User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Higher potency of fentanyl affects addiction treatment, screening
As fentanyl-related overdose deaths continue to increase, clinicians should take note of important differences that set the drug apart from the other drugs of misuse – and the troubling reality that fentanyl now contaminates most of them.
“It would be fair to tell patients, if you’re buying any illicit drugs – pills, powder, liquid, whatever it is, you’ve got to assume it’s either contaminated with or replaced by fentanyl,” said Edwin Salsitz, MD, an associate clinical professor at the Icahn School of Medicine at Mount Sinai, New York, during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In many if not most cases, he noted, patients become addicted to fentanyl unknowingly. They assume they are ingesting oxycodone, cocaine, or another drug, and have no realization that they are even exposed to fentanyl until they test positive for it – or overdose.
Meanwhile, the high potency of fentanyl can overcome the opioid blockade of addiction treatment therapies – methadone and buprenorphine – that take away the high that users get from less potent drugs such as heroin.
“Fentanyl is overcoming this blockade that methadone and buprenorphine used to provide,” Dr. Salsitz said. “With fentanyl having such a higher potency, patients are saying ‘no, I still feel the fentanyl effects,’ and they continue feeling it even with 200 milligrams of methadone or 24 milligrams of buprenorphine.”
‘Wooden chest syndrome’
Among the lesser-known dangers of fentanyl is the possibility that some overdose deaths may occur as the result of a syndrome previously reported as a rare complication following the medical use of fentanyl in critically ill patients – fentanyl-induced chest-wall rigidity, or “wooden chest syndrome,” Dr. Salsitz explained.
In such cases, the muscles of respiration become rigid and paralyzed, causing suffocation within a matter of minutes – too soon to benefit from the overdose rescue medication naloxone.
In one recent study published in Clinical Toxicology , nearly half of fentanyl overdose deaths were found to have occurred even before the body had a chance to produce norfentanyl, a metabolite of fentanyl that takes only about 2-3 minutes to appear in the system, suggesting the deaths occurred rapidly.
In the study of 48 fentanyl deaths, no appreciable concentrations of norfentanyl could be detected in 20 of the 48 overdose deaths (42%), and concentrations were less than 1 ng/mL in 25 cases (52%).
“The lack of any measurable norfentanyl in half of our cases suggests a very rapid death, consistent with acute chest rigidity,” the authors reported.
“In several cases fentanyl concentrations were strikingly high (22 ng/mL and 20 ng/mL) with no norfentanyl detected,” they said.
Dr. Salsitz noted that the syndrome is not well known among the addiction treatment community.
“This is different than the usual respiratory opioid overdose where there’s a gradual decrease in the breathing rate and a gradual decrease in how much air is going in and out of the lungs,” Dr. Salsitz explained.
“With those cases, some may survive for an hour or longer, allowing time for someone to administer naloxone or to get the patient to the emergency room,” he said. “But with this, breathing stops and people can die within minutes.
“I think that this is one of the reasons that fentanyl deaths keep going up despite more and more naloxone availability out there,” he said.
Clearance may take longer
In toxicology testing for fentanyl, clinicians should also note the important difference between fentanyl and other opioids – that fentanyl, because of its high lipophilicity, may be detected in urine toxicology testing up to 3 weeks after last use. This is much longer than the 2- to 4-day clearance observed with other opioids, possibly causing patients to continue to test positive for the drug weeks after cessation.
This effect was observed in one recent study of 12 opioid use disorder patients in a residential treatment program who had previously been exposed to daily fentanyl.
The study showed the mean amount of time of fentanyl clearance was 2 weeks, with a range of 4-26 days after last use.
The authors pointed out that the findings “might explain recent reports of difficulty in buprenorphine inductions for persons who use fentanyl, and point to a need to better understand the pharmacokinetics of fentanyl in the context of opioid withdrawal in persons who regularly use fentanyl.”
Though the study was small, Dr. Salsitz said “that’s not a stumbling block to the important finding that, with regular use of fentanyl, the drug may stay in the urine for a long time.”
Dr. Salsitz noted that similar observations have been made at his center, with clinicians logically assuming that patients were still somehow getting fentanyl.
“When we initially found this in patients, we thought that they were using on the unit, perhaps that they brought in the fentanyl, because otherwise how could it stay in the urine that long,” he noted. “But fentanyl appears to be more lipophilic and gets into the fat; it’s then excreted very slowly and then stays in the urine.”
Dr. Salsitz said most practitioners think of fentanyl as a short-acting drug, so “it’s important to realize that people may continue to test positive and it should be thought of as a long-acting opioid.”
Opiate screening tests don’t work
Dr. Salsitz warned of another misconception in fentanyl testing – the common mistake of assuming that fentanyl should show up in a test for opiates – when in fact fentanyl is not, technically, an opiate.
“The word opiate only refers to morphine, codeine, heroin and sometimes hydrocodone,” he explained. “Other opioids are classified as semisynthetic, such as oxycodone, or synthetics, such as fentanyl and methadone, buprenorphine.”
“In order to detect the synthetics, you must have a separate strip for each one of those drugs. They will not show up positive on a screen for opiates,” he noted.
The belief that fentanyl and other synthetic and semisynthetic opioids will show positive on an opiate screen is a common misconception, he said. “The misunderstanding in toxicology interpretation is a problem for many practitioners, [but] it’s essential to understand because otherwise false assumptions about the patient will be considered.”
Another important testing misreading can occur with the antidepressant drug trazodone, which Dr. Salsitz cautioned may falsely test as positive for fentanyl on immunoassays.
“Trazodone is very commonly used in addiction treatment centers, but it can give a false positive on the fentanyl immunoassay and we’ve had a number of those cases,” he said.
Dr. Salsitz had no disclosures to report.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
As fentanyl-related overdose deaths continue to increase, clinicians should take note of important differences that set the drug apart from the other drugs of misuse – and the troubling reality that fentanyl now contaminates most of them.
“It would be fair to tell patients, if you’re buying any illicit drugs – pills, powder, liquid, whatever it is, you’ve got to assume it’s either contaminated with or replaced by fentanyl,” said Edwin Salsitz, MD, an associate clinical professor at the Icahn School of Medicine at Mount Sinai, New York, during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In many if not most cases, he noted, patients become addicted to fentanyl unknowingly. They assume they are ingesting oxycodone, cocaine, or another drug, and have no realization that they are even exposed to fentanyl until they test positive for it – or overdose.
Meanwhile, the high potency of fentanyl can overcome the opioid blockade of addiction treatment therapies – methadone and buprenorphine – that take away the high that users get from less potent drugs such as heroin.
“Fentanyl is overcoming this blockade that methadone and buprenorphine used to provide,” Dr. Salsitz said. “With fentanyl having such a higher potency, patients are saying ‘no, I still feel the fentanyl effects,’ and they continue feeling it even with 200 milligrams of methadone or 24 milligrams of buprenorphine.”
‘Wooden chest syndrome’
Among the lesser-known dangers of fentanyl is the possibility that some overdose deaths may occur as the result of a syndrome previously reported as a rare complication following the medical use of fentanyl in critically ill patients – fentanyl-induced chest-wall rigidity, or “wooden chest syndrome,” Dr. Salsitz explained.
In such cases, the muscles of respiration become rigid and paralyzed, causing suffocation within a matter of minutes – too soon to benefit from the overdose rescue medication naloxone.
In one recent study published in Clinical Toxicology , nearly half of fentanyl overdose deaths were found to have occurred even before the body had a chance to produce norfentanyl, a metabolite of fentanyl that takes only about 2-3 minutes to appear in the system, suggesting the deaths occurred rapidly.
In the study of 48 fentanyl deaths, no appreciable concentrations of norfentanyl could be detected in 20 of the 48 overdose deaths (42%), and concentrations were less than 1 ng/mL in 25 cases (52%).
“The lack of any measurable norfentanyl in half of our cases suggests a very rapid death, consistent with acute chest rigidity,” the authors reported.
“In several cases fentanyl concentrations were strikingly high (22 ng/mL and 20 ng/mL) with no norfentanyl detected,” they said.
Dr. Salsitz noted that the syndrome is not well known among the addiction treatment community.
“This is different than the usual respiratory opioid overdose where there’s a gradual decrease in the breathing rate and a gradual decrease in how much air is going in and out of the lungs,” Dr. Salsitz explained.
“With those cases, some may survive for an hour or longer, allowing time for someone to administer naloxone or to get the patient to the emergency room,” he said. “But with this, breathing stops and people can die within minutes.
“I think that this is one of the reasons that fentanyl deaths keep going up despite more and more naloxone availability out there,” he said.
Clearance may take longer
In toxicology testing for fentanyl, clinicians should also note the important difference between fentanyl and other opioids – that fentanyl, because of its high lipophilicity, may be detected in urine toxicology testing up to 3 weeks after last use. This is much longer than the 2- to 4-day clearance observed with other opioids, possibly causing patients to continue to test positive for the drug weeks after cessation.
This effect was observed in one recent study of 12 opioid use disorder patients in a residential treatment program who had previously been exposed to daily fentanyl.
The study showed the mean amount of time of fentanyl clearance was 2 weeks, with a range of 4-26 days after last use.
The authors pointed out that the findings “might explain recent reports of difficulty in buprenorphine inductions for persons who use fentanyl, and point to a need to better understand the pharmacokinetics of fentanyl in the context of opioid withdrawal in persons who regularly use fentanyl.”
Though the study was small, Dr. Salsitz said “that’s not a stumbling block to the important finding that, with regular use of fentanyl, the drug may stay in the urine for a long time.”
Dr. Salsitz noted that similar observations have been made at his center, with clinicians logically assuming that patients were still somehow getting fentanyl.
“When we initially found this in patients, we thought that they were using on the unit, perhaps that they brought in the fentanyl, because otherwise how could it stay in the urine that long,” he noted. “But fentanyl appears to be more lipophilic and gets into the fat; it’s then excreted very slowly and then stays in the urine.”
