User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Arsenic levels in infant rice cereal are down
according to test results released by the Food and Drug Administration.
In April 2016, the FDA issued draft guidance calling for manufacturers of the product to reduce the level of arsenic in their cereals by establishing an action level of arsenic of 100 mcg/kg or 100 parts per billion.
Seventy-six percent of samples of infant rice cereal tested in 2018 had levels of arsenic at or below 100 parts per billion versus 47% of samples tested in 2014, according to a statement from the FDA. In 2011-2013, an even lower percentage of samples tested contained amounts of inorganic arsenic at or below the FDA’s current action level for this element, whose consumption has been associated with cancer, skin lesions, cardiovascular diseases, and diabetes.
The 2018 data is based on the testing of 149 samples of infant white and brown rice cereal samples.
“Results from our tests show that manufacturers have made significant progress in ensuring lower levels of inorganic arsenic in infant rice cereal,” Susan Mayne, PhD, director of the Center for Food Safety and Applied Nutrition, said in the FDA statement.
“Both white rice and brown rice cereals showed improvement in meeting the FDA’s 100 ppb proposed action level, but the improvement was greatest for white rice cereals, which tend to have lower levels of inorganic arsenic overall,” according to the statement.
according to test results released by the Food and Drug Administration.
In April 2016, the FDA issued draft guidance calling for manufacturers of the product to reduce the level of arsenic in their cereals by establishing an action level of arsenic of 100 mcg/kg or 100 parts per billion.
Seventy-six percent of samples of infant rice cereal tested in 2018 had levels of arsenic at or below 100 parts per billion versus 47% of samples tested in 2014, according to a statement from the FDA. In 2011-2013, an even lower percentage of samples tested contained amounts of inorganic arsenic at or below the FDA’s current action level for this element, whose consumption has been associated with cancer, skin lesions, cardiovascular diseases, and diabetes.
The 2018 data is based on the testing of 149 samples of infant white and brown rice cereal samples.
“Results from our tests show that manufacturers have made significant progress in ensuring lower levels of inorganic arsenic in infant rice cereal,” Susan Mayne, PhD, director of the Center for Food Safety and Applied Nutrition, said in the FDA statement.
“Both white rice and brown rice cereals showed improvement in meeting the FDA’s 100 ppb proposed action level, but the improvement was greatest for white rice cereals, which tend to have lower levels of inorganic arsenic overall,” according to the statement.
according to test results released by the Food and Drug Administration.
In April 2016, the FDA issued draft guidance calling for manufacturers of the product to reduce the level of arsenic in their cereals by establishing an action level of arsenic of 100 mcg/kg or 100 parts per billion.
Seventy-six percent of samples of infant rice cereal tested in 2018 had levels of arsenic at or below 100 parts per billion versus 47% of samples tested in 2014, according to a statement from the FDA. In 2011-2013, an even lower percentage of samples tested contained amounts of inorganic arsenic at or below the FDA’s current action level for this element, whose consumption has been associated with cancer, skin lesions, cardiovascular diseases, and diabetes.
The 2018 data is based on the testing of 149 samples of infant white and brown rice cereal samples.
“Results from our tests show that manufacturers have made significant progress in ensuring lower levels of inorganic arsenic in infant rice cereal,” Susan Mayne, PhD, director of the Center for Food Safety and Applied Nutrition, said in the FDA statement.
“Both white rice and brown rice cereals showed improvement in meeting the FDA’s 100 ppb proposed action level, but the improvement was greatest for white rice cereals, which tend to have lower levels of inorganic arsenic overall,” according to the statement.
Novel coronavirus may cause environmental contamination through fecal shedding
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
The toilet bowl, sink, and bathroom door handle of an isolation room housing a patient with the novel coronavirus tested positive for the virus, raising the possibility that viral shedding in the stool could represent another route of transmission, investigators reported.
Air outlet fans and other room sites also tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), though an anteroom, a corridor, and most personal protective equipment (PPE) worn by health care providers tested negative, according to the researchers, led by Sean Wei Xiang Ong, MBBS, of the National Centre for Infectious Diseases, Singapore.
Taken together, these findings suggest a “need for strict adherence to environmental and hand hygiene” to combat significant environmental contamination through respiratory droplets and fecal shedding, Dr. Ong and colleagues wrote in JAMA.
Aaron Eli Glatt, MD, chair of medicine at Mount Sinai South Nassau in New York, said these results demonstrate that SARS-CoV-2 is “clearly capable” of contaminating bathroom sinks and toilets.
“That wouldn’t have been the first place I would have thought of, before this study,” he said in an interview. “You need to pay attention to cleaning the bathrooms, which we obviously do, but that’s an important reminder.”
The report by Dr. Ong and coauthors included a total of three patients housed in airborne infection isolation rooms in a dedicated SARS-CoV-2 outbreak center in Singapore. For each patient, surface samples were taken from 26 sites in the isolation room, an anteroom, and a bathroom. Samples were also taken from PPE on physicians as they left the patient rooms.
Samples for the first patient, taken right after routine cleaning, were all negative, according to researchers. That room was sampled twice, on days 4 and 10 of the illness, while the patient was still symptomatic. Likewise, for the second patient, postcleaning samples were negative; those samples were taken 2 days after cleaning.
However, for the third patient, samples were taken before routine cleaning. In this case, Dr. Ong and colleagues said 13 of 15 room sites (87%) were positive, including air outlet fans, while 3 of 5 toilet sites (60%) were positive as well, though no contamination was found in the anteroom, corridor, or in air samples.
That patient had two stool samples that were positive for SARS-CoV-2, but no diarrhea, authors said, and had upper respiratory tract involvement without pneumonia.
The fact that swabs of the air exhaust outlets tested positive suggests that virus-laden droplets could be “displaced by airflows” and end up on vents or other equipment, Dr. Ong and coauthors reported.
All PPE samples tested negative, except for the front of one shoe.
“The risk of transmission from contaminated footwear is likely low, as evidenced by negative results in the anteroom and corridor,” they wrote.
While this study included only a small number of patients, Dr. Glatt said the findings represent an important and useful contribution to the literature on coronavirus disease 2019 (COVID-19).
“Every day we’re getting more information, and each little piece of the puzzle helps us in the overall management of individuals with COVID-19,” he said in the interview. “They’re adding to our ability to manage, control, and mitigate further spread of the disease.”
Funding for the study came from the National Medical Research Council in Singapore and DSO National Laboratories. Dr. Ong and colleagues reported no conflicts of interest.
SOURCE: Ong SWX et al. JAMA. 2020 Mar 4. doi: 10.1001/jama.2020.3227.
FROM JAMA
Telehealth seen as a key tool to help fight COVID-19
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Telehealth is increasingly being viewed as a key way to help fight the COVID-19 outbreak in the United States. Recognizing the potential of this technology to slow the spread of the disease, the House of Representatives included a provision in an $8.3 billion emergency response bill it approved today that would temporarily lift restrictions on Medicare telehealth coverage to assist in the efforts to contain the virus.
Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention (CDC), said that hospitals should be prepared to use telehealth as one of their tools in fighting the outbreak, according to a recent news release from the American Hospital Association (AHA).
Congress is responding to that need by including the service in the new coronavirus legislation now headed to the Senate, after the funding bill was approved in a 415-2 vote by the House.
The bill empowers the Secretary of Health and Human Services (HHS) to “waive or modify application of certain Medicare requirements with respect to telehealth services furnished during certain emergency periods.”
While the measure adds telehealth to the waiver authority that the HHS secretary currently has during national emergencies, it’s only for the coronavirus crisis in this case, Krista Drobac, executive director of the Alliance for Connected Care, told Medscape Medical News.
The waiver would apply to originating sites of telehealth visits, she noted. Thus Medicare coverage of telemedicine would be expanded beyond rural areas.
In addition, the waiver would allow coverage of virtual visits conducted on smartphones with audio and video capabilities. A “qualified provider,” as defined by the legislation, would be a practitioner who has an established relationship with the patient or who is in the same practice as the provider who has that relationship.
An advantage of telehealth, proponents say, is that it can enable people who believe they have COVID-19 to be seen at home rather than visit offices or emergency departments (EDs) where they might spread the disease or be in proximity to others who have it.
In an editorial published March 2 in Modern Healthcare, medical directors from Stanford Medicine, MedStar Health, and Intermountain Healthcare also noted that telehealth can give patients 24/7 access to care, allow surveillance of patients at risk while keeping them at home, ensure that treatment in hospitals is reserved for high-need patients, and enable providers to triage and screen more patients than can be handled in brick-and-mortar care settings.
However, telehealth screening would allow physicians only to judge whether a patient’s symptoms might be indicative of COVID-19, the Alliance for Connected Care, a telehealth advocacy group, noted in a letter to Congressional leaders. Patients would still have to be seen in person to be tested for the disease.
The group, which represents technology companies, health insurers, pharmacies, and other healthcare players, has been lobbying Congress to include telehealth in federal funds to combat the outbreak.
The American Telemedicine Association (ATA) also supports this goal, ATA President Joseph Kvedar, MD, told Medscape Medical News. And the authors of the Modern Healthcare editorial also advocated for this legislative solution. Because the fatality rate for COVID-19 is significantly higher for older people than for other age groups, they noted, telehealth should be an economically viable option for all seniors.
The Centers for Medicare and Medicaid Services (CMS) long covered telemedicine only in rural areas and only when initiated in healthcare settings. Recently, however, CMS loosened its approach to some extent. Virtual “check-in visits” can now be initiated from any location, including home, to determine whether a Medicare patient needs to be seen in the office. In addition, CMS allows Medicare Advantage plans to offer telemedicine as a core benefit.
