 months.26 Given the clinically meaningful results of this trial, investigating the efficacy of other PD-1 inhibitors, such as pembrolizumab and nivolumab, for treatment of advanced BCC may prove worthwhile.
Adverse Effects of Systemic Treatments
The 2 approved SHH inhibitors—vismodegib and sonidegib—appear to have similar side-effect profiles, with the most common adverse effects being muscle spasms, dysgeusia, alopecia, nausea, vomiting, diarrhea, weight loss, and fatigue.20,21,27 These side effects occur at high frequencies (>40%) for both SHH inhibitors and often lead to discontinuation of the medication.21 Rates of treatment discontinuation range from 15% to 50% on average.12-14,18 Fortunately, the majority of these adverse effects do not appear to increase in severity or frequency with prolonged use of these medications.14,16,28
Various conservative and pharmacologic measures can be implemented to help manage side effects. For muscle spasms, which are the most commonly reported adverse effect, supplementation with magnesium, transcutaneous electrical nerve stimulation, acupuncture, massages, stretching, and thermal compresses can potentially be beneficial.29 Calcium channel blockers also may be effective, as one small prospective cohort study reported a reduction in the frequency of muscle cramps with amlodipine 10 mg daily.30 For alopecia, which typically is reversible and caused by SHH inhibition of the normal hair cycle, minoxidil theoretically can help, as it reduces telogen arrest and extends the anagen growth phase.31,32 Although usually mild and self-limiting, management of dysgeusia, weight loss, and gastrointestinal upset often can be managed with dietary changes, such as smaller, more frequent meals.33,34 Finally, alternative dosing strategies and drug holidays have been employed to mitigate these side effects and increase drug tolerability.35,36 These are discussed in the Alternative Dosing section.
Given the essential role of the SHH pathway in embryologic development, SHH inhibitors carry a black box warning of embryofetal teratogenicity and are contraindicated in females who are pregnant or breastfeeding. For females of reproductive potential, verification of pregnancy status should be performed prior to initiating treatment with an SHH inhibitor. These patients should be counseled on the use of contraception during treatment and for at least 24 months and 20 months after cessation of vismodegib and sonidegib, respectively.27,37,38 Male patients, even after a vasectomy, should use barrier contraception during treatment and for at least 3 months and 8 months after the final dose of vismodegib and sonidegib, respectively.37,38
Laboratory abnormalities commonly associated with SHH inhibitors include elevated hepatic enzymes, particularly with vismodegib, and elevated creatine kinase levels, particularly with sonidegib.28,39 Other laboratory abnormalities that can occur include hypercholesterolemia, hypercreatininemia, hyperglycemia, and increased serum lipase levels.19,28 Although these laboratory abnormalities usually are asymptomatic and self-limiting, regular monitoring should be performed.
There also is concern that SHH inhibitors may induce the development of cSCC. A case-control study of 55 cases and 125 control patients found an increased risk for cSCC in those previously treated with vismodegib, with a hazard ratio of 8.12.40 However, a subsequent retrospective cohort study of 1675 patients with BCC failed to find any association with cSCC among those treated with vismodegib compared to those who received standard surgical therapy.41 Clinical data for sonidegib are lacking, but the BOLT trial found that cSCC occurred in 3 patients receiving treatment with the SHH inhibitor.18 Thus, further studies are needed to more thoroughly assess this concern. Close monitoring for cSCC may be warranted in patients prescribed SHH inhibitors at this time.
Cemiplimab has demonstrated an acceptable safety profile and is generally well tolerated. In the phase 2 trial of cemiplimab for cSCC, approximately 5% of patients discontinued treatment because of adverse effects. The most commonly reported side effects of cemiplimab were diarrhea (27%), fatigue (24%), nausea (17%), constipation (15%), and rash (15%).23 In the phase 2 trial for laBCC, grade 3 or 4 adverse events occurred in 48% of patients, with hypertension (5%) being the most common.26 Although rare, immune-mediated adverse reactions also can occur, given the mechanism of action of ICIs. These side effects, ranging in severity from mild to fatal, include pneumonitis, colitis, hepatitis, nephritis, myocarditis, and hypophysitis. Therefore, close monitoring for these immune-mediated reactions is critical, but most can be managed with corticosteroids or treatment interruption if they occur.42,43
No absolute contraindications exist for cemiplimab; however, extreme caution should be taken in immunosuppressed individuals, such as solid organ transplant recipients and those with chronic lymphocytic leukemia (CLL), as safety data are limited in these patients.44,45 Although small retrospective studies have reported reasonable tolerability in solid organ transplant recipients treated with ICIs, an allograft rejection rate of 41% was found in a meta-analysis of 64 patients.46-48 In CLL patients with keratinocyte carcinomas, ICIs have been safely used and have even demonstrated efficacy for CLL in some cases.49-52
Alternative Dosing
The side effects of SHH inhibitors have led to alternative dosing strategies to prevent medication discontinuation and improve adherence. In patients with basal cell nevus syndrome, multimonth drug holidays have been shown to increase drug tolerability without compromising efficacy.35,36 Weekly intermittent dosing regimens of vismodegib ranging from 1 week on followed by 1 to 3 weeks off demonstrated efficacy in a retrospective study of 7 patients with advanced BCC.53 All 7 patients experienced improvement in their BCCs, with 3 patients experiencing CR. Importantly, treatment-related adverse effects were mild and well tolerated, with no patients terminating the medication.53 Two other retrospective case series of patients with advanced BCC treated with vismodegib reported similar findings for those placed on an intermittent dosing schedule ranging from once every other day to once per week.54,55
In the large phase 2 randomized trial known as MIKIE, 2 different intermittent dosing regimens of 150 mg vismodegib daily for patients with multiple BCCs were found to have good activity and tolerability.56 The first group (n=116) received vismodegib for 12 weeks, then 3 rounds of 8 weeks of placebo, followed by 12 weeks of vismodegib; there was a 63% reduction in clinically evident BCCs after 73 weeks. The second group (n=113) received the medication for 24 weeks, then 3 rounds of 8 weeks of placebo, followed by 8 weeks of vismodegib; there was a 54% reduction at the end of 73 weeks.56 Subsequent analyses found improvements in health-related quality-of-life outcomes that were similar for both groups.57
Consequently, alternative dosing schedules appear to be a viable option for patients at risk of discontinuing treatment because of adverse effects, and current data support the recently approved recommendations of dose interruptions of up to 8 weeks to manage adverse effects in patients with laBCC or mBCC.58 Nevertheless, further clinical studies are required to determine the optimal intermittent dosing regimen for patients treated with SHH inhibitors.
Neoadjuvant Administration
Recently, vismodegib has been studied as a neoadjuvant therapy for BCC with promising results. Several small retrospective studies and case reports have documented successful treatment of both operable and inoperable periocular laBCC, with preservation of the eye in all patients.59-61 An open-label trial of 15 patients with advanced BCC who received neoadjuvant vismodegib for 3 to 6 months prior to surgical excision reported a mean reduction of 35% in the final surgical defect size, with no recurrence at 22 months.62,63 The latest and largest study performed was a phase 2 open-label trial known as VISMONEO, where 44 of 55 laBCC patients (80%) receiving neoadjuvant vismodegib for a mean duration of 6 months (range, 4–10 months) achieved the primary end point of tumor surgical downstaging.64 Of the 44 patients who had tumor downstaging, 27 (61%) experienced histologically proven CRs. Additionally, a 66% reduction in the average target lesion size was reported in this group compared to29% in the 11 patients who did not have tumor downstaging (P=.0002).64 Thus, SHH inhibitors may hold an important neoadjuvant role in the treatment of BCC by decreasing surgical defect size and allowing for surgical management of previously inoperable cases.
Synergism With Radiation
Preliminary data suggest SHH inhibitors may help potentiate the effects of radiation therapy for the treatment of BCC. Currently, the evidence primarily is limited to case studies, with several reports describing complete remission in patients with advanced BCCs who were considered unsuitable candidates for surgery. In these cases, vismodegib was administered either prior to or concurrently with radiation treatment.65-69 An in vitro study also documented the radiation-sensitizing effects of vismodegib in a BCC cell line.70 Recently, a phase 2 trial (ClinicalTrials.gov identifier NCT01835626) evaluating the concurrent use of vismodegib and radiotherapy for patients with advanced BCC was completed, but data has yet to be published.
Synergism With and Benefit of Antifungal Therapy
The antifungal drug itraconazole is a potent inhibitor of the SHH pathway and may have an adjunctive role in the treatment of BCC. Similar to vismodegib and sonidegib, itraconazole acts as a direct antagonist of SMO. However, it is thought to bind to a distinct site on SMO.71,72 An open-label, exploratory phase 2 trial of 19 patients with BCC found that oral itraconazole 200 to 400 mg daily decreased tumor proliferative index by 45% (P=.04), as measured by Ki-67; SHH activity by 65% (P=.03), as measured by GLI1 messenger RNA; and mean tumor area by 24%.73 In a case series of 5 patients with mBCC refractory to conventional SHH inhibitor therapy, combined treatment with itraconazole and arsenic trioxide resulted in stable disease and a 75% reduction in SHH activity (P<.001).74 One case report documented tumor regression leading to stable disease for 15 months in a patient with laBCC treated with itraconazole monotherapy due to being unable to afford vismodegib or sonidegib. However, within 2 months of treatment discontinuation, the lesion progressed considerably.75 The efficacy of a topical formulation of itraconazole also has been tested in an open-label, placebo-controlled phase 2 trial, but no benefit was observed.76
Posaconazole is a second-generation antifungal agent that may serve as a potential alternative to itraconazole.77 Although clinical data are lacking, a basic science study found that posaconazole could inhibit the growth of SHH-dependent BCC in vivo (in mice).78 Furthermore, posaconazole has demonstrated a better safety profile with fewer and more mild side effects than itraconazole and does not require dose adjustment for those with hepatic or renal failure.79,80 Thus, posaconazole may be a safer alternative to itraconazole for the treatment of BCC. Further clinical studies are needed to elucidate the potential synergistic effects of these antifungal agents with the 2 currently approved SHH inhibitors for the treatment of advanced BCC.
Drug Resistance
Treatment resistance to SHH inhibitors, though uncommon, is a growing concern. Acquired mutations in the SMO binding site or downstream mediators of the SHH pathway have been shown to confer resistance to vismodegib and sonidegib.72,81-83 In addition, it appears that there may be shared resistance among the drugs in this class. One study assessing the efficacy of sonidegib in 9 patients with laBCC resistant to vismodegib found that these patients also did not respond to sonidegib.84 Interestingly, 1 case report documented tumor regression of an intracranial BCC in a patient treated with sonidegib and itraconazole after failure with vismodegib.85 An in vitro study also found that itraconazole maintained SHH inhibitory activity for all drug-resistant SMO mutations that have been reported.72 Therefore, itraconazole monotherapy or combination therapy with a canonical SHH inhibitor may be considered for patients with recalcitrant BCC and warrants further investigation.
Taladegib is a newly developed SMO inhibitor that may serve as another promising alternative for patients who develop resistance to vismodegib or sonidegib. A phase 1 trial of taladegib for advanced BCC found an ORR of 69% (11/16) in the SHH inhibitor–naïve group and an ORR of 36% (11/32) in the group previously treated with a SHH inhibitor.86 Additionally, the safety profile and frequency of adverse effects appear to be similar to those associated with vismodegib and sonidegib.86,87 Unfortunately, no clinical trials evaluating taladegib for BCC are ongoing or in development at this time.
Recurrence
There appears to be a relatively high rate of recurrence for BCC patients who achieve a CR to SHH inhibitors. In a retrospective study of 116 laBCC patients who experienced a CR after vismodegib therapy, 54 patients (47%) relapsed at 36 months. Among the 54 patients that relapsed, 27 were re-treated with vismodegib, which resulted in an ORR of 85% (23/27), a CR rate of 37% (10/27), and a PR rate of 48% (13/27).88 Another retrospective study of 35 laBCC patients who relapsed after vismodegib treatment reported a 31% (11/35) clinical recurrence rate at 6-month follow-up.89 An observational retrospective study also assessed the efficacy of SHH inhibitor maintenance therapy for advanced BCC patients who achieved a CR.90 In the study, 27 (64%) patients received a maintenance dose of 150 mg vismodegib once per week for 1 year, while 15 (36%) patients decided not to take a maintenance dose following CR of their BCC. All patients who took the maintenance therapy did not experience clinical recurrence at 1-year follow-up, whereas 26% of patients not on the maintenance dose relapsed.90 Consequently, these results indicate that BCC recurrence is frequent after SHH inhibitor therapy and highlights the importance of close surveillance after CR is attained. Nevertheless, most patients still respond to treatment with SHH inhibitors after relapsing, and intermittent maintenance doses may be an effective means to reduce risk of recurrence.
Conclusion
Vismodegib and sonidegib are SHH inhibitors approved for the treatment of laBCC and mBCC. Cemiplimab is now also approved for patients who do not respond to SHH inhibitors or for whom SHH inhibitors are not tolerable. Although these systemic targeted therapies can lead to notable tumor shrinkage and even complete regression in some patients, recurrence is common, and adverse effects may limit their use. Drug resistance is an emerging issue that requires additional examination. Further clinical studies are needed to determine which patients are likely to respond to these targeted treatments.
Various intermittent and maintenance drug regimens should be evaluated for their potential to mitigate adverse effects and reduce risk of recurrence, respectively. The synergistic effects of these medications with other therapies as well as their neoadjuvant and adjuvant roles should be further investigated. For example, administration of an SHH inhibitor prior to surgical excision of a BCC may allow for a smaller surgical defect size, thereby improving cosmetic and functional outcomes. Moreover, these systemic targeted medications may allow for previously inoperable tumors to become amenable to surgical treatment.
Although SHH inhibitors and PD-1 inhibitors represent a major advancement in the field of oncodermatology, real-world efficacy and safety data in the upcoming years will be important for elucidating their true benefit for patients with BCC.
Basal cell carcinoma (BCC) is the most common keratinocyte carcinoma and affects more than 3 million individuals per year in the United States.1 Approximately 40% of patients diagnosed with BCC will develop another BCC within 5 years of the initial diagnosis.2 Most cases are successfully treated with surgical excision and occasionally topical therapy or radiotherapy. Despite the high cure rate with conventional treatments, BCC can recur and can cause substantial destruction of the surrounding tissue if left untreated.3-5 In some instances, BCC can even metastasize and lead to death.6 For patients who are poor candidates for surgical or topical treatment modalities because of locally advanced BCC (laBCC) or metastatic BCC (mBCC), systemic treatment may be indicated. Vismodegib, sonidegib, and cemiplimab are the only systemic medications approved by the US Food and Drug Administration (FDA) for the treatment of laBCC and/or mBCC. Vismodegib and sonidegib target the sonic hedgehog (SHH) signaling pathway that is abnormally activated in more than 90% of BCCs.7 Cemiplimab is an immune checkpoint inhibitor (ICI) that targets the programmed cell death protein 1 (PD-1) receptor.8 Herein, we review the clinical utility of these medications and their evolving roles in the treatment of BCC.
SHH Pathway Inhibitors
The SHH pathway is a key regulator of cell proliferation and differentiation during embryogenesis.7 During adulthood, SHH signaling decreases but still plays an important role in stem cell activation and in regulation of the hair follicle growth cycle.9,10 However, de novo mutations in the genes that comprise the SHH pathway can result in aberrant constitutive activation, leading to unrestricted cell proliferation. Genetic mutations resulting in activation of Smoothened (SMO), a G-protein–coupled receptor involved in the signal transduction and propagation of the SHH pathway, have been implicated in the pathogenesis of BCC. Inactivating mutations also are commonly observed in patched homolog 1, an upstream cell-surface protein that inhibits SMO.7 The mechanism by which vismodegib and sonidegib, 2 of the FDA-approved oral medications for the treatment of advanced BCC, block the SHH pathway is through the selective inhibition of SMO.7,11
Vismodegib first received FDA approval in 2012 for the treatment of laBCC and mBCC after initial results from the pivotal ERIVANCE phase 2 trial demonstrated an objective response rate (ORR) of 43% (27/63) and 30% (10/33) in patients with locally advanced and metastatic disease, respectively. In this single-arm study, all enrolled patients (63 with laBCC and 33 with mBCC) received 150 mg of oral vismodegib daily.12 Updated results at 39 months demonstrated improved ORRs of 60% (38/63) and 48% (16/33) for the laBCC and mBCC groups, respectively. A complete response (CR) and partial response (PR) were observed in 32% (n=20) and 29% (n=18) of patients with laBCC, respectively.13 These results have been confirmed in subsequent studies, including the large international open-label trial known as STEVIE, with ORRs of 68.5% for 1119 cases of laBCC and 37% for 96 cases of mBCC.14-17 The CR and PR rates were 33% and 35%, respectively, for the laBCC group. The CR and PR rates for the mBCC group were 5% and 32%, respectively.14
The FDA approval of sonidegib for laBCC—but not mBCC—occurred in 2015 after the pivotal BOLT randomized phase 2 trial demonstrated an initial ORR of 43% (18/42) for laBCC and 15% (2/13) for mBCC after administration of 200 mg of sonidegib daily.18 A final follow-up analysis at 42 months resulted in ORRs of 56% (37/66) and 8% (1/13) for the laBCC and mBCC groups, respectively.19 Additionally, improved efficacy was not observed in the 151 patients who were randomized to receive treatment with the higher 800-mg dose; however, they did experience a higher incidence of adverse events.18,19
Currently, the true clinical differences between vismodegib and sonidegib remain uncertain, as no head-to-head trials have been conducted. Moreover, direct comparison of the data from the ERIVANCE and BOLT trials is challenging owing to fundamental differences in methodologic design, including the criteria used to assess BCC severity. The ERIVANCE trial utilized the conventional Response Evaluation Criteria in Solid Tumors (RECIST), while BOLT used the rigorous modified RECIST. However, an expert consensus study attempted to compare the 2 trials by modifying the outcomes from BOLT with the former RECIST criteria. The expert group found that the 2 SHH inhibitors had comparable efficacy and adverse event profiles.20 Nevertheless, a recent meta-analysis found that although ORRs for laBCC were similar between the 2 drugs, the CR rate for vismodegib was 31% compared with 3% for sonidegib. Additionally, for mBCC, they reported the ORR of vismodegib to be 2.7 times higher than that of sonidegib (39% vs 15%).21
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors have successfully been utilized in the treatment of cutaneous squamous cell carcinoma (cSCC); however, their use for treating BCC has been limited until recently.22-25 In February 2021, cemiplimab became the first and only ICI approved for the treatment of laBCC and mBCC in patients who did not respond to or were intolerant to prior SHH inhibitor therapy.26 Cemiplimab—a human monoclonal antibody against the PD-1 receptor expressed on T cells—blocks its interaction with programmed cell death ligand 1 and programmed cell death ligand 2 present on tumor cells. The blockade of the PD-1 pathway releases the inhibition of the antitumor immune response and enables appropriate cytotoxic T-cell activity to occur.8
The FDA approval of cemiplimab for the treatment of advanced BCC was based on an open-label, multicenter, single-arm phase 2 trial (NCT03132636) evaluating 84 patients with laBCC refractory or intolerant to SHH inhibitor therapy.26 Patients received an intravenous infusion of cemiplimab 350 mg every 3 weeks for up to 93 weeks or until disease progression or unacceptable toxicity. An ORR of 31% (26/84) was observed with a CR and PR of 6% (5/84) and 25% (21/84), respectively. The median duration of follow-up was 15 months.26 Given the clinically meaningful results of this trial, investigating the efficacy of other PD-1 inhibitors, such as pembrolizumab and nivolumab, for treatment of advanced BCC may prove worthwhile.
