User login
News and Views that Matter to Physicians
VIDEO: For CABG, double arterial grafts found no better than single
NEW ORLEANS – Patients undergoing coronary artery bypass graft (CABG) surgery do not see any 5-year survival advantage when their surgeon uses both internal mammary (thoracic) arteries for grafting rather than just one of them along with a vein, finds an interim analysis from the randomized Arterial Revascularization Trial (ART).
Overall, about 8.5% of the 3,102 patients randomized had died 5 years after surgery, with no significant difference between the bilateral graft and single graft groups, according to data reported at the American Heart Association scientific sessions and simultaneously published (N Engl J Med. 2016 Nov 14. doi: 10.1056/NEJMoa1610021). The former had roughly triple the rate of sternal reconstruction, mainly driven by complications in insulin-dependent diabetes patients having high body mass index.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
There is strong angiographic evidence that vein grafts have a high rate of failure over time because of atherosclerosis, but internal mammary artery grafts retain excellent patency, he elaborated. “People have speculated that this superior patency of internal mammary arteries will translate into a clinical survival benefit,” and observational data indeed suggest that the bilateral artery strategy reduces mortality by about one-fifth relative to the single artery strategy.
Yet uptake of the bilateral procedure has been low. It is used in fewer than 5% of patients undergoing CABG in the United States and fewer than 10% of those in Europe, reflecting concerns about its greater technical complexity, potentially increased mortality and morbidity, and – until now – lack of evidence from randomized trials.
“What I think we can conclude today is that there are excellent 5-year outcomes of CABG in both groups. This study confirms that it’s at least safe to use bilateral grafts over the medium term,” Dr. Taggart commented. He discussed the results in a video interview conducted at the meeting.
These interim ART data probably won’t sway practice one way or the other, he said. “People who believe in arterial grafts will continue to do them, and those who are not enthusiastic about the prospect of a slightly technically more difficult operation [can now] remain comfortable as to why they are not using both internal mammary arteries.”
Pointed questions
The lack of difference was possibly due to a very high level of guideline-based medical therapy in the trial (which may have especially protected the vein grafts) or to the fact that the annual failure rate of vein grafts is modest and steady up to 5 years but accelerates thereafter, Dr. Taggart proposed. The trial’s primary outcome of 10-year survival, expected in 2018, will likely differ, speculated Dr. Sellke, who is also program chair for the AHA scientific sessions.
“Do you think multiple arterial grafting is superior to single internal mammary artery grafting considering the lack of improvement in survival and other outcomes in the study, with the increase in sternal wound infections?” he asked.
“I personally, if I needed the operation, would insist on having bilateral internal mammary artery grafts done by an experienced operator because it is totally counterintuitive to believe that having more patent grafts in your heart at 10 to 20 years of follow-up is of no benefit,” Dr. Taggart maintained.
When data meet clinical practice
It may require time for the benefit of the bilateral artery graft to emerge, he agreed. “I’m undeterred from my belief that ... in patients who are getting CABG done in their 40s or 50s or early 60s, betting on a graft that’s going to outperform vein grafts is the better strategy.”
Until the trial’s 10-year results become available, physicians may wish to put these interim results in the context when counseling patients, according to Dr. Gardner.
“We have indisputable evidence that arterial grafts have better long-term patency than vein grafts,” he elaborated. “If we had a very sophisticated patient, we might tell them that we were a little surprised that this head-to-head trial of single versus double didn’t show any survival benefit at 5 years, but we still are persuaded by the data that shows the better patency, and we think in the situation that the patient’s in, that we would still recommend a double mammary, assuming that the patient doesn’t have comorbidities that would make that more dangerous.”
Trial details
ART enrolled patients from 28 cardiac surgical centers in seven countries. The patients, all of whom had multivessel coronary disease and were scheduled to undergo CABG, were randomized evenly to single or bilateral internal thoracic artery grafts.
The interim results showed differences in nonadherence to the randomized operation: 2.4% of patients in the single graft group ultimately underwent got bilateral grafts, whereas 14% of patients in the bilateral graft group ultimately got a single graft.
“This raises questions about how experienced some surgeons were with the use of bilateral internal mammary artery grafts,” Dr. Taggart commented.
At 5 years of follow-up, 8.7% of patients in the bilateral graft group and 8.4% of patients in the single graft group had died, a nonsignificant difference. “Those mortalities are similar to what has been observed in other contemporary trials of CABG,” he noted. There was no difference between diabetic and nondiabetic patients with respect to this outcome.
The rate of the composite outcome of death, myocardial infarction, or stroke was 12.2% in the bilateral graft group and 12.7% in the single graft group, also a nonsignificant difference.
On the other hand, patients in the bilateral graft group had higher rates of sternal wound complications (3.5% vs. 1.9%; P = .005) and sternal reconstruction (1.9% vs. 0.6%; P = .002).
The groups were statistically indistinguishable with respect to rates of mortality, major bleeding, or need for repeat revascularization, as well as angina status and quality of life measures, according to Dr. Taggart, who disclosed that he had no relevant conflicts of interest.
NEW ORLEANS – Patients undergoing coronary artery bypass graft (CABG) surgery do not see any 5-year survival advantage when their surgeon uses both internal mammary (thoracic) arteries for grafting rather than just one of them along with a vein, finds an interim analysis from the randomized Arterial Revascularization Trial (ART).
Overall, about 8.5% of the 3,102 patients randomized had died 5 years after surgery, with no significant difference between the bilateral graft and single graft groups, according to data reported at the American Heart Association scientific sessions and simultaneously published (N Engl J Med. 2016 Nov 14. doi: 10.1056/NEJMoa1610021). The former had roughly triple the rate of sternal reconstruction, mainly driven by complications in insulin-dependent diabetes patients having high body mass index.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
There is strong angiographic evidence that vein grafts have a high rate of failure over time because of atherosclerosis, but internal mammary artery grafts retain excellent patency, he elaborated. “People have speculated that this superior patency of internal mammary arteries will translate into a clinical survival benefit,” and observational data indeed suggest that the bilateral artery strategy reduces mortality by about one-fifth relative to the single artery strategy.
Yet uptake of the bilateral procedure has been low. It is used in fewer than 5% of patients undergoing CABG in the United States and fewer than 10% of those in Europe, reflecting concerns about its greater technical complexity, potentially increased mortality and morbidity, and – until now – lack of evidence from randomized trials.
“What I think we can conclude today is that there are excellent 5-year outcomes of CABG in both groups. This study confirms that it’s at least safe to use bilateral grafts over the medium term,” Dr. Taggart commented. He discussed the results in a video interview conducted at the meeting.
These interim ART data probably won’t sway practice one way or the other, he said. “People who believe in arterial grafts will continue to do them, and those who are not enthusiastic about the prospect of a slightly technically more difficult operation [can now] remain comfortable as to why they are not using both internal mammary arteries.”
Pointed questions
The lack of difference was possibly due to a very high level of guideline-based medical therapy in the trial (which may have especially protected the vein grafts) or to the fact that the annual failure rate of vein grafts is modest and steady up to 5 years but accelerates thereafter, Dr. Taggart proposed. The trial’s primary outcome of 10-year survival, expected in 2018, will likely differ, speculated Dr. Sellke, who is also program chair for the AHA scientific sessions.
“Do you think multiple arterial grafting is superior to single internal mammary artery grafting considering the lack of improvement in survival and other outcomes in the study, with the increase in sternal wound infections?” he asked.
“I personally, if I needed the operation, would insist on having bilateral internal mammary artery grafts done by an experienced operator because it is totally counterintuitive to believe that having more patent grafts in your heart at 10 to 20 years of follow-up is of no benefit,” Dr. Taggart maintained.
When data meet clinical practice
It may require time for the benefit of the bilateral artery graft to emerge, he agreed. “I’m undeterred from my belief that ... in patients who are getting CABG done in their 40s or 50s or early 60s, betting on a graft that’s going to outperform vein grafts is the better strategy.”
Until the trial’s 10-year results become available, physicians may wish to put these interim results in the context when counseling patients, according to Dr. Gardner.
“We have indisputable evidence that arterial grafts have better long-term patency than vein grafts,” he elaborated. “If we had a very sophisticated patient, we might tell them that we were a little surprised that this head-to-head trial of single versus double didn’t show any survival benefit at 5 years, but we still are persuaded by the data that shows the better patency, and we think in the situation that the patient’s in, that we would still recommend a double mammary, assuming that the patient doesn’t have comorbidities that would make that more dangerous.”
Trial details
ART enrolled patients from 28 cardiac surgical centers in seven countries. The patients, all of whom had multivessel coronary disease and were scheduled to undergo CABG, were randomized evenly to single or bilateral internal thoracic artery grafts.
The interim results showed differences in nonadherence to the randomized operation: 2.4% of patients in the single graft group ultimately underwent got bilateral grafts, whereas 14% of patients in the bilateral graft group ultimately got a single graft.
“This raises questions about how experienced some surgeons were with the use of bilateral internal mammary artery grafts,” Dr. Taggart commented.
At 5 years of follow-up, 8.7% of patients in the bilateral graft group and 8.4% of patients in the single graft group had died, a nonsignificant difference. “Those mortalities are similar to what has been observed in other contemporary trials of CABG,” he noted. There was no difference between diabetic and nondiabetic patients with respect to this outcome.
The rate of the composite outcome of death, myocardial infarction, or stroke was 12.2% in the bilateral graft group and 12.7% in the single graft group, also a nonsignificant difference.
On the other hand, patients in the bilateral graft group had higher rates of sternal wound complications (3.5% vs. 1.9%; P = .005) and sternal reconstruction (1.9% vs. 0.6%; P = .002).
The groups were statistically indistinguishable with respect to rates of mortality, major bleeding, or need for repeat revascularization, as well as angina status and quality of life measures, according to Dr. Taggart, who disclosed that he had no relevant conflicts of interest.
NEW ORLEANS – Patients undergoing coronary artery bypass graft (CABG) surgery do not see any 5-year survival advantage when their surgeon uses both internal mammary (thoracic) arteries for grafting rather than just one of them along with a vein, finds an interim analysis from the randomized Arterial Revascularization Trial (ART).
Overall, about 8.5% of the 3,102 patients randomized had died 5 years after surgery, with no significant difference between the bilateral graft and single graft groups, according to data reported at the American Heart Association scientific sessions and simultaneously published (N Engl J Med. 2016 Nov 14. doi: 10.1056/NEJMoa1610021). The former had roughly triple the rate of sternal reconstruction, mainly driven by complications in insulin-dependent diabetes patients having high body mass index.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
There is strong angiographic evidence that vein grafts have a high rate of failure over time because of atherosclerosis, but internal mammary artery grafts retain excellent patency, he elaborated. “People have speculated that this superior patency of internal mammary arteries will translate into a clinical survival benefit,” and observational data indeed suggest that the bilateral artery strategy reduces mortality by about one-fifth relative to the single artery strategy.
Yet uptake of the bilateral procedure has been low. It is used in fewer than 5% of patients undergoing CABG in the United States and fewer than 10% of those in Europe, reflecting concerns about its greater technical complexity, potentially increased mortality and morbidity, and – until now – lack of evidence from randomized trials.
“What I think we can conclude today is that there are excellent 5-year outcomes of CABG in both groups. This study confirms that it’s at least safe to use bilateral grafts over the medium term,” Dr. Taggart commented. He discussed the results in a video interview conducted at the meeting.
These interim ART data probably won’t sway practice one way or the other, he said. “People who believe in arterial grafts will continue to do them, and those who are not enthusiastic about the prospect of a slightly technically more difficult operation [can now] remain comfortable as to why they are not using both internal mammary arteries.”
Pointed questions
The lack of difference was possibly due to a very high level of guideline-based medical therapy in the trial (which may have especially protected the vein grafts) or to the fact that the annual failure rate of vein grafts is modest and steady up to 5 years but accelerates thereafter, Dr. Taggart proposed. The trial’s primary outcome of 10-year survival, expected in 2018, will likely differ, speculated Dr. Sellke, who is also program chair for the AHA scientific sessions.
“Do you think multiple arterial grafting is superior to single internal mammary artery grafting considering the lack of improvement in survival and other outcomes in the study, with the increase in sternal wound infections?” he asked.
“I personally, if I needed the operation, would insist on having bilateral internal mammary artery grafts done by an experienced operator because it is totally counterintuitive to believe that having more patent grafts in your heart at 10 to 20 years of follow-up is of no benefit,” Dr. Taggart maintained.
When data meet clinical practice
It may require time for the benefit of the bilateral artery graft to emerge, he agreed. “I’m undeterred from my belief that ... in patients who are getting CABG done in their 40s or 50s or early 60s, betting on a graft that’s going to outperform vein grafts is the better strategy.”
Until the trial’s 10-year results become available, physicians may wish to put these interim results in the context when counseling patients, according to Dr. Gardner.
“We have indisputable evidence that arterial grafts have better long-term patency than vein grafts,” he elaborated. “If we had a very sophisticated patient, we might tell them that we were a little surprised that this head-to-head trial of single versus double didn’t show any survival benefit at 5 years, but we still are persuaded by the data that shows the better patency, and we think in the situation that the patient’s in, that we would still recommend a double mammary, assuming that the patient doesn’t have comorbidities that would make that more dangerous.”
Trial details
ART enrolled patients from 28 cardiac surgical centers in seven countries. The patients, all of whom had multivessel coronary disease and were scheduled to undergo CABG, were randomized evenly to single or bilateral internal thoracic artery grafts.
The interim results showed differences in nonadherence to the randomized operation: 2.4% of patients in the single graft group ultimately underwent got bilateral grafts, whereas 14% of patients in the bilateral graft group ultimately got a single graft.
“This raises questions about how experienced some surgeons were with the use of bilateral internal mammary artery grafts,” Dr. Taggart commented.
At 5 years of follow-up, 8.7% of patients in the bilateral graft group and 8.4% of patients in the single graft group had died, a nonsignificant difference. “Those mortalities are similar to what has been observed in other contemporary trials of CABG,” he noted. There was no difference between diabetic and nondiabetic patients with respect to this outcome.
The rate of the composite outcome of death, myocardial infarction, or stroke was 12.2% in the bilateral graft group and 12.7% in the single graft group, also a nonsignificant difference.
On the other hand, patients in the bilateral graft group had higher rates of sternal wound complications (3.5% vs. 1.9%; P = .005) and sternal reconstruction (1.9% vs. 0.6%; P = .002).
The groups were statistically indistinguishable with respect to rates of mortality, major bleeding, or need for repeat revascularization, as well as angina status and quality of life measures, according to Dr. Taggart, who disclosed that he had no relevant conflicts of interest.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: At 5 years, the rate of all-cause mortality was 8.7% in the bilateral graft group and 8.4% in the single graft group, a nonsignificant difference.
Data source: ART, a randomized trial among 3,102 patients with multivessel coronary disease undergoing CABG.
Disclosures: Dr. Taggart had no relevant conflicts of interest. The trial was funded by the U.K. Medical Research Council, the British Heart Foundation, and the U.K. National Institute of Health Research Efficacy and Mechanistic Evaluation.
VIDEO: Celecoxib just as safe as naproxen or ibuprofen in OA and RA
WASHINGTON – Celecoxib conferred a 53% decreased risk of overall mortality upon patients with rheumatoid arthritis when compared with naproxen – a surprise finding in a subanalysis of the newly released PRECISION study of anti-inflammatory drugs in arthritis.
But it’s tough to know what to make of the difference, according to the investigators at the annual meeting of the American College of Rheumatology. Although statistically significant, the mortality finding was based on just 45 events: 30 among those taking naproxen and 15 among those taking celecoxib.
“While I would say we were surprised to see this, we really can’t say what it means – or if it means anything,” primary investigator Daniel Solomon, MD, said in an interview. “This is a finding we will continue to investigate and look at, but at this point it’s not enough to base any prescribing decisions on.”
PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety Versus Ibuprofen or Naproxen) enrolled more than 24,000 patients with osteoarthritis or rheumatoid arthritis. They were randomized to celecoxib, naproxen, or ibuprofen for a mean of 20 months, with an additional mean follow-up of 34 months.
The primary outcome was the first occurrence of an adverse event from the Antiplatelet Trialists Collaboration criteria (APTC; death from cardiovascular causes, nonfatal heart attack, or nonfatal stroke). Secondary outcomes included:
• Major cardiovascular events (heart attack, stroke, cardiovascular death, revascularization, and hospitalization for unstable angina or transient ischemic attack).
