User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Innovations to expect at HM20
Course director Dr. Benji Mathews offers highlights
Benji K. Mathews, MD, SFHM, CLHM, chief of hospital medicine at Regions Hospital, HealthPartners, in St. Paul, Minn., and director of point of care ultrasound (POCUS) for hospital medicine at HealthPartners, is the course director for the Society of Hospital Medicine’s 2020 Annual Conference (HM20), which will be held April 16-18 in San Diego.
Dr. Mathews, also an associate professor of medicine at the University of Minnesota, Minneapolis, sat down with the Hospitalist to discuss the role of the course director in formulating the HM20 agenda, as well as highlighting some exciting educational sessions, workshops, and other events during the annual conference.
In your role as course director for HM20, did you have a particular theme you wanted to emphasize?
We did not go with a single theme, because we’re trying to provide a comprehensive educational and networking opportunity, so trying to focus the conference on a single theme a year in advance did not seem very prudent. There are multiple themes, from health disparities to technology to education. For a field like hospital medicine that’s rapidly evolving, we thought it best to keep it open and instead further develop the conference tracks: What new tracks can be created, what older tracks can be maintained because they have been highly successful, and which tracks do we retire?
Can you discuss some of the tracks at HM20?
The new track we have this year is the Technology track. That track will examine current and future technology that will impact care delivery, including telehealth, wearables, apps for digital learning, and for clinicians at the bedside. Innovation is at the core of hospital medicine, and we’re constantly exploring how to deliver efficient, timely, and effective care. “Future-casting” is important, and this track speaks to that.
There are some old standards that I would also recommend. The “Great Debate” is one of the hardest to finalize, because while you can create a great session topic and title, we need to find two talented speakers for a debate, as that is very different than a presentation. The speakers take opposing sides on clinical decisions, the latest literature reviews, best practices, and the audience gets to vote. Topics we’re using this year include “Procalcitonin: Friend or Foe,” “Guidelines Controversies in Inpatient Care,” and “POCUS vs. Physical Exam – Tech vs. Tradition.” Some of the debaters include Carrie Herzke, MD, of Johns Hopkins University, Baltimore; Daniel Dressler, MD, of Emory University, Atlanta; Jordan Messler, MD, of Morton Plant Hospital in Clearwater, Fla.; and Michelle Guidry, MD, of the Southeast Louisiana Veterans Health Care System and Tulane University, both in New Orleans; Ria Dancel, MD, from the University of North Carolina, and Michael Janjigian, MD, from NYU Langone Health.
One of the highlights this year is that we’re trying to bring more gender equity into our speaker lineup. Rarely will we have only two male speakers at a session, and I don’t think we have any all-male panels, jokingly called “manels” in the past.
Are there some “tried-and-true” tracks or sessions that are returning in HM20?
I’d like to highlight the Clinical Mastery track. That was a new track last year, and has returned this year. That track is focused on helping hospitalists become expert diagnosticians at the bedside. “Pitfalls, Myths and Pearls in Diagnostic Reasoning” is one session to note in that track, with Dr. Gopi Astik, Dr. Andrew Olson, and Dr. Reza Manesh. Another special focus this year within Clinical Mastery will be on using the rational clinical exam to augment your diagnostic skills.
When programming the annual conference, how do you balance the needs of community hospitalists with academic hospitalists?
The value we have on the annual conference committee is that there are a fair number of community hospitalists, advance practice clinicians, representation from med-peds, and family practice, for instance. Generally, there is a wide sampling of the decision makers from across the specialty helping to program the conference – we have great academic institutions, but we have representation from the larger impressive community as well. That said, it is hard to curate content that is solely for a specific subset of hospitalists without marginalizing other subsets. We don’t want to isolate people. A lot of our Rapid Fire topics are geared toward frontline hospitalists. This is content that will directly impact hospitalists as they care for patients. And some of the content that we’re bringing in this year with more emphasis are in health equity and disparities. Academic groups study this, however frontline clinicians from both academic and community settings deal with this every day, relating to both patients and staff. For example, in regard to patients, we have content focused on caring for the LGBTQ community, sessions on refugee health, as well as hospitalists and global health. We have an emphasis on diversity and inclusion in the workplace, with speakers from both community and academic settings. There will be good sessions with gender equity themes, practical tips in promotion and hiring practices. There are a couple workshops on gender equity; one to note is “Top 10 Ways for Men + Women to Engage in Gender Equity.”
Can you speak to the content that is targeted at nurse practitioners and physician assistants?
This is near and dear to my heart as I’m from an institution that has a positive history of strong partnerships with our advance practice clinician colleagues. Our goal this year was to continue to highlight nurse practitioners and physician assistants in a track dedicated to them. We have a core session called “Training Day: How to Onboard and Operationalize an Advanced Practice Provider Workforce” – this is a “bread-and-butter” session presented by speakers who have built programs from the ground up. Other important sessions address how to advance the careers of NPs and PAs – “Professional Development for NP/PAs” – and on mentorship, which emphasizes a culture of partnership on projects like providing high quality, safe care.
Are there any workshops that attendees should take note of?
One I would like to highlight is “Survive! The POCUS Apocalypse Adventure.” This highly anticipated offering is preregistration required, hosted for the first time on day 1 of the main conference. The workshop will introduce the gamification of POCUS to hospitalists. Each participant will be expected to perform ultrasound examinations and interpret their findings in order to gather clues that will lead to the cure for a zombie apocalypse! There are a lot of innovations this year in programming the Annual Conference, and gamification might be considered risky but I think it has a very good chance of success with entertainment and learning combined into one amazing workshop.
What are some other innovations that the annual conference committee has planned for 2020?
Another exciting innovation is what we call “Breakfast with an Expert.” This is a new rapid-fire didactic session format where we have three experts speak on different hot topics, such as “Nutritional Counseling” (led by Kate Shafto, MD), “Things I Wish I Knew Earlier in my Career” (Brad Sharpe, MD), and “Case-Based Controversies in Ethics” (Hannah Lipman, MD). These take place on the very first day of the conference, before the opening general session. Attendees can grab their breakfast and listen to any of these sessions before they head into the plenary. Hospitalists have asked for more content, so we’re adding these as a response to that hunger for more educational content. This format is supposed to be a bit cozier, with more Q&A.
Another aspect of HM20 to highlight is the Simulation Center. The Sim Center is a space that hosts a variety of hospital medicine skill development areas. This is an interactive center where attendees can learn to perform bedside procedures and learn hands-on skills with diagnostic point-of-care ultrasound during the first 2 days of the conference. The Sim Center is slightly different than the precourses, in that we are offering 1-hour blocks of small-group instruction for which attendees preregister. This aligns with larger SHM efforts to encourage hospitalists to be more confident with bedside procedures, and engage with SHM’s ultrasound offerings, including the certificate of completion program.
To register for the 2020 Annual Conference, including precourses, visit https://shmannualconference.org/register/.
Course director Dr. Benji Mathews offers highlights
Course director Dr. Benji Mathews offers highlights
Benji K. Mathews, MD, SFHM, CLHM, chief of hospital medicine at Regions Hospital, HealthPartners, in St. Paul, Minn., and director of point of care ultrasound (POCUS) for hospital medicine at HealthPartners, is the course director for the Society of Hospital Medicine’s 2020 Annual Conference (HM20), which will be held April 16-18 in San Diego.
Dr. Mathews, also an associate professor of medicine at the University of Minnesota, Minneapolis, sat down with the Hospitalist to discuss the role of the course director in formulating the HM20 agenda, as well as highlighting some exciting educational sessions, workshops, and other events during the annual conference.
In your role as course director for HM20, did you have a particular theme you wanted to emphasize?
We did not go with a single theme, because we’re trying to provide a comprehensive educational and networking opportunity, so trying to focus the conference on a single theme a year in advance did not seem very prudent. There are multiple themes, from health disparities to technology to education. For a field like hospital medicine that’s rapidly evolving, we thought it best to keep it open and instead further develop the conference tracks: What new tracks can be created, what older tracks can be maintained because they have been highly successful, and which tracks do we retire?
Can you discuss some of the tracks at HM20?
The new track we have this year is the Technology track. That track will examine current and future technology that will impact care delivery, including telehealth, wearables, apps for digital learning, and for clinicians at the bedside. Innovation is at the core of hospital medicine, and we’re constantly exploring how to deliver efficient, timely, and effective care. “Future-casting” is important, and this track speaks to that.
There are some old standards that I would also recommend. The “Great Debate” is one of the hardest to finalize, because while you can create a great session topic and title, we need to find two talented speakers for a debate, as that is very different than a presentation. The speakers take opposing sides on clinical decisions, the latest literature reviews, best practices, and the audience gets to vote. Topics we’re using this year include “Procalcitonin: Friend or Foe,” “Guidelines Controversies in Inpatient Care,” and “POCUS vs. Physical Exam – Tech vs. Tradition.” Some of the debaters include Carrie Herzke, MD, of Johns Hopkins University, Baltimore; Daniel Dressler, MD, of Emory University, Atlanta; Jordan Messler, MD, of Morton Plant Hospital in Clearwater, Fla.; and Michelle Guidry, MD, of the Southeast Louisiana Veterans Health Care System and Tulane University, both in New Orleans; Ria Dancel, MD, from the University of North Carolina, and Michael Janjigian, MD, from NYU Langone Health.
One of the highlights this year is that we’re trying to bring more gender equity into our speaker lineup. Rarely will we have only two male speakers at a session, and I don’t think we have any all-male panels, jokingly called “manels” in the past.
Are there some “tried-and-true” tracks or sessions that are returning in HM20?
I’d like to highlight the Clinical Mastery track. That was a new track last year, and has returned this year. That track is focused on helping hospitalists become expert diagnosticians at the bedside. “Pitfalls, Myths and Pearls in Diagnostic Reasoning” is one session to note in that track, with Dr. Gopi Astik, Dr. Andrew Olson, and Dr. Reza Manesh. Another special focus this year within Clinical Mastery will be on using the rational clinical exam to augment your diagnostic skills.
When programming the annual conference, how do you balance the needs of community hospitalists with academic hospitalists?
The value we have on the annual conference committee is that there are a fair number of community hospitalists, advance practice clinicians, representation from med-peds, and family practice, for instance. Generally, there is a wide sampling of the decision makers from across the specialty helping to program the conference – we have great academic institutions, but we have representation from the larger impressive community as well. That said, it is hard to curate content that is solely for a specific subset of hospitalists without marginalizing other subsets. We don’t want to isolate people. A lot of our Rapid Fire topics are geared toward frontline hospitalists. This is content that will directly impact hospitalists as they care for patients. And some of the content that we’re bringing in this year with more emphasis are in health equity and disparities. Academic groups study this, however frontline clinicians from both academic and community settings deal with this every day, relating to both patients and staff. For example, in regard to patients, we have content focused on caring for the LGBTQ community, sessions on refugee health, as well as hospitalists and global health. We have an emphasis on diversity and inclusion in the workplace, with speakers from both community and academic settings. There will be good sessions with gender equity themes, practical tips in promotion and hiring practices. There are a couple workshops on gender equity; one to note is “Top 10 Ways for Men + Women to Engage in Gender Equity.”
Can you speak to the content that is targeted at nurse practitioners and physician assistants?
This is near and dear to my heart as I’m from an institution that has a positive history of strong partnerships with our advance practice clinician colleagues. Our goal this year was to continue to highlight nurse practitioners and physician assistants in a track dedicated to them. We have a core session called “Training Day: How to Onboard and Operationalize an Advanced Practice Provider Workforce” – this is a “bread-and-butter” session presented by speakers who have built programs from the ground up. Other important sessions address how to advance the careers of NPs and PAs – “Professional Development for NP/PAs” – and on mentorship, which emphasizes a culture of partnership on projects like providing high quality, safe care.
Are there any workshops that attendees should take note of?
One I would like to highlight is “Survive! The POCUS Apocalypse Adventure.” This highly anticipated offering is preregistration required, hosted for the first time on day 1 of the main conference. The workshop will introduce the gamification of POCUS to hospitalists. Each participant will be expected to perform ultrasound examinations and interpret their findings in order to gather clues that will lead to the cure for a zombie apocalypse! There are a lot of innovations this year in programming the Annual Conference, and gamification might be considered risky but I think it has a very good chance of success with entertainment and learning combined into one amazing workshop.
What are some other innovations that the annual conference committee has planned for 2020?
Another exciting innovation is what we call “Breakfast with an Expert.” This is a new rapid-fire didactic session format where we have three experts speak on different hot topics, such as “Nutritional Counseling” (led by Kate Shafto, MD), “Things I Wish I Knew Earlier in my Career” (Brad Sharpe, MD), and “Case-Based Controversies in Ethics” (Hannah Lipman, MD). These take place on the very first day of the conference, before the opening general session. Attendees can grab their breakfast and listen to any of these sessions before they head into the plenary. Hospitalists have asked for more content, so we’re adding these as a response to that hunger for more educational content. This format is supposed to be a bit cozier, with more Q&A.