Dr. Salsitz said most practitioners think of fentanyl as a short-acting drug, so “it’s important to realize that people may continue to test positive and it should be thought of as a long-acting opioid.”
Opiate screening tests don’t work
Dr. Salsitz warned of another misconception in fentanyl testing – the common mistake of assuming that fentanyl should show up in a test for opiates – when in fact fentanyl is not, technically, an opiate.
“The word opiate only refers to morphine, codeine, heroin and sometimes hydrocodone,” he explained. “Other opioids are classified as semisynthetic, such as oxycodone, or synthetics, such as fentanyl and methadone, buprenorphine.”
“In order to detect the synthetics, you must have a separate strip for each one of those drugs. They will not show up positive on a screen for opiates,” he noted.
The belief that fentanyl and other synthetic and semisynthetic opioids will show positive on an opiate screen is a common misconception, he said. “The misunderstanding in toxicology interpretation is a problem for many practitioners, [but] it’s essential to understand because otherwise false assumptions about the patient will be considered.”
Another important testing misreading can occur with the antidepressant drug trazodone, which Dr. Salsitz cautioned may falsely test as positive for fentanyl on immunoassays.
“Trazodone is very commonly used in addiction treatment centers, but it can give a false positive on the fentanyl immunoassay and we’ve had a number of those cases,” he said.
Dr. Salsitz had no disclosures to report.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
As fentanyl-related overdose deaths continue to increase, clinicians should take note of important differences that set the drug apart from the other drugs of misuse – and the troubling reality that fentanyl now contaminates most of them.
“It would be fair to tell patients, if you’re buying any illicit drugs – pills, powder, liquid, whatever it is, you’ve got to assume it’s either contaminated with or replaced by fentanyl,” said Edwin Salsitz, MD, an associate clinical professor at the Icahn School of Medicine at Mount Sinai, New York, during a presentation on the subject at the 21st Annual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
In many if not most cases, he noted, patients become addicted to fentanyl unknowingly. They assume they are ingesting oxycodone, cocaine, or another drug, and have no realization that they are even exposed to fentanyl until they test positive for it – or overdose.
Meanwhile, the high potency of fentanyl can overcome the opioid blockade of addiction treatment therapies – methadone and buprenorphine – that take away the high that users get from less potent drugs such as heroin.
“Fentanyl is overcoming this blockade that methadone and buprenorphine used to provide,” Dr. Salsitz said. “With fentanyl having such a higher potency, patients are saying ‘no, I still feel the fentanyl effects,’ and they continue feeling it even with 200 milligrams of methadone or 24 milligrams of buprenorphine.”
‘Wooden chest syndrome’
Among the lesser-known dangers of fentanyl is the possibility that some overdose deaths may occur as the result of a syndrome previously reported as a rare complication following the medical use of fentanyl in critically ill patients – fentanyl-induced chest-wall rigidity, or “wooden chest syndrome,” Dr. Salsitz explained.
In such cases, the muscles of respiration become rigid and paralyzed, causing suffocation within a matter of minutes – too soon to benefit from the overdose rescue medication naloxone.
In one recent study published in Clinical Toxicology , nearly half of fentanyl overdose deaths were found to have occurred even before the body had a chance to produce norfentanyl, a metabolite of fentanyl that takes only about 2-3 minutes to appear in the system, suggesting the deaths occurred rapidly.
In the study of 48 fentanyl deaths, no appreciable concentrations of norfentanyl could be detected in 20 of the 48 overdose deaths (42%), and concentrations were less than 1 ng/mL in 25 cases (52%).
“The lack of any measurable norfentanyl in half of our cases suggests a very rapid death, consistent with acute chest rigidity,” the authors reported.
“In several cases fentanyl concentrations were strikingly high (22 ng/mL and 20 ng/mL) with no norfentanyl detected,” they said.
Dr. Salsitz noted that the syndrome is not well known among the addiction treatment community.
“This is different than the usual respiratory opioid overdose where there’s a gradual decrease in the breathing rate and a gradual decrease in how much air is going in and out of the lungs,” Dr. Salsitz explained.
“With those cases, some may survive for an hour or longer, allowing time for someone to administer naloxone or to get the patient to the emergency room,” he said. “But with this, breathing stops and people can die within minutes.
“I think that this is one of the reasons that fentanyl deaths keep going up despite more and more naloxone availability out there,” he said.
Clearance may take longer
In toxicology testing for fentanyl, clinicians should also note the important difference between fentanyl and other opioids – that fentanyl, because of its high lipophilicity, may be detected in urine toxicology testing up to 3 weeks after last use. This is much longer than the 2- to 4-day clearance observed with other opioids, possibly causing patients to continue to test positive for the drug weeks after cessation.
This effect was observed in one recent study of 12 opioid use disorder patients in a residential treatment program who had previously been exposed to daily fentanyl.
The study showed the mean amount of time of fentanyl clearance was 2 weeks, with a range of 4-26 days after last use.
The authors pointed out that the findings “might explain recent reports of difficulty in buprenorphine inductions for persons who use fentanyl, and point to a need to better understand the pharmacokinetics of fentanyl in the context of opioid withdrawal in persons who regularly use fentanyl.”
Though the study was small, Dr. Salsitz said “that’s not a stumbling block to the important finding that, with regular use of fentanyl, the drug may stay in the urine for a long time.”
Dr. Salsitz noted that similar observations have been made at his center, with clinicians logically assuming that patients were still somehow getting fentanyl.
“When we initially found this in patients, we thought that they were using on the unit, perhaps that they brought in the fentanyl, because otherwise how could it stay in the urine that long,” he noted. “But fentanyl appears to be more lipophilic and gets into the fat; it’s then excreted very slowly and then stays in the urine.”
Dr. Salsitz said most practitioners think of fentanyl as a short-acting drug, so “it’s important to realize that people may continue to test positive and it should be thought of as a long-acting opioid.”
Opiate screening tests don’t work
Dr. Salsitz warned of another misconception in fentanyl testing – the common mistake of assuming that fentanyl should show up in a test for opiates – when in fact fentanyl is not, technically, an opiate.
“The word opiate only refers to morphine, codeine, heroin and sometimes hydrocodone,” he explained. “Other opioids are classified as semisynthetic, such as oxycodone, or synthetics, such as fentanyl and methadone, buprenorphine.”
“In order to detect the synthetics, you must have a separate strip for each one of those drugs. They will not show up positive on a screen for opiates,” he noted.
The belief that fentanyl and other synthetic and semisynthetic opioids will show positive on an opiate screen is a common misconception, he said. “The misunderstanding in toxicology interpretation is a problem for many practitioners, [but] it’s essential to understand because otherwise false assumptions about the patient will be considered.”
Another important testing misreading can occur with the antidepressant drug trazodone, which Dr. Salsitz cautioned may falsely test as positive for fentanyl on immunoassays.
“Trazodone is very commonly used in addiction treatment centers, but it can give a false positive on the fentanyl immunoassay and we’ve had a number of those cases,” he said.
Dr. Salsitz had no disclosures to report.
The Psychopharmacology Update was sponsored by Medscape Live. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Looking for a healthy meat substitute? Consider the potato
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Newer agents for nosocomial pneumonia: The right drug for the right bug
“The right drug at the right time with the right dose for the right bug for the right duration.” That, said professor Kristina Crothers, MD, is the general guidance for optimizing antibiotic use (while awaiting an infectious disease consult). In her oral presentation at the annual meeting of the American College of Chest Physicians, “Choosing newer antibiotics for nosocomial pneumonia,” Dr. Crothers asked the question: “Beyond the guidelines: When should novel antimicrobials be used?”
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are the most common nosocomial infections at 22%, and are the leading cause of death attributable to hospital-acquired infections. They increase mortality by 20%-50%, with an economic burden of about $40,000 per patient. The incidence of multidrug-resistant (MDR) organism infections varies widely by locality, but several factors increase the likelihood: prior broad-spectrum antibiotic exposure within the past 90 days; longer hospitalization; indwelling vascular devices; tracheostomy; and ventilator dependence. The Centers for Disease Control and Prevention lists as “Serious Threat” the HAP/VAP MDR organisms methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa (PSA) with difficult-to-treat-resistance, and beta-lactamase producing Enterobacterales (ESBL). In the category of “Urgent Threat” the CDC lists: carbapenamase-resistant Enterobacterales (CRE) (carbapenamase producing or non–carbapenemase producing), and carbapenem-resistant Acinetobacter (CRAB), according to Dr. Crothers who is at the University of Washington Veterans Affairs Puget Sound Health Care System, Seattle.
Newer antibiotics for HAP/VAP that are still beyond the guidelines include telavancin and tedizolid as gram-positive agents, and as gram-negative ones: ceftazidime-avibactam, ceftolozane-tazobactam, cefiderocol, imipenem-cilastatin-relebactam and meropenem-vaborbactam, she added.
Tedizolid, Dr. Crothers stated, is a novel oxazolidinone, and is an alternative to vancomycin and linezolid for gram-positive HAP/VAP. In the VITAL noninferiority study versus linezolid with 726 patients, it was noninferior to linezolid for 28-day all-cause mortality (28% vs. 26%), but did not achieve noninferiority for investigator-assessed clinical cure (56% vs. 64%).
Televancin, a semisynthetic derivative of vancomycin, in the ATTAIN studies vs. vancomycin had overall similar cure rates. It is FDA-approved for S. aureus HAP/VAP but not other bacterial causes. It should be reserved for those who cannot receive vancomycin or linezolid, with normal renal function, according to Dr. Crothers. Excluded from first-line treatment of gram-positive HAP/VAP are daptomycin, ceftaroline, ceftobiprole, and tigecycline.
