User login
News and Views that Matter to Physicians
Medicare Trust Fund projected to run dry in 2028
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
Dos and don’ts of dealing with disruptive behavior
CHICAGO – Dealing with disruptive behavior by staff and colleagues isn’t just about knowing what to do – it’s also about knowing what not to do.
Often, mishandling disruptive behavior can make matters worse and lead to further conflict among physicians and employees, health law experts warn. At a conference held by the American Bar Association, attorneys offered guidance on the dos and don’ts of disruptive behavior management.
Don’t discipline for the wrong reasons
Know what disruptive behavior is not, advised Margo S. Struthers, a Minneapolis-based health law attorney. Criticism offered in good faith with the aim of improving patient care should not be considered disruptive, she said.
“This is a problem that comes up a lot because, often, there is some element of criticism that is offered by the supposed disruptive physician, which may or may not be justified, may or may have been done in good faith, and may or may not have been in a respectful manner.”
An isolated incident of behavior that is not reflective of a pattern of inappropriate, deep-seated, and habitual behavior should not be construed as disruptive, Ms. Struthers added. In addition, disruptive behavior is not respectful disagreement with leadership, presentation of controversial ideas, or the respectful complaining about processes that endanger patient care.
Do address behavior that is truly disruptive
According to the American Medical Association, disruptive behavior is defined as personal conduct, whether verbal or physical, that negatively affects or that potentially may negatively affect patient care, including conduct that interferes the ability to work with members of the health care team. Such behavior can be passive, such as ignoring calls or frequently missing meetings; passive-aggressive, such as excessive sarcasm or veiled threats; or aggressive, such as yelling or bullying.
Don’t focus solely on the behavior
Most disruptive behavior has a root cause, and efforts should be made to get to the bottom of the conduct, according to Sidney Welch, an Atlanta-based health law attorney.
“Often, there’s an underlying frustration in terms of clinical care or what they’re being told to do or the systems and processes [in play],” she said “Where is the sources of the tension that is creating the behavior?”
Do identify contributing factors
Personality characteristics that could lead to hostile behavior include self-centeredness, immaturity, resentfulness, or a need for power and control. Systemic factors could include increased productivity demands, cost-containment requirements, embedded hierarchies, fear of litigation, ineffective or absent conflict-resolution processes, competition between hospitals and medical staff, new care settings, and marketplace demands. Shortages of staff and high work burdens also could fuel disruptive behavior, Ms. Welch said.
“There are situations where there [is] a psychiatric disorder or a personality disorder that’s the root cause of the disruption,” she said. But “sometimes it’s just a stressful situation. A lot of these cases [in which] the physician is the disruption, we’re seeing them in high stakes emergency departments or situations where decisions have to be made very quickly, or fatigue and external stresses may be the source.”
Don’t apply corrective actions inconsistently
Make expectations clear by having a code of conduct supported by policies that apply to every employee, Ms. Welch noted. A lack of fairness among employees can create greater tension and generate increased conflict during a disruptive situation. Ensure that physicians are not be treated differently than nurses or administrators when addressing complaints, she said.
Do implement a graduated set of responses
A tiered response system (informal, formal, disciplinary, regulatory) helps manage disruptive situations based on the extent of conduct, Ms. Welch said.
“The process and disciplinary process [should] to be multileveled so that people know the rules of the road, and the parameters and the bumpers so to speak, are defined.”
Don’t necessarily involve HR
Be cautious of allowing human resource (HR) departments to direct potential disruptive physician issues, Ms. Struthers said.
“I have some concerns about HR getting involved for a couple of reasons,” she said. “If you get nonphysicians involved, it seems to exacerbate the level of tension.”
In addition, if a hospital has a significant number of both employed and independent physicians, HR can sometimes apply different standards and varied courses of action depending on employment status, she said. Of course, if the alleged disrupter is a nonphysician, HR is generally the only route for remedy within a hospital setting, Ms. Welch noted.
Do address the issue through internal processes
Every medical staff should develop and adopt bylaw provisions or policies for intervening in situations in which a physician’s behavior is identified as disruptive, according to AMA policy. Medical staff bylaw provisions or policies should contain procedural safeguards that protect due process.
For doctors in groups or small practices, employment policies and procedures should address protocols when disruption matters arise, Ms. Struthers said.
“The dynamics in a small clinic is that some doctors may more have power than others, so it may be harder in some contexts to treat everyone the same,” she said in an interview. “But that’s a really important thing to do. Any well-advised clinics would have a code of conduct or conduct policy, really to protect the clinic from employee lawsuits.”
Don’t let policies collect dust
“As we all know, you can write the policies, you can put them on the shelf, but if people aren’t reading them and understanding them and aren’t educated on them, then it really does no good,” Ms. Welch said.
Do ensure everyone knows how disruptive behavior is handled
Make certain that all staff review disruptive behavior policies and are adequately trained in how the process works, Ms. Welch added. Employees should know where to seek help if experiencing a disruption matter. Consider having staff members sign or acknowledge a code of conduct upon credentialing or hiring.
“Obviously, disruptive behavior can impact patient care, and it can come from a lot of differ directions; It’s not just physicians,” Ms. Struthers said. “Hospitals [and practices] like other places of business, need to have comprehensive polices and procedures, and they need to follow them.”
On Twitter @legal_med
CHICAGO – Dealing with disruptive behavior by staff and colleagues isn’t just about knowing what to do – it’s also about knowing what not to do.
Often, mishandling disruptive behavior can make matters worse and lead to further conflict among physicians and employees, health law experts warn. At a conference held by the American Bar Association, attorneys offered guidance on the dos and don’ts of disruptive behavior management.
Don’t discipline for the wrong reasons
Know what disruptive behavior is not, advised Margo S. Struthers, a Minneapolis-based health law attorney. Criticism offered in good faith with the aim of improving patient care should not be considered disruptive, she said.
“This is a problem that comes up a lot because, often, there is some element of criticism that is offered by the supposed disruptive physician, which may or may not be justified, may or may have been done in good faith, and may or may not have been in a respectful manner.”
An isolated incident of behavior that is not reflective of a pattern of inappropriate, deep-seated, and habitual behavior should not be construed as disruptive, Ms. Struthers added. In addition, disruptive behavior is not respectful disagreement with leadership, presentation of controversial ideas, or the respectful complaining about processes that endanger patient care.
Do address behavior that is truly disruptive
According to the American Medical Association, disruptive behavior is defined as personal conduct, whether verbal or physical, that negatively affects or that potentially may negatively affect patient care, including conduct that interferes the ability to work with members of the health care team. Such behavior can be passive, such as ignoring calls or frequently missing meetings; passive-aggressive, such as excessive sarcasm or veiled threats; or aggressive, such as yelling or bullying.
Don’t focus solely on the behavior
Most disruptive behavior has a root cause, and efforts should be made to get to the bottom of the conduct, according to Sidney Welch, an Atlanta-based health law attorney.
“Often, there’s an underlying frustration in terms of clinical care or what they’re being told to do or the systems and processes [in play],” she said “Where is the sources of the tension that is creating the behavior?”
Do identify contributing factors
Personality characteristics that could lead to hostile behavior include self-centeredness, immaturity, resentfulness, or a need for power and control. Systemic factors could include increased productivity demands, cost-containment requirements, embedded hierarchies, fear of litigation, ineffective or absent conflict-resolution processes, competition between hospitals and medical staff, new care settings, and marketplace demands. Shortages of staff and high work burdens also could fuel disruptive behavior, Ms. Welch said.
“There are situations where there [is] a psychiatric disorder or a personality disorder that’s the root cause of the disruption,” she said. But “sometimes it’s just a stressful situation. A lot of these cases [in which] the physician is the disruption, we’re seeing them in high stakes emergency departments or situations where decisions have to be made very quickly, or fatigue and external stresses may be the source.”
Don’t apply corrective actions inconsistently
Make expectations clear by having a code of conduct supported by policies that apply to every employee, Ms. Welch noted. A lack of fairness among employees can create greater tension and generate increased conflict during a disruptive situation. Ensure that physicians are not be treated differently than nurses or administrators when addressing complaints, she said.
Do implement a graduated set of responses
A tiered response system (informal, formal, disciplinary, regulatory) helps manage disruptive situations based on the extent of conduct, Ms. Welch said.
“The process and disciplinary process [should] to be multileveled so that people know the rules of the road, and the parameters and the bumpers so to speak, are defined.”
Don’t necessarily involve HR
Be cautious of allowing human resource (HR) departments to direct potential disruptive physician issues, Ms. Struthers said.
“I have some concerns about HR getting involved for a couple of reasons,” she said. “If you get nonphysicians involved, it seems to exacerbate the level of tension.”
In addition, if a hospital has a significant number of both employed and independent physicians, HR can sometimes apply different standards and varied courses of action depending on employment status, she said. Of course, if the alleged disrupter is a nonphysician, HR is generally the only route for remedy within a hospital setting, Ms. Welch noted.
Do address the issue through internal processes
Every medical staff should develop and adopt bylaw provisions or policies for intervening in situations in which a physician’s behavior is identified as disruptive, according to AMA policy. Medical staff bylaw provisions or policies should contain procedural safeguards that protect due process.
For doctors in groups or small practices, employment policies and procedures should address protocols when disruption matters arise, Ms. Struthers said.
“The dynamics in a small clinic is that some doctors may more have power than others, so it may be harder in some contexts to treat everyone the same,” she said in an interview. “But that’s a really important thing to do. Any well-advised clinics would have a code of conduct or conduct policy, really to protect the clinic from employee lawsuits.”
Don’t let policies collect dust
“As we all know, you can write the policies, you can put them on the shelf, but if people aren’t reading them and understanding them and aren’t educated on them, then it really does no good,” Ms. Welch said.
Do ensure everyone knows how disruptive behavior is handled
Make certain that all staff review disruptive behavior policies and are adequately trained in how the process works, Ms. Welch added. Employees should know where to seek help if experiencing a disruption matter. Consider having staff members sign or acknowledge a code of conduct upon credentialing or hiring.
“Obviously, disruptive behavior can impact patient care, and it can come from a lot of differ directions; It’s not just physicians,” Ms. Struthers said. “Hospitals [and practices] like other places of business, need to have comprehensive polices and procedures, and they need to follow them.”
On Twitter @legal_med
CHICAGO – Dealing with disruptive behavior by staff and colleagues isn’t just about knowing what to do – it’s also about knowing what not to do.
Often, mishandling disruptive behavior can make matters worse and lead to further conflict among physicians and employees, health law experts warn. At a conference held by the American Bar Association, attorneys offered guidance on the dos and don’ts of disruptive behavior management.
Don’t discipline for the wrong reasons
Know what disruptive behavior is not, advised Margo S. Struthers, a Minneapolis-based health law attorney. Criticism offered in good faith with the aim of improving patient care should not be considered disruptive, she said.
“This is a problem that comes up a lot because, often, there is some element of criticism that is offered by the supposed disruptive physician, which may or may not be justified, may or may have been done in good faith, and may or may not have been in a respectful manner.”
An isolated incident of behavior that is not reflective of a pattern of inappropriate, deep-seated, and habitual behavior should not be construed as disruptive, Ms. Struthers added. In addition, disruptive behavior is not respectful disagreement with leadership, presentation of controversial ideas, or the respectful complaining about processes that endanger patient care.