Are healthcare systems prepared?
Some large healthcare systems such as Stanford, MedStar, and Intermountain are already using telehealth to diagnose and treat patients who have traditional influenza. Telehealth providers at Stanford estimate that almost 50% of these patients are being prescribed the antiviral drug Tamiflu.
It’s unclear whether other healthcare systems are this well prepared to offer telehealth on a large scale. But, according to an AHA survey, Kvedar noted, three quarters of AHA members are engaged in some form of telehealth.
Drobac said “it wouldn’t require too much effort” to ramp up a wide-scale telehealth program that could help reduce the impact of the outbreak. “The technology is there,” she noted. “You need a HIPAA-compliant telehealth platform, but there are so many out there.”
Kvedar agreed. To begin with, he said, hospitals might sequester patients who visit the ED with COVID-19 symptoms in a video-equipped “isolation room.” Staff members could then do the patient intake from a different location in the hospital.
He admitted that this approach would be infeasible if a lot of patients arrived in EDs with coronavirus symptoms. However, Kvedar noted, “All the tools are in place to go well beyond that. American Well, Teladoc, and others are all offering ways to get out in front of this. There are plenty of vendors out there, and most people have a connected cell phone that you can do a video call on.”
Hospital leaders would have to decide whether to embrace telehealth, which would mean less use of services in their institutions, he said. “But it would be for the greater good of the public.”
Kvedar recalled that there was some use of telehealth in the New York area after 9/11. Telehealth was also used in the aftermath of Hurricane Katrina in 2005. But the ATA president, who is also vice president of connected health at Partners HealthCare in Boston, noted that the COVID-19 outbreak is the first public health emergency to occur in the era of Skype and smartphones.
If Congress does ultimately authorize CMS to cover telehealth across the board during this emergency, might that lead to a permanent change in Medicare coverage policy? Kvedar wouldn’t venture an opinion. “However, the current CMS leadership has been incredibly telehealth friendly,” he said. “So it’s possible they would [embrace a lifting of restrictions]. As patients get a sense of this modality of care and how convenient it is for them, they’ll start asking for more.”
Meanwhile, he said, the telehealth opportunity goes beyond video visits with doctors to mitigate the outbreak. Telehealth data could also be used to track disease spread, similar to how researchers have studied Google searches to predict the spread of the flu, he noted.
Teladoc, a major telehealth vendor, recently told stock analysts it’s already working with the CDC on disease surveillance, according to a report in FierceHealthcare.
This article first appeared on Medscape.com.
Short-course calcipotriol plus 5-FU for AKs: potential major public health impact
LAHAINA, HAWAII – The most intriguing recent development in the treatment of actinic keratosis is a study in which a short-course of topical field therapy with , with a resultant markedly reduced risk of developing squamous cell carcinoma within the next 3 years, Kishwer S. Nehal, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
The annual cost of treating actinic keratoses (AKs) exceeds $1 billion in the United States, so the billion-dollar question in dermatology is, does AK reduction lead to long-term protection against cancer? And this 3-year study by investigators at Washington University in St. Louis and Massachusetts General Hospital in Boston suggests the answer may be yes – when topical immunotherapy is utilized to induce robust T cell immunity, said Dr. Nehal, director of Mohs micrographic and dermatologic surgery, and codirector of the multidisciplinary skin cancer management program at Memorial Sloan Kettering Cancer Center in New York.
The investigators previously conducted a randomized, double-blind clinical trial in which 130 participants with a substantial AK burden received a 4-day course of 0.005% calcipotriol ointment plus 5% 5-FU cream or Vaseline plus 5-FU. The combination therapy proved more effective than the comparator in eliminating AKs at 8 weeks of follow-up. Moreover, tissue analysis pointed to the mechanism of benefit: The combination treatment induced keratinocyte expression of thymic stromal lymphopoietin (TSLP) cytokine, which led to a powerful CD4+ T cell response against AKs.
The researchers’ follow-up study addressed two key questions: Whether this epidermal T cell immunity persists long term, and if it actually achieves a reduced risk of squamous cell carcinoma (SCC) over time. The answers were yes and yes.
Seventy of the original 130 patients were prospectively followed for 3 years. Only 2 of 30 (7%) in the short-course combination therapy group developed SCC in treated areas of the face and scalp, compared with 11 of 40 controls (28%), a statistically significant difference, which constitutes a 79% relative risk reduction. This chemopreventive effect was long lasting at the cellular level, as the combination therapy group still retained measurable T cell immunity in the skin at the 3-year mark. As expected, the topical therapy had no impact on the development of basal cell carcinoma. The question now becomes how long the chemopreventive effect extends beyond 3 years.
“These remarkable findings substantiate the use of immunotherapeutic agents with minimal side effects and high efficacy against precancerous lesions in order to reduce the risk of cancer development and recurrence, which may be broadly applicable to skin and internal malignancies,” the investigators wrote in the study (JCI Insight. 2019 Mar 21;4(6). pii: 125476. doi: 10.1172/jci.insight.125476). Dr. Nehal said that this study requires confirmation in light of its post hoc design and the relatively small numbers of patients and SCCs. But the potential public health implications are profound, since roughly 40 million Americans have AKs, subclinical AKs are 10 times more common than visible ones, AKs are known precursors for SCC, and high-risk SCC is the cause of roughly 10,000 deaths per year, an underappreciated mortality burden that’s actually comparable to that of melanoma.
While awaiting further studies, this short-course combination therapy also offers the ready appeal of a field therapy without much downtime due to treatment-induced inflammation. In the study, 4 days of combo therapy resulted in moderate inflammation which quickly resolved.
“Does treatment duration and severity affect patient compliance? I would argue that in 2020 it does. People have very active, busy lives and they don’t want a lot of downtime. I can tell you that in Manhattan they want no downtime,” said Dr. Nehal, professor of dermatology at Weill Cornell Medicine, New York.
Even though a traditional 4-week, twice-daily course of 5% 5-FU cream has been convincingly shown in a recent large randomized Dutch trial (N Engl J Med. 2019 Mar 7;380[10]:935-46) to be the most effective field therapy for eradicating AKs – outperforming in descending order of efficacy at 12 months of follow-up imiquimod (Zyclara), photodynamic therapy, and ingenol mebutate (Picato) – Dr. Nehal finds few takers for 5-FU. People balk at the downtime. Her female patients with a significant AK burden typically opt for photodynamic therapy because of the aesthetic side benefit and shorter downtime, while the men – even those who’ve already had a large SCC – are more likely to prefer a watch-and-wait approach, dealing with an SCC if and when it arises.
“I love the science behind using calcipotriol with 5-FU, but I wish it was more friendly to dermatologists,” said fellow panelist Paul Nghiem, MD, PhD. “Of all the things we should have a combination product for, the pharmaceutical industry should really prepare a [calcipotriol/5-FU] cream and market it with the improved efficacy data.”
He added that he has no use for the conventional 2- to 4-week, twice-daily 5-FU regimens employed by many dermatologists.
“I don’t understand this need to feel like you’ve got to treat patients until they look like they’ve fallen off a motorcycle at 50 mph. I just can’t see that,” said Dr. Nghiem, professor and chair of dermatology at the University of Washington, Seattle.
Instead, he routinely utilizes the nearly 3-decade-old Pearlman technique of weekly pulsed dosing of topical 5-FU (J Am Acad Dermatol. 1991 Oct;25[4]:665-7).
“I almost never even ask my patients, ‘Are you OK with having a bunch of downtime?’ I just say, ‘Treat with the 5-FU until you get some erythema, until you’re bothered by it, and then stop for a while,’ ” he explained. “I’ve treated many patients with that technique over the years. It might not be quite as effective, but I hardly have to do any treatment with liquid nitrogen.”
Session chair Ashfaq A. Marghoob, MD, is of a similar mind.
“I also don’t go to the point that you’re fire engine red. Once the irritation sets in, we stop,” said Dr. Marghoob, director of clinical dermatology, Memorial Sloan Kettering Skin Cancer Center Hauppauge (New York).
Neither Dr. Nehal nor Dr. Nghiem has used short-course calcipotriol plus 5-FU therapy. When they polled the large audience as to who has, only a few hands went up.
“I feel like residents who are keeping up with the literature are using it,” Dr. Nehal observed. “My fellows say, ‘Yup, that’s what we’re doing,’ but I’m not using it.”
“I use it,” volunteered fellow panelist Trilokraj Tejasvi, MBBS. “I was educated by one of my residents, and now I use it all the time, especially in my VA population. I’ve been using it for a year. Things get red, but it clears fast,” said Dr. Tejasvi, director of the cutaneous lymphoma program and director of teledermatology services at the University of Michigan, Ann Arbor, and chief of the dermatology service at Ann Arbor Veteran Affairs Hospital.
Dr. Nehal reported having no conflicts of interest regarding her presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – The most intriguing recent development in the treatment of actinic keratosis is a study in which a short-course of topical field therapy with , with a resultant markedly reduced risk of developing squamous cell carcinoma within the next 3 years, Kishwer S. Nehal, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
The annual cost of treating actinic keratoses (AKs) exceeds $1 billion in the United States, so the billion-dollar question in dermatology is, does AK reduction lead to long-term protection against cancer? And this 3-year study by investigators at Washington University in St. Louis and Massachusetts General Hospital in Boston suggests the answer may be yes – when topical immunotherapy is utilized to induce robust T cell immunity, said Dr. Nehal, director of Mohs micrographic and dermatologic surgery, and codirector of the multidisciplinary skin cancer management program at Memorial Sloan Kettering Cancer Center in New York.
