User login
News and Views that Matter to Physicians
Same-day discharge after PCI gets a boost
PARIS – Same-day discharge after uncomplicated transradial-access percutaneous coronary intervention (PCI) in patients with stable coronary artery disease is both feasible and safe, according to the findings of a multicenter prospective Spanish registry study.
Under the Spanish investigators’ protocol for same-day discharge, roughly three-quarters of patients successfully completed the 4- to 12-hour post-PCI surveillance period and were expeditiously sent home without spending a night in the hospital, Juan Gabriel Cordoba Soriano, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The other 26% of patients were admitted, most often because they showed clinical instability during the surveillance period, less frequently due to a suboptimal angiographic result, explained Dr. Cordoba Soriano of the University of Albacete, Spain.
The rationale for same-day discharge post PCI – provided it has first been shown to be safe, as was the case using the Spanish criteria – is that it reduces costs by avoiding an expensive hospital bed. Also, most patients prefer to sleep in their own bed and avoid a hospital stay, he continued.
Eligibility for same-day discharge in the Spanish study was restricted to patients with stable coronary artery disease undergoing elective transradial PCI with no complications during the procedure and with clinical stability during the subsequent 4- to 12-hour observation period. Patients undergoing complex PCIs – for example, treatment of left main lesions, complex bifurcation lesions, or chronic total occlusions – were ineligible.
Why restrict eligibility to patients undergoing transradial PCI? Multiple studies convincingly show it is safer than femoral access. And outside of the United States, it is by far the more popular access route. In a show of hands, virtually all of Dr. Cordoba Soriano’s audience indicated they perform more than 70% of their PCIs via transradial access. And patients with stable CAD are less likely to experience stent thrombosis or acute occlusion of the treated artery or side branches, he continued.
Of 989 patients who presented to the three participating Spanish medical centers for elective PCI, 257 were immediately excluded from the registry because they underwent elective femoral access. That left 732 patients, 74% of whom got same-day discharge.
The same-day discharge and hospital admission groups were closely similar in terms of baseline characteristics with two exceptions: The prevalence of peripheral arterial disease in the same-day discharge group was less than half of the 10% figure in the hospitalized group, and kidney function was better in patients who ultimately received same-day discharge as evidenced by a serum creatinine of 0.9 mg/dL, half that of the hospitalized patients.
Procedural characteristics were mostly similar for the two groups as well. Although the same-day discharge group had a 26-minute shorter median procedure time, were less likely to undergo multivessel PCI, and had fewer stents implanted per patient, in a multivariate regression analysis the only independent predictors of admission post PCI were the presence of peripheral arterial disease, with an associated 2.2-fold increased risk; multivessel PCI, with a 1.8-fold risk; ad hoc as opposed to a scheduled PCI, with a 4.0-fold increased risk; and a history of prior transradial catheterization, which cut the risk of hospitalization in half.
Turning to the safety of same-day discharge, the cardiologist deemed the rate of major complications in the first 24 hours to be acceptable at 0.18% for a single case of significant bleeding. Minor complications were confined to a 1.8% incidence of hematomas greater than 5 cm in size.
The major complication rate from 24 hours to 30 days post PCI was 0.54% (two deaths, one stroke), with a 2.2% incidence of minor complications.
Dr. Cordoba Soriano noted that investigators at the Quebec Heart and Lung Institute have published a meta-analysis of 13 studies of same-day discharge after PCI totaling more than 111,000 patients (JACC Cardiovasc Interv. 2013 Feb;6[2]:99-112). The investigators concluded that a definitive randomized trial would require more than 17,000 subjects, and in the absence of such evidence same-day discharge after uncomplicated PCI “seems a reasonable approach in selected patients.”
Stanford University investigators have published a separate meta-analysis of same-day discharge after PCI in nearly 13,000 patients in 30 observational and 7 randomized controlled trials. They concluded that it appears to be as safe as overnight observation (J Am Coll Cardiol. 2013 Jul 23;62[4]:275-85).
Nevertheless, the Society for Cardiovascular Angiography and Interventions has yet to update its 2009 expert consensus document stating that the standard of care is an overnight stay following PCI (Catheter Cardiovasc Interv. 2009 Jun 1;73[7]:847-58), Dr. Cordoba Soriano observed.
He reported having no financial conflicts regarding the registry study, which was conducted with university research funds.
PARIS – Same-day discharge after uncomplicated transradial-access percutaneous coronary intervention (PCI) in patients with stable coronary artery disease is both feasible and safe, according to the findings of a multicenter prospective Spanish registry study.
Under the Spanish investigators’ protocol for same-day discharge, roughly three-quarters of patients successfully completed the 4- to 12-hour post-PCI surveillance period and were expeditiously sent home without spending a night in the hospital, Juan Gabriel Cordoba Soriano, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The other 26% of patients were admitted, most often because they showed clinical instability during the surveillance period, less frequently due to a suboptimal angiographic result, explained Dr. Cordoba Soriano of the University of Albacete, Spain.
The rationale for same-day discharge post PCI – provided it has first been shown to be safe, as was the case using the Spanish criteria – is that it reduces costs by avoiding an expensive hospital bed. Also, most patients prefer to sleep in their own bed and avoid a hospital stay, he continued.
Eligibility for same-day discharge in the Spanish study was restricted to patients with stable coronary artery disease undergoing elective transradial PCI with no complications during the procedure and with clinical stability during the subsequent 4- to 12-hour observation period. Patients undergoing complex PCIs – for example, treatment of left main lesions, complex bifurcation lesions, or chronic total occlusions – were ineligible.
Why restrict eligibility to patients undergoing transradial PCI? Multiple studies convincingly show it is safer than femoral access. And outside of the United States, it is by far the more popular access route. In a show of hands, virtually all of Dr. Cordoba Soriano’s audience indicated they perform more than 70% of their PCIs via transradial access. And patients with stable CAD are less likely to experience stent thrombosis or acute occlusion of the treated artery or side branches, he continued.
Of 989 patients who presented to the three participating Spanish medical centers for elective PCI, 257 were immediately excluded from the registry because they underwent elective femoral access. That left 732 patients, 74% of whom got same-day discharge.
The same-day discharge and hospital admission groups were closely similar in terms of baseline characteristics with two exceptions: The prevalence of peripheral arterial disease in the same-day discharge group was less than half of the 10% figure in the hospitalized group, and kidney function was better in patients who ultimately received same-day discharge as evidenced by a serum creatinine of 0.9 mg/dL, half that of the hospitalized patients.
Procedural characteristics were mostly similar for the two groups as well. Although the same-day discharge group had a 26-minute shorter median procedure time, were less likely to undergo multivessel PCI, and had fewer stents implanted per patient, in a multivariate regression analysis the only independent predictors of admission post PCI were the presence of peripheral arterial disease, with an associated 2.2-fold increased risk; multivessel PCI, with a 1.8-fold risk; ad hoc as opposed to a scheduled PCI, with a 4.0-fold increased risk; and a history of prior transradial catheterization, which cut the risk of hospitalization in half.
Turning to the safety of same-day discharge, the cardiologist deemed the rate of major complications in the first 24 hours to be acceptable at 0.18% for a single case of significant bleeding. Minor complications were confined to a 1.8% incidence of hematomas greater than 5 cm in size.
The major complication rate from 24 hours to 30 days post PCI was 0.54% (two deaths, one stroke), with a 2.2% incidence of minor complications.
Dr. Cordoba Soriano noted that investigators at the Quebec Heart and Lung Institute have published a meta-analysis of 13 studies of same-day discharge after PCI totaling more than 111,000 patients (JACC Cardiovasc Interv. 2013 Feb;6[2]:99-112). The investigators concluded that a definitive randomized trial would require more than 17,000 subjects, and in the absence of such evidence same-day discharge after uncomplicated PCI “seems a reasonable approach in selected patients.”
Stanford University investigators have published a separate meta-analysis of same-day discharge after PCI in nearly 13,000 patients in 30 observational and 7 randomized controlled trials. They concluded that it appears to be as safe as overnight observation (J Am Coll Cardiol. 2013 Jul 23;62[4]:275-85).
Nevertheless, the Society for Cardiovascular Angiography and Interventions has yet to update its 2009 expert consensus document stating that the standard of care is an overnight stay following PCI (Catheter Cardiovasc Interv. 2009 Jun 1;73[7]:847-58), Dr. Cordoba Soriano observed.
He reported having no financial conflicts regarding the registry study, which was conducted with university research funds.
PARIS – Same-day discharge after uncomplicated transradial-access percutaneous coronary intervention (PCI) in patients with stable coronary artery disease is both feasible and safe, according to the findings of a multicenter prospective Spanish registry study.
