User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Three-drug combo proves effective against multidrug-resistant UTIs
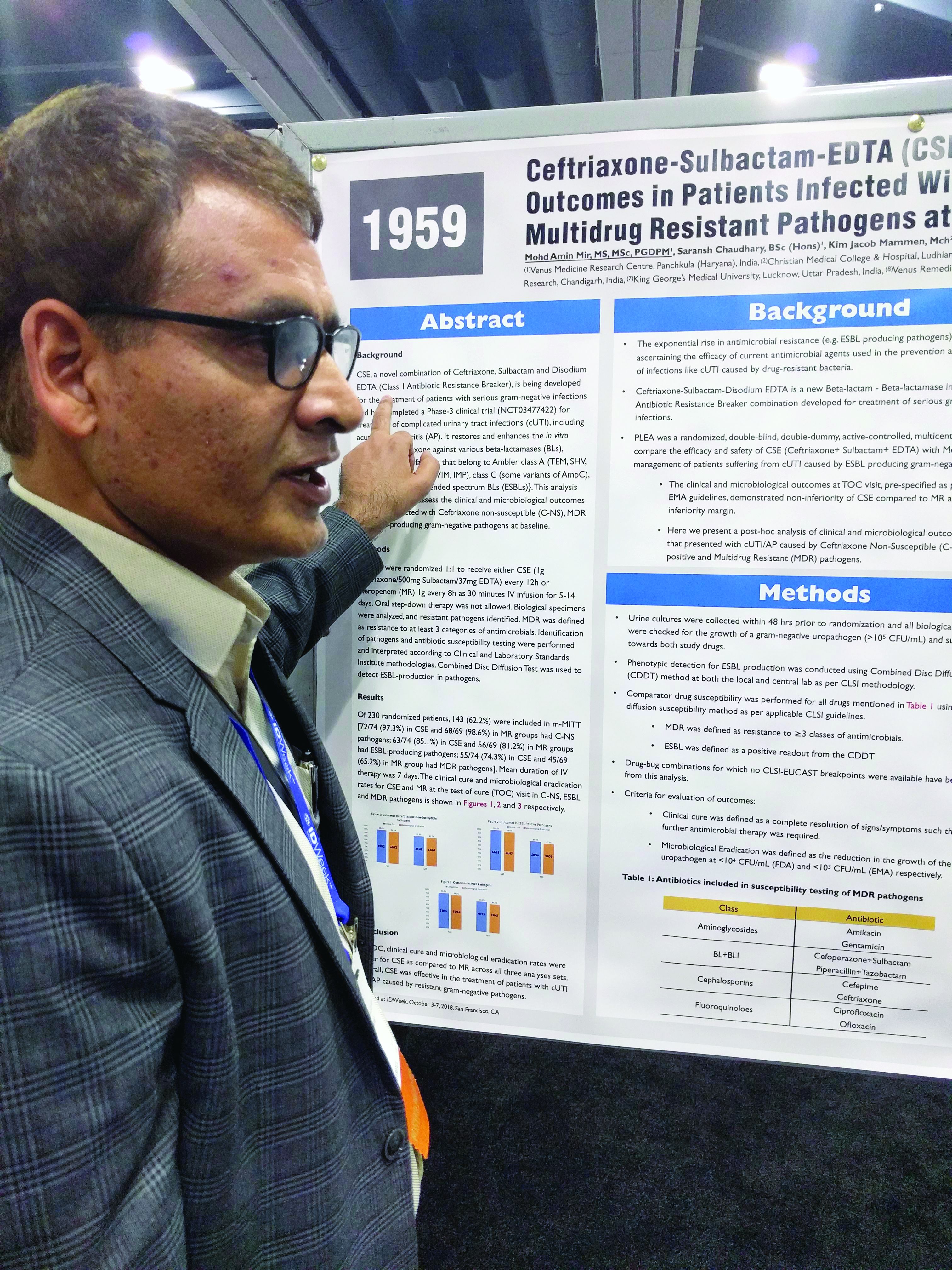
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
REPORTING FROM IDWEEK 2018
Key clinical point:
Major finding: The combination was noninferior in the context of different resistant subtypes.
Study details: Posthoc analysis of a randomized, controlled trial (n = 143).
Disclosures: The study was funded by Venus Medicine Research Center, which employs Dr. Mir.
Source: Mir MA et al. IDWeek 2018, Abstract 1959.
Launching a surgical comanagement project
Improving quality, patient satisfaction
When hospital medicine and surgical departments (usually orthopedics or neurosurgery) have joined in comanagement programs, improvements in quality metrics and patient satisfaction have often resulted.
At the Level 1 regional trauma center in which he works, Charles L. Kast, MD, and his colleagues wanted to try a comanagement agreement between hospital medicine and trauma surgery.
“The surgical team identified a need within their own department, which was to improve patient mortality and satisfaction in the inpatient setting,” said Dr. Kast, who is based at North Shore University Hospital, Manhasset, N.Y. “Their leadership sought out our hospital medicine leadership team, who then worked together to synthesize their metrics. We were able to identify other quality indicators, such as readmission rates and hospital-acquired conditions, which we felt could also benefit from our services in order to help them improve.”
Five hospitalists became members of the comanagement team. A single hospitalist rotated for 2 weeks at a time, during which they were relieved of routine hospital medicine rounding responsibilities. The hospitalist attended daily interdisciplinary rounds with the trauma surgery team, during which he/she identified patients that could benefit from hospital medicine comanagement: Patients who were over age 65 years, had multiple chronic medical conditions, or were on high-risk medications were preferentially selected. Approximately 10 patients were seen daily.
The comanagement program was well received by trauma surgeons, who talked about improved patient communication and a fostered sense of collegiality. Preliminary quality and patient satisfaction metrics were also positive.
A top takeaway is that the benefits of surgical comanagement can be demonstrated in “atypical” collaborations, depending on the needs of the department and the hospital’s vision.
“The gains in improved patient quality metrics are only half of the story,” Dr. Kast said. “Collaborating in surgical comanagement improves the satisfaction of the hospitalists and surgeons involved and can lead to future quality improvement projects or original research, both of which we are currently pursuing.”
Reference
Kast C et al. The successful development of a hospital medicine-trauma surgery co-management program [abstract]. J Hosp Med. 2017;12(suppl 2). Accessed Feb. 2, 2018.
Improving quality, patient satisfaction
Improving quality, patient satisfaction
When hospital medicine and surgical departments (usually orthopedics or neurosurgery) have joined in comanagement programs, improvements in quality metrics and patient satisfaction have often resulted.
At the Level 1 regional trauma center in which he works, Charles L. Kast, MD, and his colleagues wanted to try a comanagement agreement between hospital medicine and trauma surgery.
“The surgical team identified a need within their own department, which was to improve patient mortality and satisfaction in the inpatient setting,” said Dr. Kast, who is based at North Shore University Hospital, Manhasset, N.Y. “Their leadership sought out our hospital medicine leadership team, who then worked together to synthesize their metrics. We were able to identify other quality indicators, such as readmission rates and hospital-acquired conditions, which we felt could also benefit from our services in order to help them improve.”
Five hospitalists became members of the comanagement team. A single hospitalist rotated for 2 weeks at a time, during which they were relieved of routine hospital medicine rounding responsibilities. The hospitalist attended daily interdisciplinary rounds with the trauma surgery team, during which he/she identified patients that could benefit from hospital medicine comanagement: Patients who were over age 65 years, had multiple chronic medical conditions, or were on high-risk medications were preferentially selected. Approximately 10 patients were seen daily.
The comanagement program was well received by trauma surgeons, who talked about improved patient communication and a fostered sense of collegiality. Preliminary quality and patient satisfaction metrics were also positive.
A top takeaway is that the benefits of surgical comanagement can be demonstrated in “atypical” collaborations, depending on the needs of the department and the hospital’s vision.
