User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Higher odds for preterm, C-section births seen in women with PsA
Disease-modifying antirheumatic drugs (DMARDs) such as biologics may carry an increased risk for preterm birth or cesarean delivery for pregnant women with psoriatic arthritis (PsA), according to a recent study published in Arthritis & Rheumatology.
The risk was particularly high for women with PsA who received biologic disease-modifying antirheumatic drugs (bDMARDs), according to Katarina Remaeus, PhD, of the Karolinska Institute in Stockholm and colleagues.
“The results may indicate that a more severe or active PsA disease that requires antirheumatic treatment during pregnancy, especially bDMARDs, is associated with increased risks of adverse pregnancy outcomes compared to non-PsA pregnancies,” Dr. Remaeus and colleagues write in their study. “The risk of preterm birth in PsA pregnancies is further influenced by parity with the most increased risks observed in first pregnancies.”
In a nationwide, register-based cohort study, the researchers evaluated 921 pregnancies of women with PsA between 2007 and 2017, comparing them to the pregnancies of 9,210 women without PsA over the same time frame. The pregnancies for women with PsA were further categorized based on whether the women had not received antirheumatic treatment in the year prior to and/or during pregnancy (495 pregnancies) or had received antirheumatic treatment at any point in the year before and/or during pregnancy (426 pregnancies).
Of the women in the PsA group who were treated in the year prior to pregnancy (170 women), 39.4% received monotherapy with a conventional synthetic DMARD (csDMARD) such as an antimalarial, methotrexate, or sulfasalazine; 24.1% received oral corticosteroids, and 15.9% received a tumor necrosis factor inhibitor (TNFi), whereas about 20% of women received two or more antirheumatic drugs.
In the group of women treated during pregnancy (256 women), 153 did not receive bDMARDs; of these, 41.8% had monotherapy with either a csDMARD or corticosteroids, whereas the group treated with bDMARDs received TNFi monotherapy (43.7%) or TNFi with corticosteroids (35.9%), TNFi with csDMARD (9.7%), or TNFi with csDMARD plus corticosteroids (9.7%).
A majority of women in both groups (70.1%) were between ages 30 and 34 years (37.1%) or older than age 35 years (33%) and had delivered more than one child (63.2%). Women in the PsA group were more likely to be born in a Nordic country (91.8% vs. 82.8%), to have a body mass index between 30.0 and 60.0 kg/m2 (19.9% vs. 12.6%), to be a smoker (9.2% vs. 5.3%), to have hypertension (1.4% vs. 0.8%) or diabetes (1.3% vs. 0.5%) prior to pregnancy, and to have a higher level of education (>12 years; 50.1% vs. 43.3%), compared with women in the non-PsA group.
The results showed women in the PsA group were more likely to experience preterm birth (adjusted odds ratio, 1.69; 95% confidence interval, 1.27-2.24) and undergo an elective (aOR, 1.77; 95% CI, 1.43-2.20) or emergency C-section (aOR, 1.42; 95% CI, 1.10-1.84). The group at highest risk for preterm birth with regard to parity was women with PsA having their first child (aOR, 3.95; 95% CI, 1.43-10.95).
Women who received antirheumatic treatment were at greater risk for experiencing preterm birth (aOR, 2.30; 95% CI, 1.49-3.56), and this risk was even higher for treatment with bDMARDs, compared with women without PsA (aOR, 4.49; 95% CI, 2.60-7.79). Use of bDMARDs also was associated with higher risks for spontaneous preterm birth (aOR, 4.73; 95% CI, 2.53-8.87), preterm birth between 32 and 36 weeks’ gestation (aOR, 5.06; 95% CI, 2.91-8.79), elective C-section (aOR, 2.72; 95% CI, 1.61-4.59), emergency C-section (aOR, 2.06; 95% CI, 1.04-4.07), and preeclampsia (aOR, 2.88, 95% CI, 1.35-6.17).
The researchers note that women with PsA should be evaluated for preterm birth particularly if they are having their first child, and “from a clinical point of view, all women with PsA, regardless of antirheumatic treatment, should be counseled about pregnancy outcomes and receive individualized monitoring during pregnancy.”
Are adverse outcomes linked to disease activity or treatment?
Patients in the study had a higher risk of adverse outcomes when they had a PsA diagnosis, and when they received antirheumatic treatment – but were the adverse outcomes associated with a patient’s high disease activity or need for antirheumatic treatment?
“Our interpretation is that a PsA disease that requires continued antirheumatic treatment during pregnancy is more severe than PsA that does not require treatment,” Dr. Remaeus and colleagues write. “Thus, the increased risk of adverse outcomes in pregnancies with maternal antirheumatic treatment is probably attributed to disease severity rather than an effect of the medication itself.”
Anja Strangfeld, MD, PhD, of the German Rheumatism Research Centre in Berlin, told this news organization that the results of the study are important because it is one of the first to report differences in risk in pregnancy outcomes for women with and without PsA.
“The information is relevant to guide rheumatologists in advising patients with PsA when planning the first or subsequent pregnancies,” she said. “The results are reassuring in reporting that the elevated risk for PsA patients for adverse pregnancy outcomes is low in patients not in need of antirheumatic medication, presumably in low-disease activity.”
However, the study is still unclear on whether the association with adverse pregnancy outcomes in patients is the result of higher disease activity or the need for antirheumatic treatment, she explained.
“It was only hypothesized that those patients under bDMARD treatment are/were in high disease activity. There [is] no information on disease activity in the data sources, which limits the results,” she said. “The investigation still does not solve the important question – if adverse pregnancy outcomes are rather related to high disease activity or the medication to treat this situation.”
There was no specific funding for this study. The study authors and Dr. Strangfeld have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Disease-modifying antirheumatic drugs (DMARDs) such as biologics may carry an increased risk for preterm birth or cesarean delivery for pregnant women with psoriatic arthritis (PsA), according to a recent study published in Arthritis & Rheumatology.
The risk was particularly high for women with PsA who received biologic disease-modifying antirheumatic drugs (bDMARDs), according to Katarina Remaeus, PhD, of the Karolinska Institute in Stockholm and colleagues.
“The results may indicate that a more severe or active PsA disease that requires antirheumatic treatment during pregnancy, especially bDMARDs, is associated with increased risks of adverse pregnancy outcomes compared to non-PsA pregnancies,” Dr. Remaeus and colleagues write in their study. “The risk of preterm birth in PsA pregnancies is further influenced by parity with the most increased risks observed in first pregnancies.”
In a nationwide, register-based cohort study, the researchers evaluated 921 pregnancies of women with PsA between 2007 and 2017, comparing them to the pregnancies of 9,210 women without PsA over the same time frame. The pregnancies for women with PsA were further categorized based on whether the women had not received antirheumatic treatment in the year prior to and/or during pregnancy (495 pregnancies) or had received antirheumatic treatment at any point in the year before and/or during pregnancy (426 pregnancies).
Of the women in the PsA group who were treated in the year prior to pregnancy (170 women), 39.4% received monotherapy with a conventional synthetic DMARD (csDMARD) such as an antimalarial, methotrexate, or sulfasalazine; 24.1% received oral corticosteroids, and 15.9% received a tumor necrosis factor inhibitor (TNFi), whereas about 20% of women received two or more antirheumatic drugs.
In the group of women treated during pregnancy (256 women), 153 did not receive bDMARDs; of these, 41.8% had monotherapy with either a csDMARD or corticosteroids, whereas the group treated with bDMARDs received TNFi monotherapy (43.7%) or TNFi with corticosteroids (35.9%), TNFi with csDMARD (9.7%), or TNFi with csDMARD plus corticosteroids (9.7%).
A majority of women in both groups (70.1%) were between ages 30 and 34 years (37.1%) or older than age 35 years (33%) and had delivered more than one child (63.2%). Women in the PsA group were more likely to be born in a Nordic country (91.8% vs. 82.8%), to have a body mass index between 30.0 and 60.0 kg/m2 (19.9% vs. 12.6%), to be a smoker (9.2% vs. 5.3%), to have hypertension (1.4% vs. 0.8%) or diabetes (1.3% vs. 0.5%) prior to pregnancy, and to have a higher level of education (>12 years; 50.1% vs. 43.3%), compared with women in the non-PsA group.
The results showed women in the PsA group were more likely to experience preterm birth (adjusted odds ratio, 1.69; 95% confidence interval, 1.27-2.24) and undergo an elective (aOR, 1.77; 95% CI, 1.43-2.20) or emergency C-section (aOR, 1.42; 95% CI, 1.10-1.84). The group at highest risk for preterm birth with regard to parity was women with PsA having their first child (aOR, 3.95; 95% CI, 1.43-10.95).
Women who received antirheumatic treatment were at greater risk for experiencing preterm birth (aOR, 2.30; 95% CI, 1.49-3.56), and this risk was even higher for treatment with bDMARDs, compared with women without PsA (aOR, 4.49; 95% CI, 2.60-7.79). Use of bDMARDs also was associated with higher risks for spontaneous preterm birth (aOR, 4.73; 95% CI, 2.53-8.87), preterm birth between 32 and 36 weeks’ gestation (aOR, 5.06; 95% CI, 2.91-8.79), elective C-section (aOR, 2.72; 95% CI, 1.61-4.59), emergency C-section (aOR, 2.06; 95% CI, 1.04-4.07), and preeclampsia (aOR, 2.88, 95% CI, 1.35-6.17).
The researchers note that women with PsA should be evaluated for preterm birth particularly if they are having their first child, and “from a clinical point of view, all women with PsA, regardless of antirheumatic treatment, should be counseled about pregnancy outcomes and receive individualized monitoring during pregnancy.”
Are adverse outcomes linked to disease activity or treatment?
Patients in the study had a higher risk of adverse outcomes when they had a PsA diagnosis, and when they received antirheumatic treatment – but were the adverse outcomes associated with a patient’s high disease activity or need for antirheumatic treatment?
“Our interpretation is that a PsA disease that requires continued antirheumatic treatment during pregnancy is more severe than PsA that does not require treatment,” Dr. Remaeus and colleagues write. “Thus, the increased risk of adverse outcomes in pregnancies with maternal antirheumatic treatment is probably attributed to disease severity rather than an effect of the medication itself.”
Anja Strangfeld, MD, PhD, of the German Rheumatism Research Centre in Berlin, told this news organization that the results of the study are important because it is one of the first to report differences in risk in pregnancy outcomes for women with and without PsA.
“The information is relevant to guide rheumatologists in advising patients with PsA when planning the first or subsequent pregnancies,” she said. “The results are reassuring in reporting that the elevated risk for PsA patients for adverse pregnancy outcomes is low in patients not in need of antirheumatic medication, presumably in low-disease activity.”
However, the study is still unclear on whether the association with adverse pregnancy outcomes in patients is the result of higher disease activity or the need for antirheumatic treatment, she explained.
“It was only hypothesized that those patients under bDMARD treatment are/were in high disease activity. There [is] no information on disease activity in the data sources, which limits the results,” she said. “The investigation still does not solve the important question – if adverse pregnancy outcomes are rather related to high disease activity or the medication to treat this situation.”
