User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Special interest groups drive SHM engagement
As a professional society supporting an increasingly diverse membership base, SHM is perpetually challenged to create an environment that offers relevance and community to all. While the broad hospital medicine population and SHM are focused on the same goals – optimizing patient care and the system that delivers it – there are nuances within membership that require specific networks and platforms to build this environment of community.
SHM relies on both staff and volunteers to be an engine for leadership, innovation, and labor. Its volunteer corps is essential to delivering value to members and setting the strategic agenda for hospital medicine’s future. Over the last year, SHM has attempted to expand the infrastructure and opportunity for volunteer leadership by examining new approaches to allow pockets of membership to have their own voice. During the year to come, members will continue to help staff forge a new landscape for constituency engagement.
If you are a current volunteer leader, were interested in pursuing volunteer opportunities this past fall, or have simply been navigating SHM’s new website, you may be aware that the Committee structure has changed. There is also new publicity for things called “Special Interest Groups.” Many of our constituency-based Committees are in the process of transforming into Special Interest Groups, which will be officially launched during SHM’s Annual Conference in Orlando in April. They are adopting a more visible charge to create the most accessible and influence-able environment for the entire SHM community.
Committee-to-Special Interest Group transition is about both philosophy and mechanics. It aims to ensure that each constituency group can be readily shaped by the entire population it represents, and will work to create the infrastructure to facilitate that. SHM envisions Special Interest Groups being primary influencers over future content-development and policy objectives; their online communities serving as the principal means for socialization and dialogue around proposed ideas and initiatives. To that end, SHM invested in an entirely new platform for Hospital Medicine Exchange (HMX). If you have yet to explore the new HMX and opportunities for niche networking, visit www.hmxchange.org.
We have also developed a new governance model to encourage interactions between volunteer groups. While there is overlap within Committee and Special Interest Group constructs and likely many volunteers serving in both spheres, it is important to create parallel environments with discreet charges around function and membership engagement. As we continue to roll out the changes, we will rely on volunteers and members at large to help us best realize our intent.
During this transformation, existing volunteers are working with staff to determine the future. There will be some differences in the way Committees and Special Interest Groups function. The differences will be deliberate and designed to provide for fluid and thoughtful administration of business and membership engagement. There will also be consistent communication between Special Interest Groups and strategic and functional Committees with ongoing charges and oversight of existing SHM programs.
Special Interest Groups will have dedicated staff liaisons and volunteer leadership councils. Transforming Committees’ current volunteers will serve as inaugural council leaders with the process for future election being developed in concert by staff and volunteers over the next several months. Special Interest Group membership is open and free to all active SHM members. All current Special Interest Groups will facilitate live Special Interest Forums during SHM’s Annual Conference. If you attend Hospital Medicine 2018 in April, stop by these Special Interest Group Forums on the following topics to learn more:
• Advocacy and Public Policy
• Care for Vulnerable Populations
• Critical Care Medicine
• Health care Information Technology
• Hospitalists Trained in Family Medicine
• Med-Peds Hospitalists
• Multi-Site Hospital Leaders
• Nurse Practitioners and Physician Assistants
• Palliative Care
• Pediatric Hospitalists
• Perioperative Medicine
• Point of Care Ultrasound
• Practice Administrators/Practice Management
• Quality Improvement
• Medical Students and Residents
• Rural Hospitalists
Summaries of the live forums will be posted on corresponding HMX communities after the conference, complete with open comment periods for discussion. There will be an open application period during summer 2018 for new Special Interest Groups not defined above. The SHM Board will review applications in September 2018, and newly established groups will be convened in October to begin building HMX communities, confirming volunteer leader councils, and charting their course with a dedicated staff liaison.
The intent is simple – to provide an open-access mechanism for membership at large to collaborate amongst themselves, offer perspective, and validate or challenge SHM’s proposed initiatives and direction. Special Interest Groups and Committees alike are – and will be – an essential part of SHM’s future – as developers of content, voices of the populations we serve, and an apparatus for the implementation of our shared mission and vision.
SHM exists to serve its members and help them deliver exceptional patient care. We are always interested in your perspective and feedback. To offer your thoughts and ideas about Special Interest Groups or anything else related to membership, please email [email protected].
Mr. Gray is vice president of membership at the Society of Hospital Medicine.
