User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Reducing sepsis mortality
The CDC estimates that 1.7 million people in the United States acquire sepsis annually; sepsis accounts for nearly 270,000 patient deaths per year.
Decreasing mortality and improving patient outcomes requires early detection and appropriate timely treatment. The Joint Commission Center for Transforming Healthcare’s recent sepsis project demonstrated this by analyzing root causes and reducing sepsis mortality with five leading hospitals by an aggregate of nearly 25%.
“Most organizations can tell you how they are doing with regard to whether or not they are ordering lactates or fluids, but many can’t tell you where in the process these elements are failing,” said Kelly Barnes, Black Belt III, Joint Commission Center for Transforming Healthcare. “For instance, is the issue in ordering lactates, drawing lactates, or getting the results of lactates in a timely manner? The key is to understand where in the process things are breaking down to identify what solutions an organization needs to put in place.”
During the Joint Commission project, one organization found that patients had inadequate fluid resuscitation due to staff fear of fluid overload, while another organization found they had issues with fluids being disconnected when patients were taken for tests and then not reconnected – different problems that needed different solutions.
The Joint Commission Center for Transforming Healthcare is currently developing a Targeted Solutions Tool® (TST®), scheduled for release in 2019, to help organizations determine their issues with sepsis recognition and barriers to meeting sepsis bundle element requirements and implement targeted solutions to address their specific issues. The tool will be available free of charge to all Joint Commission-accredited customers.
Reference
1. “Hospital-Wide Sepsis Project Reduces Mortality by Nearly 25 Percent,” Kelly Barnes, The Joint Commission Center for Transforming Healthcare. 2018, Sep 25.
The CDC estimates that 1.7 million people in the United States acquire sepsis annually; sepsis accounts for nearly 270,000 patient deaths per year.
Decreasing mortality and improving patient outcomes requires early detection and appropriate timely treatment. The Joint Commission Center for Transforming Healthcare’s recent sepsis project demonstrated this by analyzing root causes and reducing sepsis mortality with five leading hospitals by an aggregate of nearly 25%.
“Most organizations can tell you how they are doing with regard to whether or not they are ordering lactates or fluids, but many can’t tell you where in the process these elements are failing,” said Kelly Barnes, Black Belt III, Joint Commission Center for Transforming Healthcare. “For instance, is the issue in ordering lactates, drawing lactates, or getting the results of lactates in a timely manner? The key is to understand where in the process things are breaking down to identify what solutions an organization needs to put in place.”
During the Joint Commission project, one organization found that patients had inadequate fluid resuscitation due to staff fear of fluid overload, while another organization found they had issues with fluids being disconnected when patients were taken for tests and then not reconnected – different problems that needed different solutions.
The Joint Commission Center for Transforming Healthcare is currently developing a Targeted Solutions Tool® (TST®), scheduled for release in 2019, to help organizations determine their issues with sepsis recognition and barriers to meeting sepsis bundle element requirements and implement targeted solutions to address their specific issues. The tool will be available free of charge to all Joint Commission-accredited customers.
Reference
1. “Hospital-Wide Sepsis Project Reduces Mortality by Nearly 25 Percent,” Kelly Barnes, The Joint Commission Center for Transforming Healthcare. 2018, Sep 25.
The CDC estimates that 1.7 million people in the United States acquire sepsis annually; sepsis accounts for nearly 270,000 patient deaths per year.
Decreasing mortality and improving patient outcomes requires early detection and appropriate timely treatment. The Joint Commission Center for Transforming Healthcare’s recent sepsis project demonstrated this by analyzing root causes and reducing sepsis mortality with five leading hospitals by an aggregate of nearly 25%.
“Most organizations can tell you how they are doing with regard to whether or not they are ordering lactates or fluids, but many can’t tell you where in the process these elements are failing,” said Kelly Barnes, Black Belt III, Joint Commission Center for Transforming Healthcare. “For instance, is the issue in ordering lactates, drawing lactates, or getting the results of lactates in a timely manner? The key is to understand where in the process things are breaking down to identify what solutions an organization needs to put in place.”
During the Joint Commission project, one organization found that patients had inadequate fluid resuscitation due to staff fear of fluid overload, while another organization found they had issues with fluids being disconnected when patients were taken for tests and then not reconnected – different problems that needed different solutions.
The Joint Commission Center for Transforming Healthcare is currently developing a Targeted Solutions Tool® (TST®), scheduled for release in 2019, to help organizations determine their issues with sepsis recognition and barriers to meeting sepsis bundle element requirements and implement targeted solutions to address their specific issues. The tool will be available free of charge to all Joint Commission-accredited customers.
Reference
1. “Hospital-Wide Sepsis Project Reduces Mortality by Nearly 25 Percent,” Kelly Barnes, The Joint Commission Center for Transforming Healthcare. 2018, Sep 25.
Just a series of fortunate events?
Building a career in hospital medicine
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Building a career in hospital medicine
Building a career in hospital medicine
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Residents and junior faculty have frequently asked me how they can attain a position similar to mine, focused on quality and leadership in a health care system. When I was first asked to offer advice on this topic, my response was generally something like, “Heck if I know! I just had a series of lucky accidents to get here!”
Back then, I would recount my career history. I established myself as a clinician educator and associate program director soon after Chief Residency. After that, I would explain, a series of fortunate events and health care trends shaped my career. Evidence-based medicine (EBM), the patient safety movement, a shift to incorporate value (as well as volume) into reimbursement models, and the hospital medicine movement all emerged in interesting and often synergistic ways.
A young SHM organization (then known as NAIP) grew rapidly even while the hospitalist programs I led in Phoenix, then at University of California, San Diego, grew in size and influence. Inevitably, it seemed, I was increasingly involved in quality improvement (QI) efforts, and began to publish and speak about them. Collaborative work with SHM and a number of hospital systems broadened my visibility regionally and nationally. Finally, in 2015, I was recruited away from UC San Diego into a new position, as chief quality officer at UC Davis.
On hearing this history, those seeking my sage advice would look a little confused, and then say something like, “So your advice is that I should get lucky??? Gee, thanks a lot! Really helpful!” (Insert sarcasm here).
The honor of being asked to contribute to the “Legacies” series in The Hospitalist gave me an opportunity to think about this a little differently. No one really wanted to know about how past changes in the health care environment led to my career success. They wanted advice on tools and strategies that will allow them to thrive in an environment of ongoing, disruptive change that is likely only going to accelerate. I now present my upgraded points of advice, intertwined with examples of how SHM positively influenced my career (and could assist yours):
Learn how your hospital works. Hospitalists obviously have an inside track on many aspects of hospital operations, but sometimes remain oblivious to the organizational and committee structure, priorities of hospital leadership, and the mechanism for implementing standardized care. Knowing where to go with new ideas, and the process of implementing protocols, will keep you from hitting political land mines and unintentionally encroaching on someone else’s turf, while aligning your efforts with institutional priorities improves the buy-in and resources available to do the work.
Start small, but think big. Don’t bite off more than you can chew, and make sure your ideas for change work on a small scale before trying to sell the world on them. On the other hand, think big! The care you and others provide is dependent on systems that go far beyond your immediate control. Policies, protocols, standardized order sets, checklists, and an array of other tools can be leveraged to influence care across an entire health system, and in the SHM Mentored Implementation programs, can impact hundreds of hospitals.
Broaden your skills. Commit to learning new skills that can increase your impact and career diversity. Procedural skills; information technology; and EMR, EBM, research, public health, QI, business, leadership, public speaking, advocacy, and telehealth, can all open up a whole world of possibilities when combined with a medical degree. These skills can move you into areas that keep you engaged and excited to go to work.
Engage in mentor/mentee relationships. As an associate program director and clinician-educator, I had a lot of opportunity to mentor residents and fellows. It is so rewarding to watch the mentee grow in experience and skills, and to eventually see many of them assume leadership and mentoring roles themselves. You don’t have to be in a teaching position to act as a mentor (my experience mentoring hospitalists and others in leadership and quality improvement now far surpasses my experience with house staff).
The mentor often benefits as much as the mentee from this relationship. I have been inspired by their passion and dedication, educated by their ideas and innovation, and frequently find I am learning more from them, than they are from me. I have had great experiences in the SHM Mentored Implementation program in the role of mentee and mentor.
Participate in a community. When I first joined NAIP, I was amazed that the giants (Wachter, Nelson, Whitcomb, Holman, Williams, Greeno, Howell, Huddleston, Wellikson, and on and on) were not only approachable, they were warm, friendly, interesting, and extraordinarily welcoming. The ever-expanding and evolving community at SHM continues that tradition and offers a forum to share innovative work, discuss common problems and solutions, contact world experts, or just find an empathetic ear. Working on toolkits and collaborative efforts with this community remains a real highlight of my career, and the source of several lasting friendships. So don’t be shy; step right up; and introduce yourself!
Avoid my past mistakes (this might be a long list). Random things you should try to avoid.
- Tribalism – It is natural to be protective of your hospitalist group, and to focus on the injustices heaped upon you from (insert favorite punching bag here, e.g., ED, orthopedists, cardiologists, nursing staff, evil administration penny pinchers, etc). While some of those injustices might be real, tribalism, defensiveness, and circling the wagons generally only makes things worse. Sit down face to face, learn a little bit about the opposing tribe (both about their work, and about them as people), and see how much more fun and productive work can be.
- Storming out of a meeting with the CMO and CEO, slamming the door, etc. – not productive. Administrative leaders are doing their own juggling act and are generally well intentioned and doing the best they can. Respect that, argue your case, but if things don’t pan out, shake their hand, and live to fight another day.
- Using e-mail (evil-mail) to resolve conflict – And if you’re a young whippersnapper, don’t use Twitter, Facebook, Snapchat, or other social media to address conflict either!
- Forgetting to put patients first – Frame decisions for your group around what best serves your patients, not your doctors. Long term, this gives your group credibility and will serve the hospitalists better as well. SHM does this on a large scale with their advocacy efforts, resulting in more credibility and influence on Capitol Hill.
Make time for friends, family, fitness, fun, and reflection. A sense of humor and an occasional laugh when dealing with ill patients, hospital medicine politics, and the EMR all day provides resilience, as does taking the time to foster self-awareness and insight into your own weaknesses, strengths, and how you react to different stressors. A little bit of exercise and time with family and friends can go a long way towards improving your outlook, work, and life in general, while reducing burnout. Oh yeah, it’s also a good idea to choose a great life partner as well. Thanks Michelle!
Dr. Maynard is chief quality officer, University of California Davis Medical Center, Sacramento, Calif.
