User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Hospitalist empathy associated with reduced patient anxiety
Clinical question: What effect does hospitalist empathy have on patient anxiety, ratings of physician communication, and duration of encounter?
Background: Physician empathy is associated with better patient-reported and medical outcomes in a number of settings. The effects of hospitalist empathy have been less well studied.
Study design: Observational study of audio recordings of hospitalist admission encounters.
Setting: General medical service at two urban hospitals within an academic medical center from August 2008 to March 2009.
Synopsis: Admission encounters (76 patients, 27 hospitalists) were recorded. Researchers detected negative emotional expressions from patients and characterized resultant physician replies as either empathic (“focuses toward further expression of emotion”), neutral (“focuses neither toward nor away from emotion”), or nonempathic (“focuses away from emotion”). Through use of regression models, response frequency was compared with change in pre/post-encounter patient anxiety, patient ratings of physician communication, and duration of encounter. Every additional empathic response was associated with a small decrease in anxiety, better ratings of physician communication, and no change in encounter duration. Nonempathic responses were associated with worse communication ratings. Limitations of the study include its observational nature, small sample size, exclusion of non–English-speaking patients, absence of data on nonverbal communication, and exclusively urban academic setting.
Bottom line: Empathic hospitalist responses during admission encounters are associated with reductions in patient anxiety and better ratings of physician communication without increases in encounter duration.
Citation: Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: What effect does hospitalist empathy have on patient anxiety, ratings of physician communication, and duration of encounter?
Background: Physician empathy is associated with better patient-reported and medical outcomes in a number of settings. The effects of hospitalist empathy have been less well studied.
Study design: Observational study of audio recordings of hospitalist admission encounters.
Setting: General medical service at two urban hospitals within an academic medical center from August 2008 to March 2009.
Synopsis: Admission encounters (76 patients, 27 hospitalists) were recorded. Researchers detected negative emotional expressions from patients and characterized resultant physician replies as either empathic (“focuses toward further expression of emotion”), neutral (“focuses neither toward nor away from emotion”), or nonempathic (“focuses away from emotion”). Through use of regression models, response frequency was compared with change in pre/post-encounter patient anxiety, patient ratings of physician communication, and duration of encounter. Every additional empathic response was associated with a small decrease in anxiety, better ratings of physician communication, and no change in encounter duration. Nonempathic responses were associated with worse communication ratings. Limitations of the study include its observational nature, small sample size, exclusion of non–English-speaking patients, absence of data on nonverbal communication, and exclusively urban academic setting.
Bottom line: Empathic hospitalist responses during admission encounters are associated with reductions in patient anxiety and better ratings of physician communication without increases in encounter duration.
Citation: Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Clinical question: What effect does hospitalist empathy have on patient anxiety, ratings of physician communication, and duration of encounter?
Background: Physician empathy is associated with better patient-reported and medical outcomes in a number of settings. The effects of hospitalist empathy have been less well studied.
Study design: Observational study of audio recordings of hospitalist admission encounters.
Setting: General medical service at two urban hospitals within an academic medical center from August 2008 to March 2009.
Synopsis: Admission encounters (76 patients, 27 hospitalists) were recorded. Researchers detected negative emotional expressions from patients and characterized resultant physician replies as either empathic (“focuses toward further expression of emotion”), neutral (“focuses neither toward nor away from emotion”), or nonempathic (“focuses away from emotion”). Through use of regression models, response frequency was compared with change in pre/post-encounter patient anxiety, patient ratings of physician communication, and duration of encounter. Every additional empathic response was associated with a small decrease in anxiety, better ratings of physician communication, and no change in encounter duration. Nonempathic responses were associated with worse communication ratings. Limitations of the study include its observational nature, small sample size, exclusion of non–English-speaking patients, absence of data on nonverbal communication, and exclusively urban academic setting.
Bottom line: Empathic hospitalist responses during admission encounters are associated with reductions in patient anxiety and better ratings of physician communication without increases in encounter duration.
Citation: Weiss R et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12(10):805-10.
Dr. Kanjee is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
National Early Warning Score discriminates deterioration of inpatients with liver disease
, within 24 hours in hospitalized patients, according to a study published in the journal Clinical Gastroenterology and Hepatology.
Although existing predictive models estimate medium- and long-term prognosis in patients with liver disease, none are validated for short-term outcomes in inpatient settings. Despite the potential concern that patients with liver disease present with chronic physiological derangements affecting National Early Warning Score (NEWS) parameters, the score accurately discriminated patients at risk of death, admission to the ICU, or cardiac arrest within a 24-hour period for a range of liver-related diagnoses achieving an area under receiver operating characteristics (AUROC) curve of 0.894 (95% confidence intervals, 0.887-0.902), 0.857 (95% CI, 0.847-0.868), and 0.722 (95% CI, 0.685-0.759), respectively.
NEWS was launched in 2012 to reduce variations among existing early warning scores by the Royal College of Physicians for use in all adults except pregnant women. Theresa J. Hydes MD, PhD, and her colleagues at the department of gastroenterology & hepatology, Portsmouth (England) Hospitals NHS Trust, sought to validate NEWS in 35,585 unselected medical patients.
The NEWS allocates weighted points, based on derangement of vital signs from defined normal ranges including pulse, respiratory rate, systolic blood pressure, an alert-verbal-painful-unresponsive scale, temperature, peripheral oxygen saturations, and use of supplemental oxygen. The summation of allocated points to directs changes in the level of care, for example, more frequent monitoring, involving senior staff, or calling a rapid response team.
The study was performed in a large, acute care hospital in southern England and analyzed a database of electronically captured vital signs recorded in real time from completed consecutive admissions of patients aged 16 years or older, during 2010-2014. International Classification of Diseases-10 codes were used to categorize patients for any finished consultant episode. The categories included patients with primary diagnosis of liver disease, those with nonprimary liver diagnosis (comorbidity), and patients not allocated any liver disease codes (controls). The NEWS performance was examined according to whether liver disease was acute or chronic, alcohol induced, or associated with portal hypertension, with four clinical subgroups: acute alcohol-induced liver injury, other acute injury, chronic liver disease without cirrhosis, or cirrhosis. The final dataset comprised 722 patients (1,112 episodes) with a primary liver diagnosis, and 2,339 patients (3,658 episodes) with a nonprimary liver diagnosis.
The primary study endpoint was any of the following events occurring within 24 hours of an observation set: in-hospital mortality, unanticipated ICU admission, or cardiac arrest. “The NEWS identified patients with primary, nonprimary, and no diagnoses of liver disease with AUROC values of 0.873 (95% CI, 0.860-0.886), 0.898 (95% CI, 0.891-0.905), and 0.879 (95% CI, 0.877-0.881), respectively. High AUROC values also were obtained for all clinical subgroups; the NEWS identified patients with alcohol-related liver disease with an AUROC value of 0.927 (95% CI, 0.912-0.941). The NEWS identified patients with liver diseases with higher AUROC values than [did] other early warning scoring systems,” according to Dr. Hydes and her colleagues.
“Because of its widespread use, the NEWS serves a ready-made, easy-to-use option for identifying patients with liver disease who require early assessment and intervention, without the need to modify parameters, weightings or escalation criteria,” wrote the authors.
The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust. Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
SOURCE: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035.
, within 24 hours in hospitalized patients, according to a study published in the journal Clinical Gastroenterology and Hepatology.
Although existing predictive models estimate medium- and long-term prognosis in patients with liver disease, none are validated for short-term outcomes in inpatient settings. Despite the potential concern that patients with liver disease present with chronic physiological derangements affecting National Early Warning Score (NEWS) parameters, the score accurately discriminated patients at risk of death, admission to the ICU, or cardiac arrest within a 24-hour period for a range of liver-related diagnoses achieving an area under receiver operating characteristics (AUROC) curve of 0.894 (95% confidence intervals, 0.887-0.902), 0.857 (95% CI, 0.847-0.868), and 0.722 (95% CI, 0.685-0.759), respectively.
NEWS was launched in 2012 to reduce variations among existing early warning scores by the Royal College of Physicians for use in all adults except pregnant women. Theresa J. Hydes MD, PhD, and her colleagues at the department of gastroenterology & hepatology, Portsmouth (England) Hospitals NHS Trust, sought to validate NEWS in 35,585 unselected medical patients.
The NEWS allocates weighted points, based on derangement of vital signs from defined normal ranges including pulse, respiratory rate, systolic blood pressure, an alert-verbal-painful-unresponsive scale, temperature, peripheral oxygen saturations, and use of supplemental oxygen. The summation of allocated points to directs changes in the level of care, for example, more frequent monitoring, involving senior staff, or calling a rapid response team.
The study was performed in a large, acute care hospital in southern England and analyzed a database of electronically captured vital signs recorded in real time from completed consecutive admissions of patients aged 16 years or older, during 2010-2014. International Classification of Diseases-10 codes were used to categorize patients for any finished consultant episode. The categories included patients with primary diagnosis of liver disease, those with nonprimary liver diagnosis (comorbidity), and patients not allocated any liver disease codes (controls). The NEWS performance was examined according to whether liver disease was acute or chronic, alcohol induced, or associated with portal hypertension, with four clinical subgroups: acute alcohol-induced liver injury, other acute injury, chronic liver disease without cirrhosis, or cirrhosis. The final dataset comprised 722 patients (1,112 episodes) with a primary liver diagnosis, and 2,339 patients (3,658 episodes) with a nonprimary liver diagnosis.
The primary study endpoint was any of the following events occurring within 24 hours of an observation set: in-hospital mortality, unanticipated ICU admission, or cardiac arrest. “The NEWS identified patients with primary, nonprimary, and no diagnoses of liver disease with AUROC values of 0.873 (95% CI, 0.860-0.886), 0.898 (95% CI, 0.891-0.905), and 0.879 (95% CI, 0.877-0.881), respectively. High AUROC values also were obtained for all clinical subgroups; the NEWS identified patients with alcohol-related liver disease with an AUROC value of 0.927 (95% CI, 0.912-0.941). The NEWS identified patients with liver diseases with higher AUROC values than [did] other early warning scoring systems,” according to Dr. Hydes and her colleagues.
“Because of its widespread use, the NEWS serves a ready-made, easy-to-use option for identifying patients with liver disease who require early assessment and intervention, without the need to modify parameters, weightings or escalation criteria,” wrote the authors.
