User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Measles cases for 2019 now at postelimination high
according to the Centers for Disease Control and Prevention.
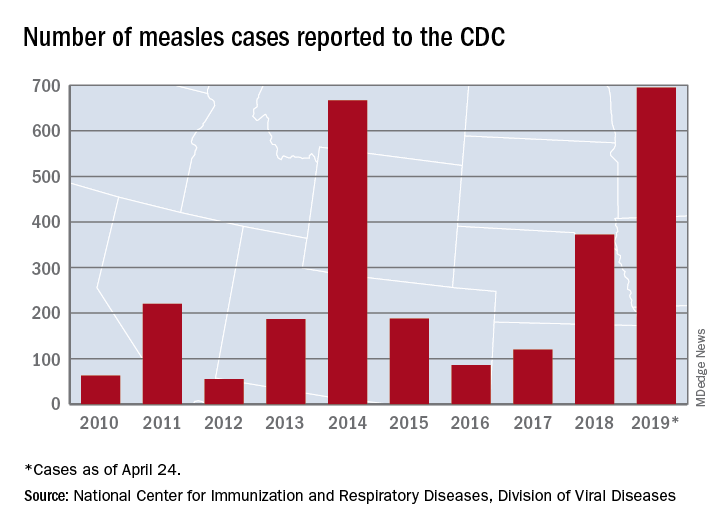
As of Wednesday, April 24, the case count for measles is 695, which eclipses the mark of 667 cases that had been the highest since the disease was declared to be eliminated from this country in 2000, the CDC reported.
“The high number of cases in 2019 is primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018. The outbreaks in New York City and New York State are among the largest and longest lasting since measles elimination in 2000. The longer these outbreaks continue, the greater the chance measles will again get a sustained foothold in the United States,” according to a written statement by the CDC.
Although these outbreaks began when the virus was brought into this country by unvaccinated travelers from other countries where there is widespread transmission, “a significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine. Some organizations are deliberately targeting these communities with inaccurate and misleading information about vaccines,” according to the statement.
“Measles is not a harmless childhood illness, but a highly contagious, potentially life-threatening disease,” Health and Human Services Secretary Alex Azar said in a separate statement. “We have the ability to safely protect our children and our communities. Vaccines are a safe, highly effective public health solution that can prevent this disease. The measles vaccines are among the most extensively studied medical products we have, and their safety has been firmly established over many years in some of the largest vaccine studies ever undertaken. With a safe and effective vaccine that protects against measles, the suffering we are seeing is avoidable.”
according to the Centers for Disease Control and Prevention.
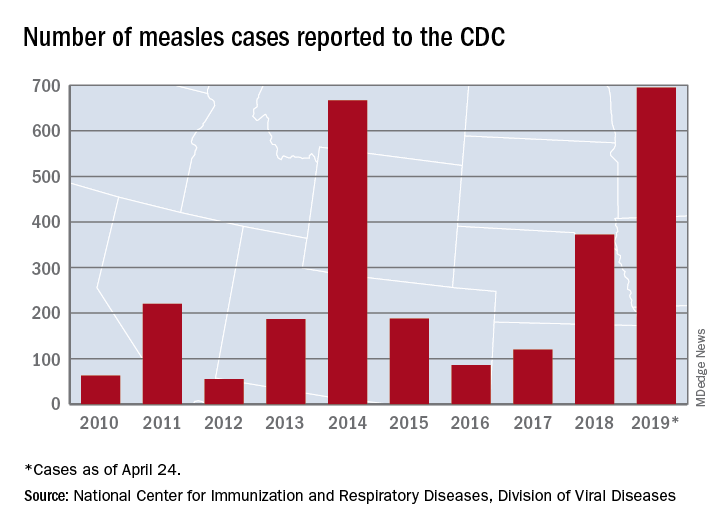
As of Wednesday, April 24, the case count for measles is 695, which eclipses the mark of 667 cases that had been the highest since the disease was declared to be eliminated from this country in 2000, the CDC reported.
“The high number of cases in 2019 is primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018. The outbreaks in New York City and New York State are among the largest and longest lasting since measles elimination in 2000. The longer these outbreaks continue, the greater the chance measles will again get a sustained foothold in the United States,” according to a written statement by the CDC.
Although these outbreaks began when the virus was brought into this country by unvaccinated travelers from other countries where there is widespread transmission, “a significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine. Some organizations are deliberately targeting these communities with inaccurate and misleading information about vaccines,” according to the statement.
“Measles is not a harmless childhood illness, but a highly contagious, potentially life-threatening disease,” Health and Human Services Secretary Alex Azar said in a separate statement. “We have the ability to safely protect our children and our communities. Vaccines are a safe, highly effective public health solution that can prevent this disease. The measles vaccines are among the most extensively studied medical products we have, and their safety has been firmly established over many years in some of the largest vaccine studies ever undertaken. With a safe and effective vaccine that protects against measles, the suffering we are seeing is avoidable.”
according to the Centers for Disease Control and Prevention.
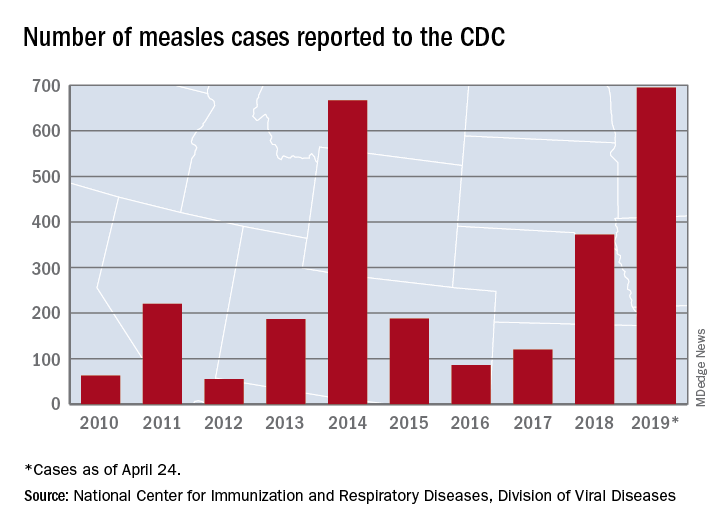
As of Wednesday, April 24, the case count for measles is 695, which eclipses the mark of 667 cases that had been the highest since the disease was declared to be eliminated from this country in 2000, the CDC reported.
“The high number of cases in 2019 is primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018. The outbreaks in New York City and New York State are among the largest and longest lasting since measles elimination in 2000. The longer these outbreaks continue, the greater the chance measles will again get a sustained foothold in the United States,” according to a written statement by the CDC.
Although these outbreaks began when the virus was brought into this country by unvaccinated travelers from other countries where there is widespread transmission, “a significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine. Some organizations are deliberately targeting these communities with inaccurate and misleading information about vaccines,” according to the statement.
“Measles is not a harmless childhood illness, but a highly contagious, potentially life-threatening disease,” Health and Human Services Secretary Alex Azar said in a separate statement. “We have the ability to safely protect our children and our communities. Vaccines are a safe, highly effective public health solution that can prevent this disease. The measles vaccines are among the most extensively studied medical products we have, and their safety has been firmly established over many years in some of the largest vaccine studies ever undertaken. With a safe and effective vaccine that protects against measles, the suffering we are seeing is avoidable.”
CDC warns against misuse of opioid-prescribing guideline
Officials at the Centers for Disease Control and Prevention are warning against the misapplication of the agency’s 2016 guidelines on opioid prescribing, as well as clarifying dosage recommendations for patients starting or stopping pain medications.
In a perspective published in the New England Journal of Medicine on April 24, lead author Deborah Dowell, MD, chief medical officer for the CDC’s National Center for Injury Prevention and Control, conveyed concern that some policies and practices derived from the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain are inconsistent with the recommendations and often go beyond their scope.
Misapplication examples include inappropriately applying the guideline to patients in active cancer treatment, patients experiencing acute sickle cell crises, or patients experiencing postsurgical pain, Dr. Dowell wrote.
The guideline offers guidance to clinicians treating chronic pain in adults who are already receiving opioids long-term at high dosages, she noted. It includes advice on maximizing nonopioid treatment, reviewing risks associated with continuing high-dose opioids, and collaborating with patients who agree to taper dosage, among other guidance.
Any application of the guideline’s dosage recommendation that results in hard limits or “cutting off” opioids is also an incorrect use of the recommendations, according to Dr. Dowell.
While the guideline advises clinicians to start opioids at the lowest effective dosage and avoid increasing dosage to 90 morphine milligram equivalents per day or more, that statement does not suggest discontinuation of opioids already prescribed at high dosages, according to the CDC’s clarification.
The guidance also does not apply to patients receiving or starting medication-assisted treatment for opioid use disorder.
The commentary comes after a trio of organizations raised concerns that insurers are inappropriately applying the recommendations to active cancer patients when making coverage determinations.
The American Society of Clinical Oncology, the National Comprehensive Cancer Network, and the American Society of Hematology, raised the issue in a letter to the CDC in February. In response, Dr. Dowell clarified that the recommendations are not intended to deny clinically appropriate opioid therapy to any patients who suffer chronic pain, but rather to ensure that physicians and patients consider all safe and effective treatment options.
In the perspective, Dr. Dowell wrote that the CDC is evaluating the intended and unintended impact of the 2016 opioid-prescribing guideline on clinician and patient outcomes and that the agency is committed to updating the recommendations when new evidence is available.
Officials at the Centers for Disease Control and Prevention are warning against the misapplication of the agency’s 2016 guidelines on opioid prescribing, as well as clarifying dosage recommendations for patients starting or stopping pain medications.
In a perspective published in the New England Journal of Medicine on April 24, lead author Deborah Dowell, MD, chief medical officer for the CDC’s National Center for Injury Prevention and Control, conveyed concern that some policies and practices derived from the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain are inconsistent with the recommendations and often go beyond their scope.
Misapplication examples include inappropriately applying the guideline to patients in active cancer treatment, patients experiencing acute sickle cell crises, or patients experiencing postsurgical pain, Dr. Dowell wrote.
The guideline offers guidance to clinicians treating chronic pain in adults who are already receiving opioids long-term at high dosages, she noted. It includes advice on maximizing nonopioid treatment, reviewing risks associated with continuing high-dose opioids, and collaborating with patients who agree to taper dosage, among other guidance.
Any application of the guideline’s dosage recommendation that results in hard limits or “cutting off” opioids is also an incorrect use of the recommendations, according to Dr. Dowell.
While the guideline advises clinicians to start opioids at the lowest effective dosage and avoid increasing dosage to 90 morphine milligram equivalents per day or more, that statement does not suggest discontinuation of opioids already prescribed at high dosages, according to the CDC’s clarification.