Most measles cases in 25 years prompts government pleas to vaccinate
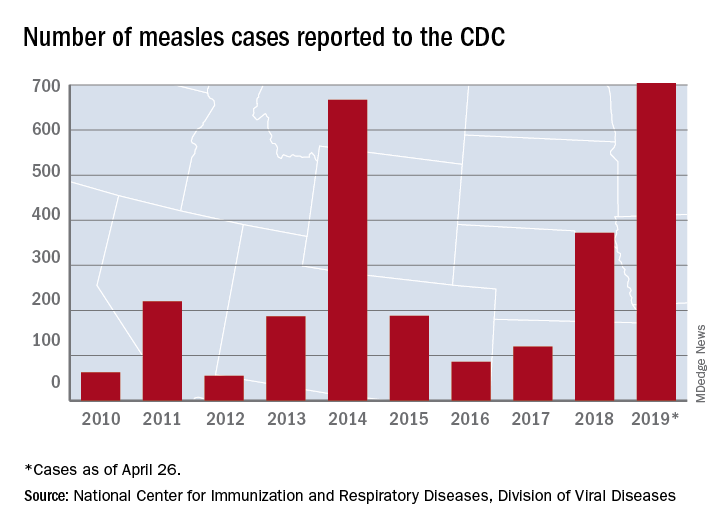
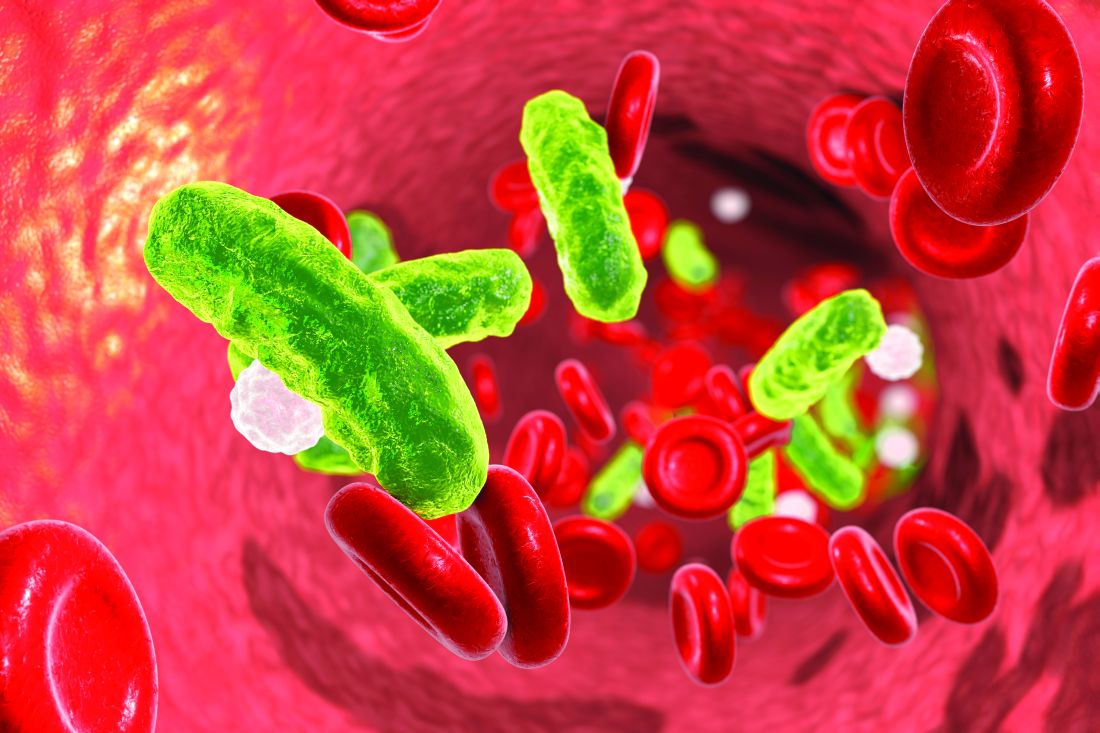
The updated figure adds 9 cases to the previous tally of 695 cases as of April 24, when the CDC announced that the number of cases in 2019 had surpassed the total for any year since the disease was considered effectively eliminated from the country in 2000.
Cases have been reported in 22 states, with the largest outbreaks in Washington and New York. The outbreak in Washington, which included 72 cases, was declared over last week. Two outbreaks in New York, however, are the largest and longest-lasting measles outbreaks since the disease was considered eliminated, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. The longer they continue, the “greater the chance that measles will again gain a foothold in the United States,” she said at CDC telebriefing on measles.
The outbreaks are linked to travelers who are exposed to measles abroad and bring it to the United States. The disease then may spread, especially in communities with high rates of unvaccinated people. “A significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine,” according to the CDC.
National Infant Immunization Week
Until last week, 2014 – with 667 measles cases – had been the year with the most cases since the disease was effectively eliminated. The last time the United States had more measles cases was in 1994, when there were 963 cases for the year.
Health and Human Services Secretary Alex Azar, also at the telebriefing, pointed out that 1994 also was the year that the United States first observed National Infant Immunization Week, which is April 27–May 4 this year. The CDC is marking the 25th anniversary of the annual observance, which highlights “the importance of protecting infants from vaccine-preventable diseases” and celebrates “the achievements of immunization programs in promoting healthy communities,” Secretary Azar said.
Message to health care providers
CDC director Robert Redfield Jr., MD, noted that measles has “no treatment, no cure, and no way to predict how bad a case will be.”
Some patients may have mild symptoms, whereas others may have serious complications such as pneumonia or encephalitis. In 2019, 3% of the patients with measles have developed pneumonia, he said. No patients have died.
Dr. Redfield, a virologist, noted that the CDC is recommending that children aged 6-12 months receive 1 dose of the measles vaccine if traveling abroad.
“As CDC director and as a physician, I have and continue to wholeheartedly advocate for infant immunization,” he said in a statement. “More importantly, as a father and grandfather I have ensured all of my children and grandchildren are vaccinated on the recommended schedule. Vaccines are safe. Vaccines do not cause autism. Vaccine-preventable diseases are dangerous.”
More than 94% of parents vaccinate their children, Dr. Redfield added. “CDC is working to reach the small percentage of vaccine-hesitant individuals so they too understand the importance of vaccines. It is imperative that we correct misinformation and reassure fearful parents so they protect their children from illnesses with long-lasting health impacts.”
About 1.3%, or 100,000 children, in the United States under 2 years old have not been vaccinated, he said.
“I call upon health care providers to encourage parents and expectant parents to vaccinate their children for their own protection and to avoid the spread of vaccine-preventable diseases within their families and communities,” he said. “We must join together as a nation to once again eliminate measles and prevent future disease outbreaks.”
The CDC has a complete list of clinical recommendations for health care providers on its website.
The president weighs in
President Donald Trump said that children should receive vaccinations – his first public comment about vaccines since his inauguration. Previously, he had questioned the safety of vaccines.
Asked by reporters about the measles outbreaks and his message for parents about having their kids vaccinated, he said: “They have to get the shot. The vaccinations are so important. This is really going around now. They have to get their shots.”
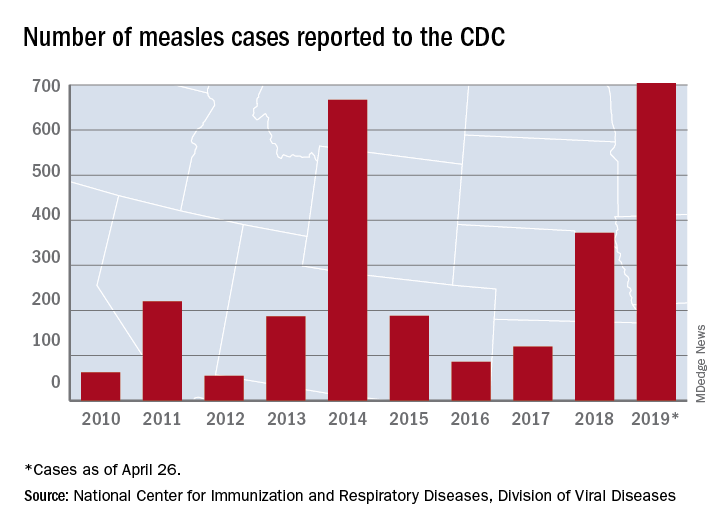
The updated figure adds 9 cases to the previous tally of 695 cases as of April 24, when the CDC announced that the number of cases in 2019 had surpassed the total for any year since the disease was considered effectively eliminated from the country in 2000.
Cases have been reported in 22 states, with the largest outbreaks in Washington and New York. The outbreak in Washington, which included 72 cases, was declared over last week. Two outbreaks in New York, however, are the largest and longest-lasting measles outbreaks since the disease was considered eliminated, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. The longer they continue, the “greater the chance that measles will again gain a foothold in the United States,” she said at CDC telebriefing on measles.
The outbreaks are linked to travelers who are exposed to measles abroad and bring it to the United States. The disease then may spread, especially in communities with high rates of unvaccinated people. “A significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine,” according to the CDC.
National Infant Immunization Week
Until last week, 2014 – with 667 measles cases – had been the year with the most cases since the disease was effectively eliminated. The last time the United States had more measles cases was in 1994, when there were 963 cases for the year.
Health and Human Services Secretary Alex Azar, also at the telebriefing, pointed out that 1994 also was the year that the United States first observed National Infant Immunization Week, which is April 27–May 4 this year. The CDC is marking the 25th anniversary of the annual observance, which highlights “the importance of protecting infants from vaccine-preventable diseases” and celebrates “the achievements of immunization programs in promoting healthy communities,” Secretary Azar said.
Message to health care providers
CDC director Robert Redfield Jr., MD, noted that measles has “no treatment, no cure, and no way to predict how bad a case will be.”
Some patients may have mild symptoms, whereas others may have serious complications such as pneumonia or encephalitis. In 2019, 3% of the patients with measles have developed pneumonia, he said. No patients have died.
Dr. Redfield, a virologist, noted that the CDC is recommending that children aged 6-12 months receive 1 dose of the measles vaccine if traveling abroad.
“As CDC director and as a physician, I have and continue to wholeheartedly advocate for infant immunization,” he said in a statement. “More importantly, as a father and grandfather I have ensured all of my children and grandchildren are vaccinated on the recommended schedule. Vaccines are safe. Vaccines do not cause autism. Vaccine-preventable diseases are dangerous.”
More than 94% of parents vaccinate their children, Dr. Redfield added. “CDC is working to reach the small percentage of vaccine-hesitant individuals so they too understand the importance of vaccines. It is imperative that we correct misinformation and reassure fearful parents so they protect their children from illnesses with long-lasting health impacts.”
About 1.3%, or 100,000 children, in the United States under 2 years old have not been vaccinated, he said.
“I call upon health care providers to encourage parents and expectant parents to vaccinate their children for their own protection and to avoid the spread of vaccine-preventable diseases within their families and communities,” he said. “We must join together as a nation to once again eliminate measles and prevent future disease outbreaks.”
The CDC has a complete list of clinical recommendations for health care providers on its website.
The president weighs in
President Donald Trump said that children should receive vaccinations – his first public comment about vaccines since his inauguration. Previously, he had questioned the safety of vaccines.
Asked by reporters about the measles outbreaks and his message for parents about having their kids vaccinated, he said: “They have to get the shot. The vaccinations are so important. This is really going around now. They have to get their shots.”
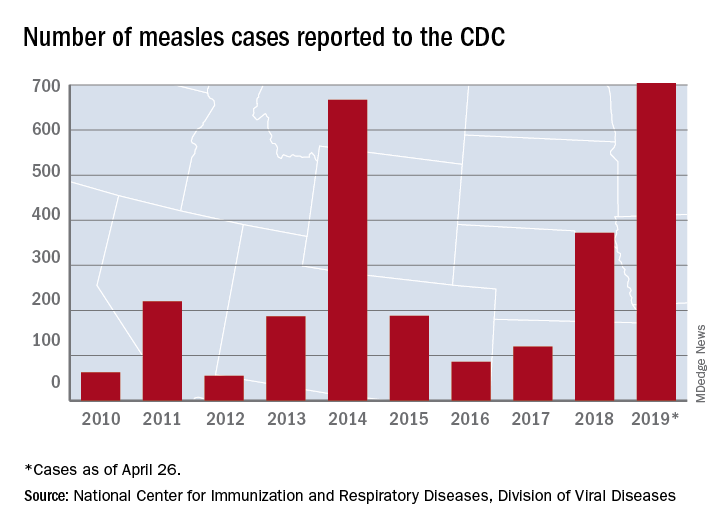
The updated figure adds 9 cases to the previous tally of 695 cases as of April 24, when the CDC announced that the number of cases in 2019 had surpassed the total for any year since the disease was considered effectively eliminated from the country in 2000.
