User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


The QI pipeline supported by SHM’s Student Scholar Grant Program
As fall arrives, new interns are rapidly gaining clinical confidence, and residency recruitment season is ramping up. It’s also time to announce the opening of the SHM Student Hospitalist Scholar Grant Program applications; we are now recruiting our sixth group of scholars for the summer and longitudinal programs.
Since its creation in 2015, the grant has supported 23 students in this incredible opportunity to allow trainees to engage in scholarly work with guidance from a mentor to better understand the practice of hospital medicine and to further grow our robust pipeline.
The 2018-2019 cohort of scholars, Matthew Fallon, Philip Huang, and Erin Rainosek, just concluded their projects and are currently preparing their abstracts for submission for Hospital Medicine 2020, where there is a track for Early-Career Hospitalists. The projects targeted a diverse set of domains, including improving upon the patient experience, readmission quality metrics, geographic cohorting, and clinical documentation integrity – all highly relevant topics for a practicing hospitalist.
Matthew Fallon collaborated with his mentor, Dr. Venkata Andukuri, at Creighton University, to reduce the rate of hospital readmission for patients with heart failure, by analyzing retrospective data in a root cause analysis to identify factors that influence readmission rate, then targeting those directly. They also integrated the patient experience by seeking out patient input as to the challenges they face in the management of their heart failure.
Philip Huang worked with his mentor, Dr. Ethan Kuperman, at the Carver College of Medicine, University of Iowa, to improve geographic localization for hospitalized patients to improve care efficiency. They worked closely with an industrial engineering team to create a workflow model integrated into the hospital EHR to designate patient location and were able to better understand the role that other professions play in improving the health care delivery.
Finally, Erin Rainosek teamed up with her mentor, Dr. Luci Leykum, at the University of Texas Health Science Center at San Antonio, to apply a design thinking strategy to redesign the health care experience for hospitalized patients. She engaged in over 120 hours of patient interviews and ultimately identified key themes that impact the experience of care, which will serve as target areas moving forward.
The student scholars in this cohort gained significant insight into the patient experience and quality issues relevant to the field of hospital medicine. We are proud of their accomplishments and look forward to their future successes and careers in hospital medicine. If you would like to learn more about the experience of our scholars this past summer, they have posted full write-ups on the Future Hospitalist RoundUp blog in HMX, SHM’s online community.
For students interested in becoming scholars, SHM offers two options to eligible medical students – the Summer Program and the Longitudinal Program. Both programs allow students to participate in projects related to quality improvement, patient safety, clinical research or hospital operations, in order to learn more about career paths in hospital medicine. Students will have the opportunity to conduct scholarly work with a mentor in these domains, with the option of participating over the summer during a 6-10-week period or longitudinally throughout the course of a year.
Discover additional benefits and how to apply on the SHM website. Applications will close in late January 2020.
Dr. Gottenborg is director of the Hospitalist Training Program within the Internal Medicine Residency Program at the University of Colorado. Dr. Duckett is assistant professor of medicine at the Medical University of South Carolina.
As fall arrives, new interns are rapidly gaining clinical confidence, and residency recruitment season is ramping up. It’s also time to announce the opening of the SHM Student Hospitalist Scholar Grant Program applications; we are now recruiting our sixth group of scholars for the summer and longitudinal programs.
Since its creation in 2015, the grant has supported 23 students in this incredible opportunity to allow trainees to engage in scholarly work with guidance from a mentor to better understand the practice of hospital medicine and to further grow our robust pipeline.
The 2018-2019 cohort of scholars, Matthew Fallon, Philip Huang, and Erin Rainosek, just concluded their projects and are currently preparing their abstracts for submission for Hospital Medicine 2020, where there is a track for Early-Career Hospitalists. The projects targeted a diverse set of domains, including improving upon the patient experience, readmission quality metrics, geographic cohorting, and clinical documentation integrity – all highly relevant topics for a practicing hospitalist.
Matthew Fallon collaborated with his mentor, Dr. Venkata Andukuri, at Creighton University, to reduce the rate of hospital readmission for patients with heart failure, by analyzing retrospective data in a root cause analysis to identify factors that influence readmission rate, then targeting those directly. They also integrated the patient experience by seeking out patient input as to the challenges they face in the management of their heart failure.
Philip Huang worked with his mentor, Dr. Ethan Kuperman, at the Carver College of Medicine, University of Iowa, to improve geographic localization for hospitalized patients to improve care efficiency. They worked closely with an industrial engineering team to create a workflow model integrated into the hospital EHR to designate patient location and were able to better understand the role that other professions play in improving the health care delivery.
Finally, Erin Rainosek teamed up with her mentor, Dr. Luci Leykum, at the University of Texas Health Science Center at San Antonio, to apply a design thinking strategy to redesign the health care experience for hospitalized patients. She engaged in over 120 hours of patient interviews and ultimately identified key themes that impact the experience of care, which will serve as target areas moving forward.
The student scholars in this cohort gained significant insight into the patient experience and quality issues relevant to the field of hospital medicine. We are proud of their accomplishments and look forward to their future successes and careers in hospital medicine. If you would like to learn more about the experience of our scholars this past summer, they have posted full write-ups on the Future Hospitalist RoundUp blog in HMX, SHM’s online community.
For students interested in becoming scholars, SHM offers two options to eligible medical students – the Summer Program and the Longitudinal Program. Both programs allow students to participate in projects related to quality improvement, patient safety, clinical research or hospital operations, in order to learn more about career paths in hospital medicine. Students will have the opportunity to conduct scholarly work with a mentor in these domains, with the option of participating over the summer during a 6-10-week period or longitudinally throughout the course of a year.
Discover additional benefits and how to apply on the SHM website. Applications will close in late January 2020.
Dr. Gottenborg is director of the Hospitalist Training Program within the Internal Medicine Residency Program at the University of Colorado. Dr. Duckett is assistant professor of medicine at the Medical University of South Carolina.
As fall arrives, new interns are rapidly gaining clinical confidence, and residency recruitment season is ramping up. It’s also time to announce the opening of the SHM Student Hospitalist Scholar Grant Program applications; we are now recruiting our sixth group of scholars for the summer and longitudinal programs.
Since its creation in 2015, the grant has supported 23 students in this incredible opportunity to allow trainees to engage in scholarly work with guidance from a mentor to better understand the practice of hospital medicine and to further grow our robust pipeline.
The 2018-2019 cohort of scholars, Matthew Fallon, Philip Huang, and Erin Rainosek, just concluded their projects and are currently preparing their abstracts for submission for Hospital Medicine 2020, where there is a track for Early-Career Hospitalists. The projects targeted a diverse set of domains, including improving upon the patient experience, readmission quality metrics, geographic cohorting, and clinical documentation integrity – all highly relevant topics for a practicing hospitalist.
Matthew Fallon collaborated with his mentor, Dr. Venkata Andukuri, at Creighton University, to reduce the rate of hospital readmission for patients with heart failure, by analyzing retrospective data in a root cause analysis to identify factors that influence readmission rate, then targeting those directly. They also integrated the patient experience by seeking out patient input as to the challenges they face in the management of their heart failure.
Philip Huang worked with his mentor, Dr. Ethan Kuperman, at the Carver College of Medicine, University of Iowa, to improve geographic localization for hospitalized patients to improve care efficiency. They worked closely with an industrial engineering team to create a workflow model integrated into the hospital EHR to designate patient location and were able to better understand the role that other professions play in improving the health care delivery.
Finally, Erin Rainosek teamed up with her mentor, Dr. Luci Leykum, at the University of Texas Health Science Center at San Antonio, to apply a design thinking strategy to redesign the health care experience for hospitalized patients. She engaged in over 120 hours of patient interviews and ultimately identified key themes that impact the experience of care, which will serve as target areas moving forward.
The student scholars in this cohort gained significant insight into the patient experience and quality issues relevant to the field of hospital medicine. We are proud of their accomplishments and look forward to their future successes and careers in hospital medicine. If you would like to learn more about the experience of our scholars this past summer, they have posted full write-ups on the Future Hospitalist RoundUp blog in HMX, SHM’s online community.
For students interested in becoming scholars, SHM offers two options to eligible medical students – the Summer Program and the Longitudinal Program. Both programs allow students to participate in projects related to quality improvement, patient safety, clinical research or hospital operations, in order to learn more about career paths in hospital medicine. Students will have the opportunity to conduct scholarly work with a mentor in these domains, with the option of participating over the summer during a 6-10-week period or longitudinally throughout the course of a year.
Discover additional benefits and how to apply on the SHM website. Applications will close in late January 2020.
Dr. Gottenborg is director of the Hospitalist Training Program within the Internal Medicine Residency Program at the University of Colorado. Dr. Duckett is assistant professor of medicine at the Medical University of South Carolina.
Experts bring clarity to end of life difficulties
Understanding family perspective is an important factor
A Vietnam veteran steered clear of the health care system for years, then showed up at the hospital with pneumonia and respiratory failure. He was whisked to the intensive care unit, and cancerous masses were found.
The situation – as described by Jeffrey Frank, MD, director of quality and performance at Vituity, a physician group in Emeryville, Calif. – then got worse.
“No one was there for him,” Dr. Frank said. “He’s laying in the ICU, he does not have the capacity to make decisions, let alone communicate. So the care team needs guidance.”
Too often, hospitalists find themselves in confusing situations involving patients near the end of their lives, having to determine how to go about treating a patient or withholding treatment when patients are not in a position to announce their wishes. When family is present, the health care team thinks the most sensible course of treatment is at odds with what the family wants to be done.
At the Society of Hospital Medicine 2019 Annual Conference, hospitalists with palliative care training offered advice on how to go about handling these difficult situations, which can sometimes become more manageable with certain strategies.
For situations in which there is no designated representative to speak for a patient who is unresponsive – the so-called “unbefriended patient” or “unrepresented patient” – any source of information can be valuable. And health care providers should seek out this input, Dr. Frank said.
“When there is a visitor at the bedside, and as long as they know the person, and they can start giving the medical providers some information about what the patient would have wanted, most of us will talk with that person and that’s actually a good habit,” he said.
Thirty-nine states and the District of Columbia have regulations on whom health care providers should talk to when there is no obvious representative, Dr. Frank said, noting that most of these regulations follow a classic family-tree order. But in the discouraging results of many surveys of health care providers on the subject, most clinicians say that they do not know the regulations in their state, Dr. Frank said. But he said such results betray a silver lining because clinicians say that they would be inclined to use a family tree–style hierarchy in deciding with whom they should speak about end of life decisions.
Hospitalists should at least know whether their hospital has a policy on unrepresented patients, Dr. Frank said.
“That’s your road map on how to get through consenting this patient – what am I going to do with Mr. Smith?” he said. “You may ask yourself, ‘Do I just keep treating him and treating him?’ If you have a policy at your hospital, it will protect you from liability, as well as give you a sense of process.”
Conflicts in communication
An even worse situation, perhaps, is one that many hospitalists have seen: A patient is teetering at the edge of life, and a spouse arrives, along with two daughters from out of state who have not seen their father in a year, said Elizabeth Gundersen, MD, director of the ethics curriculum at Florida Atlantic University, Boca Raton.
“The family requests that the medical team do everything, including intubation and attempts at resuscitation if needed,” she said. “The family says he was fine prior to this admission. Another thing I hear a lot is, ‘He was even sicker than this last year, and he got better.’ ”
Meanwhile, “the medical team consensus is that he is not going to survive this illness,” Dr. Gundersen said.
The situation is so common and problematic that it has a name – the “Daughter from California Syndrome.” (According to medical literature says, it’s called the “Daughter from Chicago Syndrome” in California.)
“This is one of the most agonizing things that happens to us in medicine,” Dr. Gundersen said. “It affects us, it affects our nurses, it affects the entire medical team. It’s agonizing when we feel like treatment has somehow turned to torture.”
Dr. Gundersen said the medical staff should avoid using the word “futile,” or similar language, with families.
“Words matter,” she said. “Inappropriate language can inadvertently convey the feeling that, ‘They’re giving up on my dad – they think it’s hopeless.’ That can make families and the medical team dig in their heels further.”
Sometimes it can be hard to define the terms of decision making. Even if the family and the medical team can agree that no “nonbeneficial treatments” should be administered, Dr. Gundersen said, what exactly does that mean? Does it mean less than a 1% chance of working; less than a 5% chance?
If the medical staff thinks a mode of care won’t be effective, but the family still insists, some states have laws that could help the medical team. In Texas, for example, if the medical team thinks the care they’re giving isn’t helping the patient, and the patient is likely going to have a poor outcome, there’s a legal process that the team can go through, Dr. Gundersen said. But even these laws are seen as potentially problematic because of concerns that they put too much power in the hands of a hospital committee.
Dr. Gundersen strongly advised getting at the root causes of a family’s apprehension. They might not have been informed early enough about the dire nature of an illness to feel they can make a decision comfortably. They also may be receiving information in a piecemeal manner or information that is inconsistent. Another common fear expressed by families is a concern over abandonment by the medical team if a decision is made to forgo a certain treatment. Also, sometimes the goals of care might not be properly detailed and discussed, she said.
