User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Laser, Radiofrequency Therapies Offer Little Benefit for Genitourinary Syndrome of Menopause
CHICAGO — Use of CO2 lasers and similar “energy-based” treatments result in little to no benefit for genitourinary syndrome of menopause (GSM) symptoms, according to research presented at the The Menopause Society 2024 Annual Meeting in Chicago on September 12.
“There was a concern that menopausal women are being targeted for treatments that may not have a lot of benefit and might have significant harms,” Elisheva Danan, MD, MPH, a physician at the Minneapolis VA Health Care System and an assistant professor of medicine at the University of Minnesota Medical School in Minneapolis, told this news organization. While she was not surprised to find little evidence of benefit, “we were a little bit surprised that we also didn’t find significant evidence of harms.”
The study was unable to evaluate the potential for financial harms, but Dr. Danan noted that these therapies are often expensive and not typically covered by insurance. The treatments appear to be used primarily in private practice, she said, while “most academic clinicians were not familiar with these and do not use these lasers.”
The American Urological Association had requested the review, Dr. Danan said, “to inform clinical guidelines that they could put out for practitioners about treating genital urinary syndrome from menopause.” Yet the evidence available remains slim. “There’s a lot of outcomes that were not looked at by most of these [trials], or they were looked at in a way that we couldn’t separate out,” she said.
Kamalini Das, MD, a professor of ob.gyn. at the University of Minnesota who was not involved in the research, was surprised by the findings because studies to date have been variable, “but since this looks at multiple studies and they find no benefits, I would take these results as more significant than any of the small studies,” she told this news organization.
Dr. Das said she has patients who ask about using these therapies and have had them done. “So far, I’ve told them the jury is out on whether it will help or not, that there are some studies that say they’re beneficial and some studies that they’re not,” Dr. Das said.
But this new review changes what she will tell patients going forward, she said. “This is a good study because it consolidates lots of little studies, so I think I would use this to say, looking at all the studies together, this treatment is not beneficial.”
GSM occurs due to the body’s reduced production of estrogen and affects anywhere from 27% to 84% of postmenopausal women. It can involve a constellation of symptoms ranging from vaginal discomfort and irritation to painful urination or intercourse. Typical recommended treatments for GSM include systemic hormone therapy, localized hormonal treatments such as vaginal estrogen or dehydroepiandrosterone, nonhormonal creams and moisturizers, and the prescription drug ospemifene.
Most of these have been found effective, according to a recent systematic review Dr. Danan published in the Annals of Internal Medicine that this news organization covered. But recent years have also seen a rapid increase in interest and the availability of energy-based treatments for GSM, such as CO2 laser and radiofrequency interventions, particularly for those who cannot or do not want to use hormonal treatments. The idea behind these newer therapies is that they “heat tissue to cause a denaturation of collagen fibers and induce a wound-healing response,” with the aim of “enhancement of vaginal elasticity, restoration of premenopausal epithelial function, and symptom improvement,” the authors wrote.
Evidence has been scant and uneven for the safety and effectiveness of these treatments, and they have not been evaluated by the US Food and Drug Administration. The agency issued a warning in 2018 with remarks from then Commissioner Scott Gottlieb that the “products have serious risks and don’t have adequate evidence to support their use for these purposes.”
Much of the evidence has focused on CO2 lasers instead of other energy-based treatments, however, and a raft of new studies have been published on these interventions in the past 2 years. Dr. Danan and colleagues, therefore, assessed the most current state of the research with a systematic review of randomized controlled trials (RCTs) and prospective observational studies with control groups published through December 11, 2023.
Included studies needed to evaluate an energy-based treatment for at least 8 weeks in a minimum of 40 postmenopausal women (20 in each group) who had one or more GSM symptoms. The authors also included nonrandomized and uncontrolled studies with a follow-up of a year or more to assess possible adverse events. The studies also needed to assess at least one of eight core outcomes: Dyspareunia; vulvovaginal dryness; vulvovaginal discomfort/irritation; dysuria; change in most bothersome symptom; treatment satisfaction; adverse events; and distress, bother, or interference associated with genitourinary symptoms.
The authors identified 32 studies, including 16 RCTs, one quasi-RCT, and 15 nonrandomized studies. The researchers extracted and analyzed data from the 10 RCTs and one quasi-RCT that were rated as having low to moderate risk for bias.
Most of these studies assessed CO2 lasers alone, while three assessed erbium:yttrium-aluminum-garnet (Er:YAG) laser, and one looked at CO2 lasers vs radiofrequency treatments.
The average age of participants ranged from 56 to 64 years, and most trials were in the United States. Results showed that CO2 lasers led to little or no difference in dysuria, dyspareunia, or quality of life when compared with sham lasers. The CO2 laser therapy also showed little to no difference compared with vaginal estrogen creams for dyspareunia, dryness, discomfort/irritation, dysuria, or quality of life.
Most CO2 laser studies reported on most outcomes, but the Er:YAG studies tended to report only on quality of life and/or one or two other outcomes. The radiofrequency study only assessed dyspareunia and quality of life.
“Treatment effects on other outcomes and effects of Er:YAG laser or radiofrequency on any outcomes are very uncertain,” the authors reported. Few adverse events and no serious adverse events were reported based on 15 studies, including the additional non-RCTs that had follow-up for at least a year.
“There are case reports and other types of studies that have shown some bad outcomes using laser therapies, and we really wanted to be expansive and include anything, especially because this is such a new treatment and all these trials were in the last couple of years,” Dr. Danan said.
The review was limited by inconsistent or nonvalidated outcome reporting in the studies as well as small populations and short follow-up, typically less than 3 months.
The research was funded by the Agency for Healthcare Research and Quality and Patient-Centered Outcomes Research Institute. Dr. Danan and Dr. Das had no disclosures.
A version of this article first appeared on Medscape.com.
CHICAGO — Use of CO2 lasers and similar “energy-based” treatments result in little to no benefit for genitourinary syndrome of menopause (GSM) symptoms, according to research presented at the The Menopause Society 2024 Annual Meeting in Chicago on September 12.
“There was a concern that menopausal women are being targeted for treatments that may not have a lot of benefit and might have significant harms,” Elisheva Danan, MD, MPH, a physician at the Minneapolis VA Health Care System and an assistant professor of medicine at the University of Minnesota Medical School in Minneapolis, told this news organization. While she was not surprised to find little evidence of benefit, “we were a little bit surprised that we also didn’t find significant evidence of harms.”
The study was unable to evaluate the potential for financial harms, but Dr. Danan noted that these therapies are often expensive and not typically covered by insurance. The treatments appear to be used primarily in private practice, she said, while “most academic clinicians were not familiar with these and do not use these lasers.”
The American Urological Association had requested the review, Dr. Danan said, “to inform clinical guidelines that they could put out for practitioners about treating genital urinary syndrome from menopause.” Yet the evidence available remains slim. “There’s a lot of outcomes that were not looked at by most of these [trials], or they were looked at in a way that we couldn’t separate out,” she said.
Kamalini Das, MD, a professor of ob.gyn. at the University of Minnesota who was not involved in the research, was surprised by the findings because studies to date have been variable, “but since this looks at multiple studies and they find no benefits, I would take these results as more significant than any of the small studies,” she told this news organization.
Dr. Das said she has patients who ask about using these therapies and have had them done. “So far, I’ve told them the jury is out on whether it will help or not, that there are some studies that say they’re beneficial and some studies that they’re not,” Dr. Das said.
But this new review changes what she will tell patients going forward, she said. “This is a good study because it consolidates lots of little studies, so I think I would use this to say, looking at all the studies together, this treatment is not beneficial.”
GSM occurs due to the body’s reduced production of estrogen and affects anywhere from 27% to 84% of postmenopausal women. It can involve a constellation of symptoms ranging from vaginal discomfort and irritation to painful urination or intercourse. Typical recommended treatments for GSM include systemic hormone therapy, localized hormonal treatments such as vaginal estrogen or dehydroepiandrosterone, nonhormonal creams and moisturizers, and the prescription drug ospemifene.
Most of these have been found effective, according to a recent systematic review Dr. Danan published in the Annals of Internal Medicine that this news organization covered. But recent years have also seen a rapid increase in interest and the availability of energy-based treatments for GSM, such as CO2 laser and radiofrequency interventions, particularly for those who cannot or do not want to use hormonal treatments. The idea behind these newer therapies is that they “heat tissue to cause a denaturation of collagen fibers and induce a wound-healing response,” with the aim of “enhancement of vaginal elasticity, restoration of premenopausal epithelial function, and symptom improvement,” the authors wrote.
Evidence has been scant and uneven for the safety and effectiveness of these treatments, and they have not been evaluated by the US Food and Drug Administration. The agency issued a warning in 2018 with remarks from then Commissioner Scott Gottlieb that the “products have serious risks and don’t have adequate evidence to support their use for these purposes.”
Much of the evidence has focused on CO2 lasers instead of other energy-based treatments, however, and a raft of new studies have been published on these interventions in the past 2 years. Dr. Danan and colleagues, therefore, assessed the most current state of the research with a systematic review of randomized controlled trials (RCTs) and prospective observational studies with control groups published through December 11, 2023.
Included studies needed to evaluate an energy-based treatment for at least 8 weeks in a minimum of 40 postmenopausal women (20 in each group) who had one or more GSM symptoms. The authors also included nonrandomized and uncontrolled studies with a follow-up of a year or more to assess possible adverse events. The studies also needed to assess at least one of eight core outcomes: Dyspareunia; vulvovaginal dryness; vulvovaginal discomfort/irritation; dysuria; change in most bothersome symptom; treatment satisfaction; adverse events; and distress, bother, or interference associated with genitourinary symptoms.
The authors identified 32 studies, including 16 RCTs, one quasi-RCT, and 15 nonrandomized studies. The researchers extracted and analyzed data from the 10 RCTs and one quasi-RCT that were rated as having low to moderate risk for bias.
Most of these studies assessed CO2 lasers alone, while three assessed erbium:yttrium-aluminum-garnet (Er:YAG) laser, and one looked at CO2 lasers vs radiofrequency treatments.
The average age of participants ranged from 56 to 64 years, and most trials were in the United States. Results showed that CO2 lasers led to little or no difference in dysuria, dyspareunia, or quality of life when compared with sham lasers. The CO2 laser therapy also showed little to no difference compared with vaginal estrogen creams for dyspareunia, dryness, discomfort/irritation, dysuria, or quality of life.
Most CO2 laser studies reported on most outcomes, but the Er:YAG studies tended to report only on quality of life and/or one or two other outcomes. The radiofrequency study only assessed dyspareunia and quality of life.
“Treatment effects on other outcomes and effects of Er:YAG laser or radiofrequency on any outcomes are very uncertain,” the authors reported. Few adverse events and no serious adverse events were reported based on 15 studies, including the additional non-RCTs that had follow-up for at least a year.
“There are case reports and other types of studies that have shown some bad outcomes using laser therapies, and we really wanted to be expansive and include anything, especially because this is such a new treatment and all these trials were in the last couple of years,” Dr. Danan said.
The review was limited by inconsistent or nonvalidated outcome reporting in the studies as well as small populations and short follow-up, typically less than 3 months.
The research was funded by the Agency for Healthcare Research and Quality and Patient-Centered Outcomes Research Institute. Dr. Danan and Dr. Das had no disclosures.
A version of this article first appeared on Medscape.com.
CHICAGO — Use of CO2 lasers and similar “energy-based” treatments result in little to no benefit for genitourinary syndrome of menopause (GSM) symptoms, according to research presented at the The Menopause Society 2024 Annual Meeting in Chicago on September 12.
“There was a concern that menopausal women are being targeted for treatments that may not have a lot of benefit and might have significant harms,” Elisheva Danan, MD, MPH, a physician at the Minneapolis VA Health Care System and an assistant professor of medicine at the University of Minnesota Medical School in Minneapolis, told this news organization. While she was not surprised to find little evidence of benefit, “we were a little bit surprised that we also didn’t find significant evidence of harms.”
The study was unable to evaluate the potential for financial harms, but Dr. Danan noted that these therapies are often expensive and not typically covered by insurance. The treatments appear to be used primarily in private practice, she said, while “most academic clinicians were not familiar with these and do not use these lasers.”
The American Urological Association had requested the review, Dr. Danan said, “to inform clinical guidelines that they could put out for practitioners about treating genital urinary syndrome from menopause.” Yet the evidence available remains slim. “There’s a lot of outcomes that were not looked at by most of these [trials], or they were looked at in a way that we couldn’t separate out,” she said.
Kamalini Das, MD, a professor of ob.gyn. at the University of Minnesota who was not involved in the research, was surprised by the findings because studies to date have been variable, “but since this looks at multiple studies and they find no benefits, I would take these results as more significant than any of the small studies,” she told this news organization.
Dr. Das said she has patients who ask about using these therapies and have had them done. “So far, I’ve told them the jury is out on whether it will help or not, that there are some studies that say they’re beneficial and some studies that they’re not,” Dr. Das said.
But this new review changes what she will tell patients going forward, she said. “This is a good study because it consolidates lots of little studies, so I think I would use this to say, looking at all the studies together, this treatment is not beneficial.”
GSM occurs due to the body’s reduced production of estrogen and affects anywhere from 27% to 84% of postmenopausal women. It can involve a constellation of symptoms ranging from vaginal discomfort and irritation to painful urination or intercourse. Typical recommended treatments for GSM include systemic hormone therapy, localized hormonal treatments such as vaginal estrogen or dehydroepiandrosterone, nonhormonal creams and moisturizers, and the prescription drug ospemifene.
Most of these have been found effective, according to a recent systematic review Dr. Danan published in the Annals of Internal Medicine that this news organization covered. But recent years have also seen a rapid increase in interest and the availability of energy-based treatments for GSM, such as CO2 laser and radiofrequency interventions, particularly for those who cannot or do not want to use hormonal treatments. The idea behind these newer therapies is that they “heat tissue to cause a denaturation of collagen fibers and induce a wound-healing response,” with the aim of “enhancement of vaginal elasticity, restoration of premenopausal epithelial function, and symptom improvement,” the authors wrote.
Evidence has been scant and uneven for the safety and effectiveness of these treatments, and they have not been evaluated by the US Food and Drug Administration. The agency issued a warning in 2018 with remarks from then Commissioner Scott Gottlieb that the “products have serious risks and don’t have adequate evidence to support their use for these purposes.”
Much of the evidence has focused on CO2 lasers instead of other energy-based treatments, however, and a raft of new studies have been published on these interventions in the past 2 years. Dr. Danan and colleagues, therefore, assessed the most current state of the research with a systematic review of randomized controlled trials (RCTs) and prospective observational studies with control groups published through December 11, 2023.
Included studies needed to evaluate an energy-based treatment for at least 8 weeks in a minimum of 40 postmenopausal women (20 in each group) who had one or more GSM symptoms. The authors also included nonrandomized and uncontrolled studies with a follow-up of a year or more to assess possible adverse events. The studies also needed to assess at least one of eight core outcomes: Dyspareunia; vulvovaginal dryness; vulvovaginal discomfort/irritation; dysuria; change in most bothersome symptom; treatment satisfaction; adverse events; and distress, bother, or interference associated with genitourinary symptoms.
The authors identified 32 studies, including 16 RCTs, one quasi-RCT, and 15 nonrandomized studies. The researchers extracted and analyzed data from the 10 RCTs and one quasi-RCT that were rated as having low to moderate risk for bias.
Most of these studies assessed CO2 lasers alone, while three assessed erbium:yttrium-aluminum-garnet (Er:YAG) laser, and one looked at CO2 lasers vs radiofrequency treatments.
The average age of participants ranged from 56 to 64 years, and most trials were in the United States. Results showed that CO2 lasers led to little or no difference in dysuria, dyspareunia, or quality of life when compared with sham lasers. The CO2 laser therapy also showed little to no difference compared with vaginal estrogen creams for dyspareunia, dryness, discomfort/irritation, dysuria, or quality of life.
Most CO2 laser studies reported on most outcomes, but the Er:YAG studies tended to report only on quality of life and/or one or two other outcomes. The radiofrequency study only assessed dyspareunia and quality of life.
“Treatment effects on other outcomes and effects of Er:YAG laser or radiofrequency on any outcomes are very uncertain,” the authors reported. Few adverse events and no serious adverse events were reported based on 15 studies, including the additional non-RCTs that had follow-up for at least a year.
“There are case reports and other types of studies that have shown some bad outcomes using laser therapies, and we really wanted to be expansive and include anything, especially because this is such a new treatment and all these trials were in the last couple of years,” Dr. Danan said.
The review was limited by inconsistent or nonvalidated outcome reporting in the studies as well as small populations and short follow-up, typically less than 3 months.
The research was funded by the Agency for Healthcare Research and Quality and Patient-Centered Outcomes Research Institute. Dr. Danan and Dr. Das had no disclosures.
A version of this article first appeared on Medscape.com.
FROM THE MENOPAUSE SOCIETY 2024
Study Helps Define Patient-Centered Definition of Atopic Dermatitis Flares
TOPLINE:
, which most agreed would help when communicating with their healthcare providers (HCPs).
METHODOLOGY:
- To develop a patient-centered definition of AD flare, researchers used a modified eDelphi method, which involved a focus group and survey to reach consensus on key aspects of an AD flare.
- The focus group included 26 US adults aged ≥ 18 years with AD who had experienced a flare within the past 12 months. The survey was conducted among 631 adults with AD to validate the identified concepts and assess their agreement with the consensus statements.
- Participants rated 98 statements on a scale from 1 to 9, with consensus defined as at least 70% rating a statement as 7-9 and less than 15% rating it as 1-3.
- In focus groups, participants identified six key concepts for a patient-centered definition of flare, including changes from baseline, mental and emotional consequences, and physical changes in skin.