Cases have been reported in 22 states, with the largest outbreaks in Washington and New York. The outbreak in Washington, which included 72 cases, was declared over last week. Two outbreaks in New York, however, are the largest and longest-lasting measles outbreaks since the disease was considered eliminated, said Nancy Messonnier, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases. The longer they continue, the “greater the chance that measles will again gain a foothold in the United States,” she said at CDC telebriefing on measles.
The outbreaks are linked to travelers who are exposed to measles abroad and bring it to the United States. The disease then may spread, especially in communities with high rates of unvaccinated people. “A significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine,” according to the CDC.
National Infant Immunization Week
Until last week, 2014 – with 667 measles cases – had been the year with the most cases since the disease was effectively eliminated. The last time the United States had more measles cases was in 1994, when there were 963 cases for the year.
Health and Human Services Secretary Alex Azar, also at the telebriefing, pointed out that 1994 also was the year that the United States first observed National Infant Immunization Week, which is April 27–May 4 this year. The CDC is marking the 25th anniversary of the annual observance, which highlights “the importance of protecting infants from vaccine-preventable diseases” and celebrates “the achievements of immunization programs in promoting healthy communities,” Secretary Azar said.
Message to health care providers
CDC director Robert Redfield Jr., MD, noted that measles has “no treatment, no cure, and no way to predict how bad a case will be.”
Some patients may have mild symptoms, whereas others may have serious complications such as pneumonia or encephalitis. In 2019, 3% of the patients with measles have developed pneumonia, he said. No patients have died.
Dr. Redfield, a virologist, noted that the CDC is recommending that children aged 6-12 months receive 1 dose of the measles vaccine if traveling abroad.
“As CDC director and as a physician, I have and continue to wholeheartedly advocate for infant immunization,” he said in a statement. “More importantly, as a father and grandfather I have ensured all of my children and grandchildren are vaccinated on the recommended schedule. Vaccines are safe. Vaccines do not cause autism. Vaccine-preventable diseases are dangerous.”
More than 94% of parents vaccinate their children, Dr. Redfield added. “CDC is working to reach the small percentage of vaccine-hesitant individuals so they too understand the importance of vaccines. It is imperative that we correct misinformation and reassure fearful parents so they protect their children from illnesses with long-lasting health impacts.”
About 1.3%, or 100,000 children, in the United States under 2 years old have not been vaccinated, he said.
“I call upon health care providers to encourage parents and expectant parents to vaccinate their children for their own protection and to avoid the spread of vaccine-preventable diseases within their families and communities,” he said. “We must join together as a nation to once again eliminate measles and prevent future disease outbreaks.”
The CDC has a complete list of clinical recommendations for health care providers on its website.
The president weighs in
President Donald Trump said that children should receive vaccinations – his first public comment about vaccines since his inauguration. Previously, he had questioned the safety of vaccines.
Asked by reporters about the measles outbreaks and his message for parents about having their kids vaccinated, he said: “They have to get the shot. The vaccinations are so important. This is really going around now. They have to get their shots.”
FROM A CDC TELEBRIEFING
Combo respiratory pathogen tests miss pertussis
BALTIMORE – Ann Arbor.
Respiratory pathogen panels are popular because they test for many things at once, but providers have to know their limits, said lead investigator Colleen Mayhew, MD, a pediatric emergency medicine fellow at the University of Michigan.
“Should RPAN be used to diagnosis pertussis? No,” she said at the Pediatric Academic Societies annual meeting. RPAN was negative for confirmed pertussis 44% of the time in the study.
“In our cohort, [it] was no better than a coin flip for detecting pertussis,” she said. Also, even when it missed pertussis, it still detected other pathogens, which raises the risk that symptoms might be attributed to a different infection. “This has serious public health implications.”
“The bottom line is, if you are concerned about pertussis, it’s important to use a dedicated pertussis PCR [polymerase chain reaction] assay, and to use comprehensive respiratory pathogen testing only if there are other, specific targets that will change your clinical management,” such as mycoplasma or the flu, Dr. Mayhew said.
In the study, 102 nasopharyngeal swabs positive for pertussis on standalone PCR testing – the university uses an assay from Focus Diagnostics – were thawed and tested with RPAN.
RPAN was negative for pertussis on 45 swabs (44%). “These are the potential missed pertussis cases if RPAN is used alone,” Dr. Mayhew said. RPAN detected other pathogens, such as coronavirus, about half the time, whether or not it tested positive for pertussis. “Those additional pathogens might represent coinfection, but might also represent asymptomatic carriage.” It’s impossible to differentiate between the two, she noted.
In short, “neither positive testing for other respiratory pathogens, nor negative testing for pertussis by RPAN, is reliable for excluding the diagnosis of pertussis. Dedicated pertussis PCR testing should be used for diagnosis,” she and her team concluded.
RPAN also is a PCR test, but with a different, perhaps less robust, genetic target.
The 102 positive swabs were from patients aged 1 month to 73 years, so “it’s important for all of us to keep pertussis on our differential diagnose” no matter how old patients are, Dr. Mayhew said.
Freezing and thawing the swabs shouldn’t have degraded the genetic material, but it might have; that was one of the limits of the study.
The team hopes to run a quality improvement project to encourage the use of standalone pertussis PCR in Ann Arbor.
There was no industry funding. Dr. Mayhew didn’t report any disclosures.
BALTIMORE – Ann Arbor.
Respiratory pathogen panels are popular because they test for many things at once, but providers have to know their limits, said lead investigator Colleen Mayhew, MD, a pediatric emergency medicine fellow at the University of Michigan.
“Should RPAN be used to diagnosis pertussis? No,” she said at the Pediatric Academic Societies annual meeting. RPAN was negative for confirmed pertussis 44% of the time in the study.
“In our cohort, [it] was no better than a coin flip for detecting pertussis,” she said. Also, even when it missed pertussis, it still detected other pathogens, which raises the risk that symptoms might be attributed to a different infection. “This has serious public health implications.”
“The bottom line is, if you are concerned about pertussis, it’s important to use a dedicated pertussis PCR [polymerase chain reaction] assay, and to use comprehensive respiratory pathogen testing only if there are other, specific targets that will change your clinical management,” such as mycoplasma or the flu, Dr. Mayhew said.
In the study, 102 nasopharyngeal swabs positive for pertussis on standalone PCR testing – the university uses an assay from Focus Diagnostics – were thawed and tested with RPAN.
RPAN was negative for pertussis on 45 swabs (44%). “These are the potential missed pertussis cases if RPAN is used alone,” Dr. Mayhew said. RPAN detected other pathogens, such as coronavirus, about half the time, whether or not it tested positive for pertussis. “Those additional pathogens might represent coinfection, but might also represent asymptomatic carriage.” It’s impossible to differentiate between the two, she noted.
In short, “neither positive testing for other respiratory pathogens, nor negative testing for pertussis by RPAN, is reliable for excluding the diagnosis of pertussis. Dedicated pertussis PCR testing should be used for diagnosis,” she and her team concluded.
RPAN also is a PCR test, but with a different, perhaps less robust, genetic target.
The 102 positive swabs were from patients aged 1 month to 73 years, so “it’s important for all of us to keep pertussis on our differential diagnose” no matter how old patients are, Dr. Mayhew said.
Freezing and thawing the swabs shouldn’t have degraded the genetic material, but it might have; that was one of the limits of the study.
The team hopes to run a quality improvement project to encourage the use of standalone pertussis PCR in Ann Arbor.
There was no industry funding. Dr. Mayhew didn’t report any disclosures.
BALTIMORE – Ann Arbor.
Respiratory pathogen panels are popular because they test for many things at once, but providers have to know their limits, said lead investigator Colleen Mayhew, MD, a pediatric emergency medicine fellow at the University of Michigan.
“Should RPAN be used to diagnosis pertussis? No,” she said at the Pediatric Academic Societies annual meeting. RPAN was negative for confirmed pertussis 44% of the time in the study.
“In our cohort, [it] was no better than a coin flip for detecting pertussis,” she said. Also, even when it missed pertussis, it still detected other pathogens, which raises the risk that symptoms might be attributed to a different infection. “This has serious public health implications.”
“The bottom line is, if you are concerned about pertussis, it’s important to use a dedicated pertussis PCR [polymerase chain reaction] assay, and to use comprehensive respiratory pathogen testing only if there are other, specific targets that will change your clinical management,” such as mycoplasma or the flu, Dr. Mayhew said.
In the study, 102 nasopharyngeal swabs positive for pertussis on standalone PCR testing – the university uses an assay from Focus Diagnostics – were thawed and tested with RPAN.
RPAN was negative for pertussis on 45 swabs (44%). “These are the potential missed pertussis cases if RPAN is used alone,” Dr. Mayhew said. RPAN detected other pathogens, such as coronavirus, about half the time, whether or not it tested positive for pertussis. “Those additional pathogens might represent coinfection, but might also represent asymptomatic carriage.” It’s impossible to differentiate between the two, she noted.
In short, “neither positive testing for other respiratory pathogens, nor negative testing for pertussis by RPAN, is reliable for excluding the diagnosis of pertussis. Dedicated pertussis PCR testing should be used for diagnosis,” she and her team concluded.
RPAN also is a PCR test, but with a different, perhaps less robust, genetic target.
The 102 positive swabs were from patients aged 1 month to 73 years, so “it’s important for all of us to keep pertussis on our differential diagnose” no matter how old patients are, Dr. Mayhew said.
Freezing and thawing the swabs shouldn’t have degraded the genetic material, but it might have; that was one of the limits of the study.
The team hopes to run a quality improvement project to encourage the use of standalone pertussis PCR in Ann Arbor.
There was no industry funding. Dr. Mayhew didn’t report any disclosures.
REPORTING FROM PAS 2019
Novel strategies may help curb bariatric SSI
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
BALTIMORE – While rates of surgical site infections after bariatric surgery have been reported in the low single digits, SSIs have continued to be a persistent complication.
At the annual meeting of the Society of American Gastrointestinal Endoscopic Surgeons, researchers reported on two strategies to reduce SSI in bariatric surgery: a predictive tool that identifies risk factors for wound infection, allowing surgeons to employ protective measures before and during surgery, and a change in surgical practice leading to a 78% reduction in wound infection rates that resulted from a single-center study.
Jerry Dang, MD, of the University of Alberta, Edmonton, reported that the BariWound predictive tool designed to stratify patients into risk categories showed a high level of accuracy with an area under the curve of 0.73. Cynthia Weber, MD, of University Hospitals, Cleveland, reported that changing the method for performing circular-stapled gastrojejunostomy (GJ) from the transoral to the transabdominal approach along with more vigilant use of wound protection reduced wound infection rates from 6% to 1.3%.
Dr. Dang noted that SSI has been reported as the most common hospital-acquired complication in bariatric surgery, with reported rates of between 1% and 10%. A 2014 analysis of the American College of Surgeons National Surgical Quality Improvement Program database reported an SSI rate of 1.8% (Surg Endosc. 2014;28:3285-92). Although these rates are low, Dr. Dang explained that his group wanted to identify factors associated with SSI within 30 days of bariatric surgery. They analyzed outcomes data of 274,187 patients in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database who had bariatric surgery in 2015 and 2016 (196,608 by laparoscopic sleeve gastrectomy [SG] and 77,579 laparoscopic Roux-en-Y gastric bypass [RYGB]). Their analysis determined an incisional SSI rate of 0.47% (n = 1,291). “Incisional SSI rates were four times higher for laparoscopic RYGB: 1.04% vs. 0.25%,” Dr. Dang said.
On multivariable logistic regression, the adjusted odds ratio of SSI after RYGB vs. SG was 3.13 (P less than .001). Other significant risk factors were chronic steroid or immunosuppressant use (odds ratio, 1.75; P = .001), female sex (OR, 1.48; P less than .001) and history of gastroesophageal reflux disease (OR, 1.45; P less than .001). Other factors with a 21%-31% greater risk of SSI were white race (P = .002), history of diabetes (P less than .001), hypertension (P less than .001), obstructive sleep apnea (P = .001), and longer operation times (P less than .001). Each single-digit increase in body mass index increased risk by 3%, and older age actually had a protective effect for unknown reasons, Dr. Dang noted.
The BariWound tool assigns points to each risk factor. Each hour of operation time and each 10 kg/m2 of weight carry a value of 1 point, with partial points allowed. RYGB equals 5 points, and chronic steroid/immunosuppressant use, 4 points. The tool assigns risk to four categories based on score and 30-day SSI rate:
- Low, less than 15 (1% risk of SSI).
- Moderate, 15-21.9 (1%-5%).
- High, 22-26.9 (5%-10%).
- Very high, greater than 27 (greater than 10%).
“The BariWound tool can help to inform clinical decision making so patients can know they’re at higher risk, and this could allow for us to target high-risk patients with preventive packages, such as the Cleveland Clinic Technique of wound protection, wound irrigation, and wound packing as a resource-saving measure,” Dr. Dang said. “Targeting high-risk populations can reduce cost and operating time.”
Dr. Weber reported on her institution’s study of SSIs using two different methods for circular stapling of GJ that involved two different surgeons who performed 333 RYGB procedures from January 2016 to March 2018. Surgeon “A” had traditionally used the transoral technique without wound protection to insert the anvil of the stapler; surgeon “B” used wound protection and the transabdominal technique for stapler insertion. Wound protection involves draping of the stapler with sterile plastic.
“In a quarterly review, we detected a higher than expected wound complication rate of 6%,” Dr. Weber said. “Of particular concern was the development of five recent wound infection cases, which all occurred in the transoral group for a rate of 8.9% in that cohort.”
That left the quality team questioning the safety profile of the transoral technique, Dr. Weber said. “We wanted to know why and whether or not the main contributor to the development of a wound infection was the technique for the anvil introduction or was it the difference between surgeons using wound protection.”
Halfway through the study period, surgeon A made two modifications: He adopted the transabdominal technique for a subset of patients; and because of the surgeon’s comfort level and expertise with the transoral approach, he continued using that approach but added wound protection. Surgeon B continued with the transabdominal approach with wound protection. The share of transabdominal insertions in the study population increased from 69.2% before the change to 75% after. Demographics between the pre- and postchange patient populations were similar, as were the rates of revision surgery between the two groups.
“We noticed a significant reduction in total wound complications from 6% to 1.3%, and we noticed a complete elimination of surgical site infections after adding wound protection to the transoral technique,” Dr. Weber said.
Dr. Weber noted a number of limitations with the study: its retrospective nature; the lack of control for other intraoperative factors that contribute to SSIs; relatively low incidence of SSI; and surgeon’s choice to determine the technique of anvil insertion.
“We found that our quality improvement intervention was efficacious and decided that it was not the technique of anvil insertion, but it was the wound protection that was key to preventing wound infections, as we saw complete elimination after we added wound protection to the transoral technique,” Dr. Weber said. “Using proper precautions with the circular stapler and anastomosis can be done using either technique for anvil insertion. Overall self-assessment of outcomes leads to best practice.”
Dr. Dang had no financial relationships to disclose. Dr. Weber’s coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
SOURCES: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
REPORTING FROM SAGES 2019
Key clinical point: .
Major findings: The BariWound predictive model had an accuracy of area under the curve of 0.73; wound infection rates decreased from 6% to 1.3% after the change in practice.
Study details: Analysis of 274,187 cases from the 2015 MBSAQIP database; and a retrospective analysis of 333 bariatric cases performed from January 2016 to March 2018 at a single center.
Disclosures: Dr. Dang has no relationships to disclose. Dr. Weber has no disclosures, although coauthor Leena Khatian, MD, MPH, disclosed relationships with Torax Medical, Medtronic, and Gore.
Sources: Weber C et al. SAGES 2109, Presentation S049; Dang J et al. SAGES 2019, Presentation S050.
Long-term antibiotic use may heighten stroke, CHD risk
, according to a study in the European Heart Journal.
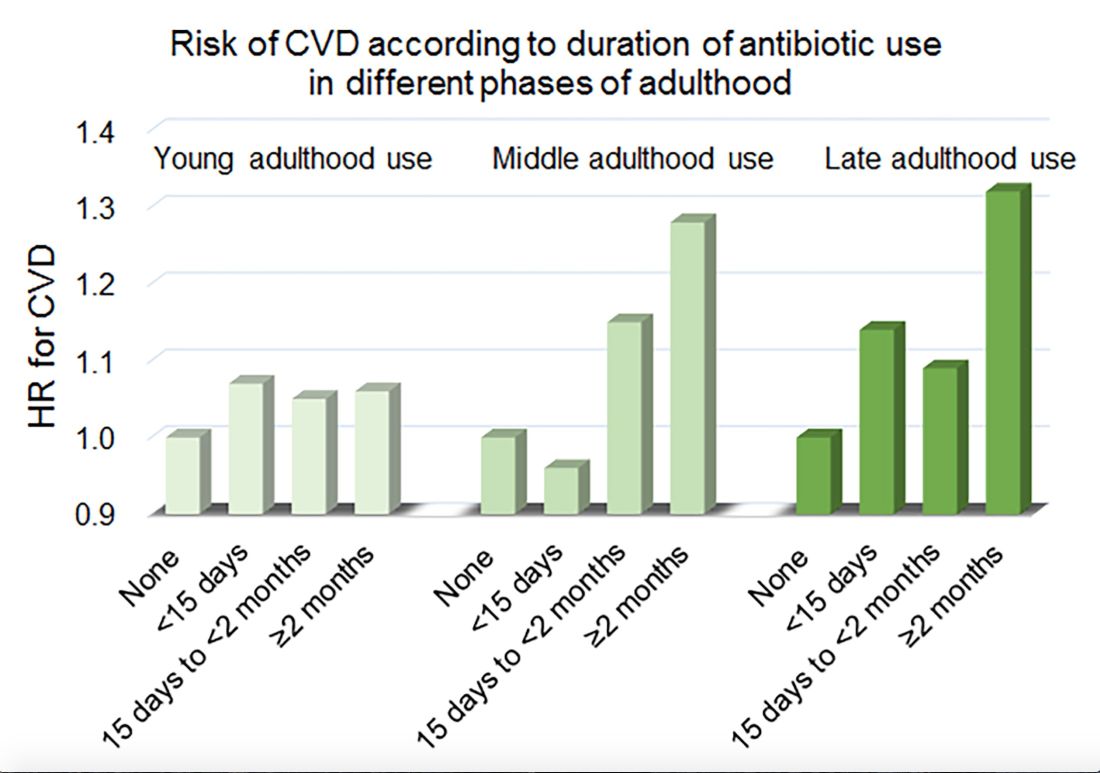
Women in the Nurses’ Health Study who used antibiotics for 2 or more months between ages 40 and 59 years or at age 60 years and older had a significantly increased risk of cardiovascular disease, compared with those who did not use antibiotics. Antibiotic use between 20 and 39 years old was not significantly related to cardiovascular disease.
Prior research has found that antibiotics may have long-lasting effects on gut microbiota and relate to cardiovascular disease risk.
“Antibiotic use is the most critical factor in altering the balance of microorganisms in the gut,” said lead investigator Lu Qi, MD, PhD, in a news release. “Previous studies have shown a link between alterations in the microbiotic environment of the gut and inflammation and narrowing of the blood vessels, stroke, and heart disease,” said Dr. Qi, who is the director of the Tulane University Obesity Research Center in New Orleans and an adjunct professor of nutrition at Harvard T.C. Chan School of Public Health in Boston.
To evaluate associations between life stage, antibiotic exposure, and subsequent cardiovascular disease, researchers analyzed data from 36,429 participants in the Nurses’ Health Study. The women were at least 60 years old and had no history of cardiovascular disease or cancer when they completed a 2004 questionnaire about antibiotic usage during young, middle, and late adulthood. The questionnaire asked participants to indicate the total time using antibiotics with eight categories ranging from none to 5 or more years.
The researchers defined incident cardiovascular disease as a composite endpoint of coronary heart disease (nonfatal myocardial infarction or fatal coronary heart disease) and stroke (nonfatal or fatal). They calculated person-years of follow-up from the questionnaire return date until date of cardiovascular disease diagnosis, death, or end of follow-up in 2012.
Women with longer duration of antibiotic use were more likely to use other medications and have unfavorable cardiovascular risk profiles, including family history of myocardial infarction and higher body mass index. Antibiotics most often were used to treat respiratory infections. During an average follow-up of 7.6 years, 1,056 participants developed cardiovascular disease.
In a multivariable model that adjusted for demographics, diet, lifestyle, reason for antibiotic use, medications, overweight status, and other factors, long-term antibiotic use – 2 months or more – in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Although antibiotic use was self-reported, which could lead to misclassification, the participants were health professionals, which may mitigate this limitation, the authors noted. Whether these findings apply to men and other populations requires further study, they said.
Because of the study’s observational design, the results “cannot show that antibiotics cause heart disease and stroke, only that there is a link between them,” Dr. Qi said. “It’s possible that women who reported more antibiotic use might be sicker in other ways that we were unable to measure, or there may be other factors that could affect the results that we have not been able take account of.”
“Our study suggests that antibiotics should be used only when they are absolutely needed,” he concluded. “Considering the potentially cumulative adverse effects, the shorter time of antibiotic use the better.”
The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
SOURCE: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
, according to a study in the European Heart Journal.
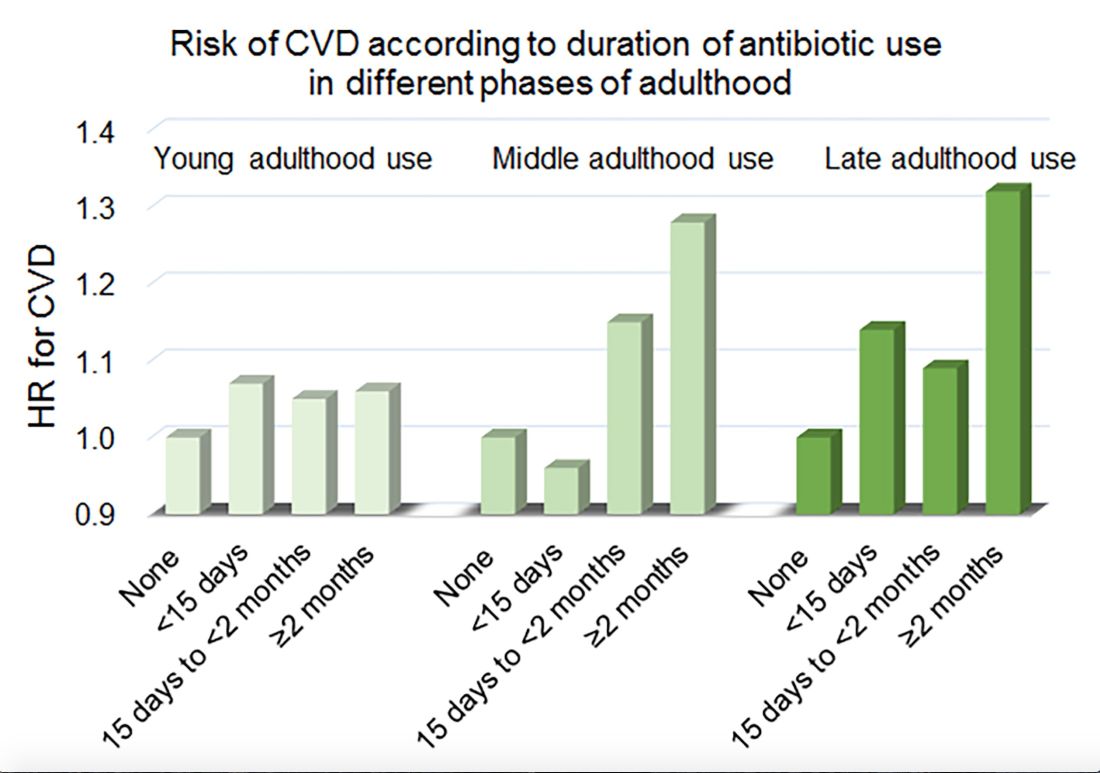
Women in the Nurses’ Health Study who used antibiotics for 2 or more months between ages 40 and 59 years or at age 60 years and older had a significantly increased risk of cardiovascular disease, compared with those who did not use antibiotics. Antibiotic use between 20 and 39 years old was not significantly related to cardiovascular disease.
Prior research has found that antibiotics may have long-lasting effects on gut microbiota and relate to cardiovascular disease risk.
“Antibiotic use is the most critical factor in altering the balance of microorganisms in the gut,” said lead investigator Lu Qi, MD, PhD, in a news release. “Previous studies have shown a link between alterations in the microbiotic environment of the gut and inflammation and narrowing of the blood vessels, stroke, and heart disease,” said Dr. Qi, who is the director of the Tulane University Obesity Research Center in New Orleans and an adjunct professor of nutrition at Harvard T.C. Chan School of Public Health in Boston.
To evaluate associations between life stage, antibiotic exposure, and subsequent cardiovascular disease, researchers analyzed data from 36,429 participants in the Nurses’ Health Study. The women were at least 60 years old and had no history of cardiovascular disease or cancer when they completed a 2004 questionnaire about antibiotic usage during young, middle, and late adulthood. The questionnaire asked participants to indicate the total time using antibiotics with eight categories ranging from none to 5 or more years.
The researchers defined incident cardiovascular disease as a composite endpoint of coronary heart disease (nonfatal myocardial infarction or fatal coronary heart disease) and stroke (nonfatal or fatal). They calculated person-years of follow-up from the questionnaire return date until date of cardiovascular disease diagnosis, death, or end of follow-up in 2012.
Women with longer duration of antibiotic use were more likely to use other medications and have unfavorable cardiovascular risk profiles, including family history of myocardial infarction and higher body mass index. Antibiotics most often were used to treat respiratory infections. During an average follow-up of 7.6 years, 1,056 participants developed cardiovascular disease.
In a multivariable model that adjusted for demographics, diet, lifestyle, reason for antibiotic use, medications, overweight status, and other factors, long-term antibiotic use – 2 months or more – in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Although antibiotic use was self-reported, which could lead to misclassification, the participants were health professionals, which may mitigate this limitation, the authors noted. Whether these findings apply to men and other populations requires further study, they said.
Because of the study’s observational design, the results “cannot show that antibiotics cause heart disease and stroke, only that there is a link between them,” Dr. Qi said. “It’s possible that women who reported more antibiotic use might be sicker in other ways that we were unable to measure, or there may be other factors that could affect the results that we have not been able take account of.”
“Our study suggests that antibiotics should be used only when they are absolutely needed,” he concluded. “Considering the potentially cumulative adverse effects, the shorter time of antibiotic use the better.”
The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
SOURCE: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
, according to a study in the European Heart Journal.
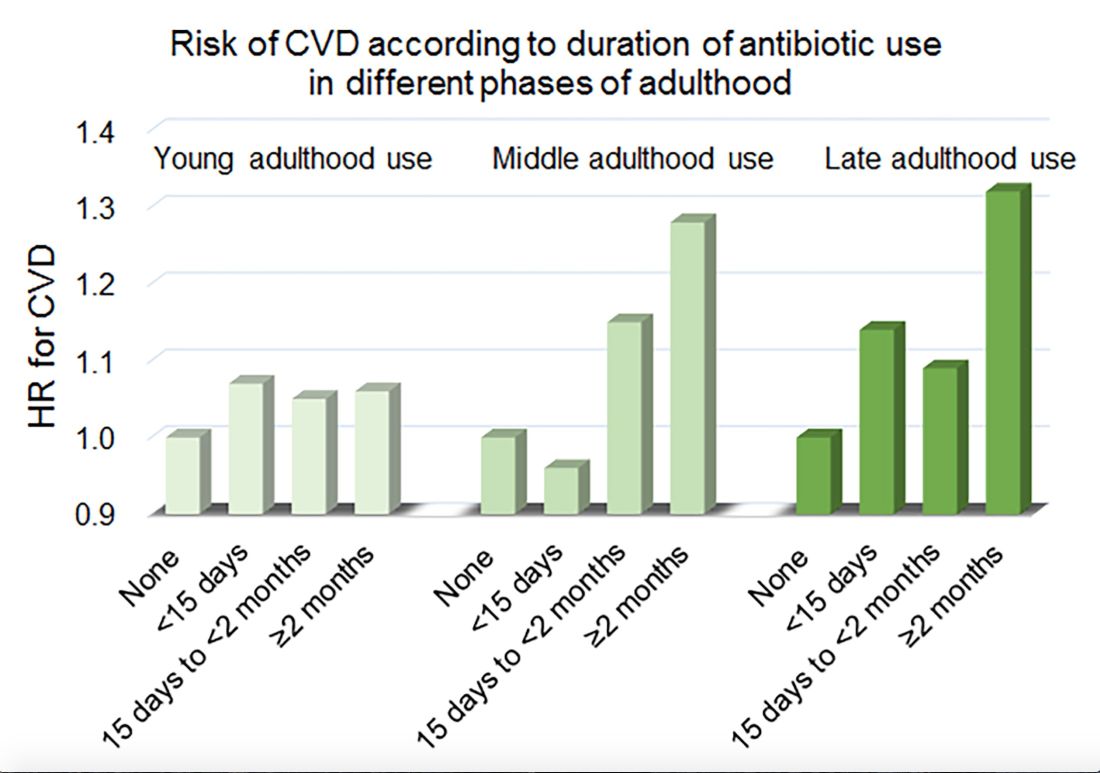
Women in the Nurses’ Health Study who used antibiotics for 2 or more months between ages 40 and 59 years or at age 60 years and older had a significantly increased risk of cardiovascular disease, compared with those who did not use antibiotics. Antibiotic use between 20 and 39 years old was not significantly related to cardiovascular disease.
Prior research has found that antibiotics may have long-lasting effects on gut microbiota and relate to cardiovascular disease risk.
“Antibiotic use is the most critical factor in altering the balance of microorganisms in the gut,” said lead investigator Lu Qi, MD, PhD, in a news release. “Previous studies have shown a link between alterations in the microbiotic environment of the gut and inflammation and narrowing of the blood vessels, stroke, and heart disease,” said Dr. Qi, who is the director of the Tulane University Obesity Research Center in New Orleans and an adjunct professor of nutrition at Harvard T.C. Chan School of Public Health in Boston.
To evaluate associations between life stage, antibiotic exposure, and subsequent cardiovascular disease, researchers analyzed data from 36,429 participants in the Nurses’ Health Study. The women were at least 60 years old and had no history of cardiovascular disease or cancer when they completed a 2004 questionnaire about antibiotic usage during young, middle, and late adulthood. The questionnaire asked participants to indicate the total time using antibiotics with eight categories ranging from none to 5 or more years.
The researchers defined incident cardiovascular disease as a composite endpoint of coronary heart disease (nonfatal myocardial infarction or fatal coronary heart disease) and stroke (nonfatal or fatal). They calculated person-years of follow-up from the questionnaire return date until date of cardiovascular disease diagnosis, death, or end of follow-up in 2012.
Women with longer duration of antibiotic use were more likely to use other medications and have unfavorable cardiovascular risk profiles, including family history of myocardial infarction and higher body mass index. Antibiotics most often were used to treat respiratory infections. During an average follow-up of 7.6 years, 1,056 participants developed cardiovascular disease.
In a multivariable model that adjusted for demographics, diet, lifestyle, reason for antibiotic use, medications, overweight status, and other factors, long-term antibiotic use – 2 months or more – in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Although antibiotic use was self-reported, which could lead to misclassification, the participants were health professionals, which may mitigate this limitation, the authors noted. Whether these findings apply to men and other populations requires further study, they said.
Because of the study’s observational design, the results “cannot show that antibiotics cause heart disease and stroke, only that there is a link between them,” Dr. Qi said. “It’s possible that women who reported more antibiotic use might be sicker in other ways that we were unable to measure, or there may be other factors that could affect the results that we have not been able take account of.”
“Our study suggests that antibiotics should be used only when they are absolutely needed,” he concluded. “Considering the potentially cumulative adverse effects, the shorter time of antibiotic use the better.”
The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
SOURCE: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
FROM THE EUROPEAN HEART JOURNAL
Key clinical point: Among middle-aged and older women, 2 or more months’ exposure to antibiotics is associated with an increased risk of coronary heart disease or stroke.
Major finding: Long-term antibiotic use in late adulthood was associated with significantly increased risk of cardiovascular disease (hazard ratio, 1.32), as was long-term antibiotic use in middle adulthood (HR, 1.28).
Study details: An analysis of data from nearly 36,500 women in the Nurses’ Health Study.
Disclosures: The study was supported by National Institutes of Health grants, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. One author received support from the Japan Society for the Promotion of Science. The authors had no conflicts of interest.
Source: Heianza Y et al. Eur Heart J. 2019 Apr 24. doi: 10.1093/eurheartj/ehz231.
Utilizing mentorship to achieve equity in leadership
Academic medicine and the health care industry
Achieving equity in leadership in academic medicine and the health care industry doesn’t have to be a pipe dream. There are clear, actionable steps that will lead us there.
The benefits of diversity are numerous and well documented. Diversity brings competitive advantage to organizations and strength to teams. With academic health centers (AHCs) facing continual stressors while at the same time being significant financial contributors to – and anchors in – their communities, ensuring their high performance is critical to society as a whole. To grow, thrive, and be ethical examples to their communities, health centers need the strongest and most innovative leaders who are reflective of the communities that they serve. This means more diversity in leadership positions.
