User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
AACE: New algorithm stresses lifestyle modification in type 2 diabetes
Lifestyle modification must be the cornerstone of any management plan for type 2 diabetes.
Effectively attending to basic problems – obesity, nutrition, and exercise – will dramatically increase the success of any long-term treatment plan for patients with type 2 diabetes (T2DM), and help prevent or delay disease development in those with prediabetes, according to a new treatment algorithm.
The document, published by the American Association of Clinical Endocrinology, is an annual update to its unique strategy of clarifying T2DM management.
The 2016 AACE/ACE Comprehensive Diabetes Management Algorithm presents an easy-to-follow stepwise decision model for diagnosis, blood glucose management, and medical management – including all of the currently approved oral diabetes medications and insulins (Endocr Pract. 2016 Jan;22[1]:84-113). The original algorithm was launched 10 years ago and was last updated in 2013.
This new iteration is the first to place lifestyle intervention as a foundation for the most effective medical management.
“Obviously, this is very important,” said Dr. Paul S. Jellinger, a member of the algorithm writing committee, and an endocrinologist in Fort Lauderdale, Fla. “Weight loss, fitness training, and nutritional management play important roles in the management of blood glucose, lipids, and blood pressure. Appropriate focus in this direction may reduce medication dosage and at times eliminate the need for pharmaceutical intervention. We have all experienced improved therapeutic results in patients who are engaged in effective lifestyle therapy.”
As well as being a text document replete with data-driven details, the algorithm is presented in a colorful poster format that is very helpful for both doctors and patients alike, said Dr. George Grunberger, AACE president. It’s an especially effective tool when considering treatment decisions in the 12 different drug classes used in T2DM management.
“It’s one thing to talk about risk and benefits but to see it graphically displayed is very helpful,” he said in an interview. “I have the poster in every exam room, and every time I am with a patient, I can point out where we are and where we are heading. Rather than me just talking, I can show exactly where we are and where we want to go.”
It is especially helpful for primary care physicians, who care for the vast majority of patients with T2DM, Dr. Grunberger said in an interview.
“We are trying to get better management information into primary care. Most people with diabetes will never see a specialist in their entire life. They need help with glycemic control, obesity, prediabetes, dyslipidemia, and these are the bread and butter of primary care. But there are so many new things going on in this field, and primary care doctors are already in over their heads with the amount of things they deal with. So we have sorted it out and provide practical, practice-oriented guidelines about how to get from A to B.”
Dr. Grunberger noted that most of the recommendations in the document are based on expert opinion. “There are no randomized, controlled trials for most of this stuff. Many of the medications are relatively new, and with 12 drug classes, there’s no way you can ever do a trial with every permutation.”
The new document is similar to the 2013 algorithm with regard to medical management, Dr. Grunberger said. Its focus on lifestyle modification as an integral part of treatment is new, however. “The initial algorithm 10 years ago was solely based on glycemic control. Now we’ve decided to look at more than blood sugar – at obesity, overweight, hypertension and dyslipidemia. You cannot ignore these things in a disease where the major morbidity and mortality are cardiovascular.”
The algorithm stresses that “lifestyle optimization” is essential for all patients with diabetes. “[It] is multifaceted, ongoing, and should engage the entire diabetes team.”
There are several key components to lifestyle modification. All of these should be addressed early.
Medical nutrition therapy
This is a fundamental issue that must be addressed. A primarily plant-based diet high in poly- and monounsaturated fats is recommended, with the goal of a 5%-10% reduction in body weight for overweight or obese patients. In addition to discussing foods that damage and promote metabolic health, patients may need help with carbohydrate and sugar intake. Structured counseling is an excellent way to achieve consistent results.
Physical activity
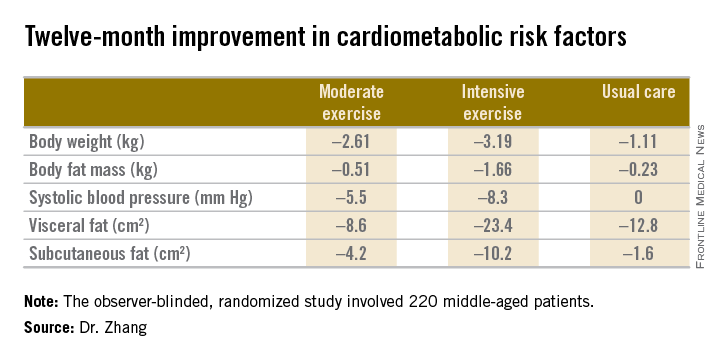
Regular exercise improves glucose control and lowers lipid and blood pressure levels. It decreases the chance of falls and fractures, promotes functional capacity, and reduces the risk of depression. The goal should be at least 150 minutes of moderate-intense exercise each week. Every patient – and particularly those with complications of diabetes and/or obesity – should have a thorough physical exam before embarking on an exercise program.
Adequate rest
Emerging data continue to confirm the importance of sleep in health and disease. Getting 6-9 hours each night is associated with a reduction in cardiometabolic risk factors. Sleep deprivation aggravates insulin resistance, hypertension, hyperglycemia, and dyslipidemia and increases proinflammatory cytokines. An evaluation for obstructive sleep apnea may be in order, especially for obese patients.
Behavioral support
It’s impossible to overstate the importance of support in a successful lifestyle modification program. Patients should be encouraged to join community groups that facilitate and teach healthy behaviors. Not only will doing so help improve compliance, but being part of a structured group also reaps social and cognitive benefits.
Smoking cessation
The final component of the program, smoking cessation, is critical. All forms of tobacco should be eliminated.
While lifestyle modification is crucial, it should not obviate prompt medical therapy. “Such efforts should not delay needed pharmacotherapy, which can be initiated simultaneously and adjusted based on patient response to lifestyle efforts,” the document notes. “The need for medical therapy should not be interpreted as a failure of lifestyle management but as an adjunct to it.”
Aggressive medical therapy really accelerates effective diabetes treatment, Dr. Jellinger said.
“Clinical inertia has been and remains a huge problem. Some studies demonstrate as much as a 2-year delay in advancing therapy while the patient still remains far from hemoglobin A1c goal. For decades a ‘treat to failure’ concept dominated, i.e., that we should advance therapy only after a prolonged period of failure on existing therapy. One of the major contributions of the earlier AACE algorithms as well as the current version has been the strong therapeutic mandate to re-evaluate the patient and make a therapeutic change in no longer than 3 months. This is a direct attempt to eliminate clinical inertia.”
Dr. Grunberger agreed.
“Why do we wait until people are sick and experiencing complications before we take them seriously? Preventing and dealing with overweight and obesity is complicated, but if you treat obesity, you are treating diabetes. We emphasize starting medical therapy early, going to combination therapy quickly because no one drug usually achieves the target, and trying to be aggressive. Get people on the right treatment as quickly as possible and sustain success – don’t go from one failure to another.”
Dr. Jellinger has received support from Amarin, Boehringer Ingelheim, Bristol-Myers Squibb/AstraZeneca, Janssen Pharmaceuticals, and Novo Nordisk.
Dr. Grunberger has received remuneration and research funding from Eli Lilly, BI-Lilly, Novo Nordisk, Sanofi, Janssen, AstraZeneca, Merck, Medtronic, and GlaxoSmithKline.
Lifestyle modification must be the cornerstone of any management plan for type 2 diabetes.
Effectively attending to basic problems – obesity, nutrition, and exercise – will dramatically increase the success of any long-term treatment plan for patients with type 2 diabetes (T2DM), and help prevent or delay disease development in those with prediabetes, according to a new treatment algorithm.
The document, published by the American Association of Clinical Endocrinology, is an annual update to its unique strategy of clarifying T2DM management.
The 2016 AACE/ACE Comprehensive Diabetes Management Algorithm presents an easy-to-follow stepwise decision model for diagnosis, blood glucose management, and medical management – including all of the currently approved oral diabetes medications and insulins (Endocr Pract. 2016 Jan;22[1]:84-113). The original algorithm was launched 10 years ago and was last updated in 2013.
This new iteration is the first to place lifestyle intervention as a foundation for the most effective medical management.
“Obviously, this is very important,” said Dr. Paul S. Jellinger, a member of the algorithm writing committee, and an endocrinologist in Fort Lauderdale, Fla. “Weight loss, fitness training, and nutritional management play important roles in the management of blood glucose, lipids, and blood pressure. Appropriate focus in this direction may reduce medication dosage and at times eliminate the need for pharmaceutical intervention. We have all experienced improved therapeutic results in patients who are engaged in effective lifestyle therapy.”
As well as being a text document replete with data-driven details, the algorithm is presented in a colorful poster format that is very helpful for both doctors and patients alike, said Dr. George Grunberger, AACE president. It’s an especially effective tool when considering treatment decisions in the 12 different drug classes used in T2DM management.
“It’s one thing to talk about risk and benefits but to see it graphically displayed is very helpful,” he said in an interview. “I have the poster in every exam room, and every time I am with a patient, I can point out where we are and where we are heading. Rather than me just talking, I can show exactly where we are and where we want to go.”
It is especially helpful for primary care physicians, who care for the vast majority of patients with T2DM, Dr. Grunberger said in an interview.
“We are trying to get better management information into primary care. Most people with diabetes will never see a specialist in their entire life. They need help with glycemic control, obesity, prediabetes, dyslipidemia, and these are the bread and butter of primary care. But there are so many new things going on in this field, and primary care doctors are already in over their heads with the amount of things they deal with. So we have sorted it out and provide practical, practice-oriented guidelines about how to get from A to B.”
Dr. Grunberger noted that most of the recommendations in the document are based on expert opinion. “There are no randomized, controlled trials for most of this stuff. Many of the medications are relatively new, and with 12 drug classes, there’s no way you can ever do a trial with every permutation.”
The new document is similar to the 2013 algorithm with regard to medical management, Dr. Grunberger said. Its focus on lifestyle modification as an integral part of treatment is new, however. “The initial algorithm 10 years ago was solely based on glycemic control. Now we’ve decided to look at more than blood sugar – at obesity, overweight, hypertension and dyslipidemia. You cannot ignore these things in a disease where the major morbidity and mortality are cardiovascular.”
The algorithm stresses that “lifestyle optimization” is essential for all patients with diabetes. “[It] is multifaceted, ongoing, and should engage the entire diabetes team.”
There are several key components to lifestyle modification. All of these should be addressed early.
Medical nutrition therapy
This is a fundamental issue that must be addressed. A primarily plant-based diet high in poly- and monounsaturated fats is recommended, with the goal of a 5%-10% reduction in body weight for overweight or obese patients. In addition to discussing foods that damage and promote metabolic health, patients may need help with carbohydrate and sugar intake. Structured counseling is an excellent way to achieve consistent results.
Physical activity
Regular exercise improves glucose control and lowers lipid and blood pressure levels. It decreases the chance of falls and fractures, promotes functional capacity, and reduces the risk of depression. The goal should be at least 150 minutes of moderate-intense exercise each week. Every patient – and particularly those with complications of diabetes and/or obesity – should have a thorough physical exam before embarking on an exercise program.
Adequate rest
Emerging data continue to confirm the importance of sleep in health and disease. Getting 6-9 hours each night is associated with a reduction in cardiometabolic risk factors. Sleep deprivation aggravates insulin resistance, hypertension, hyperglycemia, and dyslipidemia and increases proinflammatory cytokines. An evaluation for obstructive sleep apnea may be in order, especially for obese patients.
Behavioral support
It’s impossible to overstate the importance of support in a successful lifestyle modification program. Patients should be encouraged to join community groups that facilitate and teach healthy behaviors. Not only will doing so help improve compliance, but being part of a structured group also reaps social and cognitive benefits.
Smoking cessation
The final component of the program, smoking cessation, is critical. All forms of tobacco should be eliminated.
While lifestyle modification is crucial, it should not obviate prompt medical therapy. “Such efforts should not delay needed pharmacotherapy, which can be initiated simultaneously and adjusted based on patient response to lifestyle efforts,” the document notes. “The need for medical therapy should not be interpreted as a failure of lifestyle management but as an adjunct to it.”
Aggressive medical therapy really accelerates effective diabetes treatment, Dr. Jellinger said.
“Clinical inertia has been and remains a huge problem. Some studies demonstrate as much as a 2-year delay in advancing therapy while the patient still remains far from hemoglobin A1c goal. For decades a ‘treat to failure’ concept dominated, i.e., that we should advance therapy only after a prolonged period of failure on existing therapy. One of the major contributions of the earlier AACE algorithms as well as the current version has been the strong therapeutic mandate to re-evaluate the patient and make a therapeutic change in no longer than 3 months. This is a direct attempt to eliminate clinical inertia.”
Dr. Grunberger agreed.
“Why do we wait until people are sick and experiencing complications before we take them seriously? Preventing and dealing with overweight and obesity is complicated, but if you treat obesity, you are treating diabetes. We emphasize starting medical therapy early, going to combination therapy quickly because no one drug usually achieves the target, and trying to be aggressive. Get people on the right treatment as quickly as possible and sustain success – don’t go from one failure to another.”
Dr. Jellinger has received support from Amarin, Boehringer Ingelheim, Bristol-Myers Squibb/AstraZeneca, Janssen Pharmaceuticals, and Novo Nordisk.
Dr. Grunberger has received remuneration and research funding from Eli Lilly, BI-Lilly, Novo Nordisk, Sanofi, Janssen, AstraZeneca, Merck, Medtronic, and GlaxoSmithKline.
Lifestyle modification must be the cornerstone of any management plan for type 2 diabetes.
Effectively attending to basic problems – obesity, nutrition, and exercise – will dramatically increase the success of any long-term treatment plan for patients with type 2 diabetes (T2DM), and help prevent or delay disease development in those with prediabetes, according to a new treatment algorithm.