Ceftazidime-avibactam, a third-generation cephalosporin-plus novel beta-lactamase inhibitor has wide activity (Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, PSA and Haemophilus influenzae. It is also active against some extended-spectrum beta-lactamases (ESBLs), ampC beta-lactamases (AmpCs), and K. pneumoniae carbapenemase (KPC)–producing Enterobacterales, but not with metallo-beta-lactamases). Ceftazidime-avibactam is also indicated for HAP/VAP, and has a toxicity profile including nausea, vomiting, and diarrhea.
In the REPROVE trial of ceftazidime-avibactam vs. meropenem for 7-14 days with 527 clinically evaluable patients (37% K. pneumoniae, 30% P. aeruginosa, and 33%-35% VAP), the clinical cure at 21-25 days post randomization was 69% vs. 73%, respectively, with similar adverse events.
Ceftolozane-tazobactam, a novel fifth-generation cephalosporin plus a beta-lactamase inhibitor has activity against PSA including extensively drug-resistant PSA, AmpC, and ESBL-E, but it has limited activity against Acinetobacter and Stenotrophomonas. It is indicated for HAP/VAP, has reduced efficacy with creatine clearance of 50 mL/min or less, increases transaminases and renal impairment, and causes diarrhea. In ASPECT-NP (n = 726) ceftolozane-tazobactam versus meropenem for 8-14 days (HAP/VAP), showed a 28 day-mortality of 24% vs. 25%, respectively, with test of cure at 54% vs. 53% at 7-14 days post therapy. Adverse events were similar between groups.
Imipenem-cilastatin-relebactam, a novel beta-lactamase inhibitor plus carbapenem, is indicated for HAP/VAP and has activity against ESBL, CRE: KPC-producing Enterobacterales, PSA including AmpC. It can cause seizures (requires caution with central nervous system disorders and renal impairment). It increases transaminases, anemia, diarrhea, and reduces potassium and sodium. In RESTORE-IMI 2 (n = 537 with HAP/VAP) it was noninferior for 28-day all-cause mortality vs. piperacillin and tazobactam (16% vs. 21%), with similar adverse events.
Cefiderocol, a siderophore cephalosporin, is indicated for HAP/VAP. It has a wide spectrum of activity: ESBL, CRE, CR PSA, Stenotrophomonas maltophilia, Acinetobacter baumanii, Streptococcus.) It increases transaminases, diarrhea, and atrial fibrillation, and it reduces potassium and magnesium. In APEKS-NP versus linezolid plus cefiderocol or extended meropenem infusion (HAP/VAP n = 292; gram-negative pneumonia = 251; 60% invasive mechanical ventilation) it was noninferior for 14-day all-cause mortality (12.4% vs. 11.6%) with similar adverse events. In CREDIBLE-CR vs. best available therapy for carbapenem-resistant gram-negative infections, clinical cure rates were similar (50% vs. 53% in 59 HAP/VAP patients at 7 days), but with more deaths in the cefiderocol arm. Adverse events were > 90% in both groups and 34% vs. 19% died, mostly with Acinetobacter.
Meropenem-vaborbactam, a novel beta-lactamase inhibitor plus carbapenem, is approved and indicated for HAP/VAP in Europe. It has activity against MDR, Enterobacterales including CRE. Its toxicities include headache, phlebitis/infusion-site reactions and diarrhea. In TANGO-2 versus best available treatment for carbapenem-resistant Enterobacteriaceae (CRE) (n = 77, 47 with confirmed CRE), clinical cure was increased and mortality decreased compared with best available therapy. Treatment- and renal-related adverse events were lower for meropenem-vaborbactam.
In closing, Dr. Crothers cited advice from the paper by Tamma et al. (“Rethinking how Antibiotics are Prescribed” JAMA. 2018) about the need to review findings after therapy has been initiated to confirm the pneumonia diagnosis: Novel agents should be kept in reserve in the absence of MDR risk factors for MRSA and gram-negative bacilli; therapy should be deescalated after 48-72 hours if MDR organisms are not detected; and therapy should be directed to the specific organism detected. Most HAP and VAP in adults can be treated for 7 days, she added.
“Know indications for new therapeutic agents approved for nosocomial pneumonia,” she concluded.
Dr. Crothers reported having no disclosures.
“The right drug at the right time with the right dose for the right bug for the right duration.” That, said professor Kristina Crothers, MD, is the general guidance for optimizing antibiotic use (while awaiting an infectious disease consult). In her oral presentation at the annual meeting of the American College of Chest Physicians, “Choosing newer antibiotics for nosocomial pneumonia,” Dr. Crothers asked the question: “Beyond the guidelines: When should novel antimicrobials be used?”
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are the most common nosocomial infections at 22%, and are the leading cause of death attributable to hospital-acquired infections. They increase mortality by 20%-50%, with an economic burden of about $40,000 per patient. The incidence of multidrug-resistant (MDR) organism infections varies widely by locality, but several factors increase the likelihood: prior broad-spectrum antibiotic exposure within the past 90 days; longer hospitalization; indwelling vascular devices; tracheostomy; and ventilator dependence. The Centers for Disease Control and Prevention lists as “Serious Threat” the HAP/VAP MDR organisms methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa (PSA) with difficult-to-treat-resistance, and beta-lactamase producing Enterobacterales (ESBL). In the category of “Urgent Threat” the CDC lists: carbapenamase-resistant Enterobacterales (CRE) (carbapenamase producing or non–carbapenemase producing), and carbapenem-resistant Acinetobacter (CRAB), according to Dr. Crothers who is at the University of Washington Veterans Affairs Puget Sound Health Care System, Seattle.
Newer antibiotics for HAP/VAP that are still beyond the guidelines include telavancin and tedizolid as gram-positive agents, and as gram-negative ones: ceftazidime-avibactam, ceftolozane-tazobactam, cefiderocol, imipenem-cilastatin-relebactam and meropenem-vaborbactam, she added.
Tedizolid, Dr. Crothers stated, is a novel oxazolidinone, and is an alternative to vancomycin and linezolid for gram-positive HAP/VAP. In the VITAL noninferiority study versus linezolid with 726 patients, it was noninferior to linezolid for 28-day all-cause mortality (28% vs. 26%), but did not achieve noninferiority for investigator-assessed clinical cure (56% vs. 64%).
Televancin, a semisynthetic derivative of vancomycin, in the ATTAIN studies vs. vancomycin had overall similar cure rates. It is FDA-approved for S. aureus HAP/VAP but not other bacterial causes. It should be reserved for those who cannot receive vancomycin or linezolid, with normal renal function, according to Dr. Crothers. Excluded from first-line treatment of gram-positive HAP/VAP are daptomycin, ceftaroline, ceftobiprole, and tigecycline.
Ceftazidime-avibactam, a third-generation cephalosporin-plus novel beta-lactamase inhibitor has wide activity (Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, PSA and Haemophilus influenzae. It is also active against some extended-spectrum beta-lactamases (ESBLs), ampC beta-lactamases (AmpCs), and K. pneumoniae carbapenemase (KPC)–producing Enterobacterales, but not with metallo-beta-lactamases). Ceftazidime-avibactam is also indicated for HAP/VAP, and has a toxicity profile including nausea, vomiting, and diarrhea.
In the REPROVE trial of ceftazidime-avibactam vs. meropenem for 7-14 days with 527 clinically evaluable patients (37% K. pneumoniae, 30% P. aeruginosa, and 33%-35% VAP), the clinical cure at 21-25 days post randomization was 69% vs. 73%, respectively, with similar adverse events.
Ceftolozane-tazobactam, a novel fifth-generation cephalosporin plus a beta-lactamase inhibitor has activity against PSA including extensively drug-resistant PSA, AmpC, and ESBL-E, but it has limited activity against Acinetobacter and Stenotrophomonas. It is indicated for HAP/VAP, has reduced efficacy with creatine clearance of 50 mL/min or less, increases transaminases and renal impairment, and causes diarrhea. In ASPECT-NP (n = 726) ceftolozane-tazobactam versus meropenem for 8-14 days (HAP/VAP), showed a 28 day-mortality of 24% vs. 25%, respectively, with test of cure at 54% vs. 53% at 7-14 days post therapy. Adverse events were similar between groups.
Imipenem-cilastatin-relebactam, a novel beta-lactamase inhibitor plus carbapenem, is indicated for HAP/VAP and has activity against ESBL, CRE: KPC-producing Enterobacterales, PSA including AmpC. It can cause seizures (requires caution with central nervous system disorders and renal impairment). It increases transaminases, anemia, diarrhea, and reduces potassium and sodium. In RESTORE-IMI 2 (n = 537 with HAP/VAP) it was noninferior for 28-day all-cause mortality vs. piperacillin and tazobactam (16% vs. 21%), with similar adverse events.
Cefiderocol, a siderophore cephalosporin, is indicated for HAP/VAP. It has a wide spectrum of activity: ESBL, CRE, CR PSA, Stenotrophomonas maltophilia, Acinetobacter baumanii, Streptococcus.) It increases transaminases, diarrhea, and atrial fibrillation, and it reduces potassium and magnesium. In APEKS-NP versus linezolid plus cefiderocol or extended meropenem infusion (HAP/VAP n = 292; gram-negative pneumonia = 251; 60% invasive mechanical ventilation) it was noninferior for 14-day all-cause mortality (12.4% vs. 11.6%) with similar adverse events. In CREDIBLE-CR vs. best available therapy for carbapenem-resistant gram-negative infections, clinical cure rates were similar (50% vs. 53% in 59 HAP/VAP patients at 7 days), but with more deaths in the cefiderocol arm. Adverse events were > 90% in both groups and 34% vs. 19% died, mostly with Acinetobacter.