But better communication can help overcome these snags, Dr. Gundersen said.
She suggested that sometimes it’s helpful to clarify things with the family, for example, what do they mean by “Do everything”?
“Does it mean ‘I want you to do everything to prolong their life even if they suffer,’ or does it mean ‘I want you do to everything that’s reasonable to try to prolong their life but not at the risk of increased suffering,’ or anywhere in between. Really just having these clarifying conversations is helpful.”
She also emphasized the importance of talking about interests, such as not wanting a patient to suffer, instead of taking positions, such as flatly recommending the withdrawal of treatment.
“It’s easy for both sides to kind of dig in their heels and not communicate effectively,” Dr. Gundersen said.
‘Emotional torture’
There are times when, no matter how skillfully the medical team communicates, they stand at an impasse with the family.
“This is emotional torture for us,” Dr. Gundersen said. “It’s moral distress. We kind of dread these situations. In these cases, trying to support yourself and your team emotionally is the most important thing.”
Ami Doshi, MD, director of palliative care inpatient services at Rady Children’s Hospital in San Diego, described the case of a baby girl that touched on the especially painful issues that can arise in pediatric cases. The 2-month-old girl had been born after a pregnancy affected by polyhydramnios and had an abnormal neurological exam and brain MRI, as well as congenital abnormalities. She’d been intubated for respiratory failure and was now on high-flow nasal cannula therapy. The girl was intolerant to feeding and was put on a nasojejunal feeding tube and then a gastrostomy-jejunostomy tube.
But the baby’s vomiting continued, and she had bradycardia and hypoxia so severe she needed bag mask ventilation to recover. The mother started to feel like she was “torturing” the baby.
The family decided to stop respiratory support but to continue artificial nutrition and hydration, which Dr. Doshi said, has an elevated status in the human psyche. Mentioning discontinuing feeding is fraught with complexity, she said.
“The notion of feeding is such a basic instinct, especially with a baby, that tackling the notion of discontinuing any sort of feeds, orally or tube feeds, is fraught with emotion and angst at times,” Dr. Doshi said.
The girl had respiratory events but recovered from them on her own, but the vomiting and retching continued. Eventually the artificial nutrition and hydration was stopped. But after 5 days, the medical staff began feeling uncomfortable, Dr. Doshi said. “We’re starting to hear from nurses, doctors, other people, that something just doesn’t feel right about what’s happening: ‘She seems okay,’ and, ‘Is it really okay for us to be doing this?’ and ‘Gosh, this is taking a long time.’ ”
The medical staff had, in a sense, joined the family on the emotional roller coaster.
Dr. Doshi said it’s important to remember that there is no ethical or moral distinction between withdrawing a medical intervention and withholding one.
“Stopping an intervention once it has started is no different ethically or legally than not starting it in the first place,” she said.
According to Dr. Doshi, there is a general consensus among medical societies that artificial nutrition and hydration is a medical intervention just like any other and that it should be evaluated within the same framework: Is it overly burdensome? Are we doing harm? Is it consistent with the goal of care? In so doing, be sure to respect patient autonomy and obtain informed consent.
As with so much in medicine, careful communication is a must.
“Paint a picture of what the patient’s trajectory is going to look like with and without artificial nutrition and hydration. At the end of the day, having done all of that, we’re going to ultimately respect what the patient or the surrogate decision maker decides,” Dr. Doshi said.
After assessment the data and the chances of success, and still without clarity about how to proceed, a good option might be considering a “time-limited trial” in which the medical team sits with the family and agrees on a time frame for an intervention and chooses predetermined endpoints for assessing success or failure.
“This can be very powerful to help us understand whether it is beneficial, but also – from the family’s perspective – to know everything was tried,” Dr. Doshi said.
Hospitalists should emphasize what is being added to treatment so that families don’t think only of what is being taken away, she said.
“Usually we are adding a lot – symptom management, a lot of psychosocial support. So what are all the other ways that we’re going to continue to care for the patient, even when we are withdrawing or withholding a specific intervention?” Dr. Doshi noted.
Sometimes, the best healer of distress in the midst of end of life decision making is time itself, Dr. Gundersen said.
In a condolence call, she once spoke with a family member involved in an agonizing case in which the medical team and family were at odds. Yet the man told her: “I know that you all were telling us the entire time that this was going to happen, but I guess we just had to go through our own process.”
Understanding family perspective is an important factor
Understanding family perspective is an important factor
A Vietnam veteran steered clear of the health care system for years, then showed up at the hospital with pneumonia and respiratory failure. He was whisked to the intensive care unit, and cancerous masses were found.
The situation – as described by Jeffrey Frank, MD, director of quality and performance at Vituity, a physician group in Emeryville, Calif. – then got worse.
“No one was there for him,” Dr. Frank said. “He’s laying in the ICU, he does not have the capacity to make decisions, let alone communicate. So the care team needs guidance.”
Too often, hospitalists find themselves in confusing situations involving patients near the end of their lives, having to determine how to go about treating a patient or withholding treatment when patients are not in a position to announce their wishes. When family is present, the health care team thinks the most sensible course of treatment is at odds with what the family wants to be done.
At the Society of Hospital Medicine 2019 Annual Conference, hospitalists with palliative care training offered advice on how to go about handling these difficult situations, which can sometimes become more manageable with certain strategies.
For situations in which there is no designated representative to speak for a patient who is unresponsive – the so-called “unbefriended patient” or “unrepresented patient” – any source of information can be valuable. And health care providers should seek out this input, Dr. Frank said.
“When there is a visitor at the bedside, and as long as they know the person, and they can start giving the medical providers some information about what the patient would have wanted, most of us will talk with that person and that’s actually a good habit,” he said.
Thirty-nine states and the District of Columbia have regulations on whom health care providers should talk to when there is no obvious representative, Dr. Frank said, noting that most of these regulations follow a classic family-tree order. But in the discouraging results of many surveys of health care providers on the subject, most clinicians say that they do not know the regulations in their state, Dr. Frank said. But he said such results betray a silver lining because clinicians say that they would be inclined to use a family tree–style hierarchy in deciding with whom they should speak about end of life decisions.
Hospitalists should at least know whether their hospital has a policy on unrepresented patients, Dr. Frank said.
“That’s your road map on how to get through consenting this patient – what am I going to do with Mr. Smith?” he said. “You may ask yourself, ‘Do I just keep treating him and treating him?’ If you have a policy at your hospital, it will protect you from liability, as well as give you a sense of process.”
Conflicts in communication
An even worse situation, perhaps, is one that many hospitalists have seen: A patient is teetering at the edge of life, and a spouse arrives, along with two daughters from out of state who have not seen their father in a year, said Elizabeth Gundersen, MD, director of the ethics curriculum at Florida Atlantic University, Boca Raton.
“The family requests that the medical team do everything, including intubation and attempts at resuscitation if needed,” she said. “The family says he was fine prior to this admission. Another thing I hear a lot is, ‘He was even sicker than this last year, and he got better.’ ”
Meanwhile, “the medical team consensus is that he is not going to survive this illness,” Dr. Gundersen said.
The situation is so common and problematic that it has a name – the “Daughter from California Syndrome.” (According to medical literature says, it’s called the “Daughter from Chicago Syndrome” in California.)
“This is one of the most agonizing things that happens to us in medicine,” Dr. Gundersen said. “It affects us, it affects our nurses, it affects the entire medical team. It’s agonizing when we feel like treatment has somehow turned to torture.”
Dr. Gundersen said the medical staff should avoid using the word “futile,” or similar language, with families.
“Words matter,” she said. “Inappropriate language can inadvertently convey the feeling that, ‘They’re giving up on my dad – they think it’s hopeless.’ That can make families and the medical team dig in their heels further.”
Sometimes it can be hard to define the terms of decision making. Even if the family and the medical team can agree that no “nonbeneficial treatments” should be administered, Dr. Gundersen said, what exactly does that mean? Does it mean less than a 1% chance of working; less than a 5% chance?
If the medical staff thinks a mode of care won’t be effective, but the family still insists, some states have laws that could help the medical team. In Texas, for example, if the medical team thinks the care they’re giving isn’t helping the patient, and the patient is likely going to have a poor outcome, there’s a legal process that the team can go through, Dr. Gundersen said. But even these laws are seen as potentially problematic because of concerns that they put too much power in the hands of a hospital committee.
Dr. Gundersen strongly advised getting at the root causes of a family’s apprehension. They might not have been informed early enough about the dire nature of an illness to feel they can make a decision comfortably. They also may be receiving information in a piecemeal manner or information that is inconsistent. Another common fear expressed by families is a concern over abandonment by the medical team if a decision is made to forgo a certain treatment. Also, sometimes the goals of care might not be properly detailed and discussed, she said.
But better communication can help overcome these snags, Dr. Gundersen said.
She suggested that sometimes it’s helpful to clarify things with the family, for example, what do they mean by “Do everything”?
“Does it mean ‘I want you to do everything to prolong their life even if they suffer,’ or does it mean ‘I want you do to everything that’s reasonable to try to prolong their life but not at the risk of increased suffering,’ or anywhere in between. Really just having these clarifying conversations is helpful.”
She also emphasized the importance of talking about interests, such as not wanting a patient to suffer, instead of taking positions, such as flatly recommending the withdrawal of treatment.
“It’s easy for both sides to kind of dig in their heels and not communicate effectively,” Dr. Gundersen said.
‘Emotional torture’
There are times when, no matter how skillfully the medical team communicates, they stand at an impasse with the family.
“This is emotional torture for us,” Dr. Gundersen said. “It’s moral distress. We kind of dread these situations. In these cases, trying to support yourself and your team emotionally is the most important thing.”
Ami Doshi, MD, director of palliative care inpatient services at Rady Children’s Hospital in San Diego, described the case of a baby girl that touched on the especially painful issues that can arise in pediatric cases. The 2-month-old girl had been born after a pregnancy affected by polyhydramnios and had an abnormal neurological exam and brain MRI, as well as congenital abnormalities. She’d been intubated for respiratory failure and was now on high-flow nasal cannula therapy. The girl was intolerant to feeding and was put on a nasojejunal feeding tube and then a gastrostomy-jejunostomy tube.
But the baby’s vomiting continued, and she had bradycardia and hypoxia so severe she needed bag mask ventilation to recover. The mother started to feel like she was “torturing” the baby.
The family decided to stop respiratory support but to continue artificial nutrition and hydration, which Dr. Doshi said, has an elevated status in the human psyche. Mentioning discontinuing feeding is fraught with complexity, she said.
“The notion of feeding is such a basic instinct, especially with a baby, that tackling the notion of discontinuing any sort of feeds, orally or tube feeds, is fraught with emotion and angst at times,” Dr. Doshi said.
The girl had respiratory events but recovered from them on her own, but the vomiting and retching continued. Eventually the artificial nutrition and hydration was stopped. But after 5 days, the medical staff began feeling uncomfortable, Dr. Doshi said. “We’re starting to hear from nurses, doctors, other people, that something just doesn’t feel right about what’s happening: ‘She seems okay,’ and, ‘Is it really okay for us to be doing this?’ and ‘Gosh, this is taking a long time.’ ”
The medical staff had, in a sense, joined the family on the emotional roller coaster.
Dr. Doshi said it’s important to remember that there is no ethical or moral distinction between withdrawing a medical intervention and withholding one.
“Stopping an intervention once it has started is no different ethically or legally than not starting it in the first place,” she said.
According to Dr. Doshi, there is a general consensus among medical societies that artificial nutrition and hydration is a medical intervention just like any other and that it should be evaluated within the same framework: Is it overly burdensome? Are we doing harm? Is it consistent with the goal of care? In so doing, be sure to respect patient autonomy and obtain informed consent.
As with so much in medicine, careful communication is a must.
“Paint a picture of what the patient’s trajectory is going to look like with and without artificial nutrition and hydration. At the end of the day, having done all of that, we’re going to ultimately respect what the patient or the surrogate decision maker decides,” Dr. Doshi said.
After assessment the data and the chances of success, and still without clarity about how to proceed, a good option might be considering a “time-limited trial” in which the medical team sits with the family and agrees on a time frame for an intervention and chooses predetermined endpoints for assessing success or failure.
“This can be very powerful to help us understand whether it is beneficial, but also – from the family’s perspective – to know everything was tried,” Dr. Doshi said.
Hospitalists should emphasize what is being added to treatment so that families don’t think only of what is being taken away, she said.
“Usually we are adding a lot – symptom management, a lot of psychosocial support. So what are all the other ways that we’re going to continue to care for the patient, even when we are withdrawing or withholding a specific intervention?” Dr. Doshi noted.
Sometimes, the best healer of distress in the midst of end of life decision making is time itself, Dr. Gundersen said.