The document, published by the American Association of Clinical Endocrinology, is an annual update to its unique strategy of clarifying T2DM management.
The 2016 AACE/ACE Comprehensive Diabetes Management Algorithm presents an easy-to-follow stepwise decision model for diagnosis, blood glucose management, and medical management – including all of the currently approved oral diabetes medications and insulins (Endocr Pract. 2016 Jan;22[1]:84-113). The original algorithm was launched 10 years ago and was last updated in 2013.
This new iteration is the first to place lifestyle intervention as a foundation for the most effective medical management.
“Obviously, this is very important,” said Dr. Paul S. Jellinger, a member of the algorithm writing committee, and an endocrinologist in Fort Lauderdale, Fla. “Weight loss, fitness training, and nutritional management play important roles in the management of blood glucose, lipids, and blood pressure. Appropriate focus in this direction may reduce medication dosage and at times eliminate the need for pharmaceutical intervention. We have all experienced improved therapeutic results in patients who are engaged in effective lifestyle therapy.”
As well as being a text document replete with data-driven details, the algorithm is presented in a colorful poster format that is very helpful for both doctors and patients alike, said Dr. George Grunberger, AACE president. It’s an especially effective tool when considering treatment decisions in the 12 different drug classes used in T2DM management.
“It’s one thing to talk about risk and benefits but to see it graphically displayed is very helpful,” he said in an interview. “I have the poster in every exam room, and every time I am with a patient, I can point out where we are and where we are heading. Rather than me just talking, I can show exactly where we are and where we want to go.”
It is especially helpful for primary care physicians, who care for the vast majority of patients with T2DM, Dr. Grunberger said in an interview.
“We are trying to get better management information into primary care. Most people with diabetes will never see a specialist in their entire life. They need help with glycemic control, obesity, prediabetes, dyslipidemia, and these are the bread and butter of primary care. But there are so many new things going on in this field, and primary care doctors are already in over their heads with the amount of things they deal with. So we have sorted it out and provide practical, practice-oriented guidelines about how to get from A to B.”
Dr. Grunberger noted that most of the recommendations in the document are based on expert opinion. “There are no randomized, controlled trials for most of this stuff. Many of the medications are relatively new, and with 12 drug classes, there’s no way you can ever do a trial with every permutation.”
The new document is similar to the 2013 algorithm with regard to medical management, Dr. Grunberger said. Its focus on lifestyle modification as an integral part of treatment is new, however. “The initial algorithm 10 years ago was solely based on glycemic control. Now we’ve decided to look at more than blood sugar – at obesity, overweight, hypertension and dyslipidemia. You cannot ignore these things in a disease where the major morbidity and mortality are cardiovascular.”
The algorithm stresses that “lifestyle optimization” is essential for all patients with diabetes. “[It] is multifaceted, ongoing, and should engage the entire diabetes team.”
There are several key components to lifestyle modification. All of these should be addressed early.
Medical nutrition therapy
This is a fundamental issue that must be addressed. A primarily plant-based diet high in poly- and monounsaturated fats is recommended, with the goal of a 5%-10% reduction in body weight for overweight or obese patients. In addition to discussing foods that damage and promote metabolic health, patients may need help with carbohydrate and sugar intake. Structured counseling is an excellent way to achieve consistent results.
Physical activity
Regular exercise improves glucose control and lowers lipid and blood pressure levels. It decreases the chance of falls and fractures, promotes functional capacity, and reduces the risk of depression. The goal should be at least 150 minutes of moderate-intense exercise each week. Every patient – and particularly those with complications of diabetes and/or obesity – should have a thorough physical exam before embarking on an exercise program.
Adequate rest
Emerging data continue to confirm the importance of sleep in health and disease. Getting 6-9 hours each night is associated with a reduction in cardiometabolic risk factors. Sleep deprivation aggravates insulin resistance, hypertension, hyperglycemia, and dyslipidemia and increases proinflammatory cytokines. An evaluation for obstructive sleep apnea may be in order, especially for obese patients.
Behavioral support
It’s impossible to overstate the importance of support in a successful lifestyle modification program. Patients should be encouraged to join community groups that facilitate and teach healthy behaviors. Not only will doing so help improve compliance, but being part of a structured group also reaps social and cognitive benefits.
Smoking cessation
The final component of the program, smoking cessation, is critical. All forms of tobacco should be eliminated.
While lifestyle modification is crucial, it should not obviate prompt medical therapy. “Such efforts should not delay needed pharmacotherapy, which can be initiated simultaneously and adjusted based on patient response to lifestyle efforts,” the document notes. “The need for medical therapy should not be interpreted as a failure of lifestyle management but as an adjunct to it.”
Aggressive medical therapy really accelerates effective diabetes treatment, Dr. Jellinger said.
“Clinical inertia has been and remains a huge problem. Some studies demonstrate as much as a 2-year delay in advancing therapy while the patient still remains far from hemoglobin A1c goal. For decades a ‘treat to failure’ concept dominated, i.e., that we should advance therapy only after a prolonged period of failure on existing therapy. One of the major contributions of the earlier AACE algorithms as well as the current version has been the strong therapeutic mandate to re-evaluate the patient and make a therapeutic change in no longer than 3 months. This is a direct attempt to eliminate clinical inertia.”
Dr. Grunberger agreed.
“Why do we wait until people are sick and experiencing complications before we take them seriously? Preventing and dealing with overweight and obesity is complicated, but if you treat obesity, you are treating diabetes. We emphasize starting medical therapy early, going to combination therapy quickly because no one drug usually achieves the target, and trying to be aggressive. Get people on the right treatment as quickly as possible and sustain success – don’t go from one failure to another.”
Dr. Jellinger has received support from Amarin, Boehringer Ingelheim, Bristol-Myers Squibb/AstraZeneca, Janssen Pharmaceuticals, and Novo Nordisk.
Dr. Grunberger has received remuneration and research funding from Eli Lilly, BI-Lilly, Novo Nordisk, Sanofi, Janssen, AstraZeneca, Merck, Medtronic, and GlaxoSmithKline.
Antipsychotics may double to triple diabetes risk in youth
Youth who received at least 3 months of antipsychotics were about two to three times more likely to develop type 2 diabetes, compared with controls, a meta-analysis of 13 studies shows.
The risk was especially apparent for olanzapine, confirming “that [type 2 diabetes] risk with second-generation antipsychotics is not homogeneous, and that olanzapine treatment is a major modifiable risk factor,” said Dr. Britta Galling of Zucker Hillside Hospital in Glen Oaks, N.Y., and her associates. Youth should receive antipsychotics only if safer treatments have failed, for the shortest possible effective duration, with proactive monitoring of cardiovascular risk factors and counseling about possible adverse effects, healthy nutrition, and physical activity, according to the meta-analysis, published online Jan. 19.
The researchers searched PubMed and PsycINFO through May 2015 for longitudinal studies of antipsychotics and type 2 diabetes in children, adolescents, and young adults who did not have diabetes at baseline. The resulting studies included 185,105 individuals and 310,438 patient-years. Patients averaged 14.1 years of age (range, 2-24 years), were followed for an average of 1.7 years, and 60% were male (JAMA Psychiatry. 2016 Jan 20. doi: 10.1001/jamapsychiatry.2015.2923).
Antipsychotic exposure doubled the odds (95% confidence interval, 1.56-4.24; P less than .0001) and tripled the incidence (95% CI, 1.7-5.3; P less than .0001) of type 2 diabetes, compared with healthy controls. Antipsychotic-exposed youth also had double the odds and 1.8 times the incidence of type 2 diabetes, compared with psychiatric controls.
The multivariate analysis linked greater cumulative type 2 diabetes risk with longer follow-up (P less than .001), olanzapine exposure (P less than .001), and male sex (P = .002). However, the incidence of type 2 diabetes was lower in youth with autism spectrum disorders (P = .048), perhaps because of other medications or the fact that other psychiatric disorders have a higher type 2 diabetes risk, compared with ASDs, the researchers said.
“These risks should be considered in the clinical risk-benefit evaluation when initiating or continuing antipsychotic treatment in this age group,” they wrote.
The research was funded by the Zucker Hillside Hospital, the National Institute of Mental Health–funded Advanced Center for Interventions and Services Research in Schizophrenia, and the Agency for Healthcare Research & Quality. Dr. Galling had no disclosures. Senior author Dr. Christoph U. Correll, medical director of the recognition and prevention program at the Zucker Hillside Hospital, and his 11 coauthors reported financial relationships the numerous pharmaceutical companies and nonprofit institutions.
Youth who received at least 3 months of antipsychotics were about two to three times more likely to develop type 2 diabetes, compared with controls, a meta-analysis of 13 studies shows.
The risk was especially apparent for olanzapine, confirming “that [type 2 diabetes] risk with second-generation antipsychotics is not homogeneous, and that olanzapine treatment is a major modifiable risk factor,” said Dr. Britta Galling of Zucker Hillside Hospital in Glen Oaks, N.Y., and her associates. Youth should receive antipsychotics only if safer treatments have failed, for the shortest possible effective duration, with proactive monitoring of cardiovascular risk factors and counseling about possible adverse effects, healthy nutrition, and physical activity, according to the meta-analysis, published online Jan. 19.
The researchers searched PubMed and PsycINFO through May 2015 for longitudinal studies of antipsychotics and type 2 diabetes in children, adolescents, and young adults who did not have diabetes at baseline. The resulting studies included 185,105 individuals and 310,438 patient-years. Patients averaged 14.1 years of age (range, 2-24 years), were followed for an average of 1.7 years, and 60% were male (JAMA Psychiatry. 2016 Jan 20. doi: 10.1001/jamapsychiatry.2015.2923).
Antipsychotic exposure doubled the odds (95% confidence interval, 1.56-4.24; P less than .0001) and tripled the incidence (95% CI, 1.7-5.3; P less than .0001) of type 2 diabetes, compared with healthy controls. Antipsychotic-exposed youth also had double the odds and 1.8 times the incidence of type 2 diabetes, compared with psychiatric controls.
The multivariate analysis linked greater cumulative type 2 diabetes risk with longer follow-up (P less than .001), olanzapine exposure (P less than .001), and male sex (P = .002). However, the incidence of type 2 diabetes was lower in youth with autism spectrum disorders (P = .048), perhaps because of other medications or the fact that other psychiatric disorders have a higher type 2 diabetes risk, compared with ASDs, the researchers said.
“These risks should be considered in the clinical risk-benefit evaluation when initiating or continuing antipsychotic treatment in this age group,” they wrote.
The research was funded by the Zucker Hillside Hospital, the National Institute of Mental Health–funded Advanced Center for Interventions and Services Research in Schizophrenia, and the Agency for Healthcare Research & Quality. Dr. Galling had no disclosures. Senior author Dr. Christoph U. Correll, medical director of the recognition and prevention program at the Zucker Hillside Hospital, and his 11 coauthors reported financial relationships the numerous pharmaceutical companies and nonprofit institutions.
Youth who received at least 3 months of antipsychotics were about two to three times more likely to develop type 2 diabetes, compared with controls, a meta-analysis of 13 studies shows.
The risk was especially apparent for olanzapine, confirming “that [type 2 diabetes] risk with second-generation antipsychotics is not homogeneous, and that olanzapine treatment is a major modifiable risk factor,” said Dr. Britta Galling of Zucker Hillside Hospital in Glen Oaks, N.Y., and her associates. Youth should receive antipsychotics only if safer treatments have failed, for the shortest possible effective duration, with proactive monitoring of cardiovascular risk factors and counseling about possible adverse effects, healthy nutrition, and physical activity, according to the meta-analysis, published online Jan. 19.
The researchers searched PubMed and PsycINFO through May 2015 for longitudinal studies of antipsychotics and type 2 diabetes in children, adolescents, and young adults who did not have diabetes at baseline. The resulting studies included 185,105 individuals and 310,438 patient-years. Patients averaged 14.1 years of age (range, 2-24 years), were followed for an average of 1.7 years, and 60% were male (JAMA Psychiatry. 2016 Jan 20. doi: 10.1001/jamapsychiatry.2015.2923).
Antipsychotic exposure doubled the odds (95% confidence interval, 1.56-4.24; P less than .0001) and tripled the incidence (95% CI, 1.7-5.3; P less than .0001) of type 2 diabetes, compared with healthy controls. Antipsychotic-exposed youth also had double the odds and 1.8 times the incidence of type 2 diabetes, compared with psychiatric controls.
The multivariate analysis linked greater cumulative type 2 diabetes risk with longer follow-up (P less than .001), olanzapine exposure (P less than .001), and male sex (P = .002). However, the incidence of type 2 diabetes was lower in youth with autism spectrum disorders (P = .048), perhaps because of other medications or the fact that other psychiatric disorders have a higher type 2 diabetes risk, compared with ASDs, the researchers said.
“These risks should be considered in the clinical risk-benefit evaluation when initiating or continuing antipsychotic treatment in this age group,” they wrote.
The research was funded by the Zucker Hillside Hospital, the National Institute of Mental Health–funded Advanced Center for Interventions and Services Research in Schizophrenia, and the Agency for Healthcare Research & Quality. Dr. Galling had no disclosures. Senior author Dr. Christoph U. Correll, medical director of the recognition and prevention program at the Zucker Hillside Hospital, and his 11 coauthors reported financial relationships the numerous pharmaceutical companies and nonprofit institutions.
FROM JAMA PSYCHIATRY
Key clinical point: Antipsychotics, particularly olanzapine, greatly increased the risk of type 2 diabetes mellitus in young people.