Another aspect of HM20 to highlight is the Simulation Center. The Sim Center is a space that hosts a variety of hospital medicine skill development areas. This is an interactive center where attendees can learn to perform bedside procedures and learn hands-on skills with diagnostic point-of-care ultrasound during the first 2 days of the conference. The Sim Center is slightly different than the precourses, in that we are offering 1-hour blocks of small-group instruction for which attendees preregister. This aligns with larger SHM efforts to encourage hospitalists to be more confident with bedside procedures, and engage with SHM’s ultrasound offerings, including the certificate of completion program.
To register for the 2020 Annual Conference, including precourses, visit https://shmannualconference.org/register/.
Benji K. Mathews, MD, SFHM, CLHM, chief of hospital medicine at Regions Hospital, HealthPartners, in St. Paul, Minn., and director of point of care ultrasound (POCUS) for hospital medicine at HealthPartners, is the course director for the Society of Hospital Medicine’s 2020 Annual Conference (HM20), which will be held April 16-18 in San Diego.
Dr. Mathews, also an associate professor of medicine at the University of Minnesota, Minneapolis, sat down with the Hospitalist to discuss the role of the course director in formulating the HM20 agenda, as well as highlighting some exciting educational sessions, workshops, and other events during the annual conference.
In your role as course director for HM20, did you have a particular theme you wanted to emphasize?
We did not go with a single theme, because we’re trying to provide a comprehensive educational and networking opportunity, so trying to focus the conference on a single theme a year in advance did not seem very prudent. There are multiple themes, from health disparities to technology to education. For a field like hospital medicine that’s rapidly evolving, we thought it best to keep it open and instead further develop the conference tracks: What new tracks can be created, what older tracks can be maintained because they have been highly successful, and which tracks do we retire?
Can you discuss some of the tracks at HM20?
The new track we have this year is the Technology track. That track will examine current and future technology that will impact care delivery, including telehealth, wearables, apps for digital learning, and for clinicians at the bedside. Innovation is at the core of hospital medicine, and we’re constantly exploring how to deliver efficient, timely, and effective care. “Future-casting” is important, and this track speaks to that.
There are some old standards that I would also recommend. The “Great Debate” is one of the hardest to finalize, because while you can create a great session topic and title, we need to find two talented speakers for a debate, as that is very different than a presentation. The speakers take opposing sides on clinical decisions, the latest literature reviews, best practices, and the audience gets to vote. Topics we’re using this year include “Procalcitonin: Friend or Foe,” “Guidelines Controversies in Inpatient Care,” and “POCUS vs. Physical Exam – Tech vs. Tradition.” Some of the debaters include Carrie Herzke, MD, of Johns Hopkins University, Baltimore; Daniel Dressler, MD, of Emory University, Atlanta; Jordan Messler, MD, of Morton Plant Hospital in Clearwater, Fla.; and Michelle Guidry, MD, of the Southeast Louisiana Veterans Health Care System and Tulane University, both in New Orleans; Ria Dancel, MD, from the University of North Carolina, and Michael Janjigian, MD, from NYU Langone Health.
One of the highlights this year is that we’re trying to bring more gender equity into our speaker lineup. Rarely will we have only two male speakers at a session, and I don’t think we have any all-male panels, jokingly called “manels” in the past.
Are there some “tried-and-true” tracks or sessions that are returning in HM20?
I’d like to highlight the Clinical Mastery track. That was a new track last year, and has returned this year. That track is focused on helping hospitalists become expert diagnosticians at the bedside. “Pitfalls, Myths and Pearls in Diagnostic Reasoning” is one session to note in that track, with Dr. Gopi Astik, Dr. Andrew Olson, and Dr. Reza Manesh. Another special focus this year within Clinical Mastery will be on using the rational clinical exam to augment your diagnostic skills.
When programming the annual conference, how do you balance the needs of community hospitalists with academic hospitalists?
The value we have on the annual conference committee is that there are a fair number of community hospitalists, advance practice clinicians, representation from med-peds, and family practice, for instance. Generally, there is a wide sampling of the decision makers from across the specialty helping to program the conference – we have great academic institutions, but we have representation from the larger impressive community as well. That said, it is hard to curate content that is solely for a specific subset of hospitalists without marginalizing other subsets. We don’t want to isolate people. A lot of our Rapid Fire topics are geared toward frontline hospitalists. This is content that will directly impact hospitalists as they care for patients. And some of the content that we’re bringing in this year with more emphasis are in health equity and disparities. Academic groups study this, however frontline clinicians from both academic and community settings deal with this every day, relating to both patients and staff. For example, in regard to patients, we have content focused on caring for the LGBTQ community, sessions on refugee health, as well as hospitalists and global health. We have an emphasis on diversity and inclusion in the workplace, with speakers from both community and academic settings. There will be good sessions with gender equity themes, practical tips in promotion and hiring practices. There are a couple workshops on gender equity; one to note is “Top 10 Ways for Men + Women to Engage in Gender Equity.”
Can you speak to the content that is targeted at nurse practitioners and physician assistants?
This is near and dear to my heart as I’m from an institution that has a positive history of strong partnerships with our advance practice clinician colleagues. Our goal this year was to continue to highlight nurse practitioners and physician assistants in a track dedicated to them. We have a core session called “Training Day: How to Onboard and Operationalize an Advanced Practice Provider Workforce” – this is a “bread-and-butter” session presented by speakers who have built programs from the ground up. Other important sessions address how to advance the careers of NPs and PAs – “Professional Development for NP/PAs” – and on mentorship, which emphasizes a culture of partnership on projects like providing high quality, safe care.
Are there any workshops that attendees should take note of?
One I would like to highlight is “Survive! The POCUS Apocalypse Adventure.” This highly anticipated offering is preregistration required, hosted for the first time on day 1 of the main conference. The workshop will introduce the gamification of POCUS to hospitalists. Each participant will be expected to perform ultrasound examinations and interpret their findings in order to gather clues that will lead to the cure for a zombie apocalypse! There are a lot of innovations this year in programming the Annual Conference, and gamification might be considered risky but I think it has a very good chance of success with entertainment and learning combined into one amazing workshop.
What are some other innovations that the annual conference committee has planned for 2020?
Another exciting innovation is what we call “Breakfast with an Expert.” This is a new rapid-fire didactic session format where we have three experts speak on different hot topics, such as “Nutritional Counseling” (led by Kate Shafto, MD), “Things I Wish I Knew Earlier in my Career” (Brad Sharpe, MD), and “Case-Based Controversies in Ethics” (Hannah Lipman, MD). These take place on the very first day of the conference, before the opening general session. Attendees can grab their breakfast and listen to any of these sessions before they head into the plenary. Hospitalists have asked for more content, so we’re adding these as a response to that hunger for more educational content. This format is supposed to be a bit cozier, with more Q&A.
Another aspect of HM20 to highlight is the Simulation Center. The Sim Center is a space that hosts a variety of hospital medicine skill development areas. This is an interactive center where attendees can learn to perform bedside procedures and learn hands-on skills with diagnostic point-of-care ultrasound during the first 2 days of the conference. The Sim Center is slightly different than the precourses, in that we are offering 1-hour blocks of small-group instruction for which attendees preregister. This aligns with larger SHM efforts to encourage hospitalists to be more confident with bedside procedures, and engage with SHM’s ultrasound offerings, including the certificate of completion program.
To register for the 2020 Annual Conference, including precourses, visit https://shmannualconference.org/register/.
COVID-19: Time to ‘take the risk of scaring people’
It’s past time to call the novel coronavirus, COVID-19, a pandemic and “time to push people to prepare, and guide their prep,” according to risk communication experts.
Medical messaging about containing or stopping the spread of the virus is doing more harm than good, write Peter Sandman, PhD, and Jody Lanard, MD, both based in New York City, in a recent blog post.
“We are near-certain that the desperate-sounding last-ditch containment messaging of recent days is contributing to a massive global misperception,” they warn.
“The most crucial (and overdue) risk communication task … is to help people visualize their communities when ‘keeping it out’ – containment – is no longer relevant.”
That message is embraced by several experts who spoke to Medscape Medical News.
“I’m jealous of what [they] have written: It is so clear, so correct, and so practical,” said David Fisman, MD, MPH, professor of epidemiology at the University of Toronto, Canada. “I think WHO [World Health Organization] is shying away from the P word,” he continued, referring to the organization’s continuing decision not to call the outbreak a pandemic.
“I fully support exactly what [Sandman and Lanard] are saying,” said Michael Osterholm, PhD, MPH, professor of environmental health sciences and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota in Minneapolis.
Sandman and Lanard write. “Hardly any officials are telling civil society and the general public how to get ready for this pandemic.”
Effective communication should inform people of what to expect now, they continue: “[T]he end of most quarantines, travel restrictions, contact tracing, and other measures designed to keep ‘them’ from infecting ‘us,’ and the switch to measures like canceling mass events designed to keep us from infecting each other.”
Among the new messages that should be delivered are things like:
- Stockpiling nonperishable food and prescription meds.
- Considering care of sick family members.
- Cross-training work personnel so one person’s absence won’t derail an organization’s ability to function.
“We hope that governments and healthcare institutions are using this time wisely,” Sandman and Lanard continue. “We know that ordinary citizens are not being asked to do so. In most countries … ordinary citizens have not been asked to prepare. Instead, they have been led to expect that their governments will keep the virus from their doors.”
This article first appeared on Medscape.com.
It’s past time to call the novel coronavirus, COVID-19, a pandemic and “time to push people to prepare, and guide their prep,” according to risk communication experts.
Medical messaging about containing or stopping the spread of the virus is doing more harm than good, write Peter Sandman, PhD, and Jody Lanard, MD, both based in New York City, in a recent blog post.
“We are near-certain that the desperate-sounding last-ditch containment messaging of recent days is contributing to a massive global misperception,” they warn.
“The most crucial (and overdue) risk communication task … is to help people visualize their communities when ‘keeping it out’ – containment – is no longer relevant.”
That message is embraced by several experts who spoke to Medscape Medical News.
“I’m jealous of what [they] have written: It is so clear, so correct, and so practical,” said David Fisman, MD, MPH, professor of epidemiology at the University of Toronto, Canada. “I think WHO [World Health Organization] is shying away from the P word,” he continued, referring to the organization’s continuing decision not to call the outbreak a pandemic.
“I fully support exactly what [Sandman and Lanard] are saying,” said Michael Osterholm, PhD, MPH, professor of environmental health sciences and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota in Minneapolis.
Sandman and Lanard write. “Hardly any officials are telling civil society and the general public how to get ready for this pandemic.”
Effective communication should inform people of what to expect now, they continue: “[T]he end of most quarantines, travel restrictions, contact tracing, and other measures designed to keep ‘them’ from infecting ‘us,’ and the switch to measures like canceling mass events designed to keep us from infecting each other.”
Among the new messages that should be delivered are things like:
- Stockpiling nonperishable food and prescription meds.
- Considering care of sick family members.
- Cross-training work personnel so one person’s absence won’t derail an organization’s ability to function.
“We hope that governments and healthcare institutions are using this time wisely,” Sandman and Lanard continue. “We know that ordinary citizens are not being asked to do so. In most countries … ordinary citizens have not been asked to prepare. Instead, they have been led to expect that their governments will keep the virus from their doors.”
This article first appeared on Medscape.com.
It’s past time to call the novel coronavirus, COVID-19, a pandemic and “time to push people to prepare, and guide their prep,” according to risk communication experts.
Medical messaging about containing or stopping the spread of the virus is doing more harm than good, write Peter Sandman, PhD, and Jody Lanard, MD, both based in New York City, in a recent blog post.
“We are near-certain that the desperate-sounding last-ditch containment messaging of recent days is contributing to a massive global misperception,” they warn.
“The most crucial (and overdue) risk communication task … is to help people visualize their communities when ‘keeping it out’ – containment – is no longer relevant.”
That message is embraced by several experts who spoke to Medscape Medical News.
“I’m jealous of what [they] have written: It is so clear, so correct, and so practical,” said David Fisman, MD, MPH, professor of epidemiology at the University of Toronto, Canada. “I think WHO [World Health Organization] is shying away from the P word,” he continued, referring to the organization’s continuing decision not to call the outbreak a pandemic.
“I fully support exactly what [Sandman and Lanard] are saying,” said Michael Osterholm, PhD, MPH, professor of environmental health sciences and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota in Minneapolis.