Do address behavior that is truly disruptive
According to the American Medical Association, disruptive behavior is defined as personal conduct, whether verbal or physical, that negatively affects or that potentially may negatively affect patient care, including conduct that interferes the ability to work with members of the health care team. Such behavior can be passive, such as ignoring calls or frequently missing meetings; passive-aggressive, such as excessive sarcasm or veiled threats; or aggressive, such as yelling or bullying.
Don’t focus solely on the behavior
Most disruptive behavior has a root cause, and efforts should be made to get to the bottom of the conduct, according to Sidney Welch, an Atlanta-based health law attorney.
“Often, there’s an underlying frustration in terms of clinical care or what they’re being told to do or the systems and processes [in play],” she said “Where is the sources of the tension that is creating the behavior?”
Do identify contributing factors
Personality characteristics that could lead to hostile behavior include self-centeredness, immaturity, resentfulness, or a need for power and control. Systemic factors could include increased productivity demands, cost-containment requirements, embedded hierarchies, fear of litigation, ineffective or absent conflict-resolution processes, competition between hospitals and medical staff, new care settings, and marketplace demands. Shortages of staff and high work burdens also could fuel disruptive behavior, Ms. Welch said.
“There are situations where there [is] a psychiatric disorder or a personality disorder that’s the root cause of the disruption,” she said. But “sometimes it’s just a stressful situation. A lot of these cases [in which] the physician is the disruption, we’re seeing them in high stakes emergency departments or situations where decisions have to be made very quickly, or fatigue and external stresses may be the source.”
Don’t apply corrective actions inconsistently
Make expectations clear by having a code of conduct supported by policies that apply to every employee, Ms. Welch noted. A lack of fairness among employees can create greater tension and generate increased conflict during a disruptive situation. Ensure that physicians are not be treated differently than nurses or administrators when addressing complaints, she said.
Do implement a graduated set of responses
A tiered response system (informal, formal, disciplinary, regulatory) helps manage disruptive situations based on the extent of conduct, Ms. Welch said.
“The process and disciplinary process [should] to be multileveled so that people know the rules of the road, and the parameters and the bumpers so to speak, are defined.”
Don’t necessarily involve HR
Be cautious of allowing human resource (HR) departments to direct potential disruptive physician issues, Ms. Struthers said.
“I have some concerns about HR getting involved for a couple of reasons,” she said. “If you get nonphysicians involved, it seems to exacerbate the level of tension.”
In addition, if a hospital has a significant number of both employed and independent physicians, HR can sometimes apply different standards and varied courses of action depending on employment status, she said. Of course, if the alleged disrupter is a nonphysician, HR is generally the only route for remedy within a hospital setting, Ms. Welch noted.
Do address the issue through internal processes
Every medical staff should develop and adopt bylaw provisions or policies for intervening in situations in which a physician’s behavior is identified as disruptive, according to AMA policy. Medical staff bylaw provisions or policies should contain procedural safeguards that protect due process.
For doctors in groups or small practices, employment policies and procedures should address protocols when disruption matters arise, Ms. Struthers said.
“The dynamics in a small clinic is that some doctors may more have power than others, so it may be harder in some contexts to treat everyone the same,” she said in an interview. “But that’s a really important thing to do. Any well-advised clinics would have a code of conduct or conduct policy, really to protect the clinic from employee lawsuits.”
Don’t let policies collect dust
“As we all know, you can write the policies, you can put them on the shelf, but if people aren’t reading them and understanding them and aren’t educated on them, then it really does no good,” Ms. Welch said.
Do ensure everyone knows how disruptive behavior is handled
Make certain that all staff review disruptive behavior policies and are adequately trained in how the process works, Ms. Welch added. Employees should know where to seek help if experiencing a disruption matter. Consider having staff members sign or acknowledge a code of conduct upon credentialing or hiring.
“Obviously, disruptive behavior can impact patient care, and it can come from a lot of differ directions; It’s not just physicians,” Ms. Struthers said. “Hospitals [and practices] like other places of business, need to have comprehensive polices and procedures, and they need to follow them.”
On Twitter @legal_med
AT THE PHYSICIANS LEGAL ISSUES CONFERENCE
LEADER: Liraglutide lowers CVD risk in type 2 diabetes
Liraglutide is associated with a decreased risk of cardiovascular events, compared with placebo, in individuals with type 2 diabetes, according to results from the randomized, placebo-controlled, double-blind LEADER trial.
In the 9,340 patients with type 2 diabetes in LEADER, those treated with the glucagonlike peptide–1 (GLP-1) analogue liraglutide had a 13% lower risk of a composite outcome of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke over a median follow-up of 3.8 years (hazard ratio, 0.87; 95% confidence interval, 0.78-0.97; P less than .001 for noninferiority; P = .01 for superiority).
This significant reduction in the primary outcome in LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome) makes liraglutide (Victoza) the second antihyperglycemic drug to be shown to reduce cardiovascular outcomes since the Food and Drug Administration mandated that all such agents be tested in such a way in 2008. The first was the sodium-glucose cotransporter–2 inhibitor empagliflozin, which reduced the risk of the composite endpoint of hospitalization for heart failure or death due to cardiovascular disease by 34% in the EMPA-REG OUTCOME trial (N Engl J Med. 2015;373:2117-28).
In LEADER, the rate of death from cardiovascular causes was 22% lower in the liraglutide group than in the placebo group (95% CI, 0.66-0.93; P = .007). However, the lower incidences of nonfatal MI, stroke, and hospitalization for heart failure in the liraglutide group did not reach statistical significance.
The participants in LEADER all had a hemoglobin A1c level of 7.0%, and were either aged over 50 with at least one cardiovascular condition such as coronary heart disease, or aged over 60 with at least one cardiovascular risk factor such as hypertension or microalbuminuria.
The participants, who were recruited from 410 sites in 32 countries, were randomized to 1.8 mg or the maximum tolerated dose of subcutaneous liraglutide once daily or to equivalent placebo, in addition to standard care (N Engl J Med. 2016 June 13. doi: 10.1056/NEJMoa1603827).
“Although glycemic control is associated with reductions in the risk of microvascular complications, the macrovascular benefits of glycemic control are less certain,” wrote Dr. Steven P. Marso of the University of Texas Southwestern Medical Center, Dallas, and his coauthors.
“Furthermore, concern has been raised about the cardiovascular safety of antihyperglycemic therapies, [and] consequently, regulatory authorities have mandated cardiovascular safety assessments of new diabetes treatments.”
The study did see a significant interaction between liraglutide and renal function. Patients who had an estimated glomerular filtration rate (eGFR) of less than 60 mL/min per 1.73 m2 showed more benefits from the liraglutide in terms of the primary outcomes than did those with an eGFR of at least 60 mL/min.
Individuals aged over 50 years with established cardiovascular disease also showed greater benefits in reductions in the primary outcome from liraglutide than did patients aged over 60 years with cardiovascular risk factors.
The authors commented that their findings contrast with those of the Lixisenatide in Acute Coronary Syndrome (ELIXA) trial using the shorter-acting and structurally dissimilar GLP-1 receptor agonist lixisenatide. This trial failed to show any cardiovascular benefit of the drug in patients with diabetes and a recent acute coronary syndrome, as did several other trials looking at cardiovascular outcomes in high-risk patients with type 2 diabetes treated with drugs including insulin, thiazolidinediones, and dipeptidyl peptidase–4 inhibitors.
“Our trial had greater statistical power and included patients with a higher baseline glycated hemoglobin level than did most previous studies,” the authors wrote. “However, no obvious single explanation in terms of either the study designs or the included populations is apparent to explain the divergent findings across this body of medical literature.
The study also examined the incidence of adverse events, finding a nonsignificantly higher overall rate of benign or malignant neoplasms with liraglutide, compared with placebo. However, there was a trend toward an increased risk of pancreatic cancer in those taking liraglutide, which approached statistical significance.
“There has been considerable interest in a potential association between the use of GLP-1 receptor agonists and pancreatitis and pancreatic cancer, although there is no consistent preclinical, pharmacovigilance, or epidemiologic evidence to date,” the authors commented.
The study was supported by Novo Nordisk and the National Institutes of Health. Several authors declared grants, consultancies and funding from the pharmaceutical industry, including from Novo Nordisk. Several authors are employees of Novo Nordisk, are on steering committees, and/or own shares in the company.
Liraglutide is associated with a decreased risk of cardiovascular events, compared with placebo, in individuals with type 2 diabetes, according to results from the randomized, placebo-controlled, double-blind LEADER trial.
In the 9,340 patients with type 2 diabetes in LEADER, those treated with the glucagonlike peptide–1 (GLP-1) analogue liraglutide had a 13% lower risk of a composite outcome of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke over a median follow-up of 3.8 years (hazard ratio, 0.87; 95% confidence interval, 0.78-0.97; P less than .001 for noninferiority; P = .01 for superiority).
This significant reduction in the primary outcome in LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome) makes liraglutide (Victoza) the second antihyperglycemic drug to be shown to reduce cardiovascular outcomes since the Food and Drug Administration mandated that all such agents be tested in such a way in 2008. The first was the sodium-glucose cotransporter–2 inhibitor empagliflozin, which reduced the risk of the composite endpoint of hospitalization for heart failure or death due to cardiovascular disease by 34% in the EMPA-REG OUTCOME trial (N Engl J Med. 2015;373:2117-28).
In LEADER, the rate of death from cardiovascular causes was 22% lower in the liraglutide group than in the placebo group (95% CI, 0.66-0.93; P = .007). However, the lower incidences of nonfatal MI, stroke, and hospitalization for heart failure in the liraglutide group did not reach statistical significance.
The participants in LEADER all had a hemoglobin A1c level of 7.0%, and were either aged over 50 with at least one cardiovascular condition such as coronary heart disease, or aged over 60 with at least one cardiovascular risk factor such as hypertension or microalbuminuria.
The participants, who were recruited from 410 sites in 32 countries, were randomized to 1.8 mg or the maximum tolerated dose of subcutaneous liraglutide once daily or to equivalent placebo, in addition to standard care (N Engl J Med. 2016 June 13. doi: 10.1056/NEJMoa1603827).
“Although glycemic control is associated with reductions in the risk of microvascular complications, the macrovascular benefits of glycemic control are less certain,” wrote Dr. Steven P. Marso of the University of Texas Southwestern Medical Center, Dallas, and his coauthors.
“Furthermore, concern has been raised about the cardiovascular safety of antihyperglycemic therapies, [and] consequently, regulatory authorities have mandated cardiovascular safety assessments of new diabetes treatments.”
The study did see a significant interaction between liraglutide and renal function. Patients who had an estimated glomerular filtration rate (eGFR) of less than 60 mL/min per 1.73 m2 showed more benefits from the liraglutide in terms of the primary outcomes than did those with an eGFR of at least 60 mL/min.
Individuals aged over 50 years with established cardiovascular disease also showed greater benefits in reductions in the primary outcome from liraglutide than did patients aged over 60 years with cardiovascular risk factors.
The authors commented that their findings contrast with those of the Lixisenatide in Acute Coronary Syndrome (ELIXA) trial using the shorter-acting and structurally dissimilar GLP-1 receptor agonist lixisenatide. This trial failed to show any cardiovascular benefit of the drug in patients with diabetes and a recent acute coronary syndrome, as did several other trials looking at cardiovascular outcomes in high-risk patients with type 2 diabetes treated with drugs including insulin, thiazolidinediones, and dipeptidyl peptidase–4 inhibitors.