Major finding: The increase was about twofold, compared with psychiatric controls, and threefold, compared with healthy controls.
Data source: A meta-analysis of 13 studies of more than 185,000 youth aged 2-24 years who did not have type 2 diabetes at baseline.
Disclosures: The research was funded by the Zucker Hillside Hospital, the National Institute of Mental Health–funded Advanced Center for Interventions and Services Research in Schizophrenia, and the Agency for Healthcare Research & Quality. Dr. Galling had no disclosures. Senior author Dr. Christoph U. Correll, medical director of the recognition and prevention program at the Zucker Hillside Hospital, and 11 coauthors reported financial relationships to the numerous pharmaceutical companies and nonprofit institutions.
WDC: Resveratrol improves cerebral perfusion in type 2 diabetes
Vancouver, B.C. – Resveratrol increased cerebral blood vessel dilation in a small study of adults with type 2 diabetes mellitus, suggesting a possible role for slowing disease-related cognitive decline, according to investigators from the University of Newcastle (Australia).
Type 2 diabetes impairs the ability of blood vessels to dilate effectively in response to demand, which may impact mental performance and perhaps contribute to the greater risk of dementia in people with the disease, according to investigator Rachel Wong, Ph.D., a biomedical researcher at the university.
Her team previously demonstrated that resveratrol – a polyphenol found in berries, nuts, grapes, and, famously, red wine – improves vasodilation in the systemic circulation, so they wanted to see if would do the same in the brain (Nutr Metab Cardiovasc Dis. 2011 Nov;21(11):851-6).
Thirty-six dementia-free adults with type 2 diabetes took one of three doses of synthetic resveratrol – 75 mg, 150 mg, and 300 mg – or placebo at weekly intervals. Before and about an hour after each dose, the patients briefly breathed carbogen gas (95% oxygen, 5% carbon dioxide) to induce hypercapnia and subsequent cerebral vasodilation. Transcranial Doppler ultrasound was used to assess the change in blood flow in the middle and posterior cerebral arteries before and after dosing.
The percentage change in mean blood flow velocity in the middle cerebral arteries increased after all three doses of resveratrol, but not after placebo. The 75 and 300 mg doses both increased flow velocity by about 10%, while the 150 mg dose increased it by about 6%. Meanwhile, the 75 mg dose was the only one to increase vasodilator responsiveness in the posterior cerebral arteries.
“This is the first clinical evidence that resveratrol can enhance vasodilator responsiveness in people with type 2 diabetes. We are now investigating if regular supplementation can restore cerebral perfusion, and if that can attenuate the accelerated cognitive decline seen in this population,” Dr. Wong said.
They plan to test that with the 75 mg dose, the amount of resveratrol in about 30 liters of red wine. “I think it’s better to get it in the synthetic form,” she said.
The patients in the study were 68 years old on average, with a mean body mass index of 30 kg/m2. They had diabetes for about 10 years, and their mean hemoglobin A1c was 6.7%. The majority of subjects were on oral diabetes therapies; none of them was on insulin.
The investigators have no disclosures. The work was funded in part by the Australian National University and by DSM Nutritional Products, which provided the resveratrol.
Vancouver, B.C. – Resveratrol increased cerebral blood vessel dilation in a small study of adults with type 2 diabetes mellitus, suggesting a possible role for slowing disease-related cognitive decline, according to investigators from the University of Newcastle (Australia).
Type 2 diabetes impairs the ability of blood vessels to dilate effectively in response to demand, which may impact mental performance and perhaps contribute to the greater risk of dementia in people with the disease, according to investigator Rachel Wong, Ph.D., a biomedical researcher at the university.
Her team previously demonstrated that resveratrol – a polyphenol found in berries, nuts, grapes, and, famously, red wine – improves vasodilation in the systemic circulation, so they wanted to see if would do the same in the brain (Nutr Metab Cardiovasc Dis. 2011 Nov;21(11):851-6).
Thirty-six dementia-free adults with type 2 diabetes took one of three doses of synthetic resveratrol – 75 mg, 150 mg, and 300 mg – or placebo at weekly intervals. Before and about an hour after each dose, the patients briefly breathed carbogen gas (95% oxygen, 5% carbon dioxide) to induce hypercapnia and subsequent cerebral vasodilation. Transcranial Doppler ultrasound was used to assess the change in blood flow in the middle and posterior cerebral arteries before and after dosing.
The percentage change in mean blood flow velocity in the middle cerebral arteries increased after all three doses of resveratrol, but not after placebo. The 75 and 300 mg doses both increased flow velocity by about 10%, while the 150 mg dose increased it by about 6%. Meanwhile, the 75 mg dose was the only one to increase vasodilator responsiveness in the posterior cerebral arteries.
“This is the first clinical evidence that resveratrol can enhance vasodilator responsiveness in people with type 2 diabetes. We are now investigating if regular supplementation can restore cerebral perfusion, and if that can attenuate the accelerated cognitive decline seen in this population,” Dr. Wong said.
They plan to test that with the 75 mg dose, the amount of resveratrol in about 30 liters of red wine. “I think it’s better to get it in the synthetic form,” she said.
The patients in the study were 68 years old on average, with a mean body mass index of 30 kg/m2. They had diabetes for about 10 years, and their mean hemoglobin A1c was 6.7%. The majority of subjects were on oral diabetes therapies; none of them was on insulin.
The investigators have no disclosures. The work was funded in part by the Australian National University and by DSM Nutritional Products, which provided the resveratrol.
Vancouver, B.C. – Resveratrol increased cerebral blood vessel dilation in a small study of adults with type 2 diabetes mellitus, suggesting a possible role for slowing disease-related cognitive decline, according to investigators from the University of Newcastle (Australia).
Type 2 diabetes impairs the ability of blood vessels to dilate effectively in response to demand, which may impact mental performance and perhaps contribute to the greater risk of dementia in people with the disease, according to investigator Rachel Wong, Ph.D., a biomedical researcher at the university.
Her team previously demonstrated that resveratrol – a polyphenol found in berries, nuts, grapes, and, famously, red wine – improves vasodilation in the systemic circulation, so they wanted to see if would do the same in the brain (Nutr Metab Cardiovasc Dis. 2011 Nov;21(11):851-6).
Thirty-six dementia-free adults with type 2 diabetes took one of three doses of synthetic resveratrol – 75 mg, 150 mg, and 300 mg – or placebo at weekly intervals. Before and about an hour after each dose, the patients briefly breathed carbogen gas (95% oxygen, 5% carbon dioxide) to induce hypercapnia and subsequent cerebral vasodilation. Transcranial Doppler ultrasound was used to assess the change in blood flow in the middle and posterior cerebral arteries before and after dosing.
The percentage change in mean blood flow velocity in the middle cerebral arteries increased after all three doses of resveratrol, but not after placebo. The 75 and 300 mg doses both increased flow velocity by about 10%, while the 150 mg dose increased it by about 6%. Meanwhile, the 75 mg dose was the only one to increase vasodilator responsiveness in the posterior cerebral arteries.
“This is the first clinical evidence that resveratrol can enhance vasodilator responsiveness in people with type 2 diabetes. We are now investigating if regular supplementation can restore cerebral perfusion, and if that can attenuate the accelerated cognitive decline seen in this population,” Dr. Wong said.
They plan to test that with the 75 mg dose, the amount of resveratrol in about 30 liters of red wine. “I think it’s better to get it in the synthetic form,” she said.
The patients in the study were 68 years old on average, with a mean body mass index of 30 kg/m2. They had diabetes for about 10 years, and their mean hemoglobin A1c was 6.7%. The majority of subjects were on oral diabetes therapies; none of them was on insulin.
The investigators have no disclosures. The work was funded in part by the Australian National University and by DSM Nutritional Products, which provided the resveratrol.
AT The WORLD DIABETES CONGRESS
Key clinical point: Resveratrol is being investigated to slow cognitive decline in type 2 diabetes.
Major finding: Doses of 75 and 300 mg improved cerebral vasodilator responsiveness by about 10%.
Data source: Dose finding study in 36 type 2 diabetics.
Disclosures: The investigators have no disclosures. The work was funded in part by the Australian National University and DSM Nutritional Products, which provided the resveratrol.
WDC: Screen for and treat patients with diabetes distress
Vancouver, B.C. – Screening for “diabetes distress” should probably be a part of routine care for patients with type 2 diabetes mellitus, according to investigators from the University of British Columbia, Vancouver.
The team administered the Diabetes Distress Scale (DDS) questionnaire to 148 consecutive patients with type 2 diabetes at a university diabetes clinic; 39% scored positively for diabetes distress, as indicated by a score of 2 or more on the DDS, and stress correlated with poorer glycemic control. In particular, higher hemoglobin A1c scores correlated, although weakly, with a higher perception of emotional burden from diabetes (r2 = 0.198) and greater stress over treatment regimens (r2 = 0.249). The correlation between stress and worse glycemic control was strongest in patients with hemoglobin A1c above 9% (r2 = 0.387).
After its first appearance in the medical literature over a decade ago, diabetes distress has been shown to impact how well patients do. It’s a mix of negative emotions – for instance, frustration, anxiety, and burnout – related to the management of disease, and it’s been diagnosed in up to 43% of patients in previous studies. Diabetes distress is distinct from clinical depression. In fact, just 12% of the study subjects screened positive for depression on the Personal Health Questionnaire-9, which was administered along with the DDS,. Depression, although related to the use of insulin, had no impact on glycemic control.
“Diabetes distress, particularly emotional and self-care-related distress, is quite high in this population; I think it’s clinically important that we address it. We should be using some sort of screening for distress,” said investigator Dr. Evelyn Wong, an endocrinology fellow at the university.
Previous investigations have found that if distress is reduced, glycemic control improves. How exactly to do that is the subject of ongoing investigation, but education on self-management seems to help. Improving relationships with health care providers and helping patients find alternatives for problematic regimens might also help, Dr. Wong said at the World Diabetes Congress.
“Diabetes is a bit of a silent disease,” at least until complications emerge, “so patients may not understand why they need to take insulin, or why it’s important to bring down hemoglobin A1c. We” have to make sure they understand such issues and help them come to terms with their illness. Overall, “I think it’s the time spent with the patient that is important,” she said.
A unique finding of the Vancouver study was that patients who felt less satisfied with their providers had better glycemic control. Perhaps they had stricter physicians or were more vigilant about their diabetes because they didn’t have much faith in their physician.
The DDS is a 17 item scale that uses 6-point Likert scales to measure the emotional burden of diabetes; its impact on personal relationships; patient concerns about treatment regimens; and the quality of relationships with providers. For instance, patients are asked the degree to which a “feeling that I will end up with serious long-term complications no matter what I do” applies to them. A two-question diabetes distress screening scale is also available.
Subjects in the study were in their mid-50s on average, the majority were white, and two-thirds were men. They had type 2 diabetes for an average of 9 years; and 20% were on insulin; the mean hemoglobin A1c was 8.7%.
The investigators have no conflicts of interest.
Vancouver, B.C. – Screening for “diabetes distress” should probably be a part of routine care for patients with type 2 diabetes mellitus, according to investigators from the University of British Columbia, Vancouver.
The team administered the Diabetes Distress Scale (DDS) questionnaire to 148 consecutive patients with type 2 diabetes at a university diabetes clinic; 39% scored positively for diabetes distress, as indicated by a score of 2 or more on the DDS, and stress correlated with poorer glycemic control. In particular, higher hemoglobin A1c scores correlated, although weakly, with a higher perception of emotional burden from diabetes (r2 = 0.198) and greater stress over treatment regimens (r2 = 0.249). The correlation between stress and worse glycemic control was strongest in patients with hemoglobin A1c above 9% (r2 = 0.387).
After its first appearance in the medical literature over a decade ago, diabetes distress has been shown to impact how well patients do. It’s a mix of negative emotions – for instance, frustration, anxiety, and burnout – related to the management of disease, and it’s been diagnosed in up to 43% of patients in previous studies. Diabetes distress is distinct from clinical depression. In fact, just 12% of the study subjects screened positive for depression on the Personal Health Questionnaire-9, which was administered along with the DDS,. Depression, although related to the use of insulin, had no impact on glycemic control.
“Diabetes distress, particularly emotional and self-care-related distress, is quite high in this population; I think it’s clinically important that we address it. We should be using some sort of screening for distress,” said investigator Dr. Evelyn Wong, an endocrinology fellow at the university.
Previous investigations have found that if distress is reduced, glycemic control improves. How exactly to do that is the subject of ongoing investigation, but education on self-management seems to help. Improving relationships with health care providers and helping patients find alternatives for problematic regimens might also help, Dr. Wong said at the World Diabetes Congress.
“Diabetes is a bit of a silent disease,” at least until complications emerge, “so patients may not understand why they need to take insulin, or why it’s important to bring down hemoglobin A1c. We” have to make sure they understand such issues and help them come to terms with their illness. Overall, “I think it’s the time spent with the patient that is important,” she said.
A unique finding of the Vancouver study was that patients who felt less satisfied with their providers had better glycemic control. Perhaps they had stricter physicians or were more vigilant about their diabetes because they didn’t have much faith in their physician.
The DDS is a 17 item scale that uses 6-point Likert scales to measure the emotional burden of diabetes; its impact on personal relationships; patient concerns about treatment regimens; and the quality of relationships with providers. For instance, patients are asked the degree to which a “feeling that I will end up with serious long-term complications no matter what I do” applies to them. A two-question diabetes distress screening scale is also available.
Subjects in the study were in their mid-50s on average, the majority were white, and two-thirds were men. They had type 2 diabetes for an average of 9 years; and 20% were on insulin; the mean hemoglobin A1c was 8.7%.
The investigators have no conflicts of interest.