The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust. Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
SOURCE: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035.
, within 24 hours in hospitalized patients, according to a study published in the journal Clinical Gastroenterology and Hepatology.
Although existing predictive models estimate medium- and long-term prognosis in patients with liver disease, none are validated for short-term outcomes in inpatient settings. Despite the potential concern that patients with liver disease present with chronic physiological derangements affecting National Early Warning Score (NEWS) parameters, the score accurately discriminated patients at risk of death, admission to the ICU, or cardiac arrest within a 24-hour period for a range of liver-related diagnoses achieving an area under receiver operating characteristics (AUROC) curve of 0.894 (95% confidence intervals, 0.887-0.902), 0.857 (95% CI, 0.847-0.868), and 0.722 (95% CI, 0.685-0.759), respectively.
NEWS was launched in 2012 to reduce variations among existing early warning scores by the Royal College of Physicians for use in all adults except pregnant women. Theresa J. Hydes MD, PhD, and her colleagues at the department of gastroenterology & hepatology, Portsmouth (England) Hospitals NHS Trust, sought to validate NEWS in 35,585 unselected medical patients.
The NEWS allocates weighted points, based on derangement of vital signs from defined normal ranges including pulse, respiratory rate, systolic blood pressure, an alert-verbal-painful-unresponsive scale, temperature, peripheral oxygen saturations, and use of supplemental oxygen. The summation of allocated points to directs changes in the level of care, for example, more frequent monitoring, involving senior staff, or calling a rapid response team.
The study was performed in a large, acute care hospital in southern England and analyzed a database of electronically captured vital signs recorded in real time from completed consecutive admissions of patients aged 16 years or older, during 2010-2014. International Classification of Diseases-10 codes were used to categorize patients for any finished consultant episode. The categories included patients with primary diagnosis of liver disease, those with nonprimary liver diagnosis (comorbidity), and patients not allocated any liver disease codes (controls). The NEWS performance was examined according to whether liver disease was acute or chronic, alcohol induced, or associated with portal hypertension, with four clinical subgroups: acute alcohol-induced liver injury, other acute injury, chronic liver disease without cirrhosis, or cirrhosis. The final dataset comprised 722 patients (1,112 episodes) with a primary liver diagnosis, and 2,339 patients (3,658 episodes) with a nonprimary liver diagnosis.
The primary study endpoint was any of the following events occurring within 24 hours of an observation set: in-hospital mortality, unanticipated ICU admission, or cardiac arrest. “The NEWS identified patients with primary, nonprimary, and no diagnoses of liver disease with AUROC values of 0.873 (95% CI, 0.860-0.886), 0.898 (95% CI, 0.891-0.905), and 0.879 (95% CI, 0.877-0.881), respectively. High AUROC values also were obtained for all clinical subgroups; the NEWS identified patients with alcohol-related liver disease with an AUROC value of 0.927 (95% CI, 0.912-0.941). The NEWS identified patients with liver diseases with higher AUROC values than [did] other early warning scoring systems,” according to Dr. Hydes and her colleagues.
“Because of its widespread use, the NEWS serves a ready-made, easy-to-use option for identifying patients with liver disease who require early assessment and intervention, without the need to modify parameters, weightings or escalation criteria,” wrote the authors.
The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust. Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
SOURCE: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: The performance of the National Early Warning Score, used to identify deteriorating adult hospital inpatients with acute and chronic liver diseases within 24 hours of admission, was assessed.
Major finding: NEWS accurately discriminates risk of death, ICU admission, or cardiac arrest within 24 hours in patients with liver-related diagnoses.
Study details: A database of electronically captured vital signs recorded in real-time from completed consecutive admissions (episodes) of patients aged at least 16 years between Jan. 1, 2010, and Oct. 31, 2014. Nurses recorded data at the bedside using electronic devices running VitalPAC software.
Disclosures: The study was supported by VitalPAC, a collaborative development of the Learning Clinic and Portsmouth Hospitals NHS Trust (PHT). Dr. Schmidt, Dr. Aspinall, and Dr. Meredith are employed by PHT. Dr. Hydes had no conflicts of interest.
Source: Hydes TJ et al. Clin Gastroenterol Hepatol. 2017 Dec 22. doi: 10.1016/j.cgh.2017.12.035
Reported penicillin allergies hike inpatient costs
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
Total inpatient costs for patients who report being allergic to penicillin are much higher than for those who don’t report an allergy, according to a recent systematic review and meta-analysis.
The review, which eventually included 30 articles, found that total inpatient costs ranged from an average $1,145-$4,254 higher per patient with a reported penicillin allergy compared to nonallergic patients, said T. Joseph Mattingly, PharmD, and his associates. Outpatient prescription costs were also estimated to be steeper, running $14-$93 higher per patient who reported a penicillin allergy.
Although 10%-20% of patients report a penicillin allergy, “[a] majority of patients who report PCN [penicillin] allergy are not truly allergic upon confirmatory testing,” Dr. Mattingly and his colleagues wrote.
This overreporting of penicillin allergies is a problem for the patient and the health care system because “reported antibiotic allergies have been associated with suboptimal antibiotic therapy, increased antimicrobial resistance, increased length of stay, increased antibiotic-related adverse events, increased rates of C. difficile infection, intensive care unit (ICU) admission, death, as well as increased treatment cost,” said Dr. Mattingly and his coauthors.
Health care providers often “tend to take reported allergies at face value,” said coauthor Anne Fulton, suggesting that primary care practices can help by considering skin testing for those patients who carry a label of penicillin allergy, but don’t have a documented confirmatory test. The cost for a commonly used skin test for penicillin allergy runs about $200, said Ms. Fulton, a doctoral candidate at the University of Maryland, Baltimore, in an interview.
When conducting the meta-analysis, Dr. Mattingly and his coauthors converted all figures to 2017 U.S. dollars, using Consumer Price Index figures to adjust for inflation. This yields conservative estimates for cost, as drug and health care prices have far outstripped the general rate of inflation during the period in which the studies occurred, Ms. Fulton acknowledged.
The investigators highlighted the need for ongoing study in this area. “To our knowledge, there are no evaluations of long-term outpatient outcomes related to the effects of PCN allergy and the potential impact of delabeling patients who do not have a true allergy,” they wrote.
Ms. Fulton agreed, noting that the studies covered in the meta-analysis were primarily focused on short-term outcomes, though there are many potential long-term benefits to delabeling patients who are not truly penicillin allergic.
For the patient, this includes the opportunity to receive optimal antimicrobial therapy, as well as potential savings in copays and other out-of-pocket expenses for outpatient medications, she said.
As antimicrobial resistance becomes an ever more pressing problem, there are more opportunities for targeted therapy if inappropriate allergy labeling is addressed, Ms. Fulton added.
Further study should use “cost-effectiveness analysis methods that include societal and health sector perspectives capturing immediate and future outcomes and costs to evaluate the use of skin-testing procedures in either inpatient or outpatient settings,” the investigators wrote.
The study was supported by ALK, the manufacturer of Pre-Pen, a commercially available penicillin allergy skin test.
SOURCE: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
FROM JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY: IN PRACTICE
Key clinical point: Inpatient costs were $1,145 – $4,254 higher for those reporting penicillin allergy.
Major finding: Though most studies addressed inpatient admissions, outpatient costs were also significantly higher.
Study details: Systematic review and meta-analysis of 30 articles addressing reported penicillin allergy.
Disclosures: The study was sponsored by ALK.
Source: Mattingly TJ et al. J Allergy Clin Immunol Pract. 2018 Jan 31. doi: 10.1016/j.jaip.2017.12.033.
MedPAC: Medicare hospital readmissions program is working
WASHINGTON – The Medicare Hospital Readmissions Reduction Program is working, according to an original analysis of Medicare claims data presented at a meeting of the Medicare Payment Advisory Commission.
“First, readmissions declined,” MedPAC staff member Jeff Stensland, PhD, said during a congressionally mandated staff report to the commissioners. “Second, while observation stays increased, they did not fully offset the decrease in readmissions. Third, while [emergency department] visits also increased, those increases appear to largely be due to factors other than the readmission program. And fourth, in addition, all the evidence we examined suggests that the readmissions program did not result in increased mortality.”
including a reduction in readmissions and patients spending less time in the hospital with “at least equal outcomes,” Dr. Stensland said at the meeting.
Taxpayers benefited from a $2 billion reduction in spending on readmissions, which will “help extend the viability of the Medicare Trust Fund.” He noted that improvements to the program will be discussed at future MedPAC meetings.
Not all MedPAC commissioners agreed with the staff analysis.
David Nerenz, PhD, of the Henry Ford Health System, Detroit, also was not convinced the program was having an impact, noting that hospital readmissions began to decline even before the program started.
In looking at a graph presented that showed this trend, “I was impressed by the fact that the trend line started coming down all the way to the left side of the graph, and what my eye was impressed with was more just the continuation rather than a change, so I guess I feel cautious saying the program had certain effects because they certainly don’t jump off the graph visually,” Dr. Nerenz said. “I’m not disputing the numbers, but to say just as a clear unqualified conclusion the program reduced readmissions, I’m not so sure.”
It is likely premature to make any firm conclusions about how effectively this program decreases unnecessary utilization of hospitals. However, it is heartening to know that it did not increase mortality. The one variable that would best control readmissions is patient education. What constitutes an emergency requiring hospital evaluation and potential admission is often not explained to the patient by you and me.
It is likely premature to make any firm conclusions about how effectively this program decreases unnecessary utilization of hospitals. However, it is heartening to know that it did not increase mortality. The one variable that would best control readmissions is patient education. What constitutes an emergency requiring hospital evaluation and potential admission is often not explained to the patient by you and me.
It is likely premature to make any firm conclusions about how effectively this program decreases unnecessary utilization of hospitals. However, it is heartening to know that it did not increase mortality. The one variable that would best control readmissions is patient education. What constitutes an emergency requiring hospital evaluation and potential admission is often not explained to the patient by you and me.
WASHINGTON – The Medicare Hospital Readmissions Reduction Program is working, according to an original analysis of Medicare claims data presented at a meeting of the Medicare Payment Advisory Commission.