When we look at the facts of the gender makeup of academic medicine and the health care industry, we can clearly see inequity – only 22% of medical school full professors, 18% of medical school department chairs, and 17% of medical school deans are women. Note that it has taken 50 years to get from 0 women deans to the 25 women deans who are now in this role. Only 28% of full and associate professors and 21% of department chairs are nonwhite. In the health care industry, only 13% of CEOs are women. The pace toward equity has been excruciatingly slow, and it’s not only women and underrepresented minorities who lose, but also the AHCs and their communities.
So how do we reach equity? Mentorship is a key pathway to this goal. In a session at Hospital Medicine 2019 (HM19), “What Mentorship Has Meant To Me (And What It Can Do For You): High Impact Stories from Leaders in Hospital Medicine,” fellow panelists and I outlined how mentorship can positively affect your career, define the qualities of effective mentors and mentees, describe the difference between mentorship and sponsorship, and explained how to navigate common pitfalls in mentor-mentee relationships.
We spoke about the responsibility the mentee has in the relationship and the need to “manage up,” a term borrowed from the corporate world, where the mentee takes responsibility for his or her part in the relationship and takes a leadership role in the relationship. The mentee must be an “active participant” in the relationship for the relationship to be successful. We hope that attendees at the session took some key points back to their institutions to open dialogue on strategies to achieve equity through building mentoring relationships.
When I look back on my time in residency and fellowship, I recognize that I was surrounded by people who offered guidance and advice. But once I became a faculty member, that guidance was less apparent, and I struggled in the first few years. It wasn’t until I attended a conference on peer mentoring that I recognized that I didn’t just need a didactic mentor, but that I needed a portfolio of mentors and that I had to take the initiative to actively engage mentorship. So I did, and its effects on my career have been powerful and numerous.
The evidence is there that mentorship can play a major role in advancing careers. Now it is up to the leadership of academic and nonacademic health centers to take the initiative and establish formalized programs in their institutions. We all benefit when we have diversity in leadership – so let’s get there together.
Dr. Spector is executive director, Executive Leadership in Academic Medicine, associate dean of faculty development, Drexel University, Philadelphia.
Academic medicine and the health care industry
Academic medicine and the health care industry
Achieving equity in leadership in academic medicine and the health care industry doesn’t have to be a pipe dream. There are clear, actionable steps that will lead us there.
The benefits of diversity are numerous and well documented. Diversity brings competitive advantage to organizations and strength to teams. With academic health centers (AHCs) facing continual stressors while at the same time being significant financial contributors to – and anchors in – their communities, ensuring their high performance is critical to society as a whole. To grow, thrive, and be ethical examples to their communities, health centers need the strongest and most innovative leaders who are reflective of the communities that they serve. This means more diversity in leadership positions.
When we look at the facts of the gender makeup of academic medicine and the health care industry, we can clearly see inequity – only 22% of medical school full professors, 18% of medical school department chairs, and 17% of medical school deans are women. Note that it has taken 50 years to get from 0 women deans to the 25 women deans who are now in this role. Only 28% of full and associate professors and 21% of department chairs are nonwhite. In the health care industry, only 13% of CEOs are women. The pace toward equity has been excruciatingly slow, and it’s not only women and underrepresented minorities who lose, but also the AHCs and their communities.
So how do we reach equity? Mentorship is a key pathway to this goal. In a session at Hospital Medicine 2019 (HM19), “What Mentorship Has Meant To Me (And What It Can Do For You): High Impact Stories from Leaders in Hospital Medicine,” fellow panelists and I outlined how mentorship can positively affect your career, define the qualities of effective mentors and mentees, describe the difference between mentorship and sponsorship, and explained how to navigate common pitfalls in mentor-mentee relationships.
We spoke about the responsibility the mentee has in the relationship and the need to “manage up,” a term borrowed from the corporate world, where the mentee takes responsibility for his or her part in the relationship and takes a leadership role in the relationship. The mentee must be an “active participant” in the relationship for the relationship to be successful. We hope that attendees at the session took some key points back to their institutions to open dialogue on strategies to achieve equity through building mentoring relationships.
When I look back on my time in residency and fellowship, I recognize that I was surrounded by people who offered guidance and advice. But once I became a faculty member, that guidance was less apparent, and I struggled in the first few years. It wasn’t until I attended a conference on peer mentoring that I recognized that I didn’t just need a didactic mentor, but that I needed a portfolio of mentors and that I had to take the initiative to actively engage mentorship. So I did, and its effects on my career have been powerful and numerous.
The evidence is there that mentorship can play a major role in advancing careers. Now it is up to the leadership of academic and nonacademic health centers to take the initiative and establish formalized programs in their institutions. We all benefit when we have diversity in leadership – so let’s get there together.
Dr. Spector is executive director, Executive Leadership in Academic Medicine, associate dean of faculty development, Drexel University, Philadelphia.
Achieving equity in leadership in academic medicine and the health care industry doesn’t have to be a pipe dream. There are clear, actionable steps that will lead us there.
The benefits of diversity are numerous and well documented. Diversity brings competitive advantage to organizations and strength to teams. With academic health centers (AHCs) facing continual stressors while at the same time being significant financial contributors to – and anchors in – their communities, ensuring their high performance is critical to society as a whole. To grow, thrive, and be ethical examples to their communities, health centers need the strongest and most innovative leaders who are reflective of the communities that they serve. This means more diversity in leadership positions.
When we look at the facts of the gender makeup of academic medicine and the health care industry, we can clearly see inequity – only 22% of medical school full professors, 18% of medical school department chairs, and 17% of medical school deans are women. Note that it has taken 50 years to get from 0 women deans to the 25 women deans who are now in this role. Only 28% of full and associate professors and 21% of department chairs are nonwhite. In the health care industry, only 13% of CEOs are women. The pace toward equity has been excruciatingly slow, and it’s not only women and underrepresented minorities who lose, but also the AHCs and their communities.
So how do we reach equity? Mentorship is a key pathway to this goal. In a session at Hospital Medicine 2019 (HM19), “What Mentorship Has Meant To Me (And What It Can Do For You): High Impact Stories from Leaders in Hospital Medicine,” fellow panelists and I outlined how mentorship can positively affect your career, define the qualities of effective mentors and mentees, describe the difference between mentorship and sponsorship, and explained how to navigate common pitfalls in mentor-mentee relationships.
We spoke about the responsibility the mentee has in the relationship and the need to “manage up,” a term borrowed from the corporate world, where the mentee takes responsibility for his or her part in the relationship and takes a leadership role in the relationship. The mentee must be an “active participant” in the relationship for the relationship to be successful. We hope that attendees at the session took some key points back to their institutions to open dialogue on strategies to achieve equity through building mentoring relationships.
When I look back on my time in residency and fellowship, I recognize that I was surrounded by people who offered guidance and advice. But once I became a faculty member, that guidance was less apparent, and I struggled in the first few years. It wasn’t until I attended a conference on peer mentoring that I recognized that I didn’t just need a didactic mentor, but that I needed a portfolio of mentors and that I had to take the initiative to actively engage mentorship. So I did, and its effects on my career have been powerful and numerous.
The evidence is there that mentorship can play a major role in advancing careers. Now it is up to the leadership of academic and nonacademic health centers to take the initiative and establish formalized programs in their institutions. We all benefit when we have diversity in leadership – so let’s get there together.
Dr. Spector is executive director, Executive Leadership in Academic Medicine, associate dean of faculty development, Drexel University, Philadelphia.
Does BMI affect outcomes after ischemic stroke?
according to research that will be presented at the annual meeting of the American Academy of Neurology.
“One possible explanation is that people who are overweight or obese may have a nutritional reserve that may help them survive during prolonged illness,” said Zuolu Liu, MD, of the University of California, Los Angeles, in a press release. “More research is needed to investigate the relationship between BMI and stroke.”
The obesity paradox was first noted when studies suggested that being overweight improved survival in patients with kidney disease or heart disease. Investigators previously examined whether the obesity paradox is observed in stroke, but their studies were underpowered and produced ambiguous results.
Dr. Liu and colleagues sought to evaluate the relationship between BMI and 90-day outcomes of acute ischemic stroke. They examined data for all participants in the FAST-MAG trial, which studied whether prehospital treatment with magnesium improved disability outcomes of acute ischemic stroke. Dr. Liu and colleagues focused on the outcomes of death, disability or death (that is, modified Rankin Scale score of 2-6), and low stroke-related quality of life (that is, Stroke Impact Scale score less than 70). They analyzed potential relationships with BMI univariately and in multivariate models that adjusted for 12 prognostic variables, such as high blood pressure, high cholesterol, and smoking.
Dr. Liu’s group included 1,033 participants in its study. The population’s mean age was 71 years, and 45.1% of the population was female. Mean National Institutes of Health Stroke Scale (NIHSS) score was 10.6, and mean BMI was 27.5 kg/m2.
The investigators found an inverse association between the risk of death and BMI. Adjusted odds ratios for mortality were 1.67 for underweight participants, 0.85 for overweight participants, 0.54 for obese participants, and 0.38 for severely obese participants, compared with participants of normal weight. Similarly, the risk of disability had a U-shaped relationship with BMI. Odds ratios for disability or death were 1.19 for underweight participants, 0.78 for overweight participants, 0.72 for obese participants, and 0.96 for severely obese participants, compared with participants of normal weight. This relationship was attenuated after adjustment for other prognostic factors, however. Dr. Liu’s group did not find a significant association between BMI and low stroke-related quality of life.
The study was limited by the fact that all participants were from Southern California, which potentially reduced the generalizability of the results. The racial and ethnic composition of the study population, however, is similar to that of the national population, said the researchers.
No study sponsor was reported.
SOURCE: Liu Z et al. AAN 2019, Abstract P3.3-01.
according to research that will be presented at the annual meeting of the American Academy of Neurology.
“One possible explanation is that people who are overweight or obese may have a nutritional reserve that may help them survive during prolonged illness,” said Zuolu Liu, MD, of the University of California, Los Angeles, in a press release. “More research is needed to investigate the relationship between BMI and stroke.”
The obesity paradox was first noted when studies suggested that being overweight improved survival in patients with kidney disease or heart disease. Investigators previously examined whether the obesity paradox is observed in stroke, but their studies were underpowered and produced ambiguous results.
Dr. Liu and colleagues sought to evaluate the relationship between BMI and 90-day outcomes of acute ischemic stroke. They examined data for all participants in the FAST-MAG trial, which studied whether prehospital treatment with magnesium improved disability outcomes of acute ischemic stroke. Dr. Liu and colleagues focused on the outcomes of death, disability or death (that is, modified Rankin Scale score of 2-6), and low stroke-related quality of life (that is, Stroke Impact Scale score less than 70). They analyzed potential relationships with BMI univariately and in multivariate models that adjusted for 12 prognostic variables, such as high blood pressure, high cholesterol, and smoking.
Dr. Liu’s group included 1,033 participants in its study. The population’s mean age was 71 years, and 45.1% of the population was female. Mean National Institutes of Health Stroke Scale (NIHSS) score was 10.6, and mean BMI was 27.5 kg/m2.
The investigators found an inverse association between the risk of death and BMI. Adjusted odds ratios for mortality were 1.67 for underweight participants, 0.85 for overweight participants, 0.54 for obese participants, and 0.38 for severely obese participants, compared with participants of normal weight. Similarly, the risk of disability had a U-shaped relationship with BMI. Odds ratios for disability or death were 1.19 for underweight participants, 0.78 for overweight participants, 0.72 for obese participants, and 0.96 for severely obese participants, compared with participants of normal weight. This relationship was attenuated after adjustment for other prognostic factors, however. Dr. Liu’s group did not find a significant association between BMI and low stroke-related quality of life.