The investigators previously conducted a randomized, double-blind clinical trial in which 130 participants with a substantial AK burden received a 4-day course of 0.005% calcipotriol ointment plus 5% 5-FU cream or Vaseline plus 5-FU. The combination therapy proved more effective than the comparator in eliminating AKs at 8 weeks of follow-up. Moreover, tissue analysis pointed to the mechanism of benefit: The combination treatment induced keratinocyte expression of thymic stromal lymphopoietin (TSLP) cytokine, which led to a powerful CD4+ T cell response against AKs.
The researchers’ follow-up study addressed two key questions: Whether this epidermal T cell immunity persists long term, and if it actually achieves a reduced risk of squamous cell carcinoma (SCC) over time. The answers were yes and yes.
Seventy of the original 130 patients were prospectively followed for 3 years. Only 2 of 30 (7%) in the short-course combination therapy group developed SCC in treated areas of the face and scalp, compared with 11 of 40 controls (28%), a statistically significant difference, which constitutes a 79% relative risk reduction. This chemopreventive effect was long lasting at the cellular level, as the combination therapy group still retained measurable T cell immunity in the skin at the 3-year mark. As expected, the topical therapy had no impact on the development of basal cell carcinoma. The question now becomes how long the chemopreventive effect extends beyond 3 years.
“These remarkable findings substantiate the use of immunotherapeutic agents with minimal side effects and high efficacy against precancerous lesions in order to reduce the risk of cancer development and recurrence, which may be broadly applicable to skin and internal malignancies,” the investigators wrote in the study (JCI Insight. 2019 Mar 21;4(6). pii: 125476. doi: 10.1172/jci.insight.125476). Dr. Nehal said that this study requires confirmation in light of its post hoc design and the relatively small numbers of patients and SCCs. But the potential public health implications are profound, since roughly 40 million Americans have AKs, subclinical AKs are 10 times more common than visible ones, AKs are known precursors for SCC, and high-risk SCC is the cause of roughly 10,000 deaths per year, an underappreciated mortality burden that’s actually comparable to that of melanoma.
While awaiting further studies, this short-course combination therapy also offers the ready appeal of a field therapy without much downtime due to treatment-induced inflammation. In the study, 4 days of combo therapy resulted in moderate inflammation which quickly resolved.
“Does treatment duration and severity affect patient compliance? I would argue that in 2020 it does. People have very active, busy lives and they don’t want a lot of downtime. I can tell you that in Manhattan they want no downtime,” said Dr. Nehal, professor of dermatology at Weill Cornell Medicine, New York.
Even though a traditional 4-week, twice-daily course of 5% 5-FU cream has been convincingly shown in a recent large randomized Dutch trial (N Engl J Med. 2019 Mar 7;380[10]:935-46) to be the most effective field therapy for eradicating AKs – outperforming in descending order of efficacy at 12 months of follow-up imiquimod (Zyclara), photodynamic therapy, and ingenol mebutate (Picato) – Dr. Nehal finds few takers for 5-FU. People balk at the downtime. Her female patients with a significant AK burden typically opt for photodynamic therapy because of the aesthetic side benefit and shorter downtime, while the men – even those who’ve already had a large SCC – are more likely to prefer a watch-and-wait approach, dealing with an SCC if and when it arises.
“I love the science behind using calcipotriol with 5-FU, but I wish it was more friendly to dermatologists,” said fellow panelist Paul Nghiem, MD, PhD. “Of all the things we should have a combination product for, the pharmaceutical industry should really prepare a [calcipotriol/5-FU] cream and market it with the improved efficacy data.”
He added that he has no use for the conventional 2- to 4-week, twice-daily 5-FU regimens employed by many dermatologists.
“I don’t understand this need to feel like you’ve got to treat patients until they look like they’ve fallen off a motorcycle at 50 mph. I just can’t see that,” said Dr. Nghiem, professor and chair of dermatology at the University of Washington, Seattle.
Instead, he routinely utilizes the nearly 3-decade-old Pearlman technique of weekly pulsed dosing of topical 5-FU (J Am Acad Dermatol. 1991 Oct;25[4]:665-7).
“I almost never even ask my patients, ‘Are you OK with having a bunch of downtime?’ I just say, ‘Treat with the 5-FU until you get some erythema, until you’re bothered by it, and then stop for a while,’ ” he explained. “I’ve treated many patients with that technique over the years. It might not be quite as effective, but I hardly have to do any treatment with liquid nitrogen.”
Session chair Ashfaq A. Marghoob, MD, is of a similar mind.
“I also don’t go to the point that you’re fire engine red. Once the irritation sets in, we stop,” said Dr. Marghoob, director of clinical dermatology, Memorial Sloan Kettering Skin Cancer Center Hauppauge (New York).
Neither Dr. Nehal nor Dr. Nghiem has used short-course calcipotriol plus 5-FU therapy. When they polled the large audience as to who has, only a few hands went up.
“I feel like residents who are keeping up with the literature are using it,” Dr. Nehal observed. “My fellows say, ‘Yup, that’s what we’re doing,’ but I’m not using it.”
“I use it,” volunteered fellow panelist Trilokraj Tejasvi, MBBS. “I was educated by one of my residents, and now I use it all the time, especially in my VA population. I’ve been using it for a year. Things get red, but it clears fast,” said Dr. Tejasvi, director of the cutaneous lymphoma program and director of teledermatology services at the University of Michigan, Ann Arbor, and chief of the dermatology service at Ann Arbor Veteran Affairs Hospital.
Dr. Nehal reported having no conflicts of interest regarding her presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – The most intriguing recent development in the treatment of actinic keratosis is a study in which a short-course of topical field therapy with , with a resultant markedly reduced risk of developing squamous cell carcinoma within the next 3 years, Kishwer S. Nehal, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
The annual cost of treating actinic keratoses (AKs) exceeds $1 billion in the United States, so the billion-dollar question in dermatology is, does AK reduction lead to long-term protection against cancer? And this 3-year study by investigators at Washington University in St. Louis and Massachusetts General Hospital in Boston suggests the answer may be yes – when topical immunotherapy is utilized to induce robust T cell immunity, said Dr. Nehal, director of Mohs micrographic and dermatologic surgery, and codirector of the multidisciplinary skin cancer management program at Memorial Sloan Kettering Cancer Center in New York.
The investigators previously conducted a randomized, double-blind clinical trial in which 130 participants with a substantial AK burden received a 4-day course of 0.005% calcipotriol ointment plus 5% 5-FU cream or Vaseline plus 5-FU. The combination therapy proved more effective than the comparator in eliminating AKs at 8 weeks of follow-up. Moreover, tissue analysis pointed to the mechanism of benefit: The combination treatment induced keratinocyte expression of thymic stromal lymphopoietin (TSLP) cytokine, which led to a powerful CD4+ T cell response against AKs.
The researchers’ follow-up study addressed two key questions: Whether this epidermal T cell immunity persists long term, and if it actually achieves a reduced risk of squamous cell carcinoma (SCC) over time. The answers were yes and yes.
Seventy of the original 130 patients were prospectively followed for 3 years. Only 2 of 30 (7%) in the short-course combination therapy group developed SCC in treated areas of the face and scalp, compared with 11 of 40 controls (28%), a statistically significant difference, which constitutes a 79% relative risk reduction. This chemopreventive effect was long lasting at the cellular level, as the combination therapy group still retained measurable T cell immunity in the skin at the 3-year mark. As expected, the topical therapy had no impact on the development of basal cell carcinoma. The question now becomes how long the chemopreventive effect extends beyond 3 years.
“These remarkable findings substantiate the use of immunotherapeutic agents with minimal side effects and high efficacy against precancerous lesions in order to reduce the risk of cancer development and recurrence, which may be broadly applicable to skin and internal malignancies,” the investigators wrote in the study (JCI Insight. 2019 Mar 21;4(6). pii: 125476. doi: 10.1172/jci.insight.125476). Dr. Nehal said that this study requires confirmation in light of its post hoc design and the relatively small numbers of patients and SCCs. But the potential public health implications are profound, since roughly 40 million Americans have AKs, subclinical AKs are 10 times more common than visible ones, AKs are known precursors for SCC, and high-risk SCC is the cause of roughly 10,000 deaths per year, an underappreciated mortality burden that’s actually comparable to that of melanoma.
While awaiting further studies, this short-course combination therapy also offers the ready appeal of a field therapy without much downtime due to treatment-induced inflammation. In the study, 4 days of combo therapy resulted in moderate inflammation which quickly resolved.
“Does treatment duration and severity affect patient compliance? I would argue that in 2020 it does. People have very active, busy lives and they don’t want a lot of downtime. I can tell you that in Manhattan they want no downtime,” said Dr. Nehal, professor of dermatology at Weill Cornell Medicine, New York.
Even though a traditional 4-week, twice-daily course of 5% 5-FU cream has been convincingly shown in a recent large randomized Dutch trial (N Engl J Med. 2019 Mar 7;380[10]:935-46) to be the most effective field therapy for eradicating AKs – outperforming in descending order of efficacy at 12 months of follow-up imiquimod (Zyclara), photodynamic therapy, and ingenol mebutate (Picato) – Dr. Nehal finds few takers for 5-FU. People balk at the downtime. Her female patients with a significant AK burden typically opt for photodynamic therapy because of the aesthetic side benefit and shorter downtime, while the men – even those who’ve already had a large SCC – are more likely to prefer a watch-and-wait approach, dealing with an SCC if and when it arises.