Vancouver, B.C. – Screening for “diabetes distress” should probably be a part of routine care for patients with type 2 diabetes mellitus, according to investigators from the University of British Columbia, Vancouver.
The team administered the Diabetes Distress Scale (DDS) questionnaire to 148 consecutive patients with type 2 diabetes at a university diabetes clinic; 39% scored positively for diabetes distress, as indicated by a score of 2 or more on the DDS, and stress correlated with poorer glycemic control. In particular, higher hemoglobin A1c scores correlated, although weakly, with a higher perception of emotional burden from diabetes (r2 = 0.198) and greater stress over treatment regimens (r2 = 0.249). The correlation between stress and worse glycemic control was strongest in patients with hemoglobin A1c above 9% (r2 = 0.387).
After its first appearance in the medical literature over a decade ago, diabetes distress has been shown to impact how well patients do. It’s a mix of negative emotions – for instance, frustration, anxiety, and burnout – related to the management of disease, and it’s been diagnosed in up to 43% of patients in previous studies. Diabetes distress is distinct from clinical depression. In fact, just 12% of the study subjects screened positive for depression on the Personal Health Questionnaire-9, which was administered along with the DDS,. Depression, although related to the use of insulin, had no impact on glycemic control.
“Diabetes distress, particularly emotional and self-care-related distress, is quite high in this population; I think it’s clinically important that we address it. We should be using some sort of screening for distress,” said investigator Dr. Evelyn Wong, an endocrinology fellow at the university.
Previous investigations have found that if distress is reduced, glycemic control improves. How exactly to do that is the subject of ongoing investigation, but education on self-management seems to help. Improving relationships with health care providers and helping patients find alternatives for problematic regimens might also help, Dr. Wong said at the World Diabetes Congress.
“Diabetes is a bit of a silent disease,” at least until complications emerge, “so patients may not understand why they need to take insulin, or why it’s important to bring down hemoglobin A1c. We” have to make sure they understand such issues and help them come to terms with their illness. Overall, “I think it’s the time spent with the patient that is important,” she said.
A unique finding of the Vancouver study was that patients who felt less satisfied with their providers had better glycemic control. Perhaps they had stricter physicians or were more vigilant about their diabetes because they didn’t have much faith in their physician.
The DDS is a 17 item scale that uses 6-point Likert scales to measure the emotional burden of diabetes; its impact on personal relationships; patient concerns about treatment regimens; and the quality of relationships with providers. For instance, patients are asked the degree to which a “feeling that I will end up with serious long-term complications no matter what I do” applies to them. A two-question diabetes distress screening scale is also available.
Subjects in the study were in their mid-50s on average, the majority were white, and two-thirds were men. They had type 2 diabetes for an average of 9 years; and 20% were on insulin; the mean hemoglobin A1c was 8.7%.
The investigators have no conflicts of interest.
AT The WORLD DIABETES CONGRESS
Key clinical point: It’s becoming clear that patients do better when their stress about having diabetes is addressed.
Major finding: Among 148 patients with type 2 diabetes mellitis, 39% scored positively for diabetes distress.
Data source: Consecutive patients at a university diabetes clinic.
Disclosures: The investigators have no disclosures.
AHA: Bariatric surgery slashes heart failure exacerbations
ORLANDO – Bariatric surgery in obese patients with heart failure was associated with a marked decrease in the subsequent rate of ED visits and hospitalizations for heart failure in a large, real-world, case-control study presented at the American Heart Association scientific sessions.
“This decline in the rate of heart failure morbidity was rapid in onset and sustained for at least 2 years after bariatric surgery,” according to Dr. Yuichi J. Shimada of Massachusetts General Hospital, Boston.
In a separate study, however, he found that bariatric surgery for obesity in patients with atrial fibrillation didn’t produce a reduction in ED visits and hospitalizations for the arrhythmia.
The heart failure study was a case-control study of 1,664 consecutive obese patients with heart failure who underwent a single bariatric surgical procedure in California, Florida, or Nebraska. Their median age was 49 years. Women accounted for 70% of the participants. Drawing upon federal Healthcare Cost and Utility Project databases on ED visits and hospital admissions in those three states, Dr. Shimada and coinvestigators compared the group’s rates of ED visits and hospitalizations for heart failure for 2 years before and 2 years after bariatric surgery. Thus, the subjects served as their own controls.
During the reference period, which lasted from months 13-24 presurgery, the group’s combined rate of ED visits and hospital admission for heart failure exacerbation was 14.4%. The rate wasn’t significantly different during the 12 months immediately prior to surgery, at 13.3%.
The rate dropped to 8.7% during the first 12 months after bariatric surgery and remained rock solid at 8.7% during months 13-24 postsurgery. In a logistic regression analysis, this translated to a 44% reduction in the risk of ED visits or hospital admission for heart failure during the first 2 years following bariatric surgery.
These findings are consistent with previous work by other investigators showing a link between obesity and heart failure exacerbations. The new data advance the field by providing the best evidence to date of the effectiveness of substantial weight loss on heart failure morbidity, Dr. Shimada observed.
Nonbariatric surgeries such as hysterectomy or cholecysectomy in the study population had no effect on the rate of heart failure exacerbations.
Dr. Shimada’s atrial fibrillation study was structured in the same way. It included 1,056 patients with atrial fibrillation who underwent bariatric surgery for obesity in the same three states. The rate of ED visits or hospitalization for heart failure was 12.1% in months 13-24 prior to bariatric surgery, 12.6% in presurgical months 1-12, 14.2% in the first 12 months post-bariatric surgery, and 13.4% during postsurgical months 13-24. These rates weren’t statistically different.
Dr. Shimada reported having no financial conflicts of interest regarding the two studies.
ORLANDO – Bariatric surgery in obese patients with heart failure was associated with a marked decrease in the subsequent rate of ED visits and hospitalizations for heart failure in a large, real-world, case-control study presented at the American Heart Association scientific sessions.
“This decline in the rate of heart failure morbidity was rapid in onset and sustained for at least 2 years after bariatric surgery,” according to Dr. Yuichi J. Shimada of Massachusetts General Hospital, Boston.
In a separate study, however, he found that bariatric surgery for obesity in patients with atrial fibrillation didn’t produce a reduction in ED visits and hospitalizations for the arrhythmia.
The heart failure study was a case-control study of 1,664 consecutive obese patients with heart failure who underwent a single bariatric surgical procedure in California, Florida, or Nebraska. Their median age was 49 years. Women accounted for 70% of the participants. Drawing upon federal Healthcare Cost and Utility Project databases on ED visits and hospital admissions in those three states, Dr. Shimada and coinvestigators compared the group’s rates of ED visits and hospitalizations for heart failure for 2 years before and 2 years after bariatric surgery. Thus, the subjects served as their own controls.
During the reference period, which lasted from months 13-24 presurgery, the group’s combined rate of ED visits and hospital admission for heart failure exacerbation was 14.4%. The rate wasn’t significantly different during the 12 months immediately prior to surgery, at 13.3%.
The rate dropped to 8.7% during the first 12 months after bariatric surgery and remained rock solid at 8.7% during months 13-24 postsurgery. In a logistic regression analysis, this translated to a 44% reduction in the risk of ED visits or hospital admission for heart failure during the first 2 years following bariatric surgery.
These findings are consistent with previous work by other investigators showing a link between obesity and heart failure exacerbations. The new data advance the field by providing the best evidence to date of the effectiveness of substantial weight loss on heart failure morbidity, Dr. Shimada observed.
Nonbariatric surgeries such as hysterectomy or cholecysectomy in the study population had no effect on the rate of heart failure exacerbations.
Dr. Shimada’s atrial fibrillation study was structured in the same way. It included 1,056 patients with atrial fibrillation who underwent bariatric surgery for obesity in the same three states. The rate of ED visits or hospitalization for heart failure was 12.1% in months 13-24 prior to bariatric surgery, 12.6% in presurgical months 1-12, 14.2% in the first 12 months post-bariatric surgery, and 13.4% during postsurgical months 13-24. These rates weren’t statistically different.
Dr. Shimada reported having no financial conflicts of interest regarding the two studies.
ORLANDO – Bariatric surgery in obese patients with heart failure was associated with a marked decrease in the subsequent rate of ED visits and hospitalizations for heart failure in a large, real-world, case-control study presented at the American Heart Association scientific sessions.
“This decline in the rate of heart failure morbidity was rapid in onset and sustained for at least 2 years after bariatric surgery,” according to Dr. Yuichi J. Shimada of Massachusetts General Hospital, Boston.
In a separate study, however, he found that bariatric surgery for obesity in patients with atrial fibrillation didn’t produce a reduction in ED visits and hospitalizations for the arrhythmia.
The heart failure study was a case-control study of 1,664 consecutive obese patients with heart failure who underwent a single bariatric surgical procedure in California, Florida, or Nebraska. Their median age was 49 years. Women accounted for 70% of the participants. Drawing upon federal Healthcare Cost and Utility Project databases on ED visits and hospital admissions in those three states, Dr. Shimada and coinvestigators compared the group’s rates of ED visits and hospitalizations for heart failure for 2 years before and 2 years after bariatric surgery. Thus, the subjects served as their own controls.
During the reference period, which lasted from months 13-24 presurgery, the group’s combined rate of ED visits and hospital admission for heart failure exacerbation was 14.4%. The rate wasn’t significantly different during the 12 months immediately prior to surgery, at 13.3%.
The rate dropped to 8.7% during the first 12 months after bariatric surgery and remained rock solid at 8.7% during months 13-24 postsurgery. In a logistic regression analysis, this translated to a 44% reduction in the risk of ED visits or hospital admission for heart failure during the first 2 years following bariatric surgery.
These findings are consistent with previous work by other investigators showing a link between obesity and heart failure exacerbations. The new data advance the field by providing the best evidence to date of the effectiveness of substantial weight loss on heart failure morbidity, Dr. Shimada observed.
Nonbariatric surgeries such as hysterectomy or cholecysectomy in the study population had no effect on the rate of heart failure exacerbations.
Dr. Shimada’s atrial fibrillation study was structured in the same way. It included 1,056 patients with atrial fibrillation who underwent bariatric surgery for obesity in the same three states. The rate of ED visits or hospitalization for heart failure was 12.1% in months 13-24 prior to bariatric surgery, 12.6% in presurgical months 1-12, 14.2% in the first 12 months post-bariatric surgery, and 13.4% during postsurgical months 13-24. These rates weren’t statistically different.
Dr. Shimada reported having no financial conflicts of interest regarding the two studies.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Bariatric surgery in obese patients with heart failure results in a dramatic reduction in ED visits and hospital admission for heart failure.
Major finding: The combined rate of ED visits and hospital admissions for heart failure dropped by 44% during the 2 years after a large group of patients with heart failure underwent bariatric surgery for obesity.
Data source: This case-control study compared the rates of ED visits and hospital admissions for worsening heart failure in 1,664 patients with heart failure during the 2 years before and 2 years after they underwent bariatric surgery for obesity.
Disclosures: The presenter reported having no financial conflicts of interest regarding the study, which utilized publicly available patient data.
Wound-healing template approved for diabetic foot ulcers
A bilayer matrix used for dermal regeneration and first approved in 1996 as a treatment for third-degree burns is now approved as a treatment for diabetic foot ulcers.
The Integra Dermal Regeneration Template was approved for the new indication based on a study that showed that the matrix device “improved ulcer healing compared to standard diabetic foot ulcer care,” according to a Food and Drug Administration statement announcing the approval on Jan. 7. Specifically, the new indication is for treating “partial and full-thickness neuropathic diabetic foot ulcers that are greater than 6 weeks in duration, with no capsule, tendon or bone exposed, when used in conjunction with standard diabetic ulcer care.”
The product is a dermal-replacement layer that “consists of a porous, three-dimensional matrix, comprised of bovine collagen and chondroitin-6-sulfate,” with a temporary epidermal silicone layer “to provide immediate wound coverage and control moisture loss. … [It] provides an environment for new skin and tissue to regenerate and heal the wound,” according to the agency’s approval summary.
In a multicenter, randomized controlled study, 307 patients were first treated with 0.9% sodium chloride gel, a secondary dressing, and an offloading device for 2 weeks and were then randomized to a treatment or a control group that received continued treatment with the gel. After 16 weeks, 51% of those treated with the device and 32% of those in the control group had healed completely (P = .001). Among those whose wounds healed, the median time to healing was 43 days in the treatment group and 78 days in the control group.
More patients in the control group had severe adverse events (26.8% vs. 15.6%) and moderate adverse events (42.5% vs. 31.8%).The results of the study, funded and sponsored by the manufacturer, were recently published (Wound Repair Regen. 2015;23[6]:891-900).
The product is contraindicated in patients with bovine or chondroitin allergies and in patients with infected wounds.
The manufacturer, Integra LifeSciences, is marketing the device as Integra Omnigraft Dermal Regeneration Matrix for the diabetic foot ulcer indication.
A bilayer matrix used for dermal regeneration and first approved in 1996 as a treatment for third-degree burns is now approved as a treatment for diabetic foot ulcers.
The Integra Dermal Regeneration Template was approved for the new indication based on a study that showed that the matrix device “improved ulcer healing compared to standard diabetic foot ulcer care,” according to a Food and Drug Administration statement announcing the approval on Jan. 7. Specifically, the new indication is for treating “partial and full-thickness neuropathic diabetic foot ulcers that are greater than 6 weeks in duration, with no capsule, tendon or bone exposed, when used in conjunction with standard diabetic ulcer care.”