• Renal events (acute kidney injury, including hospitalization for renal failure).
• Gastrointestinal events (hemorrhage, perforation, gastroduodenal ulcer, anemia of gastrointestinal origin, and gastric outlet obstruction.
The main PRECISION findings were released Nov. 13 at the annual meeting of the American Heart Association and simultaneously published in the New England Journal of Medicine (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593).
Overall, celecoxib was just as safe as were the other drugs on the APTC endpoint, which occurred in about 2% of each groups. The study found significantly decreased risks of both GI and renal events with celecoxib, compared with either naproxen or ibuprofen. Celecoxib and naproxen were equivalent with regard to GI and renal events.
The subanalysis, released at the ACR meeting, adds important disease-specific context to the overall PRECISION results.
“We wanted to really delve into the subtle differences in how these two patient groups responded to these medications,” said PRECISION coinvestigator Elaine Husni, MD, vice chair of the department of rheumatic and immunologic diseases at the Cleveland Clinic.
“We learned that each of these NSAIDs has a unique safety profile that can be different in different groups. And in general, celecoxib seems less risky than the others.”
The cohort subanalysis broke down these endpoints among 21,600 patients with osteoarthritis and 2,400 with rheumatoid arthritis.
Among patients with osteoarthritis, celecoxib was also associated with a 16% decreased risk of a major adverse cardiovascular event, compared with ibuprofen. GI events were also less likely in this group: Celecoxib was associated with a 32% decreased risk, compared with ibuprofen, and a 27% decreased risk, compared with naproxen.
Renal outcomes were almost identical in all of the medications in both groups, Dr. Husni said.
In addition to the adverse event outcomes, the subanalysis examined how well patients responded to their assigned NSAID. There were also some subtle differences seen here, Dr. Solomon and Dr. Husni said.
For patients with RA, ibuprofen was slightly, but significantly, more effective than either celecoxib or ibuprofen at controlling pain as measured by a visual analog pain scale. Patients with osteoarthritis responded equally well to all of the drugs.
RA patients also responded best to ibuprofen as measured by the Health Assessment Questionnaire Disability Index (HAQ-DI). Again, patients with osteoarthritis responded equally well to all of the medications.
The overall findings, as well as the subanalysis, should be reassuring to both physicians and patients, said Dr. Solomon, chief of the section of clinical sciences in the divisions of rheumatology and pharmacoepidemiology at Brigham and Women’s Hospital, Boston.
“I can now stand in front of patients and say with confidence, ‘Each of these drugs is fairly safe, and together we can choose the one that will be best for you, based on your own individual history and your own individual risk factors.’ I feel good about that.”
Pfizer funded the trial. Dr. Husni has research grants from Genzyme/Sanofi on a knee osteoarthritis trial related to hyaluronic acid injections. Dr. Solomon has research grants from Pfizer on non-NSAID related topics. He also receives royalties from UpToDate on chapters related to NSAIDs and selective COX-2 inhibitors.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
WASHINGTON – Celecoxib conferred a 53% decreased risk of overall mortality upon patients with rheumatoid arthritis when compared with naproxen – a surprise finding in a subanalysis of the newly released PRECISION study of anti-inflammatory drugs in arthritis.
But it’s tough to know what to make of the difference, according to the investigators at the annual meeting of the American College of Rheumatology. Although statistically significant, the mortality finding was based on just 45 events: 30 among those taking naproxen and 15 among those taking celecoxib.
“While I would say we were surprised to see this, we really can’t say what it means – or if it means anything,” primary investigator Daniel Solomon, MD, said in an interview. “This is a finding we will continue to investigate and look at, but at this point it’s not enough to base any prescribing decisions on.”
PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety Versus Ibuprofen or Naproxen) enrolled more than 24,000 patients with osteoarthritis or rheumatoid arthritis. They were randomized to celecoxib, naproxen, or ibuprofen for a mean of 20 months, with an additional mean follow-up of 34 months.
The primary outcome was the first occurrence of an adverse event from the Antiplatelet Trialists Collaboration criteria (APTC; death from cardiovascular causes, nonfatal heart attack, or nonfatal stroke). Secondary outcomes included:
• Major cardiovascular events (heart attack, stroke, cardiovascular death, revascularization, and hospitalization for unstable angina or transient ischemic attack).
• Renal events (acute kidney injury, including hospitalization for renal failure).
• Gastrointestinal events (hemorrhage, perforation, gastroduodenal ulcer, anemia of gastrointestinal origin, and gastric outlet obstruction.
The main PRECISION findings were released Nov. 13 at the annual meeting of the American Heart Association and simultaneously published in the New England Journal of Medicine (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593).
Overall, celecoxib was just as safe as were the other drugs on the APTC endpoint, which occurred in about 2% of each groups. The study found significantly decreased risks of both GI and renal events with celecoxib, compared with either naproxen or ibuprofen. Celecoxib and naproxen were equivalent with regard to GI and renal events.
The subanalysis, released at the ACR meeting, adds important disease-specific context to the overall PRECISION results.
“We wanted to really delve into the subtle differences in how these two patient groups responded to these medications,” said PRECISION coinvestigator Elaine Husni, MD, vice chair of the department of rheumatic and immunologic diseases at the Cleveland Clinic.
“We learned that each of these NSAIDs has a unique safety profile that can be different in different groups. And in general, celecoxib seems less risky than the others.”
The cohort subanalysis broke down these endpoints among 21,600 patients with osteoarthritis and 2,400 with rheumatoid arthritis.
Among patients with osteoarthritis, celecoxib was also associated with a 16% decreased risk of a major adverse cardiovascular event, compared with ibuprofen. GI events were also less likely in this group: Celecoxib was associated with a 32% decreased risk, compared with ibuprofen, and a 27% decreased risk, compared with naproxen.
Renal outcomes were almost identical in all of the medications in both groups, Dr. Husni said.
In addition to the adverse event outcomes, the subanalysis examined how well patients responded to their assigned NSAID. There were also some subtle differences seen here, Dr. Solomon and Dr. Husni said.
For patients with RA, ibuprofen was slightly, but significantly, more effective than either celecoxib or ibuprofen at controlling pain as measured by a visual analog pain scale. Patients with osteoarthritis responded equally well to all of the drugs.
RA patients also responded best to ibuprofen as measured by the Health Assessment Questionnaire Disability Index (HAQ-DI). Again, patients with osteoarthritis responded equally well to all of the medications.
The overall findings, as well as the subanalysis, should be reassuring to both physicians and patients, said Dr. Solomon, chief of the section of clinical sciences in the divisions of rheumatology and pharmacoepidemiology at Brigham and Women’s Hospital, Boston.
“I can now stand in front of patients and say with confidence, ‘Each of these drugs is fairly safe, and together we can choose the one that will be best for you, based on your own individual history and your own individual risk factors.’ I feel good about that.”
Pfizer funded the trial. Dr. Husni has research grants from Genzyme/Sanofi on a knee osteoarthritis trial related to hyaluronic acid injections. Dr. Solomon has research grants from Pfizer on non-NSAID related topics. He also receives royalties from UpToDate on chapters related to NSAIDs and selective COX-2 inhibitors.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
WASHINGTON – Celecoxib conferred a 53% decreased risk of overall mortality upon patients with rheumatoid arthritis when compared with naproxen – a surprise finding in a subanalysis of the newly released PRECISION study of anti-inflammatory drugs in arthritis.
But it’s tough to know what to make of the difference, according to the investigators at the annual meeting of the American College of Rheumatology. Although statistically significant, the mortality finding was based on just 45 events: 30 among those taking naproxen and 15 among those taking celecoxib.
“While I would say we were surprised to see this, we really can’t say what it means – or if it means anything,” primary investigator Daniel Solomon, MD, said in an interview. “This is a finding we will continue to investigate and look at, but at this point it’s not enough to base any prescribing decisions on.”
PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety Versus Ibuprofen or Naproxen) enrolled more than 24,000 patients with osteoarthritis or rheumatoid arthritis. They were randomized to celecoxib, naproxen, or ibuprofen for a mean of 20 months, with an additional mean follow-up of 34 months.
The primary outcome was the first occurrence of an adverse event from the Antiplatelet Trialists Collaboration criteria (APTC; death from cardiovascular causes, nonfatal heart attack, or nonfatal stroke). Secondary outcomes included:
• Major cardiovascular events (heart attack, stroke, cardiovascular death, revascularization, and hospitalization for unstable angina or transient ischemic attack).
• Renal events (acute kidney injury, including hospitalization for renal failure).
• Gastrointestinal events (hemorrhage, perforation, gastroduodenal ulcer, anemia of gastrointestinal origin, and gastric outlet obstruction.
The main PRECISION findings were released Nov. 13 at the annual meeting of the American Heart Association and simultaneously published in the New England Journal of Medicine (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593).
Overall, celecoxib was just as safe as were the other drugs on the APTC endpoint, which occurred in about 2% of each groups. The study found significantly decreased risks of both GI and renal events with celecoxib, compared with either naproxen or ibuprofen. Celecoxib and naproxen were equivalent with regard to GI and renal events.
The subanalysis, released at the ACR meeting, adds important disease-specific context to the overall PRECISION results.
“We wanted to really delve into the subtle differences in how these two patient groups responded to these medications,” said PRECISION coinvestigator Elaine Husni, MD, vice chair of the department of rheumatic and immunologic diseases at the Cleveland Clinic.
“We learned that each of these NSAIDs has a unique safety profile that can be different in different groups. And in general, celecoxib seems less risky than the others.”
The cohort subanalysis broke down these endpoints among 21,600 patients with osteoarthritis and 2,400 with rheumatoid arthritis.
Among patients with osteoarthritis, celecoxib was also associated with a 16% decreased risk of a major adverse cardiovascular event, compared with ibuprofen. GI events were also less likely in this group: Celecoxib was associated with a 32% decreased risk, compared with ibuprofen, and a 27% decreased risk, compared with naproxen.
Renal outcomes were almost identical in all of the medications in both groups, Dr. Husni said.
In addition to the adverse event outcomes, the subanalysis examined how well patients responded to their assigned NSAID. There were also some subtle differences seen here, Dr. Solomon and Dr. Husni said.
For patients with RA, ibuprofen was slightly, but significantly, more effective than either celecoxib or ibuprofen at controlling pain as measured by a visual analog pain scale. Patients with osteoarthritis responded equally well to all of the drugs.
RA patients also responded best to ibuprofen as measured by the Health Assessment Questionnaire Disability Index (HAQ-DI). Again, patients with osteoarthritis responded equally well to all of the medications.
The overall findings, as well as the subanalysis, should be reassuring to both physicians and patients, said Dr. Solomon, chief of the section of clinical sciences in the divisions of rheumatology and pharmacoepidemiology at Brigham and Women’s Hospital, Boston.
“I can now stand in front of patients and say with confidence, ‘Each of these drugs is fairly safe, and together we can choose the one that will be best for you, based on your own individual history and your own individual risk factors.’ I feel good about that.”
Pfizer funded the trial. Dr. Husni has research grants from Genzyme/Sanofi on a knee osteoarthritis trial related to hyaluronic acid injections. Dr. Solomon has research grants from Pfizer on non-NSAID related topics. He also receives royalties from UpToDate on chapters related to NSAIDs and selective COX-2 inhibitors.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @alz_gal
AT THE ACR ANNUAL MEETING
Key clinical point:
Major finding: Compared with naproxen, celecoxib was associated with a 53% lower risk of overall mortality, although the clinical impact of that finding remains unknown.
Data source: PRECISION, which randomized more than 24,000 patients to celecoxib, ibuprofen, or naproxen.
Disclosures: Pfizer funded the trial. Dr. Husni has research grants from Genzyme/Sanofi on a knee osteoarthritis trial related to hyaluronic acid injections. Dr. Solomon has research grants from Pfizer on non-NSAID related topics. He also receives royalties from UpToDate on chapters related to NSAIDs and selective COX-2 inhibitors.
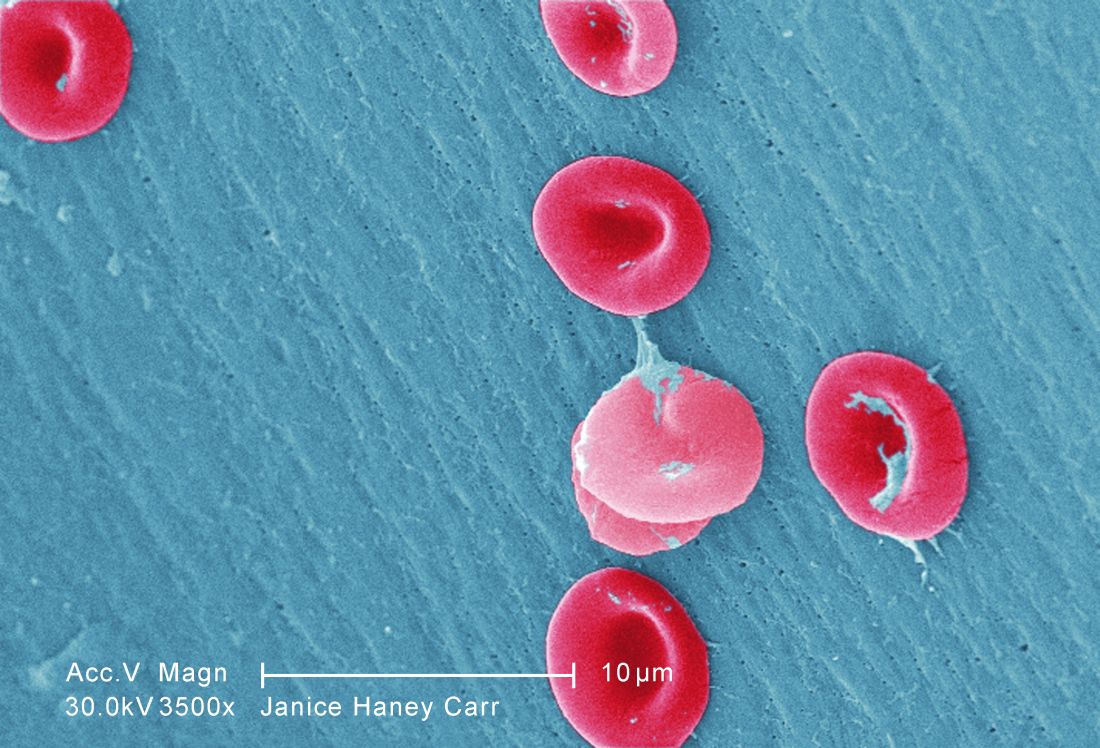
SelG1 cut pain crises in sickle cell disease
The humanized antibody SelG1 decreased the frequency of acute pain episodes in people with sickle cell disease, based on results from the multinational, randomized, double-blind, placebo-controlled SUSTAIN study that will be presented at the annual meeting of the American Society of Hematology in San Diego.
In other sickle cell disease research to be presented at the meeting, researchers will be presenting new findings from two studies conducted in Africa. One study examines a team approach to reduce mortality in pregnant women with sickle cell disease in Ghana. The other study, called SPIN, is a safety and feasibility study conducted in advance of a randomized trial in Nigerian children at risk for stroke.
After 1 year, the annual rate of sickle cell–related pain crises resulting in a visit to a medical facility was 1.6 in the group receiving the 5 mg/kg dose, compared with 3 in the placebo group. The 47% difference was statistically significant (P = .01).
Also, time to first pain crisis was a median of 4 months in those who received the 5 mg/kg dose and 1.4 months for those in the placebo group (P = .001).
Infections were not seen increased in either of the groups randomized to SelG1, and no treatment-related deaths occurred during the course of the study. The first-in-class agent “appears to be safe and well tolerated,” as well as effective in reducing pain episodes, Dr. Ataga and his colleagues wrote in their abstract.
In the Nigerian trial, led by Najibah Aliyu Galadanci, MD, MPH, of Bayero University in Kano, Nigeria, the goal was to determine whether families of children with sickle cell disease and transcranial Doppler measurements indicative of increased risk for stroke could be recruited and retained in a large clinical trial, and whether they could adhere to the medication regimen. The trial also obtained preliminary evidence for hydroxyurea’s safety in this clinical setting, where transfusion therapy is not an option for most children.