Adverse Effects of Systemic Treatments
The 2 approved SHH inhibitors—vismodegib and sonidegib—appear to have similar side-effect profiles, with the most common adverse effects being muscle spasms, dysgeusia, alopecia, nausea, vomiting, diarrhea, weight loss, and fatigue.20,21,27 These side effects occur at high frequencies (>40%) for both SHH inhibitors and often lead to discontinuation of the medication.21 Rates of treatment discontinuation range from 15% to 50% on average.12-14,18 Fortunately, the majority of these adverse effects do not appear to increase in severity or frequency with prolonged use of these medications.14,16,28
Various conservative and pharmacologic measures can be implemented to help manage side effects. For muscle spasms, which are the most commonly reported adverse effect, supplementation with magnesium, transcutaneous electrical nerve stimulation, acupuncture, massages, stretching, and thermal compresses can potentially be beneficial.29 Calcium channel blockers also may be effective, as one small prospective cohort study reported a reduction in the frequency of muscle cramps with amlodipine 10 mg daily.30 For alopecia, which typically is reversible and caused by SHH inhibition of the normal hair cycle, minoxidil theoretically can help, as it reduces telogen arrest and extends the anagen growth phase.31,32 Although usually mild and self-limiting, management of dysgeusia, weight loss, and gastrointestinal upset often can be managed with dietary changes, such as smaller, more frequent meals.33,34 Finally, alternative dosing strategies and drug holidays have been employed to mitigate these side effects and increase drug tolerability.35,36 These are discussed in the Alternative Dosing section.
Given the essential role of the SHH pathway in embryologic development, SHH inhibitors carry a black box warning of embryofetal teratogenicity and are contraindicated in females who are pregnant or breastfeeding. For females of reproductive potential, verification of pregnancy status should be performed prior to initiating treatment with an SHH inhibitor. These patients should be counseled on the use of contraception during treatment and for at least 24 months and 20 months after cessation of vismodegib and sonidegib, respectively.27,37,38 Male patients, even after a vasectomy, should use barrier contraception during treatment and for at least 3 months and 8 months after the final dose of vismodegib and sonidegib, respectively.37,38
Laboratory abnormalities commonly associated with SHH inhibitors include elevated hepatic enzymes, particularly with vismodegib, and elevated creatine kinase levels, particularly with sonidegib.28,39 Other laboratory abnormalities that can occur include hypercholesterolemia, hypercreatininemia, hyperglycemia, and increased serum lipase levels.19,28 Although these laboratory abnormalities usually are asymptomatic and self-limiting, regular monitoring should be performed.
There also is concern that SHH inhibitors may induce the development of cSCC. A case-control study of 55 cases and 125 control patients found an increased risk for cSCC in those previously treated with vismodegib, with a hazard ratio of 8.12.40 However, a subsequent retrospective cohort study of 1675 patients with BCC failed to find any association with cSCC among those treated with vismodegib compared to those who received standard surgical therapy.41 Clinical data for sonidegib are lacking, but the BOLT trial found that cSCC occurred in 3 patients receiving treatment with the SHH inhibitor.18 Thus, further studies are needed to more thoroughly assess this concern. Close monitoring for cSCC may be warranted in patients prescribed SHH inhibitors at this time.
Cemiplimab has demonstrated an acceptable safety profile and is generally well tolerated. In the phase 2 trial of cemiplimab for cSCC, approximately 5% of patients discontinued treatment because of adverse effects. The most commonly reported side effects of cemiplimab were diarrhea (27%), fatigue (24%), nausea (17%), constipation (15%), and rash (15%).23 In the phase 2 trial for laBCC, grade 3 or 4 adverse events occurred in 48% of patients, with hypertension (5%) being the most common.26 Although rare, immune-mediated adverse reactions also can occur, given the mechanism of action of ICIs. These side effects, ranging in severity from mild to fatal, include pneumonitis, colitis, hepatitis, nephritis, myocarditis, and hypophysitis. Therefore, close monitoring for these immune-mediated reactions is critical, but most can be managed with corticosteroids or treatment interruption if they occur.42,43
No absolute contraindications exist for cemiplimab; however, extreme caution should be taken in immunosuppressed individuals, such as solid organ transplant recipients and those with chronic lymphocytic leukemia (CLL), as safety data are limited in these patients.44,45 Although small retrospective studies have reported reasonable tolerability in solid organ transplant recipients treated with ICIs, an allograft rejection rate of 41% was found in a meta-analysis of 64 patients.46-48 In CLL patients with keratinocyte carcinomas, ICIs have been safely used and have even demonstrated efficacy for CLL in some cases.49-52
Alternative Dosing
The side effects of SHH inhibitors have led to alternative dosing strategies to prevent medication discontinuation and improve adherence. In patients with basal cell nevus syndrome, multimonth drug holidays have been shown to increase drug tolerability without compromising efficacy.35,36 Weekly intermittent dosing regimens of vismodegib ranging from 1 week on followed by 1 to 3 weeks off demonstrated efficacy in a retrospective study of 7 patients with advanced BCC.53 All 7 patients experienced improvement in their BCCs, with 3 patients experiencing CR. Importantly, treatment-related adverse effects were mild and well tolerated, with no patients terminating the medication.53 Two other retrospective case series of patients with advanced BCC treated with vismodegib reported similar findings for those placed on an intermittent dosing schedule ranging from once every other day to once per week.54,55
In the large phase 2 randomized trial known as MIKIE, 2 different intermittent dosing regimens of 150 mg vismodegib daily for patients with multiple BCCs were found to have good activity and tolerability.56 The first group (n=116) received vismodegib for 12 weeks, then 3 rounds of 8 weeks of placebo, followed by 12 weeks of vismodegib; there was a 63% reduction in clinically evident BCCs after 73 weeks. The second group (n=113) received the medication for 24 weeks, then 3 rounds of 8 weeks of placebo, followed by 8 weeks of vismodegib; there was a 54% reduction at the end of 73 weeks.56 Subsequent analyses found improvements in health-related quality-of-life outcomes that were similar for both groups.57
Consequently, alternative dosing schedules appear to be a viable option for patients at risk of discontinuing treatment because of adverse effects, and current data support the recently approved recommendations of dose interruptions of up to 8 weeks to manage adverse effects in patients with laBCC or mBCC.58 Nevertheless, further clinical studies are required to determine the optimal intermittent dosing regimen for patients treated with SHH inhibitors.
Neoadjuvant Administration
Recently, vismodegib has been studied as a neoadjuvant therapy for BCC with promising results. Several small retrospective studies and case reports have documented successful treatment of both operable and inoperable periocular laBCC, with preservation of the eye in all patients.59-61 An open-label trial of 15 patients with advanced BCC who received neoadjuvant vismodegib for 3 to 6 months prior to surgical excision reported a mean reduction of 35% in the final surgical defect size, with no recurrence at 22 months.62,63 The latest and largest study performed was a phase 2 open-label trial known as VISMONEO, where 44 of 55 laBCC patients (80%) receiving neoadjuvant vismodegib for a mean duration of 6 months (range, 4–10 months) achieved the primary end point of tumor surgical downstaging.64 Of the 44 patients who had tumor downstaging, 27 (61%) experienced histologically proven CRs. Additionally, a 66% reduction in the average target lesion size was reported in this group compared to29% in the 11 patients who did not have tumor downstaging (P=.0002).64 Thus, SHH inhibitors may hold an important neoadjuvant role in the treatment of BCC by decreasing surgical defect size and allowing for surgical management of previously inoperable cases.
Synergism With Radiation
Preliminary data suggest SHH inhibitors may help potentiate the effects of radiation therapy for the treatment of BCC. Currently, the evidence primarily is limited to case studies, with several reports describing complete remission in patients with advanced BCCs who were considered unsuitable candidates for surgery. In these cases, vismodegib was administered either prior to or concurrently with radiation treatment.65-69 An in vitro study also documented the radiation-sensitizing effects of vismodegib in a BCC cell line.70 Recently, a phase 2 trial (ClinicalTrials.gov identifier NCT01835626) evaluating the concurrent use of vismodegib and radiotherapy for patients with advanced BCC was completed, but data has yet to be published.
Synergism With and Benefit of Antifungal Therapy
The antifungal drug itraconazole is a potent inhibitor of the SHH pathway and may have an adjunctive role in the treatment of BCC. Similar to vismodegib and sonidegib, itraconazole acts as a direct antagonist of SMO. However, it is thought to bind to a distinct site on SMO.71,72 An open-label, exploratory phase 2 trial of 19 patients with BCC found that oral itraconazole 200 to 400 mg daily decreased tumor proliferative index by 45% (P=.04), as measured by Ki-67; SHH activity by 65% (P=.03), as measured by GLI1 messenger RNA; and mean tumor area by 24%.73 In a case series of 5 patients with mBCC refractory to conventional SHH inhibitor therapy, combined treatment with itraconazole and arsenic trioxide resulted in stable disease and a 75% reduction in SHH activity (P<.001).74 One case report documented tumor regression leading to stable disease for 15 months in a patient with laBCC treated with itraconazole monotherapy due to being unable to afford vismodegib or sonidegib. However, within 2 months of treatment discontinuation, the lesion progressed considerably.75 The efficacy of a topical formulation of itraconazole also has been tested in an open-label, placebo-controlled phase 2 trial, but no benefit was observed.76
Posaconazole is a second-generation antifungal agent that may serve as a potential alternative to itraconazole.77 Although clinical data are lacking, a basic science study found that posaconazole could inhibit the growth of SHH-dependent BCC in vivo (in mice).78 Furthermore, posaconazole has demonstrated a better safety profile with fewer and more mild side effects than itraconazole and does not require dose adjustment for those with hepatic or renal failure.79,80 Thus, posaconazole may be a safer alternative to itraconazole for the treatment of BCC. Further clinical studies are needed to elucidate the potential synergistic effects of these antifungal agents with the 2 currently approved SHH inhibitors for the treatment of advanced BCC.
Drug Resistance
Treatment resistance to SHH inhibitors, though uncommon, is a growing concern. Acquired mutations in the SMO binding site or downstream mediators of the SHH pathway have been shown to confer resistance to vismodegib and sonidegib.72,81-83 In addition, it appears that there may be shared resistance among the drugs in this class. One study assessing the efficacy of sonidegib in 9 patients with laBCC resistant to vismodegib found that these patients also did not respond to sonidegib.84 Interestingly, 1 case report documented tumor regression of an intracranial BCC in a patient treated with sonidegib and itraconazole after failure with vismodegib.85 An in vitro study also found that itraconazole maintained SHH inhibitory activity for all drug-resistant SMO mutations that have been reported.72 Therefore, itraconazole monotherapy or combination therapy with a canonical SHH inhibitor may be considered for patients with recalcitrant BCC and warrants further investigation.
Taladegib is a newly developed SMO inhibitor that may serve as another promising alternative for patients who develop resistance to vismodegib or sonidegib. A phase 1 trial of taladegib for advanced BCC found an ORR of 69% (11/16) in the SHH inhibitor–naïve group and an ORR of 36% (11/32) in the group previously treated with a SHH inhibitor.86 Additionally, the safety profile and frequency of adverse effects appear to be similar to those associated with vismodegib and sonidegib.86,87 Unfortunately, no clinical trials evaluating taladegib for BCC are ongoing or in development at this time.
Recurrence
There appears to be a relatively high rate of recurrence for BCC patients who achieve a CR to SHH inhibitors. In a retrospective study of 116 laBCC patients who experienced a CR after vismodegib therapy, 54 patients (47%) relapsed at 36 months. Among the 54 patients that relapsed, 27 were re-treated with vismodegib, which resulted in an ORR of 85% (23/27), a CR rate of 37% (10/27), and a PR rate of 48% (13/27).88 Another retrospective study of 35 laBCC patients who relapsed after vismodegib treatment reported a 31% (11/35) clinical recurrence rate at 6-month follow-up.89 An observational retrospective study also assessed the efficacy of SHH inhibitor maintenance therapy for advanced BCC patients who achieved a CR.90 In the study, 27 (64%) patients received a maintenance dose of 150 mg vismodegib once per week for 1 year, while 15 (36%) patients decided not to take a maintenance dose following CR of their BCC. All patients who took the maintenance therapy did not experience clinical recurrence at 1-year follow-up, whereas 26% of patients not on the maintenance dose relapsed.90 Consequently, these results indicate that BCC recurrence is frequent after SHH inhibitor therapy and highlights the importance of close surveillance after CR is attained. Nevertheless, most patients still respond to treatment with SHH inhibitors after relapsing, and intermittent maintenance doses may be an effective means to reduce risk of recurrence.
Conclusion
Vismodegib and sonidegib are SHH inhibitors approved for the treatment of laBCC and mBCC. Cemiplimab is now also approved for patients who do not respond to SHH inhibitors or for whom SHH inhibitors are not tolerable. Although these systemic targeted therapies can lead to notable tumor shrinkage and even complete regression in some patients, recurrence is common, and adverse effects may limit their use. Drug resistance is an emerging issue that requires additional examination. Further clinical studies are needed to determine which patients are likely to respond to these targeted treatments.
Various intermittent and maintenance drug regimens should be evaluated for their potential to mitigate adverse effects and reduce risk of recurrence, respectively. The synergistic effects of these medications with other therapies as well as their neoadjuvant and adjuvant roles should be further investigated. For example, administration of an SHH inhibitor prior to surgical excision of a BCC may allow for a smaller surgical defect size, thereby improving cosmetic and functional outcomes. Moreover, these systemic targeted medications may allow for previously inoperable tumors to become amenable to surgical treatment.
Although SHH inhibitors and PD-1 inhibitors represent a major advancement in the field of oncodermatology, real-world efficacy and safety data in the upcoming years will be important for elucidating their true benefit for patients with BCC.
- Rogers HW, Weinstock MA, Feldman SR, et al. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. population, 2012. JAMA Dermatol. 2015;151:1081-1086.
- Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80:303-317.
- Rees JR, Zens MS, Celaya MO, et al. Survival after squamous cell and basal cell carcinoma of the skin: a retrospective cohort analysis. Int J Cancer. 2015;137:878-884.
- Kasumagic-Halilovic E, Hasic M, Ovcina-Kurtovic N. A clinical study of basal cell carcinoma. Med Arch. 2019;73:394-398.
- Goldenberg G, Karagiannis T, Palmer JB, et al. Incidence and prevalence of basal cell carcinoma (BCC) and locally advanced BCC (LABCC) in a large commercially insured population in the United States: a retrospective cohort study. J Am Acad Dermatol. 2016;75:957.e952-966.e952.
- Laga AC, Schaefer IM, Sholl LM, et al. Metastatic basal cell carcinoma. Am J Clin Pathol. 2019;152:706-717.
- Rimkus TK, Carpenter RL, Qasem S, et al. Targeting the sonic hedgehog signaling pathway: review of smoothened and GLI inhibitors. Cancers (Basel). 2016;8:22.
- Burova E, Hermann A, Waite J, et al. Characterization of the anti–PD-1 antibody REGN2810 and its antitumor activity in human PD-1 knock-in mice. Mol Cancer Ther. 2017;16:861-870.
- Bhardwaj G, Murdoch B, Wu D, et al. Sonic hedgehog induces the proliferation of primitive human hematopoietic cells via BMP regulation. Nat Immunol. 2001;2:172-180.
- Paladini RD, Saleh J, Qian C, et al. Modulation of hair growth with small molecule agonists of the hedgehog signaling pathway. J Invest Dermatol. 2005;125:638-646.
- Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164-1172.
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-2179.
- Sekulic A, Migden MR, Basset-Seguin N, et al. Long-term safety and efficacy of vismodegib in patients with advanced basal cell carcinoma: final update of the pivotal ERIVANCE BCC study. BMC Cancer. 2017;17:332.
- Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
- Cozzani R, Del Aguila R, Carrizo M, et al. Efficacy and safety profile of vismodegib in a real-world setting cohort of patients with advanced basal cell carcinoma in Argentina. Int J Dermatol. 2020;59:627-632.
- Spallone G, Sollena P, Ventura A, et al. Efficacy and safety of vismodegib treatment in patients with advanced basal cell carcinoma and multiple comorbidities. Dermatol Ther. 2019;32:E13108.
- Fosko SW, Chu MB, Armbrecht E, et al. Efficacy, rate of tumor response, and safety of a short course (12-24 weeks) of oral vismodegib in various histologic subtypes (infiltrative, nodular, and superficial) of high-risk or locally advanced basal cell carcinoma, in an open-label, prospective case series clinical trial. J Am Acad Dermatol. 2020;82:946-954.
- Migden MR, Guminski A, Gutzmer R, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): a multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16:716-728.
- Dummer R, Guminksi A, Gutzmer R, et al. Long-term efficacy and safety of sonidegib in patients with advanced basal cell carcinoma: 42-month analysis of the phase II randomized, double-blind BOLT study. Br J Dermatol. 2020;182:1369-1378.
- Dummer R, Ascierto PA, Basset-Seguin N, et al. Sonidegib and vismodegib in the treatment of patients with locally advanced basal cell carcinoma: a joint expert opinion. J Eur Acad Dermatol Venereol. 2020;34:1944-1956.
- Xie P, Lefrançois P. Efficacy, safety, and comparison of sonic hedgehog inhibitors in basal cell carcinomas: a systematic review and meta-analysis. J Am Acad Dermatol. 2018;79:1089-1100.e1017.
- Gentzler R, Hall R, Kunk PR, et al. Beyond melanoma: inhibiting the PD-1/PD-L1 pathway in solid tumors. Immunotherapy. 2016;8:583-600.
- Guminski AD, Lim AML, Khushalani NI, et al. Phase 2 study of cemiplimab, a human monoclonal anti-PD-1, in patients (pts) with metastatic cutaneous squamous cell carcinoma (mCSCC; group 1): 12-month follow-up [abstract]. J Clin Oncol. 2019;37(15 suppl):9526.
- Grob JJ, Gonzalez Mendoza R, Basset-Seguin N, et al. Pembrolizumab for recurrent/metastatic cutaneous squamous cell carcinoma (cSCC): efficacy and safety results from the phase II KEYNOTE-629 study [abstract]. Ann Oncol. 2019;30 (suppl 5):v908.
- Maubec E, Boubaya M, Petrow P, et al. Pembrolizumab as first-line therapy in patients with unresectable cutaneous squamous cell carcinoma (cSCC): phase 2 results from CARSKIN [abstract]. J Clin Oncol. 2019;37(15 suppl):9547.
- Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22:848-857.
- Carpenter RL, Ray H. Safety and tolerability of sonic hedgehog pathway inhibitors in cancer. Drug Saf. 2019;42:263-279.
- Villani A, Fabbrocini G, Costa C, et al. Sonidegib: safety and efficacy in treatment of advanced basal cell carcinoma. Dermatol Ther (Heidelb). 2020;10:401-412.
- Wright A, Sluka KA. Nonpharmacological treatments for musculoskeletal pain. Clin J Pain. 2001;17:33-46.
- Ally MS, Tang JY, Lindgren J, et al. Effect of calcium channel blockade on vismodegib-induced muscle cramps. JAMA Dermatol. 2015;151:1132-1134.
- Yang X, Thai K-E. Treatment of permanent chemotherapy-induced alopecia with low dose oral minoxidil. Australas J Dermatol. 2016;57:e130-e132.
- Ferguson JS, Hannam S, Toholka R, et al. Hair loss and hedgehog inhibitors: a class effect? Br J Dermatol. 2015;173:262-264.
- Kumbargere Nagraj S, George RP, Shetty N, et al. Interventions for managing taste disturbances. Cochrane Database Syst Rev. 2017;12:CD010470.
- Jacobsen AA, Kydd AR, Strasswimmer J. Practical management of the adverse effects of hedgehog pathway inhibitor therapy for basal cell carcinoma. J Am Acad Dermatol. 2017;76:767-768.