The guidance also does not apply to patients receiving or starting medication-assisted treatment for opioid use disorder.
The commentary comes after a trio of organizations raised concerns that insurers are inappropriately applying the recommendations to active cancer patients when making coverage determinations.
The American Society of Clinical Oncology, the National Comprehensive Cancer Network, and the American Society of Hematology, raised the issue in a letter to the CDC in February. In response, Dr. Dowell clarified that the recommendations are not intended to deny clinically appropriate opioid therapy to any patients who suffer chronic pain, but rather to ensure that physicians and patients consider all safe and effective treatment options.
In the perspective, Dr. Dowell wrote that the CDC is evaluating the intended and unintended impact of the 2016 opioid-prescribing guideline on clinician and patient outcomes and that the agency is committed to updating the recommendations when new evidence is available.
Officials at the Centers for Disease Control and Prevention are warning against the misapplication of the agency’s 2016 guidelines on opioid prescribing, as well as clarifying dosage recommendations for patients starting or stopping pain medications.
In a perspective published in the New England Journal of Medicine on April 24, lead author Deborah Dowell, MD, chief medical officer for the CDC’s National Center for Injury Prevention and Control, conveyed concern that some policies and practices derived from the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain are inconsistent with the recommendations and often go beyond their scope.
Misapplication examples include inappropriately applying the guideline to patients in active cancer treatment, patients experiencing acute sickle cell crises, or patients experiencing postsurgical pain, Dr. Dowell wrote.
The guideline offers guidance to clinicians treating chronic pain in adults who are already receiving opioids long-term at high dosages, she noted. It includes advice on maximizing nonopioid treatment, reviewing risks associated with continuing high-dose opioids, and collaborating with patients who agree to taper dosage, among other guidance.
Any application of the guideline’s dosage recommendation that results in hard limits or “cutting off” opioids is also an incorrect use of the recommendations, according to Dr. Dowell.
While the guideline advises clinicians to start opioids at the lowest effective dosage and avoid increasing dosage to 90 morphine milligram equivalents per day or more, that statement does not suggest discontinuation of opioids already prescribed at high dosages, according to the CDC’s clarification.
The guidance also does not apply to patients receiving or starting medication-assisted treatment for opioid use disorder.
The commentary comes after a trio of organizations raised concerns that insurers are inappropriately applying the recommendations to active cancer patients when making coverage determinations.
The American Society of Clinical Oncology, the National Comprehensive Cancer Network, and the American Society of Hematology, raised the issue in a letter to the CDC in February. In response, Dr. Dowell clarified that the recommendations are not intended to deny clinically appropriate opioid therapy to any patients who suffer chronic pain, but rather to ensure that physicians and patients consider all safe and effective treatment options.
In the perspective, Dr. Dowell wrote that the CDC is evaluating the intended and unintended impact of the 2016 opioid-prescribing guideline on clinician and patient outcomes and that the agency is committed to updating the recommendations when new evidence is available.
Report: Part B funds stable, hospital trust running out
Medicare’s Part B trust fund is well funded and stable enough to pay physicians through the foreseeable future, according to an annual report by the Medicare Board of Trustees.
The Supplemental Medical Insurance (SMI) trust fund, which covers Medicare Part B and D, contained $104 billion in assets at the end of 2018 and is expected to be adequately financed in all years because of continued premium and general revenue income, according to the report, which was released April 22.
However, the Hospital Insurance (HI) trust fund, which funds Medicare Part A, is expected to run out by 2026, the same projection as last year, the trustees reported.
In addition, trustees said that total Medicare costs – including both HI and SMI expenditures – will grow from about 4% of gross domestic product (GDP) in 2018 to about 6% of GDP by 2038 and then increase gradually thereafter to about 6.5% of GDP by 2093.
The faster rate of growth in Medicare spending, compared with GDP growth, is attributable to a growing number of Medicare patients and increased volume and intensity of health care services, according to the report. Alone, SMI costs are projected to grow steadily from 2% of GDP in 2018 to about 4% of GDP in 2038 because of the aging population and rising health care costs.
The report delivers a dose of reality, reminding the country that the program’s main trust for hospital services can pay full benefits for only 7 more years, Seema Verma, administrator of the Centers for Medicare & Medicaid Services said.
“The Trump administration is working hard to protect and strengthen Medicare and lower costs while improving quality in order to protect the program for future generations of seniors who have paid into the program their whole lives,” Ms. Verma said in a statement. “If we do not take the fiscal crisis in Medicare seriously, we will jeopardize access to health care for millions of seniors.”
Department of Health & Human Services Secretary Alex M. Azar II said the annual report provides a sobering reminder that more work is necessary to support current and future generations of seniors.
“Instead of trying to expand Medicare into a universal entitlement that even covers wealthy Americans of working age, as some have proposed, we need to fulfill Medicare’s promise to our seniors,” Mr. Azar said in a statement, referring to proposals to expand government health care by some Democrats.
The trustees report notes that Medicare has introduced a number of initiatives to strengthen and protect the program and finalized a number of rules that advance a patient-driven health care system through competition.
“In particular, CMS is strengthening Medicare through increasing choice in Medicare Advantage and adding supplemental benefits to the program, offering more care options for people with diabetes, providing new telehealth services, and lowering prescription drug costs for seniors,” the agency stated in a press release. “CMS is also continuing work to advance policies to increase price transparency and help beneficiaries compare costs across different providers.”
Medicare’s Part B trust fund is well funded and stable enough to pay physicians through the foreseeable future, according to an annual report by the Medicare Board of Trustees.
The Supplemental Medical Insurance (SMI) trust fund, which covers Medicare Part B and D, contained $104 billion in assets at the end of 2018 and is expected to be adequately financed in all years because of continued premium and general revenue income, according to the report, which was released April 22.
However, the Hospital Insurance (HI) trust fund, which funds Medicare Part A, is expected to run out by 2026, the same projection as last year, the trustees reported.
In addition, trustees said that total Medicare costs – including both HI and SMI expenditures – will grow from about 4% of gross domestic product (GDP) in 2018 to about 6% of GDP by 2038 and then increase gradually thereafter to about 6.5% of GDP by 2093.
The faster rate of growth in Medicare spending, compared with GDP growth, is attributable to a growing number of Medicare patients and increased volume and intensity of health care services, according to the report. Alone, SMI costs are projected to grow steadily from 2% of GDP in 2018 to about 4% of GDP in 2038 because of the aging population and rising health care costs.
The report delivers a dose of reality, reminding the country that the program’s main trust for hospital services can pay full benefits for only 7 more years, Seema Verma, administrator of the Centers for Medicare & Medicaid Services said.
“The Trump administration is working hard to protect and strengthen Medicare and lower costs while improving quality in order to protect the program for future generations of seniors who have paid into the program their whole lives,” Ms. Verma said in a statement. “If we do not take the fiscal crisis in Medicare seriously, we will jeopardize access to health care for millions of seniors.”
Department of Health & Human Services Secretary Alex M. Azar II said the annual report provides a sobering reminder that more work is necessary to support current and future generations of seniors.
“Instead of trying to expand Medicare into a universal entitlement that even covers wealthy Americans of working age, as some have proposed, we need to fulfill Medicare’s promise to our seniors,” Mr. Azar said in a statement, referring to proposals to expand government health care by some Democrats.
The trustees report notes that Medicare has introduced a number of initiatives to strengthen and protect the program and finalized a number of rules that advance a patient-driven health care system through competition.
“In particular, CMS is strengthening Medicare through increasing choice in Medicare Advantage and adding supplemental benefits to the program, offering more care options for people with diabetes, providing new telehealth services, and lowering prescription drug costs for seniors,” the agency stated in a press release. “CMS is also continuing work to advance policies to increase price transparency and help beneficiaries compare costs across different providers.”
Medicare’s Part B trust fund is well funded and stable enough to pay physicians through the foreseeable future, according to an annual report by the Medicare Board of Trustees.
The Supplemental Medical Insurance (SMI) trust fund, which covers Medicare Part B and D, contained $104 billion in assets at the end of 2018 and is expected to be adequately financed in all years because of continued premium and general revenue income, according to the report, which was released April 22.
However, the Hospital Insurance (HI) trust fund, which funds Medicare Part A, is expected to run out by 2026, the same projection as last year, the trustees reported.
In addition, trustees said that total Medicare costs – including both HI and SMI expenditures – will grow from about 4% of gross domestic product (GDP) in 2018 to about 6% of GDP by 2038 and then increase gradually thereafter to about 6.5% of GDP by 2093.
The faster rate of growth in Medicare spending, compared with GDP growth, is attributable to a growing number of Medicare patients and increased volume and intensity of health care services, according to the report. Alone, SMI costs are projected to grow steadily from 2% of GDP in 2018 to about 4% of GDP in 2038 because of the aging population and rising health care costs.
The report delivers a dose of reality, reminding the country that the program’s main trust for hospital services can pay full benefits for only 7 more years, Seema Verma, administrator of the Centers for Medicare & Medicaid Services said.
“The Trump administration is working hard to protect and strengthen Medicare and lower costs while improving quality in order to protect the program for future generations of seniors who have paid into the program their whole lives,” Ms. Verma said in a statement. “If we do not take the fiscal crisis in Medicare seriously, we will jeopardize access to health care for millions of seniors.”
Department of Health & Human Services Secretary Alex M. Azar II said the annual report provides a sobering reminder that more work is necessary to support current and future generations of seniors.
“Instead of trying to expand Medicare into a universal entitlement that even covers wealthy Americans of working age, as some have proposed, we need to fulfill Medicare’s promise to our seniors,” Mr. Azar said in a statement, referring to proposals to expand government health care by some Democrats.
The trustees report notes that Medicare has introduced a number of initiatives to strengthen and protect the program and finalized a number of rules that advance a patient-driven health care system through competition.
“In particular, CMS is strengthening Medicare through increasing choice in Medicare Advantage and adding supplemental benefits to the program, offering more care options for people with diabetes, providing new telehealth services, and lowering prescription drug costs for seniors,” the agency stated in a press release. “CMS is also continuing work to advance policies to increase price transparency and help beneficiaries compare costs across different providers.”
Top 10 things physician advisors want hospitalists to know
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
The practice of hospital medicine is rapidly changing. Higher-acuity patients are being admitted to hospitals already struggling with capacity, and hospitalists are being instructed to pay attention to length of stay, improve their documentation and billing, and participate in initiatives to improve hospital throughput, all while delivering high-quality patient care.
As hospitalists and SHM members who are also physician advisors, we have a unique understanding of these pressures. In this article, we answer common questions we receive from hospitalists regarding utilization management, care coordination, clinical documentation, and CMS regulations.