Under the Spanish investigators’ protocol for same-day discharge, roughly three-quarters of patients successfully completed the 4- to 12-hour post-PCI surveillance period and were expeditiously sent home without spending a night in the hospital, Juan Gabriel Cordoba Soriano, MD, reported at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The other 26% of patients were admitted, most often because they showed clinical instability during the surveillance period, less frequently due to a suboptimal angiographic result, explained Dr. Cordoba Soriano of the University of Albacete, Spain.
The rationale for same-day discharge post PCI – provided it has first been shown to be safe, as was the case using the Spanish criteria – is that it reduces costs by avoiding an expensive hospital bed. Also, most patients prefer to sleep in their own bed and avoid a hospital stay, he continued.
Eligibility for same-day discharge in the Spanish study was restricted to patients with stable coronary artery disease undergoing elective transradial PCI with no complications during the procedure and with clinical stability during the subsequent 4- to 12-hour observation period. Patients undergoing complex PCIs – for example, treatment of left main lesions, complex bifurcation lesions, or chronic total occlusions – were ineligible.
Why restrict eligibility to patients undergoing transradial PCI? Multiple studies convincingly show it is safer than femoral access. And outside of the United States, it is by far the more popular access route. In a show of hands, virtually all of Dr. Cordoba Soriano’s audience indicated they perform more than 70% of their PCIs via transradial access. And patients with stable CAD are less likely to experience stent thrombosis or acute occlusion of the treated artery or side branches, he continued.
Of 989 patients who presented to the three participating Spanish medical centers for elective PCI, 257 were immediately excluded from the registry because they underwent elective femoral access. That left 732 patients, 74% of whom got same-day discharge.
The same-day discharge and hospital admission groups were closely similar in terms of baseline characteristics with two exceptions: The prevalence of peripheral arterial disease in the same-day discharge group was less than half of the 10% figure in the hospitalized group, and kidney function was better in patients who ultimately received same-day discharge as evidenced by a serum creatinine of 0.9 mg/dL, half that of the hospitalized patients.
Procedural characteristics were mostly similar for the two groups as well. Although the same-day discharge group had a 26-minute shorter median procedure time, were less likely to undergo multivessel PCI, and had fewer stents implanted per patient, in a multivariate regression analysis the only independent predictors of admission post PCI were the presence of peripheral arterial disease, with an associated 2.2-fold increased risk; multivessel PCI, with a 1.8-fold risk; ad hoc as opposed to a scheduled PCI, with a 4.0-fold increased risk; and a history of prior transradial catheterization, which cut the risk of hospitalization in half.
Turning to the safety of same-day discharge, the cardiologist deemed the rate of major complications in the first 24 hours to be acceptable at 0.18% for a single case of significant bleeding. Minor complications were confined to a 1.8% incidence of hematomas greater than 5 cm in size.
The major complication rate from 24 hours to 30 days post PCI was 0.54% (two deaths, one stroke), with a 2.2% incidence of minor complications.
Dr. Cordoba Soriano noted that investigators at the Quebec Heart and Lung Institute have published a meta-analysis of 13 studies of same-day discharge after PCI totaling more than 111,000 patients (JACC Cardiovasc Interv. 2013 Feb;6[2]:99-112). The investigators concluded that a definitive randomized trial would require more than 17,000 subjects, and in the absence of such evidence same-day discharge after uncomplicated PCI “seems a reasonable approach in selected patients.”
Stanford University investigators have published a separate meta-analysis of same-day discharge after PCI in nearly 13,000 patients in 30 observational and 7 randomized controlled trials. They concluded that it appears to be as safe as overnight observation (J Am Coll Cardiol. 2013 Jul 23;62[4]:275-85).
Nevertheless, the Society for Cardiovascular Angiography and Interventions has yet to update its 2009 expert consensus document stating that the standard of care is an overnight stay following PCI (Catheter Cardiovasc Interv. 2009 Jun 1;73[7]:847-58), Dr. Cordoba Soriano observed.
He reported having no financial conflicts regarding the registry study, which was conducted with university research funds.
AT EUROPCR 2016
Key clinical point: Same-day discharge following uncomplicated elective transradial PCI is feasible and safe.
Major finding: The rates of major and minor complications in the 24 hours following PCI with same-day discharge were 0.18% and 1.8%, respectively.
Data source: A prospective observational registry study including 989 PCI patients at three Spanish university hospitals.
Disclosures: The presenter reported having no financial conflicts regarding the registry study, which was conducted with university research funds.
Cardiovascular disease, gender among predictors of nonresponse early in cellulitis treatment
Nonpharmacological factors including being female and having cardiovascular disease have an impact on early response among patients hospitalized with cellulitis, a single-center prospective study found.
“Cellulitis is usually caused by beta-hemolytic streptococci (BHS) susceptible to penicillin and other narrow-spectrum antibiotics,” researchers led by Trond Bruun, MD, of the department of clinical science at the University of Bergen, Norway, wrote in a study published online on July 11, 2016, in Clinical Infectious Diseases.
“However, there are significant treatment challenges, including overuse of broad-spectrum and intravenous antibiotics, difficulties regarding when to initiate rescue therapy and when to stop treatment, as well as frequent recurrences. Toxin effects and profound local inflammation, not necessarily corresponding to bacterial burden or antibiotic needs, may contribute to these problems.”
In an effort to better understand the clinical course, response dynamics, and associated factors involved with cellulitis care, the researchers evaluated 216 patients hospitalized with the condition at Haukeland University Hospital, Norway. They analyzed clinical and biochemical response data during the first 3 days of treatment in relation to baseline factors, antibiotic use, surgery, and outcome (Clin Infect Dis. 2016 Jul 11. pii: ciw463. [Epub ahead of print]).
The median age of the patients was 55 years and 57% had a lower extremity infection. After 1 day of treatment, the researchers found that 55% of evaluable patients (116 of 211) had cessation of lesion spread and 52% (109 of 211) had improvement of local inflammation. Local clinical response – defined as a combination of cessation of lesion spread and improvement of local inflammation – was observed in 39% of patients (82 of 212), while local clinical response or biochemical response was seen in 74% of cases (148 of 200).
Nonpharmacological factors found to predict nonresponse on treatment day 3 were cardiovascular disease (odds ratio, 2.83), female gender (OR, 2.09), and a higher body mass index (OR, 1.03). A shorter duration of symptoms and cellulitis other than typical erysipelas were also predictive of nonresponse on treatment day 3. On the other hand, baseline factors were not predictive of clinical failure assessed post treatment.
Among patients who received antibiotic treatment escalation within 2 days of starting treatment, most (90%) had nonresponse on treatment day 1, but only 5% had inappropriate initial therapy. Nonresponse on treatment day 3 was a predictor of treatment duration exceeding 14 days, but not of clinical failure.
“Overall, the study indicates that nonantibiotic factors with impact on early treatment response should be considered as an integrated part of the clinical management of cellulitis,” the researchers concluded. “This may improve individualization of treatment and reduce costs and unnecessary rescue therapy.”
The study was supported by a research grant from the department of clinical science at the University of Bergen. The researchers reported having no financial disclosures.
Nonpharmacological factors including being female and having cardiovascular disease have an impact on early response among patients hospitalized with cellulitis, a single-center prospective study found.
“Cellulitis is usually caused by beta-hemolytic streptococci (BHS) susceptible to penicillin and other narrow-spectrum antibiotics,” researchers led by Trond Bruun, MD, of the department of clinical science at the University of Bergen, Norway, wrote in a study published online on July 11, 2016, in Clinical Infectious Diseases.
“However, there are significant treatment challenges, including overuse of broad-spectrum and intravenous antibiotics, difficulties regarding when to initiate rescue therapy and when to stop treatment, as well as frequent recurrences. Toxin effects and profound local inflammation, not necessarily corresponding to bacterial burden or antibiotic needs, may contribute to these problems.”
In an effort to better understand the clinical course, response dynamics, and associated factors involved with cellulitis care, the researchers evaluated 216 patients hospitalized with the condition at Haukeland University Hospital, Norway. They analyzed clinical and biochemical response data during the first 3 days of treatment in relation to baseline factors, antibiotic use, surgery, and outcome (Clin Infect Dis. 2016 Jul 11. pii: ciw463. [Epub ahead of print]).
The median age of the patients was 55 years and 57% had a lower extremity infection. After 1 day of treatment, the researchers found that 55% of evaluable patients (116 of 211) had cessation of lesion spread and 52% (109 of 211) had improvement of local inflammation. Local clinical response – defined as a combination of cessation of lesion spread and improvement of local inflammation – was observed in 39% of patients (82 of 212), while local clinical response or biochemical response was seen in 74% of cases (148 of 200).