As a professional society supporting an increasingly diverse membership base, SHM is perpetually challenged to create an environment that offers relevance and community to all. While the broad hospital medicine population and SHM are focused on the same goals – optimizing patient care and the system that delivers it – there are nuances within membership that require specific networks and platforms to build this environment of community.
SHM relies on both staff and volunteers to be an engine for leadership, innovation, and labor. Its volunteer corps is essential to delivering value to members and setting the strategic agenda for hospital medicine’s future. Over the last year, SHM has attempted to expand the infrastructure and opportunity for volunteer leadership by examining new approaches to allow pockets of membership to have their own voice. During the year to come, members will continue to help staff forge a new landscape for constituency engagement.
If you are a current volunteer leader, were interested in pursuing volunteer opportunities this past fall, or have simply been navigating SHM’s new website, you may be aware that the Committee structure has changed. There is also new publicity for things called “Special Interest Groups.” Many of our constituency-based Committees are in the process of transforming into Special Interest Groups, which will be officially launched during SHM’s Annual Conference in Orlando in April. They are adopting a more visible charge to create the most accessible and influence-able environment for the entire SHM community.
Committee-to-Special Interest Group transition is about both philosophy and mechanics. It aims to ensure that each constituency group can be readily shaped by the entire population it represents, and will work to create the infrastructure to facilitate that. SHM envisions Special Interest Groups being primary influencers over future content-development and policy objectives; their online communities serving as the principal means for socialization and dialogue around proposed ideas and initiatives. To that end, SHM invested in an entirely new platform for Hospital Medicine Exchange (HMX). If you have yet to explore the new HMX and opportunities for niche networking, visit www.hmxchange.org.
We have also developed a new governance model to encourage interactions between volunteer groups. While there is overlap within Committee and Special Interest Group constructs and likely many volunteers serving in both spheres, it is important to create parallel environments with discreet charges around function and membership engagement. As we continue to roll out the changes, we will rely on volunteers and members at large to help us best realize our intent.
During this transformation, existing volunteers are working with staff to determine the future. There will be some differences in the way Committees and Special Interest Groups function. The differences will be deliberate and designed to provide for fluid and thoughtful administration of business and membership engagement. There will also be consistent communication between Special Interest Groups and strategic and functional Committees with ongoing charges and oversight of existing SHM programs.
Special Interest Groups will have dedicated staff liaisons and volunteer leadership councils. Transforming Committees’ current volunteers will serve as inaugural council leaders with the process for future election being developed in concert by staff and volunteers over the next several months. Special Interest Group membership is open and free to all active SHM members. All current Special Interest Groups will facilitate live Special Interest Forums during SHM’s Annual Conference. If you attend Hospital Medicine 2018 in April, stop by these Special Interest Group Forums on the following topics to learn more:
• Advocacy and Public Policy
• Care for Vulnerable Populations
• Critical Care Medicine
• Health care Information Technology
• Hospitalists Trained in Family Medicine
• Med-Peds Hospitalists
• Multi-Site Hospital Leaders
• Nurse Practitioners and Physician Assistants
• Palliative Care
• Pediatric Hospitalists
• Perioperative Medicine
• Point of Care Ultrasound
• Practice Administrators/Practice Management
• Quality Improvement
• Medical Students and Residents
• Rural Hospitalists
Summaries of the live forums will be posted on corresponding HMX communities after the conference, complete with open comment periods for discussion. There will be an open application period during summer 2018 for new Special Interest Groups not defined above. The SHM Board will review applications in September 2018, and newly established groups will be convened in October to begin building HMX communities, confirming volunteer leader councils, and charting their course with a dedicated staff liaison.
The intent is simple – to provide an open-access mechanism for membership at large to collaborate amongst themselves, offer perspective, and validate or challenge SHM’s proposed initiatives and direction. Special Interest Groups and Committees alike are – and will be – an essential part of SHM’s future – as developers of content, voices of the populations we serve, and an apparatus for the implementation of our shared mission and vision.
SHM exists to serve its members and help them deliver exceptional patient care. We are always interested in your perspective and feedback. To offer your thoughts and ideas about Special Interest Groups or anything else related to membership, please email [email protected].
Mr. Gray is vice president of membership at the Society of Hospital Medicine.
As a professional society supporting an increasingly diverse membership base, SHM is perpetually challenged to create an environment that offers relevance and community to all. While the broad hospital medicine population and SHM are focused on the same goals – optimizing patient care and the system that delivers it – there are nuances within membership that require specific networks and platforms to build this environment of community.