In a condolence call, she once spoke with a family member involved in an agonizing case in which the medical team and family were at odds. Yet the man told her: “I know that you all were telling us the entire time that this was going to happen, but I guess we just had to go through our own process.”
A Vietnam veteran steered clear of the health care system for years, then showed up at the hospital with pneumonia and respiratory failure. He was whisked to the intensive care unit, and cancerous masses were found.
The situation – as described by Jeffrey Frank, MD, director of quality and performance at Vituity, a physician group in Emeryville, Calif. – then got worse.
“No one was there for him,” Dr. Frank said. “He’s laying in the ICU, he does not have the capacity to make decisions, let alone communicate. So the care team needs guidance.”
Too often, hospitalists find themselves in confusing situations involving patients near the end of their lives, having to determine how to go about treating a patient or withholding treatment when patients are not in a position to announce their wishes. When family is present, the health care team thinks the most sensible course of treatment is at odds with what the family wants to be done.
At the Society of Hospital Medicine 2019 Annual Conference, hospitalists with palliative care training offered advice on how to go about handling these difficult situations, which can sometimes become more manageable with certain strategies.
For situations in which there is no designated representative to speak for a patient who is unresponsive – the so-called “unbefriended patient” or “unrepresented patient” – any source of information can be valuable. And health care providers should seek out this input, Dr. Frank said.
“When there is a visitor at the bedside, and as long as they know the person, and they can start giving the medical providers some information about what the patient would have wanted, most of us will talk with that person and that’s actually a good habit,” he said.
Thirty-nine states and the District of Columbia have regulations on whom health care providers should talk to when there is no obvious representative, Dr. Frank said, noting that most of these regulations follow a classic family-tree order. But in the discouraging results of many surveys of health care providers on the subject, most clinicians say that they do not know the regulations in their state, Dr. Frank said. But he said such results betray a silver lining because clinicians say that they would be inclined to use a family tree–style hierarchy in deciding with whom they should speak about end of life decisions.
Hospitalists should at least know whether their hospital has a policy on unrepresented patients, Dr. Frank said.
“That’s your road map on how to get through consenting this patient – what am I going to do with Mr. Smith?” he said. “You may ask yourself, ‘Do I just keep treating him and treating him?’ If you have a policy at your hospital, it will protect you from liability, as well as give you a sense of process.”
Conflicts in communication
An even worse situation, perhaps, is one that many hospitalists have seen: A patient is teetering at the edge of life, and a spouse arrives, along with two daughters from out of state who have not seen their father in a year, said Elizabeth Gundersen, MD, director of the ethics curriculum at Florida Atlantic University, Boca Raton.
“The family requests that the medical team do everything, including intubation and attempts at resuscitation if needed,” she said. “The family says he was fine prior to this admission. Another thing I hear a lot is, ‘He was even sicker than this last year, and he got better.’ ”
Meanwhile, “the medical team consensus is that he is not going to survive this illness,” Dr. Gundersen said.
The situation is so common and problematic that it has a name – the “Daughter from California Syndrome.” (According to medical literature says, it’s called the “Daughter from Chicago Syndrome” in California.)
“This is one of the most agonizing things that happens to us in medicine,” Dr. Gundersen said. “It affects us, it affects our nurses, it affects the entire medical team. It’s agonizing when we feel like treatment has somehow turned to torture.”
Dr. Gundersen said the medical staff should avoid using the word “futile,” or similar language, with families.
“Words matter,” she said. “Inappropriate language can inadvertently convey the feeling that, ‘They’re giving up on my dad – they think it’s hopeless.’ That can make families and the medical team dig in their heels further.”
Sometimes it can be hard to define the terms of decision making. Even if the family and the medical team can agree that no “nonbeneficial treatments” should be administered, Dr. Gundersen said, what exactly does that mean? Does it mean less than a 1% chance of working; less than a 5% chance?
If the medical staff thinks a mode of care won’t be effective, but the family still insists, some states have laws that could help the medical team. In Texas, for example, if the medical team thinks the care they’re giving isn’t helping the patient, and the patient is likely going to have a poor outcome, there’s a legal process that the team can go through, Dr. Gundersen said. But even these laws are seen as potentially problematic because of concerns that they put too much power in the hands of a hospital committee.
Dr. Gundersen strongly advised getting at the root causes of a family’s apprehension. They might not have been informed early enough about the dire nature of an illness to feel they can make a decision comfortably. They also may be receiving information in a piecemeal manner or information that is inconsistent. Another common fear expressed by families is a concern over abandonment by the medical team if a decision is made to forgo a certain treatment. Also, sometimes the goals of care might not be properly detailed and discussed, she said.
But better communication can help overcome these snags, Dr. Gundersen said.
She suggested that sometimes it’s helpful to clarify things with the family, for example, what do they mean by “Do everything”?
“Does it mean ‘I want you to do everything to prolong their life even if they suffer,’ or does it mean ‘I want you do to everything that’s reasonable to try to prolong their life but not at the risk of increased suffering,’ or anywhere in between. Really just having these clarifying conversations is helpful.”
She also emphasized the importance of talking about interests, such as not wanting a patient to suffer, instead of taking positions, such as flatly recommending the withdrawal of treatment.
“It’s easy for both sides to kind of dig in their heels and not communicate effectively,” Dr. Gundersen said.
‘Emotional torture’
There are times when, no matter how skillfully the medical team communicates, they stand at an impasse with the family.
“This is emotional torture for us,” Dr. Gundersen said. “It’s moral distress. We kind of dread these situations. In these cases, trying to support yourself and your team emotionally is the most important thing.”
Ami Doshi, MD, director of palliative care inpatient services at Rady Children’s Hospital in San Diego, described the case of a baby girl that touched on the especially painful issues that can arise in pediatric cases. The 2-month-old girl had been born after a pregnancy affected by polyhydramnios and had an abnormal neurological exam and brain MRI, as well as congenital abnormalities. She’d been intubated for respiratory failure and was now on high-flow nasal cannula therapy. The girl was intolerant to feeding and was put on a nasojejunal feeding tube and then a gastrostomy-jejunostomy tube.
But the baby’s vomiting continued, and she had bradycardia and hypoxia so severe she needed bag mask ventilation to recover. The mother started to feel like she was “torturing” the baby.
The family decided to stop respiratory support but to continue artificial nutrition and hydration, which Dr. Doshi said, has an elevated status in the human psyche. Mentioning discontinuing feeding is fraught with complexity, she said.
“The notion of feeding is such a basic instinct, especially with a baby, that tackling the notion of discontinuing any sort of feeds, orally or tube feeds, is fraught with emotion and angst at times,” Dr. Doshi said.
The girl had respiratory events but recovered from them on her own, but the vomiting and retching continued. Eventually the artificial nutrition and hydration was stopped. But after 5 days, the medical staff began feeling uncomfortable, Dr. Doshi said. “We’re starting to hear from nurses, doctors, other people, that something just doesn’t feel right about what’s happening: ‘She seems okay,’ and, ‘Is it really okay for us to be doing this?’ and ‘Gosh, this is taking a long time.’ ”
The medical staff had, in a sense, joined the family on the emotional roller coaster.
Dr. Doshi said it’s important to remember that there is no ethical or moral distinction between withdrawing a medical intervention and withholding one.
“Stopping an intervention once it has started is no different ethically or legally than not starting it in the first place,” she said.
According to Dr. Doshi, there is a general consensus among medical societies that artificial nutrition and hydration is a medical intervention just like any other and that it should be evaluated within the same framework: Is it overly burdensome? Are we doing harm? Is it consistent with the goal of care? In so doing, be sure to respect patient autonomy and obtain informed consent.
As with so much in medicine, careful communication is a must.
“Paint a picture of what the patient’s trajectory is going to look like with and without artificial nutrition and hydration. At the end of the day, having done all of that, we’re going to ultimately respect what the patient or the surrogate decision maker decides,” Dr. Doshi said.
After assessment the data and the chances of success, and still without clarity about how to proceed, a good option might be considering a “time-limited trial” in which the medical team sits with the family and agrees on a time frame for an intervention and chooses predetermined endpoints for assessing success or failure.
“This can be very powerful to help us understand whether it is beneficial, but also – from the family’s perspective – to know everything was tried,” Dr. Doshi said.
Hospitalists should emphasize what is being added to treatment so that families don’t think only of what is being taken away, she said.
“Usually we are adding a lot – symptom management, a lot of psychosocial support. So what are all the other ways that we’re going to continue to care for the patient, even when we are withdrawing or withholding a specific intervention?” Dr. Doshi noted.
Sometimes, the best healer of distress in the midst of end of life decision making is time itself, Dr. Gundersen said.
In a condolence call, she once spoke with a family member involved in an agonizing case in which the medical team and family were at odds. Yet the man told her: “I know that you all were telling us the entire time that this was going to happen, but I guess we just had to go through our own process.”
Gunshot wound victims are at high risk for readmission
CHICAGO –
A study of individuals at a single institution who were hospitalized and had a prior history of gunshot wound found some patterns of injury that set patients up for a greater likelihood of readmission.
In particular, patients who sustained visceral gunshot wounds were over six times more likely to be readmitted to the hospital, Corbin Pomeranz, MD, a radiology resident at Thomas Jefferson University, Philadelphia, said in an interview at the annual meeting of the Radiological Society of North America. Dr. Pomeranz led the retrospective study that begins to fill a knowledge gap about what happens over the long term to those who sustain gunshot wounds.
“There continues to be profound lack of substantial information related to gun violence, particularly in predicting long-term outcomes,” Dr. Pomeranz and coauthors wrote in the abstract accompanying the presentation.
The researchers performed a single-site retrospective analysis over 3 months in 2018, tapping into an imaging database and looking for inpatient imaging exams that were nonacute, but related to gunshot wounds. From this information, the researchers went back to the original gunshot wound injury imaging, and recorded the pattern of injury, classifying wounds as neurologic, vascular, visceral, musculoskeletal, or involving multiple systems.
The investigators were able to glean additional information including the initial admitting hospital unit, information about interval admissions or surgeries, and demographic data. Regarding the nature of the gunshot injury itself, Dr. Pomeranz and coauthors went back to the earlier imaging studies to note bullet morphology, recording whether the bullet was intact, deformed, or had splintered into shrapnel within injured tissues.
In all, 174 imaging studies involving 110 patients were examined. Men made up 92% of the study population; the average age was 49.7 years. Neurologic and visceral gunshot wounds were moderately correlated with subsequent readmission (r = .436; P less than .001). However, some of this effect was blunted when patient age was controlled for in the statistical analysis.
Patients who were initially admitted to the intensive care unit, and who presumably had more severe injuries, were also more likely to be readmitted (r = .494, P less than .001). Here, “controlling for age had very little effect on the strength of the relationship between these two variables,” noted Dr. Pomeranz and coauthors.
A more elaborate statistical model incorporated several independent variables including age, type of injury, and body region involved, as well as bullet morphology. In this model, visceral injury was the strongest predictor for readmission, with an odds ratio of 6.44.
Dr. Pomeranz said that both the initial gunshot wound and subsequent gaps in care can contribute to readmissions. A patient who has a spinal cord injury may not be reimbursed adequately for supportive cushioning, or an appropriate wheelchair, and so may require admission for decubitus ulcers.
The number of admissions for osteomyelitis, which made up more than half of the subsequent admissions, initially surprised Dr. Pomeranz, until he realized that lack of mobility and sensory losses from gunshot-induced spinal cord injuries could easily lead to nonhealing lower extremity wounds, with osteomyelitis as a sequela.
Several patients were admitted for small bowel obstructions with no interval surgery since treatment for the gunshot wound. These readmissions, said Dr. Pomeranz, were assessed as related to the gunshot wound since it’s extremely rare for a patient with no history of abdominal surgery and no malignancy to have a small bowel obstruction. Exploratory laparotomies are common in the context of abdominal trauma caused by gunshot wounds, and either the gunshot itself or the laparotomy was the likely cause of adhesions.
Dr. Pomeranz acknowledged the many limitations of the study, but pointed out that some will be addressed when he and his coauthors conduct a larger study they have planned to look at readmissions from gunshot wounds at multiple hospitals in the Philadelphia area. The small sample size in the current study meant that the impact of socioeconomic status and other lifestyle and social variables and comorbidities couldn’t be adequately addressed in the statistical analysis. By casting a wider net within the greater Philadelphia area, the investigators should be able to track patients who receive care in more than one hospital system, increasing participant numbers, he said.
“Morbidity and outcomes from gun violence can only be assessed after a firm understanding of injury patterns on imaging,” noted Dr. Pomeranz. He said that interdisciplinary research investigating individual and societal short- and long-term costs of gun violence is sorely needed to inform public policy.
Dr. Pomeranz reported no outside sources of funding and reported that he had no conflicts of interest.
SOURCE: Pomeranz C et al. RSNA 2019, Presentation HP226-SD-THA3.
CHICAGO –
A study of individuals at a single institution who were hospitalized and had a prior history of gunshot wound found some patterns of injury that set patients up for a greater likelihood of readmission.
