User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Bad behavior by medical trainees target of new proposal
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Some instances of unprofessional behavior by medical trainees are universally deemed egregious and worthy of discipline — for example, looking up a friend’s medical data after HIPAA training.
Conversely, some professionalism lapses may be widely thought of as a teaching and consoling moment, such as the human error involved in forgetting a scheduled repositioning of a patient.
But between the extremes is a vast gray area. To deal with those cases appropriately, Jason Wasserman, PhD, and colleagues propose a new framework by which to judge each infraction.
The framework draws from “just culture” concepts used to evaluate medical errors, Wasserman, associate professor of biomedical science at Oakland University William Beaumont School of Medicine in Rochester, Michigan, told Medscape Medical News. Such an approach takes into account the environment in which the error was made, the knowledge and intent of the person making the error, and the severity and consequences of the infraction so that trainees and institutions can learn from mistakes.
“Trainees by definition are not going to fully get it,” he explained. “By definition they’re not going to fully achieve professional expectations. So how can we respond to the things we need to respond to, but do it in a way that’s educational?”
Wasserman and coauthors’ framework for remediation, which they published February 20 in The New England Journal of Medicine, takes into account several questions: Was the expectation clear? Were there factors beyond the trainees› control? What were the trainees› intentions and did they understand the consequences? Did the person genuinely believe the action was inconsequential?
An example requiring discipline, the authors say, would be using a crib sheet during an exam. In that case the intent is clear, there is no defensible belief that the action is inconsequential, and there is a clear understanding the action is wrong.
But a response of “affirm, support, and advise” is more appropriate, for example, when a student’s alarm doesn’t go off after a power outage and they miss a mandatory meeting.
Wasserman points out that this framework won’t cover all situations.
“This is not an algorithm for answering your questions about what to do,” he said. “It’s an architecture for clarifying the discussion about that. It can really tease out all the threads that need to be considered to best respond to and correct the professionalism lapse, but do it in a way that is developmentally appropriate.”
A Core Competency
For two decades, professionalism has been considered a core competency of medical education. In 1999, the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties formalized it as such. In 2013, the Association of American Medical Colleges formally required related professionalism competencies.
However, identifying lapses has operated largely on an “I-know-it-when-I-see-it” basis, leading to widely varying remediation practices judged by a small number of faculty members or administrators.
The ideas outlined by Wasserman and colleagues are “a terrific application of the ‘just-culture’ framework,” according to Nicole Treadway, MD, a first-year primary care resident at Emory School of Medicine in Atlanta, Georgia.
At Emory, discussions of professionalism start from day 1 of medical school and the subject is revisited throughout training in small groups, Treadway told Medscape Medical News.
But, she said, as the authors point out, definitions of unprofessionalism are not always clear and the examples the authors put forward help put lapses in context.
The framework also allows for looking at mistakes in light of the stress trainees encounter and the greater chance of making a professionalism error in those situations, she noted.
In her own work, she says, because she is juggling both inpatient and outpatient care, she is finding it is easy to get behind on correspondence or communicating lab results or having follow-up conversations.
Those delays could be seen as lapses in professionalism, but under this framework, there may be system solutions or training opportunities to consider.
“We do need this organizational architecture, and I think it could serve us well in really helping us identify and appropriately respond to what we see regarding professionalism,” she said.
Framework Helps Standardize Thinking
She said having a universal framework also helps because while standards of professionalism are easier to monitor in a single medical school, when students scatter to other hospitals for clinical training, those hospitals may have different professionalism standards.
Wasserman agrees, saying, “This could be easily adopted in any environment where people deal with professionalism lapses. I don’t even think it’s necessarily relegated to trainees. It’s a great way to think about any kind of lapses, just as hospitals think about medical errors.”
He said the next step is presenting the framework at various medical schools for feedback and research to see whether the framework improves processes.
Potential criticism, he said, might come from those who say such a construct avoids punishing students who make errors.
“There will always be people who say we’re pandering to medical students whenever we worry about the learning environment,” he said. “There are old-school purists who say when people screw up you should punish them.”
But he adds healthcare broadly has moved past that thinking.
“People recognized 20 years ago or more from the standpoint of improving healthcare systems and safety that is a bad strategy. You’ll never get error-free humans working in your system, and what you have to do is consider how the system is functioning and think about ways to optimize the system so people can be their best within it.”
Wasserman and Treadway have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The fate of the ACA now rests with the U.S. Supreme Court
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
Consider toys as culprits in children with contact allergies
A variety of according to the results of a review of 25 published articles.
“In recent years the products have become a reflection of the compounds used frequently in manufacturing, including metals and plastic compounds,” wrote Justine Fenner, MD, and coauthors, from the departments of dermatology and pediatrics at the Icahn School of Medicine at Mount Sinai, New York,
In a study published in Contact Dermatitis, the researchers identified 25 articles describing dermatitis, rash, or eczema associated with a range of toy and play product terms including Nintendo, PlayStation, putty, glue, doll, game, car, bicycle, slime, iPad, and iPhone.
Overall, nickel was the most common allergen. Cases of nickel dermatitis were associated with laptops, videogame controllers, iPads, and cell phones. Cell phones were the most common electronics associated with contact dermatitis, which was observed on the cheek, periauricular area, and hand, as well as the breast in one case of a patient who kept her phone in her bra.
Other sources of metal allergens were identified in toy cars and costume jewelry, the researchers noted.
In addition, temporary tattoos have been associated with contact dermatitis in children, as have homemade “slime” products, which often contain not only borax or other household detergents, but also glue, shaving cream, or coloring.
However, identification of true allergic contact dermatitis from toys “requires both identification of the chemical contents of toys, which are proprietary in nature, and then epicutaneous allergy testing of these ingredients,” the researchers said.
The study findings were limited by several factors including the consideration only of English-language articles and of cases in children, which thus eliminates other potential cases, the researchers noted. However, the results suggest that dermatologists consider toys as a source of contact dermatitis in children, especially if the time to diagnosis is months to years, they said. “Additionally, it may be useful, as it was in several of the above cases, to have the patient bring in his or her favorite toys for the dermatologist to examine and help further understand the etiology of patient’s rash,” they noted. Moreover, “there is an unmet need for corporations to reveal the chemical ingredients of their toys when allergic contact dermatitis is suspected in order to properly evaluate the patient,” they added.
“Contact dermatitis has been underreported in children and constitutes an ongoing concern,” senior author Nanette Silverberg, MD, chief of pediatric dermatology for the Mount Sinai Health System, said in an interview.
“In particular, toy-related allergy is concerning due to the rise in allergen inclusion in common play items,” she commented. The current analysis identified many case reports of allergens that pediatric dermatologists are frequently seeing in their offices, notably metals such as nickel, she pointed out. “The allergen that always stands out ahead of others is nickel,” Dr. Silverberg said. “Nickel allergy affects about 25% of Americans, often starting in early childhood,” she said. “In the European Union, legislation has been passed to reduce nickel release from metals, which has resulted in less sensitization to nickel. We lack such legislation in the United States,” she added.
Other trending allergens include methylchloroisothiazolinone/methylisothiazolinone, which may be components of glue or other ingredients in some “slime” products, Dr. Silverberg said.
She advised clinicians to consider patch testing when addressing localized or persistent dermatitis in children. “Furthermore, consider toys as potential relevant allergens that should be modified in order to achieve skin improvement,” she said.
“Greater reporting of pediatric allergic contact dermatitis is needed,” Dr. Silverberg emphasized. “Additionally, surveillance and monitoring for trends in allergen exposures in toys and personal care items is required to analyze this ongoing concern of childhood,” she said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Fenner J et al. Contact Dermatitis. 2020 Feb 22. doi: 10.1111/cod.13500.
A variety of according to the results of a review of 25 published articles.
“In recent years the products have become a reflection of the compounds used frequently in manufacturing, including metals and plastic compounds,” wrote Justine Fenner, MD, and coauthors, from the departments of dermatology and pediatrics at the Icahn School of Medicine at Mount Sinai, New York,
In a study published in Contact Dermatitis, the researchers identified 25 articles describing dermatitis, rash, or eczema associated with a range of toy and play product terms including Nintendo, PlayStation, putty, glue, doll, game, car, bicycle, slime, iPad, and iPhone.
Overall, nickel was the most common allergen. Cases of nickel dermatitis were associated with laptops, videogame controllers, iPads, and cell phones. Cell phones were the most common electronics associated with contact dermatitis, which was observed on the cheek, periauricular area, and hand, as well as the breast in one case of a patient who kept her phone in her bra.
Other sources of metal allergens were identified in toy cars and costume jewelry, the researchers noted.
In addition, temporary tattoos have been associated with contact dermatitis in children, as have homemade “slime” products, which often contain not only borax or other household detergents, but also glue, shaving cream, or coloring.
However, identification of true allergic contact dermatitis from toys “requires both identification of the chemical contents of toys, which are proprietary in nature, and then epicutaneous allergy testing of these ingredients,” the researchers said.
The study findings were limited by several factors including the consideration only of English-language articles and of cases in children, which thus eliminates other potential cases, the researchers noted. However, the results suggest that dermatologists consider toys as a source of contact dermatitis in children, especially if the time to diagnosis is months to years, they said. “Additionally, it may be useful, as it was in several of the above cases, to have the patient bring in his or her favorite toys for the dermatologist to examine and help further understand the etiology of patient’s rash,” they noted. Moreover, “there is an unmet need for corporations to reveal the chemical ingredients of their toys when allergic contact dermatitis is suspected in order to properly evaluate the patient,” they added.
“Contact dermatitis has been underreported in children and constitutes an ongoing concern,” senior author Nanette Silverberg, MD, chief of pediatric dermatology for the Mount Sinai Health System, said in an interview.
“In particular, toy-related allergy is concerning due to the rise in allergen inclusion in common play items,” she commented. The current analysis identified many case reports of allergens that pediatric dermatologists are frequently seeing in their offices, notably metals such as nickel, she pointed out. “The allergen that always stands out ahead of others is nickel,” Dr. Silverberg said. “Nickel allergy affects about 25% of Americans, often starting in early childhood,” she said. “In the European Union, legislation has been passed to reduce nickel release from metals, which has resulted in less sensitization to nickel. We lack such legislation in the United States,” she added.