Dr. Galadanci and her colleagues approached 375 families for transcranial Doppler screening, and 90% accepted. Among families of children found to have elevated measures of risk on transcranial Doppler, 92% participated in the study and received a moderate dose of hydroxyurea (20 mg/kg) for 2 years. A comparison group included 210 children without elevated measures on transcranial Doppler. These children underwent regular monitoring but were not offered medication unless transcranial Doppler measures were found to be elevated.
Study adherence was exceptionally high: the families missed no monthly research visits, and no participants in the active treatment group dropped out voluntarily.
Also, at 2 years, the children treated with hydroxyurea did not have evidence of excessive toxicity, compared with the children who did not receive the drug. “Our results provide strong preliminary evidence supporting the current multicenter randomized controlled trial comparing hydroxyurea therapy (20 mg/kg per day vs. 10 mg/kg per day) for preventing primary strokes in children with sickle cell anemia living in Nigeria,” Dr. Galadanci and her colleagues wrote in their abstract.
In the third study, a multidisciplinary team decreased mortality in pregnant women who had sickle cell disease and lived in low and middle income settings, according to Eugenia Vicky Naa Kwarley Asare, MD, of the Ghana Institute of Clinical Genetics and the Korle-Bu Teaching Hospital in Accra.
In a prospective trial in Ghana, where maternal mortality among women with sickle cell disease is estimated to be 8,300 per 100,000 live births, compared with 690 for women without sickle cell disease, Dr. Asare and her colleagues’ multidisciplinary team included obstetricians, hematologists, pulmonologists, and nurses, and the planned intervention protocols included a number of changes to make management more consistent and intensive. A total of 154 pregnancies were evaluated before the intervention, and 91 after. Median gestational age was 24 weeks at enrollment, and median maternal age was 29 years for both pre- and post-intervention cohorts.
Maternal mortality before the intervention was 9.7% (15 of 154) and after the intervention was 1.1% (1 of 91) of total deliveries.
Dr. Ataga’s study was sponsored by Selexys Pharmaceuticals, the drug’s manufacturer, and included coinvestigators who are employees of Selexys Pharmaceuticals or who disclosed relationships with other drug manufacturers. Dr. Galadanci’s and Dr. Asare’s groups disclosed no conflicts of interest.
The humanized antibody SelG1 decreased the frequency of acute pain episodes in people with sickle cell disease, based on results from the multinational, randomized, double-blind, placebo-controlled SUSTAIN study that will be presented at the annual meeting of the American Society of Hematology in San Diego.
In other sickle cell disease research to be presented at the meeting, researchers will be presenting new findings from two studies conducted in Africa. One study examines a team approach to reduce mortality in pregnant women with sickle cell disease in Ghana. The other study, called SPIN, is a safety and feasibility study conducted in advance of a randomized trial in Nigerian children at risk for stroke.
After 1 year, the annual rate of sickle cell–related pain crises resulting in a visit to a medical facility was 1.6 in the group receiving the 5 mg/kg dose, compared with 3 in the placebo group. The 47% difference was statistically significant (P = .01).
Also, time to first pain crisis was a median of 4 months in those who received the 5 mg/kg dose and 1.4 months for those in the placebo group (P = .001).
Infections were not seen increased in either of the groups randomized to SelG1, and no treatment-related deaths occurred during the course of the study. The first-in-class agent “appears to be safe and well tolerated,” as well as effective in reducing pain episodes, Dr. Ataga and his colleagues wrote in their abstract.
In the Nigerian trial, led by Najibah Aliyu Galadanci, MD, MPH, of Bayero University in Kano, Nigeria, the goal was to determine whether families of children with sickle cell disease and transcranial Doppler measurements indicative of increased risk for stroke could be recruited and retained in a large clinical trial, and whether they could adhere to the medication regimen. The trial also obtained preliminary evidence for hydroxyurea’s safety in this clinical setting, where transfusion therapy is not an option for most children.
Dr. Galadanci and her colleagues approached 375 families for transcranial Doppler screening, and 90% accepted. Among families of children found to have elevated measures of risk on transcranial Doppler, 92% participated in the study and received a moderate dose of hydroxyurea (20 mg/kg) for 2 years. A comparison group included 210 children without elevated measures on transcranial Doppler. These children underwent regular monitoring but were not offered medication unless transcranial Doppler measures were found to be elevated.
Study adherence was exceptionally high: the families missed no monthly research visits, and no participants in the active treatment group dropped out voluntarily.
Also, at 2 years, the children treated with hydroxyurea did not have evidence of excessive toxicity, compared with the children who did not receive the drug. “Our results provide strong preliminary evidence supporting the current multicenter randomized controlled trial comparing hydroxyurea therapy (20 mg/kg per day vs. 10 mg/kg per day) for preventing primary strokes in children with sickle cell anemia living in Nigeria,” Dr. Galadanci and her colleagues wrote in their abstract.
In the third study, a multidisciplinary team decreased mortality in pregnant women who had sickle cell disease and lived in low and middle income settings, according to Eugenia Vicky Naa Kwarley Asare, MD, of the Ghana Institute of Clinical Genetics and the Korle-Bu Teaching Hospital in Accra.
In a prospective trial in Ghana, where maternal mortality among women with sickle cell disease is estimated to be 8,300 per 100,000 live births, compared with 690 for women without sickle cell disease, Dr. Asare and her colleagues’ multidisciplinary team included obstetricians, hematologists, pulmonologists, and nurses, and the planned intervention protocols included a number of changes to make management more consistent and intensive. A total of 154 pregnancies were evaluated before the intervention, and 91 after. Median gestational age was 24 weeks at enrollment, and median maternal age was 29 years for both pre- and post-intervention cohorts.
Maternal mortality before the intervention was 9.7% (15 of 154) and after the intervention was 1.1% (1 of 91) of total deliveries.
Dr. Ataga’s study was sponsored by Selexys Pharmaceuticals, the drug’s manufacturer, and included coinvestigators who are employees of Selexys Pharmaceuticals or who disclosed relationships with other drug manufacturers. Dr. Galadanci’s and Dr. Asare’s groups disclosed no conflicts of interest.
The humanized antibody SelG1 decreased the frequency of acute pain episodes in people with sickle cell disease, based on results from the multinational, randomized, double-blind, placebo-controlled SUSTAIN study that will be presented at the annual meeting of the American Society of Hematology in San Diego.
In other sickle cell disease research to be presented at the meeting, researchers will be presenting new findings from two studies conducted in Africa. One study examines a team approach to reduce mortality in pregnant women with sickle cell disease in Ghana. The other study, called SPIN, is a safety and feasibility study conducted in advance of a randomized trial in Nigerian children at risk for stroke.
After 1 year, the annual rate of sickle cell–related pain crises resulting in a visit to a medical facility was 1.6 in the group receiving the 5 mg/kg dose, compared with 3 in the placebo group. The 47% difference was statistically significant (P = .01).
Also, time to first pain crisis was a median of 4 months in those who received the 5 mg/kg dose and 1.4 months for those in the placebo group (P = .001).
Infections were not seen increased in either of the groups randomized to SelG1, and no treatment-related deaths occurred during the course of the study. The first-in-class agent “appears to be safe and well tolerated,” as well as effective in reducing pain episodes, Dr. Ataga and his colleagues wrote in their abstract.
In the Nigerian trial, led by Najibah Aliyu Galadanci, MD, MPH, of Bayero University in Kano, Nigeria, the goal was to determine whether families of children with sickle cell disease and transcranial Doppler measurements indicative of increased risk for stroke could be recruited and retained in a large clinical trial, and whether they could adhere to the medication regimen. The trial also obtained preliminary evidence for hydroxyurea’s safety in this clinical setting, where transfusion therapy is not an option for most children.
Dr. Galadanci and her colleagues approached 375 families for transcranial Doppler screening, and 90% accepted. Among families of children found to have elevated measures of risk on transcranial Doppler, 92% participated in the study and received a moderate dose of hydroxyurea (20 mg/kg) for 2 years. A comparison group included 210 children without elevated measures on transcranial Doppler. These children underwent regular monitoring but were not offered medication unless transcranial Doppler measures were found to be elevated.
Study adherence was exceptionally high: the families missed no monthly research visits, and no participants in the active treatment group dropped out voluntarily.
Also, at 2 years, the children treated with hydroxyurea did not have evidence of excessive toxicity, compared with the children who did not receive the drug. “Our results provide strong preliminary evidence supporting the current multicenter randomized controlled trial comparing hydroxyurea therapy (20 mg/kg per day vs. 10 mg/kg per day) for preventing primary strokes in children with sickle cell anemia living in Nigeria,” Dr. Galadanci and her colleagues wrote in their abstract.
In the third study, a multidisciplinary team decreased mortality in pregnant women who had sickle cell disease and lived in low and middle income settings, according to Eugenia Vicky Naa Kwarley Asare, MD, of the Ghana Institute of Clinical Genetics and the Korle-Bu Teaching Hospital in Accra.
In a prospective trial in Ghana, where maternal mortality among women with sickle cell disease is estimated to be 8,300 per 100,000 live births, compared with 690 for women without sickle cell disease, Dr. Asare and her colleagues’ multidisciplinary team included obstetricians, hematologists, pulmonologists, and nurses, and the planned intervention protocols included a number of changes to make management more consistent and intensive. A total of 154 pregnancies were evaluated before the intervention, and 91 after. Median gestational age was 24 weeks at enrollment, and median maternal age was 29 years for both pre- and post-intervention cohorts.
Maternal mortality before the intervention was 9.7% (15 of 154) and after the intervention was 1.1% (1 of 91) of total deliveries.
Dr. Ataga’s study was sponsored by Selexys Pharmaceuticals, the drug’s manufacturer, and included coinvestigators who are employees of Selexys Pharmaceuticals or who disclosed relationships with other drug manufacturers. Dr. Galadanci’s and Dr. Asare’s groups disclosed no conflicts of interest.
FROM ASH 2016
USPSTF: Expand statin use beyond lipids to CVD risk
Use of statins for the primary prevention of cardiovascular disease should be based on overall cardiovascular disease risk, not necessarily blood lipid levels, according to new recommendations from the United States Preventive Services Task Force.
Despite widespread use in the elderly, USPSTF also said there’s insufficient evidence to recommend starting statins for cardiovascular disease (CVD) prevention in patients 76 years or older (JAMA. 2016 Nov;316[19]:1997-2007).
USPSTF now recommends low- to moderate-dose statins for primary prevention in adults 40-75 years old who have at least one CVD risk factor – dyslipidemia, diabetes, hypertension, or smoking – and a 10-year CVD event risk of at least 10% (B grade). It also recommended “selectively” offering low- to moderate-dose statins if patients have a 7.5%-10% risk (C grade). The task force recommends using the online American College of Cardiology/American Heart Association risk calculator.
A B grade denotes that USPSTF recommends the service as one where there is “high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial.” With a C grade, the task force recommends that the service be provided subject to professional judgment and patient preferences.
The new advices from USPSTF is consistent with the task force’s 2015 draft proposals, and is based on a pooled analysis of 19 randomized trials in 71,344 adults at risk for CVD but without prior events; 17 of the studies were sponsored at least in part by the companies that make statins. The median duration of follow-up was 3 years. Trials included atorvastatin (Lipitor) and six other statins from 1994-2016.
Few of the 19 trials enrolled patients older than 75 years, so “the balance of benefits and harms of initiating statin use for” primary prevention in elderly adults “cannot be determined.” The task force did not make a recommendation either way, and called for further investigation.
For younger patients, the scales tipped toward benefit when the group found no overall increased risk of cancer, liver damage, diabetes, or cognitive problems with statins for primary prevention. “Although muscle pain, soreness, or weakness are commonly reported with statin use, there were no statistically significant differences between the intervention and control groups for myalgia, myopathy, or rhabdomyolysis,” according to the task force.
Across the 19 trials, statin therapy was associated with a statistically significant 14% reduction in all-cause mortality; 31% reduction in cardiovascular mortality; 29% reduction in stroke; and a 36% reduction in myocardial infarction; 250 patients needed to be treated to prevent one death from any cause after 1-6 years, and 233 to prevent one cardiovascular death after 2-6 years.
The recommendations call for low to moderate doses because that’s what most of the studies used, and there were no clear benefits when trials stratified patients by dose.
USPSTF cautioned that “reliance on a risk calculator ... alone as a basis for prevention may be problematic, given its possible overestimation of risk in some populations” and noted that the benefits “of statin use may be linear according to a patient’s absolute risk level, and any cut points used are only population estimates of benefits.”
The recommendations do not pertain to adults with very high CVD risk, such as those with familial hypercholesterolemia or an LDL level greater than 190mg/dL, since they were excluded from primary prevention trials.
While the USPSTF was careful in its evidence review, “ the limitations of the evidence were not considered sufficiently, given the serious concerns about the harms of statins for primary prevention,” Rita Redberg, MD, and Mitchell Katz, MD, wrote in an editorial accompanying the recommendations.
“USPSTF also did not have access to patient-level data; they had to rely on peer-reviewed published reports,” according to the editorialists. “The actual trial data are largely held by the Cholesterol Treatment Trialists’ Collaboration on behalf of industry sponsors and have not been made available to other researchers, despite multiple requests over many years.” Further, many of the trials were industry sponsored.
Using the USPSTF data, only 2% of patients who take statins for 5 years will avoid a myocardial infarction; virtually all (98%) will not experience any benefit. At the same time, 5%-20% will experience side effects including rhabdomyolysis, cognitive dysfunction, and increased risk of diabetes (JAMA. 2016 Nov;316[19]:1979-81).
There are unintended consequences of widespread statin use in healthy persons, Dr. Redberg and Dr. Katz wrote. People taking statins are more likely to become obese and more sedentary over time, likely because they mistakenly think they do not need to eat a healthy diet and exercise.
The USPSTF analysis was funded by the Agency for Healthcare Research and Quality. Task force lead Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco, has advised the Institute for Clinical and Economic Review, which is partly funded by industry, on the cost-effectiveness of lipid-lowering drugs. Another member reported comparing how well they worked. The other 15 task force members had no disclosures.
Dare cardiovascular experts consider a future in which there are near-universal statin recommendations for middle-aged adults?
[USPSTF analysis suggests] that statin recommendations could be based primarily on a patient’s underlying CVD risk rather than on his or her cholesterol level. Disseminating a treatment strategy based largely on CVD risk alone has been a difficult message for the clinical community to accept and implement.
Nearly a generation of physicians has considered high-cholesterol levels, rather than generalized CVD risk, the target for statin treatment. Only a minority of physicians consistently use complex, risk-based probabilistic calculations to determine therapy.
Several key questions deserve careful consideration. Should LDL be considered in treatment recommendations beyond CVD risk? The decision to use absolute risk to guide statin recommendations is based on the finding that the relative risk reduction seen with statin therapy is independent of baseline risk; thus, those with the highest absolute baseline CVD risk experience the greatest reduction in CVD events.
However, the relative risk reduction of lipid-lowering therapy is also proportional to mmol/dL reduction in LDL level. This supports the contention that those with the highest baseline LDL levels should benefit the most from treatment because they have the most potential decline in LDL with intervention. One way to reconcile these findings is to incorporate both LDL levels and CVD risk into treatment recommendations, as has been done in the European guidelines. This approach recognizes that the relative benefit of statins is proportional to LDL lowering but that the absolute treatment benefit is largely driven by baseline risk.
From the resource perspective, the vast majority of statins are now available as generic products and require limited monitoring, leading to quite modest therapeutic costs. For patients in the gray area not covered by the guidelines, clinicians should be cautioned against adopting either a “treat none” or a “treat all” strategy. Rather, gaps in the evidence provide opportunities for clinicians to practice the art of medicine and engage with patients in shared decision-making regarding strategies for CVD prevention.
Ann Marie Navar, MD, PhD, and Eric Peterson, MD, MPH, are both at the Duke Clinical Research Institute in Durham, N.C. Dr. Navar reported funding from Regeneron and Sanofi. Dr. Peterson reported funding from Merck, Sanofi, Regeneron, and AstraZeneca. They made their comments in an editorial to the USPSTF report (JAMA. 2016 Nov;316[19]:1981-3).
Dare cardiovascular experts consider a future in which there are near-universal statin recommendations for middle-aged adults?