In particular, patients who sustained visceral gunshot wounds were over six times more likely to be readmitted to the hospital, Corbin Pomeranz, MD, a radiology resident at Thomas Jefferson University, Philadelphia, said in an interview at the annual meeting of the Radiological Society of North America. Dr. Pomeranz led the retrospective study that begins to fill a knowledge gap about what happens over the long term to those who sustain gunshot wounds.
“There continues to be profound lack of substantial information related to gun violence, particularly in predicting long-term outcomes,” Dr. Pomeranz and coauthors wrote in the abstract accompanying the presentation.
The researchers performed a single-site retrospective analysis over 3 months in 2018, tapping into an imaging database and looking for inpatient imaging exams that were nonacute, but related to gunshot wounds. From this information, the researchers went back to the original gunshot wound injury imaging, and recorded the pattern of injury, classifying wounds as neurologic, vascular, visceral, musculoskeletal, or involving multiple systems.
The investigators were able to glean additional information including the initial admitting hospital unit, information about interval admissions or surgeries, and demographic data. Regarding the nature of the gunshot injury itself, Dr. Pomeranz and coauthors went back to the earlier imaging studies to note bullet morphology, recording whether the bullet was intact, deformed, or had splintered into shrapnel within injured tissues.
In all, 174 imaging studies involving 110 patients were examined. Men made up 92% of the study population; the average age was 49.7 years. Neurologic and visceral gunshot wounds were moderately correlated with subsequent readmission (r = .436; P less than .001). However, some of this effect was blunted when patient age was controlled for in the statistical analysis.
Patients who were initially admitted to the intensive care unit, and who presumably had more severe injuries, were also more likely to be readmitted (r = .494, P less than .001). Here, “controlling for age had very little effect on the strength of the relationship between these two variables,” noted Dr. Pomeranz and coauthors.
A more elaborate statistical model incorporated several independent variables including age, type of injury, and body region involved, as well as bullet morphology. In this model, visceral injury was the strongest predictor for readmission, with an odds ratio of 6.44.
Dr. Pomeranz said that both the initial gunshot wound and subsequent gaps in care can contribute to readmissions. A patient who has a spinal cord injury may not be reimbursed adequately for supportive cushioning, or an appropriate wheelchair, and so may require admission for decubitus ulcers.
The number of admissions for osteomyelitis, which made up more than half of the subsequent admissions, initially surprised Dr. Pomeranz, until he realized that lack of mobility and sensory losses from gunshot-induced spinal cord injuries could easily lead to nonhealing lower extremity wounds, with osteomyelitis as a sequela.
Several patients were admitted for small bowel obstructions with no interval surgery since treatment for the gunshot wound. These readmissions, said Dr. Pomeranz, were assessed as related to the gunshot wound since it’s extremely rare for a patient with no history of abdominal surgery and no malignancy to have a small bowel obstruction. Exploratory laparotomies are common in the context of abdominal trauma caused by gunshot wounds, and either the gunshot itself or the laparotomy was the likely cause of adhesions.
Dr. Pomeranz acknowledged the many limitations of the study, but pointed out that some will be addressed when he and his coauthors conduct a larger study they have planned to look at readmissions from gunshot wounds at multiple hospitals in the Philadelphia area. The small sample size in the current study meant that the impact of socioeconomic status and other lifestyle and social variables and comorbidities couldn’t be adequately addressed in the statistical analysis. By casting a wider net within the greater Philadelphia area, the investigators should be able to track patients who receive care in more than one hospital system, increasing participant numbers, he said.
“Morbidity and outcomes from gun violence can only be assessed after a firm understanding of injury patterns on imaging,” noted Dr. Pomeranz. He said that interdisciplinary research investigating individual and societal short- and long-term costs of gun violence is sorely needed to inform public policy.
Dr. Pomeranz reported no outside sources of funding and reported that he had no conflicts of interest.
SOURCE: Pomeranz C et al. RSNA 2019, Presentation HP226-SD-THA3.
CHICAGO –
A study of individuals at a single institution who were hospitalized and had a prior history of gunshot wound found some patterns of injury that set patients up for a greater likelihood of readmission.
In particular, patients who sustained visceral gunshot wounds were over six times more likely to be readmitted to the hospital, Corbin Pomeranz, MD, a radiology resident at Thomas Jefferson University, Philadelphia, said in an interview at the annual meeting of the Radiological Society of North America. Dr. Pomeranz led the retrospective study that begins to fill a knowledge gap about what happens over the long term to those who sustain gunshot wounds.
“There continues to be profound lack of substantial information related to gun violence, particularly in predicting long-term outcomes,” Dr. Pomeranz and coauthors wrote in the abstract accompanying the presentation.
The researchers performed a single-site retrospective analysis over 3 months in 2018, tapping into an imaging database and looking for inpatient imaging exams that were nonacute, but related to gunshot wounds. From this information, the researchers went back to the original gunshot wound injury imaging, and recorded the pattern of injury, classifying wounds as neurologic, vascular, visceral, musculoskeletal, or involving multiple systems.
The investigators were able to glean additional information including the initial admitting hospital unit, information about interval admissions or surgeries, and demographic data. Regarding the nature of the gunshot injury itself, Dr. Pomeranz and coauthors went back to the earlier imaging studies to note bullet morphology, recording whether the bullet was intact, deformed, or had splintered into shrapnel within injured tissues.
In all, 174 imaging studies involving 110 patients were examined. Men made up 92% of the study population; the average age was 49.7 years. Neurologic and visceral gunshot wounds were moderately correlated with subsequent readmission (r = .436; P less than .001). However, some of this effect was blunted when patient age was controlled for in the statistical analysis.
Patients who were initially admitted to the intensive care unit, and who presumably had more severe injuries, were also more likely to be readmitted (r = .494, P less than .001). Here, “controlling for age had very little effect on the strength of the relationship between these two variables,” noted Dr. Pomeranz and coauthors.
A more elaborate statistical model incorporated several independent variables including age, type of injury, and body region involved, as well as bullet morphology. In this model, visceral injury was the strongest predictor for readmission, with an odds ratio of 6.44.
Dr. Pomeranz said that both the initial gunshot wound and subsequent gaps in care can contribute to readmissions. A patient who has a spinal cord injury may not be reimbursed adequately for supportive cushioning, or an appropriate wheelchair, and so may require admission for decubitus ulcers.
The number of admissions for osteomyelitis, which made up more than half of the subsequent admissions, initially surprised Dr. Pomeranz, until he realized that lack of mobility and sensory losses from gunshot-induced spinal cord injuries could easily lead to nonhealing lower extremity wounds, with osteomyelitis as a sequela.
Several patients were admitted for small bowel obstructions with no interval surgery since treatment for the gunshot wound. These readmissions, said Dr. Pomeranz, were assessed as related to the gunshot wound since it’s extremely rare for a patient with no history of abdominal surgery and no malignancy to have a small bowel obstruction. Exploratory laparotomies are common in the context of abdominal trauma caused by gunshot wounds, and either the gunshot itself or the laparotomy was the likely cause of adhesions.
Dr. Pomeranz acknowledged the many limitations of the study, but pointed out that some will be addressed when he and his coauthors conduct a larger study they have planned to look at readmissions from gunshot wounds at multiple hospitals in the Philadelphia area. The small sample size in the current study meant that the impact of socioeconomic status and other lifestyle and social variables and comorbidities couldn’t be adequately addressed in the statistical analysis. By casting a wider net within the greater Philadelphia area, the investigators should be able to track patients who receive care in more than one hospital system, increasing participant numbers, he said.
“Morbidity and outcomes from gun violence can only be assessed after a firm understanding of injury patterns on imaging,” noted Dr. Pomeranz. He said that interdisciplinary research investigating individual and societal short- and long-term costs of gun violence is sorely needed to inform public policy.
Dr. Pomeranz reported no outside sources of funding and reported that he had no conflicts of interest.
SOURCE: Pomeranz C et al. RSNA 2019, Presentation HP226-SD-THA3.
REPORTING FROM RSNA 2019
Quantifying the EHR connection to burnout
While plenty of anecdotal and other evidence exists to connect the use of electronic health records to physician burnout, new research puts a more standard, quantifiable measure to it in an effort to help measure progress in improving the usability of EHRs.
Researchers used the System Usability Scale (SUS), “favored as an industry standard as a short, simple, and reliable measurement of technology usability with solid benchmarks to easily interpret its results, as the measure in this research, Edward Melnick, MD, of Yale University, New Haven, Conn., and colleagues wrote in Mayo Clinic Proceedings.
“The previous studies have definitely hinted at [the link between EHRs and burnout], but never really quantified it,” Dr. Melnick said in an interview.
Among the 870 physicians evaluating their EHRs’ usability, the mean score on a scale of 0-100 (higher being more usable) was 45.9. As a point of comparison, Microsoft Excel has an SUS score of 57, digital video recorders score 74, Amazon scores 82, microwave ovens score 87, and Google search scores 93.
“A score of 45.9 is in the bottom 9% of usability scores across studies in other industries and is categorized as in the ‘not acceptable’ range with a grade of F,” the authors wrote. “In aggregate, 733 of 870 (84.2%) of respondents rated their EHR less than 68 on the SUS, the average score across industries.”
In tying the SUS results to burnout, which was measured using the Maslach Burnout Inventory, the authors noted that the scores “were strongly and independently associated with physician burnout in a dose-response relationship. The odds of burnout were lower for each 1 point more favorable SUS score, a finding that persisted after adjusting for an extensive array of other personal and professional characteristics. The relationship between SUS score and burnout also persisted when emotional exhaustion and depersonalization were treated as continuous variables.”
The authors did note that, despite the strong relationship, they could not determine a causation given the cross-sectional nature of the data.
“I’m hoping that this paper will spark conversation and drive change and be a way of tracking improvements,” Dr. Melnick said. “So, if you bring in something new and say this is going to be better, how do you know it is going to be better? Well maybe you measure it using the System Usability Scale” to give it a quantifiable measure of improvement. He said it is an advantage “of having a metric that has been standardized and used in other industries,” allowing EHR stakeholders to measure improvement. “Once you can measure it, you can manage it and make improvements faster.”
The findings “will not come as a surprise to anyone who practices medicine,” Patrice Harris, MD, president of the American Medical Association, said in a statement. “It is a national imperative to overhaul the design and use of EHRs and reframe the technology to focus primarily on its most critical function: helping physicians care for patients. Significantly enhancing EHR usability is key and the AMA is working to ensure a new generation of EHRs are designed to prioritize time with patients, rather than overload physicians with type-and-click tasks.”
Funding for the study was provided by the Stanford Medicine WebMD Center, AMA, and the Mayo Clinic Department of Medicine Program on Physician Well-Being. No conflicts of interest were reported by the authors.
SOURCE: Melnick E et al. Mayo Clinic Proceedings 2019 Nov 14. doi: 10.1016/j.mayocp.2019.09.024.
While plenty of anecdotal and other evidence exists to connect the use of electronic health records to physician burnout, new research puts a more standard, quantifiable measure to it in an effort to help measure progress in improving the usability of EHRs.
Researchers used the System Usability Scale (SUS), “favored as an industry standard as a short, simple, and reliable measurement of technology usability with solid benchmarks to easily interpret its results, as the measure in this research, Edward Melnick, MD, of Yale University, New Haven, Conn., and colleagues wrote in Mayo Clinic Proceedings.
“The previous studies have definitely hinted at [the link between EHRs and burnout], but never really quantified it,” Dr. Melnick said in an interview.
Among the 870 physicians evaluating their EHRs’ usability, the mean score on a scale of 0-100 (higher being more usable) was 45.9. As a point of comparison, Microsoft Excel has an SUS score of 57, digital video recorders score 74, Amazon scores 82, microwave ovens score 87, and Google search scores 93.
“A score of 45.9 is in the bottom 9% of usability scores across studies in other industries and is categorized as in the ‘not acceptable’ range with a grade of F,” the authors wrote. “In aggregate, 733 of 870 (84.2%) of respondents rated their EHR less than 68 on the SUS, the average score across industries.”
In tying the SUS results to burnout, which was measured using the Maslach Burnout Inventory, the authors noted that the scores “were strongly and independently associated with physician burnout in a dose-response relationship. The odds of burnout were lower for each 1 point more favorable SUS score, a finding that persisted after adjusting for an extensive array of other personal and professional characteristics. The relationship between SUS score and burnout also persisted when emotional exhaustion and depersonalization were treated as continuous variables.”
The authors did note that, despite the strong relationship, they could not determine a causation given the cross-sectional nature of the data.
“I’m hoping that this paper will spark conversation and drive change and be a way of tracking improvements,” Dr. Melnick said. “So, if you bring in something new and say this is going to be better, how do you know it is going to be better? Well maybe you measure it using the System Usability Scale” to give it a quantifiable measure of improvement. He said it is an advantage “of having a metric that has been standardized and used in other industries,” allowing EHR stakeholders to measure improvement. “Once you can measure it, you can manage it and make improvements faster.”