Other trending allergens include methylchloroisothiazolinone/methylisothiazolinone, which may be components of glue or other ingredients in some “slime” products, Dr. Silverberg said.
She advised clinicians to consider patch testing when addressing localized or persistent dermatitis in children. “Furthermore, consider toys as potential relevant allergens that should be modified in order to achieve skin improvement,” she said.
“Greater reporting of pediatric allergic contact dermatitis is needed,” Dr. Silverberg emphasized. “Additionally, surveillance and monitoring for trends in allergen exposures in toys and personal care items is required to analyze this ongoing concern of childhood,” she said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Fenner J et al. Contact Dermatitis. 2020 Feb 22. doi: 10.1111/cod.13500.
A variety of according to the results of a review of 25 published articles.
“In recent years the products have become a reflection of the compounds used frequently in manufacturing, including metals and plastic compounds,” wrote Justine Fenner, MD, and coauthors, from the departments of dermatology and pediatrics at the Icahn School of Medicine at Mount Sinai, New York,
In a study published in Contact Dermatitis, the researchers identified 25 articles describing dermatitis, rash, or eczema associated with a range of toy and play product terms including Nintendo, PlayStation, putty, glue, doll, game, car, bicycle, slime, iPad, and iPhone.
Overall, nickel was the most common allergen. Cases of nickel dermatitis were associated with laptops, videogame controllers, iPads, and cell phones. Cell phones were the most common electronics associated with contact dermatitis, which was observed on the cheek, periauricular area, and hand, as well as the breast in one case of a patient who kept her phone in her bra.
Other sources of metal allergens were identified in toy cars and costume jewelry, the researchers noted.
In addition, temporary tattoos have been associated with contact dermatitis in children, as have homemade “slime” products, which often contain not only borax or other household detergents, but also glue, shaving cream, or coloring.
However, identification of true allergic contact dermatitis from toys “requires both identification of the chemical contents of toys, which are proprietary in nature, and then epicutaneous allergy testing of these ingredients,” the researchers said.
The study findings were limited by several factors including the consideration only of English-language articles and of cases in children, which thus eliminates other potential cases, the researchers noted. However, the results suggest that dermatologists consider toys as a source of contact dermatitis in children, especially if the time to diagnosis is months to years, they said. “Additionally, it may be useful, as it was in several of the above cases, to have the patient bring in his or her favorite toys for the dermatologist to examine and help further understand the etiology of patient’s rash,” they noted. Moreover, “there is an unmet need for corporations to reveal the chemical ingredients of their toys when allergic contact dermatitis is suspected in order to properly evaluate the patient,” they added.
“Contact dermatitis has been underreported in children and constitutes an ongoing concern,” senior author Nanette Silverberg, MD, chief of pediatric dermatology for the Mount Sinai Health System, said in an interview.
“In particular, toy-related allergy is concerning due to the rise in allergen inclusion in common play items,” she commented. The current analysis identified many case reports of allergens that pediatric dermatologists are frequently seeing in their offices, notably metals such as nickel, she pointed out. “The allergen that always stands out ahead of others is nickel,” Dr. Silverberg said. “Nickel allergy affects about 25% of Americans, often starting in early childhood,” she said. “In the European Union, legislation has been passed to reduce nickel release from metals, which has resulted in less sensitization to nickel. We lack such legislation in the United States,” she added.
Other trending allergens include methylchloroisothiazolinone/methylisothiazolinone, which may be components of glue or other ingredients in some “slime” products, Dr. Silverberg said.
She advised clinicians to consider patch testing when addressing localized or persistent dermatitis in children. “Furthermore, consider toys as potential relevant allergens that should be modified in order to achieve skin improvement,” she said.
“Greater reporting of pediatric allergic contact dermatitis is needed,” Dr. Silverberg emphasized. “Additionally, surveillance and monitoring for trends in allergen exposures in toys and personal care items is required to analyze this ongoing concern of childhood,” she said.
The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Fenner J et al. Contact Dermatitis. 2020 Feb 22. doi: 10.1111/cod.13500.
FROM CONTACT DERMATITIS
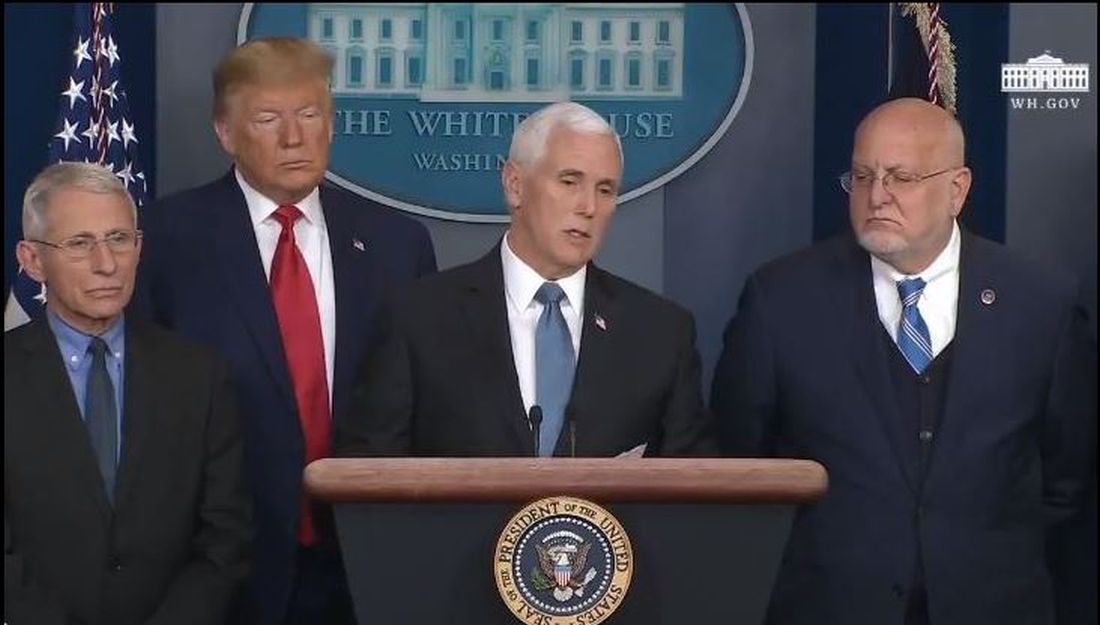
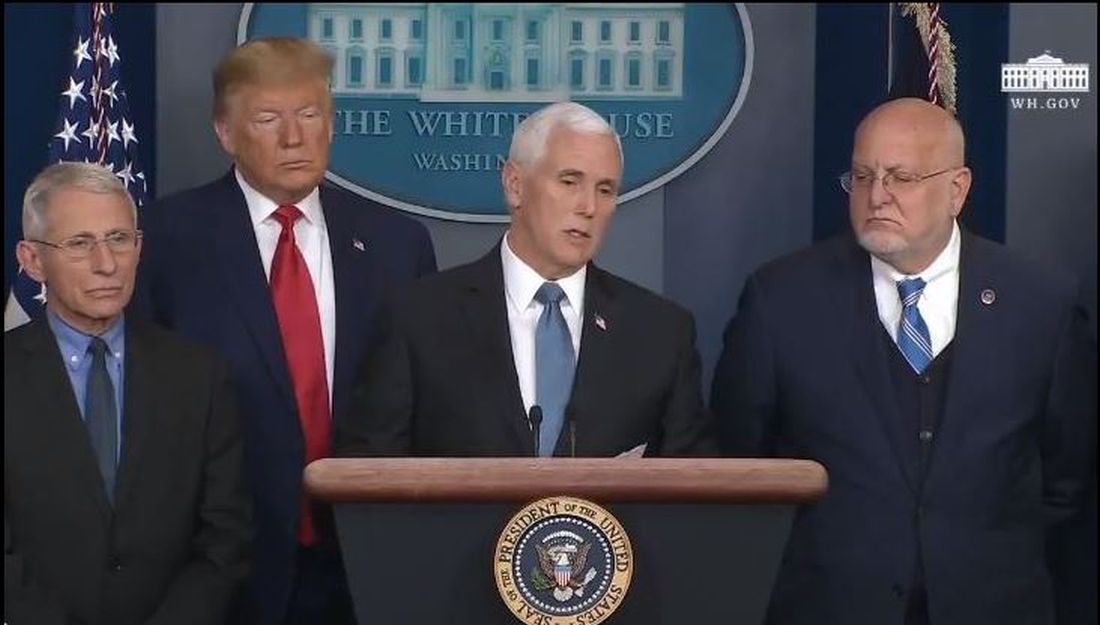
U.S. reports first death from COVID-19, possible outbreak at long-term care facility
The first death in the United States from the novel coronavirus (COVID-19) was a Washington state man in his 50s who had underlying health conditions, state health officials announced on Feb 29. At the same time, officials there are investigating a possible COVID-19 outbreak at a long-term care facility.
Washington state officials reported two other presumptive positive cases of COVID-19, both of whom are associated with LifeCare of Kirkland, Washington. One is a woman in her 70s who is a resident at the facility and the other is a woman in her 40s who is a health care worker at the facility.
Additionally, many residents and staff members at the facility have reported respiratory symptoms, according to Jeff Duchin, MD, health officer for public health in Seattle and King County. Among the more than 100 residents at the facility, 27 have respiratory symptoms; while among the 180 staff members, 25 have reported symptoms.
Overall, these reports bring the total number of U.S. COVID-19 cases detected by the public health system to 22, though that number is expected to climb as these investigations continue.
The general risk to the American public is still low, including residents in long-term care facilities, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during the Feb. 29 press briefing. Older people are are higher risk, however, and long-term care facilities should emphasize handwashing and the early identification of individuals with symptoms.
Dr. Duchin added that health care workers who are sick should stay home and that visitors should be screened for symptoms, the same advice offered to limit the spread of influenza at long-term care facilities.