[USPSTF analysis suggests] that statin recommendations could be based primarily on a patient’s underlying CVD risk rather than on his or her cholesterol level. Disseminating a treatment strategy based largely on CVD risk alone has been a difficult message for the clinical community to accept and implement.
Nearly a generation of physicians has considered high-cholesterol levels, rather than generalized CVD risk, the target for statin treatment. Only a minority of physicians consistently use complex, risk-based probabilistic calculations to determine therapy.
Several key questions deserve careful consideration. Should LDL be considered in treatment recommendations beyond CVD risk? The decision to use absolute risk to guide statin recommendations is based on the finding that the relative risk reduction seen with statin therapy is independent of baseline risk; thus, those with the highest absolute baseline CVD risk experience the greatest reduction in CVD events.
However, the relative risk reduction of lipid-lowering therapy is also proportional to mmol/dL reduction in LDL level. This supports the contention that those with the highest baseline LDL levels should benefit the most from treatment because they have the most potential decline in LDL with intervention. One way to reconcile these findings is to incorporate both LDL levels and CVD risk into treatment recommendations, as has been done in the European guidelines. This approach recognizes that the relative benefit of statins is proportional to LDL lowering but that the absolute treatment benefit is largely driven by baseline risk.
From the resource perspective, the vast majority of statins are now available as generic products and require limited monitoring, leading to quite modest therapeutic costs. For patients in the gray area not covered by the guidelines, clinicians should be cautioned against adopting either a “treat none” or a “treat all” strategy. Rather, gaps in the evidence provide opportunities for clinicians to practice the art of medicine and engage with patients in shared decision-making regarding strategies for CVD prevention.
Ann Marie Navar, MD, PhD, and Eric Peterson, MD, MPH, are both at the Duke Clinical Research Institute in Durham, N.C. Dr. Navar reported funding from Regeneron and Sanofi. Dr. Peterson reported funding from Merck, Sanofi, Regeneron, and AstraZeneca. They made their comments in an editorial to the USPSTF report (JAMA. 2016 Nov;316[19]:1981-3).
Dare cardiovascular experts consider a future in which there are near-universal statin recommendations for middle-aged adults?
[USPSTF analysis suggests] that statin recommendations could be based primarily on a patient’s underlying CVD risk rather than on his or her cholesterol level. Disseminating a treatment strategy based largely on CVD risk alone has been a difficult message for the clinical community to accept and implement.
Nearly a generation of physicians has considered high-cholesterol levels, rather than generalized CVD risk, the target for statin treatment. Only a minority of physicians consistently use complex, risk-based probabilistic calculations to determine therapy.
Several key questions deserve careful consideration. Should LDL be considered in treatment recommendations beyond CVD risk? The decision to use absolute risk to guide statin recommendations is based on the finding that the relative risk reduction seen with statin therapy is independent of baseline risk; thus, those with the highest absolute baseline CVD risk experience the greatest reduction in CVD events.
However, the relative risk reduction of lipid-lowering therapy is also proportional to mmol/dL reduction in LDL level. This supports the contention that those with the highest baseline LDL levels should benefit the most from treatment because they have the most potential decline in LDL with intervention. One way to reconcile these findings is to incorporate both LDL levels and CVD risk into treatment recommendations, as has been done in the European guidelines. This approach recognizes that the relative benefit of statins is proportional to LDL lowering but that the absolute treatment benefit is largely driven by baseline risk.
From the resource perspective, the vast majority of statins are now available as generic products and require limited monitoring, leading to quite modest therapeutic costs. For patients in the gray area not covered by the guidelines, clinicians should be cautioned against adopting either a “treat none” or a “treat all” strategy. Rather, gaps in the evidence provide opportunities for clinicians to practice the art of medicine and engage with patients in shared decision-making regarding strategies for CVD prevention.
Ann Marie Navar, MD, PhD, and Eric Peterson, MD, MPH, are both at the Duke Clinical Research Institute in Durham, N.C. Dr. Navar reported funding from Regeneron and Sanofi. Dr. Peterson reported funding from Merck, Sanofi, Regeneron, and AstraZeneca. They made their comments in an editorial to the USPSTF report (JAMA. 2016 Nov;316[19]:1981-3).
Use of statins for the primary prevention of cardiovascular disease should be based on overall cardiovascular disease risk, not necessarily blood lipid levels, according to new recommendations from the United States Preventive Services Task Force.
Despite widespread use in the elderly, USPSTF also said there’s insufficient evidence to recommend starting statins for cardiovascular disease (CVD) prevention in patients 76 years or older (JAMA. 2016 Nov;316[19]:1997-2007).
USPSTF now recommends low- to moderate-dose statins for primary prevention in adults 40-75 years old who have at least one CVD risk factor – dyslipidemia, diabetes, hypertension, or smoking – and a 10-year CVD event risk of at least 10% (B grade). It also recommended “selectively” offering low- to moderate-dose statins if patients have a 7.5%-10% risk (C grade). The task force recommends using the online American College of Cardiology/American Heart Association risk calculator.
A B grade denotes that USPSTF recommends the service as one where there is “high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial.” With a C grade, the task force recommends that the service be provided subject to professional judgment and patient preferences.
The new advices from USPSTF is consistent with the task force’s 2015 draft proposals, and is based on a pooled analysis of 19 randomized trials in 71,344 adults at risk for CVD but without prior events; 17 of the studies were sponsored at least in part by the companies that make statins. The median duration of follow-up was 3 years. Trials included atorvastatin (Lipitor) and six other statins from 1994-2016.
Few of the 19 trials enrolled patients older than 75 years, so “the balance of benefits and harms of initiating statin use for” primary prevention in elderly adults “cannot be determined.” The task force did not make a recommendation either way, and called for further investigation.
For younger patients, the scales tipped toward benefit when the group found no overall increased risk of cancer, liver damage, diabetes, or cognitive problems with statins for primary prevention. “Although muscle pain, soreness, or weakness are commonly reported with statin use, there were no statistically significant differences between the intervention and control groups for myalgia, myopathy, or rhabdomyolysis,” according to the task force.
Across the 19 trials, statin therapy was associated with a statistically significant 14% reduction in all-cause mortality; 31% reduction in cardiovascular mortality; 29% reduction in stroke; and a 36% reduction in myocardial infarction; 250 patients needed to be treated to prevent one death from any cause after 1-6 years, and 233 to prevent one cardiovascular death after 2-6 years.
The recommendations call for low to moderate doses because that’s what most of the studies used, and there were no clear benefits when trials stratified patients by dose.
USPSTF cautioned that “reliance on a risk calculator ... alone as a basis for prevention may be problematic, given its possible overestimation of risk in some populations” and noted that the benefits “of statin use may be linear according to a patient’s absolute risk level, and any cut points used are only population estimates of benefits.”
The recommendations do not pertain to adults with very high CVD risk, such as those with familial hypercholesterolemia or an LDL level greater than 190mg/dL, since they were excluded from primary prevention trials.
While the USPSTF was careful in its evidence review, “ the limitations of the evidence were not considered sufficiently, given the serious concerns about the harms of statins for primary prevention,” Rita Redberg, MD, and Mitchell Katz, MD, wrote in an editorial accompanying the recommendations.
“USPSTF also did not have access to patient-level data; they had to rely on peer-reviewed published reports,” according to the editorialists. “The actual trial data are largely held by the Cholesterol Treatment Trialists’ Collaboration on behalf of industry sponsors and have not been made available to other researchers, despite multiple requests over many years.” Further, many of the trials were industry sponsored.
Using the USPSTF data, only 2% of patients who take statins for 5 years will avoid a myocardial infarction; virtually all (98%) will not experience any benefit. At the same time, 5%-20% will experience side effects including rhabdomyolysis, cognitive dysfunction, and increased risk of diabetes (JAMA. 2016 Nov;316[19]:1979-81).
There are unintended consequences of widespread statin use in healthy persons, Dr. Redberg and Dr. Katz wrote. People taking statins are more likely to become obese and more sedentary over time, likely because they mistakenly think they do not need to eat a healthy diet and exercise.
The USPSTF analysis was funded by the Agency for Healthcare Research and Quality. Task force lead Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco, has advised the Institute for Clinical and Economic Review, which is partly funded by industry, on the cost-effectiveness of lipid-lowering drugs. Another member reported comparing how well they worked. The other 15 task force members had no disclosures.
Use of statins for the primary prevention of cardiovascular disease should be based on overall cardiovascular disease risk, not necessarily blood lipid levels, according to new recommendations from the United States Preventive Services Task Force.
Despite widespread use in the elderly, USPSTF also said there’s insufficient evidence to recommend starting statins for cardiovascular disease (CVD) prevention in patients 76 years or older (JAMA. 2016 Nov;316[19]:1997-2007).
USPSTF now recommends low- to moderate-dose statins for primary prevention in adults 40-75 years old who have at least one CVD risk factor – dyslipidemia, diabetes, hypertension, or smoking – and a 10-year CVD event risk of at least 10% (B grade). It also recommended “selectively” offering low- to moderate-dose statins if patients have a 7.5%-10% risk (C grade). The task force recommends using the online American College of Cardiology/American Heart Association risk calculator.
A B grade denotes that USPSTF recommends the service as one where there is “high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial.” With a C grade, the task force recommends that the service be provided subject to professional judgment and patient preferences.
The new advices from USPSTF is consistent with the task force’s 2015 draft proposals, and is based on a pooled analysis of 19 randomized trials in 71,344 adults at risk for CVD but without prior events; 17 of the studies were sponsored at least in part by the companies that make statins. The median duration of follow-up was 3 years. Trials included atorvastatin (Lipitor) and six other statins from 1994-2016.
Few of the 19 trials enrolled patients older than 75 years, so “the balance of benefits and harms of initiating statin use for” primary prevention in elderly adults “cannot be determined.” The task force did not make a recommendation either way, and called for further investigation.
For younger patients, the scales tipped toward benefit when the group found no overall increased risk of cancer, liver damage, diabetes, or cognitive problems with statins for primary prevention. “Although muscle pain, soreness, or weakness are commonly reported with statin use, there were no statistically significant differences between the intervention and control groups for myalgia, myopathy, or rhabdomyolysis,” according to the task force.
Across the 19 trials, statin therapy was associated with a statistically significant 14% reduction in all-cause mortality; 31% reduction in cardiovascular mortality; 29% reduction in stroke; and a 36% reduction in myocardial infarction; 250 patients needed to be treated to prevent one death from any cause after 1-6 years, and 233 to prevent one cardiovascular death after 2-6 years.
The recommendations call for low to moderate doses because that’s what most of the studies used, and there were no clear benefits when trials stratified patients by dose.
USPSTF cautioned that “reliance on a risk calculator ... alone as a basis for prevention may be problematic, given its possible overestimation of risk in some populations” and noted that the benefits “of statin use may be linear according to a patient’s absolute risk level, and any cut points used are only population estimates of benefits.”
The recommendations do not pertain to adults with very high CVD risk, such as those with familial hypercholesterolemia or an LDL level greater than 190mg/dL, since they were excluded from primary prevention trials.
While the USPSTF was careful in its evidence review, “ the limitations of the evidence were not considered sufficiently, given the serious concerns about the harms of statins for primary prevention,” Rita Redberg, MD, and Mitchell Katz, MD, wrote in an editorial accompanying the recommendations.
“USPSTF also did not have access to patient-level data; they had to rely on peer-reviewed published reports,” according to the editorialists. “The actual trial data are largely held by the Cholesterol Treatment Trialists’ Collaboration on behalf of industry sponsors and have not been made available to other researchers, despite multiple requests over many years.” Further, many of the trials were industry sponsored.
Using the USPSTF data, only 2% of patients who take statins for 5 years will avoid a myocardial infarction; virtually all (98%) will not experience any benefit. At the same time, 5%-20% will experience side effects including rhabdomyolysis, cognitive dysfunction, and increased risk of diabetes (JAMA. 2016 Nov;316[19]:1979-81).
There are unintended consequences of widespread statin use in healthy persons, Dr. Redberg and Dr. Katz wrote. People taking statins are more likely to become obese and more sedentary over time, likely because they mistakenly think they do not need to eat a healthy diet and exercise.
The USPSTF analysis was funded by the Agency for Healthcare Research and Quality. Task force lead Kirsten Bibbins-Domingo, MD, PhD, of the University of California, San Francisco, has advised the Institute for Clinical and Economic Review, which is partly funded by industry, on the cost-effectiveness of lipid-lowering drugs. Another member reported comparing how well they worked. The other 15 task force members had no disclosures.
Travel barriers can impede patient choice for pancreatectomy
AT THE ACS CLINICAL CONGRESS
WASHINGTON – Patients who have the resources to travel to higher-volume hospitals for pancreatectomy have better outcomes than do those who opt to have the surgery in local, small-volume hospitals.
A 10-year review of travel patterns associated with pancreatectomy in California found those who didn’t travel were often elderly, black or Hispanic, and were either self-pay or had public insurance.
“It’s probably because these patients don’t have the resources [finances and transportation] to travel far to the best hospitals for their surgery and have to rely on the closest hospitals for better or for worse – and it seems more like the latter,” he said in an interview at the annual clinical congress of the American College of Surgeons. “So what you see is there is an aspatial barrier to access [limited insurance], as well as spatial barriers to access.”
He and his mentor, David C. Chang, PhD, examined about 13,000 pancreatectomy records included in the California Office of Statewide Health Planning and Development database from 2005 to 2014. The research was conducted at Harvard University and the Massachusetts General Hospital, Boston.
The majority of these patients (11,000) bypassed at least one hospital that offered pancreatectomy to reach their ultimate choice. After bypassing a median of seven facilities, they ended up traveling about 16 miles from home to reach their chosen hospital. Patients who stuck to the closest hospital traveled only about 3 miles.
Generally, bypassers tended to end up in higher-volume hospitals with better outcomes. About half had their pancreatectomy at a hospital that performed more than 20 per year; 40% were at a facility that performed in excess of 40 pancreatectomies annually. Almost 50% of the bypassers also had their surgery at a teaching hospital. The median length of stay at these facilities was 10 days, and they had a median pancreatectomy mortality rate of 3%.
In contrast, patients who didn’t travel ended up at lower-volume hospitals; 60% had their pancreatectomy at a hospital that performed fewer than 10 per year and 22% at a hospital that performed 10-20 per year. Only 18% were treated at an academic center. These hospitals had a significantly longer pancreatectomy length of stay (12 days) and significantly higher pancreatectomy mortality rate (6%).
Older patients were less likely to travel. The age difference came into play beginning at age 50 and grew stronger as patients aged.
Insurance status was highly associated with hospital destination. Privately insured patients were the most likely to travel to better hospitals, followed by those on Medicare. Patients on Medicaid and those who identified as self-pay were significantly less likely to travel. Minorities traveled far less as well; blacks were the least likely to travel from their home base.
In this time of value-based surgical outcomes, the study has some interesting implications, Dr. Fong said. Many health care systems are undertaking a volume pledge, which aims to funnel patients who need high-risk procedures to centers that perform a large number of them annually. But there is a flip side to that coin, which could, in essence, make things even tougher on patients who find travel challenging.
“The Volume Pledge aims to stop hospitals that are low volume in certain procedures from continuing to do them, on the basis that high-volume hospitals often do better in terms of outcomes. But there are very much unintended consequences of the pledge, such as hampering access to surgery. Because inevitably, you’ll increase distance needed to travel for each patient to get care if low-volume hospitals stopped offering their services.”
In his study, Dr. Fong found that some California counties had only one hospital that offered pancreatectomy, and that was a low-volume facility. If that hospital was forced to stop offering the procedure, patients with less resources could face even more obstacles to getting the treatment they need.
“Eliminating [low-volume hospital procedures] will have dire consequences. Our study showed that the elderly, racial/ethnic minorities, uninsured and those on Medicaid generally don’t travel for care, and this pledge may compound on that and widen disparity or even worse, some may not even get care as a result.”
Dr. Fong had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE ACS CLINICAL CONGRESS
WASHINGTON – Patients who have the resources to travel to higher-volume hospitals for pancreatectomy have better outcomes than do those who opt to have the surgery in local, small-volume hospitals.
A 10-year review of travel patterns associated with pancreatectomy in California found those who didn’t travel were often elderly, black or Hispanic, and were either self-pay or had public insurance.