“Our trial had greater statistical power and included patients with a higher baseline glycated hemoglobin level than did most previous studies,” the authors wrote. “However, no obvious single explanation in terms of either the study designs or the included populations is apparent to explain the divergent findings across this body of medical literature.
The study also examined the incidence of adverse events, finding a nonsignificantly higher overall rate of benign or malignant neoplasms with liraglutide, compared with placebo. However, there was a trend toward an increased risk of pancreatic cancer in those taking liraglutide, which approached statistical significance.
“There has been considerable interest in a potential association between the use of GLP-1 receptor agonists and pancreatitis and pancreatic cancer, although there is no consistent preclinical, pharmacovigilance, or epidemiologic evidence to date,” the authors commented.
The study was supported by Novo Nordisk and the National Institutes of Health. Several authors declared grants, consultancies and funding from the pharmaceutical industry, including from Novo Nordisk. Several authors are employees of Novo Nordisk, are on steering committees, and/or own shares in the company.
Liraglutide is associated with a decreased risk of cardiovascular events, compared with placebo, in individuals with type 2 diabetes, according to results from the randomized, placebo-controlled, double-blind LEADER trial.
In the 9,340 patients with type 2 diabetes in LEADER, those treated with the glucagonlike peptide–1 (GLP-1) analogue liraglutide had a 13% lower risk of a composite outcome of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke over a median follow-up of 3.8 years (hazard ratio, 0.87; 95% confidence interval, 0.78-0.97; P less than .001 for noninferiority; P = .01 for superiority).
This significant reduction in the primary outcome in LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome) makes liraglutide (Victoza) the second antihyperglycemic drug to be shown to reduce cardiovascular outcomes since the Food and Drug Administration mandated that all such agents be tested in such a way in 2008. The first was the sodium-glucose cotransporter–2 inhibitor empagliflozin, which reduced the risk of the composite endpoint of hospitalization for heart failure or death due to cardiovascular disease by 34% in the EMPA-REG OUTCOME trial (N Engl J Med. 2015;373:2117-28).
In LEADER, the rate of death from cardiovascular causes was 22% lower in the liraglutide group than in the placebo group (95% CI, 0.66-0.93; P = .007). However, the lower incidences of nonfatal MI, stroke, and hospitalization for heart failure in the liraglutide group did not reach statistical significance.
The participants in LEADER all had a hemoglobin A1c level of 7.0%, and were either aged over 50 with at least one cardiovascular condition such as coronary heart disease, or aged over 60 with at least one cardiovascular risk factor such as hypertension or microalbuminuria.
The participants, who were recruited from 410 sites in 32 countries, were randomized to 1.8 mg or the maximum tolerated dose of subcutaneous liraglutide once daily or to equivalent placebo, in addition to standard care (N Engl J Med. 2016 June 13. doi: 10.1056/NEJMoa1603827).
“Although glycemic control is associated with reductions in the risk of microvascular complications, the macrovascular benefits of glycemic control are less certain,” wrote Dr. Steven P. Marso of the University of Texas Southwestern Medical Center, Dallas, and his coauthors.
“Furthermore, concern has been raised about the cardiovascular safety of antihyperglycemic therapies, [and] consequently, regulatory authorities have mandated cardiovascular safety assessments of new diabetes treatments.”
The study did see a significant interaction between liraglutide and renal function. Patients who had an estimated glomerular filtration rate (eGFR) of less than 60 mL/min per 1.73 m2 showed more benefits from the liraglutide in terms of the primary outcomes than did those with an eGFR of at least 60 mL/min.
Individuals aged over 50 years with established cardiovascular disease also showed greater benefits in reductions in the primary outcome from liraglutide than did patients aged over 60 years with cardiovascular risk factors.
The authors commented that their findings contrast with those of the Lixisenatide in Acute Coronary Syndrome (ELIXA) trial using the shorter-acting and structurally dissimilar GLP-1 receptor agonist lixisenatide. This trial failed to show any cardiovascular benefit of the drug in patients with diabetes and a recent acute coronary syndrome, as did several other trials looking at cardiovascular outcomes in high-risk patients with type 2 diabetes treated with drugs including insulin, thiazolidinediones, and dipeptidyl peptidase–4 inhibitors.
“Our trial had greater statistical power and included patients with a higher baseline glycated hemoglobin level than did most previous studies,” the authors wrote. “However, no obvious single explanation in terms of either the study designs or the included populations is apparent to explain the divergent findings across this body of medical literature.
The study also examined the incidence of adverse events, finding a nonsignificantly higher overall rate of benign or malignant neoplasms with liraglutide, compared with placebo. However, there was a trend toward an increased risk of pancreatic cancer in those taking liraglutide, which approached statistical significance.
“There has been considerable interest in a potential association between the use of GLP-1 receptor agonists and pancreatitis and pancreatic cancer, although there is no consistent preclinical, pharmacovigilance, or epidemiologic evidence to date,” the authors commented.
The study was supported by Novo Nordisk and the National Institutes of Health. Several authors declared grants, consultancies and funding from the pharmaceutical industry, including from Novo Nordisk. Several authors are employees of Novo Nordisk, are on steering committees, and/or own shares in the company.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Liraglutide is associated with a decreased risk of cardiovascular events, compared with placebo, in patients with type 2 diabetes.
Major finding: Patients with type 2 diabetes at high risk for cardiovascular disease taking liraglutide had a 13% lower risk of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke, compared with those on placebo, a significant difference.
Data source: A randomized, double-blind, placebo-controlled trial in 9,340 patients with type 2 diabetes and either established cardiovascular disease or cardiovascular risk factors.
Disclosures: The study was supported by Novo Nordisk and the National Institutes of Health. Several authors declared grants, consultancies, and funding from the pharmaceutical industry, including from Novo Nordisk. Several authors are employees of Novo Nordisk, are on steering committees, and/or own shares in the company.
Esophagectomy 30-day readmission rate pegged at 19%
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Operative length, perioperative blood transfusions, and postoperative ICU admission were significant risk factors for readmission after esophagectomy.
Major finding: The rate of unplanned 30-day readmission was 19%.
Data source: The study assessed 86 patients who underwent esophagectomy at the Mayo Clinic between August 2012 and July 2014.
Disclosures: Dr. Dickinson and her colleagues reported having no relevant disclosures.
HIV research update: Early June 2016
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Interventions that seek to promptly house homeless individuals might assist in maximizing the clinical and public health benefits of antiretroviral therapy among people living with HIV/AIDS, according to a study in AIDS Care.
MRSA colonization among HIV-infected youth is more closely related to living in a low-income or slum community than to HIV-related clinical factors, according to a study in the Pediatric Infectious Disease Journal.
Marijuana use was not associated with progression to significant liver fibrosis, in a large cohort study of HIV/hepatitis C virus (HCV) co-infected women. Alcohol use may better predict fibrosis progression in HIV/HCV co-infected women, the authors said.
More than 60% of deaths occurring in a rural South African community between 1992 and 2013 could be attributed directly or indirectly to HIV, according to a recent study. However, the authors noted that there has been an increasing level of non-HIV mortality, which has important implications for local health care provision.
A study in AIDS Care found that providers value same-day, electronic, patient-reported measures for use in clinical HIV care, with the condition that patient-reported outcomes are 1) tailored to be the most clinically relevant to their population; 2) well integrated into clinic flow; and 3) easy to interpret, highlighting chief patient concerns and changes over time.
Investigators found that nasal and salivary samples can be collected from HIV-infected patients in a standardized manner over repeated visits in both low and high resource settings, and these methods may be used in support of future HIV vaccine clinical trials.
A study in the Journal of Infectious Diseases found no intrinsic effect of viral subtype on the efficacy of tenofovir-containing regimens for treating HIV-1 subtype C infections. There were no differences between subtypes C and non-B/C in either univariate or multivariate analysis.
New research provides preliminary evidence that heavy drinking may increase a key inflammatory marker in HIV-infected individuals with suppressed infection.
The phase III Women AntiretroViral Efficacy and Safety study (WAVES) showed that clinical trials of antiretroviral regimens in global and diverse populations of treatment-naive women are possible, investigators concluded. They said their findings support guidelines recommending integrase inhibitor–based regimens in first-line antiretroviral therapy.
A hybrid mobile strategy for HIV testing of adults was leveraged successfully to reach adolescents for HIV treatment and prevention, according to a study in Kenya and Uganda.
With viral suppression induced by combination antiretroviral therapy, women have less reduction in key markers of inflammation and immune activation, compared with men, report the authors of a study in JAIDS.
The transfer of HIV-1-p17-specific T-cell receptors (TCRs) into T-cells is functional both in HIV-1–infected patients and in healthy blood donors, according to a study in the journal AIDS. The authors say TCR-transfer is a promising method to boost the immune system against HIV-1.
HIV-1 subtype C (HIV-1C) exhibits lower in vivo fitness, compared with HIV-1B, which allows successful treatment despite high baseline viral loads, a new study demonstrated. The lower fitness – and potentially lower virulence – together with high viral loads may underlie the heightened transmission potential of HIV-1C and its growing global spread.
Thailand has achieved World Health Organization targets for elimination of mother-to-child-transmission of HIV and can serve as a model for other countries, according to a report in MMWR.
Regular CD4 testing may be unnecessary for virally suppressed children aged 5-15 years with CD4 greater than or equal to 500 cells/mm3, according to a study published in the Journal of the Pediatric Infectious Diseases Society.
Investigators at Case Western Reserve University, Cleveland found that 24 weeks of 10 mg daily rosuvastatin decreases plasma coenzyme Q10 concentration and increases CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy.
Researchers from the University of California, San Francisco, and Yale University, New Haven, Conn., found that half of people newly infected with HIV experience neurologic issues that are generally not severe and usually resolve after starting antiretroviral therapy.
A study of HIV-infected individuals in metropolitan Washington identified high prevalence of transmitted drug resistance, regardless of gender. The authors said active surveillance for transmitted drug resistance is needed to guide antiretroviral usage and analyses of risk group contributions to HIV transmission and resistance.
Single-nucleotide polymorphisms in genes encoding the Toll-like receptor 4 (TLR4) and CD14 are independently associated with long-term CD4+ T-cell recovery in HIV-infected individuals after antiretroviral therapy, according to a study in the journal AIDS.
In HIV/HCV co-infected individuals, the crude incidence of hepatocellular carcinoma increased from 2001 to 2014, while other liver events declined, according to a recent study.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Interventions that seek to promptly house homeless individuals might assist in maximizing the clinical and public health benefits of antiretroviral therapy among people living with HIV/AIDS, according to a study in AIDS Care.
MRSA colonization among HIV-infected youth is more closely related to living in a low-income or slum community than to HIV-related clinical factors, according to a study in the Pediatric Infectious Disease Journal.
Marijuana use was not associated with progression to significant liver fibrosis, in a large cohort study of HIV/hepatitis C virus (HCV) co-infected women. Alcohol use may better predict fibrosis progression in HIV/HCV co-infected women, the authors said.
More than 60% of deaths occurring in a rural South African community between 1992 and 2013 could be attributed directly or indirectly to HIV, according to a recent study. However, the authors noted that there has been an increasing level of non-HIV mortality, which has important implications for local health care provision.
A study in AIDS Care found that providers value same-day, electronic, patient-reported measures for use in clinical HIV care, with the condition that patient-reported outcomes are 1) tailored to be the most clinically relevant to their population; 2) well integrated into clinic flow; and 3) easy to interpret, highlighting chief patient concerns and changes over time.