TAKEAWAY:
- The focus group reached consensus on 15 statements, and survey participants reached consensus on 12 of those statements defining an AD flare, with the highest agreement on symptoms taking more attention than normal, worsening of physical symptoms associated with AD, and worsening of itching associated with AD.
- The statement “acute worsening of symptoms of AD” was ranked as the most important, while “a worsening of physical symptoms” was ranked the least important.
- Most participants (79.7%) reported that prior definitions of AD flare did not resonate with them.
- More than half (52.9%) agreed with their HCP on what constitutes an AD flare, and the majority (77.6%) indicated that a patient-centered definition would be useful for communication with their HCP and for self-management.
IN PRACTICE:
“In this consensus survey study, we identified statements that are critical to the definition of an AD flare from the patient perspective,” the authors wrote. These findings, they added, “may be useful in clinical practice to improve communication between patients and HCPs who may be using the term flare without a mutual understanding of its meaning” and “may also be applied to the development of outcome measures focused on AD flares, which is an important treatment outcome for people with AD.”
SOURCE:
The study was led by Aaron M. Drucker, MD, ScM, of the Division of Dermatology, Department of Medicine, University of Toronto, Ontario, Canada, and was published online September 11 in JAMA Dermatology.
LIMITATIONS:
Participants had higher-than-average knowledge about AD, and the study’s findings may not be generalizable to all people with AD. The study included a higher proportion of moderate to severe AD cases than the general population, which may introduce responder bias. The findings may not be applicable to children, caregivers, or individuals in other countries.
DISCLOSURES:
This work was supported by a grant to the National Eczema Association from Pfizer. Dr. Drucker disclosed received compensation from the British Journal of Dermatology, American Academy of Dermatology, and Canadian Dermatology Today, and consultant fees from the National Eczema Association and Canadian Agency for Drugs and Technologies in Health. Another author reported receiving personal fees from pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, which most agreed would help when communicating with their healthcare providers (HCPs).
METHODOLOGY:
- To develop a patient-centered definition of AD flare, researchers used a modified eDelphi method, which involved a focus group and survey to reach consensus on key aspects of an AD flare.
- The focus group included 26 US adults aged ≥ 18 years with AD who had experienced a flare within the past 12 months. The survey was conducted among 631 adults with AD to validate the identified concepts and assess their agreement with the consensus statements.
- Participants rated 98 statements on a scale from 1 to 9, with consensus defined as at least 70% rating a statement as 7-9 and less than 15% rating it as 1-3.
- In focus groups, participants identified six key concepts for a patient-centered definition of flare, including changes from baseline, mental and emotional consequences, and physical changes in skin.
TAKEAWAY:
- The focus group reached consensus on 15 statements, and survey participants reached consensus on 12 of those statements defining an AD flare, with the highest agreement on symptoms taking more attention than normal, worsening of physical symptoms associated with AD, and worsening of itching associated with AD.
- The statement “acute worsening of symptoms of AD” was ranked as the most important, while “a worsening of physical symptoms” was ranked the least important.
- Most participants (79.7%) reported that prior definitions of AD flare did not resonate with them.
- More than half (52.9%) agreed with their HCP on what constitutes an AD flare, and the majority (77.6%) indicated that a patient-centered definition would be useful for communication with their HCP and for self-management.
IN PRACTICE:
“In this consensus survey study, we identified statements that are critical to the definition of an AD flare from the patient perspective,” the authors wrote. These findings, they added, “may be useful in clinical practice to improve communication between patients and HCPs who may be using the term flare without a mutual understanding of its meaning” and “may also be applied to the development of outcome measures focused on AD flares, which is an important treatment outcome for people with AD.”
SOURCE:
The study was led by Aaron M. Drucker, MD, ScM, of the Division of Dermatology, Department of Medicine, University of Toronto, Ontario, Canada, and was published online September 11 in JAMA Dermatology.
LIMITATIONS:
Participants had higher-than-average knowledge about AD, and the study’s findings may not be generalizable to all people with AD. The study included a higher proportion of moderate to severe AD cases than the general population, which may introduce responder bias. The findings may not be applicable to children, caregivers, or individuals in other countries.
DISCLOSURES:
This work was supported by a grant to the National Eczema Association from Pfizer. Dr. Drucker disclosed received compensation from the British Journal of Dermatology, American Academy of Dermatology, and Canadian Dermatology Today, and consultant fees from the National Eczema Association and Canadian Agency for Drugs and Technologies in Health. Another author reported receiving personal fees from pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
, which most agreed would help when communicating with their healthcare providers (HCPs).
METHODOLOGY:
- To develop a patient-centered definition of AD flare, researchers used a modified eDelphi method, which involved a focus group and survey to reach consensus on key aspects of an AD flare.
- The focus group included 26 US adults aged ≥ 18 years with AD who had experienced a flare within the past 12 months. The survey was conducted among 631 adults with AD to validate the identified concepts and assess their agreement with the consensus statements.
- Participants rated 98 statements on a scale from 1 to 9, with consensus defined as at least 70% rating a statement as 7-9 and less than 15% rating it as 1-3.
- In focus groups, participants identified six key concepts for a patient-centered definition of flare, including changes from baseline, mental and emotional consequences, and physical changes in skin.
TAKEAWAY:
- The focus group reached consensus on 15 statements, and survey participants reached consensus on 12 of those statements defining an AD flare, with the highest agreement on symptoms taking more attention than normal, worsening of physical symptoms associated with AD, and worsening of itching associated with AD.
- The statement “acute worsening of symptoms of AD” was ranked as the most important, while “a worsening of physical symptoms” was ranked the least important.
- Most participants (79.7%) reported that prior definitions of AD flare did not resonate with them.
- More than half (52.9%) agreed with their HCP on what constitutes an AD flare, and the majority (77.6%) indicated that a patient-centered definition would be useful for communication with their HCP and for self-management.
IN PRACTICE:
“In this consensus survey study, we identified statements that are critical to the definition of an AD flare from the patient perspective,” the authors wrote. These findings, they added, “may be useful in clinical practice to improve communication between patients and HCPs who may be using the term flare without a mutual understanding of its meaning” and “may also be applied to the development of outcome measures focused on AD flares, which is an important treatment outcome for people with AD.”
SOURCE:
The study was led by Aaron M. Drucker, MD, ScM, of the Division of Dermatology, Department of Medicine, University of Toronto, Ontario, Canada, and was published online September 11 in JAMA Dermatology.
LIMITATIONS:
Participants had higher-than-average knowledge about AD, and the study’s findings may not be generalizable to all people with AD. The study included a higher proportion of moderate to severe AD cases than the general population, which may introduce responder bias. The findings may not be applicable to children, caregivers, or individuals in other countries.
DISCLOSURES:
This work was supported by a grant to the National Eczema Association from Pfizer. Dr. Drucker disclosed received compensation from the British Journal of Dermatology, American Academy of Dermatology, and Canadian Dermatology Today, and consultant fees from the National Eczema Association and Canadian Agency for Drugs and Technologies in Health. Another author reported receiving personal fees from pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Imaging Tool Helps Identify Features of Nail Disorders
TOPLINE:
METHODOLOGY:
- The single-center, observational cross-sectional pilot study evaluated patients aged ≥ 7 years with newly diagnosed nail disorders between January 2022 and May 2023.
- A total of 128 patients (average age, 46.1 years; range, 8-84 years) with nail psoriasis, onychomycosis, idiopathic/traumatic onycholysis, brittle nail syndrome, nail lichen planus, retronychia, and other nail conditions and those with no nail findings (controls) were enrolled.
- Researchers performed nailfold capillaroscopy imaging and compared capillary features between patients with nail conditions and the controls.
TAKEAWAY:
- Patients with nail psoriasis had decreased capillary density and length (P < .001), more crossed and tortuous capillaries (P < .02), and increased abnormal capillary morphology (P = .03) compared with controls. Specific abnormalities, such as branching and meandering capillaries, were more common among those with nail psoriasis (both 26.5%).
- Patients with fingernail and toenail onychomycosis had a higher frequency of abnormal capillary morphology (P < .02), particularly meandering capillaries (75.0% for fingernails and 76.9% for toenails). However, other abnormalities were less frequently observed.
- Patients with nail lichen planus (P < .01), onychopapilloma (P = .01), and retronychia (P = .03) showed significantly shorter capillaries than controls. Retronychia was also associated with increased disorganized polymorphic capillaries (P = .02).
- Patients with brittle nail syndrome and eczema showed no significant differences compared with controls.
IN PRACTICE:
“Our findings highlight nailfold capillaroscopy as a potentially quick, cost-effective, and noninvasive imaging modality as an adjunct for diagnosis and treatment initiation for patients with onychodystrophies,” the authors wrote.
SOURCE:
This study was led by Jonathan K. Hwang, MD, Weill Cornell Medicine, New York City, and was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The study’s limitations included a small sample size for certain nail conditions and the single-center design, which limited generalizability. Additionally, the uneven surface, scaling, onycholysis, and thickening of toenails made some capillaroscopy images difficult to capture and interpret.
DISCLOSURES:
The study did not receive any funding. One author reported serving as a consultant for Eli Lilly, Ortho-Dermatologics, BelleTorus, and Moberg Pharma.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The single-center, observational cross-sectional pilot study evaluated patients aged ≥ 7 years with newly diagnosed nail disorders between January 2022 and May 2023.
- A total of 128 patients (average age, 46.1 years; range, 8-84 years) with nail psoriasis, onychomycosis, idiopathic/traumatic onycholysis, brittle nail syndrome, nail lichen planus, retronychia, and other nail conditions and those with no nail findings (controls) were enrolled.
- Researchers performed nailfold capillaroscopy imaging and compared capillary features between patients with nail conditions and the controls.
TAKEAWAY:
- Patients with nail psoriasis had decreased capillary density and length (P < .001), more crossed and tortuous capillaries (P < .02), and increased abnormal capillary morphology (P = .03) compared with controls. Specific abnormalities, such as branching and meandering capillaries, were more common among those with nail psoriasis (both 26.5%).
- Patients with fingernail and toenail onychomycosis had a higher frequency of abnormal capillary morphology (P < .02), particularly meandering capillaries (75.0% for fingernails and 76.9% for toenails). However, other abnormalities were less frequently observed.
- Patients with nail lichen planus (P < .01), onychopapilloma (P = .01), and retronychia (P = .03) showed significantly shorter capillaries than controls. Retronychia was also associated with increased disorganized polymorphic capillaries (P = .02).
- Patients with brittle nail syndrome and eczema showed no significant differences compared with controls.
IN PRACTICE:
“Our findings highlight nailfold capillaroscopy as a potentially quick, cost-effective, and noninvasive imaging modality as an adjunct for diagnosis and treatment initiation for patients with onychodystrophies,” the authors wrote.
SOURCE:
This study was led by Jonathan K. Hwang, MD, Weill Cornell Medicine, New York City, and was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The study’s limitations included a small sample size for certain nail conditions and the single-center design, which limited generalizability. Additionally, the uneven surface, scaling, onycholysis, and thickening of toenails made some capillaroscopy images difficult to capture and interpret.
DISCLOSURES:
The study did not receive any funding. One author reported serving as a consultant for Eli Lilly, Ortho-Dermatologics, BelleTorus, and Moberg Pharma.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The single-center, observational cross-sectional pilot study evaluated patients aged ≥ 7 years with newly diagnosed nail disorders between January 2022 and May 2023.
- A total of 128 patients (average age, 46.1 years; range, 8-84 years) with nail psoriasis, onychomycosis, idiopathic/traumatic onycholysis, brittle nail syndrome, nail lichen planus, retronychia, and other nail conditions and those with no nail findings (controls) were enrolled.
- Researchers performed nailfold capillaroscopy imaging and compared capillary features between patients with nail conditions and the controls.
TAKEAWAY:
- Patients with nail psoriasis had decreased capillary density and length (P < .001), more crossed and tortuous capillaries (P < .02), and increased abnormal capillary morphology (P = .03) compared with controls. Specific abnormalities, such as branching and meandering capillaries, were more common among those with nail psoriasis (both 26.5%).
- Patients with fingernail and toenail onychomycosis had a higher frequency of abnormal capillary morphology (P < .02), particularly meandering capillaries (75.0% for fingernails and 76.9% for toenails). However, other abnormalities were less frequently observed.
- Patients with nail lichen planus (P < .01), onychopapilloma (P = .01), and retronychia (P = .03) showed significantly shorter capillaries than controls. Retronychia was also associated with increased disorganized polymorphic capillaries (P = .02).
- Patients with brittle nail syndrome and eczema showed no significant differences compared with controls.
IN PRACTICE:
“Our findings highlight nailfold capillaroscopy as a potentially quick, cost-effective, and noninvasive imaging modality as an adjunct for diagnosis and treatment initiation for patients with onychodystrophies,” the authors wrote.
SOURCE:
This study was led by Jonathan K. Hwang, MD, Weill Cornell Medicine, New York City, and was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The study’s limitations included a small sample size for certain nail conditions and the single-center design, which limited generalizability. Additionally, the uneven surface, scaling, onycholysis, and thickening of toenails made some capillaroscopy images difficult to capture and interpret.
DISCLOSURES:
The study did not receive any funding. One author reported serving as a consultant for Eli Lilly, Ortho-Dermatologics, BelleTorus, and Moberg Pharma.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
First Combined Face and Eye Transplant Performed
In a groundbreaking procedure, a team of surgeons from New York University Langone Health successfully performed the first combined face and eye transplant on a patient with extensive craniofacial tissue loss after an electrical accident.
The highly complex surgery lasted for 21 hours and involved more than 140 surgeons, nurses, and other healthcare professionals under the leadership of Eduardo D. Rodriguez. MD. It not only restored the patient’s facial features, but also integrated a functional eyeball, potentially setting a new standard for future treatments in similar cases.
The transplant took place in May 2023, and the case report was published on September 5 this year in JAMA.
The 46-year-old man lost a large part of his craniofacial tissue and his left eyeball. The approach was highly specialized. Advanced microsurgical techniques such as anastomoses of microscopic vessels and delicate suturing techniques were crucial for the transplant’s success.
Moreover, customized surgical devices, specific implants, and tissue manipulation tools were developed specifically for this case, thus ensuring the viability of the transplant and adequate perfusion of the transplanted ocular tissue.
The initial results are encouraging. Retinal arterial perfusion has been maintained, and retinal architecture has been preserved, as demonstrated by optical coherence tomography. Electroretinography confirmed retinal responses to light, suggesting that the transplanted eye may eventually contribute to the patient’s visual perception. These results are comparable to those of previous facial tissue transplants, but with the significant addition of ocular functionality, which is a notable advance.
“The successful revascularization of the transplanted eye achieved in this study may serve as a step toward the goal of globe transplant for restoration of vision,” wrote the authors.
The complexity of the combined transplant required a deep understanding of facial and ocular anatomy, as well as tissue preservation techniques. The surgical team reported significant challenges, including the need to align delicate anatomical structures and ensure immunological compatibility between the donor and recipient. Meticulous planning from donor selection to postoperative follow-up was considered essential to maximize the likelihood of success and minimize the risk for allograft rejection.
The patient will now be continuously monitored and receive treatment with immunosuppressants such as tacrolimus and prednisone, adjusted according to his response to the transplant. According to the researchers, further studies will be needed to assess the long-term functionality of the transplanted eye and its integration with the central nervous system.
Despite being the fifth facial transplant surgery performed under Dr. Rodriguez’s leadership, this is the first record of a whole-eye transplant. “The mere fact that we have successfully performed the first whole-eye transplant along with a face transplant is a tremendous achievement that many believed to be impossible,” the doctor said in a statement. “We have taken a giant step forward and paved the way for the next chapter in vision restoration.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
In a groundbreaking procedure, a team of surgeons from New York University Langone Health successfully performed the first combined face and eye transplant on a patient with extensive craniofacial tissue loss after an electrical accident.
The highly complex surgery lasted for 21 hours and involved more than 140 surgeons, nurses, and other healthcare professionals under the leadership of Eduardo D. Rodriguez. MD. It not only restored the patient’s facial features, but also integrated a functional eyeball, potentially setting a new standard for future treatments in similar cases.
The transplant took place in May 2023, and the case report was published on September 5 this year in JAMA.
The 46-year-old man lost a large part of his craniofacial tissue and his left eyeball. The approach was highly specialized. Advanced microsurgical techniques such as anastomoses of microscopic vessels and delicate suturing techniques were crucial for the transplant’s success.
Moreover, customized surgical devices, specific implants, and tissue manipulation tools were developed specifically for this case, thus ensuring the viability of the transplant and adequate perfusion of the transplanted ocular tissue.
The initial results are encouraging. Retinal arterial perfusion has been maintained, and retinal architecture has been preserved, as demonstrated by optical coherence tomography. Electroretinography confirmed retinal responses to light, suggesting that the transplanted eye may eventually contribute to the patient’s visual perception. These results are comparable to those of previous facial tissue transplants, but with the significant addition of ocular functionality, which is a notable advance.
“The successful revascularization of the transplanted eye achieved in this study may serve as a step toward the goal of globe transplant for restoration of vision,” wrote the authors.
The complexity of the combined transplant required a deep understanding of facial and ocular anatomy, as well as tissue preservation techniques. The surgical team reported significant challenges, including the need to align delicate anatomical structures and ensure immunological compatibility between the donor and recipient. Meticulous planning from donor selection to postoperative follow-up was considered essential to maximize the likelihood of success and minimize the risk for allograft rejection.
The patient will now be continuously monitored and receive treatment with immunosuppressants such as tacrolimus and prednisone, adjusted according to his response to the transplant. According to the researchers, further studies will be needed to assess the long-term functionality of the transplanted eye and its integration with the central nervous system.