The study was limited by the fact that all participants were from Southern California, which potentially reduced the generalizability of the results. The racial and ethnic composition of the study population, however, is similar to that of the national population, said the researchers.
No study sponsor was reported.
SOURCE: Liu Z et al. AAN 2019, Abstract P3.3-01.
according to research that will be presented at the annual meeting of the American Academy of Neurology.
“One possible explanation is that people who are overweight or obese may have a nutritional reserve that may help them survive during prolonged illness,” said Zuolu Liu, MD, of the University of California, Los Angeles, in a press release. “More research is needed to investigate the relationship between BMI and stroke.”
The obesity paradox was first noted when studies suggested that being overweight improved survival in patients with kidney disease or heart disease. Investigators previously examined whether the obesity paradox is observed in stroke, but their studies were underpowered and produced ambiguous results.
Dr. Liu and colleagues sought to evaluate the relationship between BMI and 90-day outcomes of acute ischemic stroke. They examined data for all participants in the FAST-MAG trial, which studied whether prehospital treatment with magnesium improved disability outcomes of acute ischemic stroke. Dr. Liu and colleagues focused on the outcomes of death, disability or death (that is, modified Rankin Scale score of 2-6), and low stroke-related quality of life (that is, Stroke Impact Scale score less than 70). They analyzed potential relationships with BMI univariately and in multivariate models that adjusted for 12 prognostic variables, such as high blood pressure, high cholesterol, and smoking.
Dr. Liu’s group included 1,033 participants in its study. The population’s mean age was 71 years, and 45.1% of the population was female. Mean National Institutes of Health Stroke Scale (NIHSS) score was 10.6, and mean BMI was 27.5 kg/m2.
The investigators found an inverse association between the risk of death and BMI. Adjusted odds ratios for mortality were 1.67 for underweight participants, 0.85 for overweight participants, 0.54 for obese participants, and 0.38 for severely obese participants, compared with participants of normal weight. Similarly, the risk of disability had a U-shaped relationship with BMI. Odds ratios for disability or death were 1.19 for underweight participants, 0.78 for overweight participants, 0.72 for obese participants, and 0.96 for severely obese participants, compared with participants of normal weight. This relationship was attenuated after adjustment for other prognostic factors, however. Dr. Liu’s group did not find a significant association between BMI and low stroke-related quality of life.
The study was limited by the fact that all participants were from Southern California, which potentially reduced the generalizability of the results. The racial and ethnic composition of the study population, however, is similar to that of the national population, said the researchers.
No study sponsor was reported.
SOURCE: Liu Z et al. AAN 2019, Abstract P3.3-01.
FROM AAN 2019
Best of RIV highlights practical, innovative projects
Delirium, alcohol detox, and med rec
A project to improve how hospitalists address inpatient delirium, which has led to reductions in length of stay and cost, took center stage in the Best of RIV plenary session at HM19 in March.
The project, conducted at the University of California, San Francisco (UCSF), was presented alongside projects on alcohol detox at the Cleveland Veterans Affairs Medical Center and on medication reconciliation at Brigham and Women’s Hospital in Boston.
“The plenary is the top three of the 1,000 that are out there – so, impressive work,” said Benji Mathews, MD, SFHM, the chair of the Research, Innovations and Vignettes competition.
At UCSF, the project was meant to tackle the huge problem of delirium in the hospital, said Catherine Lau, MD, SFHM, associate professor of medicine there. Each year delirium affects more than 7 million people who are hospitalized, and hospital-acquired delirium is linked with prolonged stays and more emergency department visits and hospital readmissions. But research has found that as many as a third of these hospital-acquired cases can be prevented, Dr. Lau said.
New admissions and transfers – a total of more than 2,800 patients – were assessed for delirium risk, and those deemed high risk were entered into a delirium care plan, aimed at prevention with nonpharmacologic steps such as maximizing their mobility and helping them sleep at night.
All patients also were screened on every nursing shift for delirium, and those diagnosed with the disorder were placed in the delirium care plan, with notification of the patient’s team for treatment.
The average length of stay decreased by 0.8 days (P less than .001), with a decrease of 1.9 days in patients with delirium, compared with outcomes for nearly 2,600 patients before the intervention was implemented, Dr. Lau said. Researchers also found a decrease in $850 spent per patient (P less than .001), with a direct savings to the hospital of a total of $997,000, she said. The 30-day readmission rate also fell significantly, from 18.9% to 15.9% (P = .03).
The screening itself seemed to be the most important factor in the project, Dr. Lau said.
“Just the recognition that their patient was at risk for delirium or actually had delirium really raised awareness,” she said.
The project on alcohol detox used careful risk assessments at emergency department discharge, e-consults, protocols to limit benzodiazepine prescribing, and telephone follow-up to reduce hospital admissions and 30-day readmissions, as well as length of stay.
Researchers used scores on CIWA – a 10-question measurement of the severity of someone’s alcohol withdrawal – and history of complicated alcohol-use withdrawal to determine whether ED patients should be admitted to the floor or sent home with or without prescriptions for gabapentin and lorazepam, said Robert Patrick, MD, a hospitalist at the Cleveland VA.
Perhaps the most innovative feature of the program was using systolic blood pressure and heart rate in addition to CIWA to determine whether someone should receive a benzodiazepine, he said. Someone with a CIWA of 9-12, for instance, would be prescribed one of these drugs only if their vitals were elevated, Dr. Patrick said.
He encouraged other hospitalists to try a similar program at their centers.
“You don’t have to be at a VA to do this,” he said. “And most importantly, you don’t have to have a cooperative ED to do this. You can do this just within your hospitalist group.”
In another presentation, Jeffrey Schnipper MD, MPH, FHM, associate professor of medicine at Harvard Medical School, Boston, described the results from a project in which SHM’s MARQUIS program – an evidence-based “toolkit” on medication reconciliation – was implemented at 18 hospitals. The kit offers a plan to get the best possible medication history, give medication counseling on discharge, and identify patients at risk for medication discrepancies. The 18 sites were coached, with areas of improvement identified.
By months 13-18 of the study period, the number of medication discrepancies had fallen to 0.93 per patient for those who’d received at least one form of intervention, compared with 2.69 per patient among those who’d received none.
“The MARQUIS interventions, including the toolkit and mentored implementation,” Dr. Schnipper said, “are associated with a marked reduction in medication discrepancies.”
Delirium, alcohol detox, and med rec
Delirium, alcohol detox, and med rec
A project to improve how hospitalists address inpatient delirium, which has led to reductions in length of stay and cost, took center stage in the Best of RIV plenary session at HM19 in March.
The project, conducted at the University of California, San Francisco (UCSF), was presented alongside projects on alcohol detox at the Cleveland Veterans Affairs Medical Center and on medication reconciliation at Brigham and Women’s Hospital in Boston.
“The plenary is the top three of the 1,000 that are out there – so, impressive work,” said Benji Mathews, MD, SFHM, the chair of the Research, Innovations and Vignettes competition.
At UCSF, the project was meant to tackle the huge problem of delirium in the hospital, said Catherine Lau, MD, SFHM, associate professor of medicine there. Each year delirium affects more than 7 million people who are hospitalized, and hospital-acquired delirium is linked with prolonged stays and more emergency department visits and hospital readmissions. But research has found that as many as a third of these hospital-acquired cases can be prevented, Dr. Lau said.
New admissions and transfers – a total of more than 2,800 patients – were assessed for delirium risk, and those deemed high risk were entered into a delirium care plan, aimed at prevention with nonpharmacologic steps such as maximizing their mobility and helping them sleep at night.
All patients also were screened on every nursing shift for delirium, and those diagnosed with the disorder were placed in the delirium care plan, with notification of the patient’s team for treatment.
The average length of stay decreased by 0.8 days (P less than .001), with a decrease of 1.9 days in patients with delirium, compared with outcomes for nearly 2,600 patients before the intervention was implemented, Dr. Lau said. Researchers also found a decrease in $850 spent per patient (P less than .001), with a direct savings to the hospital of a total of $997,000, she said. The 30-day readmission rate also fell significantly, from 18.9% to 15.9% (P = .03).
The screening itself seemed to be the most important factor in the project, Dr. Lau said.
“Just the recognition that their patient was at risk for delirium or actually had delirium really raised awareness,” she said.
The project on alcohol detox used careful risk assessments at emergency department discharge, e-consults, protocols to limit benzodiazepine prescribing, and telephone follow-up to reduce hospital admissions and 30-day readmissions, as well as length of stay.
Researchers used scores on CIWA – a 10-question measurement of the severity of someone’s alcohol withdrawal – and history of complicated alcohol-use withdrawal to determine whether ED patients should be admitted to the floor or sent home with or without prescriptions for gabapentin and lorazepam, said Robert Patrick, MD, a hospitalist at the Cleveland VA.
Perhaps the most innovative feature of the program was using systolic blood pressure and heart rate in addition to CIWA to determine whether someone should receive a benzodiazepine, he said. Someone with a CIWA of 9-12, for instance, would be prescribed one of these drugs only if their vitals were elevated, Dr. Patrick said.
He encouraged other hospitalists to try a similar program at their centers.
“You don’t have to be at a VA to do this,” he said. “And most importantly, you don’t have to have a cooperative ED to do this. You can do this just within your hospitalist group.”
In another presentation, Jeffrey Schnipper MD, MPH, FHM, associate professor of medicine at Harvard Medical School, Boston, described the results from a project in which SHM’s MARQUIS program – an evidence-based “toolkit” on medication reconciliation – was implemented at 18 hospitals. The kit offers a plan to get the best possible medication history, give medication counseling on discharge, and identify patients at risk for medication discrepancies. The 18 sites were coached, with areas of improvement identified.
By months 13-18 of the study period, the number of medication discrepancies had fallen to 0.93 per patient for those who’d received at least one form of intervention, compared with 2.69 per patient among those who’d received none.
“The MARQUIS interventions, including the toolkit and mentored implementation,” Dr. Schnipper said, “are associated with a marked reduction in medication discrepancies.”
A project to improve how hospitalists address inpatient delirium, which has led to reductions in length of stay and cost, took center stage in the Best of RIV plenary session at HM19 in March.
The project, conducted at the University of California, San Francisco (UCSF), was presented alongside projects on alcohol detox at the Cleveland Veterans Affairs Medical Center and on medication reconciliation at Brigham and Women’s Hospital in Boston.
“The plenary is the top three of the 1,000 that are out there – so, impressive work,” said Benji Mathews, MD, SFHM, the chair of the Research, Innovations and Vignettes competition.
At UCSF, the project was meant to tackle the huge problem of delirium in the hospital, said Catherine Lau, MD, SFHM, associate professor of medicine there. Each year delirium affects more than 7 million people who are hospitalized, and hospital-acquired delirium is linked with prolonged stays and more emergency department visits and hospital readmissions. But research has found that as many as a third of these hospital-acquired cases can be prevented, Dr. Lau said.
New admissions and transfers – a total of more than 2,800 patients – were assessed for delirium risk, and those deemed high risk were entered into a delirium care plan, aimed at prevention with nonpharmacologic steps such as maximizing their mobility and helping them sleep at night.
All patients also were screened on every nursing shift for delirium, and those diagnosed with the disorder were placed in the delirium care plan, with notification of the patient’s team for treatment.
The average length of stay decreased by 0.8 days (P less than .001), with a decrease of 1.9 days in patients with delirium, compared with outcomes for nearly 2,600 patients before the intervention was implemented, Dr. Lau said. Researchers also found a decrease in $850 spent per patient (P less than .001), with a direct savings to the hospital of a total of $997,000, she said. The 30-day readmission rate also fell significantly, from 18.9% to 15.9% (P = .03).
The screening itself seemed to be the most important factor in the project, Dr. Lau said.
“Just the recognition that their patient was at risk for delirium or actually had delirium really raised awareness,” she said.
The project on alcohol detox used careful risk assessments at emergency department discharge, e-consults, protocols to limit benzodiazepine prescribing, and telephone follow-up to reduce hospital admissions and 30-day readmissions, as well as length of stay.
Researchers used scores on CIWA – a 10-question measurement of the severity of someone’s alcohol withdrawal – and history of complicated alcohol-use withdrawal to determine whether ED patients should be admitted to the floor or sent home with or without prescriptions for gabapentin and lorazepam, said Robert Patrick, MD, a hospitalist at the Cleveland VA.
Perhaps the most innovative feature of the program was using systolic blood pressure and heart rate in addition to CIWA to determine whether someone should receive a benzodiazepine, he said. Someone with a CIWA of 9-12, for instance, would be prescribed one of these drugs only if their vitals were elevated, Dr. Patrick said.
He encouraged other hospitalists to try a similar program at their centers.
“You don’t have to be at a VA to do this,” he said. “And most importantly, you don’t have to have a cooperative ED to do this. You can do this just within your hospitalist group.”
In another presentation, Jeffrey Schnipper MD, MPH, FHM, associate professor of medicine at Harvard Medical School, Boston, described the results from a project in which SHM’s MARQUIS program – an evidence-based “toolkit” on medication reconciliation – was implemented at 18 hospitals. The kit offers a plan to get the best possible medication history, give medication counseling on discharge, and identify patients at risk for medication discrepancies. The 18 sites were coached, with areas of improvement identified.
By months 13-18 of the study period, the number of medication discrepancies had fallen to 0.93 per patient for those who’d received at least one form of intervention, compared with 2.69 per patient among those who’d received none.
“The MARQUIS interventions, including the toolkit and mentored implementation,” Dr. Schnipper said, “are associated with a marked reduction in medication discrepancies.”
Speaking at a conference? Read these tips first
Recently, I was asked to present my top public speaking tips for a group of women leaders. This is a topic near and dear to my heart, and one that I teach a number of groups, from medical students to faculty.
I also benefited from just returning from the Harvard Macy Educators Course, where Victoria Brazil, MD, an experienced emergency medicine physician from Australia, provided her top tips. Here is a mash-up of the top tips to think about for any of the speakers out there among us – with a few shout-outs for the ladies out there. Please add your own!
The Dos
- Do project power: Stand tall with a relaxed stance and shoulders back – posture is everything. This is especially important for women, who may tend to shrink their bodies, or anyone who is short. A powerful messenger is just as important as the power of the message. The same also applies to sitting down, especially if you are on a panel. Do not look like you are falling into the table.
- Do look up: Think about addressing the people in the back, not in the front row. This looks better in photos as well since you are appealing to the large audience and not the front row. Dr. Brazil’s tip came from Cate Blanchett who said that before she gives talks, she literally and physically advises “picking up your crown and put it on your head.” Not only will you feel better, you will look it too.
- Do pause strategically: The human brain needs rest to process what you are about to say. You can ask people to “think of a time” and take a pause. Or “I want you to all think about what I just said for one moment.” And TAKE a moment. But think about Emma’s pause during the March For Your Lives. Pauses are powerful and serve as a way to cement what you are saying for even the most critical crowd. Think about when anyone on their phone pauses, even if you’re on a boring conference call others will wake up and wonder what is going on and are now engaged in the talk.
- Do strategically summarize: Before you end, or in between important sections, say the following: “There are three main things you can do.” Even if someone fell asleep, they will wake up to take note. It’s a way to get folks’ attention back. There is nothing like challenging others to do something.
The Don’ts
- Don’t start with an apology for “not being an expert”: Or whatever you are thinking about apologizing for. The voice in your head does not need to be broadcast to others. Just say thank you after you are introduced, and launch in. Someone has asked you to talk, so bring your own unique expertise and don’t start with undermining yourself!
- Don’t use your slides as a crutch: Make your audience look at you and not your slides. That means at times, you may be talking and your slides will not be moving. Other times, if you are starting with a story, maybe there is no slide behind you and the screen is blacked out. Some of the most powerful moments in a talk are when slides are not being used.
- Don’t stand behind the podium if you can help it. This means ask for a wireless microphone. Most podiums will overwhelm you. If you have to use a podium, go back to the posture in the “dos.” One year, I had a leg injury and definitely used the podium, so obviously there may be times you need to use a podium; even then, try as hard as possible to make sure you are seen.
- Don’t engage grandstanders during Q&A: Invariably, you will get someone who stands up and goes into a long comment that is not a question to hear themselves speak. Insert yourself, say “thank you” and take the next question. If there is not a next question, you can add, “Before I forget, I want to share another question I am often asked which may be of help to you.” Then, answer your own question. You get the final word this way!
Happy speaking! I look forward to seeing you in warmer weather during the spring conference season.
For more posts from the Hospital Leader blog, visit hospitalleader.org.
Recently, I was asked to present my top public speaking tips for a group of women leaders. This is a topic near and dear to my heart, and one that I teach a number of groups, from medical students to faculty.
I also benefited from just returning from the Harvard Macy Educators Course, where Victoria Brazil, MD, an experienced emergency medicine physician from Australia, provided her top tips. Here is a mash-up of the top tips to think about for any of the speakers out there among us – with a few shout-outs for the ladies out there. Please add your own!
The Dos
- Do project power: Stand tall with a relaxed stance and shoulders back – posture is everything. This is especially important for women, who may tend to shrink their bodies, or anyone who is short. A powerful messenger is just as important as the power of the message. The same also applies to sitting down, especially if you are on a panel. Do not look like you are falling into the table.
- Do look up: Think about addressing the people in the back, not in the front row. This looks better in photos as well since you are appealing to the large audience and not the front row. Dr. Brazil’s tip came from Cate Blanchett who said that before she gives talks, she literally and physically advises “picking up your crown and put it on your head.” Not only will you feel better, you will look it too.
- Do pause strategically: The human brain needs rest to process what you are about to say. You can ask people to “think of a time” and take a pause. Or “I want you to all think about what I just said for one moment.” And TAKE a moment. But think about Emma’s pause during the March For Your Lives. Pauses are powerful and serve as a way to cement what you are saying for even the most critical crowd. Think about when anyone on their phone pauses, even if you’re on a boring conference call others will wake up and wonder what is going on and are now engaged in the talk.
- Do strategically summarize: Before you end, or in between important sections, say the following: “There are three main things you can do.” Even if someone fell asleep, they will wake up to take note. It’s a way to get folks’ attention back. There is nothing like challenging others to do something.
The Don’ts
- Don’t start with an apology for “not being an expert”: Or whatever you are thinking about apologizing for. The voice in your head does not need to be broadcast to others. Just say thank you after you are introduced, and launch in. Someone has asked you to talk, so bring your own unique expertise and don’t start with undermining yourself!
- Don’t use your slides as a crutch: Make your audience look at you and not your slides. That means at times, you may be talking and your slides will not be moving. Other times, if you are starting with a story, maybe there is no slide behind you and the screen is blacked out. Some of the most powerful moments in a talk are when slides are not being used.
- Don’t stand behind the podium if you can help it. This means ask for a wireless microphone. Most podiums will overwhelm you. If you have to use a podium, go back to the posture in the “dos.” One year, I had a leg injury and definitely used the podium, so obviously there may be times you need to use a podium; even then, try as hard as possible to make sure you are seen.
- Don’t engage grandstanders during Q&A: Invariably, you will get someone who stands up and goes into a long comment that is not a question to hear themselves speak. Insert yourself, say “thank you” and take the next question. If there is not a next question, you can add, “Before I forget, I want to share another question I am often asked which may be of help to you.” Then, answer your own question. You get the final word this way!
Happy speaking! I look forward to seeing you in warmer weather during the spring conference season.
For more posts from the Hospital Leader blog, visit hospitalleader.org.
Recently, I was asked to present my top public speaking tips for a group of women leaders. This is a topic near and dear to my heart, and one that I teach a number of groups, from medical students to faculty.
I also benefited from just returning from the Harvard Macy Educators Course, where Victoria Brazil, MD, an experienced emergency medicine physician from Australia, provided her top tips. Here is a mash-up of the top tips to think about for any of the speakers out there among us – with a few shout-outs for the ladies out there. Please add your own!
The Dos
- Do project power: Stand tall with a relaxed stance and shoulders back – posture is everything. This is especially important for women, who may tend to shrink their bodies, or anyone who is short. A powerful messenger is just as important as the power of the message. The same also applies to sitting down, especially if you are on a panel. Do not look like you are falling into the table.
- Do look up: Think about addressing the people in the back, not in the front row. This looks better in photos as well since you are appealing to the large audience and not the front row. Dr. Brazil’s tip came from Cate Blanchett who said that before she gives talks, she literally and physically advises “picking up your crown and put it on your head.” Not only will you feel better, you will look it too.
- Do pause strategically: The human brain needs rest to process what you are about to say. You can ask people to “think of a time” and take a pause. Or “I want you to all think about what I just said for one moment.” And TAKE a moment. But think about Emma’s pause during the March For Your Lives. Pauses are powerful and serve as a way to cement what you are saying for even the most critical crowd. Think about when anyone on their phone pauses, even if you’re on a boring conference call others will wake up and wonder what is going on and are now engaged in the talk.
- Do strategically summarize: Before you end, or in between important sections, say the following: “There are three main things you can do.” Even if someone fell asleep, they will wake up to take note. It’s a way to get folks’ attention back. There is nothing like challenging others to do something.
The Don’ts
- Don’t start with an apology for “not being an expert”: Or whatever you are thinking about apologizing for. The voice in your head does not need to be broadcast to others. Just say thank you after you are introduced, and launch in. Someone has asked you to talk, so bring your own unique expertise and don’t start with undermining yourself!
- Don’t use your slides as a crutch: Make your audience look at you and not your slides. That means at times, you may be talking and your slides will not be moving. Other times, if you are starting with a story, maybe there is no slide behind you and the screen is blacked out. Some of the most powerful moments in a talk are when slides are not being used.
- Don’t stand behind the podium if you can help it. This means ask for a wireless microphone. Most podiums will overwhelm you. If you have to use a podium, go back to the posture in the “dos.” One year, I had a leg injury and definitely used the podium, so obviously there may be times you need to use a podium; even then, try as hard as possible to make sure you are seen.
- Don’t engage grandstanders during Q&A: Invariably, you will get someone who stands up and goes into a long comment that is not a question to hear themselves speak. Insert yourself, say “thank you” and take the next question. If there is not a next question, you can add, “Before I forget, I want to share another question I am often asked which may be of help to you.” Then, answer your own question. You get the final word this way!
Happy speaking! I look forward to seeing you in warmer weather during the spring conference season.
For more posts from the Hospital Leader blog, visit hospitalleader.org.