The findings “will not come as a surprise to anyone who practices medicine,” Patrice Harris, MD, president of the American Medical Association, said in a statement. “It is a national imperative to overhaul the design and use of EHRs and reframe the technology to focus primarily on its most critical function: helping physicians care for patients. Significantly enhancing EHR usability is key and the AMA is working to ensure a new generation of EHRs are designed to prioritize time with patients, rather than overload physicians with type-and-click tasks.”
Funding for the study was provided by the Stanford Medicine WebMD Center, AMA, and the Mayo Clinic Department of Medicine Program on Physician Well-Being. No conflicts of interest were reported by the authors.
SOURCE: Melnick E et al. Mayo Clinic Proceedings 2019 Nov 14. doi: 10.1016/j.mayocp.2019.09.024.
While plenty of anecdotal and other evidence exists to connect the use of electronic health records to physician burnout, new research puts a more standard, quantifiable measure to it in an effort to help measure progress in improving the usability of EHRs.
Researchers used the System Usability Scale (SUS), “favored as an industry standard as a short, simple, and reliable measurement of technology usability with solid benchmarks to easily interpret its results, as the measure in this research, Edward Melnick, MD, of Yale University, New Haven, Conn., and colleagues wrote in Mayo Clinic Proceedings.
“The previous studies have definitely hinted at [the link between EHRs and burnout], but never really quantified it,” Dr. Melnick said in an interview.
Among the 870 physicians evaluating their EHRs’ usability, the mean score on a scale of 0-100 (higher being more usable) was 45.9. As a point of comparison, Microsoft Excel has an SUS score of 57, digital video recorders score 74, Amazon scores 82, microwave ovens score 87, and Google search scores 93.
“A score of 45.9 is in the bottom 9% of usability scores across studies in other industries and is categorized as in the ‘not acceptable’ range with a grade of F,” the authors wrote. “In aggregate, 733 of 870 (84.2%) of respondents rated their EHR less than 68 on the SUS, the average score across industries.”
In tying the SUS results to burnout, which was measured using the Maslach Burnout Inventory, the authors noted that the scores “were strongly and independently associated with physician burnout in a dose-response relationship. The odds of burnout were lower for each 1 point more favorable SUS score, a finding that persisted after adjusting for an extensive array of other personal and professional characteristics. The relationship between SUS score and burnout also persisted when emotional exhaustion and depersonalization were treated as continuous variables.”
The authors did note that, despite the strong relationship, they could not determine a causation given the cross-sectional nature of the data.
“I’m hoping that this paper will spark conversation and drive change and be a way of tracking improvements,” Dr. Melnick said. “So, if you bring in something new and say this is going to be better, how do you know it is going to be better? Well maybe you measure it using the System Usability Scale” to give it a quantifiable measure of improvement. He said it is an advantage “of having a metric that has been standardized and used in other industries,” allowing EHR stakeholders to measure improvement. “Once you can measure it, you can manage it and make improvements faster.”
The findings “will not come as a surprise to anyone who practices medicine,” Patrice Harris, MD, president of the American Medical Association, said in a statement. “It is a national imperative to overhaul the design and use of EHRs and reframe the technology to focus primarily on its most critical function: helping physicians care for patients. Significantly enhancing EHR usability is key and the AMA is working to ensure a new generation of EHRs are designed to prioritize time with patients, rather than overload physicians with type-and-click tasks.”
Funding for the study was provided by the Stanford Medicine WebMD Center, AMA, and the Mayo Clinic Department of Medicine Program on Physician Well-Being. No conflicts of interest were reported by the authors.
SOURCE: Melnick E et al. Mayo Clinic Proceedings 2019 Nov 14. doi: 10.1016/j.mayocp.2019.09.024.
FROM MAYO CLINIC PROCEEDINGS
Have lower readmission rates led to higher mortality for patients with COPD?
Be careful what you wish for
There is at least one aspect of “Obamacare” that my mother-in-law and I can firmly agree on: Hospitals should not get paid for frequent readmissions.
The Hospital Readmission Reduction Program (HRRP), enacted by the Centers for Medicare & Medicaid Services in 2012 with the goal of penalizing hospitals for excessive readmissions, has great face validity – and noble intentions. Does it also have a potentially disastrous downside?
On one side of the coin, the HRRP has been a remarkable success. It moved the national needle significantly on readmission rates. Yes, there are some caveats about increases in observation status patients and other shifts that could account for some of the difference, but it is fairly uncontroversial that overall, there are fewer 30-day readmissions across the country following initiation of HRRP. That is perhaps encouraging evidence of the potential positive impact that policy can make to drive changes for specific targets.
However, there is also a murkier – and more controversial – side. There have been a number of studies that have suggested reductions in readmission rates may have been associated with an increase in mortality in some patient groups. You discharge a patient and hope they won’t return to the hospital, but perhaps you should be more careful what you actually wish for.
Overall, the evidence of an association between readmissions and mortality has been complicated and conflicting. Headlines have alternately raised alarm about increased deaths and then reassured that there has been no change or perhaps even some concordant improvements in mortality. Not necessarily surprising, considering that these studies are all unavoidably of observational design and use different criteria, datasets and analytic models, which then drive their seemingly conflicting results.
An article published recently in the Journal of Hospital Medicine enters into this fray. The researchers examined the potential association between changes in rates of chronic obstructive pulmonary disease (COPD) readmissions and 30-day mortality following HRRP introduction. While the initial HRRP program and subsequent analyses included patients with heart failure, acute MI, and pneumonia, the program was extended in 2014 to include patients with COPD. So, what happened in this patient group?
Through a number of statistical gymnastics, which as a nonstatistician I am having difficulty truly wrapping my head around, the researchers seem to have found a number of important insights:
- The all-cause 30-day risk-standardized readmission rate declined from 2010 to 2017.
- The all-cause 30-day risk-standardized mortality rate increased from 2010 to 2017, and the rate of increase in mortality appears to be accelerating.
- Hospitals with higher readmission rates prior to COPD readmission penalties had a lower rate of increase in mortalities.
- Hospitals that had a larger decrease in readmission rates had a larger rate of increase in mortality.
These researchers could not evaluate data at the patient level and could not adjust for changes in disease severity. However, taken together, these findings suggest that something bad may be truly happening here.
The authors of this study also point out that the associations with increased mortality have largely been seen in patients with heart failure – and now in patients with COPD – which are both chronic diseases characterized by exacerbations, as opposed to acute MI and pneumonia, which are episodic and treatable. Perhaps in those types of disease, efforts to avoid readmissions may be more universally helpful. Maybe.
Even if it is challenging for me to adjudicate the complicated methods and results of this study, I find it concerning that there is “biological plausibility” for this association. Hospitalists know exactly how this might have happened. Have you heard of the pop-up alerts that fire in the emergency department to let the physicians know that this patient was discharged within the past 30 days? You know that alert is not meant to tell you what to do, but you just might want to consider trying to discharge them or at least place them in observation – use your clinical judgment, if you know what I mean.
Within the past decade, observation units quickly cropped up all over the country, often not staffed by hospitalists nor cardiologists, where patients with decompensated heart failure, chest pain, and/or COPD, can be given Lasix and/or nebulizer treatments – at least just enough to let them walk on back out that door without a hospital admission.
At the end of the day, whether mortality rates have truly increased in the real world, this well-intentioned program seems to have serious issues. As Ashish Jha, MD, wrote in 2018, “Right now, a high-readmission, low-mortality hospital will be penalized at 6-10 times the rate of a low-readmission, high-mortality hospital. The signal from policy makers is clear – readmissions matter a lot more than mortality – and this signal needs to stop.”
Dr. Moriates is a hospitalist, the assistant dean for health care value, and an associate professor of internal medicine at Dell Medical School at University of Texas, Austin. He is also director of implementation initiatives at Costs of Care. This article first appeared on the Hospital Leader, SHM’s official blog, at hospitalleader.org.
Be careful what you wish for
Be careful what you wish for
There is at least one aspect of “Obamacare” that my mother-in-law and I can firmly agree on: Hospitals should not get paid for frequent readmissions.
The Hospital Readmission Reduction Program (HRRP), enacted by the Centers for Medicare & Medicaid Services in 2012 with the goal of penalizing hospitals for excessive readmissions, has great face validity – and noble intentions. Does it also have a potentially disastrous downside?
On one side of the coin, the HRRP has been a remarkable success. It moved the national needle significantly on readmission rates. Yes, there are some caveats about increases in observation status patients and other shifts that could account for some of the difference, but it is fairly uncontroversial that overall, there are fewer 30-day readmissions across the country following initiation of HRRP. That is perhaps encouraging evidence of the potential positive impact that policy can make to drive changes for specific targets.
However, there is also a murkier – and more controversial – side. There have been a number of studies that have suggested reductions in readmission rates may have been associated with an increase in mortality in some patient groups. You discharge a patient and hope they won’t return to the hospital, but perhaps you should be more careful what you actually wish for.
Overall, the evidence of an association between readmissions and mortality has been complicated and conflicting. Headlines have alternately raised alarm about increased deaths and then reassured that there has been no change or perhaps even some concordant improvements in mortality. Not necessarily surprising, considering that these studies are all unavoidably of observational design and use different criteria, datasets and analytic models, which then drive their seemingly conflicting results.
An article published recently in the Journal of Hospital Medicine enters into this fray. The researchers examined the potential association between changes in rates of chronic obstructive pulmonary disease (COPD) readmissions and 30-day mortality following HRRP introduction. While the initial HRRP program and subsequent analyses included patients with heart failure, acute MI, and pneumonia, the program was extended in 2014 to include patients with COPD. So, what happened in this patient group?
Through a number of statistical gymnastics, which as a nonstatistician I am having difficulty truly wrapping my head around, the researchers seem to have found a number of important insights:
- The all-cause 30-day risk-standardized readmission rate declined from 2010 to 2017.
- The all-cause 30-day risk-standardized mortality rate increased from 2010 to 2017, and the rate of increase in mortality appears to be accelerating.
- Hospitals with higher readmission rates prior to COPD readmission penalties had a lower rate of increase in mortalities.
- Hospitals that had a larger decrease in readmission rates had a larger rate of increase in mortality.
These researchers could not evaluate data at the patient level and could not adjust for changes in disease severity. However, taken together, these findings suggest that something bad may be truly happening here.
The authors of this study also point out that the associations with increased mortality have largely been seen in patients with heart failure – and now in patients with COPD – which are both chronic diseases characterized by exacerbations, as opposed to acute MI and pneumonia, which are episodic and treatable. Perhaps in those types of disease, efforts to avoid readmissions may be more universally helpful. Maybe.
Even if it is challenging for me to adjudicate the complicated methods and results of this study, I find it concerning that there is “biological plausibility” for this association. Hospitalists know exactly how this might have happened. Have you heard of the pop-up alerts that fire in the emergency department to let the physicians know that this patient was discharged within the past 30 days? You know that alert is not meant to tell you what to do, but you just might want to consider trying to discharge them or at least place them in observation – use your clinical judgment, if you know what I mean.
Within the past decade, observation units quickly cropped up all over the country, often not staffed by hospitalists nor cardiologists, where patients with decompensated heart failure, chest pain, and/or COPD, can be given Lasix and/or nebulizer treatments – at least just enough to let them walk on back out that door without a hospital admission.
At the end of the day, whether mortality rates have truly increased in the real world, this well-intentioned program seems to have serious issues. As Ashish Jha, MD, wrote in 2018, “Right now, a high-readmission, low-mortality hospital will be penalized at 6-10 times the rate of a low-readmission, high-mortality hospital. The signal from policy makers is clear – readmissions matter a lot more than mortality – and this signal needs to stop.”
Dr. Moriates is a hospitalist, the assistant dean for health care value, and an associate professor of internal medicine at Dell Medical School at University of Texas, Austin. He is also director of implementation initiatives at Costs of Care. This article first appeared on the Hospital Leader, SHM’s official blog, at hospitalleader.org.
There is at least one aspect of “Obamacare” that my mother-in-law and I can firmly agree on: Hospitals should not get paid for frequent readmissions.
The Hospital Readmission Reduction Program (HRRP), enacted by the Centers for Medicare & Medicaid Services in 2012 with the goal of penalizing hospitals for excessive readmissions, has great face validity – and noble intentions. Does it also have a potentially disastrous downside?
On one side of the coin, the HRRP has been a remarkable success. It moved the national needle significantly on readmission rates. Yes, there are some caveats about increases in observation status patients and other shifts that could account for some of the difference, but it is fairly uncontroversial that overall, there are fewer 30-day readmissions across the country following initiation of HRRP. That is perhaps encouraging evidence of the potential positive impact that policy can make to drive changes for specific targets.
However, there is also a murkier – and more controversial – side. There have been a number of studies that have suggested reductions in readmission rates may have been associated with an increase in mortality in some patient groups. You discharge a patient and hope they won’t return to the hospital, but perhaps you should be more careful what you actually wish for.