- Ally MS, Tang JY, Joseph T, et al. The use of vismodegib to shrink keratocystic odontogenic tumors in patients with basal cell nevus syndrome. JAMA Dermatol. 2014;150:542-545.
- Yang X, Dinehart SM. Intermittent vismodegib therapy in basal cell nevus syndrome. JAMA Dermatol. 2016;152:223-224.
- Erivedge. Prescribing information. Genentech; 2015.
- Odomzo. Prescribing information. Novartis; 2015.
- Ventarola DJ, Silverstein DI. Vismodegib-associated hepatotoxicity: a potential side effect detected in postmarketing surveillance. J Am Acad Dermatol. 2014;71:397-398.
- Mohan SV, Chang J, Li S, et al. Increased risk of cutaneous squamous cell carcinoma after vismodegib therapy for basal cell carcinoma. JAMA Dermatol. 2016;152:527-532.
- Bhutani T, Abrouk M, Sima CS, et al. Risk of cutaneous squamous cell carcinoma after treatment of basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2017;77:713-718.
- Morgado M, Plácido A, Morgado S, et al. Management of the adverse effects of immune checkpoint inhibitors. Vaccines (Basel). 2020;8:575.
- Martins F, Sofiya L, Sykiotis GP, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16:563-580.
- Ntsethe A, Dludla PV, Nyambuya TM, et al. The impact of immune checkpoint inhibitors in patients with chronic lymphocytic leukemia (CLL): a protocol for a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99:E21167.
- Johnson DB, Sullivan RJ, Menzies AM. Immune checkpoint inhibitors in challenging populations. Cancer. 2017;123:1904-1911.
- Tsung I, Worden FP, Fontana RJ. Safety and efficacy of checkpoint inhibitors in solid organ transplant recipients with cutaneous squamous cell carcinoma [abstract]. J Clin Oncol. 2020;38(15 suppl):E22014.
- Owoyemi I, Vaughan LE, Costello CM, et al. Clinical outcomes of solid organ transplant recipients with metastatic cancers who are treated with immune checkpoint inhibitors: a single-center analysis. Cancer. 2020;126:4780-4787.
- Kumar V, Shinagare AB, Rennke HG, et al. The safety and efficacy of checkpoint inhibitors in transplant recipients: a case series and systematic review of literature. Oncologist. 2020;25:505-514.
- Arenbergerova M, Fialova A, Arenberger P, et al. Killing two birds with one stone: response to pembrolizumab in a patient with metastatic melanoma and B-cell chronic lymphocytic leukaemia. J Eur Acad Dermatol Venereol. 2018;32:E72-E74.
- Archibald WJ, Meacham PJ, Williams AM, et al. Management of melanoma in patients with chronic lymphocytic leukemia. Leuk Res. 2018;71:43-46.
- Ding W, LaPlant BR, Call TG, et al. Pembrolizumab in patients with CLL and Richter transformation or with relapsed CLL. Blood. 2017;129:3419-3427.
- Leiter U, Loquai C, Reinhardt L, et al. Immune checkpoint inhibition therapy for advanced skin cancer in patients with concomitant hematological malignancy: a retrospective multicenter DeCOG study of 84 patients. J Immunother Cancer. 2020;8:E000897.
- Becker LR, Aakhus AE, Reich HC, et al. A novel alternate dosing of vismodegib for treatment of patients with advanced basal cell carcinomas. JAMA Dermatol. 2017;153:321-322.
- Woltsche N, Pichler N, Wolf I, et al. Managing adverse effects by dose reduction during routine treatment of locally advanced basal cell carcinoma with the hedgehog inhibitor vismodegib: a single centre experience. J Eur Acad Dermatol Venereol. 2019;33:E144-E145.
- Wong C, Poblete-Lopez C, Vidimos A. Comparison of daily dosing versus Monday through Friday dosing of vismodegib for locally advanced basal cell carcinoma and basal cell nevus syndrome: a retrospective case series. J Am Acad Dermatol. 2020;82:1539-1542.
- Dréno B, Kunstfeld R, Hauschild A, et al. Two intermittent vismodegib dosing regimens in patients with multiple basal-cell carcinomas (MIKIE): a randomised, regimen-controlled, double-blind, phase 2 trial. Lancet Oncol. 2017;18:404-412.
- Schadendorf D, Hauschild A, Fosko S, et al. Quality-of-life analysis with intermittent vismodegib regimens in patients with multiple basal cell carcinomas: patient-reported outcomes from the MIKIE study. J Eur Acad Dermatol Venereol. 2020;34:E526-E529.
- Chanu P, Musib L, Wang X, et al. Vismodegib efficacy in advanced basal cell carcinoma maintained with 8-week dose interruptions: a model-based evaluation. J Invest Dermatol. 2021;141:930-933.
- Su MG, Potts LB, Tsai JH. Treatment of periocular basal cell carcinoma with neoadjuvant vismodegib. Am J Ophthalmol Case Rep. 2020;19:100755.
- González AR, Etchichury D, Gil ME, et al. Neoadjuvant vismodegib and Mohs micrographic surgery for locally advanced periocular basal cell carcinoma. Ophthalmic Plast Reconstr Surg. 2019;35:56-61.
- Sagiv O, Nagarajan P, Ferrarotto R, et al. Ocular preservation with neoadjuvant vismodegib in patients with locally advanced periocular basal cell carcinoma. Br J Ophthalmol. 2019;103:775-780.
- Ally MS, Aasi S, Wysong A, et al. An investigator-initiated open-label clinical trial of vismodegib as a neoadjuvant to surgery for high-risk basal cell carcinoma. J Am Acad Dermatol. 2014;71:904-911.e1.
- Kwon GP, Ally MS, Bailey-Healy I, et al. Update to an open-label clinical trial of vismodegib as neoadjuvant before surgery for high-risk basal cell carcinoma (BCC). J Am Acad Dermatol. 2016;75:213-215.
- Mortier L, Bertrand N, Basset-Seguin N, et al. Vismodegib in neoadjuvant treatment of locally advanced basal cell carcinoma: first results of a multicenter, open-label, phase 2 trial (VISMONEO study) [abstract]. J Clin Oncol. 2018;36(15 suppl):9509.
- Strasswimmer JM. Potential synergy of radiation therapy with vismodegib for basal cell carcinoma. JAMA Dermatol. 2015;151:925-926.
- Gathings RM, Orscheln CS, Huang WW. Compassionate use of vismodegib and adjuvant radiotherapy in the treatment of multiple locally advanced and inoperable basal cell carcinomas and squamous cell carcinomas of the skin. J Am Acad Dermatol. 2014;70:E88-E89.
- Franco AI, Eastwick G, Farah R, et al. Upfront radiotherapy with concurrent and adjuvant vismodegib is effective and well-tolerated in a patient with advanced, multifocal basal cell carcinoma. Case Rep Dermatol Med. 2018;2018:2354146.
- Pollom EL, Bui TT, Chang AL, et al. Concurrent vismodegib and radiotherapy for recurrent, advanced basal cell carcinoma. JAMA Dermatol. 2015;151:998-1001.
- Janela-Lapert R, Dubray B, Duval-Modeste A, et al. Treatment of advanced basal cell carcinoma with vismodegib followed by radiotherapy [in French]. Ann Dermatol Venereol. 2020;147:780-782.
- Hehlgans S, Booms P, Güllülü Ö, et al. Radiation sensitization of basal cell and head and neck squamous cell carcinoma by the hedgehog pathway inhibitor vismodegib. Int J Mol Sci. 2018;19:2485.
- Kim J, Tang JY, Gong R, et al. Itraconazole, a commonly used antifungal that inhibits hedgehog pathway activity and cancer growth. Cancer Cell. 2010;17:388-399.
- Kim J, Aftab BT, Tang JY, et al. Itraconazole and arsenic trioxide inhibit hedgehog pathway activation and tumor growth associated with acquired resistance to smoothened antagonists. Cancer Cell. 2013;23:23-34.
- Kim DJ, Kim J, Spaunhurst K, et al. Open-label, exploratory phase II trial of oral itraconazole for the treatment of basal cell carcinoma. J Clin Oncol. 2014;32:745-751.
- Ally MS, Ransohoff K, Sarin K, et al. Effects of combined treatment with arsenic trioxide and itraconazole in patients with refractory metastatic basal cell carcinoma. JAMA Dermatol. 2016;152:452-456.
- Cia˛z˙yn´yska M, Narbutt J, Skibin´ska M, et al. Itraconazole—a new player in the therapy of advanced basal cell carcinoma: a case report. JCO Oncol Pract. 2020;16:837-838.
- Sohn GK, Kwon GP, Bailey-Healy I, et al. Topical itraconazole for the treatment of basal cell carcinoma in patients with basal cell nevus syndrome or high-frequency basal cell carcinomas: a phase 2, open-label, placebo-controlled trial. JAMA Dermatol. 2019;155:1078-1080.
- Lass-Flörl C. Triazole antifungal agents in invasive fungal infections: a comparative review. Drugs. 2011;71:2405-2419.
- Chen B, Trang V, Lee A, et al. Posaconazole, a second-generation triazole antifungal drug, inhibits the hedgehog signaling pathway and progression of basal cell carcinoma. Mol Cancer Ther. 2016;15:866-876.
- Katragkou A, Tsikopoulou F, Roilides E, et al. Posaconazole: when and how? the clinician’s view. Mycoses. 2012;55:110-122.
- Raad II, Graybill JR, Bustamante AB, et al. Safety of long-term oral posaconazole use in the treatment of refractory invasive fungal infections. Clin Infect Dis. 2006;42:1726-1734.
- Atwood SX, Sarin KY, Whitson RJ, et al. Smoothened variants explain the majority of drug resistance in basal cell carcinoma. Cancer Cell. 2015;27:342-353.
- Sun Q, Atzmony L, Zaki T, et al. Clues to primary vismodegib resistance lie in histology and genetics. J Clin Pathol. 2020;73:678-680.
- Verkouteren BJA, Wakkee M, van Geel M, et al. Molecular testing in metastatic basal cell carcinoma. J Am Acad Dermatol. 2021;85:1135-1142.
- Danial C, Sarin KY, Oro AE, et al. An investigator-initiated open-label trial of sonidegib in advanced basal cell carcinoma patients resistant to vismodegib. Clin Cancer Res. 2016;22:1325-1329.
- Yoon J, Apicelli AJ 3rd, Pavlopoulos TV. Intracranial regression of an advanced basal cell carcinoma using sonidegib and itraconazole after failure with vismodegib. JAAD Case Rep. 2017;4:10-12.
- Bendell J, Andre V, Ho A, et al. Phase I study of LY2940680, a Smo antagonist, in patients with advanced cancer including treatment-naïve and previously treated basal cell carcinoma. Clin Cancer Res. 2018;24:2082-2091.
- Ueno H, Kondo S, Yoshikawa S, et al. A phase I and pharmacokinetic study of taladegib, a Smoothened inhibitor, in Japanese patients with advanced solid tumors. Invest New Drugs. 2018;36:647-656.
- Herms F, Lambert J, Grob JJ, et al. Follow-up of patients with complete remission of locally advanced basal cell carcinoma after vismodegib discontinuation: a multicenter French study of 116 patients. J Clin Oncol. 2019;37:3275-3282.
- Villani A, Megna M, Fabbrocini G, et al. Long-term efficacy of vismodegib after its withdrawal and patients’ health-related quality of life using the Dermatology Life Quality Index (DLQI). Dermatol Ther (Heidelb). 2019;9:719-724.
- Scalvenzi M, Cappello M, Costa C, et al. Low-dose vismodegib as maintenance therapy after locally advanced basal cell carcinoma complete remission: high efficacy with minimal toxicity. Dermatol Ther (Heidelb). 2020;10:465-468.
- Rogers HW, Weinstock MA, Feldman SR, et al. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. population, 2012. JAMA Dermatol. 2015;151:1081-1086.
- Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80:303-317.
- Rees JR, Zens MS, Celaya MO, et al. Survival after squamous cell and basal cell carcinoma of the skin: a retrospective cohort analysis. Int J Cancer. 2015;137:878-884.
- Kasumagic-Halilovic E, Hasic M, Ovcina-Kurtovic N. A clinical study of basal cell carcinoma. Med Arch. 2019;73:394-398.
- Goldenberg G, Karagiannis T, Palmer JB, et al. Incidence and prevalence of basal cell carcinoma (BCC) and locally advanced BCC (LABCC) in a large commercially insured population in the United States: a retrospective cohort study. J Am Acad Dermatol. 2016;75:957.e952-966.e952.
- Laga AC, Schaefer IM, Sholl LM, et al. Metastatic basal cell carcinoma. Am J Clin Pathol. 2019;152:706-717.
- Rimkus TK, Carpenter RL, Qasem S, et al. Targeting the sonic hedgehog signaling pathway: review of smoothened and GLI inhibitors. Cancers (Basel). 2016;8:22.
- Burova E, Hermann A, Waite J, et al. Characterization of the anti–PD-1 antibody REGN2810 and its antitumor activity in human PD-1 knock-in mice. Mol Cancer Ther. 2017;16:861-870.
- Bhardwaj G, Murdoch B, Wu D, et al. Sonic hedgehog induces the proliferation of primitive human hematopoietic cells via BMP regulation. Nat Immunol. 2001;2:172-180.
- Paladini RD, Saleh J, Qian C, et al. Modulation of hair growth with small molecule agonists of the hedgehog signaling pathway. J Invest Dermatol. 2005;125:638-646.
- Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164-1172.
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-2179.
- Sekulic A, Migden MR, Basset-Seguin N, et al. Long-term safety and efficacy of vismodegib in patients with advanced basal cell carcinoma: final update of the pivotal ERIVANCE BCC study. BMC Cancer. 2017;17:332.
- Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
- Cozzani R, Del Aguila R, Carrizo M, et al. Efficacy and safety profile of vismodegib in a real-world setting cohort of patients with advanced basal cell carcinoma in Argentina. Int J Dermatol. 2020;59:627-632.
- Spallone G, Sollena P, Ventura A, et al. Efficacy and safety of vismodegib treatment in patients with advanced basal cell carcinoma and multiple comorbidities. Dermatol Ther. 2019;32:E13108.
- Fosko SW, Chu MB, Armbrecht E, et al. Efficacy, rate of tumor response, and safety of a short course (12-24 weeks) of oral vismodegib in various histologic subtypes (infiltrative, nodular, and superficial) of high-risk or locally advanced basal cell carcinoma, in an open-label, prospective case series clinical trial. J Am Acad Dermatol. 2020;82:946-954.
- Migden MR, Guminski A, Gutzmer R, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): a multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16:716-728.
- Dummer R, Guminksi A, Gutzmer R, et al. Long-term efficacy and safety of sonidegib in patients with advanced basal cell carcinoma: 42-month analysis of the phase II randomized, double-blind BOLT study. Br J Dermatol. 2020;182:1369-1378.
- Dummer R, Ascierto PA, Basset-Seguin N, et al. Sonidegib and vismodegib in the treatment of patients with locally advanced basal cell carcinoma: a joint expert opinion. J Eur Acad Dermatol Venereol. 2020;34:1944-1956.
- Xie P, Lefrançois P. Efficacy, safety, and comparison of sonic hedgehog inhibitors in basal cell carcinomas: a systematic review and meta-analysis. J Am Acad Dermatol. 2018;79:1089-1100.e1017.
- Gentzler R, Hall R, Kunk PR, et al. Beyond melanoma: inhibiting the PD-1/PD-L1 pathway in solid tumors. Immunotherapy. 2016;8:583-600.
- Guminski AD, Lim AML, Khushalani NI, et al. Phase 2 study of cemiplimab, a human monoclonal anti-PD-1, in patients (pts) with metastatic cutaneous squamous cell carcinoma (mCSCC; group 1): 12-month follow-up [abstract]. J Clin Oncol. 2019;37(15 suppl):9526.
- Grob JJ, Gonzalez Mendoza R, Basset-Seguin N, et al. Pembrolizumab for recurrent/metastatic cutaneous squamous cell carcinoma (cSCC): efficacy and safety results from the phase II KEYNOTE-629 study [abstract]. Ann Oncol. 2019;30 (suppl 5):v908.
- Maubec E, Boubaya M, Petrow P, et al. Pembrolizumab as first-line therapy in patients with unresectable cutaneous squamous cell carcinoma (cSCC): phase 2 results from CARSKIN [abstract]. J Clin Oncol. 2019;37(15 suppl):9547.
- Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22:848-857.
- Carpenter RL, Ray H. Safety and tolerability of sonic hedgehog pathway inhibitors in cancer. Drug Saf. 2019;42:263-279.
- Villani A, Fabbrocini G, Costa C, et al. Sonidegib: safety and efficacy in treatment of advanced basal cell carcinoma. Dermatol Ther (Heidelb). 2020;10:401-412.
- Wright A, Sluka KA. Nonpharmacological treatments for musculoskeletal pain. Clin J Pain. 2001;17:33-46.
- Ally MS, Tang JY, Lindgren J, et al. Effect of calcium channel blockade on vismodegib-induced muscle cramps. JAMA Dermatol. 2015;151:1132-1134.
- Yang X, Thai K-E. Treatment of permanent chemotherapy-induced alopecia with low dose oral minoxidil. Australas J Dermatol. 2016;57:e130-e132.
- Ferguson JS, Hannam S, Toholka R, et al. Hair loss and hedgehog inhibitors: a class effect? Br J Dermatol. 2015;173:262-264.
- Kumbargere Nagraj S, George RP, Shetty N, et al. Interventions for managing taste disturbances. Cochrane Database Syst Rev. 2017;12:CD010470.
- Jacobsen AA, Kydd AR, Strasswimmer J. Practical management of the adverse effects of hedgehog pathway inhibitor therapy for basal cell carcinoma. J Am Acad Dermatol. 2017;76:767-768.
- Ally MS, Tang JY, Joseph T, et al. The use of vismodegib to shrink keratocystic odontogenic tumors in patients with basal cell nevus syndrome. JAMA Dermatol. 2014;150:542-545.
- Yang X, Dinehart SM. Intermittent vismodegib therapy in basal cell nevus syndrome. JAMA Dermatol. 2016;152:223-224.
- Erivedge. Prescribing information. Genentech; 2015.
- Odomzo. Prescribing information. Novartis; 2015.
- Ventarola DJ, Silverstein DI. Vismodegib-associated hepatotoxicity: a potential side effect detected in postmarketing surveillance. J Am Acad Dermatol. 2014;71:397-398.
- Mohan SV, Chang J, Li S, et al. Increased risk of cutaneous squamous cell carcinoma after vismodegib therapy for basal cell carcinoma. JAMA Dermatol. 2016;152:527-532.
- Bhutani T, Abrouk M, Sima CS, et al. Risk of cutaneous squamous cell carcinoma after treatment of basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2017;77:713-718.
- Morgado M, Plácido A, Morgado S, et al. Management of the adverse effects of immune checkpoint inhibitors. Vaccines (Basel). 2020;8:575.
- Martins F, Sofiya L, Sykiotis GP, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16:563-580.
- Ntsethe A, Dludla PV, Nyambuya TM, et al. The impact of immune checkpoint inhibitors in patients with chronic lymphocytic leukemia (CLL): a protocol for a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99:E21167.
- Johnson DB, Sullivan RJ, Menzies AM. Immune checkpoint inhibitors in challenging populations. Cancer. 2017;123:1904-1911.
- Tsung I, Worden FP, Fontana RJ. Safety and efficacy of checkpoint inhibitors in solid organ transplant recipients with cutaneous squamous cell carcinoma [abstract]. J Clin Oncol. 2020;38(15 suppl):E22014.
- Owoyemi I, Vaughan LE, Costello CM, et al. Clinical outcomes of solid organ transplant recipients with metastatic cancers who are treated with immune checkpoint inhibitors: a single-center analysis. Cancer. 2020;126:4780-4787.