Investigators found that nasal and salivary samples can be collected from HIV-infected patients in a standardized manner over repeated visits in both low and high resource settings, and these methods may be used in support of future HIV vaccine clinical trials.
A study in the Journal of Infectious Diseases found no intrinsic effect of viral subtype on the efficacy of tenofovir-containing regimens for treating HIV-1 subtype C infections. There were no differences between subtypes C and non-B/C in either univariate or multivariate analysis.
New research provides preliminary evidence that heavy drinking may increase a key inflammatory marker in HIV-infected individuals with suppressed infection.
The phase III Women AntiretroViral Efficacy and Safety study (WAVES) showed that clinical trials of antiretroviral regimens in global and diverse populations of treatment-naive women are possible, investigators concluded. They said their findings support guidelines recommending integrase inhibitor–based regimens in first-line antiretroviral therapy.
A hybrid mobile strategy for HIV testing of adults was leveraged successfully to reach adolescents for HIV treatment and prevention, according to a study in Kenya and Uganda.
With viral suppression induced by combination antiretroviral therapy, women have less reduction in key markers of inflammation and immune activation, compared with men, report the authors of a study in JAIDS.
The transfer of HIV-1-p17-specific T-cell receptors (TCRs) into T-cells is functional both in HIV-1–infected patients and in healthy blood donors, according to a study in the journal AIDS. The authors say TCR-transfer is a promising method to boost the immune system against HIV-1.
HIV-1 subtype C (HIV-1C) exhibits lower in vivo fitness, compared with HIV-1B, which allows successful treatment despite high baseline viral loads, a new study demonstrated. The lower fitness – and potentially lower virulence – together with high viral loads may underlie the heightened transmission potential of HIV-1C and its growing global spread.
Thailand has achieved World Health Organization targets for elimination of mother-to-child-transmission of HIV and can serve as a model for other countries, according to a report in MMWR.
Regular CD4 testing may be unnecessary for virally suppressed children aged 5-15 years with CD4 greater than or equal to 500 cells/mm3, according to a study published in the Journal of the Pediatric Infectious Diseases Society.
Investigators at Case Western Reserve University, Cleveland found that 24 weeks of 10 mg daily rosuvastatin decreases plasma coenzyme Q10 concentration and increases CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy.
Researchers from the University of California, San Francisco, and Yale University, New Haven, Conn., found that half of people newly infected with HIV experience neurologic issues that are generally not severe and usually resolve after starting antiretroviral therapy.
A study of HIV-infected individuals in metropolitan Washington identified high prevalence of transmitted drug resistance, regardless of gender. The authors said active surveillance for transmitted drug resistance is needed to guide antiretroviral usage and analyses of risk group contributions to HIV transmission and resistance.
Single-nucleotide polymorphisms in genes encoding the Toll-like receptor 4 (TLR4) and CD14 are independently associated with long-term CD4+ T-cell recovery in HIV-infected individuals after antiretroviral therapy, according to a study in the journal AIDS.
In HIV/HCV co-infected individuals, the crude incidence of hepatocellular carcinoma increased from 2001 to 2014, while other liver events declined, according to a recent study.
On Twitter @richpizzi
A great volume of HIV and AIDS research enters the medical literature every month. It’s difficult to monitor everything, so here’s a quick look at some notable news items and journal articles published over the past few weeks.
Interventions that seek to promptly house homeless individuals might assist in maximizing the clinical and public health benefits of antiretroviral therapy among people living with HIV/AIDS, according to a study in AIDS Care.
MRSA colonization among HIV-infected youth is more closely related to living in a low-income or slum community than to HIV-related clinical factors, according to a study in the Pediatric Infectious Disease Journal.
Marijuana use was not associated with progression to significant liver fibrosis, in a large cohort study of HIV/hepatitis C virus (HCV) co-infected women. Alcohol use may better predict fibrosis progression in HIV/HCV co-infected women, the authors said.
More than 60% of deaths occurring in a rural South African community between 1992 and 2013 could be attributed directly or indirectly to HIV, according to a recent study. However, the authors noted that there has been an increasing level of non-HIV mortality, which has important implications for local health care provision.
A study in AIDS Care found that providers value same-day, electronic, patient-reported measures for use in clinical HIV care, with the condition that patient-reported outcomes are 1) tailored to be the most clinically relevant to their population; 2) well integrated into clinic flow; and 3) easy to interpret, highlighting chief patient concerns and changes over time.
Investigators found that nasal and salivary samples can be collected from HIV-infected patients in a standardized manner over repeated visits in both low and high resource settings, and these methods may be used in support of future HIV vaccine clinical trials.
A study in the Journal of Infectious Diseases found no intrinsic effect of viral subtype on the efficacy of tenofovir-containing regimens for treating HIV-1 subtype C infections. There were no differences between subtypes C and non-B/C in either univariate or multivariate analysis.
New research provides preliminary evidence that heavy drinking may increase a key inflammatory marker in HIV-infected individuals with suppressed infection.
The phase III Women AntiretroViral Efficacy and Safety study (WAVES) showed that clinical trials of antiretroviral regimens in global and diverse populations of treatment-naive women are possible, investigators concluded. They said their findings support guidelines recommending integrase inhibitor–based regimens in first-line antiretroviral therapy.
A hybrid mobile strategy for HIV testing of adults was leveraged successfully to reach adolescents for HIV treatment and prevention, according to a study in Kenya and Uganda.
With viral suppression induced by combination antiretroviral therapy, women have less reduction in key markers of inflammation and immune activation, compared with men, report the authors of a study in JAIDS.
The transfer of HIV-1-p17-specific T-cell receptors (TCRs) into T-cells is functional both in HIV-1–infected patients and in healthy blood donors, according to a study in the journal AIDS. The authors say TCR-transfer is a promising method to boost the immune system against HIV-1.
HIV-1 subtype C (HIV-1C) exhibits lower in vivo fitness, compared with HIV-1B, which allows successful treatment despite high baseline viral loads, a new study demonstrated. The lower fitness – and potentially lower virulence – together with high viral loads may underlie the heightened transmission potential of HIV-1C and its growing global spread.
Thailand has achieved World Health Organization targets for elimination of mother-to-child-transmission of HIV and can serve as a model for other countries, according to a report in MMWR.
Regular CD4 testing may be unnecessary for virally suppressed children aged 5-15 years with CD4 greater than or equal to 500 cells/mm3, according to a study published in the Journal of the Pediatric Infectious Diseases Society.
Investigators at Case Western Reserve University, Cleveland found that 24 weeks of 10 mg daily rosuvastatin decreases plasma coenzyme Q10 concentration and increases CoQ10/LDL ratio in HIV-infected patients on antiretroviral therapy.
Researchers from the University of California, San Francisco, and Yale University, New Haven, Conn., found that half of people newly infected with HIV experience neurologic issues that are generally not severe and usually resolve after starting antiretroviral therapy.
A study of HIV-infected individuals in metropolitan Washington identified high prevalence of transmitted drug resistance, regardless of gender. The authors said active surveillance for transmitted drug resistance is needed to guide antiretroviral usage and analyses of risk group contributions to HIV transmission and resistance.
Single-nucleotide polymorphisms in genes encoding the Toll-like receptor 4 (TLR4) and CD14 are independently associated with long-term CD4+ T-cell recovery in HIV-infected individuals after antiretroviral therapy, according to a study in the journal AIDS.
In HIV/HCV co-infected individuals, the crude incidence of hepatocellular carcinoma increased from 2001 to 2014, while other liver events declined, according to a recent study.
On Twitter @richpizzi
Artificial pancreas can improve inpatient glycemic control in type 2 diabetes
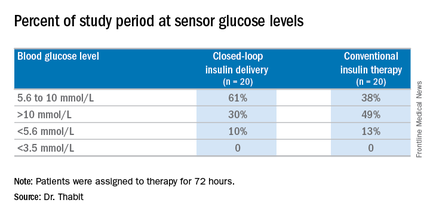
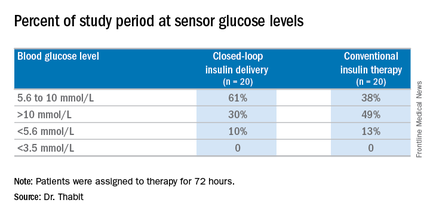
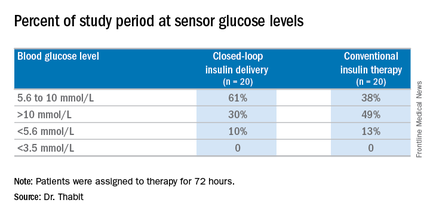
NEW ORLEANS – Having people with type 2 diabetes mellitus use an artificial pancreas during hospitalization has the potential to improve control of their glycemia when compared with conventional insulin therapy, based on the results of a small study of inpatients in the United Kingdom.
“This is the first study to show that automated subcutaneous closed-loop insulin delivery without meal-time insulin is feasible and safe in patients with insulin-treated type 2 diabetes in the general wards,” Dr. Hood Thabit of the University of Cambridge (England) reported at the ADA annual scientific sessions. “Closed-loop [delivery] increased time in target, with reduced glucose variability and reduced time spent hyperglycemic without actually increasing time spent hypoglycemic,” he said.
The study involved 40 general ward inpatients evenly assigned to the closed-loop system and conventional insulin therapy for 72 hours.
Dr. Thabit said hyperglycemia in hospital patients is a common problem that’s poorly managed. “There’s an unmet need for an effective and safe glucose control, specifically in the underserved and understudied population of type 2 diabetes in the general wards,” he said. The use of the closed-loop system in inpatients with type 2 diabetes “remains untested until now,” Dr. Thabit added.
The 20 patients randomized to the closed-loop system spent an average of 61% of the whole study period within the sensor glucose target vs. 38% of those on conventional insulin therapy. The closed-loop patients also used comparable insulin daily on average: 62.6 U (±36.3 U) vs. 66.0 U (±39.6 U), Dr. Thabit said.
He noted that those on the closed-loop system did not have to announce meals to the control algorithm, or give any meal-time insulin – “we didn’t want to trouble our nurses with this, due to the increasing workload that health care professionals in the hospital currently face,” he said – and showed “significantly improved” nighttime control of glucose while “simultaneously reducing the risk of nocturnal hypoglycemia”. “The closed loop may potentially be an effective and safe tool to manage hospital inpatient hyperglycemia in this particularly underserved population of patients whilst easing the burden of health care professionals in hospital,” he said.
The cost is not insignificant. The pump and sensor devices together with related consumables can cost up to £6,000 (about $8,600), but he did note the artificial pancreas device itself is reusable. The cost of the automated closed-loop glucose control system can also potentially be offset by the reduced time of health care professionals spent managing inpatient hyperglycemia safely. The study investigators are in the process of planning a larger trial, Dr. Thabit said.
Dr. Thabit had no financial disclosures. Some coauthors disclosed relationships with Novo Nordisk; Medtronic MiniMed; Becton, Dickinson and Co.; Abbott Diabetes Care; Roche Pharmaceuticals; Cell Novo; Animas; Eli Lilly; B. Braun Melsungen; Sanofi-Aventis Deutschland; and Profil Institute for Clinical Research.
NEW ORLEANS – Having people with type 2 diabetes mellitus use an artificial pancreas during hospitalization has the potential to improve control of their glycemia when compared with conventional insulin therapy, based on the results of a small study of inpatients in the United Kingdom.