Why do physician advisors exist, and what do they do?
A physician advisor is hired by the hospital to act as a liaison between the hospital administration, clinical staff, and support personnel in order to ensure regulatory compliance, advise physicians on medical necessity, and assist hospital leadership in meeting overall organizational goals related to the efficient utilization of health care services.1
Given their deep knowledge of hospital systems and processes, and ability to collaborate and teach, hospitalists are well-positioned to serve in this capacity. Our primary goal as physician advisors is to help physicians continue to focus on the parts of medicine they enjoy – clinical care, education, quality improvement, research etc. – by helping to demystify complex regulatory requirements and by creating streamlined processes to make following these requirements easier.
Why does this matter?
We understand that regulatory and hospital systems issues such as patient class determination, appropriate clinical documentation, and hospital throughput and capacity management can feel tedious, and sometimes overwhelming, to busy hospitalists. While it is easy to attribute these problems solely to hospitals’ desire for increased revenue, these issues directly impact the quality of care we provide to their patients.
In addition, our entire financial system is predicated on appropriate health care resource utilization, financial reimbursement, demonstration of medical acuity, and our impact on the care of a patient. Thus, our ability to advocate for our patients and for ourselves is directly connected with this endeavor. Developing a working knowledge of regulatory and systems issues allows hospitalists to be more engaged in leadership and negotiations and allows us to advocate for resources we deem most important.
Why are clinical documentation integrity teams so important?
Accurately and specifically describing how sick your patients are helps ensure that hospitals are reimbursed appropriately, coded data is accurate for research purposes, quality metrics are attributed correctly, and patients receive the correct diagnoses.
Clarification of documentation and/or addressing “clinical validity” of a given diagnosis (e.g., acute hypoxic respiratory failure requires both hypoxia and respiratory distress) may support an increase or result in a decrease in hospital reimbursement. For example, if the reason for a patient’s admission is renal failure, renal failure with true acute hypoxic respiratory failure will be reimbursed at a rate 40% higher than renal failure without the documentation of other conditions that reflect how ill the patient really is. The patient with acute hypoxic respiratory failure (or other major comorbid condition) is genuinely sicker, thus requiring more time (length of stay) and resources (deserved higher reimbursement).
What is the two-midnight rule, and why does it matter?
In October of 2013, the Centers for Medicare & Medicaid Services initiated the two-midnight rule, which states a Medicare patient can be an “inpatient” class if the admitting provider determines that 1) the patient requires medically necessary care which cannot be provided outside the hospital and 2) the patient is expected to stay at least 2 midnights in the hospital.
If, at the time of admission, an admitting provider thinks it is likely that the patient may be discharged prior to 2 midnights, then outpatient care with “observation” designation is appropriate. Incorrect patient class assignment may result in significant adverse consequences for hospitals, including improper patient billing, decreased hospital reimbursement, substantial risk for external auditing, violation of Medicare conditions of participation, and even loss of accreditation.
Who can I talk to if I have a question about a patient’s class? What should I do if I disagree with the class assigned to my patient?
The Utilization Management team typically consists of nurses and physician advisors specifically trained in UM. This team functions as a liaison between providers and payers (particularly Medicare and Medicaid) regarding medical necessity, appropriateness of care received, and efficiency of health care services.
When it comes to discussions about patient class, start by learning more about why the determination was made. The most common reason for patient class disagreements is simply that the documentation does not reflect the severity of illness or accurately reflect the care the patient is receiving. Your documentation should communicate that your patient needs services that only the hospital can provide, and/or they need monitoring that must be done in the hospital to meet the medical necessity criteria that CMS requires for a patient to be “inpatient” class.
If you disagree with a determination provided by the UM nurse and/or physician advisor, then the case will be presented to the hospital UM committee for further review. Two physicians from the UM committee must review the case and provide their own determinations of patient status, and whichever admission determination has two votes is the one that is appropriate.
How do I talk to patients about class determinations?
As media coverage continues about the two-midnight rule and the impact this has on patients, providers should expect more questions about class determination from their patients.
An AARP Bulletin article from 2012 advised patients to “ask [their] own doctor whether observation status is justified … and if not ask him or her to call the hospital to explain the medical reasons why they should be admitted as inpatient.”2 Patients should be informed that providers understand the implications of patient class determinations and are making these decisions as outlined by CMS.
We recommend informing patients that the decision about whether a patient is “inpatient” or “outpatient with observation” class is complex and involves taking into consideration a patient’s medical history, the severity of their current medical condition, need for diagnostic testing, and degree of health resource utilization, as well as a provider’s medical opinion of the risk of an adverse event occurring.
Is it true that observation patients receive higher hospital bills?
It is a common misperception that a designation of “observation” class means that a patient’s medical bill will be higher than “inpatient” class. In 2016, CMS changed the way observation class patients are billed so that, in most scenarios, patients do not receive a higher hospital bill when placed in “observation” class.
How do I approach a denial from a payer?
Commercial payers review all hospitalizations for medical necessity and appropriateness of care received during a patient’s hospitalization. If you receive notice that all or part of your patient’s hospital stay was denied coverage, you have the option of discussing the case with the medical director of the insurance company – this is called a peer-to-peer discussion.
We recommend reviewing the patient’s case and your documentation of the care you provided prior to the peer to peer, especially since these denials may come weeks to months after you have cared for the patient. Begin your conversation by learning why the insurance company denied coverage of the stay and then provide an accurate portrayal of the acuity of illness of the patient, and the resources your hospital used in caring for them. Consider consulting with your hospital’s physician advisor for other high-yield tips.
How can care management help with ‘nonmedical’ hospitalizations?
Care managers are your allies for all patients, especially those with complex discharge needs. Often patients admitted for “nonmedical” reasons do not have the ability to discharge to a skilled nursing facility, long-term care facility, or home due to lack of insurance coverage or resources and/or assistance. Care managers can help you creatively problem solve and coordinate care. Physician advisors are your allies in helping create system-level interventions that might avert some of these “nonmedical” admissions. Consider involving both care managers and physician advisors early in the admission to help navigate social complexities.
How can hospitalists get involved?
According to CMS, the decision on “whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital … can typically be made in less than 48 hours, usually in less than 24 hours.”3 In reality, this is not black and white. The “2 midnights” has brought a host of new challenges for hospitals, hospitalists, and patients to navigate. The Society of Hospital Medicine released an Observation White Paper in 2017 challenging the status quo and proposing comprehensive observation reform.4
We encourage hospital medicine providers to more routinely engage with their institutional physician advisors and consider joining the SHM Public Policy Committee to become more involved in advocacy, and/or consider becoming a physician advisor.
Dr. Singh is physician advisor for Utilization & CM in the division of hospital medicine at the University of Colorado at Denver, Aurora. Dr. Patel is a hospitalist and assistant professor of medicine at the university. Dr. Anoff is director of clinical operations and director of nights for the Hospital Medicine Group at the University of Colorado at Denver. Dr. Stella is a hospitalist at Denver Health and Hospital Authority and an associate professor of medicine at the university.
References
1. What is a physician advisor? 2017 Oct 9.
2. Barry P. Medicare: Inpatient or outpatient. AARP Bulletin. 2012 Oct.
3. Goldberg TH. The long-term and post-acute care continuum. WV Med J. 2014 Nov-Dec;10(6):24-30.
4. Society of Hospital Medicine Public Policy Committee. The hospital observation care problem. Perspectives and solutions from the Society of Hospital Medicine. 2017 Sep.
In pain treatment, racial bias common among physician trainees
MILWAUKEE – More than 40% of white physician trainees demonstrated racial bias in medical decision making about treatment of low back pain, as did 31% of nonwhite trainees. However, just 6% of white residents and fellows, and 10% of the nonwhite residents and fellows, reported that patient race had factored into their treatment decisions in a virtual patient task.
The 444 medical residents and fellows who participated viewed video vignettes presenting 12 virtual patients who presented with low back pain, wrote Alexis Grant of Indiana University–Purdue University Indianapolis and her colleagues. In a poster presentation at the scientific meeting of the American Pain Society, Ms. Grant, a doctoral student in clinical psychology, and her collaborators explained that participants agreed to view a series of 12 videos of virtual patients.
The videos presented male and female virtual patients who were black or white and who had jobs associated with low or high socioeconomic status (SES). Information in text vignettes accompanying the videos included occupation, pain etiology, physical exam findings, and pain intensity by self-report.
After viewing the videos and reading the vignettes, participating clinicians were asked to use a 0-100 visual analog scale to report their likelihood of referring patients to a pain specialist or to physical therapy and of recommending opioid or nonopioid analgesia.
“Next, they rated the degree to which they considered different sources of patient information when making treatment decision,” Ms. Grant and her coauthors wrote. Statistical analysis “examined the extent to which providers demonstrated statistically reliable treatment differences across patient race and SES.” These findings were compared with how clinicians reported they used patient race and SES in decision making.
Demonstrated race-based decision making occurred for 41% of white and 31% of nonwhite clinicians. About two-thirds of providers (67.3%) were white, and of the remainder, 26.3% were Asian, 4.4% were classified as “other,” and 2.1% were black. The respondents were aged a mean 29.7 years, and were 42.3% female.
In addition, Ms. Grant and her coauthors estimated provider SES by asking about parental SES, dividing respondents into low (less than $38,000), medium ($38,000-$75,000), and high (greater than $75,000) SES categories.
and similar across levels of provider SES, at 41%, 43%, and 38% for low, medium, and high SES residents and fellows, respectively. However, the disconnect between reported and demonstrated bias that was seen with race was not seen with SES bias, with 43%-48% of providers in each SES group reporting that they had factored patient SES into their treatment decision making.
“These results suggest that providers have low awareness of making different pain treatment decisions” for black patients, compared with decision making for white patients, Ms. Grant and her colleagues wrote. “Decision-making awareness did not substantially differ across provider race or SES.” She and her collaborators called for more research into whether raising awareness about demonstrated racial bias in decision making can improve both racial and socioeconomic gaps in pain care.
The authors reported funding from the National Institutes of Health. They reported no conflicts of interest.
MILWAUKEE – More than 40% of white physician trainees demonstrated racial bias in medical decision making about treatment of low back pain, as did 31% of nonwhite trainees. However, just 6% of white residents and fellows, and 10% of the nonwhite residents and fellows, reported that patient race had factored into their treatment decisions in a virtual patient task.
The 444 medical residents and fellows who participated viewed video vignettes presenting 12 virtual patients who presented with low back pain, wrote Alexis Grant of Indiana University–Purdue University Indianapolis and her colleagues. In a poster presentation at the scientific meeting of the American Pain Society, Ms. Grant, a doctoral student in clinical psychology, and her collaborators explained that participants agreed to view a series of 12 videos of virtual patients.
The videos presented male and female virtual patients who were black or white and who had jobs associated with low or high socioeconomic status (SES). Information in text vignettes accompanying the videos included occupation, pain etiology, physical exam findings, and pain intensity by self-report.
After viewing the videos and reading the vignettes, participating clinicians were asked to use a 0-100 visual analog scale to report their likelihood of referring patients to a pain specialist or to physical therapy and of recommending opioid or nonopioid analgesia.
“Next, they rated the degree to which they considered different sources of patient information when making treatment decision,” Ms. Grant and her coauthors wrote. Statistical analysis “examined the extent to which providers demonstrated statistically reliable treatment differences across patient race and SES.” These findings were compared with how clinicians reported they used patient race and SES in decision making.
Demonstrated race-based decision making occurred for 41% of white and 31% of nonwhite clinicians. About two-thirds of providers (67.3%) were white, and of the remainder, 26.3% were Asian, 4.4% were classified as “other,” and 2.1% were black. The respondents were aged a mean 29.7 years, and were 42.3% female.
In addition, Ms. Grant and her coauthors estimated provider SES by asking about parental SES, dividing respondents into low (less than $38,000), medium ($38,000-$75,000), and high (greater than $75,000) SES categories.
and similar across levels of provider SES, at 41%, 43%, and 38% for low, medium, and high SES residents and fellows, respectively. However, the disconnect between reported and demonstrated bias that was seen with race was not seen with SES bias, with 43%-48% of providers in each SES group reporting that they had factored patient SES into their treatment decision making.
“These results suggest that providers have low awareness of making different pain treatment decisions” for black patients, compared with decision making for white patients, Ms. Grant and her colleagues wrote. “Decision-making awareness did not substantially differ across provider race or SES.” She and her collaborators called for more research into whether raising awareness about demonstrated racial bias in decision making can improve both racial and socioeconomic gaps in pain care.
The authors reported funding from the National Institutes of Health. They reported no conflicts of interest.
MILWAUKEE – More than 40% of white physician trainees demonstrated racial bias in medical decision making about treatment of low back pain, as did 31% of nonwhite trainees. However, just 6% of white residents and fellows, and 10% of the nonwhite residents and fellows, reported that patient race had factored into their treatment decisions in a virtual patient task.
The 444 medical residents and fellows who participated viewed video vignettes presenting 12 virtual patients who presented with low back pain, wrote Alexis Grant of Indiana University–Purdue University Indianapolis and her colleagues. In a poster presentation at the scientific meeting of the American Pain Society, Ms. Grant, a doctoral student in clinical psychology, and her collaborators explained that participants agreed to view a series of 12 videos of virtual patients.
The videos presented male and female virtual patients who were black or white and who had jobs associated with low or high socioeconomic status (SES). Information in text vignettes accompanying the videos included occupation, pain etiology, physical exam findings, and pain intensity by self-report.
After viewing the videos and reading the vignettes, participating clinicians were asked to use a 0-100 visual analog scale to report their likelihood of referring patients to a pain specialist or to physical therapy and of recommending opioid or nonopioid analgesia.
“Next, they rated the degree to which they considered different sources of patient information when making treatment decision,” Ms. Grant and her coauthors wrote. Statistical analysis “examined the extent to which providers demonstrated statistically reliable treatment differences across patient race and SES.” These findings were compared with how clinicians reported they used patient race and SES in decision making.
Demonstrated race-based decision making occurred for 41% of white and 31% of nonwhite clinicians. About two-thirds of providers (67.3%) were white, and of the remainder, 26.3% were Asian, 4.4% were classified as “other,” and 2.1% were black. The respondents were aged a mean 29.7 years, and were 42.3% female.
In addition, Ms. Grant and her coauthors estimated provider SES by asking about parental SES, dividing respondents into low (less than $38,000), medium ($38,000-$75,000), and high (greater than $75,000) SES categories.
and similar across levels of provider SES, at 41%, 43%, and 38% for low, medium, and high SES residents and fellows, respectively. However, the disconnect between reported and demonstrated bias that was seen with race was not seen with SES bias, with 43%-48% of providers in each SES group reporting that they had factored patient SES into their treatment decision making.
“These results suggest that providers have low awareness of making different pain treatment decisions” for black patients, compared with decision making for white patients, Ms. Grant and her colleagues wrote. “Decision-making awareness did not substantially differ across provider race or SES.” She and her collaborators called for more research into whether raising awareness about demonstrated racial bias in decision making can improve both racial and socioeconomic gaps in pain care.
The authors reported funding from the National Institutes of Health. They reported no conflicts of interest.
REPORTING FROM APS 2019
FDA approves generic naloxone spray for opioid overdose treatment
The Food and Drug Administration on April 19 approved the first generic naloxone hydrochloride nasal spray (Narcan) as treatment for stopping or reversing an opioid overdose.
“In the wake of the opioid crisis, a number of efforts are underway to make this emergency overdose reversal treatment more readily available and more accessible,” said Douglas Throckmorton, MD, deputy center director for regulatory programs in the FDA’s Center for Drug Evaluation and Research, in a press release. “In addition to this approval of the first generic naloxone nasal spray, moving forward, we will prioritize our review of generic drug applications for naloxone.”
The agency said the naloxone nasal spray does not need assembly and can be used by anyone, regardless of medical training. If the spray is administered quickly after the overdose begins, the effect of the opioid will be countered, often within minutes. However, patients should still seek immediate medical attention.
The FDA cautioned that, when used on a patient with an opioid dependence, naloxone can cause severe opioid withdrawal, characterized by symptoms such as body aches, diarrhea, tachycardia, fever, runny nose, sneezing, goose bumps, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure.
Find the full press release on the FDA website.
The Food and Drug Administration on April 19 approved the first generic naloxone hydrochloride nasal spray (Narcan) as treatment for stopping or reversing an opioid overdose.
“In the wake of the opioid crisis, a number of efforts are underway to make this emergency overdose reversal treatment more readily available and more accessible,” said Douglas Throckmorton, MD, deputy center director for regulatory programs in the FDA’s Center for Drug Evaluation and Research, in a press release. “In addition to this approval of the first generic naloxone nasal spray, moving forward, we will prioritize our review of generic drug applications for naloxone.”
The agency said the naloxone nasal spray does not need assembly and can be used by anyone, regardless of medical training. If the spray is administered quickly after the overdose begins, the effect of the opioid will be countered, often within minutes. However, patients should still seek immediate medical attention.
The FDA cautioned that, when used on a patient with an opioid dependence, naloxone can cause severe opioid withdrawal, characterized by symptoms such as body aches, diarrhea, tachycardia, fever, runny nose, sneezing, goose bumps, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure.
Find the full press release on the FDA website.
The Food and Drug Administration on April 19 approved the first generic naloxone hydrochloride nasal spray (Narcan) as treatment for stopping or reversing an opioid overdose.
“In the wake of the opioid crisis, a number of efforts are underway to make this emergency overdose reversal treatment more readily available and more accessible,” said Douglas Throckmorton, MD, deputy center director for regulatory programs in the FDA’s Center for Drug Evaluation and Research, in a press release. “In addition to this approval of the first generic naloxone nasal spray, moving forward, we will prioritize our review of generic drug applications for naloxone.”
The agency said the naloxone nasal spray does not need assembly and can be used by anyone, regardless of medical training. If the spray is administered quickly after the overdose begins, the effect of the opioid will be countered, often within minutes. However, patients should still seek immediate medical attention.
The FDA cautioned that, when used on a patient with an opioid dependence, naloxone can cause severe opioid withdrawal, characterized by symptoms such as body aches, diarrhea, tachycardia, fever, runny nose, sneezing, goose bumps, sweating, yawning, nausea or vomiting, nervousness, restlessness or irritability, shivering or trembling, abdominal cramps, weakness, and increased blood pressure.
Find the full press release on the FDA website.
Short Takes
Short Takes
Both sleep quantity and quality is disturbed in hospitalized patients
A cross-sectional, observational, single-day study of over 2,000 hospitalized patients showed that, on average, these patients received 83 minutes less sleep time than at home. Quality of sleep – as measured by the Consensus Sleep Diary (CSD) and the Dutch-Flemish Patient-Reported-Outcomes Measurement Information System (PROMIS) Sleep Disturbance item bank – was also significantly disturbed. Sleep disruptions were most commonly caused by noise from other patients and by being awakened by hospital staff.
Citation: Wesselius H et al. Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med. 2018 Jul 16. doi: 10.1001/jamainternmed.2018.2669.
Health care costs and mortality improve in Medicare beneficiaries who receive transitional care management (TCM) service
In a retrospective cohort analysis of Medicare Fee-for-Service beneficiaries, the adjusted total Medicare costs (average, $3,358 vs. $3,033) and mortality (1.6% vs 1.0%) were higher among those beneficiaries who did not receive TCM services, compared with those who did receive TCM services, in the 31-60 days following an eligible discharge; however, use of this service by clinicians remained very low.
Citation: Bindman AB et al. Changes in health care costs and mortality associated with transitional care management services after a discharge among Medicare beneficiaries. JAMA Intern Med. 2018 Jul 30. doi: 10.1001/jamainternmed.2018.2572.
Unsafe zolpidem use is common
In a review of the 2015 US Medical Expenditure Panel Survey, investigators found that up to 77% of patients prescribed zolpidem reported being prescribed longer durations and higher doses, as well as the drug being prescribed alongside other CNS depressants, despite known risks and recommended prescription and Food and Drug Administration guidelines.
Citation: Moore T et al. Assessment of patterns of potentially unsafe use of zolpidem. JAMA Intern Med. 2018 Jul 16. doi: 10.1001/jamainternmed.2018.3031.
Short Takes
Short Takes
Both sleep quantity and quality is disturbed in hospitalized patients
A cross-sectional, observational, single-day study of over 2,000 hospitalized patients showed that, on average, these patients received 83 minutes less sleep time than at home. Quality of sleep – as measured by the Consensus Sleep Diary (CSD) and the Dutch-Flemish Patient-Reported-Outcomes Measurement Information System (PROMIS) Sleep Disturbance item bank – was also significantly disturbed. Sleep disruptions were most commonly caused by noise from other patients and by being awakened by hospital staff.
Citation: Wesselius H et al. Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med. 2018 Jul 16. doi: 10.1001/jamainternmed.2018.2669.
Health care costs and mortality improve in Medicare beneficiaries who receive transitional care management (TCM) service
In a retrospective cohort analysis of Medicare Fee-for-Service beneficiaries, the adjusted total Medicare costs (average, $3,358 vs. $3,033) and mortality (1.6% vs 1.0%) were higher among those beneficiaries who did not receive TCM services, compared with those who did receive TCM services, in the 31-60 days following an eligible discharge; however, use of this service by clinicians remained very low.