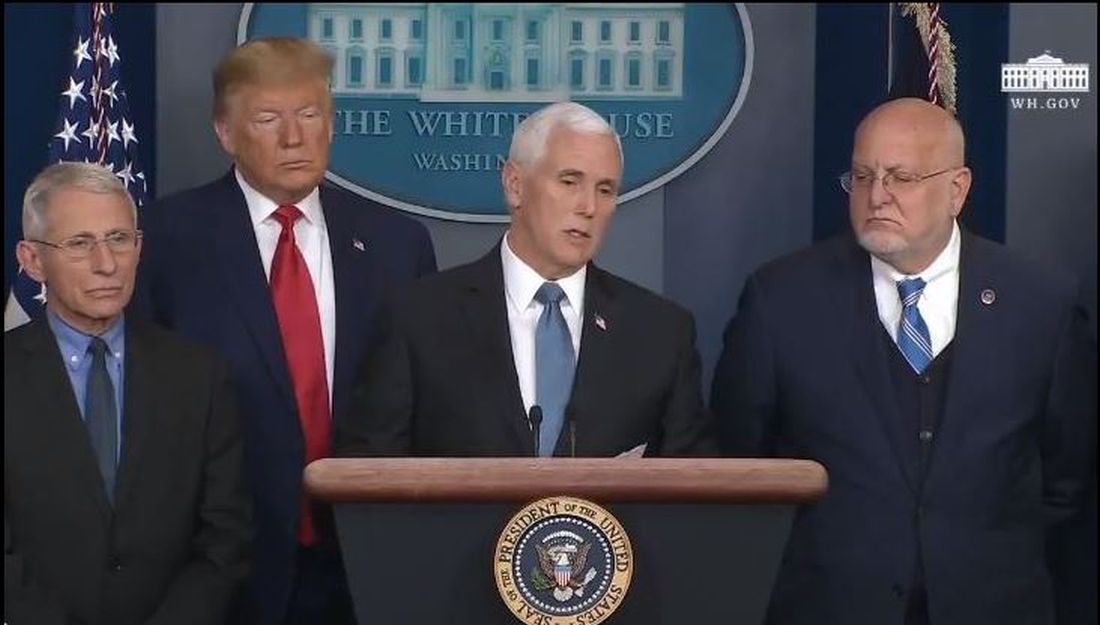
The CDC briefing comes after President Trump held his own press conference at the White House where he identified the person who had died as being a woman in her 50s who was medically at risk.
During that press conference, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said that the current pattern of disease with COVID-19 suggests that 75%-80% of patients will have mild illness and recover, while 15%-20% will require advanced medical care.
For the most part, the more serious cases will occur in those who are elderly or have underlying medical conditions. There is “no indication” that individuals who recover from the virus are becoming re-infected, Dr. Fauci said.
The administration also announced a series of actions aimed at slowing the spread of the virus and responding to it. On March 2, President Trump will meet with leaders in the pharmaceutical industry at the White House to discuss vaccine development. The administration is also working to ensure an adequate supply of face masks. Vice President Mike Pence said there are currently more than 40 million masks available, but that the administration has received promises of 35 million more masks per month from manufacturers. Access to masks will be prioritized for high-risk health care workers, Vice President Pence said. “The average American does not need to go out and buy a mask,” he added.
Additionally, Vice President Pence announced new travel restrictions with Iran that would bar entry to the United States for any foreign national who visited Iran in the last 14 days. The federal government is also advising Americans not to travel to the regions in Italy and South Korea that have been most affected by COVID-19. The government is also working with officials in Italy and South Korea to conduct medical screening of anyone coming into the United States from those countries.
The first death in the United States from the novel coronavirus (COVID-19) was a Washington state man in his 50s who had underlying health conditions, state health officials announced on Feb 29. At the same time, officials there are investigating a possible COVID-19 outbreak at a long-term care facility.
Washington state officials reported two other presumptive positive cases of COVID-19, both of whom are associated with LifeCare of Kirkland, Washington. One is a woman in her 70s who is a resident at the facility and the other is a woman in her 40s who is a health care worker at the facility.
Additionally, many residents and staff members at the facility have reported respiratory symptoms, according to Jeff Duchin, MD, health officer for public health in Seattle and King County. Among the more than 100 residents at the facility, 27 have respiratory symptoms; while among the 180 staff members, 25 have reported symptoms.
Overall, these reports bring the total number of U.S. COVID-19 cases detected by the public health system to 22, though that number is expected to climb as these investigations continue.
The general risk to the American public is still low, including residents in long-term care facilities, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during the Feb. 29 press briefing. Older people are are higher risk, however, and long-term care facilities should emphasize handwashing and the early identification of individuals with symptoms.
Dr. Duchin added that health care workers who are sick should stay home and that visitors should be screened for symptoms, the same advice offered to limit the spread of influenza at long-term care facilities.
The CDC briefing comes after President Trump held his own press conference at the White House where he identified the person who had died as being a woman in her 50s who was medically at risk.
During that press conference, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said that the current pattern of disease with COVID-19 suggests that 75%-80% of patients will have mild illness and recover, while 15%-20% will require advanced medical care.
For the most part, the more serious cases will occur in those who are elderly or have underlying medical conditions. There is “no indication” that individuals who recover from the virus are becoming re-infected, Dr. Fauci said.
The administration also announced a series of actions aimed at slowing the spread of the virus and responding to it. On March 2, President Trump will meet with leaders in the pharmaceutical industry at the White House to discuss vaccine development. The administration is also working to ensure an adequate supply of face masks. Vice President Mike Pence said there are currently more than 40 million masks available, but that the administration has received promises of 35 million more masks per month from manufacturers. Access to masks will be prioritized for high-risk health care workers, Vice President Pence said. “The average American does not need to go out and buy a mask,” he added.
Additionally, Vice President Pence announced new travel restrictions with Iran that would bar entry to the United States for any foreign national who visited Iran in the last 14 days. The federal government is also advising Americans not to travel to the regions in Italy and South Korea that have been most affected by COVID-19. The government is also working with officials in Italy and South Korea to conduct medical screening of anyone coming into the United States from those countries.
The first death in the United States from the novel coronavirus (COVID-19) was a Washington state man in his 50s who had underlying health conditions, state health officials announced on Feb 29. At the same time, officials there are investigating a possible COVID-19 outbreak at a long-term care facility.
Washington state officials reported two other presumptive positive cases of COVID-19, both of whom are associated with LifeCare of Kirkland, Washington. One is a woman in her 70s who is a resident at the facility and the other is a woman in her 40s who is a health care worker at the facility.
Additionally, many residents and staff members at the facility have reported respiratory symptoms, according to Jeff Duchin, MD, health officer for public health in Seattle and King County. Among the more than 100 residents at the facility, 27 have respiratory symptoms; while among the 180 staff members, 25 have reported symptoms.
Overall, these reports bring the total number of U.S. COVID-19 cases detected by the public health system to 22, though that number is expected to climb as these investigations continue.
The general risk to the American public is still low, including residents in long-term care facilities, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the Centers for Disease Control and Prevention, said during the Feb. 29 press briefing. Older people are are higher risk, however, and long-term care facilities should emphasize handwashing and the early identification of individuals with symptoms.
Dr. Duchin added that health care workers who are sick should stay home and that visitors should be screened for symptoms, the same advice offered to limit the spread of influenza at long-term care facilities.
The CDC briefing comes after President Trump held his own press conference at the White House where he identified the person who had died as being a woman in her 50s who was medically at risk.
During that press conference, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said that the current pattern of disease with COVID-19 suggests that 75%-80% of patients will have mild illness and recover, while 15%-20% will require advanced medical care.
For the most part, the more serious cases will occur in those who are elderly or have underlying medical conditions. There is “no indication” that individuals who recover from the virus are becoming re-infected, Dr. Fauci said.
The administration also announced a series of actions aimed at slowing the spread of the virus and responding to it. On March 2, President Trump will meet with leaders in the pharmaceutical industry at the White House to discuss vaccine development. The administration is also working to ensure an adequate supply of face masks. Vice President Mike Pence said there are currently more than 40 million masks available, but that the administration has received promises of 35 million more masks per month from manufacturers. Access to masks will be prioritized for high-risk health care workers, Vice President Pence said. “The average American does not need to go out and buy a mask,” he added.
Additionally, Vice President Pence announced new travel restrictions with Iran that would bar entry to the United States for any foreign national who visited Iran in the last 14 days. The federal government is also advising Americans not to travel to the regions in Italy and South Korea that have been most affected by COVID-19. The government is also working with officials in Italy and South Korea to conduct medical screening of anyone coming into the United States from those countries.
Isotretinoin data provide postmeal absorption guidance
LAHAINA, HAWAII – Recent , Hilary E. Baldwin, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
It is recommended that isotretinoin, which is fat-soluble, be taken with food, preferably high-fat foods. So it has been unclear what the effect would be when taken with lower-fat food, such as low-fat cereal and raspberries, for example, Dr. Baldwin, medical director of the Acne Treatment and Research Center in New York, pointed out.
“We’ve been trying for years to figure out how we’re going to get around this,” and there have not been any relevant data available until recently, other than in the setting of taking isotretinoin on an empty stomach or with a high-fat meal, she commented.
She referred to a open-label, single-dose, randomized crossover study that compared the bioavailability of the lidose formulation of isotretinoin (Absorica) and brand name Accutane, at a dose of 40 mg either on top of a fatty meal (the Food and Drug Administration-stipulated high-fat, high-calorie diet) or after a 10-hour fast; 60 patients did all four arms, with a 21-day washout period between them (J Am Acad Dermatol. 2013 Nov;69[5]:762-7).
In the fed state, both isotretinoin formulations were absorbed to the same extent, “but in the fasting state, there was a considerable difference,” Dr. Baldwin said. Absorption of both dropped in the fasting state, but the drop was more extreme with Accutane, “about a 50% difference between the two, in terms of how much drug was getting into the system,” she noted.
That is important because weight-based dosing is considered with isotretinoin, so at the end of treatment, a patient who has been taking it on an empty stomach may be getting a 60% lower dose than prescribed, “which could lead to a lessening of the effectiveness of the drug and also an increase in relapse over time.”
But how would a low-fat meal, like low-fat cereal and raspberries, affect the absorption, and ultimate efficacy?
This question was addressed in an open-label, single-arm study of 163 patients with acne, who were taking the lidose isotretinoin formulation without food, at the standard dose, for no longer than 20 weeks. Whether they relapsed was evaluated in a 2-year observational phase of the study, Dr. Baldwin said.