Nonpharmacological factors found to predict nonresponse on treatment day 3 were cardiovascular disease (odds ratio, 2.83), female gender (OR, 2.09), and a higher body mass index (OR, 1.03). A shorter duration of symptoms and cellulitis other than typical erysipelas were also predictive of nonresponse on treatment day 3. On the other hand, baseline factors were not predictive of clinical failure assessed post treatment.
Among patients who received antibiotic treatment escalation within 2 days of starting treatment, most (90%) had nonresponse on treatment day 1, but only 5% had inappropriate initial therapy. Nonresponse on treatment day 3 was a predictor of treatment duration exceeding 14 days, but not of clinical failure.
“Overall, the study indicates that nonantibiotic factors with impact on early treatment response should be considered as an integrated part of the clinical management of cellulitis,” the researchers concluded. “This may improve individualization of treatment and reduce costs and unnecessary rescue therapy.”
The study was supported by a research grant from the department of clinical science at the University of Bergen. The researchers reported having no financial disclosures.
Nonpharmacological factors including being female and having cardiovascular disease have an impact on early response among patients hospitalized with cellulitis, a single-center prospective study found.
“Cellulitis is usually caused by beta-hemolytic streptococci (BHS) susceptible to penicillin and other narrow-spectrum antibiotics,” researchers led by Trond Bruun, MD, of the department of clinical science at the University of Bergen, Norway, wrote in a study published online on July 11, 2016, in Clinical Infectious Diseases.
“However, there are significant treatment challenges, including overuse of broad-spectrum and intravenous antibiotics, difficulties regarding when to initiate rescue therapy and when to stop treatment, as well as frequent recurrences. Toxin effects and profound local inflammation, not necessarily corresponding to bacterial burden or antibiotic needs, may contribute to these problems.”
In an effort to better understand the clinical course, response dynamics, and associated factors involved with cellulitis care, the researchers evaluated 216 patients hospitalized with the condition at Haukeland University Hospital, Norway. They analyzed clinical and biochemical response data during the first 3 days of treatment in relation to baseline factors, antibiotic use, surgery, and outcome (Clin Infect Dis. 2016 Jul 11. pii: ciw463. [Epub ahead of print]).
The median age of the patients was 55 years and 57% had a lower extremity infection. After 1 day of treatment, the researchers found that 55% of evaluable patients (116 of 211) had cessation of lesion spread and 52% (109 of 211) had improvement of local inflammation. Local clinical response – defined as a combination of cessation of lesion spread and improvement of local inflammation – was observed in 39% of patients (82 of 212), while local clinical response or biochemical response was seen in 74% of cases (148 of 200).
Nonpharmacological factors found to predict nonresponse on treatment day 3 were cardiovascular disease (odds ratio, 2.83), female gender (OR, 2.09), and a higher body mass index (OR, 1.03). A shorter duration of symptoms and cellulitis other than typical erysipelas were also predictive of nonresponse on treatment day 3. On the other hand, baseline factors were not predictive of clinical failure assessed post treatment.
Among patients who received antibiotic treatment escalation within 2 days of starting treatment, most (90%) had nonresponse on treatment day 1, but only 5% had inappropriate initial therapy. Nonresponse on treatment day 3 was a predictor of treatment duration exceeding 14 days, but not of clinical failure.
“Overall, the study indicates that nonantibiotic factors with impact on early treatment response should be considered as an integrated part of the clinical management of cellulitis,” the researchers concluded. “This may improve individualization of treatment and reduce costs and unnecessary rescue therapy.”
The study was supported by a research grant from the department of clinical science at the University of Bergen. The researchers reported having no financial disclosures.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Nonpharmacological factors affect early response dynamics in patients hospitalized with cellulitis.
Major finding: Nonpharmacological factors found to predict nonresponse on treatment day 3 were female gender (OR 2.09), cardiovascular disease (OR 2.83), and higher body mass index (OR 1.03).
Data source: A prospective study of 216 patients hospitalized with cellulitis at a university hospital in Norway.
Disclosures: The study was supported by a research grant from the department of clinical science at the University of Bergen. The researchers reported having no financial disclosures.
Clindamycin confers no extra benefit for kids with SSSS
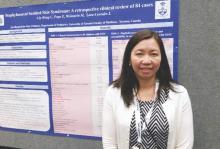
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
AT THE SPD ANNUAL MEETING
Key clinical point: Clindamycin did not benefit hospitalized children with staphylococcal scalded skin syndrome (SSSS).
Major finding: Clindamycin conferred no benefit in length of hospital stay compared with non-antitoxin antibiotics for SSSS (P = .63).
Data source: A retrospective chart review of 84 pediatric patients meeting SSSS criteria at a single children’s hospital.
Disclosures: Dr. Liy-Wong and her colleagues reported no external sources of funding, and no relevant disclosures.
Enhanced recovery protocol for colectomy patients reduced hospital stay
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A multihospital enhanced recovery process for colectomy patients decreased length of stay and morbidity.
Major finding: After implementation of an enhanced recovery protocol in colectomy patients, the average hospital length of stay decreased by 1.2 days (from a mean of 6.6 days among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01).
Data source: An analysis of 2,523 colectomies performed prior to implementation of the Enhanced Recovery in NSQIP (ERIN) Pilot process and 823 colectomies performed after implementation of the process.
Disclosures: Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
Malpractice cases serve to warn about careful use of EHRs
Buy our EHR. Come to a dinner and see our EHR. Our EHR is the best.
I hear that a lot, but am not rushing out to get one. Yes, I have an EHR, but it’s one I designed myself. It works very well for my dinky little practice, and I’m happy with it.
I get notes from practices that use commercial EHRs all the time. They’re usually a pile of gobbledygook, mixing labs, vital signs, medication lists, and ICD-10 codes that tell you absolutely nothing about the patient or the physician’s thought process.
Recently, while reviewing malpractice cases, I saw some where I thought that the EHR was contributing to the problem. Medication lists that showed everything a patient had ever taken, without showing when some were discontinued. Prescribing lists that allowed you to enter only certain doses or schedules, therefore blocking the physician from tailoring them to a specific person’s needs. Physical exam forms that allowed only positive or negative answers, with nowhere to comment on unusual findings.
Of course, I’m just one person, so I thought “maybe it’s just me.” After all, a lot of practices out there use EHRs.
But apparently I’m not the only one. A recent report by one of the nation’s largest doctor-owned malpractice companies found that EHRs may increase the risks of liability and medical errors. In 2013, The Doctor’s Company found 28 closed claims where the EHR contributed, and 26 in just the first half of 2014.
These include both technological problems with the systems and human error in their use. Troubles included erroneous medication dose and schedules, diagnosis-related errors, and the sadly common pitfall of cutting and pasting previous notes without modification.
Medicine has always been, and will always be, a thinking profession, and trying to have computers take part of this job off of us is never good. EHRs, while they have advantages in convenience and space savings, are as imperfect as those who write them.
Patients are not one-size-fits-all, and individual treatments have to be customized in ways that current systems often don’t recognize, sometimes with sad consequences for all involved.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Buy our EHR. Come to a dinner and see our EHR. Our EHR is the best.
I hear that a lot, but am not rushing out to get one. Yes, I have an EHR, but it’s one I designed myself. It works very well for my dinky little practice, and I’m happy with it.
I get notes from practices that use commercial EHRs all the time. They’re usually a pile of gobbledygook, mixing labs, vital signs, medication lists, and ICD-10 codes that tell you absolutely nothing about the patient or the physician’s thought process.
Recently, while reviewing malpractice cases, I saw some where I thought that the EHR was contributing to the problem. Medication lists that showed everything a patient had ever taken, without showing when some were discontinued. Prescribing lists that allowed you to enter only certain doses or schedules, therefore blocking the physician from tailoring them to a specific person’s needs. Physical exam forms that allowed only positive or negative answers, with nowhere to comment on unusual findings.
Of course, I’m just one person, so I thought “maybe it’s just me.” After all, a lot of practices out there use EHRs.
But apparently I’m not the only one. A recent report by one of the nation’s largest doctor-owned malpractice companies found that EHRs may increase the risks of liability and medical errors. In 2013, The Doctor’s Company found 28 closed claims where the EHR contributed, and 26 in just the first half of 2014.
These include both technological problems with the systems and human error in their use. Troubles included erroneous medication dose and schedules, diagnosis-related errors, and the sadly common pitfall of cutting and pasting previous notes without modification.
Medicine has always been, and will always be, a thinking profession, and trying to have computers take part of this job off of us is never good. EHRs, while they have advantages in convenience and space savings, are as imperfect as those who write them.
Patients are not one-size-fits-all, and individual treatments have to be customized in ways that current systems often don’t recognize, sometimes with sad consequences for all involved.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Buy our EHR. Come to a dinner and see our EHR. Our EHR is the best.