The product is a dermal-replacement layer that “consists of a porous, three-dimensional matrix, comprised of bovine collagen and chondroitin-6-sulfate,” with a temporary epidermal silicone layer “to provide immediate wound coverage and control moisture loss. … [It] provides an environment for new skin and tissue to regenerate and heal the wound,” according to the agency’s approval summary.
In a multicenter, randomized controlled study, 307 patients were first treated with 0.9% sodium chloride gel, a secondary dressing, and an offloading device for 2 weeks and were then randomized to a treatment or a control group that received continued treatment with the gel. After 16 weeks, 51% of those treated with the device and 32% of those in the control group had healed completely (P = .001). Among those whose wounds healed, the median time to healing was 43 days in the treatment group and 78 days in the control group.
More patients in the control group had severe adverse events (26.8% vs. 15.6%) and moderate adverse events (42.5% vs. 31.8%).The results of the study, funded and sponsored by the manufacturer, were recently published (Wound Repair Regen. 2015;23[6]:891-900).
The product is contraindicated in patients with bovine or chondroitin allergies and in patients with infected wounds.
The manufacturer, Integra LifeSciences, is marketing the device as Integra Omnigraft Dermal Regeneration Matrix for the diabetic foot ulcer indication.
A bilayer matrix used for dermal regeneration and first approved in 1996 as a treatment for third-degree burns is now approved as a treatment for diabetic foot ulcers.
The Integra Dermal Regeneration Template was approved for the new indication based on a study that showed that the matrix device “improved ulcer healing compared to standard diabetic foot ulcer care,” according to a Food and Drug Administration statement announcing the approval on Jan. 7. Specifically, the new indication is for treating “partial and full-thickness neuropathic diabetic foot ulcers that are greater than 6 weeks in duration, with no capsule, tendon or bone exposed, when used in conjunction with standard diabetic ulcer care.”
The product is a dermal-replacement layer that “consists of a porous, three-dimensional matrix, comprised of bovine collagen and chondroitin-6-sulfate,” with a temporary epidermal silicone layer “to provide immediate wound coverage and control moisture loss. … [It] provides an environment for new skin and tissue to regenerate and heal the wound,” according to the agency’s approval summary.
In a multicenter, randomized controlled study, 307 patients were first treated with 0.9% sodium chloride gel, a secondary dressing, and an offloading device for 2 weeks and were then randomized to a treatment or a control group that received continued treatment with the gel. After 16 weeks, 51% of those treated with the device and 32% of those in the control group had healed completely (P = .001). Among those whose wounds healed, the median time to healing was 43 days in the treatment group and 78 days in the control group.
More patients in the control group had severe adverse events (26.8% vs. 15.6%) and moderate adverse events (42.5% vs. 31.8%).The results of the study, funded and sponsored by the manufacturer, were recently published (Wound Repair Regen. 2015;23[6]:891-900).
The product is contraindicated in patients with bovine or chondroitin allergies and in patients with infected wounds.
The manufacturer, Integra LifeSciences, is marketing the device as Integra Omnigraft Dermal Regeneration Matrix for the diabetic foot ulcer indication.
Sugary beverages tied to increased visceral fat
Daily consumption of sugar-sweetened beverages was associated with a 27% increase in visceral adipose tissue over time, according to an analysis of the Framingham Heart Study published online on Jan. 11 in Circulation.
“There is evidence linking sugar-sweetened beverages with cardiovascular disease and type 2 diabetes. Our message to consumers is to follow the current dietary guidelines and to be mindful of how much sugar-sweetened beverages they drink. To policy makers, this study adds another piece of evidence to the growing body of research suggesting sugar-sweetened beverages may be harmful to our health,” Dr. Caroline Fox of the National Heart, Lung, and Blood Institute’s Framingham Heart Study and Population Sciences Branch said in a press release.
These results coincide with the recent release of the updated dietary guidelines by the U.S. Department of Health and Human Services which note to limit added sugars to less than 10% of daily caloric intake.
Furthermore, sugar-sweetened beverages are a major contributor of additional sugar in the American diet. According to the study, cardiometabolic risk can potentially be associated with an increase in abdominal adipose tissue. Likewise, type 2 diabetes and cardiovascular disease have been linked to larger amounts of visceral adipose tissue (VAT).
Dr. Fox and her colleagues conducted a prospective study of participants in the third generation cohort of the Framingham Heart Study to explore the relationship between sugar-sweetened beverage intake vs. diet soda and differences over time in VAT and subcutaneous adipose tissue (SAT) on CT scans. Measurements of the quantity and quality of abdominal adipose tissue were obtained from two CT scans taken roughly 6 years apart. Participants were assessed for frequency of sugar-sweetened beverage vs. diet soda intake, and body measurements were obtained.
The mean age of the 1,003 participants was 45.3 years, and women made up 45%. Of them, 85% (852) reported drinking a combination of diet soda and sugar-sweetened beverages and 14% (138) reported not drinking either. Sugar-sweetened beverage intake was reported as daily, frequent, occasional, or not at all, in 13%, 35%, 20%, and 32% of the participants, respectively. Those consuming sugar-sweetened beverages were less likely to have diabetes but more likely to be young, male, report more physical activity, and smoke.
Interestingly, those reporting diet soda intake had a higher prevalence of diabetes, had an increased body mass index, and reported less activity (Circulation. 2016 Jan 11).
Over the 6 years, they found more sugar-sweetened beverage consumption was associated with greater change in VAT volume, which was significant after accounting for the change in body weight (P less than .001). As the consumption of sugar-sweetened beverages increased from no consumption to daily consumption, the VAT volume increased by 658 cm3, 649 cm3, 707 cm3, and 852 cm3, respectively.
Finally, they found no association with diet soda intake and change in weight or change in VAT volume.
“In this prospective observational study of middle-aged adults, we observed that individuals who consumed at least one serving of sugar-sweetened beverages per day ... had a 27% greater increase in VAT volume over 6 years compared to non-consumers,” the investigators wrote.
The authors reported having no disclosures. The study was funded by the National Heart, Lung, and Blood Institute.
Daily consumption of sugar-sweetened beverages was associated with a 27% increase in visceral adipose tissue over time, according to an analysis of the Framingham Heart Study published online on Jan. 11 in Circulation.
“There is evidence linking sugar-sweetened beverages with cardiovascular disease and type 2 diabetes. Our message to consumers is to follow the current dietary guidelines and to be mindful of how much sugar-sweetened beverages they drink. To policy makers, this study adds another piece of evidence to the growing body of research suggesting sugar-sweetened beverages may be harmful to our health,” Dr. Caroline Fox of the National Heart, Lung, and Blood Institute’s Framingham Heart Study and Population Sciences Branch said in a press release.
These results coincide with the recent release of the updated dietary guidelines by the U.S. Department of Health and Human Services which note to limit added sugars to less than 10% of daily caloric intake.
Furthermore, sugar-sweetened beverages are a major contributor of additional sugar in the American diet. According to the study, cardiometabolic risk can potentially be associated with an increase in abdominal adipose tissue. Likewise, type 2 diabetes and cardiovascular disease have been linked to larger amounts of visceral adipose tissue (VAT).
Dr. Fox and her colleagues conducted a prospective study of participants in the third generation cohort of the Framingham Heart Study to explore the relationship between sugar-sweetened beverage intake vs. diet soda and differences over time in VAT and subcutaneous adipose tissue (SAT) on CT scans. Measurements of the quantity and quality of abdominal adipose tissue were obtained from two CT scans taken roughly 6 years apart. Participants were assessed for frequency of sugar-sweetened beverage vs. diet soda intake, and body measurements were obtained.
The mean age of the 1,003 participants was 45.3 years, and women made up 45%. Of them, 85% (852) reported drinking a combination of diet soda and sugar-sweetened beverages and 14% (138) reported not drinking either. Sugar-sweetened beverage intake was reported as daily, frequent, occasional, or not at all, in 13%, 35%, 20%, and 32% of the participants, respectively. Those consuming sugar-sweetened beverages were less likely to have diabetes but more likely to be young, male, report more physical activity, and smoke.
Interestingly, those reporting diet soda intake had a higher prevalence of diabetes, had an increased body mass index, and reported less activity (Circulation. 2016 Jan 11).
Over the 6 years, they found more sugar-sweetened beverage consumption was associated with greater change in VAT volume, which was significant after accounting for the change in body weight (P less than .001). As the consumption of sugar-sweetened beverages increased from no consumption to daily consumption, the VAT volume increased by 658 cm3, 649 cm3, 707 cm3, and 852 cm3, respectively.
Finally, they found no association with diet soda intake and change in weight or change in VAT volume.
“In this prospective observational study of middle-aged adults, we observed that individuals who consumed at least one serving of sugar-sweetened beverages per day ... had a 27% greater increase in VAT volume over 6 years compared to non-consumers,” the investigators wrote.
The authors reported having no disclosures. The study was funded by the National Heart, Lung, and Blood Institute.
Daily consumption of sugar-sweetened beverages was associated with a 27% increase in visceral adipose tissue over time, according to an analysis of the Framingham Heart Study published online on Jan. 11 in Circulation.
“There is evidence linking sugar-sweetened beverages with cardiovascular disease and type 2 diabetes. Our message to consumers is to follow the current dietary guidelines and to be mindful of how much sugar-sweetened beverages they drink. To policy makers, this study adds another piece of evidence to the growing body of research suggesting sugar-sweetened beverages may be harmful to our health,” Dr. Caroline Fox of the National Heart, Lung, and Blood Institute’s Framingham Heart Study and Population Sciences Branch said in a press release.
These results coincide with the recent release of the updated dietary guidelines by the U.S. Department of Health and Human Services which note to limit added sugars to less than 10% of daily caloric intake.
Furthermore, sugar-sweetened beverages are a major contributor of additional sugar in the American diet. According to the study, cardiometabolic risk can potentially be associated with an increase in abdominal adipose tissue. Likewise, type 2 diabetes and cardiovascular disease have been linked to larger amounts of visceral adipose tissue (VAT).
Dr. Fox and her colleagues conducted a prospective study of participants in the third generation cohort of the Framingham Heart Study to explore the relationship between sugar-sweetened beverage intake vs. diet soda and differences over time in VAT and subcutaneous adipose tissue (SAT) on CT scans. Measurements of the quantity and quality of abdominal adipose tissue were obtained from two CT scans taken roughly 6 years apart. Participants were assessed for frequency of sugar-sweetened beverage vs. diet soda intake, and body measurements were obtained.
The mean age of the 1,003 participants was 45.3 years, and women made up 45%. Of them, 85% (852) reported drinking a combination of diet soda and sugar-sweetened beverages and 14% (138) reported not drinking either. Sugar-sweetened beverage intake was reported as daily, frequent, occasional, or not at all, in 13%, 35%, 20%, and 32% of the participants, respectively. Those consuming sugar-sweetened beverages were less likely to have diabetes but more likely to be young, male, report more physical activity, and smoke.
Interestingly, those reporting diet soda intake had a higher prevalence of diabetes, had an increased body mass index, and reported less activity (Circulation. 2016 Jan 11).
Over the 6 years, they found more sugar-sweetened beverage consumption was associated with greater change in VAT volume, which was significant after accounting for the change in body weight (P less than .001). As the consumption of sugar-sweetened beverages increased from no consumption to daily consumption, the VAT volume increased by 658 cm3, 649 cm3, 707 cm3, and 852 cm3, respectively.
Finally, they found no association with diet soda intake and change in weight or change in VAT volume.
“In this prospective observational study of middle-aged adults, we observed that individuals who consumed at least one serving of sugar-sweetened beverages per day ... had a 27% greater increase in VAT volume over 6 years compared to non-consumers,” the investigators wrote.
The authors reported having no disclosures. The study was funded by the National Heart, Lung, and Blood Institute.
FROM CIRCULATION
Key clinical point: Daily consumption of sugar-sweetened beverages was associated with a 27% increase in visceral adipose tissue.
Major finding: More sugar-sweetened beverage consumption was associated with greater change in VAT volume which was significant after accounting for the change in body weight (P less than .001).
Data source: A prospective study of participants in the third-generation cohort of the Framingham Heart Study.
Disclosures: The authors report having no disclosures. The study was funded by the National Heart, Lung, and Blood Institute.
How new dietary guidelines affect health care providers
The U.S. Department of Health and Human Services and the U.S. Department of Agriculture have released the eighth iteration of the Dietary Guidelines for Americans, a set of recommendations for healthy eating habits Americans should adopt to prevent development of hypertension, heart disease, and type 2 diabetes, among other conditions.
The new guidelines, effective through 2020, highlight the importance of eating a wide variety of fruits, vegetables, grains, and dairy products, while staying away from processed foods heavy in saturated fats, sugar, and cholesterol as much as possible. The difference between this and earlier editions of the guidelines, the health agencies say, is to promote the importance of a wider variety of foods Americans should be consuming, rather than focusing on just a few isolated foods that should be integrated into an otherwise inadequate diet.
“Protecting the health of the American public includes empowering them with the tools they need to make healthy choices in their daily lives,” Secretary of Health and Human Services Sylvia M. Burwell said in a statement. “By focusing on small shifts in what we eat and drink, eating healthy becomes more manageable. The Dietary Guidelines provide science-based recommendations on food and nutrition so people can make decisions that may help keep their weight under control, and prevent chronic conditions, like Type 2 diabetes, hypertension, and heart disease.”
The American Medical Association voiced their support of the new guidelines, saying that they are “extremely pleased that the new recommendations call for significantly reducing the amount of added sugars and sugar sweetened beverages from the American diet.” Similarly, the American College of Cardiology issued a statement saying that the existence of “a source of clear science-based information about diet” is more important than ever for Americans in the face of increasingly omnipresent and often confusing information available; the college also lauded the recommendations to limit the intake of added sugars, saturated and trans fats, and sodium. The American Heart Association released a new Authoritative Review of data on the topic of nutritional balance as it related to chronic diseases.