There was no specific funding for this study. The study authors and Dr. Strangfeld have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Disease-modifying antirheumatic drugs (DMARDs) such as biologics may carry an increased risk for preterm birth or cesarean delivery for pregnant women with psoriatic arthritis (PsA), according to a recent study published in Arthritis & Rheumatology.
The risk was particularly high for women with PsA who received biologic disease-modifying antirheumatic drugs (bDMARDs), according to Katarina Remaeus, PhD, of the Karolinska Institute in Stockholm and colleagues.
“The results may indicate that a more severe or active PsA disease that requires antirheumatic treatment during pregnancy, especially bDMARDs, is associated with increased risks of adverse pregnancy outcomes compared to non-PsA pregnancies,” Dr. Remaeus and colleagues write in their study. “The risk of preterm birth in PsA pregnancies is further influenced by parity with the most increased risks observed in first pregnancies.”
In a nationwide, register-based cohort study, the researchers evaluated 921 pregnancies of women with PsA between 2007 and 2017, comparing them to the pregnancies of 9,210 women without PsA over the same time frame. The pregnancies for women with PsA were further categorized based on whether the women had not received antirheumatic treatment in the year prior to and/or during pregnancy (495 pregnancies) or had received antirheumatic treatment at any point in the year before and/or during pregnancy (426 pregnancies).
Of the women in the PsA group who were treated in the year prior to pregnancy (170 women), 39.4% received monotherapy with a conventional synthetic DMARD (csDMARD) such as an antimalarial, methotrexate, or sulfasalazine; 24.1% received oral corticosteroids, and 15.9% received a tumor necrosis factor inhibitor (TNFi), whereas about 20% of women received two or more antirheumatic drugs.
In the group of women treated during pregnancy (256 women), 153 did not receive bDMARDs; of these, 41.8% had monotherapy with either a csDMARD or corticosteroids, whereas the group treated with bDMARDs received TNFi monotherapy (43.7%) or TNFi with corticosteroids (35.9%), TNFi with csDMARD (9.7%), or TNFi with csDMARD plus corticosteroids (9.7%).
A majority of women in both groups (70.1%) were between ages 30 and 34 years (37.1%) or older than age 35 years (33%) and had delivered more than one child (63.2%). Women in the PsA group were more likely to be born in a Nordic country (91.8% vs. 82.8%), to have a body mass index between 30.0 and 60.0 kg/m2 (19.9% vs. 12.6%), to be a smoker (9.2% vs. 5.3%), to have hypertension (1.4% vs. 0.8%) or diabetes (1.3% vs. 0.5%) prior to pregnancy, and to have a higher level of education (>12 years; 50.1% vs. 43.3%), compared with women in the non-PsA group.
The results showed women in the PsA group were more likely to experience preterm birth (adjusted odds ratio, 1.69; 95% confidence interval, 1.27-2.24) and undergo an elective (aOR, 1.77; 95% CI, 1.43-2.20) or emergency C-section (aOR, 1.42; 95% CI, 1.10-1.84). The group at highest risk for preterm birth with regard to parity was women with PsA having their first child (aOR, 3.95; 95% CI, 1.43-10.95).
Women who received antirheumatic treatment were at greater risk for experiencing preterm birth (aOR, 2.30; 95% CI, 1.49-3.56), and this risk was even higher for treatment with bDMARDs, compared with women without PsA (aOR, 4.49; 95% CI, 2.60-7.79). Use of bDMARDs also was associated with higher risks for spontaneous preterm birth (aOR, 4.73; 95% CI, 2.53-8.87), preterm birth between 32 and 36 weeks’ gestation (aOR, 5.06; 95% CI, 2.91-8.79), elective C-section (aOR, 2.72; 95% CI, 1.61-4.59), emergency C-section (aOR, 2.06; 95% CI, 1.04-4.07), and preeclampsia (aOR, 2.88, 95% CI, 1.35-6.17).
The researchers note that women with PsA should be evaluated for preterm birth particularly if they are having their first child, and “from a clinical point of view, all women with PsA, regardless of antirheumatic treatment, should be counseled about pregnancy outcomes and receive individualized monitoring during pregnancy.”
Are adverse outcomes linked to disease activity or treatment?
Patients in the study had a higher risk of adverse outcomes when they had a PsA diagnosis, and when they received antirheumatic treatment – but were the adverse outcomes associated with a patient’s high disease activity or need for antirheumatic treatment?
“Our interpretation is that a PsA disease that requires continued antirheumatic treatment during pregnancy is more severe than PsA that does not require treatment,” Dr. Remaeus and colleagues write. “Thus, the increased risk of adverse outcomes in pregnancies with maternal antirheumatic treatment is probably attributed to disease severity rather than an effect of the medication itself.”
Anja Strangfeld, MD, PhD, of the German Rheumatism Research Centre in Berlin, told this news organization that the results of the study are important because it is one of the first to report differences in risk in pregnancy outcomes for women with and without PsA.
“The information is relevant to guide rheumatologists in advising patients with PsA when planning the first or subsequent pregnancies,” she said. “The results are reassuring in reporting that the elevated risk for PsA patients for adverse pregnancy outcomes is low in patients not in need of antirheumatic medication, presumably in low-disease activity.”
However, the study is still unclear on whether the association with adverse pregnancy outcomes in patients is the result of higher disease activity or the need for antirheumatic treatment, she explained.
“It was only hypothesized that those patients under bDMARD treatment are/were in high disease activity. There [is] no information on disease activity in the data sources, which limits the results,” she said. “The investigation still does not solve the important question – if adverse pregnancy outcomes are rather related to high disease activity or the medication to treat this situation.”
There was no specific funding for this study. The study authors and Dr. Strangfeld have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Some diuretics tied to increased skin cancer risk
The findings were originally reported in two Danish case-control studies in which physicians reported a fourfold increased risk of squamous cell carcinoma, and a moderate increased risk of basal cell carcinoma and cutaneous malignant melanoma in patients who used hydrochlorothiazide long-term.
And, while the new study did not find an increased risk of basal cell carcinoma and cutaneous malignant melanoma among long-term users of hydrochlorothiazide, they suggest that bendroflumethiazide “may be a safer alternative for patients at increased risk of skin cancer.” The long-term use of indapamide was associated with a moderately increased risk of cutaneous malignant melanoma but did not alter the risk of either squamous cell or basal cell carcinoma
“Our results suggest that bendroflumethiazide may be a safer alternative to hydrochlorothiazide and indapamide, especially for patients at increased risk of skin cancer, but future studies are needed to rule out a causal association between bendroflumethiazide and cutaneous malignant melanoma,” wrote authors who were led by Christoph R. Meier, PhD, a professor in pharmacy with University Hospital Basel (Switzerland) and a contributor to the Boston Collaborative Drug Surveillance Program.
This study adds to existing evidence that there is a dose-dependent increased risk of squamous cell carcinoma in users of high cumulative doses of hydrochlorothiazide, compared with non–hydrochlorothiazide users.
The study, an observational cohort study, was published earlier this year. It is based on data from the U.K.-based Clinical Practice Research Datalink. It included 271,154 new users of thiazides and thiazidelike diuretics, the majority at 87.6% having been prescribed bendroflumethiazide, 5.8% indapamide, and 3.6% hydrochlorothiazide. Outcomes were compared to those observed in 275,263 users of calcium channel blockers.
“The three primary outcomes of interest were a first-time diagnosis of cutaneous malignant melanoma, basal cell carcinoma, or squamous cell carcinoma,” the authors wrote.
Incidence rates and incidence rate ratios were estimated for both short-term and long-term users of thiazidelike diuretics and calcium channel blockers, while a propensity score (PS) analysis was done in order to control for 23 baseline covariates. The mean follow-up after PS weighting was 3.9 years for indapamide users and 5.5 years for hydrochlorothiazide users. Overall, the incidence rate ratios of squamous cell carcinoma were not markedly increased for either short-term or long-term users of thiazidelike diuretics, the authors reported.
In contrast, the incidence rate ratios of squamous cell carcinoma for hydrochlorothiazide users were increased by 29% for short-term users at an IRR of 1.29 while they were increased by almost twofold for long-term hydrochlorothiazide users at an IRR of 1.95.
Long-term use of hydrochlorothiazide was again associated with a 64% increased risk of basal cell carcinoma, compared with users of a renin-angiotensin inhibitor at a weighted IRR of 1.64.
In contrast, weighted incident rate ratios for basal cell carcinoma for both short-term and long-term thiazide users were not significantly different and results were similar for patients who took hydrochlorothiazide, indapamide, or bendroflumethiazide.
Weighted overall incident rate ratios for cutaneous malignant melanoma were not significantly different for either short-term or long-term users of thiazidelike diuretics, compared with calcium channel blocker users.
However, there was a 43% increased risk of cutaneous malignant melanoma among long-term indapamide users at a weighted IRR of 1.43, compared with calcium channel blocker users, the authors reported.
“Given the biological plausibility and the severe clinical implications of cutaneous malignant melanoma, this finding should be considered carefully,” they cautioned.
Limitations to the study include the fact that the database analyzed does not have information on sun exposure, skin characteristics, or socioeconomic status which may affect the amount of sun exposure participants received.
The authors had no conflicts of interest to declare.
The findings were originally reported in two Danish case-control studies in which physicians reported a fourfold increased risk of squamous cell carcinoma, and a moderate increased risk of basal cell carcinoma and cutaneous malignant melanoma in patients who used hydrochlorothiazide long-term.
And, while the new study did not find an increased risk of basal cell carcinoma and cutaneous malignant melanoma among long-term users of hydrochlorothiazide, they suggest that bendroflumethiazide “may be a safer alternative for patients at increased risk of skin cancer.” The long-term use of indapamide was associated with a moderately increased risk of cutaneous malignant melanoma but did not alter the risk of either squamous cell or basal cell carcinoma
“Our results suggest that bendroflumethiazide may be a safer alternative to hydrochlorothiazide and indapamide, especially for patients at increased risk of skin cancer, but future studies are needed to rule out a causal association between bendroflumethiazide and cutaneous malignant melanoma,” wrote authors who were led by Christoph R. Meier, PhD, a professor in pharmacy with University Hospital Basel (Switzerland) and a contributor to the Boston Collaborative Drug Surveillance Program.
This study adds to existing evidence that there is a dose-dependent increased risk of squamous cell carcinoma in users of high cumulative doses of hydrochlorothiazide, compared with non–hydrochlorothiazide users.
The study, an observational cohort study, was published earlier this year. It is based on data from the U.K.-based Clinical Practice Research Datalink. It included 271,154 new users of thiazides and thiazidelike diuretics, the majority at 87.6% having been prescribed bendroflumethiazide, 5.8% indapamide, and 3.6% hydrochlorothiazide. Outcomes were compared to those observed in 275,263 users of calcium channel blockers.
“The three primary outcomes of interest were a first-time diagnosis of cutaneous malignant melanoma, basal cell carcinoma, or squamous cell carcinoma,” the authors wrote.
Incidence rates and incidence rate ratios were estimated for both short-term and long-term users of thiazidelike diuretics and calcium channel blockers, while a propensity score (PS) analysis was done in order to control for 23 baseline covariates. The mean follow-up after PS weighting was 3.9 years for indapamide users and 5.5 years for hydrochlorothiazide users. Overall, the incidence rate ratios of squamous cell carcinoma were not markedly increased for either short-term or long-term users of thiazidelike diuretics, the authors reported.