At the end of the trial, the drug was considered effective, with improvements in IGA (the 5-point Investigator’s Global Assessment scale). But the change from baseline was maintained at the 2-year posttreatment period, so the benefits of treatment lasted, which indicates that patients can take it “on top of absolutely no food whatsoever ... so if they eat anything, we are headed in the right direction,” including a low-fat meal. During the 2-year period, most patients did not need to be retreated. Of those people who needed treatment, only 4.2% needed treatment with isotretinoin, which is better than the historical relapse rates with isotretinoin, she noted.
Dr. Baldwin’s disclosures included being on the speakers’ bureau, serving as an advisor, and/or an investigator for companies that include Almirall, BioPharmx, Foamix, Galderma, Ortho Dermatologics, Sun Pharmaceuticals, Johnson & Johnson, and La Roche–Posay.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Recent , Hilary E. Baldwin, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
It is recommended that isotretinoin, which is fat-soluble, be taken with food, preferably high-fat foods. So it has been unclear what the effect would be when taken with lower-fat food, such as low-fat cereal and raspberries, for example, Dr. Baldwin, medical director of the Acne Treatment and Research Center in New York, pointed out.
“We’ve been trying for years to figure out how we’re going to get around this,” and there have not been any relevant data available until recently, other than in the setting of taking isotretinoin on an empty stomach or with a high-fat meal, she commented.
She referred to a open-label, single-dose, randomized crossover study that compared the bioavailability of the lidose formulation of isotretinoin (Absorica) and brand name Accutane, at a dose of 40 mg either on top of a fatty meal (the Food and Drug Administration-stipulated high-fat, high-calorie diet) or after a 10-hour fast; 60 patients did all four arms, with a 21-day washout period between them (J Am Acad Dermatol. 2013 Nov;69[5]:762-7).
In the fed state, both isotretinoin formulations were absorbed to the same extent, “but in the fasting state, there was a considerable difference,” Dr. Baldwin said. Absorption of both dropped in the fasting state, but the drop was more extreme with Accutane, “about a 50% difference between the two, in terms of how much drug was getting into the system,” she noted.
That is important because weight-based dosing is considered with isotretinoin, so at the end of treatment, a patient who has been taking it on an empty stomach may be getting a 60% lower dose than prescribed, “which could lead to a lessening of the effectiveness of the drug and also an increase in relapse over time.”
But how would a low-fat meal, like low-fat cereal and raspberries, affect the absorption, and ultimate efficacy?
This question was addressed in an open-label, single-arm study of 163 patients with acne, who were taking the lidose isotretinoin formulation without food, at the standard dose, for no longer than 20 weeks. Whether they relapsed was evaluated in a 2-year observational phase of the study, Dr. Baldwin said.
At the end of the trial, the drug was considered effective, with improvements in IGA (the 5-point Investigator’s Global Assessment scale). But the change from baseline was maintained at the 2-year posttreatment period, so the benefits of treatment lasted, which indicates that patients can take it “on top of absolutely no food whatsoever ... so if they eat anything, we are headed in the right direction,” including a low-fat meal. During the 2-year period, most patients did not need to be retreated. Of those people who needed treatment, only 4.2% needed treatment with isotretinoin, which is better than the historical relapse rates with isotretinoin, she noted.
Dr. Baldwin’s disclosures included being on the speakers’ bureau, serving as an advisor, and/or an investigator for companies that include Almirall, BioPharmx, Foamix, Galderma, Ortho Dermatologics, Sun Pharmaceuticals, Johnson & Johnson, and La Roche–Posay.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Recent , Hilary E. Baldwin, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
It is recommended that isotretinoin, which is fat-soluble, be taken with food, preferably high-fat foods. So it has been unclear what the effect would be when taken with lower-fat food, such as low-fat cereal and raspberries, for example, Dr. Baldwin, medical director of the Acne Treatment and Research Center in New York, pointed out.
“We’ve been trying for years to figure out how we’re going to get around this,” and there have not been any relevant data available until recently, other than in the setting of taking isotretinoin on an empty stomach or with a high-fat meal, she commented.
She referred to a open-label, single-dose, randomized crossover study that compared the bioavailability of the lidose formulation of isotretinoin (Absorica) and brand name Accutane, at a dose of 40 mg either on top of a fatty meal (the Food and Drug Administration-stipulated high-fat, high-calorie diet) or after a 10-hour fast; 60 patients did all four arms, with a 21-day washout period between them (J Am Acad Dermatol. 2013 Nov;69[5]:762-7).
In the fed state, both isotretinoin formulations were absorbed to the same extent, “but in the fasting state, there was a considerable difference,” Dr. Baldwin said. Absorption of both dropped in the fasting state, but the drop was more extreme with Accutane, “about a 50% difference between the two, in terms of how much drug was getting into the system,” she noted.
That is important because weight-based dosing is considered with isotretinoin, so at the end of treatment, a patient who has been taking it on an empty stomach may be getting a 60% lower dose than prescribed, “which could lead to a lessening of the effectiveness of the drug and also an increase in relapse over time.”
But how would a low-fat meal, like low-fat cereal and raspberries, affect the absorption, and ultimate efficacy?
This question was addressed in an open-label, single-arm study of 163 patients with acne, who were taking the lidose isotretinoin formulation without food, at the standard dose, for no longer than 20 weeks. Whether they relapsed was evaluated in a 2-year observational phase of the study, Dr. Baldwin said.
At the end of the trial, the drug was considered effective, with improvements in IGA (the 5-point Investigator’s Global Assessment scale). But the change from baseline was maintained at the 2-year posttreatment period, so the benefits of treatment lasted, which indicates that patients can take it “on top of absolutely no food whatsoever ... so if they eat anything, we are headed in the right direction,” including a low-fat meal. During the 2-year period, most patients did not need to be retreated. Of those people who needed treatment, only 4.2% needed treatment with isotretinoin, which is better than the historical relapse rates with isotretinoin, she noted.
Dr. Baldwin’s disclosures included being on the speakers’ bureau, serving as an advisor, and/or an investigator for companies that include Almirall, BioPharmx, Foamix, Galderma, Ortho Dermatologics, Sun Pharmaceuticals, Johnson & Johnson, and La Roche–Posay.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
CDC revises COVID-19 test kits, broadens ‘person under investigation’ definition
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
REPORTING FROM A CDC BRIEFING
Keep your eye on tapinarof, a topical antipsoriatic therapy
LAHAINA, HAWAII – Tapinarof is an investigational drug whose novel mechanism of action – and encouraging performance in phase 2 studies – are making waves for the topical treatment of both psoriasis and atopic dermatitis, Linda F. Stein Gold, MD, observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Tapinarof is a first-in-class agonist of the aryl hydrocarbon receptor.
“An aryl hydrocarbon receptor agonist – what in the world does that mean? It means that this drug actually acts at the receptor level inside the cell, and it does a lot of different things,” explained Dr. Stein Gold, director of dermatology clinical research at the Henry Ford Health System in Detroit.
For one, tapinarof down-regulates Th17 cytokines, an attribute that positions the drug very well as a potential topical treatment for psoriasis. But in addition, the drug has a skin barrier repair element through up-regulation of the filaggrin and involucrin genes in keratinocytes, and it also down-regulates Th2 cytokines, actions desirable in a treatment for atopic dermatitis.
Dr. Stein Gold focused mainly on tapinarof’s potential as a novel treatment for psoriasis, a disease that hasn’t seen approval of a new nonsteroidal topical therapy in decades. There is a huge unmet need for safe and effective new topical therapies for this disease; despite all the attention devoted to biologics and other systemic therapies, the great majority of psoriasis patients are managed via topical therapy only.
The definitive trial was initiated based upon the results of a phase 2b, double-blind, six-arm study including 141 adults with body surface involvement of 1%-15% and a baseline Physician Global Assessment (PGA) score of 2 or more who were assigned to tapinarof at 0.5% or 1% once or twice daily or placebo. The phase 2b results, she commented, were very encouraging.
“When we look at the clinical efficacy, it looks like this drug has legs. It does work even as monotherapy to get patients clear,” she said.
The phase 2b, dose-finding study showed dose-dependent treatment efficacy. At week 12, the proportion of participants with a PGA of 0-1 and at least a 2-grade improvement – that is, clear or almost clear – was 36% with tapinarof monotherapy at 0.5% once daily, 46% with 0.5% twice daily, 56% with 1% once daily, and 65% with 1% twice daily, compared with 5% in controls on once-daily application of vehicle and 11% with twice-daily vehicle. Moreover, the improvement was maintained for 4 weeks post treatment. The drug was well tolerated other than some mild to moderate folliculitis and contact dermatitis (J Am Acad Dermatol. 2019 Mar;80[3]:714-21).
“With such small numbers in phase 2, we don’t necessarily need to see statistical significance, but we want to see a trend in the right direction. But every one of the active treatment arms was statistically significantly better than with vehicle. And at higher concentrations, greater efficacy,” noted Dr. Stein Gold.
A phase 2 study of tapinarof cream has also been completed in adults and adolescents with atopic dermatitis, again with positive results. A phase 3 study in atopic dermatitis is still in the planning stages.
Dr. Stein Gold wasn’t involved in the tapinarof psoriasis phase 2b study, sponsored by GlaxoSmithKline. She reported research funding from nine other pharmaceutical companies and serves as a consultant and/or scientific to more than a dozen companies.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Tapinarof is an investigational drug whose novel mechanism of action – and encouraging performance in phase 2 studies – are making waves for the topical treatment of both psoriasis and atopic dermatitis, Linda F. Stein Gold, MD, observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Tapinarof is a first-in-class agonist of the aryl hydrocarbon receptor.
“An aryl hydrocarbon receptor agonist – what in the world does that mean? It means that this drug actually acts at the receptor level inside the cell, and it does a lot of different things,” explained Dr. Stein Gold, director of dermatology clinical research at the Henry Ford Health System in Detroit.
For one, tapinarof down-regulates Th17 cytokines, an attribute that positions the drug very well as a potential topical treatment for psoriasis. But in addition, the drug has a skin barrier repair element through up-regulation of the filaggrin and involucrin genes in keratinocytes, and it also down-regulates Th2 cytokines, actions desirable in a treatment for atopic dermatitis.
Dr. Stein Gold focused mainly on tapinarof’s potential as a novel treatment for psoriasis, a disease that hasn’t seen approval of a new nonsteroidal topical therapy in decades. There is a huge unmet need for safe and effective new topical therapies for this disease; despite all the attention devoted to biologics and other systemic therapies, the great majority of psoriasis patients are managed via topical therapy only.
