User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Replacing warfarin with a NOAC in patients on chronic anticoagulation therapy
Hospitalists must consider clinical factors and patient preferences
Case
A 70-year old woman with hypertension, diabetes, nonischemic stroke, moderate renal insufficiency (creatinine clearance [CrCl] 45 mL/min), heart failure, and nonvalvular atrial fibrillation (AF) on warfarin is admitted because of a very supratherapeutic INR. She reports labile INR values despite strict adherence to her medication regimen. Her cancer screening tests had previously been unremarkable. She inquires about the risks and benefits of switching to a novel oral anticoagulant (NOAC) as advertised on television. Should you consider it while she is still in the hospital?
Brief overview of the issue
Lifelong anticoagulation therapy is common among patients with AF or recurrent venous thromboembolism (VTE). Until the advent of NOACs, a great majority of patients were prescribed warfarin, the oral vitamin K antagonist that requires regular blood tests for monitoring of the INR. In contrast to warfarin, NOACs are direct-acting agents (hence also known as “direct oral anticoagulants” or DOACs) that are selective for one specific coagulation factor, either thrombin (e.g., dabigatran) or factor Xa (e.g., rivaroxaban, apixaban, and edoxaban, all with an “X” in their names).
NOACS have been studied and approved by the Food and Drug Administration for nonvalvular AF, i.e., patients without rheumatic mitral stenosis, mechanical or bioprosthetic heart valve, or prior mitral valve repair. Compared to warfarin, NOACS have fewer drug or food interactions, have more predictable pharmacokinetics, and may be associated with reduced risk of major bleeding depending on the agent. The latter is a particularly attractive feature of NOAC therapy, especially when its use is considered among older patients at risk of intracranial hemorrhage (ICH), such as those with previous strokes, ICH, or reduced renal function. Unfortunately, data on the efficacy and safety of the use of NOACs in certain patient populations (e.g., those with severe renal insufficiency, active malignancy, the elderly, patients with suboptimal medication adherence) are generally lacking.
Overview of the data
There are no randomized controlled trials (RCTs) addressing the clinical benefits of switching from warfarin to NOAC therapy. However, based on a number of RCTs comparing warfarin to individual NOACs and their related meta-analyses, the following conclusions may be made about their attributes:
1. Noninferiority to warfarin in reducing the risk of ischemic stroke in AF.
2. Association with a lower rate of major bleeds (statistically significant or trend) and a lower rate of ICH and hemorrhagic strokes compared to warfarin.
3. Association with a higher rate of gastrointestinal bleeding compared to warfarin (except for apixaban, low-dose dabigatran, and edoxaban1).
4. Association with a decreased rate of all stroke and thromboembolism events compared to warfarin.
5. Association with a slightly decreased all-cause mortality in AF compared to warfarin in many studies,2-8 but not all.1,9
6. Noninferiority to warfarin in all-cause mortality in patients with VTE and for its secondary prevention.1,4
NOACS should be used with caution or avoided altogether in patients with severe liver disease or renal insufficiency (see Table 1). 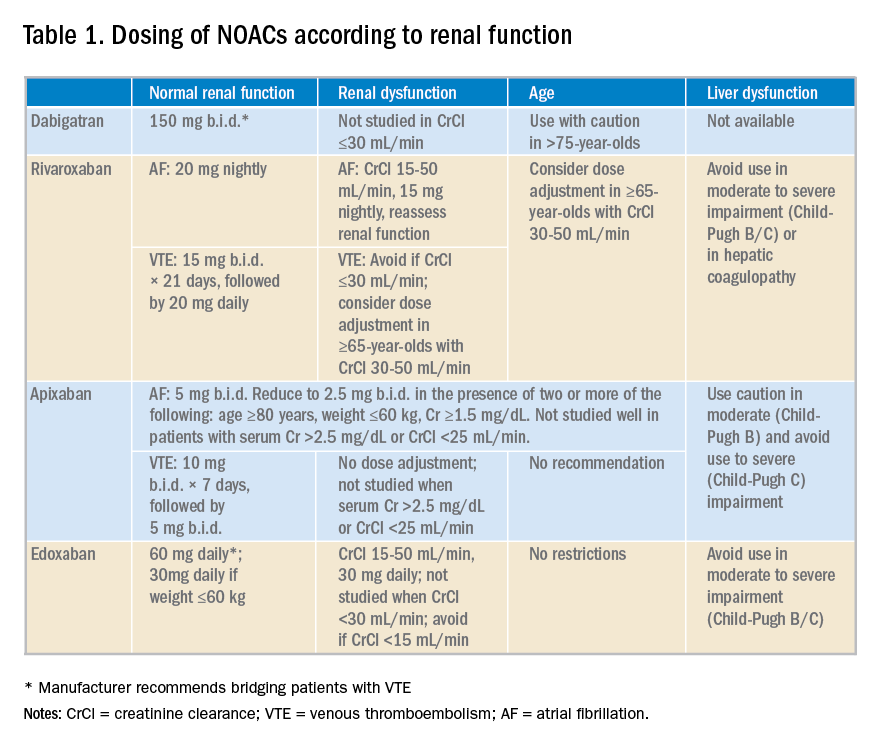
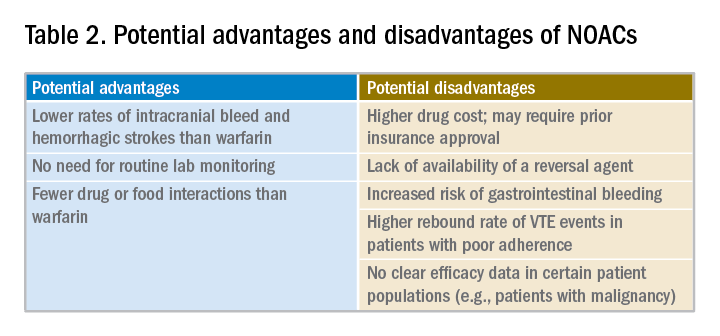
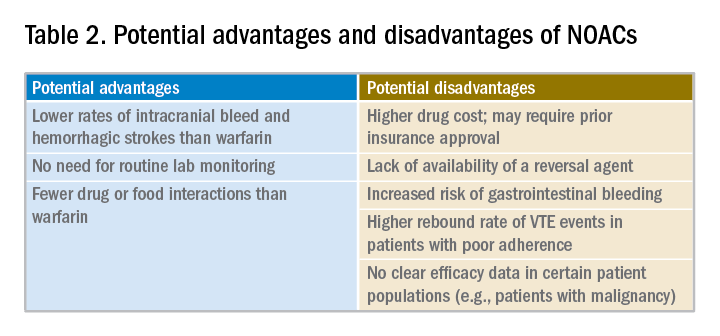
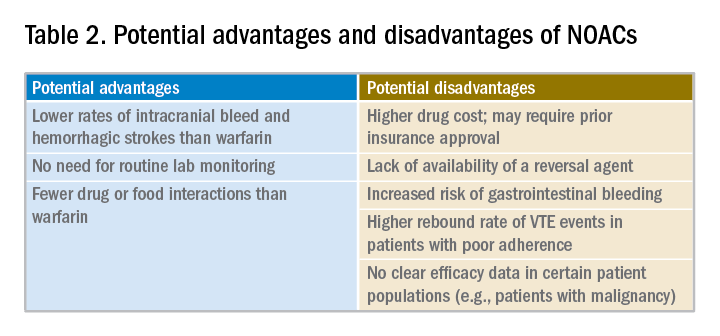
Potential advantages and disadvantages of NOAC therapy are listed in Table 2.
It should be emphasized that in patients with cancer or hypercoagulable state, no clear efficacy or safety data are currently available for the use of NOACs.
The 2016 CHEST guideline on antithrombotic therapy for VTE recommends NOACs over warfarin.10 The 2012 European Society of Cardiology AF guidelines also recommend NOACs over warfarin.11 However, the 2014 American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines on AF state that it is not necessary to change to a NOAC when patients are “stable, easily controlled, and satisfied with warfarin therapy.”12
Data from a relatively small, short-term study examining the safety of switching patients from warfarin to a NOAC suggest that although bleeding events are relatively common (12%) following such a switch, major bleeding and cardiac or cerebrovascular events are rare.10
Application of the data to our original case
Given a high calculated CHADS2VASC score of 8 in our patient, she has a clear indication for anticoagulation for AF. Her history of labile INRs, ischemic stroke, and moderate renal insufficiency place her at high risk for ICH.
A NOAC may reduce this risk but possibly at the expense of an increased risk for a gastrointestinal bleed. More importantly, however, she may be a good candidate for a switch to a NOAC because of her labile INRs despite good medication adherence. Her warfarin can be held while hospitalized and a NOAC may be initiated when the INR falls below 2.
Prior to discharge, potential cost of the drug to the patient should be explored and discussed. It is also important to involve the primary care physician in the decision-making process. Ultimately, selection of an appropriate NOAC should be based on a careful review of its risks and benefits, clinical factors, patient preference, and shared decision making.
Bottom line
Hospitalists are in a great position to discuss a switch to a NOAC in selected patients with history of good medication adherence and labile INRs or ICH risk factors.
Dr. Geisler, Dr. Liao, and Dr. Manian are hospitalists at Massachusetts General Hospital in Boston.
References
1. Sharma M et al. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: Systematic review and meta-analysis. Circulation. 2015;132(3):194-204.
2. Ruff CT et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet. 2014;383(9921):955-62.
3. Dentali F et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: A systematic review and meta-analysis of the literature. Circulation. 2012;126(20):2381-91.
4. Adam SS et al. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: A systematic review. Ann Intern Med. 2012;157(11):796-807.
5. Bruins Slot KM and Berge E. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2013(8):CD008980.
6. Gomez-Outes A et al. Dabigatran, rivaroxaban, or apixaban versus warfarin in patients with nonvalvular atrial fibrillation: A systematic review and meta-analysis of subgroups. Thrombosis. 2013;2013:640723.
7. Miller CS et al. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453-60.
8. Baker WL and Phung OJ. Systematic review and adjusted indirect comparison meta-analysis of oral anticoagulants in atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2012;5(5):711-19.
9. Ntaios G et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: A systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43(12):3298-304.
10. Kearon C et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-52.
11. Camm AJ et al. 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation – developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385-413.
12. January CT et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199-267.
Quiz
When considering a switch from warfarin to a NOAC, all the following factors should be considered a potential advantage, except:
A. No need for routing lab monitoring.
B. Lower risk of gastrointestinal bleeding.
C. Fewer drug interactions.
D. Lower rates of intracranial bleed and hemorrhagic stroke.
The correct answer is B. NOACs have been associated with lower risk of intracranial bleed and hemorrhagic stroke but not gastrointestinal bleed. Routine lab monitoring is not necessary during their use and they are associated with fewer drug interactions compared to warfarin.
Key Points
- NOACs represent a clear advancement in our anticoagulation armamentarium.
- Potential advantages of their use include lower rates of intracranial bleed and hemorrhagic strokes, fewer drug or food interactions, and lack of need for routing lab monitoring.
- Potential disadvantages of their use include increased rates of gastrointestinal bleed with some agents, general lack of availability of reversal agents, higher drug cost, unsuitability in patients with poor medication compliance, and lack of efficacy data in certain patient populations.
- Decision to switch from warfarin to a NOAC should thoroughly consider its pros and cons, clinical factors, and patient preferences.
Hospitalists must consider clinical factors and patient preferences
Hospitalists must consider clinical factors and patient preferences
Case
A 70-year old woman with hypertension, diabetes, nonischemic stroke, moderate renal insufficiency (creatinine clearance [CrCl] 45 mL/min), heart failure, and nonvalvular atrial fibrillation (AF) on warfarin is admitted because of a very supratherapeutic INR. She reports labile INR values despite strict adherence to her medication regimen. Her cancer screening tests had previously been unremarkable. She inquires about the risks and benefits of switching to a novel oral anticoagulant (NOAC) as advertised on television. Should you consider it while she is still in the hospital?
Brief overview of the issue
Lifelong anticoagulation therapy is common among patients with AF or recurrent venous thromboembolism (VTE). Until the advent of NOACs, a great majority of patients were prescribed warfarin, the oral vitamin K antagonist that requires regular blood tests for monitoring of the INR. In contrast to warfarin, NOACs are direct-acting agents (hence also known as “direct oral anticoagulants” or DOACs) that are selective for one specific coagulation factor, either thrombin (e.g., dabigatran) or factor Xa (e.g., rivaroxaban, apixaban, and edoxaban, all with an “X” in their names).
NOACS have been studied and approved by the Food and Drug Administration for nonvalvular AF, i.e., patients without rheumatic mitral stenosis, mechanical or bioprosthetic heart valve, or prior mitral valve repair. Compared to warfarin, NOACS have fewer drug or food interactions, have more predictable pharmacokinetics, and may be associated with reduced risk of major bleeding depending on the agent. The latter is a particularly attractive feature of NOAC therapy, especially when its use is considered among older patients at risk of intracranial hemorrhage (ICH), such as those with previous strokes, ICH, or reduced renal function. Unfortunately, data on the efficacy and safety of the use of NOACs in certain patient populations (e.g., those with severe renal insufficiency, active malignancy, the elderly, patients with suboptimal medication adherence) are generally lacking.
Overview of the data
There are no randomized controlled trials (RCTs) addressing the clinical benefits of switching from warfarin to NOAC therapy. However, based on a number of RCTs comparing warfarin to individual NOACs and their related meta-analyses, the following conclusions may be made about their attributes:
1. Noninferiority to warfarin in reducing the risk of ischemic stroke in AF.
2. Association with a lower rate of major bleeds (statistically significant or trend) and a lower rate of ICH and hemorrhagic strokes compared to warfarin.