Sandman and Lanard write. “Hardly any officials are telling civil society and the general public how to get ready for this pandemic.”
Effective communication should inform people of what to expect now, they continue: “[T]he end of most quarantines, travel restrictions, contact tracing, and other measures designed to keep ‘them’ from infecting ‘us,’ and the switch to measures like canceling mass events designed to keep us from infecting each other.”
Among the new messages that should be delivered are things like:
- Stockpiling nonperishable food and prescription meds.
- Considering care of sick family members.
- Cross-training work personnel so one person’s absence won’t derail an organization’s ability to function.
“We hope that governments and healthcare institutions are using this time wisely,” Sandman and Lanard continue. “We know that ordinary citizens are not being asked to do so. In most countries … ordinary citizens have not been asked to prepare. Instead, they have been led to expect that their governments will keep the virus from their doors.”
This article first appeared on Medscape.com.
CDC expects eventual community spread of coronavirus in U.S.
“We have for many weeks been saying that, while we hope this is not going to be severe, we are planning as if it is,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, said during a Feb. 25, 2020, telebriefing with reporters. “The data over the last week and the spread in other countries has certainly raised our level of concern and raised our level expectation that we are going to have community spread here.”
Dr. Messonnier noted that the coronavirus is now showing signs of community spread without a known source of exposure in a number of countries, including in Hong Kong, Iran, Italy, Japan, Singapore, South Korea, Taiwan, and Thailand. This has now raised the belief that there will be more widespread outbreaks in the United States.
“What we still don’t know is what that will look like,” she said. “As many of you know, we can have community spread in the United States and have it be reasonably mild. We can have community spread in the U.S. and have it be very severe. That is what we don’t completely know yet and we certainly also don’t exactly know when it is going to happen.”
She reiterated the number of actions being taken to slow the potential spread in the United States, including detecting, tracking, and isolating all cases, as well as restricting travel into the United States and issuing travel advisories for countries where coronavirus outbreaks are known.
“We are doing this with the goal of slowing the introduction of this new virus into the U.S. and buying us more time to prepare,” Dr. Messonnier said, noting the containment strategies have been largely successful, though it will be more difficult as more countries experience community spread of the virus.
Dr. Messonnier also reiterated that at this time there are no vaccines and no medicines to treat the coronavirus. She stressed the need to adhere to nonpharmaceutical interventions (NPIs), as they will be “the most important tools in our response to this virus.”
She said the NPIs will vary based on the severity of the outbreak in any given local community and include personal protective measures that individuals can take every day (many of which mirror the recommendations for preventing the spread of the seasonal flu virus), community NPIs that involve social distancing measures designed to keep people away from others, and environmental NPIs such as surface cleaning measures.
CDC’s latest warning comes as parent agency the Department of Health & Human Services is seeking $2.5 billion in funds from Congress to address the coronavirus outbreak.
During a separate press conference on the same day, HHS Secretary Alex Azar noted that there are five major priorities related to those funds, which would be used in the current year, including expansion of surveillance work within the influenza surveillance network; supporting public health preparedness and response for state and local governments; support the development of therapeutics and the development of vaccines; and the purchase of personal protective equipment for national stockpiles.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease at the National Institutes of Health, added during the press conference that vaccine work is in progress and could be ready for phase 1 testing within a month and a half. If all goes well, it would still be at least 12 - 18 months following the completion of a phase 2 trial before it could be produced for mass consumption.
“It is certainly conceivable that this issue with this coronavirus will go well beyond this season into next season,” Dr. Fauci said. “So a vaccine may not solve the problems of the next couple of months, but it certainly would be an important tool that we would have and we will keep you posted on that.”
He also mentioned that NIAID is looking at a number of candidates for therapeutic treatment of coronavirus. He highlighted Gilead’s remdesivir, a nucleotide analog, as one which undergoing two trials – a randomized controlled trial in China and a copy of that trial in Nebraska among patients with the coronavirus who were taken from the Diamond Princess cruise line in Japan.
“I am optimistic that we will at least get an answer if we do have do have a therapy that really is a gamechanger because then we could do something from the standpoint of intervention for those who are sick,” Dr. Fauci said.
UPDATE: This story was updated 2/25 at 4:51 p.m. ET
“We have for many weeks been saying that, while we hope this is not going to be severe, we are planning as if it is,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, said during a Feb. 25, 2020, telebriefing with reporters. “The data over the last week and the spread in other countries has certainly raised our level of concern and raised our level expectation that we are going to have community spread here.”
Dr. Messonnier noted that the coronavirus is now showing signs of community spread without a known source of exposure in a number of countries, including in Hong Kong, Iran, Italy, Japan, Singapore, South Korea, Taiwan, and Thailand. This has now raised the belief that there will be more widespread outbreaks in the United States.
“What we still don’t know is what that will look like,” she said. “As many of you know, we can have community spread in the United States and have it be reasonably mild. We can have community spread in the U.S. and have it be very severe. That is what we don’t completely know yet and we certainly also don’t exactly know when it is going to happen.”
She reiterated the number of actions being taken to slow the potential spread in the United States, including detecting, tracking, and isolating all cases, as well as restricting travel into the United States and issuing travel advisories for countries where coronavirus outbreaks are known.
“We are doing this with the goal of slowing the introduction of this new virus into the U.S. and buying us more time to prepare,” Dr. Messonnier said, noting the containment strategies have been largely successful, though it will be more difficult as more countries experience community spread of the virus.
Dr. Messonnier also reiterated that at this time there are no vaccines and no medicines to treat the coronavirus. She stressed the need to adhere to nonpharmaceutical interventions (NPIs), as they will be “the most important tools in our response to this virus.”
She said the NPIs will vary based on the severity of the outbreak in any given local community and include personal protective measures that individuals can take every day (many of which mirror the recommendations for preventing the spread of the seasonal flu virus), community NPIs that involve social distancing measures designed to keep people away from others, and environmental NPIs such as surface cleaning measures.
CDC’s latest warning comes as parent agency the Department of Health & Human Services is seeking $2.5 billion in funds from Congress to address the coronavirus outbreak.
During a separate press conference on the same day, HHS Secretary Alex Azar noted that there are five major priorities related to those funds, which would be used in the current year, including expansion of surveillance work within the influenza surveillance network; supporting public health preparedness and response for state and local governments; support the development of therapeutics and the development of vaccines; and the purchase of personal protective equipment for national stockpiles.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease at the National Institutes of Health, added during the press conference that vaccine work is in progress and could be ready for phase 1 testing within a month and a half. If all goes well, it would still be at least 12 - 18 months following the completion of a phase 2 trial before it could be produced for mass consumption.
“It is certainly conceivable that this issue with this coronavirus will go well beyond this season into next season,” Dr. Fauci said. “So a vaccine may not solve the problems of the next couple of months, but it certainly would be an important tool that we would have and we will keep you posted on that.”
He also mentioned that NIAID is looking at a number of candidates for therapeutic treatment of coronavirus. He highlighted Gilead’s remdesivir, a nucleotide analog, as one which undergoing two trials – a randomized controlled trial in China and a copy of that trial in Nebraska among patients with the coronavirus who were taken from the Diamond Princess cruise line in Japan.
“I am optimistic that we will at least get an answer if we do have do have a therapy that really is a gamechanger because then we could do something from the standpoint of intervention for those who are sick,” Dr. Fauci said.
UPDATE: This story was updated 2/25 at 4:51 p.m. ET
“We have for many weeks been saying that, while we hope this is not going to be severe, we are planning as if it is,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, said during a Feb. 25, 2020, telebriefing with reporters. “The data over the last week and the spread in other countries has certainly raised our level of concern and raised our level expectation that we are going to have community spread here.”
Dr. Messonnier noted that the coronavirus is now showing signs of community spread without a known source of exposure in a number of countries, including in Hong Kong, Iran, Italy, Japan, Singapore, South Korea, Taiwan, and Thailand. This has now raised the belief that there will be more widespread outbreaks in the United States.
“What we still don’t know is what that will look like,” she said. “As many of you know, we can have community spread in the United States and have it be reasonably mild. We can have community spread in the U.S. and have it be very severe. That is what we don’t completely know yet and we certainly also don’t exactly know when it is going to happen.”
She reiterated the number of actions being taken to slow the potential spread in the United States, including detecting, tracking, and isolating all cases, as well as restricting travel into the United States and issuing travel advisories for countries where coronavirus outbreaks are known.
“We are doing this with the goal of slowing the introduction of this new virus into the U.S. and buying us more time to prepare,” Dr. Messonnier said, noting the containment strategies have been largely successful, though it will be more difficult as more countries experience community spread of the virus.
Dr. Messonnier also reiterated that at this time there are no vaccines and no medicines to treat the coronavirus. She stressed the need to adhere to nonpharmaceutical interventions (NPIs), as they will be “the most important tools in our response to this virus.”
She said the NPIs will vary based on the severity of the outbreak in any given local community and include personal protective measures that individuals can take every day (many of which mirror the recommendations for preventing the spread of the seasonal flu virus), community NPIs that involve social distancing measures designed to keep people away from others, and environmental NPIs such as surface cleaning measures.
CDC’s latest warning comes as parent agency the Department of Health & Human Services is seeking $2.5 billion in funds from Congress to address the coronavirus outbreak.
During a separate press conference on the same day, HHS Secretary Alex Azar noted that there are five major priorities related to those funds, which would be used in the current year, including expansion of surveillance work within the influenza surveillance network; supporting public health preparedness and response for state and local governments; support the development of therapeutics and the development of vaccines; and the purchase of personal protective equipment for national stockpiles.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease at the National Institutes of Health, added during the press conference that vaccine work is in progress and could be ready for phase 1 testing within a month and a half. If all goes well, it would still be at least 12 - 18 months following the completion of a phase 2 trial before it could be produced for mass consumption.
“It is certainly conceivable that this issue with this coronavirus will go well beyond this season into next season,” Dr. Fauci said. “So a vaccine may not solve the problems of the next couple of months, but it certainly would be an important tool that we would have and we will keep you posted on that.”
He also mentioned that NIAID is looking at a number of candidates for therapeutic treatment of coronavirus. He highlighted Gilead’s remdesivir, a nucleotide analog, as one which undergoing two trials – a randomized controlled trial in China and a copy of that trial in Nebraska among patients with the coronavirus who were taken from the Diamond Princess cruise line in Japan.
“I am optimistic that we will at least get an answer if we do have do have a therapy that really is a gamechanger because then we could do something from the standpoint of intervention for those who are sick,” Dr. Fauci said.
UPDATE: This story was updated 2/25 at 4:51 p.m. ET
Guidance defines vaping-related respiratory syndrome
ORLANDO – Knowledge of vaping devices, familiarity with terminology, and the ability to quickly pinpoint individuals at risk of lung injury are just a few skills that can help critical care professionals confronted with patients who may have vaping-associated lung disease, according to a new guidance document.
The guidance offers a risk-stratification system that classifies patients into groups based on exposure, symptoms, and imaging results, and provides specific evaluation needs and management strategies for each. The guidance is designed to help critical care professionals efficiently identify those at high risk of respiratory failure.
Physicians also need to communicate with patients to identify what substances are being vaped and develop effective methods to encourage abstinence, according to the authors, led by Craig M. Lilly, MD, FCCP, professor of medicine, anesthesiology, and surgery at the University of Massachusetts, Worcester.
“I would encourage every intensivist, when they leave their intensive care unit at night, [to ask], ‘have I advised against vaping today?’ ” Dr. Lilly said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The guidelines, concurrently published as a review article in Critical Care Explorations, propose the term vaping-associated respiratory distress syndrome (VARDS), which the authors say constitutes an acute and progressive respiratory syndrome marked by pathologic changes of lung injury and potentially life-threatening hypoxemic respiratory failure.
They also introduce the three-group Worcester classification system, which is intended to triage vaping-exposed individuals for risk of VARDS based on the presence or absence of vaping-related symptoms and infiltrates, and normal or abnormal oxygen saturation.
“It’s very simple,” said Dr. Lilly, who added that the risk stratification model was developed at the request of Massachusetts public health officials.
Patients with vaping exposure but no symptoms attributable to vaping, such as cough, chest pain, or weight loss, are classified as Worcester Low Risk and testing is not recommended, he said.
By contrast, individuals are considered Worcester Medium Risk if they have vaping exposure, symptoms, and a vaping-associated abnormal pattern on imaging, but no hypoxemia; the presence of hypoxemia would tip the scale toward Worcester High Risk.
“Most patients that have died from vaping have been sent out of emergency rooms when they were noted to be hypoxic,” Dr. Lilly told meeting attendees.
Louella B. Amos, MD, a pediatric pulmonologist at Children’s Hospital of Wisconsin in Milwaukee, said she expects the guidance and risk stratification system will be useful not only for critical care specialists, but for other health care providers as well.