I hear that a lot, but am not rushing out to get one. Yes, I have an EHR, but it’s one I designed myself. It works very well for my dinky little practice, and I’m happy with it.
I get notes from practices that use commercial EHRs all the time. They’re usually a pile of gobbledygook, mixing labs, vital signs, medication lists, and ICD-10 codes that tell you absolutely nothing about the patient or the physician’s thought process.
Recently, while reviewing malpractice cases, I saw some where I thought that the EHR was contributing to the problem. Medication lists that showed everything a patient had ever taken, without showing when some were discontinued. Prescribing lists that allowed you to enter only certain doses or schedules, therefore blocking the physician from tailoring them to a specific person’s needs. Physical exam forms that allowed only positive or negative answers, with nowhere to comment on unusual findings.
Of course, I’m just one person, so I thought “maybe it’s just me.” After all, a lot of practices out there use EHRs.
But apparently I’m not the only one. A recent report by one of the nation’s largest doctor-owned malpractice companies found that EHRs may increase the risks of liability and medical errors. In 2013, The Doctor’s Company found 28 closed claims where the EHR contributed, and 26 in just the first half of 2014.
These include both technological problems with the systems and human error in their use. Troubles included erroneous medication dose and schedules, diagnosis-related errors, and the sadly common pitfall of cutting and pasting previous notes without modification.
Medicine has always been, and will always be, a thinking profession, and trying to have computers take part of this job off of us is never good. EHRs, while they have advantages in convenience and space savings, are as imperfect as those who write them.
Patients are not one-size-fits-all, and individual treatments have to be customized in ways that current systems often don’t recognize, sometimes with sad consequences for all involved.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Sickle cell trait raises exertional rhabdomyolysis risk
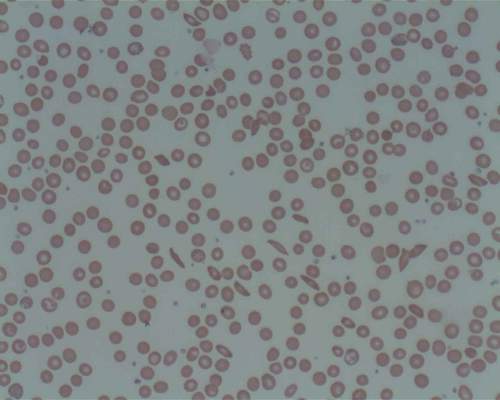
Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers, “a population that is known to engage consistently in regular and strenuous exercise while protected by exertional-injury precautions,” investigators reported. The study was published online Aug. 4 in the New England Journal of Medicine.
A number of high-profile deaths among athletes and military personnel involving exertional rhabdomyolysis have been attributed to sickle cell trait. The National Collegiate Athletic Association, the U.S. Air Force, and the U.S. Navy all require universal screening for sickle cell trait.
“However, concerns have been raised by the American Society of Hematology and other professional organizations about the possibility of stigmatization and discrimination resulting from the mandated screening for sickle cell trait,” which predominantly affects people of African descent and some of Hispanic ancestry, but usually not whites, wrote D. Alan Nelson, PhD, of Stanford (Calif.) University, and his associates.
“These concerns warrant consideration, especially given the absence of published evidence that such screening is effective in preventing exertion-related events,” added the researchers.
The U.S. Army primarily screens for sickle cell trait among personnel deployed for combat and certain specialists whose work at high altitudes puts them at risk. To study a large enough population to generate accurate data about this rare blood abnormality, the investigators analyzed data for 47,944 black soldiers who had been tested for sickle cell trait and who served on active duty during a recent 3-year period.
The researchers assessed all inpatient and outpatient health care visits at military and civilian facilities. There were 391 exertional rhabdomyolysis events and 96 deaths from all causes during 1.61 million person-months of observation. A total of 7.4% of the study cohort carried sickle cell trait. These participants were similar to noncarriers in demographic characteristics and health predictors.
Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99), and there also was no difference between carriers and noncarriers in either battle-related or non–battle-related mortality rates.
However, sickle cell trait was associated with a 54% greater risk of exertional rhabdomyolysis (HR, 1.54), Dr. Nelson and his associates noted (N Engl J Med. 2016 Aug 4. doi: 10.1056/NEJMoa1516257).
It is important to note that factors other than sickle cell trait raised the risk of exertional rhabdomyolysis to a similar or even greater degree, including obesity (HR, 1.39) and tobacco use (HR, 1.54). Recent use of antipsychotic medication tripled the risk for exertional rhabdomyolysis (HR, 3.02), and statin use nearly tripled it (HR, 2.89).
“These findings are compelling because case reports dominate the relevant literature and emphasize the presence of sickle cell trait as a risk factor for adverse outcomes, including exertional rhabdomyolysis and sudden death,” the researchers wrote. “A large longitudinal study involving a population fully tested for sickle cell trait that has formally investigated [these outcomes] while also examining other known major risk factors, such as medications, has been lacking.”
The study found that women were at much lower risk for exertional rhabdomyolysis than were men (HR, 0.51), and that risk increased with increasing age, so that soldiers aged 36 years and older had a 57% greater risk compared with those in the youngest age group.
The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers, “a population that is known to engage consistently in regular and strenuous exercise while protected by exertional-injury precautions,” investigators reported. The study was published online Aug. 4 in the New England Journal of Medicine.
A number of high-profile deaths among athletes and military personnel involving exertional rhabdomyolysis have been attributed to sickle cell trait. The National Collegiate Athletic Association, the U.S. Air Force, and the U.S. Navy all require universal screening for sickle cell trait.
“However, concerns have been raised by the American Society of Hematology and other professional organizations about the possibility of stigmatization and discrimination resulting from the mandated screening for sickle cell trait,” which predominantly affects people of African descent and some of Hispanic ancestry, but usually not whites, wrote D. Alan Nelson, PhD, of Stanford (Calif.) University, and his associates.
“These concerns warrant consideration, especially given the absence of published evidence that such screening is effective in preventing exertion-related events,” added the researchers.
The U.S. Army primarily screens for sickle cell trait among personnel deployed for combat and certain specialists whose work at high altitudes puts them at risk. To study a large enough population to generate accurate data about this rare blood abnormality, the investigators analyzed data for 47,944 black soldiers who had been tested for sickle cell trait and who served on active duty during a recent 3-year period.
The researchers assessed all inpatient and outpatient health care visits at military and civilian facilities. There were 391 exertional rhabdomyolysis events and 96 deaths from all causes during 1.61 million person-months of observation. A total of 7.4% of the study cohort carried sickle cell trait. These participants were similar to noncarriers in demographic characteristics and health predictors.
Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99), and there also was no difference between carriers and noncarriers in either battle-related or non–battle-related mortality rates.
However, sickle cell trait was associated with a 54% greater risk of exertional rhabdomyolysis (HR, 1.54), Dr. Nelson and his associates noted (N Engl J Med. 2016 Aug 4. doi: 10.1056/NEJMoa1516257).
It is important to note that factors other than sickle cell trait raised the risk of exertional rhabdomyolysis to a similar or even greater degree, including obesity (HR, 1.39) and tobacco use (HR, 1.54). Recent use of antipsychotic medication tripled the risk for exertional rhabdomyolysis (HR, 3.02), and statin use nearly tripled it (HR, 2.89).
“These findings are compelling because case reports dominate the relevant literature and emphasize the presence of sickle cell trait as a risk factor for adverse outcomes, including exertional rhabdomyolysis and sudden death,” the researchers wrote. “A large longitudinal study involving a population fully tested for sickle cell trait that has formally investigated [these outcomes] while also examining other known major risk factors, such as medications, has been lacking.”
The study found that women were at much lower risk for exertional rhabdomyolysis than were men (HR, 0.51), and that risk increased with increasing age, so that soldiers aged 36 years and older had a 57% greater risk compared with those in the youngest age group.
The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers, “a population that is known to engage consistently in regular and strenuous exercise while protected by exertional-injury precautions,” investigators reported. The study was published online Aug. 4 in the New England Journal of Medicine.
A number of high-profile deaths among athletes and military personnel involving exertional rhabdomyolysis have been attributed to sickle cell trait. The National Collegiate Athletic Association, the U.S. Air Force, and the U.S. Navy all require universal screening for sickle cell trait.
“However, concerns have been raised by the American Society of Hematology and other professional organizations about the possibility of stigmatization and discrimination resulting from the mandated screening for sickle cell trait,” which predominantly affects people of African descent and some of Hispanic ancestry, but usually not whites, wrote D. Alan Nelson, PhD, of Stanford (Calif.) University, and his associates.
“These concerns warrant consideration, especially given the absence of published evidence that such screening is effective in preventing exertion-related events,” added the researchers.
The U.S. Army primarily screens for sickle cell trait among personnel deployed for combat and certain specialists whose work at high altitudes puts them at risk. To study a large enough population to generate accurate data about this rare blood abnormality, the investigators analyzed data for 47,944 black soldiers who had been tested for sickle cell trait and who served on active duty during a recent 3-year period.
The researchers assessed all inpatient and outpatient health care visits at military and civilian facilities. There were 391 exertional rhabdomyolysis events and 96 deaths from all causes during 1.61 million person-months of observation. A total of 7.4% of the study cohort carried sickle cell trait. These participants were similar to noncarriers in demographic characteristics and health predictors.
Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99), and there also was no difference between carriers and noncarriers in either battle-related or non–battle-related mortality rates.
However, sickle cell trait was associated with a 54% greater risk of exertional rhabdomyolysis (HR, 1.54), Dr. Nelson and his associates noted (N Engl J Med. 2016 Aug 4. doi: 10.1056/NEJMoa1516257).
It is important to note that factors other than sickle cell trait raised the risk of exertional rhabdomyolysis to a similar or even greater degree, including obesity (HR, 1.39) and tobacco use (HR, 1.54). Recent use of antipsychotic medication tripled the risk for exertional rhabdomyolysis (HR, 3.02), and statin use nearly tripled it (HR, 2.89).
“These findings are compelling because case reports dominate the relevant literature and emphasize the presence of sickle cell trait as a risk factor for adverse outcomes, including exertional rhabdomyolysis and sudden death,” the researchers wrote. “A large longitudinal study involving a population fully tested for sickle cell trait that has formally investigated [these outcomes] while also examining other known major risk factors, such as medications, has been lacking.”
The study found that women were at much lower risk for exertional rhabdomyolysis than were men (HR, 0.51), and that risk increased with increasing age, so that soldiers aged 36 years and older had a 57% greater risk compared with those in the youngest age group.
The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers.
Major finding: Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99) but did have a higher risk of exertional rhabdomyolysis (HR, 1.54).
Data source: A retrospective longitudinal cohort study involving 47,944 black U.S. soldiers on active duty during 2011-2014.
Disclosures: The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
MCR-1 gene a growing concern for antibiotic resistance
The MCR-1 gene is quickly emerging as a powerful roadblock in the fight against antibiotic-resistant bacteria, according to experts from the Centers for Disease Control and Prevention.
Alex J. Kallen, MD, of the CDC in Atlanta, said in an Aug. 2 webinar – cohosted by CDC and the Partnership for Quality Care – that the CDC is closely monitoring the emergence of antibiotic resistant bacteria in the United States. The prevailing message of Dr. Kallen and his CDC colleague Arjun Srinivasan, MD was that the importance of the MCR-1 gene should not be underestimated.
First discovered in a human patient last year, the presence of the MCR-1 gene makes bacteria resistant to colistin, an antibiotic used often as a last resort to “treat patients with multidrug-resistant infections,” according to the CDC. Because the MCR-1 gene exists on a plasmid, or a small piece of DNA, it is easily transferable among bacteria, making it a problem for health care providers treating a patient infected with bacteria that has the gene.
“As of this year, all state and some local health departments will be funded to respond to [antibiotic resistance] threats, including emerging threats like [MCR-1], within their jurisdiction,” Dr. Kallen said. This funding could be used to support technical assistance, contact investigations, and laboratory testing, among other things.
In order to help prevent the spread of MCR-1 and mitigate cases of novel antimicrobial resistance, health care providers and facilities should institute recommended intensive care precautions as soon as resistance is identified, along with alerting their local public health office. Isolates should be saved, and prospective and retrospective surveillance should be implemented to “identify isolates with similar phenotypes.” If an infected patient is being transferred to another facility, that facility should be notified ahead of time about the patient and what protocols to follow.
Because antibiotic-resistant organisms do not spread through the air like influenza, the risk that these organisms pose to health care workers is relatively low, Dr. Srinivasan explained. However, he stressed that a multifaceted, team-based approach to antibiotic stewardship and decontamination of health care facilities is absolutely necessary to achieve the best results for both patients and staff.
“We are now beginning to recognize that the contamination of surfaces and items in our health care environment is increasingly a problem in the transmission of these drug-resistant organisms,” Dr. Srinivasan explained. He said that, given the complexity of a typical health care environment, such as a hospital room or operating theater, it’s perhaps not so surprising that keeping everything clean is not the top priority.
In addition to making sure hospital rooms and other areas are properly cleaned, simple things like washing hands and keeping surfaces clean are just as important. Dr. Srinivasan pointed to a 2006 study by Philip C. Carling, MD, and his associates which showed that educational interventions can lead to substantial increases in hygiene and cleanliness, and that training of new staff is also important. Furthermore, giving staff enough time to properly clean rooms could significantly contribute to curtailing MCR-1 bacteria from spreading, he said.
“The other thing to keep in mind is that if we lose effective therapy, if we lose antibiotic therapy, the infections that are currently very treatable and are seldom deadly could again become very, very serious threats to life,” Dr. Srinivasan warned, specifically citing Escherichia coli, which is the leading cause of urinary tract infections. If community strains of E.coli become resistant to typical antibiotic treatment, these cases could become “difficult, if not impossible to treat.”
According to data shared by Dr. Srinivasan, in 2013 there were 2,049,422 illnesses in the United States attributed to antibiotic resistance and 23,000 fatalities.
The MCR-1 gene is quickly emerging as a powerful roadblock in the fight against antibiotic-resistant bacteria, according to experts from the Centers for Disease Control and Prevention.
Alex J. Kallen, MD, of the CDC in Atlanta, said in an Aug. 2 webinar – cohosted by CDC and the Partnership for Quality Care – that the CDC is closely monitoring the emergence of antibiotic resistant bacteria in the United States. The prevailing message of Dr. Kallen and his CDC colleague Arjun Srinivasan, MD was that the importance of the MCR-1 gene should not be underestimated.
First discovered in a human patient last year, the presence of the MCR-1 gene makes bacteria resistant to colistin, an antibiotic used often as a last resort to “treat patients with multidrug-resistant infections,” according to the CDC. Because the MCR-1 gene exists on a plasmid, or a small piece of DNA, it is easily transferable among bacteria, making it a problem for health care providers treating a patient infected with bacteria that has the gene.
“As of this year, all state and some local health departments will be funded to respond to [antibiotic resistance] threats, including emerging threats like [MCR-1], within their jurisdiction,” Dr. Kallen said. This funding could be used to support technical assistance, contact investigations, and laboratory testing, among other things.
In order to help prevent the spread of MCR-1 and mitigate cases of novel antimicrobial resistance, health care providers and facilities should institute recommended intensive care precautions as soon as resistance is identified, along with alerting their local public health office. Isolates should be saved, and prospective and retrospective surveillance should be implemented to “identify isolates with similar phenotypes.” If an infected patient is being transferred to another facility, that facility should be notified ahead of time about the patient and what protocols to follow.
Because antibiotic-resistant organisms do not spread through the air like influenza, the risk that these organisms pose to health care workers is relatively low, Dr. Srinivasan explained. However, he stressed that a multifaceted, team-based approach to antibiotic stewardship and decontamination of health care facilities is absolutely necessary to achieve the best results for both patients and staff.
“We are now beginning to recognize that the contamination of surfaces and items in our health care environment is increasingly a problem in the transmission of these drug-resistant organisms,” Dr. Srinivasan explained. He said that, given the complexity of a typical health care environment, such as a hospital room or operating theater, it’s perhaps not so surprising that keeping everything clean is not the top priority.
In addition to making sure hospital rooms and other areas are properly cleaned, simple things like washing hands and keeping surfaces clean are just as important. Dr. Srinivasan pointed to a 2006 study by Philip C. Carling, MD, and his associates which showed that educational interventions can lead to substantial increases in hygiene and cleanliness, and that training of new staff is also important. Furthermore, giving staff enough time to properly clean rooms could significantly contribute to curtailing MCR-1 bacteria from spreading, he said.
“The other thing to keep in mind is that if we lose effective therapy, if we lose antibiotic therapy, the infections that are currently very treatable and are seldom deadly could again become very, very serious threats to life,” Dr. Srinivasan warned, specifically citing Escherichia coli, which is the leading cause of urinary tract infections. If community strains of E.coli become resistant to typical antibiotic treatment, these cases could become “difficult, if not impossible to treat.”
According to data shared by Dr. Srinivasan, in 2013 there were 2,049,422 illnesses in the United States attributed to antibiotic resistance and 23,000 fatalities.
The MCR-1 gene is quickly emerging as a powerful roadblock in the fight against antibiotic-resistant bacteria, according to experts from the Centers for Disease Control and Prevention.
Alex J. Kallen, MD, of the CDC in Atlanta, said in an Aug. 2 webinar – cohosted by CDC and the Partnership for Quality Care – that the CDC is closely monitoring the emergence of antibiotic resistant bacteria in the United States. The prevailing message of Dr. Kallen and his CDC colleague Arjun Srinivasan, MD was that the importance of the MCR-1 gene should not be underestimated.
First discovered in a human patient last year, the presence of the MCR-1 gene makes bacteria resistant to colistin, an antibiotic used often as a last resort to “treat patients with multidrug-resistant infections,” according to the CDC. Because the MCR-1 gene exists on a plasmid, or a small piece of DNA, it is easily transferable among bacteria, making it a problem for health care providers treating a patient infected with bacteria that has the gene.
“As of this year, all state and some local health departments will be funded to respond to [antibiotic resistance] threats, including emerging threats like [MCR-1], within their jurisdiction,” Dr. Kallen said. This funding could be used to support technical assistance, contact investigations, and laboratory testing, among other things.
In order to help prevent the spread of MCR-1 and mitigate cases of novel antimicrobial resistance, health care providers and facilities should institute recommended intensive care precautions as soon as resistance is identified, along with alerting their local public health office. Isolates should be saved, and prospective and retrospective surveillance should be implemented to “identify isolates with similar phenotypes.” If an infected patient is being transferred to another facility, that facility should be notified ahead of time about the patient and what protocols to follow.
Because antibiotic-resistant organisms do not spread through the air like influenza, the risk that these organisms pose to health care workers is relatively low, Dr. Srinivasan explained. However, he stressed that a multifaceted, team-based approach to antibiotic stewardship and decontamination of health care facilities is absolutely necessary to achieve the best results for both patients and staff.
“We are now beginning to recognize that the contamination of surfaces and items in our health care environment is increasingly a problem in the transmission of these drug-resistant organisms,” Dr. Srinivasan explained. He said that, given the complexity of a typical health care environment, such as a hospital room or operating theater, it’s perhaps not so surprising that keeping everything clean is not the top priority.
In addition to making sure hospital rooms and other areas are properly cleaned, simple things like washing hands and keeping surfaces clean are just as important. Dr. Srinivasan pointed to a 2006 study by Philip C. Carling, MD, and his associates which showed that educational interventions can lead to substantial increases in hygiene and cleanliness, and that training of new staff is also important. Furthermore, giving staff enough time to properly clean rooms could significantly contribute to curtailing MCR-1 bacteria from spreading, he said.
“The other thing to keep in mind is that if we lose effective therapy, if we lose antibiotic therapy, the infections that are currently very treatable and are seldom deadly could again become very, very serious threats to life,” Dr. Srinivasan warned, specifically citing Escherichia coli, which is the leading cause of urinary tract infections. If community strains of E.coli become resistant to typical antibiotic treatment, these cases could become “difficult, if not impossible to treat.”
According to data shared by Dr. Srinivasan, in 2013 there were 2,049,422 illnesses in the United States attributed to antibiotic resistance and 23,000 fatalities.
New HIV antiretroviral guidelines embrace PrEP, early ART
The International Antiviral Society–USA has updated its recommendations for the use of antiretroviral drugs to treat or to prevent HIV infection in adults.
In light of new evidence emerging since its 2014 report on antiretroviral drugs (ARVs), the International Antiviral Society–USA convened a panel of HIV experts to review data published in peer-reviewed journals, presented by regulatory agencies, or presented as conference abstracts at peer-reviewed scientific conferences that would change previous recommendations or ratings. The resulting recommendations were published online in the Journal of the American Medical Association. (JAMA. 2016;316[2]:191-210. doi:10.1001/jama.2016.8900)
The panel concluded that newer data support the “widely accepted” recommendation that antiretroviral therapy (ART) should be started in all individuals with HIV infection with detectable viremia regardless of CD4 cell count. They said optimal initial regimens for most patients should include two nucleoside reverse transcriptase inhibitors (NRTIs) plus an integrase strand transfer inhibitor (InSTI). The panel concluded that other effective regimens may include nonnucleoside reverse transcriptase inhibitors or boosted protease inhibitors with two NRTIs.
Also of note are the panel’s recommendations for certain special populations. The panel said HIV-infected pregnant women should initiate ART for their own health and to reduce the likelihood of HIV transmission to the infant. HIV-infected patients with hepatitis B virus (HBV) coinfection should initiate a recommended ART regimen that contains tenofovir disoproxil fumarate (TDF) or tenofovir alafenamide (TAF), lamivudine or emtricitabine, and a third component.
In addition, the panel said ART should be started within the first 2 weeks after diagnosis for most acute opportunistic infections, with the possible exception of acute cryptococcal meningitis, and ART should be started within the first 2 weeks of initiation of tuberculosis treatment for those with CD4 cell counts of 50/mcL or less and within the first 2-8 weeks for those with CD4 cell counts above 50/mcL.
For prevention of HIV infection, the panel concluded that preexposure prophylaxis (PrEP) should be considered for anyone from a population whose HIV incidence is at least 2% per year, or for HIV-seronegative partners of HIV-infected persons who do not have viral suppression. Daily tenofovir disoproxil fumarate/emtricitabine is recommended for use as preexposure prophylaxis to prevent HIV infection in persons at high risk. Also, postexposure prophylaxis should be started as soon as possible after exposure.
For the complete list of ARV recommendations, see the report in JAMA (doi:10.1001/jama.2016.8900).
On Twitter @richpizzi
The International Antiviral Society–USA has updated its recommendations for the use of antiretroviral drugs to treat or to prevent HIV infection in adults.
In light of new evidence emerging since its 2014 report on antiretroviral drugs (ARVs), the International Antiviral Society–USA convened a panel of HIV experts to review data published in peer-reviewed journals, presented by regulatory agencies, or presented as conference abstracts at peer-reviewed scientific conferences that would change previous recommendations or ratings. The resulting recommendations were published online in the Journal of the American Medical Association. (JAMA. 2016;316[2]:191-210. doi:10.1001/jama.2016.8900)
The panel concluded that newer data support the “widely accepted” recommendation that antiretroviral therapy (ART) should be started in all individuals with HIV infection with detectable viremia regardless of CD4 cell count. They said optimal initial regimens for most patients should include two nucleoside reverse transcriptase inhibitors (NRTIs) plus an integrase strand transfer inhibitor (InSTI). The panel concluded that other effective regimens may include nonnucleoside reverse transcriptase inhibitors or boosted protease inhibitors with two NRTIs.
Also of note are the panel’s recommendations for certain special populations. The panel said HIV-infected pregnant women should initiate ART for their own health and to reduce the likelihood of HIV transmission to the infant. HIV-infected patients with hepatitis B virus (HBV) coinfection should initiate a recommended ART regimen that contains tenofovir disoproxil fumarate (TDF) or tenofovir alafenamide (TAF), lamivudine or emtricitabine, and a third component.
In addition, the panel said ART should be started within the first 2 weeks after diagnosis for most acute opportunistic infections, with the possible exception of acute cryptococcal meningitis, and ART should be started within the first 2 weeks of initiation of tuberculosis treatment for those with CD4 cell counts of 50/mcL or less and within the first 2-8 weeks for those with CD4 cell counts above 50/mcL.
For prevention of HIV infection, the panel concluded that preexposure prophylaxis (PrEP) should be considered for anyone from a population whose HIV incidence is at least 2% per year, or for HIV-seronegative partners of HIV-infected persons who do not have viral suppression. Daily tenofovir disoproxil fumarate/emtricitabine is recommended for use as preexposure prophylaxis to prevent HIV infection in persons at high risk. Also, postexposure prophylaxis should be started as soon as possible after exposure.
For the complete list of ARV recommendations, see the report in JAMA (doi:10.1001/jama.2016.8900).
On Twitter @richpizzi
The International Antiviral Society–USA has updated its recommendations for the use of antiretroviral drugs to treat or to prevent HIV infection in adults.
In light of new evidence emerging since its 2014 report on antiretroviral drugs (ARVs), the International Antiviral Society–USA convened a panel of HIV experts to review data published in peer-reviewed journals, presented by regulatory agencies, or presented as conference abstracts at peer-reviewed scientific conferences that would change previous recommendations or ratings. The resulting recommendations were published online in the Journal of the American Medical Association. (JAMA. 2016;316[2]:191-210. doi:10.1001/jama.2016.8900)
The panel concluded that newer data support the “widely accepted” recommendation that antiretroviral therapy (ART) should be started in all individuals with HIV infection with detectable viremia regardless of CD4 cell count. They said optimal initial regimens for most patients should include two nucleoside reverse transcriptase inhibitors (NRTIs) plus an integrase strand transfer inhibitor (InSTI). The panel concluded that other effective regimens may include nonnucleoside reverse transcriptase inhibitors or boosted protease inhibitors with two NRTIs.
Also of note are the panel’s recommendations for certain special populations. The panel said HIV-infected pregnant women should initiate ART for their own health and to reduce the likelihood of HIV transmission to the infant. HIV-infected patients with hepatitis B virus (HBV) coinfection should initiate a recommended ART regimen that contains tenofovir disoproxil fumarate (TDF) or tenofovir alafenamide (TAF), lamivudine or emtricitabine, and a third component.
In addition, the panel said ART should be started within the first 2 weeks after diagnosis for most acute opportunistic infections, with the possible exception of acute cryptococcal meningitis, and ART should be started within the first 2 weeks of initiation of tuberculosis treatment for those with CD4 cell counts of 50/mcL or less and within the first 2-8 weeks for those with CD4 cell counts above 50/mcL.
For prevention of HIV infection, the panel concluded that preexposure prophylaxis (PrEP) should be considered for anyone from a population whose HIV incidence is at least 2% per year, or for HIV-seronegative partners of HIV-infected persons who do not have viral suppression. Daily tenofovir disoproxil fumarate/emtricitabine is recommended for use as preexposure prophylaxis to prevent HIV infection in persons at high risk. Also, postexposure prophylaxis should be started as soon as possible after exposure.
For the complete list of ARV recommendations, see the report in JAMA (doi:10.1001/jama.2016.8900).
On Twitter @richpizzi
FROM JAMA
Driving skills already affected with mild cognitive impairment
TORONTO – Patients with amnestic mild cognitive impairment made significantly more errors during a complex test of driving skills and showed altered brain activity while performing this test in a two-part study.
The findings are the first to show a correlation between physiologic brain activity and driving and suggest that patients with mild cognitive impairment (MCI) may already be experiencing potentially dangerous changes in their ability to operate a motor vehicle, Megan Hird said at the Alzheimer’s Association International Conference 2016.
“Driving is a highly complex behavior that requires the integration of cognitive, motor function, and perceptual abilities,” said Ms. Hird, a researcher at the University of Toronto. “Individuals with multidomain MCI can express memory, visuospatial, and executive function deficits” even before their less demanding activities of daily living are affected. Nevertheless, Ms. Hird said, “these deficits can affect someone’s ability to drive safely.”
The decision to hang up the car keys is always a tough one for patients with dementia, their families, and their physicians, and there are no guidelines in the United States or Canada to help in that decision. But Ms. Hird and her colleagues recently published a meta-analysis of driving studies in which patients with very mild Alzheimer’s were 10 times more likely to fail an on-road driving test than were cognitively healthy drivers (J Alz Dis. 2016;53[2]:713-29).
Nevertheless, both the American and Canadian Medical Associations state that a diagnosis of cognitive impairment is not sufficient to withdraw driving privileges, and no cognitive test is capable of determining driving ability.
Ms. Hird used a combination of a driving simulator and functional MRI to study driving skill and the neural correlates of that activity. There were two parts to the study. The first comprised 20 healthy controls and 24 amnestic MCI patients (11 with single-domain MCI and 13 with multidomain MCI). The driving tasks were routine right and left turns, plus left turns against traffic and left turns against traffic with auditory distraction.
Overall, those with MCI (both single- and multi-domain patients combined) committed significantly more risky driving errors than the control group (mean of 9 vs. 3). Risky errors were considered errors that could result in an imminent collision, crossing the center line into oncoming traffic, or crossing onto the sidewalk.
When the researchers examined the MCI groups separately, they determined that only those with multi-domain MCI performed significantly worse than did controls (mean of 14 vs. 2.7 errors). These errors were most often committed during the more complicated left turns. There were no significant between-group differences in routine right and left turns.
Differences in brain activation revealed
The second part comprised 32 patients: 16 with MCI and 16 age-matched, cognitively normal controls. These subjects undertook both the driving simulation and the functional MRI test.
On the uncomplicated right turns, there were no between-group differences in errors, Ms. Hird said. However, there were some differences in the way the subjects’ brains reacted to the task. “On the brain activation patterns, the healthy controls showed some negative activation in the temporal and occipital regions, areas that actually were activated in the patients. The patients also showed some increased signal in the posterior medial regions, compared with the healthy controls. Overall, however, the activation patterns looked quite similar between the two groups.”
The left turn into traffic task showed quite different results. “In the MCI group, there was more anterior activation. They also showed significantly higher activation than did the control group in the orbitofrontal, medial superior, and midfrontal cortex – all of which are involved in planning, higher-order attention, and cognitive control.”
Recognizing that there are demonstrable differences in brain activation that correlate with poor driving performance could spark the creation of an objective clinical measurement tool for determining driving status, Ms. Hird said.
“This is an important fundamental step in the development of a tool that is sensitive and specific for addressing the driving safety of these patients.”
During discussion after her presentation, she fielded a question from an Australian clinician, who said his country likewise has no objective measure of when driving is no longer safe for a dementia patient.
“We accept the fact that people do drive with some degree of cognitive impairment,” said the physician, who did not identify himself. “But there are regions where having a license is important for social engagement. And we know that social disengagement drives rapid progression of cognitive decline. I think there is a real tension here between the withdrawal of licensure and the preservation of social engagement.”
Ms. Hird agreed. “Obviously, many MCI patients do retain the ability to drive safely. But we need to achieve a balance between maintaining patient autonomy and the safety of the general public.”
Ms. Hird had no financial disclosures.
On Twitter @alz_gal
TORONTO – Patients with amnestic mild cognitive impairment made significantly more errors during a complex test of driving skills and showed altered brain activity while performing this test in a two-part study.
The findings are the first to show a correlation between physiologic brain activity and driving and suggest that patients with mild cognitive impairment (MCI) may already be experiencing potentially dangerous changes in their ability to operate a motor vehicle, Megan Hird said at the Alzheimer’s Association International Conference 2016.
“Driving is a highly complex behavior that requires the integration of cognitive, motor function, and perceptual abilities,” said Ms. Hird, a researcher at the University of Toronto. “Individuals with multidomain MCI can express memory, visuospatial, and executive function deficits” even before their less demanding activities of daily living are affected. Nevertheless, Ms. Hird said, “these deficits can affect someone’s ability to drive safely.”
The decision to hang up the car keys is always a tough one for patients with dementia, their families, and their physicians, and there are no guidelines in the United States or Canada to help in that decision. But Ms. Hird and her colleagues recently published a meta-analysis of driving studies in which patients with very mild Alzheimer’s were 10 times more likely to fail an on-road driving test than were cognitively healthy drivers (J Alz Dis. 2016;53[2]:713-29).
Nevertheless, both the American and Canadian Medical Associations state that a diagnosis of cognitive impairment is not sufficient to withdraw driving privileges, and no cognitive test is capable of determining driving ability.
Ms. Hird used a combination of a driving simulator and functional MRI to study driving skill and the neural correlates of that activity. There were two parts to the study. The first comprised 20 healthy controls and 24 amnestic MCI patients (11 with single-domain MCI and 13 with multidomain MCI). The driving tasks were routine right and left turns, plus left turns against traffic and left turns against traffic with auditory distraction.
Overall, those with MCI (both single- and multi-domain patients combined) committed significantly more risky driving errors than the control group (mean of 9 vs. 3). Risky errors were considered errors that could result in an imminent collision, crossing the center line into oncoming traffic, or crossing onto the sidewalk.
When the researchers examined the MCI groups separately, they determined that only those with multi-domain MCI performed significantly worse than did controls (mean of 14 vs. 2.7 errors). These errors were most often committed during the more complicated left turns. There were no significant between-group differences in routine right and left turns.
Differences in brain activation revealed
The second part comprised 32 patients: 16 with MCI and 16 age-matched, cognitively normal controls. These subjects undertook both the driving simulation and the functional MRI test.
On the uncomplicated right turns, there were no between-group differences in errors, Ms. Hird said. However, there were some differences in the way the subjects’ brains reacted to the task. “On the brain activation patterns, the healthy controls showed some negative activation in the temporal and occipital regions, areas that actually were activated in the patients. The patients also showed some increased signal in the posterior medial regions, compared with the healthy controls. Overall, however, the activation patterns looked quite similar between the two groups.”
The left turn into traffic task showed quite different results. “In the MCI group, there was more anterior activation. They also showed significantly higher activation than did the control group in the orbitofrontal, medial superior, and midfrontal cortex – all of which are involved in planning, higher-order attention, and cognitive control.”
Recognizing that there are demonstrable differences in brain activation that correlate with poor driving performance could spark the creation of an objective clinical measurement tool for determining driving status, Ms. Hird said.
“This is an important fundamental step in the development of a tool that is sensitive and specific for addressing the driving safety of these patients.”