“This is the first study to show that automated subcutaneous closed-loop insulin delivery without meal-time insulin is feasible and safe in patients with insulin-treated type 2 diabetes in the general wards,” Dr. Hood Thabit of the University of Cambridge (England) reported at the ADA annual scientific sessions. “Closed-loop [delivery] increased time in target, with reduced glucose variability and reduced time spent hyperglycemic without actually increasing time spent hypoglycemic,” he said.
The study involved 40 general ward inpatients evenly assigned to the closed-loop system and conventional insulin therapy for 72 hours.
Dr. Thabit said hyperglycemia in hospital patients is a common problem that’s poorly managed. “There’s an unmet need for an effective and safe glucose control, specifically in the underserved and understudied population of type 2 diabetes in the general wards,” he said. The use of the closed-loop system in inpatients with type 2 diabetes “remains untested until now,” Dr. Thabit added.
The 20 patients randomized to the closed-loop system spent an average of 61% of the whole study period within the sensor glucose target vs. 38% of those on conventional insulin therapy. The closed-loop patients also used comparable insulin daily on average: 62.6 U (±36.3 U) vs. 66.0 U (±39.6 U), Dr. Thabit said.
He noted that those on the closed-loop system did not have to announce meals to the control algorithm, or give any meal-time insulin – “we didn’t want to trouble our nurses with this, due to the increasing workload that health care professionals in the hospital currently face,” he said – and showed “significantly improved” nighttime control of glucose while “simultaneously reducing the risk of nocturnal hypoglycemia”. “The closed loop may potentially be an effective and safe tool to manage hospital inpatient hyperglycemia in this particularly underserved population of patients whilst easing the burden of health care professionals in hospital,” he said.
The cost is not insignificant. The pump and sensor devices together with related consumables can cost up to £6,000 (about $8,600), but he did note the artificial pancreas device itself is reusable. The cost of the automated closed-loop glucose control system can also potentially be offset by the reduced time of health care professionals spent managing inpatient hyperglycemia safely. The study investigators are in the process of planning a larger trial, Dr. Thabit said.
Dr. Thabit had no financial disclosures. Some coauthors disclosed relationships with Novo Nordisk; Medtronic MiniMed; Becton, Dickinson and Co.; Abbott Diabetes Care; Roche Pharmaceuticals; Cell Novo; Animas; Eli Lilly; B. Braun Melsungen; Sanofi-Aventis Deutschland; and Profil Institute for Clinical Research.
NEW ORLEANS – Having people with type 2 diabetes mellitus use an artificial pancreas during hospitalization has the potential to improve control of their glycemia when compared with conventional insulin therapy, based on the results of a small study of inpatients in the United Kingdom.
“This is the first study to show that automated subcutaneous closed-loop insulin delivery without meal-time insulin is feasible and safe in patients with insulin-treated type 2 diabetes in the general wards,” Dr. Hood Thabit of the University of Cambridge (England) reported at the ADA annual scientific sessions. “Closed-loop [delivery] increased time in target, with reduced glucose variability and reduced time spent hyperglycemic without actually increasing time spent hypoglycemic,” he said.
The study involved 40 general ward inpatients evenly assigned to the closed-loop system and conventional insulin therapy for 72 hours.
Dr. Thabit said hyperglycemia in hospital patients is a common problem that’s poorly managed. “There’s an unmet need for an effective and safe glucose control, specifically in the underserved and understudied population of type 2 diabetes in the general wards,” he said. The use of the closed-loop system in inpatients with type 2 diabetes “remains untested until now,” Dr. Thabit added.
The 20 patients randomized to the closed-loop system spent an average of 61% of the whole study period within the sensor glucose target vs. 38% of those on conventional insulin therapy. The closed-loop patients also used comparable insulin daily on average: 62.6 U (±36.3 U) vs. 66.0 U (±39.6 U), Dr. Thabit said.
He noted that those on the closed-loop system did not have to announce meals to the control algorithm, or give any meal-time insulin – “we didn’t want to trouble our nurses with this, due to the increasing workload that health care professionals in the hospital currently face,” he said – and showed “significantly improved” nighttime control of glucose while “simultaneously reducing the risk of nocturnal hypoglycemia”. “The closed loop may potentially be an effective and safe tool to manage hospital inpatient hyperglycemia in this particularly underserved population of patients whilst easing the burden of health care professionals in hospital,” he said.
The cost is not insignificant. The pump and sensor devices together with related consumables can cost up to £6,000 (about $8,600), but he did note the artificial pancreas device itself is reusable. The cost of the automated closed-loop glucose control system can also potentially be offset by the reduced time of health care professionals spent managing inpatient hyperglycemia safely. The study investigators are in the process of planning a larger trial, Dr. Thabit said.
Dr. Thabit had no financial disclosures. Some coauthors disclosed relationships with Novo Nordisk; Medtronic MiniMed; Becton, Dickinson and Co.; Abbott Diabetes Care; Roche Pharmaceuticals; Cell Novo; Animas; Eli Lilly; B. Braun Melsungen; Sanofi-Aventis Deutschland; and Profil Institute for Clinical Research.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point:Hospitalized patients in the general ward with type 2 diabetes mellitus can maintain better glycemic control by using an artificial pancreas than by taking conventional therapy.
Major finding: Patients on the closed-loop system spent an average of 61% of the study period within the sensor glucose target vs. 38% for those on conventional insulin therapy.
Data source: A single-center study of 40 patients randomized to wear the artificial pancreas or take conventional therapy.
Disclosures: Dr. Thabit had no financial disclosures. Some coauthors disclosed relationships with Novo Nordisk; Medtronic MiniMed; Becton, Dickinson and Co.; Abbott Diabetes Care; Roche Pharmaceuticals; Cell Novo; Animas; Eli Lilly; B. Braun Melsungen; Sanofi-Aventis Deutschland; and Profil Institute for Clinical Research.
Psychiatry’s role rising in hospital care
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
BALTIMORE – A team of physicians and mental health experts at Johns Hopkins Hospital is trying something new: combining mental health services with medical ones. Hospital leadership hopes the experiment will pay off in shorter lengths of stay, lower readmission rates, and better overall patient care.
“We’re still collecting that data,” Melissa Richardson, the hospital’s director of care coordination, said in an interview. “We also will look at the impact on staffing ratios on the units. For example, has the number of patient observers gone down? Has the overall severity of certain cases on the unit been reduced by embedding mental health workers there?”
The medical-surgical mental health team debuted in April, and is separate from the hospital’s other psychiatric services. Comprised of a social worker, a nurse practitioner, a nurse care coordinator, and an attending psychiatrist, the team typically works a regular day shift, beginning each morning with patient chart reviews prepared by medical-surgical personnel. They discuss which patients will be seen by whom, since all team members are trained to do psychiatric evaluations.
Not all medical patients require psychiatric care, but according to the program’s clinical director and attending psychiatrist, Dr. Patrick T. Triplett, up to 38% of all medical admissions have a psychiatric comorbidity. Addressing those comorbidities while patients are in the hospital often leads to improved outcomes.
The team’s social worker connects patients with the appropriate outpatient mental health services in the community, and the team’s nurse care coordinator arranges any necessary transfers from the medical-surgical units to the inpatient psychiatric unit. Dr. Triplett and the psychiatric nurse practitioner are the only two team members who can diagnose and prescribe. Dr. Triplett’s time is billed as consultation services, and the hospital absorbs the cost of the rest of the team, according to Ms. Richardson.
‘Complex medically ill’ patients
As some procedures and medical treatments have shifted to the outpatient setting in recent years, and joint replacements or acute conditions such as myocardial infarctions can be managed successfully in shorter stays, more complicated patients, such as joint replacement patients who develop delirium, have been left on the medical-surgical unit, said Dr. Constantine G. Lyketsos, the Elizabeth Plank Althouse Professor at Johns Hopkins Bayview, Baltimore.
“Also, these days, up to 20% of our admissions are linked to opioids. Then, there are the chronically mentally ill. They tend to be a population with high rates of obesity, smoking, and diabetes, so they end up in the hospital with higher-level, more complicated conditions, that because of the disintegration of the mental health system, receive neither good psychiatric nor outpatient medical care,” Dr. Lyketsos, also chief of psychiatry at Johns Hopkins Bayview, said in an interview.
This surge in the number of complex medically ill patients has led to a growing number of hospitals nationwide calling upon psychiatrists for help in improving overall care. Hopkins is only the latest to join the ranks of other institutions such as Massachusetts General Hospital in Boston, State University of New York Downstate Medical Center in Brooklyn (N.Y.), Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and New York–Presbyterian/Columbia University Medical Center in New York City.
The progenitor of this collaborative inpatient care model is Yale New Haven (Conn.) Hospital. The behavioral intervention team (BIT) at Yale New Haven includes nurses, social workers, and psychiatrists who proactively screen for and address behavioral barriers to care for medical patients with a co-occurring mental illness, said Dr. Hochang B. Lee, one of the psychiatrists who helped created the model in 2008. Dr. Lee is Yale’s psychological medicine section chief and director of the school’s Psychological Medicine Research Center. He also is an associate professor of psychiatry and an associate clinical professor of nursing.
“The goal was to create a proactive model of care, not the reactive one that is traditional consultation-liaison psychiatry,” Dr. Lee said in an interview. “Before the BIT model, medical teams often missed behavioral issues or made consultation requests too late in the course of hospitalization to avoid psychiatric crisis.”
LOS, costs reduced
A study
“The hospital is not making money off of us, but they’re losing less money because of us. That’s good!” Dr. Philip R. Muskin, chief of consultation-liaison psychiatry at New York–Presbyterian/Columbia, said in an interview.
Patients at New York Presbyterian have been comanaged since 2004 when, according to Dr. Muskin, a donor gift specifically intended for such a purpose was matched by the hospital’s department of medicine. The unspent money was enough to cover the cost of a consultation-liaison psychiatrist to round full time as an attending with the medical team.
“We were lucky at NYPCH, because someone gave us the gift to hire a full-time psychiatrist we could embed into the medical team,” Dr. Muskin said. “But there is no one right way to deliver collaborative care in the inpatient setting.”
The NYPCH program has grown to include a second full-time and one part-time psychiatrist, serving about half of all medical services at the campus, with plans to hire more. There is also a social worker to assist with outplacement services. Dr. Muskin said he is currently looking to hire a psychiatric nurse practitioner.
‘Nurses love us’
Restoration of staff morale is another benefit to this kind of practice, according to Maureen Lewis, an accredited psychiatric nurse practitioner who is part of the Hopkins integrated team.
“Med-surge nurses love us. Patients who come in with an overdose or who have any psychiatric conditions but need to have their medical comorbidities dealt with first, they are at their sickest with their psychiatric illnesses when they first arrive,” Ms. Lewis said. “It’s the med-surge nurses who have to care for them, but it’s not their comfort zone or their skill set. They like that we are helping them manage the patient.”
A decline in the number of assaults on the nursing staff also has been recorded since the Hopkins program began, Dr. Lyketsos said.
The psychiatrists themselves tend to be happier, too. “Knowing the cases before you even walk up on the unit is a huge benefit,” Dr. Triplett said. “To have to dive into an emergency all the time is just exhausting. It changes your relationship with the patient. When you’re not in that crisis mode, the patient isn’t a ‘problem’ anymore.”
A formal assessment of the entire medical-surgical staff satisfaction involved in the Hopkins program also is underway, said Ms. Richardson, the director of care coordination.
Having psychiatrists at the fore of this evolution in care provides more opportunities for training, too.