“It’s probably because these patients don’t have the resources [finances and transportation] to travel far to the best hospitals for their surgery and have to rely on the closest hospitals for better or for worse – and it seems more like the latter,” he said in an interview at the annual clinical congress of the American College of Surgeons. “So what you see is there is an aspatial barrier to access [limited insurance], as well as spatial barriers to access.”
He and his mentor, David C. Chang, PhD, examined about 13,000 pancreatectomy records included in the California Office of Statewide Health Planning and Development database from 2005 to 2014. The research was conducted at Harvard University and the Massachusetts General Hospital, Boston.
The majority of these patients (11,000) bypassed at least one hospital that offered pancreatectomy to reach their ultimate choice. After bypassing a median of seven facilities, they ended up traveling about 16 miles from home to reach their chosen hospital. Patients who stuck to the closest hospital traveled only about 3 miles.
Generally, bypassers tended to end up in higher-volume hospitals with better outcomes. About half had their pancreatectomy at a hospital that performed more than 20 per year; 40% were at a facility that performed in excess of 40 pancreatectomies annually. Almost 50% of the bypassers also had their surgery at a teaching hospital. The median length of stay at these facilities was 10 days, and they had a median pancreatectomy mortality rate of 3%.
In contrast, patients who didn’t travel ended up at lower-volume hospitals; 60% had their pancreatectomy at a hospital that performed fewer than 10 per year and 22% at a hospital that performed 10-20 per year. Only 18% were treated at an academic center. These hospitals had a significantly longer pancreatectomy length of stay (12 days) and significantly higher pancreatectomy mortality rate (6%).
Older patients were less likely to travel. The age difference came into play beginning at age 50 and grew stronger as patients aged.
Insurance status was highly associated with hospital destination. Privately insured patients were the most likely to travel to better hospitals, followed by those on Medicare. Patients on Medicaid and those who identified as self-pay were significantly less likely to travel. Minorities traveled far less as well; blacks were the least likely to travel from their home base.
In this time of value-based surgical outcomes, the study has some interesting implications, Dr. Fong said. Many health care systems are undertaking a volume pledge, which aims to funnel patients who need high-risk procedures to centers that perform a large number of them annually. But there is a flip side to that coin, which could, in essence, make things even tougher on patients who find travel challenging.
“The Volume Pledge aims to stop hospitals that are low volume in certain procedures from continuing to do them, on the basis that high-volume hospitals often do better in terms of outcomes. But there are very much unintended consequences of the pledge, such as hampering access to surgery. Because inevitably, you’ll increase distance needed to travel for each patient to get care if low-volume hospitals stopped offering their services.”
In his study, Dr. Fong found that some California counties had only one hospital that offered pancreatectomy, and that was a low-volume facility. If that hospital was forced to stop offering the procedure, patients with less resources could face even more obstacles to getting the treatment they need.
“Eliminating [low-volume hospital procedures] will have dire consequences. Our study showed that the elderly, racial/ethnic minorities, uninsured and those on Medicaid generally don’t travel for care, and this pledge may compound on that and widen disparity or even worse, some may not even get care as a result.”
Dr. Fong had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE ACS CLINICAL CONGRESS
WASHINGTON – Patients who have the resources to travel to higher-volume hospitals for pancreatectomy have better outcomes than do those who opt to have the surgery in local, small-volume hospitals.
A 10-year review of travel patterns associated with pancreatectomy in California found those who didn’t travel were often elderly, black or Hispanic, and were either self-pay or had public insurance.
“It’s probably because these patients don’t have the resources [finances and transportation] to travel far to the best hospitals for their surgery and have to rely on the closest hospitals for better or for worse – and it seems more like the latter,” he said in an interview at the annual clinical congress of the American College of Surgeons. “So what you see is there is an aspatial barrier to access [limited insurance], as well as spatial barriers to access.”
He and his mentor, David C. Chang, PhD, examined about 13,000 pancreatectomy records included in the California Office of Statewide Health Planning and Development database from 2005 to 2014. The research was conducted at Harvard University and the Massachusetts General Hospital, Boston.
The majority of these patients (11,000) bypassed at least one hospital that offered pancreatectomy to reach their ultimate choice. After bypassing a median of seven facilities, they ended up traveling about 16 miles from home to reach their chosen hospital. Patients who stuck to the closest hospital traveled only about 3 miles.
Generally, bypassers tended to end up in higher-volume hospitals with better outcomes. About half had their pancreatectomy at a hospital that performed more than 20 per year; 40% were at a facility that performed in excess of 40 pancreatectomies annually. Almost 50% of the bypassers also had their surgery at a teaching hospital. The median length of stay at these facilities was 10 days, and they had a median pancreatectomy mortality rate of 3%.
In contrast, patients who didn’t travel ended up at lower-volume hospitals; 60% had their pancreatectomy at a hospital that performed fewer than 10 per year and 22% at a hospital that performed 10-20 per year. Only 18% were treated at an academic center. These hospitals had a significantly longer pancreatectomy length of stay (12 days) and significantly higher pancreatectomy mortality rate (6%).
Older patients were less likely to travel. The age difference came into play beginning at age 50 and grew stronger as patients aged.
Insurance status was highly associated with hospital destination. Privately insured patients were the most likely to travel to better hospitals, followed by those on Medicare. Patients on Medicaid and those who identified as self-pay were significantly less likely to travel. Minorities traveled far less as well; blacks were the least likely to travel from their home base.
In this time of value-based surgical outcomes, the study has some interesting implications, Dr. Fong said. Many health care systems are undertaking a volume pledge, which aims to funnel patients who need high-risk procedures to centers that perform a large number of them annually. But there is a flip side to that coin, which could, in essence, make things even tougher on patients who find travel challenging.
“The Volume Pledge aims to stop hospitals that are low volume in certain procedures from continuing to do them, on the basis that high-volume hospitals often do better in terms of outcomes. But there are very much unintended consequences of the pledge, such as hampering access to surgery. Because inevitably, you’ll increase distance needed to travel for each patient to get care if low-volume hospitals stopped offering their services.”
In his study, Dr. Fong found that some California counties had only one hospital that offered pancreatectomy, and that was a low-volume facility. If that hospital was forced to stop offering the procedure, patients with less resources could face even more obstacles to getting the treatment they need.
“Eliminating [low-volume hospital procedures] will have dire consequences. Our study showed that the elderly, racial/ethnic minorities, uninsured and those on Medicaid generally don’t travel for care, and this pledge may compound on that and widen disparity or even worse, some may not even get care as a result.”
Dr. Fong had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
Key clinical point:
Major finding: About 60% of patients who didn’t travel had surgery at a low-volume hospital with a higher mortality rate and longer length of stay.
Data source: The 10-year California database review comprised 13,000 patients.
Disclosures: Dr. Fong had no financial disclosures.
VIDEO: Blood pressure and LDL lowering in elderly do not slow cognitive decline
NEW ORLEANS – Blood pressure and cholesterol lowering in elderly patients with moderate vascular risk did not prevent cognitive decline in HOPE-3, the large randomized Heart Outcomes and Prevention Evaluation-3 trial, Jackie Bosch, PhD, reported at the American Heart Association scientific sessions.
Disappointing, but the study also brought some welcome glass-half-full good news: Although treatment did not slow cognitive decline, it didn’t worsen it, either, as some had feared. That means the clinically meaningful reduction in cardiovascular events conferred with blood pressure and cholesterol lowering previously reported in HOPE-3 does not come at the cost of an increased risk of dementia.
Rosuvastatin had no adverse effect on cognitive function in HOPE-3. This is an important finding, given the black box warning for statins mandated by the Food and Drug Administration, which was based only on observational postmarketing surveillance data,” observed Dr. Bosch of the Population Health Research Institute at McMaster University in Hamilton, Ont.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bosch reported on the 1,626 subjects who were at least 70 years old at baseline – their mean age was 75 – and who completed a battery of cognitive and functional status tests and questionnaires at baseline.
The primary outcome in the HOPE-3 cognition substudy was decline over time in processing speed as measured on the Digit Symbol Substitution Test. There was an equal decline, regardless of whether patients were on blood pressure lowering, rosuvastatin, both, or double placebo.
Nor did statin- or blood pressure–lowering therapy have any impact on the secondary endpoints of decline in executive function as assessed by the modified Montreal Cognitive Assessment or the change in psychomotor speed as reflected in the Trail Making Test part B.
Moreover, treatment had no effect on age-related decline in overall functional status. During a mean of 5.6 years of follow-up, 22% of participants developed a new functional impairment regardless of whether they were on blood pressure– and/or cholesterol-lowering medication or double placebo.
Intriguingly, however, subgroup analyses provided a glimmer of hope. Patients who were in the top tertile for blood pressure at baseline, with a systolic blood pressure of 133 mm Hg or more, as well as the top tertile for LDL cholesterol, with an LDL of at least 112 mg/dL, showed significantly less decline in cognitive function over time if they were on rosuvastatin and blood pressure lowering than with double placebo. This higher-risk group showed a mean loss of only 4.65 points on the Digit Symbol Substitution Test, compared with an 11.8-point drop for those on double placebo. This is a post-hoc analysis, however, and the efficacy signal must be viewed as hypothesis generating, Dr. Bosch stressed.
Discussant Philip B. Gorelick, MD, MPH, said that he didn’t find the negative HOPE-3 cognition results surprising. After all, he coauthored a recent AHA/American Stroke Association Scientific Statement on the impact of hypertension on cognitive function that scrutinized 10 clinical hypertension trials and concluded that only two of them – SYST-EUR (Systolic Hypertension in Europe) and PROGRESS (Peridopril Protection Against Recurrent Stroke Study) – showed any indication that treating hypertension reduced cognitive decline (Hypertension. 2016. doi: 10.1161/HYP.0000000000000053).
Plus, a 2016 Cochrane Collaboration review of the published evidence concluded that, in older people at vascular risk, statins do not prevent cognitive decline or dementia after 3.5-5 years of treatment (Cochrane Database Syst Rev. 2016 Jan 4;[1]:CD003160).
“The horse may be out of the barn for many of our patients when we start intervening later in life. That’s not to say it can’t work, but the Alzheimer’s changes and disease process are beginning 20 or 30 years earlier, so we’ve got to intervene earlier,” said Dr. Gorelick, professor of translational science and molecular medicine at the Michigan State University College of Human Medicine, Grand Rapids.
Dr. Bosch concurred. “We know that, in epidemiologic studies, midlife hypertension is strongly associated with later cognitive impairment. We’ve missed the boat on the 70-year-olds,” she said. “We need to start treatment earlier and probably for longer.”
Dr. Bosch reported having no financial conflicts regarding the HOPE-3 study, which was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. Dr. Gorelick reported serving as a consultant to Novartis regarding blood pressure lowering and maintenance of cognition.
NEW ORLEANS – Blood pressure and cholesterol lowering in elderly patients with moderate vascular risk did not prevent cognitive decline in HOPE-3, the large randomized Heart Outcomes and Prevention Evaluation-3 trial, Jackie Bosch, PhD, reported at the American Heart Association scientific sessions.
Disappointing, but the study also brought some welcome glass-half-full good news: Although treatment did not slow cognitive decline, it didn’t worsen it, either, as some had feared. That means the clinically meaningful reduction in cardiovascular events conferred with blood pressure and cholesterol lowering previously reported in HOPE-3 does not come at the cost of an increased risk of dementia.
Rosuvastatin had no adverse effect on cognitive function in HOPE-3. This is an important finding, given the black box warning for statins mandated by the Food and Drug Administration, which was based only on observational postmarketing surveillance data,” observed Dr. Bosch of the Population Health Research Institute at McMaster University in Hamilton, Ont.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bosch reported on the 1,626 subjects who were at least 70 years old at baseline – their mean age was 75 – and who completed a battery of cognitive and functional status tests and questionnaires at baseline.
The primary outcome in the HOPE-3 cognition substudy was decline over time in processing speed as measured on the Digit Symbol Substitution Test. There was an equal decline, regardless of whether patients were on blood pressure lowering, rosuvastatin, both, or double placebo.
Nor did statin- or blood pressure–lowering therapy have any impact on the secondary endpoints of decline in executive function as assessed by the modified Montreal Cognitive Assessment or the change in psychomotor speed as reflected in the Trail Making Test part B.
Moreover, treatment had no effect on age-related decline in overall functional status. During a mean of 5.6 years of follow-up, 22% of participants developed a new functional impairment regardless of whether they were on blood pressure– and/or cholesterol-lowering medication or double placebo.
Intriguingly, however, subgroup analyses provided a glimmer of hope. Patients who were in the top tertile for blood pressure at baseline, with a systolic blood pressure of 133 mm Hg or more, as well as the top tertile for LDL cholesterol, with an LDL of at least 112 mg/dL, showed significantly less decline in cognitive function over time if they were on rosuvastatin and blood pressure lowering than with double placebo. This higher-risk group showed a mean loss of only 4.65 points on the Digit Symbol Substitution Test, compared with an 11.8-point drop for those on double placebo. This is a post-hoc analysis, however, and the efficacy signal must be viewed as hypothesis generating, Dr. Bosch stressed.
Discussant Philip B. Gorelick, MD, MPH, said that he didn’t find the negative HOPE-3 cognition results surprising. After all, he coauthored a recent AHA/American Stroke Association Scientific Statement on the impact of hypertension on cognitive function that scrutinized 10 clinical hypertension trials and concluded that only two of them – SYST-EUR (Systolic Hypertension in Europe) and PROGRESS (Peridopril Protection Against Recurrent Stroke Study) – showed any indication that treating hypertension reduced cognitive decline (Hypertension. 2016. doi: 10.1161/HYP.0000000000000053).
Plus, a 2016 Cochrane Collaboration review of the published evidence concluded that, in older people at vascular risk, statins do not prevent cognitive decline or dementia after 3.5-5 years of treatment (Cochrane Database Syst Rev. 2016 Jan 4;[1]:CD003160).
“The horse may be out of the barn for many of our patients when we start intervening later in life. That’s not to say it can’t work, but the Alzheimer’s changes and disease process are beginning 20 or 30 years earlier, so we’ve got to intervene earlier,” said Dr. Gorelick, professor of translational science and molecular medicine at the Michigan State University College of Human Medicine, Grand Rapids.
Dr. Bosch concurred. “We know that, in epidemiologic studies, midlife hypertension is strongly associated with later cognitive impairment. We’ve missed the boat on the 70-year-olds,” she said. “We need to start treatment earlier and probably for longer.”
Dr. Bosch reported having no financial conflicts regarding the HOPE-3 study, which was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. Dr. Gorelick reported serving as a consultant to Novartis regarding blood pressure lowering and maintenance of cognition.
NEW ORLEANS – Blood pressure and cholesterol lowering in elderly patients with moderate vascular risk did not prevent cognitive decline in HOPE-3, the large randomized Heart Outcomes and Prevention Evaluation-3 trial, Jackie Bosch, PhD, reported at the American Heart Association scientific sessions.
Disappointing, but the study also brought some welcome glass-half-full good news: Although treatment did not slow cognitive decline, it didn’t worsen it, either, as some had feared. That means the clinically meaningful reduction in cardiovascular events conferred with blood pressure and cholesterol lowering previously reported in HOPE-3 does not come at the cost of an increased risk of dementia.
Rosuvastatin had no adverse effect on cognitive function in HOPE-3. This is an important finding, given the black box warning for statins mandated by the Food and Drug Administration, which was based only on observational postmarketing surveillance data,” observed Dr. Bosch of the Population Health Research Institute at McMaster University in Hamilton, Ont.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bosch reported on the 1,626 subjects who were at least 70 years old at baseline – their mean age was 75 – and who completed a battery of cognitive and functional status tests and questionnaires at baseline.
The primary outcome in the HOPE-3 cognition substudy was decline over time in processing speed as measured on the Digit Symbol Substitution Test. There was an equal decline, regardless of whether patients were on blood pressure lowering, rosuvastatin, both, or double placebo.
Nor did statin- or blood pressure–lowering therapy have any impact on the secondary endpoints of decline in executive function as assessed by the modified Montreal Cognitive Assessment or the change in psychomotor speed as reflected in the Trail Making Test part B.