In contrast, the incidence rate ratios of squamous cell carcinoma for hydrochlorothiazide users were increased by 29% for short-term users at an IRR of 1.29 while they were increased by almost twofold for long-term hydrochlorothiazide users at an IRR of 1.95.
Long-term use of hydrochlorothiazide was again associated with a 64% increased risk of basal cell carcinoma, compared with users of a renin-angiotensin inhibitor at a weighted IRR of 1.64.
In contrast, weighted incident rate ratios for basal cell carcinoma for both short-term and long-term thiazide users were not significantly different and results were similar for patients who took hydrochlorothiazide, indapamide, or bendroflumethiazide.
Weighted overall incident rate ratios for cutaneous malignant melanoma were not significantly different for either short-term or long-term users of thiazidelike diuretics, compared with calcium channel blocker users.
However, there was a 43% increased risk of cutaneous malignant melanoma among long-term indapamide users at a weighted IRR of 1.43, compared with calcium channel blocker users, the authors reported.
“Given the biological plausibility and the severe clinical implications of cutaneous malignant melanoma, this finding should be considered carefully,” they cautioned.
Limitations to the study include the fact that the database analyzed does not have information on sun exposure, skin characteristics, or socioeconomic status which may affect the amount of sun exposure participants received.
The authors had no conflicts of interest to declare.
The findings were originally reported in two Danish case-control studies in which physicians reported a fourfold increased risk of squamous cell carcinoma, and a moderate increased risk of basal cell carcinoma and cutaneous malignant melanoma in patients who used hydrochlorothiazide long-term.
And, while the new study did not find an increased risk of basal cell carcinoma and cutaneous malignant melanoma among long-term users of hydrochlorothiazide, they suggest that bendroflumethiazide “may be a safer alternative for patients at increased risk of skin cancer.” The long-term use of indapamide was associated with a moderately increased risk of cutaneous malignant melanoma but did not alter the risk of either squamous cell or basal cell carcinoma
“Our results suggest that bendroflumethiazide may be a safer alternative to hydrochlorothiazide and indapamide, especially for patients at increased risk of skin cancer, but future studies are needed to rule out a causal association between bendroflumethiazide and cutaneous malignant melanoma,” wrote authors who were led by Christoph R. Meier, PhD, a professor in pharmacy with University Hospital Basel (Switzerland) and a contributor to the Boston Collaborative Drug Surveillance Program.
This study adds to existing evidence that there is a dose-dependent increased risk of squamous cell carcinoma in users of high cumulative doses of hydrochlorothiazide, compared with non–hydrochlorothiazide users.
The study, an observational cohort study, was published earlier this year. It is based on data from the U.K.-based Clinical Practice Research Datalink. It included 271,154 new users of thiazides and thiazidelike diuretics, the majority at 87.6% having been prescribed bendroflumethiazide, 5.8% indapamide, and 3.6% hydrochlorothiazide. Outcomes were compared to those observed in 275,263 users of calcium channel blockers.
“The three primary outcomes of interest were a first-time diagnosis of cutaneous malignant melanoma, basal cell carcinoma, or squamous cell carcinoma,” the authors wrote.
Incidence rates and incidence rate ratios were estimated for both short-term and long-term users of thiazidelike diuretics and calcium channel blockers, while a propensity score (PS) analysis was done in order to control for 23 baseline covariates. The mean follow-up after PS weighting was 3.9 years for indapamide users and 5.5 years for hydrochlorothiazide users. Overall, the incidence rate ratios of squamous cell carcinoma were not markedly increased for either short-term or long-term users of thiazidelike diuretics, the authors reported.
In contrast, the incidence rate ratios of squamous cell carcinoma for hydrochlorothiazide users were increased by 29% for short-term users at an IRR of 1.29 while they were increased by almost twofold for long-term hydrochlorothiazide users at an IRR of 1.95.
Long-term use of hydrochlorothiazide was again associated with a 64% increased risk of basal cell carcinoma, compared with users of a renin-angiotensin inhibitor at a weighted IRR of 1.64.
In contrast, weighted incident rate ratios for basal cell carcinoma for both short-term and long-term thiazide users were not significantly different and results were similar for patients who took hydrochlorothiazide, indapamide, or bendroflumethiazide.
Weighted overall incident rate ratios for cutaneous malignant melanoma were not significantly different for either short-term or long-term users of thiazidelike diuretics, compared with calcium channel blocker users.
However, there was a 43% increased risk of cutaneous malignant melanoma among long-term indapamide users at a weighted IRR of 1.43, compared with calcium channel blocker users, the authors reported.
“Given the biological plausibility and the severe clinical implications of cutaneous malignant melanoma, this finding should be considered carefully,” they cautioned.
Limitations to the study include the fact that the database analyzed does not have information on sun exposure, skin characteristics, or socioeconomic status which may affect the amount of sun exposure participants received.
The authors had no conflicts of interest to declare.
FROM BRITISH JOURNAL OF DERMATOLOGY
Uncertainty looms large in treatment options for high-risk cutaneous SCC
say the authors of a clinical review recently published in the journal Head and Neck.
The review, led by Jason G. Newman, MD, director of head and neck surgery at Penn Medicine, Philadelphia, includes evidence-based research findings from the last 10 years which describe the possible roles for adjuvant radiation, chemotherapy, immunotherapy, and/or targeted therapy in the management of high-risk cSCC.
Dr. Newman and colleagues wrote that more data – and high-quality data – are needed for physicians to determine with more confidence which adjuvant therapies would be best for specific patients with high-risk cSCC. But without that data, uncertainty in treatment decisions will persist.
“The requirements for and efficacy of adjuvant therapies in cutaneous squamous cell carcinoma are unclear, and the gap in evidence for practice decisions regarding adjuvant therapy in patients with high-risk cSCC has been apparent for more than a decade,” they wrote.
While surgical excision with clear margins of the primary cSCC lesion remains the standard of care, certain high-risk factors necessitate adjuvant therapy, the authors wrote. However, since the evidence consists of small retrospective studies with conflicting results, it is unclear which patients might benefit from adjuvant therapy. This review included recent and current trials in cutaneous SCC and the role of immune checkpoint inhibitors.
According to the review, adjuvant radiation therapy is usually considered with high-risk features, such as perineural invasion, lymph node metastasis and extracapsular/extranodal extension, if the patient is otherwise at high risk for metastasis or recurrence, or if further surgery is not possible.
The National Comprehensive Cancer Network, the American College of Radiology, and the American Society for Radiation Oncology do not recommend adjuvant radiation therapy for most patients with cSCC. However, adjuvant radiation therapy with or without systemic therapy may be considered in locally advanced disease, when further surgery is not an option, or if there is regional lymph node metastasis, but multidisciplinary consultation is recommended.
Regarding checkpoint inhibitors, the NCCN, ACR, and ASTRO do not recommend the use of systemic therapy for local disease amenable to surgery. Potential use of a checkpoint inhibitor with radiation therapy in a clinical trial is recommended for residual disease in locally advanced cSCC as palliative care when other options are not available. While the use of cemiplimab or pembrolizumab are preferred in regional recurrence when curative surgery and radiation therapy are not an option, a targeted therapy can be considered if this is not feasible.
“Given the current activity of checkpoint inhibition in this disease, enthusiasm for the addition of cytotoxic chemotherapeutic agents in the adjuvant setting may be on the decline,” the authors wrote. “Multidisciplinary approaches will most likely continue to be recommended in complicated cases, including those involving immunosuppression.”
The authors said that further study is needed on prognostic testing, such as gene expression profile testing or sentinel lymph node biopsy, as such testing early in disease could identify patients who would likely benefit from adjuvant therapy. They added that the need to identify patients at early stages of disease who are at high risk for metastasis continues to remain critical.
say the authors of a clinical review recently published in the journal Head and Neck.
The review, led by Jason G. Newman, MD, director of head and neck surgery at Penn Medicine, Philadelphia, includes evidence-based research findings from the last 10 years which describe the possible roles for adjuvant radiation, chemotherapy, immunotherapy, and/or targeted therapy in the management of high-risk cSCC.
Dr. Newman and colleagues wrote that more data – and high-quality data – are needed for physicians to determine with more confidence which adjuvant therapies would be best for specific patients with high-risk cSCC. But without that data, uncertainty in treatment decisions will persist.
“The requirements for and efficacy of adjuvant therapies in cutaneous squamous cell carcinoma are unclear, and the gap in evidence for practice decisions regarding adjuvant therapy in patients with high-risk cSCC has been apparent for more than a decade,” they wrote.
While surgical excision with clear margins of the primary cSCC lesion remains the standard of care, certain high-risk factors necessitate adjuvant therapy, the authors wrote. However, since the evidence consists of small retrospective studies with conflicting results, it is unclear which patients might benefit from adjuvant therapy. This review included recent and current trials in cutaneous SCC and the role of immune checkpoint inhibitors.
According to the review, adjuvant radiation therapy is usually considered with high-risk features, such as perineural invasion, lymph node metastasis and extracapsular/extranodal extension, if the patient is otherwise at high risk for metastasis or recurrence, or if further surgery is not possible.
The National Comprehensive Cancer Network, the American College of Radiology, and the American Society for Radiation Oncology do not recommend adjuvant radiation therapy for most patients with cSCC. However, adjuvant radiation therapy with or without systemic therapy may be considered in locally advanced disease, when further surgery is not an option, or if there is regional lymph node metastasis, but multidisciplinary consultation is recommended.
Regarding checkpoint inhibitors, the NCCN, ACR, and ASTRO do not recommend the use of systemic therapy for local disease amenable to surgery. Potential use of a checkpoint inhibitor with radiation therapy in a clinical trial is recommended for residual disease in locally advanced cSCC as palliative care when other options are not available. While the use of cemiplimab or pembrolizumab are preferred in regional recurrence when curative surgery and radiation therapy are not an option, a targeted therapy can be considered if this is not feasible.
“Given the current activity of checkpoint inhibition in this disease, enthusiasm for the addition of cytotoxic chemotherapeutic agents in the adjuvant setting may be on the decline,” the authors wrote. “Multidisciplinary approaches will most likely continue to be recommended in complicated cases, including those involving immunosuppression.”
The authors said that further study is needed on prognostic testing, such as gene expression profile testing or sentinel lymph node biopsy, as such testing early in disease could identify patients who would likely benefit from adjuvant therapy. They added that the need to identify patients at early stages of disease who are at high risk for metastasis continues to remain critical.
say the authors of a clinical review recently published in the journal Head and Neck.
The review, led by Jason G. Newman, MD, director of head and neck surgery at Penn Medicine, Philadelphia, includes evidence-based research findings from the last 10 years which describe the possible roles for adjuvant radiation, chemotherapy, immunotherapy, and/or targeted therapy in the management of high-risk cSCC.
Dr. Newman and colleagues wrote that more data – and high-quality data – are needed for physicians to determine with more confidence which adjuvant therapies would be best for specific patients with high-risk cSCC. But without that data, uncertainty in treatment decisions will persist.