The comanagement model gives medical staff a chance to learn more not just about the direct care of complex behaviorally disordered patients, but also to understand their own emotions and states of mind as they interact with these patients. The teaching happens naturally as the team discusses patients while making rounds, Dr. Muskin said. “That’s really an integral part of what consult-liaison psychiatry is supposed to be about, anyway.”
By helping the medical staff reflect on their experiences, Dr. Muskin said, psychiatrists are helping to change the culture of inpatient medicine. “Once you change the culture, if you keep the things that brought it about in place, it doesn’t change back.”
Creating bridge services
A problem with this kind of inpatient collaborative care model is that hospitals that run them aren’t able to control all the variables associated with the cost of providing them.
The hope is that by spending more up front to identify and treat high-risk behavioral health patients, they won’t need readmission; but if the appropriate follow-up care can’t be found on the outpatient side, they could still end up back in the hospital, driving up readmission rates and possibly lengths of stay.
To address such contingencies, Hopkins has participated in state-sponsored partnerships for improving community care and is using monies from accountable care organization funding to create bridge services. The hospital system also has 14 primary care practices that have embedded psychiatric services, and the plan is to create a team to care for more complicated patients who need care 60-90 days after discharge.
For Dr. Lyketsos, however, fixing what he says is a broken mental health system isn’t up to the hospital alone. “We’re not going to be able to bring about real change without working with our legislators and our payers. It’s a complex problem that needs a complex solution. But there is a commonality of mind that we need to fix things, that patients need better care – and that this is a good place to start.”
On Twitter @whitneymcknight
CORRECTION, 6/28/16: A previous version of this article misstated Dr. Hochang B. Lee's name.
Helmets trump face mask for noninvasive ventilation
Treating acute respiratory distress syndrome patients with helmets instead of face masks significantly reduced intubation rates and 90-day mortality rates, based on data from a randomized trial of 83 adults published in JAMA.
Acute respiratory distress syndrome (ARDS) can be treated using a face mask, but the mask is often inadequate, forcing patients to undergo intubation that can lead to additional problems including discomfort, delirium, and muscle deterioration, wrote Tianna Hicklin, Ph.D., in a column on the NIH website.
“The proposed mechanism for improved efficacy of these helmets is the preservation of applied pressures and avoidance of air leak. If the helmets indeed do allow clinicians both to be able to increase airway pressures above levels they typically would with mask-NIV and maintain those pressures without unpredictable system leak, that would be of great physiologic importance for patients with acute respiratory failure,” said Dr. Eric J. Gartman.
To explore the potential of noninvasive ventilation (NIV) using a helmet instead of a mask, both of which allow patients to remain awake in the ICU, the researchers randomized 83 adults with ARDS to treatment with either a helmet (44 patients) or a face mask (39 patients).
Intubation incidence was 18% in patients treated with helmets, compared with 62% for those treated with face masks. In addition, patients in the helmet group had significantly more ventilator-free days than the mask group (28 vs. 13; P less than .001), and both hospital mortality and 90-day mortality rates were significantly lower in the helmet group compared to the mask group (27% vs. 49%; P = .04 and 34% vs. 56%; P = .02, respectively)
Adverse event rates were rare, and similar between the helmet and mask groups. Three interface-related skin ulcers occurred in each group; nose ulcers in 7% of the mask group and neck ulcers in 7% of the helmet group.
The study population included adults aged 18 years and older who were admitted to the ICU at the University of Chicago between September 2012 and September 2015 and required face mask NIV. The average age of the patients was 58 years in the helmet group and 61 years in the mask group; there were no significant demographic differences between the groups. The most common causes of acute respiratory failure in both groups were pneumonia and pneumonia caused by immunosuppression.
The study results were limited by several factors including a lack of blinding, the need for a learning curve for clinicians using the helmet, and the potential for patient-ventilator dyssynchrony in the helmet group, noted Dr. Bhakti K. Patel of the University of Chicago and her colleagues (JAMA 2016;315:2435-41). Multicenter studies are needed to support the findings, they added. However, the findings “affirm the far-reaching benefits of spontaneous yet highly supported ventilation in an awake, animated patient over invasive medical ventilation via endotracheal tube,” they wrote. “These findings warrant further investigation of helmet NIV for patients with ARDS and other types of AHRF [acute hypoxemic respiratory failure], particularly with attention to long-term outcomes.”
The researchers had no financial conflicts to disclose.
“While the results of this study are very impressive, it is a single-center study, and obviously a larger multicenter trial (with all types of institutions included – not just large academic centers) would be helpful to elucidate the benefit of this technique and support a change in standard of care in the use of NIV. A change to this system would be a very large culture shift in NIV and would mean a significant amount of training (physician, nursing, respiratory care), purchasing the helmets, and ensuring that it is implemented properly and safely. As stated by the authors, this fact is similar to the change the occurred originally with NIV – but if their results reflect a true benefit over FM-NIV [face mask-noninvasive ventilation], such a large change would certainly be worth the effort,” Dr. Gartman said.
In a related study published in the Journal of Cardiothoracic and Vascular Anesthesia, patients treated with noninvasive positive pressure ventilation (NPPV) through helmets had significantly lower heart rates, lower average arterial pressure, and improved left ventricular ejection fraction at the end of treatment, compared with patients treated with ventilation masks and controls. Dr. Yi Yang of Capital Medical University in Beijing, China, and colleagues conducted the prospective study of 75 adults experiencing hypoxemia within 24 hours of extubation after Stanford type A aortic dissection. The participants were divided into three 25-patient groups. The control group was treated with high-flux inhalation of oxygen via a Venturi mask, another group was treated with NPPV via a mask, and the third group was treated with NPPV via a helmet. (J Card Vasc Anesth. 2016. http://dx.doi.org/10.1053/j.jvca.2016.03.129).
The study was funded by China’s public welfare industry of health.
“Several key clinical messages can be gained from the study by Patel et al.,” wrote Dr. Jeremy R. Beitler, Dr. Robert L. Owens, and Dr. Atul Malhotra, in an accompanying editorial (JAMA 2016 Jun; 315:2401-3.).
“The helmet interface has unique advantages and disadvantages that may influence efficacy of noninvasive positive pressure ventilation (NIV) depending on patient and disease characteristics,” they said. “External validation of the findings by Patel et al. and clarification of appropriate eligibility criteria, optimal ventilator settings, and potential mechanisms of effect are needed before clinicians could consider an expanded role for helmet NIV in routine management. Regardless, it is increasingly clear that there may be an important albeit underinvestigated role for some form of high-level noninvasive respiratory support to prevent intubation, and perhaps mortality, in acute hypoxemic respiratory failure,” they noted.
“In future studies, reporting of interruptions to wearing the prescribed NIV interface continuously, leak severity, biomarkers of lung injury, and sedative administration would help delineate potential mechanisms [of action],” they added.
Dr. Beitler, Dr. Owens, and Dr. Malhotra are all affiliated with the division of pulmonary and critical care medicine at the University of California, San Diego. They had no financial conflicts to disclose.
“Several key clinical messages can be gained from the study by Patel et al.,” wrote Dr. Jeremy R. Beitler, Dr. Robert L. Owens, and Dr. Atul Malhotra, in an accompanying editorial (JAMA 2016 Jun; 315:2401-3.).
“The helmet interface has unique advantages and disadvantages that may influence efficacy of noninvasive positive pressure ventilation (NIV) depending on patient and disease characteristics,” they said. “External validation of the findings by Patel et al. and clarification of appropriate eligibility criteria, optimal ventilator settings, and potential mechanisms of effect are needed before clinicians could consider an expanded role for helmet NIV in routine management. Regardless, it is increasingly clear that there may be an important albeit underinvestigated role for some form of high-level noninvasive respiratory support to prevent intubation, and perhaps mortality, in acute hypoxemic respiratory failure,” they noted.
“In future studies, reporting of interruptions to wearing the prescribed NIV interface continuously, leak severity, biomarkers of lung injury, and sedative administration would help delineate potential mechanisms [of action],” they added.
Dr. Beitler, Dr. Owens, and Dr. Malhotra are all affiliated with the division of pulmonary and critical care medicine at the University of California, San Diego. They had no financial conflicts to disclose.
“Several key clinical messages can be gained from the study by Patel et al.,” wrote Dr. Jeremy R. Beitler, Dr. Robert L. Owens, and Dr. Atul Malhotra, in an accompanying editorial (JAMA 2016 Jun; 315:2401-3.).
“The helmet interface has unique advantages and disadvantages that may influence efficacy of noninvasive positive pressure ventilation (NIV) depending on patient and disease characteristics,” they said. “External validation of the findings by Patel et al. and clarification of appropriate eligibility criteria, optimal ventilator settings, and potential mechanisms of effect are needed before clinicians could consider an expanded role for helmet NIV in routine management. Regardless, it is increasingly clear that there may be an important albeit underinvestigated role for some form of high-level noninvasive respiratory support to prevent intubation, and perhaps mortality, in acute hypoxemic respiratory failure,” they noted.
“In future studies, reporting of interruptions to wearing the prescribed NIV interface continuously, leak severity, biomarkers of lung injury, and sedative administration would help delineate potential mechanisms [of action],” they added.
Dr. Beitler, Dr. Owens, and Dr. Malhotra are all affiliated with the division of pulmonary and critical care medicine at the University of California, San Diego. They had no financial conflicts to disclose.
Treating acute respiratory distress syndrome patients with helmets instead of face masks significantly reduced intubation rates and 90-day mortality rates, based on data from a randomized trial of 83 adults published in JAMA.
Acute respiratory distress syndrome (ARDS) can be treated using a face mask, but the mask is often inadequate, forcing patients to undergo intubation that can lead to additional problems including discomfort, delirium, and muscle deterioration, wrote Tianna Hicklin, Ph.D., in a column on the NIH website.
“The proposed mechanism for improved efficacy of these helmets is the preservation of applied pressures and avoidance of air leak. If the helmets indeed do allow clinicians both to be able to increase airway pressures above levels they typically would with mask-NIV and maintain those pressures without unpredictable system leak, that would be of great physiologic importance for patients with acute respiratory failure,” said Dr. Eric J. Gartman.
To explore the potential of noninvasive ventilation (NIV) using a helmet instead of a mask, both of which allow patients to remain awake in the ICU, the researchers randomized 83 adults with ARDS to treatment with either a helmet (44 patients) or a face mask (39 patients).
Intubation incidence was 18% in patients treated with helmets, compared with 62% for those treated with face masks. In addition, patients in the helmet group had significantly more ventilator-free days than the mask group (28 vs. 13; P less than .001), and both hospital mortality and 90-day mortality rates were significantly lower in the helmet group compared to the mask group (27% vs. 49%; P = .04 and 34% vs. 56%; P = .02, respectively)
Adverse event rates were rare, and similar between the helmet and mask groups. Three interface-related skin ulcers occurred in each group; nose ulcers in 7% of the mask group and neck ulcers in 7% of the helmet group.
The study population included adults aged 18 years and older who were admitted to the ICU at the University of Chicago between September 2012 and September 2015 and required face mask NIV. The average age of the patients was 58 years in the helmet group and 61 years in the mask group; there were no significant demographic differences between the groups. The most common causes of acute respiratory failure in both groups were pneumonia and pneumonia caused by immunosuppression.
