User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Biden vaccine mandate rule could be ready within weeks
The emergency rule ordering large employers to require COVID-19 vaccines or weekly tests for their workers could be ready “within weeks,” officials said in a news briefing Sept. 10.
Labor Secretary Martin Walsh will oversee the Occupational Safety and Health Administration as the agency drafts what’s known as an emergency temporary standard, similar to the one that was issued a few months ago to protect health care workers during the pandemic.
The rule should be ready within weeks, said Jeff Zients, coordinator of the White House COVID-19 response team.
He said the ultimate goal of the president’s plan is to increase vaccinations as quickly as possible to keep schools open, the economy recovering, and to decrease hospitalizations and deaths from COVID.
Mr. Zients declined to set hard numbers around those goals, but other experts did.
“What we need to get to is 85% to 90% population immunity, and that’s going to be immunity both from vaccines and infections, before that really begins to have a substantial dampening effect on viral spread,” Ashish Jha, MD, dean of the Brown University School of Public Health, Providence, R.I., said on a call with reporters Sept. 9.
He said immunity needs to be that high because the Delta variant is so contagious.
Mandates are seen as the most effective way to increase immunity and do it quickly.
David Michaels, PhD, an epidemiologist and professor at George Washington University, Washington, says OSHA will have to work through a number of steps to develop the rule.
“OSHA will have to write a preamble explaining the standard, its justifications, its costs, and how it will be enforced,” says Dr. Michaels, who led OSHA for the Obama administration. After that, the rule will be reviewed by the White House. Then employers will have some time – typically 30 days – to comply.
In addition to drafting the standard, OSHA will oversee its enforcement.
Companies that refuse to follow the standard could be fined $13,600 per violation, Mr. Zients said.
Dr. Michaels said he doesn’t expect enforcement to be a big issue, and he said we’re likely to see the rule well before it is final.
“Most employers are law-abiding. When OSHA issues a standard, they try to meet whatever those requirements are, and generally that starts to happen when the rule is announced, even before it goes into effect,” he said.
The rule may face legal challenges as well. Several governors and state attorneys general, as well as the Republican National Committee, have promised lawsuits to stop the vaccine mandates.
Critics of the new mandates say they impinge on personal freedom and impose burdens on businesses.
But the president hit back at that notion Sept. 10.
“Look, I am so disappointed that, particularly some of the Republican governors, have been so cavalier with the health of these kids, so cavalier of the health of their communities,” President Biden told reporters.
“I don’t know of any scientist out there in this field who doesn’t think it makes considerable sense to do the six things I’ve suggested.”
Yet, others feel the new requirements didn’t go far enough.
“These are good steps in the right direction, but they’re not enough to get the job done,” said Leana Wen, MD, in an op-ed for The Washington Post.
Dr. Wen, an expert in public health, wondered why President Biden didn’t mandate vaccinations for plane and train travel. She was disappointed that children 12 and older weren’t required to be vaccinated, too.
“There are mandates for childhood immunizations in every state. The coronavirus vaccine should be no different,” she wrote.
Vaccines remain the cornerstone of U.S. plans to control the pandemic.
On Sept. 10, there was new research from the CDC and state health departments showing that the COVID-19 vaccines continue to be highly effective at preventing severe illness and death.
But the study also found that the vaccines became less effective in the United States after Delta became the dominant cause of infections here.
The study, which included more than 600,000 COVID-19 cases, analyzed breakthrough infections – cases where people got sick despite being fully vaccinated – in 13 jurisdictions in the United States between April 4 and July 17, 2021.
Epidemiologists compared breakthrough infections between two distinct points in time: Before and after the period when the Delta variant began causing most infections.
From April 4 to June 19, fully vaccinated people made up just 5% of cases, 7% of hospitalizations, and 8% of deaths. From June 20 to July 17, 18% of cases, 14% of hospitalizations, and 16% of deaths occurred in fully vaccinated people.
“After the week of June 20, 2021, when the SARS-CoV-2 Delta variant became predominant, the percentage of fully vaccinated persons among cases increased more than expected,” the study authors wrote.
Even after Delta swept the United States, fully vaccinated people were 5 times less likely to get a COVID-19 infection and more than 10 times less likely to be hospitalized or die from one.
“As we have shown in study after study, vaccination works,” CDC Director Rochelle Walensky, MD, said during the White House news briefing.
“We have the scientific tools we need to turn the corner on this pandemic. Vaccination works and will protect us from the severe complications of COVID-19,” she said.
A version of this article first appeared on WebMD.com.
The emergency rule ordering large employers to require COVID-19 vaccines or weekly tests for their workers could be ready “within weeks,” officials said in a news briefing Sept. 10.
Labor Secretary Martin Walsh will oversee the Occupational Safety and Health Administration as the agency drafts what’s known as an emergency temporary standard, similar to the one that was issued a few months ago to protect health care workers during the pandemic.
The rule should be ready within weeks, said Jeff Zients, coordinator of the White House COVID-19 response team.
He said the ultimate goal of the president’s plan is to increase vaccinations as quickly as possible to keep schools open, the economy recovering, and to decrease hospitalizations and deaths from COVID.
Mr. Zients declined to set hard numbers around those goals, but other experts did.
“What we need to get to is 85% to 90% population immunity, and that’s going to be immunity both from vaccines and infections, before that really begins to have a substantial dampening effect on viral spread,” Ashish Jha, MD, dean of the Brown University School of Public Health, Providence, R.I., said on a call with reporters Sept. 9.
He said immunity needs to be that high because the Delta variant is so contagious.
Mandates are seen as the most effective way to increase immunity and do it quickly.
David Michaels, PhD, an epidemiologist and professor at George Washington University, Washington, says OSHA will have to work through a number of steps to develop the rule.
“OSHA will have to write a preamble explaining the standard, its justifications, its costs, and how it will be enforced,” says Dr. Michaels, who led OSHA for the Obama administration. After that, the rule will be reviewed by the White House. Then employers will have some time – typically 30 days – to comply.
In addition to drafting the standard, OSHA will oversee its enforcement.
Companies that refuse to follow the standard could be fined $13,600 per violation, Mr. Zients said.
Dr. Michaels said he doesn’t expect enforcement to be a big issue, and he said we’re likely to see the rule well before it is final.
“Most employers are law-abiding. When OSHA issues a standard, they try to meet whatever those requirements are, and generally that starts to happen when the rule is announced, even before it goes into effect,” he said.
The rule may face legal challenges as well. Several governors and state attorneys general, as well as the Republican National Committee, have promised lawsuits to stop the vaccine mandates.
Critics of the new mandates say they impinge on personal freedom and impose burdens on businesses.
But the president hit back at that notion Sept. 10.
“Look, I am so disappointed that, particularly some of the Republican governors, have been so cavalier with the health of these kids, so cavalier of the health of their communities,” President Biden told reporters.
“I don’t know of any scientist out there in this field who doesn’t think it makes considerable sense to do the six things I’ve suggested.”
Yet, others feel the new requirements didn’t go far enough.
“These are good steps in the right direction, but they’re not enough to get the job done,” said Leana Wen, MD, in an op-ed for The Washington Post.
Dr. Wen, an expert in public health, wondered why President Biden didn’t mandate vaccinations for plane and train travel. She was disappointed that children 12 and older weren’t required to be vaccinated, too.
“There are mandates for childhood immunizations in every state. The coronavirus vaccine should be no different,” she wrote.
Vaccines remain the cornerstone of U.S. plans to control the pandemic.
On Sept. 10, there was new research from the CDC and state health departments showing that the COVID-19 vaccines continue to be highly effective at preventing severe illness and death.
But the study also found that the vaccines became less effective in the United States after Delta became the dominant cause of infections here.
The study, which included more than 600,000 COVID-19 cases, analyzed breakthrough infections – cases where people got sick despite being fully vaccinated – in 13 jurisdictions in the United States between April 4 and July 17, 2021.
Epidemiologists compared breakthrough infections between two distinct points in time: Before and after the period when the Delta variant began causing most infections.
From April 4 to June 19, fully vaccinated people made up just 5% of cases, 7% of hospitalizations, and 8% of deaths. From June 20 to July 17, 18% of cases, 14% of hospitalizations, and 16% of deaths occurred in fully vaccinated people.
“After the week of June 20, 2021, when the SARS-CoV-2 Delta variant became predominant, the percentage of fully vaccinated persons among cases increased more than expected,” the study authors wrote.
Even after Delta swept the United States, fully vaccinated people were 5 times less likely to get a COVID-19 infection and more than 10 times less likely to be hospitalized or die from one.
“As we have shown in study after study, vaccination works,” CDC Director Rochelle Walensky, MD, said during the White House news briefing.
“We have the scientific tools we need to turn the corner on this pandemic. Vaccination works and will protect us from the severe complications of COVID-19,” she said.
A version of this article first appeared on WebMD.com.
The emergency rule ordering large employers to require COVID-19 vaccines or weekly tests for their workers could be ready “within weeks,” officials said in a news briefing Sept. 10.
Labor Secretary Martin Walsh will oversee the Occupational Safety and Health Administration as the agency drafts what’s known as an emergency temporary standard, similar to the one that was issued a few months ago to protect health care workers during the pandemic.
The rule should be ready within weeks, said Jeff Zients, coordinator of the White House COVID-19 response team.
He said the ultimate goal of the president’s plan is to increase vaccinations as quickly as possible to keep schools open, the economy recovering, and to decrease hospitalizations and deaths from COVID.
Mr. Zients declined to set hard numbers around those goals, but other experts did.
“What we need to get to is 85% to 90% population immunity, and that’s going to be immunity both from vaccines and infections, before that really begins to have a substantial dampening effect on viral spread,” Ashish Jha, MD, dean of the Brown University School of Public Health, Providence, R.I., said on a call with reporters Sept. 9.
He said immunity needs to be that high because the Delta variant is so contagious.
Mandates are seen as the most effective way to increase immunity and do it quickly.
David Michaels, PhD, an epidemiologist and professor at George Washington University, Washington, says OSHA will have to work through a number of steps to develop the rule.
“OSHA will have to write a preamble explaining the standard, its justifications, its costs, and how it will be enforced,” says Dr. Michaels, who led OSHA for the Obama administration. After that, the rule will be reviewed by the White House. Then employers will have some time – typically 30 days – to comply.
In addition to drafting the standard, OSHA will oversee its enforcement.
Companies that refuse to follow the standard could be fined $13,600 per violation, Mr. Zients said.
Dr. Michaels said he doesn’t expect enforcement to be a big issue, and he said we’re likely to see the rule well before it is final.
“Most employers are law-abiding. When OSHA issues a standard, they try to meet whatever those requirements are, and generally that starts to happen when the rule is announced, even before it goes into effect,” he said.
The rule may face legal challenges as well. Several governors and state attorneys general, as well as the Republican National Committee, have promised lawsuits to stop the vaccine mandates.
Critics of the new mandates say they impinge on personal freedom and impose burdens on businesses.
But the president hit back at that notion Sept. 10.
“Look, I am so disappointed that, particularly some of the Republican governors, have been so cavalier with the health of these kids, so cavalier of the health of their communities,” President Biden told reporters.
“I don’t know of any scientist out there in this field who doesn’t think it makes considerable sense to do the six things I’ve suggested.”
Yet, others feel the new requirements didn’t go far enough.
“These are good steps in the right direction, but they’re not enough to get the job done,” said Leana Wen, MD, in an op-ed for The Washington Post.
Dr. Wen, an expert in public health, wondered why President Biden didn’t mandate vaccinations for plane and train travel. She was disappointed that children 12 and older weren’t required to be vaccinated, too.
“There are mandates for childhood immunizations in every state. The coronavirus vaccine should be no different,” she wrote.
Vaccines remain the cornerstone of U.S. plans to control the pandemic.