Meropenem-vaborbactam, a novel beta-lactamase inhibitor plus carbapenem, is approved and indicated for HAP/VAP in Europe. It has activity against MDR, Enterobacterales including CRE. Its toxicities include headache, phlebitis/infusion-site reactions and diarrhea. In TANGO-2 versus best available treatment for carbapenem-resistant Enterobacteriaceae (CRE) (n = 77, 47 with confirmed CRE), clinical cure was increased and mortality decreased compared with best available therapy. Treatment- and renal-related adverse events were lower for meropenem-vaborbactam.
In closing, Dr. Crothers cited advice from the paper by Tamma et al. (“Rethinking how Antibiotics are Prescribed” JAMA. 2018) about the need to review findings after therapy has been initiated to confirm the pneumonia diagnosis: Novel agents should be kept in reserve in the absence of MDR risk factors for MRSA and gram-negative bacilli; therapy should be deescalated after 48-72 hours if MDR organisms are not detected; and therapy should be directed to the specific organism detected. Most HAP and VAP in adults can be treated for 7 days, she added.
“Know indications for new therapeutic agents approved for nosocomial pneumonia,” she concluded.
Dr. Crothers reported having no disclosures.
“The right drug at the right time with the right dose for the right bug for the right duration.” That, said professor Kristina Crothers, MD, is the general guidance for optimizing antibiotic use (while awaiting an infectious disease consult). In her oral presentation at the annual meeting of the American College of Chest Physicians, “Choosing newer antibiotics for nosocomial pneumonia,” Dr. Crothers asked the question: “Beyond the guidelines: When should novel antimicrobials be used?”
Hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) are the most common nosocomial infections at 22%, and are the leading cause of death attributable to hospital-acquired infections. They increase mortality by 20%-50%, with an economic burden of about $40,000 per patient. The incidence of multidrug-resistant (MDR) organism infections varies widely by locality, but several factors increase the likelihood: prior broad-spectrum antibiotic exposure within the past 90 days; longer hospitalization; indwelling vascular devices; tracheostomy; and ventilator dependence. The Centers for Disease Control and Prevention lists as “Serious Threat” the HAP/VAP MDR organisms methicillin resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa (PSA) with difficult-to-treat-resistance, and beta-lactamase producing Enterobacterales (ESBL). In the category of “Urgent Threat” the CDC lists: carbapenamase-resistant Enterobacterales (CRE) (carbapenamase producing or non–carbapenemase producing), and carbapenem-resistant Acinetobacter (CRAB), according to Dr. Crothers who is at the University of Washington Veterans Affairs Puget Sound Health Care System, Seattle.
Newer antibiotics for HAP/VAP that are still beyond the guidelines include telavancin and tedizolid as gram-positive agents, and as gram-negative ones: ceftazidime-avibactam, ceftolozane-tazobactam, cefiderocol, imipenem-cilastatin-relebactam and meropenem-vaborbactam, she added.
Tedizolid, Dr. Crothers stated, is a novel oxazolidinone, and is an alternative to vancomycin and linezolid for gram-positive HAP/VAP. In the VITAL noninferiority study versus linezolid with 726 patients, it was noninferior to linezolid for 28-day all-cause mortality (28% vs. 26%), but did not achieve noninferiority for investigator-assessed clinical cure (56% vs. 64%).
Televancin, a semisynthetic derivative of vancomycin, in the ATTAIN studies vs. vancomycin had overall similar cure rates. It is FDA-approved for S. aureus HAP/VAP but not other bacterial causes. It should be reserved for those who cannot receive vancomycin or linezolid, with normal renal function, according to Dr. Crothers. Excluded from first-line treatment of gram-positive HAP/VAP are daptomycin, ceftaroline, ceftobiprole, and tigecycline.
Ceftazidime-avibactam, a third-generation cephalosporin-plus novel beta-lactamase inhibitor has wide activity (Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, PSA and Haemophilus influenzae. It is also active against some extended-spectrum beta-lactamases (ESBLs), ampC beta-lactamases (AmpCs), and K. pneumoniae carbapenemase (KPC)–producing Enterobacterales, but not with metallo-beta-lactamases). Ceftazidime-avibactam is also indicated for HAP/VAP, and has a toxicity profile including nausea, vomiting, and diarrhea.
In the REPROVE trial of ceftazidime-avibactam vs. meropenem for 7-14 days with 527 clinically evaluable patients (37% K. pneumoniae, 30% P. aeruginosa, and 33%-35% VAP), the clinical cure at 21-25 days post randomization was 69% vs. 73%, respectively, with similar adverse events.
Ceftolozane-tazobactam, a novel fifth-generation cephalosporin plus a beta-lactamase inhibitor has activity against PSA including extensively drug-resistant PSA, AmpC, and ESBL-E, but it has limited activity against Acinetobacter and Stenotrophomonas. It is indicated for HAP/VAP, has reduced efficacy with creatine clearance of 50 mL/min or less, increases transaminases and renal impairment, and causes diarrhea. In ASPECT-NP (n = 726) ceftolozane-tazobactam versus meropenem for 8-14 days (HAP/VAP), showed a 28 day-mortality of 24% vs. 25%, respectively, with test of cure at 54% vs. 53% at 7-14 days post therapy. Adverse events were similar between groups.
Imipenem-cilastatin-relebactam, a novel beta-lactamase inhibitor plus carbapenem, is indicated for HAP/VAP and has activity against ESBL, CRE: KPC-producing Enterobacterales, PSA including AmpC. It can cause seizures (requires caution with central nervous system disorders and renal impairment). It increases transaminases, anemia, diarrhea, and reduces potassium and sodium. In RESTORE-IMI 2 (n = 537 with HAP/VAP) it was noninferior for 28-day all-cause mortality vs. piperacillin and tazobactam (16% vs. 21%), with similar adverse events.
Cefiderocol, a siderophore cephalosporin, is indicated for HAP/VAP. It has a wide spectrum of activity: ESBL, CRE, CR PSA, Stenotrophomonas maltophilia, Acinetobacter baumanii, Streptococcus.) It increases transaminases, diarrhea, and atrial fibrillation, and it reduces potassium and magnesium. In APEKS-NP versus linezolid plus cefiderocol or extended meropenem infusion (HAP/VAP n = 292; gram-negative pneumonia = 251; 60% invasive mechanical ventilation) it was noninferior for 14-day all-cause mortality (12.4% vs. 11.6%) with similar adverse events. In CREDIBLE-CR vs. best available therapy for carbapenem-resistant gram-negative infections, clinical cure rates were similar (50% vs. 53% in 59 HAP/VAP patients at 7 days), but with more deaths in the cefiderocol arm. Adverse events were > 90% in both groups and 34% vs. 19% died, mostly with Acinetobacter.
Meropenem-vaborbactam, a novel beta-lactamase inhibitor plus carbapenem, is approved and indicated for HAP/VAP in Europe. It has activity against MDR, Enterobacterales including CRE. Its toxicities include headache, phlebitis/infusion-site reactions and diarrhea. In TANGO-2 versus best available treatment for carbapenem-resistant Enterobacteriaceae (CRE) (n = 77, 47 with confirmed CRE), clinical cure was increased and mortality decreased compared with best available therapy. Treatment- and renal-related adverse events were lower for meropenem-vaborbactam.
In closing, Dr. Crothers cited advice from the paper by Tamma et al. (“Rethinking how Antibiotics are Prescribed” JAMA. 2018) about the need to review findings after therapy has been initiated to confirm the pneumonia diagnosis: Novel agents should be kept in reserve in the absence of MDR risk factors for MRSA and gram-negative bacilli; therapy should be deescalated after 48-72 hours if MDR organisms are not detected; and therapy should be directed to the specific organism detected. Most HAP and VAP in adults can be treated for 7 days, she added.
“Know indications for new therapeutic agents approved for nosocomial pneumonia,” she concluded.
Dr. Crothers reported having no disclosures.
FROM CHEST 2022
U.S. flu activity already at mid-season levels
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
Your patients are rotting their teeth with vaping
Primary care physicians, and especially pediatricians, should consider telling their patients about the long-term oral health problems associated with vaping.
A new study found that patients who use vapes were at a higher risk of developing tooth decay and periodontal disease.
Vapes were introduced to the U.S. market in 2006 as an alternative to conventional cigarettes and have become widely popular among youth. According to a 2022 survey from the U.S. Centers for Disease Control and Prevention, 2.55 million middle and high school students in this country reported using the devices in the previous 30 days.
The new study, published in the Journal of the American Dental Association, expands on an initial case series published in 2020 of patients who reported use of vapes and who had severe dental decay. Karina Irusa, BDS, assistant professor of comprehensive care at Tufts University, Boston, and lead author of the case series, wanted to investigate whether her initial findings would apply to a large population of vape users.
For the new study, Dr. Irusa and colleagues collected data on 13,216 patients aged 16-40 who attended Tufts dental clinics between 2019 and 2021. All patients had received a diagnosis of tooth decay, had a tooth decay risk assessment on record, and had answered “yes” or “no” to use of vapes in a health history questionnaire.
Patients had records on file of varying types of dental lesions, cavities filled within the previous 3 years, heavy plaque on teeth, inadequate brushing and flushing, and a self-report of recreational drug use and frequent snacking. If patients had these factors on their file, they were at high risk of developing decay that leads to cavities.
The study found that 79% of patients who responded “yes” to being a current user of vapes were at high risk for dental decay, compared with 60% of those who did not report using the devices.
Materials in the vaping liquids further cause an inflammatory response that disrupts an individual’s internal microbiome, according to numerous studies.
“All the ingredients of vaping are surely a recipe for overgrowth of cavities causing bacteria,” said Jennifer Genuardi, MD, an internist and pediatrician at federally qualified community health center Urban Health Plan, in New York, who was not involved in the study.
Dr. Irusa said information on patient’s vaping habits should be included in routine dental and medical history questionnaires as part of their overall electronic health record.
“Decay in its severe form not only affects one’s ability to eat but affects facial aesthetics and self-esteem as well,” Dr. Irusa said.
Dr. Genuardi called the findings unsurprising.