The definitive trial was initiated based upon the results of a phase 2b, double-blind, six-arm study including 141 adults with body surface involvement of 1%-15% and a baseline Physician Global Assessment (PGA) score of 2 or more who were assigned to tapinarof at 0.5% or 1% once or twice daily or placebo. The phase 2b results, she commented, were very encouraging.
“When we look at the clinical efficacy, it looks like this drug has legs. It does work even as monotherapy to get patients clear,” she said.
The phase 2b, dose-finding study showed dose-dependent treatment efficacy. At week 12, the proportion of participants with a PGA of 0-1 and at least a 2-grade improvement – that is, clear or almost clear – was 36% with tapinarof monotherapy at 0.5% once daily, 46% with 0.5% twice daily, 56% with 1% once daily, and 65% with 1% twice daily, compared with 5% in controls on once-daily application of vehicle and 11% with twice-daily vehicle. Moreover, the improvement was maintained for 4 weeks post treatment. The drug was well tolerated other than some mild to moderate folliculitis and contact dermatitis (J Am Acad Dermatol. 2019 Mar;80[3]:714-21).
“With such small numbers in phase 2, we don’t necessarily need to see statistical significance, but we want to see a trend in the right direction. But every one of the active treatment arms was statistically significantly better than with vehicle. And at higher concentrations, greater efficacy,” noted Dr. Stein Gold.
A phase 2 study of tapinarof cream has also been completed in adults and adolescents with atopic dermatitis, again with positive results. A phase 3 study in atopic dermatitis is still in the planning stages.
Dr. Stein Gold wasn’t involved in the tapinarof psoriasis phase 2b study, sponsored by GlaxoSmithKline. She reported research funding from nine other pharmaceutical companies and serves as a consultant and/or scientific to more than a dozen companies.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Tapinarof is an investigational drug whose novel mechanism of action – and encouraging performance in phase 2 studies – are making waves for the topical treatment of both psoriasis and atopic dermatitis, Linda F. Stein Gold, MD, observed at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
Tapinarof is a first-in-class agonist of the aryl hydrocarbon receptor.
“An aryl hydrocarbon receptor agonist – what in the world does that mean? It means that this drug actually acts at the receptor level inside the cell, and it does a lot of different things,” explained Dr. Stein Gold, director of dermatology clinical research at the Henry Ford Health System in Detroit.
For one, tapinarof down-regulates Th17 cytokines, an attribute that positions the drug very well as a potential topical treatment for psoriasis. But in addition, the drug has a skin barrier repair element through up-regulation of the filaggrin and involucrin genes in keratinocytes, and it also down-regulates Th2 cytokines, actions desirable in a treatment for atopic dermatitis.
Dr. Stein Gold focused mainly on tapinarof’s potential as a novel treatment for psoriasis, a disease that hasn’t seen approval of a new nonsteroidal topical therapy in decades. There is a huge unmet need for safe and effective new topical therapies for this disease; despite all the attention devoted to biologics and other systemic therapies, the great majority of psoriasis patients are managed via topical therapy only.
The definitive trial was initiated based upon the results of a phase 2b, double-blind, six-arm study including 141 adults with body surface involvement of 1%-15% and a baseline Physician Global Assessment (PGA) score of 2 or more who were assigned to tapinarof at 0.5% or 1% once or twice daily or placebo. The phase 2b results, she commented, were very encouraging.
“When we look at the clinical efficacy, it looks like this drug has legs. It does work even as monotherapy to get patients clear,” she said.
The phase 2b, dose-finding study showed dose-dependent treatment efficacy. At week 12, the proportion of participants with a PGA of 0-1 and at least a 2-grade improvement – that is, clear or almost clear – was 36% with tapinarof monotherapy at 0.5% once daily, 46% with 0.5% twice daily, 56% with 1% once daily, and 65% with 1% twice daily, compared with 5% in controls on once-daily application of vehicle and 11% with twice-daily vehicle. Moreover, the improvement was maintained for 4 weeks post treatment. The drug was well tolerated other than some mild to moderate folliculitis and contact dermatitis (J Am Acad Dermatol. 2019 Mar;80[3]:714-21).
“With such small numbers in phase 2, we don’t necessarily need to see statistical significance, but we want to see a trend in the right direction. But every one of the active treatment arms was statistically significantly better than with vehicle. And at higher concentrations, greater efficacy,” noted Dr. Stein Gold.
A phase 2 study of tapinarof cream has also been completed in adults and adolescents with atopic dermatitis, again with positive results. A phase 3 study in atopic dermatitis is still in the planning stages.
Dr. Stein Gold wasn’t involved in the tapinarof psoriasis phase 2b study, sponsored by GlaxoSmithKline. She reported research funding from nine other pharmaceutical companies and serves as a consultant and/or scientific to more than a dozen companies.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
REPORTING FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
Studies add clarity to link between rosacea and Demodex, coffee
LAHAINA, HAWAII – Recent data on the roles of caffeinated coffee and two types of Demodex species play in rosacea were discussed by Linda Stein Gold, MD, at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
When considering rosacea triggers, the role of coffee has been difficult to determine, according to Dr. Stein Gold, director of dermatology research at the Henry Ford Health System in Detroit.
“We know that caffeine can vasoconstrict, it also has anti-inflammatory properties so ... that might help rosacea,” while the heat from a hot cup of coffee may cause vasodilation “and make rosacea worse,” she noted.
But a recent study of data from the Nurses’ Health Study II that evaluated intake of coffee, tea, soda, and chocolate every 4 years in over 82,000 women shed some light on the role coffee may play (JAMA Dermatol. 2018 Dec 1;154[12]:1394-1400). There were almost 5,000 cases of physician-diagnosed rosacea in the cohort. When the investigators looked at caffeinated coffee consumption, she said.
Those who consumed four or more servings of caffeinated coffee a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001).
But there was no significant association with decaffeinated coffee or with edibles that contained caffeine such as tea, soda, and chocolate, “so something about caffeinated coffee seems to be protective for the development of rosacea,” Dr. Stein Gold said.
Demodex mites
A few years ago, “we really didn’t think much of Demodex, but now we know Demodex tends to be a key player” in people with rosacea, Dr. Stein Gold said.
In adults, the colonization rate of Demodex ranges from 70% to 100%, but the skin of people with rosacea have a particularly high density of Demodex: About 35%-50% of patients with rosacea have an increased Demodex load above 5 mites per cm2, as measured with a standard skin surface biopsy, she noted. The density of Demodex in the skin of patients with rosacea has been measured at sixfold higher, compared with age-matched controls.
There also are two different Demodex species: Demodex folliculorum, which are longer, and Demodex brevis, which are short, and there is evidence that each “may cause an individual reaction,” Dr. Stein Gold said.
She referred to a study that found a difference in the Demodex population in patients with highly inflammatory disease with a high level of Demodex, mild rosacea patients who did not have a lot of Demodex, and people with no rosacea (Dermatol Reports. 2019 Jan 23;11[1]:7675).
“Those people who had really severe, inflammatory rosacea had Demodex folliculorum,” and the patients with the more mild disease or those with clear skin had Demodex brevis, she said, so “different species of Demodex might cause a different inflammatory reaction within individual rosacea patients.”
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant (now Bausch Health), Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Recent data on the roles of caffeinated coffee and two types of Demodex species play in rosacea were discussed by Linda Stein Gold, MD, at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
When considering rosacea triggers, the role of coffee has been difficult to determine, according to Dr. Stein Gold, director of dermatology research at the Henry Ford Health System in Detroit.
“We know that caffeine can vasoconstrict, it also has anti-inflammatory properties so ... that might help rosacea,” while the heat from a hot cup of coffee may cause vasodilation “and make rosacea worse,” she noted.
But a recent study of data from the Nurses’ Health Study II that evaluated intake of coffee, tea, soda, and chocolate every 4 years in over 82,000 women shed some light on the role coffee may play (JAMA Dermatol. 2018 Dec 1;154[12]:1394-1400). There were almost 5,000 cases of physician-diagnosed rosacea in the cohort. When the investigators looked at caffeinated coffee consumption, she said.
Those who consumed four or more servings of caffeinated coffee a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001).
But there was no significant association with decaffeinated coffee or with edibles that contained caffeine such as tea, soda, and chocolate, “so something about caffeinated coffee seems to be protective for the development of rosacea,” Dr. Stein Gold said.
Demodex mites
A few years ago, “we really didn’t think much of Demodex, but now we know Demodex tends to be a key player” in people with rosacea, Dr. Stein Gold said.
In adults, the colonization rate of Demodex ranges from 70% to 100%, but the skin of people with rosacea have a particularly high density of Demodex: About 35%-50% of patients with rosacea have an increased Demodex load above 5 mites per cm2, as measured with a standard skin surface biopsy, she noted. The density of Demodex in the skin of patients with rosacea has been measured at sixfold higher, compared with age-matched controls.
There also are two different Demodex species: Demodex folliculorum, which are longer, and Demodex brevis, which are short, and there is evidence that each “may cause an individual reaction,” Dr. Stein Gold said.
She referred to a study that found a difference in the Demodex population in patients with highly inflammatory disease with a high level of Demodex, mild rosacea patients who did not have a lot of Demodex, and people with no rosacea (Dermatol Reports. 2019 Jan 23;11[1]:7675).
“Those people who had really severe, inflammatory rosacea had Demodex folliculorum,” and the patients with the more mild disease or those with clear skin had Demodex brevis, she said, so “different species of Demodex might cause a different inflammatory reaction within individual rosacea patients.”
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant (now Bausch Health), Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
LAHAINA, HAWAII – Recent data on the roles of caffeinated coffee and two types of Demodex species play in rosacea were discussed by Linda Stein Gold, MD, at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
When considering rosacea triggers, the role of coffee has been difficult to determine, according to Dr. Stein Gold, director of dermatology research at the Henry Ford Health System in Detroit.
“We know that caffeine can vasoconstrict, it also has anti-inflammatory properties so ... that might help rosacea,” while the heat from a hot cup of coffee may cause vasodilation “and make rosacea worse,” she noted.
But a recent study of data from the Nurses’ Health Study II that evaluated intake of coffee, tea, soda, and chocolate every 4 years in over 82,000 women shed some light on the role coffee may play (JAMA Dermatol. 2018 Dec 1;154[12]:1394-1400). There were almost 5,000 cases of physician-diagnosed rosacea in the cohort. When the investigators looked at caffeinated coffee consumption, she said.