Moreover, treatment had no effect on age-related decline in overall functional status. During a mean of 5.6 years of follow-up, 22% of participants developed a new functional impairment regardless of whether they were on blood pressure– and/or cholesterol-lowering medication or double placebo.
Intriguingly, however, subgroup analyses provided a glimmer of hope. Patients who were in the top tertile for blood pressure at baseline, with a systolic blood pressure of 133 mm Hg or more, as well as the top tertile for LDL cholesterol, with an LDL of at least 112 mg/dL, showed significantly less decline in cognitive function over time if they were on rosuvastatin and blood pressure lowering than with double placebo. This higher-risk group showed a mean loss of only 4.65 points on the Digit Symbol Substitution Test, compared with an 11.8-point drop for those on double placebo. This is a post-hoc analysis, however, and the efficacy signal must be viewed as hypothesis generating, Dr. Bosch stressed.
Discussant Philip B. Gorelick, MD, MPH, said that he didn’t find the negative HOPE-3 cognition results surprising. After all, he coauthored a recent AHA/American Stroke Association Scientific Statement on the impact of hypertension on cognitive function that scrutinized 10 clinical hypertension trials and concluded that only two of them – SYST-EUR (Systolic Hypertension in Europe) and PROGRESS (Peridopril Protection Against Recurrent Stroke Study) – showed any indication that treating hypertension reduced cognitive decline (Hypertension. 2016. doi: 10.1161/HYP.0000000000000053).
Plus, a 2016 Cochrane Collaboration review of the published evidence concluded that, in older people at vascular risk, statins do not prevent cognitive decline or dementia after 3.5-5 years of treatment (Cochrane Database Syst Rev. 2016 Jan 4;[1]:CD003160).
“The horse may be out of the barn for many of our patients when we start intervening later in life. That’s not to say it can’t work, but the Alzheimer’s changes and disease process are beginning 20 or 30 years earlier, so we’ve got to intervene earlier,” said Dr. Gorelick, professor of translational science and molecular medicine at the Michigan State University College of Human Medicine, Grand Rapids.
Dr. Bosch concurred. “We know that, in epidemiologic studies, midlife hypertension is strongly associated with later cognitive impairment. We’ve missed the boat on the 70-year-olds,” she said. “We need to start treatment earlier and probably for longer.”
Dr. Bosch reported having no financial conflicts regarding the HOPE-3 study, which was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. Dr. Gorelick reported serving as a consultant to Novartis regarding blood pressure lowering and maintenance of cognition.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Nearly 6 years of blood pressure lowering and statin therapy in elderly patients with moderate vascular risk did not prevent cognitive decline relative to placebo, but the treatment did not worsen it, either.
Data source: This analysis of cognitive and functional outcomes in the randomized multicenter HOPE-3 trial included 1,626 participants who were at least 70 years old at baseline, when they were randomized to blood pressure lowering or placebo and rosuvastatin or placebo and followed for a mean of 5.6 years.
Disclosures: The HOPE-3 study was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. The presenter reported having no financial conflicts of interest.
VIDEO: PRECISION exonerates celecoxib: cardiovascular risk is no worse than that of nonselective NSAIDs
NEW ORLEANS – The cardiovascular safety profile of the nonsteroidal anti-inflammatory drug (NSAID) celecoxib, a selective inhibitor of COX-2, is no worse than those of the nonselective NSAIDs naproxen and ibuprofen, according to a trial reported at the American Heart Association scientific sessions.
The trial, known as PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen Or Naproxen) was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that 2%-3% of patients experienced a cardiovascular event (cardiovascular death, myocardial infarction, or stroke) during a follow-up approaching 3 years, regardless of which drug they were assigned to take, with the slight differences falling within predefined margins for noninferiority of celecoxib, investigators reported in a session and related press conference.
Additionally, celecoxib yielded a lower rate of gastrointestinal events when compared with each of the other drugs and a lower rate of renal events when compared with ibuprofen.
“After the withdrawal of rofecoxib, everybody thought they knew the answer, that COX-2 inhibitors had an unfavorable cardiovascular profile,” commented first author Steven E. Nissen, MD, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “We didn’t find that. And this is the type of study that once again teaches us that if we jump to conclusions about this based on mechanistic considerations, we often make very bad decisions.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Efforts are under way to disseminate the PRECISION findings to rheumatologists and other groups who do much of the NSAID prescribing.
“Any time you have something that has findings like the findings we have, it takes some time to trickle down to the prescribers. It’s going to be our job to communicate both the value and the important limitations of the trial so that people can make informed decisions about which of these drugs to use and in whom,” Dr. Nissen said.
A cautionary view
“The investigators addressed an extremely important question, which is what is the cardiovascular safety of agents that we administer for a general medical condition over the long term,” commented invited discussant Elliott M. Antman, MD, a senior physician at Brigham and Women’s Hospital and associate dean for Clinical and Translational Research at Harvard Medical School in Boston. “We don’t see a lot of trials like that, but we do need this information.”
“This is not a comparison of drugs; this is a comparison of drug regimens because the investigators were able to increase the dose to control the subjects’ pain,” Dr. Antman elaborated. “And they were able to increase the dose of naproxen and ibuprofen comparatively more than they could for celecoxib,” which was capped at 200 mg per day at most study sites.
Furthermore, only about one-fifth of the patients studied had known heart disease. “We know that the more likely a person is to have atherosclerosis, the more likely they are to experience harm from COX-2 inhibition,” he said. “So given the profile of the patients in this trial, it’s unlikely that we would have been able to detect that signal of harm from COX-2 inhibition, particularly at this dose.”
Dr. Antman also had concerns about the impact on concomitant aspirin therapy (the benefit of which can be affected by nonselective NSAIDs) and about possible differences in the reasons for dropouts that may have biased findings toward celecoxib. “I believe we need more information in order to more completely interpret this trial,” he summarized.
For now, he advised physicians to follow guidance put forth by the American Heart Association: Avoid NSAIDs in patients with known heart disease, and if one must use them, try to use the lowest-risk drug in the lowest dose needed for the shortest period of time.
In the future, “we should actually break out of the mold of assigning everybody in the trial a common phenotype and reporting the average result, but instead take a precision medicine approach, where we look at the polymorphisms in the COX enzyme, look at the polymorphisms in the ability to metabolize these drugs, and actually see if we can be more precise,” Dr. Antman maintained. “Finally, there is an urgent clinical need for the development of novel analgesics and other therapeutics to avoid the cardiovascular risk from all NSAIDs.”
Trial details
Patients were eligible for PRECISION, a Pfizer-funded trial, if they had osteoarthritis or rheumatoid arthritis and were at increased cardiovascular risk.
In all, 24,081 patients from 926 centers globally were randomly assigned to double-blind treatment with celecoxib, naproxen, or ibuprofen, all of which are now available as generics in the United States.
“Patients were randomized to the FDA-approved doses of these drugs, and they could have their dose increased if they had unrelieved pain up to the maximum allowed by regulatory authorities in the local jurisdictions where the study was done,” Dr. Nissen noted, pointing out that studies initially generating some concern about celecoxib used a supratherapeutic dose of 800 mg daily.
As COX-2 inhibitors are less likely than nonselective NSAIDs to cause ulcers, which might affect compliance and outcomes, all patients additionally received esomeprazole for gastroprotection “to try to level the playing field,” he explained.
The mean treatment duration was 20.3 months, and the mean follow-up duration was 34.1 months, according to data reported at the meeting and simultaneously published (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593). On average, the daily dose of drug received was 209 mg for celecoxib, 852 mg for naproxen, and 2,045 mg for ibuprofen.
In intention-to-treat analyses, the rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% in the celecoxib group, 2.5% in the naproxen group, and 2.7% in the ibuprofen group. The hazard ratio was 0.93 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.85 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Differences were more marked in the on-treatment population. Here, the rate of the primary outcome was 1.7% in the celecoxib group, 1.8% in the naproxen group, and 1.9% in the ibuprofen group. The HR was 0.90 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.81 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Secondary outcomes, which tested for superiority, showed that the rate of major adverse cardiovascular events was 15% higher in the ibuprofen group as compared with the celecoxib group in the intent-to-treat population. The difference translated to a near-significant reduction in risk with the latter (HR, 0.87; P = .06) that appeared greater in the on-treatment population.
However, Dr. Nissen cautioned that he could not state that celecoxib was superior. “Secondary and tertiary endpoints in a clinical trial are hypothesis generating, and they are not considered definitive evidence,” he commented. At the same time, “the FDA is going to have to deal with that because what do they do with labeling? What do they do with over-the-counter access to these various drugs?”
The rate of all-cause mortality was 25% higher with naproxen than with celecoxib (HR, 0.80; P = .052).
The rate of gastrointestinal events was 54% higher with ibuprofen (HR, 0.65; P = .002) and 41% higher with naproxen (HR, 0.71; P = .01) as compared with celecoxib. And the rate of renal events was 64% higher with ibuprofen than with celecoxib (HR, 0.61; P = .004).
In a post hoc analysis of global safety, the rate of serious cardiovascular, gastrointestinal, and renal events was 28% higher with ibuprofen (HR, 0.78; P less than .001) and 15% higher with naproxen (HR, 0.87; P = .03) than with celecoxib.
Of note, the findings for the primary endpoint were similar regardless of whether patients were taking low-dose aspirin or not. “There was no interaction with aspirin use,” Dr. Nissen stated. “This was not about the interference of ibuprofen or naproxen with aspirin use.”
Analyses of pain relief using a visual analogue scale showed no clinically meaningful differences, suggesting that the drug doses used were equally analgesic, he said. Stopping of study drug because of lack of efficacy was slightly more common in the celecoxib group.
“We didn’t study the low-dose, intermittent use of these drugs that most of the public engages in, and it’s really important that we crisply communicate that to the public because somebody who takes occasionally ibuprofen or naproxen for a headache should not look at these comparative data in a way that should necessarily influence their behavior. We just don’t know the answer,” cautioned Dr. Nissen, who disclosed that he received grant support from Pfizer during the conduct of the trial.
But the findings are relevant for individuals who take over-the-counter NSAIDs at doses exceeding the label, a phenomenon known as dose creep. “We need to reemphasize to the public that the labeled over-the-counter dose is what you should take. You shouldn’t double up or triple up on the drugs because the issue of high-dose therapy, which is what we studied, suggests that there are really potentially important gastrointestinal, renal, and cardiovascular risks,” he said.
NEW ORLEANS – The cardiovascular safety profile of the nonsteroidal anti-inflammatory drug (NSAID) celecoxib, a selective inhibitor of COX-2, is no worse than those of the nonselective NSAIDs naproxen and ibuprofen, according to a trial reported at the American Heart Association scientific sessions.
The trial, known as PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen Or Naproxen) was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that 2%-3% of patients experienced a cardiovascular event (cardiovascular death, myocardial infarction, or stroke) during a follow-up approaching 3 years, regardless of which drug they were assigned to take, with the slight differences falling within predefined margins for noninferiority of celecoxib, investigators reported in a session and related press conference.
Additionally, celecoxib yielded a lower rate of gastrointestinal events when compared with each of the other drugs and a lower rate of renal events when compared with ibuprofen.
“After the withdrawal of rofecoxib, everybody thought they knew the answer, that COX-2 inhibitors had an unfavorable cardiovascular profile,” commented first author Steven E. Nissen, MD, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “We didn’t find that. And this is the type of study that once again teaches us that if we jump to conclusions about this based on mechanistic considerations, we often make very bad decisions.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Efforts are under way to disseminate the PRECISION findings to rheumatologists and other groups who do much of the NSAID prescribing.
“Any time you have something that has findings like the findings we have, it takes some time to trickle down to the prescribers. It’s going to be our job to communicate both the value and the important limitations of the trial so that people can make informed decisions about which of these drugs to use and in whom,” Dr. Nissen said.
A cautionary view
“The investigators addressed an extremely important question, which is what is the cardiovascular safety of agents that we administer for a general medical condition over the long term,” commented invited discussant Elliott M. Antman, MD, a senior physician at Brigham and Women’s Hospital and associate dean for Clinical and Translational Research at Harvard Medical School in Boston. “We don’t see a lot of trials like that, but we do need this information.”
“This is not a comparison of drugs; this is a comparison of drug regimens because the investigators were able to increase the dose to control the subjects’ pain,” Dr. Antman elaborated. “And they were able to increase the dose of naproxen and ibuprofen comparatively more than they could for celecoxib,” which was capped at 200 mg per day at most study sites.
Furthermore, only about one-fifth of the patients studied had known heart disease. “We know that the more likely a person is to have atherosclerosis, the more likely they are to experience harm from COX-2 inhibition,” he said. “So given the profile of the patients in this trial, it’s unlikely that we would have been able to detect that signal of harm from COX-2 inhibition, particularly at this dose.”
Dr. Antman also had concerns about the impact on concomitant aspirin therapy (the benefit of which can be affected by nonselective NSAIDs) and about possible differences in the reasons for dropouts that may have biased findings toward celecoxib. “I believe we need more information in order to more completely interpret this trial,” he summarized.
For now, he advised physicians to follow guidance put forth by the American Heart Association: Avoid NSAIDs in patients with known heart disease, and if one must use them, try to use the lowest-risk drug in the lowest dose needed for the shortest period of time.
In the future, “we should actually break out of the mold of assigning everybody in the trial a common phenotype and reporting the average result, but instead take a precision medicine approach, where we look at the polymorphisms in the COX enzyme, look at the polymorphisms in the ability to metabolize these drugs, and actually see if we can be more precise,” Dr. Antman maintained. “Finally, there is an urgent clinical need for the development of novel analgesics and other therapeutics to avoid the cardiovascular risk from all NSAIDs.”
Trial details
Patients were eligible for PRECISION, a Pfizer-funded trial, if they had osteoarthritis or rheumatoid arthritis and were at increased cardiovascular risk.
In all, 24,081 patients from 926 centers globally were randomly assigned to double-blind treatment with celecoxib, naproxen, or ibuprofen, all of which are now available as generics in the United States.
“Patients were randomized to the FDA-approved doses of these drugs, and they could have their dose increased if they had unrelieved pain up to the maximum allowed by regulatory authorities in the local jurisdictions where the study was done,” Dr. Nissen noted, pointing out that studies initially generating some concern about celecoxib used a supratherapeutic dose of 800 mg daily.
As COX-2 inhibitors are less likely than nonselective NSAIDs to cause ulcers, which might affect compliance and outcomes, all patients additionally received esomeprazole for gastroprotection “to try to level the playing field,” he explained.
The mean treatment duration was 20.3 months, and the mean follow-up duration was 34.1 months, according to data reported at the meeting and simultaneously published (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593). On average, the daily dose of drug received was 209 mg for celecoxib, 852 mg for naproxen, and 2,045 mg for ibuprofen.
In intention-to-treat analyses, the rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% in the celecoxib group, 2.5% in the naproxen group, and 2.7% in the ibuprofen group. The hazard ratio was 0.93 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.85 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Differences were more marked in the on-treatment population. Here, the rate of the primary outcome was 1.7% in the celecoxib group, 1.8% in the naproxen group, and 1.9% in the ibuprofen group. The HR was 0.90 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.81 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Secondary outcomes, which tested for superiority, showed that the rate of major adverse cardiovascular events was 15% higher in the ibuprofen group as compared with the celecoxib group in the intent-to-treat population. The difference translated to a near-significant reduction in risk with the latter (HR, 0.87; P = .06) that appeared greater in the on-treatment population.
However, Dr. Nissen cautioned that he could not state that celecoxib was superior. “Secondary and tertiary endpoints in a clinical trial are hypothesis generating, and they are not considered definitive evidence,” he commented. At the same time, “the FDA is going to have to deal with that because what do they do with labeling? What do they do with over-the-counter access to these various drugs?”
The rate of all-cause mortality was 25% higher with naproxen than with celecoxib (HR, 0.80; P = .052).
The rate of gastrointestinal events was 54% higher with ibuprofen (HR, 0.65; P = .002) and 41% higher with naproxen (HR, 0.71; P = .01) as compared with celecoxib. And the rate of renal events was 64% higher with ibuprofen than with celecoxib (HR, 0.61; P = .004).
In a post hoc analysis of global safety, the rate of serious cardiovascular, gastrointestinal, and renal events was 28% higher with ibuprofen (HR, 0.78; P less than .001) and 15% higher with naproxen (HR, 0.87; P = .03) than with celecoxib.