3. Association with a higher rate of gastrointestinal bleeding compared to warfarin (except for apixaban, low-dose dabigatran, and edoxaban1).
4. Association with a decreased rate of all stroke and thromboembolism events compared to warfarin.
5. Association with a slightly decreased all-cause mortality in AF compared to warfarin in many studies,2-8 but not all.1,9
6. Noninferiority to warfarin in all-cause mortality in patients with VTE and for its secondary prevention.1,4
NOACS should be used with caution or avoided altogether in patients with severe liver disease or renal insufficiency (see Table 1). 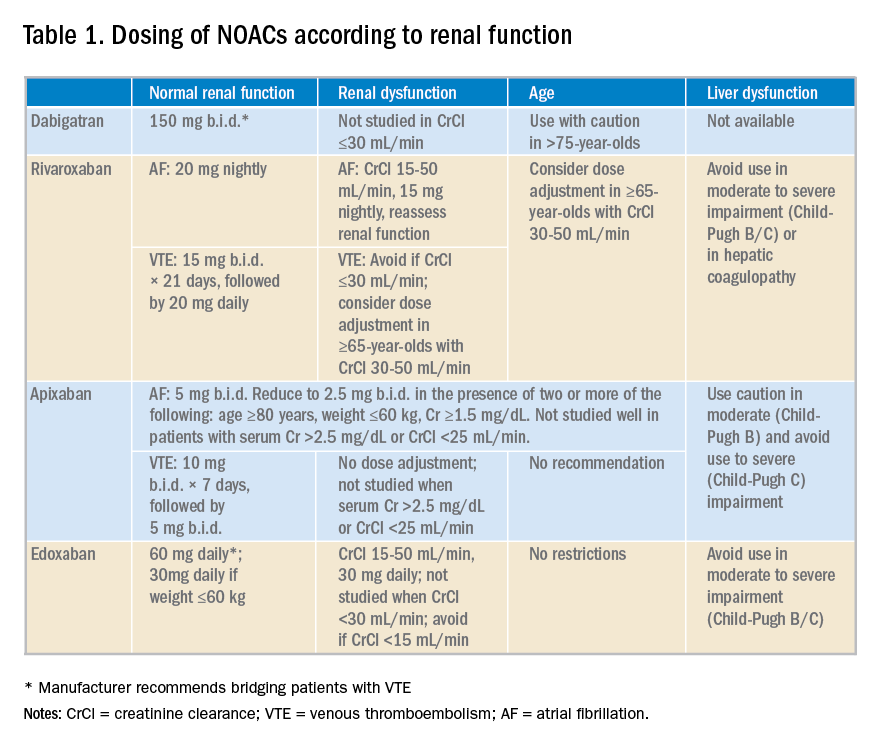
Potential advantages and disadvantages of NOAC therapy are listed in Table 2.
It should be emphasized that in patients with cancer or hypercoagulable state, no clear efficacy or safety data are currently available for the use of NOACs.
The 2016 CHEST guideline on antithrombotic therapy for VTE recommends NOACs over warfarin.10 The 2012 European Society of Cardiology AF guidelines also recommend NOACs over warfarin.11 However, the 2014 American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines on AF state that it is not necessary to change to a NOAC when patients are “stable, easily controlled, and satisfied with warfarin therapy.”12
Data from a relatively small, short-term study examining the safety of switching patients from warfarin to a NOAC suggest that although bleeding events are relatively common (12%) following such a switch, major bleeding and cardiac or cerebrovascular events are rare.10
Application of the data to our original case
Given a high calculated CHADS2VASC score of 8 in our patient, she has a clear indication for anticoagulation for AF. Her history of labile INRs, ischemic stroke, and moderate renal insufficiency place her at high risk for ICH.
A NOAC may reduce this risk but possibly at the expense of an increased risk for a gastrointestinal bleed. More importantly, however, she may be a good candidate for a switch to a NOAC because of her labile INRs despite good medication adherence. Her warfarin can be held while hospitalized and a NOAC may be initiated when the INR falls below 2.
Prior to discharge, potential cost of the drug to the patient should be explored and discussed. It is also important to involve the primary care physician in the decision-making process. Ultimately, selection of an appropriate NOAC should be based on a careful review of its risks and benefits, clinical factors, patient preference, and shared decision making.
Bottom line
Hospitalists are in a great position to discuss a switch to a NOAC in selected patients with history of good medication adherence and labile INRs or ICH risk factors.
Dr. Geisler, Dr. Liao, and Dr. Manian are hospitalists at Massachusetts General Hospital in Boston.
References
1. Sharma M et al. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: Systematic review and meta-analysis. Circulation. 2015;132(3):194-204.
2. Ruff CT et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet. 2014;383(9921):955-62.
3. Dentali F et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: A systematic review and meta-analysis of the literature. Circulation. 2012;126(20):2381-91.
4. Adam SS et al. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: A systematic review. Ann Intern Med. 2012;157(11):796-807.
5. Bruins Slot KM and Berge E. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2013(8):CD008980.
6. Gomez-Outes A et al. Dabigatran, rivaroxaban, or apixaban versus warfarin in patients with nonvalvular atrial fibrillation: A systematic review and meta-analysis of subgroups. Thrombosis. 2013;2013:640723.
7. Miller CS et al. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453-60.
8. Baker WL and Phung OJ. Systematic review and adjusted indirect comparison meta-analysis of oral anticoagulants in atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2012;5(5):711-19.
9. Ntaios G et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: A systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43(12):3298-304.
10. Kearon C et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-52.
11. Camm AJ et al. 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation – developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385-413.
12. January CT et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199-267.
Quiz
When considering a switch from warfarin to a NOAC, all the following factors should be considered a potential advantage, except:
A. No need for routing lab monitoring.
B. Lower risk of gastrointestinal bleeding.
C. Fewer drug interactions.
D. Lower rates of intracranial bleed and hemorrhagic stroke.
The correct answer is B. NOACs have been associated with lower risk of intracranial bleed and hemorrhagic stroke but not gastrointestinal bleed. Routine lab monitoring is not necessary during their use and they are associated with fewer drug interactions compared to warfarin.
Key Points
- NOACs represent a clear advancement in our anticoagulation armamentarium.
- Potential advantages of their use include lower rates of intracranial bleed and hemorrhagic strokes, fewer drug or food interactions, and lack of need for routing lab monitoring.
- Potential disadvantages of their use include increased rates of gastrointestinal bleed with some agents, general lack of availability of reversal agents, higher drug cost, unsuitability in patients with poor medication compliance, and lack of efficacy data in certain patient populations.
- Decision to switch from warfarin to a NOAC should thoroughly consider its pros and cons, clinical factors, and patient preferences.
Case
A 70-year old woman with hypertension, diabetes, nonischemic stroke, moderate renal insufficiency (creatinine clearance [CrCl] 45 mL/min), heart failure, and nonvalvular atrial fibrillation (AF) on warfarin is admitted because of a very supratherapeutic INR. She reports labile INR values despite strict adherence to her medication regimen. Her cancer screening tests had previously been unremarkable. She inquires about the risks and benefits of switching to a novel oral anticoagulant (NOAC) as advertised on television. Should you consider it while she is still in the hospital?
Brief overview of the issue
Lifelong anticoagulation therapy is common among patients with AF or recurrent venous thromboembolism (VTE). Until the advent of NOACs, a great majority of patients were prescribed warfarin, the oral vitamin K antagonist that requires regular blood tests for monitoring of the INR. In contrast to warfarin, NOACs are direct-acting agents (hence also known as “direct oral anticoagulants” or DOACs) that are selective for one specific coagulation factor, either thrombin (e.g., dabigatran) or factor Xa (e.g., rivaroxaban, apixaban, and edoxaban, all with an “X” in their names).
NOACS have been studied and approved by the Food and Drug Administration for nonvalvular AF, i.e., patients without rheumatic mitral stenosis, mechanical or bioprosthetic heart valve, or prior mitral valve repair. Compared to warfarin, NOACS have fewer drug or food interactions, have more predictable pharmacokinetics, and may be associated with reduced risk of major bleeding depending on the agent. The latter is a particularly attractive feature of NOAC therapy, especially when its use is considered among older patients at risk of intracranial hemorrhage (ICH), such as those with previous strokes, ICH, or reduced renal function. Unfortunately, data on the efficacy and safety of the use of NOACs in certain patient populations (e.g., those with severe renal insufficiency, active malignancy, the elderly, patients with suboptimal medication adherence) are generally lacking.
Overview of the data
There are no randomized controlled trials (RCTs) addressing the clinical benefits of switching from warfarin to NOAC therapy. However, based on a number of RCTs comparing warfarin to individual NOACs and their related meta-analyses, the following conclusions may be made about their attributes:
1. Noninferiority to warfarin in reducing the risk of ischemic stroke in AF.
2. Association with a lower rate of major bleeds (statistically significant or trend) and a lower rate of ICH and hemorrhagic strokes compared to warfarin.
3. Association with a higher rate of gastrointestinal bleeding compared to warfarin (except for apixaban, low-dose dabigatran, and edoxaban1).
4. Association with a decreased rate of all stroke and thromboembolism events compared to warfarin.
5. Association with a slightly decreased all-cause mortality in AF compared to warfarin in many studies,2-8 but not all.1,9
6. Noninferiority to warfarin in all-cause mortality in patients with VTE and for its secondary prevention.1,4
NOACS should be used with caution or avoided altogether in patients with severe liver disease or renal insufficiency (see Table 1). 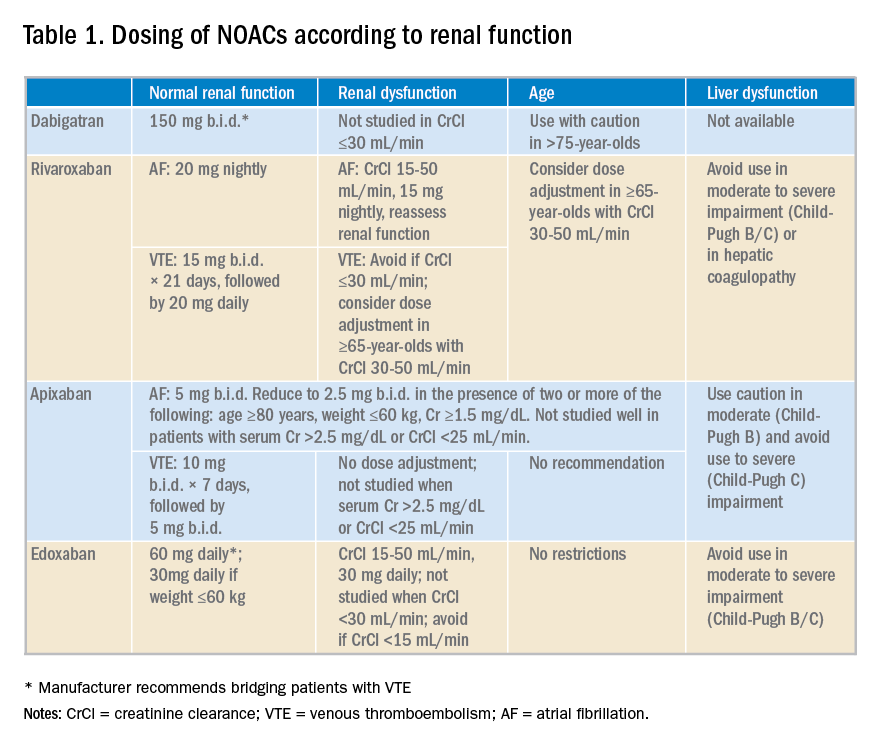
Potential advantages and disadvantages of NOAC therapy are listed in Table 2.
It should be emphasized that in patients with cancer or hypercoagulable state, no clear efficacy or safety data are currently available for the use of NOACs.
The 2016 CHEST guideline on antithrombotic therapy for VTE recommends NOACs over warfarin.10 The 2012 European Society of Cardiology AF guidelines also recommend NOACs over warfarin.11 However, the 2014 American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines on AF state that it is not necessary to change to a NOAC when patients are “stable, easily controlled, and satisfied with warfarin therapy.”12
Data from a relatively small, short-term study examining the safety of switching patients from warfarin to a NOAC suggest that although bleeding events are relatively common (12%) following such a switch, major bleeding and cardiac or cerebrovascular events are rare.10
Application of the data to our original case
Given a high calculated CHADS2VASC score of 8 in our patient, she has a clear indication for anticoagulation for AF. Her history of labile INRs, ischemic stroke, and moderate renal insufficiency place her at high risk for ICH.
A NOAC may reduce this risk but possibly at the expense of an increased risk for a gastrointestinal bleed. More importantly, however, she may be a good candidate for a switch to a NOAC because of her labile INRs despite good medication adherence. Her warfarin can be held while hospitalized and a NOAC may be initiated when the INR falls below 2.
Prior to discharge, potential cost of the drug to the patient should be explored and discussed. It is also important to involve the primary care physician in the decision-making process. Ultimately, selection of an appropriate NOAC should be based on a careful review of its risks and benefits, clinical factors, patient preference, and shared decision making.
Bottom line
Hospitalists are in a great position to discuss a switch to a NOAC in selected patients with history of good medication adherence and labile INRs or ICH risk factors.
Dr. Geisler, Dr. Liao, and Dr. Manian are hospitalists at Massachusetts General Hospital in Boston.
References
1. Sharma M et al. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: Systematic review and meta-analysis. Circulation. 2015;132(3):194-204.
2. Ruff CT et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet. 2014;383(9921):955-62.
3. Dentali F et al. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: A systematic review and meta-analysis of the literature. Circulation. 2012;126(20):2381-91.