SHM relies on both staff and volunteers to be an engine for leadership, innovation, and labor. Its volunteer corps is essential to delivering value to members and setting the strategic agenda for hospital medicine’s future. Over the last year, SHM has attempted to expand the infrastructure and opportunity for volunteer leadership by examining new approaches to allow pockets of membership to have their own voice. During the year to come, members will continue to help staff forge a new landscape for constituency engagement.
If you are a current volunteer leader, were interested in pursuing volunteer opportunities this past fall, or have simply been navigating SHM’s new website, you may be aware that the Committee structure has changed. There is also new publicity for things called “Special Interest Groups.” Many of our constituency-based Committees are in the process of transforming into Special Interest Groups, which will be officially launched during SHM’s Annual Conference in Orlando in April. They are adopting a more visible charge to create the most accessible and influence-able environment for the entire SHM community.
Committee-to-Special Interest Group transition is about both philosophy and mechanics. It aims to ensure that each constituency group can be readily shaped by the entire population it represents, and will work to create the infrastructure to facilitate that. SHM envisions Special Interest Groups being primary influencers over future content-development and policy objectives; their online communities serving as the principal means for socialization and dialogue around proposed ideas and initiatives. To that end, SHM invested in an entirely new platform for Hospital Medicine Exchange (HMX). If you have yet to explore the new HMX and opportunities for niche networking, visit www.hmxchange.org.
We have also developed a new governance model to encourage interactions between volunteer groups. While there is overlap within Committee and Special Interest Group constructs and likely many volunteers serving in both spheres, it is important to create parallel environments with discreet charges around function and membership engagement. As we continue to roll out the changes, we will rely on volunteers and members at large to help us best realize our intent.
During this transformation, existing volunteers are working with staff to determine the future. There will be some differences in the way Committees and Special Interest Groups function. The differences will be deliberate and designed to provide for fluid and thoughtful administration of business and membership engagement. There will also be consistent communication between Special Interest Groups and strategic and functional Committees with ongoing charges and oversight of existing SHM programs.
Special Interest Groups will have dedicated staff liaisons and volunteer leadership councils. Transforming Committees’ current volunteers will serve as inaugural council leaders with the process for future election being developed in concert by staff and volunteers over the next several months. Special Interest Group membership is open and free to all active SHM members. All current Special Interest Groups will facilitate live Special Interest Forums during SHM’s Annual Conference. If you attend Hospital Medicine 2018 in April, stop by these Special Interest Group Forums on the following topics to learn more:
• Advocacy and Public Policy
• Care for Vulnerable Populations
• Critical Care Medicine
• Health care Information Technology
• Hospitalists Trained in Family Medicine
• Med-Peds Hospitalists
• Multi-Site Hospital Leaders
• Nurse Practitioners and Physician Assistants
• Palliative Care
• Pediatric Hospitalists
• Perioperative Medicine
• Point of Care Ultrasound
• Practice Administrators/Practice Management
• Quality Improvement
• Medical Students and Residents
• Rural Hospitalists
Summaries of the live forums will be posted on corresponding HMX communities after the conference, complete with open comment periods for discussion. There will be an open application period during summer 2018 for new Special Interest Groups not defined above. The SHM Board will review applications in September 2018, and newly established groups will be convened in October to begin building HMX communities, confirming volunteer leader councils, and charting their course with a dedicated staff liaison.
The intent is simple – to provide an open-access mechanism for membership at large to collaborate amongst themselves, offer perspective, and validate or challenge SHM’s proposed initiatives and direction. Special Interest Groups and Committees alike are – and will be – an essential part of SHM’s future – as developers of content, voices of the populations we serve, and an apparatus for the implementation of our shared mission and vision.
SHM exists to serve its members and help them deliver exceptional patient care. We are always interested in your perspective and feedback. To offer your thoughts and ideas about Special Interest Groups or anything else related to membership, please email [email protected].
Mr. Gray is vice president of membership at the Society of Hospital Medicine.
Preventing sepsis alert fatigue
If they’re too infrequent, alerts can delay sepsis identification and treatment. If they’re too abundant, the alerts can overwhelm providers. Finding the sweet spot for sepsis alerts, QI leaders say, can require time, technology, patience – and sometimes trial and error.