“It’s important to make decisions relatively quickly, depending on the severity of symptoms, and I think this is nice and simple,” Dr. Amos said in an interview.
“We always triage when we see patients, either at the door or in our clinic, or behind that, even in the hospital,” she said. “So I think this can be a great tool for everybody, not only the intensivist, but people who are triaging at the front.”
Management of individuals at low risk of VARDS begins with encouragement of abstinence. “We think that every vaping patient should be advised to quit vaping,” Dr. Lilly said. Patients who are interested in quitting who have not yet worked with someone in their health care team whom they trust can be referred to their primary care physicians for counseling, he added, while those struggling with addiction, unable to quit, and unable to partner with a primary care physician can be referred to an addiction medicine specialist.
For moderate-risk patients, vaping cessation is “absolutely mandatory,” said Dr. Lilly, who recommended monitoring of vaping abstinence, outpatient evaluation based on imaging studies, and adequate follow-up to ensure symptoms resolve, tests normalize, and daily activities bounce back to baseline levels.
The guidance offers more extensive recommendations for the VARDS high-risk group, including supervised vaping abstinence, continuous pulse oximetry, and early intervention with noninvasive ventilation, and mechanical ventilation if required, Dr. Lilly said.
Judging vaping exposure is challenging, requiring clinicians to have a familiarity with the many different devices that are available.
Beyond device type, he added, it’s important to know the various terms for devices and lingo that patients may use to describe them, what solutions are vaped, whether those solutions are commercially prepared or off the street, the dose the device delivers, and a number of other factors, he said.
Clinical evaluation typically comes down to unexplained cough, chest pain, weight loss, fatigue, or dyspnea, though one other clue is whether there are gastrointestinal symptoms: “The same way that aerosols can go down to the lungs, they also go into the GI tract, and when nausea, vomiting, or cramping abdominal pain is tightly associated with vaping exposure, one should assume that the patient has been toxin exposed,” he explained.
Dr. Lilly said he had no financial relationships to disclose.
ORLANDO – Knowledge of vaping devices, familiarity with terminology, and the ability to quickly pinpoint individuals at risk of lung injury are just a few skills that can help critical care professionals confronted with patients who may have vaping-associated lung disease, according to a new guidance document.
The guidance offers a risk-stratification system that classifies patients into groups based on exposure, symptoms, and imaging results, and provides specific evaluation needs and management strategies for each. The guidance is designed to help critical care professionals efficiently identify those at high risk of respiratory failure.
Physicians also need to communicate with patients to identify what substances are being vaped and develop effective methods to encourage abstinence, according to the authors, led by Craig M. Lilly, MD, FCCP, professor of medicine, anesthesiology, and surgery at the University of Massachusetts, Worcester.
“I would encourage every intensivist, when they leave their intensive care unit at night, [to ask], ‘have I advised against vaping today?’ ” Dr. Lilly said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The guidelines, concurrently published as a review article in Critical Care Explorations, propose the term vaping-associated respiratory distress syndrome (VARDS), which the authors say constitutes an acute and progressive respiratory syndrome marked by pathologic changes of lung injury and potentially life-threatening hypoxemic respiratory failure.
They also introduce the three-group Worcester classification system, which is intended to triage vaping-exposed individuals for risk of VARDS based on the presence or absence of vaping-related symptoms and infiltrates, and normal or abnormal oxygen saturation.
“It’s very simple,” said Dr. Lilly, who added that the risk stratification model was developed at the request of Massachusetts public health officials.
Patients with vaping exposure but no symptoms attributable to vaping, such as cough, chest pain, or weight loss, are classified as Worcester Low Risk and testing is not recommended, he said.
By contrast, individuals are considered Worcester Medium Risk if they have vaping exposure, symptoms, and a vaping-associated abnormal pattern on imaging, but no hypoxemia; the presence of hypoxemia would tip the scale toward Worcester High Risk.
“Most patients that have died from vaping have been sent out of emergency rooms when they were noted to be hypoxic,” Dr. Lilly told meeting attendees.
Louella B. Amos, MD, a pediatric pulmonologist at Children’s Hospital of Wisconsin in Milwaukee, said she expects the guidance and risk stratification system will be useful not only for critical care specialists, but for other health care providers as well.
“It’s important to make decisions relatively quickly, depending on the severity of symptoms, and I think this is nice and simple,” Dr. Amos said in an interview.
“We always triage when we see patients, either at the door or in our clinic, or behind that, even in the hospital,” she said. “So I think this can be a great tool for everybody, not only the intensivist, but people who are triaging at the front.”
Management of individuals at low risk of VARDS begins with encouragement of abstinence. “We think that every vaping patient should be advised to quit vaping,” Dr. Lilly said. Patients who are interested in quitting who have not yet worked with someone in their health care team whom they trust can be referred to their primary care physicians for counseling, he added, while those struggling with addiction, unable to quit, and unable to partner with a primary care physician can be referred to an addiction medicine specialist.
For moderate-risk patients, vaping cessation is “absolutely mandatory,” said Dr. Lilly, who recommended monitoring of vaping abstinence, outpatient evaluation based on imaging studies, and adequate follow-up to ensure symptoms resolve, tests normalize, and daily activities bounce back to baseline levels.
The guidance offers more extensive recommendations for the VARDS high-risk group, including supervised vaping abstinence, continuous pulse oximetry, and early intervention with noninvasive ventilation, and mechanical ventilation if required, Dr. Lilly said.
Judging vaping exposure is challenging, requiring clinicians to have a familiarity with the many different devices that are available.
Beyond device type, he added, it’s important to know the various terms for devices and lingo that patients may use to describe them, what solutions are vaped, whether those solutions are commercially prepared or off the street, the dose the device delivers, and a number of other factors, he said.
Clinical evaluation typically comes down to unexplained cough, chest pain, weight loss, fatigue, or dyspnea, though one other clue is whether there are gastrointestinal symptoms: “The same way that aerosols can go down to the lungs, they also go into the GI tract, and when nausea, vomiting, or cramping abdominal pain is tightly associated with vaping exposure, one should assume that the patient has been toxin exposed,” he explained.
Dr. Lilly said he had no financial relationships to disclose.
ORLANDO – Knowledge of vaping devices, familiarity with terminology, and the ability to quickly pinpoint individuals at risk of lung injury are just a few skills that can help critical care professionals confronted with patients who may have vaping-associated lung disease, according to a new guidance document.
The guidance offers a risk-stratification system that classifies patients into groups based on exposure, symptoms, and imaging results, and provides specific evaluation needs and management strategies for each. The guidance is designed to help critical care professionals efficiently identify those at high risk of respiratory failure.
Physicians also need to communicate with patients to identify what substances are being vaped and develop effective methods to encourage abstinence, according to the authors, led by Craig M. Lilly, MD, FCCP, professor of medicine, anesthesiology, and surgery at the University of Massachusetts, Worcester.
“I would encourage every intensivist, when they leave their intensive care unit at night, [to ask], ‘have I advised against vaping today?’ ” Dr. Lilly said at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The guidelines, concurrently published as a review article in Critical Care Explorations, propose the term vaping-associated respiratory distress syndrome (VARDS), which the authors say constitutes an acute and progressive respiratory syndrome marked by pathologic changes of lung injury and potentially life-threatening hypoxemic respiratory failure.
They also introduce the three-group Worcester classification system, which is intended to triage vaping-exposed individuals for risk of VARDS based on the presence or absence of vaping-related symptoms and infiltrates, and normal or abnormal oxygen saturation.
“It’s very simple,” said Dr. Lilly, who added that the risk stratification model was developed at the request of Massachusetts public health officials.
Patients with vaping exposure but no symptoms attributable to vaping, such as cough, chest pain, or weight loss, are classified as Worcester Low Risk and testing is not recommended, he said.
By contrast, individuals are considered Worcester Medium Risk if they have vaping exposure, symptoms, and a vaping-associated abnormal pattern on imaging, but no hypoxemia; the presence of hypoxemia would tip the scale toward Worcester High Risk.
“Most patients that have died from vaping have been sent out of emergency rooms when they were noted to be hypoxic,” Dr. Lilly told meeting attendees.
Louella B. Amos, MD, a pediatric pulmonologist at Children’s Hospital of Wisconsin in Milwaukee, said she expects the guidance and risk stratification system will be useful not only for critical care specialists, but for other health care providers as well.
“It’s important to make decisions relatively quickly, depending on the severity of symptoms, and I think this is nice and simple,” Dr. Amos said in an interview.
“We always triage when we see patients, either at the door or in our clinic, or behind that, even in the hospital,” she said. “So I think this can be a great tool for everybody, not only the intensivist, but people who are triaging at the front.”
Management of individuals at low risk of VARDS begins with encouragement of abstinence. “We think that every vaping patient should be advised to quit vaping,” Dr. Lilly said. Patients who are interested in quitting who have not yet worked with someone in their health care team whom they trust can be referred to their primary care physicians for counseling, he added, while those struggling with addiction, unable to quit, and unable to partner with a primary care physician can be referred to an addiction medicine specialist.
For moderate-risk patients, vaping cessation is “absolutely mandatory,” said Dr. Lilly, who recommended monitoring of vaping abstinence, outpatient evaluation based on imaging studies, and adequate follow-up to ensure symptoms resolve, tests normalize, and daily activities bounce back to baseline levels.
The guidance offers more extensive recommendations for the VARDS high-risk group, including supervised vaping abstinence, continuous pulse oximetry, and early intervention with noninvasive ventilation, and mechanical ventilation if required, Dr. Lilly said.
Judging vaping exposure is challenging, requiring clinicians to have a familiarity with the many different devices that are available.
Beyond device type, he added, it’s important to know the various terms for devices and lingo that patients may use to describe them, what solutions are vaped, whether those solutions are commercially prepared or off the street, the dose the device delivers, and a number of other factors, he said.
Clinical evaluation typically comes down to unexplained cough, chest pain, weight loss, fatigue, or dyspnea, though one other clue is whether there are gastrointestinal symptoms: “The same way that aerosols can go down to the lungs, they also go into the GI tract, and when nausea, vomiting, or cramping abdominal pain is tightly associated with vaping exposure, one should assume that the patient has been toxin exposed,” he explained.
Dr. Lilly said he had no financial relationships to disclose.
REPORTING FROM CCC49
Medicare beneficiaries get few home health visits after ICU stay
ORLANDO – , an analysis of hospital and home health claims data suggests.
The beneficiaries, all discharged directly to home health after an intensive care unit stay, received an average of less than one visit per week in the ensuing month, while a full third received no visits at all, according to authors of the analysis, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Living alone and living in a rural area were associated with significantly fewer home health rehabilitation visits, according to investigator Jason Raymond Falvey, PT, DPT, PhD, of Yale University, New Haven, Conn.
“We identified that these patients are receiving low doses of rehabilitation in home health care settings, and perhaps doses low enough to not be physiologically adequate to overcome the deconditioning and aerobic capacity concerns that these patients have,” Dr. Falvey said.
These findings reflect an “underrecognition” of the importance of rehabilitation both outside and inside the hospital setting, according to Patricia J. Posa, RN, of Saint Joseph Mercy Hospital, Northville, Mich.
“We even struggle to provide sufficient rehabilitation while they’re in the hospital,” Ms. Posa said in an interview. “So I think that we still have a major gap in providing rehab services across the continuum, and part of that is recognizing the deficits that patients, especially our elderly patients, might be leaving the hospital with.”
Medicare beneficiaries who survive a critical illness are often discharged with referrals for physical, occupational, or speech therapy, yet there are not much data on the delivery of that care or how many visits actually take place, according to Dr. Falvey.
He and coinvestigators analyzed data on 3,176 Medicare beneficiaries discharged to home health right after an acute hospitalization with an ICU stay of at least 24 hours. To do this, they linked 2012 Medicare hospital and home health claims data with Medicare demographic and patient assessment data.
They found that the beneficiaries received just 3.5 home rehabilitation visits in 30 days, while 33% had no visits on record.
The factors most strongly associated with receiving fewer rehabilitation visits, in adjusted models, included living in a rural setting, with a rate ratio (RR) of 0.87 and living alone, with an RR of 0.88.
Higher comorbidity count also was associated with fewer visits (RR, 0.98), according to the investigators.
On the other hand, Medicare beneficiaries who received more visits were more likely to be older (RR, 1.03; 1.01-1.04; for every 5 years), more likely to have higher disability scores (RR, 1.03; 1.02-1.04; per point on the Elixhauser Comorbidity Index), and more likely to have reported severe dyspnea (RR, 1.12; 1.04-1.21), according to the report.