Despite being the fifth facial transplant surgery performed under Dr. Rodriguez’s leadership, this is the first record of a whole-eye transplant. “The mere fact that we have successfully performed the first whole-eye transplant along with a face transplant is a tremendous achievement that many believed to be impossible,” the doctor said in a statement. “We have taken a giant step forward and paved the way for the next chapter in vision restoration.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
In a groundbreaking procedure, a team of surgeons from New York University Langone Health successfully performed the first combined face and eye transplant on a patient with extensive craniofacial tissue loss after an electrical accident.
The highly complex surgery lasted for 21 hours and involved more than 140 surgeons, nurses, and other healthcare professionals under the leadership of Eduardo D. Rodriguez. MD. It not only restored the patient’s facial features, but also integrated a functional eyeball, potentially setting a new standard for future treatments in similar cases.
The transplant took place in May 2023, and the case report was published on September 5 this year in JAMA.
The 46-year-old man lost a large part of his craniofacial tissue and his left eyeball. The approach was highly specialized. Advanced microsurgical techniques such as anastomoses of microscopic vessels and delicate suturing techniques were crucial for the transplant’s success.
Moreover, customized surgical devices, specific implants, and tissue manipulation tools were developed specifically for this case, thus ensuring the viability of the transplant and adequate perfusion of the transplanted ocular tissue.
The initial results are encouraging. Retinal arterial perfusion has been maintained, and retinal architecture has been preserved, as demonstrated by optical coherence tomography. Electroretinography confirmed retinal responses to light, suggesting that the transplanted eye may eventually contribute to the patient’s visual perception. These results are comparable to those of previous facial tissue transplants, but with the significant addition of ocular functionality, which is a notable advance.
“The successful revascularization of the transplanted eye achieved in this study may serve as a step toward the goal of globe transplant for restoration of vision,” wrote the authors.
The complexity of the combined transplant required a deep understanding of facial and ocular anatomy, as well as tissue preservation techniques. The surgical team reported significant challenges, including the need to align delicate anatomical structures and ensure immunological compatibility between the donor and recipient. Meticulous planning from donor selection to postoperative follow-up was considered essential to maximize the likelihood of success and minimize the risk for allograft rejection.
The patient will now be continuously monitored and receive treatment with immunosuppressants such as tacrolimus and prednisone, adjusted according to his response to the transplant. According to the researchers, further studies will be needed to assess the long-term functionality of the transplanted eye and its integration with the central nervous system.
Despite being the fifth facial transplant surgery performed under Dr. Rodriguez’s leadership, this is the first record of a whole-eye transplant. “The mere fact that we have successfully performed the first whole-eye transplant along with a face transplant is a tremendous achievement that many believed to be impossible,” the doctor said in a statement. “We have taken a giant step forward and paved the way for the next chapter in vision restoration.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
‘Reform School’ for Pharmacy Benefit Managers: How Might Legislation Help Patients?
The term “reform school” is a bit outdated. It used to refer to institutions where young offenders were sent instead of prison. Some argue that pharmacy benefit managers (PBMs) should bypass reform school and go straight to prison. “PBM reform” has become a ubiquitous term, encompassing any legislative or regulatory efforts aimed at curbing PBMs’ bad behavior. When discussing PBM reform, it’s crucial to understand the various segments of the healthcare system affected by PBMs. This complexity often makes it challenging to determine what these reform packages would actually achieve and who they would benefit.
Pharmacists have long been vocal critics of PBMs, and while their issues are extremely important, it is essential to remember that the ultimate victims of PBM misconduct, in terms of access to care, are patients. At some point, we will all be patients, making this issue universally relevant. It has been quite challenging to follow federal legislation on this topic as these packages attempt to address a number of bad behaviors by PBMs affecting a variety of victims. This discussion will examine those reforms that would directly improve patient’s access to available and affordable medications.
Policy Categories of PBM Reform
There are five policy categories of PBM reform legislation overall, including three that have the greatest potential to directly address patient needs. The first is patient access to medications (utilization management, copay assistance, prior authorization, etc.), followed by delinking drug list prices from PBM income and pass-through of price concessions from the manufacturer. The remaining two categories involve transparency and pharmacy-facing reform, both of which are very important. However, this discussion will revolve around the first three categories. It should be noted that many of the legislation packages addressing the categories of patient access, delinking, and pass-through also include transparency issues, particularly as they relate to pharmacy-facing issues.
Patient Access to Medications — Step Therapy Legislation
One of the major obstacles to patient access to medications is the use of PBM utilization management tools such as step therapy (“fail first”), prior authorizations, nonmedical switching, and formulary exclusions. These tools dictate when patients can obtain necessary medications and for how long patients who are stable on their current treatments can remain on them.
While many states have enacted step therapy reforms to prevent stable patients from being whip-sawed between medications that maximize PBM profits (often labeled as “savings”), these state protections apply only to state-regulated health plans. These include fully insured health plans and those offered through the Affordable Care Act’s Health Insurance Marketplace. It also includes state employees, state corrections, and, in some cases, state labor unions. State legislation does not extend to patients covered by employer self-insured health plans, called ERISA plans for the federal law that governs employee benefit plans, the Employee Retirement Income Security Act. These ERISA plans include nearly 35 million people nationwide.
This is where the Safe Step Act (S.652/H.R.2630) becomes crucial, as it allows employees to request exceptions to harmful fail-first protocols. The bill has gained significant momentum, having been reported out of the Senate HELP Committee and discussed in House markups. The Safe Step Act would mandate that an exception to a step therapy protocol must be granted if:
- The required treatment has been ineffective
- The treatment is expected to be ineffective, and delaying effective treatment would lead to irreversible consequences
- The treatment will cause or is likely to cause an adverse reaction
- The treatment is expected to prevent the individual from performing daily activities or occupational responsibilities
- The individual is stable on their current prescription drugs
- There are other circumstances as determined by the Employee Benefits Security Administration
This legislation is vital for ensuring that patients have timely access to the medications they need without unnecessary delays or disruptions.
Patient Access to Medications — Prior Authorizations
Another significant issue affecting patient access to medications is prior authorizations (PAs). According to an American Medical Association survey, nearly one in four physicians (24%) report that a PA has led to a serious adverse event for a patient in their care. In rheumatology, PAs often result in delays in care (even for those initially approved) and a significant increase in steroid usage. In particular, PAs in Medicare Advantage (MA) plans are harmful to Medicare beneficiaries.
The Improving Seniors’ Timely Access to Care Act (H.R.8702 / S.4532) aims to reform PAs used in MA plans, making the process more efficient and transparent to improve access to care for seniors. Unfortunately, it does not cover Part D drugs and may only cover Part B drugs depending on the MA plan’s benefit package. Here are the key provisions of the act:
- Electronic PA: Implementing real-time decisions for routinely approved items and services.
- Transparency: Requiring annual publication of PA information, such as the percentage of requests approved and the average response time.
- Quality and Timeliness Standards: The Centers for Medicare & Medicaid Services (CMS) will set standards for the quality and timeliness of PA determinations.
- Streamlining Approvals: Simplifying the approval process and reducing the time allowed for health plans to consider PA requests.
This bill passed the House in September 2022 but stalled in the Senate because of an unfavorable Congressional Budget Office score. CMS has since finalized portions of this bill via regulation, zeroing out the CBO score and increasing the chances of its passage.
Delinking Drug Prices from PBM Income and Pass-Through of Price Concessions
Affordability is a crucial aspect of accessibility, especially when it comes to medications. Over the years, we’ve learned that PBMs often favor placing the highest list price drugs on formularies because the rebates and various fees they receive from manufacturers are based on a percentage of the list price. In other words, the higher the medication’s price, the more money the PBM makes.
This practice is evident in both commercial and government formularies, where brand-name drugs are often preferred, while lower-priced generics are either excluded or placed on higher tiers. As a result, while major PBMs benefit from these rebates and fees, patients continue to pay their cost share based on the list price of the medication.
To improve the affordability of medications, a key aspect of PBM reform should be to disincentivize PBMs from selecting higher-priced medications and/or require the pass-through of manufacturer price concessions to patients.
Several major PBM reform bills are currently being considered that address either the delinking of price concessions from the list price of the drug or some form of pass-through of these concessions. These reforms are essential to ensure that patients can access affordable medications without being burdened by inflated costs.
The legislation includes the Pharmacy Benefit Manager Reform Act (S.1339); the Modernizing & Ensuring PBM Accountability Act (S.2973); the Better Mental Health Care, Lower Cost Drugs, and Extenders Act (S.3430); the Protecting Patients Against PBM Abuses Act (H.R. 2880); the DRUG Act (S.2474 / H.R.6283); and the Share the Savings with Seniors Act (S.2474 / H.R.5376).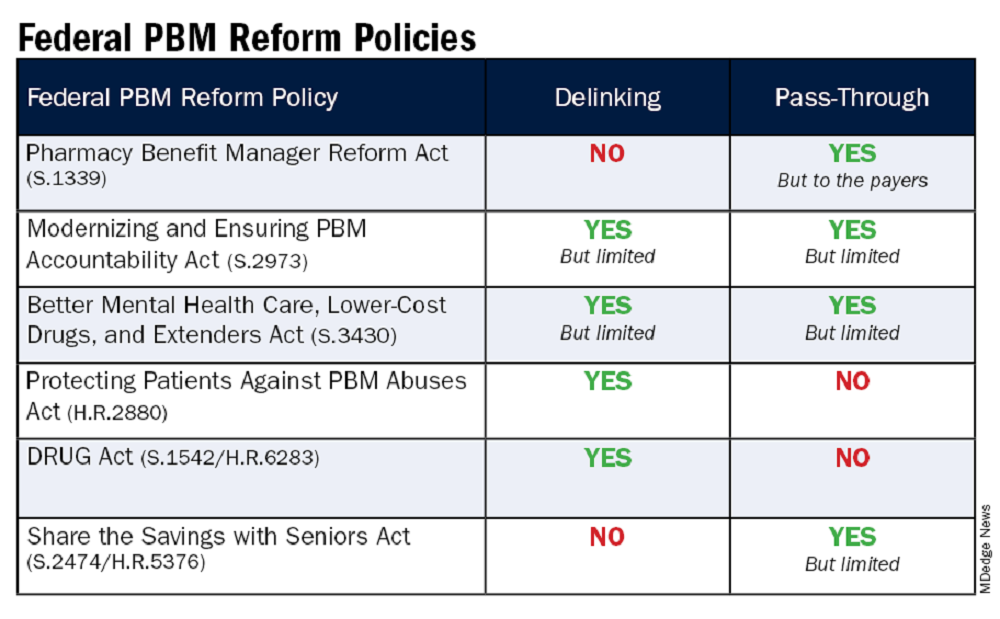
As with all legislation, there are limitations and compromises in each of these. However, these bills are a good first step in addressing PBM remuneration (rebates and fees) based on the list price of the drug and/or passing through to the patient the benefit of manufacturer price concessions. By focusing on key areas like utilization management, delinking drug prices from PBM income, and allowing patients to directly benefit from manufacturer price concessions, we can work toward a more equitable and efficient healthcare system. Reigning in PBM bad behavior is a challenge, but the potential benefits for patient care and access make it a crucial fight worth pursuing.
Please help in efforts to improve patients’ access to available and affordable medications by contacting your representatives in Congress to impart to them the importance of passing legislation. The CSRO’s legislative map tool can help to inform you of the latest information on these and other bills and assist you in engaging with your representatives on them.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of Advocacy and Government Affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. She has no relevant conflicts of interest to disclose. You can reach her at [email protected].
The term “reform school” is a bit outdated. It used to refer to institutions where young offenders were sent instead of prison. Some argue that pharmacy benefit managers (PBMs) should bypass reform school and go straight to prison. “PBM reform” has become a ubiquitous term, encompassing any legislative or regulatory efforts aimed at curbing PBMs’ bad behavior. When discussing PBM reform, it’s crucial to understand the various segments of the healthcare system affected by PBMs. This complexity often makes it challenging to determine what these reform packages would actually achieve and who they would benefit.
Pharmacists have long been vocal critics of PBMs, and while their issues are extremely important, it is essential to remember that the ultimate victims of PBM misconduct, in terms of access to care, are patients. At some point, we will all be patients, making this issue universally relevant. It has been quite challenging to follow federal legislation on this topic as these packages attempt to address a number of bad behaviors by PBMs affecting a variety of victims. This discussion will examine those reforms that would directly improve patient’s access to available and affordable medications.
Policy Categories of PBM Reform
There are five policy categories of PBM reform legislation overall, including three that have the greatest potential to directly address patient needs. The first is patient access to medications (utilization management, copay assistance, prior authorization, etc.), followed by delinking drug list prices from PBM income and pass-through of price concessions from the manufacturer. The remaining two categories involve transparency and pharmacy-facing reform, both of which are very important. However, this discussion will revolve around the first three categories. It should be noted that many of the legislation packages addressing the categories of patient access, delinking, and pass-through also include transparency issues, particularly as they relate to pharmacy-facing issues.
Patient Access to Medications — Step Therapy Legislation
One of the major obstacles to patient access to medications is the use of PBM utilization management tools such as step therapy (“fail first”), prior authorizations, nonmedical switching, and formulary exclusions. These tools dictate when patients can obtain necessary medications and for how long patients who are stable on their current treatments can remain on them.
While many states have enacted step therapy reforms to prevent stable patients from being whip-sawed between medications that maximize PBM profits (often labeled as “savings”), these state protections apply only to state-regulated health plans. These include fully insured health plans and those offered through the Affordable Care Act’s Health Insurance Marketplace. It also includes state employees, state corrections, and, in some cases, state labor unions. State legislation does not extend to patients covered by employer self-insured health plans, called ERISA plans for the federal law that governs employee benefit plans, the Employee Retirement Income Security Act. These ERISA plans include nearly 35 million people nationwide.
This is where the Safe Step Act (S.652/H.R.2630) becomes crucial, as it allows employees to request exceptions to harmful fail-first protocols. The bill has gained significant momentum, having been reported out of the Senate HELP Committee and discussed in House markups. The Safe Step Act would mandate that an exception to a step therapy protocol must be granted if:
- The required treatment has been ineffective
- The treatment is expected to be ineffective, and delaying effective treatment would lead to irreversible consequences
- The treatment will cause or is likely to cause an adverse reaction
- The treatment is expected to prevent the individual from performing daily activities or occupational responsibilities
- The individual is stable on their current prescription drugs
- There are other circumstances as determined by the Employee Benefits Security Administration
This legislation is vital for ensuring that patients have timely access to the medications they need without unnecessary delays or disruptions.
Patient Access to Medications — Prior Authorizations
Another significant issue affecting patient access to medications is prior authorizations (PAs). According to an American Medical Association survey, nearly one in four physicians (24%) report that a PA has led to a serious adverse event for a patient in their care. In rheumatology, PAs often result in delays in care (even for those initially approved) and a significant increase in steroid usage. In particular, PAs in Medicare Advantage (MA) plans are harmful to Medicare beneficiaries.
The Improving Seniors’ Timely Access to Care Act (H.R.8702 / S.4532) aims to reform PAs used in MA plans, making the process more efficient and transparent to improve access to care for seniors. Unfortunately, it does not cover Part D drugs and may only cover Part B drugs depending on the MA plan’s benefit package. Here are the key provisions of the act:
- Electronic PA: Implementing real-time decisions for routinely approved items and services.
- Transparency: Requiring annual publication of PA information, such as the percentage of requests approved and the average response time.
- Quality and Timeliness Standards: The Centers for Medicare & Medicaid Services (CMS) will set standards for the quality and timeliness of PA determinations.
- Streamlining Approvals: Simplifying the approval process and reducing the time allowed for health plans to consider PA requests.
This bill passed the House in September 2022 but stalled in the Senate because of an unfavorable Congressional Budget Office score. CMS has since finalized portions of this bill via regulation, zeroing out the CBO score and increasing the chances of its passage.
Delinking Drug Prices from PBM Income and Pass-Through of Price Concessions
Affordability is a crucial aspect of accessibility, especially when it comes to medications. Over the years, we’ve learned that PBMs often favor placing the highest list price drugs on formularies because the rebates and various fees they receive from manufacturers are based on a percentage of the list price. In other words, the higher the medication’s price, the more money the PBM makes.
This practice is evident in both commercial and government formularies, where brand-name drugs are often preferred, while lower-priced generics are either excluded or placed on higher tiers. As a result, while major PBMs benefit from these rebates and fees, patients continue to pay their cost share based on the list price of the medication.
To improve the affordability of medications, a key aspect of PBM reform should be to disincentivize PBMs from selecting higher-priced medications and/or require the pass-through of manufacturer price concessions to patients.
Several major PBM reform bills are currently being considered that address either the delinking of price concessions from the list price of the drug or some form of pass-through of these concessions. These reforms are essential to ensure that patients can access affordable medications without being burdened by inflated costs.