Those who consumed four or more servings of caffeinated coffee a day had a significantly lower risk of rosacea, compared with those who consumed one or fewer servings per month (hazard ratio, 0.77; 95% confidence interval, 0.69-0.87; P less than .001).
But there was no significant association with decaffeinated coffee or with edibles that contained caffeine such as tea, soda, and chocolate, “so something about caffeinated coffee seems to be protective for the development of rosacea,” Dr. Stein Gold said.
Demodex mites
A few years ago, “we really didn’t think much of Demodex, but now we know Demodex tends to be a key player” in people with rosacea, Dr. Stein Gold said.
In adults, the colonization rate of Demodex ranges from 70% to 100%, but the skin of people with rosacea have a particularly high density of Demodex: About 35%-50% of patients with rosacea have an increased Demodex load above 5 mites per cm2, as measured with a standard skin surface biopsy, she noted. The density of Demodex in the skin of patients with rosacea has been measured at sixfold higher, compared with age-matched controls.
There also are two different Demodex species: Demodex folliculorum, which are longer, and Demodex brevis, which are short, and there is evidence that each “may cause an individual reaction,” Dr. Stein Gold said.
She referred to a study that found a difference in the Demodex population in patients with highly inflammatory disease with a high level of Demodex, mild rosacea patients who did not have a lot of Demodex, and people with no rosacea (Dermatol Reports. 2019 Jan 23;11[1]:7675).
“Those people who had really severe, inflammatory rosacea had Demodex folliculorum,” and the patients with the more mild disease or those with clear skin had Demodex brevis, she said, so “different species of Demodex might cause a different inflammatory reaction within individual rosacea patients.”
Dr. Stein Gold reported that she has served as a consultant, investigator, or speaker for Galderma, Dermira, Foamix Pharmaceuticals, Valeant (now Bausch Health), Allergan, Actavis, and Roche.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Data overwhelmingly support use of dermoscopy in practice
LAHAINA, HAWAII – Multiple but there are still some “nonbelievers,” Ashfaq A. Marghoob, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
In fact, not one study has shown that dermoscopy is less sensitive than the naked eye alone, and at clinics where dermoscopy is used, “two-thirds of the melanomas being detected now lack the classic ABCD features of melanoma,” added Dr. Marghoob, director of clinical dermatology at Memorial Sloan Kettering in Hauppauge, N.Y.
Dr. Marghoob cited a meta-analysis of 9 prospective trials, which concluded that dermoscopy was more accurate in diagnosing melanoma than the naked eye alone and did not lower specificity, with a sensitivity and specificity of 90%, compared with 71% and 81%, respectively for the naked eye (Br J Dermatol. 2008 Sep;159[3]:669-76).
“And at least from an evidence-based standpoint ... the Cochrane library has basically endorsed that, yes, dermoscopy does indeed improve your diagnostic accuracy,” Dr. Marghoob said.
He referred to a 2018 Cochrane review on 104 dermoscopy studies, with and without visual inspection, for diagnosing melanoma in adults (Cochrane Database Syst Rev. 2018 Dec 4;12:CD011902). The review authors concluded that “the evidence suggests that melanomas will be missed if visual inspection is used on its own,” and despite limitations in the evidence, “dermoscopy is a valuable tool to support the visual inspection of a suspicious skin lesion for the detection of melanoma and atypical intraepidermal melanocytic variants.”
As for the question of specificity, Dr. Marghoob said studies have found that dermoscopy results in the detection of more melanomas and reduces the number of biopsies of benign lesions and “every study looking into this has shown that, yes, it does improve” specificity.
A 10-year multicenter survey of about 300,000 cases, which included 17,172 melanomas and 283,043 melanocytic nevi, found that the number-needed-to-excise (NNE) values improved over time in specialized clinics where newer diagnostic techniques like dermoscopy were used (from 12.8 to 6.8), but the NNE did not appear to change in the nonspecialized settings (J Am Acad Dermatol. 2012 Jul;67[1]:54-9).
Looking at the benign-to-malignant ratio, there was no change among those not using dermoscopy, where the ratio remained at about 30 to 1. When dermoscopy was used, this ratio started to improve over the 10-year period, to about 5 to 1. In addition, “the dermoscopy users were finding many more melanomas than the non–dermoscopy users,” Dr. Marghoob added. And over the 10 years, the number of nevi being removed did not change among those not using dermoscopy but dropped among those using dermoscopy.
Adding photography with the ability to digitally monitor patients helps bring this ratio down further, Dr. Marghoob noted. He referred to a study that instead evaluated the ratio of melanoma to nonmelanomas diagnosed among dermatologists in three groups: those with no digital dermoscopy with little dermoscopy training (group A, the reference group), no digital dermoscopy but more dermoscopy training (group B), and those using digital dermoscopy (group C). In the group that used digital dermoscopy, that ratio was about 1 to 2.4, compared with about 1 to 8 in group B, and about 1 to 10.7 in group A (Br J Dermatol. 2012;167[4]778-86).
The use of dermoscopy is also associated with thinner tumors. Among dermoscopy users, the thickness of the tumors detected drops, and the proportion of thin to thick lesions detected increases, Dr. Marghoob said.
For example, in one study, the mean thickness in melanomas detected with dermoscopy was 1.4 mm versus 2.59 mm when dermoscopy was not used (J Eur Acad Dermatol Venereol. 2015 Jan; 29[1]:102-8). About 55% of the tumors detected with dermoscopic examination were 1 mm or less in thickness versus 23.4% of those detected without dermoscopy, “so the dermoscopy users from a proportion standpoint were also finding thinner tumors,” Dr. Marghoob said. Dermoscopy was also identified as an independent predictor of finding thinner tumors.
Even without a study, it could be assumed that the use of dermoscopy would reduce costs, since dermoscopy increases sensitivity and the total number of melanomas detected, decreases the number of benign nevi removed, and helps detect disease earlier. But there are data showing that dermoscopy reduces health care costs, Dr. Marghoob said.* For example, a Belgian study that looked at dermoscopy in two cohorts of melanoma patients concluded that adequate dermoscopy training was cost effective (Eur J Cancer. 2016 Nov;67:38-45).
It has also been shown that adding dermoscopy to a primary care setting has cost benefits, Dr. Marghoob said. He cited a study of Dutch general practices that found that the probability of a correct diagnosis was 1.25 times higher when dermoscopy was used to evaluate suspicious skin lesions and concluded that the use of dermoscopy appeared to be cost effective (J Eur Acad Dermatol Venereol. 2014 Nov;28[11]:1442-9).
Dr. Marghoob had no disclosures relevant to this presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
*Correction, 2/28/20: An earlier version of this article mischaracterized the cost implications of dermoscopy use.
LAHAINA, HAWAII – Multiple but there are still some “nonbelievers,” Ashfaq A. Marghoob, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
In fact, not one study has shown that dermoscopy is less sensitive than the naked eye alone, and at clinics where dermoscopy is used, “two-thirds of the melanomas being detected now lack the classic ABCD features of melanoma,” added Dr. Marghoob, director of clinical dermatology at Memorial Sloan Kettering in Hauppauge, N.Y.
Dr. Marghoob cited a meta-analysis of 9 prospective trials, which concluded that dermoscopy was more accurate in diagnosing melanoma than the naked eye alone and did not lower specificity, with a sensitivity and specificity of 90%, compared with 71% and 81%, respectively for the naked eye (Br J Dermatol. 2008 Sep;159[3]:669-76).
“And at least from an evidence-based standpoint ... the Cochrane library has basically endorsed that, yes, dermoscopy does indeed improve your diagnostic accuracy,” Dr. Marghoob said.
He referred to a 2018 Cochrane review on 104 dermoscopy studies, with and without visual inspection, for diagnosing melanoma in adults (Cochrane Database Syst Rev. 2018 Dec 4;12:CD011902). The review authors concluded that “the evidence suggests that melanomas will be missed if visual inspection is used on its own,” and despite limitations in the evidence, “dermoscopy is a valuable tool to support the visual inspection of a suspicious skin lesion for the detection of melanoma and atypical intraepidermal melanocytic variants.”
As for the question of specificity, Dr. Marghoob said studies have found that dermoscopy results in the detection of more melanomas and reduces the number of biopsies of benign lesions and “every study looking into this has shown that, yes, it does improve” specificity.
A 10-year multicenter survey of about 300,000 cases, which included 17,172 melanomas and 283,043 melanocytic nevi, found that the number-needed-to-excise (NNE) values improved over time in specialized clinics where newer diagnostic techniques like dermoscopy were used (from 12.8 to 6.8), but the NNE did not appear to change in the nonspecialized settings (J Am Acad Dermatol. 2012 Jul;67[1]:54-9).
Looking at the benign-to-malignant ratio, there was no change among those not using dermoscopy, where the ratio remained at about 30 to 1. When dermoscopy was used, this ratio started to improve over the 10-year period, to about 5 to 1. In addition, “the dermoscopy users were finding many more melanomas than the non–dermoscopy users,” Dr. Marghoob added. And over the 10 years, the number of nevi being removed did not change among those not using dermoscopy but dropped among those using dermoscopy.
Adding photography with the ability to digitally monitor patients helps bring this ratio down further, Dr. Marghoob noted. He referred to a study that instead evaluated the ratio of melanoma to nonmelanomas diagnosed among dermatologists in three groups: those with no digital dermoscopy with little dermoscopy training (group A, the reference group), no digital dermoscopy but more dermoscopy training (group B), and those using digital dermoscopy (group C). In the group that used digital dermoscopy, that ratio was about 1 to 2.4, compared with about 1 to 8 in group B, and about 1 to 10.7 in group A (Br J Dermatol. 2012;167[4]778-86).
The use of dermoscopy is also associated with thinner tumors. Among dermoscopy users, the thickness of the tumors detected drops, and the proportion of thin to thick lesions detected increases, Dr. Marghoob said.
For example, in one study, the mean thickness in melanomas detected with dermoscopy was 1.4 mm versus 2.59 mm when dermoscopy was not used (J Eur Acad Dermatol Venereol. 2015 Jan; 29[1]:102-8). About 55% of the tumors detected with dermoscopic examination were 1 mm or less in thickness versus 23.4% of those detected without dermoscopy, “so the dermoscopy users from a proportion standpoint were also finding thinner tumors,” Dr. Marghoob said. Dermoscopy was also identified as an independent predictor of finding thinner tumors.
Even without a study, it could be assumed that the use of dermoscopy would reduce costs, since dermoscopy increases sensitivity and the total number of melanomas detected, decreases the number of benign nevi removed, and helps detect disease earlier. But there are data showing that dermoscopy reduces health care costs, Dr. Marghoob said.* For example, a Belgian study that looked at dermoscopy in two cohorts of melanoma patients concluded that adequate dermoscopy training was cost effective (Eur J Cancer. 2016 Nov;67:38-45).
It has also been shown that adding dermoscopy to a primary care setting has cost benefits, Dr. Marghoob said. He cited a study of Dutch general practices that found that the probability of a correct diagnosis was 1.25 times higher when dermoscopy was used to evaluate suspicious skin lesions and concluded that the use of dermoscopy appeared to be cost effective (J Eur Acad Dermatol Venereol. 2014 Nov;28[11]:1442-9).
Dr. Marghoob had no disclosures relevant to this presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
*Correction, 2/28/20: An earlier version of this article mischaracterized the cost implications of dermoscopy use.
LAHAINA, HAWAII – Multiple but there are still some “nonbelievers,” Ashfaq A. Marghoob, MD, said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
In fact, not one study has shown that dermoscopy is less sensitive than the naked eye alone, and at clinics where dermoscopy is used, “two-thirds of the melanomas being detected now lack the classic ABCD features of melanoma,” added Dr. Marghoob, director of clinical dermatology at Memorial Sloan Kettering in Hauppauge, N.Y.
Dr. Marghoob cited a meta-analysis of 9 prospective trials, which concluded that dermoscopy was more accurate in diagnosing melanoma than the naked eye alone and did not lower specificity, with a sensitivity and specificity of 90%, compared with 71% and 81%, respectively for the naked eye (Br J Dermatol. 2008 Sep;159[3]:669-76).
“And at least from an evidence-based standpoint ... the Cochrane library has basically endorsed that, yes, dermoscopy does indeed improve your diagnostic accuracy,” Dr. Marghoob said.
He referred to a 2018 Cochrane review on 104 dermoscopy studies, with and without visual inspection, for diagnosing melanoma in adults (Cochrane Database Syst Rev. 2018 Dec 4;12:CD011902). The review authors concluded that “the evidence suggests that melanomas will be missed if visual inspection is used on its own,” and despite limitations in the evidence, “dermoscopy is a valuable tool to support the visual inspection of a suspicious skin lesion for the detection of melanoma and atypical intraepidermal melanocytic variants.”
As for the question of specificity, Dr. Marghoob said studies have found that dermoscopy results in the detection of more melanomas and reduces the number of biopsies of benign lesions and “every study looking into this has shown that, yes, it does improve” specificity.
A 10-year multicenter survey of about 300,000 cases, which included 17,172 melanomas and 283,043 melanocytic nevi, found that the number-needed-to-excise (NNE) values improved over time in specialized clinics where newer diagnostic techniques like dermoscopy were used (from 12.8 to 6.8), but the NNE did not appear to change in the nonspecialized settings (J Am Acad Dermatol. 2012 Jul;67[1]:54-9).
Looking at the benign-to-malignant ratio, there was no change among those not using dermoscopy, where the ratio remained at about 30 to 1. When dermoscopy was used, this ratio started to improve over the 10-year period, to about 5 to 1. In addition, “the dermoscopy users were finding many more melanomas than the non–dermoscopy users,” Dr. Marghoob added. And over the 10 years, the number of nevi being removed did not change among those not using dermoscopy but dropped among those using dermoscopy.
Adding photography with the ability to digitally monitor patients helps bring this ratio down further, Dr. Marghoob noted. He referred to a study that instead evaluated the ratio of melanoma to nonmelanomas diagnosed among dermatologists in three groups: those with no digital dermoscopy with little dermoscopy training (group A, the reference group), no digital dermoscopy but more dermoscopy training (group B), and those using digital dermoscopy (group C). In the group that used digital dermoscopy, that ratio was about 1 to 2.4, compared with about 1 to 8 in group B, and about 1 to 10.7 in group A (Br J Dermatol. 2012;167[4]778-86).
The use of dermoscopy is also associated with thinner tumors. Among dermoscopy users, the thickness of the tumors detected drops, and the proportion of thin to thick lesions detected increases, Dr. Marghoob said.
For example, in one study, the mean thickness in melanomas detected with dermoscopy was 1.4 mm versus 2.59 mm when dermoscopy was not used (J Eur Acad Dermatol Venereol. 2015 Jan; 29[1]:102-8). About 55% of the tumors detected with dermoscopic examination were 1 mm or less in thickness versus 23.4% of those detected without dermoscopy, “so the dermoscopy users from a proportion standpoint were also finding thinner tumors,” Dr. Marghoob said. Dermoscopy was also identified as an independent predictor of finding thinner tumors.
Even without a study, it could be assumed that the use of dermoscopy would reduce costs, since dermoscopy increases sensitivity and the total number of melanomas detected, decreases the number of benign nevi removed, and helps detect disease earlier. But there are data showing that dermoscopy reduces health care costs, Dr. Marghoob said.* For example, a Belgian study that looked at dermoscopy in two cohorts of melanoma patients concluded that adequate dermoscopy training was cost effective (Eur J Cancer. 2016 Nov;67:38-45).
It has also been shown that adding dermoscopy to a primary care setting has cost benefits, Dr. Marghoob said. He cited a study of Dutch general practices that found that the probability of a correct diagnosis was 1.25 times higher when dermoscopy was used to evaluate suspicious skin lesions and concluded that the use of dermoscopy appeared to be cost effective (J Eur Acad Dermatol Venereol. 2014 Nov;28[11]:1442-9).
Dr. Marghoob had no disclosures relevant to this presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
*Correction, 2/28/20: An earlier version of this article mischaracterized the cost implications of dermoscopy use.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Secukinumab outperforms adalimumab overall for PsA
MAUI, HAWAII – The interleukin-17A inhibitor secukinumab made a strong showing versus the tumor necrosis factor inhibitor adalimumab for the treatment of psoriatic arthritis in the 52-week, randomized, head-to-head phase 3b EXCEED study, Arthur Kavanaugh, MD, reported at the 2020 Rheumatology Winter Clinical Symposium.
EXCEED was the first double-blind, randomized comparison of an IL-17A inhibitor versus a tumor necrosis factor inhibitor as first-line biologic monotherapy in 853 psoriatic arthritis (PsA) patients with an inadequate response to conventional disease-modifying antirheumatic drugs. And while secukinumab (Cosentyx) narrowly failed to demonstrate superiority over adalimumab (Humira) on the primary endpoint of at least a 20% improvement over baseline on American College of Rheumatology disease criteria at 52 weeks, or ACR20 response, the IL-17A inhibitor demonstrated far greater efficacy for the skin disease, noted Dr. Kavanaugh, a rheumatologist who is professor of medicine at the University of California, San Diego, and RWCS program director. Patients received standard dosing of either drug: secukinumab at 300 mg every 4 weeks or adalimumab at 40 mg every 2 weeks.
Dr. Kavanaugh, an EXCEED coinvestigator, characterized the articular outcomes as similar in the two study arms. The ACR20 primary outcome rate was 67.4% in the secukinumab-treated patients and 61.5% with adalimumab, a difference that didn’t quite reach statistical significance (P = .07). However, in a prespecified secondary analysis of ACR20 rates based upon nonresponder imputation – the most conservative method of statistical analysis, in which all subjects who don’t complete the full study period are counted as treatment failures – secukinumab proved superior to adalimumab by a margin of 66.9% versus 59.5% (P = .02). That result was heavily influenced by the significantly higher dropout rate in the adalimumab group: 23.7%, compared with 14.2% in the secukinumab group.
The ACR50 response rate was 49% in the secukinumab group and 44.6% with adalimumab, a nonsignificant difference. Enthesitis resolution rates at 52 weeks were 60.5% and 54.2%, respectively, also a nonsignificant difference. The mean improvement in Health Assessment Questionnaire–Disability Index scores was closely similar in the two groups. However, a 90% improvement in Psoriasis Area and Severity Index scores, or PASI90 response, was achieved in 65.4% of the secukinumab group, far better than the 43.2% rate with adalimumab.
Dr. Kavanaugh observed that the EXCEED outcomes are consistent with the recently published 24-week results of the SPIRIT-H2H trial, an open-label, assessor-blinded randomized comparison of adalimumab versus another IL-17A inhibitor, ixekizumab (Taltz), in 566 PsA patients. Ixekizumab proved superior to adalimumab for the primary composite endpoint composed of an ACR50 response and simultaneous achievement of a PASI100 response, with rates of 36% and 28%, respectively. The ACR50 rates were similar for the two biologics, while the skin results were superior with ixekizumab.
Eric M. Ruderman, MD, said that, taken together, the EXCEED and SPIRIT-H2H results raise an important issue for clinical practice: Even though both secukinumab and ixekizumab are approved for the treatment of PsA, rheumatologists tend to reflexively reach for a TNF inhibitor as the first biologic in affected patients.
“I don’t know that that necessarily needs to be so. There’s absolutely no reason why an IL-17 inhibitor shouldn’t be equally an option as first-line treatment when you think about starting a biologic in these patients. It’s inertia: We like what we like, we do what we’ve been doing for a long time,” said Dr. Ruderman, professor of medicine and associate chief for clinical affairs in the division of rheumatology at Northwestern University, Chicago.
Indeed, an IL-17A inhibitor may actually be a better first-line option in certain circumstances, such as in the PsA patient with more extensive skin involvement, he continued. Also, there is a possibility that the IL-17A inhibitors are less immunogenic than the anti-TNF biologics, which may result in a more durable response. This concept, while still speculative, is supported by the recently published results of the long-term extension of the phase 3 FUTURE 1 study, in which 82% of patients randomized to secukinumab were still on the biologic after 5 years. That’s a far better retention rate than is seen with TNF inhibitors, he noted.