More research will be needed to determine the appropriate number of home health rehabilitation visits for older hospitalized patients, according to Ms. Pena, a member of the Society of Critical Care Medicine’s ICU Liberation initiative, which aims to free patients from the harmful effects of pain, agitation/sedation, delirium, immobility, and sleep disruption in the ICU, as well as improve patient outcomes after an ICU stay.
The literature is already fairly robust, she said, on how frequently visits are warranted following specific scenarios such as postsurgical hip or knee replacement or stroke.
“For the general hospitalized patients that are just losing function because they were sick and didn’t get out of bed enough, we don’t really have good data to say, ‘you know, they need three visits a week, or they need two visits a week for an hour in order to improve,’ ” she said, “so the science is still not caught up with the frequency.”
In the absence of data, the number of visits may be left up to an individual clinician’s knowledge and past experience as well as what insurance will pay for, Ms. Pena said.
Dr. Falvey reported royalties related to an online continuing education course on hospital readmissions. No other disclosures were reported.
SOURCE: Falvey J et al. Crit Care Med. 2020 Jan;48(1):28.
ORLANDO – , an analysis of hospital and home health claims data suggests.
The beneficiaries, all discharged directly to home health after an intensive care unit stay, received an average of less than one visit per week in the ensuing month, while a full third received no visits at all, according to authors of the analysis, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Living alone and living in a rural area were associated with significantly fewer home health rehabilitation visits, according to investigator Jason Raymond Falvey, PT, DPT, PhD, of Yale University, New Haven, Conn.
“We identified that these patients are receiving low doses of rehabilitation in home health care settings, and perhaps doses low enough to not be physiologically adequate to overcome the deconditioning and aerobic capacity concerns that these patients have,” Dr. Falvey said.
These findings reflect an “underrecognition” of the importance of rehabilitation both outside and inside the hospital setting, according to Patricia J. Posa, RN, of Saint Joseph Mercy Hospital, Northville, Mich.
“We even struggle to provide sufficient rehabilitation while they’re in the hospital,” Ms. Posa said in an interview. “So I think that we still have a major gap in providing rehab services across the continuum, and part of that is recognizing the deficits that patients, especially our elderly patients, might be leaving the hospital with.”
Medicare beneficiaries who survive a critical illness are often discharged with referrals for physical, occupational, or speech therapy, yet there are not much data on the delivery of that care or how many visits actually take place, according to Dr. Falvey.
He and coinvestigators analyzed data on 3,176 Medicare beneficiaries discharged to home health right after an acute hospitalization with an ICU stay of at least 24 hours. To do this, they linked 2012 Medicare hospital and home health claims data with Medicare demographic and patient assessment data.
They found that the beneficiaries received just 3.5 home rehabilitation visits in 30 days, while 33% had no visits on record.
The factors most strongly associated with receiving fewer rehabilitation visits, in adjusted models, included living in a rural setting, with a rate ratio (RR) of 0.87 and living alone, with an RR of 0.88.
Higher comorbidity count also was associated with fewer visits (RR, 0.98), according to the investigators.
On the other hand, Medicare beneficiaries who received more visits were more likely to be older (RR, 1.03; 1.01-1.04; for every 5 years), more likely to have higher disability scores (RR, 1.03; 1.02-1.04; per point on the Elixhauser Comorbidity Index), and more likely to have reported severe dyspnea (RR, 1.12; 1.04-1.21), according to the report.
More research will be needed to determine the appropriate number of home health rehabilitation visits for older hospitalized patients, according to Ms. Pena, a member of the Society of Critical Care Medicine’s ICU Liberation initiative, which aims to free patients from the harmful effects of pain, agitation/sedation, delirium, immobility, and sleep disruption in the ICU, as well as improve patient outcomes after an ICU stay.
The literature is already fairly robust, she said, on how frequently visits are warranted following specific scenarios such as postsurgical hip or knee replacement or stroke.
“For the general hospitalized patients that are just losing function because they were sick and didn’t get out of bed enough, we don’t really have good data to say, ‘you know, they need three visits a week, or they need two visits a week for an hour in order to improve,’ ” she said, “so the science is still not caught up with the frequency.”
In the absence of data, the number of visits may be left up to an individual clinician’s knowledge and past experience as well as what insurance will pay for, Ms. Pena said.
Dr. Falvey reported royalties related to an online continuing education course on hospital readmissions. No other disclosures were reported.
SOURCE: Falvey J et al. Crit Care Med. 2020 Jan;48(1):28.
ORLANDO – , an analysis of hospital and home health claims data suggests.
The beneficiaries, all discharged directly to home health after an intensive care unit stay, received an average of less than one visit per week in the ensuing month, while a full third received no visits at all, according to authors of the analysis, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
Living alone and living in a rural area were associated with significantly fewer home health rehabilitation visits, according to investigator Jason Raymond Falvey, PT, DPT, PhD, of Yale University, New Haven, Conn.
“We identified that these patients are receiving low doses of rehabilitation in home health care settings, and perhaps doses low enough to not be physiologically adequate to overcome the deconditioning and aerobic capacity concerns that these patients have,” Dr. Falvey said.
These findings reflect an “underrecognition” of the importance of rehabilitation both outside and inside the hospital setting, according to Patricia J. Posa, RN, of Saint Joseph Mercy Hospital, Northville, Mich.
“We even struggle to provide sufficient rehabilitation while they’re in the hospital,” Ms. Posa said in an interview. “So I think that we still have a major gap in providing rehab services across the continuum, and part of that is recognizing the deficits that patients, especially our elderly patients, might be leaving the hospital with.”
Medicare beneficiaries who survive a critical illness are often discharged with referrals for physical, occupational, or speech therapy, yet there are not much data on the delivery of that care or how many visits actually take place, according to Dr. Falvey.
He and coinvestigators analyzed data on 3,176 Medicare beneficiaries discharged to home health right after an acute hospitalization with an ICU stay of at least 24 hours. To do this, they linked 2012 Medicare hospital and home health claims data with Medicare demographic and patient assessment data.
They found that the beneficiaries received just 3.5 home rehabilitation visits in 30 days, while 33% had no visits on record.
The factors most strongly associated with receiving fewer rehabilitation visits, in adjusted models, included living in a rural setting, with a rate ratio (RR) of 0.87 and living alone, with an RR of 0.88.
Higher comorbidity count also was associated with fewer visits (RR, 0.98), according to the investigators.
On the other hand, Medicare beneficiaries who received more visits were more likely to be older (RR, 1.03; 1.01-1.04; for every 5 years), more likely to have higher disability scores (RR, 1.03; 1.02-1.04; per point on the Elixhauser Comorbidity Index), and more likely to have reported severe dyspnea (RR, 1.12; 1.04-1.21), according to the report.
More research will be needed to determine the appropriate number of home health rehabilitation visits for older hospitalized patients, according to Ms. Pena, a member of the Society of Critical Care Medicine’s ICU Liberation initiative, which aims to free patients from the harmful effects of pain, agitation/sedation, delirium, immobility, and sleep disruption in the ICU, as well as improve patient outcomes after an ICU stay.
The literature is already fairly robust, she said, on how frequently visits are warranted following specific scenarios such as postsurgical hip or knee replacement or stroke.
“For the general hospitalized patients that are just losing function because they were sick and didn’t get out of bed enough, we don’t really have good data to say, ‘you know, they need three visits a week, or they need two visits a week for an hour in order to improve,’ ” she said, “so the science is still not caught up with the frequency.”
In the absence of data, the number of visits may be left up to an individual clinician’s knowledge and past experience as well as what insurance will pay for, Ms. Pena said.
Dr. Falvey reported royalties related to an online continuing education course on hospital readmissions. No other disclosures were reported.
SOURCE: Falvey J et al. Crit Care Med. 2020 Jan;48(1):28.
REPORTING FROM CCC49
Opioid use disorder up in sepsis hospitalizations
ORLANDO –
The prevalence of opioid use disorder (OUD) has significantly increased over the past 15 years, the analysis further shows.
Results of the study, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine, further suggested that OUD disproportionately contributes to sepsis deaths in younger, healthier patients.
Together, these findings underscore the importance of ongoing efforts to address the opioid epidemic in the United States, according to researcher Mohammad Alrawashdeh, PhD, MSN, a postdoctoral research fellow with Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston.
“In addition to ongoing efforts to combat the opioid crisis, future public health interventions should focus on increasing awareness, recognition, and aggressive treatment of sepsis in this population,” Dr. Alrawashdeh said in an oral presentation of the study.
This study fills an important knowledge gap regarding the connection between OUD and sepsis, according to Greg S. Martin, MD, MS, FCCM, professor of medicine in pulmonary critical care at Emory University, Atlanta, and secretary for the Society of Critical Care Medicine.
“We’ve not really ever been able to piece together the relationship between opioid use disorders and sepsis,” Dr. Martin said in an interview. “It’s not that people wouldn’t suspect that there’s a connection – it’s more that we have simply not been able to get the kind of data that you can use, like they’ve done here, that really helps you to answer that question.”
The study suggests not only that OUD and sepsis are linked, Dr. Martin added, but that health care providers need to be prepared to potentially see further increases in the number of patients with OUD seen in the intensive care unit.
“Both of those are things that we certainly need to be aware of, both from the individual practitioner perspective and also the public health planning perspective,” he said.
The retrospective study by Dr. Alrawashdeh and coinvestigators focused on electronic health record data for adults admitted to 373 hospitals in the United States between 2009 and 2015, including 375,479 who had sepsis.
Over time, there was a significant increase in the prevalence of OUD among those hospitalized for sepsis, from less than 2.0% in 2009 to more than 3% in 2015, representing a significant 77.3% increase. In general, the prevalence of sepsis was significantly higher among hospitalized patients with OUD compared with patients without the disorder, at 7.2% and 5.6%, respectively.
The sepsis patients with OUD tended to be younger, healthier, and more likely to be white compared with patients without OUD, according to the report. Moreover, the sepsis patients with OUD more often had endocarditis and gram-positive and fungal bloodstream infections. They also required more mechanical ventilation and had more ICU admissions, with longer stays in both the ICU and hospital.
The OUD patients accounted for 2.1% of sepsis-associated deaths overall, but 3.3% of those deaths in healthy patients, and 7.1% of deaths among younger patients, according to the report.
Those findings provide some clues that could help guide clinical practice, according to Dr. Martin. For example, the data show a nearly fivefold increased risk of endocarditis with OUD (3.9% versus 0.7%), which may inform screening practices.
“While we don’t necessarily screen every sepsis patient for endocarditis, if it’s an opioid use disorder patient – particularly one with a bloodstream infection – then that’s almost certainly something you should be doing,” Dr. Martin said.
The data suggest gram-positive bacterial and fungal infections will more likely be encountered among these patients, which could guide empiric treatment, he said.
Providers specializing in OUD should have a heightened awareness of the potential for infection and sepsis among those patients, and perhaps be more attuned to fever and other signs of infection that might warrant a referral or additional care, Dr. Martin added.
Dr. Alrawashdeh reported no disclosures related to the study.
SOURCE: Alrawashdeh M et al. Crit Care Med. 2020 Jan;48(1):28. Abstract 56.
ORLANDO –
The prevalence of opioid use disorder (OUD) has significantly increased over the past 15 years, the analysis further shows.
Results of the study, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine, further suggested that OUD disproportionately contributes to sepsis deaths in younger, healthier patients.
Together, these findings underscore the importance of ongoing efforts to address the opioid epidemic in the United States, according to researcher Mohammad Alrawashdeh, PhD, MSN, a postdoctoral research fellow with Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston.
“In addition to ongoing efforts to combat the opioid crisis, future public health interventions should focus on increasing awareness, recognition, and aggressive treatment of sepsis in this population,” Dr. Alrawashdeh said in an oral presentation of the study.
This study fills an important knowledge gap regarding the connection between OUD and sepsis, according to Greg S. Martin, MD, MS, FCCM, professor of medicine in pulmonary critical care at Emory University, Atlanta, and secretary for the Society of Critical Care Medicine.
“We’ve not really ever been able to piece together the relationship between opioid use disorders and sepsis,” Dr. Martin said in an interview. “It’s not that people wouldn’t suspect that there’s a connection – it’s more that we have simply not been able to get the kind of data that you can use, like they’ve done here, that really helps you to answer that question.”
The study suggests not only that OUD and sepsis are linked, Dr. Martin added, but that health care providers need to be prepared to potentially see further increases in the number of patients with OUD seen in the intensive care unit.
“Both of those are things that we certainly need to be aware of, both from the individual practitioner perspective and also the public health planning perspective,” he said.
The retrospective study by Dr. Alrawashdeh and coinvestigators focused on electronic health record data for adults admitted to 373 hospitals in the United States between 2009 and 2015, including 375,479 who had sepsis.