“First, readmissions declined,” MedPAC staff member Jeff Stensland, PhD, said during a congressionally mandated staff report to the commissioners. “Second, while observation stays increased, they did not fully offset the decrease in readmissions. Third, while [emergency department] visits also increased, those increases appear to largely be due to factors other than the readmission program. And fourth, in addition, all the evidence we examined suggests that the readmissions program did not result in increased mortality.”
including a reduction in readmissions and patients spending less time in the hospital with “at least equal outcomes,” Dr. Stensland said at the meeting.
Taxpayers benefited from a $2 billion reduction in spending on readmissions, which will “help extend the viability of the Medicare Trust Fund.” He noted that improvements to the program will be discussed at future MedPAC meetings.
Not all MedPAC commissioners agreed with the staff analysis.
David Nerenz, PhD, of the Henry Ford Health System, Detroit, also was not convinced the program was having an impact, noting that hospital readmissions began to decline even before the program started.
In looking at a graph presented that showed this trend, “I was impressed by the fact that the trend line started coming down all the way to the left side of the graph, and what my eye was impressed with was more just the continuation rather than a change, so I guess I feel cautious saying the program had certain effects because they certainly don’t jump off the graph visually,” Dr. Nerenz said. “I’m not disputing the numbers, but to say just as a clear unqualified conclusion the program reduced readmissions, I’m not so sure.”
WASHINGTON – The Medicare Hospital Readmissions Reduction Program is working, according to an original analysis of Medicare claims data presented at a meeting of the Medicare Payment Advisory Commission.
“First, readmissions declined,” MedPAC staff member Jeff Stensland, PhD, said during a congressionally mandated staff report to the commissioners. “Second, while observation stays increased, they did not fully offset the decrease in readmissions. Third, while [emergency department] visits also increased, those increases appear to largely be due to factors other than the readmission program. And fourth, in addition, all the evidence we examined suggests that the readmissions program did not result in increased mortality.”
including a reduction in readmissions and patients spending less time in the hospital with “at least equal outcomes,” Dr. Stensland said at the meeting.
Taxpayers benefited from a $2 billion reduction in spending on readmissions, which will “help extend the viability of the Medicare Trust Fund.” He noted that improvements to the program will be discussed at future MedPAC meetings.
Not all MedPAC commissioners agreed with the staff analysis.
David Nerenz, PhD, of the Henry Ford Health System, Detroit, also was not convinced the program was having an impact, noting that hospital readmissions began to decline even before the program started.
In looking at a graph presented that showed this trend, “I was impressed by the fact that the trend line started coming down all the way to the left side of the graph, and what my eye was impressed with was more just the continuation rather than a change, so I guess I feel cautious saying the program had certain effects because they certainly don’t jump off the graph visually,” Dr. Nerenz said. “I’m not disputing the numbers, but to say just as a clear unqualified conclusion the program reduced readmissions, I’m not so sure.”
REPORTING FROM MEDPAC
REPROVE: Ceftazidime-avibactam noninferior to meropenem for nosocomial pneumonia
Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia including ventilator-associated pneumonia from gram-negative organisms, results from the REPROVE trial demonstrated.
Nosocomial or hospital-acquired pneumonia is a common hospital-acquired infection associated with increased cost and mortality. Further, nosocomial pneumonia is associated with gram-negative pathogens such as Pseudomonas aeruginosa and Enterobacteriaceae that may carry extended-spectrum beta-lactamases and carbapenemase, thereby limiting the treatment options. However, ceftazidime-avibactam has both antipseudomonal and extended beta-lactamase coverage for multidrug-resistant gram-negative infections, and may provide an alternative to meropenem.
Antoni Torres, MD, of the University of Barcelona and his colleagues sought to compare the safety and efficacy of ceftazidime-avibactam to meropenem in patients with nosocomial and ventilator-associated pneumonia. The REPROVE study was a phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries. Patients were randomly assigned 1:1 to receive either ceftazidime-avibactam (500-2,000 mg every 8 hours) or meropenem (1,000 mg every 8 hours) with adjustment as needed for renal function.
Participants included in the study were 18-90 years of age with nosocomial pneumonia as evidenced by pneumonia 48 hours or more after admission or within 7 days after discharge from an inpatient facility. Patients with ventilator-associated pneumonia had lung infection within 48 hours of intubation and mechanical ventilation. Sputum culture and gram stains were obtained within 48 hours before randomization, and patients were excluded for evidence of gram-positive–only pathogens or those not expected to respond to meropenem or ceftazidime-avibactam.
The study involved a safety population (808 patients), a clinically modified intention-to-treat population (726), and a clinically evaluable population (527). The intention-to-treat population demonstrated a predominance of Klebsiella pneumoniae (37%), and Pseudomonas aeruginosa (30%); 28% of the intention-to-treat population were identified as not susceptible to ceftazidime.
Overall, the clinically modified intention-to-treat group demonstrated a clinical cure rate of 68.8% (245/356) in the ceftazidime-avibactam and 73.0% (270/370) for the meropenem group (difference, –4.2%; 95% confidence interval, –10.8 to 2.5). The evaluable population demonstrated a clinical cure rate of 77.4% (199/257) in the ceftazidime-avibactam group and 78.1% (211/270) in the meropenem group (–0.7%; 95% CI, –7.9 to 6.4).
The all-cause mortality rate was similar between groups at the test-of-cure date and at day 28. The clinically modified intention-to-treat population demonstrated a mortality of 8.1% vs. 6.8% at the test-of-cure date and 8.4% vs. 7.3% at day 28 for ceftazidime-avibactam and meropenem, respectively.
Adverse events were noted in 75% vs. 74% of patients in the ceftazidime-avibactam groups and meropenem groups, respectively. Most adverse events were rated as mild to moderate and deemed likely unrelated to the treatment.
However, serious adverse events occurred in 19% (n = 75) in the ceftazidime-avibactam group and 13% (n = 54) in the meropenem group. Four serious adverse events were thought to be possibly related to the study drug ceftazidime-avibactam and included diarrhea, acute coronary syndrome, subacute hepatic failure, and abnormal liver function test results. The authors noted the adverse events in the trial were consistent and detected no new safety concerns for ceftazidime-avibactam.
Limitations of the study included an inability to establish the optimal duration of treatment for nosocomial pneumonia treated with meropenem or ceftazidime-avibactam.
“Our results show noninferiority for the treatment of nosocomial pneumonia caused by ceftazidime-nonsusceptible or ceftazidime-susceptible gram-negative aerobic pathogens,” the authors concluded.
The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
SOURCE: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia including ventilator-associated pneumonia from gram-negative organisms, results from the REPROVE trial demonstrated.
Nosocomial or hospital-acquired pneumonia is a common hospital-acquired infection associated with increased cost and mortality. Further, nosocomial pneumonia is associated with gram-negative pathogens such as Pseudomonas aeruginosa and Enterobacteriaceae that may carry extended-spectrum beta-lactamases and carbapenemase, thereby limiting the treatment options. However, ceftazidime-avibactam has both antipseudomonal and extended beta-lactamase coverage for multidrug-resistant gram-negative infections, and may provide an alternative to meropenem.
Antoni Torres, MD, of the University of Barcelona and his colleagues sought to compare the safety and efficacy of ceftazidime-avibactam to meropenem in patients with nosocomial and ventilator-associated pneumonia. The REPROVE study was a phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries. Patients were randomly assigned 1:1 to receive either ceftazidime-avibactam (500-2,000 mg every 8 hours) or meropenem (1,000 mg every 8 hours) with adjustment as needed for renal function.
Participants included in the study were 18-90 years of age with nosocomial pneumonia as evidenced by pneumonia 48 hours or more after admission or within 7 days after discharge from an inpatient facility. Patients with ventilator-associated pneumonia had lung infection within 48 hours of intubation and mechanical ventilation. Sputum culture and gram stains were obtained within 48 hours before randomization, and patients were excluded for evidence of gram-positive–only pathogens or those not expected to respond to meropenem or ceftazidime-avibactam.
The study involved a safety population (808 patients), a clinically modified intention-to-treat population (726), and a clinically evaluable population (527). The intention-to-treat population demonstrated a predominance of Klebsiella pneumoniae (37%), and Pseudomonas aeruginosa (30%); 28% of the intention-to-treat population were identified as not susceptible to ceftazidime.
Overall, the clinically modified intention-to-treat group demonstrated a clinical cure rate of 68.8% (245/356) in the ceftazidime-avibactam and 73.0% (270/370) for the meropenem group (difference, –4.2%; 95% confidence interval, –10.8 to 2.5). The evaluable population demonstrated a clinical cure rate of 77.4% (199/257) in the ceftazidime-avibactam group and 78.1% (211/270) in the meropenem group (–0.7%; 95% CI, –7.9 to 6.4).
The all-cause mortality rate was similar between groups at the test-of-cure date and at day 28. The clinically modified intention-to-treat population demonstrated a mortality of 8.1% vs. 6.8% at the test-of-cure date and 8.4% vs. 7.3% at day 28 for ceftazidime-avibactam and meropenem, respectively.
Adverse events were noted in 75% vs. 74% of patients in the ceftazidime-avibactam groups and meropenem groups, respectively. Most adverse events were rated as mild to moderate and deemed likely unrelated to the treatment.
However, serious adverse events occurred in 19% (n = 75) in the ceftazidime-avibactam group and 13% (n = 54) in the meropenem group. Four serious adverse events were thought to be possibly related to the study drug ceftazidime-avibactam and included diarrhea, acute coronary syndrome, subacute hepatic failure, and abnormal liver function test results. The authors noted the adverse events in the trial were consistent and detected no new safety concerns for ceftazidime-avibactam.
Limitations of the study included an inability to establish the optimal duration of treatment for nosocomial pneumonia treated with meropenem or ceftazidime-avibactam.
“Our results show noninferiority for the treatment of nosocomial pneumonia caused by ceftazidime-nonsusceptible or ceftazidime-susceptible gram-negative aerobic pathogens,” the authors concluded.
The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
SOURCE: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia including ventilator-associated pneumonia from gram-negative organisms, results from the REPROVE trial demonstrated.
Nosocomial or hospital-acquired pneumonia is a common hospital-acquired infection associated with increased cost and mortality. Further, nosocomial pneumonia is associated with gram-negative pathogens such as Pseudomonas aeruginosa and Enterobacteriaceae that may carry extended-spectrum beta-lactamases and carbapenemase, thereby limiting the treatment options. However, ceftazidime-avibactam has both antipseudomonal and extended beta-lactamase coverage for multidrug-resistant gram-negative infections, and may provide an alternative to meropenem.