While the recommendations may seem common sense and geared more towards patients and laymen, they are of equal importance to health care providers. Dr. Carolyn Lopez – a Chicago-area family physician and adjunct professor of medicine at Northwestern University – called the guidelines an important resource for physicians, with several elements that will be of particular benefit to physicians and clinicians looking to improve the quality of care given to their patients.
“People [should] understand that while individual food choices are important, the pattern of eating is paramount,” Dr. Lopez explained in an interview. “It’s not impossible to bring vegetables into breakfast – veggie omelettes are great – but it’s hard to imagine bringing a vegetable into the whole grain cereals with skim milk breakfast.”
As a family practitioner, however, Dr. Lopez stressed the difficulty of any doctor having a significant enough amount of time with each patient to really go in-depth into what needs to be done to enact meaningful nutritional and lifestyle changes. “These guidelines can only be effective if the whole team is talking to patients,” she explained. “On its own, it would be extraordinarily difficult [or] impossible to accomplish.
Dr. Nazrat Mirza, a pediatrician who is medical director of the IDEAL Pediatric Weight Management Clinic at Children’s National Health System, Washington, said in an interview that the guidelines are “significant in that they are leading us even closer to healthier dietary living – and from my pediatric perspective, healthier children who will grow into healthier adults. We must keep in mind that these guidelines are not prescriptive – but generalized to relatively healthy people. In particular, the recommendation to reduce sugar intake with specification of an upper limit of 10% of calories from added sugar factored into the suggested daily nutritional intake is an excellent update. Added sugar consumption is linked to diabetes, so any reduction in recommended intake will steer people away from potentially developing diabetes.”
She continued, “In my clinic and day-to-day counseling of patients, being able to point to helpful resources such as these guidelines is crucial. These guidelines will continue to serve as yet another way to reach parents and affect the daily dietary habits they practice at home. I was happy to see resources such as MyPlate.gov referenced in the guidelines; that is a tool I use regularly. When educating families on what a healthy plate looks like, I’m able to point directly to the MyPlate.gov posters hanging in the clinic. Comprehensive resources such as these guidelines, [which] give parents actual examples of foods, and deliver the information in a clear, concise, implementable way, are the best methods to reach parents and kids.”
“As a medical provider, such guidelines provide us with tools and reinforcement to say ‘this is policy,’ when approaching schools about the food and drink options they offer children on a daily basis – because the schools are going to have to follow these guidelines. If these guidelines can enforce public policy for the kids to eat healthy, ... and we can implement changes according to the guidelines, that would help greatly in the prevention of chronic disorders such as obesity, hypertension and diabetes – which is a step in the right direction,” said Dr. Mirza, also of George Washington University, Washington.
“Most physicians are so rushed nowadays by the health care system that they typically do not have adequate time to discuss these very important issues,” Dr. Rodbard said in an interview. “It takes time and perseverance to educate the patient and provide individualized care, assessing their current diet, assessing their willingness or potential for changing their diet or increasing their physical activity.”
On that last point. Dr. Rodbard criticized the new guidelines for not emphasizing the importance of exercise enough. “More clarity and emphasis on physical activity should have been provided,” she said, adding that “people need continual, gentle reminders with repetition and long-term follow-up.” Dr. Rodbard summed up the guidelines as “marginally adequate” but “a step in the right direction.”
An endocrinologist who practices in Winter Park, Fla., Dr. Victor L. Roberts – a Fellow of the ACP and ACE – agreed that time with the patients is critical in order for these guidelines to have any effect, calling the guidelines “just the GPS, not the destination.”
Preaching an ABC strategy – accountability, behavior, and calories, the latter of which he stressed is the most important part of any dietary strategy – Dr. Roberts explained that clinicians and physicians should leave the more specific dietary advice to nutritional experts and focus on telling their patients to watch calories, watch the amount of food they’re eating of any given type, and to exercise more.
“These guidelines crystallize and summarize what we’ve already known, and what we should have been practicing and advocating, for decades,” Dr. Roberts said in an interview, adding that “the difficulty is putting these recommendations into practice and having patients and doctors accept responsibility.”
Ultimately, the three doctors who treat adult patients concurred that the new guidelines are imperfect, and likely won’t result in any automatic widespread change. Dr. Rodbard admitted that she does not anticipate the guidelines affecting the way she treats her patients very much, if at all, while Dr. Lopez said that she’s “not sure it’s going to have a major effect.” Furthermore, the sheer volume of data and information available often leads to patients simply not knowing what to believe, which Dr. Roberts described as a “glazed over” effect of being told so many different things from so many different sources, patients just tune everything out.
Ultimately, while it’s important for health care providers to give advice and recommendations as necessary, these should be done on an individual basis. And, if a patient requires extensive dietary and nutritional intervention, that should be left in the hands of specialist who can accurately determine what the patient is capable of, what their goals should be, and how to tailor a plan specifically for them.
“I don’t know many clinicians, even in my own specialty, who know much about what specifically to eat,” said Dr. Roberts. “That should come from nutritional medicine people, not us.”
Dr. Lopez, Dr. Rodbard, and Dr. Roberts did not report any relevant financial disclosures.
*This article was updated 1/12/2016.
The U.S. Department of Health and Human Services and the U.S. Department of Agriculture have released the eighth iteration of the Dietary Guidelines for Americans, a set of recommendations for healthy eating habits Americans should adopt to prevent development of hypertension, heart disease, and type 2 diabetes, among other conditions.
The new guidelines, effective through 2020, highlight the importance of eating a wide variety of fruits, vegetables, grains, and dairy products, while staying away from processed foods heavy in saturated fats, sugar, and cholesterol as much as possible. The difference between this and earlier editions of the guidelines, the health agencies say, is to promote the importance of a wider variety of foods Americans should be consuming, rather than focusing on just a few isolated foods that should be integrated into an otherwise inadequate diet.
“Protecting the health of the American public includes empowering them with the tools they need to make healthy choices in their daily lives,” Secretary of Health and Human Services Sylvia M. Burwell said in a statement. “By focusing on small shifts in what we eat and drink, eating healthy becomes more manageable. The Dietary Guidelines provide science-based recommendations on food and nutrition so people can make decisions that may help keep their weight under control, and prevent chronic conditions, like Type 2 diabetes, hypertension, and heart disease.”
The American Medical Association voiced their support of the new guidelines, saying that they are “extremely pleased that the new recommendations call for significantly reducing the amount of added sugars and sugar sweetened beverages from the American diet.” Similarly, the American College of Cardiology issued a statement saying that the existence of “a source of clear science-based information about diet” is more important than ever for Americans in the face of increasingly omnipresent and often confusing information available; the college also lauded the recommendations to limit the intake of added sugars, saturated and trans fats, and sodium. The American Heart Association released a new Authoritative Review of data on the topic of nutritional balance as it related to chronic diseases.
While the recommendations may seem common sense and geared more towards patients and laymen, they are of equal importance to health care providers. Dr. Carolyn Lopez – a Chicago-area family physician and adjunct professor of medicine at Northwestern University – called the guidelines an important resource for physicians, with several elements that will be of particular benefit to physicians and clinicians looking to improve the quality of care given to their patients.
“People [should] understand that while individual food choices are important, the pattern of eating is paramount,” Dr. Lopez explained in an interview. “It’s not impossible to bring vegetables into breakfast – veggie omelettes are great – but it’s hard to imagine bringing a vegetable into the whole grain cereals with skim milk breakfast.”
As a family practitioner, however, Dr. Lopez stressed the difficulty of any doctor having a significant enough amount of time with each patient to really go in-depth into what needs to be done to enact meaningful nutritional and lifestyle changes. “These guidelines can only be effective if the whole team is talking to patients,” she explained. “On its own, it would be extraordinarily difficult [or] impossible to accomplish.
Dr. Nazrat Mirza, a pediatrician who is medical director of the IDEAL Pediatric Weight Management Clinic at Children’s National Health System, Washington, said in an interview that the guidelines are “significant in that they are leading us even closer to healthier dietary living – and from my pediatric perspective, healthier children who will grow into healthier adults. We must keep in mind that these guidelines are not prescriptive – but generalized to relatively healthy people. In particular, the recommendation to reduce sugar intake with specification of an upper limit of 10% of calories from added sugar factored into the suggested daily nutritional intake is an excellent update. Added sugar consumption is linked to diabetes, so any reduction in recommended intake will steer people away from potentially developing diabetes.”
She continued, “In my clinic and day-to-day counseling of patients, being able to point to helpful resources such as these guidelines is crucial. These guidelines will continue to serve as yet another way to reach parents and affect the daily dietary habits they practice at home. I was happy to see resources such as MyPlate.gov referenced in the guidelines; that is a tool I use regularly. When educating families on what a healthy plate looks like, I’m able to point directly to the MyPlate.gov posters hanging in the clinic. Comprehensive resources such as these guidelines, [which] give parents actual examples of foods, and deliver the information in a clear, concise, implementable way, are the best methods to reach parents and kids.”
“As a medical provider, such guidelines provide us with tools and reinforcement to say ‘this is policy,’ when approaching schools about the food and drink options they offer children on a daily basis – because the schools are going to have to follow these guidelines. If these guidelines can enforce public policy for the kids to eat healthy, ... and we can implement changes according to the guidelines, that would help greatly in the prevention of chronic disorders such as obesity, hypertension and diabetes – which is a step in the right direction,” said Dr. Mirza, also of George Washington University, Washington.
“Most physicians are so rushed nowadays by the health care system that they typically do not have adequate time to discuss these very important issues,” Dr. Rodbard said in an interview. “It takes time and perseverance to educate the patient and provide individualized care, assessing their current diet, assessing their willingness or potential for changing their diet or increasing their physical activity.”
On that last point. Dr. Rodbard criticized the new guidelines for not emphasizing the importance of exercise enough. “More clarity and emphasis on physical activity should have been provided,” she said, adding that “people need continual, gentle reminders with repetition and long-term follow-up.” Dr. Rodbard summed up the guidelines as “marginally adequate” but “a step in the right direction.”
An endocrinologist who practices in Winter Park, Fla., Dr. Victor L. Roberts – a Fellow of the ACP and ACE – agreed that time with the patients is critical in order for these guidelines to have any effect, calling the guidelines “just the GPS, not the destination.”
Preaching an ABC strategy – accountability, behavior, and calories, the latter of which he stressed is the most important part of any dietary strategy – Dr. Roberts explained that clinicians and physicians should leave the more specific dietary advice to nutritional experts and focus on telling their patients to watch calories, watch the amount of food they’re eating of any given type, and to exercise more.
“These guidelines crystallize and summarize what we’ve already known, and what we should have been practicing and advocating, for decades,” Dr. Roberts said in an interview, adding that “the difficulty is putting these recommendations into practice and having patients and doctors accept responsibility.”
Ultimately, the three doctors who treat adult patients concurred that the new guidelines are imperfect, and likely won’t result in any automatic widespread change. Dr. Rodbard admitted that she does not anticipate the guidelines affecting the way she treats her patients very much, if at all, while Dr. Lopez said that she’s “not sure it’s going to have a major effect.” Furthermore, the sheer volume of data and information available often leads to patients simply not knowing what to believe, which Dr. Roberts described as a “glazed over” effect of being told so many different things from so many different sources, patients just tune everything out.
Ultimately, while it’s important for health care providers to give advice and recommendations as necessary, these should be done on an individual basis. And, if a patient requires extensive dietary and nutritional intervention, that should be left in the hands of specialist who can accurately determine what the patient is capable of, what their goals should be, and how to tailor a plan specifically for them.
“I don’t know many clinicians, even in my own specialty, who know much about what specifically to eat,” said Dr. Roberts. “That should come from nutritional medicine people, not us.”
Dr. Lopez, Dr. Rodbard, and Dr. Roberts did not report any relevant financial disclosures.
*This article was updated 1/12/2016.
The U.S. Department of Health and Human Services and the U.S. Department of Agriculture have released the eighth iteration of the Dietary Guidelines for Americans, a set of recommendations for healthy eating habits Americans should adopt to prevent development of hypertension, heart disease, and type 2 diabetes, among other conditions.
The new guidelines, effective through 2020, highlight the importance of eating a wide variety of fruits, vegetables, grains, and dairy products, while staying away from processed foods heavy in saturated fats, sugar, and cholesterol as much as possible. The difference between this and earlier editions of the guidelines, the health agencies say, is to promote the importance of a wider variety of foods Americans should be consuming, rather than focusing on just a few isolated foods that should be integrated into an otherwise inadequate diet.
“Protecting the health of the American public includes empowering them with the tools they need to make healthy choices in their daily lives,” Secretary of Health and Human Services Sylvia M. Burwell said in a statement. “By focusing on small shifts in what we eat and drink, eating healthy becomes more manageable. The Dietary Guidelines provide science-based recommendations on food and nutrition so people can make decisions that may help keep their weight under control, and prevent chronic conditions, like Type 2 diabetes, hypertension, and heart disease.”
The American Medical Association voiced their support of the new guidelines, saying that they are “extremely pleased that the new recommendations call for significantly reducing the amount of added sugars and sugar sweetened beverages from the American diet.” Similarly, the American College of Cardiology issued a statement saying that the existence of “a source of clear science-based information about diet” is more important than ever for Americans in the face of increasingly omnipresent and often confusing information available; the college also lauded the recommendations to limit the intake of added sugars, saturated and trans fats, and sodium. The American Heart Association released a new Authoritative Review of data on the topic of nutritional balance as it related to chronic diseases.