Over time, there was a significant increase in the prevalence of OUD among those hospitalized for sepsis, from less than 2.0% in 2009 to more than 3% in 2015, representing a significant 77.3% increase. In general, the prevalence of sepsis was significantly higher among hospitalized patients with OUD compared with patients without the disorder, at 7.2% and 5.6%, respectively.
The sepsis patients with OUD tended to be younger, healthier, and more likely to be white compared with patients without OUD, according to the report. Moreover, the sepsis patients with OUD more often had endocarditis and gram-positive and fungal bloodstream infections. They also required more mechanical ventilation and had more ICU admissions, with longer stays in both the ICU and hospital.
The OUD patients accounted for 2.1% of sepsis-associated deaths overall, but 3.3% of those deaths in healthy patients, and 7.1% of deaths among younger patients, according to the report.
Those findings provide some clues that could help guide clinical practice, according to Dr. Martin. For example, the data show a nearly fivefold increased risk of endocarditis with OUD (3.9% versus 0.7%), which may inform screening practices.
“While we don’t necessarily screen every sepsis patient for endocarditis, if it’s an opioid use disorder patient – particularly one with a bloodstream infection – then that’s almost certainly something you should be doing,” Dr. Martin said.
The data suggest gram-positive bacterial and fungal infections will more likely be encountered among these patients, which could guide empiric treatment, he said.
Providers specializing in OUD should have a heightened awareness of the potential for infection and sepsis among those patients, and perhaps be more attuned to fever and other signs of infection that might warrant a referral or additional care, Dr. Martin added.
Dr. Alrawashdeh reported no disclosures related to the study.
SOURCE: Alrawashdeh M et al. Crit Care Med. 2020 Jan;48(1):28. Abstract 56.
ORLANDO –
The prevalence of opioid use disorder (OUD) has significantly increased over the past 15 years, the analysis further shows.
Results of the study, presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine, further suggested that OUD disproportionately contributes to sepsis deaths in younger, healthier patients.
Together, these findings underscore the importance of ongoing efforts to address the opioid epidemic in the United States, according to researcher Mohammad Alrawashdeh, PhD, MSN, a postdoctoral research fellow with Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston.
“In addition to ongoing efforts to combat the opioid crisis, future public health interventions should focus on increasing awareness, recognition, and aggressive treatment of sepsis in this population,” Dr. Alrawashdeh said in an oral presentation of the study.
This study fills an important knowledge gap regarding the connection between OUD and sepsis, according to Greg S. Martin, MD, MS, FCCM, professor of medicine in pulmonary critical care at Emory University, Atlanta, and secretary for the Society of Critical Care Medicine.
“We’ve not really ever been able to piece together the relationship between opioid use disorders and sepsis,” Dr. Martin said in an interview. “It’s not that people wouldn’t suspect that there’s a connection – it’s more that we have simply not been able to get the kind of data that you can use, like they’ve done here, that really helps you to answer that question.”
The study suggests not only that OUD and sepsis are linked, Dr. Martin added, but that health care providers need to be prepared to potentially see further increases in the number of patients with OUD seen in the intensive care unit.
“Both of those are things that we certainly need to be aware of, both from the individual practitioner perspective and also the public health planning perspective,” he said.
The retrospective study by Dr. Alrawashdeh and coinvestigators focused on electronic health record data for adults admitted to 373 hospitals in the United States between 2009 and 2015, including 375,479 who had sepsis.
Over time, there was a significant increase in the prevalence of OUD among those hospitalized for sepsis, from less than 2.0% in 2009 to more than 3% in 2015, representing a significant 77.3% increase. In general, the prevalence of sepsis was significantly higher among hospitalized patients with OUD compared with patients without the disorder, at 7.2% and 5.6%, respectively.
The sepsis patients with OUD tended to be younger, healthier, and more likely to be white compared with patients without OUD, according to the report. Moreover, the sepsis patients with OUD more often had endocarditis and gram-positive and fungal bloodstream infections. They also required more mechanical ventilation and had more ICU admissions, with longer stays in both the ICU and hospital.
The OUD patients accounted for 2.1% of sepsis-associated deaths overall, but 3.3% of those deaths in healthy patients, and 7.1% of deaths among younger patients, according to the report.
Those findings provide some clues that could help guide clinical practice, according to Dr. Martin. For example, the data show a nearly fivefold increased risk of endocarditis with OUD (3.9% versus 0.7%), which may inform screening practices.
“While we don’t necessarily screen every sepsis patient for endocarditis, if it’s an opioid use disorder patient – particularly one with a bloodstream infection – then that’s almost certainly something you should be doing,” Dr. Martin said.
The data suggest gram-positive bacterial and fungal infections will more likely be encountered among these patients, which could guide empiric treatment, he said.
Providers specializing in OUD should have a heightened awareness of the potential for infection and sepsis among those patients, and perhaps be more attuned to fever and other signs of infection that might warrant a referral or additional care, Dr. Martin added.
Dr. Alrawashdeh reported no disclosures related to the study.
SOURCE: Alrawashdeh M et al. Crit Care Med. 2020 Jan;48(1):28. Abstract 56.
REPORTING FROM CCC49
Vitamin E acetate found in more vapers’ lung fluid
Analysis of additional lung fluid samples confirms the presence of vitamin E acetate in patients with electronic-cigarette, or vaping, product use–associated lung injury, according to a report on 51 patients in 16 states.
The average age of the patients was 23 years; 69% were male.
The report extends previous work by the Centers for Disease Control and Prevention to test for harmful substances in bronchoalveolar-lavage (BAL) fluid obtained from patients with electronic-cigarette, or vaping, product use–associated lung injury (EVALI) as part of a strategy to understand and manage the recent outbreak of EVALI cases in the United States, wrote Benjamin C. Blount, PhD, of the Division of Laboratory Sciences at the CDC’s National Center for Environmental Health, and colleagues.
“CDC was addressing a serious outbreak of lung injury that was sometimes lethal; but after the first 10 weeks of the outbreak investigation, the cause was still unknown,” Dr. Blount said in an interview. “Possible theories could not be evaluated unless the laboratory could develop tests that could confidently connect exposure to lung injury. Detection of toxicants in bronchoalveolar-lavage fluid from patients with EVALI can provide direct information on exposure within the lung.”
In a study published in the New England Journal of Medicine, the researchers examined the BAL of 51 cases of EVALI from 16 states. They analyzed the samples for multiple toxicants, including vitamin E acetate, plant oils, medium-chain triglyceride oil, coconut oil, petroleum distillates, and diluent terpenes.
Overall, 77% of the patients reported using products containing THC, 67% reported using products containing nicotine, and 51% reported using both types.
Researchers found vitamin E acetate in 48 of the 51 patients (94%); no vitamin E acetate was found in the BAL of healthy controls. Coconut oil and limonene were found in one patient each, but none of the other toxicants was found in the samples from the patients or controls.
In addition, 47 of the 50 patients for whom data were available either had detectable tetrahydrocannabinol (THC) or its metabolites in their BAL fluid samples, or they reported vaping THC products within 90 days before they became ill. Nicotine or its metabolites were found in 30 of 47 patients (64%).
The study findings were limited by several factors, including the potential role of vitamin E acetate as a marker for exposure to other toxicants, the uncertainty of the role of aerosolized constituents formed when vitamin E acetate is heated, and the lack of data on the timing and burden of toxicant exposure, the investigators noted.
As for the next steps in research, “additional studies are needed to examine the respiratory effects of inhaling aerosolized vitamin E acetate and provide information on whether vitamin E acetate in isolation causes lung injury,” Dr. Blount explained. Analysis of the aerosol and gases generated by case-associated product fluids is ongoing.
“When CDC developed the BAL study for this response, we considered several possible toxicants in this investigation to find a possible cause of the outbreak,” Dr. Blount noted. “To accomplish the study, CDC’s Environmental Health Laboratory developed 12 analytical methods and validated them in less than 3 weeks because of the urgent nature of the emergency.”
Dr. Blount said he would advise clinicians to “continue to reference CDC guidance on treating suspected or EVALI patients.” In December, the CDC published updated guidance for clinicians on hospitalized EVALI patients. “Following this guidance and other recommendations could reduce EVALI-associated morbidity and mortality,” Dr. Blount said.
The study was supported in part by the National Cancer Institute, the FDA Center for Tobacco Products, and Ohio State University Pelotonia Intramural Research. The researchers had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2020 Feb 20. doi: 10.1056/NEJMoa1916433.
Analysis of additional lung fluid samples confirms the presence of vitamin E acetate in patients with electronic-cigarette, or vaping, product use–associated lung injury, according to a report on 51 patients in 16 states.
The average age of the patients was 23 years; 69% were male.
The report extends previous work by the Centers for Disease Control and Prevention to test for harmful substances in bronchoalveolar-lavage (BAL) fluid obtained from patients with electronic-cigarette, or vaping, product use–associated lung injury (EVALI) as part of a strategy to understand and manage the recent outbreak of EVALI cases in the United States, wrote Benjamin C. Blount, PhD, of the Division of Laboratory Sciences at the CDC’s National Center for Environmental Health, and colleagues.
“CDC was addressing a serious outbreak of lung injury that was sometimes lethal; but after the first 10 weeks of the outbreak investigation, the cause was still unknown,” Dr. Blount said in an interview. “Possible theories could not be evaluated unless the laboratory could develop tests that could confidently connect exposure to lung injury. Detection of toxicants in bronchoalveolar-lavage fluid from patients with EVALI can provide direct information on exposure within the lung.”
In a study published in the New England Journal of Medicine, the researchers examined the BAL of 51 cases of EVALI from 16 states. They analyzed the samples for multiple toxicants, including vitamin E acetate, plant oils, medium-chain triglyceride oil, coconut oil, petroleum distillates, and diluent terpenes.
Overall, 77% of the patients reported using products containing THC, 67% reported using products containing nicotine, and 51% reported using both types.
Researchers found vitamin E acetate in 48 of the 51 patients (94%); no vitamin E acetate was found in the BAL of healthy controls. Coconut oil and limonene were found in one patient each, but none of the other toxicants was found in the samples from the patients or controls.
In addition, 47 of the 50 patients for whom data were available either had detectable tetrahydrocannabinol (THC) or its metabolites in their BAL fluid samples, or they reported vaping THC products within 90 days before they became ill. Nicotine or its metabolites were found in 30 of 47 patients (64%).
The study findings were limited by several factors, including the potential role of vitamin E acetate as a marker for exposure to other toxicants, the uncertainty of the role of aerosolized constituents formed when vitamin E acetate is heated, and the lack of data on the timing and burden of toxicant exposure, the investigators noted.
As for the next steps in research, “additional studies are needed to examine the respiratory effects of inhaling aerosolized vitamin E acetate and provide information on whether vitamin E acetate in isolation causes lung injury,” Dr. Blount explained. Analysis of the aerosol and gases generated by case-associated product fluids is ongoing.
“When CDC developed the BAL study for this response, we considered several possible toxicants in this investigation to find a possible cause of the outbreak,” Dr. Blount noted. “To accomplish the study, CDC’s Environmental Health Laboratory developed 12 analytical methods and validated them in less than 3 weeks because of the urgent nature of the emergency.”
Dr. Blount said he would advise clinicians to “continue to reference CDC guidance on treating suspected or EVALI patients.” In December, the CDC published updated guidance for clinicians on hospitalized EVALI patients. “Following this guidance and other recommendations could reduce EVALI-associated morbidity and mortality,” Dr. Blount said.
The study was supported in part by the National Cancer Institute, the FDA Center for Tobacco Products, and Ohio State University Pelotonia Intramural Research. The researchers had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2020 Feb 20. doi: 10.1056/NEJMoa1916433.
Analysis of additional lung fluid samples confirms the presence of vitamin E acetate in patients with electronic-cigarette, or vaping, product use–associated lung injury, according to a report on 51 patients in 16 states.
The average age of the patients was 23 years; 69% were male.
The report extends previous work by the Centers for Disease Control and Prevention to test for harmful substances in bronchoalveolar-lavage (BAL) fluid obtained from patients with electronic-cigarette, or vaping, product use–associated lung injury (EVALI) as part of a strategy to understand and manage the recent outbreak of EVALI cases in the United States, wrote Benjamin C. Blount, PhD, of the Division of Laboratory Sciences at the CDC’s National Center for Environmental Health, and colleagues.
“CDC was addressing a serious outbreak of lung injury that was sometimes lethal; but after the first 10 weeks of the outbreak investigation, the cause was still unknown,” Dr. Blount said in an interview. “Possible theories could not be evaluated unless the laboratory could develop tests that could confidently connect exposure to lung injury. Detection of toxicants in bronchoalveolar-lavage fluid from patients with EVALI can provide direct information on exposure within the lung.”