Antoni Torres, MD, of the University of Barcelona and his colleagues sought to compare the safety and efficacy of ceftazidime-avibactam to meropenem in patients with nosocomial and ventilator-associated pneumonia. The REPROVE study was a phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries. Patients were randomly assigned 1:1 to receive either ceftazidime-avibactam (500-2,000 mg every 8 hours) or meropenem (1,000 mg every 8 hours) with adjustment as needed for renal function.
Participants included in the study were 18-90 years of age with nosocomial pneumonia as evidenced by pneumonia 48 hours or more after admission or within 7 days after discharge from an inpatient facility. Patients with ventilator-associated pneumonia had lung infection within 48 hours of intubation and mechanical ventilation. Sputum culture and gram stains were obtained within 48 hours before randomization, and patients were excluded for evidence of gram-positive–only pathogens or those not expected to respond to meropenem or ceftazidime-avibactam.
The study involved a safety population (808 patients), a clinically modified intention-to-treat population (726), and a clinically evaluable population (527). The intention-to-treat population demonstrated a predominance of Klebsiella pneumoniae (37%), and Pseudomonas aeruginosa (30%); 28% of the intention-to-treat population were identified as not susceptible to ceftazidime.
Overall, the clinically modified intention-to-treat group demonstrated a clinical cure rate of 68.8% (245/356) in the ceftazidime-avibactam and 73.0% (270/370) for the meropenem group (difference, –4.2%; 95% confidence interval, –10.8 to 2.5). The evaluable population demonstrated a clinical cure rate of 77.4% (199/257) in the ceftazidime-avibactam group and 78.1% (211/270) in the meropenem group (–0.7%; 95% CI, –7.9 to 6.4).
The all-cause mortality rate was similar between groups at the test-of-cure date and at day 28. The clinically modified intention-to-treat population demonstrated a mortality of 8.1% vs. 6.8% at the test-of-cure date and 8.4% vs. 7.3% at day 28 for ceftazidime-avibactam and meropenem, respectively.
Adverse events were noted in 75% vs. 74% of patients in the ceftazidime-avibactam groups and meropenem groups, respectively. Most adverse events were rated as mild to moderate and deemed likely unrelated to the treatment.
However, serious adverse events occurred in 19% (n = 75) in the ceftazidime-avibactam group and 13% (n = 54) in the meropenem group. Four serious adverse events were thought to be possibly related to the study drug ceftazidime-avibactam and included diarrhea, acute coronary syndrome, subacute hepatic failure, and abnormal liver function test results. The authors noted the adverse events in the trial were consistent and detected no new safety concerns for ceftazidime-avibactam.
Limitations of the study included an inability to establish the optimal duration of treatment for nosocomial pneumonia treated with meropenem or ceftazidime-avibactam.
“Our results show noninferiority for the treatment of nosocomial pneumonia caused by ceftazidime-nonsusceptible or ceftazidime-susceptible gram-negative aerobic pathogens,” the authors concluded.
The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
SOURCE: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
FROM THE LANCET INFECTIOUS DISEASES
Key clinical point: Ceftazidime-avibactam was noninferior to meropenem for nosocomial pneumonia.
Major finding: The clinically modified intention-to-treat group demonstrated clinical cure rates of 69% and 73% in the ceftazidime-avibactam vs. the meropenem group, respectively.
Data source: A phase 3, double-blind, noninferiority trial performed at 136 centers in 23 countries.
Disclosures: The study was initially funded by AstraZeneca until the rights to ceftazidime-avibactam were acquired by Pfizer. Multiple authors reported financial relationships with AstraZeneca including grant funding, employment, and shareholding.
Source: Torres A et al. Lancet Infect Dis. 2017. doi: 10.1016/S1473-3099(17)30747-8.
Paring the risk of antibiotic resistance
One unintended consequence of the increased attention to early sepsis identification and intervention can be unnecessary or excessive antibiotic use. Overuse of broad-spectrum antibiotics, in turn, can fuel the emergence of life-threatening infections such as antibiotic-resistant Clostridium difficile, a scourge in many hospitals.
For a sepsis quality improvement (QI) initiative at the University of Utah, Salt Lake City, the hospitalist coleaders took several precautions to lessen the risk of antibiotic overuse. Kencee K. Graves, MD, said she and her colleague Devin J. Horton, MD, designed the hospital’s order sets in collaboration with an infectious disease specialist and pharmacist so they could avoid overly broad antibiotics whenever possible. The project also included an educational effort to get pharmacists in the habit of prompting medical providers to initiate antibiotic de-escalation at 48 hours. The hospital had an antibiotic stewardship program that likely helped as well, she said. As a result of their precautions, the team found no significant difference in the amount of broad-spectrum antibiotics doled out before and after their QI pilot project.
Infection control and antimicrobial specialists also can help; they can monitor an area’s resistance profile, create a antibiogram and reevaluate sepsis pathways and order sets to adjust the recommended antibiotics as the resistance profile changes. “I think we still have a long ways to go,” said Andy Odden, MD, SFHM, patient safety officer in the department of medicine at Washington University in St. Louis. “The initial risk of mortality is so much more dramatic than the long-term risks of developing antimicrobial resistors that unless you have the antimicrobial stewardship people with a seat at the table, that voice can get drowned out very easily.”
The antimicrobial stewardship program at University of Pennsylvania, Philadelphia, has received a boost from technology. The program offers initial guidance on which broad-spectrum antibiotics to consider depending on the suspected source of the sepsis-linked infection. Software by Jackson, Wyo.–based biotech company Teqqa also synthesizes the university hospital’s resistance data based on blood, urine, and sputum cultures. “It can predict the antibiotic sensitivity of a given bug growing out of a given culture on a given unit,” said Craig A. Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine at the university.
The bigger issue, Dr. Umscheid said, is when and how to de-escalate antibiotic treatment. “If somebody is feeling better in 48 hours or 72 hours and no cultures have grown back, they have no more fever, and their white counts have normalized, do you start pulling off the antibiotics slowly and, if so, how do you do that?” Several trials are examining such questions, including a multicenter collaboration called DETOURS (De-Escalating Empiric Treatment: Opting-Out of Rx for Selected Patients With Suspected Sepsis). One of the trial’s chief aims is to set up a new opt-out protocol for acute care patients in the wards.
One unintended consequence of the increased attention to early sepsis identification and intervention can be unnecessary or excessive antibiotic use. Overuse of broad-spectrum antibiotics, in turn, can fuel the emergence of life-threatening infections such as antibiotic-resistant Clostridium difficile, a scourge in many hospitals.
For a sepsis quality improvement (QI) initiative at the University of Utah, Salt Lake City, the hospitalist coleaders took several precautions to lessen the risk of antibiotic overuse. Kencee K. Graves, MD, said she and her colleague Devin J. Horton, MD, designed the hospital’s order sets in collaboration with an infectious disease specialist and pharmacist so they could avoid overly broad antibiotics whenever possible. The project also included an educational effort to get pharmacists in the habit of prompting medical providers to initiate antibiotic de-escalation at 48 hours. The hospital had an antibiotic stewardship program that likely helped as well, she said. As a result of their precautions, the team found no significant difference in the amount of broad-spectrum antibiotics doled out before and after their QI pilot project.
Infection control and antimicrobial specialists also can help; they can monitor an area’s resistance profile, create a antibiogram and reevaluate sepsis pathways and order sets to adjust the recommended antibiotics as the resistance profile changes. “I think we still have a long ways to go,” said Andy Odden, MD, SFHM, patient safety officer in the department of medicine at Washington University in St. Louis. “The initial risk of mortality is so much more dramatic than the long-term risks of developing antimicrobial resistors that unless you have the antimicrobial stewardship people with a seat at the table, that voice can get drowned out very easily.”
The antimicrobial stewardship program at University of Pennsylvania, Philadelphia, has received a boost from technology. The program offers initial guidance on which broad-spectrum antibiotics to consider depending on the suspected source of the sepsis-linked infection. Software by Jackson, Wyo.–based biotech company Teqqa also synthesizes the university hospital’s resistance data based on blood, urine, and sputum cultures. “It can predict the antibiotic sensitivity of a given bug growing out of a given culture on a given unit,” said Craig A. Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine at the university.
The bigger issue, Dr. Umscheid said, is when and how to de-escalate antibiotic treatment. “If somebody is feeling better in 48 hours or 72 hours and no cultures have grown back, they have no more fever, and their white counts have normalized, do you start pulling off the antibiotics slowly and, if so, how do you do that?” Several trials are examining such questions, including a multicenter collaboration called DETOURS (De-Escalating Empiric Treatment: Opting-Out of Rx for Selected Patients With Suspected Sepsis). One of the trial’s chief aims is to set up a new opt-out protocol for acute care patients in the wards.
One unintended consequence of the increased attention to early sepsis identification and intervention can be unnecessary or excessive antibiotic use. Overuse of broad-spectrum antibiotics, in turn, can fuel the emergence of life-threatening infections such as antibiotic-resistant Clostridium difficile, a scourge in many hospitals.
For a sepsis quality improvement (QI) initiative at the University of Utah, Salt Lake City, the hospitalist coleaders took several precautions to lessen the risk of antibiotic overuse. Kencee K. Graves, MD, said she and her colleague Devin J. Horton, MD, designed the hospital’s order sets in collaboration with an infectious disease specialist and pharmacist so they could avoid overly broad antibiotics whenever possible. The project also included an educational effort to get pharmacists in the habit of prompting medical providers to initiate antibiotic de-escalation at 48 hours. The hospital had an antibiotic stewardship program that likely helped as well, she said. As a result of their precautions, the team found no significant difference in the amount of broad-spectrum antibiotics doled out before and after their QI pilot project.
Infection control and antimicrobial specialists also can help; they can monitor an area’s resistance profile, create a antibiogram and reevaluate sepsis pathways and order sets to adjust the recommended antibiotics as the resistance profile changes. “I think we still have a long ways to go,” said Andy Odden, MD, SFHM, patient safety officer in the department of medicine at Washington University in St. Louis. “The initial risk of mortality is so much more dramatic than the long-term risks of developing antimicrobial resistors that unless you have the antimicrobial stewardship people with a seat at the table, that voice can get drowned out very easily.”