While the recommendations may seem common sense and geared more towards patients and laymen, they are of equal importance to health care providers. Dr. Carolyn Lopez – a Chicago-area family physician and adjunct professor of medicine at Northwestern University – called the guidelines an important resource for physicians, with several elements that will be of particular benefit to physicians and clinicians looking to improve the quality of care given to their patients.
“People [should] understand that while individual food choices are important, the pattern of eating is paramount,” Dr. Lopez explained in an interview. “It’s not impossible to bring vegetables into breakfast – veggie omelettes are great – but it’s hard to imagine bringing a vegetable into the whole grain cereals with skim milk breakfast.”
As a family practitioner, however, Dr. Lopez stressed the difficulty of any doctor having a significant enough amount of time with each patient to really go in-depth into what needs to be done to enact meaningful nutritional and lifestyle changes. “These guidelines can only be effective if the whole team is talking to patients,” she explained. “On its own, it would be extraordinarily difficult [or] impossible to accomplish.
Dr. Nazrat Mirza, a pediatrician who is medical director of the IDEAL Pediatric Weight Management Clinic at Children’s National Health System, Washington, said in an interview that the guidelines are “significant in that they are leading us even closer to healthier dietary living – and from my pediatric perspective, healthier children who will grow into healthier adults. We must keep in mind that these guidelines are not prescriptive – but generalized to relatively healthy people. In particular, the recommendation to reduce sugar intake with specification of an upper limit of 10% of calories from added sugar factored into the suggested daily nutritional intake is an excellent update. Added sugar consumption is linked to diabetes, so any reduction in recommended intake will steer people away from potentially developing diabetes.”
She continued, “In my clinic and day-to-day counseling of patients, being able to point to helpful resources such as these guidelines is crucial. These guidelines will continue to serve as yet another way to reach parents and affect the daily dietary habits they practice at home. I was happy to see resources such as MyPlate.gov referenced in the guidelines; that is a tool I use regularly. When educating families on what a healthy plate looks like, I’m able to point directly to the MyPlate.gov posters hanging in the clinic. Comprehensive resources such as these guidelines, [which] give parents actual examples of foods, and deliver the information in a clear, concise, implementable way, are the best methods to reach parents and kids.”
“As a medical provider, such guidelines provide us with tools and reinforcement to say ‘this is policy,’ when approaching schools about the food and drink options they offer children on a daily basis – because the schools are going to have to follow these guidelines. If these guidelines can enforce public policy for the kids to eat healthy, ... and we can implement changes according to the guidelines, that would help greatly in the prevention of chronic disorders such as obesity, hypertension and diabetes – which is a step in the right direction,” said Dr. Mirza, also of George Washington University, Washington.
“Most physicians are so rushed nowadays by the health care system that they typically do not have adequate time to discuss these very important issues,” Dr. Rodbard said in an interview. “It takes time and perseverance to educate the patient and provide individualized care, assessing their current diet, assessing their willingness or potential for changing their diet or increasing their physical activity.”
On that last point. Dr. Rodbard criticized the new guidelines for not emphasizing the importance of exercise enough. “More clarity and emphasis on physical activity should have been provided,” she said, adding that “people need continual, gentle reminders with repetition and long-term follow-up.” Dr. Rodbard summed up the guidelines as “marginally adequate” but “a step in the right direction.”
An endocrinologist who practices in Winter Park, Fla., Dr. Victor L. Roberts – a Fellow of the ACP and ACE – agreed that time with the patients is critical in order for these guidelines to have any effect, calling the guidelines “just the GPS, not the destination.”
Preaching an ABC strategy – accountability, behavior, and calories, the latter of which he stressed is the most important part of any dietary strategy – Dr. Roberts explained that clinicians and physicians should leave the more specific dietary advice to nutritional experts and focus on telling their patients to watch calories, watch the amount of food they’re eating of any given type, and to exercise more.
“These guidelines crystallize and summarize what we’ve already known, and what we should have been practicing and advocating, for decades,” Dr. Roberts said in an interview, adding that “the difficulty is putting these recommendations into practice and having patients and doctors accept responsibility.”
Ultimately, the three doctors who treat adult patients concurred that the new guidelines are imperfect, and likely won’t result in any automatic widespread change. Dr. Rodbard admitted that she does not anticipate the guidelines affecting the way she treats her patients very much, if at all, while Dr. Lopez said that she’s “not sure it’s going to have a major effect.” Furthermore, the sheer volume of data and information available often leads to patients simply not knowing what to believe, which Dr. Roberts described as a “glazed over” effect of being told so many different things from so many different sources, patients just tune everything out.
Ultimately, while it’s important for health care providers to give advice and recommendations as necessary, these should be done on an individual basis. And, if a patient requires extensive dietary and nutritional intervention, that should be left in the hands of specialist who can accurately determine what the patient is capable of, what their goals should be, and how to tailor a plan specifically for them.
“I don’t know many clinicians, even in my own specialty, who know much about what specifically to eat,” said Dr. Roberts. “That should come from nutritional medicine people, not us.”
Dr. Lopez, Dr. Rodbard, and Dr. Roberts did not report any relevant financial disclosures.
*This article was updated 1/12/2016.
FROM THE USDA AND HHS
Moderate, intensive exercise cut triglycerides equally in NAFLD
ORLANDO – Moderate aerobic exercise and a more intensive regimen proved equally effective in reducing intrahepatic triglyceride content in centrally obese patients with nonalcoholic fatty liver disease in a 12-month randomized, controlled trial.
However, the more intensive exercise program had the edge in terms of favorable impact on metabolic risk factors. While both exercise prescriptions reduced body weight and blood pressure to a similar extent over the course of 12 months, the intensive-exercise group showed bigger reductions in body fat mass, visceral fat, and subcutaneous fat (see graphic), Dr. Hui-Jie Zhang of Xiamen (China) University said at the American Heart Association scientific sessions.
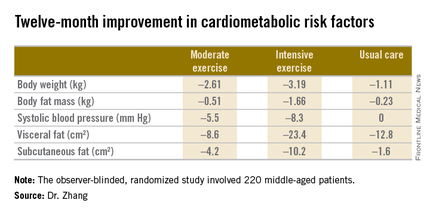
The observer-blinded study included 220 middle-age Chinese patients with central obesity and confirmed nonalcoholic fatty liver disease (NAFLD), a common risk factor for cardiovascular disease. They were randomized to three groups: a moderate exercise program that consisted of brisk walking for 150 minutes per week for 12 months; an intensive exercise regimen involving 30 minutes of treadmill running at 65%-80% of maximum oxygen consumption 5 days per week for 6 months, followed by 6 months of brisk walking on the same schedule as the moderate exercise group; or a usual-care control group that received lifestyle counseling.
The primary endpoint was change in intrahepatic triglyceride content as measured by proton magnetic resonance spectroscopy at 12 months. It was reduced from baseline by 6.45% in the intensive exercise group and similarly by 6.19% with moderate exercise, both significantly greater effects than the 2.85% decrease in the control group.
Dr. Zhang reported having no financial conflicts of interest regarding this study.
ORLANDO – Moderate aerobic exercise and a more intensive regimen proved equally effective in reducing intrahepatic triglyceride content in centrally obese patients with nonalcoholic fatty liver disease in a 12-month randomized, controlled trial.
However, the more intensive exercise program had the edge in terms of favorable impact on metabolic risk factors. While both exercise prescriptions reduced body weight and blood pressure to a similar extent over the course of 12 months, the intensive-exercise group showed bigger reductions in body fat mass, visceral fat, and subcutaneous fat (see graphic), Dr. Hui-Jie Zhang of Xiamen (China) University said at the American Heart Association scientific sessions.
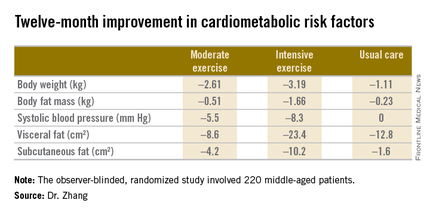
The observer-blinded study included 220 middle-age Chinese patients with central obesity and confirmed nonalcoholic fatty liver disease (NAFLD), a common risk factor for cardiovascular disease. They were randomized to three groups: a moderate exercise program that consisted of brisk walking for 150 minutes per week for 12 months; an intensive exercise regimen involving 30 minutes of treadmill running at 65%-80% of maximum oxygen consumption 5 days per week for 6 months, followed by 6 months of brisk walking on the same schedule as the moderate exercise group; or a usual-care control group that received lifestyle counseling.
The primary endpoint was change in intrahepatic triglyceride content as measured by proton magnetic resonance spectroscopy at 12 months. It was reduced from baseline by 6.45% in the intensive exercise group and similarly by 6.19% with moderate exercise, both significantly greater effects than the 2.85% decrease in the control group.
Dr. Zhang reported having no financial conflicts of interest regarding this study.
ORLANDO – Moderate aerobic exercise and a more intensive regimen proved equally effective in reducing intrahepatic triglyceride content in centrally obese patients with nonalcoholic fatty liver disease in a 12-month randomized, controlled trial.
However, the more intensive exercise program had the edge in terms of favorable impact on metabolic risk factors. While both exercise prescriptions reduced body weight and blood pressure to a similar extent over the course of 12 months, the intensive-exercise group showed bigger reductions in body fat mass, visceral fat, and subcutaneous fat (see graphic), Dr. Hui-Jie Zhang of Xiamen (China) University said at the American Heart Association scientific sessions.
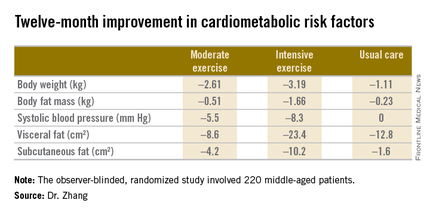
The observer-blinded study included 220 middle-age Chinese patients with central obesity and confirmed nonalcoholic fatty liver disease (NAFLD), a common risk factor for cardiovascular disease. They were randomized to three groups: a moderate exercise program that consisted of brisk walking for 150 minutes per week for 12 months; an intensive exercise regimen involving 30 minutes of treadmill running at 65%-80% of maximum oxygen consumption 5 days per week for 6 months, followed by 6 months of brisk walking on the same schedule as the moderate exercise group; or a usual-care control group that received lifestyle counseling.
The primary endpoint was change in intrahepatic triglyceride content as measured by proton magnetic resonance spectroscopy at 12 months. It was reduced from baseline by 6.45% in the intensive exercise group and similarly by 6.19% with moderate exercise, both significantly greater effects than the 2.85% decrease in the control group.
Dr. Zhang reported having no financial conflicts of interest regarding this study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Moderate and intensive aerobic exercise, done regularly, are equally effective in reducing the intrahepatic triglyceride level in patients with nonalcoholic fatty liver disease.
Major finding: Intrahepatic triglyceride concentration in patients with NAFLD was reduced by a mean of 6.19% after 12 months on a moderate exercise program and 6.45% with a more intensive exercise regimen, compared with 2.85% in usual-care controls.
Data source: A 12-month, observer-blinded randomized trial in which 220 middle-age Chinese patients with NAFLD and central obesity were randomized to a program of moderate aerobic exercise, a more intensive regimen, or a usual-care control group.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study.
Does poverty predetermine pediatric obesity?
WASHINGTON – Childhood obesity is soaring in the United States, especially among Hispanic and African-American children. At the heart of this “epidemic” are dietary and behavioral factors that are linked to stress and poverty rather than race and ethnicity, and the risks may even begin prenatally, according to experts attending an Institute of Medicine forum on early childhood obesity.
Based on data from the 2009-2010 NHANES (National Health and Nutrition Examination Survey), over 8% of children aged 2-5 years in the United States are obese; based on ethnicity, 18% of Hispanic boys and 15% of Hispanic girls in this age group are obese. Nearly 18% of U.S. children aged 6-11 years are obese; nearly 29% of Hispanic boys and 26% of non-Hispanic black girls in this age group are obese.
“If we’re looking for reasons why black and Hispanic children have these disparities ... then we’re looking at what happens in their early years and during pregnancy,” Dr. Elsie Taveras, chief of general academic pediatrics at Massachusetts General Hospital, Boston, said at the IOM meeting.
Chief among the culprits responsible for the “metabolic programming of risk” is the mother’s pregestational weight, according to Dr. Lisa Bodnar, associate professor of endocrinology at the University of Pittsburgh. “Children may already be programmed to become obese as a result of their intrauterine exposure to an obesogenic environment.”
A 2013 report from the Centers for Disease Control and Prevention found that about 1 in 5 women aged 20 years and older who delivered a live-born infant in 2009 were obese prior to becoming pregnant. The prevalence of obesity was highest among women who were 35 years of age and older (24%); were black, non-Hispanic (32%); had a high school education (28%); and reported Medicaid as their source of insurance coverage before pregnancy (30%). The prevalence of obesity was lowest among women who were 20-34 years of age (22%); were of “other” race/ethnicity (13%); had more than a high school education (20%); and who reported having private insurance coverage before pregnancy (20%), according to the report.
Studies have established that pre-pregnancy body mass index is highly correlated with rates of childhood obesity, but Dr. Bodnar believes the most elegant study, published in Pediatrics in 2004, links the birth records of 8,500 children born to low-income mothers in Ohio with corresponding Women, Infants, and Children data for their children’s respective weights and heights at ages 2, 3, and 4 years. Mothers with pre-pregnancy BMIs in the obese and severely obese ranges had a 3-4 times greater probability that their children had similar BMIs.