On Sept. 10, there was new research from the CDC and state health departments showing that the COVID-19 vaccines continue to be highly effective at preventing severe illness and death.
But the study also found that the vaccines became less effective in the United States after Delta became the dominant cause of infections here.
The study, which included more than 600,000 COVID-19 cases, analyzed breakthrough infections – cases where people got sick despite being fully vaccinated – in 13 jurisdictions in the United States between April 4 and July 17, 2021.
Epidemiologists compared breakthrough infections between two distinct points in time: Before and after the period when the Delta variant began causing most infections.
From April 4 to June 19, fully vaccinated people made up just 5% of cases, 7% of hospitalizations, and 8% of deaths. From June 20 to July 17, 18% of cases, 14% of hospitalizations, and 16% of deaths occurred in fully vaccinated people.
“After the week of June 20, 2021, when the SARS-CoV-2 Delta variant became predominant, the percentage of fully vaccinated persons among cases increased more than expected,” the study authors wrote.
Even after Delta swept the United States, fully vaccinated people were 5 times less likely to get a COVID-19 infection and more than 10 times less likely to be hospitalized or die from one.
“As we have shown in study after study, vaccination works,” CDC Director Rochelle Walensky, MD, said during the White House news briefing.
“We have the scientific tools we need to turn the corner on this pandemic. Vaccination works and will protect us from the severe complications of COVID-19,” she said.
A version of this article first appeared on WebMD.com.
Microbiome startups promise to improve your gut health, but is the science solid?
The gym owner in Sacramento, had always consumed large quantities of leafy greens. But the results from the test – which sequenced and analyzed the microbes in a pea-sized stool sample – recommended he steer clear of spinach, kale, and broccoli.
“Things I’ve been eating for the better part of 30 years,” said Mr. Jordan, 31. “And it worked.” Soon, his mild indigestion subsided. He recommended the product to his girlfriend.
She took the test in late February, when the company – which sells its “Gut Intelligence” test for $129 and a more extensive “Health Intelligence” test, which requires a blood sample, for $199 – began experiencing hiccups. Viome had promised results within 4 weeks once the sample arrived at a testing facility, but Mr. Jordan said his girlfriend has been waiting more than 5 months and has submitted fresh blood and stool samples – twice.
Other Viome customers have flocked to social media to complain about similar problems: stool samples lost in the mail, months-long waits with no communication from the company, samples being rejected because of shipping or lab-processing snafus. (I, too, have a stool sample lost in transit, which I mailed after a first vial was rejected because it “leaked.”) The company’s CEO, Naveen Jain, took to Facebook to apologize in late July.
Viome’s troubles provide a cautionary tale for consumers in the wild west of microbiome startups, which have been alternately hailed for health breakthroughs and indicted for fraud.
The nascent industry offers individualized diet regimens based on analyzing gut bacteria – collectively known as the gut microbiome. Consumers pay hundreds of dollars for tests not covered by insurance, hoping to get answers to health problems ranging from irritable bowel syndrome to obesity.
Venture capitalists pumped $1 billion into these kinds of startups from 2015 to 2020, according to Crunchbase, buoyed by promising research and consumers’ embrace of at-home testing. PitchBook has identified more than a dozen direct-to-consumer gut health providers.
But not all the startups are equal. Some are supported by peer-reviewed studies. Others are peddling murky science – and not just because poop samples are getting lost in the mail.
“A lot of companies are interested in the space, but they don’t have the research to show that it’s actually working,” said Christopher Lynch, acting director of the National Institutes of Health Office of Nutrition Research. “And the research is really expensive.”
With nearly $160 million in government funding, the NIH Common Fund’s Nutrition for Precision Health research program, expected to launch by early 2022, seeks to enroll 1 million people to study the interactions among diet, the microbiome, genes, metabolism and other factors.
The gut microbiome is a complex community of trillions of bacteria. Research over the past 15 years has determined that these microbes, both good and bad, are an integral part of human biology, and that altering a person’s gut microbes can fundamentally change their metabolism, immune function – and, potentially, cure diseases, explained Justin Sonnenburg, PhD, a microbiology and immunology associate professor at Stanford (Calif.) University.
Metagenomic sequencing, which identifies the unique set of bugs in someone’s gut (similar to what 23andMe does with its saliva test), has also improved dramatically, making the process cheaper for companies to reproduce.
“It’s seen as one of the exciting areas of precision health,” said Dr. Sonnenburg, who recently coauthored a study that found a fermented food diet increases microbiome diversity – which is considered positive – and reduces markers of inflammation. That includes foods like yogurt, kefir, and kimchi.
“The difficulty for the consumer is to differentiate which of these companies is based on solid science versus overreaching the current limits of the field,” he added via email. “And for those companies based on solid science, what are the limits of what they should be recommending?”
San Francisco–based uBiome, founded in 2012, was one of the first to offer fecal sample testing.
But as uBiome began marketing its tests as “clinical” – and seeking reimbursement from insurers for up to nearly $3,000 – its business tactics came under scrutiny. The company was raided by the FBI and later filed for bankruptcy. Earlier this year, its cofounders were indicted for defrauding insurers into paying for tests that “were not validated and not medically necessary” in order to please investors, the Department of Justice alleges.
But for Tim Spector, a professor of genetic epidemiology at King’s College London and cofounder of the startup Zoe, being associated with uBiome is insulting.
Zoe has spent more than 2 years conducting trials, which have included dietary assessments, standardized meals, testing glycemic responses and gut microbiome profiling on thousands of participants. In January, the findings were published in Nature Medicine.
The company offers a $354 test that requires a stool sample, a completed questionnaire, and then a blood sample after eating muffins designed to test blood fat and sugar levels. Customers can also opt in to a 2-week, continuous glucose monitoring test.
The results are run through the company’s algorithm to create a customized library of foods and meals – and how customers are likely to respond to those foods.
DayTwo, a Walnut Creek, Calif., company that recently raised $37 million to expand its precision nutrition program, focuses on people with prediabetes or diabetes. It sells to large employers – and, soon, to health insurance plans – rather than directly to consumers, charging “a few thousand dollars” per person, said Jan Berger, MD, chief clinical strategist.
Based on a decade of research, DayTwo has worked with nearly 75,000 people. It sends participants a testing kit and survey, and arranges for them to chat with a dietitian while their stool sample is processing. Then, when the results come in, it makes recommendations, Dr. Berger said.
“I can still eat two scoops of ice cream, but I need to add walnuts in it to regulate my blood sugar,” she offered as an example.
Viome says it has tested more than 200,000 customers and has published its methodology for analyzing stool samples, which is different from other gut health companies. But the paper does not address Viome’s larger claims of connecting the microbiome to dietary advice, and researcher Elisabeth Bik called the claims “far fetched” in a 2019 review of the preprint version.
Viome makes additional money by selling supplements, probiotics and prebiotics based on consumers’ test results. It has also rebranded as Viome Life Sciences, expanding into precision diagnostics and therapeutics, such as saliva tests to detect throat cancer. Meanwhile, its gut health program has been mired in logistical missteps.
One customer who posted on Facebook tracked her sample through the U.S. Postal Service as it boomeranged between Los Alamos, N.M., and Bothell, Wash., where it was supposed to be picked up. Another fought for a refund after waiting 6 weeks to hear her sample was not viable and learning a second attempt had expired after spending too long in transit. The company’s expected lab processing time jumped from 4 weeks in February, when Mr. Jordan said his girlfriend took her first test, to 6 in summer. (Three weeks after I mailed my second sample in July, it still hadn’t made it to the lab, so I called it quits and asked for a refund.)
In Mr. Jain’s July apology posted to the private Facebook group for Viome users, he said the company recently moved its lab from New Mexico to Washington state, close to its headquarters, which prompted a mail-forwarding fiasco. It bought new robotics that “refused to cooperate,” he wrote. “Many things didn’t go as planned during the move.”
Spokesperson Kendall Donohue said Viome has been working on the problems but laid much of the blame on the Postal Service.
She also said Viome has been notifying customers – even though many (including myself) had not been contacted.
It is Viome’s “top priority right now to ensure complete customer satisfaction, but unfortunately USPS needs to sort the issue internally for further action to be taken,” she said.
She also offered me a free “Health Intelligence” test. I declined.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The gym owner in Sacramento, had always consumed large quantities of leafy greens. But the results from the test – which sequenced and analyzed the microbes in a pea-sized stool sample – recommended he steer clear of spinach, kale, and broccoli.
“Things I’ve been eating for the better part of 30 years,” said Mr. Jordan, 31. “And it worked.” Soon, his mild indigestion subsided. He recommended the product to his girlfriend.
She took the test in late February, when the company – which sells its “Gut Intelligence” test for $129 and a more extensive “Health Intelligence” test, which requires a blood sample, for $199 – began experiencing hiccups. Viome had promised results within 4 weeks once the sample arrived at a testing facility, but Mr. Jordan said his girlfriend has been waiting more than 5 months and has submitted fresh blood and stool samples – twice.
Other Viome customers have flocked to social media to complain about similar problems: stool samples lost in the mail, months-long waits with no communication from the company, samples being rejected because of shipping or lab-processing snafus. (I, too, have a stool sample lost in transit, which I mailed after a first vial was rejected because it “leaked.”) The company’s CEO, Naveen Jain, took to Facebook to apologize in late July.
Viome’s troubles provide a cautionary tale for consumers in the wild west of microbiome startups, which have been alternately hailed for health breakthroughs and indicted for fraud.
The nascent industry offers individualized diet regimens based on analyzing gut bacteria – collectively known as the gut microbiome. Consumers pay hundreds of dollars for tests not covered by insurance, hoping to get answers to health problems ranging from irritable bowel syndrome to obesity.
Venture capitalists pumped $1 billion into these kinds of startups from 2015 to 2020, according to Crunchbase, buoyed by promising research and consumers’ embrace of at-home testing. PitchBook has identified more than a dozen direct-to-consumer gut health providers.
But not all the startups are equal. Some are supported by peer-reviewed studies. Others are peddling murky science – and not just because poop samples are getting lost in the mail.
“A lot of companies are interested in the space, but they don’t have the research to show that it’s actually working,” said Christopher Lynch, acting director of the National Institutes of Health Office of Nutrition Research. “And the research is really expensive.”
With nearly $160 million in government funding, the NIH Common Fund’s Nutrition for Precision Health research program, expected to launch by early 2022, seeks to enroll 1 million people to study the interactions among diet, the microbiome, genes, metabolism and other factors.
The gut microbiome is a complex community of trillions of bacteria. Research over the past 15 years has determined that these microbes, both good and bad, are an integral part of human biology, and that altering a person’s gut microbes can fundamentally change their metabolism, immune function – and, potentially, cure diseases, explained Justin Sonnenburg, PhD, a microbiology and immunology associate professor at Stanford (Calif.) University.
Metagenomic sequencing, which identifies the unique set of bugs in someone’s gut (similar to what 23andMe does with its saliva test), has also improved dramatically, making the process cheaper for companies to reproduce.
“It’s seen as one of the exciting areas of precision health,” said Dr. Sonnenburg, who recently coauthored a study that found a fermented food diet increases microbiome diversity – which is considered positive – and reduces markers of inflammation. That includes foods like yogurt, kefir, and kimchi.
“The difficulty for the consumer is to differentiate which of these companies is based on solid science versus overreaching the current limits of the field,” he added via email. “And for those companies based on solid science, what are the limits of what they should be recommending?”
San Francisco–based uBiome, founded in 2012, was one of the first to offer fecal sample testing.
But as uBiome began marketing its tests as “clinical” – and seeking reimbursement from insurers for up to nearly $3,000 – its business tactics came under scrutiny. The company was raided by the FBI and later filed for bankruptcy. Earlier this year, its cofounders were indicted for defrauding insurers into paying for tests that “were not validated and not medically necessary” in order to please investors, the Department of Justice alleges.
But for Tim Spector, a professor of genetic epidemiology at King’s College London and cofounder of the startup Zoe, being associated with uBiome is insulting.
Zoe has spent more than 2 years conducting trials, which have included dietary assessments, standardized meals, testing glycemic responses and gut microbiome profiling on thousands of participants. In January, the findings were published in Nature Medicine.
The company offers a $354 test that requires a stool sample, a completed questionnaire, and then a blood sample after eating muffins designed to test blood fat and sugar levels. Customers can also opt in to a 2-week, continuous glucose monitoring test.
The results are run through the company’s algorithm to create a customized library of foods and meals – and how customers are likely to respond to those foods.
DayTwo, a Walnut Creek, Calif., company that recently raised $37 million to expand its precision nutrition program, focuses on people with prediabetes or diabetes. It sells to large employers – and, soon, to health insurance plans – rather than directly to consumers, charging “a few thousand dollars” per person, said Jan Berger, MD, chief clinical strategist.
Based on a decade of research, DayTwo has worked with nearly 75,000 people. It sends participants a testing kit and survey, and arranges for them to chat with a dietitian while their stool sample is processing. Then, when the results come in, it makes recommendations, Dr. Berger said.
“I can still eat two scoops of ice cream, but I need to add walnuts in it to regulate my blood sugar,” she offered as an example.
Viome says it has tested more than 200,000 customers and has published its methodology for analyzing stool samples, which is different from other gut health companies. But the paper does not address Viome’s larger claims of connecting the microbiome to dietary advice, and researcher Elisabeth Bik called the claims “far fetched” in a 2019 review of the preprint version.
Viome makes additional money by selling supplements, probiotics and prebiotics based on consumers’ test results. It has also rebranded as Viome Life Sciences, expanding into precision diagnostics and therapeutics, such as saliva tests to detect throat cancer. Meanwhile, its gut health program has been mired in logistical missteps.
One customer who posted on Facebook tracked her sample through the U.S. Postal Service as it boomeranged between Los Alamos, N.M., and Bothell, Wash., where it was supposed to be picked up. Another fought for a refund after waiting 6 weeks to hear her sample was not viable and learning a second attempt had expired after spending too long in transit. The company’s expected lab processing time jumped from 4 weeks in February, when Mr. Jordan said his girlfriend took her first test, to 6 in summer. (Three weeks after I mailed my second sample in July, it still hadn’t made it to the lab, so I called it quits and asked for a refund.)
In Mr. Jain’s July apology posted to the private Facebook group for Viome users, he said the company recently moved its lab from New Mexico to Washington state, close to its headquarters, which prompted a mail-forwarding fiasco. It bought new robotics that “refused to cooperate,” he wrote. “Many things didn’t go as planned during the move.”
Spokesperson Kendall Donohue said Viome has been working on the problems but laid much of the blame on the Postal Service.
She also said Viome has been notifying customers – even though many (including myself) had not been contacted.
It is Viome’s “top priority right now to ensure complete customer satisfaction, but unfortunately USPS needs to sort the issue internally for further action to be taken,” she said.
She also offered me a free “Health Intelligence” test. I declined.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The gym owner in Sacramento, had always consumed large quantities of leafy greens. But the results from the test – which sequenced and analyzed the microbes in a pea-sized stool sample – recommended he steer clear of spinach, kale, and broccoli.
“Things I’ve been eating for the better part of 30 years,” said Mr. Jordan, 31. “And it worked.” Soon, his mild indigestion subsided. He recommended the product to his girlfriend.
She took the test in late February, when the company – which sells its “Gut Intelligence” test for $129 and a more extensive “Health Intelligence” test, which requires a blood sample, for $199 – began experiencing hiccups. Viome had promised results within 4 weeks once the sample arrived at a testing facility, but Mr. Jordan said his girlfriend has been waiting more than 5 months and has submitted fresh blood and stool samples – twice.
Other Viome customers have flocked to social media to complain about similar problems: stool samples lost in the mail, months-long waits with no communication from the company, samples being rejected because of shipping or lab-processing snafus. (I, too, have a stool sample lost in transit, which I mailed after a first vial was rejected because it “leaked.”) The company’s CEO, Naveen Jain, took to Facebook to apologize in late July.
Viome’s troubles provide a cautionary tale for consumers in the wild west of microbiome startups, which have been alternately hailed for health breakthroughs and indicted for fraud.
The nascent industry offers individualized diet regimens based on analyzing gut bacteria – collectively known as the gut microbiome. Consumers pay hundreds of dollars for tests not covered by insurance, hoping to get answers to health problems ranging from irritable bowel syndrome to obesity.
Venture capitalists pumped $1 billion into these kinds of startups from 2015 to 2020, according to Crunchbase, buoyed by promising research and consumers’ embrace of at-home testing. PitchBook has identified more than a dozen direct-to-consumer gut health providers.
But not all the startups are equal. Some are supported by peer-reviewed studies. Others are peddling murky science – and not just because poop samples are getting lost in the mail.
“A lot of companies are interested in the space, but they don’t have the research to show that it’s actually working,” said Christopher Lynch, acting director of the National Institutes of Health Office of Nutrition Research. “And the research is really expensive.”
With nearly $160 million in government funding, the NIH Common Fund’s Nutrition for Precision Health research program, expected to launch by early 2022, seeks to enroll 1 million people to study the interactions among diet, the microbiome, genes, metabolism and other factors.
The gut microbiome is a complex community of trillions of bacteria. Research over the past 15 years has determined that these microbes, both good and bad, are an integral part of human biology, and that altering a person’s gut microbes can fundamentally change their metabolism, immune function – and, potentially, cure diseases, explained Justin Sonnenburg, PhD, a microbiology and immunology associate professor at Stanford (Calif.) University.
Metagenomic sequencing, which identifies the unique set of bugs in someone’s gut (similar to what 23andMe does with its saliva test), has also improved dramatically, making the process cheaper for companies to reproduce.
“It’s seen as one of the exciting areas of precision health,” said Dr. Sonnenburg, who recently coauthored a study that found a fermented food diet increases microbiome diversity – which is considered positive – and reduces markers of inflammation. That includes foods like yogurt, kefir, and kimchi.
“The difficulty for the consumer is to differentiate which of these companies is based on solid science versus overreaching the current limits of the field,” he added via email. “And for those companies based on solid science, what are the limits of what they should be recommending?”
San Francisco–based uBiome, founded in 2012, was one of the first to offer fecal sample testing.
But as uBiome began marketing its tests as “clinical” – and seeking reimbursement from insurers for up to nearly $3,000 – its business tactics came under scrutiny. The company was raided by the FBI and later filed for bankruptcy. Earlier this year, its cofounders were indicted for defrauding insurers into paying for tests that “were not validated and not medically necessary” in order to please investors, the Department of Justice alleges.
But for Tim Spector, a professor of genetic epidemiology at King’s College London and cofounder of the startup Zoe, being associated with uBiome is insulting.
Zoe has spent more than 2 years conducting trials, which have included dietary assessments, standardized meals, testing glycemic responses and gut microbiome profiling on thousands of participants. In January, the findings were published in Nature Medicine.
The company offers a $354 test that requires a stool sample, a completed questionnaire, and then a blood sample after eating muffins designed to test blood fat and sugar levels. Customers can also opt in to a 2-week, continuous glucose monitoring test.
The results are run through the company’s algorithm to create a customized library of foods and meals – and how customers are likely to respond to those foods.
DayTwo, a Walnut Creek, Calif., company that recently raised $37 million to expand its precision nutrition program, focuses on people with prediabetes or diabetes. It sells to large employers – and, soon, to health insurance plans – rather than directly to consumers, charging “a few thousand dollars” per person, said Jan Berger, MD, chief clinical strategist.
Based on a decade of research, DayTwo has worked with nearly 75,000 people. It sends participants a testing kit and survey, and arranges for them to chat with a dietitian while their stool sample is processing. Then, when the results come in, it makes recommendations, Dr. Berger said.
“I can still eat two scoops of ice cream, but I need to add walnuts in it to regulate my blood sugar,” she offered as an example.
Viome says it has tested more than 200,000 customers and has published its methodology for analyzing stool samples, which is different from other gut health companies. But the paper does not address Viome’s larger claims of connecting the microbiome to dietary advice, and researcher Elisabeth Bik called the claims “far fetched” in a 2019 review of the preprint version.
Viome makes additional money by selling supplements, probiotics and prebiotics based on consumers’ test results. It has also rebranded as Viome Life Sciences, expanding into precision diagnostics and therapeutics, such as saliva tests to detect throat cancer. Meanwhile, its gut health program has been mired in logistical missteps.
One customer who posted on Facebook tracked her sample through the U.S. Postal Service as it boomeranged between Los Alamos, N.M., and Bothell, Wash., where it was supposed to be picked up. Another fought for a refund after waiting 6 weeks to hear her sample was not viable and learning a second attempt had expired after spending too long in transit. The company’s expected lab processing time jumped from 4 weeks in February, when Mr. Jordan said his girlfriend took her first test, to 6 in summer. (Three weeks after I mailed my second sample in July, it still hadn’t made it to the lab, so I called it quits and asked for a refund.)
In Mr. Jain’s July apology posted to the private Facebook group for Viome users, he said the company recently moved its lab from New Mexico to Washington state, close to its headquarters, which prompted a mail-forwarding fiasco. It bought new robotics that “refused to cooperate,” he wrote. “Many things didn’t go as planned during the move.”
Spokesperson Kendall Donohue said Viome has been working on the problems but laid much of the blame on the Postal Service.
She also said Viome has been notifying customers – even though many (including myself) had not been contacted.
It is Viome’s “top priority right now to ensure complete customer satisfaction, but unfortunately USPS needs to sort the issue internally for further action to be taken,” she said.
She also offered me a free “Health Intelligence” test. I declined.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
New guidance on preventing cutaneous SCC in solid organ transplant patients
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.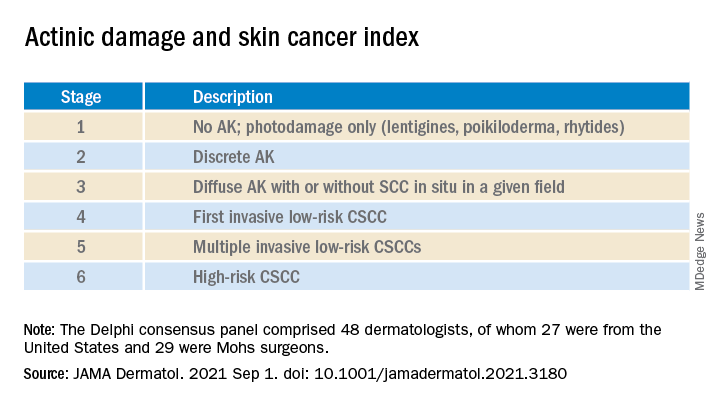
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.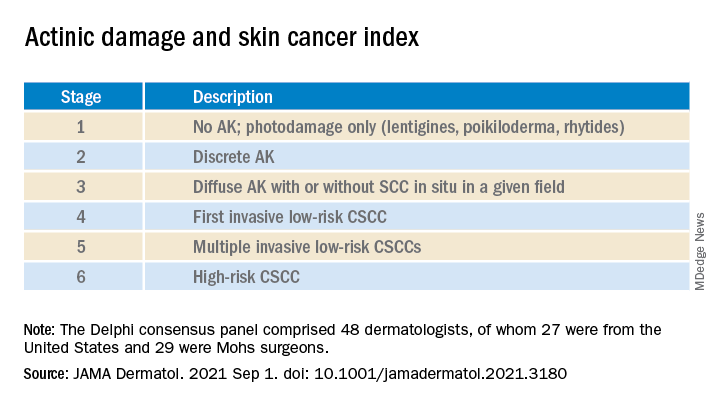
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
An expert panel of 48 dermatologists from 13 countries has developed recommendations to guide efforts aimed at preventing cutaneous squamous cell carcinoma (CSCC) in solid organ transplant recipients.