The antimicrobial stewardship program at University of Pennsylvania, Philadelphia, has received a boost from technology. The program offers initial guidance on which broad-spectrum antibiotics to consider depending on the suspected source of the sepsis-linked infection. Software by Jackson, Wyo.–based biotech company Teqqa also synthesizes the university hospital’s resistance data based on blood, urine, and sputum cultures. “It can predict the antibiotic sensitivity of a given bug growing out of a given culture on a given unit,” said Craig A. Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine at the university.
The bigger issue, Dr. Umscheid said, is when and how to de-escalate antibiotic treatment. “If somebody is feeling better in 48 hours or 72 hours and no cultures have grown back, they have no more fever, and their white counts have normalized, do you start pulling off the antibiotics slowly and, if so, how do you do that?” Several trials are examining such questions, including a multicenter collaboration called DETOURS (De-Escalating Empiric Treatment: Opting-Out of Rx for Selected Patients With Suspected Sepsis). One of the trial’s chief aims is to set up a new opt-out protocol for acute care patients in the wards.
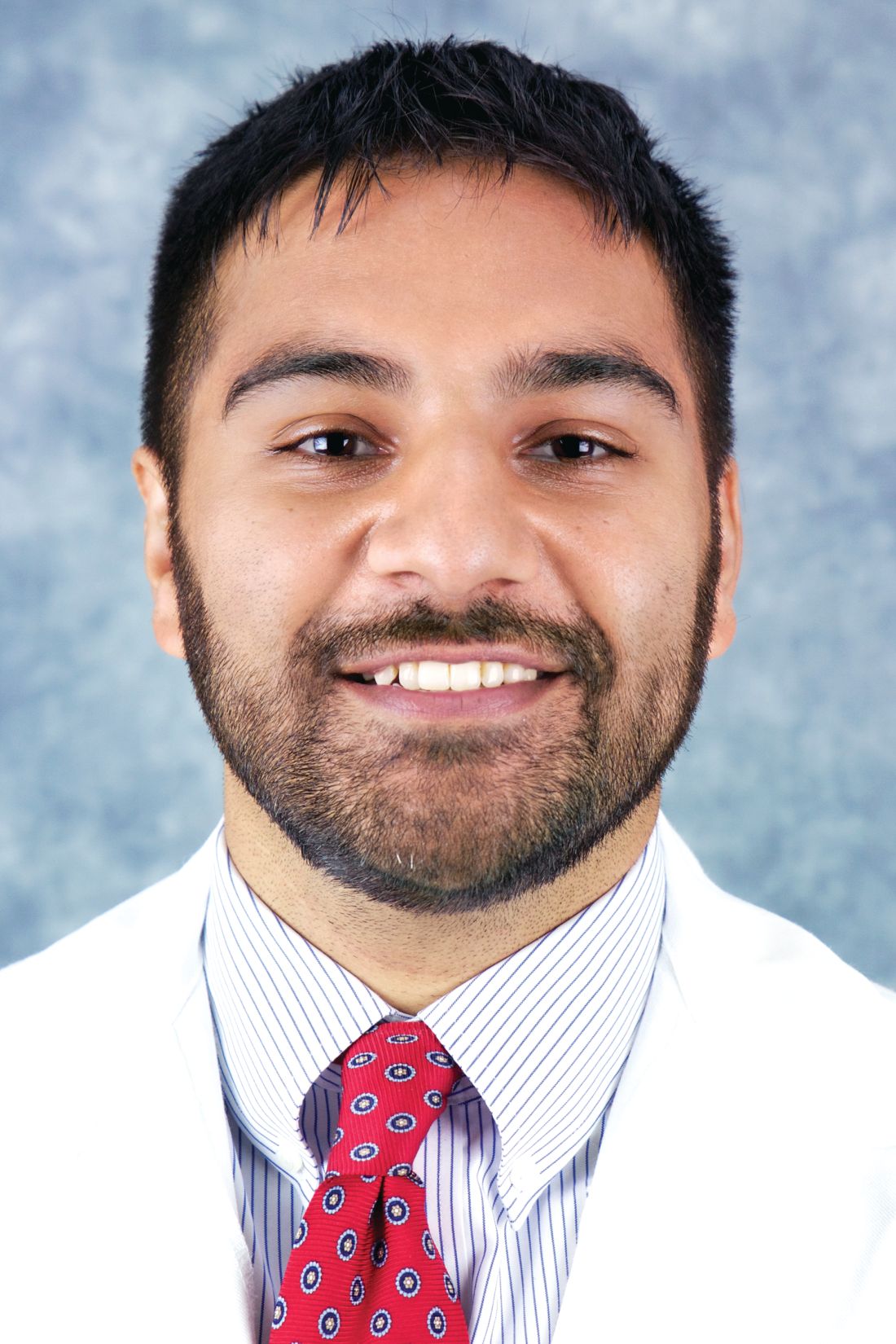
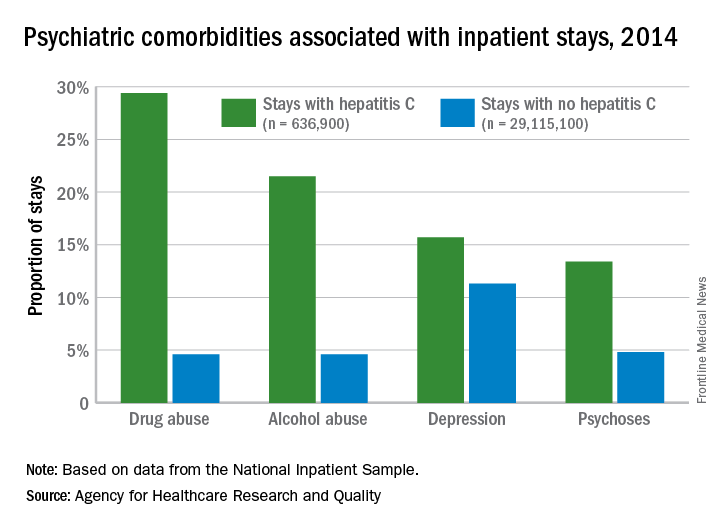
Psychiatric issues common among hepatitis C inpatients
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
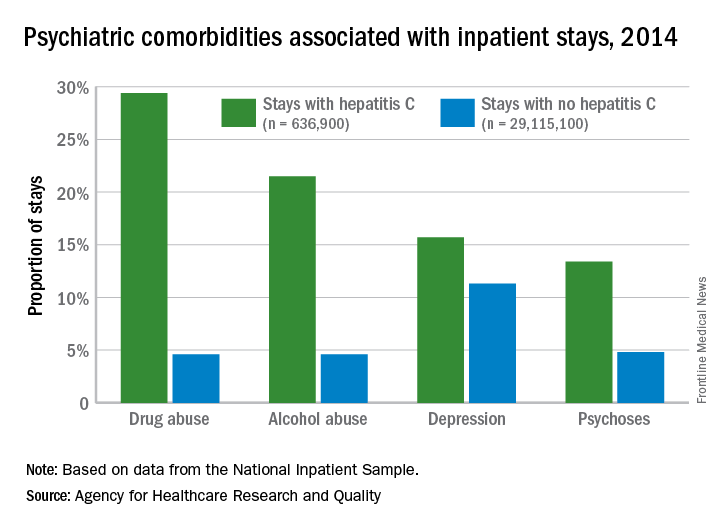
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Adult inpatients with hepatitis C are much more likely to have mental health comorbidities, compared with those who do not have hepatitis C, according to the Agency for Healthcare Research and Quality.
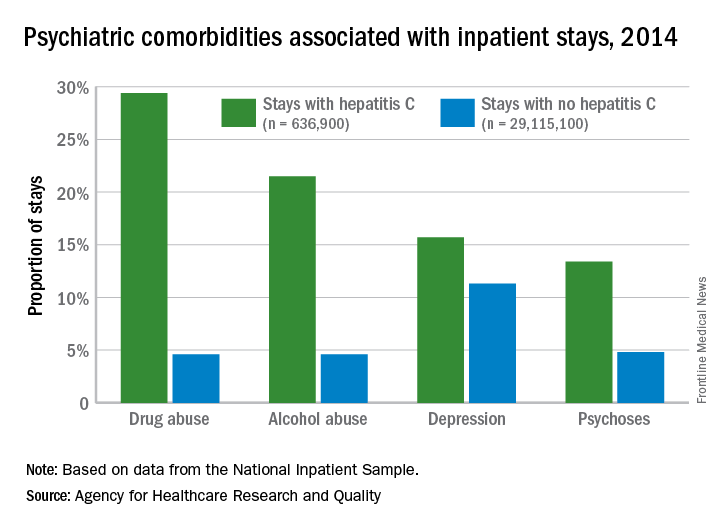
All four comorbidities skewed younger, and the oldest patients (73 years and older) with hepatitis C presented with each condition at about the same rate as the non–hepatitis C population. The proportions of hepatitis C–related inpatient stays with alcohol abuse by age, for example, were 20.5% for 18-51 years, 23.3% for those aged 52-72, and 5.8% for the 73-and-older group, according to data from the National Inpatient Sample, which includes more than 95% of all discharges from community (short-term, nonfederal, nonrehabilitation) hospitals in the United States.
Drug combo indicated for bacterial pneumonia
(Avycaz) to include hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults.
Specifically, the approved indication is for infections caused by certain Gram-negative bacteria – some of which are increasingly resistant to available antibiotics – including, Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, and Haemophilus influenzae.
There have not been new treatment options for HABP/VABP caused by Gram-negative bacteria in more than 15 years, according to Allergan, the drug’s manufacturer.
This is the third approved indication for ceftazidime/avibactam; the other two indications are for complicated intra-abdominal infections (in combination with metronidazole) and for complicated urinary tract infections.
(Avycaz) to include hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults.
Specifically, the approved indication is for infections caused by certain Gram-negative bacteria – some of which are increasingly resistant to available antibiotics – including, Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, and Haemophilus influenzae.
There have not been new treatment options for HABP/VABP caused by Gram-negative bacteria in more than 15 years, according to Allergan, the drug’s manufacturer.
This is the third approved indication for ceftazidime/avibactam; the other two indications are for complicated intra-abdominal infections (in combination with metronidazole) and for complicated urinary tract infections.
(Avycaz) to include hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults.