Citation: Bindman AB et al. Changes in health care costs and mortality associated with transitional care management services after a discharge among Medicare beneficiaries. JAMA Intern Med. 2018 Jul 30. doi: 10.1001/jamainternmed.2018.2572.
Unsafe zolpidem use is common
In a review of the 2015 US Medical Expenditure Panel Survey, investigators found that up to 77% of patients prescribed zolpidem reported being prescribed longer durations and higher doses, as well as the drug being prescribed alongside other CNS depressants, despite known risks and recommended prescription and Food and Drug Administration guidelines.
Citation: Moore T et al. Assessment of patterns of potentially unsafe use of zolpidem. JAMA Intern Med. 2018 Jul 16. doi: 10.1001/jamainternmed.2018.3031.
Both sleep quantity and quality is disturbed in hospitalized patients
A cross-sectional, observational, single-day study of over 2,000 hospitalized patients showed that, on average, these patients received 83 minutes less sleep time than at home. Quality of sleep – as measured by the Consensus Sleep Diary (CSD) and the Dutch-Flemish Patient-Reported-Outcomes Measurement Information System (PROMIS) Sleep Disturbance item bank – was also significantly disturbed. Sleep disruptions were most commonly caused by noise from other patients and by being awakened by hospital staff.
Citation: Wesselius H et al. Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med. 2018 Jul 16. doi: 10.1001/jamainternmed.2018.2669.
Health care costs and mortality improve in Medicare beneficiaries who receive transitional care management (TCM) service
In a retrospective cohort analysis of Medicare Fee-for-Service beneficiaries, the adjusted total Medicare costs (average, $3,358 vs. $3,033) and mortality (1.6% vs 1.0%) were higher among those beneficiaries who did not receive TCM services, compared with those who did receive TCM services, in the 31-60 days following an eligible discharge; however, use of this service by clinicians remained very low.
Citation: Bindman AB et al. Changes in health care costs and mortality associated with transitional care management services after a discharge among Medicare beneficiaries. JAMA Intern Med. 2018 Jul 30. doi: 10.1001/jamainternmed.2018.2572.
Unsafe zolpidem use is common
In a review of the 2015 US Medical Expenditure Panel Survey, investigators found that up to 77% of patients prescribed zolpidem reported being prescribed longer durations and higher doses, as well as the drug being prescribed alongside other CNS depressants, despite known risks and recommended prescription and Food and Drug Administration guidelines.
Citation: Moore T et al. Assessment of patterns of potentially unsafe use of zolpidem. JAMA Intern Med. 2018 Jul 16. doi: 10.1001/jamainternmed.2018.3031.
How to incorporate the gender wage gap into contract negotiations
PHILADELPHIA – that they need to account for: the gender wage gap.
“Find a lawyer ... that will support your fight for pay equity,” Michael Sinha, MD, advised in a presentation at the annual meeting of the American College of Physicians.
“Definitely interview them,” said Dr. Sinha of Harvard Medical School, Boston. “Get a sense of how committed they are to that cause. Seek recommendations from other women in medicine. Maybe they will point you to the person who really is committed to this cause and wants to help you.”
He also cautioned that physicians might have to help their lawyer fill in the knowledge gap. “Sometimes you need to provide that lawyer with data. There are a lot of reports that have been published from various organizations [including the ACP]. Don’t assume that the lawyer has the evidence.”
Armed with evidence, he said there is opportunity to address gender pay gaps in the contract. “You can put a lot of things into your contract, why not some of these things? If there is institutional evidence of a pay gap or a leaky promotional pipeline, you are telling them you have a problem with salary discrepancies between male and female physicians and I need to protect my own self-worth.”
Dr. Sinha recommended prospective employees develop strategies with their lawyers, which could mean letting the lawyer take the lead in the negotiations.
“Maybe that reduces stress or emotion in the process. That will preserve a good relationship with the employer,” he said. “A confident, knowledgeable lawyer may help mitigate gender differences in negotiation strategy.”
In order to help close the gender gap, Dr. Sinha said he advises his male colleagues to help female physicians by being open about their compensation, especially if compensation is not public information. “I have been encouraging male physician colleagues of mine to share that information when you are asked. Don’t make it impossible for someone to figure out.”
He noted that it is not likely that closing the gender gap by raising women’s compensation is going to result in male physicians losing money, but rather in the long run it will mean better compensation for everyone.
Dr. Sinha also had this advice for employers: “Before you do anything else, level your pay gap. ... For every physician that works in your organization, level your pay gap. Offer equitable salary packages up front to men and women. Understand your responsibilities under federal and state equal pay laws.”
When it comes to equitable compensation packages, all offerings, including salary and fringe benefits, should be offered to both male and female physicians or to neither.
“Don’t make something nonnegotiable for women but engage men in negotiations,” he said. “I think that is obvious but I have seen that happen.”
Dr. Sinha also said it is important to check your gender biases at the door before entering negotiations. Don’t view a woman asking for something as demanding or harsh when a male asking for the same exact thing is viewed as assertive and self-confident.
“Don’t fall into those traps. And if you have people that can call out your biases and help you see that, that’s important,” Dr. Sinha noted.
He also stated that hiring committees need to show diversity in terms of gender, race, and ethnicity, adding that it is “hugely important” that you do that.
The bottom line is to not force women to negotiate for equal pay, Dr. Sinha noted. “The gender gap is well documented in medicine, and you really have to do your part.”
PHILADELPHIA – that they need to account for: the gender wage gap.
“Find a lawyer ... that will support your fight for pay equity,” Michael Sinha, MD, advised in a presentation at the annual meeting of the American College of Physicians.
“Definitely interview them,” said Dr. Sinha of Harvard Medical School, Boston. “Get a sense of how committed they are to that cause. Seek recommendations from other women in medicine. Maybe they will point you to the person who really is committed to this cause and wants to help you.”
He also cautioned that physicians might have to help their lawyer fill in the knowledge gap. “Sometimes you need to provide that lawyer with data. There are a lot of reports that have been published from various organizations [including the ACP]. Don’t assume that the lawyer has the evidence.”
Armed with evidence, he said there is opportunity to address gender pay gaps in the contract. “You can put a lot of things into your contract, why not some of these things? If there is institutional evidence of a pay gap or a leaky promotional pipeline, you are telling them you have a problem with salary discrepancies between male and female physicians and I need to protect my own self-worth.”
Dr. Sinha recommended prospective employees develop strategies with their lawyers, which could mean letting the lawyer take the lead in the negotiations.
“Maybe that reduces stress or emotion in the process. That will preserve a good relationship with the employer,” he said. “A confident, knowledgeable lawyer may help mitigate gender differences in negotiation strategy.”
In order to help close the gender gap, Dr. Sinha said he advises his male colleagues to help female physicians by being open about their compensation, especially if compensation is not public information. “I have been encouraging male physician colleagues of mine to share that information when you are asked. Don’t make it impossible for someone to figure out.”
He noted that it is not likely that closing the gender gap by raising women’s compensation is going to result in male physicians losing money, but rather in the long run it will mean better compensation for everyone.
Dr. Sinha also had this advice for employers: “Before you do anything else, level your pay gap. ... For every physician that works in your organization, level your pay gap. Offer equitable salary packages up front to men and women. Understand your responsibilities under federal and state equal pay laws.”
When it comes to equitable compensation packages, all offerings, including salary and fringe benefits, should be offered to both male and female physicians or to neither.
“Don’t make something nonnegotiable for women but engage men in negotiations,” he said. “I think that is obvious but I have seen that happen.”
Dr. Sinha also said it is important to check your gender biases at the door before entering negotiations. Don’t view a woman asking for something as demanding or harsh when a male asking for the same exact thing is viewed as assertive and self-confident.
“Don’t fall into those traps. And if you have people that can call out your biases and help you see that, that’s important,” Dr. Sinha noted.
He also stated that hiring committees need to show diversity in terms of gender, race, and ethnicity, adding that it is “hugely important” that you do that.
The bottom line is to not force women to negotiate for equal pay, Dr. Sinha noted. “The gender gap is well documented in medicine, and you really have to do your part.”
PHILADELPHIA – that they need to account for: the gender wage gap.
“Find a lawyer ... that will support your fight for pay equity,” Michael Sinha, MD, advised in a presentation at the annual meeting of the American College of Physicians.
“Definitely interview them,” said Dr. Sinha of Harvard Medical School, Boston. “Get a sense of how committed they are to that cause. Seek recommendations from other women in medicine. Maybe they will point you to the person who really is committed to this cause and wants to help you.”
He also cautioned that physicians might have to help their lawyer fill in the knowledge gap. “Sometimes you need to provide that lawyer with data. There are a lot of reports that have been published from various organizations [including the ACP]. Don’t assume that the lawyer has the evidence.”
Armed with evidence, he said there is opportunity to address gender pay gaps in the contract. “You can put a lot of things into your contract, why not some of these things? If there is institutional evidence of a pay gap or a leaky promotional pipeline, you are telling them you have a problem with salary discrepancies between male and female physicians and I need to protect my own self-worth.”
Dr. Sinha recommended prospective employees develop strategies with their lawyers, which could mean letting the lawyer take the lead in the negotiations.
“Maybe that reduces stress or emotion in the process. That will preserve a good relationship with the employer,” he said. “A confident, knowledgeable lawyer may help mitigate gender differences in negotiation strategy.”
In order to help close the gender gap, Dr. Sinha said he advises his male colleagues to help female physicians by being open about their compensation, especially if compensation is not public information. “I have been encouraging male physician colleagues of mine to share that information when you are asked. Don’t make it impossible for someone to figure out.”
He noted that it is not likely that closing the gender gap by raising women’s compensation is going to result in male physicians losing money, but rather in the long run it will mean better compensation for everyone.
Dr. Sinha also had this advice for employers: “Before you do anything else, level your pay gap. ... For every physician that works in your organization, level your pay gap. Offer equitable salary packages up front to men and women. Understand your responsibilities under federal and state equal pay laws.”
When it comes to equitable compensation packages, all offerings, including salary and fringe benefits, should be offered to both male and female physicians or to neither.
“Don’t make something nonnegotiable for women but engage men in negotiations,” he said. “I think that is obvious but I have seen that happen.”
Dr. Sinha also said it is important to check your gender biases at the door before entering negotiations. Don’t view a woman asking for something as demanding or harsh when a male asking for the same exact thing is viewed as assertive and self-confident.
“Don’t fall into those traps. And if you have people that can call out your biases and help you see that, that’s important,” Dr. Sinha noted.
He also stated that hiring committees need to show diversity in terms of gender, race, and ethnicity, adding that it is “hugely important” that you do that.
The bottom line is to not force women to negotiate for equal pay, Dr. Sinha noted. “The gender gap is well documented in medicine, and you really have to do your part.”
REPORTING FROM INTERNAL MEDICINE 2019
In defense of hospital administrators
Improving relationships between leaders and clinicians
In the March 2019 issue of The Hospitalist, I wrote about some key findings from a 2018 survey of U.S. physicians by The Physicians Foundation. It’s no surprise to anyone working in health care today that the survey found alarming levels of professional dissatisfaction, burnout, and pessimism about the future of medicine among respondent physicians. Sadly, it appears that much of that pessimism is directed toward hospitals and their leaders: 46% of survey respondents viewed the relationships between physicians and hospitals as somewhat or mostly negative and adversarial.
Several physicians posted comments online, and they deeply saddened me. My heart hurt for those doctors who wrote, “I loved medicine. It was good for my soul, but medicine left me. Doctors gave up most of their power and large corporations without an ethical foundation and no god, but money took over.” Or “They are waiting so all the senior physicians will retire. Nurses will become leaders who will follow administration’s lead and control physicians. Money and cost cutting is the major driver. Physicians are not valuable anymore because they have different opinions which cost a lot. There is a lot of window dressing, but they actually don’t care. They just want to run a business.” I also read “I was tossed out like dirty laundry water at age 59.” And “On a personal basis, I will try to reason with management exactly once before I bail.” Sigh.
These commenters are well-meaning physicians who had bad experiences with hospital leaders they saw as uncaring and unresponsive to their concerns as clinicians. Their experiences left them demoralized and embittered. I’m truly sorry for that.
I’m a recovering hospital administrator myself. My business partner John Nelson, MD, MHM, likes to tell people that he has successfully deprogrammed me from the way most administrators think about doctors, but he’s mostly joking (at least I think he is). I can tell you that most of the hospital leaders I have met – both when I was still an administrator and now in my consulting work – are well-intentioned people who care deeply about patients and their fellow health care professionals and are trying hard to do the right thing. Many of them could have earned more and had better career opportunities doing similar work in a field other than health care, but they chose health care out of a sincere desire to do good and help people.
A big part of the problem is that doctors and administrators come to health care from very different starting points, and so have very different perspectives. They generally function in separate silos, each paying attention to their own comfortable little part of that monster we call a health care delivery system. Often, neither administrators nor doctors have made enough effort to cross over and understand the issues and perspectives of people in other silos. As a result, it’s easy for assumptions and biases to creep in and poison our interactions.
When we interpret the behavior of others, we humans tend to overemphasize dispositional factors, such as personality or motives, and to discount situational factors, such as external stressors. Psychologists call this the fundamental attribution error or correspondence bias, and the result is usually heightened conflict as a result of presumed negative intentions on the part of others (“All she cares about is making a profit”) and discounting circumstantial factors that might be influencing others’ behavior (“She is facing reduced market share and a funding shortfall, and she’s fearful for the future of the institution”).
Add in another phenomenon known as the actor-observer bias, in which we tend to attribute others’ behavior to their dispositions but attribute our own behavior to the circumstances (“That administrator lost his temper because he’s a demanding jerk, but I only lost my temper because he pushed me over the edge”).
Is it possible that hospital leaders and doctors are reading each other inaccurately and that they’re making assumptions about each other’s intentions that get in the way of having constructive dialogue? How can we get to a place of greater trust? I don’t know the whole answer, of course, but I have a few ideas to offer.
Read the full post at hospitalleader.org.
Improving relationships between leaders and clinicians
Improving relationships between leaders and clinicians
In the March 2019 issue of The Hospitalist, I wrote about some key findings from a 2018 survey of U.S. physicians by The Physicians Foundation. It’s no surprise to anyone working in health care today that the survey found alarming levels of professional dissatisfaction, burnout, and pessimism about the future of medicine among respondent physicians. Sadly, it appears that much of that pessimism is directed toward hospitals and their leaders: 46% of survey respondents viewed the relationships between physicians and hospitals as somewhat or mostly negative and adversarial.
Several physicians posted comments online, and they deeply saddened me. My heart hurt for those doctors who wrote, “I loved medicine. It was good for my soul, but medicine left me. Doctors gave up most of their power and large corporations without an ethical foundation and no god, but money took over.” Or “They are waiting so all the senior physicians will retire. Nurses will become leaders who will follow administration’s lead and control physicians. Money and cost cutting is the major driver. Physicians are not valuable anymore because they have different opinions which cost a lot. There is a lot of window dressing, but they actually don’t care. They just want to run a business.” I also read “I was tossed out like dirty laundry water at age 59.” And “On a personal basis, I will try to reason with management exactly once before I bail.” Sigh.
These commenters are well-meaning physicians who had bad experiences with hospital leaders they saw as uncaring and unresponsive to their concerns as clinicians. Their experiences left them demoralized and embittered. I’m truly sorry for that.
I’m a recovering hospital administrator myself. My business partner John Nelson, MD, MHM, likes to tell people that he has successfully deprogrammed me from the way most administrators think about doctors, but he’s mostly joking (at least I think he is). I can tell you that most of the hospital leaders I have met – both when I was still an administrator and now in my consulting work – are well-intentioned people who care deeply about patients and their fellow health care professionals and are trying hard to do the right thing. Many of them could have earned more and had better career opportunities doing similar work in a field other than health care, but they chose health care out of a sincere desire to do good and help people.
A big part of the problem is that doctors and administrators come to health care from very different starting points, and so have very different perspectives. They generally function in separate silos, each paying attention to their own comfortable little part of that monster we call a health care delivery system. Often, neither administrators nor doctors have made enough effort to cross over and understand the issues and perspectives of people in other silos. As a result, it’s easy for assumptions and biases to creep in and poison our interactions.
When we interpret the behavior of others, we humans tend to overemphasize dispositional factors, such as personality or motives, and to discount situational factors, such as external stressors. Psychologists call this the fundamental attribution error or correspondence bias, and the result is usually heightened conflict as a result of presumed negative intentions on the part of others (“All she cares about is making a profit”) and discounting circumstantial factors that might be influencing others’ behavior (“She is facing reduced market share and a funding shortfall, and she’s fearful for the future of the institution”).
Add in another phenomenon known as the actor-observer bias, in which we tend to attribute others’ behavior to their dispositions but attribute our own behavior to the circumstances (“That administrator lost his temper because he’s a demanding jerk, but I only lost my temper because he pushed me over the edge”).
Is it possible that hospital leaders and doctors are reading each other inaccurately and that they’re making assumptions about each other’s intentions that get in the way of having constructive dialogue? How can we get to a place of greater trust? I don’t know the whole answer, of course, but I have a few ideas to offer.
Read the full post at hospitalleader.org.
In the March 2019 issue of The Hospitalist, I wrote about some key findings from a 2018 survey of U.S. physicians by The Physicians Foundation. It’s no surprise to anyone working in health care today that the survey found alarming levels of professional dissatisfaction, burnout, and pessimism about the future of medicine among respondent physicians. Sadly, it appears that much of that pessimism is directed toward hospitals and their leaders: 46% of survey respondents viewed the relationships between physicians and hospitals as somewhat or mostly negative and adversarial.
Several physicians posted comments online, and they deeply saddened me. My heart hurt for those doctors who wrote, “I loved medicine. It was good for my soul, but medicine left me. Doctors gave up most of their power and large corporations without an ethical foundation and no god, but money took over.” Or “They are waiting so all the senior physicians will retire. Nurses will become leaders who will follow administration’s lead and control physicians. Money and cost cutting is the major driver. Physicians are not valuable anymore because they have different opinions which cost a lot. There is a lot of window dressing, but they actually don’t care. They just want to run a business.” I also read “I was tossed out like dirty laundry water at age 59.” And “On a personal basis, I will try to reason with management exactly once before I bail.” Sigh.
These commenters are well-meaning physicians who had bad experiences with hospital leaders they saw as uncaring and unresponsive to their concerns as clinicians. Their experiences left them demoralized and embittered. I’m truly sorry for that.
I’m a recovering hospital administrator myself. My business partner John Nelson, MD, MHM, likes to tell people that he has successfully deprogrammed me from the way most administrators think about doctors, but he’s mostly joking (at least I think he is). I can tell you that most of the hospital leaders I have met – both when I was still an administrator and now in my consulting work – are well-intentioned people who care deeply about patients and their fellow health care professionals and are trying hard to do the right thing. Many of them could have earned more and had better career opportunities doing similar work in a field other than health care, but they chose health care out of a sincere desire to do good and help people.
A big part of the problem is that doctors and administrators come to health care from very different starting points, and so have very different perspectives. They generally function in separate silos, each paying attention to their own comfortable little part of that monster we call a health care delivery system. Often, neither administrators nor doctors have made enough effort to cross over and understand the issues and perspectives of people in other silos. As a result, it’s easy for assumptions and biases to creep in and poison our interactions.
When we interpret the behavior of others, we humans tend to overemphasize dispositional factors, such as personality or motives, and to discount situational factors, such as external stressors. Psychologists call this the fundamental attribution error or correspondence bias, and the result is usually heightened conflict as a result of presumed negative intentions on the part of others (“All she cares about is making a profit”) and discounting circumstantial factors that might be influencing others’ behavior (“She is facing reduced market share and a funding shortfall, and she’s fearful for the future of the institution”).
Add in another phenomenon known as the actor-observer bias, in which we tend to attribute others’ behavior to their dispositions but attribute our own behavior to the circumstances (“That administrator lost his temper because he’s a demanding jerk, but I only lost my temper because he pushed me over the edge”).
Is it possible that hospital leaders and doctors are reading each other inaccurately and that they’re making assumptions about each other’s intentions that get in the way of having constructive dialogue? How can we get to a place of greater trust? I don’t know the whole answer, of course, but I have a few ideas to offer.
Read the full post at hospitalleader.org.
Embracing an executive leadership role
Dr. Bryce Gartland says hospitalists thrive as leaders
Bryce Gartland, MD, was working as a full-time hospitalist at Emory University Hospital in Atlanta when hospital administrators first started asking him to take on administrative roles, such as clinical site director or medical director of care coordination.
Today, Dr. Gartland is hospital group president and cochief of clinical operations for Emory Healthcare, with responsibility for overall performance and achievement across all 11 Emory hospitals. In that role, he keeps his eyes open for similar talent and leadership potential in younger physicians.
Following internal medicine residency at Cedars-Sinai Medical Center in Los Angeles, Dr. Gartland moved into a traditional private practice setting in Beverly Hills. “Two years later, my wife and I decided to move back to my home town of Atlanta. This was 2005 and hospital medicine was a nascent movement in health care. I was intrigued, and Emory had a strong hospitalist program based in a major academic medical setting, which has since grown from approximately 20 physicians to over 120 across seven hospitals,” he said.
Senior leaders at Emory recognized something in Dr. Gartland and more administrative offers were forthcoming.
“After a year of practicing at Emory, the system’s chief financial officer knocked on my door to ask if I would be interested in becoming medical director for care coordination. This role afforded me tremendous opportunities to get involved in clinical/administrative activities at Emory – utilization review, hospice and palliative care, transitions of care, interface with managed care organizations. The role was very rewarding. In some ways, I became a kind of chief translator at the hospital for anything clinical that also had financial implications,” he recalled.
“Then we went through a reorganization and I was offered the opportunity to step into the chief operating officer position at Emory University Hospital. Shortly thereafter, there was leadership turnover within the division of hospital medicine and I was asked by the CEO of Emory Healthcare and chair of the department of medicine to serve as section head for hospital medicine.” Dr. Gartland wore both of those hats for about 2 years, later becoming the CEO of Emory University Hospital and two other facilities within the system. He was appointed to his current position as hospital group president and cochief of clinical operations for Emory Healthcare in 2018.
Consumed with administrative responsibilities, he largely had to step away from patient care, although with mixed emotions.
“Over the years, I worked hard to maintain a strong clinical role, but the reality is that if you are not delivering patient care routinely, it’s difficult to practice at the highest level of current medical practice,” he said. Nonetheless, Dr. Gartland tries to keep a hand in patient care by routinely rounding with hospitalist teams and attending care conferences.
Fixing the larger health care system
“I am a huge supporter of more physicians becoming actively engaged in administrative positions in health care. They are key to helping us best fix the larger health care system,” Dr. Gartland said. “However, we’ve all seen clinicians drafted into administrative positions who were not great administrators. One needs to be bilingual in both medicine and business. While some skills, such as strong communication, may cross over, it’s important to recognize that clinical strength and success do not necessarily equate to administrative achievement.”
Dr. Gartland also believes in the importance of mentorship in developing future leaders and in seeking and engaging mentors from other disciplines outside of one’s own specialty. “I’ve been fortunate to have a number of mentors who saw something in me and supported investment in my personal and professional development. I am now fortunate to be in the position to give back by mentoring a number of younger hospitalists who are interested in growing their nonclinical roles.”
“One bit of advice from a mentor that really resonated with me was: Don’t let the urgent get in the way of the important,” Dr. Gartland said. “Life is busy and full of urgent day-to-day fires. It’s important to take the time to pause and consider where you are going and what you are doing to enhance your career development. Are you getting the right kinds of feedback?” He explained that a coach or mentor who can provide constructive feedback is important and is something he has relied upon throughout his own professional development.
Different paths to learning business
Dr. Gartland did not pursue formal business training before the administrative opportunities started to multiply for him at Emory, although in college he had a strong interest in both business and medicine and at one time contemplated going into either.
“Over the years, my mentors have given me a lot of advice, one of which was that a medical degree can be a passport to a lot of different career paths, with real opportunities for merging business and medicine,” he said.
He has since intentionally pursued business training opportunities wherever they came up, such as courses offered by the American College of Physician Executives (now the American Association for Physician Leadership). “At one point, I considered going back to college in an MBA program, but that’s when John Fox – then Emory Healthcare’s CEO – called and said he wanted to send me to the Harvard Business School’s Managing Health Care Delivery executive education program, with an Emory team comprising the chief nurse executive, chief of human resources, and CEO for one of our hospitals.” Harvard’s roughly 9-month program involves 3 weeks on campus with assignments between the on-campus visits.
“In my current role as hospital group president, I have direct responsibility for our hospitals’ and system’s clinically essential services such as radiology, laboratory, pharmacy, and perioperative medicine. I also still serve as CEO for Emory University Hospital while we recruit my replacement,” Dr. Gartland said. “Overall, my work time breaks down roughly into thirds. One-third is spent on strategy and strategic initiatives – such as organizational and program design. Our system recently acquired a large community health system whose strategic and operational integration I am actively leading.”
Another third of his time is focused on operations, and the final third is focused on talent management and development. “People are truly the most valuable asset any organization has, particularly in health care,” he noted. “Being intentional about organizational design, coaching, and supporting the development and deployment of talent at all levels of the organization helps everyone achieve their full potential. It is one of the most important roles a leader can play.”
Dr. Gartland said that Emory is committed to Lean-based management systems, using both horizontal and vertical strategies for process improvement and waste reduction, with implementation beginning in urology, transplant, and heart and vascular services. Experts say Lean success starts at the very top, and Emory and Dr. Gartland are all in.
“These types of changes are measured in 5- to 7-year increments or more, not in months. We believe this is key to creating the best workplace to support the highest quality, experience, and value in health care delivery. It creates and supports the right culture within an organization, and we have made the commitment to following that path,” he said.
Recognizing leadership potential
What does Dr. Gartland look for in physicians with leadership potential?
“Are you someone who collaborates well?” he asked. “Someone who raises your hand at meetings or gets engaged with the issues? Do you volunteer to take on assignments? Are you someone with a balanced perspective, system minded in thinking and inquisitive, with a positive approach to problem solving?”
A lot of physicians might come to a meeting with the hospital or their boss and complain about all the things that aren’t working, he said, but “it’s rarer for them to come in and say: ‘I see these problems, and here’s where I think we can make improvements. How can I help?’ ” Dr. Gartland looks for evidence of emotional intelligence and the ability to effect change management across disciplines. Another skill with ever-greater importance is comfort with data and data-driven decision making.
“When our national health care system is experiencing so much change and upheaval, much of which is captured in newspaper headlines, it can sound scary,” he said. “I encourage people to see that complex, dynamic times like these, filled with so much change, are also a tremendous opportunity. Run towards and embrace the opportunity for change. Hospitalists, by nature, bring with them a tremendous background and experience set that is invaluable to help lead positive change in these dynamic times.”
The SHM has offerings for hospitalists wanting to advance in leadership positions, Dr. Gartland said, including its annual Leadership Academy. The next one is scheduled to be held in Nashville, Tenn., Nov. 4-7, 2019.
“The Leadership Academy is a great initial step for physicians, especially those early in their careers. Also, try to gain exposure to a variety of perspectives outside of hospital medicine,” he said. “I’d love to see further advances in leadership for our specialty – growing the number of hospitalists who serve as hospital CEOs or CMOs and in other leadership roles. We have more to learn collectively about leadership as a specialty, and I’d love to see us grow that capacity by offering further learning opportunities and bringing together hospitalists who have an interest in advancing leadership.”
Dr. Bryce Gartland says hospitalists thrive as leaders
Dr. Bryce Gartland says hospitalists thrive as leaders
Bryce Gartland, MD, was working as a full-time hospitalist at Emory University Hospital in Atlanta when hospital administrators first started asking him to take on administrative roles, such as clinical site director or medical director of care coordination.
Today, Dr. Gartland is hospital group president and cochief of clinical operations for Emory Healthcare, with responsibility for overall performance and achievement across all 11 Emory hospitals. In that role, he keeps his eyes open for similar talent and leadership potential in younger physicians.
Following internal medicine residency at Cedars-Sinai Medical Center in Los Angeles, Dr. Gartland moved into a traditional private practice setting in Beverly Hills. “Two years later, my wife and I decided to move back to my home town of Atlanta. This was 2005 and hospital medicine was a nascent movement in health care. I was intrigued, and Emory had a strong hospitalist program based in a major academic medical setting, which has since grown from approximately 20 physicians to over 120 across seven hospitals,” he said.
Senior leaders at Emory recognized something in Dr. Gartland and more administrative offers were forthcoming.
“After a year of practicing at Emory, the system’s chief financial officer knocked on my door to ask if I would be interested in becoming medical director for care coordination. This role afforded me tremendous opportunities to get involved in clinical/administrative activities at Emory – utilization review, hospice and palliative care, transitions of care, interface with managed care organizations. The role was very rewarding. In some ways, I became a kind of chief translator at the hospital for anything clinical that also had financial implications,” he recalled.
“Then we went through a reorganization and I was offered the opportunity to step into the chief operating officer position at Emory University Hospital. Shortly thereafter, there was leadership turnover within the division of hospital medicine and I was asked by the CEO of Emory Healthcare and chair of the department of medicine to serve as section head for hospital medicine.” Dr. Gartland wore both of those hats for about 2 years, later becoming the CEO of Emory University Hospital and two other facilities within the system. He was appointed to his current position as hospital group president and cochief of clinical operations for Emory Healthcare in 2018.
Consumed with administrative responsibilities, he largely had to step away from patient care, although with mixed emotions.
“Over the years, I worked hard to maintain a strong clinical role, but the reality is that if you are not delivering patient care routinely, it’s difficult to practice at the highest level of current medical practice,” he said. Nonetheless, Dr. Gartland tries to keep a hand in patient care by routinely rounding with hospitalist teams and attending care conferences.
Fixing the larger health care system
“I am a huge supporter of more physicians becoming actively engaged in administrative positions in health care. They are key to helping us best fix the larger health care system,” Dr. Gartland said. “However, we’ve all seen clinicians drafted into administrative positions who were not great administrators. One needs to be bilingual in both medicine and business. While some skills, such as strong communication, may cross over, it’s important to recognize that clinical strength and success do not necessarily equate to administrative achievement.”
Dr. Gartland also believes in the importance of mentorship in developing future leaders and in seeking and engaging mentors from other disciplines outside of one’s own specialty. “I’ve been fortunate to have a number of mentors who saw something in me and supported investment in my personal and professional development. I am now fortunate to be in the position to give back by mentoring a number of younger hospitalists who are interested in growing their nonclinical roles.”
“One bit of advice from a mentor that really resonated with me was: Don’t let the urgent get in the way of the important,” Dr. Gartland said. “Life is busy and full of urgent day-to-day fires. It’s important to take the time to pause and consider where you are going and what you are doing to enhance your career development. Are you getting the right kinds of feedback?” He explained that a coach or mentor who can provide constructive feedback is important and is something he has relied upon throughout his own professional development.
Different paths to learning business
Dr. Gartland did not pursue formal business training before the administrative opportunities started to multiply for him at Emory, although in college he had a strong interest in both business and medicine and at one time contemplated going into either.
“Over the years, my mentors have given me a lot of advice, one of which was that a medical degree can be a passport to a lot of different career paths, with real opportunities for merging business and medicine,” he said.