- Kumar V, Shinagare AB, Rennke HG, et al. The safety and efficacy of checkpoint inhibitors in transplant recipients: a case series and systematic review of literature. Oncologist. 2020;25:505-514.
- Arenbergerova M, Fialova A, Arenberger P, et al. Killing two birds with one stone: response to pembrolizumab in a patient with metastatic melanoma and B-cell chronic lymphocytic leukaemia. J Eur Acad Dermatol Venereol. 2018;32:E72-E74.
- Archibald WJ, Meacham PJ, Williams AM, et al. Management of melanoma in patients with chronic lymphocytic leukemia. Leuk Res. 2018;71:43-46.
- Ding W, LaPlant BR, Call TG, et al. Pembrolizumab in patients with CLL and Richter transformation or with relapsed CLL. Blood. 2017;129:3419-3427.
- Leiter U, Loquai C, Reinhardt L, et al. Immune checkpoint inhibition therapy for advanced skin cancer in patients with concomitant hematological malignancy: a retrospective multicenter DeCOG study of 84 patients. J Immunother Cancer. 2020;8:E000897.
- Becker LR, Aakhus AE, Reich HC, et al. A novel alternate dosing of vismodegib for treatment of patients with advanced basal cell carcinomas. JAMA Dermatol. 2017;153:321-322.
- Woltsche N, Pichler N, Wolf I, et al. Managing adverse effects by dose reduction during routine treatment of locally advanced basal cell carcinoma with the hedgehog inhibitor vismodegib: a single centre experience. J Eur Acad Dermatol Venereol. 2019;33:E144-E145.
- Wong C, Poblete-Lopez C, Vidimos A. Comparison of daily dosing versus Monday through Friday dosing of vismodegib for locally advanced basal cell carcinoma and basal cell nevus syndrome: a retrospective case series. J Am Acad Dermatol. 2020;82:1539-1542.
- Dréno B, Kunstfeld R, Hauschild A, et al. Two intermittent vismodegib dosing regimens in patients with multiple basal-cell carcinomas (MIKIE): a randomised, regimen-controlled, double-blind, phase 2 trial. Lancet Oncol. 2017;18:404-412.
- Schadendorf D, Hauschild A, Fosko S, et al. Quality-of-life analysis with intermittent vismodegib regimens in patients with multiple basal cell carcinomas: patient-reported outcomes from the MIKIE study. J Eur Acad Dermatol Venereol. 2020;34:E526-E529.
- Chanu P, Musib L, Wang X, et al. Vismodegib efficacy in advanced basal cell carcinoma maintained with 8-week dose interruptions: a model-based evaluation. J Invest Dermatol. 2021;141:930-933.
- Su MG, Potts LB, Tsai JH. Treatment of periocular basal cell carcinoma with neoadjuvant vismodegib. Am J Ophthalmol Case Rep. 2020;19:100755.
- González AR, Etchichury D, Gil ME, et al. Neoadjuvant vismodegib and Mohs micrographic surgery for locally advanced periocular basal cell carcinoma. Ophthalmic Plast Reconstr Surg. 2019;35:56-61.
- Sagiv O, Nagarajan P, Ferrarotto R, et al. Ocular preservation with neoadjuvant vismodegib in patients with locally advanced periocular basal cell carcinoma. Br J Ophthalmol. 2019;103:775-780.
- Ally MS, Aasi S, Wysong A, et al. An investigator-initiated open-label clinical trial of vismodegib as a neoadjuvant to surgery for high-risk basal cell carcinoma. J Am Acad Dermatol. 2014;71:904-911.e1.
- Kwon GP, Ally MS, Bailey-Healy I, et al. Update to an open-label clinical trial of vismodegib as neoadjuvant before surgery for high-risk basal cell carcinoma (BCC). J Am Acad Dermatol. 2016;75:213-215.
- Mortier L, Bertrand N, Basset-Seguin N, et al. Vismodegib in neoadjuvant treatment of locally advanced basal cell carcinoma: first results of a multicenter, open-label, phase 2 trial (VISMONEO study) [abstract]. J Clin Oncol. 2018;36(15 suppl):9509.
- Strasswimmer JM. Potential synergy of radiation therapy with vismodegib for basal cell carcinoma. JAMA Dermatol. 2015;151:925-926.
- Gathings RM, Orscheln CS, Huang WW. Compassionate use of vismodegib and adjuvant radiotherapy in the treatment of multiple locally advanced and inoperable basal cell carcinomas and squamous cell carcinomas of the skin. J Am Acad Dermatol. 2014;70:E88-E89.
- Franco AI, Eastwick G, Farah R, et al. Upfront radiotherapy with concurrent and adjuvant vismodegib is effective and well-tolerated in a patient with advanced, multifocal basal cell carcinoma. Case Rep Dermatol Med. 2018;2018:2354146.
- Pollom EL, Bui TT, Chang AL, et al. Concurrent vismodegib and radiotherapy for recurrent, advanced basal cell carcinoma. JAMA Dermatol. 2015;151:998-1001.
- Janela-Lapert R, Dubray B, Duval-Modeste A, et al. Treatment of advanced basal cell carcinoma with vismodegib followed by radiotherapy [in French]. Ann Dermatol Venereol. 2020;147:780-782.
- Hehlgans S, Booms P, Güllülü Ö, et al. Radiation sensitization of basal cell and head and neck squamous cell carcinoma by the hedgehog pathway inhibitor vismodegib. Int J Mol Sci. 2018;19:2485.
- Kim J, Tang JY, Gong R, et al. Itraconazole, a commonly used antifungal that inhibits hedgehog pathway activity and cancer growth. Cancer Cell. 2010;17:388-399.
- Kim J, Aftab BT, Tang JY, et al. Itraconazole and arsenic trioxide inhibit hedgehog pathway activation and tumor growth associated with acquired resistance to smoothened antagonists. Cancer Cell. 2013;23:23-34.
- Kim DJ, Kim J, Spaunhurst K, et al. Open-label, exploratory phase II trial of oral itraconazole for the treatment of basal cell carcinoma. J Clin Oncol. 2014;32:745-751.
- Ally MS, Ransohoff K, Sarin K, et al. Effects of combined treatment with arsenic trioxide and itraconazole in patients with refractory metastatic basal cell carcinoma. JAMA Dermatol. 2016;152:452-456.
- Cia˛z˙yn´yska M, Narbutt J, Skibin´ska M, et al. Itraconazole—a new player in the therapy of advanced basal cell carcinoma: a case report. JCO Oncol Pract. 2020;16:837-838.
- Sohn GK, Kwon GP, Bailey-Healy I, et al. Topical itraconazole for the treatment of basal cell carcinoma in patients with basal cell nevus syndrome or high-frequency basal cell carcinomas: a phase 2, open-label, placebo-controlled trial. JAMA Dermatol. 2019;155:1078-1080.
- Lass-Flörl C. Triazole antifungal agents in invasive fungal infections: a comparative review. Drugs. 2011;71:2405-2419.
- Chen B, Trang V, Lee A, et al. Posaconazole, a second-generation triazole antifungal drug, inhibits the hedgehog signaling pathway and progression of basal cell carcinoma. Mol Cancer Ther. 2016;15:866-876.
- Katragkou A, Tsikopoulou F, Roilides E, et al. Posaconazole: when and how? the clinician’s view. Mycoses. 2012;55:110-122.
- Raad II, Graybill JR, Bustamante AB, et al. Safety of long-term oral posaconazole use in the treatment of refractory invasive fungal infections. Clin Infect Dis. 2006;42:1726-1734.
- Atwood SX, Sarin KY, Whitson RJ, et al. Smoothened variants explain the majority of drug resistance in basal cell carcinoma. Cancer Cell. 2015;27:342-353.
- Sun Q, Atzmony L, Zaki T, et al. Clues to primary vismodegib resistance lie in histology and genetics. J Clin Pathol. 2020;73:678-680.
- Verkouteren BJA, Wakkee M, van Geel M, et al. Molecular testing in metastatic basal cell carcinoma. J Am Acad Dermatol. 2021;85:1135-1142.
- Danial C, Sarin KY, Oro AE, et al. An investigator-initiated open-label trial of sonidegib in advanced basal cell carcinoma patients resistant to vismodegib. Clin Cancer Res. 2016;22:1325-1329.
- Yoon J, Apicelli AJ 3rd, Pavlopoulos TV. Intracranial regression of an advanced basal cell carcinoma using sonidegib and itraconazole after failure with vismodegib. JAAD Case Rep. 2017;4:10-12.
- Bendell J, Andre V, Ho A, et al. Phase I study of LY2940680, a Smo antagonist, in patients with advanced cancer including treatment-naïve and previously treated basal cell carcinoma. Clin Cancer Res. 2018;24:2082-2091.
- Ueno H, Kondo S, Yoshikawa S, et al. A phase I and pharmacokinetic study of taladegib, a Smoothened inhibitor, in Japanese patients with advanced solid tumors. Invest New Drugs. 2018;36:647-656.
- Herms F, Lambert J, Grob JJ, et al. Follow-up of patients with complete remission of locally advanced basal cell carcinoma after vismodegib discontinuation: a multicenter French study of 116 patients. J Clin Oncol. 2019;37:3275-3282.
- Villani A, Megna M, Fabbrocini G, et al. Long-term efficacy of vismodegib after its withdrawal and patients’ health-related quality of life using the Dermatology Life Quality Index (DLQI). Dermatol Ther (Heidelb). 2019;9:719-724.
- Scalvenzi M, Cappello M, Costa C, et al. Low-dose vismodegib as maintenance therapy after locally advanced basal cell carcinoma complete remission: high efficacy with minimal toxicity. Dermatol Ther (Heidelb). 2020;10:465-468.
Practice Points
- The sonic hedgehog (SHH) inhibitors vismodegib and sonidegib currently are the only 2 oral medications approved by the US Food and Drug Administration for the first-line treatment of locally advanced basal cell carcinoma (BCC). Vismodegib also is approved for metastatic BCC.
- Cemiplimab, a programmed cell death protein 1 inhibitor, is now an approved treatment for patients with advanced BCC refractory or intolerant to SHH inhibitor therapy.
- Adverse effects of SHH inhibitors, most commonly muscle spasms, often lead to treatment discontinuation, but intermittent dosing regimens can be used to increase tolerability and adherence.
- Combining SHH inhibitors with radiotherapy or antifungal therapy as well as maintenance dosing strategies may help reduce the risk of recurrence.
- Neoadjuvant administration of a SHH inhibitor may enable surgical excision of previously inoperable cases through tumor shrinkage.
No more ‘escape hatch’: Post Roe, new worries about meds linked to birth defects
As states ban or limit abortion in the wake of the demise of Roe v. Wade, physicians are turning their attention to widely-used drugs that can cause birth defects. At issue: Should these drugs still be prescribed to women of childbearing age if they don’t have the option of terminating their pregnancies?
“Doctors are going to understandably be terrified that a patient may become pregnant using a teratogen that they have prescribed,” said University of Pittsburgh rheumatologist Mehret Birru Talabi, MD, PhD, who works in a state where the future of abortion rights is uncertain. “While this was a feared outcome before Roe v. Wade was overturned, abortion provided an escape hatch by which women could avoid having to continue a pregnancy and potentially raise a child with congenital anomalies. I believe that prescribing is going to become much more defensive and conservative. Some clinicians may choose not to prescribe these medications to patients who have childbearing potential, even if they don’t have much risk for pregnancy.”
Other physicians expressed similar concerns in interviews. Duke University, Durham, N.C., rheumatologist Megan E. B. Clowse, MD, MPH, fears that physicians will be wary of prescribing a variety of medications – including new ones for which there are few pregnancy data – if abortion is unavailable. “Women who receive these new or teratogenic medications will likely lose their reproductive autonomy and be forced to choose between having sexual relationships with men, obtaining procedures that make them permanently sterile, or using contraception that may cause intolerable side effects,” she said. “I am very concerned that young women with rheumatic disease will now be left with active disease resulting in joint damage and renal failure.”
Abortion is now banned in at least six states, according to The New York Times. That number may rise to 16 as more restrictions become law. Another five states aren’t expected to ban abortion soon but have implemented gestational age limits on abortion or are expected to adopt them. In another nine states, courts or lawmakers will decide whether abortion remains legal.
Only 20 states and the District of Columbia have firm abortion protections in place.
Numerous drugs are considered teratogens, which means they may cause birth defects. Thalidomide is the most infamous, but there are many more, including several used in rheumatology, dermatology, and gastroenterology. Among the most widely used teratogenic medications are the acne drugs isotretinoin and methotrexate, which are used to treat a variety of conditions, such as cancer, rheumatoid arthritis, and psoriasis.
Dr. Clowse, who helps manage an industry-supported website devoted to reproductive care for women with lupus (www.LupusPregnancy.org), noted that several drugs linked to birth defects and pregnancy loss are commonly prescribed in rheumatology.
“Methotrexate is the most common medication and has been the cornerstone of rheumatoid arthritis [treatment] for at least two decades,” she said. “Mycophenolate is our best medication to treat lupus nephritis, which is inflammation in the kidneys caused by lupus. This is a common complication for young women with lupus, and all of our guideline-recommended treatment regimens include a medication that causes pregnancy loss and birth defects, either mycophenolate or cyclophosphamide.”
Rheumatologists also prescribe a large number of new drugs for which there are few data about pregnancy risks. “It typically takes about two decades to have sufficient data about the safety of our medications,” she said.
Reflecting the sensitivity of the topic, Dr. Clowse made clear that her opinions don’t represent the views of her institution. She works in North Carolina, where the fate of abortion rights is uncertain, according to The New York Times.
What about alternatives? “The short answer is that some of these medications work really well and sometimes much better than the nonteratogenic alternatives,” said Dr. Birru Talabi. “I’m worried about methotrexate. It has been used to induce abortions but is primarily used in the United States as a highly effective treatment for cancer as well as a myriad of rheumatic diseases. If legislators try to restrict access to methotrexate, we may see increasing disability and even death among people who need this medication but cannot access it.”
Rheumatologists aren’t the only physicians who are worrying about the fates of their patients in a new era of abortion restrictions. Gastroenterologist Sunanda Kane, MD, MSPH, of the Mayo Clinic, Rochester, Minn., said several teratogenic medications are used in her field to treat constipation, viral hepatitis, and inflammatory bowel disease.
“When treating women of childbearing age, there are usually alternatives. If we do prescribe a medication with a high teratogenic potential, we counsel and document that we have discussed two forms of birth control to avoid pregnancy. We usually do not prescribe a drug with teratogenic potential with the ‘out’ being an abortion if a pregnancy does occur,” she said. However, “if abortion is not even on the table as an option, we may be much less likely to prescribe these medications. This will be particularly true in patients who clearly do not have the means to travel to have an abortion in any situation.”
Abortion is expected to remain legal in Minnesota, where Dr. Kane practices, but it may be restricted or banned in nearby Wisconsin, depending on the state legislature. None of her patients have had abortions after becoming pregnant while taking the medications, she said, although she “did have a patient who because of her religious faith did not have an abortion after exposure and ended up with a stillbirth.”
The crackdown on abortion won’t just pose risks to patients who take potentially dangerous medications, physicians said. Dr. Kane said pregnancy itself is a significant risk for patients with “very active, uncontrolled gastrointestinal conditions where a pregnancy could be harmful to the mother’s health or result in offspring that are very unhealthy.” These include decompensated cirrhosis, uncontrolled Crohn’s disease or ulcerative colitis, refractory gastroparesis, uncontrolled celiac sprue, and chronic pancreatitis, she said.
“There have been times when after shared decisionmaking, a patient with very active inflammatory bowel disease has decided to terminate the pregnancy because of her own ongoing health issues,” she said. “Not having this option will potentially lead to disastrous results.”
Dr. Clowse, the Duke University rheumatologist, echoed Dr. Kane’s concerns about women who are too sick to bear children. “The removal of abortion rights puts the lives and quality of life for women with rheumatic disease at risk. For patients with lupus and other systemic rheumatic disease, pregnancy can be medically catastrophic, leading to permanent harm and even death to the woman and her offspring. I am worried that women in these conditions will die without lifesaving pregnancy terminations, due to worries about the legal consequences for their physicians.”
The U.S. Supreme Court’s ruling that overturned Roe v. Wade has also raised the prospect that the court could ultimately allow birth control to be restricted or outlawed.
While the ruling states that “nothing in this opinion should be understood to cast doubt on precedents that do not concern abortion,” Justice Clarence Thomas wrote a concurrence in which he said that the court should reconsider a 1960s ruling that forbids the banning of contraceptives. Republicans have dismissed concerns about bans being allowed, although Democrats, including the president and vice president, starkly warn that they could happen.
“If we as providers have to be concerned that there will be an unplanned pregnancy because of the lack of access to contraception,” Dr. Kane said, “this will have significant downstream consequences to the kind of care we can provide and might just drive some providers to not give care to female patients at all given this concern.”
The physicians quoted in this article report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As states ban or limit abortion in the wake of the demise of Roe v. Wade, physicians are turning their attention to widely-used drugs that can cause birth defects. At issue: Should these drugs still be prescribed to women of childbearing age if they don’t have the option of terminating their pregnancies?
“Doctors are going to understandably be terrified that a patient may become pregnant using a teratogen that they have prescribed,” said University of Pittsburgh rheumatologist Mehret Birru Talabi, MD, PhD, who works in a state where the future of abortion rights is uncertain. “While this was a feared outcome before Roe v. Wade was overturned, abortion provided an escape hatch by which women could avoid having to continue a pregnancy and potentially raise a child with congenital anomalies. I believe that prescribing is going to become much more defensive and conservative. Some clinicians may choose not to prescribe these medications to patients who have childbearing potential, even if they don’t have much risk for pregnancy.”
Other physicians expressed similar concerns in interviews. Duke University, Durham, N.C., rheumatologist Megan E. B. Clowse, MD, MPH, fears that physicians will be wary of prescribing a variety of medications – including new ones for which there are few pregnancy data – if abortion is unavailable. “Women who receive these new or teratogenic medications will likely lose their reproductive autonomy and be forced to choose between having sexual relationships with men, obtaining procedures that make them permanently sterile, or using contraception that may cause intolerable side effects,” she said. “I am very concerned that young women with rheumatic disease will now be left with active disease resulting in joint damage and renal failure.”
Abortion is now banned in at least six states, according to The New York Times. That number may rise to 16 as more restrictions become law. Another five states aren’t expected to ban abortion soon but have implemented gestational age limits on abortion or are expected to adopt them. In another nine states, courts or lawmakers will decide whether abortion remains legal.
Only 20 states and the District of Columbia have firm abortion protections in place.
Numerous drugs are considered teratogens, which means they may cause birth defects. Thalidomide is the most infamous, but there are many more, including several used in rheumatology, dermatology, and gastroenterology. Among the most widely used teratogenic medications are the acne drugs isotretinoin and methotrexate, which are used to treat a variety of conditions, such as cancer, rheumatoid arthritis, and psoriasis.
Dr. Clowse, who helps manage an industry-supported website devoted to reproductive care for women with lupus (www.LupusPregnancy.org), noted that several drugs linked to birth defects and pregnancy loss are commonly prescribed in rheumatology.
“Methotrexate is the most common medication and has been the cornerstone of rheumatoid arthritis [treatment] for at least two decades,” she said. “Mycophenolate is our best medication to treat lupus nephritis, which is inflammation in the kidneys caused by lupus. This is a common complication for young women with lupus, and all of our guideline-recommended treatment regimens include a medication that causes pregnancy loss and birth defects, either mycophenolate or cyclophosphamide.”
Rheumatologists also prescribe a large number of new drugs for which there are few data about pregnancy risks. “It typically takes about two decades to have sufficient data about the safety of our medications,” she said.