University Hospital in Salt Lake City wanted to broaden its sepsis recognition system to ensure that decompensating patients were seen and resuscitated quickly, regardless of the cause. Another hospital offered a lesson in what not to do when a staff member cautioned that a sepsis alert system based on SIRS alone had been a “total disaster” and left providers fuming. One report suggested that nearly half of all ward patients meet SIRS criteria at some point during their hospitalization, and that using the criteria for sepsis screening in hospital wards is both “time consuming and impractical.”1
Instead, University Hospital tweaked its MEWS or Modified Early Warning System, based on consultations with hospitalists, ICU physicians, and other providers about the appropriate thresholds for vital signs. “It’s kind of like asking someone, ‘Well, when are you really scared of the heart rate and when are you sort of scared and when are you not scared at all?’ ” said project coleader Devin J. Horton, MD, an academic hospitalist.
The team also analyzed the number of alerts per week per unit and their sensitivity and specificity in detecting sepsis. As junior faculty members, Dr. Horton and his collaborator, academic hospitalist Kencee K. Graves, MD, were mindful to avoid angering other doctors over being alerted too often. For their MEWS scoring system, they sacrificed a bit of sensitivity to ensure that the number of alerts remained manageable.
Before going live with its own new alert system, Middlesex Hospital in Middletown, Conn., had a subgroup spend several weeks testing the system in silent mode and tweaking different parameters such as respiratory rate and heart rate to reduce the potential for too many alerts. “If you look at each and every alert, then you can identify how to make your adjustment so that it’s not overly sensitive,” said Terri Savino, MSN, RN, CPHQ, the hospital’s manager of patient experience and service excellence.
A sepsis task force also shared data showing the hospital’s significant reductions in sepsis mortality, total hospital mortality, and sepsis length of stay. “Medical staff were willing to accept the frequency and high sensitivity of the alert because the data demonstrated that it was making a difference in the lives of our patients,” said David M. Cosentino, MD, the hospital’s chief medical information officer.
Other alert systems’ mixed performances have yielded important lessons. At the University of Pennsylvania, Philadelphia, one prototype detected clinically deteriorating patients and sent an alert to the nurse, physician, and a rapid response team. Alerted providers converged on the patient’s bedside within 30 minutes and decided whether to elevate the level of care. Craig Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine, said the system was associated with a suggestion of reduced mortality.2 But it was noisy and less helpful than it could have been, he said, because it didn’t separate out declining patients already known to the team from those who were still unrecognized.
Tools to predict which patients may develop severe sepsis or septic shock have worked even less well, he said. One triggered an alarm before patients showed signs of clinical deterioration. “The team didn’t know what to do with that prediction,” Dr. Umscheid said. As a result, the alert didn’t improve mortality or discharges to home. “If you’re making this prediction too early and providers don’t know what to do with the information, it’s not going to change care or affect patient outcomes,” he said. “It’s just going to frustrate providers.”
References
1. Churpek MM et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 Oct 15;192(8):958-64.
2. Umscheid CA et al. Development, implementation, and impact of an automated early warning and response system for sepsis. J Hosp Med. 2015 Jan;10: 26-31.
If they’re too infrequent, alerts can delay sepsis identification and treatment. If they’re too abundant, the alerts can overwhelm providers. Finding the sweet spot for sepsis alerts, QI leaders say, can require time, technology, patience – and sometimes trial and error.
University Hospital in Salt Lake City wanted to broaden its sepsis recognition system to ensure that decompensating patients were seen and resuscitated quickly, regardless of the cause. Another hospital offered a lesson in what not to do when a staff member cautioned that a sepsis alert system based on SIRS alone had been a “total disaster” and left providers fuming. One report suggested that nearly half of all ward patients meet SIRS criteria at some point during their hospitalization, and that using the criteria for sepsis screening in hospital wards is both “time consuming and impractical.”1
Instead, University Hospital tweaked its MEWS or Modified Early Warning System, based on consultations with hospitalists, ICU physicians, and other providers about the appropriate thresholds for vital signs. “It’s kind of like asking someone, ‘Well, when are you really scared of the heart rate and when are you sort of scared and when are you not scared at all?’ ” said project coleader Devin J. Horton, MD, an academic hospitalist.