“I love the science behind using calcipotriol with 5-FU, but I wish it was more friendly to dermatologists,” said fellow panelist Paul Nghiem, MD, PhD. “Of all the things we should have a combination product for, the pharmaceutical industry should really prepare a [calcipotriol/5-FU] cream and market it with the improved efficacy data.”
He added that he has no use for the conventional 2- to 4-week, twice-daily 5-FU regimens employed by many dermatologists.
“I don’t understand this need to feel like you’ve got to treat patients until they look like they’ve fallen off a motorcycle at 50 mph. I just can’t see that,” said Dr. Nghiem, professor and chair of dermatology at the University of Washington, Seattle.
Instead, he routinely utilizes the nearly 3-decade-old Pearlman technique of weekly pulsed dosing of topical 5-FU (J Am Acad Dermatol. 1991 Oct;25[4]:665-7).
“I almost never even ask my patients, ‘Are you OK with having a bunch of downtime?’ I just say, ‘Treat with the 5-FU until you get some erythema, until you’re bothered by it, and then stop for a while,’ ” he explained. “I’ve treated many patients with that technique over the years. It might not be quite as effective, but I hardly have to do any treatment with liquid nitrogen.”
Session chair Ashfaq A. Marghoob, MD, is of a similar mind.
“I also don’t go to the point that you’re fire engine red. Once the irritation sets in, we stop,” said Dr. Marghoob, director of clinical dermatology, Memorial Sloan Kettering Skin Cancer Center Hauppauge (New York).
Neither Dr. Nehal nor Dr. Nghiem has used short-course calcipotriol plus 5-FU therapy. When they polled the large audience as to who has, only a few hands went up.
“I feel like residents who are keeping up with the literature are using it,” Dr. Nehal observed. “My fellows say, ‘Yup, that’s what we’re doing,’ but I’m not using it.”
“I use it,” volunteered fellow panelist Trilokraj Tejasvi, MBBS. “I was educated by one of my residents, and now I use it all the time, especially in my VA population. I’ve been using it for a year. Things get red, but it clears fast,” said Dr. Tejasvi, director of the cutaneous lymphoma program and director of teledermatology services at the University of Michigan, Ann Arbor, and chief of the dermatology service at Ann Arbor Veteran Affairs Hospital.
Dr. Nehal reported having no conflicts of interest regarding her presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM SDEF HAWAII DERMATOLOGY SEMINAR
CMS issues guidance on containing spread of coronavirus
The first guidance document, “Guidance for Infection Control and Prevention Concerning Coronavirus Disease (COVID-19): FAQs and Considerations for Patient Triage, Placement and Hospital Discharge,” issued March 4, provides some basic guidance, including identifying which patients are at risk, how facilities should screen for COVID-19, how facilities should monitor or restrict health care facility staff, and other recommendations for infection prevention and control.
“Hospitals should identify visitors and patients at risk for having COVID-19 infection before or immediately upon arrival to the healthcare facility,” the guidance document notes. “For patients, implement respiratory hygiene and cough etiquette (i.e., placing a face mask over the patient’s nose and mouth if that has not already been done) and isolate the patient in an examination room with the door closed. If the patient cannot be immediately moved to an examination room, ensure they are not allowed to wait among other patients seeking care.”
The document offers further information regarding the care of patients and provides numerous links to existing guidance from the Centers for Disease Control and Prevention.
The second document, “Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes,” issued the same day, provides information on how to limit and monitor visitors as well as monitor and restrict health staff. It details when to transfer residents with suspected or confirmed coronavirus infection, and when a nursing home should accept a resident diagnosed with COVID-19.
Facilities “should contact their local health department if they have questions or suspect a resident of a nursing home has COVID-19,” the document states. “Per CDC, prompt detection, triage and isolation of potentially infectious patients are essential to prevent unnecessary exposure among patients, healthcare personnel, and visitors at the facility.”
The CMS also announced that it is suspending all nonemergency survey activity.
“CMS is suspending nonemergency inspections across the country, allowing inspectors to turn their focus on the most serious health and safety threats like infectious diseases and abuse,” the agency stated in a March 4 memo. “This shift in approach will also allow inspectors to focus on addressing the spread of ... COVID-19. CMS is issuing this memorandum to State Survey Agencies to provide important guidelines for the inspection process in situations in which a COVID-19 is suspected.”
In a statement, CMS Administrator Seema Verma said these actions “represent a call to action across the health care system. All health care providers must immediately review their procedures to ensure compliance with CMS’ infection control requirements, as well as the guidelines from the Centers for Disease Control and Prevention.”
The first guidance document, “Guidance for Infection Control and Prevention Concerning Coronavirus Disease (COVID-19): FAQs and Considerations for Patient Triage, Placement and Hospital Discharge,” issued March 4, provides some basic guidance, including identifying which patients are at risk, how facilities should screen for COVID-19, how facilities should monitor or restrict health care facility staff, and other recommendations for infection prevention and control.
“Hospitals should identify visitors and patients at risk for having COVID-19 infection before or immediately upon arrival to the healthcare facility,” the guidance document notes. “For patients, implement respiratory hygiene and cough etiquette (i.e., placing a face mask over the patient’s nose and mouth if that has not already been done) and isolate the patient in an examination room with the door closed. If the patient cannot be immediately moved to an examination room, ensure they are not allowed to wait among other patients seeking care.”
The document offers further information regarding the care of patients and provides numerous links to existing guidance from the Centers for Disease Control and Prevention.
The second document, “Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes,” issued the same day, provides information on how to limit and monitor visitors as well as monitor and restrict health staff. It details when to transfer residents with suspected or confirmed coronavirus infection, and when a nursing home should accept a resident diagnosed with COVID-19.
Facilities “should contact their local health department if they have questions or suspect a resident of a nursing home has COVID-19,” the document states. “Per CDC, prompt detection, triage and isolation of potentially infectious patients are essential to prevent unnecessary exposure among patients, healthcare personnel, and visitors at the facility.”
The CMS also announced that it is suspending all nonemergency survey activity.
“CMS is suspending nonemergency inspections across the country, allowing inspectors to turn their focus on the most serious health and safety threats like infectious diseases and abuse,” the agency stated in a March 4 memo. “This shift in approach will also allow inspectors to focus on addressing the spread of ... COVID-19. CMS is issuing this memorandum to State Survey Agencies to provide important guidelines for the inspection process in situations in which a COVID-19 is suspected.”
In a statement, CMS Administrator Seema Verma said these actions “represent a call to action across the health care system. All health care providers must immediately review their procedures to ensure compliance with CMS’ infection control requirements, as well as the guidelines from the Centers for Disease Control and Prevention.”
The first guidance document, “Guidance for Infection Control and Prevention Concerning Coronavirus Disease (COVID-19): FAQs and Considerations for Patient Triage, Placement and Hospital Discharge,” issued March 4, provides some basic guidance, including identifying which patients are at risk, how facilities should screen for COVID-19, how facilities should monitor or restrict health care facility staff, and other recommendations for infection prevention and control.
“Hospitals should identify visitors and patients at risk for having COVID-19 infection before or immediately upon arrival to the healthcare facility,” the guidance document notes. “For patients, implement respiratory hygiene and cough etiquette (i.e., placing a face mask over the patient’s nose and mouth if that has not already been done) and isolate the patient in an examination room with the door closed. If the patient cannot be immediately moved to an examination room, ensure they are not allowed to wait among other patients seeking care.”
The document offers further information regarding the care of patients and provides numerous links to existing guidance from the Centers for Disease Control and Prevention.
The second document, “Guidance for Infection Control and Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes,” issued the same day, provides information on how to limit and monitor visitors as well as monitor and restrict health staff. It details when to transfer residents with suspected or confirmed coronavirus infection, and when a nursing home should accept a resident diagnosed with COVID-19.
Facilities “should contact their local health department if they have questions or suspect a resident of a nursing home has COVID-19,” the document states. “Per CDC, prompt detection, triage and isolation of potentially infectious patients are essential to prevent unnecessary exposure among patients, healthcare personnel, and visitors at the facility.”
The CMS also announced that it is suspending all nonemergency survey activity.
“CMS is suspending nonemergency inspections across the country, allowing inspectors to turn their focus on the most serious health and safety threats like infectious diseases and abuse,” the agency stated in a March 4 memo. “This shift in approach will also allow inspectors to focus on addressing the spread of ... COVID-19. CMS is issuing this memorandum to State Survey Agencies to provide important guidelines for the inspection process in situations in which a COVID-19 is suspected.”
In a statement, CMS Administrator Seema Verma said these actions “represent a call to action across the health care system. All health care providers must immediately review their procedures to ensure compliance with CMS’ infection control requirements, as well as the guidelines from the Centers for Disease Control and Prevention.”
Emollients didn’t prevent atopic dermatitis in high-risk infants
The use of including those at high risk, in two new clinical trials.
The BEEP (Barrier Enhancement for Eczema Prevention) study compared the rates of AD among infants identified as at risk of AD because of family history who had daily applications of emollients (Diprobase cream or Doublebase gel) for the first year of life, compared with a standard skin care group. PreventADALL (Preventing Atopic Dermatitis and Allergies in Children) is a randomized, primary-prevention study conducted in Norway and Sweden that randomized infants into one of four groups: controls whose parents followed regular skin care advice and nutrition guidelines; those who received skin emollients (the addition of emulsified oil to their bath and application of facial cream on at least 4 days a week from age 2 weeks to 8 months); those who received early complementary feeding of peanut, cow’s milk, wheat, and egg introduced between aged 12 and 16 weeks; and a group that combined both the emollient and diet interventions.