The study results were limited by several factors including a lack of blinding, the need for a learning curve for clinicians using the helmet, and the potential for patient-ventilator dyssynchrony in the helmet group, noted Dr. Bhakti K. Patel of the University of Chicago and her colleagues (JAMA 2016;315:2435-41). Multicenter studies are needed to support the findings, they added. However, the findings “affirm the far-reaching benefits of spontaneous yet highly supported ventilation in an awake, animated patient over invasive medical ventilation via endotracheal tube,” they wrote. “These findings warrant further investigation of helmet NIV for patients with ARDS and other types of AHRF [acute hypoxemic respiratory failure], particularly with attention to long-term outcomes.”
The researchers had no financial conflicts to disclose.
“While the results of this study are very impressive, it is a single-center study, and obviously a larger multicenter trial (with all types of institutions included – not just large academic centers) would be helpful to elucidate the benefit of this technique and support a change in standard of care in the use of NIV. A change to this system would be a very large culture shift in NIV and would mean a significant amount of training (physician, nursing, respiratory care), purchasing the helmets, and ensuring that it is implemented properly and safely. As stated by the authors, this fact is similar to the change the occurred originally with NIV – but if their results reflect a true benefit over FM-NIV [face mask-noninvasive ventilation], such a large change would certainly be worth the effort,” Dr. Gartman said.
In a related study published in the Journal of Cardiothoracic and Vascular Anesthesia, patients treated with noninvasive positive pressure ventilation (NPPV) through helmets had significantly lower heart rates, lower average arterial pressure, and improved left ventricular ejection fraction at the end of treatment, compared with patients treated with ventilation masks and controls. Dr. Yi Yang of Capital Medical University in Beijing, China, and colleagues conducted the prospective study of 75 adults experiencing hypoxemia within 24 hours of extubation after Stanford type A aortic dissection. The participants were divided into three 25-patient groups. The control group was treated with high-flux inhalation of oxygen via a Venturi mask, another group was treated with NPPV via a mask, and the third group was treated with NPPV via a helmet. (J Card Vasc Anesth. 2016. http://dx.doi.org/10.1053/j.jvca.2016.03.129).
The study was funded by China’s public welfare industry of health.
Treating acute respiratory distress syndrome patients with helmets instead of face masks significantly reduced intubation rates and 90-day mortality rates, based on data from a randomized trial of 83 adults published in JAMA.
Acute respiratory distress syndrome (ARDS) can be treated using a face mask, but the mask is often inadequate, forcing patients to undergo intubation that can lead to additional problems including discomfort, delirium, and muscle deterioration, wrote Tianna Hicklin, Ph.D., in a column on the NIH website.
“The proposed mechanism for improved efficacy of these helmets is the preservation of applied pressures and avoidance of air leak. If the helmets indeed do allow clinicians both to be able to increase airway pressures above levels they typically would with mask-NIV and maintain those pressures without unpredictable system leak, that would be of great physiologic importance for patients with acute respiratory failure,” said Dr. Eric J. Gartman.
To explore the potential of noninvasive ventilation (NIV) using a helmet instead of a mask, both of which allow patients to remain awake in the ICU, the researchers randomized 83 adults with ARDS to treatment with either a helmet (44 patients) or a face mask (39 patients).
Intubation incidence was 18% in patients treated with helmets, compared with 62% for those treated with face masks. In addition, patients in the helmet group had significantly more ventilator-free days than the mask group (28 vs. 13; P less than .001), and both hospital mortality and 90-day mortality rates were significantly lower in the helmet group compared to the mask group (27% vs. 49%; P = .04 and 34% vs. 56%; P = .02, respectively)
Adverse event rates were rare, and similar between the helmet and mask groups. Three interface-related skin ulcers occurred in each group; nose ulcers in 7% of the mask group and neck ulcers in 7% of the helmet group.
The study population included adults aged 18 years and older who were admitted to the ICU at the University of Chicago between September 2012 and September 2015 and required face mask NIV. The average age of the patients was 58 years in the helmet group and 61 years in the mask group; there were no significant demographic differences between the groups. The most common causes of acute respiratory failure in both groups were pneumonia and pneumonia caused by immunosuppression.
The study results were limited by several factors including a lack of blinding, the need for a learning curve for clinicians using the helmet, and the potential for patient-ventilator dyssynchrony in the helmet group, noted Dr. Bhakti K. Patel of the University of Chicago and her colleagues (JAMA 2016;315:2435-41). Multicenter studies are needed to support the findings, they added. However, the findings “affirm the far-reaching benefits of spontaneous yet highly supported ventilation in an awake, animated patient over invasive medical ventilation via endotracheal tube,” they wrote. “These findings warrant further investigation of helmet NIV for patients with ARDS and other types of AHRF [acute hypoxemic respiratory failure], particularly with attention to long-term outcomes.”
The researchers had no financial conflicts to disclose.
“While the results of this study are very impressive, it is a single-center study, and obviously a larger multicenter trial (with all types of institutions included – not just large academic centers) would be helpful to elucidate the benefit of this technique and support a change in standard of care in the use of NIV. A change to this system would be a very large culture shift in NIV and would mean a significant amount of training (physician, nursing, respiratory care), purchasing the helmets, and ensuring that it is implemented properly and safely. As stated by the authors, this fact is similar to the change the occurred originally with NIV – but if their results reflect a true benefit over FM-NIV [face mask-noninvasive ventilation], such a large change would certainly be worth the effort,” Dr. Gartman said.
In a related study published in the Journal of Cardiothoracic and Vascular Anesthesia, patients treated with noninvasive positive pressure ventilation (NPPV) through helmets had significantly lower heart rates, lower average arterial pressure, and improved left ventricular ejection fraction at the end of treatment, compared with patients treated with ventilation masks and controls. Dr. Yi Yang of Capital Medical University in Beijing, China, and colleagues conducted the prospective study of 75 adults experiencing hypoxemia within 24 hours of extubation after Stanford type A aortic dissection. The participants were divided into three 25-patient groups. The control group was treated with high-flux inhalation of oxygen via a Venturi mask, another group was treated with NPPV via a mask, and the third group was treated with NPPV via a helmet. (J Card Vasc Anesth. 2016. http://dx.doi.org/10.1053/j.jvca.2016.03.129).
The study was funded by China’s public welfare industry of health.
FROM JAMA
Key clinical point: Patients with ARDS who were treated with noninvasive continuous positive airway pressure ventilation via a helmet needed significantly less intubation and had significantly higher survival rates through 90 days than did those treated with noninvasive ventilation via face masks.
Major finding: Intubation incidence was 18% in patients treated with helmets vs. 62% for those treated with face masks; 90-day survival rates for the helmet and mask groups were 66% and 44%, respectively.
Data source: A randomized, single center study of 83 patients with ARDS.
Disclosures: The researchers had no financial conflicts to disclose. The study was funded in part by the National Heart, Lung, and Blood Institute at the National Institutes of Health.
Updated Behçet’s disease recommendations expand biologic treatment
LONDON – A EULAR task force issued the first update to recommendations for managing Behçet’s disease since 2008, with revised recommendations that reflect expanded use of biologic agents, and increased evidence to guide management of gastrointestinal involvement, use of anticoagulants in patients with venous involvement, and use of surgical and interventional treatments, Dr. Gülen Hatemi said while presenting the update at the European Congress of Rheumatology.
The task force, which included more than 20 members, identified 304 articles to apply to the update, and produced five overarching principal and 18 specific recommendations divided among six categories of clinical manifestations of Behçet’s disease, said Dr. Hatemi, convenor of the task force and a rheumatologist at Istanbul University.
For mucocutaneous involvement, the update included five items that all received a “strong” recommendation from the task force: For an oral or genital ulcer, use a topical agent, such as a local steroid. Try colchicine first to prevent recurrent mucocutaneous lesions, especially when the dominant lesion is erythema nodosum or a genital ulcer. Treat papulopustular or acnelike lesions with topical or systemic agents, as when treating acne vulgaris. Coordinate treatment of leg ulcers, which can be caused by venous stasis or obliterative vasculitis, with a dermatologist and vascular surgeon. And azathioprine, thalidomide, interferon-alpha, a tumor necrosis factor (TNF)–alpha antagonist, or apremilast (Otezla) may be necessary for selected patients.
The task force issued two strong recommendations for managing eye involvement along with one conditional recommendation. The first strong recommendation was that managing uveitis requires close collaboration with an ophthalmologist, with the goal of inducing and maintaining remission. Patients with an inflammatory eye disease affecting the posterior segment should receive treatment with azathioprine, cyclosporine, interferon-alpha, or a monoclonal TNF-alpha antagonist. Treatment with a systemic corticosteroid should occur only when combined with azathioprine or another systemic immunosuppressant.
The second strong recommendation was that patients who present with an initial or recurrent acute episode of sight-threatening uveitis should receive treatment with a high-dose glucocorticoid, infliximab, or interferon-alpha. Intravitreal injection with a glucocorticoid as an adjunct to systemic therapy is an option for patients with a unilateral exacerbation. The conditional recommendation was for patients with isolated anterior uveitis. When these patients have markers of a poor prognosis – such as young age, male sex, or early disease onset – systemic treatment with an immunosuppressant is a possible option.
The panel issued three strong recommendations along with one conditional recommendation for managing vascular involvement. One of the strong recommendations called for treating acute deep vein thrombosis with a glucocorticoid as well as an immunosuppresant such as azathioprine, cyclophosphamide, or cyclosporine. A conditional recommendation said patients with refractory venous thrombosis could be considered for treatment with a monoclonal TNF-alpha antagonist, along with an anticoagulant if the patient’s risk for bleeding was generally low and a coexistent pulmonary artery aneurysm was ruled out.
Management of arterial aneurysms received the other two strong recommendations. The panel recommended high-dose glucocorticoid plus cyclophosphamide for a pulmonary artery aneurysm, followed by a monoclonal TNF-alpha antagonist for refractory cases. Patients with these aneurysms who are at high risk for major bleeding should undergo embolization in preference to open surgery. When patients have aortic or peripheral artery aneurysms, treatment should start with cyclophosphamide and a corticosteroid before an aneurysm repair is attempted. But surgery or stenting of the aneurysm should not be delayed when patients are symptomatic.
Gastrointestinal involvement received one strong and two conditional recommendations. The panel strongly recommended confirming gastrointestinal involvement using endoscopy, imaging, or both, while also ruling out treatment with a nonsteroidal anti-inflammatory drug, inflammatory bowel disease, or an infection such as tuberculosis as the cause of gastrointestinal symptoms. One of the conditional recommendations called for an urgent surgical consult when patients have perforation, major bleeding, or obstruction. The second conditional recommendation called for considering glucocorticoid treatment to treat an acute exacerbation of gastrointestinal involvement. Additional treatment options to pair with a glucocorticoid include a disease-modifying drug such as 5-aminosalicylic acid or azathioprine. For patients with severe or refractory gastrointestinal symptoms or both, a monoclonal TNF-alpha antagonist or thalidomide is another potential option.
The panel issued two strong recommendations for managing nervous system involvement. The top treatment option for parenchymal involvement is a high-dose glucocorticoid followed by slow tapering while also treating with an immunosuppressant such as azathioprine. Treatment with cyclosporine should be avoided, the panel said. Treatment with a monoclonal TNF-alpha antagonist is an option to consider as first-line treatment for patients with severe nervous system involvement or for those with refractory disease. The second strong recommendation was to treat a cerebral venous thrombus with a high-dose glucocorticoid followed by tapering, with short-term anticoagulant treatment as an option. Patients also need screening for the presence of vascular disease at an extracranial location.