In a study published in the New England Journal of Medicine, the researchers examined the BAL of 51 cases of EVALI from 16 states. They analyzed the samples for multiple toxicants, including vitamin E acetate, plant oils, medium-chain triglyceride oil, coconut oil, petroleum distillates, and diluent terpenes.
Overall, 77% of the patients reported using products containing THC, 67% reported using products containing nicotine, and 51% reported using both types.
Researchers found vitamin E acetate in 48 of the 51 patients (94%); no vitamin E acetate was found in the BAL of healthy controls. Coconut oil and limonene were found in one patient each, but none of the other toxicants was found in the samples from the patients or controls.
In addition, 47 of the 50 patients for whom data were available either had detectable tetrahydrocannabinol (THC) or its metabolites in their BAL fluid samples, or they reported vaping THC products within 90 days before they became ill. Nicotine or its metabolites were found in 30 of 47 patients (64%).
The study findings were limited by several factors, including the potential role of vitamin E acetate as a marker for exposure to other toxicants, the uncertainty of the role of aerosolized constituents formed when vitamin E acetate is heated, and the lack of data on the timing and burden of toxicant exposure, the investigators noted.
As for the next steps in research, “additional studies are needed to examine the respiratory effects of inhaling aerosolized vitamin E acetate and provide information on whether vitamin E acetate in isolation causes lung injury,” Dr. Blount explained. Analysis of the aerosol and gases generated by case-associated product fluids is ongoing.
“When CDC developed the BAL study for this response, we considered several possible toxicants in this investigation to find a possible cause of the outbreak,” Dr. Blount noted. “To accomplish the study, CDC’s Environmental Health Laboratory developed 12 analytical methods and validated them in less than 3 weeks because of the urgent nature of the emergency.”
Dr. Blount said he would advise clinicians to “continue to reference CDC guidance on treating suspected or EVALI patients.” In December, the CDC published updated guidance for clinicians on hospitalized EVALI patients. “Following this guidance and other recommendations could reduce EVALI-associated morbidity and mortality,” Dr. Blount said.
The study was supported in part by the National Cancer Institute, the FDA Center for Tobacco Products, and Ohio State University Pelotonia Intramural Research. The researchers had no financial conflicts to disclose.
SOURCE: Blount BC et al. N Engl J Med. 2020 Feb 20. doi: 10.1056/NEJMoa1916433.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Drop in flu activity suggests season may have peaked
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
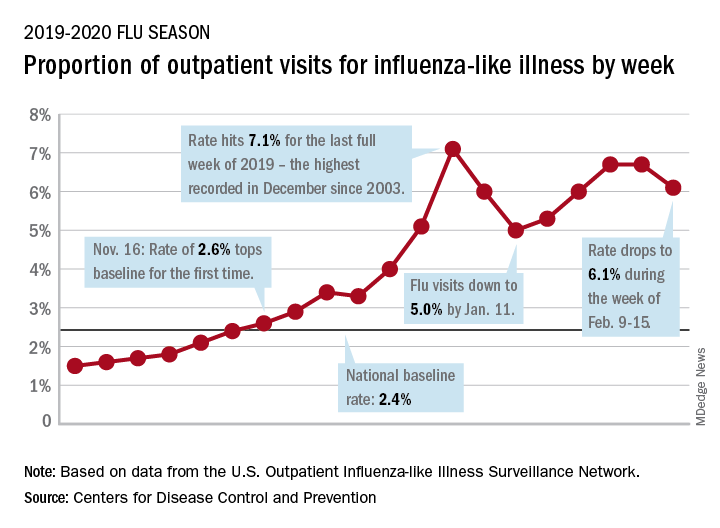
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.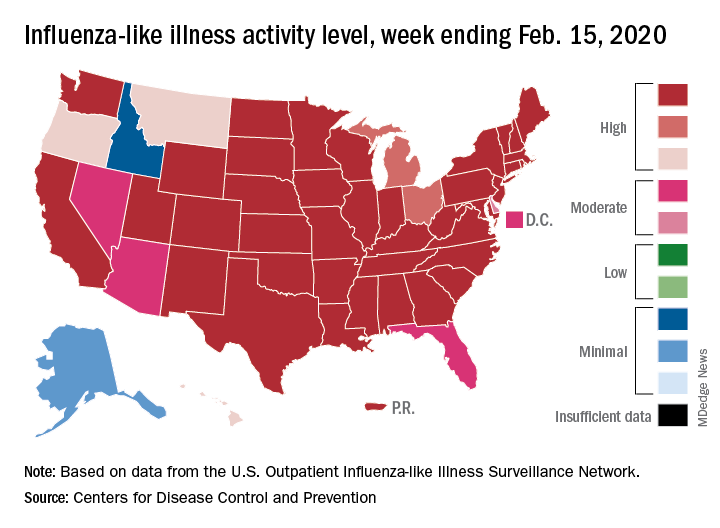
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
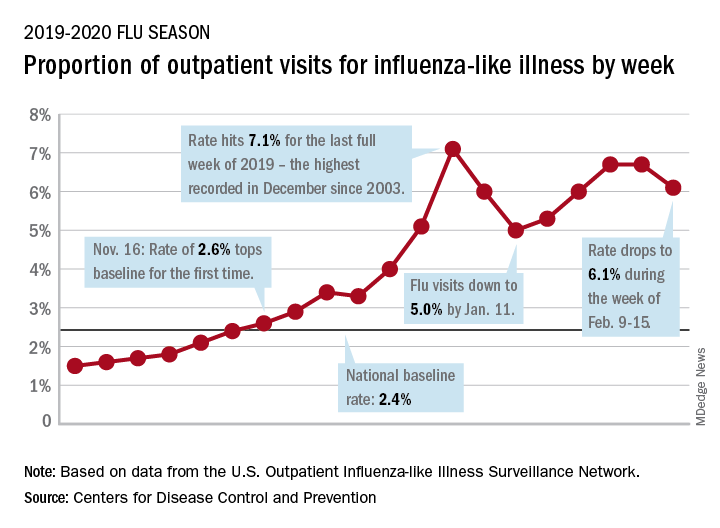
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.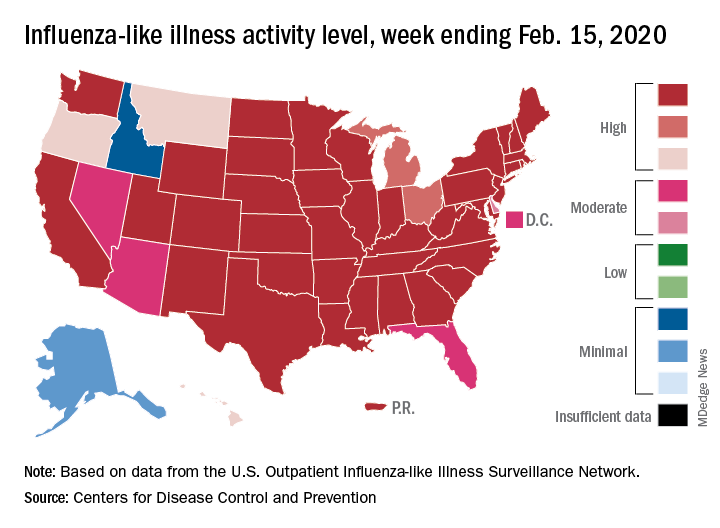
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
Influenza activity dropped during the week ending Feb. 15, according to the Centers for Disease Control and Prevention. That decline, along with revised data from the 2 previous weeks, suggests that the 2019-2020 season has peaked for the second time. The rate of outpatient visits for influenza-like illness (ILI) came in at 6.1% for the week ending Feb. 15, after two straight weeks at 6.7%, the CDC’s influenza division reported Feb. 21.
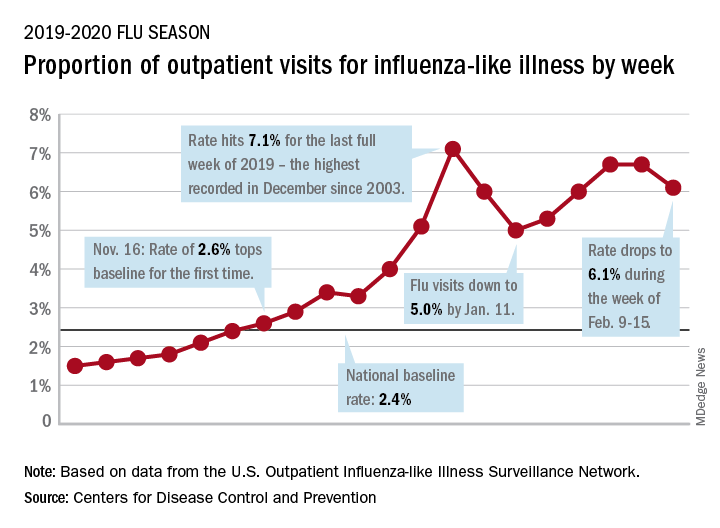
The rates for those 2 earlier weeks had previously been reported at 6.8% (Feb. 8) and 6.6% (Feb. 1), which means that there have now been 2 consecutive weeks without an increase in national ILI activity.
State-level activity was down slightly as well. For the week ending Feb. 15, there were 39 states and Puerto Rico at the highest level of activity on the CDC’s 1-10 scale, compared with 41 states and Puerto Rico the week before. The number of states in the “high” range, which includes levels 8 and 9, went from 44 to 45, however, CDC data show.
Laboratory measures also dropped a bit. For the week, 29.6% of respiratory specimens tested positive for influenza, compared with 30.3% the previous week. The predominance of influenza A continued to increase, as type A went from 59.4% to 63.5% of positive specimens and type B dropped from 40.6% to 36.5%, the influenza division said.
In a separate report, the CDC announced interim flu vaccine effectiveness estimates.For the 2019-2020 season so far, “flu vaccines are reducing doctor’s visits for flu illness by almost half (45%). This is consistent with estimates of flu vaccine effectiveness (VE) from previous flu seasons that ranged from 40% to 60% when flu vaccine viruses were similar to circulating influenza viruses,” the CDC said.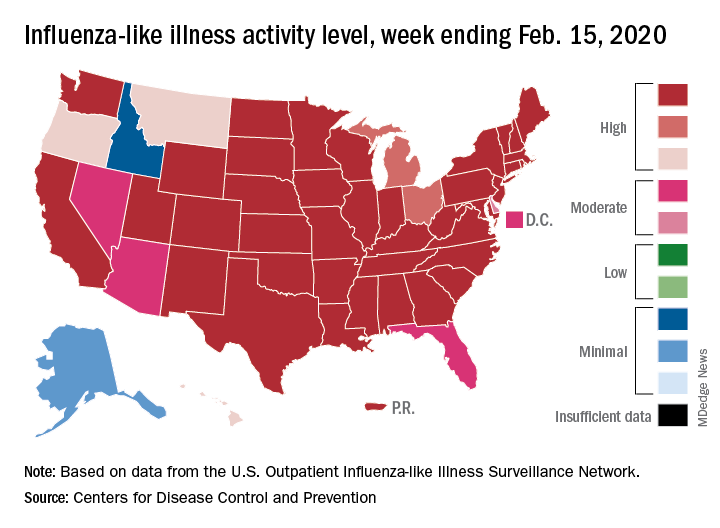
Although VE among children aged 6 months to 17 years is even higher, at 55%, this season “has been especially bad for children. Flu hospitalization rates among children are higher than at this time in other recent seasons, including the 2017-18 season,” the CDC noted.
The number of pediatric flu deaths for 2019-2020 – now up to 105 – is “higher for the same time period than in every season since reporting began in 2004-05, with the exception of the 2009 pandemic,” the CDC added.
Interim VE estimates for other age groups are 25% for adults aged 18-49 and 43% for those 50 years and older. “The lower VE point estimates observed among adults 18-49 years appear to be associated with a trend suggesting lower VE in this age group against A(H1N1)pdm09 viruses,” the CDC said.
FROM THE CDC
Dr. Eric Howell selected as next CEO of SHM
The Society of Hospital Medicine has announced that Eric Howell, MD, MHM, will become its next CEO effective July 1, 2020. Dr. Howell will replace Laurence Wellikson, MD, MHM, who helped to found the society, and has been its first and only CEO since 2000.
“On behalf of the SHM board of directors, we welcome Dr. Howell as the incoming CEO for our organization who, with the mission-driven commitment and dedication of SHM staff, will take SHM into the future,” said Danielle Scheurer, MD, MSRC, SFHM, president-elect of SHM and chair of the CEO search committee. “With his broad knowledge of hospital medicine and extensive volunteer leadership at SHM, Dr. Howell’s experience is a natural complement to SHM’s core mission.”
