User login
News and Views that Matter to Physicians
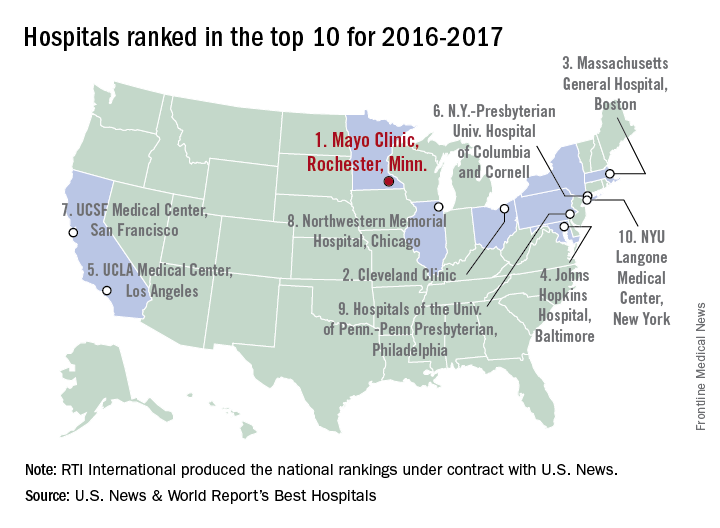
Mayo Clinic tops hospital rankings for 2016-2017
The Mayo Clinic in Rochester, Minn., was named the top hospital in the United States, according to the U.S. News & World Report Best Hospitals ranking for 2016-2017.
After finishing second to Massachusetts General Hospital in Boston last year, the Mayo Clinic regained the top spot it earned in 2014-2015. This year, the Cleveland Clinic finished second in the U.S. News Honor Roll, with Massachusetts General third, Johns Hopkins Hospital in Baltimore fourth, and the University of California, Los Angeles, Medical Center in fifth.
For 2016-2017, there were 20 hospitals in the Honor Roll, which is reserved for those institutions that finish at or near the top among the 16 specialties included in the U.S. News rankings. This year, 153 hospitals did well enough to be nationally ranked in one or more specialties, which is up from the 144 that were ranked nationally in at least one specialty last year.
The 16 specialties used in the analysis are cancer, cardiology and heart surgery, diabetes and endocrinology, otolaryngology, gastroenterology and gastrointestinal surgery, geriatrics, gynecology, nephrology, neurology and neurosurgery, ophthalmology, orthopedics, psychiatry, pulmonology, rehabilitation, rheumatology, and urology.
This year’s ranking process initially included 4,667 nonfederal community hospitals. The research organization RTI International conducted the physician survey and produced the Best Hospitals methodology and national rankings under contract with U.S. News.
The Mayo Clinic in Rochester, Minn., was named the top hospital in the United States, according to the U.S. News & World Report Best Hospitals ranking for 2016-2017.
After finishing second to Massachusetts General Hospital in Boston last year, the Mayo Clinic regained the top spot it earned in 2014-2015. This year, the Cleveland Clinic finished second in the U.S. News Honor Roll, with Massachusetts General third, Johns Hopkins Hospital in Baltimore fourth, and the University of California, Los Angeles, Medical Center in fifth.
For 2016-2017, there were 20 hospitals in the Honor Roll, which is reserved for those institutions that finish at or near the top among the 16 specialties included in the U.S. News rankings. This year, 153 hospitals did well enough to be nationally ranked in one or more specialties, which is up from the 144 that were ranked nationally in at least one specialty last year.
The 16 specialties used in the analysis are cancer, cardiology and heart surgery, diabetes and endocrinology, otolaryngology, gastroenterology and gastrointestinal surgery, geriatrics, gynecology, nephrology, neurology and neurosurgery, ophthalmology, orthopedics, psychiatry, pulmonology, rehabilitation, rheumatology, and urology.
This year’s ranking process initially included 4,667 nonfederal community hospitals. The research organization RTI International conducted the physician survey and produced the Best Hospitals methodology and national rankings under contract with U.S. News.
The Mayo Clinic in Rochester, Minn., was named the top hospital in the United States, according to the U.S. News & World Report Best Hospitals ranking for 2016-2017.
After finishing second to Massachusetts General Hospital in Boston last year, the Mayo Clinic regained the top spot it earned in 2014-2015. This year, the Cleveland Clinic finished second in the U.S. News Honor Roll, with Massachusetts General third, Johns Hopkins Hospital in Baltimore fourth, and the University of California, Los Angeles, Medical Center in fifth.
For 2016-2017, there were 20 hospitals in the Honor Roll, which is reserved for those institutions that finish at or near the top among the 16 specialties included in the U.S. News rankings. This year, 153 hospitals did well enough to be nationally ranked in one or more specialties, which is up from the 144 that were ranked nationally in at least one specialty last year.
The 16 specialties used in the analysis are cancer, cardiology and heart surgery, diabetes and endocrinology, otolaryngology, gastroenterology and gastrointestinal surgery, geriatrics, gynecology, nephrology, neurology and neurosurgery, ophthalmology, orthopedics, psychiatry, pulmonology, rehabilitation, rheumatology, and urology.
This year’s ranking process initially included 4,667 nonfederal community hospitals. The research organization RTI International conducted the physician survey and produced the Best Hospitals methodology and national rankings under contract with U.S. News.
Preop G-tubes save money in head and neck cancer resections
SEATTLE – It’s better to place gastrostomy tubes before head and neck cancer surgery rather than after, according to a review of 184 patients.
The 73 patients in the study who got preoperative gastrostomy tubes (G-tubes) were sicker than the 111 who had G-tubes placed after surgery, with significantly higher American Society of Anesthesiologists scores, lower body mass indexes, and greater likelihoods of having both prior radiation and more extensive resections requiring flap reconstructions. They were, overall, a higher-risk population with a greater potential for bad outcomes, which is why tubes were placed preemptively.
Even so, at 6 months, the total average cost for the preop G-tube group was $39,751 versus $48,999 for the postoperative group, a savings of $9,248 per patient. The difference was driven by inpatient savings; the preop group left the hospital an average of 3.2 days sooner than their postop G-tube peers (9.4 days versus 12.6 days; P less than .001). Readmissions and other postdischarge costs were similar between the two groups, as were wound and nonwound complications.
“This data suggests that preoperative placement of G-tubes is associated with lower total health care costs. It appears there’s a potential for health care cost savings if candidates for G-tubes can be identified” before surgery and the tubes placed preoperatively, said investigator Joshua Waltonen, MD, of Wake Forest University, Winston-Salem, N.C.
That’s exactly what Wake Forest is doing now. Physicians there use a scoring system to determine how likely patients are to need G-tubes after surgery. If the risk is high, patients are counseled that putting one in beforehand is a good idea, he said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
The team previously found that risk factors include, among others, supracricoid laryngectomy, prior radiation, flap reconstruction, tracheostomy placement, and preop dysphagia and weight loss (JAMA Otolaryngol Head Neck Surg. 2014 Dec;140[12]:1198-206).
Two factors probably account for the shorter lengths of stay, Dr. Waltonen said. First, patients with preop feeding tubes go into surgery with a nutritional boost, which helps with recovery. Also, with a preop tube, patients don’t have to wait for general surgery to get around to placing one postoperatively.
Both groups were about 60 years old on average. The mean body mass index of the preop group was 23 kg/m2 and 26 kg/m2 in the postop group (P = .009). Almost two-thirds of preop patients had prior radiation versus a quarter of postop patients (P less than .001). Tumor and nodal stages were similar.
There was no outside funding for the work, and Dr. Waltonen had no disclosures.
SEATTLE – It’s better to place gastrostomy tubes before head and neck cancer surgery rather than after, according to a review of 184 patients.
The 73 patients in the study who got preoperative gastrostomy tubes (G-tubes) were sicker than the 111 who had G-tubes placed after surgery, with significantly higher American Society of Anesthesiologists scores, lower body mass indexes, and greater likelihoods of having both prior radiation and more extensive resections requiring flap reconstructions. They were, overall, a higher-risk population with a greater potential for bad outcomes, which is why tubes were placed preemptively.
Even so, at 6 months, the total average cost for the preop G-tube group was $39,751 versus $48,999 for the postoperative group, a savings of $9,248 per patient. The difference was driven by inpatient savings; the preop group left the hospital an average of 3.2 days sooner than their postop G-tube peers (9.4 days versus 12.6 days; P less than .001). Readmissions and other postdischarge costs were similar between the two groups, as were wound and nonwound complications.
“This data suggests that preoperative placement of G-tubes is associated with lower total health care costs. It appears there’s a potential for health care cost savings if candidates for G-tubes can be identified” before surgery and the tubes placed preoperatively, said investigator Joshua Waltonen, MD, of Wake Forest University, Winston-Salem, N.C.
That’s exactly what Wake Forest is doing now. Physicians there use a scoring system to determine how likely patients are to need G-tubes after surgery. If the risk is high, patients are counseled that putting one in beforehand is a good idea, he said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
The team previously found that risk factors include, among others, supracricoid laryngectomy, prior radiation, flap reconstruction, tracheostomy placement, and preop dysphagia and weight loss (JAMA Otolaryngol Head Neck Surg. 2014 Dec;140[12]:1198-206).
Two factors probably account for the shorter lengths of stay, Dr. Waltonen said. First, patients with preop feeding tubes go into surgery with a nutritional boost, which helps with recovery. Also, with a preop tube, patients don’t have to wait for general surgery to get around to placing one postoperatively.
Both groups were about 60 years old on average. The mean body mass index of the preop group was 23 kg/m2 and 26 kg/m2 in the postop group (P = .009). Almost two-thirds of preop patients had prior radiation versus a quarter of postop patients (P less than .001). Tumor and nodal stages were similar.
There was no outside funding for the work, and Dr. Waltonen had no disclosures.
SEATTLE – It’s better to place gastrostomy tubes before head and neck cancer surgery rather than after, according to a review of 184 patients.
The 73 patients in the study who got preoperative gastrostomy tubes (G-tubes) were sicker than the 111 who had G-tubes placed after surgery, with significantly higher American Society of Anesthesiologists scores, lower body mass indexes, and greater likelihoods of having both prior radiation and more extensive resections requiring flap reconstructions. They were, overall, a higher-risk population with a greater potential for bad outcomes, which is why tubes were placed preemptively.
Even so, at 6 months, the total average cost for the preop G-tube group was $39,751 versus $48,999 for the postoperative group, a savings of $9,248 per patient. The difference was driven by inpatient savings; the preop group left the hospital an average of 3.2 days sooner than their postop G-tube peers (9.4 days versus 12.6 days; P less than .001). Readmissions and other postdischarge costs were similar between the two groups, as were wound and nonwound complications.