In addition, SPIRIT-H2H participants randomized to ixekizumab didn’t derive added benefit from concomitant methotrexate, while those on adalimumab did. Thus, PsA patients who desire a simpler, methotrexate-free regimen may prefer an IL-17A inhibitor, Dr. Ruderman said.
Dr. Kavanaugh noted that differences in the side effect profiles of the two classes of biologics may be relevant in treatment decisions. The TNF inhibitors have a higher risk of serious infections than do the IL-17A inhibitors, which in turn are associated with more Candida infections.
Dr. Kavanaugh reported receiving research funding from and serving as a consultant to Novartis, which sponsored EXCEED, as well as more than a dozen other pharmaceutical companies. Dr. Ruderman reported serving as a consultant to Pfizer.
MAUI, HAWAII – The interleukin-17A inhibitor secukinumab made a strong showing versus the tumor necrosis factor inhibitor adalimumab for the treatment of psoriatic arthritis in the 52-week, randomized, head-to-head phase 3b EXCEED study, Arthur Kavanaugh, MD, reported at the 2020 Rheumatology Winter Clinical Symposium.
EXCEED was the first double-blind, randomized comparison of an IL-17A inhibitor versus a tumor necrosis factor inhibitor as first-line biologic monotherapy in 853 psoriatic arthritis (PsA) patients with an inadequate response to conventional disease-modifying antirheumatic drugs. And while secukinumab (Cosentyx) narrowly failed to demonstrate superiority over adalimumab (Humira) on the primary endpoint of at least a 20% improvement over baseline on American College of Rheumatology disease criteria at 52 weeks, or ACR20 response, the IL-17A inhibitor demonstrated far greater efficacy for the skin disease, noted Dr. Kavanaugh, a rheumatologist who is professor of medicine at the University of California, San Diego, and RWCS program director. Patients received standard dosing of either drug: secukinumab at 300 mg every 4 weeks or adalimumab at 40 mg every 2 weeks.
Dr. Kavanaugh, an EXCEED coinvestigator, characterized the articular outcomes as similar in the two study arms. The ACR20 primary outcome rate was 67.4% in the secukinumab-treated patients and 61.5% with adalimumab, a difference that didn’t quite reach statistical significance (P = .07). However, in a prespecified secondary analysis of ACR20 rates based upon nonresponder imputation – the most conservative method of statistical analysis, in which all subjects who don’t complete the full study period are counted as treatment failures – secukinumab proved superior to adalimumab by a margin of 66.9% versus 59.5% (P = .02). That result was heavily influenced by the significantly higher dropout rate in the adalimumab group: 23.7%, compared with 14.2% in the secukinumab group.
The ACR50 response rate was 49% in the secukinumab group and 44.6% with adalimumab, a nonsignificant difference. Enthesitis resolution rates at 52 weeks were 60.5% and 54.2%, respectively, also a nonsignificant difference. The mean improvement in Health Assessment Questionnaire–Disability Index scores was closely similar in the two groups. However, a 90% improvement in Psoriasis Area and Severity Index scores, or PASI90 response, was achieved in 65.4% of the secukinumab group, far better than the 43.2% rate with adalimumab.
Dr. Kavanaugh observed that the EXCEED outcomes are consistent with the recently published 24-week results of the SPIRIT-H2H trial, an open-label, assessor-blinded randomized comparison of adalimumab versus another IL-17A inhibitor, ixekizumab (Taltz), in 566 PsA patients. Ixekizumab proved superior to adalimumab for the primary composite endpoint composed of an ACR50 response and simultaneous achievement of a PASI100 response, with rates of 36% and 28%, respectively. The ACR50 rates were similar for the two biologics, while the skin results were superior with ixekizumab.
Eric M. Ruderman, MD, said that, taken together, the EXCEED and SPIRIT-H2H results raise an important issue for clinical practice: Even though both secukinumab and ixekizumab are approved for the treatment of PsA, rheumatologists tend to reflexively reach for a TNF inhibitor as the first biologic in affected patients.
“I don’t know that that necessarily needs to be so. There’s absolutely no reason why an IL-17 inhibitor shouldn’t be equally an option as first-line treatment when you think about starting a biologic in these patients. It’s inertia: We like what we like, we do what we’ve been doing for a long time,” said Dr. Ruderman, professor of medicine and associate chief for clinical affairs in the division of rheumatology at Northwestern University, Chicago.
Indeed, an IL-17A inhibitor may actually be a better first-line option in certain circumstances, such as in the PsA patient with more extensive skin involvement, he continued. Also, there is a possibility that the IL-17A inhibitors are less immunogenic than the anti-TNF biologics, which may result in a more durable response. This concept, while still speculative, is supported by the recently published results of the long-term extension of the phase 3 FUTURE 1 study, in which 82% of patients randomized to secukinumab were still on the biologic after 5 years. That’s a far better retention rate than is seen with TNF inhibitors, he noted.
In addition, SPIRIT-H2H participants randomized to ixekizumab didn’t derive added benefit from concomitant methotrexate, while those on adalimumab did. Thus, PsA patients who desire a simpler, methotrexate-free regimen may prefer an IL-17A inhibitor, Dr. Ruderman said.
Dr. Kavanaugh noted that differences in the side effect profiles of the two classes of biologics may be relevant in treatment decisions. The TNF inhibitors have a higher risk of serious infections than do the IL-17A inhibitors, which in turn are associated with more Candida infections.
Dr. Kavanaugh reported receiving research funding from and serving as a consultant to Novartis, which sponsored EXCEED, as well as more than a dozen other pharmaceutical companies. Dr. Ruderman reported serving as a consultant to Pfizer.
MAUI, HAWAII – The interleukin-17A inhibitor secukinumab made a strong showing versus the tumor necrosis factor inhibitor adalimumab for the treatment of psoriatic arthritis in the 52-week, randomized, head-to-head phase 3b EXCEED study, Arthur Kavanaugh, MD, reported at the 2020 Rheumatology Winter Clinical Symposium.
EXCEED was the first double-blind, randomized comparison of an IL-17A inhibitor versus a tumor necrosis factor inhibitor as first-line biologic monotherapy in 853 psoriatic arthritis (PsA) patients with an inadequate response to conventional disease-modifying antirheumatic drugs. And while secukinumab (Cosentyx) narrowly failed to demonstrate superiority over adalimumab (Humira) on the primary endpoint of at least a 20% improvement over baseline on American College of Rheumatology disease criteria at 52 weeks, or ACR20 response, the IL-17A inhibitor demonstrated far greater efficacy for the skin disease, noted Dr. Kavanaugh, a rheumatologist who is professor of medicine at the University of California, San Diego, and RWCS program director. Patients received standard dosing of either drug: secukinumab at 300 mg every 4 weeks or adalimumab at 40 mg every 2 weeks.
Dr. Kavanaugh, an EXCEED coinvestigator, characterized the articular outcomes as similar in the two study arms. The ACR20 primary outcome rate was 67.4% in the secukinumab-treated patients and 61.5% with adalimumab, a difference that didn’t quite reach statistical significance (P = .07). However, in a prespecified secondary analysis of ACR20 rates based upon nonresponder imputation – the most conservative method of statistical analysis, in which all subjects who don’t complete the full study period are counted as treatment failures – secukinumab proved superior to adalimumab by a margin of 66.9% versus 59.5% (P = .02). That result was heavily influenced by the significantly higher dropout rate in the adalimumab group: 23.7%, compared with 14.2% in the secukinumab group.
The ACR50 response rate was 49% in the secukinumab group and 44.6% with adalimumab, a nonsignificant difference. Enthesitis resolution rates at 52 weeks were 60.5% and 54.2%, respectively, also a nonsignificant difference. The mean improvement in Health Assessment Questionnaire–Disability Index scores was closely similar in the two groups. However, a 90% improvement in Psoriasis Area and Severity Index scores, or PASI90 response, was achieved in 65.4% of the secukinumab group, far better than the 43.2% rate with adalimumab.
Dr. Kavanaugh observed that the EXCEED outcomes are consistent with the recently published 24-week results of the SPIRIT-H2H trial, an open-label, assessor-blinded randomized comparison of adalimumab versus another IL-17A inhibitor, ixekizumab (Taltz), in 566 PsA patients. Ixekizumab proved superior to adalimumab for the primary composite endpoint composed of an ACR50 response and simultaneous achievement of a PASI100 response, with rates of 36% and 28%, respectively. The ACR50 rates were similar for the two biologics, while the skin results were superior with ixekizumab.
Eric M. Ruderman, MD, said that, taken together, the EXCEED and SPIRIT-H2H results raise an important issue for clinical practice: Even though both secukinumab and ixekizumab are approved for the treatment of PsA, rheumatologists tend to reflexively reach for a TNF inhibitor as the first biologic in affected patients.
“I don’t know that that necessarily needs to be so. There’s absolutely no reason why an IL-17 inhibitor shouldn’t be equally an option as first-line treatment when you think about starting a biologic in these patients. It’s inertia: We like what we like, we do what we’ve been doing for a long time,” said Dr. Ruderman, professor of medicine and associate chief for clinical affairs in the division of rheumatology at Northwestern University, Chicago.
Indeed, an IL-17A inhibitor may actually be a better first-line option in certain circumstances, such as in the PsA patient with more extensive skin involvement, he continued. Also, there is a possibility that the IL-17A inhibitors are less immunogenic than the anti-TNF biologics, which may result in a more durable response. This concept, while still speculative, is supported by the recently published results of the long-term extension of the phase 3 FUTURE 1 study, in which 82% of patients randomized to secukinumab were still on the biologic after 5 years. That’s a far better retention rate than is seen with TNF inhibitors, he noted.
In addition, SPIRIT-H2H participants randomized to ixekizumab didn’t derive added benefit from concomitant methotrexate, while those on adalimumab did. Thus, PsA patients who desire a simpler, methotrexate-free regimen may prefer an IL-17A inhibitor, Dr. Ruderman said.
Dr. Kavanaugh noted that differences in the side effect profiles of the two classes of biologics may be relevant in treatment decisions. The TNF inhibitors have a higher risk of serious infections than do the IL-17A inhibitors, which in turn are associated with more Candida infections.
Dr. Kavanaugh reported receiving research funding from and serving as a consultant to Novartis, which sponsored EXCEED, as well as more than a dozen other pharmaceutical companies. Dr. Ruderman reported serving as a consultant to Pfizer.
REPORTING FROM RWCS 2020