“The gains in improved patient quality metrics are only half of the story,” Dr. Kast said. “Collaborating in surgical comanagement improves the satisfaction of the hospitalists and surgeons involved and can lead to future quality improvement projects or original research, both of which we are currently pursuing.”
Reference
Kast C et al. The successful development of a hospital medicine-trauma surgery co-management program [abstract]. J Hosp Med. 2017;12(suppl 2). Accessed Feb. 2, 2018.
When hospital medicine and surgical departments (usually orthopedics or neurosurgery) have joined in comanagement programs, improvements in quality metrics and patient satisfaction have often resulted.
At the Level 1 regional trauma center in which he works, Charles L. Kast, MD, and his colleagues wanted to try a comanagement agreement between hospital medicine and trauma surgery.
“The surgical team identified a need within their own department, which was to improve patient mortality and satisfaction in the inpatient setting,” said Dr. Kast, who is based at North Shore University Hospital, Manhasset, N.Y. “Their leadership sought out our hospital medicine leadership team, who then worked together to synthesize their metrics. We were able to identify other quality indicators, such as readmission rates and hospital-acquired conditions, which we felt could also benefit from our services in order to help them improve.”
Five hospitalists became members of the comanagement team. A single hospitalist rotated for 2 weeks at a time, during which they were relieved of routine hospital medicine rounding responsibilities. The hospitalist attended daily interdisciplinary rounds with the trauma surgery team, during which he/she identified patients that could benefit from hospital medicine comanagement: Patients who were over age 65 years, had multiple chronic medical conditions, or were on high-risk medications were preferentially selected. Approximately 10 patients were seen daily.
The comanagement program was well received by trauma surgeons, who talked about improved patient communication and a fostered sense of collegiality. Preliminary quality and patient satisfaction metrics were also positive.
A top takeaway is that the benefits of surgical comanagement can be demonstrated in “atypical” collaborations, depending on the needs of the department and the hospital’s vision.
“The gains in improved patient quality metrics are only half of the story,” Dr. Kast said. “Collaborating in surgical comanagement improves the satisfaction of the hospitalists and surgeons involved and can lead to future quality improvement projects or original research, both of which we are currently pursuing.”
Reference
Kast C et al. The successful development of a hospital medicine-trauma surgery co-management program [abstract]. J Hosp Med. 2017;12(suppl 2). Accessed Feb. 2, 2018.
Statins cut all-cause mortality in spinal cord injury
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
AT ANA 2018
Key clinical point:
Major finding: The mortality rate for patients on statins was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins (P less than .0052).
Study details: A retrospective review of 163 individuals with traumatic spinal cord injuries.
Disclosures: Dr. Rabadi reported having no financial disclosures.
Source: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
Septic shock: Innovative treatment options in the wings
BOSTON– treatment that require more investigation, but nevertheless appear promising, Rishi Rattan, MD, said at the annual clinical congress of the American College of Surgeons.
Trials evaluating vitamin C in this setting have demonstrated a large mortality impact with an absence of side effects, according to Dr. Rattan, a trauma and critical care surgeon with the Ryder Trauma Center at the University of Miami.
“It’s something that I have decided to start early adopting, and many of my colleagues at University of Miami do as well,” Dr. Rattan said in a panel session on updates in septic shock. “We’re anecdotally so far at least seeing good results and are going to be excited to see what these ongoing trials show.”
As an antioxidant, vitamin C has anti-inflammatory properties that may possibly attenuate the overly exuberant inflammatory response seen in septic shock, Dr. Rattan said in his presentation.
The limited clinical data for vitamin C in refractory shock include three studies, of which two are randomized controlled trials, comprising a total of 146 patients, he added.
“I will admit an N of 146 is hardly practice-changing for most people,” Dr. Rattan said. “There’s still a significant and sustained large mortality effect for the use of vitamin C, with nearly no adverse effects.”
Pooled analysis of all three studies revealed a marked reduction in mortality with the use of vitamin C (odds ratio, 0.17, 95% confidence interval 0.07–0.40; P less than .001), according to a meta-analysis recently just published in Critical Care that Dr. Rattan referenced in his presentation (Critical Care 2018;22:258, DOI:10.1186/s13054-018-2191-x).
When taken in recommended dosages, vitamin C given with corticosteroids and thiamine is without known side effects, researcher Paul E. Marik wrote earlier this year in an editorial in Pharmacology & Therapeutics (2018;189[9]:63-70, DOI:10.1016/j.pharmthera.2018.04.007) noted Dr. Rattan, who said he uses the intravenous vitamin C, thiamine, and hydrocortisone protocol previously reported by Dr. Marik and colleagues.
There are 13 ongoing trials, including some prospective blinded, randomized trials, looking at the role of vitamin C in refractory shock, he added.
Angiotensin-II is another intervention that may be promising in refractory septic shock, Dr. Rattan told attendees, pointing to the 2017 publication of the ATHOS-3 trial in the New England Journal of Medicine (2017; 377:419-430,DOI: 10.1056/NEJMoa1704154) showing that treatment increased blood pressure in patients with vasodilatory shock not responding to conventional vasopressors at high doses.
Likewise, methylene blue has shown promise in septic shock, at least in some limited clinical investigations and anecdotally in patients not improving despite standard interventions. “I’ve been able to have a couple patients walk out of the hospital with the use of methylene blue,” Dr. Rattan said. “Again, the plural of ‘anecdote’ is not ‘data,’ but it’s something to consider for the early adopters.”
Dr. Rattan had no disclosures related to his presentation.
BOSTON– treatment that require more investigation, but nevertheless appear promising, Rishi Rattan, MD, said at the annual clinical congress of the American College of Surgeons.
Trials evaluating vitamin C in this setting have demonstrated a large mortality impact with an absence of side effects, according to Dr. Rattan, a trauma and critical care surgeon with the Ryder Trauma Center at the University of Miami.
“It’s something that I have decided to start early adopting, and many of my colleagues at University of Miami do as well,” Dr. Rattan said in a panel session on updates in septic shock. “We’re anecdotally so far at least seeing good results and are going to be excited to see what these ongoing trials show.”
As an antioxidant, vitamin C has anti-inflammatory properties that may possibly attenuate the overly exuberant inflammatory response seen in septic shock, Dr. Rattan said in his presentation.
The limited clinical data for vitamin C in refractory shock include three studies, of which two are randomized controlled trials, comprising a total of 146 patients, he added.
“I will admit an N of 146 is hardly practice-changing for most people,” Dr. Rattan said. “There’s still a significant and sustained large mortality effect for the use of vitamin C, with nearly no adverse effects.”
Pooled analysis of all three studies revealed a marked reduction in mortality with the use of vitamin C (odds ratio, 0.17, 95% confidence interval 0.07–0.40; P less than .001), according to a meta-analysis recently just published in Critical Care that Dr. Rattan referenced in his presentation (Critical Care 2018;22:258, DOI:10.1186/s13054-018-2191-x).
When taken in recommended dosages, vitamin C given with corticosteroids and thiamine is without known side effects, researcher Paul E. Marik wrote earlier this year in an editorial in Pharmacology & Therapeutics (2018;189[9]:63-70, DOI:10.1016/j.pharmthera.2018.04.007) noted Dr. Rattan, who said he uses the intravenous vitamin C, thiamine, and hydrocortisone protocol previously reported by Dr. Marik and colleagues.
There are 13 ongoing trials, including some prospective blinded, randomized trials, looking at the role of vitamin C in refractory shock, he added.
Angiotensin-II is another intervention that may be promising in refractory septic shock, Dr. Rattan told attendees, pointing to the 2017 publication of the ATHOS-3 trial in the New England Journal of Medicine (2017; 377:419-430,DOI: 10.1056/NEJMoa1704154) showing that treatment increased blood pressure in patients with vasodilatory shock not responding to conventional vasopressors at high doses.