The panel’s final recommendation was a strong endorsement of colchicine as first-line treatment for arthritis in Behçet’s patients, although patients with acute monoarticular disease can be managed with an intra-articular injection of a glucocorticoid. For patients with recurrent or chronic arthritis, treatment options include azathioprine, interferon-alpha, or a TNF-alpha antagonist.
Dr. Hatemi has received research support from, received honoraria from, or has been a speaker for AbbVie, Celgene, Merck Sharp & Dohme, and Pfizer.
On Twitter @mitchelzoler
LONDON – A EULAR task force issued the first update to recommendations for managing Behçet’s disease since 2008, with revised recommendations that reflect expanded use of biologic agents, and increased evidence to guide management of gastrointestinal involvement, use of anticoagulants in patients with venous involvement, and use of surgical and interventional treatments, Dr. Gülen Hatemi said while presenting the update at the European Congress of Rheumatology.
The task force, which included more than 20 members, identified 304 articles to apply to the update, and produced five overarching principal and 18 specific recommendations divided among six categories of clinical manifestations of Behçet’s disease, said Dr. Hatemi, convenor of the task force and a rheumatologist at Istanbul University.
For mucocutaneous involvement, the update included five items that all received a “strong” recommendation from the task force: For an oral or genital ulcer, use a topical agent, such as a local steroid. Try colchicine first to prevent recurrent mucocutaneous lesions, especially when the dominant lesion is erythema nodosum or a genital ulcer. Treat papulopustular or acnelike lesions with topical or systemic agents, as when treating acne vulgaris. Coordinate treatment of leg ulcers, which can be caused by venous stasis or obliterative vasculitis, with a dermatologist and vascular surgeon. And azathioprine, thalidomide, interferon-alpha, a tumor necrosis factor (TNF)–alpha antagonist, or apremilast (Otezla) may be necessary for selected patients.
The task force issued two strong recommendations for managing eye involvement along with one conditional recommendation. The first strong recommendation was that managing uveitis requires close collaboration with an ophthalmologist, with the goal of inducing and maintaining remission. Patients with an inflammatory eye disease affecting the posterior segment should receive treatment with azathioprine, cyclosporine, interferon-alpha, or a monoclonal TNF-alpha antagonist. Treatment with a systemic corticosteroid should occur only when combined with azathioprine or another systemic immunosuppressant.
The second strong recommendation was that patients who present with an initial or recurrent acute episode of sight-threatening uveitis should receive treatment with a high-dose glucocorticoid, infliximab, or interferon-alpha. Intravitreal injection with a glucocorticoid as an adjunct to systemic therapy is an option for patients with a unilateral exacerbation. The conditional recommendation was for patients with isolated anterior uveitis. When these patients have markers of a poor prognosis – such as young age, male sex, or early disease onset – systemic treatment with an immunosuppressant is a possible option.
The panel issued three strong recommendations along with one conditional recommendation for managing vascular involvement. One of the strong recommendations called for treating acute deep vein thrombosis with a glucocorticoid as well as an immunosuppresant such as azathioprine, cyclophosphamide, or cyclosporine. A conditional recommendation said patients with refractory venous thrombosis could be considered for treatment with a monoclonal TNF-alpha antagonist, along with an anticoagulant if the patient’s risk for bleeding was generally low and a coexistent pulmonary artery aneurysm was ruled out.
Management of arterial aneurysms received the other two strong recommendations. The panel recommended high-dose glucocorticoid plus cyclophosphamide for a pulmonary artery aneurysm, followed by a monoclonal TNF-alpha antagonist for refractory cases. Patients with these aneurysms who are at high risk for major bleeding should undergo embolization in preference to open surgery. When patients have aortic or peripheral artery aneurysms, treatment should start with cyclophosphamide and a corticosteroid before an aneurysm repair is attempted. But surgery or stenting of the aneurysm should not be delayed when patients are symptomatic.
Gastrointestinal involvement received one strong and two conditional recommendations. The panel strongly recommended confirming gastrointestinal involvement using endoscopy, imaging, or both, while also ruling out treatment with a nonsteroidal anti-inflammatory drug, inflammatory bowel disease, or an infection such as tuberculosis as the cause of gastrointestinal symptoms. One of the conditional recommendations called for an urgent surgical consult when patients have perforation, major bleeding, or obstruction. The second conditional recommendation called for considering glucocorticoid treatment to treat an acute exacerbation of gastrointestinal involvement. Additional treatment options to pair with a glucocorticoid include a disease-modifying drug such as 5-aminosalicylic acid or azathioprine. For patients with severe or refractory gastrointestinal symptoms or both, a monoclonal TNF-alpha antagonist or thalidomide is another potential option.
The panel issued two strong recommendations for managing nervous system involvement. The top treatment option for parenchymal involvement is a high-dose glucocorticoid followed by slow tapering while also treating with an immunosuppressant such as azathioprine. Treatment with cyclosporine should be avoided, the panel said. Treatment with a monoclonal TNF-alpha antagonist is an option to consider as first-line treatment for patients with severe nervous system involvement or for those with refractory disease. The second strong recommendation was to treat a cerebral venous thrombus with a high-dose glucocorticoid followed by tapering, with short-term anticoagulant treatment as an option. Patients also need screening for the presence of vascular disease at an extracranial location.
The panel’s final recommendation was a strong endorsement of colchicine as first-line treatment for arthritis in Behçet’s patients, although patients with acute monoarticular disease can be managed with an intra-articular injection of a glucocorticoid. For patients with recurrent or chronic arthritis, treatment options include azathioprine, interferon-alpha, or a TNF-alpha antagonist.
Dr. Hatemi has received research support from, received honoraria from, or has been a speaker for AbbVie, Celgene, Merck Sharp & Dohme, and Pfizer.
On Twitter @mitchelzoler
LONDON – A EULAR task force issued the first update to recommendations for managing Behçet’s disease since 2008, with revised recommendations that reflect expanded use of biologic agents, and increased evidence to guide management of gastrointestinal involvement, use of anticoagulants in patients with venous involvement, and use of surgical and interventional treatments, Dr. Gülen Hatemi said while presenting the update at the European Congress of Rheumatology.
The task force, which included more than 20 members, identified 304 articles to apply to the update, and produced five overarching principal and 18 specific recommendations divided among six categories of clinical manifestations of Behçet’s disease, said Dr. Hatemi, convenor of the task force and a rheumatologist at Istanbul University.
For mucocutaneous involvement, the update included five items that all received a “strong” recommendation from the task force: For an oral or genital ulcer, use a topical agent, such as a local steroid. Try colchicine first to prevent recurrent mucocutaneous lesions, especially when the dominant lesion is erythema nodosum or a genital ulcer. Treat papulopustular or acnelike lesions with topical or systemic agents, as when treating acne vulgaris. Coordinate treatment of leg ulcers, which can be caused by venous stasis or obliterative vasculitis, with a dermatologist and vascular surgeon. And azathioprine, thalidomide, interferon-alpha, a tumor necrosis factor (TNF)–alpha antagonist, or apremilast (Otezla) may be necessary for selected patients.
The task force issued two strong recommendations for managing eye involvement along with one conditional recommendation. The first strong recommendation was that managing uveitis requires close collaboration with an ophthalmologist, with the goal of inducing and maintaining remission. Patients with an inflammatory eye disease affecting the posterior segment should receive treatment with azathioprine, cyclosporine, interferon-alpha, or a monoclonal TNF-alpha antagonist. Treatment with a systemic corticosteroid should occur only when combined with azathioprine or another systemic immunosuppressant.
The second strong recommendation was that patients who present with an initial or recurrent acute episode of sight-threatening uveitis should receive treatment with a high-dose glucocorticoid, infliximab, or interferon-alpha. Intravitreal injection with a glucocorticoid as an adjunct to systemic therapy is an option for patients with a unilateral exacerbation. The conditional recommendation was for patients with isolated anterior uveitis. When these patients have markers of a poor prognosis – such as young age, male sex, or early disease onset – systemic treatment with an immunosuppressant is a possible option.
The panel issued three strong recommendations along with one conditional recommendation for managing vascular involvement. One of the strong recommendations called for treating acute deep vein thrombosis with a glucocorticoid as well as an immunosuppresant such as azathioprine, cyclophosphamide, or cyclosporine. A conditional recommendation said patients with refractory venous thrombosis could be considered for treatment with a monoclonal TNF-alpha antagonist, along with an anticoagulant if the patient’s risk for bleeding was generally low and a coexistent pulmonary artery aneurysm was ruled out.
Management of arterial aneurysms received the other two strong recommendations. The panel recommended high-dose glucocorticoid plus cyclophosphamide for a pulmonary artery aneurysm, followed by a monoclonal TNF-alpha antagonist for refractory cases. Patients with these aneurysms who are at high risk for major bleeding should undergo embolization in preference to open surgery. When patients have aortic or peripheral artery aneurysms, treatment should start with cyclophosphamide and a corticosteroid before an aneurysm repair is attempted. But surgery or stenting of the aneurysm should not be delayed when patients are symptomatic.
Gastrointestinal involvement received one strong and two conditional recommendations. The panel strongly recommended confirming gastrointestinal involvement using endoscopy, imaging, or both, while also ruling out treatment with a nonsteroidal anti-inflammatory drug, inflammatory bowel disease, or an infection such as tuberculosis as the cause of gastrointestinal symptoms. One of the conditional recommendations called for an urgent surgical consult when patients have perforation, major bleeding, or obstruction. The second conditional recommendation called for considering glucocorticoid treatment to treat an acute exacerbation of gastrointestinal involvement. Additional treatment options to pair with a glucocorticoid include a disease-modifying drug such as 5-aminosalicylic acid or azathioprine. For patients with severe or refractory gastrointestinal symptoms or both, a monoclonal TNF-alpha antagonist or thalidomide is another potential option.
The panel issued two strong recommendations for managing nervous system involvement. The top treatment option for parenchymal involvement is a high-dose glucocorticoid followed by slow tapering while also treating with an immunosuppressant such as azathioprine. Treatment with cyclosporine should be avoided, the panel said. Treatment with a monoclonal TNF-alpha antagonist is an option to consider as first-line treatment for patients with severe nervous system involvement or for those with refractory disease. The second strong recommendation was to treat a cerebral venous thrombus with a high-dose glucocorticoid followed by tapering, with short-term anticoagulant treatment as an option. Patients also need screening for the presence of vascular disease at an extracranial location.
The panel’s final recommendation was a strong endorsement of colchicine as first-line treatment for arthritis in Behçet’s patients, although patients with acute monoarticular disease can be managed with an intra-articular injection of a glucocorticoid. For patients with recurrent or chronic arthritis, treatment options include azathioprine, interferon-alpha, or a TNF-alpha antagonist.
Dr. Hatemi has received research support from, received honoraria from, or has been a speaker for AbbVie, Celgene, Merck Sharp & Dohme, and Pfizer.
On Twitter @mitchelzoler
AT THE EULAR 2016 CONGRESS
Hospital-acquired respiratory viruses cause significant morbidity, mortality
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
AT ASM MICROBE 2016
Key clinical point: Hospital-acquired respiratory viral illnesses had a 39% mortality rate.
Major finding: Of 44 symptomatic patients with positive respiratory virus panel screens, 17 died and 2/3 of the survivors went to advanced care settings on discharge.
Data source: Retrospective multisite chart review of 44 patients with HA-RVIs and positive RVP screens.
Disclosures: No external funding source was reported, and the study authors had no disclosures.