Dr. Howell has a long history with SHM and has a wealth of expertise in hospital medicine. Since July 2018, he has served as chief operating officer of SHM, leading senior management’s planning and defining organizational goals to drive extensive, sustainable growth. Dr. Howell has also served as the senior physician advisor to SHM’s Center for Quality Improvement, the society’s arm that conducts quality improvement programs for hospitalist teams, since 2015. He is a past president of SHM’s board of directors and currently serves as the course director for the SHM Leadership Academies.
“Having been involved with SHM in many capacities since first joining, I am truly honored to become SHM’s CEO,” Dr. Howell said. “I always tell everyone that my goal is to make the world a better place, and I know that SHM’s staff will be able to do just that through the development and deployment of a variety of products, tools, and services to help hospitalists improve patient care.”
In addition to serving in various capacities at SHM, Dr. Howell has been a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center in Baltimore, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals.
Dr. Howell received his electrical engineering degree from the University of Maryland, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput, and patient outcomes.
The search process was led by a CEO search committee, comprised of members of the SHM board of directors and assisted by the executive search firm Spencer Stuart. Launching a nationwide search, the firm identified candidates with the values and leadership qualities necessary to ensure the future growth of the organization.
“After a thorough search process, Dr. Eric Howell emerged as the right person to lead SHM,” said SHM board president Christopher Frost, MD, SFHM, “His experience in hospital medicine and his servant leadership style make him an ideal fit to lead SHM to even greater future success.”
In the coming weeks, the SHM board of directors will work with Dr. Howell and Dr. Wellikson on a smooth transition plan to have Dr. Howell assume the role on July 1, 2020.
The Society of Hospital Medicine has announced that Eric Howell, MD, MHM, will become its next CEO effective July 1, 2020. Dr. Howell will replace Laurence Wellikson, MD, MHM, who helped to found the society, and has been its first and only CEO since 2000.
“On behalf of the SHM board of directors, we welcome Dr. Howell as the incoming CEO for our organization who, with the mission-driven commitment and dedication of SHM staff, will take SHM into the future,” said Danielle Scheurer, MD, MSRC, SFHM, president-elect of SHM and chair of the CEO search committee. “With his broad knowledge of hospital medicine and extensive volunteer leadership at SHM, Dr. Howell’s experience is a natural complement to SHM’s core mission.”
Dr. Howell has a long history with SHM and has a wealth of expertise in hospital medicine. Since July 2018, he has served as chief operating officer of SHM, leading senior management’s planning and defining organizational goals to drive extensive, sustainable growth. Dr. Howell has also served as the senior physician advisor to SHM’s Center for Quality Improvement, the society’s arm that conducts quality improvement programs for hospitalist teams, since 2015. He is a past president of SHM’s board of directors and currently serves as the course director for the SHM Leadership Academies.
“Having been involved with SHM in many capacities since first joining, I am truly honored to become SHM’s CEO,” Dr. Howell said. “I always tell everyone that my goal is to make the world a better place, and I know that SHM’s staff will be able to do just that through the development and deployment of a variety of products, tools, and services to help hospitalists improve patient care.”
In addition to serving in various capacities at SHM, Dr. Howell has been a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center in Baltimore, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals.
Dr. Howell received his electrical engineering degree from the University of Maryland, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput, and patient outcomes.
The search process was led by a CEO search committee, comprised of members of the SHM board of directors and assisted by the executive search firm Spencer Stuart. Launching a nationwide search, the firm identified candidates with the values and leadership qualities necessary to ensure the future growth of the organization.
“After a thorough search process, Dr. Eric Howell emerged as the right person to lead SHM,” said SHM board president Christopher Frost, MD, SFHM, “His experience in hospital medicine and his servant leadership style make him an ideal fit to lead SHM to even greater future success.”
In the coming weeks, the SHM board of directors will work with Dr. Howell and Dr. Wellikson on a smooth transition plan to have Dr. Howell assume the role on July 1, 2020.
The Society of Hospital Medicine has announced that Eric Howell, MD, MHM, will become its next CEO effective July 1, 2020. Dr. Howell will replace Laurence Wellikson, MD, MHM, who helped to found the society, and has been its first and only CEO since 2000.
“On behalf of the SHM board of directors, we welcome Dr. Howell as the incoming CEO for our organization who, with the mission-driven commitment and dedication of SHM staff, will take SHM into the future,” said Danielle Scheurer, MD, MSRC, SFHM, president-elect of SHM and chair of the CEO search committee. “With his broad knowledge of hospital medicine and extensive volunteer leadership at SHM, Dr. Howell’s experience is a natural complement to SHM’s core mission.”
Dr. Howell has a long history with SHM and has a wealth of expertise in hospital medicine. Since July 2018, he has served as chief operating officer of SHM, leading senior management’s planning and defining organizational goals to drive extensive, sustainable growth. Dr. Howell has also served as the senior physician advisor to SHM’s Center for Quality Improvement, the society’s arm that conducts quality improvement programs for hospitalist teams, since 2015. He is a past president of SHM’s board of directors and currently serves as the course director for the SHM Leadership Academies.
“Having been involved with SHM in many capacities since first joining, I am truly honored to become SHM’s CEO,” Dr. Howell said. “I always tell everyone that my goal is to make the world a better place, and I know that SHM’s staff will be able to do just that through the development and deployment of a variety of products, tools, and services to help hospitalists improve patient care.”
In addition to serving in various capacities at SHM, Dr. Howell has been a professor of medicine in the department of medicine at Johns Hopkins University, Baltimore. He has held multiple titles within the Johns Hopkins medical institutions, including chief of the division of hospital medicine at Johns Hopkins Bayview Medical Center in Baltimore, section chief of hospital medicine for Johns Hopkins Community Physicians, deputy director of hospital operations for the department of medicine at Johns Hopkins Bayview, and chief medical officer of operations at Johns Hopkins Bayview. Dr. Howell joined the Johns Hopkins Bayview hospitalist program in 2000, began the Howard County (Md.) General Hospital hospitalist program in 2010, and oversaw nearly 200 physicians and clinical staff providing patient care in three hospitals.
Dr. Howell received his electrical engineering degree from the University of Maryland, which has proven instrumental in his mastery of managing and implementing change in the hospital. His research has focused on the relationship between the emergency department and medicine floors, improving communication, throughput, and patient outcomes.
The search process was led by a CEO search committee, comprised of members of the SHM board of directors and assisted by the executive search firm Spencer Stuart. Launching a nationwide search, the firm identified candidates with the values and leadership qualities necessary to ensure the future growth of the organization.
“After a thorough search process, Dr. Eric Howell emerged as the right person to lead SHM,” said SHM board president Christopher Frost, MD, SFHM, “His experience in hospital medicine and his servant leadership style make him an ideal fit to lead SHM to even greater future success.”
In the coming weeks, the SHM board of directors will work with Dr. Howell and Dr. Wellikson on a smooth transition plan to have Dr. Howell assume the role on July 1, 2020.
Medical malpractice insurance premiums likely to rise in 2020
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.
For more than a decade, most physicians have paid a steady amount for medical liability insurance. But that price stability appears to be ending, according to a recent analysis.
In 2019, more than 25% of medical liability insurance premiums rose for internists, ob.gyns., and surgeons, a review by the Medical Liability Monitor (MLM) found. The MLM survey, published annually, analyzes premium data from major malpractice insurers based on mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
The increases mark a shift in the long-stable market and suggest rising premiums in the future, said Michael Matray, editor for the Medical Liability Monitor.
“It’s my impression that rates will increase again in [2020]. It’s almost a foregone conclusion,” he said in an interview. “We can expect more firming within the market.”
Most of the premium increases in 2019 were small – between 0.1% and 10%, Mr. Matray said. At the same time, close to 70% of premium rates were flat in 2019 and about 5% of premium rates decreased, according to the survey, released in late 2019.
Comparatively, about 58% of premium rates were flat from 2007 to 2014, about 30% of rates went down during that time frame, and 12% of rates went up. From 2015 to 2018, nearly 76% of rates were steady, 10% went down, and 15% of rates increased, according to the latest analysis. 2019 was the first time since 2006 that more than 25% of premium rates rose, the survey noted.
“This is a normal cycle for the insurance industry – years of feast, followed by years of famine. Eventually companies reach a point where they feel enough pain and one response is to raise rates,” said Alyssa Gittleman, a coauthor of the survey and senior associate in the insurance research department at Conning, an investment management firm for the insurance industry.
“We could also point out many of the rate increases reported in the survey came from the larger [medical professional liability] companies. These companies are well capitalized, and the fact that they are raising rates could be a bellwether that a hard market is coming. However, as we said in the survey, it will probably take another 12-24 months before we know for certain,” she added.
Location, location, location
Physicians continue to pay vastly different premiums depending on where they practice. Ob.gyns. in eastern New York for example, paid about $201,000 in 2019, while their Minnesota colleagues paid about $16,500. Internists in southern Florida, meanwhile, paid about $49,000 in 2019, while their counterparts in northern California paid about $4,100. General surgeons in southern Florida paid about $195,000 for malpractice insurance, while some Wisconsin general surgeons paid about $11,000.
“Medical malpractice rates are determined locally, that’s why we don’t give state averages or national averages [in the survey],” Mr. Matray said. “It’s all determined by malpractice claims history within that territory and how aggressive the plaintiffs bar is in those areas.”
Two states – Arizona and Pennsylvania – experienced exceptional rate decreases in 2019. In Arizona, The Doctors Company lowered their rates by more than 60% for internists, general surgeons, and ob.gyns. In Pennsylvania, which operates a patient compensation fund, The Doctors Company decreased its rates between 20% and 46% for each of the three specialties. The insurer reported it made the decreases to align its rates with other insurers in those states, according to the survey. The Doctors Company did not respond to messages seeking comment for this article.
When individual companies greatly increase or greatly decrease rates in a given state, it’s generally to bring their rates in line with those of larger companies in the market, said Bill Burns, a coauthor of the MLM report and a vice president in the insurance research department at Conning. In 2018, The Doctors Company held about 2% of the market in Arizona, and the company held about 1% of the Pennsylvania market, he noted.
“These decreases, which get them in line with the larger writers, should tighten up the range of rates in those states,” Mr. Burns said in an interview. “To sell the product, they’re going to have be close to the competition.”
For a clear picture of the overall premium landscape, the survey authors analyzed the data both with and without the exceptional rate decreases in Arizona and Pennsylvania. Regionally – excluding the exceptional decreases – the average premium rate increase was 2% in the Midwest, 1.4% in the Northeast, 1.1% in the South, and 0.3% in the West.
For all three specialties surveyed, premiums rose slightly in 2019, with surgeons experiencing the largest increase. Internists saw a nearly 1% average rate increase, ob.gyns. experienced a 0.5% rise, and surgeons experienced a 2.3% rate increase, the survey found. For doctors in the seven states that have patient compensation funds, internists experienced a nearly 2.1% average rate increase, ob.gyns. saw a 1.4% rise, and surgeons experienced a 2.1% rate increase. (These data sets exclude the exceptional rate decreases in Arizona and Pennsylvania.)
The change in rates for general surgery could mean more claims are being filed against surgeons or that the cost of claims are rising, Mr. Burns said.
“The differences are not terribly significant, but suggest something is happening with general surgery,” he said.
Why are rates on the rise?
A number of factors are behind the changing medical liability insurance market, said Brian Atchinson, president and CEO for the Medical Professional Liability Association (MPL Association), a trade association for medical liability insurers.
While the frequency of claims against physicians has remained flat for an extended period of time, the cost of managing those claims has continued to increase, he said.
“Medical liability insurers insuring physicians and other clinicians, they need to defend every claim that they believe warrants defense,” Mr. Atchinson said in an interview. “When the medical treatment provided is within the appropriate standards, even though there may be claims or lawsuits, every one of those [cases] can be very expensive to defend.”
Other contributers to the increasing rates include the trend of high-dollar settlements and judgments, particularly in the hospital space, Mr. Atchinson noted. Such large payouts are generally tied to hospital and health system claims, but they still affect the broader medical liability insurance marketplace, he said.
Additionally, a growing number of medical liability tort reform measures enacted over the last 20 years are being eliminated, Mr. Atchinson said. In June 2019, the Kansas Supreme Court for instance, struck down the state’s cap on damages for noneconomic injuries in medical liability cases. In a 2017 ruling, the Pennsylvania Supreme Court changed the state’s statue of limitations for medical malpractice wrongful death claims from 2 years from the time of the patient’s injury to 2 years from the time of the patient’s death.
When legislatures change state laws and courts invalidate protections against nonmeritorious lawsuits, the actions can have serious consequences for physicians and companies operating in those states, Mr. Atchinson said.
“These [changes] will all ultimately work their way into the rates that physicians are paying,” he said.