The team also analyzed the number of alerts per week per unit and their sensitivity and specificity in detecting sepsis. As junior faculty members, Dr. Horton and his collaborator, academic hospitalist Kencee K. Graves, MD, were mindful to avoid angering other doctors over being alerted too often. For their MEWS scoring system, they sacrificed a bit of sensitivity to ensure that the number of alerts remained manageable.
Before going live with its own new alert system, Middlesex Hospital in Middletown, Conn., had a subgroup spend several weeks testing the system in silent mode and tweaking different parameters such as respiratory rate and heart rate to reduce the potential for too many alerts. “If you look at each and every alert, then you can identify how to make your adjustment so that it’s not overly sensitive,” said Terri Savino, MSN, RN, CPHQ, the hospital’s manager of patient experience and service excellence.
A sepsis task force also shared data showing the hospital’s significant reductions in sepsis mortality, total hospital mortality, and sepsis length of stay. “Medical staff were willing to accept the frequency and high sensitivity of the alert because the data demonstrated that it was making a difference in the lives of our patients,” said David M. Cosentino, MD, the hospital’s chief medical information officer.
Other alert systems’ mixed performances have yielded important lessons. At the University of Pennsylvania, Philadelphia, one prototype detected clinically deteriorating patients and sent an alert to the nurse, physician, and a rapid response team. Alerted providers converged on the patient’s bedside within 30 minutes and decided whether to elevate the level of care. Craig Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine, said the system was associated with a suggestion of reduced mortality.2 But it was noisy and less helpful than it could have been, he said, because it didn’t separate out declining patients already known to the team from those who were still unrecognized.
Tools to predict which patients may develop severe sepsis or septic shock have worked even less well, he said. One triggered an alarm before patients showed signs of clinical deterioration. “The team didn’t know what to do with that prediction,” Dr. Umscheid said. As a result, the alert didn’t improve mortality or discharges to home. “If you’re making this prediction too early and providers don’t know what to do with the information, it’s not going to change care or affect patient outcomes,” he said. “It’s just going to frustrate providers.”
References
1. Churpek MM et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 Oct 15;192(8):958-64.
2. Umscheid CA et al. Development, implementation, and impact of an automated early warning and response system for sepsis. J Hosp Med. 2015 Jan;10: 26-31.
If they’re too infrequent, alerts can delay sepsis identification and treatment. If they’re too abundant, the alerts can overwhelm providers. Finding the sweet spot for sepsis alerts, QI leaders say, can require time, technology, patience – and sometimes trial and error.
University Hospital in Salt Lake City wanted to broaden its sepsis recognition system to ensure that decompensating patients were seen and resuscitated quickly, regardless of the cause. Another hospital offered a lesson in what not to do when a staff member cautioned that a sepsis alert system based on SIRS alone had been a “total disaster” and left providers fuming. One report suggested that nearly half of all ward patients meet SIRS criteria at some point during their hospitalization, and that using the criteria for sepsis screening in hospital wards is both “time consuming and impractical.”1
Instead, University Hospital tweaked its MEWS or Modified Early Warning System, based on consultations with hospitalists, ICU physicians, and other providers about the appropriate thresholds for vital signs. “It’s kind of like asking someone, ‘Well, when are you really scared of the heart rate and when are you sort of scared and when are you not scared at all?’ ” said project coleader Devin J. Horton, MD, an academic hospitalist.
The team also analyzed the number of alerts per week per unit and their sensitivity and specificity in detecting sepsis. As junior faculty members, Dr. Horton and his collaborator, academic hospitalist Kencee K. Graves, MD, were mindful to avoid angering other doctors over being alerted too often. For their MEWS scoring system, they sacrificed a bit of sensitivity to ensure that the number of alerts remained manageable.
Before going live with its own new alert system, Middlesex Hospital in Middletown, Conn., had a subgroup spend several weeks testing the system in silent mode and tweaking different parameters such as respiratory rate and heart rate to reduce the potential for too many alerts. “If you look at each and every alert, then you can identify how to make your adjustment so that it’s not overly sensitive,” said Terri Savino, MSN, RN, CPHQ, the hospital’s manager of patient experience and service excellence.
A sepsis task force also shared data showing the hospital’s significant reductions in sepsis mortality, total hospital mortality, and sepsis length of stay. “Medical staff were willing to accept the frequency and high sensitivity of the alert because the data demonstrated that it was making a difference in the lives of our patients,” said David M. Cosentino, MD, the hospital’s chief medical information officer.