“The requirements for and efficacy of adjuvant therapies in cutaneous squamous cell carcinoma are unclear, and the gap in evidence for practice decisions regarding adjuvant therapy in patients with high-risk cSCC has been apparent for more than a decade,” they wrote.
While surgical excision with clear margins of the primary cSCC lesion remains the standard of care, certain high-risk factors necessitate adjuvant therapy, the authors wrote. However, since the evidence consists of small retrospective studies with conflicting results, it is unclear which patients might benefit from adjuvant therapy. This review included recent and current trials in cutaneous SCC and the role of immune checkpoint inhibitors.
According to the review, adjuvant radiation therapy is usually considered with high-risk features, such as perineural invasion, lymph node metastasis and extracapsular/extranodal extension, if the patient is otherwise at high risk for metastasis or recurrence, or if further surgery is not possible.
The National Comprehensive Cancer Network, the American College of Radiology, and the American Society for Radiation Oncology do not recommend adjuvant radiation therapy for most patients with cSCC. However, adjuvant radiation therapy with or without systemic therapy may be considered in locally advanced disease, when further surgery is not an option, or if there is regional lymph node metastasis, but multidisciplinary consultation is recommended.
Regarding checkpoint inhibitors, the NCCN, ACR, and ASTRO do not recommend the use of systemic therapy for local disease amenable to surgery. Potential use of a checkpoint inhibitor with radiation therapy in a clinical trial is recommended for residual disease in locally advanced cSCC as palliative care when other options are not available. While the use of cemiplimab or pembrolizumab are preferred in regional recurrence when curative surgery and radiation therapy are not an option, a targeted therapy can be considered if this is not feasible.
“Given the current activity of checkpoint inhibition in this disease, enthusiasm for the addition of cytotoxic chemotherapeutic agents in the adjuvant setting may be on the decline,” the authors wrote. “Multidisciplinary approaches will most likely continue to be recommended in complicated cases, including those involving immunosuppression.”
The authors said that further study is needed on prognostic testing, such as gene expression profile testing or sentinel lymph node biopsy, as such testing early in disease could identify patients who would likely benefit from adjuvant therapy. They added that the need to identify patients at early stages of disease who are at high risk for metastasis continues to remain critical.
FROM HEAD AND NECK
One of the keys to success on social media? Entertain and educate the public
Social media isn’t everyone’s cup of tea, but
“I admit that I’m somewhat obsessed with it. I kind of blame it on my work as a dermatologist, that I’m trying to grow my social media as well. It’s interesting to me, fascinating, and I want to understand it more. I think that’s the mindset you need to approach it with.”
Perhaps no other public figure in dermatology has enjoyed success in social media more than Dr. Lee, a board-certified dermatologist who practices in Upland, Calif. In the fall of 2014, she started using Instagram to provide followers a glimpse into her life as a dermatologist, everything from Mohs surgery and Botox to keloid removals and ear lobe repair surgeries. From this she formed her alter ego, “Dr. Pimple Popper,” and became a YouTube sensation, building 7.1 million subscribers over the course of a few years, amounting to 4.5 billion lifetime views. She also grew 12 million followers on TikTok, 4.4 million followers on Instagram, 3 million on Facebook, and more than 139,000 on Twitter. About 80% of her followers are women who range between 18 and 40 years of age.
During the meeting she offered five social media marketing tips for busy clinicians:
You have to ‘play’ to ‘win.’ Active participation in social media is required to develop followers. “You cannot delegate this content,” Dr. Lee said. “You can hire people to help you or leave the task to a social media-savvy medical assistant in your office, but the content should be your responsibility ultimately, because you are the physician,” she added. Not everyone chooses to participate in social media, but it’s also something not to shy away from out of intimidation. “There is some talent associated with it, but it takes a lot of persistence as well,” she said.
Patients come first. Protect them at all costs. Dr. Lee rarely posts the faces of patients she cares for unless they grant consent in advance. “I try to show the work that I do and the beauty of dermatology,” she said during the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. She added that taking part in social media can help you improve communication skills by engaging with followers who like, share, or respond to the material posted. “When you look back at your posts objectively, you learn about yourself and how you relate to your patients,” she said. “It helps to hone my bedside manner and my skills as a dermatologist.”
Show that you are human. Many dermatologists and other “skin influencers” have established their presence on the Internet and may be direct competitors for patients, but that doesn’t mean you can’t establish your own identity. One way to stand out is by posting content related to your authentic self, such as a photo or video that shows you engaged in a hobby, dining at a favorite restaurant, or visiting a beloved vacation spot. “Your followers don’t want a robot, someone who thinks they’re amazing and can do everything,” said Dr. Lee, who stars in her own TV reality show on TLC. “Show that you have a funny side. You want them to fall in love with you and see a little bit of your world, whatever it might be. Charm the socks off of them.”
Entertain first, educate a close second. The main way you’re going to get people to follow and watch you is to provide some entertainment, “not at the expense of a patient or your practice, though,” she said. “Then you’re going to educate people. We dermatologists have something to teach the world because we are experts on skin, hair, and nails. You want to impart this knowledge in a way that captivates people.” It’s like the sense of accomplishment that comes from learning something new after reading a book or watching a movie, she explained. “You feel good about it, and you can take that knowledge with you somewhere else. I love it when kids come up to me and tell me they know what a lipoma is, what a cyst is, and what psoriasis is because they’ve seen my show, or because they follow me on social media. It’s wonderful because I can see that I’ve educated them.”
Be kind and don’t activate the trolls. Dr. Lee allows positivity and kindness to rule the day on her social media content. “This is what I try to relay to followers, but I also do not engage with the negativity,” she said. “Every now and then, there will be someone who tries to insult what you do or who insults you personally. If you engage with them, it almost invites them to do it more. It almost gives them the ability to fight with you. Try to stay above that; just put out goodness and kindness.”
Several years ago, YouTube and Instagram temporarily shut down Dr. Lee’s accounts because she posted graphic images of skin lesions and procedures – a practice that wasn’t so commonplace at the time. “Don’t just post a graphic image just to be graphic,” she advised. “Make sure it has an educational message associated with it. That will help to validate your content. Posting a warning sign that some images may be graphic could help, too.”
Dr. Lee reported having no relevant financial disclosures.
Social media isn’t everyone’s cup of tea, but
“I admit that I’m somewhat obsessed with it. I kind of blame it on my work as a dermatologist, that I’m trying to grow my social media as well. It’s interesting to me, fascinating, and I want to understand it more. I think that’s the mindset you need to approach it with.”
Perhaps no other public figure in dermatology has enjoyed success in social media more than Dr. Lee, a board-certified dermatologist who practices in Upland, Calif. In the fall of 2014, she started using Instagram to provide followers a glimpse into her life as a dermatologist, everything from Mohs surgery and Botox to keloid removals and ear lobe repair surgeries. From this she formed her alter ego, “Dr. Pimple Popper,” and became a YouTube sensation, building 7.1 million subscribers over the course of a few years, amounting to 4.5 billion lifetime views. She also grew 12 million followers on TikTok, 4.4 million followers on Instagram, 3 million on Facebook, and more than 139,000 on Twitter. About 80% of her followers are women who range between 18 and 40 years of age.
During the meeting she offered five social media marketing tips for busy clinicians:
You have to ‘play’ to ‘win.’ Active participation in social media is required to develop followers. “You cannot delegate this content,” Dr. Lee said. “You can hire people to help you or leave the task to a social media-savvy medical assistant in your office, but the content should be your responsibility ultimately, because you are the physician,” she added. Not everyone chooses to participate in social media, but it’s also something not to shy away from out of intimidation. “There is some talent associated with it, but it takes a lot of persistence as well,” she said.
Patients come first. Protect them at all costs. Dr. Lee rarely posts the faces of patients she cares for unless they grant consent in advance. “I try to show the work that I do and the beauty of dermatology,” she said during the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. She added that taking part in social media can help you improve communication skills by engaging with followers who like, share, or respond to the material posted. “When you look back at your posts objectively, you learn about yourself and how you relate to your patients,” she said. “It helps to hone my bedside manner and my skills as a dermatologist.”
Show that you are human. Many dermatologists and other “skin influencers” have established their presence on the Internet and may be direct competitors for patients, but that doesn’t mean you can’t establish your own identity. One way to stand out is by posting content related to your authentic self, such as a photo or video that shows you engaged in a hobby, dining at a favorite restaurant, or visiting a beloved vacation spot. “Your followers don’t want a robot, someone who thinks they’re amazing and can do everything,” said Dr. Lee, who stars in her own TV reality show on TLC. “Show that you have a funny side. You want them to fall in love with you and see a little bit of your world, whatever it might be. Charm the socks off of them.”
Entertain first, educate a close second. The main way you’re going to get people to follow and watch you is to provide some entertainment, “not at the expense of a patient or your practice, though,” she said. “Then you’re going to educate people. We dermatologists have something to teach the world because we are experts on skin, hair, and nails. You want to impart this knowledge in a way that captivates people.” It’s like the sense of accomplishment that comes from learning something new after reading a book or watching a movie, she explained. “You feel good about it, and you can take that knowledge with you somewhere else. I love it when kids come up to me and tell me they know what a lipoma is, what a cyst is, and what psoriasis is because they’ve seen my show, or because they follow me on social media. It’s wonderful because I can see that I’ve educated them.”
Be kind and don’t activate the trolls. Dr. Lee allows positivity and kindness to rule the day on her social media content. “This is what I try to relay to followers, but I also do not engage with the negativity,” she said. “Every now and then, there will be someone who tries to insult what you do or who insults you personally. If you engage with them, it almost invites them to do it more. It almost gives them the ability to fight with you. Try to stay above that; just put out goodness and kindness.”
Several years ago, YouTube and Instagram temporarily shut down Dr. Lee’s accounts because she posted graphic images of skin lesions and procedures – a practice that wasn’t so commonplace at the time. “Don’t just post a graphic image just to be graphic,” she advised. “Make sure it has an educational message associated with it. That will help to validate your content. Posting a warning sign that some images may be graphic could help, too.”
Dr. Lee reported having no relevant financial disclosures.
Social media isn’t everyone’s cup of tea, but
“I admit that I’m somewhat obsessed with it. I kind of blame it on my work as a dermatologist, that I’m trying to grow my social media as well. It’s interesting to me, fascinating, and I want to understand it more. I think that’s the mindset you need to approach it with.”
Perhaps no other public figure in dermatology has enjoyed success in social media more than Dr. Lee, a board-certified dermatologist who practices in Upland, Calif. In the fall of 2014, she started using Instagram to provide followers a glimpse into her life as a dermatologist, everything from Mohs surgery and Botox to keloid removals and ear lobe repair surgeries. From this she formed her alter ego, “Dr. Pimple Popper,” and became a YouTube sensation, building 7.1 million subscribers over the course of a few years, amounting to 4.5 billion lifetime views. She also grew 12 million followers on TikTok, 4.4 million followers on Instagram, 3 million on Facebook, and more than 139,000 on Twitter. About 80% of her followers are women who range between 18 and 40 years of age.