More recent U.S. data show that nearly half of all expectant mothers with normal pregravid weights also gain more weight prenatally than the IOM-recommended amounts. The tendency is even more prevalent in those with BMIs in the overweight and obese ranges: 70% of women with pre-gestational BMIs between 25 and 29.9, and 65% of those with BMIs of 30 and over gain too much weight. A 2013 meta-analysis published in JAMA correlated these weight gain patterns with a 90% increased risk of children being obese before the age of 5 years, and a 40% overall lifetime increased risk of obesity.
Stress and sociodemographic factors also can contribute to overeating and unhealthy eating, Dr. Mary Jo Messito, director of the Starting Early Child Obesity Prevention Program at Bellevue Hospital, New York, said in an interview. “High stress can lead to eating higher levels of sugary and processed food.” In lower socioeconomic neighborhoods, processed and fast foods can also be more affordable and more readily available, she added.
At least one study (Sleep Med Rev. 2012 Jun;16[3]:203-11) has established a link between later bedtimes and obesity.
This generation of children sleeps nearly a half hour less per night than did their parents, Dr. Taveras said, and the culprits include later bedtimes, the intake of caffeinated and sugary beverages, and electronic intrusions. A television left on in the room where the child sleeps can make the child dependent upon external means rather than self regulation for putting themselves to sleep, according to Dr. Taveras’ research, published in Pediatrics.
Dr. Taveras also lead a 7-year prospective prebirth cohort study (JAMA Pediatr. 2013 Aug 1;167[8]:731-8) of 1,116 mother and child dyads. In that study, the higher levels of obesity in racial and ethnic minority children were linked to modifiable risk factors. Black and Hispanic 2-year-olds were twice as likely as white ones to have had a cola or other sweetened or caffeinated drink prior to bedtime. By age 4 years, 6.4% of white children, 53% of black children, and 61% of Hispanic children in the study fell to sleep with a television on.
“Dietary patterns in the U.S. are poor, start early, and persist,” Dr. Jose M. Saavedra, chief medical officer for the nutrition division of Nestle USA, said at the meeting. Recently published data in Journal of Obesity (doi: 10.1155/2012/123023) indicate that children who consume sugar-sweetened beverages during infancy are twice as likely to consume them at age 6 years. Similarly, children who do not consume fruits and vegetables daily in infancy were also found to consume them infrequently at the age of 6.
“The patterns start much earlier than what we’ve been paying attention to,” said Dr. Saavedra. He thinks that the window of behavioral plasticity is widest at age 20 months, and urged his peers to find ways to help parents to establish good habits in their children during that time.
Discussing healthy behaviors with parents can help, and may elicit some parental behaviors that can be corrected. During the question and answer session at the meeting, for example, an audience member shared an anecdote about a mother who would only serve her children soda because she’d come from an island nation where the water supply was often unsafe.
Others noted that parents and grandparents who have grown up under conditions of food scarcity can view a “chubby” baby as a healthy baby. Mothers also can feel pressured into overfeeding infants, beginning with supplementing formula.
Also, food is often used as a quick and easy reward, Dr. Messito said. When money is tight, a cookie is an inexpensive treat.
On Twitter @whitneymcknight
WASHINGTON – Childhood obesity is soaring in the United States, especially among Hispanic and African-American children. At the heart of this “epidemic” are dietary and behavioral factors that are linked to stress and poverty rather than race and ethnicity, and the risks may even begin prenatally, according to experts attending an Institute of Medicine forum on early childhood obesity.
Based on data from the 2009-2010 NHANES (National Health and Nutrition Examination Survey), over 8% of children aged 2-5 years in the United States are obese; based on ethnicity, 18% of Hispanic boys and 15% of Hispanic girls in this age group are obese. Nearly 18% of U.S. children aged 6-11 years are obese; nearly 29% of Hispanic boys and 26% of non-Hispanic black girls in this age group are obese.
“If we’re looking for reasons why black and Hispanic children have these disparities ... then we’re looking at what happens in their early years and during pregnancy,” Dr. Elsie Taveras, chief of general academic pediatrics at Massachusetts General Hospital, Boston, said at the IOM meeting.
Chief among the culprits responsible for the “metabolic programming of risk” is the mother’s pregestational weight, according to Dr. Lisa Bodnar, associate professor of endocrinology at the University of Pittsburgh. “Children may already be programmed to become obese as a result of their intrauterine exposure to an obesogenic environment.”
A 2013 report from the Centers for Disease Control and Prevention found that about 1 in 5 women aged 20 years and older who delivered a live-born infant in 2009 were obese prior to becoming pregnant. The prevalence of obesity was highest among women who were 35 years of age and older (24%); were black, non-Hispanic (32%); had a high school education (28%); and reported Medicaid as their source of insurance coverage before pregnancy (30%). The prevalence of obesity was lowest among women who were 20-34 years of age (22%); were of “other” race/ethnicity (13%); had more than a high school education (20%); and who reported having private insurance coverage before pregnancy (20%), according to the report.
Studies have established that pre-pregnancy body mass index is highly correlated with rates of childhood obesity, but Dr. Bodnar believes the most elegant study, published in Pediatrics in 2004, links the birth records of 8,500 children born to low-income mothers in Ohio with corresponding Women, Infants, and Children data for their children’s respective weights and heights at ages 2, 3, and 4 years. Mothers with pre-pregnancy BMIs in the obese and severely obese ranges had a 3-4 times greater probability that their children had similar BMIs.
More recent U.S. data show that nearly half of all expectant mothers with normal pregravid weights also gain more weight prenatally than the IOM-recommended amounts. The tendency is even more prevalent in those with BMIs in the overweight and obese ranges: 70% of women with pre-gestational BMIs between 25 and 29.9, and 65% of those with BMIs of 30 and over gain too much weight. A 2013 meta-analysis published in JAMA correlated these weight gain patterns with a 90% increased risk of children being obese before the age of 5 years, and a 40% overall lifetime increased risk of obesity.
Stress and sociodemographic factors also can contribute to overeating and unhealthy eating, Dr. Mary Jo Messito, director of the Starting Early Child Obesity Prevention Program at Bellevue Hospital, New York, said in an interview. “High stress can lead to eating higher levels of sugary and processed food.” In lower socioeconomic neighborhoods, processed and fast foods can also be more affordable and more readily available, she added.
At least one study (Sleep Med Rev. 2012 Jun;16[3]:203-11) has established a link between later bedtimes and obesity.
This generation of children sleeps nearly a half hour less per night than did their parents, Dr. Taveras said, and the culprits include later bedtimes, the intake of caffeinated and sugary beverages, and electronic intrusions. A television left on in the room where the child sleeps can make the child dependent upon external means rather than self regulation for putting themselves to sleep, according to Dr. Taveras’ research, published in Pediatrics.
Dr. Taveras also lead a 7-year prospective prebirth cohort study (JAMA Pediatr. 2013 Aug 1;167[8]:731-8) of 1,116 mother and child dyads. In that study, the higher levels of obesity in racial and ethnic minority children were linked to modifiable risk factors. Black and Hispanic 2-year-olds were twice as likely as white ones to have had a cola or other sweetened or caffeinated drink prior to bedtime. By age 4 years, 6.4% of white children, 53% of black children, and 61% of Hispanic children in the study fell to sleep with a television on.
“Dietary patterns in the U.S. are poor, start early, and persist,” Dr. Jose M. Saavedra, chief medical officer for the nutrition division of Nestle USA, said at the meeting. Recently published data in Journal of Obesity (doi: 10.1155/2012/123023) indicate that children who consume sugar-sweetened beverages during infancy are twice as likely to consume them at age 6 years. Similarly, children who do not consume fruits and vegetables daily in infancy were also found to consume them infrequently at the age of 6.
“The patterns start much earlier than what we’ve been paying attention to,” said Dr. Saavedra. He thinks that the window of behavioral plasticity is widest at age 20 months, and urged his peers to find ways to help parents to establish good habits in their children during that time.
Discussing healthy behaviors with parents can help, and may elicit some parental behaviors that can be corrected. During the question and answer session at the meeting, for example, an audience member shared an anecdote about a mother who would only serve her children soda because she’d come from an island nation where the water supply was often unsafe.
Others noted that parents and grandparents who have grown up under conditions of food scarcity can view a “chubby” baby as a healthy baby. Mothers also can feel pressured into overfeeding infants, beginning with supplementing formula.
Also, food is often used as a quick and easy reward, Dr. Messito said. When money is tight, a cookie is an inexpensive treat.
On Twitter @whitneymcknight
WASHINGTON – Childhood obesity is soaring in the United States, especially among Hispanic and African-American children. At the heart of this “epidemic” are dietary and behavioral factors that are linked to stress and poverty rather than race and ethnicity, and the risks may even begin prenatally, according to experts attending an Institute of Medicine forum on early childhood obesity.
Based on data from the 2009-2010 NHANES (National Health and Nutrition Examination Survey), over 8% of children aged 2-5 years in the United States are obese; based on ethnicity, 18% of Hispanic boys and 15% of Hispanic girls in this age group are obese. Nearly 18% of U.S. children aged 6-11 years are obese; nearly 29% of Hispanic boys and 26% of non-Hispanic black girls in this age group are obese.
“If we’re looking for reasons why black and Hispanic children have these disparities ... then we’re looking at what happens in their early years and during pregnancy,” Dr. Elsie Taveras, chief of general academic pediatrics at Massachusetts General Hospital, Boston, said at the IOM meeting.
Chief among the culprits responsible for the “metabolic programming of risk” is the mother’s pregestational weight, according to Dr. Lisa Bodnar, associate professor of endocrinology at the University of Pittsburgh. “Children may already be programmed to become obese as a result of their intrauterine exposure to an obesogenic environment.”
A 2013 report from the Centers for Disease Control and Prevention found that about 1 in 5 women aged 20 years and older who delivered a live-born infant in 2009 were obese prior to becoming pregnant. The prevalence of obesity was highest among women who were 35 years of age and older (24%); were black, non-Hispanic (32%); had a high school education (28%); and reported Medicaid as their source of insurance coverage before pregnancy (30%). The prevalence of obesity was lowest among women who were 20-34 years of age (22%); were of “other” race/ethnicity (13%); had more than a high school education (20%); and who reported having private insurance coverage before pregnancy (20%), according to the report.
Studies have established that pre-pregnancy body mass index is highly correlated with rates of childhood obesity, but Dr. Bodnar believes the most elegant study, published in Pediatrics in 2004, links the birth records of 8,500 children born to low-income mothers in Ohio with corresponding Women, Infants, and Children data for their children’s respective weights and heights at ages 2, 3, and 4 years. Mothers with pre-pregnancy BMIs in the obese and severely obese ranges had a 3-4 times greater probability that their children had similar BMIs.
More recent U.S. data show that nearly half of all expectant mothers with normal pregravid weights also gain more weight prenatally than the IOM-recommended amounts. The tendency is even more prevalent in those with BMIs in the overweight and obese ranges: 70% of women with pre-gestational BMIs between 25 and 29.9, and 65% of those with BMIs of 30 and over gain too much weight. A 2013 meta-analysis published in JAMA correlated these weight gain patterns with a 90% increased risk of children being obese before the age of 5 years, and a 40% overall lifetime increased risk of obesity.
Stress and sociodemographic factors also can contribute to overeating and unhealthy eating, Dr. Mary Jo Messito, director of the Starting Early Child Obesity Prevention Program at Bellevue Hospital, New York, said in an interview. “High stress can lead to eating higher levels of sugary and processed food.” In lower socioeconomic neighborhoods, processed and fast foods can also be more affordable and more readily available, she added.
At least one study (Sleep Med Rev. 2012 Jun;16[3]:203-11) has established a link between later bedtimes and obesity.
This generation of children sleeps nearly a half hour less per night than did their parents, Dr. Taveras said, and the culprits include later bedtimes, the intake of caffeinated and sugary beverages, and electronic intrusions. A television left on in the room where the child sleeps can make the child dependent upon external means rather than self regulation for putting themselves to sleep, according to Dr. Taveras’ research, published in Pediatrics.
Dr. Taveras also lead a 7-year prospective prebirth cohort study (JAMA Pediatr. 2013 Aug 1;167[8]:731-8) of 1,116 mother and child dyads. In that study, the higher levels of obesity in racial and ethnic minority children were linked to modifiable risk factors. Black and Hispanic 2-year-olds were twice as likely as white ones to have had a cola or other sweetened or caffeinated drink prior to bedtime. By age 4 years, 6.4% of white children, 53% of black children, and 61% of Hispanic children in the study fell to sleep with a television on.
“Dietary patterns in the U.S. are poor, start early, and persist,” Dr. Jose M. Saavedra, chief medical officer for the nutrition division of Nestle USA, said at the meeting. Recently published data in Journal of Obesity (doi: 10.1155/2012/123023) indicate that children who consume sugar-sweetened beverages during infancy are twice as likely to consume them at age 6 years. Similarly, children who do not consume fruits and vegetables daily in infancy were also found to consume them infrequently at the age of 6.
“The patterns start much earlier than what we’ve been paying attention to,” said Dr. Saavedra. He thinks that the window of behavioral plasticity is widest at age 20 months, and urged his peers to find ways to help parents to establish good habits in their children during that time.
Discussing healthy behaviors with parents can help, and may elicit some parental behaviors that can be corrected. During the question and answer session at the meeting, for example, an audience member shared an anecdote about a mother who would only serve her children soda because she’d come from an island nation where the water supply was often unsafe.
Others noted that parents and grandparents who have grown up under conditions of food scarcity can view a “chubby” baby as a healthy baby. Mothers also can feel pressured into overfeeding infants, beginning with supplementing formula.
Also, food is often used as a quick and easy reward, Dr. Messito said. When money is tight, a cookie is an inexpensive treat.
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM AN EARLY CHILDHOOD OBESITY ROUNDTABLE