“We are learning daily more and more about the dangers of vaping,” Dr. Genuardi said. “There’s a focus of today’s research on the effect of actions on our microbiome and the subsequent effects on our health.”
Dr. Genuardi also said many of her teenage patients do not enjoy dental visits or having cavities filled, which could serve as a useful deterrent to vaping for a demographic that has been targeted with marketing from vape manufacturers.
“Cavity formation and the experience of having cavities filled is an experience teens can identify with, so this to me seems like perhaps an even more effective angle to try to curb this unhealthy behavior of vaping,” Dr. Genuardi said.
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians, and especially pediatricians, should consider telling their patients about the long-term oral health problems associated with vaping.
A new study found that patients who use vapes were at a higher risk of developing tooth decay and periodontal disease.
Vapes were introduced to the U.S. market in 2006 as an alternative to conventional cigarettes and have become widely popular among youth. According to a 2022 survey from the U.S. Centers for Disease Control and Prevention, 2.55 million middle and high school students in this country reported using the devices in the previous 30 days.
The new study, published in the Journal of the American Dental Association, expands on an initial case series published in 2020 of patients who reported use of vapes and who had severe dental decay. Karina Irusa, BDS, assistant professor of comprehensive care at Tufts University, Boston, and lead author of the case series, wanted to investigate whether her initial findings would apply to a large population of vape users.
For the new study, Dr. Irusa and colleagues collected data on 13,216 patients aged 16-40 who attended Tufts dental clinics between 2019 and 2021. All patients had received a diagnosis of tooth decay, had a tooth decay risk assessment on record, and had answered “yes” or “no” to use of vapes in a health history questionnaire.
Patients had records on file of varying types of dental lesions, cavities filled within the previous 3 years, heavy plaque on teeth, inadequate brushing and flushing, and a self-report of recreational drug use and frequent snacking. If patients had these factors on their file, they were at high risk of developing decay that leads to cavities.
The study found that 79% of patients who responded “yes” to being a current user of vapes were at high risk for dental decay, compared with 60% of those who did not report using the devices.
Materials in the vaping liquids further cause an inflammatory response that disrupts an individual’s internal microbiome, according to numerous studies.
“All the ingredients of vaping are surely a recipe for overgrowth of cavities causing bacteria,” said Jennifer Genuardi, MD, an internist and pediatrician at federally qualified community health center Urban Health Plan, in New York, who was not involved in the study.
Dr. Irusa said information on patient’s vaping habits should be included in routine dental and medical history questionnaires as part of their overall electronic health record.
“Decay in its severe form not only affects one’s ability to eat but affects facial aesthetics and self-esteem as well,” Dr. Irusa said.
Dr. Genuardi called the findings unsurprising.
“We are learning daily more and more about the dangers of vaping,” Dr. Genuardi said. “There’s a focus of today’s research on the effect of actions on our microbiome and the subsequent effects on our health.”
Dr. Genuardi also said many of her teenage patients do not enjoy dental visits or having cavities filled, which could serve as a useful deterrent to vaping for a demographic that has been targeted with marketing from vape manufacturers.
“Cavity formation and the experience of having cavities filled is an experience teens can identify with, so this to me seems like perhaps an even more effective angle to try to curb this unhealthy behavior of vaping,” Dr. Genuardi said.
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Primary care physicians, and especially pediatricians, should consider telling their patients about the long-term oral health problems associated with vaping.
A new study found that patients who use vapes were at a higher risk of developing tooth decay and periodontal disease.
Vapes were introduced to the U.S. market in 2006 as an alternative to conventional cigarettes and have become widely popular among youth. According to a 2022 survey from the U.S. Centers for Disease Control and Prevention, 2.55 million middle and high school students in this country reported using the devices in the previous 30 days.
The new study, published in the Journal of the American Dental Association, expands on an initial case series published in 2020 of patients who reported use of vapes and who had severe dental decay. Karina Irusa, BDS, assistant professor of comprehensive care at Tufts University, Boston, and lead author of the case series, wanted to investigate whether her initial findings would apply to a large population of vape users.
For the new study, Dr. Irusa and colleagues collected data on 13,216 patients aged 16-40 who attended Tufts dental clinics between 2019 and 2021. All patients had received a diagnosis of tooth decay, had a tooth decay risk assessment on record, and had answered “yes” or “no” to use of vapes in a health history questionnaire.
Patients had records on file of varying types of dental lesions, cavities filled within the previous 3 years, heavy plaque on teeth, inadequate brushing and flushing, and a self-report of recreational drug use and frequent snacking. If patients had these factors on their file, they were at high risk of developing decay that leads to cavities.
The study found that 79% of patients who responded “yes” to being a current user of vapes were at high risk for dental decay, compared with 60% of those who did not report using the devices.
Materials in the vaping liquids further cause an inflammatory response that disrupts an individual’s internal microbiome, according to numerous studies.
“All the ingredients of vaping are surely a recipe for overgrowth of cavities causing bacteria,” said Jennifer Genuardi, MD, an internist and pediatrician at federally qualified community health center Urban Health Plan, in New York, who was not involved in the study.
Dr. Irusa said information on patient’s vaping habits should be included in routine dental and medical history questionnaires as part of their overall electronic health record.
“Decay in its severe form not only affects one’s ability to eat but affects facial aesthetics and self-esteem as well,” Dr. Irusa said.
Dr. Genuardi called the findings unsurprising.
“We are learning daily more and more about the dangers of vaping,” Dr. Genuardi said. “There’s a focus of today’s research on the effect of actions on our microbiome and the subsequent effects on our health.”
Dr. Genuardi also said many of her teenage patients do not enjoy dental visits or having cavities filled, which could serve as a useful deterrent to vaping for a demographic that has been targeted with marketing from vape manufacturers.
“Cavity formation and the experience of having cavities filled is an experience teens can identify with, so this to me seems like perhaps an even more effective angle to try to curb this unhealthy behavior of vaping,” Dr. Genuardi said.
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN DENTAL ASSOCIATION
Rates of health care use after bariatric surgery in teens
Researchers found significantly lower rates of both emergency department (ED) use and hospitalization 5 years after sleeve gastrectomy compared with gastric bypass, and similarly low rates of adverse events.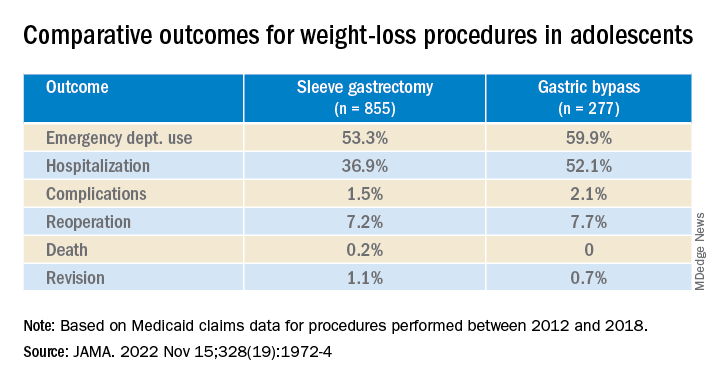
The study, by researchers with the department of surgery and Center for Health Outcomes and Policy, University of Michigan, Ann Arbor, was published in JAMA.
Studies have shown that sleeve gastrectomy and gastric bypass both lead to significant weight loss and are associated with low complication rates among adolescents with severe obesity.
Until now, however, comparative outcomes for these two weight-loss procedures have not been described for adolescents insured by Medicaid, the largest insurer of adolescents in the United States.
Using Medicaid claims data, Ryan Howard, MD, and colleagues identified 855 adolescents who underwent sleeve gastrectomy and 277 who underwent Roux-en-Y gastric bypass between 2012 and 2018.
Adolescents in both groups were about 18 years old on average at the time of surgery, and about three-quarters were female.
Sleeve gastrectomy became more common over the study period. The annual percentage of sleeve gastrectomy relative to gastric bypass increased from 48.8% in 2012 to 82.6% in 2018.
There was no significant difference in rates of complications (P = .31) or reoperation (P = .78), defined as abdominal operation potentially related to the index procedure, including biliary procedures and abdominal wall, internal, and paraesophageal hernia repair.
Researchers also found no difference between sleeve gastrectomy and gastric bypass in rates of death (P = .42) or revision (P = .63), which included any operation that directly modified the index procedure.
The results “may help inform the treatment of severe obesity in adolescents insured by Medicaid, although future studies should also evaluate long-term weight loss and comorbidity resolution in this population,” Dr. Howard and colleagues write.
They caution that their analysis is subject to selection bias because patient characteristics may influence the choice of procedure, although appropriate statistical adjustment was used.
Other limitations include the small sample size, which increases the possibility of type II error; the relatively short follow-up period; and the inability to directly attribute outcomes to the index procedure.
Funding for the study was provided by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers found significantly lower rates of both emergency department (ED) use and hospitalization 5 years after sleeve gastrectomy compared with gastric bypass, and similarly low rates of adverse events.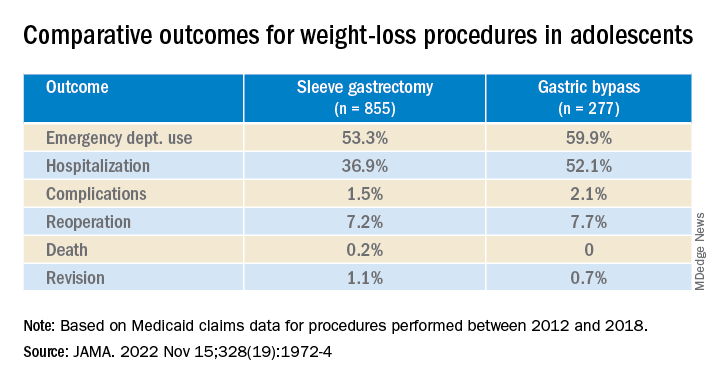
The study, by researchers with the department of surgery and Center for Health Outcomes and Policy, University of Michigan, Ann Arbor, was published in JAMA.