Specifically, the approved indication is for infections caused by certain Gram-negative bacteria – some of which are increasingly resistant to available antibiotics – including, Klebsiella pneumoniae, Enterobacter cloacae, Escherichia coli, Serratia marcescens, Proteus mirabilis, Pseudomonas aeruginosa, and Haemophilus influenzae.
There have not been new treatment options for HABP/VABP caused by Gram-negative bacteria in more than 15 years, according to Allergan, the drug’s manufacturer.
This is the third approved indication for ceftazidime/avibactam; the other two indications are for complicated intra-abdominal infections (in combination with metronidazole) and for complicated urinary tract infections.
Hospitals filling as flu season worsens
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
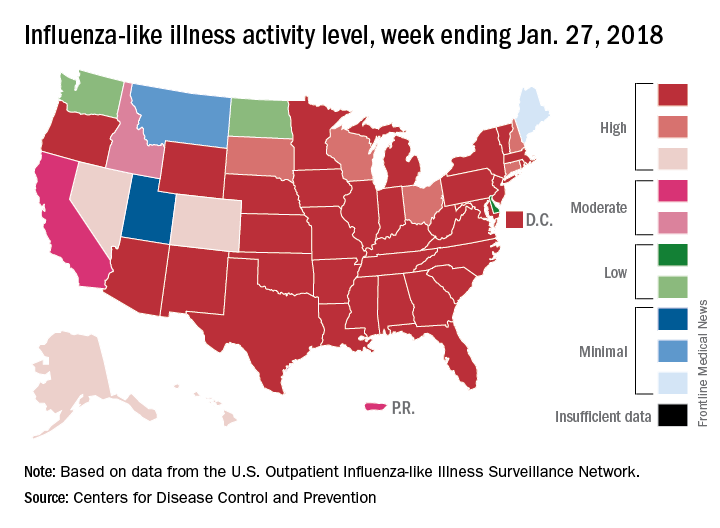
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
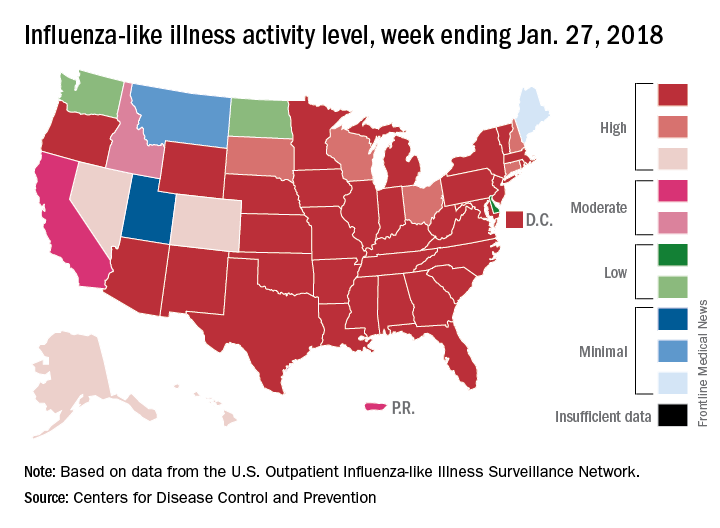
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.
Through the last full week of January, the cumulative “hospitalization rate is the highest we’ve seen,” acting Centers for Disease Control and Prevention director Anne Schuchat, MD, said. For the current season so far, the hospitalization rate stands at 51.4 per 100,000 population, putting it on pace to top the total of 710,000 flu-related admissions that occurred during the 2014-2015 season, she said in a weekly briefing Feb. 2.
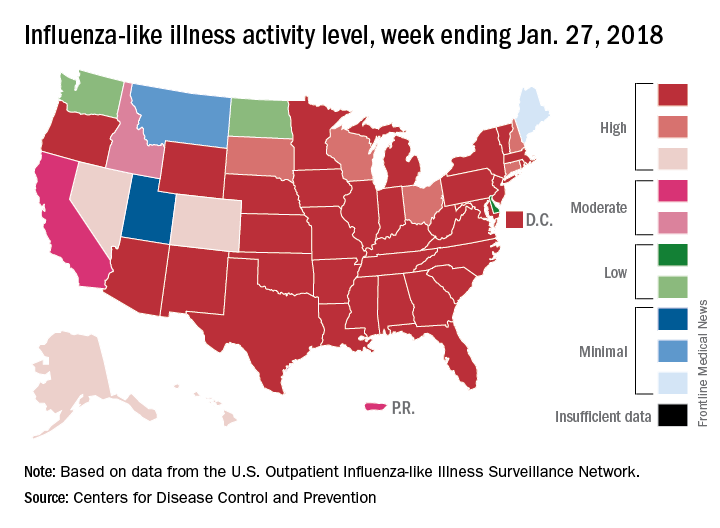
Flu-related pediatric deaths also took a big jump for the week as another 16 were reported, which brings the total for the season to 53. Of the children who have died so far, only 20% were vaccinated, said Dan Jernigan, MD, MPH, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta. He also noted that half of the children who have been hospitalized did not had an underlying condition.
The one bit of good news for the week was that activity in the West seems to be easing up, Dr. Schuchat said. The geographic spread of ILI was reported as widespread in 48 states, which is down from 49 the previous week because Oregon dropped off the list. To go along with that, the ILI activity level in California has dropped 2 weeks in a row and now stands at level 7, the CDC data show.
Making hospital medicine a lifelong, enjoyable, and engaging career
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Amith Skandhan, MD, FHM, a hospitalist, a director/physician liaison for clinical documentation improvement and core faculty member in the Internal Medicine Residency Program at Southeast Alabama Medical Center in Dothan, Ala., and clinical faculty member at the Alabama College of Osteopathic Medicine also in Dothan. Dr. Skandhan is the cofounder and current president of the SHM Wiregrass Chapter and is an active member of SHM’s Annual Conference and Performance Measurement Reporting committees.
When did you join SHM, and what prompted you to apply for your current committee roles?
There were many things that were not sufficiently taught during clinical training that were required in my day-to-day practice, like clinical documentation improvement, practice management, billing, coding, and so forth. I also quickly understood how vast and dynamic hospital medicine really was. While looking for an outlet to voice my questions, concerns, and curiosity, I decided to join SHM, which has helped me find and apply the techniques I’d been looking for to further my career as a hospitalist.
I’m now fortunate to be a part of SHM’s national committees, which involve hospitalists of various backgrounds and experiences, who work together to improve the overall quality of inpatient medicine. I currently serve on the Performance Reporting Measurement Committee and the Annual Conference Committee. My interests in reviewing the ever-evolving policies of health care made me apply to be a part of the Performance Reporting Measurement Committee. We work very closely with the Public Policy Committee, analyzing written policies and subsequently offering our recommendations. It’s been fulfilling to be a part of a committee that works towards developing policies that support a good quality of care on such a large scale.
My penchant for organizing events and bringing people together based on common ground led me to apply for the Annual Conference Committee. We meet every week to discuss various topics, choose and invite speakers, and help organize the entire event, which will host close to 5,000 hospitalists later this year. It has made me appreciate being a member of an organization that provides hospitalists with opportunities for education and growth. I’m hopeful that the attendees next year will find the conference to be a worthwhile experience!
As the president of SHM’s Wiregrass Chapter, how has the chapter grown since its establishment in May 2015?
Our chapter is based in Dothan, a small, rural Alabama town where Southeast Alabama Medical Center is located. The chapter covers the counties of lower Alabama and the panhandle of Florida. We named the chapter after a special species of grass that grows in this region.
When we started the chapter, our goal was to bring the best and brightest of hospital medicine to our region to give talks on hot topics in the field and also to use their expertise to guide inpatient care in our hospital system. We aggressively marketed the events to bring in large crowds of medical professionals, and we consistently average around 70-80 attendees in our meetings. Bringing in leaders from the field helped create an atmosphere of learning and inspired us to grow and develop our hospitalist program. We now closely work with hospital medicine groups in surrounding rural areas toward improving inpatient hospital care.
During these past years, we also realized that, for the further growth of our chapter, we would need to nurture an interest in hospital medicine among future generations of doctors, and this realization led to the creation of our medical student and resident wing. So far, the students have been very enthusiastic about participating in SHM-related events, and I hope that continues. We also developed a mentor-mentee program, in which we paired selected medical students with hospitalists to help guide future careers in acute care medicine. This year, we have also been helping the hospital medicine division at Southeast Alabama Medical Center create a clinical research track for medical students. To that end, we have just completed our second annual poster competition where we presented around 50 posters in the areas of clinical vignettes, quality improvement, and original research.
In addition, the chapter is very active with community activities. We took notice of the fact that many of our patients and community members were unaware of what hospitalists did because they could not understand how our work was different from that of primary care physicians. Our members have therefore participated in TV, radio, and newspaper interviews to help elucidate the role of hospitalists in patient care. We have also periodically visited primary care physician offices, nursing homes, senior citizen groups, and cancer support groups to educate these patients on various facets of health care and how hospitalists influence these areas.
In 2014, we organized a “walk with a hospitalist” event, for which we set up a half-mile “admission to discharge” scenario explaining the role of hospitalists and other departments involved in patient care. This year, in hopes of improving patient literacy in our region, we held a “shop with a doc” event, where the Southeast Alabama Medical Center hospitalists teamed up with dietitians and taught patients how food and lifestyle influenced their chronic medical illnesses. This was followed by physicians and dietitians shopping with patients in the grocery store, educating them on healthy choices and label reading.
We’re incredibly grateful for the support that we’ve received from our medical and patient communities; they’ve been critical in helping our chapter grow as much as it has, and they motivate us to work harder and do more with the chapter. We were honored to receive the SHM’s Rising Star Award at the Hospital Medicine 2017 conference in Las Vegas. We never thought that our little chapter in the American countryside would be chosen, but we’re very thankful to have our efforts recognized on the national stage!
Which SHM conferences have you attended? Tell TH about your most memorable highlights or takeaways.
When I started out as a hospitalist in 2014, I decided to attend the annual conference in Las Vegas, and I can honestly say that conference changed the course of my career. I can still remember listening to the opening speech and realizing that I was surrounded by more than 3,000 hospitalists who understood the power we had to influence inpatient care. I’ve attended all the national conferences since then and am grateful that I now get to help organize the Hospital Medicine 2018 annual conference, also known as HM18.