The legislation includes the Pharmacy Benefit Manager Reform Act (S.1339); the Modernizing & Ensuring PBM Accountability Act (S.2973); the Better Mental Health Care, Lower Cost Drugs, and Extenders Act (S.3430); the Protecting Patients Against PBM Abuses Act (H.R. 2880); the DRUG Act (S.2474 / H.R.6283); and the Share the Savings with Seniors Act (S.2474 / H.R.5376).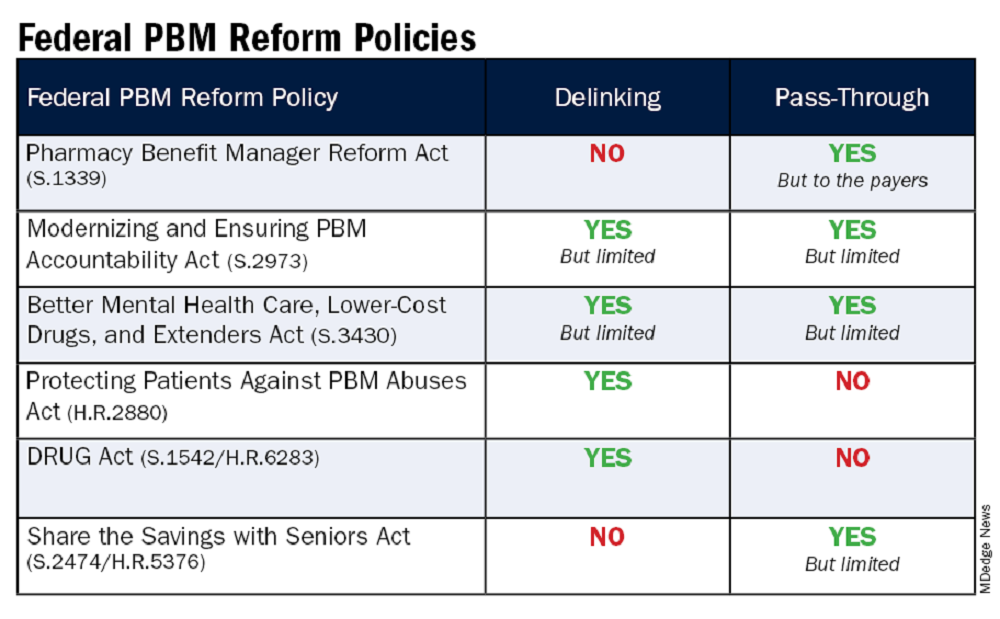
As with all legislation, there are limitations and compromises in each of these. However, these bills are a good first step in addressing PBM remuneration (rebates and fees) based on the list price of the drug and/or passing through to the patient the benefit of manufacturer price concessions. By focusing on key areas like utilization management, delinking drug prices from PBM income, and allowing patients to directly benefit from manufacturer price concessions, we can work toward a more equitable and efficient healthcare system. Reigning in PBM bad behavior is a challenge, but the potential benefits for patient care and access make it a crucial fight worth pursuing.
Please help in efforts to improve patients’ access to available and affordable medications by contacting your representatives in Congress to impart to them the importance of passing legislation. The CSRO’s legislative map tool can help to inform you of the latest information on these and other bills and assist you in engaging with your representatives on them.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of Advocacy and Government Affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. She has no relevant conflicts of interest to disclose. You can reach her at [email protected].
The term “reform school” is a bit outdated. It used to refer to institutions where young offenders were sent instead of prison. Some argue that pharmacy benefit managers (PBMs) should bypass reform school and go straight to prison. “PBM reform” has become a ubiquitous term, encompassing any legislative or regulatory efforts aimed at curbing PBMs’ bad behavior. When discussing PBM reform, it’s crucial to understand the various segments of the healthcare system affected by PBMs. This complexity often makes it challenging to determine what these reform packages would actually achieve and who they would benefit.
Pharmacists have long been vocal critics of PBMs, and while their issues are extremely important, it is essential to remember that the ultimate victims of PBM misconduct, in terms of access to care, are patients. At some point, we will all be patients, making this issue universally relevant. It has been quite challenging to follow federal legislation on this topic as these packages attempt to address a number of bad behaviors by PBMs affecting a variety of victims. This discussion will examine those reforms that would directly improve patient’s access to available and affordable medications.
Policy Categories of PBM Reform
There are five policy categories of PBM reform legislation overall, including three that have the greatest potential to directly address patient needs. The first is patient access to medications (utilization management, copay assistance, prior authorization, etc.), followed by delinking drug list prices from PBM income and pass-through of price concessions from the manufacturer. The remaining two categories involve transparency and pharmacy-facing reform, both of which are very important. However, this discussion will revolve around the first three categories. It should be noted that many of the legislation packages addressing the categories of patient access, delinking, and pass-through also include transparency issues, particularly as they relate to pharmacy-facing issues.
Patient Access to Medications — Step Therapy Legislation
One of the major obstacles to patient access to medications is the use of PBM utilization management tools such as step therapy (“fail first”), prior authorizations, nonmedical switching, and formulary exclusions. These tools dictate when patients can obtain necessary medications and for how long patients who are stable on their current treatments can remain on them.
While many states have enacted step therapy reforms to prevent stable patients from being whip-sawed between medications that maximize PBM profits (often labeled as “savings”), these state protections apply only to state-regulated health plans. These include fully insured health plans and those offered through the Affordable Care Act’s Health Insurance Marketplace. It also includes state employees, state corrections, and, in some cases, state labor unions. State legislation does not extend to patients covered by employer self-insured health plans, called ERISA plans for the federal law that governs employee benefit plans, the Employee Retirement Income Security Act. These ERISA plans include nearly 35 million people nationwide.
This is where the Safe Step Act (S.652/H.R.2630) becomes crucial, as it allows employees to request exceptions to harmful fail-first protocols. The bill has gained significant momentum, having been reported out of the Senate HELP Committee and discussed in House markups. The Safe Step Act would mandate that an exception to a step therapy protocol must be granted if:
- The required treatment has been ineffective
- The treatment is expected to be ineffective, and delaying effective treatment would lead to irreversible consequences
- The treatment will cause or is likely to cause an adverse reaction
- The treatment is expected to prevent the individual from performing daily activities or occupational responsibilities
- The individual is stable on their current prescription drugs
- There are other circumstances as determined by the Employee Benefits Security Administration
This legislation is vital for ensuring that patients have timely access to the medications they need without unnecessary delays or disruptions.
Patient Access to Medications — Prior Authorizations
Another significant issue affecting patient access to medications is prior authorizations (PAs). According to an American Medical Association survey, nearly one in four physicians (24%) report that a PA has led to a serious adverse event for a patient in their care. In rheumatology, PAs often result in delays in care (even for those initially approved) and a significant increase in steroid usage. In particular, PAs in Medicare Advantage (MA) plans are harmful to Medicare beneficiaries.
The Improving Seniors’ Timely Access to Care Act (H.R.8702 / S.4532) aims to reform PAs used in MA plans, making the process more efficient and transparent to improve access to care for seniors. Unfortunately, it does not cover Part D drugs and may only cover Part B drugs depending on the MA plan’s benefit package. Here are the key provisions of the act:
- Electronic PA: Implementing real-time decisions for routinely approved items and services.
- Transparency: Requiring annual publication of PA information, such as the percentage of requests approved and the average response time.
- Quality and Timeliness Standards: The Centers for Medicare & Medicaid Services (CMS) will set standards for the quality and timeliness of PA determinations.
- Streamlining Approvals: Simplifying the approval process and reducing the time allowed for health plans to consider PA requests.
This bill passed the House in September 2022 but stalled in the Senate because of an unfavorable Congressional Budget Office score. CMS has since finalized portions of this bill via regulation, zeroing out the CBO score and increasing the chances of its passage.
Delinking Drug Prices from PBM Income and Pass-Through of Price Concessions
Affordability is a crucial aspect of accessibility, especially when it comes to medications. Over the years, we’ve learned that PBMs often favor placing the highest list price drugs on formularies because the rebates and various fees they receive from manufacturers are based on a percentage of the list price. In other words, the higher the medication’s price, the more money the PBM makes.
This practice is evident in both commercial and government formularies, where brand-name drugs are often preferred, while lower-priced generics are either excluded or placed on higher tiers. As a result, while major PBMs benefit from these rebates and fees, patients continue to pay their cost share based on the list price of the medication.
To improve the affordability of medications, a key aspect of PBM reform should be to disincentivize PBMs from selecting higher-priced medications and/or require the pass-through of manufacturer price concessions to patients.
Several major PBM reform bills are currently being considered that address either the delinking of price concessions from the list price of the drug or some form of pass-through of these concessions. These reforms are essential to ensure that patients can access affordable medications without being burdened by inflated costs.
The legislation includes the Pharmacy Benefit Manager Reform Act (S.1339); the Modernizing & Ensuring PBM Accountability Act (S.2973); the Better Mental Health Care, Lower Cost Drugs, and Extenders Act (S.3430); the Protecting Patients Against PBM Abuses Act (H.R. 2880); the DRUG Act (S.2474 / H.R.6283); and the Share the Savings with Seniors Act (S.2474 / H.R.5376).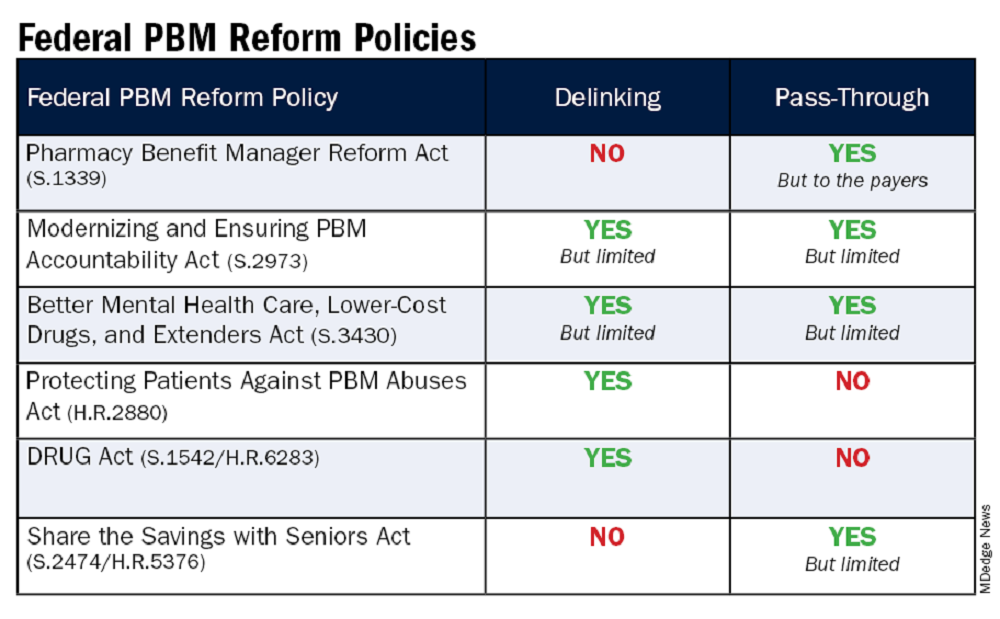
As with all legislation, there are limitations and compromises in each of these. However, these bills are a good first step in addressing PBM remuneration (rebates and fees) based on the list price of the drug and/or passing through to the patient the benefit of manufacturer price concessions. By focusing on key areas like utilization management, delinking drug prices from PBM income, and allowing patients to directly benefit from manufacturer price concessions, we can work toward a more equitable and efficient healthcare system. Reigning in PBM bad behavior is a challenge, but the potential benefits for patient care and access make it a crucial fight worth pursuing.
Please help in efforts to improve patients’ access to available and affordable medications by contacting your representatives in Congress to impart to them the importance of passing legislation. The CSRO’s legislative map tool can help to inform you of the latest information on these and other bills and assist you in engaging with your representatives on them.
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s vice president of Advocacy and Government Affairs and its immediate past president, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. She has no relevant conflicts of interest to disclose. You can reach her at [email protected].
Belimumab Hits Newer Remission, Low Disease Activity Metrics
TOPLINE:
A greater proportion of patients with active systemic lupus erythematosus (SLE) treated with belimumab plus standard therapy achieved the newest definitions for remission and low disease activity compared with those treated with placebo plus standard therapy, with benefits observed as early as week 28 for remission and week 8 for disease activity, according to pooled results from five clinical trials.
METHODOLOGY:
- Researchers conducted an integrated post hoc analysis of five randomized phase 3 clinical trials to evaluate the attainment of remission and low disease activity in adult patients with active, autoantibody-positive SLE.
- A total of 3086 patients (median age, 36 years; 94% women) were randomly assigned to receive standard therapy with intravenous belimumab 10 mg/kg monthly or subcutaneous belimumab 200 mg weekly (n = 1869) or placebo (n = 1217).
- The proportion of patients who achieved definitions of remission in SLE (DORIS) remission and lupus low disease activity state (LLDAS) by visit up to week 52 was assessed.
- The analysis also evaluated the time taken to achieve sustained (at least two consecutive visits) and maintained (up to week 52) DORIS remission and LLDAS.
TAKEAWAY:
- At week 52, a higher proportion of patients receiving belimumab vs placebo achieved DORIS remission (8% vs 6%; risk ratio [RR], 1.51; P = .0055) and LLDAS (17% vs 10%; RR, 1.74; P < .0001).
- The earliest observed significant benefit of belimumab over placebo in patients with a higher baseline disease activity was at week 20 for DORIS remission (RR, 2.09; P = .043) and at week 16 for LLDAS (RR, 1.46; P = .034), with both maintained through week 52.
- The proportion of patients who attained DORIS remission and LLDAS as early as week 28 and week 8, respectively, was higher in the belimumab group than in the placebo group, with both maintained through week 52.
- Patients on belimumab were more likely to have a sustained and maintained DORIS remission (hazard ratio [HR], 1.53; P = .013) and LLDAS (HR, 1.79; P < .0001) at any timepoint.
IN PRACTICE:
“The data clearly support that belimumab is a valuable addition toward accomplishing and maintaining remission or LLDAS,” George Bertsias, MD, PhD, University of Crete Medical School, Heraklion, Greece, and Jinoos Yazdany, MD, University of California San Francisco, wrote in a related comment.
SOURCE:
This study, led by Ioannis Parodis, MD, Karolinska Institutet and Karolinska University Hospital, Stockholm, Sweden, was published online on August 26, 2024, in The Lancet Rheumatology.
LIMITATIONS:
Due to the post hoc nature of the analysis, the trials were not specifically designed to have adequate statistical power to demonstrate the difference between patients who did or did not achieve DORIS remission or LLDAS. The analysis was limited to patients who met the eligibility criteria, and the outcomes are not generalizable to populations outside a clinical trial setting. The study population had high disease activity, which made it challenging to attain the treatment targets.
DISCLOSURES:
The five trials included in this analysis were funded by GSK. The study was supported by the Swedish Rheumatism Association, King Gustaf V’s 80-year Foundation, the Swedish Society of Medicine, Nyckelfonden, Professor Nanna Svartz Foundation, Ulla and Roland Gustafsson Foundation, Region Stockholm, and Karolinska Institutet. Some authors reported receiving grants, speaker honoraria, or consulting fees from various pharmaceutical companies. Some authors reported being employees and owning stocks and shares of GSK.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
A greater proportion of patients with active systemic lupus erythematosus (SLE) treated with belimumab plus standard therapy achieved the newest definitions for remission and low disease activity compared with those treated with placebo plus standard therapy, with benefits observed as early as week 28 for remission and week 8 for disease activity, according to pooled results from five clinical trials.
METHODOLOGY:
- Researchers conducted an integrated post hoc analysis of five randomized phase 3 clinical trials to evaluate the attainment of remission and low disease activity in adult patients with active, autoantibody-positive SLE.
- A total of 3086 patients (median age, 36 years; 94% women) were randomly assigned to receive standard therapy with intravenous belimumab 10 mg/kg monthly or subcutaneous belimumab 200 mg weekly (n = 1869) or placebo (n = 1217).
- The proportion of patients who achieved definitions of remission in SLE (DORIS) remission and lupus low disease activity state (LLDAS) by visit up to week 52 was assessed.
- The analysis also evaluated the time taken to achieve sustained (at least two consecutive visits) and maintained (up to week 52) DORIS remission and LLDAS.
TAKEAWAY:
- At week 52, a higher proportion of patients receiving belimumab vs placebo achieved DORIS remission (8% vs 6%; risk ratio [RR], 1.51; P = .0055) and LLDAS (17% vs 10%; RR, 1.74; P < .0001).
- The earliest observed significant benefit of belimumab over placebo in patients with a higher baseline disease activity was at week 20 for DORIS remission (RR, 2.09; P = .043) and at week 16 for LLDAS (RR, 1.46; P = .034), with both maintained through week 52.
- The proportion of patients who attained DORIS remission and LLDAS as early as week 28 and week 8, respectively, was higher in the belimumab group than in the placebo group, with both maintained through week 52.
- Patients on belimumab were more likely to have a sustained and maintained DORIS remission (hazard ratio [HR], 1.53; P = .013) and LLDAS (HR, 1.79; P < .0001) at any timepoint.
IN PRACTICE:
“The data clearly support that belimumab is a valuable addition toward accomplishing and maintaining remission or LLDAS,” George Bertsias, MD, PhD, University of Crete Medical School, Heraklion, Greece, and Jinoos Yazdany, MD, University of California San Francisco, wrote in a related comment.
SOURCE:
This study, led by Ioannis Parodis, MD, Karolinska Institutet and Karolinska University Hospital, Stockholm, Sweden, was published online on August 26, 2024, in The Lancet Rheumatology.
LIMITATIONS:
Due to the post hoc nature of the analysis, the trials were not specifically designed to have adequate statistical power to demonstrate the difference between patients who did or did not achieve DORIS remission or LLDAS. The analysis was limited to patients who met the eligibility criteria, and the outcomes are not generalizable to populations outside a clinical trial setting. The study population had high disease activity, which made it challenging to attain the treatment targets.
DISCLOSURES:
The five trials included in this analysis were funded by GSK. The study was supported by the Swedish Rheumatism Association, King Gustaf V’s 80-year Foundation, the Swedish Society of Medicine, Nyckelfonden, Professor Nanna Svartz Foundation, Ulla and Roland Gustafsson Foundation, Region Stockholm, and Karolinska Institutet. Some authors reported receiving grants, speaker honoraria, or consulting fees from various pharmaceutical companies. Some authors reported being employees and owning stocks and shares of GSK.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
A greater proportion of patients with active systemic lupus erythematosus (SLE) treated with belimumab plus standard therapy achieved the newest definitions for remission and low disease activity compared with those treated with placebo plus standard therapy, with benefits observed as early as week 28 for remission and week 8 for disease activity, according to pooled results from five clinical trials.