During the meeting she offered five social media marketing tips for busy clinicians:
You have to ‘play’ to ‘win.’ Active participation in social media is required to develop followers. “You cannot delegate this content,” Dr. Lee said. “You can hire people to help you or leave the task to a social media-savvy medical assistant in your office, but the content should be your responsibility ultimately, because you are the physician,” she added. Not everyone chooses to participate in social media, but it’s also something not to shy away from out of intimidation. “There is some talent associated with it, but it takes a lot of persistence as well,” she said.
Patients come first. Protect them at all costs. Dr. Lee rarely posts the faces of patients she cares for unless they grant consent in advance. “I try to show the work that I do and the beauty of dermatology,” she said during the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. She added that taking part in social media can help you improve communication skills by engaging with followers who like, share, or respond to the material posted. “When you look back at your posts objectively, you learn about yourself and how you relate to your patients,” she said. “It helps to hone my bedside manner and my skills as a dermatologist.”
Show that you are human. Many dermatologists and other “skin influencers” have established their presence on the Internet and may be direct competitors for patients, but that doesn’t mean you can’t establish your own identity. One way to stand out is by posting content related to your authentic self, such as a photo or video that shows you engaged in a hobby, dining at a favorite restaurant, or visiting a beloved vacation spot. “Your followers don’t want a robot, someone who thinks they’re amazing and can do everything,” said Dr. Lee, who stars in her own TV reality show on TLC. “Show that you have a funny side. You want them to fall in love with you and see a little bit of your world, whatever it might be. Charm the socks off of them.”
Entertain first, educate a close second. The main way you’re going to get people to follow and watch you is to provide some entertainment, “not at the expense of a patient or your practice, though,” she said. “Then you’re going to educate people. We dermatologists have something to teach the world because we are experts on skin, hair, and nails. You want to impart this knowledge in a way that captivates people.” It’s like the sense of accomplishment that comes from learning something new after reading a book or watching a movie, she explained. “You feel good about it, and you can take that knowledge with you somewhere else. I love it when kids come up to me and tell me they know what a lipoma is, what a cyst is, and what psoriasis is because they’ve seen my show, or because they follow me on social media. It’s wonderful because I can see that I’ve educated them.”
Be kind and don’t activate the trolls. Dr. Lee allows positivity and kindness to rule the day on her social media content. “This is what I try to relay to followers, but I also do not engage with the negativity,” she said. “Every now and then, there will be someone who tries to insult what you do or who insults you personally. If you engage with them, it almost invites them to do it more. It almost gives them the ability to fight with you. Try to stay above that; just put out goodness and kindness.”
Several years ago, YouTube and Instagram temporarily shut down Dr. Lee’s accounts because she posted graphic images of skin lesions and procedures – a practice that wasn’t so commonplace at the time. “Don’t just post a graphic image just to be graphic,” she advised. “Make sure it has an educational message associated with it. That will help to validate your content. Posting a warning sign that some images may be graphic could help, too.”
Dr. Lee reported having no relevant financial disclosures.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE
Accused: Doc increases patient’s penis size with improper fillers; more
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
Immunocompromised people face highest risk of cutaneous SCC metastasis
However, no study has thoroughly evaluated the prognostic factors associated with metastasis until now.
In the Journal of Otolaryngology – Head & Neck Surgery, researchers wrote that immunocompromised individuals, such as solid organ transplant patients, make up 73.3% of all patients with cutaneous SCC who are at risk of metastasis and decreased overall survival.
Led by Alex M. Mlynarek, MD, a specialist in head and neck oncology and microvascular reconstruction at McGill University, Montreal, the finding is based on a systematic literature review of 40 studies involving 8,535 patients.
“The prognostic factors for head and neck cutaneous squamous cell carcinoma that were most consistently reported as significant in the literature are a state of immunosuppression, tumor depth, margins involved, number of lymph nodes affected by carcinoma, parotideal disease, and age,” Dr. Mlynarek and colleagues wrote.
Cutaneous SCC is the second most common nonmelanoma skin cancer with an increase of 263% between 2000 and 2010, shows research from the Mayo Clinic Rochester Epidemiology Project.
Patients in this study with tumors that are 6 mm or greater, or whose tumor invaded fat tissue, were found to have a poor prognosis followed by patients with perineural and lymphovascular invasion and in particular, patients with a poorer grade of cellular differentiation. The number of lymph nodes was significant at 70%, with more than two nodes involved linked to a worse the prognosis, followed by 66.7% for margins involved with carcinoma and 50% for tumor depth.
“The majority of patients with cutaneous SCC undergoes electrodesiccation and curettage, cryosurgery, or Mohs surgery, and have an excellent prognosis,” the authors wrote. “However, there is a subset of patients in which these therapies are unsuccessful and where cutaneous SCC appears to be far more aggressive, often resulting in metastasis and recurrence.”
Age was shown to be a significant factor in 53.3% of the studies, but the extent of its effect on prognosis was questionable.
Sentinel lymph node biopsy is commonly used to stage melanoma and has been used in oral SCC.
“A patient post biopsy with either two major criteria or one major and two minor criteria should be considered as a candidate for sentinel lymph node biopsy,” the authors wrote, adding that the findings were consistent with those for cutaneous SCC generally, not specified to the head and neck.
Limitations of the systematic review include potential selection bias as the majority of the studies were based in Australia and most studies were not specified to cutaneous SCC of the head and neck region.
“Given the low rate of metastasis from head and neck cutaneous SCC lesions, it can be challenging to identify the patients who are at high risk of having metastatic disease,” the authors wrote. “We believe this review could help identify patients that would require a closer follow-up and those that could possibly profit from a sentinel lymph node biopsy.”
No disclosures were disclosed for the authors.
However, no study has thoroughly evaluated the prognostic factors associated with metastasis until now.
In the Journal of Otolaryngology – Head & Neck Surgery, researchers wrote that immunocompromised individuals, such as solid organ transplant patients, make up 73.3% of all patients with cutaneous SCC who are at risk of metastasis and decreased overall survival.
Led by Alex M. Mlynarek, MD, a specialist in head and neck oncology and microvascular reconstruction at McGill University, Montreal, the finding is based on a systematic literature review of 40 studies involving 8,535 patients.
“The prognostic factors for head and neck cutaneous squamous cell carcinoma that were most consistently reported as significant in the literature are a state of immunosuppression, tumor depth, margins involved, number of lymph nodes affected by carcinoma, parotideal disease, and age,” Dr. Mlynarek and colleagues wrote.
Cutaneous SCC is the second most common nonmelanoma skin cancer with an increase of 263% between 2000 and 2010, shows research from the Mayo Clinic Rochester Epidemiology Project.
Patients in this study with tumors that are 6 mm or greater, or whose tumor invaded fat tissue, were found to have a poor prognosis followed by patients with perineural and lymphovascular invasion and in particular, patients with a poorer grade of cellular differentiation. The number of lymph nodes was significant at 70%, with more than two nodes involved linked to a worse the prognosis, followed by 66.7% for margins involved with carcinoma and 50% for tumor depth.
“The majority of patients with cutaneous SCC undergoes electrodesiccation and curettage, cryosurgery, or Mohs surgery, and have an excellent prognosis,” the authors wrote. “However, there is a subset of patients in which these therapies are unsuccessful and where cutaneous SCC appears to be far more aggressive, often resulting in metastasis and recurrence.”
Age was shown to be a significant factor in 53.3% of the studies, but the extent of its effect on prognosis was questionable.
Sentinel lymph node biopsy is commonly used to stage melanoma and has been used in oral SCC.
“A patient post biopsy with either two major criteria or one major and two minor criteria should be considered as a candidate for sentinel lymph node biopsy,” the authors wrote, adding that the findings were consistent with those for cutaneous SCC generally, not specified to the head and neck.
Limitations of the systematic review include potential selection bias as the majority of the studies were based in Australia and most studies were not specified to cutaneous SCC of the head and neck region.
“Given the low rate of metastasis from head and neck cutaneous SCC lesions, it can be challenging to identify the patients who are at high risk of having metastatic disease,” the authors wrote. “We believe this review could help identify patients that would require a closer follow-up and those that could possibly profit from a sentinel lymph node biopsy.”
No disclosures were disclosed for the authors.
However, no study has thoroughly evaluated the prognostic factors associated with metastasis until now.
In the Journal of Otolaryngology – Head & Neck Surgery, researchers wrote that immunocompromised individuals, such as solid organ transplant patients, make up 73.3% of all patients with cutaneous SCC who are at risk of metastasis and decreased overall survival.
Led by Alex M. Mlynarek, MD, a specialist in head and neck oncology and microvascular reconstruction at McGill University, Montreal, the finding is based on a systematic literature review of 40 studies involving 8,535 patients.
“The prognostic factors for head and neck cutaneous squamous cell carcinoma that were most consistently reported as significant in the literature are a state of immunosuppression, tumor depth, margins involved, number of lymph nodes affected by carcinoma, parotideal disease, and age,” Dr. Mlynarek and colleagues wrote.
Cutaneous SCC is the second most common nonmelanoma skin cancer with an increase of 263% between 2000 and 2010, shows research from the Mayo Clinic Rochester Epidemiology Project.
Patients in this study with tumors that are 6 mm or greater, or whose tumor invaded fat tissue, were found to have a poor prognosis followed by patients with perineural and lymphovascular invasion and in particular, patients with a poorer grade of cellular differentiation. The number of lymph nodes was significant at 70%, with more than two nodes involved linked to a worse the prognosis, followed by 66.7% for margins involved with carcinoma and 50% for tumor depth.
“The majority of patients with cutaneous SCC undergoes electrodesiccation and curettage, cryosurgery, or Mohs surgery, and have an excellent prognosis,” the authors wrote. “However, there is a subset of patients in which these therapies are unsuccessful and where cutaneous SCC appears to be far more aggressive, often resulting in metastasis and recurrence.”
Age was shown to be a significant factor in 53.3% of the studies, but the extent of its effect on prognosis was questionable.
Sentinel lymph node biopsy is commonly used to stage melanoma and has been used in oral SCC.
“A patient post biopsy with either two major criteria or one major and two minor criteria should be considered as a candidate for sentinel lymph node biopsy,” the authors wrote, adding that the findings were consistent with those for cutaneous SCC generally, not specified to the head and neck.
Limitations of the systematic review include potential selection bias as the majority of the studies were based in Australia and most studies were not specified to cutaneous SCC of the head and neck region.
“Given the low rate of metastasis from head and neck cutaneous SCC lesions, it can be challenging to identify the patients who are at high risk of having metastatic disease,” the authors wrote. “We believe this review could help identify patients that would require a closer follow-up and those that could possibly profit from a sentinel lymph node biopsy.”
No disclosures were disclosed for the authors.
FROM THE JOURNAL OF OTOLARYNGOLOGY – HEAD AND NECK SURGERY
The devil in the (masking) details
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
Which specialties get the biggest markups over Medicare rates?