Reflecting the sensitivity of the topic, Dr. Clowse made clear that her opinions don’t represent the views of her institution. She works in North Carolina, where the fate of abortion rights is uncertain, according to The New York Times.
What about alternatives? “The short answer is that some of these medications work really well and sometimes much better than the nonteratogenic alternatives,” said Dr. Birru Talabi. “I’m worried about methotrexate. It has been used to induce abortions but is primarily used in the United States as a highly effective treatment for cancer as well as a myriad of rheumatic diseases. If legislators try to restrict access to methotrexate, we may see increasing disability and even death among people who need this medication but cannot access it.”
Rheumatologists aren’t the only physicians who are worrying about the fates of their patients in a new era of abortion restrictions. Gastroenterologist Sunanda Kane, MD, MSPH, of the Mayo Clinic, Rochester, Minn., said several teratogenic medications are used in her field to treat constipation, viral hepatitis, and inflammatory bowel disease.
“When treating women of childbearing age, there are usually alternatives. If we do prescribe a medication with a high teratogenic potential, we counsel and document that we have discussed two forms of birth control to avoid pregnancy. We usually do not prescribe a drug with teratogenic potential with the ‘out’ being an abortion if a pregnancy does occur,” she said. However, “if abortion is not even on the table as an option, we may be much less likely to prescribe these medications. This will be particularly true in patients who clearly do not have the means to travel to have an abortion in any situation.”
Abortion is expected to remain legal in Minnesota, where Dr. Kane practices, but it may be restricted or banned in nearby Wisconsin, depending on the state legislature. None of her patients have had abortions after becoming pregnant while taking the medications, she said, although she “did have a patient who because of her religious faith did not have an abortion after exposure and ended up with a stillbirth.”
The crackdown on abortion won’t just pose risks to patients who take potentially dangerous medications, physicians said. Dr. Kane said pregnancy itself is a significant risk for patients with “very active, uncontrolled gastrointestinal conditions where a pregnancy could be harmful to the mother’s health or result in offspring that are very unhealthy.” These include decompensated cirrhosis, uncontrolled Crohn’s disease or ulcerative colitis, refractory gastroparesis, uncontrolled celiac sprue, and chronic pancreatitis, she said.
“There have been times when after shared decisionmaking, a patient with very active inflammatory bowel disease has decided to terminate the pregnancy because of her own ongoing health issues,” she said. “Not having this option will potentially lead to disastrous results.”
Dr. Clowse, the Duke University rheumatologist, echoed Dr. Kane’s concerns about women who are too sick to bear children. “The removal of abortion rights puts the lives and quality of life for women with rheumatic disease at risk. For patients with lupus and other systemic rheumatic disease, pregnancy can be medically catastrophic, leading to permanent harm and even death to the woman and her offspring. I am worried that women in these conditions will die without lifesaving pregnancy terminations, due to worries about the legal consequences for their physicians.”
The U.S. Supreme Court’s ruling that overturned Roe v. Wade has also raised the prospect that the court could ultimately allow birth control to be restricted or outlawed.
While the ruling states that “nothing in this opinion should be understood to cast doubt on precedents that do not concern abortion,” Justice Clarence Thomas wrote a concurrence in which he said that the court should reconsider a 1960s ruling that forbids the banning of contraceptives. Republicans have dismissed concerns about bans being allowed, although Democrats, including the president and vice president, starkly warn that they could happen.
“If we as providers have to be concerned that there will be an unplanned pregnancy because of the lack of access to contraception,” Dr. Kane said, “this will have significant downstream consequences to the kind of care we can provide and might just drive some providers to not give care to female patients at all given this concern.”
The physicians quoted in this article report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As states ban or limit abortion in the wake of the demise of Roe v. Wade, physicians are turning their attention to widely-used drugs that can cause birth defects. At issue: Should these drugs still be prescribed to women of childbearing age if they don’t have the option of terminating their pregnancies?
“Doctors are going to understandably be terrified that a patient may become pregnant using a teratogen that they have prescribed,” said University of Pittsburgh rheumatologist Mehret Birru Talabi, MD, PhD, who works in a state where the future of abortion rights is uncertain. “While this was a feared outcome before Roe v. Wade was overturned, abortion provided an escape hatch by which women could avoid having to continue a pregnancy and potentially raise a child with congenital anomalies. I believe that prescribing is going to become much more defensive and conservative. Some clinicians may choose not to prescribe these medications to patients who have childbearing potential, even if they don’t have much risk for pregnancy.”
Other physicians expressed similar concerns in interviews. Duke University, Durham, N.C., rheumatologist Megan E. B. Clowse, MD, MPH, fears that physicians will be wary of prescribing a variety of medications – including new ones for which there are few pregnancy data – if abortion is unavailable. “Women who receive these new or teratogenic medications will likely lose their reproductive autonomy and be forced to choose between having sexual relationships with men, obtaining procedures that make them permanently sterile, or using contraception that may cause intolerable side effects,” she said. “I am very concerned that young women with rheumatic disease will now be left with active disease resulting in joint damage and renal failure.”
Abortion is now banned in at least six states, according to The New York Times. That number may rise to 16 as more restrictions become law. Another five states aren’t expected to ban abortion soon but have implemented gestational age limits on abortion or are expected to adopt them. In another nine states, courts or lawmakers will decide whether abortion remains legal.
Only 20 states and the District of Columbia have firm abortion protections in place.
Numerous drugs are considered teratogens, which means they may cause birth defects. Thalidomide is the most infamous, but there are many more, including several used in rheumatology, dermatology, and gastroenterology. Among the most widely used teratogenic medications are the acne drugs isotretinoin and methotrexate, which are used to treat a variety of conditions, such as cancer, rheumatoid arthritis, and psoriasis.
Dr. Clowse, who helps manage an industry-supported website devoted to reproductive care for women with lupus (www.LupusPregnancy.org), noted that several drugs linked to birth defects and pregnancy loss are commonly prescribed in rheumatology.
“Methotrexate is the most common medication and has been the cornerstone of rheumatoid arthritis [treatment] for at least two decades,” she said. “Mycophenolate is our best medication to treat lupus nephritis, which is inflammation in the kidneys caused by lupus. This is a common complication for young women with lupus, and all of our guideline-recommended treatment regimens include a medication that causes pregnancy loss and birth defects, either mycophenolate or cyclophosphamide.”
Rheumatologists also prescribe a large number of new drugs for which there are few data about pregnancy risks. “It typically takes about two decades to have sufficient data about the safety of our medications,” she said.
Reflecting the sensitivity of the topic, Dr. Clowse made clear that her opinions don’t represent the views of her institution. She works in North Carolina, where the fate of abortion rights is uncertain, according to The New York Times.
What about alternatives? “The short answer is that some of these medications work really well and sometimes much better than the nonteratogenic alternatives,” said Dr. Birru Talabi. “I’m worried about methotrexate. It has been used to induce abortions but is primarily used in the United States as a highly effective treatment for cancer as well as a myriad of rheumatic diseases. If legislators try to restrict access to methotrexate, we may see increasing disability and even death among people who need this medication but cannot access it.”
Rheumatologists aren’t the only physicians who are worrying about the fates of their patients in a new era of abortion restrictions. Gastroenterologist Sunanda Kane, MD, MSPH, of the Mayo Clinic, Rochester, Minn., said several teratogenic medications are used in her field to treat constipation, viral hepatitis, and inflammatory bowel disease.
“When treating women of childbearing age, there are usually alternatives. If we do prescribe a medication with a high teratogenic potential, we counsel and document that we have discussed two forms of birth control to avoid pregnancy. We usually do not prescribe a drug with teratogenic potential with the ‘out’ being an abortion if a pregnancy does occur,” she said. However, “if abortion is not even on the table as an option, we may be much less likely to prescribe these medications. This will be particularly true in patients who clearly do not have the means to travel to have an abortion in any situation.”
Abortion is expected to remain legal in Minnesota, where Dr. Kane practices, but it may be restricted or banned in nearby Wisconsin, depending on the state legislature. None of her patients have had abortions after becoming pregnant while taking the medications, she said, although she “did have a patient who because of her religious faith did not have an abortion after exposure and ended up with a stillbirth.”
The crackdown on abortion won’t just pose risks to patients who take potentially dangerous medications, physicians said. Dr. Kane said pregnancy itself is a significant risk for patients with “very active, uncontrolled gastrointestinal conditions where a pregnancy could be harmful to the mother’s health or result in offspring that are very unhealthy.” These include decompensated cirrhosis, uncontrolled Crohn’s disease or ulcerative colitis, refractory gastroparesis, uncontrolled celiac sprue, and chronic pancreatitis, she said.
“There have been times when after shared decisionmaking, a patient with very active inflammatory bowel disease has decided to terminate the pregnancy because of her own ongoing health issues,” she said. “Not having this option will potentially lead to disastrous results.”
Dr. Clowse, the Duke University rheumatologist, echoed Dr. Kane’s concerns about women who are too sick to bear children. “The removal of abortion rights puts the lives and quality of life for women with rheumatic disease at risk. For patients with lupus and other systemic rheumatic disease, pregnancy can be medically catastrophic, leading to permanent harm and even death to the woman and her offspring. I am worried that women in these conditions will die without lifesaving pregnancy terminations, due to worries about the legal consequences for their physicians.”
The U.S. Supreme Court’s ruling that overturned Roe v. Wade has also raised the prospect that the court could ultimately allow birth control to be restricted or outlawed.
While the ruling states that “nothing in this opinion should be understood to cast doubt on precedents that do not concern abortion,” Justice Clarence Thomas wrote a concurrence in which he said that the court should reconsider a 1960s ruling that forbids the banning of contraceptives. Republicans have dismissed concerns about bans being allowed, although Democrats, including the president and vice president, starkly warn that they could happen.
“If we as providers have to be concerned that there will be an unplanned pregnancy because of the lack of access to contraception,” Dr. Kane said, “this will have significant downstream consequences to the kind of care we can provide and might just drive some providers to not give care to female patients at all given this concern.”
The physicians quoted in this article report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rapidly Evolving Papulonodular Eruption in the Axilla
The Diagnosis: Lymphomatoid Papulosis
At the time of the initial visit, a punch biopsy was performed on the posterior shoulder girdle. Histopathology revealed mild epidermal spongiosis and acanthosis with associated parakeratosis and a dermal lymphocytic infiltrate with extravasated erythrocytes consistent with pityriasis rosea (Figure 1). Two weeks after the biopsy, the patient returned for suture removal and to discuss the biopsy results. The patient reported more evolving lesions despite completing the prescribed course of dicloxacillin. At this time, physical examination revealed the persistence of several reddishbrown papules along with new nodular lesions on the arms and thighs, some with central ulceration and crusting (Figure 2). A second biopsy of a nodular lesion on the right distal forearm was performed at this visit along with a superficial tissue culture, which was negative for bacterial or fungal elements. The biopsy revealed an atypical CD30+ lymphoid proliferation (Figure 3). These cells were strongly PD-L1 positive and also positive for CD3, CD4, and granzyme-B. Ki67 showed a high proliferation rate, and T-cell gene rearrangement studies were positive. Given these histologic findings and the clinical context of rapidly evolving skin lesions from small papules to nodular skin tumors, a diagnosis of lymphomatoid papulosis (LyP) was established.
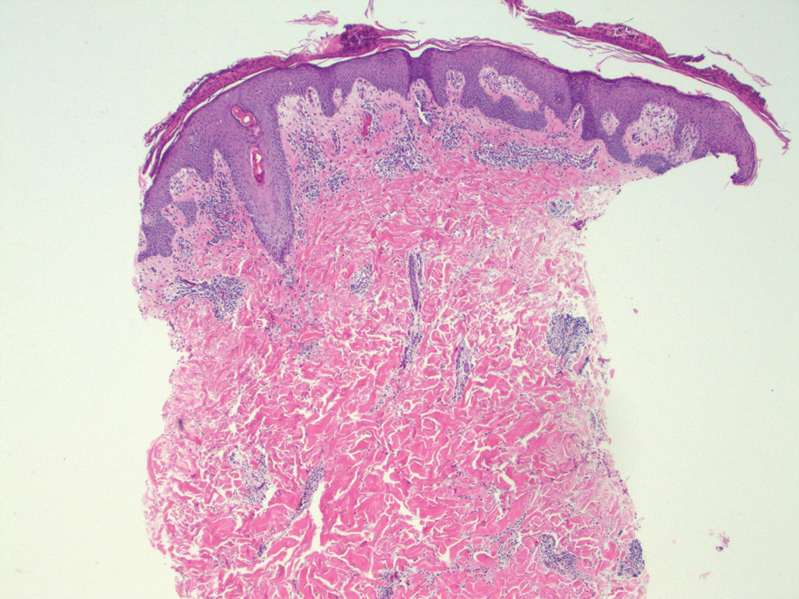
Because of the notable pathologic discordance between the 2 biopsy specimens, re-evaluation of the initial specimen was requested. The initial biopsy was subsequently found to be CD30+ with an identical peak on gene rearrangement studies as the second biopsy, further validating the diagnosis of LyP (Figure 4). Our patient was offered low-dose methotrexate therapy but declined the treatment plan, as the skin lesions had begun to resolve.

Lymphomatoid papulosis is a chronic CD30+ lymphoproliferative disorder with a characteristic recurrent and self-remitting disease course.1,2 Although it typically has a benign clinical course, it is histologically malignant and considered a low-grade variant of cutaneous T-cell lymphoma. 2,3 The classic clinical presentation of LyP involves the presence of reddish-brown papules and nodules typically measuring less than 2.0 cm, which may show evidence of central ulceration, hemorrhage, necrosis, and/or crust formation.1-5 It is characteristic that a patient may present with these skin lesions in different stages of evolution and that biopsies of these lesions may reflect different histologic features depending on the age of the lesion, making a definitive diagnosis more difficult to obtain if not clinically correlated.1,2 Any part of the body may be involved; however, there appears to be a predilection for the trunk and extremities in most cases.1-3,5 The skin eruptions usually are asymptomatic, but pruritus is a commonly associated concern.1,2,4,5
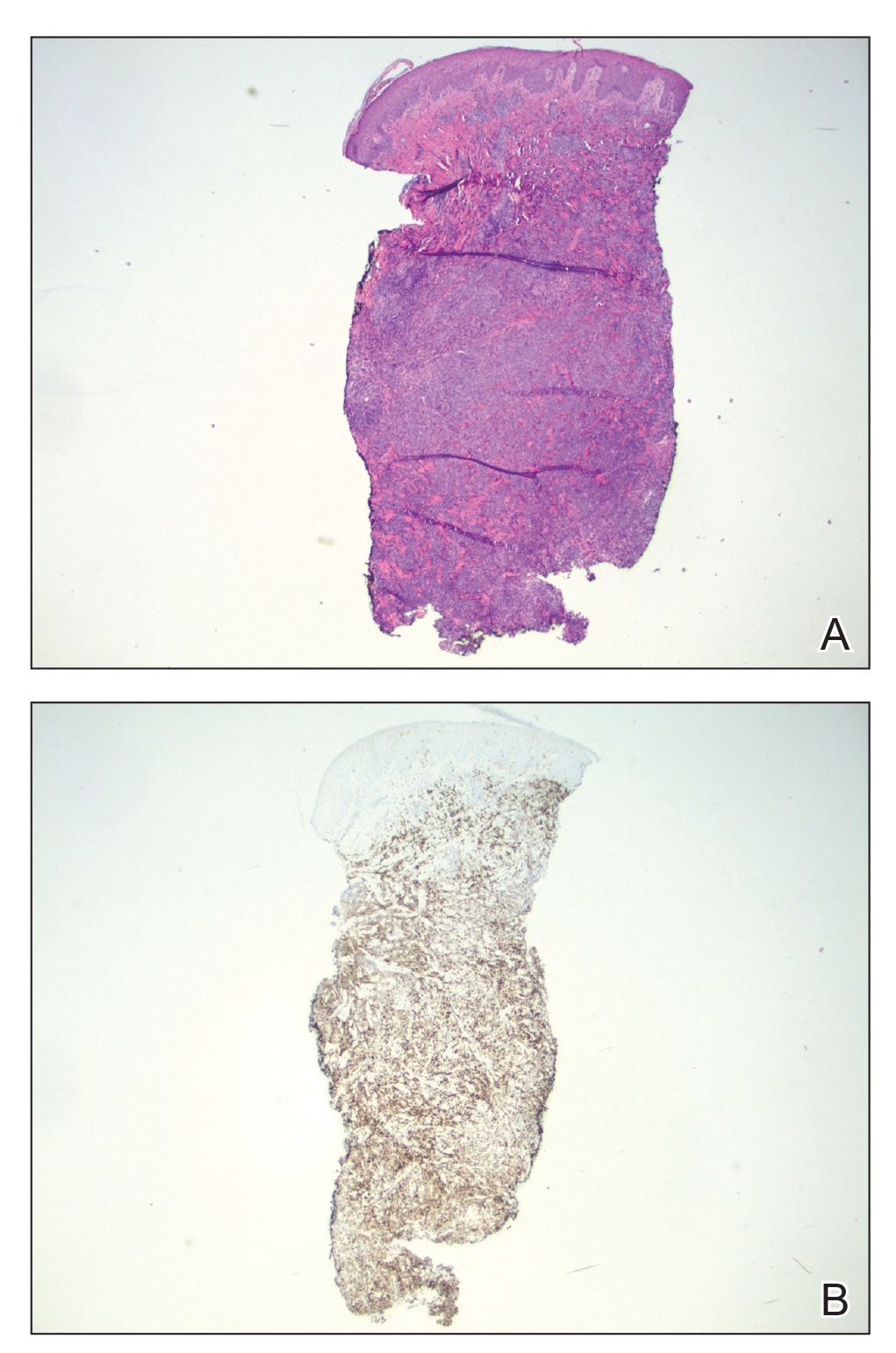
Lymphomatoid papulosis can have a localized, clustered, or generalized distribution pattern and typically will spontaneously regress without treatment within 3 to 12 weeks of symptom onset.2,3 Lymphomatoid papulosis has a slight male predominance with a male to female ratio of 1.5:1. It occurs most commonly between 35 and 45 years of age, though it can present at any age. The overall duration of the disease can range from months to decades.2,3 Lymphomatoid papulosis makes up approximately 15% of all cutaneous T-cell lymphomas.2,3 Although the overall prognosis is excellent, patients with LyP are at an increased risk of developing cutaneous or systemic lymphoma, most commonly mycosis fungoides, anaplastic large cell lymphoma, or Hodgkin lymphoma.1-3 This increased lifelong risk is the reason that patients with LyP must be followed long-term every 6 to 12 months for surveillance of emerging malignancy.1,2,6
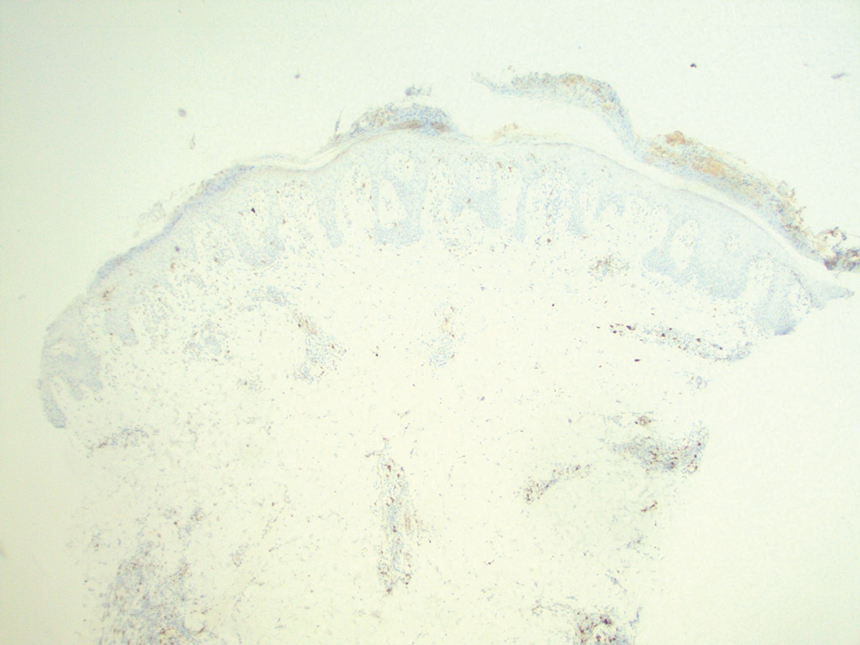
The pathogenesis of LyP remains unknown. Some have hypothesized a possible viral trigger; however, there is insufficient data to support this theory.2,6 A diagnostic hallmark of LyP is its CD30 positivity, which is a known marker for T-cell activation.6 The spontaneous regression of skin lesions that is characteristic of LyP is believed to involve the interactions between CD30 and its ligand (CD30L), which may contribute to apoptosis of neoplastic T cells.2,3,6 With regards to the possible mechanisms contributing to tumor progression in LyP, a mutation in the transforming growth factor β receptor gene on CD30+ tumor cells within LyP lesions may allow for these cells to evade growth regulation and progress to lymphoma.2,6 A large percentage of LyP biopsy specimens show evidence of T-cell receptor gene monoclonal rearrangement, which can aid in establishing a diagnosis.1,2
The histologic features of LyP can vary greatly depending on the age of the lesion sampled.1,2 Histologic subtypes of LyP have been established, with type A being the most common (approximately 75% of cases), displaying a wedge-shaped infiltrate of scattered or clustered, large, atypical CD30+ T cells.1,2 Types B through E vary in histologic features, with the exception that all subtypes contain a CD30+ lymphocytic infiltrate.2,3
Treatment of LyP depends on the symptom/disease burden that the patient is experiencing. For patients with a limited number of nonscarring skin lesions in areas that are not cosmetically sensitive, observation is recommended. 1-3 For symptomatic patients with an extensive number of lesions, particularly those that may be scarring and/or in cosmetically sensitive areas, low-dose oral methotrexate therapy is considered first-line treatment.1-4 A methotrexate dose of 5 to 20 mg weekly can be effective in reducing the number and severity of lesions, with duration of treatment depending on clinical response.1,2 For patients who have contraindications to or who cannot tolerate oral methotrexate, phototherapy using psoralen plus UVA twice weekly for 6 to 8 weeks is another treatment option.1,2 Topical corticosteroids also can be used in children or for patients experiencing substantial pruritus.1,2,4 Oral or topical retinoids, topical carmustine or mechlorethamine, and brentuximab (an anti-CD30 monoclonal antibody) are all alternative therapies that have shown some beneficial effects.1,2 In the event that any of the skin lesions do not spontaneously regress within a 3- to 12-week time frame, surgical excision or radiotherapy can be performed on those lesions.2
Primary cutaneous anaplastic large cell lymphoma (C-ALCL) is another CD30+ lymphoproliferative disorder with overlapping clinical and histopathological features of LyP. Recurrent crops of multiple lesions favor a diagnosis of LyP, whereas solitary lesions favor C-ALCL; however, multifocal C-ALCL cases may occur.2 Mycosis fungoides is the most common type of cutaneous T-cell lymphoma that characteristically presents in a patch, plaque, tumor progression. Although mycosis fungoides eventually may transform into a CD30+ lymphoma, our patient did not display the characteristic clinical progression to suggest this diagnosis. Pityriasis lichenoides et varioliformis acuta and pityriasis lichenoides chronica also fall into the spectrum of clonal T-cell cutaneous disorders that more commonly affect the pediatric population. Pityriasis lichenoides et varioliformis acuta has a marked CD8+ lymphocyte infiltrate, whereas pityriasis lichenoides chronica has more CD4+ lymphocytes. These disorders typically do not stain positive for CD30.2
All patients with a diagnosis of LyP should maintain lifelong, regular, 6- to 12-month follow-up visits to monitor disease status and screen for any evidence of developing malignancy.1,2,6 A thorough review of clinical history, complete skin examination, and physical examination with a particular focus on detection of lymphadenopathy and hepatosplenomegaly should be included at every followup visit.1 Systemic symptoms such as fever, night sweats, or weight loss are not typical features of LyP; therefore, patients who begin to develop these symptoms should be promptly evaluated for systemic lymphoma.1
- Kadin ME. Lymphomatoid papulosis. UpToDate website. Accessed June 4, 2022. https://www.uptodate.com/contents/lymphomatoid-papulosis
- Willemze R. Cutaneous T-cell lymphoma. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. Vol 2. 4th ed. Elsevier Saunders; 2017:2141-2143.