METHODOLOGY:
- Researchers conducted an integrated post hoc analysis of five randomized phase 3 clinical trials to evaluate the attainment of remission and low disease activity in adult patients with active, autoantibody-positive SLE.
- A total of 3086 patients (median age, 36 years; 94% women) were randomly assigned to receive standard therapy with intravenous belimumab 10 mg/kg monthly or subcutaneous belimumab 200 mg weekly (n = 1869) or placebo (n = 1217).
- The proportion of patients who achieved definitions of remission in SLE (DORIS) remission and lupus low disease activity state (LLDAS) by visit up to week 52 was assessed.
- The analysis also evaluated the time taken to achieve sustained (at least two consecutive visits) and maintained (up to week 52) DORIS remission and LLDAS.
TAKEAWAY:
- At week 52, a higher proportion of patients receiving belimumab vs placebo achieved DORIS remission (8% vs 6%; risk ratio [RR], 1.51; P = .0055) and LLDAS (17% vs 10%; RR, 1.74; P < .0001).
- The earliest observed significant benefit of belimumab over placebo in patients with a higher baseline disease activity was at week 20 for DORIS remission (RR, 2.09; P = .043) and at week 16 for LLDAS (RR, 1.46; P = .034), with both maintained through week 52.
- The proportion of patients who attained DORIS remission and LLDAS as early as week 28 and week 8, respectively, was higher in the belimumab group than in the placebo group, with both maintained through week 52.
- Patients on belimumab were more likely to have a sustained and maintained DORIS remission (hazard ratio [HR], 1.53; P = .013) and LLDAS (HR, 1.79; P < .0001) at any timepoint.
IN PRACTICE:
“The data clearly support that belimumab is a valuable addition toward accomplishing and maintaining remission or LLDAS,” George Bertsias, MD, PhD, University of Crete Medical School, Heraklion, Greece, and Jinoos Yazdany, MD, University of California San Francisco, wrote in a related comment.
SOURCE:
This study, led by Ioannis Parodis, MD, Karolinska Institutet and Karolinska University Hospital, Stockholm, Sweden, was published online on August 26, 2024, in The Lancet Rheumatology.
LIMITATIONS:
Due to the post hoc nature of the analysis, the trials were not specifically designed to have adequate statistical power to demonstrate the difference between patients who did or did not achieve DORIS remission or LLDAS. The analysis was limited to patients who met the eligibility criteria, and the outcomes are not generalizable to populations outside a clinical trial setting. The study population had high disease activity, which made it challenging to attain the treatment targets.
DISCLOSURES:
The five trials included in this analysis were funded by GSK. The study was supported by the Swedish Rheumatism Association, King Gustaf V’s 80-year Foundation, the Swedish Society of Medicine, Nyckelfonden, Professor Nanna Svartz Foundation, Ulla and Roland Gustafsson Foundation, Region Stockholm, and Karolinska Institutet. Some authors reported receiving grants, speaker honoraria, or consulting fees from various pharmaceutical companies. Some authors reported being employees and owning stocks and shares of GSK.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
AI-Powered Clinical Documentation Tool Reduces EHR Time for Clinicians
TOPLINE:
An artificial intelligence (AI)-powered clinical documentation tool helped reduce time spent on electronic health records (EHR) at home for almost 48% physicians, and nearly 45% reported less weekly time spent on EHR tasks outside of normal work hours.
METHODOLOGY:
- Researchers recruited 112 clinicians from family medicine, internal medicine, and general pediatrics in North Carolina and Georgia.
- Patients were divided into an intervention group (n = 85) and control group (n = 55), with the intervention group receiving a 1-hour training program on a commercially available AI tool.
- A seven-question survey was administered to participants before and 5 weeks after the intervention to evaluate their experience.
TAKEAWAY:
- The researchers found 47.1% of clinicians in the intervention group reported spending less time on the EHR at home compared with 14.5% in the control group (P < .001); 44.7% reported decreased weekly time on the EHR outside normal work hours compared with 20% in the control group (P = .003).
- The study revealed 43.5% of physicians who used the AI instrument reported spending less time on documentation after visits compared with 18.2% in the control group (P = .002).
- Further, 44.7% reported less frustration when using the EHR compared with 14.5% in the control group (P < .001).
IN PRACTICE:
“Approximately half of clinicians using the AI-powered clinical documentation tool based on interest reported a positive outcome, potentially reducing burnout. However, a significant subset did not find time-saving benefits or improved EHR experience,” the authors of the study wrote.
SOURCE:
The study was led by Tsai-Ling Liu, PhD, Center for Health System Sciences, Atrium Health in Charlotte, North Carolina. It was published online in JAMA Network Open.
LIMITATIONS:
The researchers reported potential selection and recall bias in both groups. Additional research is needed to find areas of improvement and assess the effects on clinician groups and health systems, they said.
DISCLOSURES:
Andrew McWilliams, MD, MPH, reported receiving grants from the Agency for Healthcare Research Quality, the National Institutes of Health, and the Duke Endowment unrelated to this work. Ajay Dharod, MD, reported his role as an electronic health record consultant for the Association of American Medical College CORE program. Jeffrey Cleveland, MD, disclosed his participation on the Executive Client Council, a noncompensated advisory group, for Nuance/Microsoft.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
An artificial intelligence (AI)-powered clinical documentation tool helped reduce time spent on electronic health records (EHR) at home for almost 48% physicians, and nearly 45% reported less weekly time spent on EHR tasks outside of normal work hours.
METHODOLOGY:
- Researchers recruited 112 clinicians from family medicine, internal medicine, and general pediatrics in North Carolina and Georgia.
- Patients were divided into an intervention group (n = 85) and control group (n = 55), with the intervention group receiving a 1-hour training program on a commercially available AI tool.
- A seven-question survey was administered to participants before and 5 weeks after the intervention to evaluate their experience.
TAKEAWAY:
- The researchers found 47.1% of clinicians in the intervention group reported spending less time on the EHR at home compared with 14.5% in the control group (P < .001); 44.7% reported decreased weekly time on the EHR outside normal work hours compared with 20% in the control group (P = .003).
- The study revealed 43.5% of physicians who used the AI instrument reported spending less time on documentation after visits compared with 18.2% in the control group (P = .002).
- Further, 44.7% reported less frustration when using the EHR compared with 14.5% in the control group (P < .001).
IN PRACTICE:
“Approximately half of clinicians using the AI-powered clinical documentation tool based on interest reported a positive outcome, potentially reducing burnout. However, a significant subset did not find time-saving benefits or improved EHR experience,” the authors of the study wrote.
SOURCE:
The study was led by Tsai-Ling Liu, PhD, Center for Health System Sciences, Atrium Health in Charlotte, North Carolina. It was published online in JAMA Network Open.
LIMITATIONS:
The researchers reported potential selection and recall bias in both groups. Additional research is needed to find areas of improvement and assess the effects on clinician groups and health systems, they said.
DISCLOSURES:
Andrew McWilliams, MD, MPH, reported receiving grants from the Agency for Healthcare Research Quality, the National Institutes of Health, and the Duke Endowment unrelated to this work. Ajay Dharod, MD, reported his role as an electronic health record consultant for the Association of American Medical College CORE program. Jeffrey Cleveland, MD, disclosed his participation on the Executive Client Council, a noncompensated advisory group, for Nuance/Microsoft.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
An artificial intelligence (AI)-powered clinical documentation tool helped reduce time spent on electronic health records (EHR) at home for almost 48% physicians, and nearly 45% reported less weekly time spent on EHR tasks outside of normal work hours.
METHODOLOGY:
- Researchers recruited 112 clinicians from family medicine, internal medicine, and general pediatrics in North Carolina and Georgia.
- Patients were divided into an intervention group (n = 85) and control group (n = 55), with the intervention group receiving a 1-hour training program on a commercially available AI tool.
- A seven-question survey was administered to participants before and 5 weeks after the intervention to evaluate their experience.
TAKEAWAY:
- The researchers found 47.1% of clinicians in the intervention group reported spending less time on the EHR at home compared with 14.5% in the control group (P < .001); 44.7% reported decreased weekly time on the EHR outside normal work hours compared with 20% in the control group (P = .003).
- The study revealed 43.5% of physicians who used the AI instrument reported spending less time on documentation after visits compared with 18.2% in the control group (P = .002).
- Further, 44.7% reported less frustration when using the EHR compared with 14.5% in the control group (P < .001).
IN PRACTICE:
“Approximately half of clinicians using the AI-powered clinical documentation tool based on interest reported a positive outcome, potentially reducing burnout. However, a significant subset did not find time-saving benefits or improved EHR experience,” the authors of the study wrote.
SOURCE:
The study was led by Tsai-Ling Liu, PhD, Center for Health System Sciences, Atrium Health in Charlotte, North Carolina. It was published online in JAMA Network Open.
LIMITATIONS:
The researchers reported potential selection and recall bias in both groups. Additional research is needed to find areas of improvement and assess the effects on clinician groups and health systems, they said.
DISCLOSURES:
Andrew McWilliams, MD, MPH, reported receiving grants from the Agency for Healthcare Research Quality, the National Institutes of Health, and the Duke Endowment unrelated to this work. Ajay Dharod, MD, reported his role as an electronic health record consultant for the Association of American Medical College CORE program. Jeffrey Cleveland, MD, disclosed his participation on the Executive Client Council, a noncompensated advisory group, for Nuance/Microsoft.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Rare Case of Photodistributed Hyperpigmentation Linked to Kratom Consumption
To the Editor:
Kratom (Mitragyna speciosa) is an evergreen tree native to Southeast Asia.1 Its leaves contain psychoactive compounds including mitragynine and 7-hydroxymitragynine, which exert dose-dependent effects on the central nervous system through opioid and monoaminergic receptors.2,3 At low doses (1–5 g), kratom elicits mild stimulant effects such as increased sociability, alertness, and talkativeness. At high doses (5–15 g), kratom has depressant effects that can provide relief from pain and opioid-withdrawal symptoms.3
Traditionally, kratom has been used in Southeast Asia for recreational and ceremonial purposes, to ease opioid-withdrawal symptoms, and to reduce fatigue from manual labor.4 In the 21st century, availability of kratom expanded to Europe, Australia, and the United States, largely facilitated by widespread dissemination of deceitful marketing and unregulated sales on the internet.1 Although large-scale epidemiologic studies evaluating kratom’s prevalence are scarce, available evidence indicates rising worldwide usage, with a notable increase in kratom-related poison center calls between 2011 and 2017 in the United States.5 In July 2023, kratom made headlines due to the death of a woman in Florida following use of the substance.6
A cross-sectional study revealed that in the United States, kratom typically is used by White individuals for self-treatment of anxiety, depression, pain, and opioid withdrawal.7 However, the potential for severe adverse effects and dependence on kratom can outweigh the benefits.6,8 Reported adverse effects of kratom include tachycardia, hypercholesteremia, liver injury, hallucinations, respiratory depression, seizure, coma, and death.9,10 We present a case of kratom-induced photodistributed hyperpigmentation.
A 63-year-old man presented to the dermatology clinic with diffuse tender, pruritic, hyperpigmented skin lesions that developed over the course of 1 year. The lesions were distributed on sun-exposed areas, including the face, neck, and forearms (Figure 1). The patient reported no other major symptoms, and his health was otherwise unremarkable. He had a medical history of psoriasiform and spongiotic dermatitis consistent with eczema, psoriasis, hypercholesteremia, and hyperlipidemia. The patient was not taking any medications at the time of presentation. He had a family history of plaque psoriasis in his father. Five years prior to the current presentation, the patient was treated with adalimumab for steroid-resistant psoriasis; however, despite initial improvement, he experienced recurrence of scaly erythematous plaques and had discontinued adalimumab the year prior to presentation.

When adalimumab was discontinued, the patient sought alternative treatment for the skin symptoms and began self-administering kratom in an attempt to alleviate associated physical discomfort. He ingested approximately 3 bottles of liquid kratom per day, with each bottle containing 180 mg of mitragynine and less than 8 mg of 7-hydroxymitragynine. Although not scientifically proven, kratom has been colloquially advertised to improve psoriasis.11 The patient reported no other medication use or allergies.
Shave biopsies of hyperpigmented lesions on the right side of the neck, ear, and forearm were performed. Histopathology revealed a sparse superficial, perivascular, lymphocytic infiltrate accompanied by a prominent number of melanophages in the superficial dermis (Figure 2). Special stains further confirmed that the pigment was melanin; the specimens stained positive with Fontana-Masson stain (Figure 3) and negative with an iron stain (Figure 4).
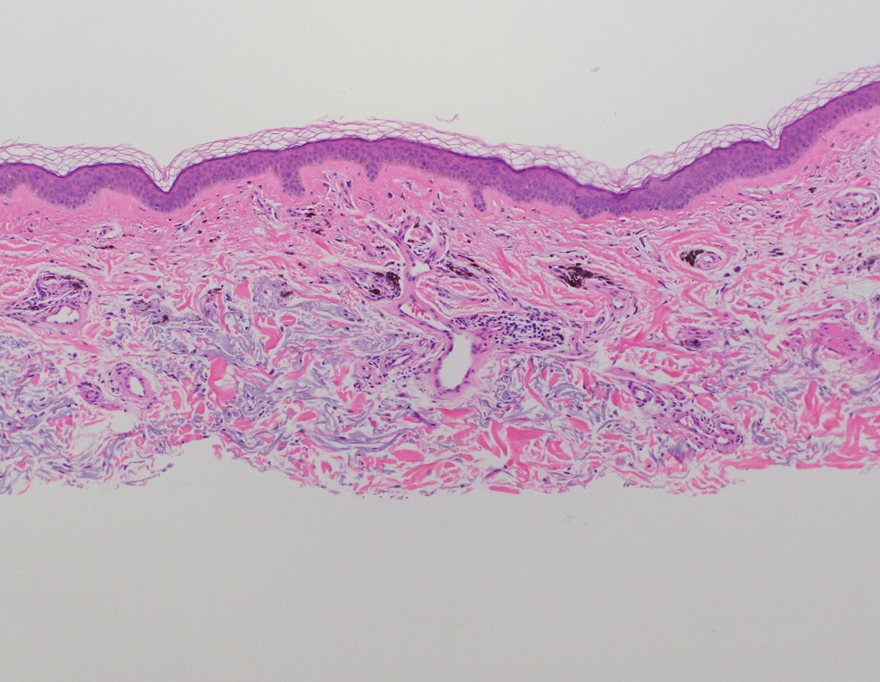
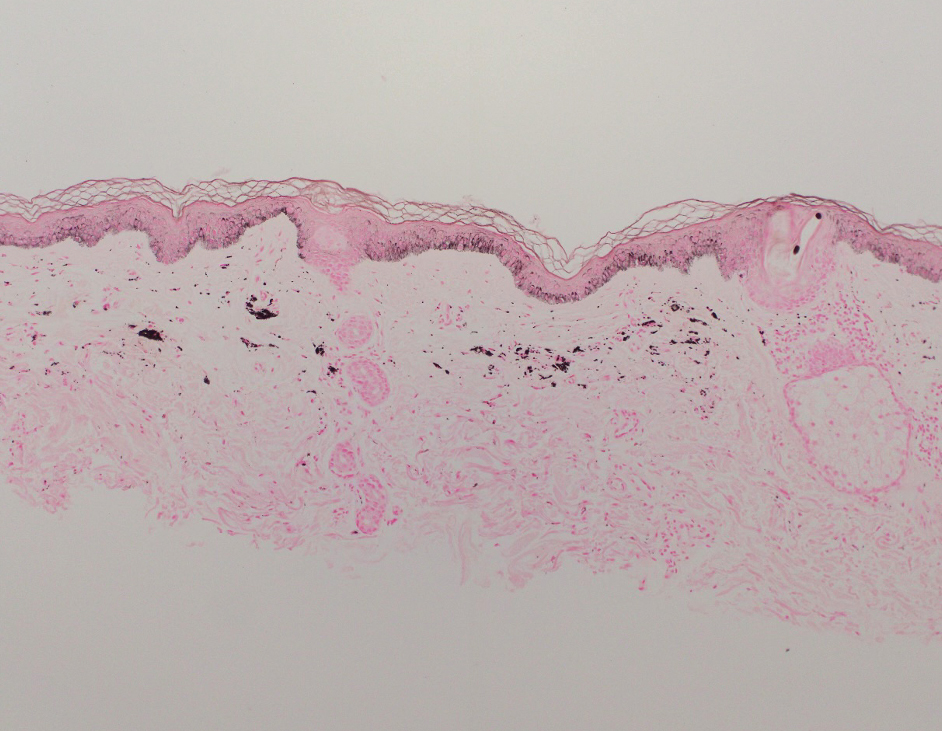
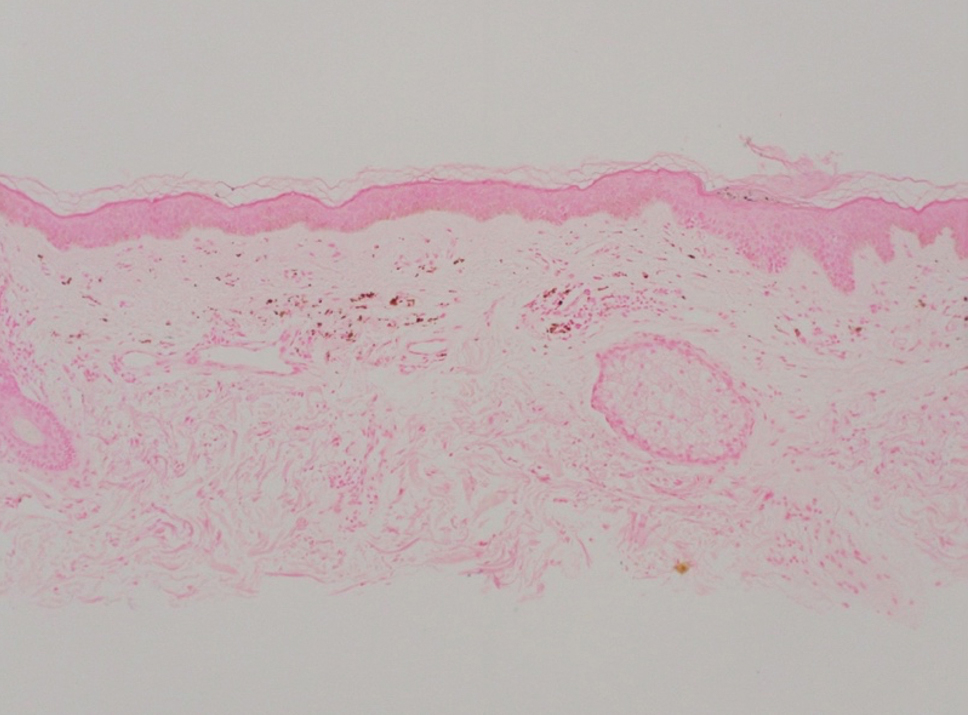
Adalimumab-induced hyperpigmentation was considered. A prior case of adalimumab-induced hyperpigmentation manifested on the face. Histopathology was consistent with a superficial, perivascular, lymphocytic infiltrate with melanophages in the dermis; however, hyperpigmentation was absent in the periorbital area, and affected areas faded 4 months after discontinuation of adalimumab.12 Our patient presented with hyperpigmentation 1 year after adalimumab cessation, and the hyperpigmented areas included the periorbital region. Because of the distinct temporal and clinical features, adalimumab-induced hyperpigmentation was eliminated from the differential diagnosis.