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .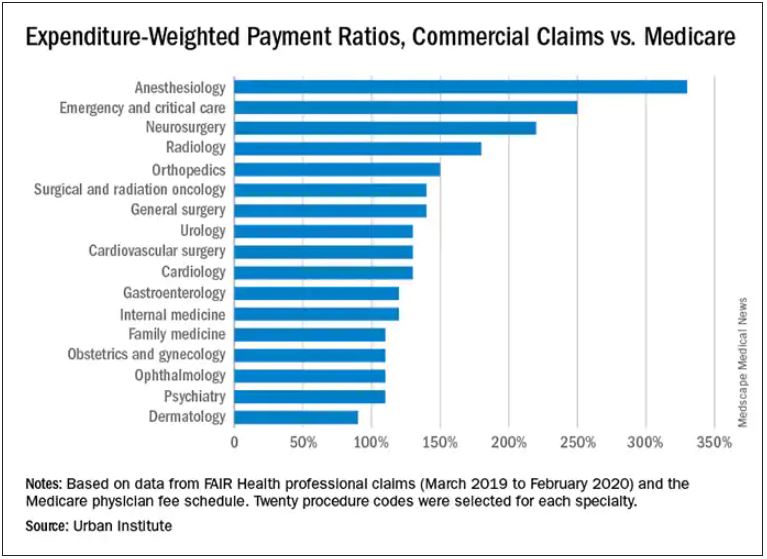
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .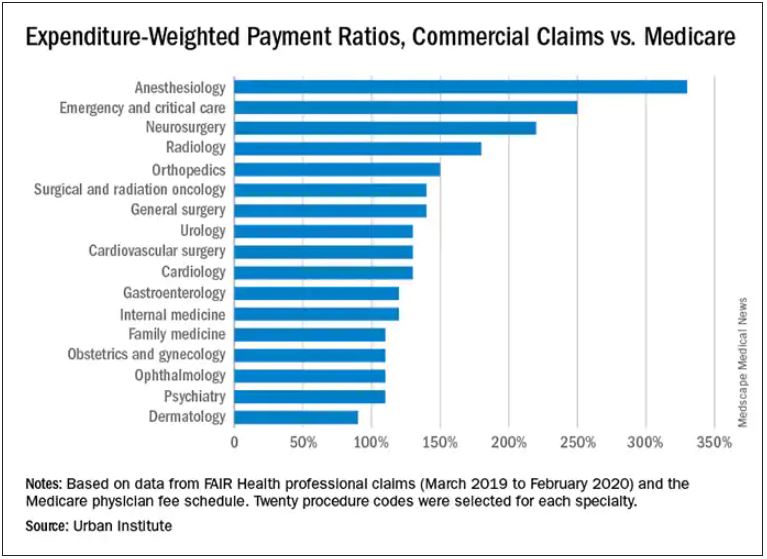
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .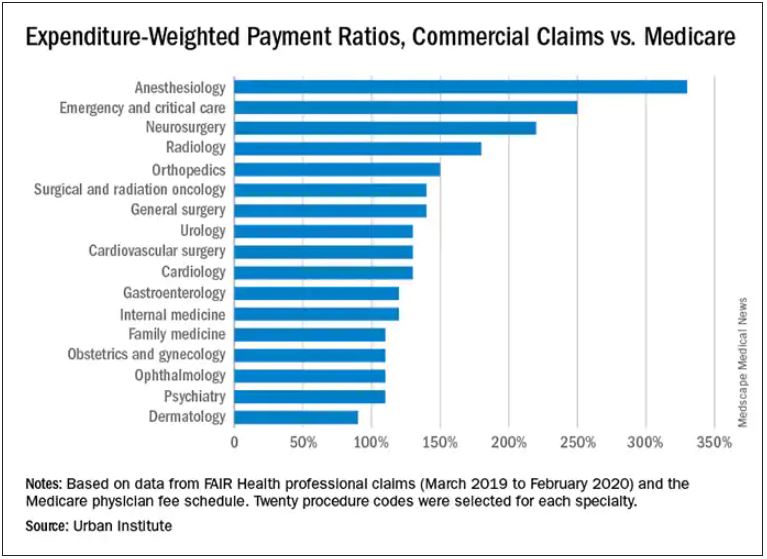
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Hot temperatures in outdoor lockboxes increase sample errors
, according to results from a recent study published in the American Journal of Clinical Pathology.
“Our findings indicate that samples (centrifuged or not centrifuged) were impacted by extreme summer temperatures when stored for short periods of time inside commonly used steel lockboxes,” Joseph R. Wiencek, PhD, medical director of clinical chemistry, Vanderbilt University School of Medicine Core Laboratory in Nashville, said in an interview.
Dr. Wiencek and colleagues picked two dates during the summer of 2019 in a mid-Atlantic state to place two courier lockboxes (LabLocker-KF300) outside in hot temperatures (32º C) starting at 11 a.m., with one lockbox containing two 24-oz cold packs (Nordic NI24) and the other containing no cold packs. The researchers monitored the temperatures of each lockbox over the course of 4 hours.
Overall, eight participants had seven samples in lithium heparin drawn for two studies evaluating centrifuged or not centrifuged samples. In the first study, four participants had seven samples drawn, with one centrifuged sample serving as a control for each patient. The other six samples were wrapped in paper towels, placed in resealable plastic bags, and distributed evenly in the warm and cold lockboxes. The samples did not directly touch the cold packs in the cold lockbox. At 1 hour, 2 hours, and 4 hours, a participant’s sample was removed from each lockbox and centrifuged.
In the second study, another four participants had seven samples drawn. As in the first study, all samples were centrifuged and placed in the lockboxes. For both studies, when samples were centrifuged, plasma from samples was left on the gel barrier when analyzed for concentrations of C-reactive protein, a comprehensive metabolic panel, lactate dehydrogenase (LDH), a lipid panel, magnesium, and phosphorus (Abbott Architect c16000).
In the study of uncentrifuged samples, Dr. Wiencek and colleagues found that when the temperature outside ranged from 28.2º to 44.0º C (mean 40.4º C), the temperature of the cold lockbox was between 16.5º to 22.3º C (mean 22.3º C). The temperature ranged between 34.4º to 46.9º C (mean 42.6º C) in the warm lockbox. For centrifuged samples, the cold lockbox temperature was between 12.2º to 23.0º C (mean 18.0º C) and the warm lockbox was between 25. to 40.8º C (mean 35.2º C) when the outdoor temperature ranged from 27.2º to 46.3º C (mean 37.9º C).
The researchers also calculated the significant change limit (SCL) for each analyte in each sample, finding that aspartate aminotransferase, glucose, LDH, and potassium significantly exceeded the SCL in both the centrifuged and uncentrifuged samples, with the greatest changes seen at the 4-hour timepoint for samples in the warm lockbox (P < .05 for all).
Lockbox instructions are “consistently inconsistent”
In viewing instructions for lockboxes across institutions, Dr. Wiencek said the “outdoor courier lockbox instructions among private, academic and reference laboratories were consistently inconsistent.” For example, no laboratories cited time restrictions for samples in lockboxes, and their descriptions on the number of cold packs a laboratory should use and where the lockbox should be placed varied. The inconsistencies “highlighted the emergent need for standardization and guidance documents for institutions to implement,” Dr. Wiencek said.
One unanswered question is how widespread the problem is. It is unclear how many outdoor courier lockboxes are currently in use in the United States or globally; however, experts agreed it was a common occurrence, with some of the largest laboratory service providers offering outdoor courier lockboxes to their clients.
“Courier lockboxes are everywhere. All you need to do is walk around your clinics that are at your hospitals or clinics located around your grocery store to find them,” Dr. Wiencek said. “Some hang on doors, while others can be found on the ground in direct sunlight on a hot summer day.”
What’s more, institutions may not realize how leaving samples outdoors for extended periods can affect results. “Care teams are commonly unaware that samples placed in these poorly designed lockboxes can experience extreme summer or winter temperatures that may lead to incorrect results,” Dr. Wiencek said. “Healthcare providers need to understand the hidden dangers courier lockboxes have on the quality of their patient’s test results.”
Amy L. Pyle-Eilola, PhD, clinical chemistry director at Nationwide Children’s Hospital in Columbus, Ohio, said a major strength of the study by Dr. Wiencek and colleagues “is just that it was done at all.”
“I appreciate the real-world nature of this study and that it provides a snapshot of what conditions are really like in a lockbox in the summer,” she said in an interview.
In the clinical lab, receiving samples that had been sitting in a courier lockbox “is not uncommon,” Dr. Pyle-Eilola said.
“When I have encountered these situations, I have struggled to decide if it is still appropriate to run the tests. I always look to the medical literature for assistance with these situations, but there has been a paucity of information available on the impact of lockbox storage,” she explained.
The study by Dr. Wiencek and colleagues “provides some much-needed evidence for what is acceptable for lockbox storage conditions,” she said.
Areas of future research
Rodney E. Rohde, PhD, university distinguished chair and professor of the Clinical Laboratory Science (CLS) Program at Texas State University in San Marcos, said in an interview that the study “does a nice job of looking at multiple analytes and controlling for several variables,” but the sample size is small and the results may be difficult to generalize.
Dr. Pyle-Eilola highlighted another limitation — “a common shortcoming of these kinds of studies” — in the use of healthy donors for patient samples, which narrows the range of assay results.
“It is possible that more significant variation in results may be observed in additional analytes if the samples had higher concentrations of those analytes,” she said. “Moreover, this is clinically relevant as the samples stored in such lockboxes are not always from healthy individuals and have abnormal concentrations of analytes.”
Mario Plebani, MD, professor of clinical biochemistry and clinical molecular biology and chief of the department of laboratory medicine at University Hospital of Padova in Padova, Italy, agreed with that assessment.
“[T]he risks for errors and patient safety are higher for values near to the upper or lower reference value, and in general for samples collected in patients with particular diseases and clinical conditions,” he said in an interview.
“This paper deserves a commenting editorial to better highlight the urgent need for further studies on the same issue and in general on the risk in the pre-pre-analytical phase, including sample storage and transportation,” he noted.
Another area of future research is studying patient samples exposed to hotter or colder temperatures in outdoor courier lockboxes outside the mid-Atlantic area. “Here in Texas, temperatures can reach extreme heat levels,” Dr. Rohde said, who added that use of outdoor lockboxes is “very common in my region.”
Dr. Wiencek disclosed he has been a consultant on this research topic for Roche Diagnostics and received an honorarium for speaking on the subject from the American Association for Clinical Chemistry and American Society of Clinical Pathology. The other authors have no relevant conflict of interest. Dr. Pyle-Eilola, Dr. Rohde, and Dr. Plebani have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results from a recent study published in the American Journal of Clinical Pathology.
“Our findings indicate that samples (centrifuged or not centrifuged) were impacted by extreme summer temperatures when stored for short periods of time inside commonly used steel lockboxes,” Joseph R. Wiencek, PhD, medical director of clinical chemistry, Vanderbilt University School of Medicine Core Laboratory in Nashville, said in an interview.
Dr. Wiencek and colleagues picked two dates during the summer of 2019 in a mid-Atlantic state to place two courier lockboxes (LabLocker-KF300) outside in hot temperatures (32º C) starting at 11 a.m., with one lockbox containing two 24-oz cold packs (Nordic NI24) and the other containing no cold packs. The researchers monitored the temperatures of each lockbox over the course of 4 hours.
Overall, eight participants had seven samples in lithium heparin drawn for two studies evaluating centrifuged or not centrifuged samples. In the first study, four participants had seven samples drawn, with one centrifuged sample serving as a control for each patient. The other six samples were wrapped in paper towels, placed in resealable plastic bags, and distributed evenly in the warm and cold lockboxes. The samples did not directly touch the cold packs in the cold lockbox. At 1 hour, 2 hours, and 4 hours, a participant’s sample was removed from each lockbox and centrifuged.