I had been working to find a way to improve documentation within my group, as well as change the culture and perception towards billing and coding practices, which prompted me to attend the Quality and Safety Educators Academy. During one of the problem-solving sessions, I explained the challenges that I faced to my conference group. The exercise required me to explain the problem at hand, and the players of my group then discussed their thoughts while I took notes. It was a fantastic experience, as the participants at my table offered strong solutions to my problems within a matter of minutes. Their advice led to meaningful changes in our group’s hospital documentation practices, and in turn, I’ve been promoted to physician advisor in Southeast Alabama Medical Center.
After such a great experience at Quality and Safety Educators Academy, I went on to attend SHM’s Leadership Academy, where I had the opportunity to meet some of the top leaders and pioneers in the field of hospital medicine. It’s empowering to be mentored by the very people you look up to and aspire to be like. Not only was I able to bring ideas home to my institution, but I was able to reflect and improve my own professional and personal growth. I’m happy to say that I’ve completed all three levels of Leadership Academy.
As I’ve become involved with the medical student and residency programs at my medical center, I recently attended the Academic Hospitalist Academy to help my transition into academic hospital medicine. Meeting and spending time with the faculty at Academic Hospitalist Academy made me further realize the roles that academic hospitalists play in the education of future physicians, emphasizing the idea that we can all be champions in quality and patient safety.
If you’re looking to advance your career as a hospitalist, take advantage of the conferences that SHM offers. I’ve gained so much from each experience, and I’m looking forward to returning to these conferences as a potential facilitator, in hopes of offering what I’ve learned to hospitalists looking to bring about change in their fields and careers.
What can attendees at HM18 expect to see in the area of career development, and how is this different than previous years?
Hospital medicine is only about 2 decades old, making it one of the youngest branches in medicine today. Given this fact, the Annual Conference Committee feels that it is paramount to focus on career development for both new and midcareer hospitalists alike.
One question that we wish to explore and answer this year is: “How do you make hospital medicine a life-long, enjoyable, and engaging career?” In turn, our committee has created several new additions to HM18. This includes a “Seasoning Your Career” track, which will provide ideas on how to advance in leadership, use emotional intelligence to achieve success, change your roles midcareer, and change hospitalist schedules. Another unique addition this year are career development workshops, which will aim to developing various aspects of a hospitalist’s career, such as working on leadership skills, refining presentation and communication skills, providing constructive feedback, promoting women in hospital medicine, preventing burnout, and turning ideas into clinical research. We also plan to incorporate an education track, which will focus on how hospitalists can expand their careers towards educational leadership.
Given your involvement in SHM at both the local and national levels, do you have any advice for young hospital medicine professionals looking to build their professional profiles?
I’ve frequently noticed that young hospitalists don’t realize the potential influence they hold within their own institutions or the power they have to elicit change in health care at the national level.
Though we don’t often admit it, some hospitalists feel like they are glorified residents, which definitely is not the case. As a provider on the front lines, you have the unique opportunity to implement changes pertaining to issues of cost, utilization of resources, process management, quality and patient safety, and bottlenecks in care, to name a few. These are issues that keep the administrators of your organization and leaders of hospital medicine up at night. Don’t sit around and complain about how things could be or should be; look toward creating change. Bring up possible solutions to these problems with your leaders. They will appreciate the effort, and hopefully together you can find ways to tackle these problems.
I will conclude by saying this: Hospital medicine is such a unique specialty in that it’s constantly evolving, and the pioneers of this field are still alive and practicing medicine. You can meet and interact with them during the SHM conferences and look to them as sources of inspiration or guidance. Meeting people you look up to and having them as your mentors can take you places.
Ms. Steele is the marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Amith Skandhan, MD, FHM, a hospitalist, a director/physician liaison for clinical documentation improvement and core faculty member in the Internal Medicine Residency Program at Southeast Alabama Medical Center in Dothan, Ala., and clinical faculty member at the Alabama College of Osteopathic Medicine also in Dothan. Dr. Skandhan is the cofounder and current president of the SHM Wiregrass Chapter and is an active member of SHM’s Annual Conference and Performance Measurement Reporting committees.
When did you join SHM, and what prompted you to apply for your current committee roles?
There were many things that were not sufficiently taught during clinical training that were required in my day-to-day practice, like clinical documentation improvement, practice management, billing, coding, and so forth. I also quickly understood how vast and dynamic hospital medicine really was. While looking for an outlet to voice my questions, concerns, and curiosity, I decided to join SHM, which has helped me find and apply the techniques I’d been looking for to further my career as a hospitalist.
I’m now fortunate to be a part of SHM’s national committees, which involve hospitalists of various backgrounds and experiences, who work together to improve the overall quality of inpatient medicine. I currently serve on the Performance Reporting Measurement Committee and the Annual Conference Committee. My interests in reviewing the ever-evolving policies of health care made me apply to be a part of the Performance Reporting Measurement Committee. We work very closely with the Public Policy Committee, analyzing written policies and subsequently offering our recommendations. It’s been fulfilling to be a part of a committee that works towards developing policies that support a good quality of care on such a large scale.
My penchant for organizing events and bringing people together based on common ground led me to apply for the Annual Conference Committee. We meet every week to discuss various topics, choose and invite speakers, and help organize the entire event, which will host close to 5,000 hospitalists later this year. It has made me appreciate being a member of an organization that provides hospitalists with opportunities for education and growth. I’m hopeful that the attendees next year will find the conference to be a worthwhile experience!
As the president of SHM’s Wiregrass Chapter, how has the chapter grown since its establishment in May 2015?
Our chapter is based in Dothan, a small, rural Alabama town where Southeast Alabama Medical Center is located. The chapter covers the counties of lower Alabama and the panhandle of Florida. We named the chapter after a special species of grass that grows in this region.
When we started the chapter, our goal was to bring the best and brightest of hospital medicine to our region to give talks on hot topics in the field and also to use their expertise to guide inpatient care in our hospital system. We aggressively marketed the events to bring in large crowds of medical professionals, and we consistently average around 70-80 attendees in our meetings. Bringing in leaders from the field helped create an atmosphere of learning and inspired us to grow and develop our hospitalist program. We now closely work with hospital medicine groups in surrounding rural areas toward improving inpatient hospital care.
During these past years, we also realized that, for the further growth of our chapter, we would need to nurture an interest in hospital medicine among future generations of doctors, and this realization led to the creation of our medical student and resident wing. So far, the students have been very enthusiastic about participating in SHM-related events, and I hope that continues. We also developed a mentor-mentee program, in which we paired selected medical students with hospitalists to help guide future careers in acute care medicine. This year, we have also been helping the hospital medicine division at Southeast Alabama Medical Center create a clinical research track for medical students. To that end, we have just completed our second annual poster competition where we presented around 50 posters in the areas of clinical vignettes, quality improvement, and original research.
In addition, the chapter is very active with community activities. We took notice of the fact that many of our patients and community members were unaware of what hospitalists did because they could not understand how our work was different from that of primary care physicians. Our members have therefore participated in TV, radio, and newspaper interviews to help elucidate the role of hospitalists in patient care. We have also periodically visited primary care physician offices, nursing homes, senior citizen groups, and cancer support groups to educate these patients on various facets of health care and how hospitalists influence these areas.
In 2014, we organized a “walk with a hospitalist” event, for which we set up a half-mile “admission to discharge” scenario explaining the role of hospitalists and other departments involved in patient care. This year, in hopes of improving patient literacy in our region, we held a “shop with a doc” event, where the Southeast Alabama Medical Center hospitalists teamed up with dietitians and taught patients how food and lifestyle influenced their chronic medical illnesses. This was followed by physicians and dietitians shopping with patients in the grocery store, educating them on healthy choices and label reading.
We’re incredibly grateful for the support that we’ve received from our medical and patient communities; they’ve been critical in helping our chapter grow as much as it has, and they motivate us to work harder and do more with the chapter. We were honored to receive the SHM’s Rising Star Award at the Hospital Medicine 2017 conference in Las Vegas. We never thought that our little chapter in the American countryside would be chosen, but we’re very thankful to have our efforts recognized on the national stage!
Which SHM conferences have you attended? Tell TH about your most memorable highlights or takeaways.
When I started out as a hospitalist in 2014, I decided to attend the annual conference in Las Vegas, and I can honestly say that conference changed the course of my career. I can still remember listening to the opening speech and realizing that I was surrounded by more than 3,000 hospitalists who understood the power we had to influence inpatient care. I’ve attended all the national conferences since then and am grateful that I now get to help organize the Hospital Medicine 2018 annual conference, also known as HM18.
I had been working to find a way to improve documentation within my group, as well as change the culture and perception towards billing and coding practices, which prompted me to attend the Quality and Safety Educators Academy. During one of the problem-solving sessions, I explained the challenges that I faced to my conference group. The exercise required me to explain the problem at hand, and the players of my group then discussed their thoughts while I took notes. It was a fantastic experience, as the participants at my table offered strong solutions to my problems within a matter of minutes. Their advice led to meaningful changes in our group’s hospital documentation practices, and in turn, I’ve been promoted to physician advisor in Southeast Alabama Medical Center.
After such a great experience at Quality and Safety Educators Academy, I went on to attend SHM’s Leadership Academy, where I had the opportunity to meet some of the top leaders and pioneers in the field of hospital medicine. It’s empowering to be mentored by the very people you look up to and aspire to be like. Not only was I able to bring ideas home to my institution, but I was able to reflect and improve my own professional and personal growth. I’m happy to say that I’ve completed all three levels of Leadership Academy.
As I’ve become involved with the medical student and residency programs at my medical center, I recently attended the Academic Hospitalist Academy to help my transition into academic hospital medicine. Meeting and spending time with the faculty at Academic Hospitalist Academy made me further realize the roles that academic hospitalists play in the education of future physicians, emphasizing the idea that we can all be champions in quality and patient safety.
If you’re looking to advance your career as a hospitalist, take advantage of the conferences that SHM offers. I’ve gained so much from each experience, and I’m looking forward to returning to these conferences as a potential facilitator, in hopes of offering what I’ve learned to hospitalists looking to bring about change in their fields and careers.
What can attendees at HM18 expect to see in the area of career development, and how is this different than previous years?
Hospital medicine is only about 2 decades old, making it one of the youngest branches in medicine today. Given this fact, the Annual Conference Committee feels that it is paramount to focus on career development for both new and midcareer hospitalists alike.