Based on the photodistributed pattern of hyperpigmentation, histopathology, and the temporal relationship between hyperpigmentation onset and kratom usage, a diagnosis of kratom-induced photodistributed hyperpigmentation was made. The patient was advised to discontinue kratom use and use sun protection to prevent further photodamage. The patient subsequently was lost to follow-up.
Kratom alkaloids bind all 3 opioid receptors—μOP, δOP, and κOPs—in a G-protein–biased manner with 7-hydroxymitragynine, the most pharmacologically active alkaloid, exhibiting a higher affinity for μ-opioid receptors.13,14 In human epidermal melanocytes, binding between μ-opioid receptors and β-endorphin, an endogenous opioid, is associated with increased melanin production. This melanogenesis has been linked to hyperpigmentation.15 Given the similarity between kratom alkaloids and β-endorphin in opioid-receptor binding, it is possible that kratom-induced hyperpigmentation may occur through a similar mechanism involving μ-opioid receptors and melanogenesis in epidermal melanocytes. Moreover, some researchers have theorized that sun exposure may result in free radical formation of certain drugs or their metabolites. These free radicals then can interact with cellular DNA, triggering the release of pigmentary mediators and resulting in hyperpigmentation.16 This theory may explain the photodistributed pattern of kratom-induced hyperpigmentation. Further studies are needed to understand the mechanism behind this adverse reaction and its implications for patient treatment.
Literature on kratom-induced hyperpigmentation is limited. Powell et al17 reported a similar case of kratom-induced photodistributed hyperpigmentation—a White man had taken kratom to reduce opioid use and subsequently developed hyperpigmented patches on the arms and face. Moreover, anonymous Reddit users have shared anecdotal reports of hyperpigmentation following kratom use.18
Physicians should be aware of hyperpigmentation as a potential adverse reaction of kratom use as its prevalence increases globally. Further research is warranted to elucidate the mechanism behind this adverse reaction and identify risk factors.
- Prozialeck WC, Avery BA, Boyer EW, et al. Kratom policy: the challenge of balancing therapeutic potential with public safety. Int J Drug Policy. 2019;70:70-77. doi:10.1016/j.drugpo.2019.05.003
- Bergen-Cico D, MacClurg K. Kratom (Mitragyna speciosa) use, addiction potential, and legal status. In: Preedy VR, ed. Neuropathology of Drug Addictions and Substance Misuse. 2016:903-911. doi:10.1016/B978-0-12-800634-4.00089-5
- Warner ML, Kaufman NC, Grundmann O. The pharmacology and toxicology of kratom: from traditional herb to drug of abuse. Int J Legal Med. 2016;130:127-138. doi:10.1007/s00414-015-1279-y
- Transnational Institute. Kratom in Thailand: decriminalisation and community control? May 3, 2011. Accessed August 23, 2024. https://www.tni.org/en/publication/kratom-in-thailand-decriminalisation-and-community-control
- Eastlack SC, Cornett EM, Kaye AD. Kratom—pharmacology, clinical implications, and outlook: a comprehensive review. Pain Ther. 2020;9:55-69. doi:10.1007/s40122-020-00151-x
- Reyes R. Family of Florida mom who died from herbal substance kratom wins $11M suit. New York Post. July 30, 2023. Updated July 31, 2023. Accessed August 23, 2024. https://nypost.com/2023/07/30/family-of-florida-mom-who-died-from-herbal-substance-kratom-wins-11m-suit/
- Garcia-Romeu A, Cox DJ, Smith KE, et al. Kratom (Mitragyna speciosa): user demographics, use patterns, and implications for the opioid epidemic. Drug Alcohol Depend. 2020;208:107849. doi:10.1016/j.drugalcdep.2020.107849
- Mayo Clinic. Kratom: unsafe and ineffective. Accessed August 23, 2024. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/kratom/art-20402171
- Sethi R, Hoang N, Ravishankar DA, et al. Kratom (Mitragyna speciosa): friend or foe? Prim Care Companion CNS Disord. 2020;22:19nr02507.
- Eggleston W, Stoppacher R, Suen K, et al. Kratom use and toxicities in the United States. Pharmacother J Hum Pharmacol Drug Ther. 2019;39:775-777. doi:10.1002/phar.2280
- Qrius. 6 benefits of kratom you should know for healthy skin. March 21, 2023. Accessed August 23, 2024. https://qrius.com/6-benefits-of-kratom-you-should-know-for-healthy-skin/
- Blomberg M, Zachariae COC, Grønhøj F. Hyperpigmentation of the face following adalimumab treatment. Acta Derm Venereol. 2009;89:546-547. doi:10.2340/00015555-0697
- Matsumoto K, Hatori Y, Murayama T, et al. Involvement of μ-opioid receptors in antinociception and inhibition of gastrointestinal transit induced by 7-hydroxymitragynine, isolated from Thai herbal medicine Mitragyna speciosa. Eur J Pharmacol. 2006;549:63-70. doi:10.1016/j.ejphar.2006.08.013
- Jentsch MJ, Pippin MM. Kratom. In: StatPearls. StatPearls Publishing; 2023.
- Bigliardi PL, Tobin DJ, Gaveriaux-Ruff C, et al. Opioids and the skin—where do we stand? Exp Dermatol. 2009;18:424-430.
- Boyer M, Katta R, Markus R. Diltiazem-induced photodistributed hyperpigmentation. Dermatol Online J. 2003;9:10. doi:10.5070/D33c97j4z5
- Powell LR, Ryser TJ, Morey GE, et al. Kratom as a novel cause of photodistributed hyperpigmentation. JAAD Case Rep. 2022;28:145-148. doi:10.1016/j.jdcr.2022.07.033
- Haccoon. Skin discoloring? Reddit. June 30, 2019. Accessed August 23, 2024. https://www.reddit.com/r/quittingkratom/comments/c7b1cm/skin_discoloring/
To the Editor:
Kratom (Mitragyna speciosa) is an evergreen tree native to Southeast Asia.1 Its leaves contain psychoactive compounds including mitragynine and 7-hydroxymitragynine, which exert dose-dependent effects on the central nervous system through opioid and monoaminergic receptors.2,3 At low doses (1–5 g), kratom elicits mild stimulant effects such as increased sociability, alertness, and talkativeness. At high doses (5–15 g), kratom has depressant effects that can provide relief from pain and opioid-withdrawal symptoms.3
Traditionally, kratom has been used in Southeast Asia for recreational and ceremonial purposes, to ease opioid-withdrawal symptoms, and to reduce fatigue from manual labor.4 In the 21st century, availability of kratom expanded to Europe, Australia, and the United States, largely facilitated by widespread dissemination of deceitful marketing and unregulated sales on the internet.1 Although large-scale epidemiologic studies evaluating kratom’s prevalence are scarce, available evidence indicates rising worldwide usage, with a notable increase in kratom-related poison center calls between 2011 and 2017 in the United States.5 In July 2023, kratom made headlines due to the death of a woman in Florida following use of the substance.6
A cross-sectional study revealed that in the United States, kratom typically is used by White individuals for self-treatment of anxiety, depression, pain, and opioid withdrawal.7 However, the potential for severe adverse effects and dependence on kratom can outweigh the benefits.6,8 Reported adverse effects of kratom include tachycardia, hypercholesteremia, liver injury, hallucinations, respiratory depression, seizure, coma, and death.9,10 We present a case of kratom-induced photodistributed hyperpigmentation.
A 63-year-old man presented to the dermatology clinic with diffuse tender, pruritic, hyperpigmented skin lesions that developed over the course of 1 year. The lesions were distributed on sun-exposed areas, including the face, neck, and forearms (Figure 1). The patient reported no other major symptoms, and his health was otherwise unremarkable. He had a medical history of psoriasiform and spongiotic dermatitis consistent with eczema, psoriasis, hypercholesteremia, and hyperlipidemia. The patient was not taking any medications at the time of presentation. He had a family history of plaque psoriasis in his father. Five years prior to the current presentation, the patient was treated with adalimumab for steroid-resistant psoriasis; however, despite initial improvement, he experienced recurrence of scaly erythematous plaques and had discontinued adalimumab the year prior to presentation.

When adalimumab was discontinued, the patient sought alternative treatment for the skin symptoms and began self-administering kratom in an attempt to alleviate associated physical discomfort. He ingested approximately 3 bottles of liquid kratom per day, with each bottle containing 180 mg of mitragynine and less than 8 mg of 7-hydroxymitragynine. Although not scientifically proven, kratom has been colloquially advertised to improve psoriasis.11 The patient reported no other medication use or allergies.
Shave biopsies of hyperpigmented lesions on the right side of the neck, ear, and forearm were performed. Histopathology revealed a sparse superficial, perivascular, lymphocytic infiltrate accompanied by a prominent number of melanophages in the superficial dermis (Figure 2). Special stains further confirmed that the pigment was melanin; the specimens stained positive with Fontana-Masson stain (Figure 3) and negative with an iron stain (Figure 4).
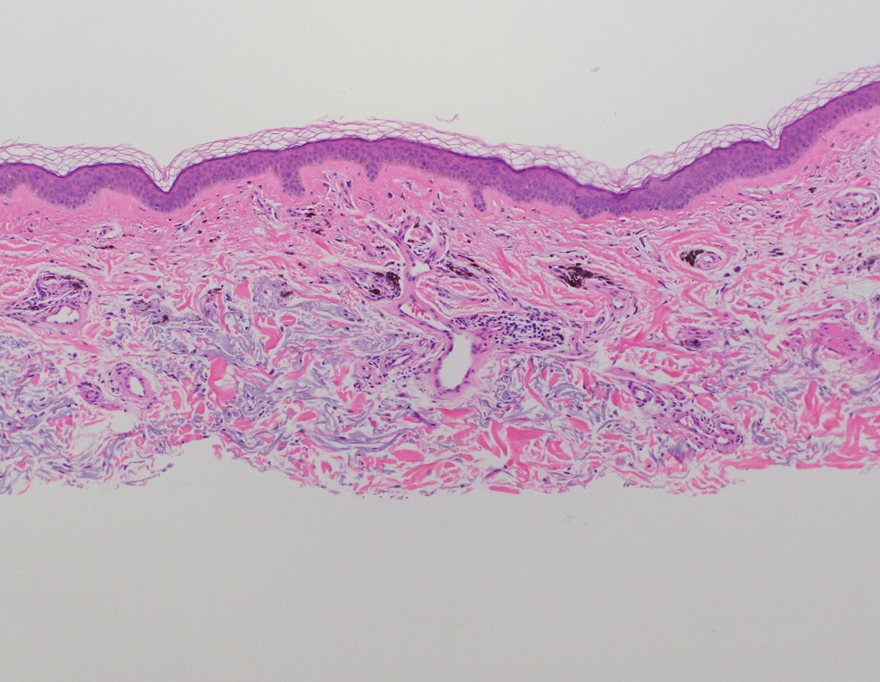
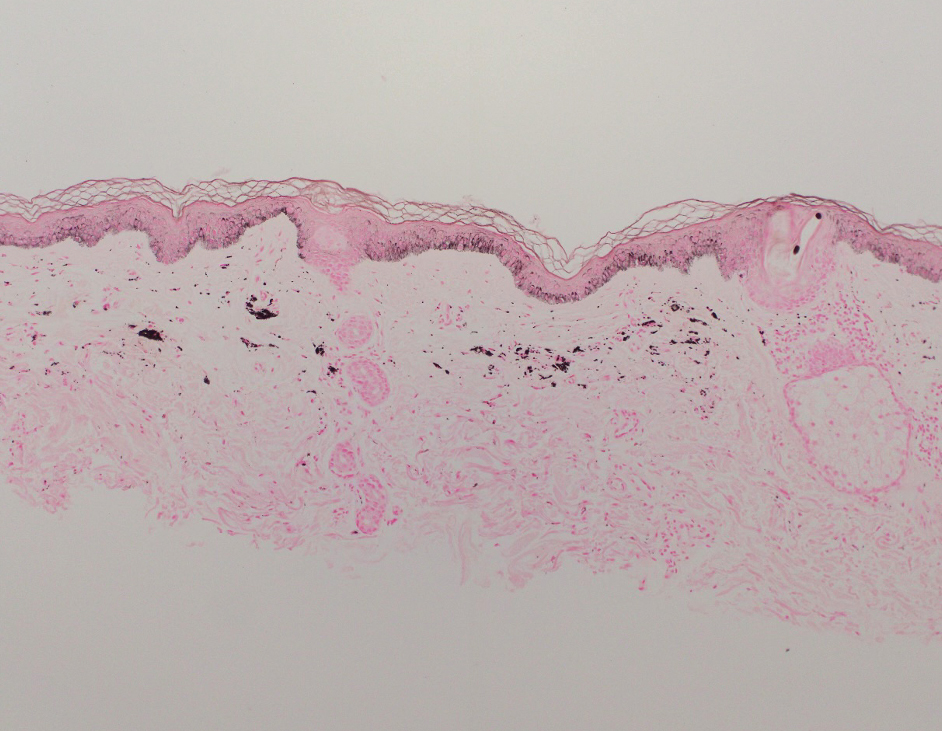
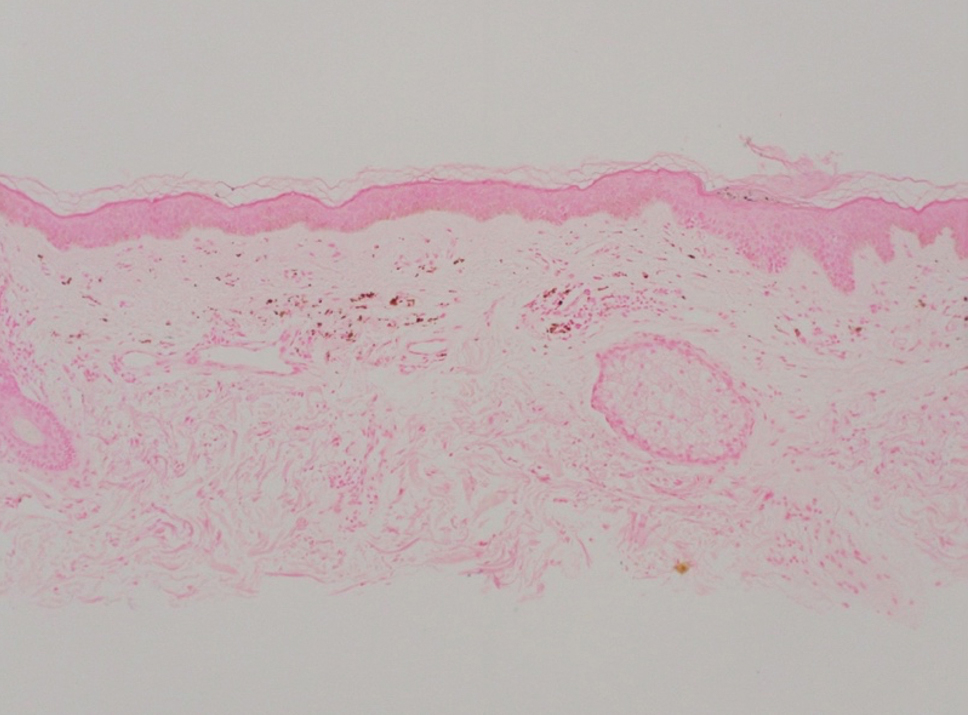
Adalimumab-induced hyperpigmentation was considered. A prior case of adalimumab-induced hyperpigmentation manifested on the face. Histopathology was consistent with a superficial, perivascular, lymphocytic infiltrate with melanophages in the dermis; however, hyperpigmentation was absent in the periorbital area, and affected areas faded 4 months after discontinuation of adalimumab.12 Our patient presented with hyperpigmentation 1 year after adalimumab cessation, and the hyperpigmented areas included the periorbital region. Because of the distinct temporal and clinical features, adalimumab-induced hyperpigmentation was eliminated from the differential diagnosis.
Based on the photodistributed pattern of hyperpigmentation, histopathology, and the temporal relationship between hyperpigmentation onset and kratom usage, a diagnosis of kratom-induced photodistributed hyperpigmentation was made. The patient was advised to discontinue kratom use and use sun protection to prevent further photodamage. The patient subsequently was lost to follow-up.
Kratom alkaloids bind all 3 opioid receptors—μOP, δOP, and κOPs—in a G-protein–biased manner with 7-hydroxymitragynine, the most pharmacologically active alkaloid, exhibiting a higher affinity for μ-opioid receptors.13,14 In human epidermal melanocytes, binding between μ-opioid receptors and β-endorphin, an endogenous opioid, is associated with increased melanin production. This melanogenesis has been linked to hyperpigmentation.15 Given the similarity between kratom alkaloids and β-endorphin in opioid-receptor binding, it is possible that kratom-induced hyperpigmentation may occur through a similar mechanism involving μ-opioid receptors and melanogenesis in epidermal melanocytes. Moreover, some researchers have theorized that sun exposure may result in free radical formation of certain drugs or their metabolites. These free radicals then can interact with cellular DNA, triggering the release of pigmentary mediators and resulting in hyperpigmentation.16 This theory may explain the photodistributed pattern of kratom-induced hyperpigmentation. Further studies are needed to understand the mechanism behind this adverse reaction and its implications for patient treatment.
Literature on kratom-induced hyperpigmentation is limited. Powell et al17 reported a similar case of kratom-induced photodistributed hyperpigmentation—a White man had taken kratom to reduce opioid use and subsequently developed hyperpigmented patches on the arms and face. Moreover, anonymous Reddit users have shared anecdotal reports of hyperpigmentation following kratom use.18
Physicians should be aware of hyperpigmentation as a potential adverse reaction of kratom use as its prevalence increases globally. Further research is warranted to elucidate the mechanism behind this adverse reaction and identify risk factors.
To the Editor:
Kratom (Mitragyna speciosa) is an evergreen tree native to Southeast Asia.1 Its leaves contain psychoactive compounds including mitragynine and 7-hydroxymitragynine, which exert dose-dependent effects on the central nervous system through opioid and monoaminergic receptors.2,3 At low doses (1–5 g), kratom elicits mild stimulant effects such as increased sociability, alertness, and talkativeness. At high doses (5–15 g), kratom has depressant effects that can provide relief from pain and opioid-withdrawal symptoms.3
Traditionally, kratom has been used in Southeast Asia for recreational and ceremonial purposes, to ease opioid-withdrawal symptoms, and to reduce fatigue from manual labor.4 In the 21st century, availability of kratom expanded to Europe, Australia, and the United States, largely facilitated by widespread dissemination of deceitful marketing and unregulated sales on the internet.1 Although large-scale epidemiologic studies evaluating kratom’s prevalence are scarce, available evidence indicates rising worldwide usage, with a notable increase in kratom-related poison center calls between 2011 and 2017 in the United States.5 In July 2023, kratom made headlines due to the death of a woman in Florida following use of the substance.6
A cross-sectional study revealed that in the United States, kratom typically is used by White individuals for self-treatment of anxiety, depression, pain, and opioid withdrawal.7 However, the potential for severe adverse effects and dependence on kratom can outweigh the benefits.6,8 Reported adverse effects of kratom include tachycardia, hypercholesteremia, liver injury, hallucinations, respiratory depression, seizure, coma, and death.9,10 We present a case of kratom-induced photodistributed hyperpigmentation.
A 63-year-old man presented to the dermatology clinic with diffuse tender, pruritic, hyperpigmented skin lesions that developed over the course of 1 year. The lesions were distributed on sun-exposed areas, including the face, neck, and forearms (Figure 1). The patient reported no other major symptoms, and his health was otherwise unremarkable. He had a medical history of psoriasiform and spongiotic dermatitis consistent with eczema, psoriasis, hypercholesteremia, and hyperlipidemia. The patient was not taking any medications at the time of presentation. He had a family history of plaque psoriasis in his father. Five years prior to the current presentation, the patient was treated with adalimumab for steroid-resistant psoriasis; however, despite initial improvement, he experienced recurrence of scaly erythematous plaques and had discontinued adalimumab the year prior to presentation.

When adalimumab was discontinued, the patient sought alternative treatment for the skin symptoms and began self-administering kratom in an attempt to alleviate associated physical discomfort. He ingested approximately 3 bottles of liquid kratom per day, with each bottle containing 180 mg of mitragynine and less than 8 mg of 7-hydroxymitragynine. Although not scientifically proven, kratom has been colloquially advertised to improve psoriasis.11 The patient reported no other medication use or allergies.
Shave biopsies of hyperpigmented lesions on the right side of the neck, ear, and forearm were performed. Histopathology revealed a sparse superficial, perivascular, lymphocytic infiltrate accompanied by a prominent number of melanophages in the superficial dermis (Figure 2). Special stains further confirmed that the pigment was melanin; the specimens stained positive with Fontana-Masson stain (Figure 3) and negative with an iron stain (Figure 4).
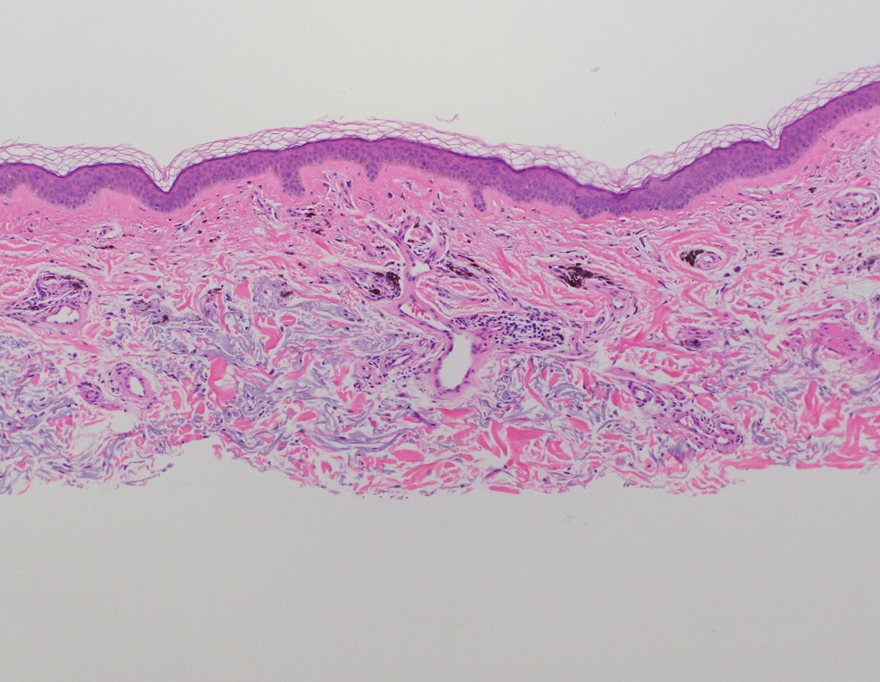
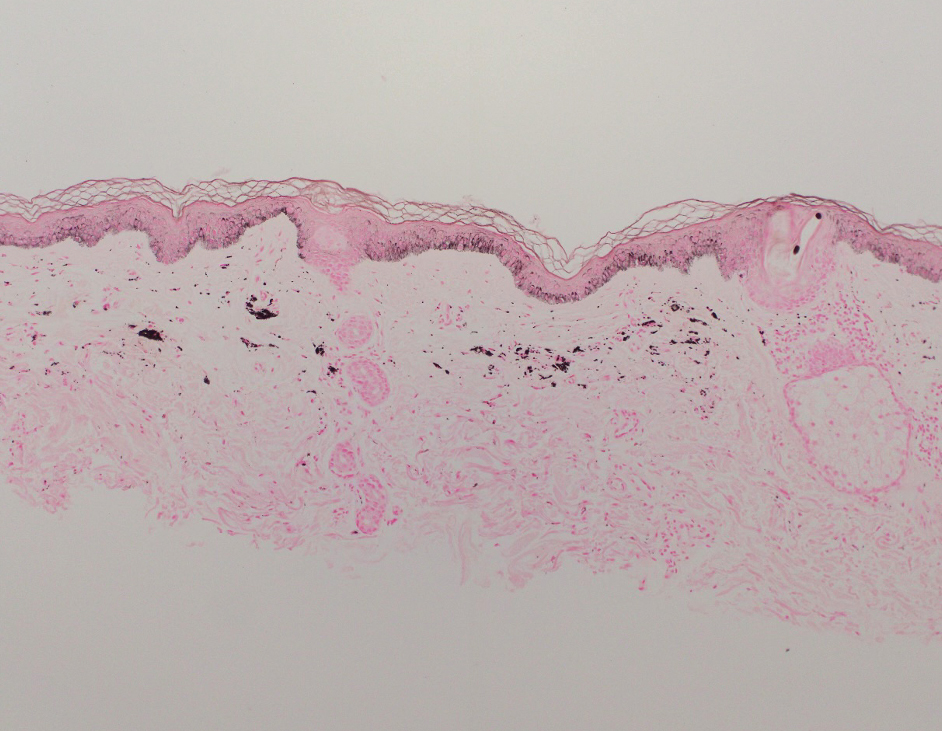
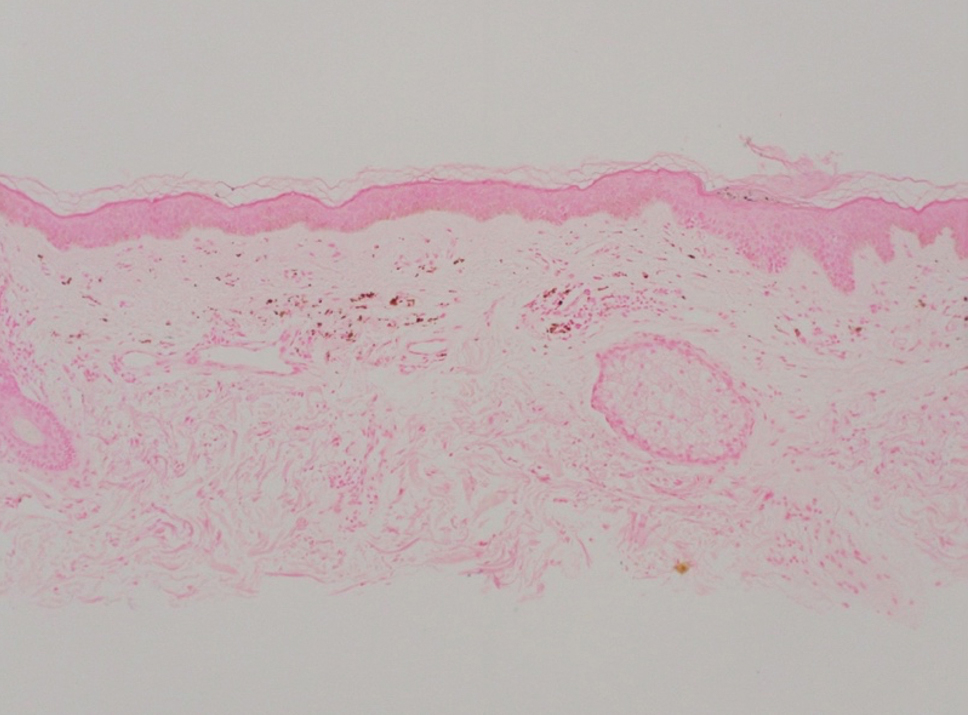
Adalimumab-induced hyperpigmentation was considered. A prior case of adalimumab-induced hyperpigmentation manifested on the face. Histopathology was consistent with a superficial, perivascular, lymphocytic infiltrate with melanophages in the dermis; however, hyperpigmentation was absent in the periorbital area, and affected areas faded 4 months after discontinuation of adalimumab.12 Our patient presented with hyperpigmentation 1 year after adalimumab cessation, and the hyperpigmented areas included the periorbital region. Because of the distinct temporal and clinical features, adalimumab-induced hyperpigmentation was eliminated from the differential diagnosis.
Based on the photodistributed pattern of hyperpigmentation, histopathology, and the temporal relationship between hyperpigmentation onset and kratom usage, a diagnosis of kratom-induced photodistributed hyperpigmentation was made. The patient was advised to discontinue kratom use and use sun protection to prevent further photodamage. The patient subsequently was lost to follow-up.
Kratom alkaloids bind all 3 opioid receptors—μOP, δOP, and κOPs—in a G-protein–biased manner with 7-hydroxymitragynine, the most pharmacologically active alkaloid, exhibiting a higher affinity for μ-opioid receptors.13,14 In human epidermal melanocytes, binding between μ-opioid receptors and β-endorphin, an endogenous opioid, is associated with increased melanin production. This melanogenesis has been linked to hyperpigmentation.15 Given the similarity between kratom alkaloids and β-endorphin in opioid-receptor binding, it is possible that kratom-induced hyperpigmentation may occur through a similar mechanism involving μ-opioid receptors and melanogenesis in epidermal melanocytes. Moreover, some researchers have theorized that sun exposure may result in free radical formation of certain drugs or their metabolites. These free radicals then can interact with cellular DNA, triggering the release of pigmentary mediators and resulting in hyperpigmentation.16 This theory may explain the photodistributed pattern of kratom-induced hyperpigmentation. Further studies are needed to understand the mechanism behind this adverse reaction and its implications for patient treatment.
Literature on kratom-induced hyperpigmentation is limited. Powell et al17 reported a similar case of kratom-induced photodistributed hyperpigmentation—a White man had taken kratom to reduce opioid use and subsequently developed hyperpigmented patches on the arms and face. Moreover, anonymous Reddit users have shared anecdotal reports of hyperpigmentation following kratom use.18
Physicians should be aware of hyperpigmentation as a potential adverse reaction of kratom use as its prevalence increases globally. Further research is warranted to elucidate the mechanism behind this adverse reaction and identify risk factors.
- Prozialeck WC, Avery BA, Boyer EW, et al. Kratom policy: the challenge of balancing therapeutic potential with public safety. Int J Drug Policy. 2019;70:70-77. doi:10.1016/j.drugpo.2019.05.003
- Bergen-Cico D, MacClurg K. Kratom (Mitragyna speciosa) use, addiction potential, and legal status. In: Preedy VR, ed. Neuropathology of Drug Addictions and Substance Misuse. 2016:903-911. doi:10.1016/B978-0-12-800634-4.00089-5
- Warner ML, Kaufman NC, Grundmann O. The pharmacology and toxicology of kratom: from traditional herb to drug of abuse. Int J Legal Med. 2016;130:127-138. doi:10.1007/s00414-015-1279-y
- Transnational Institute. Kratom in Thailand: decriminalisation and community control? May 3, 2011. Accessed August 23, 2024. https://www.tni.org/en/publication/kratom-in-thailand-decriminalisation-and-community-control
- Eastlack SC, Cornett EM, Kaye AD. Kratom—pharmacology, clinical implications, and outlook: a comprehensive review. Pain Ther. 2020;9:55-69. doi:10.1007/s40122-020-00151-x
- Reyes R. Family of Florida mom who died from herbal substance kratom wins $11M suit. New York Post. July 30, 2023. Updated July 31, 2023. Accessed August 23, 2024. https://nypost.com/2023/07/30/family-of-florida-mom-who-died-from-herbal-substance-kratom-wins-11m-suit/
- Garcia-Romeu A, Cox DJ, Smith KE, et al. Kratom (Mitragyna speciosa): user demographics, use patterns, and implications for the opioid epidemic. Drug Alcohol Depend. 2020;208:107849. doi:10.1016/j.drugalcdep.2020.107849
- Mayo Clinic. Kratom: unsafe and ineffective. Accessed August 23, 2024. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/kratom/art-20402171
- Sethi R, Hoang N, Ravishankar DA, et al. Kratom (Mitragyna speciosa): friend or foe? Prim Care Companion CNS Disord. 2020;22:19nr02507.
- Eggleston W, Stoppacher R, Suen K, et al. Kratom use and toxicities in the United States. Pharmacother J Hum Pharmacol Drug Ther. 2019;39:775-777. doi:10.1002/phar.2280
- Qrius. 6 benefits of kratom you should know for healthy skin. March 21, 2023. Accessed August 23, 2024. https://qrius.com/6-benefits-of-kratom-you-should-know-for-healthy-skin/
- Blomberg M, Zachariae COC, Grønhøj F. Hyperpigmentation of the face following adalimumab treatment. Acta Derm Venereol. 2009;89:546-547. doi:10.2340/00015555-0697
- Matsumoto K, Hatori Y, Murayama T, et al. Involvement of μ-opioid receptors in antinociception and inhibition of gastrointestinal transit induced by 7-hydroxymitragynine, isolated from Thai herbal medicine Mitragyna speciosa. Eur J Pharmacol. 2006;549:63-70. doi:10.1016/j.ejphar.2006.08.013
- Jentsch MJ, Pippin MM. Kratom. In: StatPearls. StatPearls Publishing; 2023.
- Bigliardi PL, Tobin DJ, Gaveriaux-Ruff C, et al. Opioids and the skin—where do we stand? Exp Dermatol. 2009;18:424-430.
- Boyer M, Katta R, Markus R. Diltiazem-induced photodistributed hyperpigmentation. Dermatol Online J. 2003;9:10. doi:10.5070/D33c97j4z5
- Powell LR, Ryser TJ, Morey GE, et al. Kratom as a novel cause of photodistributed hyperpigmentation. JAAD Case Rep. 2022;28:145-148. doi:10.1016/j.jdcr.2022.07.033
- Haccoon. Skin discoloring? Reddit. June 30, 2019. Accessed August 23, 2024. https://www.reddit.com/r/quittingkratom/comments/c7b1cm/skin_discoloring/
- Prozialeck WC, Avery BA, Boyer EW, et al. Kratom policy: the challenge of balancing therapeutic potential with public safety. Int J Drug Policy. 2019;70:70-77. doi:10.1016/j.drugpo.2019.05.003
- Bergen-Cico D, MacClurg K. Kratom (Mitragyna speciosa) use, addiction potential, and legal status. In: Preedy VR, ed. Neuropathology of Drug Addictions and Substance Misuse. 2016:903-911. doi:10.1016/B978-0-12-800634-4.00089-5
- Warner ML, Kaufman NC, Grundmann O. The pharmacology and toxicology of kratom: from traditional herb to drug of abuse. Int J Legal Med. 2016;130:127-138. doi:10.1007/s00414-015-1279-y
- Transnational Institute. Kratom in Thailand: decriminalisation and community control? May 3, 2011. Accessed August 23, 2024. https://www.tni.org/en/publication/kratom-in-thailand-decriminalisation-and-community-control
- Eastlack SC, Cornett EM, Kaye AD. Kratom—pharmacology, clinical implications, and outlook: a comprehensive review. Pain Ther. 2020;9:55-69. doi:10.1007/s40122-020-00151-x
- Reyes R. Family of Florida mom who died from herbal substance kratom wins $11M suit. New York Post. July 30, 2023. Updated July 31, 2023. Accessed August 23, 2024. https://nypost.com/2023/07/30/family-of-florida-mom-who-died-from-herbal-substance-kratom-wins-11m-suit/
- Garcia-Romeu A, Cox DJ, Smith KE, et al. Kratom (Mitragyna speciosa): user demographics, use patterns, and implications for the opioid epidemic. Drug Alcohol Depend. 2020;208:107849. doi:10.1016/j.drugalcdep.2020.107849
- Mayo Clinic. Kratom: unsafe and ineffective. Accessed August 23, 2024. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/kratom/art-20402171
- Sethi R, Hoang N, Ravishankar DA, et al. Kratom (Mitragyna speciosa): friend or foe? Prim Care Companion CNS Disord. 2020;22:19nr02507.
- Eggleston W, Stoppacher R, Suen K, et al. Kratom use and toxicities in the United States. Pharmacother J Hum Pharmacol Drug Ther. 2019;39:775-777. doi:10.1002/phar.2280
- Qrius. 6 benefits of kratom you should know for healthy skin. March 21, 2023. Accessed August 23, 2024. https://qrius.com/6-benefits-of-kratom-you-should-know-for-healthy-skin/
- Blomberg M, Zachariae COC, Grønhøj F. Hyperpigmentation of the face following adalimumab treatment. Acta Derm Venereol. 2009;89:546-547. doi:10.2340/00015555-0697
- Matsumoto K, Hatori Y, Murayama T, et al. Involvement of μ-opioid receptors in antinociception and inhibition of gastrointestinal transit induced by 7-hydroxymitragynine, isolated from Thai herbal medicine Mitragyna speciosa. Eur J Pharmacol. 2006;549:63-70. doi:10.1016/j.ejphar.2006.08.013
- Jentsch MJ, Pippin MM. Kratom. In: StatPearls. StatPearls Publishing; 2023.
- Bigliardi PL, Tobin DJ, Gaveriaux-Ruff C, et al. Opioids and the skin—where do we stand? Exp Dermatol. 2009;18:424-430.
- Boyer M, Katta R, Markus R. Diltiazem-induced photodistributed hyperpigmentation. Dermatol Online J. 2003;9:10. doi:10.5070/D33c97j4z5
- Powell LR, Ryser TJ, Morey GE, et al. Kratom as a novel cause of photodistributed hyperpigmentation. JAAD Case Rep. 2022;28:145-148. doi:10.1016/j.jdcr.2022.07.033
- Haccoon. Skin discoloring? Reddit. June 30, 2019. Accessed August 23, 2024. https://www.reddit.com/r/quittingkratom/comments/c7b1cm/skin_discoloring/
Practice Points
- Clinicians should be aware of photodistributed hyperpigmentation as a potential adverse effect of kratom usage.
- Kratom-induced photodistributed hyperpigmentation should be suspected in patients with hyperpigmented lesions in sun-exposed areas of the skin following kratom use. A biopsy of lesions should be obtained to confirm the diagnosis.
- Cessation of kratom should be recommended.
Study Reports Safety Data in Children on JAK Inhibitors
TOPLINE:
which also found that acne was the most common skin-related AE in children, and serious AEs were less common.
METHODOLOGY:
- Researchers analyzed 399,649 AEs in 133,216 adult patients and 2883 AEs in 955 pediatric patients (age, < 18 years) from November 2011 to February 2023 using the US Food and Drug Administration Adverse Event Reporting System and the Canada Vigilance Adverse Reaction Online Database.
- AEs were categorized on the basis of the Medical Dictionary for Regulatory Activities system organ class.
- Five JAK inhibitors approved for use in children were included in the study: Baricitinib, upadacitinib, abrocitinib, ruxolitinib, and tofacitinib.
TAKEAWAY:
- The most frequently reported AEs in children were blood and lymphatic system disorders, including neutropenia, thrombocytopenia, and anemia (24%); viral, fungal, and bacterial infections, such as pneumonia and sepsis (17.2%); constitutional symptoms and administrative concerns, including pyrexia and fatigue (15.7%); gastrointestinal disorders, such as vomiting and abdominal pain (13.6%); and respiratory disorders, such as cough and respiratory distress (5.3%).
- In adults, the most common AEs were viral, fungal, and bacterial infections (16.8%); constitutional symptoms and administrative concerns (13.5%); musculoskeletal and connective tissue disorders (7.04%); and gastrointestinal (5.8%) and nervous system (5%) disorders.
- Acne (30.6%), atopic dermatitis (22.2%), and psoriasis (16.7%) were the most common skin and subcutaneous tissue AEs reported in children. Skin and subcutaneous AEs were more common with upadacitinib (21.1%), abrocitinib (9.1%), and tofacitinib (6.3%) in children.
- Serious AEs included in the boxed warning for JAK inhibitors — serious infection, mortality, malignancy, cardiovascular events, and thrombosis — were similar for baricitinib in children (4 of 49 patients, 8.2%) and adults (325 of 3707, 8.8%). For other JAK inhibitors, absolute numbers of these AEs in children were small and rates were lower in children than in adults.
IN PRACTICE:
“This information can support customized treatment and minimize the potential for undesired or intolerable AEs,” the authors wrote.
SOURCE:
This study was led by Sahithi Talasila, BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and was published online in Pediatric Dermatology.
LIMITATIONS:
Pharmacovigilance registries did not fully capture the complete range of AEs because of potential reporting bias or recall bias. Additionally, events lacking sufficient objective evidence were underreported, while common AEs associated with JAK inhibitor therapy were overreported.
DISCLOSURES:
No specific funding sources for the study were reported. One author reported being a consultant, one reported serving as a principal investigator in clinical trials, and another reported serving on data and safety monitoring boards of various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
which also found that acne was the most common skin-related AE in children, and serious AEs were less common.
METHODOLOGY:
- Researchers analyzed 399,649 AEs in 133,216 adult patients and 2883 AEs in 955 pediatric patients (age, < 18 years) from November 2011 to February 2023 using the US Food and Drug Administration Adverse Event Reporting System and the Canada Vigilance Adverse Reaction Online Database.
- AEs were categorized on the basis of the Medical Dictionary for Regulatory Activities system organ class.
- Five JAK inhibitors approved for use in children were included in the study: Baricitinib, upadacitinib, abrocitinib, ruxolitinib, and tofacitinib.
TAKEAWAY:
- The most frequently reported AEs in children were blood and lymphatic system disorders, including neutropenia, thrombocytopenia, and anemia (24%); viral, fungal, and bacterial infections, such as pneumonia and sepsis (17.2%); constitutional symptoms and administrative concerns, including pyrexia and fatigue (15.7%); gastrointestinal disorders, such as vomiting and abdominal pain (13.6%); and respiratory disorders, such as cough and respiratory distress (5.3%).
- In adults, the most common AEs were viral, fungal, and bacterial infections (16.8%); constitutional symptoms and administrative concerns (13.5%); musculoskeletal and connective tissue disorders (7.04%); and gastrointestinal (5.8%) and nervous system (5%) disorders.
- Acne (30.6%), atopic dermatitis (22.2%), and psoriasis (16.7%) were the most common skin and subcutaneous tissue AEs reported in children. Skin and subcutaneous AEs were more common with upadacitinib (21.1%), abrocitinib (9.1%), and tofacitinib (6.3%) in children.
- Serious AEs included in the boxed warning for JAK inhibitors — serious infection, mortality, malignancy, cardiovascular events, and thrombosis — were similar for baricitinib in children (4 of 49 patients, 8.2%) and adults (325 of 3707, 8.8%). For other JAK inhibitors, absolute numbers of these AEs in children were small and rates were lower in children than in adults.
IN PRACTICE:
“This information can support customized treatment and minimize the potential for undesired or intolerable AEs,” the authors wrote.
SOURCE:
This study was led by Sahithi Talasila, BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and was published online in Pediatric Dermatology.
LIMITATIONS:
Pharmacovigilance registries did not fully capture the complete range of AEs because of potential reporting bias or recall bias. Additionally, events lacking sufficient objective evidence were underreported, while common AEs associated with JAK inhibitor therapy were overreported.
DISCLOSURES:
No specific funding sources for the study were reported. One author reported being a consultant, one reported serving as a principal investigator in clinical trials, and another reported serving on data and safety monitoring boards of various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
which also found that acne was the most common skin-related AE in children, and serious AEs were less common.
METHODOLOGY:
- Researchers analyzed 399,649 AEs in 133,216 adult patients and 2883 AEs in 955 pediatric patients (age, < 18 years) from November 2011 to February 2023 using the US Food and Drug Administration Adverse Event Reporting System and the Canada Vigilance Adverse Reaction Online Database.
- AEs were categorized on the basis of the Medical Dictionary for Regulatory Activities system organ class.
- Five JAK inhibitors approved for use in children were included in the study: Baricitinib, upadacitinib, abrocitinib, ruxolitinib, and tofacitinib.
TAKEAWAY:
- The most frequently reported AEs in children were blood and lymphatic system disorders, including neutropenia, thrombocytopenia, and anemia (24%); viral, fungal, and bacterial infections, such as pneumonia and sepsis (17.2%); constitutional symptoms and administrative concerns, including pyrexia and fatigue (15.7%); gastrointestinal disorders, such as vomiting and abdominal pain (13.6%); and respiratory disorders, such as cough and respiratory distress (5.3%).
- In adults, the most common AEs were viral, fungal, and bacterial infections (16.8%); constitutional symptoms and administrative concerns (13.5%); musculoskeletal and connective tissue disorders (7.04%); and gastrointestinal (5.8%) and nervous system (5%) disorders.
- Acne (30.6%), atopic dermatitis (22.2%), and psoriasis (16.7%) were the most common skin and subcutaneous tissue AEs reported in children. Skin and subcutaneous AEs were more common with upadacitinib (21.1%), abrocitinib (9.1%), and tofacitinib (6.3%) in children.
- Serious AEs included in the boxed warning for JAK inhibitors — serious infection, mortality, malignancy, cardiovascular events, and thrombosis — were similar for baricitinib in children (4 of 49 patients, 8.2%) and adults (325 of 3707, 8.8%). For other JAK inhibitors, absolute numbers of these AEs in children were small and rates were lower in children than in adults.
IN PRACTICE:
“This information can support customized treatment and minimize the potential for undesired or intolerable AEs,” the authors wrote.
SOURCE:
This study was led by Sahithi Talasila, BS, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and was published online in Pediatric Dermatology.
LIMITATIONS:
Pharmacovigilance registries did not fully capture the complete range of AEs because of potential reporting bias or recall bias. Additionally, events lacking sufficient objective evidence were underreported, while common AEs associated with JAK inhibitor therapy were overreported.
DISCLOSURES:
No specific funding sources for the study were reported. One author reported being a consultant, one reported serving as a principal investigator in clinical trials, and another reported serving on data and safety monitoring boards of various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
FDA OKs Subcutaneous Atezolizumab Formulation for Multiple Cancer Indications
Approved indications include non–small cell lung cancer (NSCLC), SCLC, hepatocellular carcinoma, melanoma, and alveolar soft part sarcoma. Specific indications are available with the full prescribing information at Drugs@FDA.
This is the first programmed death–ligand 1 inhibitor to gain approval for subcutaneous administration.
“This approval represents a significant option to improve the patient experience,” Ann Fish-Steagall, RN, Senior Vice President of Patient Services at the LUNGevity Foundation stated in a Genentech press release.
Subcutaneous atezolizumab and hyaluronidase-tqjs was evaluated in the open-label, randomized IMscin001 trial of 371 adult patients with locally advanced or metastatic NSCLC who were not previously exposed to cancer immunotherapy and who had disease progression following treatment with platinum-based chemotherapy. Patients were randomized 2:1 to receive subcutaneous or IV administration until disease progression or unacceptable toxicity.
Atezolizumab exposure, the primary outcome measure of the study, met the lower limit of geometric mean ratio above the prespecified threshold of 0.8 (cycle 1C trough, 1.05; area under the curve for days 0-21, 0.87).
No notable differences were observed in overall response rate, progression-free survival, or overall survival between the two formulations, according to the FDA approval notice.
The confirmed overall response rate was 9% in the subcutaneous arm and 8% intravenous arm.
Adverse events of any grade occurring in at least 10% of patients were fatigue, musculoskeletal pain, cough, dyspnea, and decreased appetite.
The recommended dose for subcutaneous injection is one 15 mL injection, which contains 1875 mg of atezolizumab and 30,000 units of hyaluronidase.
Injections should be administered in the thigh over approximately 7 minutes every 3 weeks. By contrast, IV administration generally takes 30-60 minutes.
A version of this article first appeared on Medscape.com.
Approved indications include non–small cell lung cancer (NSCLC), SCLC, hepatocellular carcinoma, melanoma, and alveolar soft part sarcoma. Specific indications are available with the full prescribing information at Drugs@FDA.
This is the first programmed death–ligand 1 inhibitor to gain approval for subcutaneous administration.
“This approval represents a significant option to improve the patient experience,” Ann Fish-Steagall, RN, Senior Vice President of Patient Services at the LUNGevity Foundation stated in a Genentech press release.
Subcutaneous atezolizumab and hyaluronidase-tqjs was evaluated in the open-label, randomized IMscin001 trial of 371 adult patients with locally advanced or metastatic NSCLC who were not previously exposed to cancer immunotherapy and who had disease progression following treatment with platinum-based chemotherapy. Patients were randomized 2:1 to receive subcutaneous or IV administration until disease progression or unacceptable toxicity.
Atezolizumab exposure, the primary outcome measure of the study, met the lower limit of geometric mean ratio above the prespecified threshold of 0.8 (cycle 1C trough, 1.05; area under the curve for days 0-21, 0.87).
No notable differences were observed in overall response rate, progression-free survival, or overall survival between the two formulations, according to the FDA approval notice.
The confirmed overall response rate was 9% in the subcutaneous arm and 8% intravenous arm.
Adverse events of any grade occurring in at least 10% of patients were fatigue, musculoskeletal pain, cough, dyspnea, and decreased appetite.
The recommended dose for subcutaneous injection is one 15 mL injection, which contains 1875 mg of atezolizumab and 30,000 units of hyaluronidase.
Injections should be administered in the thigh over approximately 7 minutes every 3 weeks. By contrast, IV administration generally takes 30-60 minutes.
A version of this article first appeared on Medscape.com.
Approved indications include non–small cell lung cancer (NSCLC), SCLC, hepatocellular carcinoma, melanoma, and alveolar soft part sarcoma. Specific indications are available with the full prescribing information at Drugs@FDA.
This is the first programmed death–ligand 1 inhibitor to gain approval for subcutaneous administration.
“This approval represents a significant option to improve the patient experience,” Ann Fish-Steagall, RN, Senior Vice President of Patient Services at the LUNGevity Foundation stated in a Genentech press release.
Subcutaneous atezolizumab and hyaluronidase-tqjs was evaluated in the open-label, randomized IMscin001 trial of 371 adult patients with locally advanced or metastatic NSCLC who were not previously exposed to cancer immunotherapy and who had disease progression following treatment with platinum-based chemotherapy. Patients were randomized 2:1 to receive subcutaneous or IV administration until disease progression or unacceptable toxicity.
Atezolizumab exposure, the primary outcome measure of the study, met the lower limit of geometric mean ratio above the prespecified threshold of 0.8 (cycle 1C trough, 1.05; area under the curve for days 0-21, 0.87).
No notable differences were observed in overall response rate, progression-free survival, or overall survival between the two formulations, according to the FDA approval notice.
The confirmed overall response rate was 9% in the subcutaneous arm and 8% intravenous arm.
Adverse events of any grade occurring in at least 10% of patients were fatigue, musculoskeletal pain, cough, dyspnea, and decreased appetite.
The recommended dose for subcutaneous injection is one 15 mL injection, which contains 1875 mg of atezolizumab and 30,000 units of hyaluronidase.
Injections should be administered in the thigh over approximately 7 minutes every 3 weeks. By contrast, IV administration generally takes 30-60 minutes.
A version of this article first appeared on Medscape.com.