In the second study, another four participants had seven samples drawn. As in the first study, all samples were centrifuged and placed in the lockboxes. For both studies, when samples were centrifuged, plasma from samples was left on the gel barrier when analyzed for concentrations of C-reactive protein, a comprehensive metabolic panel, lactate dehydrogenase (LDH), a lipid panel, magnesium, and phosphorus (Abbott Architect c16000).
In the study of uncentrifuged samples, Dr. Wiencek and colleagues found that when the temperature outside ranged from 28.2º to 44.0º C (mean 40.4º C), the temperature of the cold lockbox was between 16.5º to 22.3º C (mean 22.3º C). The temperature ranged between 34.4º to 46.9º C (mean 42.6º C) in the warm lockbox. For centrifuged samples, the cold lockbox temperature was between 12.2º to 23.0º C (mean 18.0º C) and the warm lockbox was between 25. to 40.8º C (mean 35.2º C) when the outdoor temperature ranged from 27.2º to 46.3º C (mean 37.9º C).
The researchers also calculated the significant change limit (SCL) for each analyte in each sample, finding that aspartate aminotransferase, glucose, LDH, and potassium significantly exceeded the SCL in both the centrifuged and uncentrifuged samples, with the greatest changes seen at the 4-hour timepoint for samples in the warm lockbox (P < .05 for all).
Lockbox instructions are “consistently inconsistent”
In viewing instructions for lockboxes across institutions, Dr. Wiencek said the “outdoor courier lockbox instructions among private, academic and reference laboratories were consistently inconsistent.” For example, no laboratories cited time restrictions for samples in lockboxes, and their descriptions on the number of cold packs a laboratory should use and where the lockbox should be placed varied. The inconsistencies “highlighted the emergent need for standardization and guidance documents for institutions to implement,” Dr. Wiencek said.
One unanswered question is how widespread the problem is. It is unclear how many outdoor courier lockboxes are currently in use in the United States or globally; however, experts agreed it was a common occurrence, with some of the largest laboratory service providers offering outdoor courier lockboxes to their clients.
“Courier lockboxes are everywhere. All you need to do is walk around your clinics that are at your hospitals or clinics located around your grocery store to find them,” Dr. Wiencek said. “Some hang on doors, while others can be found on the ground in direct sunlight on a hot summer day.”
What’s more, institutions may not realize how leaving samples outdoors for extended periods can affect results. “Care teams are commonly unaware that samples placed in these poorly designed lockboxes can experience extreme summer or winter temperatures that may lead to incorrect results,” Dr. Wiencek said. “Healthcare providers need to understand the hidden dangers courier lockboxes have on the quality of their patient’s test results.”
Amy L. Pyle-Eilola, PhD, clinical chemistry director at Nationwide Children’s Hospital in Columbus, Ohio, said a major strength of the study by Dr. Wiencek and colleagues “is just that it was done at all.”
“I appreciate the real-world nature of this study and that it provides a snapshot of what conditions are really like in a lockbox in the summer,” she said in an interview.
In the clinical lab, receiving samples that had been sitting in a courier lockbox “is not uncommon,” Dr. Pyle-Eilola said.
“When I have encountered these situations, I have struggled to decide if it is still appropriate to run the tests. I always look to the medical literature for assistance with these situations, but there has been a paucity of information available on the impact of lockbox storage,” she explained.
The study by Dr. Wiencek and colleagues “provides some much-needed evidence for what is acceptable for lockbox storage conditions,” she said.
Areas of future research
Rodney E. Rohde, PhD, university distinguished chair and professor of the Clinical Laboratory Science (CLS) Program at Texas State University in San Marcos, said in an interview that the study “does a nice job of looking at multiple analytes and controlling for several variables,” but the sample size is small and the results may be difficult to generalize.
Dr. Pyle-Eilola highlighted another limitation — “a common shortcoming of these kinds of studies” — in the use of healthy donors for patient samples, which narrows the range of assay results.
“It is possible that more significant variation in results may be observed in additional analytes if the samples had higher concentrations of those analytes,” she said. “Moreover, this is clinically relevant as the samples stored in such lockboxes are not always from healthy individuals and have abnormal concentrations of analytes.”
Mario Plebani, MD, professor of clinical biochemistry and clinical molecular biology and chief of the department of laboratory medicine at University Hospital of Padova in Padova, Italy, agreed with that assessment.
“[T]he risks for errors and patient safety are higher for values near to the upper or lower reference value, and in general for samples collected in patients with particular diseases and clinical conditions,” he said in an interview.
“This paper deserves a commenting editorial to better highlight the urgent need for further studies on the same issue and in general on the risk in the pre-pre-analytical phase, including sample storage and transportation,” he noted.
Another area of future research is studying patient samples exposed to hotter or colder temperatures in outdoor courier lockboxes outside the mid-Atlantic area. “Here in Texas, temperatures can reach extreme heat levels,” Dr. Rohde said, who added that use of outdoor lockboxes is “very common in my region.”
Dr. Wiencek disclosed he has been a consultant on this research topic for Roche Diagnostics and received an honorarium for speaking on the subject from the American Association for Clinical Chemistry and American Society of Clinical Pathology. The other authors have no relevant conflict of interest. Dr. Pyle-Eilola, Dr. Rohde, and Dr. Plebani have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results from a recent study published in the American Journal of Clinical Pathology.
“Our findings indicate that samples (centrifuged or not centrifuged) were impacted by extreme summer temperatures when stored for short periods of time inside commonly used steel lockboxes,” Joseph R. Wiencek, PhD, medical director of clinical chemistry, Vanderbilt University School of Medicine Core Laboratory in Nashville, said in an interview.
Dr. Wiencek and colleagues picked two dates during the summer of 2019 in a mid-Atlantic state to place two courier lockboxes (LabLocker-KF300) outside in hot temperatures (32º C) starting at 11 a.m., with one lockbox containing two 24-oz cold packs (Nordic NI24) and the other containing no cold packs. The researchers monitored the temperatures of each lockbox over the course of 4 hours.
Overall, eight participants had seven samples in lithium heparin drawn for two studies evaluating centrifuged or not centrifuged samples. In the first study, four participants had seven samples drawn, with one centrifuged sample serving as a control for each patient. The other six samples were wrapped in paper towels, placed in resealable plastic bags, and distributed evenly in the warm and cold lockboxes. The samples did not directly touch the cold packs in the cold lockbox. At 1 hour, 2 hours, and 4 hours, a participant’s sample was removed from each lockbox and centrifuged.
In the second study, another four participants had seven samples drawn. As in the first study, all samples were centrifuged and placed in the lockboxes. For both studies, when samples were centrifuged, plasma from samples was left on the gel barrier when analyzed for concentrations of C-reactive protein, a comprehensive metabolic panel, lactate dehydrogenase (LDH), a lipid panel, magnesium, and phosphorus (Abbott Architect c16000).
In the study of uncentrifuged samples, Dr. Wiencek and colleagues found that when the temperature outside ranged from 28.2º to 44.0º C (mean 40.4º C), the temperature of the cold lockbox was between 16.5º to 22.3º C (mean 22.3º C). The temperature ranged between 34.4º to 46.9º C (mean 42.6º C) in the warm lockbox. For centrifuged samples, the cold lockbox temperature was between 12.2º to 23.0º C (mean 18.0º C) and the warm lockbox was between 25. to 40.8º C (mean 35.2º C) when the outdoor temperature ranged from 27.2º to 46.3º C (mean 37.9º C).
The researchers also calculated the significant change limit (SCL) for each analyte in each sample, finding that aspartate aminotransferase, glucose, LDH, and potassium significantly exceeded the SCL in both the centrifuged and uncentrifuged samples, with the greatest changes seen at the 4-hour timepoint for samples in the warm lockbox (P < .05 for all).
Lockbox instructions are “consistently inconsistent”
In viewing instructions for lockboxes across institutions, Dr. Wiencek said the “outdoor courier lockbox instructions among private, academic and reference laboratories were consistently inconsistent.” For example, no laboratories cited time restrictions for samples in lockboxes, and their descriptions on the number of cold packs a laboratory should use and where the lockbox should be placed varied. The inconsistencies “highlighted the emergent need for standardization and guidance documents for institutions to implement,” Dr. Wiencek said.
One unanswered question is how widespread the problem is. It is unclear how many outdoor courier lockboxes are currently in use in the United States or globally; however, experts agreed it was a common occurrence, with some of the largest laboratory service providers offering outdoor courier lockboxes to their clients.
“Courier lockboxes are everywhere. All you need to do is walk around your clinics that are at your hospitals or clinics located around your grocery store to find them,” Dr. Wiencek said. “Some hang on doors, while others can be found on the ground in direct sunlight on a hot summer day.”
What’s more, institutions may not realize how leaving samples outdoors for extended periods can affect results. “Care teams are commonly unaware that samples placed in these poorly designed lockboxes can experience extreme summer or winter temperatures that may lead to incorrect results,” Dr. Wiencek said. “Healthcare providers need to understand the hidden dangers courier lockboxes have on the quality of their patient’s test results.”
Amy L. Pyle-Eilola, PhD, clinical chemistry director at Nationwide Children’s Hospital in Columbus, Ohio, said a major strength of the study by Dr. Wiencek and colleagues “is just that it was done at all.”
“I appreciate the real-world nature of this study and that it provides a snapshot of what conditions are really like in a lockbox in the summer,” she said in an interview.
In the clinical lab, receiving samples that had been sitting in a courier lockbox “is not uncommon,” Dr. Pyle-Eilola said.
“When I have encountered these situations, I have struggled to decide if it is still appropriate to run the tests. I always look to the medical literature for assistance with these situations, but there has been a paucity of information available on the impact of lockbox storage,” she explained.
The study by Dr. Wiencek and colleagues “provides some much-needed evidence for what is acceptable for lockbox storage conditions,” she said.
Areas of future research
Rodney E. Rohde, PhD, university distinguished chair and professor of the Clinical Laboratory Science (CLS) Program at Texas State University in San Marcos, said in an interview that the study “does a nice job of looking at multiple analytes and controlling for several variables,” but the sample size is small and the results may be difficult to generalize.
Dr. Pyle-Eilola highlighted another limitation — “a common shortcoming of these kinds of studies” — in the use of healthy donors for patient samples, which narrows the range of assay results.
“It is possible that more significant variation in results may be observed in additional analytes if the samples had higher concentrations of those analytes,” she said. “Moreover, this is clinically relevant as the samples stored in such lockboxes are not always from healthy individuals and have abnormal concentrations of analytes.”
Mario Plebani, MD, professor of clinical biochemistry and clinical molecular biology and chief of the department of laboratory medicine at University Hospital of Padova in Padova, Italy, agreed with that assessment.
“[T]he risks for errors and patient safety are higher for values near to the upper or lower reference value, and in general for samples collected in patients with particular diseases and clinical conditions,” he said in an interview.
“This paper deserves a commenting editorial to better highlight the urgent need for further studies on the same issue and in general on the risk in the pre-pre-analytical phase, including sample storage and transportation,” he noted.