Studies have shown that sleeve gastrectomy and gastric bypass both lead to significant weight loss and are associated with low complication rates among adolescents with severe obesity.
Until now, however, comparative outcomes for these two weight-loss procedures have not been described for adolescents insured by Medicaid, the largest insurer of adolescents in the United States.
Using Medicaid claims data, Ryan Howard, MD, and colleagues identified 855 adolescents who underwent sleeve gastrectomy and 277 who underwent Roux-en-Y gastric bypass between 2012 and 2018.
Adolescents in both groups were about 18 years old on average at the time of surgery, and about three-quarters were female.
Sleeve gastrectomy became more common over the study period. The annual percentage of sleeve gastrectomy relative to gastric bypass increased from 48.8% in 2012 to 82.6% in 2018.
There was no significant difference in rates of complications (P = .31) or reoperation (P = .78), defined as abdominal operation potentially related to the index procedure, including biliary procedures and abdominal wall, internal, and paraesophageal hernia repair.
Researchers also found no difference between sleeve gastrectomy and gastric bypass in rates of death (P = .42) or revision (P = .63), which included any operation that directly modified the index procedure.
The results “may help inform the treatment of severe obesity in adolescents insured by Medicaid, although future studies should also evaluate long-term weight loss and comorbidity resolution in this population,” Dr. Howard and colleagues write.
They caution that their analysis is subject to selection bias because patient characteristics may influence the choice of procedure, although appropriate statistical adjustment was used.
Other limitations include the small sample size, which increases the possibility of type II error; the relatively short follow-up period; and the inability to directly attribute outcomes to the index procedure.
Funding for the study was provided by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers found significantly lower rates of both emergency department (ED) use and hospitalization 5 years after sleeve gastrectomy compared with gastric bypass, and similarly low rates of adverse events.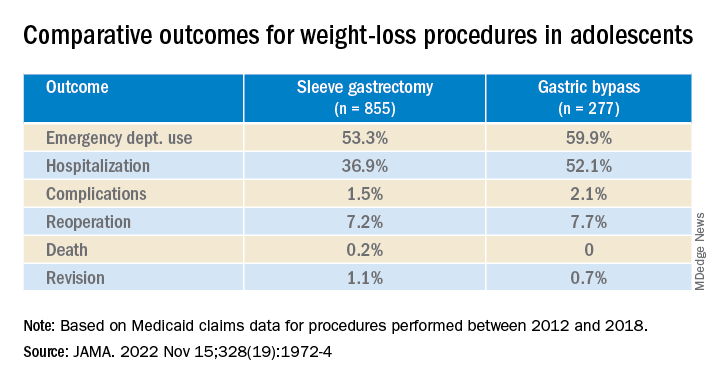
The study, by researchers with the department of surgery and Center for Health Outcomes and Policy, University of Michigan, Ann Arbor, was published in JAMA.
Studies have shown that sleeve gastrectomy and gastric bypass both lead to significant weight loss and are associated with low complication rates among adolescents with severe obesity.
Until now, however, comparative outcomes for these two weight-loss procedures have not been described for adolescents insured by Medicaid, the largest insurer of adolescents in the United States.
Using Medicaid claims data, Ryan Howard, MD, and colleagues identified 855 adolescents who underwent sleeve gastrectomy and 277 who underwent Roux-en-Y gastric bypass between 2012 and 2018.
Adolescents in both groups were about 18 years old on average at the time of surgery, and about three-quarters were female.
Sleeve gastrectomy became more common over the study period. The annual percentage of sleeve gastrectomy relative to gastric bypass increased from 48.8% in 2012 to 82.6% in 2018.
There was no significant difference in rates of complications (P = .31) or reoperation (P = .78), defined as abdominal operation potentially related to the index procedure, including biliary procedures and abdominal wall, internal, and paraesophageal hernia repair.
Researchers also found no difference between sleeve gastrectomy and gastric bypass in rates of death (P = .42) or revision (P = .63), which included any operation that directly modified the index procedure.
The results “may help inform the treatment of severe obesity in adolescents insured by Medicaid, although future studies should also evaluate long-term weight loss and comorbidity resolution in this population,” Dr. Howard and colleagues write.
They caution that their analysis is subject to selection bias because patient characteristics may influence the choice of procedure, although appropriate statistical adjustment was used.
Other limitations include the small sample size, which increases the possibility of type II error; the relatively short follow-up period; and the inability to directly attribute outcomes to the index procedure.
Funding for the study was provided by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
Is it long COVID, or dementia, or both?
In early September, about a week after recovering from COVID-19, Barri Sanders went to the bank to pay a bill. But by mistake, she transferred a large amount of money from the wrong account.
“I’m talking about $20,000,” she said. “I had to go back [later] and fix it.”
Ms. Sanders, 83, had not had confusion like that before. Suddenly, the Albuquerque, N.M., resident found herself looking up from a book and not remembering what she had just read. She would stand up from her chair and forget what she meant to do.
“I kind of thought it was just the aging process,” she said. Combined with sudden balance issues, insomnia, and a nagging postnasal drip, the overall effect was “subtle, but scary,” she said.
After 5 days of this, she went to bed and slept the whole night through. She woke up in the morning to find her balanced restored, her sinuses clear, and the mental fog gone. What she’d had, she realized, wasn’t a rapid start of dementia, but rather a mercifully short form of long COVID.
Somewhere between 22% and 32% of people who recover from COVID-19 get “brain fog,” a nonscientific term used to describe slow or sluggish thinking. While this is disturbing at any age, And some scientists are starting to confirm what doctors, patients, and their families can already see: Older patients who have had COVID-19 have a higher risk of getting dementia or, if they already have mental confusion, the illness may worsen their condition.
British scientists who studied medical records from around the world reported in the journal The Lancet Psychiatry that people who recovered from COVID-19 had a higher risk of problems with their thinking and dementia even after 2 years had passed.
Another 2022 study, published in JAMA Neurology, looked at older COVID-19 patients for a year after they were discharged from hospitals in Wuhan, China. Compared with uninfected people, those who survived a severe case of COVID-19 were at higher risk for early onset, late-onset, and progressive decline in their thinking skills. Those who survived a mild infection were at a higher risk for early onset decline, the study found.
Eran Metzger, MD, assistant professor of psychiatry at Beth Israel Deaconess Medical Center in Boston, said he’s noticed that COVID-19 makes some older patients confused, and their brains don’t regain their former clarity.
“We see a stepwise decline in their cognition during the COVID episode, and then they never get back up to their baseline,” said Dr. Metzger, medical director at Hebrew SeniorLife.
New research is beginning to back up such findings.
People who got COVID-19 were twice as likely to receive a diagnosis of Alzheimer’s disease in the 12 months after infection, compared to those who didn’t get COVID, according to a study published in the journal Nature Medicine , which analyzed the health care databases of the U.S. Department of Veterans Affairs.
Joshua Cahan, MD, a cognitive neurologist at Northwestern University, Chicago, advises caution about applying such a specific label simply from a patient’s medical chart. After all, he noted, few patients get tested to confirm that they have the proteins linked to Alzheimer’s.
“Probably the most appropriate conclusion from that is that there’s an increased risk of dementia after a COVID infection,” he said, “but we don’t know whether it’s truly Alzheimer’s disease or not.”
There could be a number of reasons why COVID-19 triggers a decline in thinking skills, says Michelle Monje, MD, a neuroscientist and neuro-oncologist at Stanford (Calif.) University.
In a paper published in the journal Neuron, Dr. Monje and her coauthor, Akiko Iwasaki, PhD, professor of immunobiology at Yale University, New Haven, Conn., propose possible triggers for brain fog caused by COVID: inflammation in the lungs and respiratory passages that leads to inflammation and dysregulation of the central nervous system; autoimmune reactions that damage the central nervous system; brain infection directly caused by the coronavirus (though, they note, this appears rare); a reactivation of an Epstein-Barr virus, which can lead to neuroinflammation; triggered by the coronavirus; and/or complications from severe cases of COVID-19, possibly involving periods of low blood oxygen and multi-organ failure.
Scientific understanding of brain fog is “part of an emerging picture that inflammation elsewhere in the body can be transmitted to become inflammation in the brain,” Dr. Monje said. “And once there’s inflammation in the brain … that can dysregulate other cell types that normally support healthy cognitive function.”
One issue with the concept of brain fog is that, like the term itself, the condition can be tough to define for doctors and patients alike and difficult, if not impossible, to capture on common cognition tests.
These days, patients often arrive at the Center of Excellence for Alzheimer’s Disease, in Syracuse, N.Y., complaining that they “don’t feel the same” as they did before contracting COVID-19, said Sharon Brangman, MD, the center’s director and the chair of the geriatrics department at Upstate Medical University.
But the evidence of diminished cognition just isn’t there.
“There’s nothing that we can find, objectively, that’s wrong with them,” she said. “They’re not severe enough to score low on mental status testing.”
But specialized, directed testing can find some probable signs, said Dr. Cahan, who evaluates patient cognition in a long COVID clinic at Northwestern University.
He often finds that his long COVID patients score in the low normal range on cognitive testing.
“Patients do have a complaint that something’s changed, and we don’t have prior testing,” he said. “So it’s possible that they were maybe in the high normal range or the superior range, but you just don’t know.”
He said he has seen very high-performing people, such as lawyers, executives, PhDs, and other professionals, who have tests that might be interpreted as normal, but given their level of achievement, “you would expect [higher scores].”
Like Ms. Sanders, many of those who do have muddled thinking after a COVID infection return to their former mental status. A study published in the journal Brain Communications found that people who had recovered from COVID-19, even if they had a mild illness, were significantly more likely to have memory and other cognition issues in the months after infection. But after 9 months, the former COVID patients had returned to their normal level of cognition, the team at Britain’s University of Oxford reported.