Likewise, methylene blue has shown promise in septic shock, at least in some limited clinical investigations and anecdotally in patients not improving despite standard interventions. “I’ve been able to have a couple patients walk out of the hospital with the use of methylene blue,” Dr. Rattan said. “Again, the plural of ‘anecdote’ is not ‘data,’ but it’s something to consider for the early adopters.”
Dr. Rattan had no disclosures related to his presentation.
BOSTON– treatment that require more investigation, but nevertheless appear promising, Rishi Rattan, MD, said at the annual clinical congress of the American College of Surgeons.
Trials evaluating vitamin C in this setting have demonstrated a large mortality impact with an absence of side effects, according to Dr. Rattan, a trauma and critical care surgeon with the Ryder Trauma Center at the University of Miami.
“It’s something that I have decided to start early adopting, and many of my colleagues at University of Miami do as well,” Dr. Rattan said in a panel session on updates in septic shock. “We’re anecdotally so far at least seeing good results and are going to be excited to see what these ongoing trials show.”
As an antioxidant, vitamin C has anti-inflammatory properties that may possibly attenuate the overly exuberant inflammatory response seen in septic shock, Dr. Rattan said in his presentation.
The limited clinical data for vitamin C in refractory shock include three studies, of which two are randomized controlled trials, comprising a total of 146 patients, he added.
“I will admit an N of 146 is hardly practice-changing for most people,” Dr. Rattan said. “There’s still a significant and sustained large mortality effect for the use of vitamin C, with nearly no adverse effects.”
Pooled analysis of all three studies revealed a marked reduction in mortality with the use of vitamin C (odds ratio, 0.17, 95% confidence interval 0.07–0.40; P less than .001), according to a meta-analysis recently just published in Critical Care that Dr. Rattan referenced in his presentation (Critical Care 2018;22:258, DOI:10.1186/s13054-018-2191-x).
When taken in recommended dosages, vitamin C given with corticosteroids and thiamine is without known side effects, researcher Paul E. Marik wrote earlier this year in an editorial in Pharmacology & Therapeutics (2018;189[9]:63-70, DOI:10.1016/j.pharmthera.2018.04.007) noted Dr. Rattan, who said he uses the intravenous vitamin C, thiamine, and hydrocortisone protocol previously reported by Dr. Marik and colleagues.
There are 13 ongoing trials, including some prospective blinded, randomized trials, looking at the role of vitamin C in refractory shock, he added.
Angiotensin-II is another intervention that may be promising in refractory septic shock, Dr. Rattan told attendees, pointing to the 2017 publication of the ATHOS-3 trial in the New England Journal of Medicine (2017; 377:419-430,DOI: 10.1056/NEJMoa1704154) showing that treatment increased blood pressure in patients with vasodilatory shock not responding to conventional vasopressors at high doses.
Likewise, methylene blue has shown promise in septic shock, at least in some limited clinical investigations and anecdotally in patients not improving despite standard interventions. “I’ve been able to have a couple patients walk out of the hospital with the use of methylene blue,” Dr. Rattan said. “Again, the plural of ‘anecdote’ is not ‘data,’ but it’s something to consider for the early adopters.”
Dr. Rattan had no disclosures related to his presentation.
AT THE ACS CLINICAL CONGRESS
Endoscopy-related infections found higher than expected, prophylaxis overused
ATLANTA – The risk of infection from flexible endoscopes is far greater than generally believed, despite the excessive use of prophylactic antimicrobials in patients undergoing endoscopy, recent studies show.
Many gastroenterologists and guidelines from professional organizations use a reference point of “less than one per million” regarding the risk of infection from scopes, but a Johns Hopkins University study of more than 2.3 million patients in 6 states showed that the infection risk with colonoscopy is about 1 per 1,000, the risk for upper gastrointestinal endoscopy is about 3 per 1,000, and the risk with cystoscopy is about 4 per 1,000, Cori Ofstead said at the International Conference on Emerging Infectious Diseases.
“For bronchoscopy [the infection risk] was 15.6 in 1,000, which is 1.6% – not anywhere in the 1 in a million range,” said Ms. Ofstead, president and chief executive officer of Ofstead & Associates, a St. Paul, Minn. health care research firm.
It also turns out that prophylactic antibiotics are frequently given to patients undergoing routine endoscopy procedures, she said, noting that four major associations – two gastroenterology associations and two urology associations in the United States and Europe – recommend that prophylactic antimicrobials be given with routine endoscopies for certain patients undergoing certain types of procedures.
One U.S. organization is recommending prophylactic antimicrobials for every patient undergoing ureteroscopy, she added.
A Cleveland Clinic study looking at the impact of those American Urological Association guidelines for prophylactic antimicrobials showed that in a subset of patients with negative urine cultures before ureteroscopy, 100% received the prophylaxis, and 68% were also given other antimicrobials to take home.
“So the question, of course, is how well does this work...,” Ms. Ofstead said. “They found 3%-4% infection, with the rates exactly the same – no statistically significant differences – between patients who got prophylaxis just in the hospital or who went home with prophylactic meds, and they concluded that there was no benefit to the extra take-home antimicrobials.”
Others studies in multiple countries show either no impact or only minor impact of this prophylaxis on infection rates, and yet all show infection rates after endoscopy that are not one in a million, but in “the percentage point range,” she said.
“As we move toward more of these minimally invasive procedures, we need to be aware that we’re using extremely complex instruments that are very difficult to clean and disinfect or sterilize,” she said, adding that “in the field we’re seeing that improper reprocessing is actually business as usual.”
Infections have been seen with all kinds of scopes, Ms. Ofstead noted.
“The potential for this becoming a bit of a monster is enhanced by the widespread use of prophylactic antimicrobials during endoscopy, and I’m also troubled by the quick reaction of giving people antimicrobials when they have a positive culture from a scope rather than making sure the scope is clean,” she said, explaining that while most scopes have microbes and patients could be getting infections, they also may be reacting to soil and endotoxins in the scope rather than microbes.
“In any case, to reduce risks there are a number of things people can do,” she said. When using reusable scopes, proper cleaning is essential. “I think we should be moving toward scopes that can be disassembled so we can see inside and get those channels clean,” adding that efforts should also be made to move toward single-use scopes.
“Particularly in these outbreak situations where we’re using bronchoscopy on multiple patients, there’s just no excuse for reusing bronchoscopes and not sterilizing them between uses and making darn sure that they’re not full of whatever our outbreak pathogen is,” Ms. Ofstead said. “And lastly, I’m hoping that some folks here can talk some sense into people at the professional associations who are recommending prophylactic antimicrobial use, because if we don’t get some stewardship going, we’re going to be in big trouble.”
The guidelines create a conundrum for doctors who are torn between that stewardship and a failure to follow the recommendations.
“Their professional organization is telling them to give prophylactic antimicrobials. If they don’t do it and a patients gets an infection, that’s a malpractice issue. So we’ve got to go through those associations and get them to stop recommending prophylactic antimicrobials when there is no evidence of their effectiveness,” she said.
Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
SOURCE: Ofstead C., ICEID 2018 Presentation.
ATLANTA – The risk of infection from flexible endoscopes is far greater than generally believed, despite the excessive use of prophylactic antimicrobials in patients undergoing endoscopy, recent studies show.
Many gastroenterologists and guidelines from professional organizations use a reference point of “less than one per million” regarding the risk of infection from scopes, but a Johns Hopkins University study of more than 2.3 million patients in 6 states showed that the infection risk with colonoscopy is about 1 per 1,000, the risk for upper gastrointestinal endoscopy is about 3 per 1,000, and the risk with cystoscopy is about 4 per 1,000, Cori Ofstead said at the International Conference on Emerging Infectious Diseases.