Neither of the studies, published in the Lancet, found statistically significant differences in AD rates between the intervention and control groups.
The results put a damper on hopes raised by previous studies that included two small pilot studies, which found that daily use of leave-on emollients in infants considered at high risk of AD prevented the development of AD (J Allergy Clin Immunol 2014 Oct;134:824-30.e6; J Allergy Clin Immunol Oct 2014;134:818-23).
“It was maybe a little bit overly hopeful to think that we could just moisturize and prevent such a complex disorder,” Robert Sidbury, MD, chief of dermatology at Seattle Children’s Hospital, said in an interview. He emphasized that the studies only addressed emollients as a preventative, and that “there’s no question that emollients are still critical for the therapy of eczema.”
Bruce Brod, MD, clinical professor of dermatology at the University of Pennsylvania, Philadelphia, suggested that homogeneous patient populations or insufficient numbers might explain the negative findings. PreventADALL drew patients from Norway and Sweden, while BEEP recruited from the United Kingdom. “They’re important studies, but I think they still lend themselves to further studies with different patient populations and larger groups of patients,” Dr. Brod said in an interview.
BEEP was headed by Joanne Chalmers, PhD, and Hywel Williams, DSc, of the Centre of Evidence-Based Dermatology at the University of Nottingham (England). Håvard Ove Skjerven, PhD, and Karin C Lødrup Carlsen, PhD, of Oslo University Hospital led the PreventADALL study.
The BEEP study randomized 1,394 newborns at 16 sites in the United Kingdom to daily emollient treatment with standard skin care, or standard skin care alone. At one year, compliance was 74% in the intervention group. At age 2, 23% of the intervention group had AD, compared with 25% of controls (hazard ratio, 0.95; P =.61). Skin infections were also higher in the treatment arm (mean, 0.23 per year vs. 0.15 per year; adjusted incidence ratio, 1.55; 95% confidence interval, 1.15-2.09).
“Our study does not support the use of emollients for preventing eczema in high-risk infants, a finding supported by PreventADALL, another large trial using a skin barrier enhancing intervention,” they concluded. Their data “relate only to prevention of eczema and do not directly challenge the practice of using emollients as first-line treatment for eczema.”
In the PreventADALL study, 2,397 newborn infants born between 2015 and 2017 were randomized to one of the four groups. Use of facial cream and emollients during bathing began at 2 weeks, and early complementary feeding of peanut, cow’s milk, wheat, and egg at 3-4 months. The frequency of AD at aged 12 months in the control group was 8%, compared with 11% in the skin-intervention group, 9% in the food-intervention group, and 5% in the combined-intervention group.
These differences were not statistically significant, and “the primary hypothesis that either skin intervention or food intervention reduced atopic dermatitis were not confirmed,” the authors wrote. Parental atopy did not influence the effects of the interventions. Their results were in line with the BEEP results, and the authors “cannot recommend these interventions as primary prevention strategies.”
The researchers will continue to follow children until age 3 years to evaluate the food allergy rates, if the combined-treatment group experiences a long-term benefit. Adherence to the protocol was poor, with 44% compliance with the facial cream application and 27% compliance with bathing emollients; 32% fully adhered to the diet protocols.
The studies were funded by the National Institute for Health Research Health Technology Assessment (BEEP); and a range of public and private funders (PreventADALL). One author of the PreventADALL study disclosed receiving honoraria for presentations from several pharmaceutical companies, and one author received honoraria for presentations from Thermo Fisher Scientific; the rest had no disclosures. Dr. Sidbury has been an investigator for Regeneron. Dr. Brod had no relevant financial disclosures.
SOURCES: Chalmers JR et al. Lancet. 2020 Feb 19. doi: 10.1016/S0140-6736(19)32984-8; Skjerven HO et al. Lancet. 2020 Feb 19. doi: 10.1016/S0140-6736(19)32983-6.
The “null findings” of these two studies were “unexpected,” Kirsten P. Perrett, MBBS, Phd, and Rachel L. Peters, PhD, of the department of population allergy at Murdoch Children’s Research Institute, Parkville, Australia, wrote in an accompanying editorial. They noted that emollients are used regularly in the management of atopic dermatitis, where they help maintain the skin barrier and reduce the need for anti-inflammatory therapies.
These two large prevention studies were “prompted” by the results of small, proof-of-concept pilot studies, which “provided strong efficacy signals for the hypothesis that daily emollient use could prevent atopic dermatitis,” they wrote. But the two studies “found no evidence that daily emollient use in either a population-based or high-risk cohort of infants during the first year of life could delay, suppress, or prevent atopic dermatitis.” The lower incidence of atopic dermatitis among those in the dietary and emollient combination, compared with controls (5% vs. 8%) in PreventADALL, could be a chance finding.
The large, randomized Prevention of Eczema by a Barrier Lipid Equilibrium Strategy (PEBBLES) trial is ongoing to confirm results from a small study suggesting the efficacy of a ceramide-dominant emollient. But the PreventADALL study showed low compliance, suggesting that this intervention, if effective, a twice-daily emollient regimen may be tough to implement. “At this stage, emollients should not be recommended for the primary prevention of atopic dermatitis in infants,” they concluded.
Dr. Perrett and Dr. Peters declared no competing interests. Their comments appeared in the Lancet (2020 Feb 19. doi: 10.1016/S0140-6736[19]33174-5).
The “null findings” of these two studies were “unexpected,” Kirsten P. Perrett, MBBS, Phd, and Rachel L. Peters, PhD, of the department of population allergy at Murdoch Children’s Research Institute, Parkville, Australia, wrote in an accompanying editorial. They noted that emollients are used regularly in the management of atopic dermatitis, where they help maintain the skin barrier and reduce the need for anti-inflammatory therapies.
These two large prevention studies were “prompted” by the results of small, proof-of-concept pilot studies, which “provided strong efficacy signals for the hypothesis that daily emollient use could prevent atopic dermatitis,” they wrote. But the two studies “found no evidence that daily emollient use in either a population-based or high-risk cohort of infants during the first year of life could delay, suppress, or prevent atopic dermatitis.” The lower incidence of atopic dermatitis among those in the dietary and emollient combination, compared with controls (5% vs. 8%) in PreventADALL, could be a chance finding.
The large, randomized Prevention of Eczema by a Barrier Lipid Equilibrium Strategy (PEBBLES) trial is ongoing to confirm results from a small study suggesting the efficacy of a ceramide-dominant emollient. But the PreventADALL study showed low compliance, suggesting that this intervention, if effective, a twice-daily emollient regimen may be tough to implement. “At this stage, emollients should not be recommended for the primary prevention of atopic dermatitis in infants,” they concluded.
Dr. Perrett and Dr. Peters declared no competing interests. Their comments appeared in the Lancet (2020 Feb 19. doi: 10.1016/S0140-6736[19]33174-5).
The “null findings” of these two studies were “unexpected,” Kirsten P. Perrett, MBBS, Phd, and Rachel L. Peters, PhD, of the department of population allergy at Murdoch Children’s Research Institute, Parkville, Australia, wrote in an accompanying editorial. They noted that emollients are used regularly in the management of atopic dermatitis, where they help maintain the skin barrier and reduce the need for anti-inflammatory therapies.
These two large prevention studies were “prompted” by the results of small, proof-of-concept pilot studies, which “provided strong efficacy signals for the hypothesis that daily emollient use could prevent atopic dermatitis,” they wrote. But the two studies “found no evidence that daily emollient use in either a population-based or high-risk cohort of infants during the first year of life could delay, suppress, or prevent atopic dermatitis.” The lower incidence of atopic dermatitis among those in the dietary and emollient combination, compared with controls (5% vs. 8%) in PreventADALL, could be a chance finding.
The large, randomized Prevention of Eczema by a Barrier Lipid Equilibrium Strategy (PEBBLES) trial is ongoing to confirm results from a small study suggesting the efficacy of a ceramide-dominant emollient. But the PreventADALL study showed low compliance, suggesting that this intervention, if effective, a twice-daily emollient regimen may be tough to implement. “At this stage, emollients should not be recommended for the primary prevention of atopic dermatitis in infants,” they concluded.
Dr. Perrett and Dr. Peters declared no competing interests. Their comments appeared in the Lancet (2020 Feb 19. doi: 10.1016/S0140-6736[19]33174-5).
The use of including those at high risk, in two new clinical trials.
The BEEP (Barrier Enhancement for Eczema Prevention) study compared the rates of AD among infants identified as at risk of AD because of family history who had daily applications of emollients (Diprobase cream or Doublebase gel) for the first year of life, compared with a standard skin care group. PreventADALL (Preventing Atopic Dermatitis and Allergies in Children) is a randomized, primary-prevention study conducted in Norway and Sweden that randomized infants into one of four groups: controls whose parents followed regular skin care advice and nutrition guidelines; those who received skin emollients (the addition of emulsified oil to their bath and application of facial cream on at least 4 days a week from age 2 weeks to 8 months); those who received early complementary feeding of peanut, cow’s milk, wheat, and egg introduced between aged 12 and 16 weeks; and a group that combined both the emollient and diet interventions.
Neither of the studies, published in the Lancet, found statistically significant differences in AD rates between the intervention and control groups.