Another area of future research is studying patient samples exposed to hotter or colder temperatures in outdoor courier lockboxes outside the mid-Atlantic area. “Here in Texas, temperatures can reach extreme heat levels,” Dr. Rohde said, who added that use of outdoor lockboxes is “very common in my region.”
Dr. Wiencek disclosed he has been a consultant on this research topic for Roche Diagnostics and received an honorarium for speaking on the subject from the American Association for Clinical Chemistry and American Society of Clinical Pathology. The other authors have no relevant conflict of interest. Dr. Pyle-Eilola, Dr. Rohde, and Dr. Plebani have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treatment with novel laser in acne studies targets sebaceous glands
at 12 months, a development that indicates the promise this has a treatment for acne in the future.
Currently, “there is no strong evidence that lasers are better than conventional treatments for acne,” Fernanda H. Sakamoto, MD, PhD, said during a virtual course on laser and aesthetic skin therapy. Some patients struggling with acne “search for so many different options and they end up spending a lot of money,” which, she said, includes an estimated $222 million for laser treatment alone in 2019.
Unlike other existing laser and light options for acne treatment, however, Accure is the first light-based platform to selectively target and injure sebaceous glands, the main source of sebum production and the key to a durable solution for acne. The laser, which uses a 1,726-nm wavelength, is being developed by researchers at the Wellman Center for Photomedicine, at Massachusetts General Hospital, Boston and was granted the European CE mark, which allows marketing of the product in Europe, in May of 2020.
In 2012, Dr. Sakamoto, a dermatologist at the center, and her Wellman colleagues were the first to describe the use of selective photothermolysis to target sebaceous glands. “We found that the peak absorption of lipids in sebaceous glands occurs between 1,700 and 1,720 nm,” she said. “Compared to water, the contrast is not high, so for us to develop a laser that is selective for acne, we needed to develop a strong cooling system and we had to create different methods to make it more selective.” She said that it took about 10 years to develop this laser.
The latest Accure prototype features a smart laser handpiece for real time thermal monitoring and precise delivery of laser emissions. “We have developed a mathematical model which permits us to predict safe and effective treatment patterns,” Dr. Sakamoto said at the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “It has a unique cooling system that can control and protect the skin.”
The clinical trial for Food and Drug Administration clearance, which was delayed because of the COVID-19 pandemic, is still underway, she said, and the hope is that the laser will cleared by the FDA by next year. She and her Wellman colleagues have been working with four veteran dermatologists to conduct clinical trials of the device: Emil Tanghetti, MD, in California; Roy Geronemus, MD, in New York; Joel Cohen, MD, in Colorado; and Daniel Friedmann, MD, in Texas. As of Oct. 2, 2021, more than 50 patients were enrolled in four IRB-approved studies and an additional 30 are enrolled in a pilot facial acne trial, Dr. Sakamoto said. In the trials, patients are followed at 4, 8, 12, and 24 weeks post treatment.
Among patients enrolled in the pilot facial acne trial, researchers have observed a 100% responder rate for patients with more than five acne lesions at 4, 8, 12, and 24 weeks post treatment. The average lesion reduction at week 12 was 82% and the mean Visual Analog Scale score immediately after treatment was 2.10 out of 10. Each patient received more than 12,000 trigger pulls of energy from the device with no adverse events.
“This laser is absorbed in the near-infrared spectrum, so there is no melanin absorption,” Dr. Sakamoto explained. “It’s pretty much a color-blind laser, so we can treat darker skin types safely, with no side effects.” In other findings, researchers observed a 45% reduction in acne lesions after one treatment session, which “keeps improving over time,” she said. “At 12 weeks, we have clearance of over 80% of the lesions.”
At 12 months, they observed a 90% inflammatory lesion count reduction from baseline and a rapid response to treatment: a 73% reduction achieved after the first two treatment sessions. Histological studies revealed selective sebaceous gland destruction with no damage to the epidermis, surrounding dermis, or other follicular structures.
Dr. Sakamoto disclosed that she has received portions of patent royalties from Massachusetts General Hospital. Accure was cofounded by R. Rox Anderson, MD, the director of the Wellman Center.
at 12 months, a development that indicates the promise this has a treatment for acne in the future.
Currently, “there is no strong evidence that lasers are better than conventional treatments for acne,” Fernanda H. Sakamoto, MD, PhD, said during a virtual course on laser and aesthetic skin therapy. Some patients struggling with acne “search for so many different options and they end up spending a lot of money,” which, she said, includes an estimated $222 million for laser treatment alone in 2019.
Unlike other existing laser and light options for acne treatment, however, Accure is the first light-based platform to selectively target and injure sebaceous glands, the main source of sebum production and the key to a durable solution for acne. The laser, which uses a 1,726-nm wavelength, is being developed by researchers at the Wellman Center for Photomedicine, at Massachusetts General Hospital, Boston and was granted the European CE mark, which allows marketing of the product in Europe, in May of 2020.
In 2012, Dr. Sakamoto, a dermatologist at the center, and her Wellman colleagues were the first to describe the use of selective photothermolysis to target sebaceous glands. “We found that the peak absorption of lipids in sebaceous glands occurs between 1,700 and 1,720 nm,” she said. “Compared to water, the contrast is not high, so for us to develop a laser that is selective for acne, we needed to develop a strong cooling system and we had to create different methods to make it more selective.” She said that it took about 10 years to develop this laser.
The latest Accure prototype features a smart laser handpiece for real time thermal monitoring and precise delivery of laser emissions. “We have developed a mathematical model which permits us to predict safe and effective treatment patterns,” Dr. Sakamoto said at the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “It has a unique cooling system that can control and protect the skin.”
The clinical trial for Food and Drug Administration clearance, which was delayed because of the COVID-19 pandemic, is still underway, she said, and the hope is that the laser will cleared by the FDA by next year. She and her Wellman colleagues have been working with four veteran dermatologists to conduct clinical trials of the device: Emil Tanghetti, MD, in California; Roy Geronemus, MD, in New York; Joel Cohen, MD, in Colorado; and Daniel Friedmann, MD, in Texas. As of Oct. 2, 2021, more than 50 patients were enrolled in four IRB-approved studies and an additional 30 are enrolled in a pilot facial acne trial, Dr. Sakamoto said. In the trials, patients are followed at 4, 8, 12, and 24 weeks post treatment.
Among patients enrolled in the pilot facial acne trial, researchers have observed a 100% responder rate for patients with more than five acne lesions at 4, 8, 12, and 24 weeks post treatment. The average lesion reduction at week 12 was 82% and the mean Visual Analog Scale score immediately after treatment was 2.10 out of 10. Each patient received more than 12,000 trigger pulls of energy from the device with no adverse events.
“This laser is absorbed in the near-infrared spectrum, so there is no melanin absorption,” Dr. Sakamoto explained. “It’s pretty much a color-blind laser, so we can treat darker skin types safely, with no side effects.” In other findings, researchers observed a 45% reduction in acne lesions after one treatment session, which “keeps improving over time,” she said. “At 12 weeks, we have clearance of over 80% of the lesions.”
At 12 months, they observed a 90% inflammatory lesion count reduction from baseline and a rapid response to treatment: a 73% reduction achieved after the first two treatment sessions. Histological studies revealed selective sebaceous gland destruction with no damage to the epidermis, surrounding dermis, or other follicular structures.
Dr. Sakamoto disclosed that she has received portions of patent royalties from Massachusetts General Hospital. Accure was cofounded by R. Rox Anderson, MD, the director of the Wellman Center.
at 12 months, a development that indicates the promise this has a treatment for acne in the future.
Currently, “there is no strong evidence that lasers are better than conventional treatments for acne,” Fernanda H. Sakamoto, MD, PhD, said during a virtual course on laser and aesthetic skin therapy. Some patients struggling with acne “search for so many different options and they end up spending a lot of money,” which, she said, includes an estimated $222 million for laser treatment alone in 2019.
Unlike other existing laser and light options for acne treatment, however, Accure is the first light-based platform to selectively target and injure sebaceous glands, the main source of sebum production and the key to a durable solution for acne. The laser, which uses a 1,726-nm wavelength, is being developed by researchers at the Wellman Center for Photomedicine, at Massachusetts General Hospital, Boston and was granted the European CE mark, which allows marketing of the product in Europe, in May of 2020.
In 2012, Dr. Sakamoto, a dermatologist at the center, and her Wellman colleagues were the first to describe the use of selective photothermolysis to target sebaceous glands. “We found that the peak absorption of lipids in sebaceous glands occurs between 1,700 and 1,720 nm,” she said. “Compared to water, the contrast is not high, so for us to develop a laser that is selective for acne, we needed to develop a strong cooling system and we had to create different methods to make it more selective.” She said that it took about 10 years to develop this laser.
The latest Accure prototype features a smart laser handpiece for real time thermal monitoring and precise delivery of laser emissions. “We have developed a mathematical model which permits us to predict safe and effective treatment patterns,” Dr. Sakamoto said at the meeting, which was named “Laser & Aesthetic Skin Therapy: What’s the Truth?” and was sponsored by Harvard Medical School, Massachusetts General Hospital, and the Wellman Center for Photomedicine. “It has a unique cooling system that can control and protect the skin.”
The clinical trial for Food and Drug Administration clearance, which was delayed because of the COVID-19 pandemic, is still underway, she said, and the hope is that the laser will cleared by the FDA by next year. She and her Wellman colleagues have been working with four veteran dermatologists to conduct clinical trials of the device: Emil Tanghetti, MD, in California; Roy Geronemus, MD, in New York; Joel Cohen, MD, in Colorado; and Daniel Friedmann, MD, in Texas. As of Oct. 2, 2021, more than 50 patients were enrolled in four IRB-approved studies and an additional 30 are enrolled in a pilot facial acne trial, Dr. Sakamoto said. In the trials, patients are followed at 4, 8, 12, and 24 weeks post treatment.
Among patients enrolled in the pilot facial acne trial, researchers have observed a 100% responder rate for patients with more than five acne lesions at 4, 8, 12, and 24 weeks post treatment. The average lesion reduction at week 12 was 82% and the mean Visual Analog Scale score immediately after treatment was 2.10 out of 10. Each patient received more than 12,000 trigger pulls of energy from the device with no adverse events.
“This laser is absorbed in the near-infrared spectrum, so there is no melanin absorption,” Dr. Sakamoto explained. “It’s pretty much a color-blind laser, so we can treat darker skin types safely, with no side effects.” In other findings, researchers observed a 45% reduction in acne lesions after one treatment session, which “keeps improving over time,” she said. “At 12 weeks, we have clearance of over 80% of the lesions.”
At 12 months, they observed a 90% inflammatory lesion count reduction from baseline and a rapid response to treatment: a 73% reduction achieved after the first two treatment sessions. Histological studies revealed selective sebaceous gland destruction with no damage to the epidermis, surrounding dermis, or other follicular structures.
Dr. Sakamoto disclosed that she has received portions of patent royalties from Massachusetts General Hospital. Accure was cofounded by R. Rox Anderson, MD, the director of the Wellman Center.
FROM A LASER & AESTHETIC SKIN THERAPY COURSE