Notably, though, the average age of the people in the study was 28.6.
At the Northwestern clinic, Dr. Cahan treats patients who have struggled with COVID-induced cognition issues for months or even years. A rehabilitation program involves working with patients to come up with ways to compensate for cognitive deficits – such as making lists – as well as brain exercises, Dr. Cahan said. Over time, patients may achieve a 75% to 85% improvement, he said.
Dr. Monje hopes that one day, science will come up with ways to fully reverse the decline.
“I think what is likely the most common contributor to brain fog is this neuroinflammation, causing dysfunction of other cell types,” she said. “And, at least in the laboratory, we can rescue that in mouse models of chemotherapy brain fog, which gives me hope that we can rescue that for people.”
A version of this article first appeared on WebMD.com.
In early September, about a week after recovering from COVID-19, Barri Sanders went to the bank to pay a bill. But by mistake, she transferred a large amount of money from the wrong account.
“I’m talking about $20,000,” she said. “I had to go back [later] and fix it.”
Ms. Sanders, 83, had not had confusion like that before. Suddenly, the Albuquerque, N.M., resident found herself looking up from a book and not remembering what she had just read. She would stand up from her chair and forget what she meant to do.
“I kind of thought it was just the aging process,” she said. Combined with sudden balance issues, insomnia, and a nagging postnasal drip, the overall effect was “subtle, but scary,” she said.
After 5 days of this, she went to bed and slept the whole night through. She woke up in the morning to find her balanced restored, her sinuses clear, and the mental fog gone. What she’d had, she realized, wasn’t a rapid start of dementia, but rather a mercifully short form of long COVID.
Somewhere between 22% and 32% of people who recover from COVID-19 get “brain fog,” a nonscientific term used to describe slow or sluggish thinking. While this is disturbing at any age, And some scientists are starting to confirm what doctors, patients, and their families can already see: Older patients who have had COVID-19 have a higher risk of getting dementia or, if they already have mental confusion, the illness may worsen their condition.
British scientists who studied medical records from around the world reported in the journal The Lancet Psychiatry that people who recovered from COVID-19 had a higher risk of problems with their thinking and dementia even after 2 years had passed.
Another 2022 study, published in JAMA Neurology, looked at older COVID-19 patients for a year after they were discharged from hospitals in Wuhan, China. Compared with uninfected people, those who survived a severe case of COVID-19 were at higher risk for early onset, late-onset, and progressive decline in their thinking skills. Those who survived a mild infection were at a higher risk for early onset decline, the study found.
Eran Metzger, MD, assistant professor of psychiatry at Beth Israel Deaconess Medical Center in Boston, said he’s noticed that COVID-19 makes some older patients confused, and their brains don’t regain their former clarity.
“We see a stepwise decline in their cognition during the COVID episode, and then they never get back up to their baseline,” said Dr. Metzger, medical director at Hebrew SeniorLife.
New research is beginning to back up such findings.
People who got COVID-19 were twice as likely to receive a diagnosis of Alzheimer’s disease in the 12 months after infection, compared to those who didn’t get COVID, according to a study published in the journal Nature Medicine , which analyzed the health care databases of the U.S. Department of Veterans Affairs.
Joshua Cahan, MD, a cognitive neurologist at Northwestern University, Chicago, advises caution about applying such a specific label simply from a patient’s medical chart. After all, he noted, few patients get tested to confirm that they have the proteins linked to Alzheimer’s.
“Probably the most appropriate conclusion from that is that there’s an increased risk of dementia after a COVID infection,” he said, “but we don’t know whether it’s truly Alzheimer’s disease or not.”
There could be a number of reasons why COVID-19 triggers a decline in thinking skills, says Michelle Monje, MD, a neuroscientist and neuro-oncologist at Stanford (Calif.) University.
In a paper published in the journal Neuron, Dr. Monje and her coauthor, Akiko Iwasaki, PhD, professor of immunobiology at Yale University, New Haven, Conn., propose possible triggers for brain fog caused by COVID: inflammation in the lungs and respiratory passages that leads to inflammation and dysregulation of the central nervous system; autoimmune reactions that damage the central nervous system; brain infection directly caused by the coronavirus (though, they note, this appears rare); a reactivation of an Epstein-Barr virus, which can lead to neuroinflammation; triggered by the coronavirus; and/or complications from severe cases of COVID-19, possibly involving periods of low blood oxygen and multi-organ failure.
Scientific understanding of brain fog is “part of an emerging picture that inflammation elsewhere in the body can be transmitted to become inflammation in the brain,” Dr. Monje said. “And once there’s inflammation in the brain … that can dysregulate other cell types that normally support healthy cognitive function.”
One issue with the concept of brain fog is that, like the term itself, the condition can be tough to define for doctors and patients alike and difficult, if not impossible, to capture on common cognition tests.
These days, patients often arrive at the Center of Excellence for Alzheimer’s Disease, in Syracuse, N.Y., complaining that they “don’t feel the same” as they did before contracting COVID-19, said Sharon Brangman, MD, the center’s director and the chair of the geriatrics department at Upstate Medical University.
But the evidence of diminished cognition just isn’t there.
“There’s nothing that we can find, objectively, that’s wrong with them,” she said. “They’re not severe enough to score low on mental status testing.”
But specialized, directed testing can find some probable signs, said Dr. Cahan, who evaluates patient cognition in a long COVID clinic at Northwestern University.
He often finds that his long COVID patients score in the low normal range on cognitive testing.
“Patients do have a complaint that something’s changed, and we don’t have prior testing,” he said. “So it’s possible that they were maybe in the high normal range or the superior range, but you just don’t know.”
He said he has seen very high-performing people, such as lawyers, executives, PhDs, and other professionals, who have tests that might be interpreted as normal, but given their level of achievement, “you would expect [higher scores].”
Like Ms. Sanders, many of those who do have muddled thinking after a COVID infection return to their former mental status. A study published in the journal Brain Communications found that people who had recovered from COVID-19, even if they had a mild illness, were significantly more likely to have memory and other cognition issues in the months after infection. But after 9 months, the former COVID patients had returned to their normal level of cognition, the team at Britain’s University of Oxford reported.
Notably, though, the average age of the people in the study was 28.6.
At the Northwestern clinic, Dr. Cahan treats patients who have struggled with COVID-induced cognition issues for months or even years. A rehabilitation program involves working with patients to come up with ways to compensate for cognitive deficits – such as making lists – as well as brain exercises, Dr. Cahan said. Over time, patients may achieve a 75% to 85% improvement, he said.
Dr. Monje hopes that one day, science will come up with ways to fully reverse the decline.
“I think what is likely the most common contributor to brain fog is this neuroinflammation, causing dysfunction of other cell types,” she said. “And, at least in the laboratory, we can rescue that in mouse models of chemotherapy brain fog, which gives me hope that we can rescue that for people.”
A version of this article first appeared on WebMD.com.
In early September, about a week after recovering from COVID-19, Barri Sanders went to the bank to pay a bill. But by mistake, she transferred a large amount of money from the wrong account.
“I’m talking about $20,000,” she said. “I had to go back [later] and fix it.”
Ms. Sanders, 83, had not had confusion like that before. Suddenly, the Albuquerque, N.M., resident found herself looking up from a book and not remembering what she had just read. She would stand up from her chair and forget what she meant to do.
“I kind of thought it was just the aging process,” she said. Combined with sudden balance issues, insomnia, and a nagging postnasal drip, the overall effect was “subtle, but scary,” she said.
After 5 days of this, she went to bed and slept the whole night through. She woke up in the morning to find her balanced restored, her sinuses clear, and the mental fog gone. What she’d had, she realized, wasn’t a rapid start of dementia, but rather a mercifully short form of long COVID.
Somewhere between 22% and 32% of people who recover from COVID-19 get “brain fog,” a nonscientific term used to describe slow or sluggish thinking. While this is disturbing at any age, And some scientists are starting to confirm what doctors, patients, and their families can already see: Older patients who have had COVID-19 have a higher risk of getting dementia or, if they already have mental confusion, the illness may worsen their condition.
British scientists who studied medical records from around the world reported in the journal The Lancet Psychiatry that people who recovered from COVID-19 had a higher risk of problems with their thinking and dementia even after 2 years had passed.
Another 2022 study, published in JAMA Neurology, looked at older COVID-19 patients for a year after they were discharged from hospitals in Wuhan, China. Compared with uninfected people, those who survived a severe case of COVID-19 were at higher risk for early onset, late-onset, and progressive decline in their thinking skills. Those who survived a mild infection were at a higher risk for early onset decline, the study found.
Eran Metzger, MD, assistant professor of psychiatry at Beth Israel Deaconess Medical Center in Boston, said he’s noticed that COVID-19 makes some older patients confused, and their brains don’t regain their former clarity.
“We see a stepwise decline in their cognition during the COVID episode, and then they never get back up to their baseline,” said Dr. Metzger, medical director at Hebrew SeniorLife.
New research is beginning to back up such findings.
People who got COVID-19 were twice as likely to receive a diagnosis of Alzheimer’s disease in the 12 months after infection, compared to those who didn’t get COVID, according to a study published in the journal Nature Medicine , which analyzed the health care databases of the U.S. Department of Veterans Affairs.
Joshua Cahan, MD, a cognitive neurologist at Northwestern University, Chicago, advises caution about applying such a specific label simply from a patient’s medical chart. After all, he noted, few patients get tested to confirm that they have the proteins linked to Alzheimer’s.
“Probably the most appropriate conclusion from that is that there’s an increased risk of dementia after a COVID infection,” he said, “but we don’t know whether it’s truly Alzheimer’s disease or not.”
There could be a number of reasons why COVID-19 triggers a decline in thinking skills, says Michelle Monje, MD, a neuroscientist and neuro-oncologist at Stanford (Calif.) University.