The results put a damper on hopes raised by previous studies that included two small pilot studies, which found that daily use of leave-on emollients in infants considered at high risk of AD prevented the development of AD (J Allergy Clin Immunol 2014 Oct;134:824-30.e6; J Allergy Clin Immunol Oct 2014;134:818-23).
“It was maybe a little bit overly hopeful to think that we could just moisturize and prevent such a complex disorder,” Robert Sidbury, MD, chief of dermatology at Seattle Children’s Hospital, said in an interview. He emphasized that the studies only addressed emollients as a preventative, and that “there’s no question that emollients are still critical for the therapy of eczema.”
Bruce Brod, MD, clinical professor of dermatology at the University of Pennsylvania, Philadelphia, suggested that homogeneous patient populations or insufficient numbers might explain the negative findings. PreventADALL drew patients from Norway and Sweden, while BEEP recruited from the United Kingdom. “They’re important studies, but I think they still lend themselves to further studies with different patient populations and larger groups of patients,” Dr. Brod said in an interview.
BEEP was headed by Joanne Chalmers, PhD, and Hywel Williams, DSc, of the Centre of Evidence-Based Dermatology at the University of Nottingham (England). Håvard Ove Skjerven, PhD, and Karin C Lødrup Carlsen, PhD, of Oslo University Hospital led the PreventADALL study.
The BEEP study randomized 1,394 newborns at 16 sites in the United Kingdom to daily emollient treatment with standard skin care, or standard skin care alone. At one year, compliance was 74% in the intervention group. At age 2, 23% of the intervention group had AD, compared with 25% of controls (hazard ratio, 0.95; P =.61). Skin infections were also higher in the treatment arm (mean, 0.23 per year vs. 0.15 per year; adjusted incidence ratio, 1.55; 95% confidence interval, 1.15-2.09).
“Our study does not support the use of emollients for preventing eczema in high-risk infants, a finding supported by PreventADALL, another large trial using a skin barrier enhancing intervention,” they concluded. Their data “relate only to prevention of eczema and do not directly challenge the practice of using emollients as first-line treatment for eczema.”
In the PreventADALL study, 2,397 newborn infants born between 2015 and 2017 were randomized to one of the four groups. Use of facial cream and emollients during bathing began at 2 weeks, and early complementary feeding of peanut, cow’s milk, wheat, and egg at 3-4 months. The frequency of AD at aged 12 months in the control group was 8%, compared with 11% in the skin-intervention group, 9% in the food-intervention group, and 5% in the combined-intervention group.
These differences were not statistically significant, and “the primary hypothesis that either skin intervention or food intervention reduced atopic dermatitis were not confirmed,” the authors wrote. Parental atopy did not influence the effects of the interventions. Their results were in line with the BEEP results, and the authors “cannot recommend these interventions as primary prevention strategies.”
The researchers will continue to follow children until age 3 years to evaluate the food allergy rates, if the combined-treatment group experiences a long-term benefit. Adherence to the protocol was poor, with 44% compliance with the facial cream application and 27% compliance with bathing emollients; 32% fully adhered to the diet protocols.
The studies were funded by the National Institute for Health Research Health Technology Assessment (BEEP); and a range of public and private funders (PreventADALL). One author of the PreventADALL study disclosed receiving honoraria for presentations from several pharmaceutical companies, and one author received honoraria for presentations from Thermo Fisher Scientific; the rest had no disclosures. Dr. Sidbury has been an investigator for Regeneron. Dr. Brod had no relevant financial disclosures.
SOURCES: Chalmers JR et al. Lancet. 2020 Feb 19. doi: 10.1016/S0140-6736(19)32984-8; Skjerven HO et al. Lancet. 2020 Feb 19. doi: 10.1016/S0140-6736(19)32983-6.
The use of including those at high risk, in two new clinical trials.
The BEEP (Barrier Enhancement for Eczema Prevention) study compared the rates of AD among infants identified as at risk of AD because of family history who had daily applications of emollients (Diprobase cream or Doublebase gel) for the first year of life, compared with a standard skin care group. PreventADALL (Preventing Atopic Dermatitis and Allergies in Children) is a randomized, primary-prevention study conducted in Norway and Sweden that randomized infants into one of four groups: controls whose parents followed regular skin care advice and nutrition guidelines; those who received skin emollients (the addition of emulsified oil to their bath and application of facial cream on at least 4 days a week from age 2 weeks to 8 months); those who received early complementary feeding of peanut, cow’s milk, wheat, and egg introduced between aged 12 and 16 weeks; and a group that combined both the emollient and diet interventions.
Neither of the studies, published in the Lancet, found statistically significant differences in AD rates between the intervention and control groups.
The results put a damper on hopes raised by previous studies that included two small pilot studies, which found that daily use of leave-on emollients in infants considered at high risk of AD prevented the development of AD (J Allergy Clin Immunol 2014 Oct;134:824-30.e6; J Allergy Clin Immunol Oct 2014;134:818-23).
“It was maybe a little bit overly hopeful to think that we could just moisturize and prevent such a complex disorder,” Robert Sidbury, MD, chief of dermatology at Seattle Children’s Hospital, said in an interview. He emphasized that the studies only addressed emollients as a preventative, and that “there’s no question that emollients are still critical for the therapy of eczema.”
Bruce Brod, MD, clinical professor of dermatology at the University of Pennsylvania, Philadelphia, suggested that homogeneous patient populations or insufficient numbers might explain the negative findings. PreventADALL drew patients from Norway and Sweden, while BEEP recruited from the United Kingdom. “They’re important studies, but I think they still lend themselves to further studies with different patient populations and larger groups of patients,” Dr. Brod said in an interview.
BEEP was headed by Joanne Chalmers, PhD, and Hywel Williams, DSc, of the Centre of Evidence-Based Dermatology at the University of Nottingham (England). Håvard Ove Skjerven, PhD, and Karin C Lødrup Carlsen, PhD, of Oslo University Hospital led the PreventADALL study.
The BEEP study randomized 1,394 newborns at 16 sites in the United Kingdom to daily emollient treatment with standard skin care, or standard skin care alone. At one year, compliance was 74% in the intervention group. At age 2, 23% of the intervention group had AD, compared with 25% of controls (hazard ratio, 0.95; P =.61). Skin infections were also higher in the treatment arm (mean, 0.23 per year vs. 0.15 per year; adjusted incidence ratio, 1.55; 95% confidence interval, 1.15-2.09).
“Our study does not support the use of emollients for preventing eczema in high-risk infants, a finding supported by PreventADALL, another large trial using a skin barrier enhancing intervention,” they concluded. Their data “relate only to prevention of eczema and do not directly challenge the practice of using emollients as first-line treatment for eczema.”
In the PreventADALL study, 2,397 newborn infants born between 2015 and 2017 were randomized to one of the four groups. Use of facial cream and emollients during bathing began at 2 weeks, and early complementary feeding of peanut, cow’s milk, wheat, and egg at 3-4 months. The frequency of AD at aged 12 months in the control group was 8%, compared with 11% in the skin-intervention group, 9% in the food-intervention group, and 5% in the combined-intervention group.
These differences were not statistically significant, and “the primary hypothesis that either skin intervention or food intervention reduced atopic dermatitis were not confirmed,” the authors wrote. Parental atopy did not influence the effects of the interventions. Their results were in line with the BEEP results, and the authors “cannot recommend these interventions as primary prevention strategies.”
The researchers will continue to follow children until age 3 years to evaluate the food allergy rates, if the combined-treatment group experiences a long-term benefit. Adherence to the protocol was poor, with 44% compliance with the facial cream application and 27% compliance with bathing emollients; 32% fully adhered to the diet protocols.
The studies were funded by the National Institute for Health Research Health Technology Assessment (BEEP); and a range of public and private funders (PreventADALL). One author of the PreventADALL study disclosed receiving honoraria for presentations from several pharmaceutical companies, and one author received honoraria for presentations from Thermo Fisher Scientific; the rest had no disclosures. Dr. Sidbury has been an investigator for Regeneron. Dr. Brod had no relevant financial disclosures.
SOURCES: Chalmers JR et al. Lancet. 2020 Feb 19. doi: 10.1016/S0140-6736(19)32984-8; Skjerven HO et al. Lancet. 2020 Feb 19. doi: 10.1016/S0140-6736(19)32983-6.