“For bronchoscopy [the infection risk] was 15.6 in 1,000, which is 1.6% – not anywhere in the 1 in a million range,” said Ms. Ofstead, president and chief executive officer of Ofstead & Associates, a St. Paul, Minn. health care research firm.
It also turns out that prophylactic antibiotics are frequently given to patients undergoing routine endoscopy procedures, she said, noting that four major associations – two gastroenterology associations and two urology associations in the United States and Europe – recommend that prophylactic antimicrobials be given with routine endoscopies for certain patients undergoing certain types of procedures.
One U.S. organization is recommending prophylactic antimicrobials for every patient undergoing ureteroscopy, she added.
A Cleveland Clinic study looking at the impact of those American Urological Association guidelines for prophylactic antimicrobials showed that in a subset of patients with negative urine cultures before ureteroscopy, 100% received the prophylaxis, and 68% were also given other antimicrobials to take home.
“So the question, of course, is how well does this work...,” Ms. Ofstead said. “They found 3%-4% infection, with the rates exactly the same – no statistically significant differences – between patients who got prophylaxis just in the hospital or who went home with prophylactic meds, and they concluded that there was no benefit to the extra take-home antimicrobials.”
Others studies in multiple countries show either no impact or only minor impact of this prophylaxis on infection rates, and yet all show infection rates after endoscopy that are not one in a million, but in “the percentage point range,” she said.
“As we move toward more of these minimally invasive procedures, we need to be aware that we’re using extremely complex instruments that are very difficult to clean and disinfect or sterilize,” she said, adding that “in the field we’re seeing that improper reprocessing is actually business as usual.”
Infections have been seen with all kinds of scopes, Ms. Ofstead noted.
“The potential for this becoming a bit of a monster is enhanced by the widespread use of prophylactic antimicrobials during endoscopy, and I’m also troubled by the quick reaction of giving people antimicrobials when they have a positive culture from a scope rather than making sure the scope is clean,” she said, explaining that while most scopes have microbes and patients could be getting infections, they also may be reacting to soil and endotoxins in the scope rather than microbes.
“In any case, to reduce risks there are a number of things people can do,” she said. When using reusable scopes, proper cleaning is essential. “I think we should be moving toward scopes that can be disassembled so we can see inside and get those channels clean,” adding that efforts should also be made to move toward single-use scopes.
“Particularly in these outbreak situations where we’re using bronchoscopy on multiple patients, there’s just no excuse for reusing bronchoscopes and not sterilizing them between uses and making darn sure that they’re not full of whatever our outbreak pathogen is,” Ms. Ofstead said. “And lastly, I’m hoping that some folks here can talk some sense into people at the professional associations who are recommending prophylactic antimicrobial use, because if we don’t get some stewardship going, we’re going to be in big trouble.”
The guidelines create a conundrum for doctors who are torn between that stewardship and a failure to follow the recommendations.
“Their professional organization is telling them to give prophylactic antimicrobials. If they don’t do it and a patients gets an infection, that’s a malpractice issue. So we’ve got to go through those associations and get them to stop recommending prophylactic antimicrobials when there is no evidence of their effectiveness,” she said.
Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
SOURCE: Ofstead C., ICEID 2018 Presentation.
ATLANTA – The risk of infection from flexible endoscopes is far greater than generally believed, despite the excessive use of prophylactic antimicrobials in patients undergoing endoscopy, recent studies show.
Many gastroenterologists and guidelines from professional organizations use a reference point of “less than one per million” regarding the risk of infection from scopes, but a Johns Hopkins University study of more than 2.3 million patients in 6 states showed that the infection risk with colonoscopy is about 1 per 1,000, the risk for upper gastrointestinal endoscopy is about 3 per 1,000, and the risk with cystoscopy is about 4 per 1,000, Cori Ofstead said at the International Conference on Emerging Infectious Diseases.
“For bronchoscopy [the infection risk] was 15.6 in 1,000, which is 1.6% – not anywhere in the 1 in a million range,” said Ms. Ofstead, president and chief executive officer of Ofstead & Associates, a St. Paul, Minn. health care research firm.
It also turns out that prophylactic antibiotics are frequently given to patients undergoing routine endoscopy procedures, she said, noting that four major associations – two gastroenterology associations and two urology associations in the United States and Europe – recommend that prophylactic antimicrobials be given with routine endoscopies for certain patients undergoing certain types of procedures.
One U.S. organization is recommending prophylactic antimicrobials for every patient undergoing ureteroscopy, she added.
A Cleveland Clinic study looking at the impact of those American Urological Association guidelines for prophylactic antimicrobials showed that in a subset of patients with negative urine cultures before ureteroscopy, 100% received the prophylaxis, and 68% were also given other antimicrobials to take home.
“So the question, of course, is how well does this work...,” Ms. Ofstead said. “They found 3%-4% infection, with the rates exactly the same – no statistically significant differences – between patients who got prophylaxis just in the hospital or who went home with prophylactic meds, and they concluded that there was no benefit to the extra take-home antimicrobials.”
Others studies in multiple countries show either no impact or only minor impact of this prophylaxis on infection rates, and yet all show infection rates after endoscopy that are not one in a million, but in “the percentage point range,” she said.
“As we move toward more of these minimally invasive procedures, we need to be aware that we’re using extremely complex instruments that are very difficult to clean and disinfect or sterilize,” she said, adding that “in the field we’re seeing that improper reprocessing is actually business as usual.”
Infections have been seen with all kinds of scopes, Ms. Ofstead noted.
“The potential for this becoming a bit of a monster is enhanced by the widespread use of prophylactic antimicrobials during endoscopy, and I’m also troubled by the quick reaction of giving people antimicrobials when they have a positive culture from a scope rather than making sure the scope is clean,” she said, explaining that while most scopes have microbes and patients could be getting infections, they also may be reacting to soil and endotoxins in the scope rather than microbes.
“In any case, to reduce risks there are a number of things people can do,” she said. When using reusable scopes, proper cleaning is essential. “I think we should be moving toward scopes that can be disassembled so we can see inside and get those channels clean,” adding that efforts should also be made to move toward single-use scopes.
“Particularly in these outbreak situations where we’re using bronchoscopy on multiple patients, there’s just no excuse for reusing bronchoscopes and not sterilizing them between uses and making darn sure that they’re not full of whatever our outbreak pathogen is,” Ms. Ofstead said. “And lastly, I’m hoping that some folks here can talk some sense into people at the professional associations who are recommending prophylactic antimicrobial use, because if we don’t get some stewardship going, we’re going to be in big trouble.”
The guidelines create a conundrum for doctors who are torn between that stewardship and a failure to follow the recommendations.
“Their professional organization is telling them to give prophylactic antimicrobials. If they don’t do it and a patients gets an infection, that’s a malpractice issue. So we’ve got to go through those associations and get them to stop recommending prophylactic antimicrobials when there is no evidence of their effectiveness,” she said.
Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
SOURCE: Ofstead C., ICEID 2018 Presentation.
REPORTING FROM ICEID 2018
Key clinical point:
Major finding: Infection risk is about 1 per 1,000 with colonoscopy; 3 per 1,000 with upper gastrointestinal endoscopy; and 4 per 1,000 with cystoscopy.
Study details: Endoscopic procedures performed at ASCs in 2014 all-payer claims data from 6 U.S. states.
Disclosures: Ms. Ofstead has been a consultant for 3M Company, Ambu, Auris, Boston Scientific, Cogentix, Convergascent, Healthmark, Invendo Medical, Nanosonics, and Advanced Sterilization Products, and has received grant/research support from 3M Company, Advanced Sterilization Products, Ambu, Boston Scientific, Cogentix, Healthmark, Invendo Medical, Medivators, and Steris.
Source: Ofstead C et al. ICEID 2018 Presentation.
EHR-guided strategy reduces postop VTE events
BOSTON – Avoiding could result in a reduction in VTE rates, a speaker said at the annual clinical congress of the American College of Surgeons.
The VTE rate dropped by about one-quarter in the trauma care pathway at the University of Pittsburgh Medical Center (UPMC) after implementation of algorithms to risk-stratify patients and guide nursing staff, said Matthew D. Neal, MD, FACS, the Roberta G. Simmons Assistant Professor of Surgery at the University of Pittsburgh.
By incorporating algorithms into the electronic health record (EHR), UPMC was able to realize a “dramatic” 72% reduction in missed doses, from 4,331 missed doses in 2014 to 1,193 in 2015, Dr. Neal told attendees in a session focused on hot topics in surgical patient safety.
That decrease in missed doses has translated into a decreased rate of VTE, from an already relatively low rate of 1.5% in 2015, to 1.1% in 2017, representing a 26.7% reduction, according to data Dr. Neal shared in his podium presentation.
“This has been a sustainable event for us, largely linked to the implementation of an EHR-guided risk assessment pathway to guide the implementation of VTE prophylaxis,” he said.
The change was safe, he added, noting that, since utilization of this pathway, there have been no significant increases in the rate of bleeding events among patients who have mandatory orders.
These results corroborate those of some previous investigations, including one key study from the Johns Hopkins Hospital that described the adoption of a mandatory computerized clinical decision support tool to improve adherence to best practices for VTE prophylaxis.
After incorporation of the tool in the computerized order entry system, there was a significant increase in VTE prophylaxis, translating into a significant drop in preventable harm from VTE, from 1.0% to 0.17% (P = .04), investigators reported in JAMA Surgery.
Reducing missed doses is one of the major contributing factors to decreased VTE rates, according to Dr. Neal.
Missed doses of enoxaparin correlate with increased incidence of deep vein thrombosis (DVT) in trauma and general surgery patients, according to results of one prospective study Dr. Neal described. In that study of 202 patients, reported in JAMA Surgery, DVTs were seen in 23.5% of patients with missed doses, compared with 4.8 for patients with no missed doses (P < .01).
“We need to understand how to risk assess and how to utilize our EHR as a tool,” Dr. Neal told attendees.
Dr. Neal reported disclosures related to Janssen Pharmaceuticals, CSL Behring, Accriva Diagnostics, and Haemonetics, as well as a U.S. patent for a treatment of infectious and inflammatory disorders, and laboratory funding from the National Institutes of Health, Department of Defense, and the Biomedical Advanced Research and Development Authority.
SOURCE: Neal MD. Presentation at the American College of Surgeons Clinical Congress. 2018 Oct 25.
BOSTON – Avoiding could result in a reduction in VTE rates, a speaker said at the annual clinical congress of the American College of Surgeons.
The VTE rate dropped by about one-quarter in the trauma care pathway at the University of Pittsburgh Medical Center (UPMC) after implementation of algorithms to risk-stratify patients and guide nursing staff, said Matthew D. Neal, MD, FACS, the Roberta G. Simmons Assistant Professor of Surgery at the University of Pittsburgh.
By incorporating algorithms into the electronic health record (EHR), UPMC was able to realize a “dramatic” 72% reduction in missed doses, from 4,331 missed doses in 2014 to 1,193 in 2015, Dr. Neal told attendees in a session focused on hot topics in surgical patient safety.
That decrease in missed doses has translated into a decreased rate of VTE, from an already relatively low rate of 1.5% in 2015, to 1.1% in 2017, representing a 26.7% reduction, according to data Dr. Neal shared in his podium presentation.
“This has been a sustainable event for us, largely linked to the implementation of an EHR-guided risk assessment pathway to guide the implementation of VTE prophylaxis,” he said.
The change was safe, he added, noting that, since utilization of this pathway, there have been no significant increases in the rate of bleeding events among patients who have mandatory orders.
These results corroborate those of some previous investigations, including one key study from the Johns Hopkins Hospital that described the adoption of a mandatory computerized clinical decision support tool to improve adherence to best practices for VTE prophylaxis.
After incorporation of the tool in the computerized order entry system, there was a significant increase in VTE prophylaxis, translating into a significant drop in preventable harm from VTE, from 1.0% to 0.17% (P = .04), investigators reported in JAMA Surgery.
Reducing missed doses is one of the major contributing factors to decreased VTE rates, according to Dr. Neal.
Missed doses of enoxaparin correlate with increased incidence of deep vein thrombosis (DVT) in trauma and general surgery patients, according to results of one prospective study Dr. Neal described. In that study of 202 patients, reported in JAMA Surgery, DVTs were seen in 23.5% of patients with missed doses, compared with 4.8 for patients with no missed doses (P < .01).
“We need to understand how to risk assess and how to utilize our EHR as a tool,” Dr. Neal told attendees.
Dr. Neal reported disclosures related to Janssen Pharmaceuticals, CSL Behring, Accriva Diagnostics, and Haemonetics, as well as a U.S. patent for a treatment of infectious and inflammatory disorders, and laboratory funding from the National Institutes of Health, Department of Defense, and the Biomedical Advanced Research and Development Authority.
SOURCE: Neal MD. Presentation at the American College of Surgeons Clinical Congress. 2018 Oct 25.
BOSTON – Avoiding could result in a reduction in VTE rates, a speaker said at the annual clinical congress of the American College of Surgeons.
The VTE rate dropped by about one-quarter in the trauma care pathway at the University of Pittsburgh Medical Center (UPMC) after implementation of algorithms to risk-stratify patients and guide nursing staff, said Matthew D. Neal, MD, FACS, the Roberta G. Simmons Assistant Professor of Surgery at the University of Pittsburgh.
By incorporating algorithms into the electronic health record (EHR), UPMC was able to realize a “dramatic” 72% reduction in missed doses, from 4,331 missed doses in 2014 to 1,193 in 2015, Dr. Neal told attendees in a session focused on hot topics in surgical patient safety.
That decrease in missed doses has translated into a decreased rate of VTE, from an already relatively low rate of 1.5% in 2015, to 1.1% in 2017, representing a 26.7% reduction, according to data Dr. Neal shared in his podium presentation.
“This has been a sustainable event for us, largely linked to the implementation of an EHR-guided risk assessment pathway to guide the implementation of VTE prophylaxis,” he said.
The change was safe, he added, noting that, since utilization of this pathway, there have been no significant increases in the rate of bleeding events among patients who have mandatory orders.
These results corroborate those of some previous investigations, including one key study from the Johns Hopkins Hospital that described the adoption of a mandatory computerized clinical decision support tool to improve adherence to best practices for VTE prophylaxis.
After incorporation of the tool in the computerized order entry system, there was a significant increase in VTE prophylaxis, translating into a significant drop in preventable harm from VTE, from 1.0% to 0.17% (P = .04), investigators reported in JAMA Surgery.
Reducing missed doses is one of the major contributing factors to decreased VTE rates, according to Dr. Neal.
Missed doses of enoxaparin correlate with increased incidence of deep vein thrombosis (DVT) in trauma and general surgery patients, according to results of one prospective study Dr. Neal described. In that study of 202 patients, reported in JAMA Surgery, DVTs were seen in 23.5% of patients with missed doses, compared with 4.8 for patients with no missed doses (P < .01).
“We need to understand how to risk assess and how to utilize our EHR as a tool,” Dr. Neal told attendees.
Dr. Neal reported disclosures related to Janssen Pharmaceuticals, CSL Behring, Accriva Diagnostics, and Haemonetics, as well as a U.S. patent for a treatment of infectious and inflammatory disorders, and laboratory funding from the National Institutes of Health, Department of Defense, and the Biomedical Advanced Research and Development Authority.
SOURCE: Neal MD. Presentation at the American College of Surgeons Clinical Congress. 2018 Oct 25.
AT THE ACS CLINICAL CONGRESS
Post-mastectomy pain strategy allows for safe, same-day discharge
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: Of 72 women who had same-day discharge after mastectomy, only 3 presented for pain in the 30-day postoperative period.
Study details: A retrospective review of 72 consecutive mastectomies performed at a single surgical center.
Disclosures: The lead author had no disclosures related to the presentation.
Source: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
Acute kidney injury linked to later dementia
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
REPORTING FROM KIDNEY WEEK 2018
Key clinical point: Patients with acute kidney injury seem to face a much higher risk of dementia.
Major finding: Hospitalized patients with AKI were 3.4 times more likely to develop dementia within a median of 6 years, compared with other hospitalized patients.
Study details: A retrospective study of 2,082 propensity-matched hospitalized patients, 1,041 who had AKI and fully recovered, and 1,041 who did not have AKI.
Disclosures: The National Heart, Lung, and Blood Institute funded the study. The authors had no disclosures.
Source: Kendrick JB et al. Kidney Week 2018. Abstract No. TH-OR116.
Challenging Dogma: The banana bag
Necessary, or just another pretty fluid?
The dogma
Patients with alcohol use disorders (AUD) are at risk for nutritional and vitamin deficiencies and may suffer from linked disease states, including Wernicke’s encephalopathy. These conditions may be underrecognized; for instance, an autopsy study suggests that Wernicke’s encephalopathy may have a prevalence rate of 12.5% among alcoholics.1
When patients with AUD are hospitalized, they have often already received a standard IV solution (100 mg of thiamine, 1 mg of folate, 1-2 g of magnesium, and a multivitamin dissolved in saline or dextrose). The practice is common enough that the solution is informally referred to as a “banana bag,” due to the yellow hue imparted by thiamine and multivitamin. These fluids might then be readministered daily during the inpatient stay. But what is the evidence supporting this widespread practice?
The evidence
While the banana bag (or “rally pack”, as it’s also colloquially known) hanging at the patient’s side may look cool, it may not be helping her. Let’s break down the ingredients:
- Folate: Patients with alcohol use disorder are at higher risk for folate deficiency (attributable to poor intake and decreased absorption), but overall rates of folate deficiency are still quite low.2 In addition, most oral and parenteral multivitamins already contain at least 400 mcg folate – the benefit of adding further intravenous folate is not clear.
- Magnesium. Patients with AUD are also at higher risk for magnesium deficiency attributable to increased excretion. While decreased magnesium levels could theoretically increase the risk of alcohol withdrawal symptoms, a Cochrane review found no evidence to support routine supplementation.3
- Multivitamin. Despite theoretical advantages in these (often) malnourished patients, there are no published studies on the benefit or harm of administering a “pan-vitamin” injection. The standard IV formulation is slightly different than an oral vitamin (the IV contains vitamin K, for instance, and lacks calcium), but the bioavailability should be roughly the same, except in rare patients with intestinal malabsorption.4
- IV fluids. Pharmacies typically mix these ingredients in a liter of normal saline or 5% dextrose. Once again, though, individual patients will have different needs. A dehydrated patient would benefit more from normal saline, a patient with alcoholic ketoacidosis would benefit more from dextrose, and a patient with alcohol-related cardiomyopathy likely shouldn’t be getting large volume IV fluids at all.
- Thiamine. Thiamine deficiency is likely the most common and most concerning vitamin deficiency in this patient population. The typical banana bag contains 100 mg of thiamine, which has been the traditional recommended daily amount for Wernicke’s treatment. This dosage, however, was apparently chosen arbitrarily in the 1950s (based on what the authors considered to be a high dose) and current recommendations suggest higher doses given more frequently because of the relatively short half-life of parenteral thiamine.5
Takeaway
The banana bag is a “one-size-fits-all” approach that offers too much of some of its ingredients and not enough of others. It’s better to individualize treatment based on a patient’s needs and consider high-dose thiamine (500 mg one to three times daily) for those at risk for, or showing signs of, Wernicke’s encephalopathy.
Dr. Sehgal and Dr. Hanson are clinical associate professors of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. Dr. Sehgal (@rtsehgal) is a member of the editorial advisory board for The Hospitalist.
References
1. Torvik A et al. Brain lesions in alcoholics: a neuropathological study with clinical correlation. J Neurol Sci. 1982 Nov;56(2-3):233-48.
2. Schwab RA et al. Prevalence in folate deficiency in emergency department patients with alcohol-related illness or injury. Am J Emerg Med. 1992 May;10(3):203-7.
3. Sarai M et al. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358.
4. Krishel S et al. Intravenous vitamins for alcoholics in the emergency department: a review. J Emerg Med. 1998 May-Jun;16(3):419-24.
5. Donnino MW et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6): 715-21.
Necessary, or just another pretty fluid?
Necessary, or just another pretty fluid?
The dogma
Patients with alcohol use disorders (AUD) are at risk for nutritional and vitamin deficiencies and may suffer from linked disease states, including Wernicke’s encephalopathy. These conditions may be underrecognized; for instance, an autopsy study suggests that Wernicke’s encephalopathy may have a prevalence rate of 12.5% among alcoholics.1
When patients with AUD are hospitalized, they have often already received a standard IV solution (100 mg of thiamine, 1 mg of folate, 1-2 g of magnesium, and a multivitamin dissolved in saline or dextrose). The practice is common enough that the solution is informally referred to as a “banana bag,” due to the yellow hue imparted by thiamine and multivitamin. These fluids might then be readministered daily during the inpatient stay. But what is the evidence supporting this widespread practice?
The evidence
While the banana bag (or “rally pack”, as it’s also colloquially known) hanging at the patient’s side may look cool, it may not be helping her. Let’s break down the ingredients:
- Folate: Patients with alcohol use disorder are at higher risk for folate deficiency (attributable to poor intake and decreased absorption), but overall rates of folate deficiency are still quite low.2 In addition, most oral and parenteral multivitamins already contain at least 400 mcg folate – the benefit of adding further intravenous folate is not clear.
- Magnesium. Patients with AUD are also at higher risk for magnesium deficiency attributable to increased excretion. While decreased magnesium levels could theoretically increase the risk of alcohol withdrawal symptoms, a Cochrane review found no evidence to support routine supplementation.3
- Multivitamin. Despite theoretical advantages in these (often) malnourished patients, there are no published studies on the benefit or harm of administering a “pan-vitamin” injection. The standard IV formulation is slightly different than an oral vitamin (the IV contains vitamin K, for instance, and lacks calcium), but the bioavailability should be roughly the same, except in rare patients with intestinal malabsorption.4
- IV fluids. Pharmacies typically mix these ingredients in a liter of normal saline or 5% dextrose. Once again, though, individual patients will have different needs. A dehydrated patient would benefit more from normal saline, a patient with alcoholic ketoacidosis would benefit more from dextrose, and a patient with alcohol-related cardiomyopathy likely shouldn’t be getting large volume IV fluids at all.
- Thiamine. Thiamine deficiency is likely the most common and most concerning vitamin deficiency in this patient population. The typical banana bag contains 100 mg of thiamine, which has been the traditional recommended daily amount for Wernicke’s treatment. This dosage, however, was apparently chosen arbitrarily in the 1950s (based on what the authors considered to be a high dose) and current recommendations suggest higher doses given more frequently because of the relatively short half-life of parenteral thiamine.5
Takeaway
The banana bag is a “one-size-fits-all” approach that offers too much of some of its ingredients and not enough of others. It’s better to individualize treatment based on a patient’s needs and consider high-dose thiamine (500 mg one to three times daily) for those at risk for, or showing signs of, Wernicke’s encephalopathy.
Dr. Sehgal and Dr. Hanson are clinical associate professors of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. Dr. Sehgal (@rtsehgal) is a member of the editorial advisory board for The Hospitalist.
References
1. Torvik A et al. Brain lesions in alcoholics: a neuropathological study with clinical correlation. J Neurol Sci. 1982 Nov;56(2-3):233-48.
2. Schwab RA et al. Prevalence in folate deficiency in emergency department patients with alcohol-related illness or injury. Am J Emerg Med. 1992 May;10(3):203-7.
3. Sarai M et al. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358.
4. Krishel S et al. Intravenous vitamins for alcoholics in the emergency department: a review. J Emerg Med. 1998 May-Jun;16(3):419-24.
5. Donnino MW et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6): 715-21.
The dogma
Patients with alcohol use disorders (AUD) are at risk for nutritional and vitamin deficiencies and may suffer from linked disease states, including Wernicke’s encephalopathy. These conditions may be underrecognized; for instance, an autopsy study suggests that Wernicke’s encephalopathy may have a prevalence rate of 12.5% among alcoholics.1
When patients with AUD are hospitalized, they have often already received a standard IV solution (100 mg of thiamine, 1 mg of folate, 1-2 g of magnesium, and a multivitamin dissolved in saline or dextrose). The practice is common enough that the solution is informally referred to as a “banana bag,” due to the yellow hue imparted by thiamine and multivitamin. These fluids might then be readministered daily during the inpatient stay. But what is the evidence supporting this widespread practice?
The evidence
While the banana bag (or “rally pack”, as it’s also colloquially known) hanging at the patient’s side may look cool, it may not be helping her. Let’s break down the ingredients:
- Folate: Patients with alcohol use disorder are at higher risk for folate deficiency (attributable to poor intake and decreased absorption), but overall rates of folate deficiency are still quite low.2 In addition, most oral and parenteral multivitamins already contain at least 400 mcg folate – the benefit of adding further intravenous folate is not clear.
- Magnesium. Patients with AUD are also at higher risk for magnesium deficiency attributable to increased excretion. While decreased magnesium levels could theoretically increase the risk of alcohol withdrawal symptoms, a Cochrane review found no evidence to support routine supplementation.3
- Multivitamin. Despite theoretical advantages in these (often) malnourished patients, there are no published studies on the benefit or harm of administering a “pan-vitamin” injection. The standard IV formulation is slightly different than an oral vitamin (the IV contains vitamin K, for instance, and lacks calcium), but the bioavailability should be roughly the same, except in rare patients with intestinal malabsorption.4
- IV fluids. Pharmacies typically mix these ingredients in a liter of normal saline or 5% dextrose. Once again, though, individual patients will have different needs. A dehydrated patient would benefit more from normal saline, a patient with alcoholic ketoacidosis would benefit more from dextrose, and a patient with alcohol-related cardiomyopathy likely shouldn’t be getting large volume IV fluids at all.
- Thiamine. Thiamine deficiency is likely the most common and most concerning vitamin deficiency in this patient population. The typical banana bag contains 100 mg of thiamine, which has been the traditional recommended daily amount for Wernicke’s treatment. This dosage, however, was apparently chosen arbitrarily in the 1950s (based on what the authors considered to be a high dose) and current recommendations suggest higher doses given more frequently because of the relatively short half-life of parenteral thiamine.5
Takeaway
The banana bag is a “one-size-fits-all” approach that offers too much of some of its ingredients and not enough of others. It’s better to individualize treatment based on a patient’s needs and consider high-dose thiamine (500 mg one to three times daily) for those at risk for, or showing signs of, Wernicke’s encephalopathy.
Dr. Sehgal and Dr. Hanson are clinical associate professors of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. Dr. Sehgal (@rtsehgal) is a member of the editorial advisory board for The Hospitalist.
References
1. Torvik A et al. Brain lesions in alcoholics: a neuropathological study with clinical correlation. J Neurol Sci. 1982 Nov;56(2-3):233-48.
2. Schwab RA et al. Prevalence in folate deficiency in emergency department patients with alcohol-related illness or injury. Am J Emerg Med. 1992 May;10(3):203-7.
3. Sarai M et al. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358.
4. Krishel S et al. Intravenous vitamins for alcoholics in the emergency department: a review. J Emerg Med. 1998 May-Jun;16(3):419-24.
5. Donnino MW et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6): 715-21.
Antipsychotic drugs failed to shorten ICU delirium
The antipsychotic medications in patients in intensive care, new research has found.
In a paper published in the New England Journal of Medicine, researchers reported the results of a randomized, double-blind, placebo-controlled trial in 566 patients with acute respiratory failure or shock and hypoactive or hyperactive delirium. Participants were randomized either to a maximum of 20 mg IV haloperidol daily, maximum 40 mg ziprasidone daily, or placebo.
At the end of the 14-day intervention period, the placebo group had a median of 8.5 days alive without delirium or coma, the haloperidol group had a median of 7.9 days, and the ziprasidone group had a median of 8.7 days. The difference between groups was not statistically significant.
There were also no significant differences between the three groups in the secondary end point of duration of delirium and coma, 30-day and 90-day survival, time to freedom from mechanical ventilation, ICU discharge, ICU readmission, or hospital discharge.
Timothy D. Girard, MD, from the department of critical care at the University of Pittsburgh, and his coauthors wrote that their findings echoed those of two previous placebo-controlled trials in smaller numbers of ICU patients.
“One possible reason that we found no evidence that the use of haloperidol or ziprasidone resulted in a fewer days with delirium or coma than placebo is that the mechanism of brain dysfunction that is considered to be targeted by antipsychotic medications – increased dopamine signaling – may not play a major role in the pathogenesis of delirium during critical illness,” they wrote.
“In the current trial, approximately 90% of the patients received one or more doses of sedatives or analgesics, and the doses of sedatives and offtrial antipsychotic medications and the durations of exposures to those agents were similar in all trial groups,” the authors added.
Most of the patients in the trial had hypotensive delirium, which made it difficult to assess the effects of antipsychotics on hypertensive delirium.
The authors also commented that the patients enrolled were a mixed group, so their findings did not rule out the possibility that certain subgroups of patients – such as nonintubated patients with hyperactive delirium, those with alcohol withdrawal, or with other delirium phenotypes – may still benefit from antipsychotics.
Patients treated with ziprasidone were more likely to experience prolongation of the corrected QT interval. Two patients in the haloperidol group developed torsades de pointes but neither had received haloperidol in the 4 days preceding the onset of the arrhythmia.
One patient in each group – including the placebo group – experienced extrapyramidal symptoms and had treatment withheld. One patient in the haloperidol group also had the trial drug withheld because of suspected neuroleptic malignant syndrome, but this was later ruled out, and one patient had haloperidol withheld because of dystonia.
The dose of haloperidol used in the study was considered high, the authors said, but they left open the possibility that even higher doses might help. However, they also noted that doses of 25 mg and above were known to have adverse effects on cognition, which is why they chose the 20-mg dosage.
The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors declared support from the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
SOURCE: Girard TD et al. N Engl J Med.2018 Oct 22. doi: 10.1056/NEJMoa1808217.
In a comment published with this study, Thomas P. Bleck, MD, of the department of neurologic sciences at Rush Medical College, Chicago, wrote, “A change in mental status in a patient in intensive care can be one of the most vexing problems. In the past 2 decades, the idea has arisen that antipsychotic drugs – and particularly dopamine antagonists, which ameliorate thought disorders in psychotic patients – could help patients with disordered thinking in other contexts, such as the intensive care unit. However, yet another trial has now called this idea into question.”
He noted that, in the study group, a bolus of placebo was just as effective as a bolus of active medication, which may be because of the majority of patients having hypoactive delirium, which the active drugs may not impact.
“I would still consider using dopamine agonists in patients at imminent risk of injurious behaviors but have less confidence in their benefits than I once had,” Dr. Bleck wrote.
Dr. Bleck did not report any conflicts of interest.
In a comment published with this study, Thomas P. Bleck, MD, of the department of neurologic sciences at Rush Medical College, Chicago, wrote, “A change in mental status in a patient in intensive care can be one of the most vexing problems. In the past 2 decades, the idea has arisen that antipsychotic drugs – and particularly dopamine antagonists, which ameliorate thought disorders in psychotic patients – could help patients with disordered thinking in other contexts, such as the intensive care unit. However, yet another trial has now called this idea into question.”
He noted that, in the study group, a bolus of placebo was just as effective as a bolus of active medication, which may be because of the majority of patients having hypoactive delirium, which the active drugs may not impact.
“I would still consider using dopamine agonists in patients at imminent risk of injurious behaviors but have less confidence in their benefits than I once had,” Dr. Bleck wrote.
Dr. Bleck did not report any conflicts of interest.
In a comment published with this study, Thomas P. Bleck, MD, of the department of neurologic sciences at Rush Medical College, Chicago, wrote, “A change in mental status in a patient in intensive care can be one of the most vexing problems. In the past 2 decades, the idea has arisen that antipsychotic drugs – and particularly dopamine antagonists, which ameliorate thought disorders in psychotic patients – could help patients with disordered thinking in other contexts, such as the intensive care unit. However, yet another trial has now called this idea into question.”
He noted that, in the study group, a bolus of placebo was just as effective as a bolus of active medication, which may be because of the majority of patients having hypoactive delirium, which the active drugs may not impact.
“I would still consider using dopamine agonists in patients at imminent risk of injurious behaviors but have less confidence in their benefits than I once had,” Dr. Bleck wrote.
Dr. Bleck did not report any conflicts of interest.
The antipsychotic medications in patients in intensive care, new research has found.
In a paper published in the New England Journal of Medicine, researchers reported the results of a randomized, double-blind, placebo-controlled trial in 566 patients with acute respiratory failure or shock and hypoactive or hyperactive delirium. Participants were randomized either to a maximum of 20 mg IV haloperidol daily, maximum 40 mg ziprasidone daily, or placebo.
At the end of the 14-day intervention period, the placebo group had a median of 8.5 days alive without delirium or coma, the haloperidol group had a median of 7.9 days, and the ziprasidone group had a median of 8.7 days. The difference between groups was not statistically significant.
There were also no significant differences between the three groups in the secondary end point of duration of delirium and coma, 30-day and 90-day survival, time to freedom from mechanical ventilation, ICU discharge, ICU readmission, or hospital discharge.
Timothy D. Girard, MD, from the department of critical care at the University of Pittsburgh, and his coauthors wrote that their findings echoed those of two previous placebo-controlled trials in smaller numbers of ICU patients.
“One possible reason that we found no evidence that the use of haloperidol or ziprasidone resulted in a fewer days with delirium or coma than placebo is that the mechanism of brain dysfunction that is considered to be targeted by antipsychotic medications – increased dopamine signaling – may not play a major role in the pathogenesis of delirium during critical illness,” they wrote.
“In the current trial, approximately 90% of the patients received one or more doses of sedatives or analgesics, and the doses of sedatives and offtrial antipsychotic medications and the durations of exposures to those agents were similar in all trial groups,” the authors added.
Most of the patients in the trial had hypotensive delirium, which made it difficult to assess the effects of antipsychotics on hypertensive delirium.
The authors also commented that the patients enrolled were a mixed group, so their findings did not rule out the possibility that certain subgroups of patients – such as nonintubated patients with hyperactive delirium, those with alcohol withdrawal, or with other delirium phenotypes – may still benefit from antipsychotics.
Patients treated with ziprasidone were more likely to experience prolongation of the corrected QT interval. Two patients in the haloperidol group developed torsades de pointes but neither had received haloperidol in the 4 days preceding the onset of the arrhythmia.
One patient in each group – including the placebo group – experienced extrapyramidal symptoms and had treatment withheld. One patient in the haloperidol group also had the trial drug withheld because of suspected neuroleptic malignant syndrome, but this was later ruled out, and one patient had haloperidol withheld because of dystonia.
The dose of haloperidol used in the study was considered high, the authors said, but they left open the possibility that even higher doses might help. However, they also noted that doses of 25 mg and above were known to have adverse effects on cognition, which is why they chose the 20-mg dosage.
The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors declared support from the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
SOURCE: Girard TD et al. N Engl J Med.2018 Oct 22. doi: 10.1056/NEJMoa1808217.
The antipsychotic medications in patients in intensive care, new research has found.
In a paper published in the New England Journal of Medicine, researchers reported the results of a randomized, double-blind, placebo-controlled trial in 566 patients with acute respiratory failure or shock and hypoactive or hyperactive delirium. Participants were randomized either to a maximum of 20 mg IV haloperidol daily, maximum 40 mg ziprasidone daily, or placebo.
At the end of the 14-day intervention period, the placebo group had a median of 8.5 days alive without delirium or coma, the haloperidol group had a median of 7.9 days, and the ziprasidone group had a median of 8.7 days. The difference between groups was not statistically significant.
There were also no significant differences between the three groups in the secondary end point of duration of delirium and coma, 30-day and 90-day survival, time to freedom from mechanical ventilation, ICU discharge, ICU readmission, or hospital discharge.
Timothy D. Girard, MD, from the department of critical care at the University of Pittsburgh, and his coauthors wrote that their findings echoed those of two previous placebo-controlled trials in smaller numbers of ICU patients.
“One possible reason that we found no evidence that the use of haloperidol or ziprasidone resulted in a fewer days with delirium or coma than placebo is that the mechanism of brain dysfunction that is considered to be targeted by antipsychotic medications – increased dopamine signaling – may not play a major role in the pathogenesis of delirium during critical illness,” they wrote.
“In the current trial, approximately 90% of the patients received one or more doses of sedatives or analgesics, and the doses of sedatives and offtrial antipsychotic medications and the durations of exposures to those agents were similar in all trial groups,” the authors added.
Most of the patients in the trial had hypotensive delirium, which made it difficult to assess the effects of antipsychotics on hypertensive delirium.
The authors also commented that the patients enrolled were a mixed group, so their findings did not rule out the possibility that certain subgroups of patients – such as nonintubated patients with hyperactive delirium, those with alcohol withdrawal, or with other delirium phenotypes – may still benefit from antipsychotics.
Patients treated with ziprasidone were more likely to experience prolongation of the corrected QT interval. Two patients in the haloperidol group developed torsades de pointes but neither had received haloperidol in the 4 days preceding the onset of the arrhythmia.
One patient in each group – including the placebo group – experienced extrapyramidal symptoms and had treatment withheld. One patient in the haloperidol group also had the trial drug withheld because of suspected neuroleptic malignant syndrome, but this was later ruled out, and one patient had haloperidol withheld because of dystonia.
The dose of haloperidol used in the study was considered high, the authors said, but they left open the possibility that even higher doses might help. However, they also noted that doses of 25 mg and above were known to have adverse effects on cognition, which is why they chose the 20-mg dosage.
The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors declared support from the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
SOURCE: Girard TD et al. N Engl J Med.2018 Oct 22. doi: 10.1056/NEJMoa1808217.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Antipsychotics do not reduce the duration or incidence of delirium in intensive care.
Major finding: Patients treated with antipsychotics showed similar median days without delirium or coma, compared with those treated with placebo.
Study details: A randomized, double-blind, placebo-controlled trial in 566 intensive care patients.
Disclosures: The study was supported by the National Institutes of Health and the Department of Veterans Affairs Geriatric Research Education and Clinical Center. Most authors were supported by the NIH or VA during the course of the study. Four authors also reported fees and grants from private industry outside the context of the study.
Source: Girard TD et al. N Engl J Med. 2018 Oct 22. doi: 10.1056/NEJMoa1808217.