One question that we wish to explore and answer this year is: “How do you make hospital medicine a life-long, enjoyable, and engaging career?” In turn, our committee has created several new additions to HM18. This includes a “Seasoning Your Career” track, which will provide ideas on how to advance in leadership, use emotional intelligence to achieve success, change your roles midcareer, and change hospitalist schedules. Another unique addition this year are career development workshops, which will aim to developing various aspects of a hospitalist’s career, such as working on leadership skills, refining presentation and communication skills, providing constructive feedback, promoting women in hospital medicine, preventing burnout, and turning ideas into clinical research. We also plan to incorporate an education track, which will focus on how hospitalists can expand their careers towards educational leadership.
Given your involvement in SHM at both the local and national levels, do you have any advice for young hospital medicine professionals looking to build their professional profiles?
I’ve frequently noticed that young hospitalists don’t realize the potential influence they hold within their own institutions or the power they have to elicit change in health care at the national level.
Though we don’t often admit it, some hospitalists feel like they are glorified residents, which definitely is not the case. As a provider on the front lines, you have the unique opportunity to implement changes pertaining to issues of cost, utilization of resources, process management, quality and patient safety, and bottlenecks in care, to name a few. These are issues that keep the administrators of your organization and leaders of hospital medicine up at night. Don’t sit around and complain about how things could be or should be; look toward creating change. Bring up possible solutions to these problems with your leaders. They will appreciate the effort, and hopefully together you can find ways to tackle these problems.
I will conclude by saying this: Hospital medicine is such a unique specialty in that it’s constantly evolving, and the pioneers of this field are still alive and practicing medicine. You can meet and interact with them during the SHM conferences and look to them as sources of inspiration or guidance. Meeting people you look up to and having them as your mentors can take you places.
Ms. Steele is the marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Amith Skandhan, MD, FHM, a hospitalist, a director/physician liaison for clinical documentation improvement and core faculty member in the Internal Medicine Residency Program at Southeast Alabama Medical Center in Dothan, Ala., and clinical faculty member at the Alabama College of Osteopathic Medicine also in Dothan. Dr. Skandhan is the cofounder and current president of the SHM Wiregrass Chapter and is an active member of SHM’s Annual Conference and Performance Measurement Reporting committees.
When did you join SHM, and what prompted you to apply for your current committee roles?
There were many things that were not sufficiently taught during clinical training that were required in my day-to-day practice, like clinical documentation improvement, practice management, billing, coding, and so forth. I also quickly understood how vast and dynamic hospital medicine really was. While looking for an outlet to voice my questions, concerns, and curiosity, I decided to join SHM, which has helped me find and apply the techniques I’d been looking for to further my career as a hospitalist.
I’m now fortunate to be a part of SHM’s national committees, which involve hospitalists of various backgrounds and experiences, who work together to improve the overall quality of inpatient medicine. I currently serve on the Performance Reporting Measurement Committee and the Annual Conference Committee. My interests in reviewing the ever-evolving policies of health care made me apply to be a part of the Performance Reporting Measurement Committee. We work very closely with the Public Policy Committee, analyzing written policies and subsequently offering our recommendations. It’s been fulfilling to be a part of a committee that works towards developing policies that support a good quality of care on such a large scale.
My penchant for organizing events and bringing people together based on common ground led me to apply for the Annual Conference Committee. We meet every week to discuss various topics, choose and invite speakers, and help organize the entire event, which will host close to 5,000 hospitalists later this year. It has made me appreciate being a member of an organization that provides hospitalists with opportunities for education and growth. I’m hopeful that the attendees next year will find the conference to be a worthwhile experience!
As the president of SHM’s Wiregrass Chapter, how has the chapter grown since its establishment in May 2015?
Our chapter is based in Dothan, a small, rural Alabama town where Southeast Alabama Medical Center is located. The chapter covers the counties of lower Alabama and the panhandle of Florida. We named the chapter after a special species of grass that grows in this region.
When we started the chapter, our goal was to bring the best and brightest of hospital medicine to our region to give talks on hot topics in the field and also to use their expertise to guide inpatient care in our hospital system. We aggressively marketed the events to bring in large crowds of medical professionals, and we consistently average around 70-80 attendees in our meetings. Bringing in leaders from the field helped create an atmosphere of learning and inspired us to grow and develop our hospitalist program. We now closely work with hospital medicine groups in surrounding rural areas toward improving inpatient hospital care.
During these past years, we also realized that, for the further growth of our chapter, we would need to nurture an interest in hospital medicine among future generations of doctors, and this realization led to the creation of our medical student and resident wing. So far, the students have been very enthusiastic about participating in SHM-related events, and I hope that continues. We also developed a mentor-mentee program, in which we paired selected medical students with hospitalists to help guide future careers in acute care medicine. This year, we have also been helping the hospital medicine division at Southeast Alabama Medical Center create a clinical research track for medical students. To that end, we have just completed our second annual poster competition where we presented around 50 posters in the areas of clinical vignettes, quality improvement, and original research.
In addition, the chapter is very active with community activities. We took notice of the fact that many of our patients and community members were unaware of what hospitalists did because they could not understand how our work was different from that of primary care physicians. Our members have therefore participated in TV, radio, and newspaper interviews to help elucidate the role of hospitalists in patient care. We have also periodically visited primary care physician offices, nursing homes, senior citizen groups, and cancer support groups to educate these patients on various facets of health care and how hospitalists influence these areas.
In 2014, we organized a “walk with a hospitalist” event, for which we set up a half-mile “admission to discharge” scenario explaining the role of hospitalists and other departments involved in patient care. This year, in hopes of improving patient literacy in our region, we held a “shop with a doc” event, where the Southeast Alabama Medical Center hospitalists teamed up with dietitians and taught patients how food and lifestyle influenced their chronic medical illnesses. This was followed by physicians and dietitians shopping with patients in the grocery store, educating them on healthy choices and label reading.
We’re incredibly grateful for the support that we’ve received from our medical and patient communities; they’ve been critical in helping our chapter grow as much as it has, and they motivate us to work harder and do more with the chapter. We were honored to receive the SHM’s Rising Star Award at the Hospital Medicine 2017 conference in Las Vegas. We never thought that our little chapter in the American countryside would be chosen, but we’re very thankful to have our efforts recognized on the national stage!
Which SHM conferences have you attended? Tell TH about your most memorable highlights or takeaways.
When I started out as a hospitalist in 2014, I decided to attend the annual conference in Las Vegas, and I can honestly say that conference changed the course of my career. I can still remember listening to the opening speech and realizing that I was surrounded by more than 3,000 hospitalists who understood the power we had to influence inpatient care. I’ve attended all the national conferences since then and am grateful that I now get to help organize the Hospital Medicine 2018 annual conference, also known as HM18.
I had been working to find a way to improve documentation within my group, as well as change the culture and perception towards billing and coding practices, which prompted me to attend the Quality and Safety Educators Academy. During one of the problem-solving sessions, I explained the challenges that I faced to my conference group. The exercise required me to explain the problem at hand, and the players of my group then discussed their thoughts while I took notes. It was a fantastic experience, as the participants at my table offered strong solutions to my problems within a matter of minutes. Their advice led to meaningful changes in our group’s hospital documentation practices, and in turn, I’ve been promoted to physician advisor in Southeast Alabama Medical Center.
After such a great experience at Quality and Safety Educators Academy, I went on to attend SHM’s Leadership Academy, where I had the opportunity to meet some of the top leaders and pioneers in the field of hospital medicine. It’s empowering to be mentored by the very people you look up to and aspire to be like. Not only was I able to bring ideas home to my institution, but I was able to reflect and improve my own professional and personal growth. I’m happy to say that I’ve completed all three levels of Leadership Academy.
As I’ve become involved with the medical student and residency programs at my medical center, I recently attended the Academic Hospitalist Academy to help my transition into academic hospital medicine. Meeting and spending time with the faculty at Academic Hospitalist Academy made me further realize the roles that academic hospitalists play in the education of future physicians, emphasizing the idea that we can all be champions in quality and patient safety.
If you’re looking to advance your career as a hospitalist, take advantage of the conferences that SHM offers. I’ve gained so much from each experience, and I’m looking forward to returning to these conferences as a potential facilitator, in hopes of offering what I’ve learned to hospitalists looking to bring about change in their fields and careers.
What can attendees at HM18 expect to see in the area of career development, and how is this different than previous years?
Hospital medicine is only about 2 decades old, making it one of the youngest branches in medicine today. Given this fact, the Annual Conference Committee feels that it is paramount to focus on career development for both new and midcareer hospitalists alike.
One question that we wish to explore and answer this year is: “How do you make hospital medicine a life-long, enjoyable, and engaging career?” In turn, our committee has created several new additions to HM18. This includes a “Seasoning Your Career” track, which will provide ideas on how to advance in leadership, use emotional intelligence to achieve success, change your roles midcareer, and change hospitalist schedules. Another unique addition this year are career development workshops, which will aim to developing various aspects of a hospitalist’s career, such as working on leadership skills, refining presentation and communication skills, providing constructive feedback, promoting women in hospital medicine, preventing burnout, and turning ideas into clinical research. We also plan to incorporate an education track, which will focus on how hospitalists can expand their careers towards educational leadership.
Given your involvement in SHM at both the local and national levels, do you have any advice for young hospital medicine professionals looking to build their professional profiles?
I’ve frequently noticed that young hospitalists don’t realize the potential influence they hold within their own institutions or the power they have to elicit change in health care at the national level.
Though we don’t often admit it, some hospitalists feel like they are glorified residents, which definitely is not the case. As a provider on the front lines, you have the unique opportunity to implement changes pertaining to issues of cost, utilization of resources, process management, quality and patient safety, and bottlenecks in care, to name a few. These are issues that keep the administrators of your organization and leaders of hospital medicine up at night. Don’t sit around and complain about how things could be or should be; look toward creating change. Bring up possible solutions to these problems with your leaders. They will appreciate the effort, and hopefully together you can find ways to tackle these problems.
I will conclude by saying this: Hospital medicine is such a unique specialty in that it’s constantly evolving, and the pioneers of this field are still alive and practicing medicine. You can meet and interact with them during the SHM conferences and look to them as sources of inspiration or guidance. Meeting people you look up to and having them as your mentors can take you places.
Ms. Steele is the marketing communications specialist at the Society of Hospital Medicine.