Of note, the findings for the primary endpoint were similar regardless of whether patients were taking low-dose aspirin or not. “There was no interaction with aspirin use,” Dr. Nissen stated. “This was not about the interference of ibuprofen or naproxen with aspirin use.”
Analyses of pain relief using a visual analogue scale showed no clinically meaningful differences, suggesting that the drug doses used were equally analgesic, he said. Stopping of study drug because of lack of efficacy was slightly more common in the celecoxib group.
“We didn’t study the low-dose, intermittent use of these drugs that most of the public engages in, and it’s really important that we crisply communicate that to the public because somebody who takes occasionally ibuprofen or naproxen for a headache should not look at these comparative data in a way that should necessarily influence their behavior. We just don’t know the answer,” cautioned Dr. Nissen, who disclosed that he received grant support from Pfizer during the conduct of the trial.
But the findings are relevant for individuals who take over-the-counter NSAIDs at doses exceeding the label, a phenomenon known as dose creep. “We need to reemphasize to the public that the labeled over-the-counter dose is what you should take. You shouldn’t double up or triple up on the drugs because the issue of high-dose therapy, which is what we studied, suggests that there are really potentially important gastrointestinal, renal, and cardiovascular risks,” he said.
NEW ORLEANS – The cardiovascular safety profile of the nonsteroidal anti-inflammatory drug (NSAID) celecoxib, a selective inhibitor of COX-2, is no worse than those of the nonselective NSAIDs naproxen and ibuprofen, according to a trial reported at the American Heart Association scientific sessions.
The trial, known as PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen Or Naproxen) was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that 2%-3% of patients experienced a cardiovascular event (cardiovascular death, myocardial infarction, or stroke) during a follow-up approaching 3 years, regardless of which drug they were assigned to take, with the slight differences falling within predefined margins for noninferiority of celecoxib, investigators reported in a session and related press conference.
Additionally, celecoxib yielded a lower rate of gastrointestinal events when compared with each of the other drugs and a lower rate of renal events when compared with ibuprofen.
“After the withdrawal of rofecoxib, everybody thought they knew the answer, that COX-2 inhibitors had an unfavorable cardiovascular profile,” commented first author Steven E. Nissen, MD, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “We didn’t find that. And this is the type of study that once again teaches us that if we jump to conclusions about this based on mechanistic considerations, we often make very bad decisions.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Efforts are under way to disseminate the PRECISION findings to rheumatologists and other groups who do much of the NSAID prescribing.
“Any time you have something that has findings like the findings we have, it takes some time to trickle down to the prescribers. It’s going to be our job to communicate both the value and the important limitations of the trial so that people can make informed decisions about which of these drugs to use and in whom,” Dr. Nissen said.
A cautionary view
“The investigators addressed an extremely important question, which is what is the cardiovascular safety of agents that we administer for a general medical condition over the long term,” commented invited discussant Elliott M. Antman, MD, a senior physician at Brigham and Women’s Hospital and associate dean for Clinical and Translational Research at Harvard Medical School in Boston. “We don’t see a lot of trials like that, but we do need this information.”
“This is not a comparison of drugs; this is a comparison of drug regimens because the investigators were able to increase the dose to control the subjects’ pain,” Dr. Antman elaborated. “And they were able to increase the dose of naproxen and ibuprofen comparatively more than they could for celecoxib,” which was capped at 200 mg per day at most study sites.
Furthermore, only about one-fifth of the patients studied had known heart disease. “We know that the more likely a person is to have atherosclerosis, the more likely they are to experience harm from COX-2 inhibition,” he said. “So given the profile of the patients in this trial, it’s unlikely that we would have been able to detect that signal of harm from COX-2 inhibition, particularly at this dose.”
Dr. Antman also had concerns about the impact on concomitant aspirin therapy (the benefit of which can be affected by nonselective NSAIDs) and about possible differences in the reasons for dropouts that may have biased findings toward celecoxib. “I believe we need more information in order to more completely interpret this trial,” he summarized.
For now, he advised physicians to follow guidance put forth by the American Heart Association: Avoid NSAIDs in patients with known heart disease, and if one must use them, try to use the lowest-risk drug in the lowest dose needed for the shortest period of time.
In the future, “we should actually break out of the mold of assigning everybody in the trial a common phenotype and reporting the average result, but instead take a precision medicine approach, where we look at the polymorphisms in the COX enzyme, look at the polymorphisms in the ability to metabolize these drugs, and actually see if we can be more precise,” Dr. Antman maintained. “Finally, there is an urgent clinical need for the development of novel analgesics and other therapeutics to avoid the cardiovascular risk from all NSAIDs.”
Trial details
Patients were eligible for PRECISION, a Pfizer-funded trial, if they had osteoarthritis or rheumatoid arthritis and were at increased cardiovascular risk.
In all, 24,081 patients from 926 centers globally were randomly assigned to double-blind treatment with celecoxib, naproxen, or ibuprofen, all of which are now available as generics in the United States.
“Patients were randomized to the FDA-approved doses of these drugs, and they could have their dose increased if they had unrelieved pain up to the maximum allowed by regulatory authorities in the local jurisdictions where the study was done,” Dr. Nissen noted, pointing out that studies initially generating some concern about celecoxib used a supratherapeutic dose of 800 mg daily.
As COX-2 inhibitors are less likely than nonselective NSAIDs to cause ulcers, which might affect compliance and outcomes, all patients additionally received esomeprazole for gastroprotection “to try to level the playing field,” he explained.
The mean treatment duration was 20.3 months, and the mean follow-up duration was 34.1 months, according to data reported at the meeting and simultaneously published (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593). On average, the daily dose of drug received was 209 mg for celecoxib, 852 mg for naproxen, and 2,045 mg for ibuprofen.
In intention-to-treat analyses, the rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% in the celecoxib group, 2.5% in the naproxen group, and 2.7% in the ibuprofen group. The hazard ratio was 0.93 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.85 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Differences were more marked in the on-treatment population. Here, the rate of the primary outcome was 1.7% in the celecoxib group, 1.8% in the naproxen group, and 1.9% in the ibuprofen group. The HR was 0.90 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.81 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Secondary outcomes, which tested for superiority, showed that the rate of major adverse cardiovascular events was 15% higher in the ibuprofen group as compared with the celecoxib group in the intent-to-treat population. The difference translated to a near-significant reduction in risk with the latter (HR, 0.87; P = .06) that appeared greater in the on-treatment population.
However, Dr. Nissen cautioned that he could not state that celecoxib was superior. “Secondary and tertiary endpoints in a clinical trial are hypothesis generating, and they are not considered definitive evidence,” he commented. At the same time, “the FDA is going to have to deal with that because what do they do with labeling? What do they do with over-the-counter access to these various drugs?”
The rate of all-cause mortality was 25% higher with naproxen than with celecoxib (HR, 0.80; P = .052).
The rate of gastrointestinal events was 54% higher with ibuprofen (HR, 0.65; P = .002) and 41% higher with naproxen (HR, 0.71; P = .01) as compared with celecoxib. And the rate of renal events was 64% higher with ibuprofen than with celecoxib (HR, 0.61; P = .004).
In a post hoc analysis of global safety, the rate of serious cardiovascular, gastrointestinal, and renal events was 28% higher with ibuprofen (HR, 0.78; P less than .001) and 15% higher with naproxen (HR, 0.87; P = .03) than with celecoxib.
Of note, the findings for the primary endpoint were similar regardless of whether patients were taking low-dose aspirin or not. “There was no interaction with aspirin use,” Dr. Nissen stated. “This was not about the interference of ibuprofen or naproxen with aspirin use.”
Analyses of pain relief using a visual analogue scale showed no clinically meaningful differences, suggesting that the drug doses used were equally analgesic, he said. Stopping of study drug because of lack of efficacy was slightly more common in the celecoxib group.
“We didn’t study the low-dose, intermittent use of these drugs that most of the public engages in, and it’s really important that we crisply communicate that to the public because somebody who takes occasionally ibuprofen or naproxen for a headache should not look at these comparative data in a way that should necessarily influence their behavior. We just don’t know the answer,” cautioned Dr. Nissen, who disclosed that he received grant support from Pfizer during the conduct of the trial.
But the findings are relevant for individuals who take over-the-counter NSAIDs at doses exceeding the label, a phenomenon known as dose creep. “We need to reemphasize to the public that the labeled over-the-counter dose is what you should take. You shouldn’t double up or triple up on the drugs because the issue of high-dose therapy, which is what we studied, suggests that there are really potentially important gastrointestinal, renal, and cardiovascular risks,” he said.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% with celecoxib, 2.5% with naproxen, and 2.7% with ibuprofen (P less than .001 for noninferiority).
Data source: A randomized, controlled trial among 24,081 patients who required NSAIDs for painful arthritis and were at increased cardiovascular risk (PRECISION trial).
Disclosures: Dr. Nissen disclosed that he received grant support from Pfizer during the conduct of the trial. The trial was funded by Pfizer.
VIDEO: Cardiac inflammation present in RA patients, but resolves with RA therapy
WASHINGTON – Chronic cardiac inflammation is present in rheumatoid arthritis patients and appears to resolve when they achieve a good clinical response to medical therapy.
The findings of two cardiac imaging studies offer a tantalizing clue to the link between RA and heart failure, said Isabelle Amigues, MD, who reported the findings at the annual meeting of the American College of Rheumatology.
“We know that the inflammation of RA is not just restricted to joints,” said Dr. Amigues, a rheumatology fellow at Columbia University, New York. “We see it throughout the body, so of course it makes sense that we would see it in the heart as well. And now we see that we may be able to manage this with good disease management.
The study that found improvement of myocarditis with RA therapy was very small – just 8 patients and 12 controls – but the results were surprising and encouraging, Dr. Amigues said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The initial study examined chronic myocarditis in 119 patients with active RA; most (76%) were positive for anti-cyclic citrullinated peptides. They had a mean disease duration of 7 years. The mean Disease Activity Score was 3.8; 28% had low disease activity. About a third of the patients were taking a tumor necrosis factor inhibitor.
These patients were age- and gender-matched with 13 controls who did not have RA. All underwent cardiac FDG-PET scans as a marker of inflammation, as well as 3-D echocardiography to assess left ventricular mass and volume, and both systolic and diastolic function.
The maximum standard uptake value (SUVmax) in the scans was 12% higher in study patients than in the controls. This finding was associated with a higher body mass index and moderate to severe disease activity. After adjustment for BMI and RA treatment, the mean SUVmax was 30% higher for the patients with moderate to severe disease activity than in those who had low disease activity. Patients taking non-TNF biologics had 35% less cardiac inflammation than did those taking a TNF inhibitor or those not taking a biologic.
There were no significant associations with age, gender, race, diabetes, C-reactive protein or IL-6, coronary flow reserve, or coronary calcium. Inflammation was not related to any measure of cardiac structure or function on echocardiography.
“This finding makes sense, because we know that RA causes systemic inflammation, so it’s not surprising to see inflammation at the level of the heart,” Dr. Amigues said in an interview. “We do need longitudinal studies though to determine if structural or functional changes occur later on in the disease process.”
While the initial study didn’t look at cardiac changes in the disease process, Dr. Amigues’ subsequent study did find these associated with successful RA treatment. This follow-up study comprised eight patients who underwent PET scans and 3-D echocardiography at baseline and 6 months after initiation of a step-up treatment regimen. These were compared to 12 age- and gender-matched controls without RA, who had one baseline scan.
Most patients (87%) were women; their mean age was 62 years, and mean disease duration, 5 months. Most of the patients received TNF inhibitors with methotrexate as their step-up therapy; the rest were given triple therapy.
At the baseline scan, mean SUVmax was significantly higher in the patients than in controls (7.2 vs. 3.4 units). After 6 months of treatment, the mean DAS28 score among patients had decreased more than 1 point (4.57-3.51). Their mean SUVmax had also decreased to the level seen in controls. This was a significant improvement, Dr. Amigues said.
Again, there were no structural or functional differences between the two groups at baseline or follow-up, suggesting that cardiac inflammation is not inducing structural change – at least early in the RA disease process, Dr. Amigues said.
She reported having no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
WASHINGTON – Chronic cardiac inflammation is present in rheumatoid arthritis patients and appears to resolve when they achieve a good clinical response to medical therapy.
The findings of two cardiac imaging studies offer a tantalizing clue to the link between RA and heart failure, said Isabelle Amigues, MD, who reported the findings at the annual meeting of the American College of Rheumatology.
“We know that the inflammation of RA is not just restricted to joints,” said Dr. Amigues, a rheumatology fellow at Columbia University, New York. “We see it throughout the body, so of course it makes sense that we would see it in the heart as well. And now we see that we may be able to manage this with good disease management.
The study that found improvement of myocarditis with RA therapy was very small – just 8 patients and 12 controls – but the results were surprising and encouraging, Dr. Amigues said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The initial study examined chronic myocarditis in 119 patients with active RA; most (76%) were positive for anti-cyclic citrullinated peptides. They had a mean disease duration of 7 years. The mean Disease Activity Score was 3.8; 28% had low disease activity. About a third of the patients were taking a tumor necrosis factor inhibitor.
These patients were age- and gender-matched with 13 controls who did not have RA. All underwent cardiac FDG-PET scans as a marker of inflammation, as well as 3-D echocardiography to assess left ventricular mass and volume, and both systolic and diastolic function.
The maximum standard uptake value (SUVmax) in the scans was 12% higher in study patients than in the controls. This finding was associated with a higher body mass index and moderate to severe disease activity. After adjustment for BMI and RA treatment, the mean SUVmax was 30% higher for the patients with moderate to severe disease activity than in those who had low disease activity. Patients taking non-TNF biologics had 35% less cardiac inflammation than did those taking a TNF inhibitor or those not taking a biologic.
There were no significant associations with age, gender, race, diabetes, C-reactive protein or IL-6, coronary flow reserve, or coronary calcium. Inflammation was not related to any measure of cardiac structure or function on echocardiography.
“This finding makes sense, because we know that RA causes systemic inflammation, so it’s not surprising to see inflammation at the level of the heart,” Dr. Amigues said in an interview. “We do need longitudinal studies though to determine if structural or functional changes occur later on in the disease process.”
While the initial study didn’t look at cardiac changes in the disease process, Dr. Amigues’ subsequent study did find these associated with successful RA treatment. This follow-up study comprised eight patients who underwent PET scans and 3-D echocardiography at baseline and 6 months after initiation of a step-up treatment regimen. These were compared to 12 age- and gender-matched controls without RA, who had one baseline scan.
Most patients (87%) were women; their mean age was 62 years, and mean disease duration, 5 months. Most of the patients received TNF inhibitors with methotrexate as their step-up therapy; the rest were given triple therapy.
At the baseline scan, mean SUVmax was significantly higher in the patients than in controls (7.2 vs. 3.4 units). After 6 months of treatment, the mean DAS28 score among patients had decreased more than 1 point (4.57-3.51). Their mean SUVmax had also decreased to the level seen in controls. This was a significant improvement, Dr. Amigues said.
Again, there were no structural or functional differences between the two groups at baseline or follow-up, suggesting that cardiac inflammation is not inducing structural change – at least early in the RA disease process, Dr. Amigues said.
She reported having no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
WASHINGTON – Chronic cardiac inflammation is present in rheumatoid arthritis patients and appears to resolve when they achieve a good clinical response to medical therapy.
The findings of two cardiac imaging studies offer a tantalizing clue to the link between RA and heart failure, said Isabelle Amigues, MD, who reported the findings at the annual meeting of the American College of Rheumatology.
“We know that the inflammation of RA is not just restricted to joints,” said Dr. Amigues, a rheumatology fellow at Columbia University, New York. “We see it throughout the body, so of course it makes sense that we would see it in the heart as well. And now we see that we may be able to manage this with good disease management.
The study that found improvement of myocarditis with RA therapy was very small – just 8 patients and 12 controls – but the results were surprising and encouraging, Dr. Amigues said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The initial study examined chronic myocarditis in 119 patients with active RA; most (76%) were positive for anti-cyclic citrullinated peptides. They had a mean disease duration of 7 years. The mean Disease Activity Score was 3.8; 28% had low disease activity. About a third of the patients were taking a tumor necrosis factor inhibitor.