4. Adam SS et al. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: A systematic review. Ann Intern Med. 2012;157(11):796-807.
5. Bruins Slot KM and Berge E. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2013(8):CD008980.
6. Gomez-Outes A et al. Dabigatran, rivaroxaban, or apixaban versus warfarin in patients with nonvalvular atrial fibrillation: A systematic review and meta-analysis of subgroups. Thrombosis. 2013;2013:640723.
7. Miller CS et al. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453-60.
8. Baker WL and Phung OJ. Systematic review and adjusted indirect comparison meta-analysis of oral anticoagulants in atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2012;5(5):711-19.
9. Ntaios G et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: A systematic review and meta-analysis of randomized controlled trials. Stroke. 2012;43(12):3298-304.
10. Kearon C et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315-52.
11. Camm AJ et al. 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation – developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385-413.
12. January CT et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199-267.
Quiz
When considering a switch from warfarin to a NOAC, all the following factors should be considered a potential advantage, except:
A. No need for routing lab monitoring.
B. Lower risk of gastrointestinal bleeding.
C. Fewer drug interactions.
D. Lower rates of intracranial bleed and hemorrhagic stroke.
The correct answer is B. NOACs have been associated with lower risk of intracranial bleed and hemorrhagic stroke but not gastrointestinal bleed. Routine lab monitoring is not necessary during their use and they are associated with fewer drug interactions compared to warfarin.
Key Points
- NOACs represent a clear advancement in our anticoagulation armamentarium.
- Potential advantages of their use include lower rates of intracranial bleed and hemorrhagic strokes, fewer drug or food interactions, and lack of need for routing lab monitoring.
- Potential disadvantages of their use include increased rates of gastrointestinal bleed with some agents, general lack of availability of reversal agents, higher drug cost, unsuitability in patients with poor medication compliance, and lack of efficacy data in certain patient populations.
- Decision to switch from warfarin to a NOAC should thoroughly consider its pros and cons, clinical factors, and patient preferences.
New Valsalva maneuver for SVT beats all others
NEW ORLEANS – , according to Jeet Mehta, MD, a resident in the combined medicine/pediatrics program at the University of Kansas, Wichita.
The 2015 American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines recommended vagal maneuvers as first-line treatment of supraventricular tachycardia, but added that there was no gold standard method. Since then, the situation has changed. Two well-conducted randomized clinical trials have been published that bring clarity as to the vagal maneuver of choice, Dr. Mehta reported at the annual meeting of the American College of Physicians.
He and his coinvestigators performed a meta-analysis of the three pre-2000 randomized controlled trials that compared the standard Valsalva maneuver to carotid sinus massage plus the two newer studies, both of which systematically compared a modified Valsalva maneuver with the standard version.
The clear winner in terms of efficacy was the modified Valsalva maneuver, in which patients with supraventricular tachycardia (SVT) performed a standardized strain while in a semirecumbent position, then immediately laid flat and had their legs raised to 45 degrees for 15 seconds before returning to the semirecumbent position. The purpose of this postural modification is to boost relaxation phase venous return and vagal stimulation.
In the 433-patient multicenter REVERT trial in the United Kingdom, 43% of those assigned to the modified Valsalva maneuver returned to sinus rhythm 1 minute after completing the task, compared with 17% of those randomized to the standard semirecumbent Valsalva maneuver. This resulted in significantly less need for adenosine and other treatments. Although REVERT investigators had the patients blow into a manometer at 40 mm Hg for 15 seconds, they noted that the same intensity of strain can be achieved more practically by blowing into a 10-mL syringe sufficient to just move the plunger (Lancet. 2015 Oct 31;386[10005]:1747-53).
The REVERT findings were confirmed by a second trial conducted by Turkish investigators, in which the modified Valsalva maneuver was successful in 43% of patients, compared with 11% in the standard Valsalva maneuver group (Am J Emerg Med. 2017 Nov;35[11]:1662-5).
Extrapolating from the published evidence, including a Cochrane Collaboration review (Cochrane Database Syst Rev. 2015 Feb 18;[2]:CD009502. doi: 10.1002/14651858.CD009502.pub3), Dr. Mehta and his coinvestigators ranked the likelihood of successful conversion of SVT to sinus rhythm from a high of 48% for the modified Valsalva maneuver, descending to 43% for a supine Valsalva maneuver, 36% for a standard semirecumbent Valsalva, 21% for a seated Valsalva, 19% for a standing one, and just 11% for carotid sinus massage.
“Based on evidence of high quality, we encourage that the modified Valsalva maneuver be done due its safety and low cost,” Dr. Mehta concluded.
He reported having no financial conflicts regarding his study, conducted free of commercial support.
NEW ORLEANS – , according to Jeet Mehta, MD, a resident in the combined medicine/pediatrics program at the University of Kansas, Wichita.
The 2015 American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines recommended vagal maneuvers as first-line treatment of supraventricular tachycardia, but added that there was no gold standard method. Since then, the situation has changed. Two well-conducted randomized clinical trials have been published that bring clarity as to the vagal maneuver of choice, Dr. Mehta reported at the annual meeting of the American College of Physicians.
He and his coinvestigators performed a meta-analysis of the three pre-2000 randomized controlled trials that compared the standard Valsalva maneuver to carotid sinus massage plus the two newer studies, both of which systematically compared a modified Valsalva maneuver with the standard version.
The clear winner in terms of efficacy was the modified Valsalva maneuver, in which patients with supraventricular tachycardia (SVT) performed a standardized strain while in a semirecumbent position, then immediately laid flat and had their legs raised to 45 degrees for 15 seconds before returning to the semirecumbent position. The purpose of this postural modification is to boost relaxation phase venous return and vagal stimulation.
In the 433-patient multicenter REVERT trial in the United Kingdom, 43% of those assigned to the modified Valsalva maneuver returned to sinus rhythm 1 minute after completing the task, compared with 17% of those randomized to the standard semirecumbent Valsalva maneuver. This resulted in significantly less need for adenosine and other treatments. Although REVERT investigators had the patients blow into a manometer at 40 mm Hg for 15 seconds, they noted that the same intensity of strain can be achieved more practically by blowing into a 10-mL syringe sufficient to just move the plunger (Lancet. 2015 Oct 31;386[10005]:1747-53).
The REVERT findings were confirmed by a second trial conducted by Turkish investigators, in which the modified Valsalva maneuver was successful in 43% of patients, compared with 11% in the standard Valsalva maneuver group (Am J Emerg Med. 2017 Nov;35[11]:1662-5).
Extrapolating from the published evidence, including a Cochrane Collaboration review (Cochrane Database Syst Rev. 2015 Feb 18;[2]:CD009502. doi: 10.1002/14651858.CD009502.pub3), Dr. Mehta and his coinvestigators ranked the likelihood of successful conversion of SVT to sinus rhythm from a high of 48% for the modified Valsalva maneuver, descending to 43% for a supine Valsalva maneuver, 36% for a standard semirecumbent Valsalva, 21% for a seated Valsalva, 19% for a standing one, and just 11% for carotid sinus massage.
“Based on evidence of high quality, we encourage that the modified Valsalva maneuver be done due its safety and low cost,” Dr. Mehta concluded.
He reported having no financial conflicts regarding his study, conducted free of commercial support.
NEW ORLEANS – , according to Jeet Mehta, MD, a resident in the combined medicine/pediatrics program at the University of Kansas, Wichita.
The 2015 American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines recommended vagal maneuvers as first-line treatment of supraventricular tachycardia, but added that there was no gold standard method. Since then, the situation has changed. Two well-conducted randomized clinical trials have been published that bring clarity as to the vagal maneuver of choice, Dr. Mehta reported at the annual meeting of the American College of Physicians.
He and his coinvestigators performed a meta-analysis of the three pre-2000 randomized controlled trials that compared the standard Valsalva maneuver to carotid sinus massage plus the two newer studies, both of which systematically compared a modified Valsalva maneuver with the standard version.
The clear winner in terms of efficacy was the modified Valsalva maneuver, in which patients with supraventricular tachycardia (SVT) performed a standardized strain while in a semirecumbent position, then immediately laid flat and had their legs raised to 45 degrees for 15 seconds before returning to the semirecumbent position. The purpose of this postural modification is to boost relaxation phase venous return and vagal stimulation.
In the 433-patient multicenter REVERT trial in the United Kingdom, 43% of those assigned to the modified Valsalva maneuver returned to sinus rhythm 1 minute after completing the task, compared with 17% of those randomized to the standard semirecumbent Valsalva maneuver. This resulted in significantly less need for adenosine and other treatments. Although REVERT investigators had the patients blow into a manometer at 40 mm Hg for 15 seconds, they noted that the same intensity of strain can be achieved more practically by blowing into a 10-mL syringe sufficient to just move the plunger (Lancet. 2015 Oct 31;386[10005]:1747-53).
The REVERT findings were confirmed by a second trial conducted by Turkish investigators, in which the modified Valsalva maneuver was successful in 43% of patients, compared with 11% in the standard Valsalva maneuver group (Am J Emerg Med. 2017 Nov;35[11]:1662-5).
Extrapolating from the published evidence, including a Cochrane Collaboration review (Cochrane Database Syst Rev. 2015 Feb 18;[2]:CD009502. doi: 10.1002/14651858.CD009502.pub3), Dr. Mehta and his coinvestigators ranked the likelihood of successful conversion of SVT to sinus rhythm from a high of 48% for the modified Valsalva maneuver, descending to 43% for a supine Valsalva maneuver, 36% for a standard semirecumbent Valsalva, 21% for a seated Valsalva, 19% for a standing one, and just 11% for carotid sinus massage.
“Based on evidence of high quality, we encourage that the modified Valsalva maneuver be done due its safety and low cost,” Dr. Mehta concluded.
He reported having no financial conflicts regarding his study, conducted free of commercial support.
REPORTING FROM ACP INTERNAL MEDICINE
Key clinical point: A simple postural modification to the standard Valsalva maneuver boosts conversion rate.
Major finding: Nearly half of patients in SVT converted to sinus rhythm in response to a modified Valsalva maneuver.
Study details: This was a meta-analysis of five randomized clinical trials of vagal maneuvers for conversion of supraventricular tachycardia to sinus rhythm.
Disclosures: The presenter reported having no financial conflicts regarding the study, conducted free of commercial support.
A systems-based charter on physician well-being
Don’t blame the burned-out clinician
“You can teach a canary in a coal mine to meditate, but it is still going to die.”
I have seen the canary sentiment above – used as a metaphor for health care and burnout – pop up a few times on Twitter, attributed to a few different thoughtful doctors, including Jenny Ramsey, MD, of the Cleveland Clinic (at Hospital Medicine 2018); Lucy Kalanithi, MD, a clinical assistant professor of medicine at Stanford (Calif.) University and widow of Paul Kalanithi, MD, of “When Breath Becomes Air” fame; and Stuart Slavin, MD, associate dean for curriculum and a professor of pediatrics at Saint Louis University.
To be honest, I am rather burned out on reading about physician burnout at this point. Nevertheless, I love the canary idea; it is such a perfect visual of the current problem facing physicians.
I was thinking about the meditating canary when I read the new “Charter on Physician Well-Being,” published in JAMA and already endorsed by most major medical organizations/acronyms, including SHM, ACP, SGIM, AMA, AAMC, AAIM, ABIM, ACCME, APA, and the IHI. This physician well-being charter was created by the Collaborative for Healing and Renewal in Medicine, a group that includes leading medical centers and organizations.
What makes this different from previous attempts at addressing burnout? The charter takes a systems-based approach to physician well-being. Aha, of course! As the patient safety movement realized more than 2 decades ago, real progress would only be made when we stopped focusing our attention, blame, and interventions on individuals and instead looked at systems; now, the physician well-being movement has officially made the same bold proclamation.
It is not the fault of the burned-out physician who apparently just needs to be hammered over the head with better coping skills – just as the majority of medical errors would not be fixed by continuing to tell physicians that they screwed up and should figure out how not to do that again!
We need to make real changes to the system. For example, one of the charter’s authors, Colin P. West, MD, PhD, highlighted why it is important that organizations commit to optimizing highly functioning interprofessional teams: “Can you imagine @KingJames [LeBron James] or @Oprah applying their unique skills AND personally seating the crowd, collecting stats, assessing satisfaction, etc.? So why do we?”
The authors also call for organizations to commit to reducing time spent on documentation and administration. Hallelujah!
Now the question is whether this charter will actually have any teeth or whether it will have the same fate as our canary, slowly fading away, never to be heard from again?
Read the full post at hospitalleader.org.
Dr. Moriates is the assistant dean for health care value and an associate professor of internal medicine at the University of Texas, Austin.
Also in The Hospital Leader
“What’s a Cost, Charge, and Price?” by Brad Flansbaum, DO, MPH, MHM
“There Is a ‘You’ in Team,” by Tracy Cardin, ACNP-BC, SFHM
“‘Harper’s Index’ of Hospital Medicine 2018,” by Jordan Messler, MD, SFHM
Don’t blame the burned-out clinician
Don’t blame the burned-out clinician
“You can teach a canary in a coal mine to meditate, but it is still going to die.”
I have seen the canary sentiment above – used as a metaphor for health care and burnout – pop up a few times on Twitter, attributed to a few different thoughtful doctors, including Jenny Ramsey, MD, of the Cleveland Clinic (at Hospital Medicine 2018); Lucy Kalanithi, MD, a clinical assistant professor of medicine at Stanford (Calif.) University and widow of Paul Kalanithi, MD, of “When Breath Becomes Air” fame; and Stuart Slavin, MD, associate dean for curriculum and a professor of pediatrics at Saint Louis University.
To be honest, I am rather burned out on reading about physician burnout at this point. Nevertheless, I love the canary idea; it is such a perfect visual of the current problem facing physicians.
I was thinking about the meditating canary when I read the new “Charter on Physician Well-Being,” published in JAMA and already endorsed by most major medical organizations/acronyms, including SHM, ACP, SGIM, AMA, AAMC, AAIM, ABIM, ACCME, APA, and the IHI. This physician well-being charter was created by the Collaborative for Healing and Renewal in Medicine, a group that includes leading medical centers and organizations.
What makes this different from previous attempts at addressing burnout? The charter takes a systems-based approach to physician well-being. Aha, of course! As the patient safety movement realized more than 2 decades ago, real progress would only be made when we stopped focusing our attention, blame, and interventions on individuals and instead looked at systems; now, the physician well-being movement has officially made the same bold proclamation.
It is not the fault of the burned-out physician who apparently just needs to be hammered over the head with better coping skills – just as the majority of medical errors would not be fixed by continuing to tell physicians that they screwed up and should figure out how not to do that again!
We need to make real changes to the system. For example, one of the charter’s authors, Colin P. West, MD, PhD, highlighted why it is important that organizations commit to optimizing highly functioning interprofessional teams: “Can you imagine @KingJames [LeBron James] or @Oprah applying their unique skills AND personally seating the crowd, collecting stats, assessing satisfaction, etc.? So why do we?”
The authors also call for organizations to commit to reducing time spent on documentation and administration. Hallelujah!
Now the question is whether this charter will actually have any teeth or whether it will have the same fate as our canary, slowly fading away, never to be heard from again?
Read the full post at hospitalleader.org.
Dr. Moriates is the assistant dean for health care value and an associate professor of internal medicine at the University of Texas, Austin.
Also in The Hospital Leader
“What’s a Cost, Charge, and Price?” by Brad Flansbaum, DO, MPH, MHM
“There Is a ‘You’ in Team,” by Tracy Cardin, ACNP-BC, SFHM
“‘Harper’s Index’ of Hospital Medicine 2018,” by Jordan Messler, MD, SFHM
“You can teach a canary in a coal mine to meditate, but it is still going to die.”
I have seen the canary sentiment above – used as a metaphor for health care and burnout – pop up a few times on Twitter, attributed to a few different thoughtful doctors, including Jenny Ramsey, MD, of the Cleveland Clinic (at Hospital Medicine 2018); Lucy Kalanithi, MD, a clinical assistant professor of medicine at Stanford (Calif.) University and widow of Paul Kalanithi, MD, of “When Breath Becomes Air” fame; and Stuart Slavin, MD, associate dean for curriculum and a professor of pediatrics at Saint Louis University.
To be honest, I am rather burned out on reading about physician burnout at this point. Nevertheless, I love the canary idea; it is such a perfect visual of the current problem facing physicians.
I was thinking about the meditating canary when I read the new “Charter on Physician Well-Being,” published in JAMA and already endorsed by most major medical organizations/acronyms, including SHM, ACP, SGIM, AMA, AAMC, AAIM, ABIM, ACCME, APA, and the IHI. This physician well-being charter was created by the Collaborative for Healing and Renewal in Medicine, a group that includes leading medical centers and organizations.
What makes this different from previous attempts at addressing burnout? The charter takes a systems-based approach to physician well-being. Aha, of course! As the patient safety movement realized more than 2 decades ago, real progress would only be made when we stopped focusing our attention, blame, and interventions on individuals and instead looked at systems; now, the physician well-being movement has officially made the same bold proclamation.
It is not the fault of the burned-out physician who apparently just needs to be hammered over the head with better coping skills – just as the majority of medical errors would not be fixed by continuing to tell physicians that they screwed up and should figure out how not to do that again!
We need to make real changes to the system. For example, one of the charter’s authors, Colin P. West, MD, PhD, highlighted why it is important that organizations commit to optimizing highly functioning interprofessional teams: “Can you imagine @KingJames [LeBron James] or @Oprah applying their unique skills AND personally seating the crowd, collecting stats, assessing satisfaction, etc.? So why do we?”
The authors also call for organizations to commit to reducing time spent on documentation and administration. Hallelujah!
Now the question is whether this charter will actually have any teeth or whether it will have the same fate as our canary, slowly fading away, never to be heard from again?
Read the full post at hospitalleader.org.
Dr. Moriates is the assistant dean for health care value and an associate professor of internal medicine at the University of Texas, Austin.
Also in The Hospital Leader
“What’s a Cost, Charge, and Price?” by Brad Flansbaum, DO, MPH, MHM
“There Is a ‘You’ in Team,” by Tracy Cardin, ACNP-BC, SFHM
“‘Harper’s Index’ of Hospital Medicine 2018,” by Jordan Messler, MD, SFHM
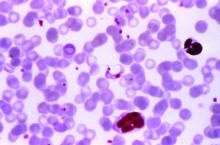
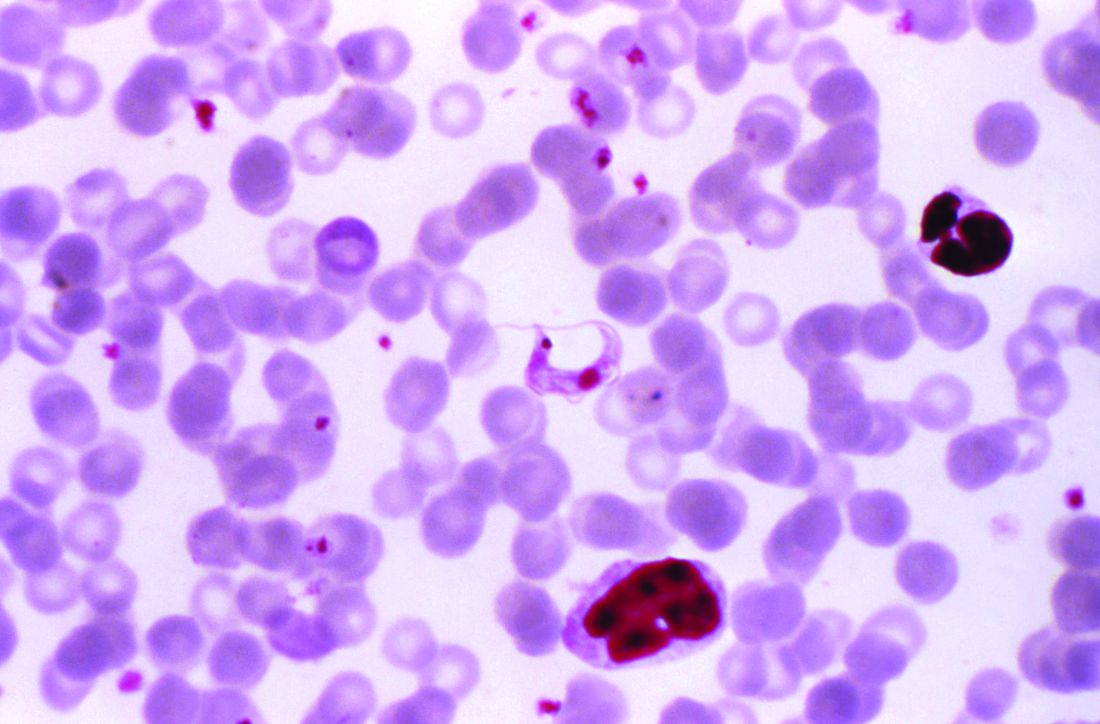
Some PE patients don’t require hospitalization
A new study suggests that
Researchers tested outpatient anticoagulant therapy in 200 patients with PE with a low mortality risk. At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism (VTE), but one patient experienced major bleeding after a traumatic injury.
A majority of patients said they were satisfied with outpatient care.
Joseph R. Bledsoe, MD, of Intermountain Medical Center in Salt Lake City, and his colleagues reported these results in Chest.
The researchers tracked patients who were treated for acute PE in five Intermountain Healthcare emergency departments (EDs) from 2013 to 2016. The patients had to have a low mortality risk according to the Pulmonary Embolism Severity Index (score less than 86), echocardiography (no signs of right heart strain), and whole-leg compression ultrasound. Patients could not have deep vein thrombosis proximal to the popliteal vein, hypoxia, hypotension, hepatic failure, or renal failure. They had to be eligible for therapeutic anticoagulation and could not have any condition requiring hospitalization.
With these criteria, the researchers selected 200 patients. They were observed in the ED or hospital for 12-24 hours and then discharged with anticoagulant therapy. Patients received rivaroxaban (n = 149), enoxaparin transitioned to warfarin (n = 26), apixaban (n = 24), or enoxaparin alone (n = 1).
Results
The study’s primary outcome was the 90-day composite rate of all-cause mortality, recurrent symptomatic VTE, and major bleeding. There were no deaths and no cases of recurrent VTE, but one patient did experience major bleeding at day 61 because of a traumatic thigh injury.
Within 7 days of study enrollment, there were 19 patients (9.5%) who returned to the ED and 2 patients (1%) who were admitted to the hospital. One patient with pulmonary infarct was admitted for pain control (day 2); the other was admitted for an elective coronary intervention (day 7) because of a positive cardiac stress test.
Within 30 days, 32 patients (16%) returned to the ED, and 5 (3%) were admitted to the hospital for events unrelated to their PE.
The study also showed that patients were largely satisfied with outpatient care. Of the 146 patients who completed a satisfaction survey at 90 days, 89% said they would choose outpatient management if they had another PE in the future.
“We found a large subset of patients with blood clots who’d do well at home; in fact, who probably did better at home,” Dr. Bledsoe said. “When patients are sent home versus staying in the hospital, they’re at lower risk of getting another infection. It’s a lot less expensive, too.”
Currently, the standard of care in the United States for acute PE is hospitalization for all patients. That’s recommended, in part, because their overall mortality rate is 17%. However, the lower mortality rate among some appropriately risk-stratified patients suggests that at-home care, which has become the norm in some European countries, leads to better outcomes for those patients overall and less chance of a hospital-introduced infection, according to Dr. Bledsoe. “Our findings show that if you appropriately risk-stratify patients, there are a lot of people with blood clots who are safe to go home.”
He added that similar research should be conducted outside of the Intermountain Healthcare system to confirm the results of this study and that a larger group of patients should be studied.
The investigators reported no conflicts related to this study.
SOURCE: Bledsoe JR et al. Chest. 2018 Aug;154(2):249-56.
A new study suggests that
Researchers tested outpatient anticoagulant therapy in 200 patients with PE with a low mortality risk. At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism (VTE), but one patient experienced major bleeding after a traumatic injury.
A majority of patients said they were satisfied with outpatient care.
Joseph R. Bledsoe, MD, of Intermountain Medical Center in Salt Lake City, and his colleagues reported these results in Chest.
The researchers tracked patients who were treated for acute PE in five Intermountain Healthcare emergency departments (EDs) from 2013 to 2016. The patients had to have a low mortality risk according to the Pulmonary Embolism Severity Index (score less than 86), echocardiography (no signs of right heart strain), and whole-leg compression ultrasound. Patients could not have deep vein thrombosis proximal to the popliteal vein, hypoxia, hypotension, hepatic failure, or renal failure. They had to be eligible for therapeutic anticoagulation and could not have any condition requiring hospitalization.
With these criteria, the researchers selected 200 patients. They were observed in the ED or hospital for 12-24 hours and then discharged with anticoagulant therapy. Patients received rivaroxaban (n = 149), enoxaparin transitioned to warfarin (n = 26), apixaban (n = 24), or enoxaparin alone (n = 1).
Results
The study’s primary outcome was the 90-day composite rate of all-cause mortality, recurrent symptomatic VTE, and major bleeding. There were no deaths and no cases of recurrent VTE, but one patient did experience major bleeding at day 61 because of a traumatic thigh injury.
Within 7 days of study enrollment, there were 19 patients (9.5%) who returned to the ED and 2 patients (1%) who were admitted to the hospital. One patient with pulmonary infarct was admitted for pain control (day 2); the other was admitted for an elective coronary intervention (day 7) because of a positive cardiac stress test.
Within 30 days, 32 patients (16%) returned to the ED, and 5 (3%) were admitted to the hospital for events unrelated to their PE.
The study also showed that patients were largely satisfied with outpatient care. Of the 146 patients who completed a satisfaction survey at 90 days, 89% said they would choose outpatient management if they had another PE in the future.
“We found a large subset of patients with blood clots who’d do well at home; in fact, who probably did better at home,” Dr. Bledsoe said. “When patients are sent home versus staying in the hospital, they’re at lower risk of getting another infection. It’s a lot less expensive, too.”
Currently, the standard of care in the United States for acute PE is hospitalization for all patients. That’s recommended, in part, because their overall mortality rate is 17%. However, the lower mortality rate among some appropriately risk-stratified patients suggests that at-home care, which has become the norm in some European countries, leads to better outcomes for those patients overall and less chance of a hospital-introduced infection, according to Dr. Bledsoe. “Our findings show that if you appropriately risk-stratify patients, there are a lot of people with blood clots who are safe to go home.”
He added that similar research should be conducted outside of the Intermountain Healthcare system to confirm the results of this study and that a larger group of patients should be studied.
The investigators reported no conflicts related to this study.
SOURCE: Bledsoe JR et al. Chest. 2018 Aug;154(2):249-56.
A new study suggests that
Researchers tested outpatient anticoagulant therapy in 200 patients with PE with a low mortality risk. At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism (VTE), but one patient experienced major bleeding after a traumatic injury.
A majority of patients said they were satisfied with outpatient care.
Joseph R. Bledsoe, MD, of Intermountain Medical Center in Salt Lake City, and his colleagues reported these results in Chest.
The researchers tracked patients who were treated for acute PE in five Intermountain Healthcare emergency departments (EDs) from 2013 to 2016. The patients had to have a low mortality risk according to the Pulmonary Embolism Severity Index (score less than 86), echocardiography (no signs of right heart strain), and whole-leg compression ultrasound. Patients could not have deep vein thrombosis proximal to the popliteal vein, hypoxia, hypotension, hepatic failure, or renal failure. They had to be eligible for therapeutic anticoagulation and could not have any condition requiring hospitalization.
With these criteria, the researchers selected 200 patients. They were observed in the ED or hospital for 12-24 hours and then discharged with anticoagulant therapy. Patients received rivaroxaban (n = 149), enoxaparin transitioned to warfarin (n = 26), apixaban (n = 24), or enoxaparin alone (n = 1).
Results
The study’s primary outcome was the 90-day composite rate of all-cause mortality, recurrent symptomatic VTE, and major bleeding. There were no deaths and no cases of recurrent VTE, but one patient did experience major bleeding at day 61 because of a traumatic thigh injury.
Within 7 days of study enrollment, there were 19 patients (9.5%) who returned to the ED and 2 patients (1%) who were admitted to the hospital. One patient with pulmonary infarct was admitted for pain control (day 2); the other was admitted for an elective coronary intervention (day 7) because of a positive cardiac stress test.
Within 30 days, 32 patients (16%) returned to the ED, and 5 (3%) were admitted to the hospital for events unrelated to their PE.
The study also showed that patients were largely satisfied with outpatient care. Of the 146 patients who completed a satisfaction survey at 90 days, 89% said they would choose outpatient management if they had another PE in the future.
“We found a large subset of patients with blood clots who’d do well at home; in fact, who probably did better at home,” Dr. Bledsoe said. “When patients are sent home versus staying in the hospital, they’re at lower risk of getting another infection. It’s a lot less expensive, too.”
Currently, the standard of care in the United States for acute PE is hospitalization for all patients. That’s recommended, in part, because their overall mortality rate is 17%. However, the lower mortality rate among some appropriately risk-stratified patients suggests that at-home care, which has become the norm in some European countries, leads to better outcomes for those patients overall and less chance of a hospital-introduced infection, according to Dr. Bledsoe. “Our findings show that if you appropriately risk-stratify patients, there are a lot of people with blood clots who are safe to go home.”
He added that similar research should be conducted outside of the Intermountain Healthcare system to confirm the results of this study and that a larger group of patients should be studied.
The investigators reported no conflicts related to this study.
SOURCE: Bledsoe JR et al. Chest. 2018 Aug;154(2):249-56.
FROM CHEST
Key clinical point: There were no deaths or recurrences of pulmonary embolism at 90 days in a group of patients stratified by criteria for low risk.
Major finding: At 90 days of follow-up, there were no deaths or recurrences of venous thromboembolism.
Study details: Researchers tested outpatient anticoagulant therapy in 200 patients with pulmonary embolism with a low mortality risk.
Disclosures: The investigators reported no conflicts related to this study.
Source: Bledsoe JR et al. Chest. 2018 Aug;154(2):249-56.
Comparison of analgesia methods for neonatal circumcision
Multiple pain management interventions exist
Clinical question
What is the optimal way to manage analgesia during neonatal circumcision?
Background
Neonatal circumcision is one of the most commonly performed surgical procedures. The American Academy of Pediatrics in 2012 noted that the health benefits outweigh the minor risks of the procedure, but that parents should make the decision to circumcise based on their own cultural, ethical, and religious beliefs.
One of the primary risks of neonatal circumcision is pain during and after the procedure. Multiple methods for managing analgesia exist, but it is unknown what combination of methods is optimal. Usual analgesia techniques include: local anesthetic cream composed of lidocaine and prilocaine (EMLA) applied to the skin prior to the procedure; oral sucrose solution given throughout the procedure; dorsal penile nerve block (DPNB); and penile ring block (RB).
Study design
Single-center, double-blinded, randomized, controlled trial.
Setting
Multispecialty freestanding hospital.
Synopsis
Parents of infant boys born at 36-41 weeks’ gestation who chose to have their children circumcised were offered participation in the study. Of 83 eligible participants, 70 were randomized, with 10 in the control group (EMLA only) and 20 in each intervention (EMLA + sucrose, EMLA + sucrose + RB, EMLA + sucrose + DPNB). A single pediatric urologist performed all circumcisions using the Gomco clamp technique.
A video camera recorded the infant’s face and upper torso during the procedure. Two researchers, who were blinded to the analgesia plan, scored these videos using a modified Neonatal Infant Pain Scale (NIPS). The NIPS used ranged from 0 to 6, with 6 considered severe pain. For rating purposes, the procedure was divided into 6 stages with a NIPS score assigned at each stage. There were no significant differences in baseline characteristics among the groups; no significant differences in the duration of the procedure by intervention; and there were no complications. Interrater reliability for the NIPS was good (kappa, 0.84). All interventions were superior to EMLA alone, with significantly decreased NIPS for all stages of the procedure. No significant differences in NIPS were found among the following:
EMLA + sucrose.
EMLA + sucrose + RB.
EMLA + sucrose + DPNB (for any stage of the procedure).
The one exception was that following lysis of foreskin adhesions, EMLA + sucrose + RB was superior (NIPS 2.25 for EMLA + sucrose + RB vs. NIPS 4.4 for EMLA + sucrose + DPNB vs. NIPS 4.3 for EMLA + sucrose vs. NIPS 5.8 for EMLA alone). In terms of crying time during the procedure, all interventions were significantly superior to EMLA alone. Of the interventions, crying time was statistically and clinically significantly shorter with EMLA + sucrose + RB (5.78 seconds vs. 11.5 for EMLA + sucrose + DPNB vs. 16.5 for EMLA + sucrose vs. 45.4 for EMLA alone). This was a single-center study and the procedures were performed by a pediatric urologist rather than by a general pediatrician, which potentially limits applicability.
Bottom line
All tested analgesia modalities for neonatal circumcision were superior to EMLA alone. The most effective analgesia of those tested was EMLA + sucrose + penile ring block.
Citation
Sharara-Chami R et al. Combination analgesia for neonatal circumcision: a randomized controlled trial. Pediatrics. 2017. doi: 10.1542/peds.2017-1935.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Multiple pain management interventions exist
Multiple pain management interventions exist
Clinical question
What is the optimal way to manage analgesia during neonatal circumcision?
Background
Neonatal circumcision is one of the most commonly performed surgical procedures. The American Academy of Pediatrics in 2012 noted that the health benefits outweigh the minor risks of the procedure, but that parents should make the decision to circumcise based on their own cultural, ethical, and religious beliefs.
One of the primary risks of neonatal circumcision is pain during and after the procedure. Multiple methods for managing analgesia exist, but it is unknown what combination of methods is optimal. Usual analgesia techniques include: local anesthetic cream composed of lidocaine and prilocaine (EMLA) applied to the skin prior to the procedure; oral sucrose solution given throughout the procedure; dorsal penile nerve block (DPNB); and penile ring block (RB).
Study design
Single-center, double-blinded, randomized, controlled trial.
Setting
Multispecialty freestanding hospital.
Synopsis
Parents of infant boys born at 36-41 weeks’ gestation who chose to have their children circumcised were offered participation in the study. Of 83 eligible participants, 70 were randomized, with 10 in the control group (EMLA only) and 20 in each intervention (EMLA + sucrose, EMLA + sucrose + RB, EMLA + sucrose + DPNB). A single pediatric urologist performed all circumcisions using the Gomco clamp technique.
A video camera recorded the infant’s face and upper torso during the procedure. Two researchers, who were blinded to the analgesia plan, scored these videos using a modified Neonatal Infant Pain Scale (NIPS). The NIPS used ranged from 0 to 6, with 6 considered severe pain. For rating purposes, the procedure was divided into 6 stages with a NIPS score assigned at each stage. There were no significant differences in baseline characteristics among the groups; no significant differences in the duration of the procedure by intervention; and there were no complications. Interrater reliability for the NIPS was good (kappa, 0.84). All interventions were superior to EMLA alone, with significantly decreased NIPS for all stages of the procedure. No significant differences in NIPS were found among the following:
EMLA + sucrose.
EMLA + sucrose + RB.
EMLA + sucrose + DPNB (for any stage of the procedure).
The one exception was that following lysis of foreskin adhesions, EMLA + sucrose + RB was superior (NIPS 2.25 for EMLA + sucrose + RB vs. NIPS 4.4 for EMLA + sucrose + DPNB vs. NIPS 4.3 for EMLA + sucrose vs. NIPS 5.8 for EMLA alone). In terms of crying time during the procedure, all interventions were significantly superior to EMLA alone. Of the interventions, crying time was statistically and clinically significantly shorter with EMLA + sucrose + RB (5.78 seconds vs. 11.5 for EMLA + sucrose + DPNB vs. 16.5 for EMLA + sucrose vs. 45.4 for EMLA alone). This was a single-center study and the procedures were performed by a pediatric urologist rather than by a general pediatrician, which potentially limits applicability.
Bottom line
All tested analgesia modalities for neonatal circumcision were superior to EMLA alone. The most effective analgesia of those tested was EMLA + sucrose + penile ring block.
Citation
Sharara-Chami R et al. Combination analgesia for neonatal circumcision: a randomized controlled trial. Pediatrics. 2017. doi: 10.1542/peds.2017-1935.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
Clinical question
What is the optimal way to manage analgesia during neonatal circumcision?
Background
Neonatal circumcision is one of the most commonly performed surgical procedures. The American Academy of Pediatrics in 2012 noted that the health benefits outweigh the minor risks of the procedure, but that parents should make the decision to circumcise based on their own cultural, ethical, and religious beliefs.
One of the primary risks of neonatal circumcision is pain during and after the procedure. Multiple methods for managing analgesia exist, but it is unknown what combination of methods is optimal. Usual analgesia techniques include: local anesthetic cream composed of lidocaine and prilocaine (EMLA) applied to the skin prior to the procedure; oral sucrose solution given throughout the procedure; dorsal penile nerve block (DPNB); and penile ring block (RB).
Study design
Single-center, double-blinded, randomized, controlled trial.
Setting
Multispecialty freestanding hospital.
Synopsis
Parents of infant boys born at 36-41 weeks’ gestation who chose to have their children circumcised were offered participation in the study. Of 83 eligible participants, 70 were randomized, with 10 in the control group (EMLA only) and 20 in each intervention (EMLA + sucrose, EMLA + sucrose + RB, EMLA + sucrose + DPNB). A single pediatric urologist performed all circumcisions using the Gomco clamp technique.
A video camera recorded the infant’s face and upper torso during the procedure. Two researchers, who were blinded to the analgesia plan, scored these videos using a modified Neonatal Infant Pain Scale (NIPS). The NIPS used ranged from 0 to 6, with 6 considered severe pain. For rating purposes, the procedure was divided into 6 stages with a NIPS score assigned at each stage. There were no significant differences in baseline characteristics among the groups; no significant differences in the duration of the procedure by intervention; and there were no complications. Interrater reliability for the NIPS was good (kappa, 0.84). All interventions were superior to EMLA alone, with significantly decreased NIPS for all stages of the procedure. No significant differences in NIPS were found among the following:
EMLA + sucrose.
EMLA + sucrose + RB.
EMLA + sucrose + DPNB (for any stage of the procedure).
The one exception was that following lysis of foreskin adhesions, EMLA + sucrose + RB was superior (NIPS 2.25 for EMLA + sucrose + RB vs. NIPS 4.4 for EMLA + sucrose + DPNB vs. NIPS 4.3 for EMLA + sucrose vs. NIPS 5.8 for EMLA alone). In terms of crying time during the procedure, all interventions were significantly superior to EMLA alone. Of the interventions, crying time was statistically and clinically significantly shorter with EMLA + sucrose + RB (5.78 seconds vs. 11.5 for EMLA + sucrose + DPNB vs. 16.5 for EMLA + sucrose vs. 45.4 for EMLA alone). This was a single-center study and the procedures were performed by a pediatric urologist rather than by a general pediatrician, which potentially limits applicability.
Bottom line
All tested analgesia modalities for neonatal circumcision were superior to EMLA alone. The most effective analgesia of those tested was EMLA + sucrose + penile ring block.
Citation
Sharara-Chami R et al. Combination analgesia for neonatal circumcision: a randomized controlled trial. Pediatrics. 2017. doi: 10.1542/peds.2017-1935.
Dr. Stubblefield is a pediatric hospitalist at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a clinical assistant professor of pediatrics at Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia.
A new, simple, inexpensive DVT diagnostic aid
NEW ORLEANS – Both the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio proved to be better predictors of the presence or absence of deep vein thrombosis than the ubiquitous D-dimer test in a retrospective study, Jason Mouabbi, MD, reported at the annual meeting of the American College of Physicians.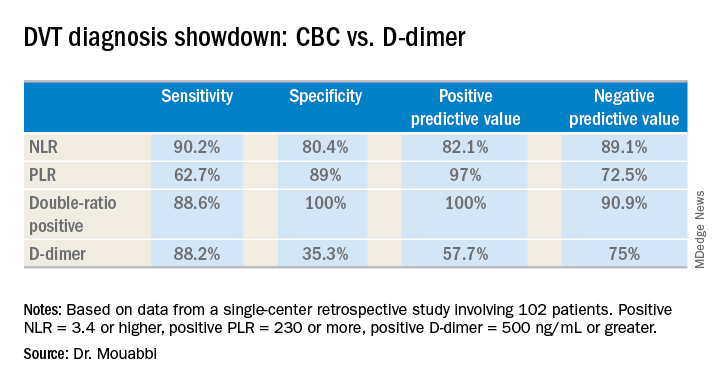
What’s more, both the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be readily calculated from the readout of a complete blood count (CBC) with differential. A CBC costs an average of $16, and everybody that comes through a hospital emergency department gets one. In contrast, the average charge for a D-dimer test is about $231 nationwide, and depending upon the specific test used the results can take up to a couple of hours to come back, noted Dr. Mouabbi of St. John Hospital and Medical Center in Detroit.
“The NLR and PLR ratios offer a new, powerful, affordable, simple, and readily available tool in the hands of clinicians to help them in the diagnosis of DVT,” he said. “The NLR can be useful to rule out DVT when it’s negative, whereas PLR can be useful in ruling DVT when positive.”
Investigators in a variety of fields are looking at the NLR and PLR as emerging practical, easily obtainable biomarkers for systemic inflammation. And DVT is thought to be an inflammatory process, he explained.
Dr. Mouabbi presented a single-center retrospective study of 102 matched patients who presented with lower extremity swelling and had a CBC drawn, as well as a D-dimer test, on the same day they underwent a lower extremity Doppler ultrasound evaluation. In 51 patients, the ultrasound revealed the presence of DVT and anticoagulation was started. In the other 51 patients, the ultrasound exam was negative and they weren’t anticoagulated. Since the study purpose was to assess the implications of a primary elevation of NLR and/or PLR, patients with rheumatic diseases, inflammatory bowel disease, recent surgery, chronic renal or liver disease, inherited thrombophilia, infection, or other possible secondary causes of altered ratios were excluded from the study.
A positive NLR was considered 3.4 or higher, a positive PLR was a ratio of 230 or more, and a positive D-dimer level was 500 ng/mL or greater. The NLR and PLR collectively outperformed the D-dimer test in terms of sensitivity, specificity, positive predictive value, and negative predictive value.
In addition, 89% of the DVT group were classified as “double-positive,” meaning they were both NLR and PLR positive. That combination provided the best diagnostic value of all, since none of the controls were double-positive and only 2% were PLR positive.
While the results are encouraging, before NLR and PLR can supplant D-dimer in patients with suspected DVT in clinical practice a confirmatory prospective study should be carried out, according to Dr. Mouabbi. Ideally it should include the use of the Wells score, which is part of most diagnostic algorithms as a preliminary means of categorizing DVT probability as low, moderate, or high. However, the popularity of the Wells score has fallen off in the face of reports that the results are subjective and variable. Indeed, the Wells score was included in the electronic medical record of so few participants in Dr. Mouabbi’s study that he couldn’t evaluate its utility.
He reported having no financial conflicts regarding his study, which was conducted free of commercial support.
NEW ORLEANS – Both the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio proved to be better predictors of the presence or absence of deep vein thrombosis than the ubiquitous D-dimer test in a retrospective study, Jason Mouabbi, MD, reported at the annual meeting of the American College of Physicians.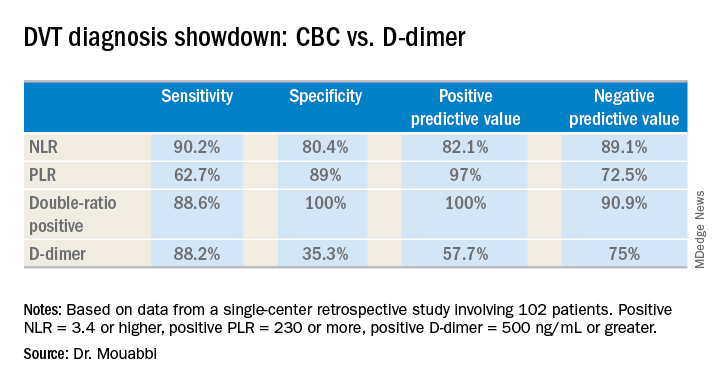
What’s more, both the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be readily calculated from the readout of a complete blood count (CBC) with differential. A CBC costs an average of $16, and everybody that comes through a hospital emergency department gets one. In contrast, the average charge for a D-dimer test is about $231 nationwide, and depending upon the specific test used the results can take up to a couple of hours to come back, noted Dr. Mouabbi of St. John Hospital and Medical Center in Detroit.
“The NLR and PLR ratios offer a new, powerful, affordable, simple, and readily available tool in the hands of clinicians to help them in the diagnosis of DVT,” he said. “The NLR can be useful to rule out DVT when it’s negative, whereas PLR can be useful in ruling DVT when positive.”
Investigators in a variety of fields are looking at the NLR and PLR as emerging practical, easily obtainable biomarkers for systemic inflammation. And DVT is thought to be an inflammatory process, he explained.
Dr. Mouabbi presented a single-center retrospective study of 102 matched patients who presented with lower extremity swelling and had a CBC drawn, as well as a D-dimer test, on the same day they underwent a lower extremity Doppler ultrasound evaluation. In 51 patients, the ultrasound revealed the presence of DVT and anticoagulation was started. In the other 51 patients, the ultrasound exam was negative and they weren’t anticoagulated. Since the study purpose was to assess the implications of a primary elevation of NLR and/or PLR, patients with rheumatic diseases, inflammatory bowel disease, recent surgery, chronic renal or liver disease, inherited thrombophilia, infection, or other possible secondary causes of altered ratios were excluded from the study.
A positive NLR was considered 3.4 or higher, a positive PLR was a ratio of 230 or more, and a positive D-dimer level was 500 ng/mL or greater. The NLR and PLR collectively outperformed the D-dimer test in terms of sensitivity, specificity, positive predictive value, and negative predictive value.
In addition, 89% of the DVT group were classified as “double-positive,” meaning they were both NLR and PLR positive. That combination provided the best diagnostic value of all, since none of the controls were double-positive and only 2% were PLR positive.
While the results are encouraging, before NLR and PLR can supplant D-dimer in patients with suspected DVT in clinical practice a confirmatory prospective study should be carried out, according to Dr. Mouabbi. Ideally it should include the use of the Wells score, which is part of most diagnostic algorithms as a preliminary means of categorizing DVT probability as low, moderate, or high. However, the popularity of the Wells score has fallen off in the face of reports that the results are subjective and variable. Indeed, the Wells score was included in the electronic medical record of so few participants in Dr. Mouabbi’s study that he couldn’t evaluate its utility.
He reported having no financial conflicts regarding his study, which was conducted free of commercial support.
NEW ORLEANS – Both the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio proved to be better predictors of the presence or absence of deep vein thrombosis than the ubiquitous D-dimer test in a retrospective study, Jason Mouabbi, MD, reported at the annual meeting of the American College of Physicians.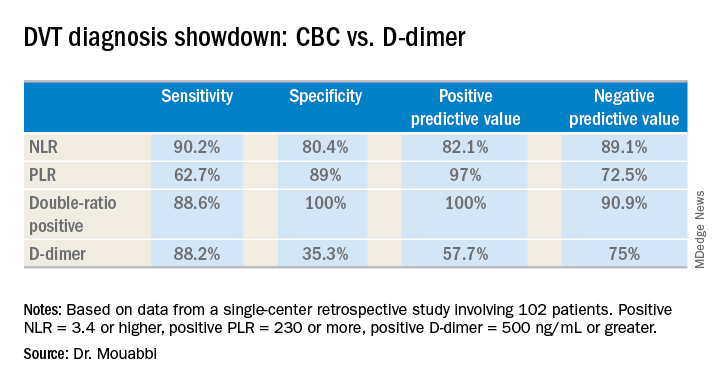
What’s more, both the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) can be readily calculated from the readout of a complete blood count (CBC) with differential. A CBC costs an average of $16, and everybody that comes through a hospital emergency department gets one. In contrast, the average charge for a D-dimer test is about $231 nationwide, and depending upon the specific test used the results can take up to a couple of hours to come back, noted Dr. Mouabbi of St. John Hospital and Medical Center in Detroit.
“The NLR and PLR ratios offer a new, powerful, affordable, simple, and readily available tool in the hands of clinicians to help them in the diagnosis of DVT,” he said. “The NLR can be useful to rule out DVT when it’s negative, whereas PLR can be useful in ruling DVT when positive.”
Investigators in a variety of fields are looking at the NLR and PLR as emerging practical, easily obtainable biomarkers for systemic inflammation. And DVT is thought to be an inflammatory process, he explained.
Dr. Mouabbi presented a single-center retrospective study of 102 matched patients who presented with lower extremity swelling and had a CBC drawn, as well as a D-dimer test, on the same day they underwent a lower extremity Doppler ultrasound evaluation. In 51 patients, the ultrasound revealed the presence of DVT and anticoagulation was started. In the other 51 patients, the ultrasound exam was negative and they weren’t anticoagulated. Since the study purpose was to assess the implications of a primary elevation of NLR and/or PLR, patients with rheumatic diseases, inflammatory bowel disease, recent surgery, chronic renal or liver disease, inherited thrombophilia, infection, or other possible secondary causes of altered ratios were excluded from the study.
A positive NLR was considered 3.4 or higher, a positive PLR was a ratio of 230 or more, and a positive D-dimer level was 500 ng/mL or greater. The NLR and PLR collectively outperformed the D-dimer test in terms of sensitivity, specificity, positive predictive value, and negative predictive value.
In addition, 89% of the DVT group were classified as “double-positive,” meaning they were both NLR and PLR positive. That combination provided the best diagnostic value of all, since none of the controls were double-positive and only 2% were PLR positive.
While the results are encouraging, before NLR and PLR can supplant D-dimer in patients with suspected DVT in clinical practice a confirmatory prospective study should be carried out, according to Dr. Mouabbi. Ideally it should include the use of the Wells score, which is part of most diagnostic algorithms as a preliminary means of categorizing DVT probability as low, moderate, or high. However, the popularity of the Wells score has fallen off in the face of reports that the results are subjective and variable. Indeed, the Wells score was included in the electronic medical record of so few participants in Dr. Mouabbi’s study that he couldn’t evaluate its utility.
He reported having no financial conflicts regarding his study, which was conducted free of commercial support.
REPORTING FROM ACP INTERNAL MEDICINE
Key clinical point:
Major finding: The neutrophil-to-lymphocyte ratio was better than the D-dimer test at helping to rule out DVT, while the platelet-to-lymphocyte ratio bested the D-dimer at ruling in DVT.
Study details: A retrospective study of 102 patients with suspected DVT.
Disclosures: Dr. Mouabbi reported no financial conflicts regarding his study, which was conducted free of commercial support.
5 HIPAA myths in the digital age
The nexus of new technology and privacy rules springing from the Health Insurance Portability and Accountability Act of 1996 (HIPAA) leads to a lot of stress and trepidation for health care professionals. Lucia Savage, chief privacy and regulatory officer for Omada Health, and Matthew Fisher, a health law attorney based in Worcester, Mass., who specializes in compliance issues, dispel common HIPAA myths and offer advice on how to protect yourself and your practice.
Truth: Physicians are not responsible for email security flaws from patient servers, said Ms. Savage, who served as chief privacy officer for the Office of the National Coordinator for Health IT under President Obama. HIPAA requires only that health providers send emails from a secure system that protects a doctor’s message from their end, she said.
“There’s this myth out there that you cannot send an electronic message to a patient’s email box if that email is unsecured, and that’s not true,” Ms. Savage said at a recent American Bar Association meeting. “The obligation is to secure what you send, not to secure what an unregulated, private person receives.”
Just remember to warn patients that they’re responsible for the safe storage of an email message once it arrives.
Truth: An email with protected health information (PHI) accidentally sent to the wrong health provider is not likely to get doctors in trouble with the Office for Civil Rights. In the last 12 years, there have been 184,000 HIPAA-related complaints to OCR and only 55 resulted in financial settlements, according to research Ms. Savage conducted through the Department of Health & Human Services website. Of the 55 settlements, none were associated with PHI accidentally sent from one health provider to another, she said in an interview.
“[The OCR] tends to seek fines for really eye-poppingly bad behavior,” Ms. Savage said, not small-scale accidents. For example, OCR fined one hospital for including the name of a patient in a press release without patient permission. Another health professional was fined for repeated failures to encrypt their computer system.
If a document with PHI does end up in the wrong inbox, Ms. Savage advises calling the receiver and asking that they immediately delete the email.
Truth: Breaches alone are not the reason most fines are levied, nor do breach notifications mean an instant penalty, Mr. Fisher said in an interview. Fines by OCR are more often tied to further noncompliance found when the agency begins investigating the entity after the breach report.
“Most breach reports will result in OCR conducting a follow-up investigation, usually with paper-based requests,” he said. “If responses to those requests reveal widespread or consistent noncompliance, then OCR may latch on and dig in order to impose a fine.”
For example, a breach could be the result of a lost USB drive or laptop, but OCR’s investigation might ultimately find that the practice failed to conduct an adequate risk analysis. Because a risk analysis is a fundamental component of HIPAA compliance, the inadequate risk analysis becomes the basis for a fine, Mr. Fisher said.
The best way to avoid an OCR fine is to ensure that proper HIPAA protocols are in place to assess security risks, prevent breaches, and mitigate breaches should they occur. “Part of good compliance is constant review and revision of policies as well,” Mr. Fisher said. “It is not sufficient to put the policies into place and then never revisit those policies. Circumstances change all of the time and policies need to keep up.”
Truth: Health professionals are obligated to provide copies of health information to patients and that includes electronic copies if practices have such technology. The electronic copy requirement was adopted in 2009 as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Despite the electronic amendment’s existence for nearly 10 years, Ms. Savage said she frequently hears from patients about the difficulty of obtaining health information and the extended time and high cost that come with requests.
“[Providing health information to patients] is an obligation,” Ms. Savage stressed. “A 21st century physician might want to be thinking about how to build on that obligation to really engage their patients in a partnership of care. If you give the patient the data, they can actually become a more valuable [participant] with you and engage in self-management.”
More information on HITECH and giving patients access to protected health information can be found here.
Truth: HIPAA is flexible and can adapt to newer technology more easily than many people think, Mr. Fisher says.
“[There is the perception] that HIPAA is archaic and does not fit with modern technology,” he said. “There are a lot of misplaced fears that digital tools cannot satisfy security requirements or will place data where they should not go.”
In actuality, many health care applications enable doctors to satisfy HIPAA requirements, while using updated technology. Secure email to send patients messages is one example, he said, as well as secure text messaging between providers.
At the same time, new technology can often assist health care privacy and advance security, Mr. Fisher noted. Technology solutions frequently automate routine tasks, such as auditing. Tools like machine learning and artificial intelligence can enhance security and catch up with attacker intelligence, he added.
“Technology should be viewed as a means of enhancing and expanding capabilities,” he said. “Using the auditing example, an individual really cannot adequately review all records or access points, but a program may be able to do so and begin to identify small trends that represent a security concern. From this perspective, the technology, as indicated, is about enhancing what can be done.”
The nexus of new technology and privacy rules springing from the Health Insurance Portability and Accountability Act of 1996 (HIPAA) leads to a lot of stress and trepidation for health care professionals. Lucia Savage, chief privacy and regulatory officer for Omada Health, and Matthew Fisher, a health law attorney based in Worcester, Mass., who specializes in compliance issues, dispel common HIPAA myths and offer advice on how to protect yourself and your practice.
Truth: Physicians are not responsible for email security flaws from patient servers, said Ms. Savage, who served as chief privacy officer for the Office of the National Coordinator for Health IT under President Obama. HIPAA requires only that health providers send emails from a secure system that protects a doctor’s message from their end, she said.
“There’s this myth out there that you cannot send an electronic message to a patient’s email box if that email is unsecured, and that’s not true,” Ms. Savage said at a recent American Bar Association meeting. “The obligation is to secure what you send, not to secure what an unregulated, private person receives.”
Just remember to warn patients that they’re responsible for the safe storage of an email message once it arrives.
Truth: An email with protected health information (PHI) accidentally sent to the wrong health provider is not likely to get doctors in trouble with the Office for Civil Rights. In the last 12 years, there have been 184,000 HIPAA-related complaints to OCR and only 55 resulted in financial settlements, according to research Ms. Savage conducted through the Department of Health & Human Services website. Of the 55 settlements, none were associated with PHI accidentally sent from one health provider to another, she said in an interview.
“[The OCR] tends to seek fines for really eye-poppingly bad behavior,” Ms. Savage said, not small-scale accidents. For example, OCR fined one hospital for including the name of a patient in a press release without patient permission. Another health professional was fined for repeated failures to encrypt their computer system.
If a document with PHI does end up in the wrong inbox, Ms. Savage advises calling the receiver and asking that they immediately delete the email.
Truth: Breaches alone are not the reason most fines are levied, nor do breach notifications mean an instant penalty, Mr. Fisher said in an interview. Fines by OCR are more often tied to further noncompliance found when the agency begins investigating the entity after the breach report.
“Most breach reports will result in OCR conducting a follow-up investigation, usually with paper-based requests,” he said. “If responses to those requests reveal widespread or consistent noncompliance, then OCR may latch on and dig in order to impose a fine.”
For example, a breach could be the result of a lost USB drive or laptop, but OCR’s investigation might ultimately find that the practice failed to conduct an adequate risk analysis. Because a risk analysis is a fundamental component of HIPAA compliance, the inadequate risk analysis becomes the basis for a fine, Mr. Fisher said.
The best way to avoid an OCR fine is to ensure that proper HIPAA protocols are in place to assess security risks, prevent breaches, and mitigate breaches should they occur. “Part of good compliance is constant review and revision of policies as well,” Mr. Fisher said. “It is not sufficient to put the policies into place and then never revisit those policies. Circumstances change all of the time and policies need to keep up.”
Truth: Health professionals are obligated to provide copies of health information to patients and that includes electronic copies if practices have such technology. The electronic copy requirement was adopted in 2009 as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Despite the electronic amendment’s existence for nearly 10 years, Ms. Savage said she frequently hears from patients about the difficulty of obtaining health information and the extended time and high cost that come with requests.
“[Providing health information to patients] is an obligation,” Ms. Savage stressed. “A 21st century physician might want to be thinking about how to build on that obligation to really engage their patients in a partnership of care. If you give the patient the data, they can actually become a more valuable [participant] with you and engage in self-management.”
More information on HITECH and giving patients access to protected health information can be found here.
Truth: HIPAA is flexible and can adapt to newer technology more easily than many people think, Mr. Fisher says.
“[There is the perception] that HIPAA is archaic and does not fit with modern technology,” he said. “There are a lot of misplaced fears that digital tools cannot satisfy security requirements or will place data where they should not go.”
In actuality, many health care applications enable doctors to satisfy HIPAA requirements, while using updated technology. Secure email to send patients messages is one example, he said, as well as secure text messaging between providers.
At the same time, new technology can often assist health care privacy and advance security, Mr. Fisher noted. Technology solutions frequently automate routine tasks, such as auditing. Tools like machine learning and artificial intelligence can enhance security and catch up with attacker intelligence, he added.
“Technology should be viewed as a means of enhancing and expanding capabilities,” he said. “Using the auditing example, an individual really cannot adequately review all records or access points, but a program may be able to do so and begin to identify small trends that represent a security concern. From this perspective, the technology, as indicated, is about enhancing what can be done.”
The nexus of new technology and privacy rules springing from the Health Insurance Portability and Accountability Act of 1996 (HIPAA) leads to a lot of stress and trepidation for health care professionals. Lucia Savage, chief privacy and regulatory officer for Omada Health, and Matthew Fisher, a health law attorney based in Worcester, Mass., who specializes in compliance issues, dispel common HIPAA myths and offer advice on how to protect yourself and your practice.
Truth: Physicians are not responsible for email security flaws from patient servers, said Ms. Savage, who served as chief privacy officer for the Office of the National Coordinator for Health IT under President Obama. HIPAA requires only that health providers send emails from a secure system that protects a doctor’s message from their end, she said.
“There’s this myth out there that you cannot send an electronic message to a patient’s email box if that email is unsecured, and that’s not true,” Ms. Savage said at a recent American Bar Association meeting. “The obligation is to secure what you send, not to secure what an unregulated, private person receives.”
Just remember to warn patients that they’re responsible for the safe storage of an email message once it arrives.
Truth: An email with protected health information (PHI) accidentally sent to the wrong health provider is not likely to get doctors in trouble with the Office for Civil Rights. In the last 12 years, there have been 184,000 HIPAA-related complaints to OCR and only 55 resulted in financial settlements, according to research Ms. Savage conducted through the Department of Health & Human Services website. Of the 55 settlements, none were associated with PHI accidentally sent from one health provider to another, she said in an interview.
“[The OCR] tends to seek fines for really eye-poppingly bad behavior,” Ms. Savage said, not small-scale accidents. For example, OCR fined one hospital for including the name of a patient in a press release without patient permission. Another health professional was fined for repeated failures to encrypt their computer system.
If a document with PHI does end up in the wrong inbox, Ms. Savage advises calling the receiver and asking that they immediately delete the email.
Truth: Breaches alone are not the reason most fines are levied, nor do breach notifications mean an instant penalty, Mr. Fisher said in an interview. Fines by OCR are more often tied to further noncompliance found when the agency begins investigating the entity after the breach report.
“Most breach reports will result in OCR conducting a follow-up investigation, usually with paper-based requests,” he said. “If responses to those requests reveal widespread or consistent noncompliance, then OCR may latch on and dig in order to impose a fine.”
For example, a breach could be the result of a lost USB drive or laptop, but OCR’s investigation might ultimately find that the practice failed to conduct an adequate risk analysis. Because a risk analysis is a fundamental component of HIPAA compliance, the inadequate risk analysis becomes the basis for a fine, Mr. Fisher said.
The best way to avoid an OCR fine is to ensure that proper HIPAA protocols are in place to assess security risks, prevent breaches, and mitigate breaches should they occur. “Part of good compliance is constant review and revision of policies as well,” Mr. Fisher said. “It is not sufficient to put the policies into place and then never revisit those policies. Circumstances change all of the time and policies need to keep up.”
Truth: Health professionals are obligated to provide copies of health information to patients and that includes electronic copies if practices have such technology. The electronic copy requirement was adopted in 2009 as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act.
Despite the electronic amendment’s existence for nearly 10 years, Ms. Savage said she frequently hears from patients about the difficulty of obtaining health information and the extended time and high cost that come with requests.
“[Providing health information to patients] is an obligation,” Ms. Savage stressed. “A 21st century physician might want to be thinking about how to build on that obligation to really engage their patients in a partnership of care. If you give the patient the data, they can actually become a more valuable [participant] with you and engage in self-management.”
More information on HITECH and giving patients access to protected health information can be found here.
Truth: HIPAA is flexible and can adapt to newer technology more easily than many people think, Mr. Fisher says.
“[There is the perception] that HIPAA is archaic and does not fit with modern technology,” he said. “There are a lot of misplaced fears that digital tools cannot satisfy security requirements or will place data where they should not go.”
In actuality, many health care applications enable doctors to satisfy HIPAA requirements, while using updated technology. Secure email to send patients messages is one example, he said, as well as secure text messaging between providers.
At the same time, new technology can often assist health care privacy and advance security, Mr. Fisher noted. Technology solutions frequently automate routine tasks, such as auditing. Tools like machine learning and artificial intelligence can enhance security and catch up with attacker intelligence, he added.
“Technology should be viewed as a means of enhancing and expanding capabilities,” he said. “Using the auditing example, an individual really cannot adequately review all records or access points, but a program may be able to do so and begin to identify small trends that represent a security concern. From this perspective, the technology, as indicated, is about enhancing what can be done.”
AHA: Chagas disease and its heart effects have come to the U.S.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
FROM CIRCULATION
CDC: 2017 worst year yet for drug overdoses
An estimated 72,000 drug overdose deaths occurred in 2017 in the United States, making it the worst year on record, according to preliminary data released by the Centers for Disease Control and Prevention.
The record high was driven by a sharp increase in deaths attributed to synthetic opioids, such as fentanyl and tramadol, data published on the agency’s website show.
The provisional counts are based on death records sent to the CDC’s National Center for Health Statistics from state vital registration offices in all 50 states and the District of Columbia, reported lead author Farida B. Ahmad, MPH, of the division of vital statistics at the NCHS. Overall, the predicted number of drug overdose deaths has climbed steadily, from 54,207 in November 2015 to 66,012 in November 2016, and to 72,287 in November 2017, according to an interactive chart accessible on the website.
Deaths attributable to synthetic opioids have climbed faster than any other drug class, soaring from just 9,983 in 2015 to 20,310 in 2016, and to 29,418 in 2017.
The next-largest category, heroin-related deaths, increased from 13,407 in 2015 to 16,012 in 2016, but appeared to plateau at 15,959 in 2017. However, the CDC cautioned that flat or declining numbers could be attributable to incomplete data, true decreases in deaths, or some combination of the two. “True declines or plateaus in the numbers of drug overdose deaths across the U.S. cannot be ascertained until final data become available.”
Cocaine-related deaths were fewer in number but appear to have risen substantially to the point where the number of deaths now nearly rival that of heroin. The number of deaths was 7,106 in 2015, 10,868 in 2016, and 14,614 in 2017.
The count of drug overdose deaths varied by state. coming in at 33.3%, though the absolute numbers of cases were low (114 through January 2017 and 152 through January 2018). North Carolina also showed substantial increases (from 2,053 to 2,515 cases, 22.5%), as did New Jersey (2,219 to 2,687 cases, 21.1%), the CDC data showed.
Provisional data will be updated on a monthly basis as additional records are received, the CDC said.
An estimated 72,000 drug overdose deaths occurred in 2017 in the United States, making it the worst year on record, according to preliminary data released by the Centers for Disease Control and Prevention.
The record high was driven by a sharp increase in deaths attributed to synthetic opioids, such as fentanyl and tramadol, data published on the agency’s website show.
The provisional counts are based on death records sent to the CDC’s National Center for Health Statistics from state vital registration offices in all 50 states and the District of Columbia, reported lead author Farida B. Ahmad, MPH, of the division of vital statistics at the NCHS. Overall, the predicted number of drug overdose deaths has climbed steadily, from 54,207 in November 2015 to 66,012 in November 2016, and to 72,287 in November 2017, according to an interactive chart accessible on the website.
Deaths attributable to synthetic opioids have climbed faster than any other drug class, soaring from just 9,983 in 2015 to 20,310 in 2016, and to 29,418 in 2017.
The next-largest category, heroin-related deaths, increased from 13,407 in 2015 to 16,012 in 2016, but appeared to plateau at 15,959 in 2017. However, the CDC cautioned that flat or declining numbers could be attributable to incomplete data, true decreases in deaths, or some combination of the two. “True declines or plateaus in the numbers of drug overdose deaths across the U.S. cannot be ascertained until final data become available.”
Cocaine-related deaths were fewer in number but appear to have risen substantially to the point where the number of deaths now nearly rival that of heroin. The number of deaths was 7,106 in 2015, 10,868 in 2016, and 14,614 in 2017.
The count of drug overdose deaths varied by state. coming in at 33.3%, though the absolute numbers of cases were low (114 through January 2017 and 152 through January 2018). North Carolina also showed substantial increases (from 2,053 to 2,515 cases, 22.5%), as did New Jersey (2,219 to 2,687 cases, 21.1%), the CDC data showed.
Provisional data will be updated on a monthly basis as additional records are received, the CDC said.
An estimated 72,000 drug overdose deaths occurred in 2017 in the United States, making it the worst year on record, according to preliminary data released by the Centers for Disease Control and Prevention.
The record high was driven by a sharp increase in deaths attributed to synthetic opioids, such as fentanyl and tramadol, data published on the agency’s website show.
The provisional counts are based on death records sent to the CDC’s National Center for Health Statistics from state vital registration offices in all 50 states and the District of Columbia, reported lead author Farida B. Ahmad, MPH, of the division of vital statistics at the NCHS. Overall, the predicted number of drug overdose deaths has climbed steadily, from 54,207 in November 2015 to 66,012 in November 2016, and to 72,287 in November 2017, according to an interactive chart accessible on the website.
Deaths attributable to synthetic opioids have climbed faster than any other drug class, soaring from just 9,983 in 2015 to 20,310 in 2016, and to 29,418 in 2017.
The next-largest category, heroin-related deaths, increased from 13,407 in 2015 to 16,012 in 2016, but appeared to plateau at 15,959 in 2017. However, the CDC cautioned that flat or declining numbers could be attributable to incomplete data, true decreases in deaths, or some combination of the two. “True declines or plateaus in the numbers of drug overdose deaths across the U.S. cannot be ascertained until final data become available.”
Cocaine-related deaths were fewer in number but appear to have risen substantially to the point where the number of deaths now nearly rival that of heroin. The number of deaths was 7,106 in 2015, 10,868 in 2016, and 14,614 in 2017.
The count of drug overdose deaths varied by state. coming in at 33.3%, though the absolute numbers of cases were low (114 through January 2017 and 152 through January 2018). North Carolina also showed substantial increases (from 2,053 to 2,515 cases, 22.5%), as did New Jersey (2,219 to 2,687 cases, 21.1%), the CDC data showed.
Provisional data will be updated on a monthly basis as additional records are received, the CDC said.
Join an SHM committee!
Opportunities to develop new mentoring relationships
Society of Hospital Medicine committee participation is an exciting opportunity available to all medical students and resident physicians. Whether you are hoping to explore new facets of hospital medicine, or take the next step in shaping your career, committee involvement creates opportunities for individuals to share their insight and work collaboratively on key SHM priorities to shape the future of hospital medicine.
If you are interested, the application is short and straightforward. Requisite SHM membership is free for students and discounted for resident members. And the benefits of committee participation are far reaching.
SHM committee opportunities will cater to most interests and career paths. Our personal interest in academic hospital medicine and medical education led us to the Physicians-In-Training (PIT) committee, but seventeen committees are available (see the complete list below). Review the committee descriptions online and select the one that best aligns with your individual interests. A mentor’s insight may be valuable in determining which committee is the best opportunity.
SHM Committee Opportunities:
- Academic Hospitalist Committee
- Annual Meeting Committee
- Awards Committee
- Chapter Support Committee
- Communications Strategy Committee
- Digital Learning Committee
- Education Committee
- Hospital Quality and Patient Safety Committee
- Membership Committee
- Patient Experience Committee
- Performance Measurement & Reporting Committee
- Physicians in Training Committee
- Practice Analysis Committee
- Practice Management Committee
- Public Policy Committee
- Research Committee
- Special Interest Group Support Committee
Membership is a boon. While opportunities for personal and professional growth are less tangible than committee work products, they remain vitally important for trainees. Through their engagement, medical students and resident physicians will have the opportunity to develop new mentoring relationships beyond the confines of their training site. We believe that committee engagement offers a “leg up” on the competition for residency and fellowship applications. Moreover, networking with hospital medicine leaders from across the country has allowed us to meet and engage with current and future colleagues, as well as potential future employers. In the long term, these experiences are sure to shape our future careers. More than a line on one’s curriculum vitae, meaningful contributions will open doors to new and exciting opportunities at our home institutions and nationally through SHM.
Balancing your training requirements with committee involvement is feasible with a little foresight and flexibility. Committee participation typically requires no more than 3-5 hours per month. Monthly committee calls account for 1 hour. Time is also spent preparing for committee calls as well as working on the action items you volunteered to complete. Individual scheduling is flexible, and contributions can occur offline if one is temporarily unavailable because of training obligations. Commitments are for at least 1 year and attendance at the SHM annual conference is highly encouraged but not required. Akin to other facets of life, the degree of participation will be linked with the value derived from the experience.
SHM committees are filled by seasoned hospitalists with dizzying accomplishments. This inherent strength can lead to feelings of uncertainty among newcomers (i.e., impostor syndrome). What can I offer? Does my perspective matter? Reflecting on these fears, we are certain that we could not have been welcomed with more enthusiasm. Our committee colleagues have been 110% supportive, receptive of our viewpoints, committed to our professional growth, and genuine when reaching out to collaborate. Treated as peers, we believe that members are valued based on their commitment and not their level of training or experience.
Committees are looking for capable individuals who have a demonstrated commitment to hospital medicine, as well as specific interests and value-added skills that will enhance the objectives of the committee they are applying for. For medical students and resident physicians, selection to a committee is competitive. While not required, a letter of support from a close mentor may be beneficial. Experience has demonstrated time and again that SHM is looking to engage and cultivate future hospital medicine leaders. To that end, all should take advantage.
Ultimately, we believe that our participation has helped motivate and influence our professional paths. We encourage all medical students and resident physicians to take the next step in their hospital medicine career by applying for committee membership. Our voice as trainees is one that needs further representation within SHM. We hope this call to action will encourage you to apply to a committee. The application can be found at the following link: https://www.hospitalmedicine.org/membership/committees/#Apply_for_a_Committee.
Dr. Bartlett is a hospitalist at the University of New Mexico Hospital, Albuquerque. Mr. Namavar is a medical student at Stritch School of Medicine, Loyola University Chicago.
Opportunities to develop new mentoring relationships
Opportunities to develop new mentoring relationships
Society of Hospital Medicine committee participation is an exciting opportunity available to all medical students and resident physicians. Whether you are hoping to explore new facets of hospital medicine, or take the next step in shaping your career, committee involvement creates opportunities for individuals to share their insight and work collaboratively on key SHM priorities to shape the future of hospital medicine.
If you are interested, the application is short and straightforward. Requisite SHM membership is free for students and discounted for resident members. And the benefits of committee participation are far reaching.
SHM committee opportunities will cater to most interests and career paths. Our personal interest in academic hospital medicine and medical education led us to the Physicians-In-Training (PIT) committee, but seventeen committees are available (see the complete list below). Review the committee descriptions online and select the one that best aligns with your individual interests. A mentor’s insight may be valuable in determining which committee is the best opportunity.
SHM Committee Opportunities:
- Academic Hospitalist Committee
- Annual Meeting Committee
- Awards Committee
- Chapter Support Committee
- Communications Strategy Committee
- Digital Learning Committee
- Education Committee
- Hospital Quality and Patient Safety Committee
- Membership Committee
- Patient Experience Committee
- Performance Measurement & Reporting Committee
- Physicians in Training Committee
- Practice Analysis Committee
- Practice Management Committee
- Public Policy Committee
- Research Committee
- Special Interest Group Support Committee
Membership is a boon. While opportunities for personal and professional growth are less tangible than committee work products, they remain vitally important for trainees. Through their engagement, medical students and resident physicians will have the opportunity to develop new mentoring relationships beyond the confines of their training site. We believe that committee engagement offers a “leg up” on the competition for residency and fellowship applications. Moreover, networking with hospital medicine leaders from across the country has allowed us to meet and engage with current and future colleagues, as well as potential future employers. In the long term, these experiences are sure to shape our future careers. More than a line on one’s curriculum vitae, meaningful contributions will open doors to new and exciting opportunities at our home institutions and nationally through SHM.
Balancing your training requirements with committee involvement is feasible with a little foresight and flexibility. Committee participation typically requires no more than 3-5 hours per month. Monthly committee calls account for 1 hour. Time is also spent preparing for committee calls as well as working on the action items you volunteered to complete. Individual scheduling is flexible, and contributions can occur offline if one is temporarily unavailable because of training obligations. Commitments are for at least 1 year and attendance at the SHM annual conference is highly encouraged but not required. Akin to other facets of life, the degree of participation will be linked with the value derived from the experience.
SHM committees are filled by seasoned hospitalists with dizzying accomplishments. This inherent strength can lead to feelings of uncertainty among newcomers (i.e., impostor syndrome). What can I offer? Does my perspective matter? Reflecting on these fears, we are certain that we could not have been welcomed with more enthusiasm. Our committee colleagues have been 110% supportive, receptive of our viewpoints, committed to our professional growth, and genuine when reaching out to collaborate. Treated as peers, we believe that members are valued based on their commitment and not their level of training or experience.
Committees are looking for capable individuals who have a demonstrated commitment to hospital medicine, as well as specific interests and value-added skills that will enhance the objectives of the committee they are applying for. For medical students and resident physicians, selection to a committee is competitive. While not required, a letter of support from a close mentor may be beneficial. Experience has demonstrated time and again that SHM is looking to engage and cultivate future hospital medicine leaders. To that end, all should take advantage.
Ultimately, we believe that our participation has helped motivate and influence our professional paths. We encourage all medical students and resident physicians to take the next step in their hospital medicine career by applying for committee membership. Our voice as trainees is one that needs further representation within SHM. We hope this call to action will encourage you to apply to a committee. The application can be found at the following link: https://www.hospitalmedicine.org/membership/committees/#Apply_for_a_Committee.
Dr. Bartlett is a hospitalist at the University of New Mexico Hospital, Albuquerque. Mr. Namavar is a medical student at Stritch School of Medicine, Loyola University Chicago.
Society of Hospital Medicine committee participation is an exciting opportunity available to all medical students and resident physicians. Whether you are hoping to explore new facets of hospital medicine, or take the next step in shaping your career, committee involvement creates opportunities for individuals to share their insight and work collaboratively on key SHM priorities to shape the future of hospital medicine.
If you are interested, the application is short and straightforward. Requisite SHM membership is free for students and discounted for resident members. And the benefits of committee participation are far reaching.
SHM committee opportunities will cater to most interests and career paths. Our personal interest in academic hospital medicine and medical education led us to the Physicians-In-Training (PIT) committee, but seventeen committees are available (see the complete list below). Review the committee descriptions online and select the one that best aligns with your individual interests. A mentor’s insight may be valuable in determining which committee is the best opportunity.
SHM Committee Opportunities:
- Academic Hospitalist Committee
- Annual Meeting Committee
- Awards Committee
- Chapter Support Committee
- Communications Strategy Committee
- Digital Learning Committee
- Education Committee
- Hospital Quality and Patient Safety Committee
- Membership Committee
- Patient Experience Committee
- Performance Measurement & Reporting Committee
- Physicians in Training Committee
- Practice Analysis Committee
- Practice Management Committee
- Public Policy Committee
- Research Committee
- Special Interest Group Support Committee
Membership is a boon. While opportunities for personal and professional growth are less tangible than committee work products, they remain vitally important for trainees. Through their engagement, medical students and resident physicians will have the opportunity to develop new mentoring relationships beyond the confines of their training site. We believe that committee engagement offers a “leg up” on the competition for residency and fellowship applications. Moreover, networking with hospital medicine leaders from across the country has allowed us to meet and engage with current and future colleagues, as well as potential future employers. In the long term, these experiences are sure to shape our future careers. More than a line on one’s curriculum vitae, meaningful contributions will open doors to new and exciting opportunities at our home institutions and nationally through SHM.
Balancing your training requirements with committee involvement is feasible with a little foresight and flexibility. Committee participation typically requires no more than 3-5 hours per month. Monthly committee calls account for 1 hour. Time is also spent preparing for committee calls as well as working on the action items you volunteered to complete. Individual scheduling is flexible, and contributions can occur offline if one is temporarily unavailable because of training obligations. Commitments are for at least 1 year and attendance at the SHM annual conference is highly encouraged but not required. Akin to other facets of life, the degree of participation will be linked with the value derived from the experience.
SHM committees are filled by seasoned hospitalists with dizzying accomplishments. This inherent strength can lead to feelings of uncertainty among newcomers (i.e., impostor syndrome). What can I offer? Does my perspective matter? Reflecting on these fears, we are certain that we could not have been welcomed with more enthusiasm. Our committee colleagues have been 110% supportive, receptive of our viewpoints, committed to our professional growth, and genuine when reaching out to collaborate. Treated as peers, we believe that members are valued based on their commitment and not their level of training or experience.
Committees are looking for capable individuals who have a demonstrated commitment to hospital medicine, as well as specific interests and value-added skills that will enhance the objectives of the committee they are applying for. For medical students and resident physicians, selection to a committee is competitive. While not required, a letter of support from a close mentor may be beneficial. Experience has demonstrated time and again that SHM is looking to engage and cultivate future hospital medicine leaders. To that end, all should take advantage.
Ultimately, we believe that our participation has helped motivate and influence our professional paths. We encourage all medical students and resident physicians to take the next step in their hospital medicine career by applying for committee membership. Our voice as trainees is one that needs further representation within SHM. We hope this call to action will encourage you to apply to a committee. The application can be found at the following link: https://www.hospitalmedicine.org/membership/committees/#Apply_for_a_Committee.
Dr. Bartlett is a hospitalist at the University of New Mexico Hospital, Albuquerque. Mr. Namavar is a medical student at Stritch School of Medicine, Loyola University Chicago.