FROM THE LANCET
Survey: 2020 will see more attacks on ACA
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
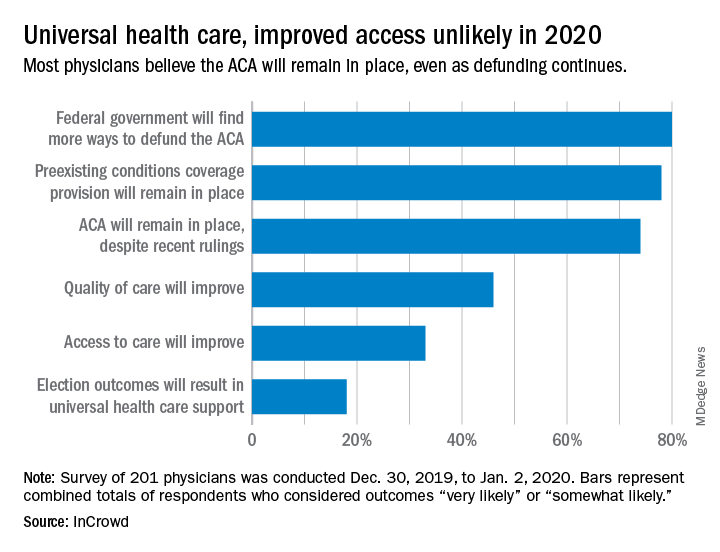
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
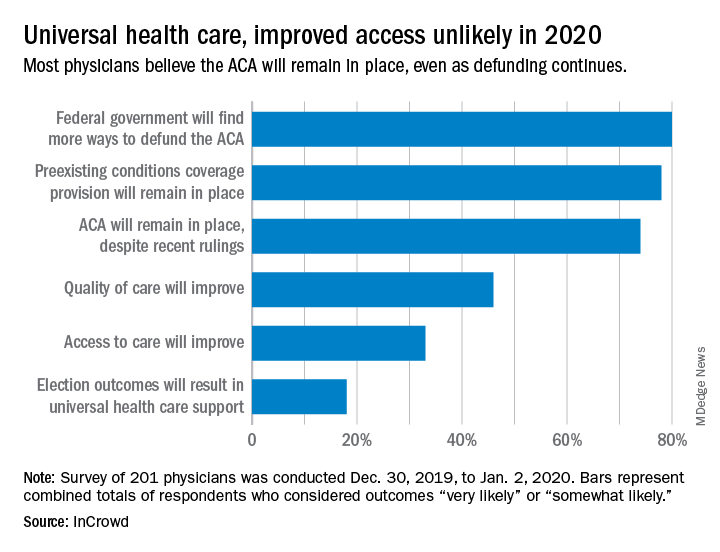
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
What medical conferences are being canceled by coronavirus?
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
Washington State grapples with coronavirus outbreak
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
FROM A KING COUNTY, WASH. NEWS BRIEFING
Esophageal stricture signals urgent treatment in kids with butterfly skin
LONDON – A quarter of urgent contacts in 20 children with generalized severe recessive dystrophic epidermolysis bullosa (GS-RDEB) were tied to esophageal narrowing, according data from a 12-month review of electronic health records.
Urgent advice was sought 102 times outside of regular or scheduled appointments by the parents of 20 children with GS-RDEB, Christine Prodinger, MD, of the University Clinic of Dermatology at Paracelsus Medical University, Salzburg, Austria, and colleagues reported in a poster presentation at the EB World Congress, organized by the Dystrophic Epidermolysis Bullosa Association (DEBRA). The researchers looked at the records from the EB clinic at Great Ormond Street Hospital for Children NHS Foundation Trust, London, during April 2018–April 2019.
The mean number of urgent contacts with the specialist unit was 5.1 per patient per year, the researchers reported, with 24 of the 102 contacts (23.5%) resulting in the child being admitted to a hospital. Most of the contacts were made via email or telephone to EB nurses (94%), by contacts during home visits (3%), or in an appointment with the palliative or symptom care team (3%).
“The most common reason [for the urgent contact] was acute dysphagia,” which was experienced as choking, throat pain, difficulty eating, reflux, and vomiting, the researchers observed. Dysphagia affected children in 27 of the contacts (26.5%), and resulted in esophageal dilatation in 90% of the cases. Other reasons for urgent contact were skin infection (15.7% of contacts), uncontrolled pain (15.7% of the contacts), and eye problems (11.8%).
Esophageal dilatation
Strictures are just one of the esophageal manifestations of the disease, noted Anna Bruckner, MD, associate professor of dermatology and pediatrics in the department of dermatology at the University of Colorado at Denver, Aurora, during an oral presentation. Other possible manifestations include blisters and erosions, the formation of webs – a thin extension of esophageal tissue, perforations, and rupture. “These are primarily problems with dystrophic EB” but can occur with other EB subtypes, she noted.
“We don’t have great evidence” on whether the onset of esophageal strictures can be delayed or prevented, Dr. Bruckner observed. As for management, “fluoroscopy-guided balloon dilatation is probably best” for most patients, but the best procedural approach needs to be discussed on a patient-by-patient basis.
Citing a paper that documents her own experience on the use of esophageal dilatation in 24 children who underwent 231 fluoroscopy-guided balloon dilatation procedures, Dr. Bruckner noted that strictures were most commonly located in the proximal part of the esophagus, with a median distance of 13 cm down from the lips (J Pediatr Gastroenterol Nutr. 2018;67[6]:701-5).
The retrospective chart review reported by Dr. Bruckner showed that there were a median of seven dilatation procedures per patient, and 20 patients had repeated procedures at a median interval of 164 days. About 10% of procedures resulted in adverse events – mostly vomiting, pain, and fever – but there were no perforations or other serious effects, and the rate of subsequent hospitalization was 6.9%.
Dysphagia
Dysphagia was the predominant symptom caused by esophageal stricture in another dataset reported in a poster by Elena Pope, MD, MSc, of the Hospital for Sick Children at the University of Toronto, and colleagues.
Of 125 EB patients who had experienced at least 1 esophageal stricture episode, 497 esophageal stricture events were reported, and 85.5% of patients had difficulty swallowing at presentation, with 29.8% unable to swallow solids and 7.2% unable to swallow liquids. Other symptoms at presentation were painful swallowing (11%), food being stuck in the esophagus (8%), regurgitation (5%), coughing (4.8%), and dyspepsia (2.8%).
The aim of the retrospective, multicenter cohort study was to determine the prevalence of, and predisposing factors for, restenosis of esophageal strictures and factors that may predispose to restenosis. The study population consisted of 66 men and 59 women who had experienced their esophageal stricture at around ages 12-13 years. The majority (98.4%) had dystrophic EB, of which almost half (46.5%) had GS-RDEB.
The researchers found that the location of the esophageal stricture was important for restenosis, and that strictures occurring in the lower esophagus were 67.5% less likely to result in restenosis than if they occurred in the upper esophagus (P = .057; hazard ratio, 0.675).
A higher number of strictures was associated with a higher rate of restenosis, they reported. Indeed, patients who had two esophageal strictures had a 29.4% increased risk of restenosis, compared with those who had just one stricture (P = .038; HR, 1.294), and those with three or more strictures had an increased risk of 78.5%, compared with those having one stricture (P = .005; HR, 1.785).
Strictures longer than 1 cm also were associated with a greater (34.7%) risk of restenosis, compared with shorter strictures (P = .032; HR, 1.347). Various methods of resolving the stricture were used, from fluoroscopy-guided balloon dilatation to retro- or antegrade endoscopy. “Irrespective of method, dilatations are successful,” Dr. Pope and colleagues reported. The overall success of dilatation was 99.3%, with full dilatation achieved in almost all of the patients (96%). Of note is that there was a low risk (2.6%) of complications, they observed.
Medications were used in 46.8% of the patients, with the most popular choice being corticosteroids (90.3%), but the researchers noted that the “potential benefit of periprocedural corticosteroids use in decreasing the risk of restenosis needs further exploration.”
Dr. Bruckner had noted in her presentation that her group did not favor the use of periprocedural corticosteroids, but that antifibrotic therapy “could be attractive” for preventing future strictures.
Dr. Prodinger, Dr. Pope, and their colleagues did not provide disclosure information. Dr. Bruckner is the principal investigator for the Epidermolysis Bullosa Clinical Characterization and Outcomes Database. She disclosed the receipt of grants or research funding, honoraria, or consultation fees from a number of drug companies, as well as other support from the EB Research Partnership and the EB Medical Research Foundation.
SOURCES: Prodinger et al. EB 2020. Poster 3; Bruckner A et al. Pediatr Gastroenterol Nutr. 2018;67(6):701-5; Pope et al. EB 2020. Poster 8.
LONDON – A quarter of urgent contacts in 20 children with generalized severe recessive dystrophic epidermolysis bullosa (GS-RDEB) were tied to esophageal narrowing, according data from a 12-month review of electronic health records.
Urgent advice was sought 102 times outside of regular or scheduled appointments by the parents of 20 children with GS-RDEB, Christine Prodinger, MD, of the University Clinic of Dermatology at Paracelsus Medical University, Salzburg, Austria, and colleagues reported in a poster presentation at the EB World Congress, organized by the Dystrophic Epidermolysis Bullosa Association (DEBRA). The researchers looked at the records from the EB clinic at Great Ormond Street Hospital for Children NHS Foundation Trust, London, during April 2018–April 2019.
The mean number of urgent contacts with the specialist unit was 5.1 per patient per year, the researchers reported, with 24 of the 102 contacts (23.5%) resulting in the child being admitted to a hospital. Most of the contacts were made via email or telephone to EB nurses (94%), by contacts during home visits (3%), or in an appointment with the palliative or symptom care team (3%).
“The most common reason [for the urgent contact] was acute dysphagia,” which was experienced as choking, throat pain, difficulty eating, reflux, and vomiting, the researchers observed. Dysphagia affected children in 27 of the contacts (26.5%), and resulted in esophageal dilatation in 90% of the cases. Other reasons for urgent contact were skin infection (15.7% of contacts), uncontrolled pain (15.7% of the contacts), and eye problems (11.8%).
Esophageal dilatation
Strictures are just one of the esophageal manifestations of the disease, noted Anna Bruckner, MD, associate professor of dermatology and pediatrics in the department of dermatology at the University of Colorado at Denver, Aurora, during an oral presentation. Other possible manifestations include blisters and erosions, the formation of webs – a thin extension of esophageal tissue, perforations, and rupture. “These are primarily problems with dystrophic EB” but can occur with other EB subtypes, she noted.
“We don’t have great evidence” on whether the onset of esophageal strictures can be delayed or prevented, Dr. Bruckner observed. As for management, “fluoroscopy-guided balloon dilatation is probably best” for most patients, but the best procedural approach needs to be discussed on a patient-by-patient basis.
Citing a paper that documents her own experience on the use of esophageal dilatation in 24 children who underwent 231 fluoroscopy-guided balloon dilatation procedures, Dr. Bruckner noted that strictures were most commonly located in the proximal part of the esophagus, with a median distance of 13 cm down from the lips (J Pediatr Gastroenterol Nutr. 2018;67[6]:701-5).
The retrospective chart review reported by Dr. Bruckner showed that there were a median of seven dilatation procedures per patient, and 20 patients had repeated procedures at a median interval of 164 days. About 10% of procedures resulted in adverse events – mostly vomiting, pain, and fever – but there were no perforations or other serious effects, and the rate of subsequent hospitalization was 6.9%.
Dysphagia
Dysphagia was the predominant symptom caused by esophageal stricture in another dataset reported in a poster by Elena Pope, MD, MSc, of the Hospital for Sick Children at the University of Toronto, and colleagues.
Of 125 EB patients who had experienced at least 1 esophageal stricture episode, 497 esophageal stricture events were reported, and 85.5% of patients had difficulty swallowing at presentation, with 29.8% unable to swallow solids and 7.2% unable to swallow liquids. Other symptoms at presentation were painful swallowing (11%), food being stuck in the esophagus (8%), regurgitation (5%), coughing (4.8%), and dyspepsia (2.8%).
The aim of the retrospective, multicenter cohort study was to determine the prevalence of, and predisposing factors for, restenosis of esophageal strictures and factors that may predispose to restenosis. The study population consisted of 66 men and 59 women who had experienced their esophageal stricture at around ages 12-13 years. The majority (98.4%) had dystrophic EB, of which almost half (46.5%) had GS-RDEB.
The researchers found that the location of the esophageal stricture was important for restenosis, and that strictures occurring in the lower esophagus were 67.5% less likely to result in restenosis than if they occurred in the upper esophagus (P = .057; hazard ratio, 0.675).
A higher number of strictures was associated with a higher rate of restenosis, they reported. Indeed, patients who had two esophageal strictures had a 29.4% increased risk of restenosis, compared with those who had just one stricture (P = .038; HR, 1.294), and those with three or more strictures had an increased risk of 78.5%, compared with those having one stricture (P = .005; HR, 1.785).
Strictures longer than 1 cm also were associated with a greater (34.7%) risk of restenosis, compared with shorter strictures (P = .032; HR, 1.347). Various methods of resolving the stricture were used, from fluoroscopy-guided balloon dilatation to retro- or antegrade endoscopy. “Irrespective of method, dilatations are successful,” Dr. Pope and colleagues reported. The overall success of dilatation was 99.3%, with full dilatation achieved in almost all of the patients (96%). Of note is that there was a low risk (2.6%) of complications, they observed.
Medications were used in 46.8% of the patients, with the most popular choice being corticosteroids (90.3%), but the researchers noted that the “potential benefit of periprocedural corticosteroids use in decreasing the risk of restenosis needs further exploration.”
Dr. Bruckner had noted in her presentation that her group did not favor the use of periprocedural corticosteroids, but that antifibrotic therapy “could be attractive” for preventing future strictures.
Dr. Prodinger, Dr. Pope, and their colleagues did not provide disclosure information. Dr. Bruckner is the principal investigator for the Epidermolysis Bullosa Clinical Characterization and Outcomes Database. She disclosed the receipt of grants or research funding, honoraria, or consultation fees from a number of drug companies, as well as other support from the EB Research Partnership and the EB Medical Research Foundation.
SOURCES: Prodinger et al. EB 2020. Poster 3; Bruckner A et al. Pediatr Gastroenterol Nutr. 2018;67(6):701-5; Pope et al. EB 2020. Poster 8.
LONDON – A quarter of urgent contacts in 20 children with generalized severe recessive dystrophic epidermolysis bullosa (GS-RDEB) were tied to esophageal narrowing, according data from a 12-month review of electronic health records.
Urgent advice was sought 102 times outside of regular or scheduled appointments by the parents of 20 children with GS-RDEB, Christine Prodinger, MD, of the University Clinic of Dermatology at Paracelsus Medical University, Salzburg, Austria, and colleagues reported in a poster presentation at the EB World Congress, organized by the Dystrophic Epidermolysis Bullosa Association (DEBRA). The researchers looked at the records from the EB clinic at Great Ormond Street Hospital for Children NHS Foundation Trust, London, during April 2018–April 2019.
The mean number of urgent contacts with the specialist unit was 5.1 per patient per year, the researchers reported, with 24 of the 102 contacts (23.5%) resulting in the child being admitted to a hospital. Most of the contacts were made via email or telephone to EB nurses (94%), by contacts during home visits (3%), or in an appointment with the palliative or symptom care team (3%).
“The most common reason [for the urgent contact] was acute dysphagia,” which was experienced as choking, throat pain, difficulty eating, reflux, and vomiting, the researchers observed. Dysphagia affected children in 27 of the contacts (26.5%), and resulted in esophageal dilatation in 90% of the cases. Other reasons for urgent contact were skin infection (15.7% of contacts), uncontrolled pain (15.7% of the contacts), and eye problems (11.8%).
Esophageal dilatation
Strictures are just one of the esophageal manifestations of the disease, noted Anna Bruckner, MD, associate professor of dermatology and pediatrics in the department of dermatology at the University of Colorado at Denver, Aurora, during an oral presentation. Other possible manifestations include blisters and erosions, the formation of webs – a thin extension of esophageal tissue, perforations, and rupture. “These are primarily problems with dystrophic EB” but can occur with other EB subtypes, she noted.
“We don’t have great evidence” on whether the onset of esophageal strictures can be delayed or prevented, Dr. Bruckner observed. As for management, “fluoroscopy-guided balloon dilatation is probably best” for most patients, but the best procedural approach needs to be discussed on a patient-by-patient basis.
Citing a paper that documents her own experience on the use of esophageal dilatation in 24 children who underwent 231 fluoroscopy-guided balloon dilatation procedures, Dr. Bruckner noted that strictures were most commonly located in the proximal part of the esophagus, with a median distance of 13 cm down from the lips (J Pediatr Gastroenterol Nutr. 2018;67[6]:701-5).
The retrospective chart review reported by Dr. Bruckner showed that there were a median of seven dilatation procedures per patient, and 20 patients had repeated procedures at a median interval of 164 days. About 10% of procedures resulted in adverse events – mostly vomiting, pain, and fever – but there were no perforations or other serious effects, and the rate of subsequent hospitalization was 6.9%.
Dysphagia
Dysphagia was the predominant symptom caused by esophageal stricture in another dataset reported in a poster by Elena Pope, MD, MSc, of the Hospital for Sick Children at the University of Toronto, and colleagues.
Of 125 EB patients who had experienced at least 1 esophageal stricture episode, 497 esophageal stricture events were reported, and 85.5% of patients had difficulty swallowing at presentation, with 29.8% unable to swallow solids and 7.2% unable to swallow liquids. Other symptoms at presentation were painful swallowing (11%), food being stuck in the esophagus (8%), regurgitation (5%), coughing (4.8%), and dyspepsia (2.8%).
The aim of the retrospective, multicenter cohort study was to determine the prevalence of, and predisposing factors for, restenosis of esophageal strictures and factors that may predispose to restenosis. The study population consisted of 66 men and 59 women who had experienced their esophageal stricture at around ages 12-13 years. The majority (98.4%) had dystrophic EB, of which almost half (46.5%) had GS-RDEB.
The researchers found that the location of the esophageal stricture was important for restenosis, and that strictures occurring in the lower esophagus were 67.5% less likely to result in restenosis than if they occurred in the upper esophagus (P = .057; hazard ratio, 0.675).
A higher number of strictures was associated with a higher rate of restenosis, they reported. Indeed, patients who had two esophageal strictures had a 29.4% increased risk of restenosis, compared with those who had just one stricture (P = .038; HR, 1.294), and those with three or more strictures had an increased risk of 78.5%, compared with those having one stricture (P = .005; HR, 1.785).
Strictures longer than 1 cm also were associated with a greater (34.7%) risk of restenosis, compared with shorter strictures (P = .032; HR, 1.347). Various methods of resolving the stricture were used, from fluoroscopy-guided balloon dilatation to retro- or antegrade endoscopy. “Irrespective of method, dilatations are successful,” Dr. Pope and colleagues reported. The overall success of dilatation was 99.3%, with full dilatation achieved in almost all of the patients (96%). Of note is that there was a low risk (2.6%) of complications, they observed.
Medications were used in 46.8% of the patients, with the most popular choice being corticosteroids (90.3%), but the researchers noted that the “potential benefit of periprocedural corticosteroids use in decreasing the risk of restenosis needs further exploration.”
Dr. Bruckner had noted in her presentation that her group did not favor the use of periprocedural corticosteroids, but that antifibrotic therapy “could be attractive” for preventing future strictures.
Dr. Prodinger, Dr. Pope, and their colleagues did not provide disclosure information. Dr. Bruckner is the principal investigator for the Epidermolysis Bullosa Clinical Characterization and Outcomes Database. She disclosed the receipt of grants or research funding, honoraria, or consultation fees from a number of drug companies, as well as other support from the EB Research Partnership and the EB Medical Research Foundation.
SOURCES: Prodinger et al. EB 2020. Poster 3; Bruckner A et al. Pediatr Gastroenterol Nutr. 2018;67(6):701-5; Pope et al. EB 2020. Poster 8.
REPORTING FROM EB 2020