“This data suggests that preoperative placement of G-tubes is associated with lower total health care costs. It appears there’s a potential for health care cost savings if candidates for G-tubes can be identified” before surgery and the tubes placed preoperatively, said investigator Joshua Waltonen, MD, of Wake Forest University, Winston-Salem, N.C.
That’s exactly what Wake Forest is doing now. Physicians there use a scoring system to determine how likely patients are to need G-tubes after surgery. If the risk is high, patients are counseled that putting one in beforehand is a good idea, he said at the International Conference on Head and Neck Cancer, held by the American Head and Neck Society.
The team previously found that risk factors include, among others, supracricoid laryngectomy, prior radiation, flap reconstruction, tracheostomy placement, and preop dysphagia and weight loss (JAMA Otolaryngol Head Neck Surg. 2014 Dec;140[12]:1198-206).
Two factors probably account for the shorter lengths of stay, Dr. Waltonen said. First, patients with preop feeding tubes go into surgery with a nutritional boost, which helps with recovery. Also, with a preop tube, patients don’t have to wait for general surgery to get around to placing one postoperatively.
Both groups were about 60 years old on average. The mean body mass index of the preop group was 23 kg/m2 and 26 kg/m2 in the postop group (P = .009). Almost two-thirds of preop patients had prior radiation versus a quarter of postop patients (P less than .001). Tumor and nodal stages were similar.
There was no outside funding for the work, and Dr. Waltonen had no disclosures.
AT AHNS 2016
Key clinical point: It’s better to place gastrostomy tubes before head and neck cancer surgery rather than after.
Major finding: At 6 months, the total average cost for the preop G-tube group was $39,751 versus $48,999 for the postop group, a savings of $9,248 per patient.
Data source: Review of 184 patients.
Disclosures: There was no outside funding for the work, and the presenter had no disclosures.
Medicaid expansion leads to better access to care
Low-income adults living in two states that expanded Medicaid enrollment are showing significant increases in outpatient utilization and preventive care, improved health care quality, and reductions in emergency department use, compared with those living in a state that did not expand Medicaid, according to a new study.
The study also found similar improvements in care whether a state expanded traditional Medicaid or increased coverage through a private insurance option.
Benjamin D. Sommers, MD, PhD, of Harvard University, Boston, and his colleagues examined outcomes for nearly 9,000 low-income Medicaid enrollees in Kentucky (where officials expanded traditional Medicaid), Arkansas (where the state used funds to purchase private insurance to expand coverage), and Texas (which did not expand Medicaid) in November and December of 2013, 2014, and 2015. They looked specifically at changes in use of healthcare services, preventive care, and self-reported health (JAMA Intern Med. 2016 Aug 8. doi: 10.1001/jamainternmed.2016.4419).
“By the end of 2015, we found marked increases in coverage and reduced cost-related barriers to care in the expansion states, with associated increases in preventive care, outpatient visits, annual checkups, and chronic disease care, as well as decreased reliance on the [emergency department],” the researchers wrote.
They found that by 2015 there was a 6 percentage point drop in the likelihood of ED visits (P = 0.04), an increase of 0.69 office visits per person in the outpatient setting (P = 0.04), and an increase likelihood of getting a checkup (16.1 percentage points, P less than .001) in Medicaid expansion states. In Medicaid expansion states the share of adults obtaining regular care for chronic conditions increased by 12 percentage points after expansion (P = .008), compared with Texas. Additionally, adults reporting fair or poor quality of care dropped by 7.1 percentage points (P = .03).
One significant difference between the expansion states was changes in glucose monitoring rates for patients with diabetes were lower in Arkansas than Kentucky (–11.6 percentage points, P = .04).
“Of note, we found improvements in receipt of checkups, care for chronic conditions, and quality of care even in areas with primary care shortages, suggesting that while clinician capacity is undoubtedly an important consideration, insurance expansion can have a demonstrable positive impact even in areas with relative shortages, perhaps partially due to increased use of safety net providers,” the researchers added.
The study was supported by a research grant from the Commonwealth Fund and a grant from the Agency for Healthcare Research and Quality. The researchers reported having no financial disclosures.
Whether the premium assistance model proves to be durable and effective remains an open question. On the upside, the findings of Sommers et al suggest that the Arkansas initiative is living up to its promises. Moreover, the waiver seems to have increased the number of insurers participating in the marketplaces and contributed to lower premiums.
But other evidence concerning premium assistance waivers suggests the need for caution in assessing their effectiveness. The Government Accountability Office has questioned whether these waivers are budget neutral – a federal requirement. In this vein, the Congressional Budget Office has estimated that it will cost 50% more per enrollee to cover the expansion population on the exchanges than in the conventional Medicaid program. Nor are premium assistance waivers necessarily sustainable. In Pennsylvania, for instance, a newly elected Democratic governor worked to phase out that state’s existing alternative waiver, which had been negotiated by a prior Republican administration, in favor of a traditional expansion of the Medicaid entitlement.
Frank J. Thompson, PhD, and Joel C. Cantor, ScD, are both at Rutgers University in New Brunswick, N.J. They reported having no financial disclosures. Their comments were excerpted from a commentary in JAMA Internal Medicine (2016 Aug 8. doi: 10.1001/jamainternmed.2016.4422).
Whether the premium assistance model proves to be durable and effective remains an open question. On the upside, the findings of Sommers et al suggest that the Arkansas initiative is living up to its promises. Moreover, the waiver seems to have increased the number of insurers participating in the marketplaces and contributed to lower premiums.
But other evidence concerning premium assistance waivers suggests the need for caution in assessing their effectiveness. The Government Accountability Office has questioned whether these waivers are budget neutral – a federal requirement. In this vein, the Congressional Budget Office has estimated that it will cost 50% more per enrollee to cover the expansion population on the exchanges than in the conventional Medicaid program. Nor are premium assistance waivers necessarily sustainable. In Pennsylvania, for instance, a newly elected Democratic governor worked to phase out that state’s existing alternative waiver, which had been negotiated by a prior Republican administration, in favor of a traditional expansion of the Medicaid entitlement.
Frank J. Thompson, PhD, and Joel C. Cantor, ScD, are both at Rutgers University in New Brunswick, N.J. They reported having no financial disclosures. Their comments were excerpted from a commentary in JAMA Internal Medicine (2016 Aug 8. doi: 10.1001/jamainternmed.2016.4422).
Whether the premium assistance model proves to be durable and effective remains an open question. On the upside, the findings of Sommers et al suggest that the Arkansas initiative is living up to its promises. Moreover, the waiver seems to have increased the number of insurers participating in the marketplaces and contributed to lower premiums.
But other evidence concerning premium assistance waivers suggests the need for caution in assessing their effectiveness. The Government Accountability Office has questioned whether these waivers are budget neutral – a federal requirement. In this vein, the Congressional Budget Office has estimated that it will cost 50% more per enrollee to cover the expansion population on the exchanges than in the conventional Medicaid program. Nor are premium assistance waivers necessarily sustainable. In Pennsylvania, for instance, a newly elected Democratic governor worked to phase out that state’s existing alternative waiver, which had been negotiated by a prior Republican administration, in favor of a traditional expansion of the Medicaid entitlement.
Frank J. Thompson, PhD, and Joel C. Cantor, ScD, are both at Rutgers University in New Brunswick, N.J. They reported having no financial disclosures. Their comments were excerpted from a commentary in JAMA Internal Medicine (2016 Aug 8. doi: 10.1001/jamainternmed.2016.4422).
Low-income adults living in two states that expanded Medicaid enrollment are showing significant increases in outpatient utilization and preventive care, improved health care quality, and reductions in emergency department use, compared with those living in a state that did not expand Medicaid, according to a new study.
The study also found similar improvements in care whether a state expanded traditional Medicaid or increased coverage through a private insurance option.
Benjamin D. Sommers, MD, PhD, of Harvard University, Boston, and his colleagues examined outcomes for nearly 9,000 low-income Medicaid enrollees in Kentucky (where officials expanded traditional Medicaid), Arkansas (where the state used funds to purchase private insurance to expand coverage), and Texas (which did not expand Medicaid) in November and December of 2013, 2014, and 2015. They looked specifically at changes in use of healthcare services, preventive care, and self-reported health (JAMA Intern Med. 2016 Aug 8. doi: 10.1001/jamainternmed.2016.4419).
“By the end of 2015, we found marked increases in coverage and reduced cost-related barriers to care in the expansion states, with associated increases in preventive care, outpatient visits, annual checkups, and chronic disease care, as well as decreased reliance on the [emergency department],” the researchers wrote.
They found that by 2015 there was a 6 percentage point drop in the likelihood of ED visits (P = 0.04), an increase of 0.69 office visits per person in the outpatient setting (P = 0.04), and an increase likelihood of getting a checkup (16.1 percentage points, P less than .001) in Medicaid expansion states. In Medicaid expansion states the share of adults obtaining regular care for chronic conditions increased by 12 percentage points after expansion (P = .008), compared with Texas. Additionally, adults reporting fair or poor quality of care dropped by 7.1 percentage points (P = .03).
One significant difference between the expansion states was changes in glucose monitoring rates for patients with diabetes were lower in Arkansas than Kentucky (–11.6 percentage points, P = .04).
“Of note, we found improvements in receipt of checkups, care for chronic conditions, and quality of care even in areas with primary care shortages, suggesting that while clinician capacity is undoubtedly an important consideration, insurance expansion can have a demonstrable positive impact even in areas with relative shortages, perhaps partially due to increased use of safety net providers,” the researchers added.
The study was supported by a research grant from the Commonwealth Fund and a grant from the Agency for Healthcare Research and Quality. The researchers reported having no financial disclosures.
Low-income adults living in two states that expanded Medicaid enrollment are showing significant increases in outpatient utilization and preventive care, improved health care quality, and reductions in emergency department use, compared with those living in a state that did not expand Medicaid, according to a new study.
The study also found similar improvements in care whether a state expanded traditional Medicaid or increased coverage through a private insurance option.
Benjamin D. Sommers, MD, PhD, of Harvard University, Boston, and his colleagues examined outcomes for nearly 9,000 low-income Medicaid enrollees in Kentucky (where officials expanded traditional Medicaid), Arkansas (where the state used funds to purchase private insurance to expand coverage), and Texas (which did not expand Medicaid) in November and December of 2013, 2014, and 2015. They looked specifically at changes in use of healthcare services, preventive care, and self-reported health (JAMA Intern Med. 2016 Aug 8. doi: 10.1001/jamainternmed.2016.4419).
“By the end of 2015, we found marked increases in coverage and reduced cost-related barriers to care in the expansion states, with associated increases in preventive care, outpatient visits, annual checkups, and chronic disease care, as well as decreased reliance on the [emergency department],” the researchers wrote.
They found that by 2015 there was a 6 percentage point drop in the likelihood of ED visits (P = 0.04), an increase of 0.69 office visits per person in the outpatient setting (P = 0.04), and an increase likelihood of getting a checkup (16.1 percentage points, P less than .001) in Medicaid expansion states. In Medicaid expansion states the share of adults obtaining regular care for chronic conditions increased by 12 percentage points after expansion (P = .008), compared with Texas. Additionally, adults reporting fair or poor quality of care dropped by 7.1 percentage points (P = .03).
One significant difference between the expansion states was changes in glucose monitoring rates for patients with diabetes were lower in Arkansas than Kentucky (–11.6 percentage points, P = .04).
“Of note, we found improvements in receipt of checkups, care for chronic conditions, and quality of care even in areas with primary care shortages, suggesting that while clinician capacity is undoubtedly an important consideration, insurance expansion can have a demonstrable positive impact even in areas with relative shortages, perhaps partially due to increased use of safety net providers,” the researchers added.
The study was supported by a research grant from the Commonwealth Fund and a grant from the Agency for Healthcare Research and Quality. The researchers reported having no financial disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Medicaid expansion improved self-reported health outcomes and access to care.
Major finding: By 2015 there was a 6 percentage point drop in the likelihood of emergency department visits (P = .04) and an increase of 0.69 outpatient office visits per person (P = .04).
Data source: A differences-in-differences analysis of survey data from Nov. 2013 through Dec. 2015 of 8,676 low-income adults in Kentucky, Arkansas, and Texas.
Disclosures: The study was supported by a research grant from the Commonwealth Fund and a grant from the Agency for Healthcare Research and Quality. The researchers reported having no financial disclosures.
Solid INRs on warfarin don’t predict future stability
Six months of stable international normalized ratio values [INRs] while on warfarin therapy doesn’t predict continued INR stability, according to a Research Letter to the Editor published August 9 in JAMA.
Whether or not to switch patients with atrial fibrillation from warfarin to non–vitamin K anticoagulants remains controversial. “A common belief has been that patients with stable INRs while taking warfarin would continue to be stable and derive less benefit from switching to non–vitamin K oral anticoagulants,” said Sean D. Pokorney, MD, of the division of cardiology, Duke University Medical Center, Durham, N.C., and his associates.
But the results of their observational study of 3,749 patients enrolled in an atrial fibrillation registry show that such stability cannot be predicted, and “challenge the notion that patients who have done well taking warfarin should maintain taking warfarin,” the investigators said (JAMA. 2016;316:661-3).
They assessed INRs over the course of 3 years of follow-up using data from patients enrolled in the registry through 176 clinics. INR stability was defined as having 80% or more of INRs in the therapeutic range (2-3). The mean patient age was 75 years, and 43% were women.
A total of 968 patients showed such INR stability throughout the first 6 months of the study. However, 36% of them went on to have at least one “well out of range” INR during the following year. Even in the subgroup of 376 patients who had 100% of their INRs within the therapeutic range during the first 6 months, 33% went on to have at least one “well out of range” INR during the following year, according to Dr. Pokorney and his associates.
No sponsor was cited for this study. Dr. Pokorney reported ties to AstraZeneca, Boston Scientific, Gilead, Janssen, and Medtronic; his associates reported ties to numerous industry sources.
Six months of stable international normalized ratio values [INRs] while on warfarin therapy doesn’t predict continued INR stability, according to a Research Letter to the Editor published August 9 in JAMA.
Whether or not to switch patients with atrial fibrillation from warfarin to non–vitamin K anticoagulants remains controversial. “A common belief has been that patients with stable INRs while taking warfarin would continue to be stable and derive less benefit from switching to non–vitamin K oral anticoagulants,” said Sean D. Pokorney, MD, of the division of cardiology, Duke University Medical Center, Durham, N.C., and his associates.
But the results of their observational study of 3,749 patients enrolled in an atrial fibrillation registry show that such stability cannot be predicted, and “challenge the notion that patients who have done well taking warfarin should maintain taking warfarin,” the investigators said (JAMA. 2016;316:661-3).
They assessed INRs over the course of 3 years of follow-up using data from patients enrolled in the registry through 176 clinics. INR stability was defined as having 80% or more of INRs in the therapeutic range (2-3). The mean patient age was 75 years, and 43% were women.
A total of 968 patients showed such INR stability throughout the first 6 months of the study. However, 36% of them went on to have at least one “well out of range” INR during the following year. Even in the subgroup of 376 patients who had 100% of their INRs within the therapeutic range during the first 6 months, 33% went on to have at least one “well out of range” INR during the following year, according to Dr. Pokorney and his associates.
No sponsor was cited for this study. Dr. Pokorney reported ties to AstraZeneca, Boston Scientific, Gilead, Janssen, and Medtronic; his associates reported ties to numerous industry sources.
Six months of stable international normalized ratio values [INRs] while on warfarin therapy doesn’t predict continued INR stability, according to a Research Letter to the Editor published August 9 in JAMA.
Whether or not to switch patients with atrial fibrillation from warfarin to non–vitamin K anticoagulants remains controversial. “A common belief has been that patients with stable INRs while taking warfarin would continue to be stable and derive less benefit from switching to non–vitamin K oral anticoagulants,” said Sean D. Pokorney, MD, of the division of cardiology, Duke University Medical Center, Durham, N.C., and his associates.
But the results of their observational study of 3,749 patients enrolled in an atrial fibrillation registry show that such stability cannot be predicted, and “challenge the notion that patients who have done well taking warfarin should maintain taking warfarin,” the investigators said (JAMA. 2016;316:661-3).
They assessed INRs over the course of 3 years of follow-up using data from patients enrolled in the registry through 176 clinics. INR stability was defined as having 80% or more of INRs in the therapeutic range (2-3). The mean patient age was 75 years, and 43% were women.
A total of 968 patients showed such INR stability throughout the first 6 months of the study. However, 36% of them went on to have at least one “well out of range” INR during the following year. Even in the subgroup of 376 patients who had 100% of their INRs within the therapeutic range during the first 6 months, 33% went on to have at least one “well out of range” INR during the following year, according to Dr. Pokorney and his associates.
No sponsor was cited for this study. Dr. Pokorney reported ties to AstraZeneca, Boston Scientific, Gilead, Janssen, and Medtronic; his associates reported ties to numerous industry sources.
FROM JAMA
Key clinical point: Six months of stable INRs while on warfarin doesn’t predict continued INR stability.
Major finding: Of the 968 patients who showed INR stability throughout the first 6 months of the study, 36% went on to have at least one “well out of range” INR during the following year.
Data source: An observational cohort study involving 3,749 patients with atrial fibrillation who were followed for 3 years.
Disclosures: No sponsor was cited for this study. Dr. Pokorney reported ties to AstraZeneca, Boston Scientific, Gilead, Janssen, and Medtronic; his associates reported ties to numerous industry sources.
Hospital safety culture may influence surgical outcomes
SAN DIEGO – Hospital safety culture may positively influence certain surgical patient outcomes, results from a study of 56 Illinois hospitals demonstrated.
“Efforts to improve awareness of safety and quality improvement principles should be encouraged at both the surgical system and hospital levels,” David D. Odell, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Safety culture itself is a concept [that] is increasingly viewed as important in the delivery of high-quality care. Yet in the surgical world, very little is known about how hospital culture actually influences outcomes for our patients.”
Dr. Odell, a thoracic surgeon at Northwestern Memorial Hospital, Chicago, discussed results from a study by the Illinois Surgical Quality Improvement Collaborative, a group of Illinois hospitals working together to improve the quality of surgical care in the state. Participants in the Collaborative include 56 hospitals, including all academic medical centers in the state, as well as 11 rural hospitals. Combined, these facilities perform 60% of general surgery operations in the state and 80% of all complex operations, impacting more than 600,000 patients each year.
In an effort to evaluate the relationship between hospital safety culture and surgical patient outcomes, Dr. Odell and his associates invited staff of Collaborative members to complete the Safety Attitudes Questionnaire (SAQ), a 56-item validated tool for assessment of hospital culture. Domains focused on were teamwork, communication, engagement, and leadership. The SAQ was given to administrators, staff, and front-line providers “to measure safety culture across all levels of the hospital,” Dr. Odell said. Percent positive responses were calculated at the hospital level for each of the eight domains to calculate a composite measure of safety. The researchers measured the impact of safety culture by assessing positive SAQ response rates. Outcome variables of interest were morbidity, mortality, death or serious morbidity, and readmission. Hospital-level risk-adjusted event rates and linear regression models were used to assess the impact of safety culture while controlling for teaching status, rural location, trauma center designation, hospital control (management), and the annual surgical volume.
Of the 49 participating hospitals represented in the survey responses, 49% had an Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program, 12% were rural, 61% provided trauma care, 35% had a religious affiliation, 57% were “other” not-for-profit, and the mean total surgical volume was 11,412 cases.
Dr. Odell reported that by domain, SAQ responses were most positive for operating room safety and lowest for hospital management. “That doesn’t necessarily reflect the management’s outcomes only, but the views of those who took the survey toward management,” he said.
When the researchers evaluated the impact of a more-positive safety culture on the risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02). The trend was similar although not statistically significant for death/serious morbidity (P = .08), mortality (P =. 20), or readmission (P = .68).
Dr. Odell acknowledged certain limitations of the study, including its retrospective design and the fact that the SAQ is a subjective assessment tool. “Not all [staff invited] were surveyed,” he added. “We sent out just under 1,400 surveys and we had a response rate of 44%.”
Staff from participating institutions of the Collaborative meet on a semiannual basis to share ideas, celebrate successes and learn from each other’s experiences, Dr. Odell said. Ongoing efforts to improve safety culture include fostering opportunities for mentorship in quality improvement and process improvement endeavors, as well as the provision of educational materials targeted at all levels of hospital staff “so that we can get everyone thinking and speaking the same language when it comes to quality improvement,” he said.
The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
SAN DIEGO – Hospital safety culture may positively influence certain surgical patient outcomes, results from a study of 56 Illinois hospitals demonstrated.
“Efforts to improve awareness of safety and quality improvement principles should be encouraged at both the surgical system and hospital levels,” David D. Odell, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Safety culture itself is a concept [that] is increasingly viewed as important in the delivery of high-quality care. Yet in the surgical world, very little is known about how hospital culture actually influences outcomes for our patients.”
Dr. Odell, a thoracic surgeon at Northwestern Memorial Hospital, Chicago, discussed results from a study by the Illinois Surgical Quality Improvement Collaborative, a group of Illinois hospitals working together to improve the quality of surgical care in the state. Participants in the Collaborative include 56 hospitals, including all academic medical centers in the state, as well as 11 rural hospitals. Combined, these facilities perform 60% of general surgery operations in the state and 80% of all complex operations, impacting more than 600,000 patients each year.
In an effort to evaluate the relationship between hospital safety culture and surgical patient outcomes, Dr. Odell and his associates invited staff of Collaborative members to complete the Safety Attitudes Questionnaire (SAQ), a 56-item validated tool for assessment of hospital culture. Domains focused on were teamwork, communication, engagement, and leadership. The SAQ was given to administrators, staff, and front-line providers “to measure safety culture across all levels of the hospital,” Dr. Odell said. Percent positive responses were calculated at the hospital level for each of the eight domains to calculate a composite measure of safety. The researchers measured the impact of safety culture by assessing positive SAQ response rates. Outcome variables of interest were morbidity, mortality, death or serious morbidity, and readmission. Hospital-level risk-adjusted event rates and linear regression models were used to assess the impact of safety culture while controlling for teaching status, rural location, trauma center designation, hospital control (management), and the annual surgical volume.
Of the 49 participating hospitals represented in the survey responses, 49% had an Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program, 12% were rural, 61% provided trauma care, 35% had a religious affiliation, 57% were “other” not-for-profit, and the mean total surgical volume was 11,412 cases.
Dr. Odell reported that by domain, SAQ responses were most positive for operating room safety and lowest for hospital management. “That doesn’t necessarily reflect the management’s outcomes only, but the views of those who took the survey toward management,” he said.
When the researchers evaluated the impact of a more-positive safety culture on the risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02). The trend was similar although not statistically significant for death/serious morbidity (P = .08), mortality (P =. 20), or readmission (P = .68).
Dr. Odell acknowledged certain limitations of the study, including its retrospective design and the fact that the SAQ is a subjective assessment tool. “Not all [staff invited] were surveyed,” he added. “We sent out just under 1,400 surveys and we had a response rate of 44%.”
Staff from participating institutions of the Collaborative meet on a semiannual basis to share ideas, celebrate successes and learn from each other’s experiences, Dr. Odell said. Ongoing efforts to improve safety culture include fostering opportunities for mentorship in quality improvement and process improvement endeavors, as well as the provision of educational materials targeted at all levels of hospital staff “so that we can get everyone thinking and speaking the same language when it comes to quality improvement,” he said.
The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
SAN DIEGO – Hospital safety culture may positively influence certain surgical patient outcomes, results from a study of 56 Illinois hospitals demonstrated.
“Efforts to improve awareness of safety and quality improvement principles should be encouraged at both the surgical system and hospital levels,” David D. Odell, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Safety culture itself is a concept [that] is increasingly viewed as important in the delivery of high-quality care. Yet in the surgical world, very little is known about how hospital culture actually influences outcomes for our patients.”
Dr. Odell, a thoracic surgeon at Northwestern Memorial Hospital, Chicago, discussed results from a study by the Illinois Surgical Quality Improvement Collaborative, a group of Illinois hospitals working together to improve the quality of surgical care in the state. Participants in the Collaborative include 56 hospitals, including all academic medical centers in the state, as well as 11 rural hospitals. Combined, these facilities perform 60% of general surgery operations in the state and 80% of all complex operations, impacting more than 600,000 patients each year.
In an effort to evaluate the relationship between hospital safety culture and surgical patient outcomes, Dr. Odell and his associates invited staff of Collaborative members to complete the Safety Attitudes Questionnaire (SAQ), a 56-item validated tool for assessment of hospital culture. Domains focused on were teamwork, communication, engagement, and leadership. The SAQ was given to administrators, staff, and front-line providers “to measure safety culture across all levels of the hospital,” Dr. Odell said. Percent positive responses were calculated at the hospital level for each of the eight domains to calculate a composite measure of safety. The researchers measured the impact of safety culture by assessing positive SAQ response rates. Outcome variables of interest were morbidity, mortality, death or serious morbidity, and readmission. Hospital-level risk-adjusted event rates and linear regression models were used to assess the impact of safety culture while controlling for teaching status, rural location, trauma center designation, hospital control (management), and the annual surgical volume.
Of the 49 participating hospitals represented in the survey responses, 49% had an Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program, 12% were rural, 61% provided trauma care, 35% had a religious affiliation, 57% were “other” not-for-profit, and the mean total surgical volume was 11,412 cases.
Dr. Odell reported that by domain, SAQ responses were most positive for operating room safety and lowest for hospital management. “That doesn’t necessarily reflect the management’s outcomes only, but the views of those who took the survey toward management,” he said.
When the researchers evaluated the impact of a more-positive safety culture on the risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02). The trend was similar although not statistically significant for death/serious morbidity (P = .08), mortality (P =. 20), or readmission (P = .68).
Dr. Odell acknowledged certain limitations of the study, including its retrospective design and the fact that the SAQ is a subjective assessment tool. “Not all [staff invited] were surveyed,” he added. “We sent out just under 1,400 surveys and we had a response rate of 44%.”
Staff from participating institutions of the Collaborative meet on a semiannual basis to share ideas, celebrate successes and learn from each other’s experiences, Dr. Odell said. Ongoing efforts to improve safety culture include fostering opportunities for mentorship in quality improvement and process improvement endeavors, as well as the provision of educational materials targeted at all levels of hospital staff “so that we can get everyone thinking and speaking the same language when it comes to quality improvement,” he said.
The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A positive hospital safety culture significantly impacted morbidity following surgery.
Major finding: When the researchers evaluated the impact of a positive safety culture on risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02).
Data source: A retrospective study by the Illinois Surgical Quality Improvement Collaborative, a group of 56 hospitals in the state.
Disclosures: The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
ACS NSQIP Geriatric Surgery Pilot Collaborative: Evaluating variables for inclusion
SAN DIEGO – A project to assess geriatric-specific variables for inclusion in the American College of Surgeons/National Surgical Quality Improvement Program National Conference is underway, according to Thomas N. Robinson, MD.
Dr. Robinson discussed results from the ACS-NSQIP Geriatric Surgery Pilot Collaborative, an effort launched in January 2014 with the ultimate goal of evaluating specific geriatric variables for incorporation into the ACS NSQIP set of essential variables collected by all participating hospitals.
Dr. Robinson, professor of surgery at the University of Colorado, Denver, said that 23 clinical sites in the United States are currently studying the following geriatric-specific variables in surgery patients aged 65 and older:
• Origin from home with support (to determine baseline functional status: lives alone at home, lives with support in home, origin status not from home).
• Discharge functional health status (ability to perform activities of daily living).
• Discharge with/without services (to capture care needs upon discharge).
• Preoperative use of a mobility aid.
• Preoperative history of prior falls.
• Postoperative history of pressure ulcer.
• Fall risk on discharge.
• New mobility aid on discharge.
• History of dementia.
• Competency status on admission.
• Postoperative delirium (yes or no).
• Hospice care on admission (yes or no).
• Do Not Resuscitate (DNR) order in place on admission (yes or no).
• DNR order during hospitalization (yes or no).
• Setting where DNR order was placed.
• Postoperative palliative care consult (yes or no).
• 30-day postoperative outcomes: functional health status (ability to perform activities of daily living), physical function compared with baseline, and living location.
The number of surgery cases in the collaborative grew from 7,235 in the first 6 months of 2014 to 24,835 cases in the last 6 months of 2015. The top 10 operations were total joint arthroplasty (29%), colectomy (12%), spine (8%), hip fracture (7%), carotid endarterectomy (4%), hysterectomy (4%), lung resection (2%), open lower extremity bypass (2%), laparoscopic cholecystectomy (2%), and pancreatectomy (2%).
Dr. Robinson reported that the rate of preoperative dementia among cases studied in the collaborative was 10%. “The incorporation of dementia into a surgical dataset represents an important step forward in providing quality surgical care for the elderly,” he said. “Dementia is a global public health concern.” He went on to note that patients with dementia have a 2.5-fold increased risk of developing postoperative delirium, making it “the perfect place to start a quality project. One in three cases of delirium is preventable. In our data set, delirium is associated with a hospital stay that’s 4 days longer, an increased chance of requiring discharge to an institutional care facility, an increased chance of a serious complication, and a higher 30-day mortality.”
Simple, low-tech bedside interventions such as ambulating in the hall three times a day, orienting the person, having the person sleep at night rather than sleep during the day, and avoiding medications with high risk for adverse events in older adults can prevent postoperative delirium, Dr. Robinson said.
One way that the Geriatric Surgery Pilot Collaborative can improve the surgical care of older adults is by fostering quality programs initiated at the participating local hospitals. “Preserving function after hospital stays is a first major goal,” he said. Another strategy involves creating a multidisciplinary frailty assessment to aid with decision making and risk assessment. “This takes into consideration NSQIP variables such as function, nutrition, comorbidity burden, cognition, social vulnerability, and mobility,” he said. The final and ultimate goal of the geriatric surgery collaborative is to establish a foundation of quality measurement for the Coalition for Quality in Geriatric Surgery, a project initiated by the American College of Surgeons to systematically improve the surgical care of older adults.
Dr. Robinson reported having no relevant financial disclosures.
SAN DIEGO – A project to assess geriatric-specific variables for inclusion in the American College of Surgeons/National Surgical Quality Improvement Program National Conference is underway, according to Thomas N. Robinson, MD.
Dr. Robinson discussed results from the ACS-NSQIP Geriatric Surgery Pilot Collaborative, an effort launched in January 2014 with the ultimate goal of evaluating specific geriatric variables for incorporation into the ACS NSQIP set of essential variables collected by all participating hospitals.
Dr. Robinson, professor of surgery at the University of Colorado, Denver, said that 23 clinical sites in the United States are currently studying the following geriatric-specific variables in surgery patients aged 65 and older:
• Origin from home with support (to determine baseline functional status: lives alone at home, lives with support in home, origin status not from home).
• Discharge functional health status (ability to perform activities of daily living).
• Discharge with/without services (to capture care needs upon discharge).
• Preoperative use of a mobility aid.
• Preoperative history of prior falls.
• Postoperative history of pressure ulcer.
• Fall risk on discharge.
• New mobility aid on discharge.
• History of dementia.
• Competency status on admission.
• Postoperative delirium (yes or no).
• Hospice care on admission (yes or no).
• Do Not Resuscitate (DNR) order in place on admission (yes or no).
• DNR order during hospitalization (yes or no).
• Setting where DNR order was placed.
• Postoperative palliative care consult (yes or no).
• 30-day postoperative outcomes: functional health status (ability to perform activities of daily living), physical function compared with baseline, and living location.
The number of surgery cases in the collaborative grew from 7,235 in the first 6 months of 2014 to 24,835 cases in the last 6 months of 2015. The top 10 operations were total joint arthroplasty (29%), colectomy (12%), spine (8%), hip fracture (7%), carotid endarterectomy (4%), hysterectomy (4%), lung resection (2%), open lower extremity bypass (2%), laparoscopic cholecystectomy (2%), and pancreatectomy (2%).
Dr. Robinson reported that the rate of preoperative dementia among cases studied in the collaborative was 10%. “The incorporation of dementia into a surgical dataset represents an important step forward in providing quality surgical care for the elderly,” he said. “Dementia is a global public health concern.” He went on to note that patients with dementia have a 2.5-fold increased risk of developing postoperative delirium, making it “the perfect place to start a quality project. One in three cases of delirium is preventable. In our data set, delirium is associated with a hospital stay that’s 4 days longer, an increased chance of requiring discharge to an institutional care facility, an increased chance of a serious complication, and a higher 30-day mortality.”
Simple, low-tech bedside interventions such as ambulating in the hall three times a day, orienting the person, having the person sleep at night rather than sleep during the day, and avoiding medications with high risk for adverse events in older adults can prevent postoperative delirium, Dr. Robinson said.
One way that the Geriatric Surgery Pilot Collaborative can improve the surgical care of older adults is by fostering quality programs initiated at the participating local hospitals. “Preserving function after hospital stays is a first major goal,” he said. Another strategy involves creating a multidisciplinary frailty assessment to aid with decision making and risk assessment. “This takes into consideration NSQIP variables such as function, nutrition, comorbidity burden, cognition, social vulnerability, and mobility,” he said. The final and ultimate goal of the geriatric surgery collaborative is to establish a foundation of quality measurement for the Coalition for Quality in Geriatric Surgery, a project initiated by the American College of Surgeons to systematically improve the surgical care of older adults.
Dr. Robinson reported having no relevant financial disclosures.
SAN DIEGO – A project to assess geriatric-specific variables for inclusion in the American College of Surgeons/National Surgical Quality Improvement Program National Conference is underway, according to Thomas N. Robinson, MD.
Dr. Robinson discussed results from the ACS-NSQIP Geriatric Surgery Pilot Collaborative, an effort launched in January 2014 with the ultimate goal of evaluating specific geriatric variables for incorporation into the ACS NSQIP set of essential variables collected by all participating hospitals.
Dr. Robinson, professor of surgery at the University of Colorado, Denver, said that 23 clinical sites in the United States are currently studying the following geriatric-specific variables in surgery patients aged 65 and older:
• Origin from home with support (to determine baseline functional status: lives alone at home, lives with support in home, origin status not from home).
• Discharge functional health status (ability to perform activities of daily living).
• Discharge with/without services (to capture care needs upon discharge).
• Preoperative use of a mobility aid.
• Preoperative history of prior falls.
• Postoperative history of pressure ulcer.
• Fall risk on discharge.
• New mobility aid on discharge.
• History of dementia.
• Competency status on admission.
• Postoperative delirium (yes or no).
• Hospice care on admission (yes or no).
• Do Not Resuscitate (DNR) order in place on admission (yes or no).
• DNR order during hospitalization (yes or no).
• Setting where DNR order was placed.
• Postoperative palliative care consult (yes or no).
• 30-day postoperative outcomes: functional health status (ability to perform activities of daily living), physical function compared with baseline, and living location.
The number of surgery cases in the collaborative grew from 7,235 in the first 6 months of 2014 to 24,835 cases in the last 6 months of 2015. The top 10 operations were total joint arthroplasty (29%), colectomy (12%), spine (8%), hip fracture (7%), carotid endarterectomy (4%), hysterectomy (4%), lung resection (2%), open lower extremity bypass (2%), laparoscopic cholecystectomy (2%), and pancreatectomy (2%).
Dr. Robinson reported that the rate of preoperative dementia among cases studied in the collaborative was 10%. “The incorporation of dementia into a surgical dataset represents an important step forward in providing quality surgical care for the elderly,” he said. “Dementia is a global public health concern.” He went on to note that patients with dementia have a 2.5-fold increased risk of developing postoperative delirium, making it “the perfect place to start a quality project. One in three cases of delirium is preventable. In our data set, delirium is associated with a hospital stay that’s 4 days longer, an increased chance of requiring discharge to an institutional care facility, an increased chance of a serious complication, and a higher 30-day mortality.”
Simple, low-tech bedside interventions such as ambulating in the hall three times a day, orienting the person, having the person sleep at night rather than sleep during the day, and avoiding medications with high risk for adverse events in older adults can prevent postoperative delirium, Dr. Robinson said.
One way that the Geriatric Surgery Pilot Collaborative can improve the surgical care of older adults is by fostering quality programs initiated at the participating local hospitals. “Preserving function after hospital stays is a first major goal,” he said. Another strategy involves creating a multidisciplinary frailty assessment to aid with decision making and risk assessment. “This takes into consideration NSQIP variables such as function, nutrition, comorbidity burden, cognition, social vulnerability, and mobility,” he said. The final and ultimate goal of the geriatric surgery collaborative is to establish a foundation of quality measurement for the Coalition for Quality in Geriatric Surgery, a project initiated by the American College of Surgeons to systematically improve the surgical care of older adults.
Dr. Robinson reported having no relevant financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
Study aims to better understand readmissions in pediatric surgery
SAN DIEGO – Readmission rates and the underlying reasons for them vary between medical specialties following surgery in children, a study of national data suggests.
“Hospital readmission is a very hot topic, particularly in light of the Affordable Care Act,” Afif N. Kulaylat, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Beyond economic costs there are very tangible costs to patients that we must consider. Readmissions have been associated with significant morbidity for patients. They often herald or implicate a postoperative complication. There are also indirect costs to patients and families such as time off from school or work.”
Dr. Kulaylat, of the division of pediatric surgery at Penn State Children’s Hospital, Hershey, Penn., presented findings from a retrospective analysis of NSQIP Pediatric (NSQIP-P), an ongoing collaboration between the ACS and the American Pediatric Surgical Association to improve the care of young patients. The researchers evaluated NSQIP-P data from 2013 and 2014 and focused on unplanned readmission within 30 days, including reasons for readmission based on NSQIP-P readmission categories and ICD-9 readmission codes as categorized by the AHRQ Clinical Classification Software. Multivariate logistic regression was used to evaluate factors associated with unplanned readmission.
Dr. Kulaylat reported results from a cohort of 129,849 patients cared for by 64 NSQIP-P participating hospitals. Among these, the all-cause readmission rate was 4.7%. After excluding patients with planned readmissions, the unplanned readmission rate was found to be 3.9%. From this cohort, 28% required reoperation within 30 days, and the median time from discharge to unplanned readmission was 8 days, with an interquartile range between 3 and 14 days.
Among the procedures captured in NSQIP-P, neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%). The most common reason for readmission was surgical site infection at 23%, followed by GI complications such as ileus, obstruction, and constipation (17%); pulmonary-related complications (9%); device-related complications including shunt malfunction (8%); neurologic (7%); pain (6%); other medical diseases (6%); sepsis (5%); electrolytes/dehydration (5%); and urinary tract infection (UTI, 3%). It is estimated that at least two-thirds of unplanned readmissions (63%) were directly related to surgery. “These reasons for readmission and their frequency closely parallel what is seen in adults, with the exception of bleeding complications, which were rare in children compared to adults,” Dr. Kulaylat said.
The top five CPT codes associated with readmissions were laparoscopic appendectomy, laparoscopic gastrostomy tube placement, and three additional codes related to placement and replacement/revision of ventricular shunts/catheters.
Reasons for readmission varied among specialties. For example, among general and thoracic surgery, surgical-site infections (SSI) and GI-related issues dominated, while in neurosurgery SSI and device issues dominated. In urology, UTIs were the most frequent, while ENT had a greater proportion of pulmonary complications. Certain patient variables were also associated with an increased risk of hospital readmission, including comorbidities related to GI, CNS, renal, and immunosuppression and nutrition (P less than .001 for all). The strongest association was the occurrence of a postoperative complication, namely a post-discharge complication.
“The granularity of NSQIP-P can continue to be refined to help predict who is likely to get readmitted or if specific follow-up strategies might identify those headed to readmission,” remarked Robert E. Cilley, MD, a senior author and surgeon-in-chief at Penn State Children’s Hospital. Dr. Kulaylat acknowledged certain limitations of the study, including its retrospective design, the potential for data entry/data interpretation error, and that the researchers were unable to adjust for clustering at the hospital level. Directions of future research include a plan to study readmissions and predictive factors at the procedural level, establish risk-adjusted specialty/procedural-specific benchmarks for readmission rates, and refine the accuracy and reliability of the readmission data. “With these NSQIP-P data there is substantial opportunity for quality improvement as we strive to improve the care of children everywhere,” Dr. Kulaylat said. He reported having no relevant disclosures.
SAN DIEGO – Readmission rates and the underlying reasons for them vary between medical specialties following surgery in children, a study of national data suggests.
“Hospital readmission is a very hot topic, particularly in light of the Affordable Care Act,” Afif N. Kulaylat, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Beyond economic costs there are very tangible costs to patients that we must consider. Readmissions have been associated with significant morbidity for patients. They often herald or implicate a postoperative complication. There are also indirect costs to patients and families such as time off from school or work.”
Dr. Kulaylat, of the division of pediatric surgery at Penn State Children’s Hospital, Hershey, Penn., presented findings from a retrospective analysis of NSQIP Pediatric (NSQIP-P), an ongoing collaboration between the ACS and the American Pediatric Surgical Association to improve the care of young patients. The researchers evaluated NSQIP-P data from 2013 and 2014 and focused on unplanned readmission within 30 days, including reasons for readmission based on NSQIP-P readmission categories and ICD-9 readmission codes as categorized by the AHRQ Clinical Classification Software. Multivariate logistic regression was used to evaluate factors associated with unplanned readmission.
Dr. Kulaylat reported results from a cohort of 129,849 patients cared for by 64 NSQIP-P participating hospitals. Among these, the all-cause readmission rate was 4.7%. After excluding patients with planned readmissions, the unplanned readmission rate was found to be 3.9%. From this cohort, 28% required reoperation within 30 days, and the median time from discharge to unplanned readmission was 8 days, with an interquartile range between 3 and 14 days.
Among the procedures captured in NSQIP-P, neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%). The most common reason for readmission was surgical site infection at 23%, followed by GI complications such as ileus, obstruction, and constipation (17%); pulmonary-related complications (9%); device-related complications including shunt malfunction (8%); neurologic (7%); pain (6%); other medical diseases (6%); sepsis (5%); electrolytes/dehydration (5%); and urinary tract infection (UTI, 3%). It is estimated that at least two-thirds of unplanned readmissions (63%) were directly related to surgery. “These reasons for readmission and their frequency closely parallel what is seen in adults, with the exception of bleeding complications, which were rare in children compared to adults,” Dr. Kulaylat said.
The top five CPT codes associated with readmissions were laparoscopic appendectomy, laparoscopic gastrostomy tube placement, and three additional codes related to placement and replacement/revision of ventricular shunts/catheters.
Reasons for readmission varied among specialties. For example, among general and thoracic surgery, surgical-site infections (SSI) and GI-related issues dominated, while in neurosurgery SSI and device issues dominated. In urology, UTIs were the most frequent, while ENT had a greater proportion of pulmonary complications. Certain patient variables were also associated with an increased risk of hospital readmission, including comorbidities related to GI, CNS, renal, and immunosuppression and nutrition (P less than .001 for all). The strongest association was the occurrence of a postoperative complication, namely a post-discharge complication.
“The granularity of NSQIP-P can continue to be refined to help predict who is likely to get readmitted or if specific follow-up strategies might identify those headed to readmission,” remarked Robert E. Cilley, MD, a senior author and surgeon-in-chief at Penn State Children’s Hospital. Dr. Kulaylat acknowledged certain limitations of the study, including its retrospective design, the potential for data entry/data interpretation error, and that the researchers were unable to adjust for clustering at the hospital level. Directions of future research include a plan to study readmissions and predictive factors at the procedural level, establish risk-adjusted specialty/procedural-specific benchmarks for readmission rates, and refine the accuracy and reliability of the readmission data. “With these NSQIP-P data there is substantial opportunity for quality improvement as we strive to improve the care of children everywhere,” Dr. Kulaylat said. He reported having no relevant disclosures.
SAN DIEGO – Readmission rates and the underlying reasons for them vary between medical specialties following surgery in children, a study of national data suggests.
“Hospital readmission is a very hot topic, particularly in light of the Affordable Care Act,” Afif N. Kulaylat, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Beyond economic costs there are very tangible costs to patients that we must consider. Readmissions have been associated with significant morbidity for patients. They often herald or implicate a postoperative complication. There are also indirect costs to patients and families such as time off from school or work.”
Dr. Kulaylat, of the division of pediatric surgery at Penn State Children’s Hospital, Hershey, Penn., presented findings from a retrospective analysis of NSQIP Pediatric (NSQIP-P), an ongoing collaboration between the ACS and the American Pediatric Surgical Association to improve the care of young patients. The researchers evaluated NSQIP-P data from 2013 and 2014 and focused on unplanned readmission within 30 days, including reasons for readmission based on NSQIP-P readmission categories and ICD-9 readmission codes as categorized by the AHRQ Clinical Classification Software. Multivariate logistic regression was used to evaluate factors associated with unplanned readmission.
Dr. Kulaylat reported results from a cohort of 129,849 patients cared for by 64 NSQIP-P participating hospitals. Among these, the all-cause readmission rate was 4.7%. After excluding patients with planned readmissions, the unplanned readmission rate was found to be 3.9%. From this cohort, 28% required reoperation within 30 days, and the median time from discharge to unplanned readmission was 8 days, with an interquartile range between 3 and 14 days.
Among the procedures captured in NSQIP-P, neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%). The most common reason for readmission was surgical site infection at 23%, followed by GI complications such as ileus, obstruction, and constipation (17%); pulmonary-related complications (9%); device-related complications including shunt malfunction (8%); neurologic (7%); pain (6%); other medical diseases (6%); sepsis (5%); electrolytes/dehydration (5%); and urinary tract infection (UTI, 3%). It is estimated that at least two-thirds of unplanned readmissions (63%) were directly related to surgery. “These reasons for readmission and their frequency closely parallel what is seen in adults, with the exception of bleeding complications, which were rare in children compared to adults,” Dr. Kulaylat said.
The top five CPT codes associated with readmissions were laparoscopic appendectomy, laparoscopic gastrostomy tube placement, and three additional codes related to placement and replacement/revision of ventricular shunts/catheters.
Reasons for readmission varied among specialties. For example, among general and thoracic surgery, surgical-site infections (SSI) and GI-related issues dominated, while in neurosurgery SSI and device issues dominated. In urology, UTIs were the most frequent, while ENT had a greater proportion of pulmonary complications. Certain patient variables were also associated with an increased risk of hospital readmission, including comorbidities related to GI, CNS, renal, and immunosuppression and nutrition (P less than .001 for all). The strongest association was the occurrence of a postoperative complication, namely a post-discharge complication.
“The granularity of NSQIP-P can continue to be refined to help predict who is likely to get readmitted or if specific follow-up strategies might identify those headed to readmission,” remarked Robert E. Cilley, MD, a senior author and surgeon-in-chief at Penn State Children’s Hospital. Dr. Kulaylat acknowledged certain limitations of the study, including its retrospective design, the potential for data entry/data interpretation error, and that the researchers were unable to adjust for clustering at the hospital level. Directions of future research include a plan to study readmissions and predictive factors at the procedural level, establish risk-adjusted specialty/procedural-specific benchmarks for readmission rates, and refine the accuracy and reliability of the readmission data. “With these NSQIP-P data there is substantial opportunity for quality improvement as we strive to improve the care of children everywhere,” Dr. Kulaylat said. He reported having no relevant disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Readmission rates following pediatric surgery vary between medical specialties.
Major finding: Among the procedures captured in ACS NSQIP Pediatric (NSQIP-P), neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%).
Data source: An analysis of 129,849 pediatric patients cared for by 64 NSQIP-P participating hospitals.
Disclosures: Dr. Kulaylat reported having no financial disclosures.
Age, not infusion frequency, affects hemophilia prophylaxis adherence
ORLANDO – The frequency of prophylactic clotting factor infusions does not appear to adversely affect adherence to hemophilia therapy in children, but age seems to play a role in compliance to prescribed regimens, investigators in two separate studies report.
A study of pediatric patients with moderate to severe hemophilia A or B on bleeding prophylaxis showed no significant differences in adherence between patients receiving two clotting factor infusions per week and those receiving three or four per week, reported Karen Strike, a physiotherapist at McMaster Children’s Hospital in Hamilton, Ont., and colleagues.
“This study demonstrates that our patients have a very high degree of adherence, and it doesn’t appear to be related to infusion frequency,” she said in an interview at a scientific poster session at the World Federation of Hemophilia World Congress.
Although their sample size was small – just 23 patients – the median levels of adherence were high for both twice-weekly infusers (99.5%) and 3-4 times per week infusers (96%; P = .053).
Ms. Strike acknowledges that the borderline P value could be due to the small sample size instead of a lack of association. Additionally, because the patients are managed by a regional hemophilia treatment center, they tend to be more engaged and more likely to cooperate with clinician instructions, she said.
“Basically, patients are either going to do what’s prescribed or they’re not. What that actual prescription is doesn’t seem to matter. If they prescribe you twice a week or they prescribe me every other day, you’re going to be adherent to twice a week or you’re not.
The investigators have expanded their study to include adult patients on primary prophylaxis and to look at additional co-variates that might have an effect on adherence, including interactions with a health care team, geographical distance from a hemophilia treatment center, joint health status, and infusion delivery method (peripheral vs. port).
Age may be a factor
In a separate study, German investigators report that adherence appears to vary by age.
Wolfgang Miesbach, MD, from Goethe University Hospital in Frankfurt, Germany, and colleagues asked all members of the German hemophilia patient organization with moderate or severe hemophilia to fill out the VERITAS-PRO (Validated Hemophilia Regimen Treatment Adherence Scale-Prophylaxis) questionnaire and compared scores across age groups.
Data were available on a total of 364 patients. The investigators found that among 131 children from birth to age 19, adherence to prescribed regimens was 100%. In contrast, the adherence rate among 189 adults aged 20-59 was 88.1%. After age 59, adherence rates began to improve as those 60 and older (44 patients) reported 93.9% adherence.
“Within the patients aged 20+, care by a hemophilia center was the only significant indicator for better adherence. The tendency of better adherence of patients aged greater than 60 compared to patients 20-59 may be explained by the significant association of the occurrence of pain with increasing age although a significant influence of pain on the adherence levels could not be demonstrated,” the investigators wrote.
Their findings point the way to possible interventions to facilitate adherence to prophylaxis among patients with hemophilia, they wrote.
Both studies were internally funded. The authors reported no relevant disclosures.
ORLANDO – The frequency of prophylactic clotting factor infusions does not appear to adversely affect adherence to hemophilia therapy in children, but age seems to play a role in compliance to prescribed regimens, investigators in two separate studies report.
A study of pediatric patients with moderate to severe hemophilia A or B on bleeding prophylaxis showed no significant differences in adherence between patients receiving two clotting factor infusions per week and those receiving three or four per week, reported Karen Strike, a physiotherapist at McMaster Children’s Hospital in Hamilton, Ont., and colleagues.
“This study demonstrates that our patients have a very high degree of adherence, and it doesn’t appear to be related to infusion frequency,” she said in an interview at a scientific poster session at the World Federation of Hemophilia World Congress.
Although their sample size was small – just 23 patients – the median levels of adherence were high for both twice-weekly infusers (99.5%) and 3-4 times per week infusers (96%; P = .053).
Ms. Strike acknowledges that the borderline P value could be due to the small sample size instead of a lack of association. Additionally, because the patients are managed by a regional hemophilia treatment center, they tend to be more engaged and more likely to cooperate with clinician instructions, she said.
“Basically, patients are either going to do what’s prescribed or they’re not. What that actual prescription is doesn’t seem to matter. If they prescribe you twice a week or they prescribe me every other day, you’re going to be adherent to twice a week or you’re not.
The investigators have expanded their study to include adult patients on primary prophylaxis and to look at additional co-variates that might have an effect on adherence, including interactions with a health care team, geographical distance from a hemophilia treatment center, joint health status, and infusion delivery method (peripheral vs. port).
Age may be a factor
In a separate study, German investigators report that adherence appears to vary by age.
Wolfgang Miesbach, MD, from Goethe University Hospital in Frankfurt, Germany, and colleagues asked all members of the German hemophilia patient organization with moderate or severe hemophilia to fill out the VERITAS-PRO (Validated Hemophilia Regimen Treatment Adherence Scale-Prophylaxis) questionnaire and compared scores across age groups.
Data were available on a total of 364 patients. The investigators found that among 131 children from birth to age 19, adherence to prescribed regimens was 100%. In contrast, the adherence rate among 189 adults aged 20-59 was 88.1%. After age 59, adherence rates began to improve as those 60 and older (44 patients) reported 93.9% adherence.
“Within the patients aged 20+, care by a hemophilia center was the only significant indicator for better adherence. The tendency of better adherence of patients aged greater than 60 compared to patients 20-59 may be explained by the significant association of the occurrence of pain with increasing age although a significant influence of pain on the adherence levels could not be demonstrated,” the investigators wrote.
Their findings point the way to possible interventions to facilitate adherence to prophylaxis among patients with hemophilia, they wrote.
Both studies were internally funded. The authors reported no relevant disclosures.
ORLANDO – The frequency of prophylactic clotting factor infusions does not appear to adversely affect adherence to hemophilia therapy in children, but age seems to play a role in compliance to prescribed regimens, investigators in two separate studies report.
A study of pediatric patients with moderate to severe hemophilia A or B on bleeding prophylaxis showed no significant differences in adherence between patients receiving two clotting factor infusions per week and those receiving three or four per week, reported Karen Strike, a physiotherapist at McMaster Children’s Hospital in Hamilton, Ont., and colleagues.
“This study demonstrates that our patients have a very high degree of adherence, and it doesn’t appear to be related to infusion frequency,” she said in an interview at a scientific poster session at the World Federation of Hemophilia World Congress.
Although their sample size was small – just 23 patients – the median levels of adherence were high for both twice-weekly infusers (99.5%) and 3-4 times per week infusers (96%; P = .053).
Ms. Strike acknowledges that the borderline P value could be due to the small sample size instead of a lack of association. Additionally, because the patients are managed by a regional hemophilia treatment center, they tend to be more engaged and more likely to cooperate with clinician instructions, she said.
“Basically, patients are either going to do what’s prescribed or they’re not. What that actual prescription is doesn’t seem to matter. If they prescribe you twice a week or they prescribe me every other day, you’re going to be adherent to twice a week or you’re not.
The investigators have expanded their study to include adult patients on primary prophylaxis and to look at additional co-variates that might have an effect on adherence, including interactions with a health care team, geographical distance from a hemophilia treatment center, joint health status, and infusion delivery method (peripheral vs. port).
Age may be a factor
In a separate study, German investigators report that adherence appears to vary by age.
Wolfgang Miesbach, MD, from Goethe University Hospital in Frankfurt, Germany, and colleagues asked all members of the German hemophilia patient organization with moderate or severe hemophilia to fill out the VERITAS-PRO (Validated Hemophilia Regimen Treatment Adherence Scale-Prophylaxis) questionnaire and compared scores across age groups.
Data were available on a total of 364 patients. The investigators found that among 131 children from birth to age 19, adherence to prescribed regimens was 100%. In contrast, the adherence rate among 189 adults aged 20-59 was 88.1%. After age 59, adherence rates began to improve as those 60 and older (44 patients) reported 93.9% adherence.
“Within the patients aged 20+, care by a hemophilia center was the only significant indicator for better adherence. The tendency of better adherence of patients aged greater than 60 compared to patients 20-59 may be explained by the significant association of the occurrence of pain with increasing age although a significant influence of pain on the adherence levels could not be demonstrated,” the investigators wrote.
Their findings point the way to possible interventions to facilitate adherence to prophylaxis among patients with hemophilia, they wrote.
Both studies were internally funded. The authors reported no relevant disclosures.
AT WFH 2016 WORLD CONGRESS
Key clinical point: Adherence to hemophilia prophylaxis regimens may be influenced by age but not frequency of infusions.
Major finding: Infusion frequency did not make a difference in adherence rates, but young and middle-aged adults reported lower adherence than did children or seniors.
Data source: A study of 23 pediatric hemophilia patients in Canada, and a separate study of 364 children and adults with moderate to severe hemophilia in Germany.
Disclosures: Both studies were internally funded. The authors reported no relevant disclosures.
Blood viral RNA may indicate severity of MERS coronavirus clinical course
The presence of blood viral RNA in patients presenting with possible Middle East respiratory syndrome coronavirus (MERS-CoV) may be a very reliable indicator of the severity of the infection’s clinical course, according to a new study published in Emerging Infectious Diseases.
“Our study aimed to evaluate the diagnostic utility of blood specimens for MERS-CoV infection by using large numbers of patients with a single viral origin and to determine the relationship between blood viral detection and clinical characteristics,” wrote the authors, led by So Yeon Kim, MD, of the National Medical Center in Seoul, South Korea.
The investigators recruited 21 MERS-CoV patients within South Korea, all of whom had been previously diagnosed by the Korea Centers for Disease Control and Prevention via respiratory samples and were of “a single viral origin.” All subjects contributed ethylenediaminetetraacetic acid (EDTA)-treated whole blood and serum specimens, from which viral RNA was extracted (Emerg Infect Dis. 2016 Oct 15;22[10]. doi: 10.3201/eid2210.160218).
Viral RNA was detected in 6 of 21 whole blood samples and 6 of 21 serum samples at hospital admission. However, because two patients were viral positive in either specimen subtype of EDTA-treated whole blood or serum, the overall detection rate for the population was 7 of 21 (33%). Being positive for blood viral RNA at admission was found to be associated with a fever of higher than 37.5 °C (99.5 °F) on the date of sample collection (P = .007), being placed on mechanical ventilation at some point during the clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and death (P = .025).
However, “between the blood viral RNA-positive and -negative groups, we found no differences in age, duration from symptom onset to diagnosis of MERS-CoV infection, or an invasive procedure before the specimens were obtained,” the investigators noted.
The takeaway, the authors underscore, is that although early blood viral RNA presence may not be a useful diagnostic tool, it “might be a good prognostic indicator of severe outcome” due to its high association with worse clinical course.
The research was funded by the National Medical Center Research Institute.
The presence of blood viral RNA in patients presenting with possible Middle East respiratory syndrome coronavirus (MERS-CoV) may be a very reliable indicator of the severity of the infection’s clinical course, according to a new study published in Emerging Infectious Diseases.
“Our study aimed to evaluate the diagnostic utility of blood specimens for MERS-CoV infection by using large numbers of patients with a single viral origin and to determine the relationship between blood viral detection and clinical characteristics,” wrote the authors, led by So Yeon Kim, MD, of the National Medical Center in Seoul, South Korea.
The investigators recruited 21 MERS-CoV patients within South Korea, all of whom had been previously diagnosed by the Korea Centers for Disease Control and Prevention via respiratory samples and were of “a single viral origin.” All subjects contributed ethylenediaminetetraacetic acid (EDTA)-treated whole blood and serum specimens, from which viral RNA was extracted (Emerg Infect Dis. 2016 Oct 15;22[10]. doi: 10.3201/eid2210.160218).
Viral RNA was detected in 6 of 21 whole blood samples and 6 of 21 serum samples at hospital admission. However, because two patients were viral positive in either specimen subtype of EDTA-treated whole blood or serum, the overall detection rate for the population was 7 of 21 (33%). Being positive for blood viral RNA at admission was found to be associated with a fever of higher than 37.5 °C (99.5 °F) on the date of sample collection (P = .007), being placed on mechanical ventilation at some point during the clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and death (P = .025).
However, “between the blood viral RNA-positive and -negative groups, we found no differences in age, duration from symptom onset to diagnosis of MERS-CoV infection, or an invasive procedure before the specimens were obtained,” the investigators noted.
The takeaway, the authors underscore, is that although early blood viral RNA presence may not be a useful diagnostic tool, it “might be a good prognostic indicator of severe outcome” due to its high association with worse clinical course.
The research was funded by the National Medical Center Research Institute.
The presence of blood viral RNA in patients presenting with possible Middle East respiratory syndrome coronavirus (MERS-CoV) may be a very reliable indicator of the severity of the infection’s clinical course, according to a new study published in Emerging Infectious Diseases.
“Our study aimed to evaluate the diagnostic utility of blood specimens for MERS-CoV infection by using large numbers of patients with a single viral origin and to determine the relationship between blood viral detection and clinical characteristics,” wrote the authors, led by So Yeon Kim, MD, of the National Medical Center in Seoul, South Korea.
The investigators recruited 21 MERS-CoV patients within South Korea, all of whom had been previously diagnosed by the Korea Centers for Disease Control and Prevention via respiratory samples and were of “a single viral origin.” All subjects contributed ethylenediaminetetraacetic acid (EDTA)-treated whole blood and serum specimens, from which viral RNA was extracted (Emerg Infect Dis. 2016 Oct 15;22[10]. doi: 10.3201/eid2210.160218).
Viral RNA was detected in 6 of 21 whole blood samples and 6 of 21 serum samples at hospital admission. However, because two patients were viral positive in either specimen subtype of EDTA-treated whole blood or serum, the overall detection rate for the population was 7 of 21 (33%). Being positive for blood viral RNA at admission was found to be associated with a fever of higher than 37.5 °C (99.5 °F) on the date of sample collection (P = .007), being placed on mechanical ventilation at some point during the clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and death (P = .025).
However, “between the blood viral RNA-positive and -negative groups, we found no differences in age, duration from symptom onset to diagnosis of MERS-CoV infection, or an invasive procedure before the specimens were obtained,” the investigators noted.
The takeaway, the authors underscore, is that although early blood viral RNA presence may not be a useful diagnostic tool, it “might be a good prognostic indicator of severe outcome” due to its high association with worse clinical course.
The research was funded by the National Medical Center Research Institute.
FROM EMERGING INFECTIOUS DISEASES
Key clinical point: Checking for blood viral RNA at hospital admission may be a reliable indicator of the severity of MERS coronavirus infection clinical course.
Major finding: Blood viral RNA positivity at admission was associated with fever higher than 37.5 °C on the sampling date (P = .007), requirement for mechanical ventilation during the following clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and patient death (P = .025).
Data source: Prospective analysis of 21 patients with Middle East respiratory syndrome coronavirus (MERS-CoV).
Disclosures: The research was funded by the National Medical Center Research Institute.
Early Alzheimer’s treatment decreases both costs and mortality
TORONTO – For patients with Alzheimer’s disease, early treatment may translate into lower health care costs and better survival, based on study results reported at the Alzheimer’s Association International Conference 2016.
A review of Medicare claims data from more than 1,300 patients who received a diagnosis of Alzheimer’s disease during 2010-2013 found that patients who got standard anti-dementia therapy within a month of an Alzheimer’s diagnosis had a 28% lower risk of dying by 6 months than did patients who weren’t treated. And while their health care costs spiked at the time of diagnosis, monthly costs were consistently lower, yielding an overall savings of about $1,700 by the end of the study.
It’s not that the drugs themselves exerted any lifesaving effects, said study co-author Christopher Black, associate director of outcomes research at Merck Research Laboratories, Rahway, N.J. Rather, the observed benefit is probably because the patients who got treated also then got consistent medical attention for health-threatening comorbidities.
“This is an important caveat,” Mr. Black said in an interview at the meeting. “We are not saying that anti-dementia treatment is causing longer survival. It’s a proxy for better care. Typically, dementia patients die of complications from comorbidities that are exacerbated by Alzheimer’s symptoms.”
Mr. Black and his colleagues examined healthcare costs and utilization during the 12 months before diagnosis and in the 6 months after diagnosis. They also looked at mortality incidence. He and his colleagues identified 6,553 incident Alzheimer’s patients. Just 35% received a prescription for an anti-dementia medication within the month after diagnosis. Most patients (67%) got donepezil. Other prescribed medications were memantine (19%), rivastigmine (12%) and galantamine (2%).
There were several significant differences between the treated and untreated groups. Untreated patients were older (84 vs. 81 years) and had a significantly higher Charlson comorbidity index (3.5 vs. 3.2). To account for these differences, the researchers used propensity score matching on the basis of medical comorbidities, age, and other demographics to compare 694 patients from each group.
At the end of 6 months, treated patients had a 28% lower risk of dying (hazard ratio, 0.72) than did non-treated patients. Health care costs and utilization showed significant differences as well. Before diagnosis, monthly medical costs were similar (average $665). During the month of diagnosis, costs surged for both groups, although more so in the group that was untreated (mean $6,711 vs. $5,535). This probably reflected the general health differences between the two groups, as well as the cost of transitioning into a hospital, or from a hospital to a long-term care facility, Mr. Black said.
“This spike at the time of diagnosis is important,” he said in an interview. “The major cost driver was inpatient hospitalization and skilled nursing home placement, and this was driven by 10% of the patients.”
After the first month, costs declined and stabilized in each group. However, the between-group differences remained. There were half as many hospice visits per month among the treated patients (0.04 vs. 0.09; P = .0001). Monthly costs overall were lower, but not to a statistically significant extent ($2,207 vs. $2,349; P = .3037). Total health care costs by the end of the follow-up period averaged about $1,700 less in treated patients.
“Even after adjusting for demographic and clinical differences, results suggested that treated Alzheimer’s patients had lower all-cause health care costs and lower mortality rates compared to untreated patients,” Mr. Black said. “The arguments for early treatment are myriad, but this study shows greater survival and less all-cause health care costs among those receiving treatment for dementia. These results indicate that choosing not to treat, or even a delay in starting treatment, may lead to less favorable results. Early diagnosis and time to treatment should be a priority for policymakers, physicians and the public.”
On Twitter @alz_gal
TORONTO – For patients with Alzheimer’s disease, early treatment may translate into lower health care costs and better survival, based on study results reported at the Alzheimer’s Association International Conference 2016.
A review of Medicare claims data from more than 1,300 patients who received a diagnosis of Alzheimer’s disease during 2010-2013 found that patients who got standard anti-dementia therapy within a month of an Alzheimer’s diagnosis had a 28% lower risk of dying by 6 months than did patients who weren’t treated. And while their health care costs spiked at the time of diagnosis, monthly costs were consistently lower, yielding an overall savings of about $1,700 by the end of the study.
It’s not that the drugs themselves exerted any lifesaving effects, said study co-author Christopher Black, associate director of outcomes research at Merck Research Laboratories, Rahway, N.J. Rather, the observed benefit is probably because the patients who got treated also then got consistent medical attention for health-threatening comorbidities.
“This is an important caveat,” Mr. Black said in an interview at the meeting. “We are not saying that anti-dementia treatment is causing longer survival. It’s a proxy for better care. Typically, dementia patients die of complications from comorbidities that are exacerbated by Alzheimer’s symptoms.”
Mr. Black and his colleagues examined healthcare costs and utilization during the 12 months before diagnosis and in the 6 months after diagnosis. They also looked at mortality incidence. He and his colleagues identified 6,553 incident Alzheimer’s patients. Just 35% received a prescription for an anti-dementia medication within the month after diagnosis. Most patients (67%) got donepezil. Other prescribed medications were memantine (19%), rivastigmine (12%) and galantamine (2%).
There were several significant differences between the treated and untreated groups. Untreated patients were older (84 vs. 81 years) and had a significantly higher Charlson comorbidity index (3.5 vs. 3.2). To account for these differences, the researchers used propensity score matching on the basis of medical comorbidities, age, and other demographics to compare 694 patients from each group.
At the end of 6 months, treated patients had a 28% lower risk of dying (hazard ratio, 0.72) than did non-treated patients. Health care costs and utilization showed significant differences as well. Before diagnosis, monthly medical costs were similar (average $665). During the month of diagnosis, costs surged for both groups, although more so in the group that was untreated (mean $6,711 vs. $5,535). This probably reflected the general health differences between the two groups, as well as the cost of transitioning into a hospital, or from a hospital to a long-term care facility, Mr. Black said.
“This spike at the time of diagnosis is important,” he said in an interview. “The major cost driver was inpatient hospitalization and skilled nursing home placement, and this was driven by 10% of the patients.”
After the first month, costs declined and stabilized in each group. However, the between-group differences remained. There were half as many hospice visits per month among the treated patients (0.04 vs. 0.09; P = .0001). Monthly costs overall were lower, but not to a statistically significant extent ($2,207 vs. $2,349; P = .3037). Total health care costs by the end of the follow-up period averaged about $1,700 less in treated patients.
“Even after adjusting for demographic and clinical differences, results suggested that treated Alzheimer’s patients had lower all-cause health care costs and lower mortality rates compared to untreated patients,” Mr. Black said. “The arguments for early treatment are myriad, but this study shows greater survival and less all-cause health care costs among those receiving treatment for dementia. These results indicate that choosing not to treat, or even a delay in starting treatment, may lead to less favorable results. Early diagnosis and time to treatment should be a priority for policymakers, physicians and the public.”
On Twitter @alz_gal
TORONTO – For patients with Alzheimer’s disease, early treatment may translate into lower health care costs and better survival, based on study results reported at the Alzheimer’s Association International Conference 2016.
A review of Medicare claims data from more than 1,300 patients who received a diagnosis of Alzheimer’s disease during 2010-2013 found that patients who got standard anti-dementia therapy within a month of an Alzheimer’s diagnosis had a 28% lower risk of dying by 6 months than did patients who weren’t treated. And while their health care costs spiked at the time of diagnosis, monthly costs were consistently lower, yielding an overall savings of about $1,700 by the end of the study.
It’s not that the drugs themselves exerted any lifesaving effects, said study co-author Christopher Black, associate director of outcomes research at Merck Research Laboratories, Rahway, N.J. Rather, the observed benefit is probably because the patients who got treated also then got consistent medical attention for health-threatening comorbidities.
“This is an important caveat,” Mr. Black said in an interview at the meeting. “We are not saying that anti-dementia treatment is causing longer survival. It’s a proxy for better care. Typically, dementia patients die of complications from comorbidities that are exacerbated by Alzheimer’s symptoms.”
Mr. Black and his colleagues examined healthcare costs and utilization during the 12 months before diagnosis and in the 6 months after diagnosis. They also looked at mortality incidence. He and his colleagues identified 6,553 incident Alzheimer’s patients. Just 35% received a prescription for an anti-dementia medication within the month after diagnosis. Most patients (67%) got donepezil. Other prescribed medications were memantine (19%), rivastigmine (12%) and galantamine (2%).
There were several significant differences between the treated and untreated groups. Untreated patients were older (84 vs. 81 years) and had a significantly higher Charlson comorbidity index (3.5 vs. 3.2). To account for these differences, the researchers used propensity score matching on the basis of medical comorbidities, age, and other demographics to compare 694 patients from each group.
At the end of 6 months, treated patients had a 28% lower risk of dying (hazard ratio, 0.72) than did non-treated patients. Health care costs and utilization showed significant differences as well. Before diagnosis, monthly medical costs were similar (average $665). During the month of diagnosis, costs surged for both groups, although more so in the group that was untreated (mean $6,711 vs. $5,535). This probably reflected the general health differences between the two groups, as well as the cost of transitioning into a hospital, or from a hospital to a long-term care facility, Mr. Black said.
“This spike at the time of diagnosis is important,” he said in an interview. “The major cost driver was inpatient hospitalization and skilled nursing home placement, and this was driven by 10% of the patients.”
After the first month, costs declined and stabilized in each group. However, the between-group differences remained. There were half as many hospice visits per month among the treated patients (0.04 vs. 0.09; P = .0001). Monthly costs overall were lower, but not to a statistically significant extent ($2,207 vs. $2,349; P = .3037). Total health care costs by the end of the follow-up period averaged about $1,700 less in treated patients.
“Even after adjusting for demographic and clinical differences, results suggested that treated Alzheimer’s patients had lower all-cause health care costs and lower mortality rates compared to untreated patients,” Mr. Black said. “The arguments for early treatment are myriad, but this study shows greater survival and less all-cause health care costs among those receiving treatment for dementia. These results indicate that choosing not to treat, or even a delay in starting treatment, may lead to less favorable results. Early diagnosis and time to treatment should be a priority for policymakers, physicians and the public.”
On Twitter @alz_gal
AT AAIC 2016
Key clinical point: Alzheimer’s patients who get early medical treatment have less risk of dying and incur lower health care costs.
Major finding: By 6 months after diagnosis, treated patients had a 28% lower risk of dying, and had incurred about $1,700 less in health care expenditures.
Data source: The Medicare claims database study comprised about 1,300 patients.
Disclosures: Christopher Black is an associate director of outcomes research at Merck Research Laboratories, Rahway, N.J.