- Wiznia LE, Cohen JM, Beasley JM, et al. Lymphomatoid papulosis. Dermatol Online J. 2018;24:13030/qt4xt046c9.
- Wieser I, Oh CW, Talpur R, et al. Lymphomatoid papulosis: treatment response and associated lymphomas in a study of 180 patients. J Am Acad Dermatol. 2016;74:59-67. doi:10.1016/j.jaad.2015.09.013
- Wolff K, Johnson RA, Saavedra AP, et al. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 8th ed. McGraw-Hill Education; 2017.
- Kunishige JH, McDonald H, Alvarez G, et al. Lymphomatoid papulosis and associated lymphomas: a retrospective case series of 84 patients. Clin Exp Dermatol. 2009;34:576-581. doi:10.1111 /j.1365-2230.2008.03024.x
The Diagnosis: Lymphomatoid Papulosis
At the time of the initial visit, a punch biopsy was performed on the posterior shoulder girdle. Histopathology revealed mild epidermal spongiosis and acanthosis with associated parakeratosis and a dermal lymphocytic infiltrate with extravasated erythrocytes consistent with pityriasis rosea (Figure 1). Two weeks after the biopsy, the patient returned for suture removal and to discuss the biopsy results. The patient reported more evolving lesions despite completing the prescribed course of dicloxacillin. At this time, physical examination revealed the persistence of several reddishbrown papules along with new nodular lesions on the arms and thighs, some with central ulceration and crusting (Figure 2). A second biopsy of a nodular lesion on the right distal forearm was performed at this visit along with a superficial tissue culture, which was negative for bacterial or fungal elements. The biopsy revealed an atypical CD30+ lymphoid proliferation (Figure 3). These cells were strongly PD-L1 positive and also positive for CD3, CD4, and granzyme-B. Ki67 showed a high proliferation rate, and T-cell gene rearrangement studies were positive. Given these histologic findings and the clinical context of rapidly evolving skin lesions from small papules to nodular skin tumors, a diagnosis of lymphomatoid papulosis (LyP) was established.
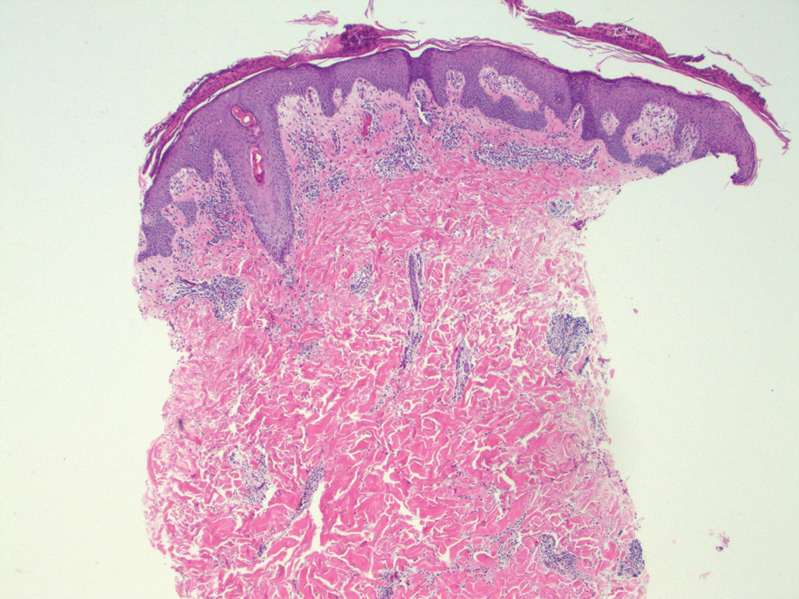
Because of the notable pathologic discordance between the 2 biopsy specimens, re-evaluation of the initial specimen was requested. The initial biopsy was subsequently found to be CD30+ with an identical peak on gene rearrangement studies as the second biopsy, further validating the diagnosis of LyP (Figure 4). Our patient was offered low-dose methotrexate therapy but declined the treatment plan, as the skin lesions had begun to resolve.

Lymphomatoid papulosis is a chronic CD30+ lymphoproliferative disorder with a characteristic recurrent and self-remitting disease course.1,2 Although it typically has a benign clinical course, it is histologically malignant and considered a low-grade variant of cutaneous T-cell lymphoma. 2,3 The classic clinical presentation of LyP involves the presence of reddish-brown papules and nodules typically measuring less than 2.0 cm, which may show evidence of central ulceration, hemorrhage, necrosis, and/or crust formation.1-5 It is characteristic that a patient may present with these skin lesions in different stages of evolution and that biopsies of these lesions may reflect different histologic features depending on the age of the lesion, making a definitive diagnosis more difficult to obtain if not clinically correlated.1,2 Any part of the body may be involved; however, there appears to be a predilection for the trunk and extremities in most cases.1-3,5 The skin eruptions usually are asymptomatic, but pruritus is a commonly associated concern.1,2,4,5
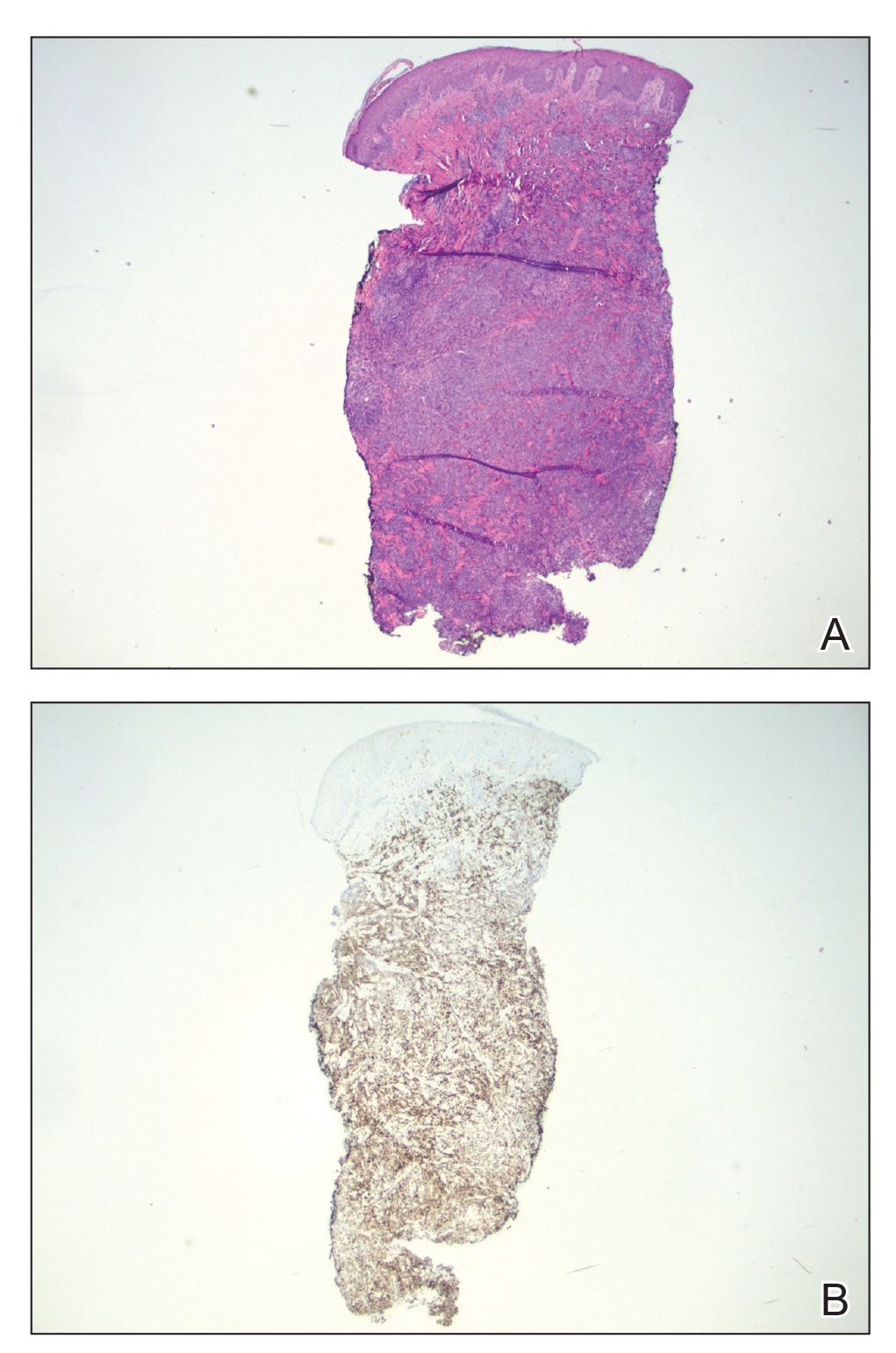
Lymphomatoid papulosis can have a localized, clustered, or generalized distribution pattern and typically will spontaneously regress without treatment within 3 to 12 weeks of symptom onset.2,3 Lymphomatoid papulosis has a slight male predominance with a male to female ratio of 1.5:1. It occurs most commonly between 35 and 45 years of age, though it can present at any age. The overall duration of the disease can range from months to decades.2,3 Lymphomatoid papulosis makes up approximately 15% of all cutaneous T-cell lymphomas.2,3 Although the overall prognosis is excellent, patients with LyP are at an increased risk of developing cutaneous or systemic lymphoma, most commonly mycosis fungoides, anaplastic large cell lymphoma, or Hodgkin lymphoma.1-3 This increased lifelong risk is the reason that patients with LyP must be followed long-term every 6 to 12 months for surveillance of emerging malignancy.1,2,6
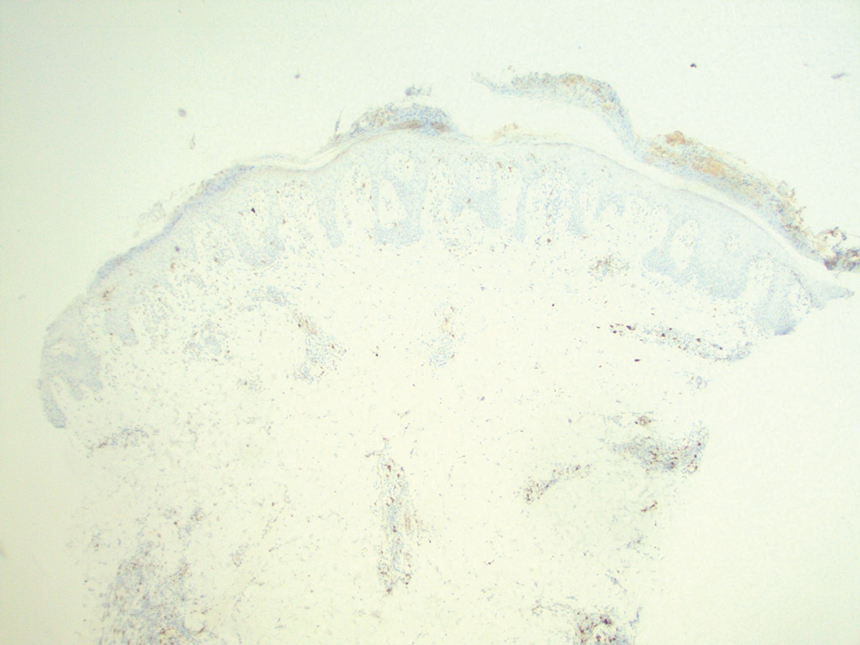
The pathogenesis of LyP remains unknown. Some have hypothesized a possible viral trigger; however, there is insufficient data to support this theory.2,6 A diagnostic hallmark of LyP is its CD30 positivity, which is a known marker for T-cell activation.6 The spontaneous regression of skin lesions that is characteristic of LyP is believed to involve the interactions between CD30 and its ligand (CD30L), which may contribute to apoptosis of neoplastic T cells.2,3,6 With regards to the possible mechanisms contributing to tumor progression in LyP, a mutation in the transforming growth factor β receptor gene on CD30+ tumor cells within LyP lesions may allow for these cells to evade growth regulation and progress to lymphoma.2,6 A large percentage of LyP biopsy specimens show evidence of T-cell receptor gene monoclonal rearrangement, which can aid in establishing a diagnosis.1,2
The histologic features of LyP can vary greatly depending on the age of the lesion sampled.1,2 Histologic subtypes of LyP have been established, with type A being the most common (approximately 75% of cases), displaying a wedge-shaped infiltrate of scattered or clustered, large, atypical CD30+ T cells.1,2 Types B through E vary in histologic features, with the exception that all subtypes contain a CD30+ lymphocytic infiltrate.2,3
Treatment of LyP depends on the symptom/disease burden that the patient is experiencing. For patients with a limited number of nonscarring skin lesions in areas that are not cosmetically sensitive, observation is recommended. 1-3 For symptomatic patients with an extensive number of lesions, particularly those that may be scarring and/or in cosmetically sensitive areas, low-dose oral methotrexate therapy is considered first-line treatment.1-4 A methotrexate dose of 5 to 20 mg weekly can be effective in reducing the number and severity of lesions, with duration of treatment depending on clinical response.1,2 For patients who have contraindications to or who cannot tolerate oral methotrexate, phototherapy using psoralen plus UVA twice weekly for 6 to 8 weeks is another treatment option.1,2 Topical corticosteroids also can be used in children or for patients experiencing substantial pruritus.1,2,4 Oral or topical retinoids, topical carmustine or mechlorethamine, and brentuximab (an anti-CD30 monoclonal antibody) are all alternative therapies that have shown some beneficial effects.1,2 In the event that any of the skin lesions do not spontaneously regress within a 3- to 12-week time frame, surgical excision or radiotherapy can be performed on those lesions.2
Primary cutaneous anaplastic large cell lymphoma (C-ALCL) is another CD30+ lymphoproliferative disorder with overlapping clinical and histopathological features of LyP. Recurrent crops of multiple lesions favor a diagnosis of LyP, whereas solitary lesions favor C-ALCL; however, multifocal C-ALCL cases may occur.2 Mycosis fungoides is the most common type of cutaneous T-cell lymphoma that characteristically presents in a patch, plaque, tumor progression. Although mycosis fungoides eventually may transform into a CD30+ lymphoma, our patient did not display the characteristic clinical progression to suggest this diagnosis. Pityriasis lichenoides et varioliformis acuta and pityriasis lichenoides chronica also fall into the spectrum of clonal T-cell cutaneous disorders that more commonly affect the pediatric population. Pityriasis lichenoides et varioliformis acuta has a marked CD8+ lymphocyte infiltrate, whereas pityriasis lichenoides chronica has more CD4+ lymphocytes. These disorders typically do not stain positive for CD30.2
All patients with a diagnosis of LyP should maintain lifelong, regular, 6- to 12-month follow-up visits to monitor disease status and screen for any evidence of developing malignancy.1,2,6 A thorough review of clinical history, complete skin examination, and physical examination with a particular focus on detection of lymphadenopathy and hepatosplenomegaly should be included at every followup visit.1 Systemic symptoms such as fever, night sweats, or weight loss are not typical features of LyP; therefore, patients who begin to develop these symptoms should be promptly evaluated for systemic lymphoma.1
The Diagnosis: Lymphomatoid Papulosis
At the time of the initial visit, a punch biopsy was performed on the posterior shoulder girdle. Histopathology revealed mild epidermal spongiosis and acanthosis with associated parakeratosis and a dermal lymphocytic infiltrate with extravasated erythrocytes consistent with pityriasis rosea (Figure 1). Two weeks after the biopsy, the patient returned for suture removal and to discuss the biopsy results. The patient reported more evolving lesions despite completing the prescribed course of dicloxacillin. At this time, physical examination revealed the persistence of several reddishbrown papules along with new nodular lesions on the arms and thighs, some with central ulceration and crusting (Figure 2). A second biopsy of a nodular lesion on the right distal forearm was performed at this visit along with a superficial tissue culture, which was negative for bacterial or fungal elements. The biopsy revealed an atypical CD30+ lymphoid proliferation (Figure 3). These cells were strongly PD-L1 positive and also positive for CD3, CD4, and granzyme-B. Ki67 showed a high proliferation rate, and T-cell gene rearrangement studies were positive. Given these histologic findings and the clinical context of rapidly evolving skin lesions from small papules to nodular skin tumors, a diagnosis of lymphomatoid papulosis (LyP) was established.