Overall, the evidence of an association between readmissions and mortality has been complicated and conflicting. Headlines have alternately raised alarm about increased deaths and then reassured that there has been no change or perhaps even some concordant improvements in mortality. Not necessarily surprising, considering that these studies are all unavoidably of observational design and use different criteria, datasets and analytic models, which then drive their seemingly conflicting results.
An article published recently in the Journal of Hospital Medicine enters into this fray. The researchers examined the potential association between changes in rates of chronic obstructive pulmonary disease (COPD) readmissions and 30-day mortality following HRRP introduction. While the initial HRRP program and subsequent analyses included patients with heart failure, acute MI, and pneumonia, the program was extended in 2014 to include patients with COPD. So, what happened in this patient group?
Through a number of statistical gymnastics, which as a nonstatistician I am having difficulty truly wrapping my head around, the researchers seem to have found a number of important insights:
- The all-cause 30-day risk-standardized readmission rate declined from 2010 to 2017.
- The all-cause 30-day risk-standardized mortality rate increased from 2010 to 2017, and the rate of increase in mortality appears to be accelerating.
- Hospitals with higher readmission rates prior to COPD readmission penalties had a lower rate of increase in mortalities.
- Hospitals that had a larger decrease in readmission rates had a larger rate of increase in mortality.
These researchers could not evaluate data at the patient level and could not adjust for changes in disease severity. However, taken together, these findings suggest that something bad may be truly happening here.
The authors of this study also point out that the associations with increased mortality have largely been seen in patients with heart failure – and now in patients with COPD – which are both chronic diseases characterized by exacerbations, as opposed to acute MI and pneumonia, which are episodic and treatable. Perhaps in those types of disease, efforts to avoid readmissions may be more universally helpful. Maybe.
Even if it is challenging for me to adjudicate the complicated methods and results of this study, I find it concerning that there is “biological plausibility” for this association. Hospitalists know exactly how this might have happened. Have you heard of the pop-up alerts that fire in the emergency department to let the physicians know that this patient was discharged within the past 30 days? You know that alert is not meant to tell you what to do, but you just might want to consider trying to discharge them or at least place them in observation – use your clinical judgment, if you know what I mean.
Within the past decade, observation units quickly cropped up all over the country, often not staffed by hospitalists nor cardiologists, where patients with decompensated heart failure, chest pain, and/or COPD, can be given Lasix and/or nebulizer treatments – at least just enough to let them walk on back out that door without a hospital admission.
At the end of the day, whether mortality rates have truly increased in the real world, this well-intentioned program seems to have serious issues. As Ashish Jha, MD, wrote in 2018, “Right now, a high-readmission, low-mortality hospital will be penalized at 6-10 times the rate of a low-readmission, high-mortality hospital. The signal from policy makers is clear – readmissions matter a lot more than mortality – and this signal needs to stop.”
Dr. Moriates is a hospitalist, the assistant dean for health care value, and an associate professor of internal medicine at Dell Medical School at University of Texas, Austin. He is also director of implementation initiatives at Costs of Care. This article first appeared on the Hospital Leader, SHM’s official blog, at hospitalleader.org.
2019-2020 flu season starts off full throttle
For the week ending Nov. 23, there were five states, along with Puerto Rico, at the highest level of the Centers for Disease Control and Prevention’s 1-10 scale of flu activity. That’s more than any year since 2012, including the pandemic season of 2017-2018, according to CDC data, and may suggest either an early peak or the beginning of a particularly bad winter.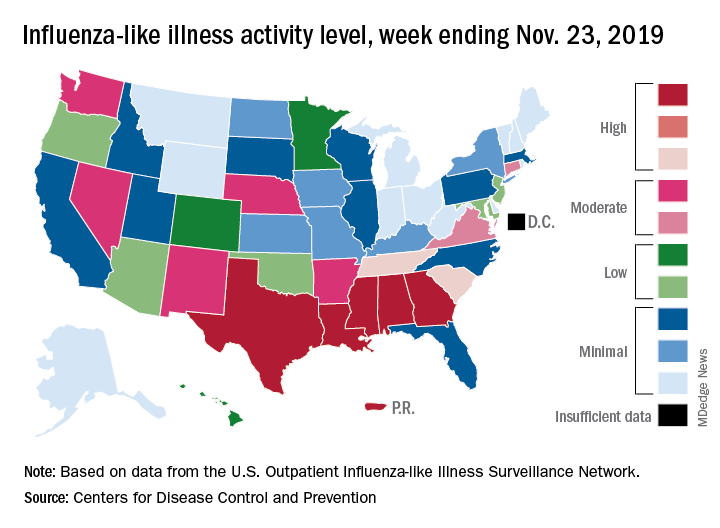
“Nationally, ILI [influenza-like illness] activity has been at or above baseline for 3 weeks; however, the amount of influenza activity across the country varies with the south and parts of the west seeing elevated activity while other parts of the country are still seeing low activity,” the CDC’s influenza division said in its weekly FluView report.
The five highest-activity states – Alabama, Georgia, Louisiana, Mississippi, and Texas – are all at level 10, and they join two others – South Carolina and Tennessee, which are at level 8 – in the “high” range from 8-10 on the ILI activity scale; Puerto Rico also is at level 10. ILI is defined as “fever (temperature of 100° F [37.8° C] or greater) and a cough and/or a sore throat without a known cause other than influenza,” the CDC said.
The activity scale is based on the percentage of outpatient visits for ILI in each state, which is reported to the CDC’s Outpatient Influenza-like Illness Surveillance Network (ILINet) each week. The national rate for the week ending Nov. 23 was 2.9%, which is above the new-for-this-season baseline rate of 2.4%. For the three previous flu seasons, the national baseline was 2.2%, having been raised from its previous level of 2.1% in 2015-2016, CDC data show.
The peak month of flu activity occurs most often in February – 15 times from 1982-1983 to 2017-2018 – but there were seven peaks in December and six each in January and March over that time period, along with one peak each in October and November, the CDC said. The October peak occurred during the H1N1 pandemic year of 2009, when the national outpatient ILI rate climbed to just over 7.7%.
For the week ending Nov. 23, there were five states, along with Puerto Rico, at the highest level of the Centers for Disease Control and Prevention’s 1-10 scale of flu activity. That’s more than any year since 2012, including the pandemic season of 2017-2018, according to CDC data, and may suggest either an early peak or the beginning of a particularly bad winter.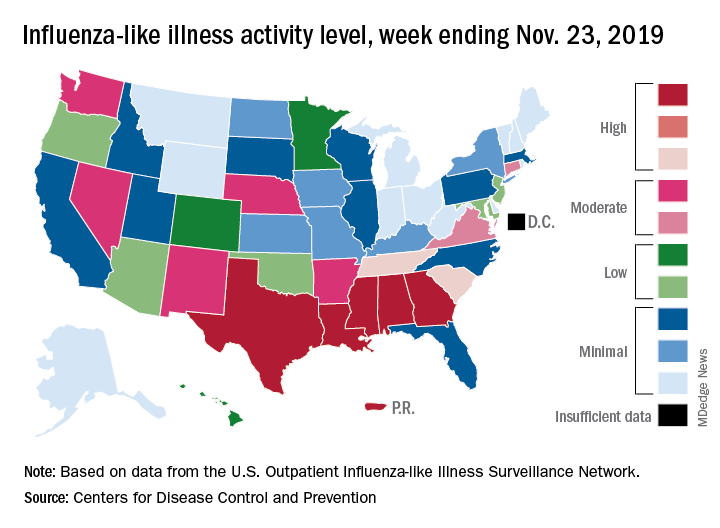
“Nationally, ILI [influenza-like illness] activity has been at or above baseline for 3 weeks; however, the amount of influenza activity across the country varies with the south and parts of the west seeing elevated activity while other parts of the country are still seeing low activity,” the CDC’s influenza division said in its weekly FluView report.
The five highest-activity states – Alabama, Georgia, Louisiana, Mississippi, and Texas – are all at level 10, and they join two others – South Carolina and Tennessee, which are at level 8 – in the “high” range from 8-10 on the ILI activity scale; Puerto Rico also is at level 10. ILI is defined as “fever (temperature of 100° F [37.8° C] or greater) and a cough and/or a sore throat without a known cause other than influenza,” the CDC said.
The activity scale is based on the percentage of outpatient visits for ILI in each state, which is reported to the CDC’s Outpatient Influenza-like Illness Surveillance Network (ILINet) each week. The national rate for the week ending Nov. 23 was 2.9%, which is above the new-for-this-season baseline rate of 2.4%. For the three previous flu seasons, the national baseline was 2.2%, having been raised from its previous level of 2.1% in 2015-2016, CDC data show.
The peak month of flu activity occurs most often in February – 15 times from 1982-1983 to 2017-2018 – but there were seven peaks in December and six each in January and March over that time period, along with one peak each in October and November, the CDC said. The October peak occurred during the H1N1 pandemic year of 2009, when the national outpatient ILI rate climbed to just over 7.7%.
For the week ending Nov. 23, there were five states, along with Puerto Rico, at the highest level of the Centers for Disease Control and Prevention’s 1-10 scale of flu activity. That’s more than any year since 2012, including the pandemic season of 2017-2018, according to CDC data, and may suggest either an early peak or the beginning of a particularly bad winter.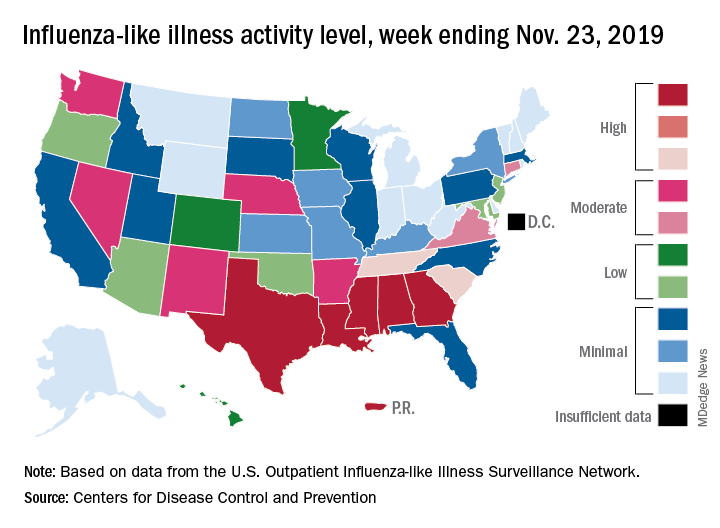
“Nationally, ILI [influenza-like illness] activity has been at or above baseline for 3 weeks; however, the amount of influenza activity across the country varies with the south and parts of the west seeing elevated activity while other parts of the country are still seeing low activity,” the CDC’s influenza division said in its weekly FluView report.
The five highest-activity states – Alabama, Georgia, Louisiana, Mississippi, and Texas – are all at level 10, and they join two others – South Carolina and Tennessee, which are at level 8 – in the “high” range from 8-10 on the ILI activity scale; Puerto Rico also is at level 10. ILI is defined as “fever (temperature of 100° F [37.8° C] or greater) and a cough and/or a sore throat without a known cause other than influenza,” the CDC said.
The activity scale is based on the percentage of outpatient visits for ILI in each state, which is reported to the CDC’s Outpatient Influenza-like Illness Surveillance Network (ILINet) each week. The national rate for the week ending Nov. 23 was 2.9%, which is above the new-for-this-season baseline rate of 2.4%. For the three previous flu seasons, the national baseline was 2.2%, having been raised from its previous level of 2.1% in 2015-2016, CDC data show.
The peak month of flu activity occurs most often in February – 15 times from 1982-1983 to 2017-2018 – but there were seven peaks in December and six each in January and March over that time period, along with one peak each in October and November, the CDC said. The October peak occurred during the H1N1 pandemic year of 2009, when the national outpatient ILI rate climbed to just over 7.7%.
Supporting quality improvement strategies
Keys to improve PDSA cycle fidelity
As many hospitalists know, a frequently deployed approach to quality improvement (QI) is the Plan-Do-Study-Act (PDSA) cycle method. But it comes with challenges, according to a recent paper in BMJ Quality & Safety.
“There is little evidence on the fidelity of PDSA cycles used by frontline teams, nor how to support and improve the method’s use,” according to the authors. They used document analysis and interviews to review 421 PDSA cycles, tracking fidelity over three annual rounds of projects.
The researchers found that modest, statistically significant improvements in PDSA fidelity occurred, but overall fidelity was low.
“Challenges to achieving greater fidelity reflected problems with understanding the PDSA methodology, intention to use and application in practice,” the authors reported. “These problems were exacerbated by assumptions made in the original QI training and support strategies: that PDSA was easy to understand, that teams would be motivated and willing to use PDSA, and that PDSA is easy to apply.”
The study describes several strategies to help improve PDSA cycle fidelity: different project selection process, redesign of training, increased hands-on support, and investment in training quality improvement support staff. “The findings suggest achieving high PDSA fidelity requires a gradual and negotiated process to explore different perspectives and encourage new ways of working,” the authors concluded.
Reference
1. McNicholas C et al. Evolving quality improvement support strategies to improve Plan-Do-Study–Act cycle fidelity: A retrospective mixed-methods study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2017-007605.
Keys to improve PDSA cycle fidelity
Keys to improve PDSA cycle fidelity
As many hospitalists know, a frequently deployed approach to quality improvement (QI) is the Plan-Do-Study-Act (PDSA) cycle method. But it comes with challenges, according to a recent paper in BMJ Quality & Safety.
“There is little evidence on the fidelity of PDSA cycles used by frontline teams, nor how to support and improve the method’s use,” according to the authors. They used document analysis and interviews to review 421 PDSA cycles, tracking fidelity over three annual rounds of projects.
The researchers found that modest, statistically significant improvements in PDSA fidelity occurred, but overall fidelity was low.
“Challenges to achieving greater fidelity reflected problems with understanding the PDSA methodology, intention to use and application in practice,” the authors reported. “These problems were exacerbated by assumptions made in the original QI training and support strategies: that PDSA was easy to understand, that teams would be motivated and willing to use PDSA, and that PDSA is easy to apply.”
The study describes several strategies to help improve PDSA cycle fidelity: different project selection process, redesign of training, increased hands-on support, and investment in training quality improvement support staff. “The findings suggest achieving high PDSA fidelity requires a gradual and negotiated process to explore different perspectives and encourage new ways of working,” the authors concluded.
Reference
1. McNicholas C et al. Evolving quality improvement support strategies to improve Plan-Do-Study–Act cycle fidelity: A retrospective mixed-methods study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2017-007605.
As many hospitalists know, a frequently deployed approach to quality improvement (QI) is the Plan-Do-Study-Act (PDSA) cycle method. But it comes with challenges, according to a recent paper in BMJ Quality & Safety.
“There is little evidence on the fidelity of PDSA cycles used by frontline teams, nor how to support and improve the method’s use,” according to the authors. They used document analysis and interviews to review 421 PDSA cycles, tracking fidelity over three annual rounds of projects.
The researchers found that modest, statistically significant improvements in PDSA fidelity occurred, but overall fidelity was low.
“Challenges to achieving greater fidelity reflected problems with understanding the PDSA methodology, intention to use and application in practice,” the authors reported. “These problems were exacerbated by assumptions made in the original QI training and support strategies: that PDSA was easy to understand, that teams would be motivated and willing to use PDSA, and that PDSA is easy to apply.”
The study describes several strategies to help improve PDSA cycle fidelity: different project selection process, redesign of training, increased hands-on support, and investment in training quality improvement support staff. “The findings suggest achieving high PDSA fidelity requires a gradual and negotiated process to explore different perspectives and encourage new ways of working,” the authors concluded.
Reference
1. McNicholas C et al. Evolving quality improvement support strategies to improve Plan-Do-Study–Act cycle fidelity: A retrospective mixed-methods study. BMJ Qual Saf. 2019 Mar 18. doi: 10.1136/bmjqs-2017-007605.
Benefiting from hospitalist-directed transfers
A ‘unique opportunity’ for hospitalists
Emergency department overcrowding is common, and it can result in both increased costs and poor clinical outcomes.
“We sought to evaluate the impact and safety of hospitalist-directed transfers on patients boarding in the ER as a means to alleviate overcrowding,” said Yihan Chen, MD, MPH, of the University of California, Los Angeles. “High inpatient census has been shown to impair ER throughput by increasing the number of ER ‘boarders,’ which creates a suboptimal care environment for practicing hospitalists. For example, some studies have shown associations with delays in medical decision making when admitted patients remain and receive care in the emergency department.”
Dr. Chen was the lead author of an abstract describing a chart review on 1,016 admissions to the hospitalist service. About half remained at the reference hospital and half were transferred to a nearby affiliate hospital.
In analyzing the data, the researchers’ top takeaway was the many benefits for the transferred patients. “Hospitalist-directed transfer and direct admission of stable ER patients to an affiliate facility with greater bed availability is associated with shorter ER lengths of stay, fewer adverse events, and lower rates of readmission within 30 days of hospitalization,” Dr. Chen said. “Having a system in place to transfer patients to an affiliate hospital with lower census is a way to improve flow.”
Hospitalists have a unique opportunity to take on a triage role in the ED to safely and effectively decrease ED overcrowding and throughput, improve resource utilization at the hospital level, and allow for other hospitalists at their institution to optimize patient care on the inpatient ward rather than in the ED, Dr. Chen said.
“Health systems privileged to have more than one facility should consider an intra–health system transfer process lead by triage hospitalists to identify stable patients who can be directly admitted to the off-site, affiliate hospital,” she said. “By improving patient throughput, hospitalists would play a critical role in relieving institutional stressors, impacting cost and quality of care, and enhancing clinical outcomes.”
Reference
1. Chen Y et al. Hospitalist-Directed Transfers Improve Emergency Room Length of Stay. Hospital Medicine 2018, Abstract 12. Accessed April 3, 2019.
A ‘unique opportunity’ for hospitalists
A ‘unique opportunity’ for hospitalists
Emergency department overcrowding is common, and it can result in both increased costs and poor clinical outcomes.
“We sought to evaluate the impact and safety of hospitalist-directed transfers on patients boarding in the ER as a means to alleviate overcrowding,” said Yihan Chen, MD, MPH, of the University of California, Los Angeles. “High inpatient census has been shown to impair ER throughput by increasing the number of ER ‘boarders,’ which creates a suboptimal care environment for practicing hospitalists. For example, some studies have shown associations with delays in medical decision making when admitted patients remain and receive care in the emergency department.”
Dr. Chen was the lead author of an abstract describing a chart review on 1,016 admissions to the hospitalist service. About half remained at the reference hospital and half were transferred to a nearby affiliate hospital.
In analyzing the data, the researchers’ top takeaway was the many benefits for the transferred patients. “Hospitalist-directed transfer and direct admission of stable ER patients to an affiliate facility with greater bed availability is associated with shorter ER lengths of stay, fewer adverse events, and lower rates of readmission within 30 days of hospitalization,” Dr. Chen said. “Having a system in place to transfer patients to an affiliate hospital with lower census is a way to improve flow.”
Hospitalists have a unique opportunity to take on a triage role in the ED to safely and effectively decrease ED overcrowding and throughput, improve resource utilization at the hospital level, and allow for other hospitalists at their institution to optimize patient care on the inpatient ward rather than in the ED, Dr. Chen said.
“Health systems privileged to have more than one facility should consider an intra–health system transfer process lead by triage hospitalists to identify stable patients who can be directly admitted to the off-site, affiliate hospital,” she said. “By improving patient throughput, hospitalists would play a critical role in relieving institutional stressors, impacting cost and quality of care, and enhancing clinical outcomes.”
Reference
1. Chen Y et al. Hospitalist-Directed Transfers Improve Emergency Room Length of Stay. Hospital Medicine 2018, Abstract 12. Accessed April 3, 2019.
Emergency department overcrowding is common, and it can result in both increased costs and poor clinical outcomes.
“We sought to evaluate the impact and safety of hospitalist-directed transfers on patients boarding in the ER as a means to alleviate overcrowding,” said Yihan Chen, MD, MPH, of the University of California, Los Angeles. “High inpatient census has been shown to impair ER throughput by increasing the number of ER ‘boarders,’ which creates a suboptimal care environment for practicing hospitalists. For example, some studies have shown associations with delays in medical decision making when admitted patients remain and receive care in the emergency department.”
Dr. Chen was the lead author of an abstract describing a chart review on 1,016 admissions to the hospitalist service. About half remained at the reference hospital and half were transferred to a nearby affiliate hospital.
In analyzing the data, the researchers’ top takeaway was the many benefits for the transferred patients. “Hospitalist-directed transfer and direct admission of stable ER patients to an affiliate facility with greater bed availability is associated with shorter ER lengths of stay, fewer adverse events, and lower rates of readmission within 30 days of hospitalization,” Dr. Chen said. “Having a system in place to transfer patients to an affiliate hospital with lower census is a way to improve flow.”
Hospitalists have a unique opportunity to take on a triage role in the ED to safely and effectively decrease ED overcrowding and throughput, improve resource utilization at the hospital level, and allow for other hospitalists at their institution to optimize patient care on the inpatient ward rather than in the ED, Dr. Chen said.
“Health systems privileged to have more than one facility should consider an intra–health system transfer process lead by triage hospitalists to identify stable patients who can be directly admitted to the off-site, affiliate hospital,” she said. “By improving patient throughput, hospitalists would play a critical role in relieving institutional stressors, impacting cost and quality of care, and enhancing clinical outcomes.”
Reference
1. Chen Y et al. Hospitalist-Directed Transfers Improve Emergency Room Length of Stay. Hospital Medicine 2018, Abstract 12. Accessed April 3, 2019.
PHM19: MOC Part 4 projects for community pediatric hospitalists
PHM19 session
MOC Part 4 projects for community pediatric hospitalists
Presenters
Jack M. Percelay, MD, MPH, FAAP, MHM
Nancy Chen, MD, FAAP
Elizabeth Dobler, MD, FAAP
Lindsay Fox, MD
Beth C. Natt, MD, MPH, SFHM
Clota Snow, MD, FAAP
Session summary
Dr. Jack Percelay, of Sutter Health in San Francisco, started this session at Pediatric Hospital Medicine 2019 by outlining the process of submitting a small group (n = 1-10) project for Maintenance of Certification (MOC) Part 4 credit including the basics of what is needed for the application:
- Aim statement.
- Metrics used.
- Data required (3 data points: pre, post, and sustain).
He also shared the requirement of “meaningful participation” for participants to be eligible for MOC Part 4 credit.
Examples of successful projects were shared by members of the presenting group:
- Dr. Natt: Improving the timing of the birth dose of the hepatitis B vaccination.
- Dr. Dobler: Improving the hepatitis B vaccination rate within 24 hours of birth.
- Dr. Snow: Supplementing vitamin D in the newborn nursery.
- Dr. Fox: Improving newborn discharge efficiency, improving screening for smoking exposure, and offering smoking cessation.
- Dr. Percelay: Improving hospitalist billing and coding using time as a factor.
- Dr. Chen: Improving patient satisfaction through improvement of family-centered rounds.
The workshop audience divided into groups to brainstorm/troubleshoot projects and to elicit general advice regarding the process. Sample submissions were provided.
Key takeaways
- Even small projects (i.e. single metric) can be submitted/accepted with pre- and postintervention data.
- Be creative! Think about changes you are making at your institution and gather the data to support the intervention.
- Always double-dip on QI projects to gain valuable MOC Part 4 credit!
Dr. Fox is site director, Pediatric Hospital Medicine Division at MetroWest Medical Center, Framingham, Mass.
PHM19 session
MOC Part 4 projects for community pediatric hospitalists
Presenters
Jack M. Percelay, MD, MPH, FAAP, MHM
Nancy Chen, MD, FAAP
Elizabeth Dobler, MD, FAAP
Lindsay Fox, MD
Beth C. Natt, MD, MPH, SFHM
Clota Snow, MD, FAAP
Session summary
Dr. Jack Percelay, of Sutter Health in San Francisco, started this session at Pediatric Hospital Medicine 2019 by outlining the process of submitting a small group (n = 1-10) project for Maintenance of Certification (MOC) Part 4 credit including the basics of what is needed for the application:
- Aim statement.
- Metrics used.
- Data required (3 data points: pre, post, and sustain).
He also shared the requirement of “meaningful participation” for participants to be eligible for MOC Part 4 credit.
Examples of successful projects were shared by members of the presenting group:
- Dr. Natt: Improving the timing of the birth dose of the hepatitis B vaccination.
- Dr. Dobler: Improving the hepatitis B vaccination rate within 24 hours of birth.
- Dr. Snow: Supplementing vitamin D in the newborn nursery.
- Dr. Fox: Improving newborn discharge efficiency, improving screening for smoking exposure, and offering smoking cessation.
- Dr. Percelay: Improving hospitalist billing and coding using time as a factor.
- Dr. Chen: Improving patient satisfaction through improvement of family-centered rounds.
The workshop audience divided into groups to brainstorm/troubleshoot projects and to elicit general advice regarding the process. Sample submissions were provided.
Key takeaways
- Even small projects (i.e. single metric) can be submitted/accepted with pre- and postintervention data.
- Be creative! Think about changes you are making at your institution and gather the data to support the intervention.
- Always double-dip on QI projects to gain valuable MOC Part 4 credit!
Dr. Fox is site director, Pediatric Hospital Medicine Division at MetroWest Medical Center, Framingham, Mass.
PHM19 session
MOC Part 4 projects for community pediatric hospitalists
Presenters
Jack M. Percelay, MD, MPH, FAAP, MHM
Nancy Chen, MD, FAAP
Elizabeth Dobler, MD, FAAP
Lindsay Fox, MD
Beth C. Natt, MD, MPH, SFHM
Clota Snow, MD, FAAP
Session summary
Dr. Jack Percelay, of Sutter Health in San Francisco, started this session at Pediatric Hospital Medicine 2019 by outlining the process of submitting a small group (n = 1-10) project for Maintenance of Certification (MOC) Part 4 credit including the basics of what is needed for the application:
- Aim statement.
- Metrics used.
- Data required (3 data points: pre, post, and sustain).
He also shared the requirement of “meaningful participation” for participants to be eligible for MOC Part 4 credit.
Examples of successful projects were shared by members of the presenting group:
- Dr. Natt: Improving the timing of the birth dose of the hepatitis B vaccination.
- Dr. Dobler: Improving the hepatitis B vaccination rate within 24 hours of birth.
- Dr. Snow: Supplementing vitamin D in the newborn nursery.
- Dr. Fox: Improving newborn discharge efficiency, improving screening for smoking exposure, and offering smoking cessation.
- Dr. Percelay: Improving hospitalist billing and coding using time as a factor.
- Dr. Chen: Improving patient satisfaction through improvement of family-centered rounds.
The workshop audience divided into groups to brainstorm/troubleshoot projects and to elicit general advice regarding the process. Sample submissions were provided.
Key takeaways
- Even small projects (i.e. single metric) can be submitted/accepted with pre- and postintervention data.
- Be creative! Think about changes you are making at your institution and gather the data to support the intervention.
- Always double-dip on QI projects to gain valuable MOC Part 4 credit!
Dr. Fox is site director, Pediatric Hospital Medicine Division at MetroWest Medical Center, Framingham, Mass.
ACGME deepening its commitment to physician well-being, leader says
NEW ORLEANS – When Timothy P. Brigham, MDiv, PhD, thinks about the impact of burnout and stress on the ability of physicians to practice medicine, Lewin’s equation comes to mind.
Developed by psychologist Kurt Lewin in 1936, the equation holds that behavior stems from a person’s personality and the environment that person inhabits.
Dr. Brigham, chief of staff and chief education and organizational development officer at the Chicago-based Accreditation Council for Graduate Medical Education (ACGME), said at the annual meeting of the American Academy of Pediatrics.
“It’s a toxic mine, in some ways. What we tend to do is when we detect that physicians in general are, or a particular residency program is, too stressed out or burned out, we give them resilience training. Not that that’s unimportant, but it’s like putting a canary in a toxic mine full of poison and saying, ‘We’re going to teach you to hold your breath a little bit longer.’ Our job is to detoxify the mine.”
Troubled by the rise of suicides among physicians in recent years as well as mounting evidence about the adverse impact of burnout and stress on the practice of medicine, Dr. Brigham said that the ACGME is deepening its commitment to the well-being of faculty, residents, patients, and all members of the health care team. Since launching a “call to arms” on the topic at its annual educational conference in 2015, the ACGME has added courses on well-being to its annual meeting and remolded its Clinical Learning Environmental Review program to include all clinicians, “because everybody is affected by this: nurses, coordinators, et cetera,” he said. The ACGME also has revised Common Program Requirements, disseminated tools and resources to promote well-being and new knowledge on the topic, and partnered with the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience – all in an effort to bring about culture change.
“But we’re well aware that the ACGME can’t do this alone,” Dr. Brigham said. “We can’t ‘requirement’ our way out of this problem. It’s going to take a culture shift. Only you physicians, in collaboration with everyone in your community of learning, can create the systemic change required to improve our culture. We have a good handle on the problem at this point, but the solutions are a little bit more difficult to get a hold of. As Martin Luther King Jr. once said, ‘You don’t have to see the whole staircase, just take the first step.’ ”
The ACGME wants to work with physicians “to collect data and do joint research, to share insights, and to share tools and resources to create a better world for practicing physicians, for other members of the health care team, and for patients. After all, clinicians who care for themselves provide better care for others. They’re less likely to make errors or leave the profession,” Dr. Brigham told attendees.
He added that clinicians can gauge their risk for burnout by asking themselves three simple questions about their work environment: Does it support self-care? Does it increase and support connection with colleagues? Does it connect people to purpose and meaningful work?
“One of the problems with our resident clinical work hours is not terrible program directors saying, ‘work longer.’ It’s residents who want to take care of families for 1 more hour,” Dr. Brigham continued. “It’s residents who want to take care of patients who are going through a difficult time. You represent the top 2% in the world in terms of your intelligence and achievement, yet that’s not what makes you special. What makes you special is that the level of self-doubt in this room exceeds that of the general population by about 10 times. You also tend to run toward what everyone else runs away from: disease, despair, people who are injured and suffering. That takes a toll.”
He emphasized that positive social relationships with others are crucial to joy and well-being in the practice of medicine. “Burnout isn’t just about exhaustion; it’s about loneliness,” Dr. Brigham said. “There’s a surprising power in just asking people how they’re doing, and really wanting to know the answer.”
Negative social connections are highly correlated with burnout and depression, such as harassment, bullying, mistreatment, discrimination, “and using the power gradient to squash somebody who’s trying their best to be a physician,” he said.
Dr. Brigham acknowledged the tall task of bringing a spotlight to well-being as physicians continue to engage in tasks such as the burden and lack of standardization of prior authorization requirements, the burden of clinical documentation requirements, electronic health records and related work flow, and quality payment programs. “This is what we need to shift; this is what we need to take away so you can get back in touch with why you became a physician in the first place.”
Dr. Brigham reported having no financial disclosures.
NEW ORLEANS – When Timothy P. Brigham, MDiv, PhD, thinks about the impact of burnout and stress on the ability of physicians to practice medicine, Lewin’s equation comes to mind.
Developed by psychologist Kurt Lewin in 1936, the equation holds that behavior stems from a person’s personality and the environment that person inhabits.
Dr. Brigham, chief of staff and chief education and organizational development officer at the Chicago-based Accreditation Council for Graduate Medical Education (ACGME), said at the annual meeting of the American Academy of Pediatrics.
“It’s a toxic mine, in some ways. What we tend to do is when we detect that physicians in general are, or a particular residency program is, too stressed out or burned out, we give them resilience training. Not that that’s unimportant, but it’s like putting a canary in a toxic mine full of poison and saying, ‘We’re going to teach you to hold your breath a little bit longer.’ Our job is to detoxify the mine.”
Troubled by the rise of suicides among physicians in recent years as well as mounting evidence about the adverse impact of burnout and stress on the practice of medicine, Dr. Brigham said that the ACGME is deepening its commitment to the well-being of faculty, residents, patients, and all members of the health care team. Since launching a “call to arms” on the topic at its annual educational conference in 2015, the ACGME has added courses on well-being to its annual meeting and remolded its Clinical Learning Environmental Review program to include all clinicians, “because everybody is affected by this: nurses, coordinators, et cetera,” he said. The ACGME also has revised Common Program Requirements, disseminated tools and resources to promote well-being and new knowledge on the topic, and partnered with the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience – all in an effort to bring about culture change.
“But we’re well aware that the ACGME can’t do this alone,” Dr. Brigham said. “We can’t ‘requirement’ our way out of this problem. It’s going to take a culture shift. Only you physicians, in collaboration with everyone in your community of learning, can create the systemic change required to improve our culture. We have a good handle on the problem at this point, but the solutions are a little bit more difficult to get a hold of. As Martin Luther King Jr. once said, ‘You don’t have to see the whole staircase, just take the first step.’ ”
The ACGME wants to work with physicians “to collect data and do joint research, to share insights, and to share tools and resources to create a better world for practicing physicians, for other members of the health care team, and for patients. After all, clinicians who care for themselves provide better care for others. They’re less likely to make errors or leave the profession,” Dr. Brigham told attendees.
He added that clinicians can gauge their risk for burnout by asking themselves three simple questions about their work environment: Does it support self-care? Does it increase and support connection with colleagues? Does it connect people to purpose and meaningful work?
“One of the problems with our resident clinical work hours is not terrible program directors saying, ‘work longer.’ It’s residents who want to take care of families for 1 more hour,” Dr. Brigham continued. “It’s residents who want to take care of patients who are going through a difficult time. You represent the top 2% in the world in terms of your intelligence and achievement, yet that’s not what makes you special. What makes you special is that the level of self-doubt in this room exceeds that of the general population by about 10 times. You also tend to run toward what everyone else runs away from: disease, despair, people who are injured and suffering. That takes a toll.”
He emphasized that positive social relationships with others are crucial to joy and well-being in the practice of medicine. “Burnout isn’t just about exhaustion; it’s about loneliness,” Dr. Brigham said. “There’s a surprising power in just asking people how they’re doing, and really wanting to know the answer.”
Negative social connections are highly correlated with burnout and depression, such as harassment, bullying, mistreatment, discrimination, “and using the power gradient to squash somebody who’s trying their best to be a physician,” he said.
Dr. Brigham acknowledged the tall task of bringing a spotlight to well-being as physicians continue to engage in tasks such as the burden and lack of standardization of prior authorization requirements, the burden of clinical documentation requirements, electronic health records and related work flow, and quality payment programs. “This is what we need to shift; this is what we need to take away so you can get back in touch with why you became a physician in the first place.”
Dr. Brigham reported having no financial disclosures.
NEW ORLEANS – When Timothy P. Brigham, MDiv, PhD, thinks about the impact of burnout and stress on the ability of physicians to practice medicine, Lewin’s equation comes to mind.
Developed by psychologist Kurt Lewin in 1936, the equation holds that behavior stems from a person’s personality and the environment that person inhabits.
Dr. Brigham, chief of staff and chief education and organizational development officer at the Chicago-based Accreditation Council for Graduate Medical Education (ACGME), said at the annual meeting of the American Academy of Pediatrics.
“It’s a toxic mine, in some ways. What we tend to do is when we detect that physicians in general are, or a particular residency program is, too stressed out or burned out, we give them resilience training. Not that that’s unimportant, but it’s like putting a canary in a toxic mine full of poison and saying, ‘We’re going to teach you to hold your breath a little bit longer.’ Our job is to detoxify the mine.”
Troubled by the rise of suicides among physicians in recent years as well as mounting evidence about the adverse impact of burnout and stress on the practice of medicine, Dr. Brigham said that the ACGME is deepening its commitment to the well-being of faculty, residents, patients, and all members of the health care team. Since launching a “call to arms” on the topic at its annual educational conference in 2015, the ACGME has added courses on well-being to its annual meeting and remolded its Clinical Learning Environmental Review program to include all clinicians, “because everybody is affected by this: nurses, coordinators, et cetera,” he said. The ACGME also has revised Common Program Requirements, disseminated tools and resources to promote well-being and new knowledge on the topic, and partnered with the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience – all in an effort to bring about culture change.
“But we’re well aware that the ACGME can’t do this alone,” Dr. Brigham said. “We can’t ‘requirement’ our way out of this problem. It’s going to take a culture shift. Only you physicians, in collaboration with everyone in your community of learning, can create the systemic change required to improve our culture. We have a good handle on the problem at this point, but the solutions are a little bit more difficult to get a hold of. As Martin Luther King Jr. once said, ‘You don’t have to see the whole staircase, just take the first step.’ ”
The ACGME wants to work with physicians “to collect data and do joint research, to share insights, and to share tools and resources to create a better world for practicing physicians, for other members of the health care team, and for patients. After all, clinicians who care for themselves provide better care for others. They’re less likely to make errors or leave the profession,” Dr. Brigham told attendees.
He added that clinicians can gauge their risk for burnout by asking themselves three simple questions about their work environment: Does it support self-care? Does it increase and support connection with colleagues? Does it connect people to purpose and meaningful work?
“One of the problems with our resident clinical work hours is not terrible program directors saying, ‘work longer.’ It’s residents who want to take care of families for 1 more hour,” Dr. Brigham continued. “It’s residents who want to take care of patients who are going through a difficult time. You represent the top 2% in the world in terms of your intelligence and achievement, yet that’s not what makes you special. What makes you special is that the level of self-doubt in this room exceeds that of the general population by about 10 times. You also tend to run toward what everyone else runs away from: disease, despair, people who are injured and suffering. That takes a toll.”
He emphasized that positive social relationships with others are crucial to joy and well-being in the practice of medicine. “Burnout isn’t just about exhaustion; it’s about loneliness,” Dr. Brigham said. “There’s a surprising power in just asking people how they’re doing, and really wanting to know the answer.”
Negative social connections are highly correlated with burnout and depression, such as harassment, bullying, mistreatment, discrimination, “and using the power gradient to squash somebody who’s trying their best to be a physician,” he said.
Dr. Brigham acknowledged the tall task of bringing a spotlight to well-being as physicians continue to engage in tasks such as the burden and lack of standardization of prior authorization requirements, the burden of clinical documentation requirements, electronic health records and related work flow, and quality payment programs. “This is what we need to shift; this is what we need to take away so you can get back in touch with why you became a physician in the first place.”
Dr. Brigham reported having no financial disclosures.
EXPERT ANALYSIS AT AAP 2019