In a paper published in the journal Neuron, Dr. Monje and her coauthor, Akiko Iwasaki, PhD, professor of immunobiology at Yale University, New Haven, Conn., propose possible triggers for brain fog caused by COVID: inflammation in the lungs and respiratory passages that leads to inflammation and dysregulation of the central nervous system; autoimmune reactions that damage the central nervous system; brain infection directly caused by the coronavirus (though, they note, this appears rare); a reactivation of an Epstein-Barr virus, which can lead to neuroinflammation; triggered by the coronavirus; and/or complications from severe cases of COVID-19, possibly involving periods of low blood oxygen and multi-organ failure.
Scientific understanding of brain fog is “part of an emerging picture that inflammation elsewhere in the body can be transmitted to become inflammation in the brain,” Dr. Monje said. “And once there’s inflammation in the brain … that can dysregulate other cell types that normally support healthy cognitive function.”
One issue with the concept of brain fog is that, like the term itself, the condition can be tough to define for doctors and patients alike and difficult, if not impossible, to capture on common cognition tests.
These days, patients often arrive at the Center of Excellence for Alzheimer’s Disease, in Syracuse, N.Y., complaining that they “don’t feel the same” as they did before contracting COVID-19, said Sharon Brangman, MD, the center’s director and the chair of the geriatrics department at Upstate Medical University.
But the evidence of diminished cognition just isn’t there.
“There’s nothing that we can find, objectively, that’s wrong with them,” she said. “They’re not severe enough to score low on mental status testing.”
But specialized, directed testing can find some probable signs, said Dr. Cahan, who evaluates patient cognition in a long COVID clinic at Northwestern University.
He often finds that his long COVID patients score in the low normal range on cognitive testing.
“Patients do have a complaint that something’s changed, and we don’t have prior testing,” he said. “So it’s possible that they were maybe in the high normal range or the superior range, but you just don’t know.”
He said he has seen very high-performing people, such as lawyers, executives, PhDs, and other professionals, who have tests that might be interpreted as normal, but given their level of achievement, “you would expect [higher scores].”
Like Ms. Sanders, many of those who do have muddled thinking after a COVID infection return to their former mental status. A study published in the journal Brain Communications found that people who had recovered from COVID-19, even if they had a mild illness, were significantly more likely to have memory and other cognition issues in the months after infection. But after 9 months, the former COVID patients had returned to their normal level of cognition, the team at Britain’s University of Oxford reported.
Notably, though, the average age of the people in the study was 28.6.
At the Northwestern clinic, Dr. Cahan treats patients who have struggled with COVID-induced cognition issues for months or even years. A rehabilitation program involves working with patients to come up with ways to compensate for cognitive deficits – such as making lists – as well as brain exercises, Dr. Cahan said. Over time, patients may achieve a 75% to 85% improvement, he said.
Dr. Monje hopes that one day, science will come up with ways to fully reverse the decline.
“I think what is likely the most common contributor to brain fog is this neuroinflammation, causing dysfunction of other cell types,” she said. “And, at least in the laboratory, we can rescue that in mouse models of chemotherapy brain fog, which gives me hope that we can rescue that for people.”
A version of this article first appeared on WebMD.com.
Just 8 minutes of exercise a day is all you need
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
FROM EUROPEAN HEART JOURNAL
More vaccinated people dying of COVID as fewer get booster shots
“We can no longer say this is a pandemic of the unvaccinated,” Kaiser Family Foundation Vice President Cynthia Cox, who conducted the analysis, told The Washington Post.
People who had been vaccinated or boosted made up 58% of COVID-19 deaths in August, the analysis showed. The rate has been on the rise: 23% of coronavirus deaths were among vaccinated people in September 2021, and the vaccinated made up 42% of deaths in January and February 2022, the Post reported.
Research continues to show that people who are vaccinated or boosted have a lower risk of death. The rise in deaths among the vaccinated is the result of three factors, Ms. Cox said.
- A large majority of people in the United States have been vaccinated (267 million people, the said).
- People who are at the greatest risk of dying from COVID-19 are more likely to be vaccinated and boosted, such as the elderly.
- Vaccines lose their effectiveness over time; the virus changes to avoid vaccines; and people need to choose to get boosters to continue to be protected.
The case for the effectiveness of vaccines and boosters versus skipping the shots remains strong. People age 6 months and older who are unvaccinated are six times more likely to die of COVID-19, compared to those who got the primary series of shots, the Post reported. Survival rates were even better with additional booster shots, particularly among older people.
“I feel very confident that if people continue to get vaccinated at good numbers, if people get boosted, we can absolutely have a very safe and healthy holiday season,” Ashish Jha, White House coronavirus czar, said on Nov. 22.
The number of Americans who have gotten the most recent booster has been increasing ahead of the holidays. CDC data show that 12% of the U.S. population age 5 and older has received a booster.
A new study by a team of researchers from Harvard University and Yale University estimates that 94% of the U.S. population has been infected with COVID-19 at least once, leaving just 1 in 20 people who have never had the virus.
“Despite these high exposure numbers, there is still substantial population susceptibility to infection with an Omicron variant,” the authors wrote.
They said that if all states achieved the vaccination levels of Vermont, where 55% of people had at least one booster and 22% got a second one, there would be “an appreciable improvement in population immunity, with greater relative impact for protection against infection versus severe disease. This additional protection results from both the recovery of immunity lost due to waning and the increased effectiveness of the bivalent booster against Omicron infections.”
A version of this article first appeared on WebMD.com.
“We can no longer say this is a pandemic of the unvaccinated,” Kaiser Family Foundation Vice President Cynthia Cox, who conducted the analysis, told The Washington Post.
People who had been vaccinated or boosted made up 58% of COVID-19 deaths in August, the analysis showed. The rate has been on the rise: 23% of coronavirus deaths were among vaccinated people in September 2021, and the vaccinated made up 42% of deaths in January and February 2022, the Post reported.
Research continues to show that people who are vaccinated or boosted have a lower risk of death. The rise in deaths among the vaccinated is the result of three factors, Ms. Cox said.
- A large majority of people in the United States have been vaccinated (267 million people, the said).
- People who are at the greatest risk of dying from COVID-19 are more likely to be vaccinated and boosted, such as the elderly.
- Vaccines lose their effectiveness over time; the virus changes to avoid vaccines; and people need to choose to get boosters to continue to be protected.
The case for the effectiveness of vaccines and boosters versus skipping the shots remains strong. People age 6 months and older who are unvaccinated are six times more likely to die of COVID-19, compared to those who got the primary series of shots, the Post reported. Survival rates were even better with additional booster shots, particularly among older people.
“I feel very confident that if people continue to get vaccinated at good numbers, if people get boosted, we can absolutely have a very safe and healthy holiday season,” Ashish Jha, White House coronavirus czar, said on Nov. 22.
The number of Americans who have gotten the most recent booster has been increasing ahead of the holidays. CDC data show that 12% of the U.S. population age 5 and older has received a booster.
A new study by a team of researchers from Harvard University and Yale University estimates that 94% of the U.S. population has been infected with COVID-19 at least once, leaving just 1 in 20 people who have never had the virus.
“Despite these high exposure numbers, there is still substantial population susceptibility to infection with an Omicron variant,” the authors wrote.
They said that if all states achieved the vaccination levels of Vermont, where 55% of people had at least one booster and 22% got a second one, there would be “an appreciable improvement in population immunity, with greater relative impact for protection against infection versus severe disease. This additional protection results from both the recovery of immunity lost due to waning and the increased effectiveness of the bivalent booster against Omicron infections.”
A version of this article first appeared on WebMD.com.
“We can no longer say this is a pandemic of the unvaccinated,” Kaiser Family Foundation Vice President Cynthia Cox, who conducted the analysis, told The Washington Post.
People who had been vaccinated or boosted made up 58% of COVID-19 deaths in August, the analysis showed. The rate has been on the rise: 23% of coronavirus deaths were among vaccinated people in September 2021, and the vaccinated made up 42% of deaths in January and February 2022, the Post reported.
Research continues to show that people who are vaccinated or boosted have a lower risk of death. The rise in deaths among the vaccinated is the result of three factors, Ms. Cox said.
- A large majority of people in the United States have been vaccinated (267 million people, the said).
- People who are at the greatest risk of dying from COVID-19 are more likely to be vaccinated and boosted, such as the elderly.
- Vaccines lose their effectiveness over time; the virus changes to avoid vaccines; and people need to choose to get boosters to continue to be protected.
The case for the effectiveness of vaccines and boosters versus skipping the shots remains strong. People age 6 months and older who are unvaccinated are six times more likely to die of COVID-19, compared to those who got the primary series of shots, the Post reported. Survival rates were even better with additional booster shots, particularly among older people.
“I feel very confident that if people continue to get vaccinated at good numbers, if people get boosted, we can absolutely have a very safe and healthy holiday season,” Ashish Jha, White House coronavirus czar, said on Nov. 22.
The number of Americans who have gotten the most recent booster has been increasing ahead of the holidays. CDC data show that 12% of the U.S. population age 5 and older has received a booster.
A new study by a team of researchers from Harvard University and Yale University estimates that 94% of the U.S. population has been infected with COVID-19 at least once, leaving just 1 in 20 people who have never had the virus.
“Despite these high exposure numbers, there is still substantial population susceptibility to infection with an Omicron variant,” the authors wrote.
They said that if all states achieved the vaccination levels of Vermont, where 55% of people had at least one booster and 22% got a second one, there would be “an appreciable improvement in population immunity, with greater relative impact for protection against infection versus severe disease. This additional protection results from both the recovery of immunity lost due to waning and the increased effectiveness of the bivalent booster against Omicron infections.”
A version of this article first appeared on WebMD.com.
Don’t call me ‘Dr.,’ say some physicians – but most prefer the title
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN