User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Overcoming COVID-related stress
As a department chief managing during this crisis, everyone greets me sympathetically: “This must be so stressful for you! Are you doing OK?” “Um, I’m great,” I answer contritely. Yes, this is hard, yet I feel fine. But why? Shouldn’t I be fretting the damage done by the COVID cyclone? Our operations are smashed and our staff scrambled, my family and friends are out of work; these are difficult times. But a harmful effect on my health or yours is not inevitable. There are things we can do to inoculate ourselves.
No doubt, exercise (if you can find weights!), eating well, sleeping, and meditating help, but they are secondary. None of these protect much if you still believe stress is killing you. You must first reframe what is happening. Health psychologist Kelly McGonigal, PhD, from Stanford (Calif.) University, is a world expert on this topic. If you’ve not seen her TED talk about stress, then watch it now. She teaches how stress is indeed harmful to your health – but only if you believe it to be so. Many studies have borne this out. One showed that people who reported high stress in the previous year were 43% more likely to die than those who did not. But that risk held only when they believed stress was harmful to them. Those who did not think that stress was harmful not only fared better but also had the lowest likelihood of death, lower even than those who reported little stress! So it wasn’t the stress that mattered, it was the physiologic response to it. And that you can control.
Changing your beliefs is no easy feat. There is work to be done, Dr. McGonigal would argue. You must not only reframe our stress as healthful, but also act in ways to make this true. This is easier for us as physicians. First, we understand better than most that difficulty is a normal part of life. We have countless stories of hardship, tragedy, pain and suffering from the work we do. The pandemic may be extraordinary in breadth, but not in depth. We’ve seen worse happen to patients. Second, we have firsthand experience that suffering ends and often leads to strength and resilience. Even in our own lives, it was by traveling through the extraordinary stress of medical school and residency that we arrived here.
Cortisol increases when we are under duress. So does oxytocin. The former gets most of the press, the latter is more interesting. That oxytocin release during stress conferred survival benefits to us as a species: When a threat arrived, we not only ran, but also grabbed the kids, too! Oxytocin is the “tend and befriend” compliment to cortisol’s “fight or flight.” Focusing on this priming to strengthen social ties, listen, spend (Zoom) time together, and provide emotional support is key to our recovery. Even small acts of giving for our staff, friends, family, and strangers can significantly shift consequences of this stress from harmful to beneficial.
Last year, my uncle died in a tragic accident. My aunt, who is alone, is now also isolated. She’s lost her partner, her guardian, and she is afraid. Rather than succumb to the stress, she imagined something she could do to wrest some control. Last week, she filled her minivan with pink and yellow tulips bunched in bouquets and tied with handwritten notes of encouragement. She then drove up and down the streets in her North Attleboro, Mass., neighborhood and left the flowers on doorsteps until her van was empty. She did so to share with them the bit of joy that spring brings, she says, and to encourage people to stay inside!
This is a difficult time for us, and yet even more difficult for others. Perhaps the best we can do is to find ways to bring a bit of joy or comfort to others.
“In some ways suffering ceases to be suffering at the moment it finds a meaning, such as the meaning of a sacrifice.” – Viktor Frankl
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He had no relevant disclosures. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
As a department chief managing during this crisis, everyone greets me sympathetically: “This must be so stressful for you! Are you doing OK?” “Um, I’m great,” I answer contritely. Yes, this is hard, yet I feel fine. But why? Shouldn’t I be fretting the damage done by the COVID cyclone? Our operations are smashed and our staff scrambled, my family and friends are out of work; these are difficult times. But a harmful effect on my health or yours is not inevitable. There are things we can do to inoculate ourselves.
No doubt, exercise (if you can find weights!), eating well, sleeping, and meditating help, but they are secondary. None of these protect much if you still believe stress is killing you. You must first reframe what is happening. Health psychologist Kelly McGonigal, PhD, from Stanford (Calif.) University, is a world expert on this topic. If you’ve not seen her TED talk about stress, then watch it now. She teaches how stress is indeed harmful to your health – but only if you believe it to be so. Many studies have borne this out. One showed that people who reported high stress in the previous year were 43% more likely to die than those who did not. But that risk held only when they believed stress was harmful to them. Those who did not think that stress was harmful not only fared better but also had the lowest likelihood of death, lower even than those who reported little stress! So it wasn’t the stress that mattered, it was the physiologic response to it. And that you can control.
Changing your beliefs is no easy feat. There is work to be done, Dr. McGonigal would argue. You must not only reframe our stress as healthful, but also act in ways to make this true. This is easier for us as physicians. First, we understand better than most that difficulty is a normal part of life. We have countless stories of hardship, tragedy, pain and suffering from the work we do. The pandemic may be extraordinary in breadth, but not in depth. We’ve seen worse happen to patients. Second, we have firsthand experience that suffering ends and often leads to strength and resilience. Even in our own lives, it was by traveling through the extraordinary stress of medical school and residency that we arrived here.
Cortisol increases when we are under duress. So does oxytocin. The former gets most of the press, the latter is more interesting. That oxytocin release during stress conferred survival benefits to us as a species: When a threat arrived, we not only ran, but also grabbed the kids, too! Oxytocin is the “tend and befriend” compliment to cortisol’s “fight or flight.” Focusing on this priming to strengthen social ties, listen, spend (Zoom) time together, and provide emotional support is key to our recovery. Even small acts of giving for our staff, friends, family, and strangers can significantly shift consequences of this stress from harmful to beneficial.
Last year, my uncle died in a tragic accident. My aunt, who is alone, is now also isolated. She’s lost her partner, her guardian, and she is afraid. Rather than succumb to the stress, she imagined something she could do to wrest some control. Last week, she filled her minivan with pink and yellow tulips bunched in bouquets and tied with handwritten notes of encouragement. She then drove up and down the streets in her North Attleboro, Mass., neighborhood and left the flowers on doorsteps until her van was empty. She did so to share with them the bit of joy that spring brings, she says, and to encourage people to stay inside!
This is a difficult time for us, and yet even more difficult for others. Perhaps the best we can do is to find ways to bring a bit of joy or comfort to others.
“In some ways suffering ceases to be suffering at the moment it finds a meaning, such as the meaning of a sacrifice.” – Viktor Frankl
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He had no relevant disclosures. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
As a department chief managing during this crisis, everyone greets me sympathetically: “This must be so stressful for you! Are you doing OK?” “Um, I’m great,” I answer contritely. Yes, this is hard, yet I feel fine. But why? Shouldn’t I be fretting the damage done by the COVID cyclone? Our operations are smashed and our staff scrambled, my family and friends are out of work; these are difficult times. But a harmful effect on my health or yours is not inevitable. There are things we can do to inoculate ourselves.
No doubt, exercise (if you can find weights!), eating well, sleeping, and meditating help, but they are secondary. None of these protect much if you still believe stress is killing you. You must first reframe what is happening. Health psychologist Kelly McGonigal, PhD, from Stanford (Calif.) University, is a world expert on this topic. If you’ve not seen her TED talk about stress, then watch it now. She teaches how stress is indeed harmful to your health – but only if you believe it to be so. Many studies have borne this out. One showed that people who reported high stress in the previous year were 43% more likely to die than those who did not. But that risk held only when they believed stress was harmful to them. Those who did not think that stress was harmful not only fared better but also had the lowest likelihood of death, lower even than those who reported little stress! So it wasn’t the stress that mattered, it was the physiologic response to it. And that you can control.
Changing your beliefs is no easy feat. There is work to be done, Dr. McGonigal would argue. You must not only reframe our stress as healthful, but also act in ways to make this true. This is easier for us as physicians. First, we understand better than most that difficulty is a normal part of life. We have countless stories of hardship, tragedy, pain and suffering from the work we do. The pandemic may be extraordinary in breadth, but not in depth. We’ve seen worse happen to patients. Second, we have firsthand experience that suffering ends and often leads to strength and resilience. Even in our own lives, it was by traveling through the extraordinary stress of medical school and residency that we arrived here.
Cortisol increases when we are under duress. So does oxytocin. The former gets most of the press, the latter is more interesting. That oxytocin release during stress conferred survival benefits to us as a species: When a threat arrived, we not only ran, but also grabbed the kids, too! Oxytocin is the “tend and befriend” compliment to cortisol’s “fight or flight.” Focusing on this priming to strengthen social ties, listen, spend (Zoom) time together, and provide emotional support is key to our recovery. Even small acts of giving for our staff, friends, family, and strangers can significantly shift consequences of this stress from harmful to beneficial.
Last year, my uncle died in a tragic accident. My aunt, who is alone, is now also isolated. She’s lost her partner, her guardian, and she is afraid. Rather than succumb to the stress, she imagined something she could do to wrest some control. Last week, she filled her minivan with pink and yellow tulips bunched in bouquets and tied with handwritten notes of encouragement. She then drove up and down the streets in her North Attleboro, Mass., neighborhood and left the flowers on doorsteps until her van was empty. She did so to share with them the bit of joy that spring brings, she says, and to encourage people to stay inside!
This is a difficult time for us, and yet even more difficult for others. Perhaps the best we can do is to find ways to bring a bit of joy or comfort to others.
“In some ways suffering ceases to be suffering at the moment it finds a meaning, such as the meaning of a sacrifice.” – Viktor Frankl
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He had no relevant disclosures. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
FDA authorizes first COVID-19 test kit with home collection option
a reissue of the emergency use authorization allowing for testing of samples self-collected by patients at home with the Pixel by LabCorp COVID-19 RT-PCR Test.
The reissued authorization allows for testing of a sample taken from the nose by way of a self-collection kit that contains nasal swabs and saline, according to the FDA press release. After self-swabbing, users should send the samples in an insulated package to a LabCorp laboratory for testing. LabCorp intends to make the Pixel test available to consumers in most states, accessible through doctors’ orders.
The Pixel test includes a specific Q-tip–style cotton swab for patients to use to collect their samples, the FDA noted. Because of concerns with sterility and cross-reactivity caused by inherent genetic material in cotton swabs, generic cotton swabs should not be used as a substitute. The FDA will work with test developers to determine if generic cotton swabs can be used safely and effectively with other tests.
“Throughout this pandemic we have been facilitating test development to ensure patients’ access to accurate diagnostics, which includes supporting the development of reliable and accurate at-home sample collection options. ... [The FDA] worked with LabCorp to ensure the data demonstrated from at-home patient sample collection is as safe and accurate as sample collection at a doctor’s office, hospital, or other testing site. With this action, there is now a convenient and reliable option for patient sample collection from the comfort and safety of their home,” FDA Commissioner Stephen M. Hahn, MD, said in the press release.
a reissue of the emergency use authorization allowing for testing of samples self-collected by patients at home with the Pixel by LabCorp COVID-19 RT-PCR Test.
The reissued authorization allows for testing of a sample taken from the nose by way of a self-collection kit that contains nasal swabs and saline, according to the FDA press release. After self-swabbing, users should send the samples in an insulated package to a LabCorp laboratory for testing. LabCorp intends to make the Pixel test available to consumers in most states, accessible through doctors’ orders.
The Pixel test includes a specific Q-tip–style cotton swab for patients to use to collect their samples, the FDA noted. Because of concerns with sterility and cross-reactivity caused by inherent genetic material in cotton swabs, generic cotton swabs should not be used as a substitute. The FDA will work with test developers to determine if generic cotton swabs can be used safely and effectively with other tests.
“Throughout this pandemic we have been facilitating test development to ensure patients’ access to accurate diagnostics, which includes supporting the development of reliable and accurate at-home sample collection options. ... [The FDA] worked with LabCorp to ensure the data demonstrated from at-home patient sample collection is as safe and accurate as sample collection at a doctor’s office, hospital, or other testing site. With this action, there is now a convenient and reliable option for patient sample collection from the comfort and safety of their home,” FDA Commissioner Stephen M. Hahn, MD, said in the press release.
a reissue of the emergency use authorization allowing for testing of samples self-collected by patients at home with the Pixel by LabCorp COVID-19 RT-PCR Test.
The reissued authorization allows for testing of a sample taken from the nose by way of a self-collection kit that contains nasal swabs and saline, according to the FDA press release. After self-swabbing, users should send the samples in an insulated package to a LabCorp laboratory for testing. LabCorp intends to make the Pixel test available to consumers in most states, accessible through doctors’ orders.
The Pixel test includes a specific Q-tip–style cotton swab for patients to use to collect their samples, the FDA noted. Because of concerns with sterility and cross-reactivity caused by inherent genetic material in cotton swabs, generic cotton swabs should not be used as a substitute. The FDA will work with test developers to determine if generic cotton swabs can be used safely and effectively with other tests.
“Throughout this pandemic we have been facilitating test development to ensure patients’ access to accurate diagnostics, which includes supporting the development of reliable and accurate at-home sample collection options. ... [The FDA] worked with LabCorp to ensure the data demonstrated from at-home patient sample collection is as safe and accurate as sample collection at a doctor’s office, hospital, or other testing site. With this action, there is now a convenient and reliable option for patient sample collection from the comfort and safety of their home,” FDA Commissioner Stephen M. Hahn, MD, said in the press release.
PCSK9 inhibitors unexpectedly link with lower VTE, aortic stenosis
Post hoc analyses of recent large, clinical outcomes studies of PCSK9 inhibitors have revealed two tantalizing and unexpected potential benefits from these drugs: an ability to substantially reduce the incidence or severity of venous thromboembolism and aortic stenosis.
The evidence also suggests that these effects are linked to the ability of these drugs to reduce blood levels of Lp(a) lipoprotein by roughly a quarter, currently the biggest known effect on Lp(a) levels of any approved medication.
One study ran post hoc analyses of venous thromboembolism (VTE) events in the FOURIER pivotal trial of evolocumab (Repatha), with more than 27,500 randomized patients (N Engl J Med. 2017 May 4; 376[18]:1713-22), and in the ODYSSEY OUTCOMES pivotal trial of alirocumab (Praluent), with nearly 19,000 randomized patients (N Engl J Med. 2018 Nov 29;379[22]:2097-2107). The analyses showed that, with evolocumab treatment, the incidence of VTE events fell by a statistically significant 29%, compared with patients on placebo, while in ODYSSEY OUTCOMES patients treated with alirocumab had a 33% cut in VTE events, compared with placebo-treated patients, a difference that just missed statistical significance (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046524) in analyses that were not prespecified before these trials started, Nicholas A. Marston, MD, said in a presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
A combined analysis of 46,488 patients from both studies showed a 31% cut in VTE events with PCSK9 inhibitor treatment, a highly significant finding using VTE endpoints that were not specifically tallied nor adjudicated but collected as part of the serious adverse event reporting in the two pivotal trials, said Dr. Marston, a cardiologist at Brigham and Women’s Hospital in Boston. This is the first report of a statistically significant link between treatment with PCSK9-inhibiting agents and a reduction in VTE, he added. Researchers from the ODYSSEY OUTCOMES trial had reported a VTE analysis in 2019, and while data from that trial on its own showed a nominal 33% lower VTE rate with alirocumab treatment, it just missed statistical significance.
The VTE effect took about a year on treatment to start to manifest. During the first 12 months of FOURIER, the rate of VTE events among patients in the two treatment arms was virtually identical. But starting during months 13-18 on treatment, the event curves in the two arms began to increasingly diverge, and overall during the period from month 13 to the end of the study treatment with evolocumab was linked with a statistically significant 46% reduction in VTE events, compared with patients who received placebo. The results Dr. Marston reported were also published online (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046397).
The suggestion that this association may be linked to the impact of PCSK9 inhibitors on Lp(a) came from an additional analysis that Dr. Marston presented, which looked at the link between evolocumab use and a change in VTE event rates, compared with placebo, depending on baseline lipoprotein levels. Evolocumab treatment was associated with a roughly similar, modest, and not statistically significant reduction in VTE events, compared with placebo regardless of whether patients had baseline levels of LDL cholesterol below the median or at or above the median. In contrast, when a similar analysis divided patients based on whether their Lp(a) level at baseline was below, or at or above, the median the results showed no discernible effect of evolocumab treatment, compared with on VTE events in patients with lower baseline Lp(a), but in those with higher levels treatment with evolocumab linked with a 48% cut in VTE events, compared with placebo, a statistically significant difference.
In FOURIER, treatment with evolocumab lowered baseline Lp(a) levels by a median of 27%, compared with placebo, among the 25,096 enrolled patients who had their baseline levels measured. As previously reported, prespecified analysis of FOURIER data also showed that the impact of evolocumab, compared with placebo, on the combined rate of coronary heart disease death, MI, or need for urgent coronary revascularization was enhanced among patients with elevated baseline Lp(a) and moderated in those who entered with lower levels. Among patients who entered FOURIER with Lp(a) levels at or below the median treatment with evolocumab cut the primary endpoint by 7%, compared with placebo, a difference that was not statistically significant. Among patients who began the study with Lp(a) levels above the median, evolocumab treatment cut the primary endpoint by 23%, compared with placebo, a statistically significant effect (Circulation. 2019 Mar 19;139[12]:1483-92).
The aortic stenosis connection
A second study reported in the online scientific sessions (Abstract 914-08) used only FOURIER data, and showed that patients treated with evolocumab had a roughly similar response pattern in their incidence of aortic stenosis (AS) events as they did for VTE events.
During the first year of the study, the incidence of AS events was virtually identical among patients treated with evolocumab and those who received placebo. But after the first 12 months and through the study’s end, patients on evolocumab showed a statistically significant 52% relative reduction in AS events, compared with control patients, said Brian A. Bergmark, MD. For the entire study duration, treatment with evolocumab linked with a 34% relative reduction in AS events, compared with placebo, a difference that did not reach statistical significance, added Dr. Bergmark, an interventional cardiologist also at Brigham and Women’s Hospital. The observed halving in total AS events that linked with evolocumab treatment after the first year of the study included a similar-magnitude reduction specifically in the incidence of aortic valve replacement procedures in the evolocumab-treated patients.
Further analysis of both total AS events and aortic valve replacements in FOURIER patients showed that they occurred at a significantly elevated rate in patients who entered the study with higher baseline Lp(a) levels in a multivariate analysis, but a similar analysis showed no significant association between the incidence of these AS-related events and baseline levels of LDL cholesterol, he said.
The AS analysis carried the same important limitations as the VTE analysis: It ran on a post hoc basis and focused on events that were relatively uncommon and not adjudicated, Dr. Bergmark cautioned. Nonetheless, other investigators saw important potential implications from both the VTE and AS observations, with the huge caveat that they need replication in prospective studies designed to specifically address the validity of these findings.
What it could mean
These observed associations between PCSK9 inhibitor treatment and apparent reductions in the rate of both VTE and AS events “represent a tremendous clinical breakthrough,” commented Michelle L. O’Donoghue, MD, a cardiologist at Brigham and Women’s Hospital who is a FOURIER coinvestigator and has led some of the Lp(a) analyses run from that study.
“To date, we have not identified any therapies that slow progression of AS. Other classes of lipid-lowering therapies, such as statins, have been tested and not demonstrated a significant effect,” Dr. O’Donoghue said in an interview.
“For AS, the results are very intriguing. If confirmed, it could be groundbreaking. AS is the most common valve disease in the developed world, and no medical therapy exists. The potential is immense,” commented George Thanassoulis, MD, director of preventive and genomic cardiology at McGill University, Montreal. “Having a medical treatment that could slow AS progression would completely change the disease. It’s conceivable to slow the disease enough that patients may never require valve replacement.” But an interview he cautioned that, “although the results are exciting, the analysis has many limitations. What we need is a dedicated, randomized trial for AS. I hope this stimulates that.”
“For VTE, it’s an interesting finding, but I don’t think it will have clinical utility because we have good treatment for VTE,” added Dr. Thanassoulis, but others saw more opportunity from what could be a new way to reduce VTE risk.
“Given that many patients have difficulty with the bleeding risk from anticoagulants, this option [a PCSK9 inhibitor] may be quite welcome for preventing VTE,” commented Gregory Piazza, MD, a cardiologist and VTE specialist at Brigham and Women’s Hospital who was not involved in any of the PCSK9 inhibitor studies.
“At this time we would not suggest that PCSK9 inhibitors replace an anticoagulant for patients with an established clot or at high risk for a recurrent clot, but if patients have an indication for a PCSK9 inhibitor, the further reduction in venous clot can be viewed as an additional benefit of this therapy,” said Dr. O’Donoghue.
How it might work
A possible mechanism underlying a VTE effect is unclear. Results from the JUPITER trial more than a decade ago had shown a significant association between treatment with 20 mg/day of rosuvastatin and a cut in VTE episodes, compared with placebo, in a prespecified, secondary analysis of the trial with nearly 18,000 patients selected for having a relatively high level of high-sensitivity C-reactive protein (N Engl J Med. 2009 Apr 30;360[18]:1851-61). But a meta-analysis of 29 controlled statin trials that used a variety of statin types and dosages (and included the JUPITER results) failed to confirm a statistically significant change in VTE rates from statins, though they produced a small, nominal reduction (PLoS Med. 2012 Sep 18. doi: 10.1371/journal.pmed.1001310).
Lp(a) “has long been linked to thrombosis, in particular arterial thrombosis,” so the link observed in the PCSK9 inhibitor trials “is not surprising,” said Dr. Piazza. Dr. O’Donoghue agreed that prior evidence had “suggested a prothrombotic role for Lp(a).”
Dr. Thanassoulis was more skeptical of a Lp(a) connection to VTE. “There has always been controversy regarding the prothrombotic effects of Lp(a) and whether it’s clinically relevant,” he said. “The genetic data, from Mendelian randomization studies, is not consistent” with a Lp(a) and VTE link.
The association of AS and Lp(a) may be stronger. “Our team showed that people with genetic variants that predispose to high Lp(a) have a much higher incidence of AS,” Dr. Thanassoulis noted. “We and others have also demonstrated that both Lp(a) and LDL are likely causal mediators of aortic valve calcification and stenosis.”
Dr. O’Donoghue also cited observational genetic data that linked elevated Lp(a) with AS. “Mendelian randomization studies have demonstrated that Lp(a) is a causal contributer to AS, and evolocumab reduced Lp(a) by 25%-30%, raising the possibility that Lp(a) lowering with these drugs may be the mechanism,” she said.
The future of Lp(a) lowering
This last point from Dr. O’Donoghue, that PCSK9 inhibitors cut Lp(a) levels by about 25%-30%, means that they are the most potent Lp(a)-lowering agents currently available, but it also leaves lots of room for other agents to do even better in cutting Lp(a).
“There are now drugs in development that block production of the Lp(a) protein and dramatically reduce its concentration, by about 80%,” Dr. O’Donoghue noted. “It will be of interest to study whether these novel therapies, now in phase 2 and phase 3 studies, have any effect on the risk for VTE and AS.”
“Several drugs in development, including antisense RNA and RNA-interfering molecules, are much more potent and lower Lp(a) by 80%-90%. Because of this potency they can completely normalize Lp(a) in most patients. For Lp(a) lowering, the future is in these new molecules. Randomized trials have started, and we will hopefully have some results in about 5 years,” said Dr. Thanassoulis.
Until then, the prospect of possibly soon documenting benefits from PCSK9 inhibitors beyond their impact on cutting LDL cholesterol raises some hope to get more bang for the considerable buck these drugs cost. But Dr. Thanassoulis was skeptical it would move the cost-benefit ratio much. “VTE and AS are relatively rare, compared with atherosclerotic cardiovascular events, and therefore the added value at the population level would be small,” he predicted. But if treatment with a drug could help patients avoid surgical or percutaneous valve interventions “that could be really interesting from a cost-benefit perspective.”
FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). ODYSSEY OUTCOMES was funded by Sanofi and Regeneron, the companies that developed and market alirocumab (Praluent). Dr. Marston had no disclosures. Dr. Bergmark has been a consultant to Daiichi Sankyo, Janssen, Quark, and Servier and has received research funding from Abbott Vascular, AstraZeneca, and MedImmune. Dr. O’Donoghue has been a consultant to and has received research funding from Amgen; has been a consultant to Janssen and Novartis; and has received research funding from AstraZeneca, Eisai, GlaxoSmithKline, Janssen, Medimmune, Merck, and The Medicines Company. Dr. Thanassoulis has been an adviser to and speaker for Amgen; an adviser to Ionis and Sanofi/Regeneron; a speaker on behalf of Boehringer Ingelheim, Sanofi, and Servier; and has received research funding from Ionis and Servier. Dr. Piazza has been a consultant to Optum, Pfizer, and Thrombolex and he has received research funding from Bayer, Bristol-Myers Squibb, Daiichi Sankyo, Ekos, Janssen, and Portola.
Post hoc analyses of recent large, clinical outcomes studies of PCSK9 inhibitors have revealed two tantalizing and unexpected potential benefits from these drugs: an ability to substantially reduce the incidence or severity of venous thromboembolism and aortic stenosis.
The evidence also suggests that these effects are linked to the ability of these drugs to reduce blood levels of Lp(a) lipoprotein by roughly a quarter, currently the biggest known effect on Lp(a) levels of any approved medication.
One study ran post hoc analyses of venous thromboembolism (VTE) events in the FOURIER pivotal trial of evolocumab (Repatha), with more than 27,500 randomized patients (N Engl J Med. 2017 May 4; 376[18]:1713-22), and in the ODYSSEY OUTCOMES pivotal trial of alirocumab (Praluent), with nearly 19,000 randomized patients (N Engl J Med. 2018 Nov 29;379[22]:2097-2107). The analyses showed that, with evolocumab treatment, the incidence of VTE events fell by a statistically significant 29%, compared with patients on placebo, while in ODYSSEY OUTCOMES patients treated with alirocumab had a 33% cut in VTE events, compared with placebo-treated patients, a difference that just missed statistical significance (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046524) in analyses that were not prespecified before these trials started, Nicholas A. Marston, MD, said in a presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
A combined analysis of 46,488 patients from both studies showed a 31% cut in VTE events with PCSK9 inhibitor treatment, a highly significant finding using VTE endpoints that were not specifically tallied nor adjudicated but collected as part of the serious adverse event reporting in the two pivotal trials, said Dr. Marston, a cardiologist at Brigham and Women’s Hospital in Boston. This is the first report of a statistically significant link between treatment with PCSK9-inhibiting agents and a reduction in VTE, he added. Researchers from the ODYSSEY OUTCOMES trial had reported a VTE analysis in 2019, and while data from that trial on its own showed a nominal 33% lower VTE rate with alirocumab treatment, it just missed statistical significance.
The VTE effect took about a year on treatment to start to manifest. During the first 12 months of FOURIER, the rate of VTE events among patients in the two treatment arms was virtually identical. But starting during months 13-18 on treatment, the event curves in the two arms began to increasingly diverge, and overall during the period from month 13 to the end of the study treatment with evolocumab was linked with a statistically significant 46% reduction in VTE events, compared with patients who received placebo. The results Dr. Marston reported were also published online (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046397).
The suggestion that this association may be linked to the impact of PCSK9 inhibitors on Lp(a) came from an additional analysis that Dr. Marston presented, which looked at the link between evolocumab use and a change in VTE event rates, compared with placebo, depending on baseline lipoprotein levels. Evolocumab treatment was associated with a roughly similar, modest, and not statistically significant reduction in VTE events, compared with placebo regardless of whether patients had baseline levels of LDL cholesterol below the median or at or above the median. In contrast, when a similar analysis divided patients based on whether their Lp(a) level at baseline was below, or at or above, the median the results showed no discernible effect of evolocumab treatment, compared with on VTE events in patients with lower baseline Lp(a), but in those with higher levels treatment with evolocumab linked with a 48% cut in VTE events, compared with placebo, a statistically significant difference.
In FOURIER, treatment with evolocumab lowered baseline Lp(a) levels by a median of 27%, compared with placebo, among the 25,096 enrolled patients who had their baseline levels measured. As previously reported, prespecified analysis of FOURIER data also showed that the impact of evolocumab, compared with placebo, on the combined rate of coronary heart disease death, MI, or need for urgent coronary revascularization was enhanced among patients with elevated baseline Lp(a) and moderated in those who entered with lower levels. Among patients who entered FOURIER with Lp(a) levels at or below the median treatment with evolocumab cut the primary endpoint by 7%, compared with placebo, a difference that was not statistically significant. Among patients who began the study with Lp(a) levels above the median, evolocumab treatment cut the primary endpoint by 23%, compared with placebo, a statistically significant effect (Circulation. 2019 Mar 19;139[12]:1483-92).
The aortic stenosis connection
A second study reported in the online scientific sessions (Abstract 914-08) used only FOURIER data, and showed that patients treated with evolocumab had a roughly similar response pattern in their incidence of aortic stenosis (AS) events as they did for VTE events.
During the first year of the study, the incidence of AS events was virtually identical among patients treated with evolocumab and those who received placebo. But after the first 12 months and through the study’s end, patients on evolocumab showed a statistically significant 52% relative reduction in AS events, compared with control patients, said Brian A. Bergmark, MD. For the entire study duration, treatment with evolocumab linked with a 34% relative reduction in AS events, compared with placebo, a difference that did not reach statistical significance, added Dr. Bergmark, an interventional cardiologist also at Brigham and Women’s Hospital. The observed halving in total AS events that linked with evolocumab treatment after the first year of the study included a similar-magnitude reduction specifically in the incidence of aortic valve replacement procedures in the evolocumab-treated patients.
Further analysis of both total AS events and aortic valve replacements in FOURIER patients showed that they occurred at a significantly elevated rate in patients who entered the study with higher baseline Lp(a) levels in a multivariate analysis, but a similar analysis showed no significant association between the incidence of these AS-related events and baseline levels of LDL cholesterol, he said.
The AS analysis carried the same important limitations as the VTE analysis: It ran on a post hoc basis and focused on events that were relatively uncommon and not adjudicated, Dr. Bergmark cautioned. Nonetheless, other investigators saw important potential implications from both the VTE and AS observations, with the huge caveat that they need replication in prospective studies designed to specifically address the validity of these findings.
What it could mean
These observed associations between PCSK9 inhibitor treatment and apparent reductions in the rate of both VTE and AS events “represent a tremendous clinical breakthrough,” commented Michelle L. O’Donoghue, MD, a cardiologist at Brigham and Women’s Hospital who is a FOURIER coinvestigator and has led some of the Lp(a) analyses run from that study.
“To date, we have not identified any therapies that slow progression of AS. Other classes of lipid-lowering therapies, such as statins, have been tested and not demonstrated a significant effect,” Dr. O’Donoghue said in an interview.
“For AS, the results are very intriguing. If confirmed, it could be groundbreaking. AS is the most common valve disease in the developed world, and no medical therapy exists. The potential is immense,” commented George Thanassoulis, MD, director of preventive and genomic cardiology at McGill University, Montreal. “Having a medical treatment that could slow AS progression would completely change the disease. It’s conceivable to slow the disease enough that patients may never require valve replacement.” But an interview he cautioned that, “although the results are exciting, the analysis has many limitations. What we need is a dedicated, randomized trial for AS. I hope this stimulates that.”
“For VTE, it’s an interesting finding, but I don’t think it will have clinical utility because we have good treatment for VTE,” added Dr. Thanassoulis, but others saw more opportunity from what could be a new way to reduce VTE risk.
“Given that many patients have difficulty with the bleeding risk from anticoagulants, this option [a PCSK9 inhibitor] may be quite welcome for preventing VTE,” commented Gregory Piazza, MD, a cardiologist and VTE specialist at Brigham and Women’s Hospital who was not involved in any of the PCSK9 inhibitor studies.
“At this time we would not suggest that PCSK9 inhibitors replace an anticoagulant for patients with an established clot or at high risk for a recurrent clot, but if patients have an indication for a PCSK9 inhibitor, the further reduction in venous clot can be viewed as an additional benefit of this therapy,” said Dr. O’Donoghue.
How it might work
A possible mechanism underlying a VTE effect is unclear. Results from the JUPITER trial more than a decade ago had shown a significant association between treatment with 20 mg/day of rosuvastatin and a cut in VTE episodes, compared with placebo, in a prespecified, secondary analysis of the trial with nearly 18,000 patients selected for having a relatively high level of high-sensitivity C-reactive protein (N Engl J Med. 2009 Apr 30;360[18]:1851-61). But a meta-analysis of 29 controlled statin trials that used a variety of statin types and dosages (and included the JUPITER results) failed to confirm a statistically significant change in VTE rates from statins, though they produced a small, nominal reduction (PLoS Med. 2012 Sep 18. doi: 10.1371/journal.pmed.1001310).
Lp(a) “has long been linked to thrombosis, in particular arterial thrombosis,” so the link observed in the PCSK9 inhibitor trials “is not surprising,” said Dr. Piazza. Dr. O’Donoghue agreed that prior evidence had “suggested a prothrombotic role for Lp(a).”
Dr. Thanassoulis was more skeptical of a Lp(a) connection to VTE. “There has always been controversy regarding the prothrombotic effects of Lp(a) and whether it’s clinically relevant,” he said. “The genetic data, from Mendelian randomization studies, is not consistent” with a Lp(a) and VTE link.
The association of AS and Lp(a) may be stronger. “Our team showed that people with genetic variants that predispose to high Lp(a) have a much higher incidence of AS,” Dr. Thanassoulis noted. “We and others have also demonstrated that both Lp(a) and LDL are likely causal mediators of aortic valve calcification and stenosis.”
Dr. O’Donoghue also cited observational genetic data that linked elevated Lp(a) with AS. “Mendelian randomization studies have demonstrated that Lp(a) is a causal contributer to AS, and evolocumab reduced Lp(a) by 25%-30%, raising the possibility that Lp(a) lowering with these drugs may be the mechanism,” she said.
The future of Lp(a) lowering
This last point from Dr. O’Donoghue, that PCSK9 inhibitors cut Lp(a) levels by about 25%-30%, means that they are the most potent Lp(a)-lowering agents currently available, but it also leaves lots of room for other agents to do even better in cutting Lp(a).
“There are now drugs in development that block production of the Lp(a) protein and dramatically reduce its concentration, by about 80%,” Dr. O’Donoghue noted. “It will be of interest to study whether these novel therapies, now in phase 2 and phase 3 studies, have any effect on the risk for VTE and AS.”
“Several drugs in development, including antisense RNA and RNA-interfering molecules, are much more potent and lower Lp(a) by 80%-90%. Because of this potency they can completely normalize Lp(a) in most patients. For Lp(a) lowering, the future is in these new molecules. Randomized trials have started, and we will hopefully have some results in about 5 years,” said Dr. Thanassoulis.
Until then, the prospect of possibly soon documenting benefits from PCSK9 inhibitors beyond their impact on cutting LDL cholesterol raises some hope to get more bang for the considerable buck these drugs cost. But Dr. Thanassoulis was skeptical it would move the cost-benefit ratio much. “VTE and AS are relatively rare, compared with atherosclerotic cardiovascular events, and therefore the added value at the population level would be small,” he predicted. But if treatment with a drug could help patients avoid surgical or percutaneous valve interventions “that could be really interesting from a cost-benefit perspective.”
FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). ODYSSEY OUTCOMES was funded by Sanofi and Regeneron, the companies that developed and market alirocumab (Praluent). Dr. Marston had no disclosures. Dr. Bergmark has been a consultant to Daiichi Sankyo, Janssen, Quark, and Servier and has received research funding from Abbott Vascular, AstraZeneca, and MedImmune. Dr. O’Donoghue has been a consultant to and has received research funding from Amgen; has been a consultant to Janssen and Novartis; and has received research funding from AstraZeneca, Eisai, GlaxoSmithKline, Janssen, Medimmune, Merck, and The Medicines Company. Dr. Thanassoulis has been an adviser to and speaker for Amgen; an adviser to Ionis and Sanofi/Regeneron; a speaker on behalf of Boehringer Ingelheim, Sanofi, and Servier; and has received research funding from Ionis and Servier. Dr. Piazza has been a consultant to Optum, Pfizer, and Thrombolex and he has received research funding from Bayer, Bristol-Myers Squibb, Daiichi Sankyo, Ekos, Janssen, and Portola.
Post hoc analyses of recent large, clinical outcomes studies of PCSK9 inhibitors have revealed two tantalizing and unexpected potential benefits from these drugs: an ability to substantially reduce the incidence or severity of venous thromboembolism and aortic stenosis.
The evidence also suggests that these effects are linked to the ability of these drugs to reduce blood levels of Lp(a) lipoprotein by roughly a quarter, currently the biggest known effect on Lp(a) levels of any approved medication.
One study ran post hoc analyses of venous thromboembolism (VTE) events in the FOURIER pivotal trial of evolocumab (Repatha), with more than 27,500 randomized patients (N Engl J Med. 2017 May 4; 376[18]:1713-22), and in the ODYSSEY OUTCOMES pivotal trial of alirocumab (Praluent), with nearly 19,000 randomized patients (N Engl J Med. 2018 Nov 29;379[22]:2097-2107). The analyses showed that, with evolocumab treatment, the incidence of VTE events fell by a statistically significant 29%, compared with patients on placebo, while in ODYSSEY OUTCOMES patients treated with alirocumab had a 33% cut in VTE events, compared with placebo-treated patients, a difference that just missed statistical significance (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046524) in analyses that were not prespecified before these trials started, Nicholas A. Marston, MD, said in a presentation of his research during the joint scientific sessions of the American College of Cardiology and the World Heart Federation, which was presented online this year. ACC organizers chose to present parts of the meeting virtually after COVID-19 concerns caused them to cancel the meeting.
A combined analysis of 46,488 patients from both studies showed a 31% cut in VTE events with PCSK9 inhibitor treatment, a highly significant finding using VTE endpoints that were not specifically tallied nor adjudicated but collected as part of the serious adverse event reporting in the two pivotal trials, said Dr. Marston, a cardiologist at Brigham and Women’s Hospital in Boston. This is the first report of a statistically significant link between treatment with PCSK9-inhibiting agents and a reduction in VTE, he added. Researchers from the ODYSSEY OUTCOMES trial had reported a VTE analysis in 2019, and while data from that trial on its own showed a nominal 33% lower VTE rate with alirocumab treatment, it just missed statistical significance.
The VTE effect took about a year on treatment to start to manifest. During the first 12 months of FOURIER, the rate of VTE events among patients in the two treatment arms was virtually identical. But starting during months 13-18 on treatment, the event curves in the two arms began to increasingly diverge, and overall during the period from month 13 to the end of the study treatment with evolocumab was linked with a statistically significant 46% reduction in VTE events, compared with patients who received placebo. The results Dr. Marston reported were also published online (Circulation. 2020 Mar 29. doi: 10.1161/CIRCULATIONAHA.120.046397).
The suggestion that this association may be linked to the impact of PCSK9 inhibitors on Lp(a) came from an additional analysis that Dr. Marston presented, which looked at the link between evolocumab use and a change in VTE event rates, compared with placebo, depending on baseline lipoprotein levels. Evolocumab treatment was associated with a roughly similar, modest, and not statistically significant reduction in VTE events, compared with placebo regardless of whether patients had baseline levels of LDL cholesterol below the median or at or above the median. In contrast, when a similar analysis divided patients based on whether their Lp(a) level at baseline was below, or at or above, the median the results showed no discernible effect of evolocumab treatment, compared with on VTE events in patients with lower baseline Lp(a), but in those with higher levels treatment with evolocumab linked with a 48% cut in VTE events, compared with placebo, a statistically significant difference.
In FOURIER, treatment with evolocumab lowered baseline Lp(a) levels by a median of 27%, compared with placebo, among the 25,096 enrolled patients who had their baseline levels measured. As previously reported, prespecified analysis of FOURIER data also showed that the impact of evolocumab, compared with placebo, on the combined rate of coronary heart disease death, MI, or need for urgent coronary revascularization was enhanced among patients with elevated baseline Lp(a) and moderated in those who entered with lower levels. Among patients who entered FOURIER with Lp(a) levels at or below the median treatment with evolocumab cut the primary endpoint by 7%, compared with placebo, a difference that was not statistically significant. Among patients who began the study with Lp(a) levels above the median, evolocumab treatment cut the primary endpoint by 23%, compared with placebo, a statistically significant effect (Circulation. 2019 Mar 19;139[12]:1483-92).
The aortic stenosis connection
A second study reported in the online scientific sessions (Abstract 914-08) used only FOURIER data, and showed that patients treated with evolocumab had a roughly similar response pattern in their incidence of aortic stenosis (AS) events as they did for VTE events.
During the first year of the study, the incidence of AS events was virtually identical among patients treated with evolocumab and those who received placebo. But after the first 12 months and through the study’s end, patients on evolocumab showed a statistically significant 52% relative reduction in AS events, compared with control patients, said Brian A. Bergmark, MD. For the entire study duration, treatment with evolocumab linked with a 34% relative reduction in AS events, compared with placebo, a difference that did not reach statistical significance, added Dr. Bergmark, an interventional cardiologist also at Brigham and Women’s Hospital. The observed halving in total AS events that linked with evolocumab treatment after the first year of the study included a similar-magnitude reduction specifically in the incidence of aortic valve replacement procedures in the evolocumab-treated patients.
Further analysis of both total AS events and aortic valve replacements in FOURIER patients showed that they occurred at a significantly elevated rate in patients who entered the study with higher baseline Lp(a) levels in a multivariate analysis, but a similar analysis showed no significant association between the incidence of these AS-related events and baseline levels of LDL cholesterol, he said.
The AS analysis carried the same important limitations as the VTE analysis: It ran on a post hoc basis and focused on events that were relatively uncommon and not adjudicated, Dr. Bergmark cautioned. Nonetheless, other investigators saw important potential implications from both the VTE and AS observations, with the huge caveat that they need replication in prospective studies designed to specifically address the validity of these findings.
What it could mean
These observed associations between PCSK9 inhibitor treatment and apparent reductions in the rate of both VTE and AS events “represent a tremendous clinical breakthrough,” commented Michelle L. O’Donoghue, MD, a cardiologist at Brigham and Women’s Hospital who is a FOURIER coinvestigator and has led some of the Lp(a) analyses run from that study.
“To date, we have not identified any therapies that slow progression of AS. Other classes of lipid-lowering therapies, such as statins, have been tested and not demonstrated a significant effect,” Dr. O’Donoghue said in an interview.
“For AS, the results are very intriguing. If confirmed, it could be groundbreaking. AS is the most common valve disease in the developed world, and no medical therapy exists. The potential is immense,” commented George Thanassoulis, MD, director of preventive and genomic cardiology at McGill University, Montreal. “Having a medical treatment that could slow AS progression would completely change the disease. It’s conceivable to slow the disease enough that patients may never require valve replacement.” But an interview he cautioned that, “although the results are exciting, the analysis has many limitations. What we need is a dedicated, randomized trial for AS. I hope this stimulates that.”
“For VTE, it’s an interesting finding, but I don’t think it will have clinical utility because we have good treatment for VTE,” added Dr. Thanassoulis, but others saw more opportunity from what could be a new way to reduce VTE risk.
“Given that many patients have difficulty with the bleeding risk from anticoagulants, this option [a PCSK9 inhibitor] may be quite welcome for preventing VTE,” commented Gregory Piazza, MD, a cardiologist and VTE specialist at Brigham and Women’s Hospital who was not involved in any of the PCSK9 inhibitor studies.
“At this time we would not suggest that PCSK9 inhibitors replace an anticoagulant for patients with an established clot or at high risk for a recurrent clot, but if patients have an indication for a PCSK9 inhibitor, the further reduction in venous clot can be viewed as an additional benefit of this therapy,” said Dr. O’Donoghue.
How it might work
A possible mechanism underlying a VTE effect is unclear. Results from the JUPITER trial more than a decade ago had shown a significant association between treatment with 20 mg/day of rosuvastatin and a cut in VTE episodes, compared with placebo, in a prespecified, secondary analysis of the trial with nearly 18,000 patients selected for having a relatively high level of high-sensitivity C-reactive protein (N Engl J Med. 2009 Apr 30;360[18]:1851-61). But a meta-analysis of 29 controlled statin trials that used a variety of statin types and dosages (and included the JUPITER results) failed to confirm a statistically significant change in VTE rates from statins, though they produced a small, nominal reduction (PLoS Med. 2012 Sep 18. doi: 10.1371/journal.pmed.1001310).
Lp(a) “has long been linked to thrombosis, in particular arterial thrombosis,” so the link observed in the PCSK9 inhibitor trials “is not surprising,” said Dr. Piazza. Dr. O’Donoghue agreed that prior evidence had “suggested a prothrombotic role for Lp(a).”
Dr. Thanassoulis was more skeptical of a Lp(a) connection to VTE. “There has always been controversy regarding the prothrombotic effects of Lp(a) and whether it’s clinically relevant,” he said. “The genetic data, from Mendelian randomization studies, is not consistent” with a Lp(a) and VTE link.
The association of AS and Lp(a) may be stronger. “Our team showed that people with genetic variants that predispose to high Lp(a) have a much higher incidence of AS,” Dr. Thanassoulis noted. “We and others have also demonstrated that both Lp(a) and LDL are likely causal mediators of aortic valve calcification and stenosis.”
Dr. O’Donoghue also cited observational genetic data that linked elevated Lp(a) with AS. “Mendelian randomization studies have demonstrated that Lp(a) is a causal contributer to AS, and evolocumab reduced Lp(a) by 25%-30%, raising the possibility that Lp(a) lowering with these drugs may be the mechanism,” she said.
The future of Lp(a) lowering
This last point from Dr. O’Donoghue, that PCSK9 inhibitors cut Lp(a) levels by about 25%-30%, means that they are the most potent Lp(a)-lowering agents currently available, but it also leaves lots of room for other agents to do even better in cutting Lp(a).
“There are now drugs in development that block production of the Lp(a) protein and dramatically reduce its concentration, by about 80%,” Dr. O’Donoghue noted. “It will be of interest to study whether these novel therapies, now in phase 2 and phase 3 studies, have any effect on the risk for VTE and AS.”
“Several drugs in development, including antisense RNA and RNA-interfering molecules, are much more potent and lower Lp(a) by 80%-90%. Because of this potency they can completely normalize Lp(a) in most patients. For Lp(a) lowering, the future is in these new molecules. Randomized trials have started, and we will hopefully have some results in about 5 years,” said Dr. Thanassoulis.
Until then, the prospect of possibly soon documenting benefits from PCSK9 inhibitors beyond their impact on cutting LDL cholesterol raises some hope to get more bang for the considerable buck these drugs cost. But Dr. Thanassoulis was skeptical it would move the cost-benefit ratio much. “VTE and AS are relatively rare, compared with atherosclerotic cardiovascular events, and therefore the added value at the population level would be small,” he predicted. But if treatment with a drug could help patients avoid surgical or percutaneous valve interventions “that could be really interesting from a cost-benefit perspective.”
FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). ODYSSEY OUTCOMES was funded by Sanofi and Regeneron, the companies that developed and market alirocumab (Praluent). Dr. Marston had no disclosures. Dr. Bergmark has been a consultant to Daiichi Sankyo, Janssen, Quark, and Servier and has received research funding from Abbott Vascular, AstraZeneca, and MedImmune. Dr. O’Donoghue has been a consultant to and has received research funding from Amgen; has been a consultant to Janssen and Novartis; and has received research funding from AstraZeneca, Eisai, GlaxoSmithKline, Janssen, Medimmune, Merck, and The Medicines Company. Dr. Thanassoulis has been an adviser to and speaker for Amgen; an adviser to Ionis and Sanofi/Regeneron; a speaker on behalf of Boehringer Ingelheim, Sanofi, and Servier; and has received research funding from Ionis and Servier. Dr. Piazza has been a consultant to Optum, Pfizer, and Thrombolex and he has received research funding from Bayer, Bristol-Myers Squibb, Daiichi Sankyo, Ekos, Janssen, and Portola.
REPORTING FROM ACC 20
Interim guidance for CPR in patients with COVID-19
The American Heart Association (AHA) and seven other medical societies have issued interim guidance to inform treatment of victims of cardiac arrest with suspected or confirmed COVID-19, focusing on reducing provider exposure, and prioritizing oxygenation and ventilation strategies, goals of care, and appropriateness of resuscitation.
“We were very specific in calling this ‘interim guidance’ based on expert opinion because things are evolving so quickly and we are learning more and more every day as more and more patients with COVID-19 are taken care of,” corresponding author Comilla Sasson, MD, PhD, vice president, Emergency Cardiovascular Care (ECC) Science and Innovation, American Heart Association, told theheart.org | Medscape Cardiology.
“We wanted this to be a starting point for providing the clinical guidance that everyone is looking for and, as we collect more data, the guidance will change, as it has for CDC [Centers for Disease Control and Prevention] and WHO [World Health Organization],” she said.
“The guidance sought to balance the provision of timely, high-quality resuscitation to patients while simultaneously protecting rescuers,” she added.
The guidance was published online April 9 in Circulation. The AHA produced the guidelines in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with support from the American Association of Critical Care Nurses and National EMS Physicians.
Respiratory Etiologies
“We think of cardiac arrest in adults, especially as related to cardiac etiologies, but we are now thinking of it in COVID-19 more as hypoxemia or respiratory failure, which can predispose patients to cardiac arrest,” Sasson explained.
Healthcare workers are the “highest-risk profession” for contracting the COVID-19, with resuscitations carrying “added risk” for several reasons, the authors note.
Administering CPR involves performing numerous aerosol-generating procedures that can cause viral particles to remain suspended in the air and be inhaled by those nearby, with a half-life of approximately 1 hour, they point out.
Moreover, resuscitation efforts “require numerous providers to work in close proximity to one another and the patient,” and the high-stress emergent nature of these events may result in lapses in infection-control procedures.
The guidance is designed “to protect not only the patient but also the provider and involves strategies regarding oxygenation and ventilation that differ from what we’ve done in the past since we have a strong feeling that this is a different disease process that may require different approaches than what we’ve dealt with in the past,” Sasson commented.
Reducing Provider Exposure
Providers should don PPE to protect both themselves and their colleagues from unnecessary exposure, the authors advise, noting that recommendations for PPE standards may “vary considerably,” so health or emergency medical services (EMS) standards should be taken into account.
Moreover, it is important to allow only the most essential providers into the room or on the scene. In keeping with reducing the number of rescuers, the authors recommend replacing manual chest compressions with mechanical CPR devices for patients who meet height and weight criteria in settings with “protocols and expertise in place for their use.”
COVID-19 status should be communicated to any new providers prior to their arrival on the scene, the authors stress.
Oxygenation and Ventilation Strategies
“Reducing risk of aerosolization during the process of intubation is key,” Sasson emphasized.
For this reason, a high-efficiency particulate air HEPA filter (if available) should be attached to any manual or mechanical ventilation device, specifically in the path of exhaled gas, before any breaths are administered.
Moreover, it is important to intubate early with a cuffed tube and connect to a mechanical ventilator, if possible. The intubator should be engaged with the “highest chance of first-pass success,” and chest compression should be paused to intubate.
To further increase the chance of a successful first intubation, use of video laryngoscopy (if available) is helpful.
Additional guidance includes:
- Using a bag-mask device (or T-piece in neonates) with a HEPA filter and a tight seal prior to intubation
- Considering passive oxygenation with non-rebreathing face mask as an alternative to bag-mask device for short duration (in adults)
- Considering supraglottic airway if intubation is delayed
- Minimizing closed circuit disconnections.
Resuscitation Considerations
“One big take-home point of the guidance is to consider resuscitation appropriateness, starting with goals of care when the patient comes to us, and continuing or stopping resuscitation when needed, based on the discussion with the family as well as local protocol,” Sasson said.
A variety of factors need to be taken into account, including age, comorbidities, and illness severity to determine the appropriateness of resuscitation, and “the likelihood of success” must be balanced “against the risk to rescuers and patients from whom resources are being diverted,” the authors state.
An Array of Scenarios
“We divided bystander CPR into adults vs pediatrics and into those who are living with a person who is in cardiac arrest – because they have already been exposed [to COVID-19] – vs those who are not living with the patient,” Sasson reported. “We also addressed the role of lay bystanders.”
For lay rescuers:
- Household members should perform at least hands-only CPR, if willing and able to do so
- Use of a face mark or cloth covering of the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold member
- In children, lay rescuers should perform chest compressions and “consider mouth-to-mouth resuscitation,” especially if they are household members.
- If available, an automated external defibrillator should be used to assess and treat victims of out-of-hospital cardiac arrest (OHCA).
The authors offer additional guidance for in-hospital cardiac arrest (IHCA), including addressing advanced care directives, closing the door when possible to prevent airborne contamination of adjacent space, and considering leaving the patient on a mechanical ventilator with HEPA filter.
They additionally address the special needs of neonates, recommending the presence of a “skilled attendant prepared to resuscitate, irrespective of COVID-19 status,” and stressing the importance of PPE since the mother may be a “potential source of aerosolization for the neonatal team.” Additional measures include avoidance of routine airway suctioning and the use of endotracheal medications.
Critically ill pregnant women with COVID-19 are more vulnerable to acute decompensation because of the cardiopulmonary physiological changes associated with pregnancy, the authors note. Preparation for a potential perimortem delivery should take place after 4 minutes of resuscitation and be initiated early in the resuscitation algorithm so as to allow specialized obstetrical and neonatal teams with PPE to convene.
“We will be continually updating this guidance and we are encouraging people to ask questions,” Sasson summarized.
She noted that a hospital-based COVID-19 registry is being formed to collect “clinically relevant data” that will inform and update the current guidance.
Sasson reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper.
This article first appeared on Medscape.com.
The American Heart Association (AHA) and seven other medical societies have issued interim guidance to inform treatment of victims of cardiac arrest with suspected or confirmed COVID-19, focusing on reducing provider exposure, and prioritizing oxygenation and ventilation strategies, goals of care, and appropriateness of resuscitation.
“We were very specific in calling this ‘interim guidance’ based on expert opinion because things are evolving so quickly and we are learning more and more every day as more and more patients with COVID-19 are taken care of,” corresponding author Comilla Sasson, MD, PhD, vice president, Emergency Cardiovascular Care (ECC) Science and Innovation, American Heart Association, told theheart.org | Medscape Cardiology.
“We wanted this to be a starting point for providing the clinical guidance that everyone is looking for and, as we collect more data, the guidance will change, as it has for CDC [Centers for Disease Control and Prevention] and WHO [World Health Organization],” she said.
“The guidance sought to balance the provision of timely, high-quality resuscitation to patients while simultaneously protecting rescuers,” she added.
The guidance was published online April 9 in Circulation. The AHA produced the guidelines in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with support from the American Association of Critical Care Nurses and National EMS Physicians.
Respiratory Etiologies
“We think of cardiac arrest in adults, especially as related to cardiac etiologies, but we are now thinking of it in COVID-19 more as hypoxemia or respiratory failure, which can predispose patients to cardiac arrest,” Sasson explained.
Healthcare workers are the “highest-risk profession” for contracting the COVID-19, with resuscitations carrying “added risk” for several reasons, the authors note.
Administering CPR involves performing numerous aerosol-generating procedures that can cause viral particles to remain suspended in the air and be inhaled by those nearby, with a half-life of approximately 1 hour, they point out.
Moreover, resuscitation efforts “require numerous providers to work in close proximity to one another and the patient,” and the high-stress emergent nature of these events may result in lapses in infection-control procedures.
The guidance is designed “to protect not only the patient but also the provider and involves strategies regarding oxygenation and ventilation that differ from what we’ve done in the past since we have a strong feeling that this is a different disease process that may require different approaches than what we’ve dealt with in the past,” Sasson commented.
Reducing Provider Exposure
Providers should don PPE to protect both themselves and their colleagues from unnecessary exposure, the authors advise, noting that recommendations for PPE standards may “vary considerably,” so health or emergency medical services (EMS) standards should be taken into account.
Moreover, it is important to allow only the most essential providers into the room or on the scene. In keeping with reducing the number of rescuers, the authors recommend replacing manual chest compressions with mechanical CPR devices for patients who meet height and weight criteria in settings with “protocols and expertise in place for their use.”
COVID-19 status should be communicated to any new providers prior to their arrival on the scene, the authors stress.
Oxygenation and Ventilation Strategies
“Reducing risk of aerosolization during the process of intubation is key,” Sasson emphasized.
For this reason, a high-efficiency particulate air HEPA filter (if available) should be attached to any manual or mechanical ventilation device, specifically in the path of exhaled gas, before any breaths are administered.
Moreover, it is important to intubate early with a cuffed tube and connect to a mechanical ventilator, if possible. The intubator should be engaged with the “highest chance of first-pass success,” and chest compression should be paused to intubate.
To further increase the chance of a successful first intubation, use of video laryngoscopy (if available) is helpful.
Additional guidance includes:
- Using a bag-mask device (or T-piece in neonates) with a HEPA filter and a tight seal prior to intubation
- Considering passive oxygenation with non-rebreathing face mask as an alternative to bag-mask device for short duration (in adults)
- Considering supraglottic airway if intubation is delayed
- Minimizing closed circuit disconnections.
Resuscitation Considerations
“One big take-home point of the guidance is to consider resuscitation appropriateness, starting with goals of care when the patient comes to us, and continuing or stopping resuscitation when needed, based on the discussion with the family as well as local protocol,” Sasson said.
A variety of factors need to be taken into account, including age, comorbidities, and illness severity to determine the appropriateness of resuscitation, and “the likelihood of success” must be balanced “against the risk to rescuers and patients from whom resources are being diverted,” the authors state.
An Array of Scenarios
“We divided bystander CPR into adults vs pediatrics and into those who are living with a person who is in cardiac arrest – because they have already been exposed [to COVID-19] – vs those who are not living with the patient,” Sasson reported. “We also addressed the role of lay bystanders.”
For lay rescuers:
- Household members should perform at least hands-only CPR, if willing and able to do so
- Use of a face mark or cloth covering of the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold member
- In children, lay rescuers should perform chest compressions and “consider mouth-to-mouth resuscitation,” especially if they are household members.
- If available, an automated external defibrillator should be used to assess and treat victims of out-of-hospital cardiac arrest (OHCA).
The authors offer additional guidance for in-hospital cardiac arrest (IHCA), including addressing advanced care directives, closing the door when possible to prevent airborne contamination of adjacent space, and considering leaving the patient on a mechanical ventilator with HEPA filter.
They additionally address the special needs of neonates, recommending the presence of a “skilled attendant prepared to resuscitate, irrespective of COVID-19 status,” and stressing the importance of PPE since the mother may be a “potential source of aerosolization for the neonatal team.” Additional measures include avoidance of routine airway suctioning and the use of endotracheal medications.
Critically ill pregnant women with COVID-19 are more vulnerable to acute decompensation because of the cardiopulmonary physiological changes associated with pregnancy, the authors note. Preparation for a potential perimortem delivery should take place after 4 minutes of resuscitation and be initiated early in the resuscitation algorithm so as to allow specialized obstetrical and neonatal teams with PPE to convene.
“We will be continually updating this guidance and we are encouraging people to ask questions,” Sasson summarized.
She noted that a hospital-based COVID-19 registry is being formed to collect “clinically relevant data” that will inform and update the current guidance.
Sasson reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper.
This article first appeared on Medscape.com.
The American Heart Association (AHA) and seven other medical societies have issued interim guidance to inform treatment of victims of cardiac arrest with suspected or confirmed COVID-19, focusing on reducing provider exposure, and prioritizing oxygenation and ventilation strategies, goals of care, and appropriateness of resuscitation.
“We were very specific in calling this ‘interim guidance’ based on expert opinion because things are evolving so quickly and we are learning more and more every day as more and more patients with COVID-19 are taken care of,” corresponding author Comilla Sasson, MD, PhD, vice president, Emergency Cardiovascular Care (ECC) Science and Innovation, American Heart Association, told theheart.org | Medscape Cardiology.
“We wanted this to be a starting point for providing the clinical guidance that everyone is looking for and, as we collect more data, the guidance will change, as it has for CDC [Centers for Disease Control and Prevention] and WHO [World Health Organization],” she said.
“The guidance sought to balance the provision of timely, high-quality resuscitation to patients while simultaneously protecting rescuers,” she added.
The guidance was published online April 9 in Circulation. The AHA produced the guidelines in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with support from the American Association of Critical Care Nurses and National EMS Physicians.
Respiratory Etiologies
“We think of cardiac arrest in adults, especially as related to cardiac etiologies, but we are now thinking of it in COVID-19 more as hypoxemia or respiratory failure, which can predispose patients to cardiac arrest,” Sasson explained.
Healthcare workers are the “highest-risk profession” for contracting the COVID-19, with resuscitations carrying “added risk” for several reasons, the authors note.
Administering CPR involves performing numerous aerosol-generating procedures that can cause viral particles to remain suspended in the air and be inhaled by those nearby, with a half-life of approximately 1 hour, they point out.
Moreover, resuscitation efforts “require numerous providers to work in close proximity to one another and the patient,” and the high-stress emergent nature of these events may result in lapses in infection-control procedures.
The guidance is designed “to protect not only the patient but also the provider and involves strategies regarding oxygenation and ventilation that differ from what we’ve done in the past since we have a strong feeling that this is a different disease process that may require different approaches than what we’ve dealt with in the past,” Sasson commented.
Reducing Provider Exposure
Providers should don PPE to protect both themselves and their colleagues from unnecessary exposure, the authors advise, noting that recommendations for PPE standards may “vary considerably,” so health or emergency medical services (EMS) standards should be taken into account.
Moreover, it is important to allow only the most essential providers into the room or on the scene. In keeping with reducing the number of rescuers, the authors recommend replacing manual chest compressions with mechanical CPR devices for patients who meet height and weight criteria in settings with “protocols and expertise in place for their use.”
COVID-19 status should be communicated to any new providers prior to their arrival on the scene, the authors stress.
Oxygenation and Ventilation Strategies
“Reducing risk of aerosolization during the process of intubation is key,” Sasson emphasized.
For this reason, a high-efficiency particulate air HEPA filter (if available) should be attached to any manual or mechanical ventilation device, specifically in the path of exhaled gas, before any breaths are administered.
Moreover, it is important to intubate early with a cuffed tube and connect to a mechanical ventilator, if possible. The intubator should be engaged with the “highest chance of first-pass success,” and chest compression should be paused to intubate.
To further increase the chance of a successful first intubation, use of video laryngoscopy (if available) is helpful.
Additional guidance includes:
- Using a bag-mask device (or T-piece in neonates) with a HEPA filter and a tight seal prior to intubation
- Considering passive oxygenation with non-rebreathing face mask as an alternative to bag-mask device for short duration (in adults)
- Considering supraglottic airway if intubation is delayed
- Minimizing closed circuit disconnections.
Resuscitation Considerations
“One big take-home point of the guidance is to consider resuscitation appropriateness, starting with goals of care when the patient comes to us, and continuing or stopping resuscitation when needed, based on the discussion with the family as well as local protocol,” Sasson said.
A variety of factors need to be taken into account, including age, comorbidities, and illness severity to determine the appropriateness of resuscitation, and “the likelihood of success” must be balanced “against the risk to rescuers and patients from whom resources are being diverted,” the authors state.
An Array of Scenarios
“We divided bystander CPR into adults vs pediatrics and into those who are living with a person who is in cardiac arrest – because they have already been exposed [to COVID-19] – vs those who are not living with the patient,” Sasson reported. “We also addressed the role of lay bystanders.”
For lay rescuers:
- Household members should perform at least hands-only CPR, if willing and able to do so
- Use of a face mark or cloth covering of the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold member
- In children, lay rescuers should perform chest compressions and “consider mouth-to-mouth resuscitation,” especially if they are household members.
- If available, an automated external defibrillator should be used to assess and treat victims of out-of-hospital cardiac arrest (OHCA).
The authors offer additional guidance for in-hospital cardiac arrest (IHCA), including addressing advanced care directives, closing the door when possible to prevent airborne contamination of adjacent space, and considering leaving the patient on a mechanical ventilator with HEPA filter.
They additionally address the special needs of neonates, recommending the presence of a “skilled attendant prepared to resuscitate, irrespective of COVID-19 status,” and stressing the importance of PPE since the mother may be a “potential source of aerosolization for the neonatal team.” Additional measures include avoidance of routine airway suctioning and the use of endotracheal medications.
Critically ill pregnant women with COVID-19 are more vulnerable to acute decompensation because of the cardiopulmonary physiological changes associated with pregnancy, the authors note. Preparation for a potential perimortem delivery should take place after 4 minutes of resuscitation and be initiated early in the resuscitation algorithm so as to allow specialized obstetrical and neonatal teams with PPE to convene.
“We will be continually updating this guidance and we are encouraging people to ask questions,” Sasson summarized.
She noted that a hospital-based COVID-19 registry is being formed to collect “clinically relevant data” that will inform and update the current guidance.
Sasson reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper.
This article first appeared on Medscape.com.
EHA and TIF explore how COVID-19 is affecting thalassemia and SCD patients
In a webinar designed to guide physicians in the care of hematology patients during the COVID-19 pandemic, three world experts on thalassemia and sickle cell disease (SCD) provided on-the-ground information from physicians who were dealing with the height of the crisis in their countries.
The webinar was organized by the European Hematology Association (EHA) and the Thalassemia International Federation (TIF).
Moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, led the discussion with three guest speakers: Maria-Domenica Cappellini, MD, PhD, professor of hematology at the University of Milan; Androulla Eleftheriou, MD, executive director of TIF in Cyprus; and Raffaella Colombatti , MD, of the University of Padova in Italy, coordinator of the Red Cell Reserve Working Group of the Italian Association of Pediatric Hematology and Oncology.
Italian experience with thalassemia and COVID-19
Dr. Cappellini discussed the Italian experience with 11 thalassemia patients followed by a network survey who developed COVID-19 in the northern part of Italy, where the pandemic has been most widespread.
There are no published data focusing specifically on SARS-CoV-2 infection in patients with thalassemic syndromes, but patients with preexisting comorbidities are likely to be more severely affected by SARS-CoV-2, according to Dr. Cappellini.
Of particular concern is the fact that patients with thalassemia, especially older ones, are frequently splenectomized, which renders them more vulnerable to bacterial infections and can trigger life-threatening sepsis. However, splenectomy is not known to increase the risk of viral infection or severe viral illness. Of additional concern is the fact that many thalassemia patients need routine and frequent transfusions.
Overall, the 11 thalassemia patients who developed COVID-19 experienced only mild to moderate symptoms. This is despite the fact that 72% of the patients were splenectomized, which did not appear to affect the clinical course, and all of the patients had thalassemia-related comorbidities.
Around half of the patients were hospitalized, but none of them required transfer to the ICU. One patient who was treated with chemotherapy for diffuse large B-cell lymphoma in 2019 but is now in remission required more intense ventilation support with the use of continuous positive airway pressure.
Only three patients received specific treatment for COVID-19: one with hydroxychloroquine (HCQ) alone, one with HCQ plus anakinra, and one with HCQ plus ritonavir/darunavir.
Overall, “the number of infected thalassemia patients was lower than expected, likely due to earlier and more vigilant self-isolation compared to the general population,” Dr. Cappellini said. She pointed out that the first early response in February by thalassemia physicians was to warn their patients via email and phone calls about the need for self-isolation and precautions against the pandemic.
Physicians “rapidly reorganized activities, postponing nonessential ones” and managed to provide patients “a safe track at the hospital to receive their life-saving treatment in COVID-19–free areas with health care personnel wearing protective equipment” and assessment of all entering patients for COVID-19 infection, Dr. Cappellini said.
Results in additional thalassemia patients and SCD patients
Dr. Eleftheriou described 51 cases of thalassemia patients with SARS-CoV-2 infection reported to TIF as of April 16. Patients were from Cyprus, Italy, the United Kingdom, France, Turkey, Iran, Pakistan, and Indonesia.
Of the 51 patients, 46 presented with mild to moderate symptoms. Five patients had severe respiratory symptoms and required hospitalization, two were hospitalized and discharged, and three died between day 5 and day 15 post hospitalization.
Dr. Colombatti followed with a brief presentation of the intersection of COVID-19 with SCD patients. She presented anecdotal data involving 32 SCD patients who exhibited COVID-19 symptoms. Dr. Colombatti obtained the data via personal communication with Pablo Bartolucci, of Hôpitaux Universitaires Henri Mondor in Créteil, France.
All 32 SCD patients were screened and treated for COVID-19, and 17 of them continued treatment for 10 days. In all, 22 patients were hospitalized, 11 were transferred to the ICU, and 1 died.
Ensuring adequate blood supply
Dr. Eleftheriou also discussed the TIF response to the COVID-19 pandemic, which focused on the adequacy of blood supplies for these patients who so often need transfusions.
Dr. Eleftheriou stated that a shortage of blood was reported in 75% of the 62 member countries of the TIF, with 58% reporting severe shortages and 35% reporting moderate to severe shortages.
The shortages resulted in many countries returning to older family/friends donation practices, rare use of whole blood transfusions, and the use of older blood transfusions (older than 28 days).
In addition, physicians have modified their transfusion strategy. They have reduced the amount of blood given to thalassemia patients from two units to one unit during any transfusion, while making arrangements for more frequent transfusions; for example, one transfusion per week but with precautions made to “limit the time spent in the clinic and to control blood supplies while safeguarding that all [thalassemia] patients will be able to get their transfusion,” Dr. Eleftheriou said.
The information in the webinar was provided with the caveat that “no general evidence-based guidance can be derived from this discussion.” There were no other disclosures given.
In a webinar designed to guide physicians in the care of hematology patients during the COVID-19 pandemic, three world experts on thalassemia and sickle cell disease (SCD) provided on-the-ground information from physicians who were dealing with the height of the crisis in their countries.
The webinar was organized by the European Hematology Association (EHA) and the Thalassemia International Federation (TIF).
Moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, led the discussion with three guest speakers: Maria-Domenica Cappellini, MD, PhD, professor of hematology at the University of Milan; Androulla Eleftheriou, MD, executive director of TIF in Cyprus; and Raffaella Colombatti , MD, of the University of Padova in Italy, coordinator of the Red Cell Reserve Working Group of the Italian Association of Pediatric Hematology and Oncology.
Italian experience with thalassemia and COVID-19
Dr. Cappellini discussed the Italian experience with 11 thalassemia patients followed by a network survey who developed COVID-19 in the northern part of Italy, where the pandemic has been most widespread.
There are no published data focusing specifically on SARS-CoV-2 infection in patients with thalassemic syndromes, but patients with preexisting comorbidities are likely to be more severely affected by SARS-CoV-2, according to Dr. Cappellini.
Of particular concern is the fact that patients with thalassemia, especially older ones, are frequently splenectomized, which renders them more vulnerable to bacterial infections and can trigger life-threatening sepsis. However, splenectomy is not known to increase the risk of viral infection or severe viral illness. Of additional concern is the fact that many thalassemia patients need routine and frequent transfusions.
Overall, the 11 thalassemia patients who developed COVID-19 experienced only mild to moderate symptoms. This is despite the fact that 72% of the patients were splenectomized, which did not appear to affect the clinical course, and all of the patients had thalassemia-related comorbidities.
Around half of the patients were hospitalized, but none of them required transfer to the ICU. One patient who was treated with chemotherapy for diffuse large B-cell lymphoma in 2019 but is now in remission required more intense ventilation support with the use of continuous positive airway pressure.
Only three patients received specific treatment for COVID-19: one with hydroxychloroquine (HCQ) alone, one with HCQ plus anakinra, and one with HCQ plus ritonavir/darunavir.
Overall, “the number of infected thalassemia patients was lower than expected, likely due to earlier and more vigilant self-isolation compared to the general population,” Dr. Cappellini said. She pointed out that the first early response in February by thalassemia physicians was to warn their patients via email and phone calls about the need for self-isolation and precautions against the pandemic.
Physicians “rapidly reorganized activities, postponing nonessential ones” and managed to provide patients “a safe track at the hospital to receive their life-saving treatment in COVID-19–free areas with health care personnel wearing protective equipment” and assessment of all entering patients for COVID-19 infection, Dr. Cappellini said.
Results in additional thalassemia patients and SCD patients
Dr. Eleftheriou described 51 cases of thalassemia patients with SARS-CoV-2 infection reported to TIF as of April 16. Patients were from Cyprus, Italy, the United Kingdom, France, Turkey, Iran, Pakistan, and Indonesia.
Of the 51 patients, 46 presented with mild to moderate symptoms. Five patients had severe respiratory symptoms and required hospitalization, two were hospitalized and discharged, and three died between day 5 and day 15 post hospitalization.
Dr. Colombatti followed with a brief presentation of the intersection of COVID-19 with SCD patients. She presented anecdotal data involving 32 SCD patients who exhibited COVID-19 symptoms. Dr. Colombatti obtained the data via personal communication with Pablo Bartolucci, of Hôpitaux Universitaires Henri Mondor in Créteil, France.
All 32 SCD patients were screened and treated for COVID-19, and 17 of them continued treatment for 10 days. In all, 22 patients were hospitalized, 11 were transferred to the ICU, and 1 died.
Ensuring adequate blood supply
Dr. Eleftheriou also discussed the TIF response to the COVID-19 pandemic, which focused on the adequacy of blood supplies for these patients who so often need transfusions.
Dr. Eleftheriou stated that a shortage of blood was reported in 75% of the 62 member countries of the TIF, with 58% reporting severe shortages and 35% reporting moderate to severe shortages.
The shortages resulted in many countries returning to older family/friends donation practices, rare use of whole blood transfusions, and the use of older blood transfusions (older than 28 days).
In addition, physicians have modified their transfusion strategy. They have reduced the amount of blood given to thalassemia patients from two units to one unit during any transfusion, while making arrangements for more frequent transfusions; for example, one transfusion per week but with precautions made to “limit the time spent in the clinic and to control blood supplies while safeguarding that all [thalassemia] patients will be able to get their transfusion,” Dr. Eleftheriou said.
The information in the webinar was provided with the caveat that “no general evidence-based guidance can be derived from this discussion.” There were no other disclosures given.
In a webinar designed to guide physicians in the care of hematology patients during the COVID-19 pandemic, three world experts on thalassemia and sickle cell disease (SCD) provided on-the-ground information from physicians who were dealing with the height of the crisis in their countries.
The webinar was organized by the European Hematology Association (EHA) and the Thalassemia International Federation (TIF).
Moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, led the discussion with three guest speakers: Maria-Domenica Cappellini, MD, PhD, professor of hematology at the University of Milan; Androulla Eleftheriou, MD, executive director of TIF in Cyprus; and Raffaella Colombatti , MD, of the University of Padova in Italy, coordinator of the Red Cell Reserve Working Group of the Italian Association of Pediatric Hematology and Oncology.
Italian experience with thalassemia and COVID-19
Dr. Cappellini discussed the Italian experience with 11 thalassemia patients followed by a network survey who developed COVID-19 in the northern part of Italy, where the pandemic has been most widespread.
There are no published data focusing specifically on SARS-CoV-2 infection in patients with thalassemic syndromes, but patients with preexisting comorbidities are likely to be more severely affected by SARS-CoV-2, according to Dr. Cappellini.
Of particular concern is the fact that patients with thalassemia, especially older ones, are frequently splenectomized, which renders them more vulnerable to bacterial infections and can trigger life-threatening sepsis. However, splenectomy is not known to increase the risk of viral infection or severe viral illness. Of additional concern is the fact that many thalassemia patients need routine and frequent transfusions.
Overall, the 11 thalassemia patients who developed COVID-19 experienced only mild to moderate symptoms. This is despite the fact that 72% of the patients were splenectomized, which did not appear to affect the clinical course, and all of the patients had thalassemia-related comorbidities.
Around half of the patients were hospitalized, but none of them required transfer to the ICU. One patient who was treated with chemotherapy for diffuse large B-cell lymphoma in 2019 but is now in remission required more intense ventilation support with the use of continuous positive airway pressure.
Only three patients received specific treatment for COVID-19: one with hydroxychloroquine (HCQ) alone, one with HCQ plus anakinra, and one with HCQ plus ritonavir/darunavir.
Overall, “the number of infected thalassemia patients was lower than expected, likely due to earlier and more vigilant self-isolation compared to the general population,” Dr. Cappellini said. She pointed out that the first early response in February by thalassemia physicians was to warn their patients via email and phone calls about the need for self-isolation and precautions against the pandemic.
Physicians “rapidly reorganized activities, postponing nonessential ones” and managed to provide patients “a safe track at the hospital to receive their life-saving treatment in COVID-19–free areas with health care personnel wearing protective equipment” and assessment of all entering patients for COVID-19 infection, Dr. Cappellini said.
Results in additional thalassemia patients and SCD patients
Dr. Eleftheriou described 51 cases of thalassemia patients with SARS-CoV-2 infection reported to TIF as of April 16. Patients were from Cyprus, Italy, the United Kingdom, France, Turkey, Iran, Pakistan, and Indonesia.
Of the 51 patients, 46 presented with mild to moderate symptoms. Five patients had severe respiratory symptoms and required hospitalization, two were hospitalized and discharged, and three died between day 5 and day 15 post hospitalization.
Dr. Colombatti followed with a brief presentation of the intersection of COVID-19 with SCD patients. She presented anecdotal data involving 32 SCD patients who exhibited COVID-19 symptoms. Dr. Colombatti obtained the data via personal communication with Pablo Bartolucci, of Hôpitaux Universitaires Henri Mondor in Créteil, France.
All 32 SCD patients were screened and treated for COVID-19, and 17 of them continued treatment for 10 days. In all, 22 patients were hospitalized, 11 were transferred to the ICU, and 1 died.
Ensuring adequate blood supply
Dr. Eleftheriou also discussed the TIF response to the COVID-19 pandemic, which focused on the adequacy of blood supplies for these patients who so often need transfusions.
Dr. Eleftheriou stated that a shortage of blood was reported in 75% of the 62 member countries of the TIF, with 58% reporting severe shortages and 35% reporting moderate to severe shortages.
The shortages resulted in many countries returning to older family/friends donation practices, rare use of whole blood transfusions, and the use of older blood transfusions (older than 28 days).
In addition, physicians have modified their transfusion strategy. They have reduced the amount of blood given to thalassemia patients from two units to one unit during any transfusion, while making arrangements for more frequent transfusions; for example, one transfusion per week but with precautions made to “limit the time spent in the clinic and to control blood supplies while safeguarding that all [thalassemia] patients will be able to get their transfusion,” Dr. Eleftheriou said.
The information in the webinar was provided with the caveat that “no general evidence-based guidance can be derived from this discussion.” There were no other disclosures given.
Flexibility and speed mark the race to a COVID-19 vaccine
Extraordinary cooperation and accommodations are needed in the race to build a COVID-19 vaccine from scratch while chasing a pandemic, said members of industry and government who convened for an update on the vaccine clinical trial process.
The message came from representatives from the Food and Drug Administration, a think tank, and the nonprofit sector who provided some insight into the vaccine development process for COVID-19 at a press briefing hosted by the Commonwealth Fund.
Even in the best of times, vaccine development is not simple, said Litjen (L.J.) Tan, PhD, chief strategy officer for the Immunization Action Coalition. Ordinarily, the process can take from 10 to 20 years and cost well over a billion dollars. Many vaccines wind up being abandoned before phase 3 development just because the cost is prohibitive, he said.
Vaccines undergo extensive ongoing postmarketing surveillance even after approval, licensing, and distribution, noted Dr. Tan, adding that the development of a safe, effective vaccine is a “very complicated, significant process.”
In these extraordinary times, many adjustments to the usual trial trajectory are needed, agreed all participants. To speed the process, the traditional vaccine trajectory is being accelerated and compressed; changes may include simultaneous rather than sequential clinical trials that are run in parallel. These trials may be optimized for multiple target populations at the same time, and run in different countries, explained Dr. Tan.
“We are likely going to use something called adaptive trial designs” in which results are gathered during the trial and used to modify the trial according to prespecified rules, he said. “These trials shift to accommodate data as it comes up.”
Regulatory agencies are actively engaging in the process much earlier than usual, with input including how to incentivize scaling up production of vaccines and ensuring that vaccines will be fairly and equitably distributed across the globe, he added.
Esther Krofah is the executive director of FasterCures, a center within the nonprofit Milken Institute. Currently 86 different active COVID-19 vaccine projects are underway, she said, with 6 currently in clinical trials and about two dozen more expected to enter the clinical trial phase by the summer of 2020.
Many of these projects will involve a smaller biotech company or an academic research group with deep knowledge of a particular immune strategy partnering with a large pharmaceutical company that has economic capacity and global resources and reach, said Ms. Krofah.
From a policy perspective, she said, it’s important for the FDA to have surge capacity with “enough arms, legs, and staff to actively provide input into clinical design and protocols of studies.” The goal is to be able to review data in real-time and provide rapid feedback as studies are occurring so adaptive clinical trial design can be implemented.
As COVID-19 vaccine trials are rolled out, necessary compromises may include incorporation of real world evidence in later clinical trial stages. “There is a way to do randomized trials in the real world in situations that come up like this,” said Peter Marks, MD, the FDA’s director of the Center for Biologics Evaluation and Research. Long-term data about vaccine efficacy may be accrued over time, once a vaccine is being administered beyond the clinical trial stage, to see if efficacy wanes over time.
However, he said, “a lot will depend on where the vaccine is and what we encounter with whether there’s circulating virus or not” in terms of clinical trial design, including whether surrogate efficacy markers such as antibody production would be used.
Unvaccinated members of a population may be used as controls against a vaccinated group during an active outbreak, he said, a break from traditional trial design. “It’s not perfect. I’ll acknowledge right away there are certain people at the [National Institutes of Health] that would like to tell me that’s a horrible idea, but I think we are going to entertain and discuss all potential designs” for COVID-19 vaccine trials, he said. “We can’t out-of-hand dismiss any design here, whether real world based or evidence based.”
“This may be a little unusual hearing this from the FDA,” he said, “but this is possibly one of the most important things we are going to have to do in the next few years.” He added, “It’s unfortunately not unlikely that we will see a second wave, or maybe even a third wave, if we don’t get it right.”
He pointed out that there was no candidate vaccine in the pipeline when the pandemic blossomed and began its race around the globe. Current coronavirus candidates aren’t useful against COVID-19. “We know that there might be some complexities in development” related to the contributions of immune enhancement to the pathogenicity of the SARS-CoV-2 virus, he said.
The agency is currently working closely with sponsors of various candidate vaccines to take a hard look at preclinical data and trial design.
“Low efficacy could distract from capacity for more robust candidates to come forward,” he said. “We’d like to encourage people to have the absolute best vaccines. ... We hope to be able to facilitate rapid development of these,” he said.
Moving forward, a whole-government approach is necessary for development and delivery of the best vaccine. Ms. Krofah elaborated that the FDA and the Centers for Medicare & Medicaid will need to collaborate closely as studies evolve. In particular, CMS needs to be ready with reimbursement codes, recognizing that both public and private payers will likely be providing reimbursement for COVID-19 vaccinations.
“When these vaccines get approved, we are going to have to decide who is going to pay for them,” said Dr. Tan, who previously served as the director of medicine and public health at the American Medical Association. He noted that CPT coding comes through the AMA.
Dr. Marks stressed that ultimately, although treatments or prophylactic regimes against COVID-19 may be developed, “a vaccine is the most efficient way to protect large numbers of people.” Though there’s going to have to be a balancing act so speed doesn’t come at the expense of vaccine safety and efficacy. “We are very much hoping that we can find vaccines that have relatively high levels of efficacy,” he said, adding a hopeful point: “Right now there have not been mutations that have occurred … that would alter vaccine development programs in terms of the targets they’re going after.”
Dr. Marks offered a wildly optimistic – and then a more realistic – judgment as to when a successful vaccine might emerge from the development, trial, and approval process. After acknowledging that the FDA might consider an Emergency Use Authorization (EUA) if coronavirus activity is high when a candidate vaccine emerges, he said that “if everything goes perfectly,” an EUA for a vaccine might be issued within 9-12 months.
“The most likely timeline – and this is total speculation – is that it could be 12-18 months,” he said.
Ms. Krofah concurred, adding, “We’re seeing the big companies put a big bet on that timeline as well.” She cited Johnson & Johnson, which has committed to a $1 billion COVID-19 vaccine development program by the end of 2021.
Finally, when a vaccine does become available, who is first in line to receive it? Ms. Krofah said that it will be important for the public to know that there will be a tiering scheme for vaccine administration in the early days. Healthcare workers, emergency responders, and the particularly vulnerable may be among the first to receive protection, she said.
Extraordinary cooperation and accommodations are needed in the race to build a COVID-19 vaccine from scratch while chasing a pandemic, said members of industry and government who convened for an update on the vaccine clinical trial process.
The message came from representatives from the Food and Drug Administration, a think tank, and the nonprofit sector who provided some insight into the vaccine development process for COVID-19 at a press briefing hosted by the Commonwealth Fund.
Even in the best of times, vaccine development is not simple, said Litjen (L.J.) Tan, PhD, chief strategy officer for the Immunization Action Coalition. Ordinarily, the process can take from 10 to 20 years and cost well over a billion dollars. Many vaccines wind up being abandoned before phase 3 development just because the cost is prohibitive, he said.
Vaccines undergo extensive ongoing postmarketing surveillance even after approval, licensing, and distribution, noted Dr. Tan, adding that the development of a safe, effective vaccine is a “very complicated, significant process.”
In these extraordinary times, many adjustments to the usual trial trajectory are needed, agreed all participants. To speed the process, the traditional vaccine trajectory is being accelerated and compressed; changes may include simultaneous rather than sequential clinical trials that are run in parallel. These trials may be optimized for multiple target populations at the same time, and run in different countries, explained Dr. Tan.
“We are likely going to use something called adaptive trial designs” in which results are gathered during the trial and used to modify the trial according to prespecified rules, he said. “These trials shift to accommodate data as it comes up.”
Regulatory agencies are actively engaging in the process much earlier than usual, with input including how to incentivize scaling up production of vaccines and ensuring that vaccines will be fairly and equitably distributed across the globe, he added.
Esther Krofah is the executive director of FasterCures, a center within the nonprofit Milken Institute. Currently 86 different active COVID-19 vaccine projects are underway, she said, with 6 currently in clinical trials and about two dozen more expected to enter the clinical trial phase by the summer of 2020.
Many of these projects will involve a smaller biotech company or an academic research group with deep knowledge of a particular immune strategy partnering with a large pharmaceutical company that has economic capacity and global resources and reach, said Ms. Krofah.
From a policy perspective, she said, it’s important for the FDA to have surge capacity with “enough arms, legs, and staff to actively provide input into clinical design and protocols of studies.” The goal is to be able to review data in real-time and provide rapid feedback as studies are occurring so adaptive clinical trial design can be implemented.
As COVID-19 vaccine trials are rolled out, necessary compromises may include incorporation of real world evidence in later clinical trial stages. “There is a way to do randomized trials in the real world in situations that come up like this,” said Peter Marks, MD, the FDA’s director of the Center for Biologics Evaluation and Research. Long-term data about vaccine efficacy may be accrued over time, once a vaccine is being administered beyond the clinical trial stage, to see if efficacy wanes over time.
However, he said, “a lot will depend on where the vaccine is and what we encounter with whether there’s circulating virus or not” in terms of clinical trial design, including whether surrogate efficacy markers such as antibody production would be used.
Unvaccinated members of a population may be used as controls against a vaccinated group during an active outbreak, he said, a break from traditional trial design. “It’s not perfect. I’ll acknowledge right away there are certain people at the [National Institutes of Health] that would like to tell me that’s a horrible idea, but I think we are going to entertain and discuss all potential designs” for COVID-19 vaccine trials, he said. “We can’t out-of-hand dismiss any design here, whether real world based or evidence based.”
“This may be a little unusual hearing this from the FDA,” he said, “but this is possibly one of the most important things we are going to have to do in the next few years.” He added, “It’s unfortunately not unlikely that we will see a second wave, or maybe even a third wave, if we don’t get it right.”
He pointed out that there was no candidate vaccine in the pipeline when the pandemic blossomed and began its race around the globe. Current coronavirus candidates aren’t useful against COVID-19. “We know that there might be some complexities in development” related to the contributions of immune enhancement to the pathogenicity of the SARS-CoV-2 virus, he said.
The agency is currently working closely with sponsors of various candidate vaccines to take a hard look at preclinical data and trial design.
“Low efficacy could distract from capacity for more robust candidates to come forward,” he said. “We’d like to encourage people to have the absolute best vaccines. ... We hope to be able to facilitate rapid development of these,” he said.
Moving forward, a whole-government approach is necessary for development and delivery of the best vaccine. Ms. Krofah elaborated that the FDA and the Centers for Medicare & Medicaid will need to collaborate closely as studies evolve. In particular, CMS needs to be ready with reimbursement codes, recognizing that both public and private payers will likely be providing reimbursement for COVID-19 vaccinations.
“When these vaccines get approved, we are going to have to decide who is going to pay for them,” said Dr. Tan, who previously served as the director of medicine and public health at the American Medical Association. He noted that CPT coding comes through the AMA.
Dr. Marks stressed that ultimately, although treatments or prophylactic regimes against COVID-19 may be developed, “a vaccine is the most efficient way to protect large numbers of people.” Though there’s going to have to be a balancing act so speed doesn’t come at the expense of vaccine safety and efficacy. “We are very much hoping that we can find vaccines that have relatively high levels of efficacy,” he said, adding a hopeful point: “Right now there have not been mutations that have occurred … that would alter vaccine development programs in terms of the targets they’re going after.”
Dr. Marks offered a wildly optimistic – and then a more realistic – judgment as to when a successful vaccine might emerge from the development, trial, and approval process. After acknowledging that the FDA might consider an Emergency Use Authorization (EUA) if coronavirus activity is high when a candidate vaccine emerges, he said that “if everything goes perfectly,” an EUA for a vaccine might be issued within 9-12 months.
“The most likely timeline – and this is total speculation – is that it could be 12-18 months,” he said.
Ms. Krofah concurred, adding, “We’re seeing the big companies put a big bet on that timeline as well.” She cited Johnson & Johnson, which has committed to a $1 billion COVID-19 vaccine development program by the end of 2021.
Finally, when a vaccine does become available, who is first in line to receive it? Ms. Krofah said that it will be important for the public to know that there will be a tiering scheme for vaccine administration in the early days. Healthcare workers, emergency responders, and the particularly vulnerable may be among the first to receive protection, she said.
Extraordinary cooperation and accommodations are needed in the race to build a COVID-19 vaccine from scratch while chasing a pandemic, said members of industry and government who convened for an update on the vaccine clinical trial process.
The message came from representatives from the Food and Drug Administration, a think tank, and the nonprofit sector who provided some insight into the vaccine development process for COVID-19 at a press briefing hosted by the Commonwealth Fund.
Even in the best of times, vaccine development is not simple, said Litjen (L.J.) Tan, PhD, chief strategy officer for the Immunization Action Coalition. Ordinarily, the process can take from 10 to 20 years and cost well over a billion dollars. Many vaccines wind up being abandoned before phase 3 development just because the cost is prohibitive, he said.
Vaccines undergo extensive ongoing postmarketing surveillance even after approval, licensing, and distribution, noted Dr. Tan, adding that the development of a safe, effective vaccine is a “very complicated, significant process.”
In these extraordinary times, many adjustments to the usual trial trajectory are needed, agreed all participants. To speed the process, the traditional vaccine trajectory is being accelerated and compressed; changes may include simultaneous rather than sequential clinical trials that are run in parallel. These trials may be optimized for multiple target populations at the same time, and run in different countries, explained Dr. Tan.
“We are likely going to use something called adaptive trial designs” in which results are gathered during the trial and used to modify the trial according to prespecified rules, he said. “These trials shift to accommodate data as it comes up.”
Regulatory agencies are actively engaging in the process much earlier than usual, with input including how to incentivize scaling up production of vaccines and ensuring that vaccines will be fairly and equitably distributed across the globe, he added.
Esther Krofah is the executive director of FasterCures, a center within the nonprofit Milken Institute. Currently 86 different active COVID-19 vaccine projects are underway, she said, with 6 currently in clinical trials and about two dozen more expected to enter the clinical trial phase by the summer of 2020.
Many of these projects will involve a smaller biotech company or an academic research group with deep knowledge of a particular immune strategy partnering with a large pharmaceutical company that has economic capacity and global resources and reach, said Ms. Krofah.
From a policy perspective, she said, it’s important for the FDA to have surge capacity with “enough arms, legs, and staff to actively provide input into clinical design and protocols of studies.” The goal is to be able to review data in real-time and provide rapid feedback as studies are occurring so adaptive clinical trial design can be implemented.
As COVID-19 vaccine trials are rolled out, necessary compromises may include incorporation of real world evidence in later clinical trial stages. “There is a way to do randomized trials in the real world in situations that come up like this,” said Peter Marks, MD, the FDA’s director of the Center for Biologics Evaluation and Research. Long-term data about vaccine efficacy may be accrued over time, once a vaccine is being administered beyond the clinical trial stage, to see if efficacy wanes over time.
However, he said, “a lot will depend on where the vaccine is and what we encounter with whether there’s circulating virus or not” in terms of clinical trial design, including whether surrogate efficacy markers such as antibody production would be used.
Unvaccinated members of a population may be used as controls against a vaccinated group during an active outbreak, he said, a break from traditional trial design. “It’s not perfect. I’ll acknowledge right away there are certain people at the [National Institutes of Health] that would like to tell me that’s a horrible idea, but I think we are going to entertain and discuss all potential designs” for COVID-19 vaccine trials, he said. “We can’t out-of-hand dismiss any design here, whether real world based or evidence based.”
“This may be a little unusual hearing this from the FDA,” he said, “but this is possibly one of the most important things we are going to have to do in the next few years.” He added, “It’s unfortunately not unlikely that we will see a second wave, or maybe even a third wave, if we don’t get it right.”
He pointed out that there was no candidate vaccine in the pipeline when the pandemic blossomed and began its race around the globe. Current coronavirus candidates aren’t useful against COVID-19. “We know that there might be some complexities in development” related to the contributions of immune enhancement to the pathogenicity of the SARS-CoV-2 virus, he said.
The agency is currently working closely with sponsors of various candidate vaccines to take a hard look at preclinical data and trial design.
“Low efficacy could distract from capacity for more robust candidates to come forward,” he said. “We’d like to encourage people to have the absolute best vaccines. ... We hope to be able to facilitate rapid development of these,” he said.
Moving forward, a whole-government approach is necessary for development and delivery of the best vaccine. Ms. Krofah elaborated that the FDA and the Centers for Medicare & Medicaid will need to collaborate closely as studies evolve. In particular, CMS needs to be ready with reimbursement codes, recognizing that both public and private payers will likely be providing reimbursement for COVID-19 vaccinations.
“When these vaccines get approved, we are going to have to decide who is going to pay for them,” said Dr. Tan, who previously served as the director of medicine and public health at the American Medical Association. He noted that CPT coding comes through the AMA.
Dr. Marks stressed that ultimately, although treatments or prophylactic regimes against COVID-19 may be developed, “a vaccine is the most efficient way to protect large numbers of people.” Though there’s going to have to be a balancing act so speed doesn’t come at the expense of vaccine safety and efficacy. “We are very much hoping that we can find vaccines that have relatively high levels of efficacy,” he said, adding a hopeful point: “Right now there have not been mutations that have occurred … that would alter vaccine development programs in terms of the targets they’re going after.”
Dr. Marks offered a wildly optimistic – and then a more realistic – judgment as to when a successful vaccine might emerge from the development, trial, and approval process. After acknowledging that the FDA might consider an Emergency Use Authorization (EUA) if coronavirus activity is high when a candidate vaccine emerges, he said that “if everything goes perfectly,” an EUA for a vaccine might be issued within 9-12 months.
“The most likely timeline – and this is total speculation – is that it could be 12-18 months,” he said.
Ms. Krofah concurred, adding, “We’re seeing the big companies put a big bet on that timeline as well.” She cited Johnson & Johnson, which has committed to a $1 billion COVID-19 vaccine development program by the end of 2021.
Finally, when a vaccine does become available, who is first in line to receive it? Ms. Krofah said that it will be important for the public to know that there will be a tiering scheme for vaccine administration in the early days. Healthcare workers, emergency responders, and the particularly vulnerable may be among the first to receive protection, she said.
Researchers investigate impact of smoking on COVID-19 risk
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
Switching gears at high speed
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
Michigan hospitalists prepare for COVID-19 care
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
In praise of parents and children
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
The COVID-19 pandemic has changed the lives of children, teenagers, and parents worldwide. While some families are experiencing the unburdening of overly packed schedules and may be having a romantic or nostalgic “Little House on the Prairie” experience, for most it is at a minimum uncomfortable and inconvenient. For others it’s unbearable as they experience loss and feel relationship strain intensified by social distancing, seclusion, or quarantine. Some children have found respite from bullying at school, while other children have lost their only respite from being mistreated at home. Now may be as critical a time as ever for health care providers to listen carefully, empathize, validate, and proactively reach out to provide encouraging guidance and counsel, as well as express concern for families and children.
Many parents across the country are taking on an enormous, unanticipated task. Many parents have lost employment and income, while many mandatory professionals now struggle to keep up with increased work hours and work stress. Parents are trying to become multitaskers who assume the role of the music teacher, the soccer coach, the drama instructor, the friend, and of course their original role as a parent.
This seems an appropriate time to consider the work of Donald W. Winnicott, FRCP, the English pediatrician known for the concept of the “good enough parent.”1 This notion of parental competence was in part born out of a desire to defend parents against possible erosion of their confidence in following loving instincts by encroachment from professional expertise. The concept of the “good enough” parent is also related to the idea that young children who believe their parent is perfect will eventually know better. Now is a fitting time for pediatricians to buoy up imperfect but striving parents who are plenty “good enough” as they follow loving instincts to support their children during unforeseen changes associated with the pandemic.
Social distancing has led to family condensing. Many parents and children remain within the same four walls all day, every day. For many parents, the outlet of water cooler banter or yoga classes is gone. Even the commute home, with all its frustration, may have allowed decompression in the form of an audiobook, favorite music, or verbal transference of frustration onto the stranger who just cut you off. That commute might be gone too. Now, for many the good, bad, and the ugly is all happening at home. The 3-year-old may still adorably see a parent who can do no wrong, but in the end, the truth will prevail. A timely word of encouragement to parents: It’s okay to not be omnipotent. In fact, it will help children have a richer view of the world and more realistic expectations of themselves.
For children, they’ll need praise too, and the upheaval caused by the pandemic may be a fitting opportunity to make that praise more meaningful. But sports are off, the school musical is canceled, and the spelling bee is gone. The dojo is closed, the art fair is postponed, and the dance recital isn’t happening. Report cards in many schools may now transition from letter grades to pass/fail. Parents may be asking, “How on earth are we going to celebrate and praise the children?”
Research has shown us that praising the process is more valuable than praising the person.2 If Lucy participates in a soccer game and Javier gets his math results back, there are many possible approaches to praise. “You scored a goal!” or “You got an A on your math test!” is outcome- or product-focused praise. “You’re a good soccer player” or “You’re smart at math!” is person-focused praise. Instead, the most effective praise is process-focused praise: “You worked hard and ran hard even when it looked tiring” or “I noticed that you kept trying different strategies on those math problems until you figured them out.”
This may be a time when children face less comparison, less ranking, and receive less direct reward. With help, they can focus more on the process of learning and less on the outcomes of learning. They may more readily enjoy the efforts in their hobbies, not just the outcomes of their hobbies. When children receive praise for their work, effort, and actions rather than outcomes, externally validating things may be pleasantly replaced by internally validating traits. With process praise, children are more likely to feel self-confident, to set higher learning goals, and to accurately believe that intelligence is related to effort rather than a fixed trait that has been divided up among haves and have nots.3
Families currently face immense change, uncertainty, and discouragement largely unprecedented in their lifetimes. As care providers, we can look to lasting principles as we encourage parents in their provision of love. We can effectively provide praise and celebrate effort using evidence-based strategies uniquely fitted to our current circumstances. As we do this, we can provide healing of some of the less visible ailments associated with the COVID-19 pandemic.
Dr. Jackson is in the department of psychiatry at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email Dr. Jackson at [email protected].
References
1. “The Child, the Family, and the Outside World.” London: Penguin; 1973. p. 173.
2. Dev Psychol. 1999;35(3):835-47.
3. J Exp Child Psychol. 2018;173:116-35.
2019-2020 flu season ends with ‘very high’ activity in New Jersey
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
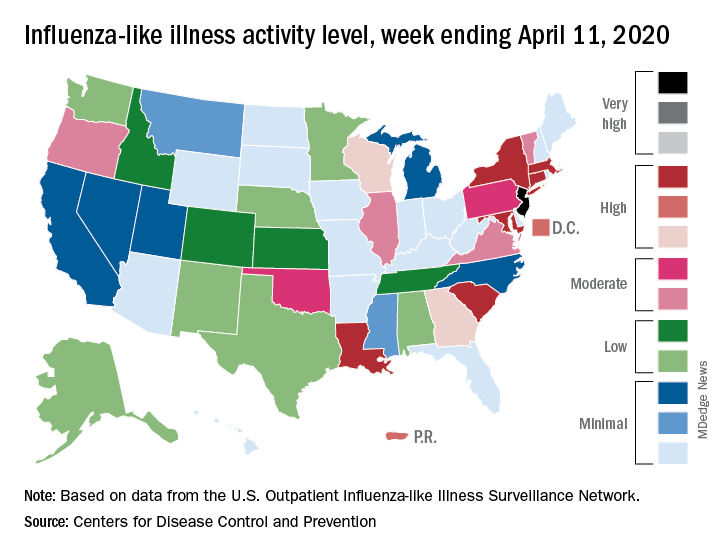
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
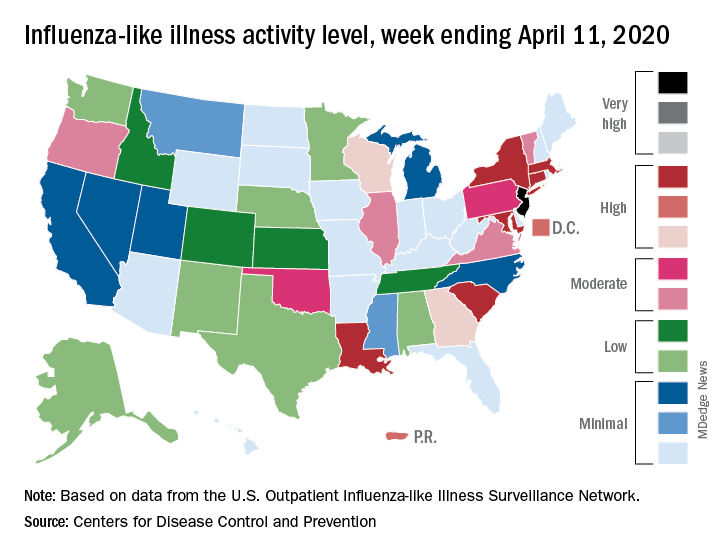
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
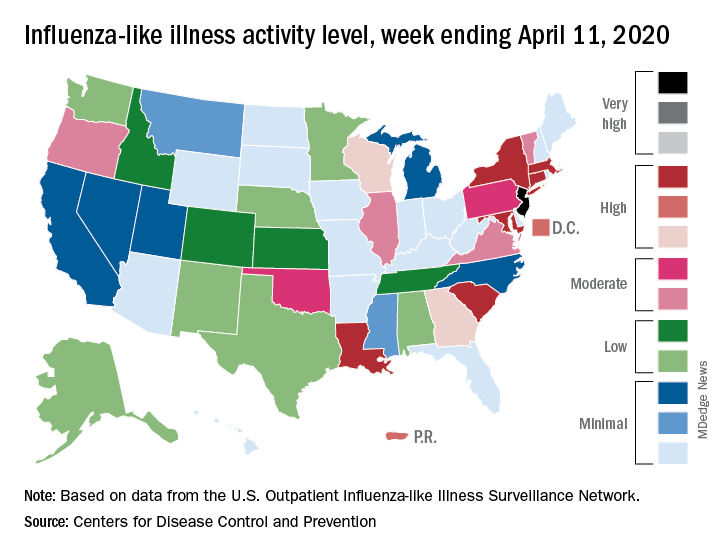
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.