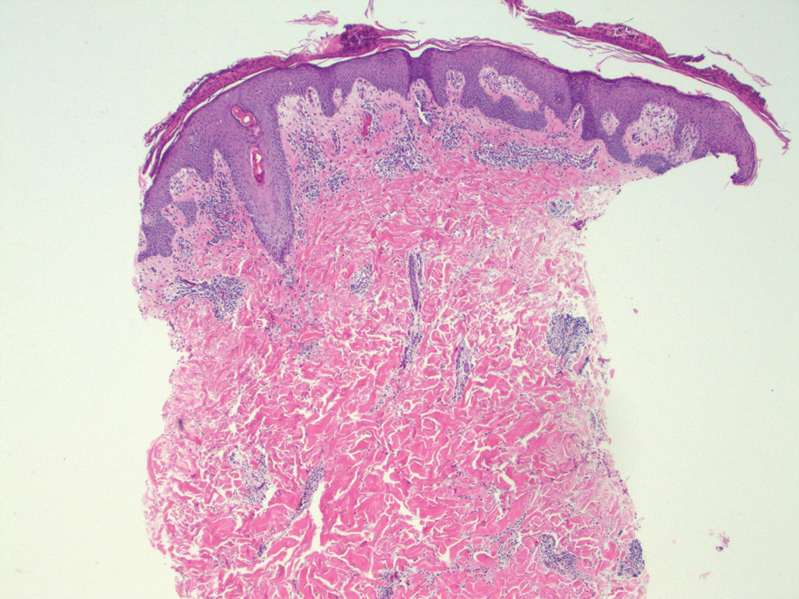
Because of the notable pathologic discordance between the 2 biopsy specimens, re-evaluation of the initial specimen was requested. The initial biopsy was subsequently found to be CD30+ with an identical peak on gene rearrangement studies as the second biopsy, further validating the diagnosis of LyP (Figure 4). Our patient was offered low-dose methotrexate therapy but declined the treatment plan, as the skin lesions had begun to resolve.

Lymphomatoid papulosis is a chronic CD30+ lymphoproliferative disorder with a characteristic recurrent and self-remitting disease course.1,2 Although it typically has a benign clinical course, it is histologically malignant and considered a low-grade variant of cutaneous T-cell lymphoma. 2,3 The classic clinical presentation of LyP involves the presence of reddish-brown papules and nodules typically measuring less than 2.0 cm, which may show evidence of central ulceration, hemorrhage, necrosis, and/or crust formation.1-5 It is characteristic that a patient may present with these skin lesions in different stages of evolution and that biopsies of these lesions may reflect different histologic features depending on the age of the lesion, making a definitive diagnosis more difficult to obtain if not clinically correlated.1,2 Any part of the body may be involved; however, there appears to be a predilection for the trunk and extremities in most cases.1-3,5 The skin eruptions usually are asymptomatic, but pruritus is a commonly associated concern.1,2,4,5
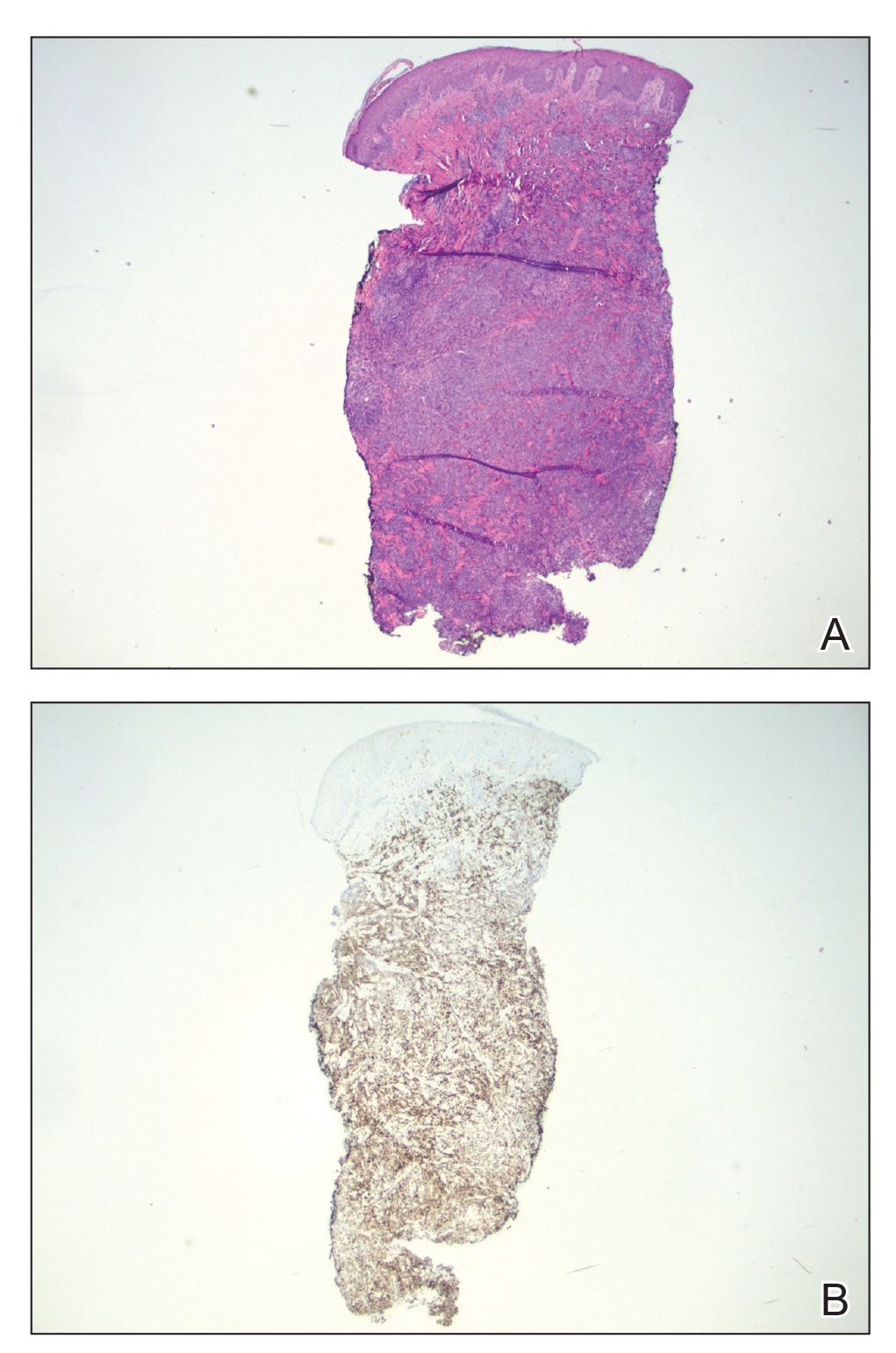
Lymphomatoid papulosis can have a localized, clustered, or generalized distribution pattern and typically will spontaneously regress without treatment within 3 to 12 weeks of symptom onset.2,3 Lymphomatoid papulosis has a slight male predominance with a male to female ratio of 1.5:1. It occurs most commonly between 35 and 45 years of age, though it can present at any age. The overall duration of the disease can range from months to decades.2,3 Lymphomatoid papulosis makes up approximately 15% of all cutaneous T-cell lymphomas.2,3 Although the overall prognosis is excellent, patients with LyP are at an increased risk of developing cutaneous or systemic lymphoma, most commonly mycosis fungoides, anaplastic large cell lymphoma, or Hodgkin lymphoma.1-3 This increased lifelong risk is the reason that patients with LyP must be followed long-term every 6 to 12 months for surveillance of emerging malignancy.1,2,6
The pathogenesis of LyP remains unknown. Some have hypothesized a possible viral trigger; however, there is insufficient data to support this theory.2,6 A diagnostic hallmark of LyP is its CD30 positivity, which is a known marker for T-cell activation.6 The spontaneous regression of skin lesions that is characteristic of LyP is believed to involve the interactions between CD30 and its ligand (CD30L), which may contribute to apoptosis of neoplastic T cells.2,3,6 With regards to the possible mechanisms contributing to tumor progression in LyP, a mutation in the transforming growth factor β receptor gene on CD30+ tumor cells within LyP lesions may allow for these cells to evade growth regulation and progress to lymphoma.2,6 A large percentage of LyP biopsy specimens show evidence of T-cell receptor gene monoclonal rearrangement, which can aid in establishing a diagnosis.1,2
The histologic features of LyP can vary greatly depending on the age of the lesion sampled.1,2 Histologic subtypes of LyP have been established, with type A being the most common (approximately 75% of cases), displaying a wedge-shaped infiltrate of scattered or clustered, large, atypical CD30+ T cells.1,2 Types B through E vary in histologic features, with the exception that all subtypes contain a CD30+ lymphocytic infiltrate.2,3
Treatment of LyP depends on the symptom/disease burden that the patient is experiencing. For patients with a limited number of nonscarring skin lesions in areas that are not cosmetically sensitive, observation is recommended. 1-3 For symptomatic patients with an extensive number of lesions, particularly those that may be scarring and/or in cosmetically sensitive areas, low-dose oral methotrexate therapy is considered first-line treatment.1-4 A methotrexate dose of 5 to 20 mg weekly can be effective in reducing the number and severity of lesions, with duration of treatment depending on clinical response.1,2 For patients who have contraindications to or who cannot tolerate oral methotrexate, phototherapy using psoralen plus UVA twice weekly for 6 to 8 weeks is another treatment option.1,2 Topical corticosteroids also can be used in children or for patients experiencing substantial pruritus.1,2,4 Oral or topical retinoids, topical carmustine or mechlorethamine, and brentuximab (an anti-CD30 monoclonal antibody) are all alternative therapies that have shown some beneficial effects.1,2 In the event that any of the skin lesions do not spontaneously regress within a 3- to 12-week time frame, surgical excision or radiotherapy can be performed on those lesions.2
Primary cutaneous anaplastic large cell lymphoma (C-ALCL) is another CD30+ lymphoproliferative disorder with overlapping clinical and histopathological features of LyP. Recurrent crops of multiple lesions favor a diagnosis of LyP, whereas solitary lesions favor C-ALCL; however, multifocal C-ALCL cases may occur.2 Mycosis fungoides is the most common type of cutaneous T-cell lymphoma that characteristically presents in a patch, plaque, tumor progression. Although mycosis fungoides eventually may transform into a CD30+ lymphoma, our patient did not display the characteristic clinical progression to suggest this diagnosis. Pityriasis lichenoides et varioliformis acuta and pityriasis lichenoides chronica also fall into the spectrum of clonal T-cell cutaneous disorders that more commonly affect the pediatric population. Pityriasis lichenoides et varioliformis acuta has a marked CD8+ lymphocyte infiltrate, whereas pityriasis lichenoides chronica has more CD4+ lymphocytes. These disorders typically do not stain positive for CD30.2
All patients with a diagnosis of LyP should maintain lifelong, regular, 6- to 12-month follow-up visits to monitor disease status and screen for any evidence of developing malignancy.1,2,6 A thorough review of clinical history, complete skin examination, and physical examination with a particular focus on detection of lymphadenopathy and hepatosplenomegaly should be included at every followup visit.1 Systemic symptoms such as fever, night sweats, or weight loss are not typical features of LyP; therefore, patients who begin to develop these symptoms should be promptly evaluated for systemic lymphoma.1
- Kadin ME. Lymphomatoid papulosis. UpToDate website. Accessed June 4, 2022. https://www.uptodate.com/contents/lymphomatoid-papulosis
- Willemze R. Cutaneous T-cell lymphoma. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. Vol 2. 4th ed. Elsevier Saunders; 2017:2141-2143.
- Wiznia LE, Cohen JM, Beasley JM, et al. Lymphomatoid papulosis. Dermatol Online J. 2018;24:13030/qt4xt046c9.
- Wieser I, Oh CW, Talpur R, et al. Lymphomatoid papulosis: treatment response and associated lymphomas in a study of 180 patients. J Am Acad Dermatol. 2016;74:59-67. doi:10.1016/j.jaad.2015.09.013
- Wolff K, Johnson RA, Saavedra AP, et al. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 8th ed. McGraw-Hill Education; 2017.
- Kunishige JH, McDonald H, Alvarez G, et al. Lymphomatoid papulosis and associated lymphomas: a retrospective case series of 84 patients. Clin Exp Dermatol. 2009;34:576-581. doi:10.1111 /j.1365-2230.2008.03024.x
- Kadin ME. Lymphomatoid papulosis. UpToDate website. Accessed June 4, 2022. https://www.uptodate.com/contents/lymphomatoid-papulosis
- Willemze R. Cutaneous T-cell lymphoma. In: Bolognia JL, Jorizzo JL, Schaffer JV, eds. Dermatology. Vol 2. 4th ed. Elsevier Saunders; 2017:2141-2143.
- Wiznia LE, Cohen JM, Beasley JM, et al. Lymphomatoid papulosis. Dermatol Online J. 2018;24:13030/qt4xt046c9.
- Wieser I, Oh CW, Talpur R, et al. Lymphomatoid papulosis: treatment response and associated lymphomas in a study of 180 patients. J Am Acad Dermatol. 2016;74:59-67. doi:10.1016/j.jaad.2015.09.013
- Wolff K, Johnson RA, Saavedra AP, et al. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 8th ed. McGraw-Hill Education; 2017.
- Kunishige JH, McDonald H, Alvarez G, et al. Lymphomatoid papulosis and associated lymphomas: a retrospective case series of 84 patients. Clin Exp Dermatol. 2009;34:576-581. doi:10.1111 /j.1365-2230.2008.03024.x
A 37-year-old woman presented to our dermatology clinic with a pruritic erythematous eruption involving the trunk, axillae, and proximal extremities of 10 days’ duration. Her medical history was notable only for eczema, and she denied taking any medications. Physical examination revealed scattered erythematous papules and crusts involving the trunk bilaterally and the extremities. We initially made a clinical diagnosis of bullous impetigo, and the patient was prescribed mupirocin ointment and dicloxacillin. At 1-week follow-up, the patient reported persistent skin lesions that were evolving despite therapy. Physical examination at this visit revealed an evolving eruption of multiple reddish-brown scaly papules involving the axillae, arms, forearms, and thighs, as depicted here.

Commentary: Support for the Use of Dupilumab in AD, and a Link Between AD and Depression, July 2022
First, Blauvelt and colleagues presented findings from the ongoing LIBERTY AD PED-OLE open-label extension study, including 294 adolescents with moderate to severe AD who participated in previous dupilumab trials. Patients received a maintenance dose of 300 mg dupilumab every 4 weeks, which was increased to a weight-based every-other-week regimen if there was inadequate clinical response to every-4-week dosing. They found that 81.2% of patients achieved an Eczema Area and Severity Index (EASI-75) response at week 52 with every-4-week dosing, and 51.9% of patients at week 48 after switching to every-2-week doing. These results indicate that some adolescents may be able to maintain clinical efficacy with monthly dosing, while others may require every-2-week dosing. Of note, no new safety signals emerged during the study and most adverse events were mild to moderate.
Two more studies were published showing real-world effectiveness and safety of dupilumab. Eichenfield and colleagues performed a retrospective, observational study of the effectiveness of dupilumab after 4 months of treatment using data from national electronic medical records in adults with moderate-to-severe AD. They found that most patients achieved at least a one-grade (81.8%) or two-grade (62.8%) improvement of their Investigator's Global Assessment (IGA) scores, with 42.8% achieving IGA scores of 0/1 (clear/minimal). There were also significant improvements in itch and lesional extent. The results were remarkably similar to those observed in the phase 3 clinical trial program of dupilumab in adults with moderate-to-severe AD.
Bagel and colleagues published baseline characteristics of patients enrolled in the ongoing PROSE longitudinal real-world registry of dupilumab use in adults with moderate-to-severe AD. Almost half of the patients (49.5%) previously received systemic medications, including 41.0% with systemic corticosteroids, 16.8% with nonsteroidal systemic therapies, such as cyclosporine and methotrexate, and 10.2% with phototherapy. This result indicates that many medical professionals are not using dupilumab as a first-line systemic therapy, despite its established record on safety and efficacy. It appears that many clinicians prefer a short-term treatment regimen, such as systemic corticosteroids, prior to initiating long-term treatment with dupilumab. However, short-term treatment approaches are not ideal for this chronic and often lifelong disease. It is important that clinicians develop appropriate long-term treatment approaches for atopic dermatitis in general, regardless of any specific therapy.
On a different research note, my research group just published the results of a longitudinal dermatology practice–based study of depressive symptoms in 695 adults with AD over time.1 We found that approximately half of the patients experienced fluctuating severity of depressive symptoms, and 45.65% experienced persistent severity of depression. Severity of AD lesions and itch were the strongest predictors of more severe symptoms of depression. Perhaps most fascinating about this research was that symptoms of depression improved dramatically in a very large subset of patients who experienced reduced AD severity with standard-of-care treatment. These results highlight the broader impacts of AD on mental health, which were recently recognized by the American Academy of Dermatology's guideline update on AD comorbidities.2 Moreover, our study demonstrated that many of these mental health impacts were modifiable with optimized AD therapy.
Additional References
1. Chatrath S, Lei D, Yousaf M, et al. vc Longitudinal course and predictors of depressive symptoms in atopic dermatitis. J Am Acad Dermatol. 2022 (May 9). Doi: 10.1016/j.jaad.2022.04.061
2. Davis DMR, Drucker AM, Alikhan A, et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86:1335-1336.e18. Doi: 10.1016/j.jaad.2022.01.009
First, Blauvelt and colleagues presented findings from the ongoing LIBERTY AD PED-OLE open-label extension study, including 294 adolescents with moderate to severe AD who participated in previous dupilumab trials. Patients received a maintenance dose of 300 mg dupilumab every 4 weeks, which was increased to a weight-based every-other-week regimen if there was inadequate clinical response to every-4-week dosing. They found that 81.2% of patients achieved an Eczema Area and Severity Index (EASI-75) response at week 52 with every-4-week dosing, and 51.9% of patients at week 48 after switching to every-2-week doing. These results indicate that some adolescents may be able to maintain clinical efficacy with monthly dosing, while others may require every-2-week dosing. Of note, no new safety signals emerged during the study and most adverse events were mild to moderate.