The recommendations were published online on Sept. 1 in JAMA Dermatology.
Because of lifelong immunosuppression, solid organ transplant recipients (SOTRs) have a risk of CSCC that is 20-200 times higher than in the general population and despite a growing literature on prevention of CSCC in these patients, uncertainty remains regarding best practices for various patient scenarios.
Paul Massey, MD, MPH, of the department of dermatology, Brigham and Women’s Hospital, Boston, and colleagues used a Delphi process to identify consensus-based medical management recommendations for prevention of CSCC in SOTRs.
The survey design was guided by a novel actinic damage and skin cancer index (AD-SCI) made up of six ordinal stages corresponding to an increasing burden of actinic damage and CSCC.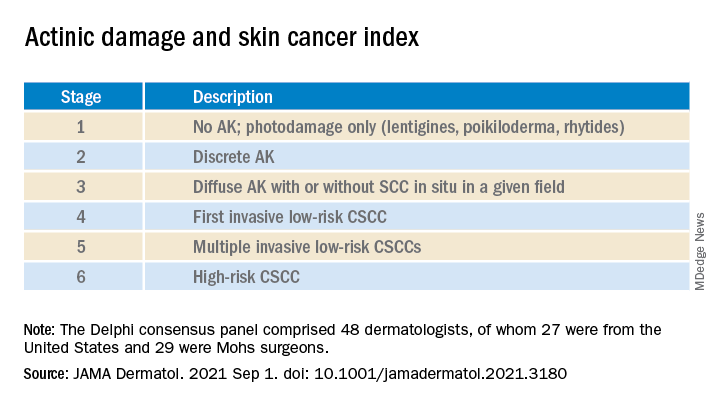
The AD-SCI stage-based recommendations were established when consensus was reached (80% or higher concordance) or near consensus was reached (70%-80% concordance) among panel members.
For five of the six AD-SCI stages, the panel was able to make recommendations. Key recommendations include:
- Cryotherapy for scattered AK.
- Field therapy for AK when grouped in one site, unless AKs are thick, in which case field therapy and cryotherapy are recommended.
- Combination lesion-directed and field therapy with fluorouracil for field cancerized skin.
- Initiation of acitretin therapy and discussion of immunosuppression reduction or modification for patients who develop multiple CSCCs at a high rate (10 per year) or develop high-risk CSCC (defined by a tumor with roughly ≥20% risk of nodal metastasis). The panel did not make a recommendation as to the best immunosuppression modification strategy to pursue.
Lingering questions
The panel was unable to reach consensus on a recommendation for SOTRs with a first low-risk CSCC, reflecting “clinical equipoise” in this situation and the need for further study in this clinical scenario, they say.
The panel did not make a recommendation for use of nicotinamide or capecitabine in any of the six stages, which is “notable,” they acknowledge, given results of a double-blind randomized controlled trial in immunocompetent patients demonstrating benefit in preventing AKs and CSCCs, as reported previously.
Nearly three-quarters of the panel felt that a lack of efficacy data specifically for the SOTR population limited their use of nicotinamide. “Given the low cost, high safety, and demonstration of CSCC reduction in non-SOTRs, nicotinamide administration may be an area for further consideration and expanded study,” the panel wrote.
As for capecitabine, the panel notes that case series in SOTRs have found efficacy for chemoprevention, but randomized controlled studies are lacking. More than half of the panel noted that they did not have routine access to capecitabine in their practice.
The panel recommended routine skin surveillance and sunscreen use for all patients.
“These recommendations reflect consensus among expert transplant dermatologists and the incorporation of limited and sometimes contradictory evidence into real-world clinical experience across a range of CSCC disease severity,” the panel said.
“Areas of consensus may aid physicians in establishing best practices regarding prevention of CSCC in SOTRs in the setting of limited high level of evidence data in this population,” they added.
This research had no specific funding. Author disclosures included serving as a consultant to Regeneron, Sanofi, and receiving research funding from Castle Biosciences, Regeneron, Novartis, and Genentech. A complete list of disclosures for panel members is available with the original article.
Even those who just test positive at more risk for long COVID: CDC
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term symptoms, like those linked with COVID-19, were common in people who had even just a single positive test, new Centers for Disease Control and Prevention data show.
The data show that symptoms in this group – including fatigue, cough, and headache – tended to last for more than a month.
Frequency of symptoms in people with a positive test was 1.5 times higher, compared with people whose tests had always been negative, according to the research published in the CDC’s latest Morbidity and Mortality Weekly Report.
Lead author Valentine Wanga, PhD, with the CDC’s COVID-19 response team, and colleagues conducted a non–probability-based internet panel survey of about 6,000 U.S. adults to assess long-term symptoms often associated with COVID-19 among those who had ever tested positive or always tested negative for COVID-19 between January 2020 and April 2021.
William Schaffner, MD, an infectious disease expert at Vanderbilt University, Nashville, Tenn., said in an interview that this research “establishes more securely than before that you don’t have to be hospitalized with COVID in order to develop long COVID symptoms.”
That’s better known among infectious disease experts, he said, but added that “this survey really gives a firm database for that.”
Study results
The study’s results showed that, compared with respondents who had a negative test result, those who received a positive result reported a significantly higher prevalence of any long-term symptom (65.9% vs. 42.9%), fatigue (22.5% vs. 12.0%), change in sense of smell or taste (17.3% vs. 1.7%), shortness of breath (15.5% vs. 5.2%), cough (14.5% vs. 4.9%), and headache (13.8% vs. 9.9%).
More people who had a positive test result (76.2%) reported persistence for more than a month of at least one initially occurring symptom, compared with those whose test results were always negative (69.6%).
The numbers are further proof, Dr. Schaffner said, that COVID not only will be an acute stressor on the health care system but patients with long COVID will need help with managing care for the long term.
“We still don’t know what the COVID virus does that results in these long COVID symptoms,” he said. Vanderbilt and many other institutions have developed “long COVID” centers as a testament to how important the problem is.
Long COVID symptoms are not well understood and most studies have looked at the effects from patients who had been hospitalized with COVID-19.
In this survey, respondents self-reported whether they had ever had a positive SARS-CoV-2 test result (698), always received a negative test result (2,437), or never were tested for SARS-CoV-2 (2,750).
Compared with those who always tested negative, a larger proportion of those who tested positive (28.7% vs. 15.7%) reported believing that receiving a COVID-19 vaccine made their long-term symptoms better. No difference was found in reported beliefs that a vaccine made long-term symptoms worse.
Dr. Schaffner said he found that survey result interesting, but said that is not backed up by current data and would need further study.
“I would treat that with great caution,” he said. “I’m not dismissing it, but you can’t take that at face value. All of us who get sick and those of us who care for people who are sick – if there’s an intervention, we all hope for the best. We’re being optimistic. It’s when you do a randomized, double-blind, placebo-controlled study that you can find out whether your instincts or hopes were correct.”
The authors said that findings can inform public health preparedness, help guide care for people with post-COVID conditions, and help make the case for vaccines.
The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hair regrowth stimulated by microneedle patch in preclinical study
Those who are unhappy about losing their hair might be interested to hear about a new approach where scientists use mechanical stimulation to promote hair regrowth.
Currently, Food and Drug Administration–approved drugs for hair loss include minoxidil (Rogaine) and finasteride (Propecia). But there are side effects, and the treatments only work when continuously used for an extended time.
Some people may opt instead to have hair follicle transplants, but study coauthor Fangyuan Li, PhD, from the College of Pharmaceutical Sciences at Zhejiang University in Hangzhou, China, explains, the surgery is painful and not always successful because it depends a lot on the quality of donor hair follicles, which can vary.
Seeking to develop a new nonsurgical option, the scientists, led by Jianqing Gao, vice dean of the College of Pharmaceutical Sciences at Zhejiang University, designed a dissolvable microneedle patch to deliver treatment near hair roots beneath the skin.
Male- or female-pattern baldness can be permanent when there aren’t enough blood vessels surrounding hair follicles to deliver nutrients and other essential molecules. A buildup of reactive oxygen in the scalp can prompt the death of cells that would otherwise grow new hair.
In a previous investigation, the researchers found that nanoparticles containing cerium, a silvery-white metal, can mimic the enzymes inside the body that can help ease oxidative stress.
The scientists coated cerium nanoparticles with a biodegradable compound. Then they made the microneedle patch by pouring a mixture of hyaluronic acid with cerium-containing nanoparticles into a mold.
The small needles don’t hurt when applied, Dr. Li said, as they deliver treatment to a region under the skin with no pain receptors.
The researchers tested control patches and the cerium-containing ones on male mice with bald spots created by a hair-removal cream. Both applications stimulated new blood vessels to form around the mice hair follicles. But those treated with the nanoparticle patch showed faster signs of hair recuperation at the root.
The mice also had fewer oxidative stress compounds in their skin. Microneedle patch use resulted in faster hair regrowth, compared with a cream-based treatment, and could be applied less frequently.
And though the idea is not yet ready to be tried on people, it represents an inventive step forward in addressing a common problem.
A version of this article first appeared on WebMD.com.
Those who are unhappy about losing their hair might be interested to hear about a new approach where scientists use mechanical stimulation to promote hair regrowth.
Currently, Food and Drug Administration–approved drugs for hair loss include minoxidil (Rogaine) and finasteride (Propecia). But there are side effects, and the treatments only work when continuously used for an extended time.
Some people may opt instead to have hair follicle transplants, but study coauthor Fangyuan Li, PhD, from the College of Pharmaceutical Sciences at Zhejiang University in Hangzhou, China, explains, the surgery is painful and not always successful because it depends a lot on the quality of donor hair follicles, which can vary.
Seeking to develop a new nonsurgical option, the scientists, led by Jianqing Gao, vice dean of the College of Pharmaceutical Sciences at Zhejiang University, designed a dissolvable microneedle patch to deliver treatment near hair roots beneath the skin.
Male- or female-pattern baldness can be permanent when there aren’t enough blood vessels surrounding hair follicles to deliver nutrients and other essential molecules. A buildup of reactive oxygen in the scalp can prompt the death of cells that would otherwise grow new hair.
In a previous investigation, the researchers found that nanoparticles containing cerium, a silvery-white metal, can mimic the enzymes inside the body that can help ease oxidative stress.
The scientists coated cerium nanoparticles with a biodegradable compound. Then they made the microneedle patch by pouring a mixture of hyaluronic acid with cerium-containing nanoparticles into a mold.
The small needles don’t hurt when applied, Dr. Li said, as they deliver treatment to a region under the skin with no pain receptors.
The researchers tested control patches and the cerium-containing ones on male mice with bald spots created by a hair-removal cream. Both applications stimulated new blood vessels to form around the mice hair follicles. But those treated with the nanoparticle patch showed faster signs of hair recuperation at the root.
The mice also had fewer oxidative stress compounds in their skin. Microneedle patch use resulted in faster hair regrowth, compared with a cream-based treatment, and could be applied less frequently.
And though the idea is not yet ready to be tried on people, it represents an inventive step forward in addressing a common problem.
A version of this article first appeared on WebMD.com.
Those who are unhappy about losing their hair might be interested to hear about a new approach where scientists use mechanical stimulation to promote hair regrowth.
Currently, Food and Drug Administration–approved drugs for hair loss include minoxidil (Rogaine) and finasteride (Propecia). But there are side effects, and the treatments only work when continuously used for an extended time.
Some people may opt instead to have hair follicle transplants, but study coauthor Fangyuan Li, PhD, from the College of Pharmaceutical Sciences at Zhejiang University in Hangzhou, China, explains, the surgery is painful and not always successful because it depends a lot on the quality of donor hair follicles, which can vary.
Seeking to develop a new nonsurgical option, the scientists, led by Jianqing Gao, vice dean of the College of Pharmaceutical Sciences at Zhejiang University, designed a dissolvable microneedle patch to deliver treatment near hair roots beneath the skin.
Male- or female-pattern baldness can be permanent when there aren’t enough blood vessels surrounding hair follicles to deliver nutrients and other essential molecules. A buildup of reactive oxygen in the scalp can prompt the death of cells that would otherwise grow new hair.
In a previous investigation, the researchers found that nanoparticles containing cerium, a silvery-white metal, can mimic the enzymes inside the body that can help ease oxidative stress.
The scientists coated cerium nanoparticles with a biodegradable compound. Then they made the microneedle patch by pouring a mixture of hyaluronic acid with cerium-containing nanoparticles into a mold.
The small needles don’t hurt when applied, Dr. Li said, as they deliver treatment to a region under the skin with no pain receptors.
The researchers tested control patches and the cerium-containing ones on male mice with bald spots created by a hair-removal cream. Both applications stimulated new blood vessels to form around the mice hair follicles. But those treated with the nanoparticle patch showed faster signs of hair recuperation at the root.
The mice also had fewer oxidative stress compounds in their skin. Microneedle patch use resulted in faster hair regrowth, compared with a cream-based treatment, and could be applied less frequently.
And though the idea is not yet ready to be tried on people, it represents an inventive step forward in addressing a common problem.
A version of this article first appeared on WebMD.com.
Atopic dermatitis subtype worsens into midlife, predicting poor health
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
giving reason to observe patients beyond the pediatric stage, according to a cohort study of more than 30,000 patients.
Early-life environmental factors, such as tobacco smoke exposure, were not reliable predictors of increasing AD into mid-adulthood, suggesting that a patient’s contemporaneous environment may impact disease course throughout life, reported lead author Katrina Abuabara, MD, associate professor of dermatology at the University of California, San Francisco, and colleagues.
“There is a lack of studies that prospectively examine the course of atopic eczema beyond adolescence/early adulthood, and a more comprehensive understanding of disease activity across the life span is needed,” the investigators wrote in JAMA Dermatology. “Data on long-term disease course may offer insight into mechanisms for disease onset and persistence, are important when counseling patients, and would establish baseline trajectories for future studies of whether new treatments can modify disease course and development of comorbidities.”
The present study included 30,905 patients from two population-based birth cohorts: the 1958 National Childhood Development Study (NCDS) and the 1970 British Cohort Study (BCS70). Follow-up data were collected between 1958 and 2016 via nine waves of standardized questionnaires, and subtypes of atopic eczema patterns were identified “based on parent-reported or self-reported atopic eczema period prevalence.”
This measure “was previously shown to coincide with standardized clinical examinations among children in the NCDS, and a similar questionnaire demonstrated high sensitivity and specificity for physician-diagnosed atopic eczema in U.S. populations,” the investigators noted.
Latent class analysis identified four disease subtypes based on probability of reporting prevalent AD into midlife: low (88%-91%), decreasing (4%), increasing (2%-6%), and persistently high (2%-3%) probability.
Next, the investigators looked for associations between these subtypes and established early-life risk factors, such as history of breastfeeding and childhood smoke exposure. None of the childhood environmental factors differentiated between high versus decreasing disease in adulthood, or increasing versus decreasing disease in adulthood. In contrast, female sex predicted the high versus decreasing adult subtype (odds ratio, 1.99; 95% confidence interval, 1.66-2.38), and the increasing versus decreasing adult subtype (OR, 1.99; 95% CI, 1.69-2.35).
These findings suggest that “disease trajectory is modifiable and may be influenced by environmental factors throughout life,” the investigators wrote.
Further analysis uncovered associations between adult AD subtypes and other health outcomes. For example, compared with adults in the low probability group, those in the high probability group were significantly more likely to report rhinitis (OR, 2.70; 95% CI, 2.24-3.26) and asthma (OR, 3.45; 95% CI, 2.82-4.21). Adults with the increasing subtype also had elevated rates of asthma and rhinitis, along with worse self-reported mental health at age 42 (OR, 1.45; 95% CI, 1.23-1.72) and poor general health at age 46/50 (OR, 1.29; 95% CI, 1.09-1.53).
“When extending the window of observation beyond childhood, clear subtypes of atopic eczema based on patterns of disease activity emerged,” the investigators concluded. “In particular, a newly identified subtype with increasing probability of activity in adulthood warrants additional attention given associations with poor self-reported physical and mental health in midlife.”
Commenting on these results, Robert Sidbury, MD, professor of dermatology at the University of Washington, Seattle, said that this is an “important study” because it adds to our understanding of natural disease course over time.
This knowledge, as a pediatric dermatologist, will help Dr. Sidbury answer one of the most common questions he hears from parents: When is it going to stop?
“Trying to put a little bit more evidence-based heft behind the answer ... is really important,” he said in an interview.
Based on available data, up to 10% of children with AD may have disease activity into adulthood, according to Dr. Sidbury, who is also chief of dermatology at Seattle Children’s Hospital.
“I would hazard to guess that most of those adults who have atopic dermatitis – at least the ones who had it in childhood – were told that they would grow out of it,” he said. “And so I think awareness is important – that [resolution with age] does not always happen.”
The findings also support the possibility that AD is a systemic disease, and that underlying immune dysregulation may be linked with serious health consequences later in life, Dr. Sidbury said, noting that “the stakes get higher and higher when you start speculating in that way.”
According to Dr. Sidbury, the reported link between childhood AD and poor midlife health raises questions about how modifiable the disease course may be, particularly in response to earlier intervention with emerging AD medications, which “seem to be much more effective and potent.”
“Will the advent of these medications and their adoption and use in treatment perhaps have a significant impact, not just on the prevention of atopic dermatitis itself, but maybe other comorbidities?” he asked.
For the time being, this question remains unanswered.
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Wellcome Trust. Dr. Abuabara received grants from the National Institutes of Health during the study, as well as personal fees from Target RWE and Pfizer outside of this study. One author reported receiving NIH grants during the study, another reported receiving grants from the Wellcome Trust and the Innovative Medicine Initiative Horizon 2020 (BIOMAP project) during the study; there were no other disclosures. Dr. Sidbury disclosed relationships with Galderma, Regeneron, and Pfizer.
FROM JAMA DERMATOLOGY
Sweeping new vaccine mandates will impact most U.S. workers
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
, including sweeping vaccine mandates that will affect 100 million American workers, nearly two-thirds of the country’s workforce.
“As your president, I’m announcing tonight a new plan to get more Americans vaccinated to combat those blocking public health,” he said Sept. 9.
As part of a six-part plan unveiled in a speech from the State Dining Room of the White House, President Biden said he would require vaccinations for nearly 4 million federal workers and the employees of companies that contract with the federal government.
He has also directed the Occupational Safety and Health Administration to develop a rule that will require large employers -- those with at least 100 employees -- to ensure their workers are vaccinated or tested weekly.
Nearly 17 million health care workers will face new vaccine mandates as part of the conditions of participation in the Medicare and Medicaid programs.
President Biden said the federal government will require staff at federally funded Head Start programs and schools to be vaccinated. He’s also calling on all states to mandate vaccines for teachers.
“A distinct minority of Americans, supported by a distinct minority of elected officials, are keeping us from turning the corner,” PresidentBiden said. “These pandemic politics, as I refer to them, are making people sick, causing unvaccinated people to die.”
One public health official said he was glad to see the president’s bold action.
“What I saw today was the federal government trying to use its powers to create greater safety in the American population,” said Ashish K. Jha, MD, dean of the school of public health at Brown University, Providence, R.I., in a call with reporters after the speech.
National Nurses United, the largest union of registered nurses in the United States, issued a statement in support of President Biden’s new vaccination requirements, but pushed back on his language.
“…as advocates for public health, registered nurses want to be extremely clear: There is no such thing as a pandemic of only the unvaccinated. The science of epidemiology tells us there is just one deadly, global pandemic that has not yet ended, and we are all in it together. To get out of it, we must act together. All of us,” the statement says.
A host of other professional groups, including the American Medical Association and the Association of State and Territorial Health Officials, also issued statements of support for President Biden’s plan.
But the plan was not well received by all.
“I will pursue every legal option available to the state of Georgia to stop this blatantly unlawful overreach by the Biden Administration,” said Georgia Governor Brian Kemp, a Republican, in a Tweet.
The National Council for Occupational Safety and Health called the plan “a missed opportunity” because it failed to include workplace protections for essential workers such as grocery, postal, and transit workers.
“Social distancing, improved ventilation, shift rotation, and protective equipment to reduce exposure are important components of an overall plan to reduce risk and stop the virus. These tools are missing from the new steps President Biden announced today,” said Jessica Martinez, co-executive director of the group.
In addition to the new vaccination requirements, President Biden said extra doses would be on the way for people who have already been fully vaccinated in order to protect against waning immunity, starting on Sept. 20. But he noted that those plans would be contingent on the Food and Drug Administration’s approval for third doses and the Centers for Disease Control and Prevention’s recommendation of the shots.
President Biden pledged to use the Defense Production Act to ramp up production of at-home tests, which have been selling out across the nation as the Delta variant spreads.
He also announced plans to expand access to COVID-19 testing, including offering testing for free at thousands of pharmacies nationwide and getting major retailers to sell at-home COVID-19 tests at cost.
The BinaxNow test kit, which currently retails for $23.99, will now cost about $15 for two tests at Kroger, Amazon, and Walmart, according to the White House. Food banks and community health centers will get free tests, too.
He called on states to set up COVID-19 testing programs at all schools.
Jha said that in his view, the big, game-changing news out of the president’s speech was the expansion of testing.
“Our country has failed to deploy tests in a way that can really bring this pandemic under control,” Jha said. “There are plenty of reasons, data, experience to indicate that if these were widely available, it would make a dramatic difference in reducing infection numbers across our country.”.
Dr. Jha said the private market had not worked effectively to make testing more widely available, so it was “absolutely a requirement of the federal government to step in and make testing more widely available,” he said.
President Biden also announced new economic stimulus programs, saying he’s expanding loan programs to small businesses and streamlining the loan forgiveness process.
President Biden said he’s boosting help for overburdened hospitals, doubling the number of federal surge response teams sent to hard-hit areas to reduce the strain on local health care workers. He said he would increase the pace of antibody treatments to states by 50%.
“We made so much progress during the past 7 months of this pandemic. Even so, we remain at a critical moment, a critical time,” he said. “We have the tools. Now, we just have to finish the job with truth, with science, with confidence and together as one nation.”
A version of this article first appeared on WebMD.com.
FDA inaction on hair loss drug’s suicide, depression, erectile dysfunction risk sparks lawsuit
Consumer advocacy group 4 years ago.
The September 2017 petition requested that the FDA take the popular hair-loss drug (1 mg finasteride, Propecia) off the market because of evidence of serious risk of patient injury, including depression and suicidal ideation.
As an alternative, PFSF requested that the FDA require the drug’s manufacturers revise the safety information on the labeling and add boxed warnings to disclose the potential for side effects, another of which is erectile dysfunction.
Public Citizen points to a recent analysis of the VigiBase global database, which tracks adverse effects from global pharmacovigilance agencies, lists 356 reports of suicidality and 2,926 reports of psychological adverse events in finasteride users. Yet, 4 years after submitting the petition, the FDA has neither granted nor denied it.
The lawsuit claims that FDA has acted unlawfully in failing to act on PFSF’s petition, and further cites “88 cases of completed suicide associated with finasteride use” per data from the VigiBase database.
“On the same day that PFSF submitted the petition, FDA’s docket management division acknowledged receipt and assigned the petition a docket number,” Michael Kirkpatrick, the Public Citizen attorney serving as lead counsel for PFSF, told this news organization.
Yet, to date, “there has been no substantive response to the petition. The lawsuit filed today seeks to force FDA to issue a decision on PFSF’s petition,” Mr. Kirkpatrick said.
“The FDA needs to act in a timely way to protect the public from the risks associated with use of Propecia. The FDA’s failure to act exposes consumers to potentially life-threatening harm,” he added in a statement.
The complaint filed today by Public Citizen in the U.S. District Court for the District of Columbia is available online.
This news organization reached out to the FDA for comment but did not receive a response by press time.
A version of this article first appeared on Medscape.com.
Consumer advocacy group 4 years ago.
The September 2017 petition requested that the FDA take the popular hair-loss drug (1 mg finasteride, Propecia) off the market because of evidence of serious risk of patient injury, including depression and suicidal ideation.
As an alternative, PFSF requested that the FDA require the drug’s manufacturers revise the safety information on the labeling and add boxed warnings to disclose the potential for side effects, another of which is erectile dysfunction.
Public Citizen points to a recent analysis of the VigiBase global database, which tracks adverse effects from global pharmacovigilance agencies, lists 356 reports of suicidality and 2,926 reports of psychological adverse events in finasteride users. Yet, 4 years after submitting the petition, the FDA has neither granted nor denied it.
The lawsuit claims that FDA has acted unlawfully in failing to act on PFSF’s petition, and further cites “88 cases of completed suicide associated with finasteride use” per data from the VigiBase database.
“On the same day that PFSF submitted the petition, FDA’s docket management division acknowledged receipt and assigned the petition a docket number,” Michael Kirkpatrick, the Public Citizen attorney serving as lead counsel for PFSF, told this news organization.
Yet, to date, “there has been no substantive response to the petition. The lawsuit filed today seeks to force FDA to issue a decision on PFSF’s petition,” Mr. Kirkpatrick said.
“The FDA needs to act in a timely way to protect the public from the risks associated with use of Propecia. The FDA’s failure to act exposes consumers to potentially life-threatening harm,” he added in a statement.
The complaint filed today by Public Citizen in the U.S. District Court for the District of Columbia is available online.
This news organization reached out to the FDA for comment but did not receive a response by press time.
A version of this article first appeared on Medscape.com.
Consumer advocacy group 4 years ago.
The September 2017 petition requested that the FDA take the popular hair-loss drug (1 mg finasteride, Propecia) off the market because of evidence of serious risk of patient injury, including depression and suicidal ideation.
As an alternative, PFSF requested that the FDA require the drug’s manufacturers revise the safety information on the labeling and add boxed warnings to disclose the potential for side effects, another of which is erectile dysfunction.
Public Citizen points to a recent analysis of the VigiBase global database, which tracks adverse effects from global pharmacovigilance agencies, lists 356 reports of suicidality and 2,926 reports of psychological adverse events in finasteride users. Yet, 4 years after submitting the petition, the FDA has neither granted nor denied it.
The lawsuit claims that FDA has acted unlawfully in failing to act on PFSF’s petition, and further cites “88 cases of completed suicide associated with finasteride use” per data from the VigiBase database.
“On the same day that PFSF submitted the petition, FDA’s docket management division acknowledged receipt and assigned the petition a docket number,” Michael Kirkpatrick, the Public Citizen attorney serving as lead counsel for PFSF, told this news organization.
Yet, to date, “there has been no substantive response to the petition. The lawsuit filed today seeks to force FDA to issue a decision on PFSF’s petition,” Mr. Kirkpatrick said.
“The FDA needs to act in a timely way to protect the public from the risks associated with use of Propecia. The FDA’s failure to act exposes consumers to potentially life-threatening harm,” he added in a statement.
The complaint filed today by Public Citizen in the U.S. District Court for the District of Columbia is available online.
This news organization reached out to the FDA for comment but did not receive a response by press time.
A version of this article first appeared on Medscape.com.
Elderly mice receive the gift of warmth
Steal from the warm, give to the cold
If there’s one constant in life other than taxes, it’s elderly people moving to Florida. The Sunshine State’s reputation as a giant retirement home needs no elaboration, but why do senior citizens gravitate there? Well, many reasons, but a big one is that, the older you get, the more susceptible and sensitive you are to the cold. And now, according to a new study, we may have identified a culprit.
Researchers from Yale University examined a group of mice and found that the older ones lacked ICL2 cells in their fatty tissue. These cells, at least in younger mice, help restore body heat when exposed to cold temperatures. Lacking these cells meant that older mice had a limited ability to burn their fat and raise their temperature in response to cold.
Well, job done, all we need to do now is stimulate production of ICL2 cells in elderly people, and they’ll be able to go outside in 80-degree weather without a sweater again. Except there’s a problem. In a cruel twist of fate, when the elderly mice were given a molecule to boost ICL2 cell production, they actually became less tolerant of the cold than at baseline. Oops.
The scientists didn’t give up though, and gave their elderly mice ICL2 cells from young mice. This finally did the trick, though we have to admit, if that treatment does eventually scale up to humans, the prospect of a bunch of senior citizens taking ICL2 cells from young people to stay warm does sound a bit like a bad vampire movie premise. “I vant to suck your immune cell group 2 innate lymphoid cells!” Not the most pithy catch phrase in the world.
Grocery store tapping your subconscious? It’s a good thing
We all know there’s marketing and functionality elements to grocery stores and how they’re set up for your shopping pleasure. But what if I told you that the good old supermarket subconscious trick works on how healthy food decisions are?
In a recent study, researchers at the University of Southampton in England found that if you placed a wider selection of fruits and vegetables near the entrances and more nonfood items near checkouts, sales decreased on the sweets and increased on the produce. “The findings of our study suggest that a healthier store layout could lead to nearly 10,000 extra portions of fruit and vegetables and approximately 1,500 fewer portions of confectionery being sold on a weekly basis in each store,” lead author Dr. Christina Vogel explained.
You’re probably thinking that food placement studies aren’t new. That’s true, but this one went above and beyond. Instead of just looking at the influence placement has on purchase, this one took it further by trying to reduce the consumers’ “calorie opportunities” and examining the effect on sales. Also, customer loyalty, patterns, and diets were taken into account across multiple household members.
The researchers think shifting the layouts in grocery stores could shift people’s food choices, producing a domino effect on the population’s overall diet. With obesity, diabetes, and cardiology concerns always looming, swaying consumers toward healthier food choices makes for better public health overall.
So if you feel like you’re being subconsciously assaulted by veggies every time you walk into Trader Joe’s, just know it’s for your own good.
TikTokers take on tics
We know TikTok is what makes a lot of teens and young adults tick, but what if TikTokers are actually catching tic disorders from other TikTokers?
TikTok blew up during the pandemic. Many people were stuck at home and had nothing better to do than make and watch TikTok videos. The pandemic brought isolation, uncertainty, and anxiety. The stress that followed may have caused many people, mostly women and young girls, to develop tic disorders.
There’s a TikTok for everything, whether it’s a new dance or a recipe. Many people even use TikTok to speak out about their illnesses. Several TikTokers have Tourette’s syndrome and show their tics on their videos. It appears that some audience members actually “catch” the tics from watching the videos and are then unable to stop certain jerking movements or saying specific words.
Neurologists at the University of Calgary (Alta.), who were hearing from colleagues and getting referrals of such patients, called it “an epidemic within the pandemic.” The behavior is not actually Tourette’s, they told Vice, but the patients “cannot stop, and we have absolutely witnessed that.”
There is, of course, controversy over the issue. One individual with the condition said, “I feel like there’s a lot of really weird, backwards stigma on TikTok about tic disorders. Like, you aren’t allowed to have one unless it’s this one.”
Who would have guessed that people would disagree over stuff on the Internet?
Look on the bright side: Obesity edition
The pandemic may have postponed “Top Gun: Maverick” and “The Marvelous Mrs. Maisel” until who-knows-when, but we here at LOTME are happy to announce the nearly-as-anticipated return of Bacteria vs. the World.
As you may recall from our last edition of BVTW, bacteria battled the ghost of Charles Darwin, who had taken the earthly form of antibiotics capable of stopping bacterial evolution. Tonight, our prokaryotic protagonists take on an equally relentless and ubiquitous challenger: obesity.
Specifically, we’re putting bacteria up against the obesity survival paradox, that phenomenon in which obesity and overweight seem to protect against – yes, you guessed it – bacterial infections.
A Swedish research team observed a group of 2,196 individual adults who received care for suspected severe bacterial infection at Skaraborg Hospital in Skövde. One year after hospitalization, 26% of normal-weight (body mass index, 18.5-24.99) patients were dead, compared with 17% of overweight (BMI, 25.0-29.99), 16% of obese (BMI, 30.0-34.99), and 9% of very obese (BMI >35) patients.
These results confirm the obesity survival paradox, but “what we don’t know is how being overweight can benefit the patient with a bacterial infection, or whether it’s connected with functions in the immune system and how they’re regulated,” lead author Dr. Åsa Alsiö said in a written statement.
A spokes-cell for the bacteria disputed the results and challenged the legitimacy of the investigators. When asked if there should be some sort of reexamination of the findings, he/she/it replied: “You bet your flagella.” We then pointed out that humans don’t have flagellum, and the representative raised his/her/its flagella in what could only be considered an obscene gesture.
Steal from the warm, give to the cold
If there’s one constant in life other than taxes, it’s elderly people moving to Florida. The Sunshine State’s reputation as a giant retirement home needs no elaboration, but why do senior citizens gravitate there? Well, many reasons, but a big one is that, the older you get, the more susceptible and sensitive you are to the cold. And now, according to a new study, we may have identified a culprit.
Researchers from Yale University examined a group of mice and found that the older ones lacked ICL2 cells in their fatty tissue. These cells, at least in younger mice, help restore body heat when exposed to cold temperatures. Lacking these cells meant that older mice had a limited ability to burn their fat and raise their temperature in response to cold.
Well, job done, all we need to do now is stimulate production of ICL2 cells in elderly people, and they’ll be able to go outside in 80-degree weather without a sweater again. Except there’s a problem. In a cruel twist of fate, when the elderly mice were given a molecule to boost ICL2 cell production, they actually became less tolerant of the cold than at baseline. Oops.
The scientists didn’t give up though, and gave their elderly mice ICL2 cells from young mice. This finally did the trick, though we have to admit, if that treatment does eventually scale up to humans, the prospect of a bunch of senior citizens taking ICL2 cells from young people to stay warm does sound a bit like a bad vampire movie premise. “I vant to suck your immune cell group 2 innate lymphoid cells!” Not the most pithy catch phrase in the world.
Grocery store tapping your subconscious? It’s a good thing
We all know there’s marketing and functionality elements to grocery stores and how they’re set up for your shopping pleasure. But what if I told you that the good old supermarket subconscious trick works on how healthy food decisions are?
In a recent study, researchers at the University of Southampton in England found that if you placed a wider selection of fruits and vegetables near the entrances and more nonfood items near checkouts, sales decreased on the sweets and increased on the produce. “The findings of our study suggest that a healthier store layout could lead to nearly 10,000 extra portions of fruit and vegetables and approximately 1,500 fewer portions of confectionery being sold on a weekly basis in each store,” lead author Dr. Christina Vogel explained.
You’re probably thinking that food placement studies aren’t new. That’s true, but this one went above and beyond. Instead of just looking at the influence placement has on purchase, this one took it further by trying to reduce the consumers’ “calorie opportunities” and examining the effect on sales. Also, customer loyalty, patterns, and diets were taken into account across multiple household members.
The researchers think shifting the layouts in grocery stores could shift people’s food choices, producing a domino effect on the population’s overall diet. With obesity, diabetes, and cardiology concerns always looming, swaying consumers toward healthier food choices makes for better public health overall.
So if you feel like you’re being subconsciously assaulted by veggies every time you walk into Trader Joe’s, just know it’s for your own good.
TikTokers take on tics
We know TikTok is what makes a lot of teens and young adults tick, but what if TikTokers are actually catching tic disorders from other TikTokers?
TikTok blew up during the pandemic. Many people were stuck at home and had nothing better to do than make and watch TikTok videos. The pandemic brought isolation, uncertainty, and anxiety. The stress that followed may have caused many people, mostly women and young girls, to develop tic disorders.
There’s a TikTok for everything, whether it’s a new dance or a recipe. Many people even use TikTok to speak out about their illnesses. Several TikTokers have Tourette’s syndrome and show their tics on their videos. It appears that some audience members actually “catch” the tics from watching the videos and are then unable to stop certain jerking movements or saying specific words.
Neurologists at the University of Calgary (Alta.), who were hearing from colleagues and getting referrals of such patients, called it “an epidemic within the pandemic.” The behavior is not actually Tourette’s, they told Vice, but the patients “cannot stop, and we have absolutely witnessed that.”
There is, of course, controversy over the issue. One individual with the condition said, “I feel like there’s a lot of really weird, backwards stigma on TikTok about tic disorders. Like, you aren’t allowed to have one unless it’s this one.”
Who would have guessed that people would disagree over stuff on the Internet?
Look on the bright side: Obesity edition
The pandemic may have postponed “Top Gun: Maverick” and “The Marvelous Mrs. Maisel” until who-knows-when, but we here at LOTME are happy to announce the nearly-as-anticipated return of Bacteria vs. the World.
As you may recall from our last edition of BVTW, bacteria battled the ghost of Charles Darwin, who had taken the earthly form of antibiotics capable of stopping bacterial evolution. Tonight, our prokaryotic protagonists take on an equally relentless and ubiquitous challenger: obesity.
Specifically, we’re putting bacteria up against the obesity survival paradox, that phenomenon in which obesity and overweight seem to protect against – yes, you guessed it – bacterial infections.
A Swedish research team observed a group of 2,196 individual adults who received care for suspected severe bacterial infection at Skaraborg Hospital in Skövde. One year after hospitalization, 26% of normal-weight (body mass index, 18.5-24.99) patients were dead, compared with 17% of overweight (BMI, 25.0-29.99), 16% of obese (BMI, 30.0-34.99), and 9% of very obese (BMI >35) patients.
These results confirm the obesity survival paradox, but “what we don’t know is how being overweight can benefit the patient with a bacterial infection, or whether it’s connected with functions in the immune system and how they’re regulated,” lead author Dr. Åsa Alsiö said in a written statement.
A spokes-cell for the bacteria disputed the results and challenged the legitimacy of the investigators. When asked if there should be some sort of reexamination of the findings, he/she/it replied: “You bet your flagella.” We then pointed out that humans don’t have flagellum, and the representative raised his/her/its flagella in what could only be considered an obscene gesture.
Steal from the warm, give to the cold
If there’s one constant in life other than taxes, it’s elderly people moving to Florida. The Sunshine State’s reputation as a giant retirement home needs no elaboration, but why do senior citizens gravitate there? Well, many reasons, but a big one is that, the older you get, the more susceptible and sensitive you are to the cold. And now, according to a new study, we may have identified a culprit.
Researchers from Yale University examined a group of mice and found that the older ones lacked ICL2 cells in their fatty tissue. These cells, at least in younger mice, help restore body heat when exposed to cold temperatures. Lacking these cells meant that older mice had a limited ability to burn their fat and raise their temperature in response to cold.
Well, job done, all we need to do now is stimulate production of ICL2 cells in elderly people, and they’ll be able to go outside in 80-degree weather without a sweater again. Except there’s a problem. In a cruel twist of fate, when the elderly mice were given a molecule to boost ICL2 cell production, they actually became less tolerant of the cold than at baseline. Oops.
The scientists didn’t give up though, and gave their elderly mice ICL2 cells from young mice. This finally did the trick, though we have to admit, if that treatment does eventually scale up to humans, the prospect of a bunch of senior citizens taking ICL2 cells from young people to stay warm does sound a bit like a bad vampire movie premise. “I vant to suck your immune cell group 2 innate lymphoid cells!” Not the most pithy catch phrase in the world.
Grocery store tapping your subconscious? It’s a good thing
We all know there’s marketing and functionality elements to grocery stores and how they’re set up for your shopping pleasure. But what if I told you that the good old supermarket subconscious trick works on how healthy food decisions are?
In a recent study, researchers at the University of Southampton in England found that if you placed a wider selection of fruits and vegetables near the entrances and more nonfood items near checkouts, sales decreased on the sweets and increased on the produce. “The findings of our study suggest that a healthier store layout could lead to nearly 10,000 extra portions of fruit and vegetables and approximately 1,500 fewer portions of confectionery being sold on a weekly basis in each store,” lead author Dr. Christina Vogel explained.
You’re probably thinking that food placement studies aren’t new. That’s true, but this one went above and beyond. Instead of just looking at the influence placement has on purchase, this one took it further by trying to reduce the consumers’ “calorie opportunities” and examining the effect on sales. Also, customer loyalty, patterns, and diets were taken into account across multiple household members.
The researchers think shifting the layouts in grocery stores could shift people’s food choices, producing a domino effect on the population’s overall diet. With obesity, diabetes, and cardiology concerns always looming, swaying consumers toward healthier food choices makes for better public health overall.
So if you feel like you’re being subconsciously assaulted by veggies every time you walk into Trader Joe’s, just know it’s for your own good.
TikTokers take on tics
We know TikTok is what makes a lot of teens and young adults tick, but what if TikTokers are actually catching tic disorders from other TikTokers?
TikTok blew up during the pandemic. Many people were stuck at home and had nothing better to do than make and watch TikTok videos. The pandemic brought isolation, uncertainty, and anxiety. The stress that followed may have caused many people, mostly women and young girls, to develop tic disorders.
There’s a TikTok for everything, whether it’s a new dance or a recipe. Many people even use TikTok to speak out about their illnesses. Several TikTokers have Tourette’s syndrome and show their tics on their videos. It appears that some audience members actually “catch” the tics from watching the videos and are then unable to stop certain jerking movements or saying specific words.
Neurologists at the University of Calgary (Alta.), who were hearing from colleagues and getting referrals of such patients, called it “an epidemic within the pandemic.” The behavior is not actually Tourette’s, they told Vice, but the patients “cannot stop, and we have absolutely witnessed that.”
There is, of course, controversy over the issue. One individual with the condition said, “I feel like there’s a lot of really weird, backwards stigma on TikTok about tic disorders. Like, you aren’t allowed to have one unless it’s this one.”
Who would have guessed that people would disagree over stuff on the Internet?
Look on the bright side: Obesity edition
The pandemic may have postponed “Top Gun: Maverick” and “The Marvelous Mrs. Maisel” until who-knows-when, but we here at LOTME are happy to announce the nearly-as-anticipated return of Bacteria vs. the World.
As you may recall from our last edition of BVTW, bacteria battled the ghost of Charles Darwin, who had taken the earthly form of antibiotics capable of stopping bacterial evolution. Tonight, our prokaryotic protagonists take on an equally relentless and ubiquitous challenger: obesity.
Specifically, we’re putting bacteria up against the obesity survival paradox, that phenomenon in which obesity and overweight seem to protect against – yes, you guessed it – bacterial infections.
A Swedish research team observed a group of 2,196 individual adults who received care for suspected severe bacterial infection at Skaraborg Hospital in Skövde. One year after hospitalization, 26% of normal-weight (body mass index, 18.5-24.99) patients were dead, compared with 17% of overweight (BMI, 25.0-29.99), 16% of obese (BMI, 30.0-34.99), and 9% of very obese (BMI >35) patients.
These results confirm the obesity survival paradox, but “what we don’t know is how being overweight can benefit the patient with a bacterial infection, or whether it’s connected with functions in the immune system and how they’re regulated,” lead author Dr. Åsa Alsiö said in a written statement.
A spokes-cell for the bacteria disputed the results and challenged the legitimacy of the investigators. When asked if there should be some sort of reexamination of the findings, he/she/it replied: “You bet your flagella.” We then pointed out that humans don’t have flagellum, and the representative raised his/her/its flagella in what could only be considered an obscene gesture.
Study finds most adverse events from microneedling are minimal
according to the results of a systematic review of nearly 3,000 patients.
Microneedling involves the use of instruments including dermarollers and microneedling pens to cause controlled microtraumas at various skin depths and induce a wounding cascade that ultimately improves the visual appearance of the skin, Sherman Chu, DO, of the department of dermatology at the University of California, Irvine, and colleagues wrote.
Microneedling has increased in popularity because of its relatively low cost, effectiveness, and ease of use, and is often promoted as “a safe alternative treatment, particularly in skin of color, but the safety of microneedling and its complications are not often discussed,” the researchers noted.
In the study, published in Dermatologic Surgery, Dr. Chu and coauthors identified 85 articles for the systematic review of safety data on microneedling. The studies included 30 randomized, controlled trials; 24 prospective studies; 16 case series; 12 case reports; and 3 retrospective cohort studies, with a total of 2,805 patients treated with microneedling.
The devices used in the studies were primarily dermarollers (1,758 procedures), but 425 procedures involved dermapens, and 176 involved unidentified microneedling devices.
The most common adverse effect after microneedling with any device was any of anticipated transient procedural side effects including transient erythema or edema, pain, burning, bruising, pruritus, stinging, bleeding, crusting, and desquamation. Overall, these effects resolved within a week with little or no treatment, the researchers said.
The most commonly reported postprocedure side effects of microneedling were postinflammatory hyperpigmentation (46 incidents), followed by dry skin and exfoliation (41 incidents). Fewer than 15 incidents were reported of each the following: acne flare, pruritus, persistent erythema, herpetic infection, flushing, seborrheic dermatitis, burning, headache, stinging, milia, tram-track scarring, facial allergic granulomatous reaction and systematic hypersensitivity, and tender cervical lymphadenopathy. In addition, one incident each was reported of periorbital dermatitis, phototoxic reaction, pressure urticaria, irritant contact dermatitis, widespread facial inoculation of varicella, pustular folliculitis, and tinea corporis.
The studies suggest that microneedling is generally well tolerated, the researchers wrote. Factors that increased the risk of adverse events included the presence of active infections, darker skin types, metal allergies, and the use of combination therapies. For example, they noted, one randomized, controlled trial showed greater skin irritation in patients treated with both microneedling and tranexamic acid compared with those treated with tranexamic acid alone.
Other studies described increased risk of postinflammatory hyperpigmentation in patients treated with both microneedling and platelet-rich plasma, and with microneedling and topical 5-FU or tacrolimus. Also, in one of the studies in the review, “the development of a delayed granulomatous hypersensitivity reaction in 2 patients was attributed to a reaction to vitamin C serum, whereas another study attributes vitamin A and vitamin C oil to be the cause of a patient’s prolonged erythema and pruritus,” the researchers said.
The study findings were limited to adverse events reported by clinicians in published literature, and did not account for adverse events that occur when microneedling is performed at home or in medical spas. Although the results suggest that microneedling is relatively safe for patients of most skin types, “great caution should be taken when performing microneedling with products not approved to be used intradermally,” they emphasized.
“Further studies are needed to determine which patients are at a higher chance of developing scarring because depth of the needle and skin type do not directly correlate as initially believed,” they concluded.
Microneedling offers safe alternative to lasers
“Microneedling is a popular procedure that can be used as an alternative to laser treatments to provide low down time, and lower-cost treatments for similar indications in which lasers are used, such as rhytides and scars,” Catherine M. DiGiorgio, MD, a laser and cosmetic dermatologist at the Boston Center for Facial Rejuvenation, said in an interview.
“Many clinicians and/or providers utilize microneedling in their practice also because they may not have the ability to perform laser and energy-based device treatments,” noted Dr. DiGiorgio, who was asked to comment on the study findings. “Microneedling is safer than energy-based devices in darker skin types due to the lack of energy or heat being delivered to the epidermis. However, as shown in this study, darker skin types remain at risk for [postinflammatory hyperpigmentation], particularly in the hands of an unskilled, inexperienced operator.”
Dr. DiGiorgio said she was not surprised by the study findings. “Microneedling creates microwounds in the skin, which contributes to the risk of all of the side effects listed in the study. Further, the proper use of microneedling devices by the providers performing the procedure is variable and depths of penetration can vary based on which device or roller pen is used and the experience of the person performing the procedures. Depth, after a certain point, can be inaccurate and can superficially abrade the epidermis rather than the intended individual microneedle punctures.”
Laser and energy-based device treatments can be performed safely in patients with darker skin types in the hands of skilled and experienced laser surgeons, said Dr. DiGiorgio. However, “more studies are needed to determine the effectiveness of microneedling alone compared to other treatment modalities. Patients tend to select microneedling due to affordability and less down time; however, sometimes it may not be the best treatment option for their skin condition.
“Patient education is an important factor because one treatment that worked for one of their friends, for example, may not be the best treatment option for their skin complaints.”
Dr. DiGiorgio added that there are few randomized, controlled trials comparing microneedling to laser treatment. “More studies of this nature would benefit the scientific literature and the addition of histological analysis would help us better understand how these treatments compare on a microscopic level.”
The study received no outside funding and the author has no disclosures. Dr. DiGiorgio has served as a consultant for Allergan Aesthetics.
according to the results of a systematic review of nearly 3,000 patients.
Microneedling involves the use of instruments including dermarollers and microneedling pens to cause controlled microtraumas at various skin depths and induce a wounding cascade that ultimately improves the visual appearance of the skin, Sherman Chu, DO, of the department of dermatology at the University of California, Irvine, and colleagues wrote.
Microneedling has increased in popularity because of its relatively low cost, effectiveness, and ease of use, and is often promoted as “a safe alternative treatment, particularly in skin of color, but the safety of microneedling and its complications are not often discussed,” the researchers noted.
In the study, published in Dermatologic Surgery, Dr. Chu and coauthors identified 85 articles for the systematic review of safety data on microneedling. The studies included 30 randomized, controlled trials; 24 prospective studies; 16 case series; 12 case reports; and 3 retrospective cohort studies, with a total of 2,805 patients treated with microneedling.
The devices used in the studies were primarily dermarollers (1,758 procedures), but 425 procedures involved dermapens, and 176 involved unidentified microneedling devices.
The most common adverse effect after microneedling with any device was any of anticipated transient procedural side effects including transient erythema or edema, pain, burning, bruising, pruritus, stinging, bleeding, crusting, and desquamation. Overall, these effects resolved within a week with little or no treatment, the researchers said.
The most commonly reported postprocedure side effects of microneedling were postinflammatory hyperpigmentation (46 incidents), followed by dry skin and exfoliation (41 incidents). Fewer than 15 incidents were reported of each the following: acne flare, pruritus, persistent erythema, herpetic infection, flushing, seborrheic dermatitis, burning, headache, stinging, milia, tram-track scarring, facial allergic granulomatous reaction and systematic hypersensitivity, and tender cervical lymphadenopathy. In addition, one incident each was reported of periorbital dermatitis, phototoxic reaction, pressure urticaria, irritant contact dermatitis, widespread facial inoculation of varicella, pustular folliculitis, and tinea corporis.
The studies suggest that microneedling is generally well tolerated, the researchers wrote. Factors that increased the risk of adverse events included the presence of active infections, darker skin types, metal allergies, and the use of combination therapies. For example, they noted, one randomized, controlled trial showed greater skin irritation in patients treated with both microneedling and tranexamic acid compared with those treated with tranexamic acid alone.
Other studies described increased risk of postinflammatory hyperpigmentation in patients treated with both microneedling and platelet-rich plasma, and with microneedling and topical 5-FU or tacrolimus. Also, in one of the studies in the review, “the development of a delayed granulomatous hypersensitivity reaction in 2 patients was attributed to a reaction to vitamin C serum, whereas another study attributes vitamin A and vitamin C oil to be the cause of a patient’s prolonged erythema and pruritus,” the researchers said.
The study findings were limited to adverse events reported by clinicians in published literature, and did not account for adverse events that occur when microneedling is performed at home or in medical spas. Although the results suggest that microneedling is relatively safe for patients of most skin types, “great caution should be taken when performing microneedling with products not approved to be used intradermally,” they emphasized.
“Further studies are needed to determine which patients are at a higher chance of developing scarring because depth of the needle and skin type do not directly correlate as initially believed,” they concluded.
Microneedling offers safe alternative to lasers
“Microneedling is a popular procedure that can be used as an alternative to laser treatments to provide low down time, and lower-cost treatments for similar indications in which lasers are used, such as rhytides and scars,” Catherine M. DiGiorgio, MD, a laser and cosmetic dermatologist at the Boston Center for Facial Rejuvenation, said in an interview.
“Many clinicians and/or providers utilize microneedling in their practice also because they may not have the ability to perform laser and energy-based device treatments,” noted Dr. DiGiorgio, who was asked to comment on the study findings. “Microneedling is safer than energy-based devices in darker skin types due to the lack of energy or heat being delivered to the epidermis. However, as shown in this study, darker skin types remain at risk for [postinflammatory hyperpigmentation], particularly in the hands of an unskilled, inexperienced operator.”
Dr. DiGiorgio said she was not surprised by the study findings. “Microneedling creates microwounds in the skin, which contributes to the risk of all of the side effects listed in the study. Further, the proper use of microneedling devices by the providers performing the procedure is variable and depths of penetration can vary based on which device or roller pen is used and the experience of the person performing the procedures. Depth, after a certain point, can be inaccurate and can superficially abrade the epidermis rather than the intended individual microneedle punctures.”
Laser and energy-based device treatments can be performed safely in patients with darker skin types in the hands of skilled and experienced laser surgeons, said Dr. DiGiorgio. However, “more studies are needed to determine the effectiveness of microneedling alone compared to other treatment modalities. Patients tend to select microneedling due to affordability and less down time; however, sometimes it may not be the best treatment option for their skin condition.
“Patient education is an important factor because one treatment that worked for one of their friends, for example, may not be the best treatment option for their skin complaints.”
Dr. DiGiorgio added that there are few randomized, controlled trials comparing microneedling to laser treatment. “More studies of this nature would benefit the scientific literature and the addition of histological analysis would help us better understand how these treatments compare on a microscopic level.”
The study received no outside funding and the author has no disclosures. Dr. DiGiorgio has served as a consultant for Allergan Aesthetics.
according to the results of a systematic review of nearly 3,000 patients.
Microneedling involves the use of instruments including dermarollers and microneedling pens to cause controlled microtraumas at various skin depths and induce a wounding cascade that ultimately improves the visual appearance of the skin, Sherman Chu, DO, of the department of dermatology at the University of California, Irvine, and colleagues wrote.
Microneedling has increased in popularity because of its relatively low cost, effectiveness, and ease of use, and is often promoted as “a safe alternative treatment, particularly in skin of color, but the safety of microneedling and its complications are not often discussed,” the researchers noted.
In the study, published in Dermatologic Surgery, Dr. Chu and coauthors identified 85 articles for the systematic review of safety data on microneedling. The studies included 30 randomized, controlled trials; 24 prospective studies; 16 case series; 12 case reports; and 3 retrospective cohort studies, with a total of 2,805 patients treated with microneedling.
The devices used in the studies were primarily dermarollers (1,758 procedures), but 425 procedures involved dermapens, and 176 involved unidentified microneedling devices.
The most common adverse effect after microneedling with any device was any of anticipated transient procedural side effects including transient erythema or edema, pain, burning, bruising, pruritus, stinging, bleeding, crusting, and desquamation. Overall, these effects resolved within a week with little or no treatment, the researchers said.
The most commonly reported postprocedure side effects of microneedling were postinflammatory hyperpigmentation (46 incidents), followed by dry skin and exfoliation (41 incidents). Fewer than 15 incidents were reported of each the following: acne flare, pruritus, persistent erythema, herpetic infection, flushing, seborrheic dermatitis, burning, headache, stinging, milia, tram-track scarring, facial allergic granulomatous reaction and systematic hypersensitivity, and tender cervical lymphadenopathy. In addition, one incident each was reported of periorbital dermatitis, phototoxic reaction, pressure urticaria, irritant contact dermatitis, widespread facial inoculation of varicella, pustular folliculitis, and tinea corporis.
The studies suggest that microneedling is generally well tolerated, the researchers wrote. Factors that increased the risk of adverse events included the presence of active infections, darker skin types, metal allergies, and the use of combination therapies. For example, they noted, one randomized, controlled trial showed greater skin irritation in patients treated with both microneedling and tranexamic acid compared with those treated with tranexamic acid alone.
Other studies described increased risk of postinflammatory hyperpigmentation in patients treated with both microneedling and platelet-rich plasma, and with microneedling and topical 5-FU or tacrolimus. Also, in one of the studies in the review, “the development of a delayed granulomatous hypersensitivity reaction in 2 patients was attributed to a reaction to vitamin C serum, whereas another study attributes vitamin A and vitamin C oil to be the cause of a patient’s prolonged erythema and pruritus,” the researchers said.
The study findings were limited to adverse events reported by clinicians in published literature, and did not account for adverse events that occur when microneedling is performed at home or in medical spas. Although the results suggest that microneedling is relatively safe for patients of most skin types, “great caution should be taken when performing microneedling with products not approved to be used intradermally,” they emphasized.
“Further studies are needed to determine which patients are at a higher chance of developing scarring because depth of the needle and skin type do not directly correlate as initially believed,” they concluded.
Microneedling offers safe alternative to lasers
“Microneedling is a popular procedure that can be used as an alternative to laser treatments to provide low down time, and lower-cost treatments for similar indications in which lasers are used, such as rhytides and scars,” Catherine M. DiGiorgio, MD, a laser and cosmetic dermatologist at the Boston Center for Facial Rejuvenation, said in an interview.
“Many clinicians and/or providers utilize microneedling in their practice also because they may not have the ability to perform laser and energy-based device treatments,” noted Dr. DiGiorgio, who was asked to comment on the study findings. “Microneedling is safer than energy-based devices in darker skin types due to the lack of energy or heat being delivered to the epidermis. However, as shown in this study, darker skin types remain at risk for [postinflammatory hyperpigmentation], particularly in the hands of an unskilled, inexperienced operator.”
Dr. DiGiorgio said she was not surprised by the study findings. “Microneedling creates microwounds in the skin, which contributes to the risk of all of the side effects listed in the study. Further, the proper use of microneedling devices by the providers performing the procedure is variable and depths of penetration can vary based on which device or roller pen is used and the experience of the person performing the procedures. Depth, after a certain point, can be inaccurate and can superficially abrade the epidermis rather than the intended individual microneedle punctures.”
Laser and energy-based device treatments can be performed safely in patients with darker skin types in the hands of skilled and experienced laser surgeons, said Dr. DiGiorgio. However, “more studies are needed to determine the effectiveness of microneedling alone compared to other treatment modalities. Patients tend to select microneedling due to affordability and less down time; however, sometimes it may not be the best treatment option for their skin condition.
“Patient education is an important factor because one treatment that worked for one of their friends, for example, may not be the best treatment option for their skin complaints.”
Dr. DiGiorgio added that there are few randomized, controlled trials comparing microneedling to laser treatment. “More studies of this nature would benefit the scientific literature and the addition of histological analysis would help us better understand how these treatments compare on a microscopic level.”
The study received no outside funding and the author has no disclosures. Dr. DiGiorgio has served as a consultant for Allergan Aesthetics.
FROM DERMATOLOGIC SURGERY