He has since intentionally pursued business training opportunities wherever they came up, such as courses offered by the American College of Physician Executives (now the American Association for Physician Leadership). “At one point, I considered going back to college in an MBA program, but that’s when John Fox – then Emory Healthcare’s CEO – called and said he wanted to send me to the Harvard Business School’s Managing Health Care Delivery executive education program, with an Emory team comprising the chief nurse executive, chief of human resources, and CEO for one of our hospitals.” Harvard’s roughly 9-month program involves 3 weeks on campus with assignments between the on-campus visits.
“In my current role as hospital group president, I have direct responsibility for our hospitals’ and system’s clinically essential services such as radiology, laboratory, pharmacy, and perioperative medicine. I also still serve as CEO for Emory University Hospital while we recruit my replacement,” Dr. Gartland said. “Overall, my work time breaks down roughly into thirds. One-third is spent on strategy and strategic initiatives – such as organizational and program design. Our system recently acquired a large community health system whose strategic and operational integration I am actively leading.”
Another third of his time is focused on operations, and the final third is focused on talent management and development. “People are truly the most valuable asset any organization has, particularly in health care,” he noted. “Being intentional about organizational design, coaching, and supporting the development and deployment of talent at all levels of the organization helps everyone achieve their full potential. It is one of the most important roles a leader can play.”
Dr. Gartland said that Emory is committed to Lean-based management systems, using both horizontal and vertical strategies for process improvement and waste reduction, with implementation beginning in urology, transplant, and heart and vascular services. Experts say Lean success starts at the very top, and Emory and Dr. Gartland are all in.
“These types of changes are measured in 5- to 7-year increments or more, not in months. We believe this is key to creating the best workplace to support the highest quality, experience, and value in health care delivery. It creates and supports the right culture within an organization, and we have made the commitment to following that path,” he said.
Recognizing leadership potential
What does Dr. Gartland look for in physicians with leadership potential?
“Are you someone who collaborates well?” he asked. “Someone who raises your hand at meetings or gets engaged with the issues? Do you volunteer to take on assignments? Are you someone with a balanced perspective, system minded in thinking and inquisitive, with a positive approach to problem solving?”
A lot of physicians might come to a meeting with the hospital or their boss and complain about all the things that aren’t working, he said, but “it’s rarer for them to come in and say: ‘I see these problems, and here’s where I think we can make improvements. How can I help?’ ” Dr. Gartland looks for evidence of emotional intelligence and the ability to effect change management across disciplines. Another skill with ever-greater importance is comfort with data and data-driven decision making.
“When our national health care system is experiencing so much change and upheaval, much of which is captured in newspaper headlines, it can sound scary,” he said. “I encourage people to see that complex, dynamic times like these, filled with so much change, are also a tremendous opportunity. Run towards and embrace the opportunity for change. Hospitalists, by nature, bring with them a tremendous background and experience set that is invaluable to help lead positive change in these dynamic times.”
The SHM has offerings for hospitalists wanting to advance in leadership positions, Dr. Gartland said, including its annual Leadership Academy. The next one is scheduled to be held in Nashville, Tenn., Nov. 4-7, 2019.
“The Leadership Academy is a great initial step for physicians, especially those early in their careers. Also, try to gain exposure to a variety of perspectives outside of hospital medicine,” he said. “I’d love to see further advances in leadership for our specialty – growing the number of hospitalists who serve as hospital CEOs or CMOs and in other leadership roles. We have more to learn collectively about leadership as a specialty, and I’d love to see us grow that capacity by offering further learning opportunities and bringing together hospitalists who have an interest in advancing leadership.”
Bryce Gartland, MD, was working as a full-time hospitalist at Emory University Hospital in Atlanta when hospital administrators first started asking him to take on administrative roles, such as clinical site director or medical director of care coordination.
Today, Dr. Gartland is hospital group president and cochief of clinical operations for Emory Healthcare, with responsibility for overall performance and achievement across all 11 Emory hospitals. In that role, he keeps his eyes open for similar talent and leadership potential in younger physicians.
Following internal medicine residency at Cedars-Sinai Medical Center in Los Angeles, Dr. Gartland moved into a traditional private practice setting in Beverly Hills. “Two years later, my wife and I decided to move back to my home town of Atlanta. This was 2005 and hospital medicine was a nascent movement in health care. I was intrigued, and Emory had a strong hospitalist program based in a major academic medical setting, which has since grown from approximately 20 physicians to over 120 across seven hospitals,” he said.
Senior leaders at Emory recognized something in Dr. Gartland and more administrative offers were forthcoming.
“After a year of practicing at Emory, the system’s chief financial officer knocked on my door to ask if I would be interested in becoming medical director for care coordination. This role afforded me tremendous opportunities to get involved in clinical/administrative activities at Emory – utilization review, hospice and palliative care, transitions of care, interface with managed care organizations. The role was very rewarding. In some ways, I became a kind of chief translator at the hospital for anything clinical that also had financial implications,” he recalled.
“Then we went through a reorganization and I was offered the opportunity to step into the chief operating officer position at Emory University Hospital. Shortly thereafter, there was leadership turnover within the division of hospital medicine and I was asked by the CEO of Emory Healthcare and chair of the department of medicine to serve as section head for hospital medicine.” Dr. Gartland wore both of those hats for about 2 years, later becoming the CEO of Emory University Hospital and two other facilities within the system. He was appointed to his current position as hospital group president and cochief of clinical operations for Emory Healthcare in 2018.
Consumed with administrative responsibilities, he largely had to step away from patient care, although with mixed emotions.
“Over the years, I worked hard to maintain a strong clinical role, but the reality is that if you are not delivering patient care routinely, it’s difficult to practice at the highest level of current medical practice,” he said. Nonetheless, Dr. Gartland tries to keep a hand in patient care by routinely rounding with hospitalist teams and attending care conferences.
Fixing the larger health care system
“I am a huge supporter of more physicians becoming actively engaged in administrative positions in health care. They are key to helping us best fix the larger health care system,” Dr. Gartland said. “However, we’ve all seen clinicians drafted into administrative positions who were not great administrators. One needs to be bilingual in both medicine and business. While some skills, such as strong communication, may cross over, it’s important to recognize that clinical strength and success do not necessarily equate to administrative achievement.”
Dr. Gartland also believes in the importance of mentorship in developing future leaders and in seeking and engaging mentors from other disciplines outside of one’s own specialty. “I’ve been fortunate to have a number of mentors who saw something in me and supported investment in my personal and professional development. I am now fortunate to be in the position to give back by mentoring a number of younger hospitalists who are interested in growing their nonclinical roles.”
“One bit of advice from a mentor that really resonated with me was: Don’t let the urgent get in the way of the important,” Dr. Gartland said. “Life is busy and full of urgent day-to-day fires. It’s important to take the time to pause and consider where you are going and what you are doing to enhance your career development. Are you getting the right kinds of feedback?” He explained that a coach or mentor who can provide constructive feedback is important and is something he has relied upon throughout his own professional development.
Different paths to learning business
Dr. Gartland did not pursue formal business training before the administrative opportunities started to multiply for him at Emory, although in college he had a strong interest in both business and medicine and at one time contemplated going into either.
“Over the years, my mentors have given me a lot of advice, one of which was that a medical degree can be a passport to a lot of different career paths, with real opportunities for merging business and medicine,” he said.
He has since intentionally pursued business training opportunities wherever they came up, such as courses offered by the American College of Physician Executives (now the American Association for Physician Leadership). “At one point, I considered going back to college in an MBA program, but that’s when John Fox – then Emory Healthcare’s CEO – called and said he wanted to send me to the Harvard Business School’s Managing Health Care Delivery executive education program, with an Emory team comprising the chief nurse executive, chief of human resources, and CEO for one of our hospitals.” Harvard’s roughly 9-month program involves 3 weeks on campus with assignments between the on-campus visits.
“In my current role as hospital group president, I have direct responsibility for our hospitals’ and system’s clinically essential services such as radiology, laboratory, pharmacy, and perioperative medicine. I also still serve as CEO for Emory University Hospital while we recruit my replacement,” Dr. Gartland said. “Overall, my work time breaks down roughly into thirds. One-third is spent on strategy and strategic initiatives – such as organizational and program design. Our system recently acquired a large community health system whose strategic and operational integration I am actively leading.”
Another third of his time is focused on operations, and the final third is focused on talent management and development. “People are truly the most valuable asset any organization has, particularly in health care,” he noted. “Being intentional about organizational design, coaching, and supporting the development and deployment of talent at all levels of the organization helps everyone achieve their full potential. It is one of the most important roles a leader can play.”
Dr. Gartland said that Emory is committed to Lean-based management systems, using both horizontal and vertical strategies for process improvement and waste reduction, with implementation beginning in urology, transplant, and heart and vascular services. Experts say Lean success starts at the very top, and Emory and Dr. Gartland are all in.
“These types of changes are measured in 5- to 7-year increments or more, not in months. We believe this is key to creating the best workplace to support the highest quality, experience, and value in health care delivery. It creates and supports the right culture within an organization, and we have made the commitment to following that path,” he said.
Recognizing leadership potential
What does Dr. Gartland look for in physicians with leadership potential?
“Are you someone who collaborates well?” he asked. “Someone who raises your hand at meetings or gets engaged with the issues? Do you volunteer to take on assignments? Are you someone with a balanced perspective, system minded in thinking and inquisitive, with a positive approach to problem solving?”
A lot of physicians might come to a meeting with the hospital or their boss and complain about all the things that aren’t working, he said, but “it’s rarer for them to come in and say: ‘I see these problems, and here’s where I think we can make improvements. How can I help?’ ” Dr. Gartland looks for evidence of emotional intelligence and the ability to effect change management across disciplines. Another skill with ever-greater importance is comfort with data and data-driven decision making.
“When our national health care system is experiencing so much change and upheaval, much of which is captured in newspaper headlines, it can sound scary,” he said. “I encourage people to see that complex, dynamic times like these, filled with so much change, are also a tremendous opportunity. Run towards and embrace the opportunity for change. Hospitalists, by nature, bring with them a tremendous background and experience set that is invaluable to help lead positive change in these dynamic times.”
The SHM has offerings for hospitalists wanting to advance in leadership positions, Dr. Gartland said, including its annual Leadership Academy. The next one is scheduled to be held in Nashville, Tenn., Nov. 4-7, 2019.
“The Leadership Academy is a great initial step for physicians, especially those early in their careers. Also, try to gain exposure to a variety of perspectives outside of hospital medicine,” he said. “I’d love to see further advances in leadership for our specialty – growing the number of hospitalists who serve as hospital CEOs or CMOs and in other leadership roles. We have more to learn collectively about leadership as a specialty, and I’d love to see us grow that capacity by offering further learning opportunities and bringing together hospitalists who have an interest in advancing leadership.”