Two more studies were published showing real-world effectiveness and safety of dupilumab. Eichenfield and colleagues performed a retrospective, observational study of the effectiveness of dupilumab after 4 months of treatment using data from national electronic medical records in adults with moderate-to-severe AD. They found that most patients achieved at least a one-grade (81.8%) or two-grade (62.8%) improvement of their Investigator's Global Assessment (IGA) scores, with 42.8% achieving IGA scores of 0/1 (clear/minimal). There were also significant improvements in itch and lesional extent. The results were remarkably similar to those observed in the phase 3 clinical trial program of dupilumab in adults with moderate-to-severe AD.
Bagel and colleagues published baseline characteristics of patients enrolled in the ongoing PROSE longitudinal real-world registry of dupilumab use in adults with moderate-to-severe AD. Almost half of the patients (49.5%) previously received systemic medications, including 41.0% with systemic corticosteroids, 16.8% with nonsteroidal systemic therapies, such as cyclosporine and methotrexate, and 10.2% with phototherapy. This result indicates that many medical professionals are not using dupilumab as a first-line systemic therapy, despite its established record on safety and efficacy. It appears that many clinicians prefer a short-term treatment regimen, such as systemic corticosteroids, prior to initiating long-term treatment with dupilumab. However, short-term treatment approaches are not ideal for this chronic and often lifelong disease. It is important that clinicians develop appropriate long-term treatment approaches for atopic dermatitis in general, regardless of any specific therapy.
On a different research note, my research group just published the results of a longitudinal dermatology practice–based study of depressive symptoms in 695 adults with AD over time.1 We found that approximately half of the patients experienced fluctuating severity of depressive symptoms, and 45.65% experienced persistent severity of depression. Severity of AD lesions and itch were the strongest predictors of more severe symptoms of depression. Perhaps most fascinating about this research was that symptoms of depression improved dramatically in a very large subset of patients who experienced reduced AD severity with standard-of-care treatment. These results highlight the broader impacts of AD on mental health, which were recently recognized by the American Academy of Dermatology's guideline update on AD comorbidities.2 Moreover, our study demonstrated that many of these mental health impacts were modifiable with optimized AD therapy.
Additional References
1. Chatrath S, Lei D, Yousaf M, et al. vc Longitudinal course and predictors of depressive symptoms in atopic dermatitis. J Am Acad Dermatol. 2022 (May 9). Doi: 10.1016/j.jaad.2022.04.061
2. Davis DMR, Drucker AM, Alikhan A, et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86:1335-1336.e18. Doi: 10.1016/j.jaad.2022.01.009
First, Blauvelt and colleagues presented findings from the ongoing LIBERTY AD PED-OLE open-label extension study, including 294 adolescents with moderate to severe AD who participated in previous dupilumab trials. Patients received a maintenance dose of 300 mg dupilumab every 4 weeks, which was increased to a weight-based every-other-week regimen if there was inadequate clinical response to every-4-week dosing. They found that 81.2% of patients achieved an Eczema Area and Severity Index (EASI-75) response at week 52 with every-4-week dosing, and 51.9% of patients at week 48 after switching to every-2-week doing. These results indicate that some adolescents may be able to maintain clinical efficacy with monthly dosing, while others may require every-2-week dosing. Of note, no new safety signals emerged during the study and most adverse events were mild to moderate.
Two more studies were published showing real-world effectiveness and safety of dupilumab. Eichenfield and colleagues performed a retrospective, observational study of the effectiveness of dupilumab after 4 months of treatment using data from national electronic medical records in adults with moderate-to-severe AD. They found that most patients achieved at least a one-grade (81.8%) or two-grade (62.8%) improvement of their Investigator's Global Assessment (IGA) scores, with 42.8% achieving IGA scores of 0/1 (clear/minimal). There were also significant improvements in itch and lesional extent. The results were remarkably similar to those observed in the phase 3 clinical trial program of dupilumab in adults with moderate-to-severe AD.
Bagel and colleagues published baseline characteristics of patients enrolled in the ongoing PROSE longitudinal real-world registry of dupilumab use in adults with moderate-to-severe AD. Almost half of the patients (49.5%) previously received systemic medications, including 41.0% with systemic corticosteroids, 16.8% with nonsteroidal systemic therapies, such as cyclosporine and methotrexate, and 10.2% with phototherapy. This result indicates that many medical professionals are not using dupilumab as a first-line systemic therapy, despite its established record on safety and efficacy. It appears that many clinicians prefer a short-term treatment regimen, such as systemic corticosteroids, prior to initiating long-term treatment with dupilumab. However, short-term treatment approaches are not ideal for this chronic and often lifelong disease. It is important that clinicians develop appropriate long-term treatment approaches for atopic dermatitis in general, regardless of any specific therapy.
On a different research note, my research group just published the results of a longitudinal dermatology practice–based study of depressive symptoms in 695 adults with AD over time.1 We found that approximately half of the patients experienced fluctuating severity of depressive symptoms, and 45.65% experienced persistent severity of depression. Severity of AD lesions and itch were the strongest predictors of more severe symptoms of depression. Perhaps most fascinating about this research was that symptoms of depression improved dramatically in a very large subset of patients who experienced reduced AD severity with standard-of-care treatment. These results highlight the broader impacts of AD on mental health, which were recently recognized by the American Academy of Dermatology's guideline update on AD comorbidities.2 Moreover, our study demonstrated that many of these mental health impacts were modifiable with optimized AD therapy.
Additional References
1. Chatrath S, Lei D, Yousaf M, et al. vc Longitudinal course and predictors of depressive symptoms in atopic dermatitis. J Am Acad Dermatol. 2022 (May 9). Doi: 10.1016/j.jaad.2022.04.061
2. Davis DMR, Drucker AM, Alikhan A, et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86:1335-1336.e18. Doi: 10.1016/j.jaad.2022.01.009
Race drives disparities in life expectancy across states
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
FROM ANNALS OF INTERNAL MEDICINE
Study finds higher risk of skin cancer after childhood organ transplant
A large study showing an increased risk of keratinocyte carcinoma (KC) in children who receive a solid-organ transplant highlights the need for early education about risk reduction and more research to determine optimal timing for screening, say an investigator and two dermatologists with expertise in transplant-related skin issues.
The increased incidence of KC in pediatric transplant recipients is “really high, so we definitely know there’s risk there,” just as there is for adult recipients of solid-organ transplants, said Cathryn Sibbald, MD, MSc, a dermatologist at the Hospital for Sick Children in Toronto and coauthor of a research letter published in June in JAMA Dermatology.
For their study, Dr. Sibbald and her coinvestigators turned to the Ontario Health Insurance plan database, which covers health care for Canadian citizens and qualified residents in the province. They identified 951 patients younger than the age of 18 who received a solid-organ transplant between 1991 and 2004 at an Ontario hospital
They then used a validated health insurance claims–based algorithm to identify diagnoses of KC for the transplant recipients and for more than 5 million age-matched controls. KC, including squamous and basal cell carcinoma, is the most prevalent skin cancer for people who have had a solid-organ transplant.
Fifteen posttransplant KCs (10 patients, 1.1%) were reported a mean of 13.1 years after transplant, with none reported in the first 4 years. The mean age at transplant was 7.8 years, and the mean age at KC diagnosis was 25.2 years. Kidney transplants were the most common (42.1% of transplantations). Most of the transplants recipients (eight patients) who developed KC had kidney transplantation, and most of them had functional graft at the time of KC diagnosis.
Researchers found an increased incidence of KC compared with that of the general population (standardized incidence ratio, 9.09; 95% confidence interval, 5.48-15.08). And the risk for KC increased with time since transplant, with adjusted hazard ratios for KC of 3.63 (95% CI, 0.51-25.77) for 1-5 years, 5.14 (95% CI, 1.28-20.55) for 5-10 years, and 4.80 (95% CI, 2.29-10.08) for 10 years or more, compared with the control population.
Several years ago, another research team performed a similar population-based cohort study of adult transplant recipients in Ontario and found a 6.6-times increased risk of KC in transplant recipients compared with the general population.
Sun protection and skin cancer screening
In commenting on the study, Sarah Arron, MD, PhD, a San Francisco Bay area dermatologist and immediate past president of the International Immunosuppression and Transplant Skin Cancer Collaborative (www.itscc.org), said she feels “reassured” that young transplant patients tend not to develop the skin cancer until young adulthood.
A ”large study like this is important because the overall rate of KC is low in this age group,” she noted.
The findings “suggest that we can focus our efforts on prevention during childhood, with sun protection and skin cancer education,” she said. “Then, as these children move into adulthood, we can begin screening with skin examinations. Of course, [any child] with a skin lesion or mole that concerns their parents or transplant team should be referred to dermatology for evaluation.”
Pediatric transplant recipients and their parents are most interested in learning about skin cancer prevention either before or immediately after transplantation, according to a survey by other researchers.
Intervention studies needed
The increased risk of KC probably stems largely from immunosuppression, said Dr. Sibbald in an interview. “We know [this is the case] in the older population, and it’s likely true in the younger population as well that it’s one of the primary drivers,” she said.
More research to extensively analyze risk factors should come next, she said. This includes “the granularity of what [immunosuppressants and other] medications are received, and at what dose and for what periods of time, so we can calculate cumulative exposure and its relation to risk,” she said.
Kristin Bibee, MD, PhD, assistant professor of dermatology at Johns Hopkins University in Baltimore, said she’d like to see further studies “evaluate appropriate interventions, like sun-protective behavior in childhood and adolescence or immunosuppression modulation, to prevent malignancy development.”
The optimal time and intensity of screening for young transplant recipients must still be determined, both Dr. Bibee and Dr. Arron said. Patients deemed through further research to be at higher risk may need earlier and/or more intensive surveillance.
The role of race in skin cancer risk in this population is “one question the study leaves open,” said Dr. Arron. U.S. studies have shown that among adult transplant recipients White patients are “at highest risk for the ultraviolet-associated melanoma and squamous cell carcinoma, followed by Asian and Latino patients. African Americans have had the lowest risk, but some still developed skin cancer after transplant,” she said.
Prior studies of cancer in pediatric transplant recipients have reported primarily on internal malignant neoplasms, with limited data on KC, Dr. Sibbald and coauthors wrote. It is possible the incidence of KS is underestimated in the new study because of “undiagnosed or unreported KCs,” they noted.
The new study was funded by a grant from the Pediatric Dermatology Research Alliance and a Hospital for Sick Children grant. In disclosures, Dr. Sibbald reported to JAMA Dermatology receiving grants from the alliance and from Paediatric Consultants Partnership during the conduct of the study. Dr. Arron and Dr. Bibee both said they have no disclosures relevant to the study and its content.
A large study showing an increased risk of keratinocyte carcinoma (KC) in children who receive a solid-organ transplant highlights the need for early education about risk reduction and more research to determine optimal timing for screening, say an investigator and two dermatologists with expertise in transplant-related skin issues.
The increased incidence of KC in pediatric transplant recipients is “really high, so we definitely know there’s risk there,” just as there is for adult recipients of solid-organ transplants, said Cathryn Sibbald, MD, MSc, a dermatologist at the Hospital for Sick Children in Toronto and coauthor of a research letter published in June in JAMA Dermatology.
For their study, Dr. Sibbald and her coinvestigators turned to the Ontario Health Insurance plan database, which covers health care for Canadian citizens and qualified residents in the province. They identified 951 patients younger than the age of 18 who received a solid-organ transplant between 1991 and 2004 at an Ontario hospital
They then used a validated health insurance claims–based algorithm to identify diagnoses of KC for the transplant recipients and for more than 5 million age-matched controls. KC, including squamous and basal cell carcinoma, is the most prevalent skin cancer for people who have had a solid-organ transplant.
Fifteen posttransplant KCs (10 patients, 1.1%) were reported a mean of 13.1 years after transplant, with none reported in the first 4 years. The mean age at transplant was 7.8 years, and the mean age at KC diagnosis was 25.2 years. Kidney transplants were the most common (42.1% of transplantations). Most of the transplants recipients (eight patients) who developed KC had kidney transplantation, and most of them had functional graft at the time of KC diagnosis.
Researchers found an increased incidence of KC compared with that of the general population (standardized incidence ratio, 9.09; 95% confidence interval, 5.48-15.08). And the risk for KC increased with time since transplant, with adjusted hazard ratios for KC of 3.63 (95% CI, 0.51-25.77) for 1-5 years, 5.14 (95% CI, 1.28-20.55) for 5-10 years, and 4.80 (95% CI, 2.29-10.08) for 10 years or more, compared with the control population.
Several years ago, another research team performed a similar population-based cohort study of adult transplant recipients in Ontario and found a 6.6-times increased risk of KC in transplant recipients compared with the general population.
Sun protection and skin cancer screening
In commenting on the study, Sarah Arron, MD, PhD, a San Francisco Bay area dermatologist and immediate past president of the International Immunosuppression and Transplant Skin Cancer Collaborative (www.itscc.org), said she feels “reassured” that young transplant patients tend not to develop the skin cancer until young adulthood.
A ”large study like this is important because the overall rate of KC is low in this age group,” she noted.
The findings “suggest that we can focus our efforts on prevention during childhood, with sun protection and skin cancer education,” she said. “Then, as these children move into adulthood, we can begin screening with skin examinations. Of course, [any child] with a skin lesion or mole that concerns their parents or transplant team should be referred to dermatology for evaluation.”
Pediatric transplant recipients and their parents are most interested in learning about skin cancer prevention either before or immediately after transplantation, according to a survey by other researchers.
Intervention studies needed
The increased risk of KC probably stems largely from immunosuppression, said Dr. Sibbald in an interview. “We know [this is the case] in the older population, and it’s likely true in the younger population as well that it’s one of the primary drivers,” she said.
More research to extensively analyze risk factors should come next, she said. This includes “the granularity of what [immunosuppressants and other] medications are received, and at what dose and for what periods of time, so we can calculate cumulative exposure and its relation to risk,” she said.
Kristin Bibee, MD, PhD, assistant professor of dermatology at Johns Hopkins University in Baltimore, said she’d like to see further studies “evaluate appropriate interventions, like sun-protective behavior in childhood and adolescence or immunosuppression modulation, to prevent malignancy development.”
The optimal time and intensity of screening for young transplant recipients must still be determined, both Dr. Bibee and Dr. Arron said. Patients deemed through further research to be at higher risk may need earlier and/or more intensive surveillance.
The role of race in skin cancer risk in this population is “one question the study leaves open,” said Dr. Arron. U.S. studies have shown that among adult transplant recipients White patients are “at highest risk for the ultraviolet-associated melanoma and squamous cell carcinoma, followed by Asian and Latino patients. African Americans have had the lowest risk, but some still developed skin cancer after transplant,” she said.
Prior studies of cancer in pediatric transplant recipients have reported primarily on internal malignant neoplasms, with limited data on KC, Dr. Sibbald and coauthors wrote. It is possible the incidence of KS is underestimated in the new study because of “undiagnosed or unreported KCs,” they noted.
The new study was funded by a grant from the Pediatric Dermatology Research Alliance and a Hospital for Sick Children grant. In disclosures, Dr. Sibbald reported to JAMA Dermatology receiving grants from the alliance and from Paediatric Consultants Partnership during the conduct of the study. Dr. Arron and Dr. Bibee both said they have no disclosures relevant to the study and its content.
A large study showing an increased risk of keratinocyte carcinoma (KC) in children who receive a solid-organ transplant highlights the need for early education about risk reduction and more research to determine optimal timing for screening, say an investigator and two dermatologists with expertise in transplant-related skin issues.
The increased incidence of KC in pediatric transplant recipients is “really high, so we definitely know there’s risk there,” just as there is for adult recipients of solid-organ transplants, said Cathryn Sibbald, MD, MSc, a dermatologist at the Hospital for Sick Children in Toronto and coauthor of a research letter published in June in JAMA Dermatology.
For their study, Dr. Sibbald and her coinvestigators turned to the Ontario Health Insurance plan database, which covers health care for Canadian citizens and qualified residents in the province. They identified 951 patients younger than the age of 18 who received a solid-organ transplant between 1991 and 2004 at an Ontario hospital
They then used a validated health insurance claims–based algorithm to identify diagnoses of KC for the transplant recipients and for more than 5 million age-matched controls. KC, including squamous and basal cell carcinoma, is the most prevalent skin cancer for people who have had a solid-organ transplant.
Fifteen posttransplant KCs (10 patients, 1.1%) were reported a mean of 13.1 years after transplant, with none reported in the first 4 years. The mean age at transplant was 7.8 years, and the mean age at KC diagnosis was 25.2 years. Kidney transplants were the most common (42.1% of transplantations). Most of the transplants recipients (eight patients) who developed KC had kidney transplantation, and most of them had functional graft at the time of KC diagnosis.
Researchers found an increased incidence of KC compared with that of the general population (standardized incidence ratio, 9.09; 95% confidence interval, 5.48-15.08). And the risk for KC increased with time since transplant, with adjusted hazard ratios for KC of 3.63 (95% CI, 0.51-25.77) for 1-5 years, 5.14 (95% CI, 1.28-20.55) for 5-10 years, and 4.80 (95% CI, 2.29-10.08) for 10 years or more, compared with the control population.
Several years ago, another research team performed a similar population-based cohort study of adult transplant recipients in Ontario and found a 6.6-times increased risk of KC in transplant recipients compared with the general population.
Sun protection and skin cancer screening
In commenting on the study, Sarah Arron, MD, PhD, a San Francisco Bay area dermatologist and immediate past president of the International Immunosuppression and Transplant Skin Cancer Collaborative (www.itscc.org), said she feels “reassured” that young transplant patients tend not to develop the skin cancer until young adulthood.
A ”large study like this is important because the overall rate of KC is low in this age group,” she noted.
The findings “suggest that we can focus our efforts on prevention during childhood, with sun protection and skin cancer education,” she said. “Then, as these children move into adulthood, we can begin screening with skin examinations. Of course, [any child] with a skin lesion or mole that concerns their parents or transplant team should be referred to dermatology for evaluation.”
Pediatric transplant recipients and their parents are most interested in learning about skin cancer prevention either before or immediately after transplantation, according to a survey by other researchers.
Intervention studies needed
The increased risk of KC probably stems largely from immunosuppression, said Dr. Sibbald in an interview. “We know [this is the case] in the older population, and it’s likely true in the younger population as well that it’s one of the primary drivers,” she said.
More research to extensively analyze risk factors should come next, she said. This includes “the granularity of what [immunosuppressants and other] medications are received, and at what dose and for what periods of time, so we can calculate cumulative exposure and its relation to risk,” she said.
Kristin Bibee, MD, PhD, assistant professor of dermatology at Johns Hopkins University in Baltimore, said she’d like to see further studies “evaluate appropriate interventions, like sun-protective behavior in childhood and adolescence or immunosuppression modulation, to prevent malignancy development.”
The optimal time and intensity of screening for young transplant recipients must still be determined, both Dr. Bibee and Dr. Arron said. Patients deemed through further research to be at higher risk may need earlier and/or more intensive surveillance.
The role of race in skin cancer risk in this population is “one question the study leaves open,” said Dr. Arron. U.S. studies have shown that among adult transplant recipients White patients are “at highest risk for the ultraviolet-associated melanoma and squamous cell carcinoma, followed by Asian and Latino patients. African Americans have had the lowest risk, but some still developed skin cancer after transplant,” she said.
Prior studies of cancer in pediatric transplant recipients have reported primarily on internal malignant neoplasms, with limited data on KC, Dr. Sibbald and coauthors wrote. It is possible the incidence of KS is underestimated in the new study because of “undiagnosed or unreported KCs,” they noted.
The new study was funded by a grant from the Pediatric Dermatology Research Alliance and a Hospital for Sick Children grant. In disclosures, Dr. Sibbald reported to JAMA Dermatology receiving grants from the alliance and from Paediatric Consultants Partnership during the conduct of the study. Dr. Arron and Dr. Bibee both said they have no disclosures relevant to the study and its content.
FROM JAMA DERMATOLOGY