These patients were age- and gender-matched with 13 controls who did not have RA. All underwent cardiac FDG-PET scans as a marker of inflammation, as well as 3-D echocardiography to assess left ventricular mass and volume, and both systolic and diastolic function.
The maximum standard uptake value (SUVmax) in the scans was 12% higher in study patients than in the controls. This finding was associated with a higher body mass index and moderate to severe disease activity. After adjustment for BMI and RA treatment, the mean SUVmax was 30% higher for the patients with moderate to severe disease activity than in those who had low disease activity. Patients taking non-TNF biologics had 35% less cardiac inflammation than did those taking a TNF inhibitor or those not taking a biologic.
There were no significant associations with age, gender, race, diabetes, C-reactive protein or IL-6, coronary flow reserve, or coronary calcium. Inflammation was not related to any measure of cardiac structure or function on echocardiography.
“This finding makes sense, because we know that RA causes systemic inflammation, so it’s not surprising to see inflammation at the level of the heart,” Dr. Amigues said in an interview. “We do need longitudinal studies though to determine if structural or functional changes occur later on in the disease process.”
While the initial study didn’t look at cardiac changes in the disease process, Dr. Amigues’ subsequent study did find these associated with successful RA treatment. This follow-up study comprised eight patients who underwent PET scans and 3-D echocardiography at baseline and 6 months after initiation of a step-up treatment regimen. These were compared to 12 age- and gender-matched controls without RA, who had one baseline scan.
Most patients (87%) were women; their mean age was 62 years, and mean disease duration, 5 months. Most of the patients received TNF inhibitors with methotrexate as their step-up therapy; the rest were given triple therapy.
At the baseline scan, mean SUVmax was significantly higher in the patients than in controls (7.2 vs. 3.4 units). After 6 months of treatment, the mean DAS28 score among patients had decreased more than 1 point (4.57-3.51). Their mean SUVmax had also decreased to the level seen in controls. This was a significant improvement, Dr. Amigues said.
Again, there were no structural or functional differences between the two groups at baseline or follow-up, suggesting that cardiac inflammation is not inducing structural change – at least early in the RA disease process, Dr. Amigues said.
She reported having no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE ACR ANNUAL MEETING
Key clinical point:
Major finding: PET imaging showed 12% more inflammatory activity in the hearts of patients than in those of controls; this decreased significantly as disease activity remitted with treatment.
Data source: The myocarditis study comprised 119 patients; the therapeutic response study comprised 8 patients and 12 controls.
Disclosures: Dr. Amigues reported having no relevant financial disclosures.
Robotic surgery instruments ‘virtually impossible’ to clean completely
Instruments used for robotic surgery are “virtually impossible” to clean completely, according to a report published in Infection Control & Hospital Epidemiology.
“A new standard for the cleaning of complex surgical instruments needs to be established, especially for those used in robotic surgery,” wrote Yuhei Saito of the surgical center at the University of Tokyo Hospital and associates.
They assessed the residual contamination of both robotic and regular surgical instruments at their medical center because “hospital staff in central sterile supply departments are troubled by the reprocessing of robotic instruments because they cannot be disassembled for cleaning like other endoscopic instruments. Their complex structure impairs brushing the inner surface of narrow lumens, resulting in failure to [completely] remove contaminants,” the researchers wrote.
In the first phase of the study, the researchers examined 41 instruments immediately after they were used in robotic surgery (7 radical prostatectomies and 2 anterior resections of the rectum) and 27 regular instruments immediately after they were used for open surgery (gastrectomy and colectomy). The robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on the regular instruments, the investigators reported (Infect Control Hosp Epidemiol. 2016 Oct 31. doi: 10.1017/ice.2016.249).
In the second phase of the study, the researchers examined another 24 robotic instruments and 40 regular instruments after they were used in surgery and then cleaned according to the manufacturers’ instructions three successive times. For the robotic instruments, this involved manually brushing the outer surface while moving the instrument “wrists” through their full range of motion, followed by 15 minutes of ultrasonication with enzymatic detergent, flushing the lumen with a water gun through flush ports, and rinsing the entire instrument. For regular instruments, cleaning involved washer-disinfectors and included 5 minutes of ultrasonication, 10 minutes of spraying with an alkaline detergent, and 10 minutes of disinfection via heating.
The level of contamination declined with each successive cleaning but still remained comparatively high for the robotic instruments. The amount of protein contaminants released in the three cleanings was 650, 550, and 530 mcg per robotic instrument, compared with 16, 17, and 17 mcg per ordinary instrument.
The efficacy of cleaning was 97.6% for robotic instruments and 99.1% for regular instruments, the researchers reported.
This study was not designed to assess whether residual contamination is associated with adverse events such as infection in subsequent patients, and there are few data available on this topic.
“We have to recognize that there might be a considerable volume of insufficient cleaning or occult surgical site infections,” the investigators wrote.
New instrument washers equipped with a specific cleaning function for narrow lumens are becoming available, they noted, and “further study should be conducted using these washers with improved cleaning efficacy.”
The study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
Instruments used for robotic surgery are “virtually impossible” to clean completely, according to a report published in Infection Control & Hospital Epidemiology.
“A new standard for the cleaning of complex surgical instruments needs to be established, especially for those used in robotic surgery,” wrote Yuhei Saito of the surgical center at the University of Tokyo Hospital and associates.
They assessed the residual contamination of both robotic and regular surgical instruments at their medical center because “hospital staff in central sterile supply departments are troubled by the reprocessing of robotic instruments because they cannot be disassembled for cleaning like other endoscopic instruments. Their complex structure impairs brushing the inner surface of narrow lumens, resulting in failure to [completely] remove contaminants,” the researchers wrote.
In the first phase of the study, the researchers examined 41 instruments immediately after they were used in robotic surgery (7 radical prostatectomies and 2 anterior resections of the rectum) and 27 regular instruments immediately after they were used for open surgery (gastrectomy and colectomy). The robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on the regular instruments, the investigators reported (Infect Control Hosp Epidemiol. 2016 Oct 31. doi: 10.1017/ice.2016.249).
In the second phase of the study, the researchers examined another 24 robotic instruments and 40 regular instruments after they were used in surgery and then cleaned according to the manufacturers’ instructions three successive times. For the robotic instruments, this involved manually brushing the outer surface while moving the instrument “wrists” through their full range of motion, followed by 15 minutes of ultrasonication with enzymatic detergent, flushing the lumen with a water gun through flush ports, and rinsing the entire instrument. For regular instruments, cleaning involved washer-disinfectors and included 5 minutes of ultrasonication, 10 minutes of spraying with an alkaline detergent, and 10 minutes of disinfection via heating.
The level of contamination declined with each successive cleaning but still remained comparatively high for the robotic instruments. The amount of protein contaminants released in the three cleanings was 650, 550, and 530 mcg per robotic instrument, compared with 16, 17, and 17 mcg per ordinary instrument.
The efficacy of cleaning was 97.6% for robotic instruments and 99.1% for regular instruments, the researchers reported.
This study was not designed to assess whether residual contamination is associated with adverse events such as infection in subsequent patients, and there are few data available on this topic.
“We have to recognize that there might be a considerable volume of insufficient cleaning or occult surgical site infections,” the investigators wrote.
New instrument washers equipped with a specific cleaning function for narrow lumens are becoming available, they noted, and “further study should be conducted using these washers with improved cleaning efficacy.”
The study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
Instruments used for robotic surgery are “virtually impossible” to clean completely, according to a report published in Infection Control & Hospital Epidemiology.
“A new standard for the cleaning of complex surgical instruments needs to be established, especially for those used in robotic surgery,” wrote Yuhei Saito of the surgical center at the University of Tokyo Hospital and associates.
They assessed the residual contamination of both robotic and regular surgical instruments at their medical center because “hospital staff in central sterile supply departments are troubled by the reprocessing of robotic instruments because they cannot be disassembled for cleaning like other endoscopic instruments. Their complex structure impairs brushing the inner surface of narrow lumens, resulting in failure to [completely] remove contaminants,” the researchers wrote.
In the first phase of the study, the researchers examined 41 instruments immediately after they were used in robotic surgery (7 radical prostatectomies and 2 anterior resections of the rectum) and 27 regular instruments immediately after they were used for open surgery (gastrectomy and colectomy). The robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on the regular instruments, the investigators reported (Infect Control Hosp Epidemiol. 2016 Oct 31. doi: 10.1017/ice.2016.249).
In the second phase of the study, the researchers examined another 24 robotic instruments and 40 regular instruments after they were used in surgery and then cleaned according to the manufacturers’ instructions three successive times. For the robotic instruments, this involved manually brushing the outer surface while moving the instrument “wrists” through their full range of motion, followed by 15 minutes of ultrasonication with enzymatic detergent, flushing the lumen with a water gun through flush ports, and rinsing the entire instrument. For regular instruments, cleaning involved washer-disinfectors and included 5 minutes of ultrasonication, 10 minutes of spraying with an alkaline detergent, and 10 minutes of disinfection via heating.
The level of contamination declined with each successive cleaning but still remained comparatively high for the robotic instruments. The amount of protein contaminants released in the three cleanings was 650, 550, and 530 mcg per robotic instrument, compared with 16, 17, and 17 mcg per ordinary instrument.
The efficacy of cleaning was 97.6% for robotic instruments and 99.1% for regular instruments, the researchers reported.
This study was not designed to assess whether residual contamination is associated with adverse events such as infection in subsequent patients, and there are few data available on this topic.
“We have to recognize that there might be a considerable volume of insufficient cleaning or occult surgical site infections,” the investigators wrote.
New instrument washers equipped with a specific cleaning function for narrow lumens are becoming available, they noted, and “further study should be conducted using these washers with improved cleaning efficacy.”
The study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
FROM INFECTION CONTROL AND HOSPITAL EPIDEMIOLOGY
Key clinical point:
Major finding: Immediately after surgery, robotic instruments were contaminated with 72.3 × 103 mcg of protein each, compared with 5.5 × 103 mcg of protein on regular instruments.
Data source: A single-center analysis of protein contamination before and after three successive cleanings on 65 instruments used for robotic surgery and 67 regular instruments used for open surgery.
Disclosures: This study was supported by the Japan Society for the Promotion of Science. The investigators reported having no relevant financial disclosures.
Long-term opioid use uncommon among trauma patients
WASHINGTON – Patients with traumatic injuries don’t appear to be at undue risk of sustained opioid use, a large database review has demonstrated.
More than half of the 13,000 patients in the study were discharged on opioids, but they were able to discontinue them fairly rapidly, Muhammad Chaudhary, MD, said at the annual clinical congress of the American College of Surgeons. Within 3 months, less than one-third were still using the drugs, and 1 year later, only 1% were still taking an opioid pain medication.
Dr. Chaudhary examined opioid use among 13,624 patients included in the Tricare military insurance database. The patients were treated for traumatic injuries they received during 2007-2013. Most of the patients were men (82%), and the largest age group was 18- to 24-year-olds (39%). Military rank was used as a proxy for socioeconomic status in this study: 15% of the cohort had an officer rank, while the rest were junior or senior enlisted personnel.
The group was very healthy, with a median Charlson Comorbidity Index score of 0. They were somewhat seriously injured, however. The median Injury Severity Score was 13, and the range was 9-17. Anxiety and depression were uncommon (9% and 7%, respectively).
More than half the patients (54%) were discharged on an opioid medication. That percentage dropped very rapidly. By 90 days after discharge, just 9% of patients were still taking the drugs. By 1 year, only 1% were using opioids.
Dr. Chaudhary conducted a multivariate analysis that controlled for a number of factors, including age, gender, marital status, rank, mental health status, injury severity, comorbidities, and treatment environment. Two factors – black race and younger age (18-24 years) – significantly increased the likelihood of early opioid discontinuation (8% and 11%, respectively). There were no significant interactions with anxiety or depression.
Junior enlisted personnel – the proxy group for lower socioeconomic status – and those with a prolonged length of stay were significantly less likely to get off the medications, Dr. Chaudhary said.
“While we strongly believe that these factors should not be used to determine who can get opioids, it might make sense to enhance perioperative surveillance and engage pain management services early on in patients with risk factors, to reduce the risk of sustained opioid use,” he concluded.
Dr. Chaudhary had no financial disclosures.
[email protected]
On Twitter @alz_gal
WASHINGTON – Patients with traumatic injuries don’t appear to be at undue risk of sustained opioid use, a large database review has demonstrated.
More than half of the 13,000 patients in the study were discharged on opioids, but they were able to discontinue them fairly rapidly, Muhammad Chaudhary, MD, said at the annual clinical congress of the American College of Surgeons. Within 3 months, less than one-third were still using the drugs, and 1 year later, only 1% were still taking an opioid pain medication.
Dr. Chaudhary examined opioid use among 13,624 patients included in the Tricare military insurance database. The patients were treated for traumatic injuries they received during 2007-2013. Most of the patients were men (82%), and the largest age group was 18- to 24-year-olds (39%). Military rank was used as a proxy for socioeconomic status in this study: 15% of the cohort had an officer rank, while the rest were junior or senior enlisted personnel.
The group was very healthy, with a median Charlson Comorbidity Index score of 0. They were somewhat seriously injured, however. The median Injury Severity Score was 13, and the range was 9-17. Anxiety and depression were uncommon (9% and 7%, respectively).
More than half the patients (54%) were discharged on an opioid medication. That percentage dropped very rapidly. By 90 days after discharge, just 9% of patients were still taking the drugs. By 1 year, only 1% were using opioids.
Dr. Chaudhary conducted a multivariate analysis that controlled for a number of factors, including age, gender, marital status, rank, mental health status, injury severity, comorbidities, and treatment environment. Two factors – black race and younger age (18-24 years) – significantly increased the likelihood of early opioid discontinuation (8% and 11%, respectively). There were no significant interactions with anxiety or depression.
Junior enlisted personnel – the proxy group for lower socioeconomic status – and those with a prolonged length of stay were significantly less likely to get off the medications, Dr. Chaudhary said.
“While we strongly believe that these factors should not be used to determine who can get opioids, it might make sense to enhance perioperative surveillance and engage pain management services early on in patients with risk factors, to reduce the risk of sustained opioid use,” he concluded.
Dr. Chaudhary had no financial disclosures.
[email protected]
On Twitter @alz_gal
WASHINGTON – Patients with traumatic injuries don’t appear to be at undue risk of sustained opioid use, a large database review has demonstrated.
More than half of the 13,000 patients in the study were discharged on opioids, but they were able to discontinue them fairly rapidly, Muhammad Chaudhary, MD, said at the annual clinical congress of the American College of Surgeons. Within 3 months, less than one-third were still using the drugs, and 1 year later, only 1% were still taking an opioid pain medication.
Dr. Chaudhary examined opioid use among 13,624 patients included in the Tricare military insurance database. The patients were treated for traumatic injuries they received during 2007-2013. Most of the patients were men (82%), and the largest age group was 18- to 24-year-olds (39%). Military rank was used as a proxy for socioeconomic status in this study: 15% of the cohort had an officer rank, while the rest were junior or senior enlisted personnel.
The group was very healthy, with a median Charlson Comorbidity Index score of 0. They were somewhat seriously injured, however. The median Injury Severity Score was 13, and the range was 9-17. Anxiety and depression were uncommon (9% and 7%, respectively).
More than half the patients (54%) were discharged on an opioid medication. That percentage dropped very rapidly. By 90 days after discharge, just 9% of patients were still taking the drugs. By 1 year, only 1% were using opioids.
Dr. Chaudhary conducted a multivariate analysis that controlled for a number of factors, including age, gender, marital status, rank, mental health status, injury severity, comorbidities, and treatment environment. Two factors – black race and younger age (18-24 years) – significantly increased the likelihood of early opioid discontinuation (8% and 11%, respectively). There were no significant interactions with anxiety or depression.
Junior enlisted personnel – the proxy group for lower socioeconomic status – and those with a prolonged length of stay were significantly less likely to get off the medications, Dr. Chaudhary said.
“While we strongly believe that these factors should not be used to determine who can get opioids, it might make sense to enhance perioperative surveillance and engage pain management services early on in patients with risk factors, to reduce the risk of sustained opioid use,” he concluded.
Dr. Chaudhary had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: A year after discharge, only 1% of the patients were still using a prescription opioid pain medication.
Data source: A database review including 13,642 patients.
Disclosures: Dr. Chaudhary had no financial disclosures.