During discussion after her presentation, she fielded a question from an Australian clinician, who said his country likewise has no objective measure of when driving is no longer safe for a dementia patient.
“We accept the fact that people do drive with some degree of cognitive impairment,” said the physician, who did not identify himself. “But there are regions where having a license is important for social engagement. And we know that social disengagement drives rapid progression of cognitive decline. I think there is a real tension here between the withdrawal of licensure and the preservation of social engagement.”
Ms. Hird agreed. “Obviously, many MCI patients do retain the ability to drive safely. But we need to achieve a balance between maintaining patient autonomy and the safety of the general public.”
Ms. Hird had no financial disclosures.
On Twitter @alz_gal
TORONTO – Patients with amnestic mild cognitive impairment made significantly more errors during a complex test of driving skills and showed altered brain activity while performing this test in a two-part study.
The findings are the first to show a correlation between physiologic brain activity and driving and suggest that patients with mild cognitive impairment (MCI) may already be experiencing potentially dangerous changes in their ability to operate a motor vehicle, Megan Hird said at the Alzheimer’s Association International Conference 2016.
“Driving is a highly complex behavior that requires the integration of cognitive, motor function, and perceptual abilities,” said Ms. Hird, a researcher at the University of Toronto. “Individuals with multidomain MCI can express memory, visuospatial, and executive function deficits” even before their less demanding activities of daily living are affected. Nevertheless, Ms. Hird said, “these deficits can affect someone’s ability to drive safely.”
The decision to hang up the car keys is always a tough one for patients with dementia, their families, and their physicians, and there are no guidelines in the United States or Canada to help in that decision. But Ms. Hird and her colleagues recently published a meta-analysis of driving studies in which patients with very mild Alzheimer’s were 10 times more likely to fail an on-road driving test than were cognitively healthy drivers (J Alz Dis. 2016;53[2]:713-29).
Nevertheless, both the American and Canadian Medical Associations state that a diagnosis of cognitive impairment is not sufficient to withdraw driving privileges, and no cognitive test is capable of determining driving ability.
Ms. Hird used a combination of a driving simulator and functional MRI to study driving skill and the neural correlates of that activity. There were two parts to the study. The first comprised 20 healthy controls and 24 amnestic MCI patients (11 with single-domain MCI and 13 with multidomain MCI). The driving tasks were routine right and left turns, plus left turns against traffic and left turns against traffic with auditory distraction.
Overall, those with MCI (both single- and multi-domain patients combined) committed significantly more risky driving errors than the control group (mean of 9 vs. 3). Risky errors were considered errors that could result in an imminent collision, crossing the center line into oncoming traffic, or crossing onto the sidewalk.
When the researchers examined the MCI groups separately, they determined that only those with multi-domain MCI performed significantly worse than did controls (mean of 14 vs. 2.7 errors). These errors were most often committed during the more complicated left turns. There were no significant between-group differences in routine right and left turns.
Differences in brain activation revealed
The second part comprised 32 patients: 16 with MCI and 16 age-matched, cognitively normal controls. These subjects undertook both the driving simulation and the functional MRI test.
On the uncomplicated right turns, there were no between-group differences in errors, Ms. Hird said. However, there were some differences in the way the subjects’ brains reacted to the task. “On the brain activation patterns, the healthy controls showed some negative activation in the temporal and occipital regions, areas that actually were activated in the patients. The patients also showed some increased signal in the posterior medial regions, compared with the healthy controls. Overall, however, the activation patterns looked quite similar between the two groups.”
The left turn into traffic task showed quite different results. “In the MCI group, there was more anterior activation. They also showed significantly higher activation than did the control group in the orbitofrontal, medial superior, and midfrontal cortex – all of which are involved in planning, higher-order attention, and cognitive control.”
Recognizing that there are demonstrable differences in brain activation that correlate with poor driving performance could spark the creation of an objective clinical measurement tool for determining driving status, Ms. Hird said.
“This is an important fundamental step in the development of a tool that is sensitive and specific for addressing the driving safety of these patients.”
During discussion after her presentation, she fielded a question from an Australian clinician, who said his country likewise has no objective measure of when driving is no longer safe for a dementia patient.
“We accept the fact that people do drive with some degree of cognitive impairment,” said the physician, who did not identify himself. “But there are regions where having a license is important for social engagement. And we know that social disengagement drives rapid progression of cognitive decline. I think there is a real tension here between the withdrawal of licensure and the preservation of social engagement.”
Ms. Hird agreed. “Obviously, many MCI patients do retain the ability to drive safely. But we need to achieve a balance between maintaining patient autonomy and the safety of the general public.”
Ms. Hird had no financial disclosures.
On Twitter @alz_gal
AT AAIC 2016
Key clinical point: Patients with mild cognitive impairment may already be unsafe drivers.
Major finding: Patients with multidomain MCI made significantly more driving errors than did healthy controls (mean of 14 vs. 2.7 errors).
Data source: The studies comprised 40 patients with MCI and 36 age-matched cognitively healthy controls.
Disclosures: Megan Hird had no financial disclosures.
FDA grants fast track status to volixibat
The Food and Drug Administration has granted fast track status to volixibat, an investigational treatment manufactured by Shire.
“The FDA’s fast track is a process designed to facilitate the development, and expedite the review, of drugs to treat serious conditions and fill an unmet medical need,” the Dublin-based pharmaceutical company explained in a statement. “However, it does not guarantee that the FDA will ultimately approve [volixibat] for NASH [nonalcoholic steatohepatitis] or the timing of any such approval.”
Volixibat, also known as SHP626, is meant to treat NASH with liver fibrosis in adult patients via an apical sodium-dependent bile acid transporter inhibitor, which is a protein that recycles bile acids from the intestine and into the liver. This orally administered, once-daily treatment would be the first ever treatment available for NASH.
“This fast track designation is further recognition of the critical need to develop new, effective therapeutic options for patients with this serious condition,” said Philip J. Vickers, PhD, head of research and development for Shire, in a statement.
Preclinical and phase I studies have already been completed, the results of which contributed to the FDA granting volixibat fast track status. A randomized, placebo-controlled, double-blind phase II trial is set to get underway shortly at centers in the United States, Canada, and the United Kingdom, which will examine safety, tolerability, and efficacy of a three-dose volixibat regimen administered over the course of 48 weeks.
The Food and Drug Administration has granted fast track status to volixibat, an investigational treatment manufactured by Shire.
“The FDA’s fast track is a process designed to facilitate the development, and expedite the review, of drugs to treat serious conditions and fill an unmet medical need,” the Dublin-based pharmaceutical company explained in a statement. “However, it does not guarantee that the FDA will ultimately approve [volixibat] for NASH [nonalcoholic steatohepatitis] or the timing of any such approval.”
Volixibat, also known as SHP626, is meant to treat NASH with liver fibrosis in adult patients via an apical sodium-dependent bile acid transporter inhibitor, which is a protein that recycles bile acids from the intestine and into the liver. This orally administered, once-daily treatment would be the first ever treatment available for NASH.
“This fast track designation is further recognition of the critical need to develop new, effective therapeutic options for patients with this serious condition,” said Philip J. Vickers, PhD, head of research and development for Shire, in a statement.
Preclinical and phase I studies have already been completed, the results of which contributed to the FDA granting volixibat fast track status. A randomized, placebo-controlled, double-blind phase II trial is set to get underway shortly at centers in the United States, Canada, and the United Kingdom, which will examine safety, tolerability, and efficacy of a three-dose volixibat regimen administered over the course of 48 weeks.
The Food and Drug Administration has granted fast track status to volixibat, an investigational treatment manufactured by Shire.
“The FDA’s fast track is a process designed to facilitate the development, and expedite the review, of drugs to treat serious conditions and fill an unmet medical need,” the Dublin-based pharmaceutical company explained in a statement. “However, it does not guarantee that the FDA will ultimately approve [volixibat] for NASH [nonalcoholic steatohepatitis] or the timing of any such approval.”
Volixibat, also known as SHP626, is meant to treat NASH with liver fibrosis in adult patients via an apical sodium-dependent bile acid transporter inhibitor, which is a protein that recycles bile acids from the intestine and into the liver. This orally administered, once-daily treatment would be the first ever treatment available for NASH.
“This fast track designation is further recognition of the critical need to develop new, effective therapeutic options for patients with this serious condition,” said Philip J. Vickers, PhD, head of research and development for Shire, in a statement.
Preclinical and phase I studies have already been completed, the results of which contributed to the FDA granting volixibat fast track status. A randomized, placebo-controlled, double-blind phase II trial is set to get underway shortly at centers in the United States, Canada, and the United Kingdom, which will examine safety, tolerability, and efficacy of a three-dose volixibat regimen administered over the course of 48 weeks.