Other alert systems’ mixed performances have yielded important lessons. At the University of Pennsylvania, Philadelphia, one prototype detected clinically deteriorating patients and sent an alert to the nurse, physician, and a rapid response team. Alerted providers converged on the patient’s bedside within 30 minutes and decided whether to elevate the level of care. Craig Umscheid, MD, MSCE, of the department of epidemiology and vice chair for quality and safety in the department of medicine, said the system was associated with a suggestion of reduced mortality.2 But it was noisy and less helpful than it could have been, he said, because it didn’t separate out declining patients already known to the team from those who were still unrecognized.
Tools to predict which patients may develop severe sepsis or septic shock have worked even less well, he said. One triggered an alarm before patients showed signs of clinical deterioration. “The team didn’t know what to do with that prediction,” Dr. Umscheid said. As a result, the alert didn’t improve mortality or discharges to home. “If you’re making this prediction too early and providers don’t know what to do with the information, it’s not going to change care or affect patient outcomes,” he said. “It’s just going to frustrate providers.”
References
1. Churpek MM et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 Oct 15;192(8):958-64.
2. Umscheid CA et al. Development, implementation, and impact of an automated early warning and response system for sepsis. J Hosp Med. 2015 Jan;10: 26-31.
Controversy surrounds calf vein thrombosis treatment
CHICAGO – The use of therapeutic-dose anticoagulation in hospitalized patients with calf vein thrombosis significantly reduces the risk of venous thromboembolic complications, compared with lower-dose prophylactic anticoagulation or surveillance alone, Heron E. Rodriguez, MD, said at a symposium on vascular surgery sponsored by Northwestern University.
Moreover, placement of an inferior vena cava filter in patients with calf vein thrombosis when anticoagulation is contraindicated accomplishes nothing beneficial and had a 10% complication rate in a large retrospective single-center study, added Dr. Rodriguez of Northwestern University, Chicago.
Deep vein thrombosis (DVT) remains a significant source of morbidity and mortality despite worldwide awareness of the problem.
“Specifically, calf vein thrombosis [CVT] is very common, and we know that in some series up to 30% of patients end up propagating proximally if they’re not treated, and a good number of them develop chronic venous insufficiency, with long-term consequences,” he noted.
“Unfortunately there is no consensus regarding treatment. The guidelines are very vague. For example, there is no mention [in current American College of Chest Physicians guidelines] of how to manage muscular vein thrombosis and much ambiguity on how to treat calf vein thrombosis,” he continued.
Dr. Rodriguez cited as an indication of the lack of consensus on management of CVT a single-institution survey by other investigators of the practices of physicians in various specialties. Forty-nine percent of respondents indicated they anticoagulate patients with CVT; 51% don’t. Of those who did, 62% prescribed low-molecular-weight heparin and 11% intravenous heparin. Fifty-eight percent of physicians who anticoagulated did so for 3 months, 30% for 6. And 46% of physicians used an inferior vena cava (IVC) filter when anticoagulation was contraindicated (Vascular. 2014 Apr;22[2]:93-7).
That rate of IVC placement “seemed really high” given the paucity of supporting evidence for safety and efficacy of filter placement in the setting of CVT, so Dr. Rodriguez and coinvestigators decided to conduct a retrospective review of practices at Northwestern Memorial Hospital. He explained the study hypothesis: “Our thinking was that these kinds of thrombi are associated with low risk of propagation and pulmonary embolism, and they can and should be managed conservatively.”
Of 647 patients with isolated thrombosis of the anterior and posterior tibial, soleal, peroneal, or gastrocnemius veins, 44% received an IVC filter, and the rest got medical treatment alone. Of the 362 patients managed medically, 49% received therapeutic anticoagulation, 12% got low-dose prophylactic anticoagulation, and 39% underwent surveillance without anticoagulation.
The primary outcome was the incidence of venous thromboembolic complications – that is, propagation of DVT or pulmonary embolism. The incidence was 35% in the surveillance-only group, 30% with prophylactic anticoagulation, and 10% in patients who got therapeutic anticoagulation.
Of note, the rate of the most feared complication, pulmonary embolism, was low and similar in the filter recipients and medically managed group: 2.5% in the IVC group, 3.3% with medical management.
“Distal vein thromboses have low rates of pulmonary embolism, regardless of whether or not they are so-called protected with a filter. On the other hand, a filter was associated with a 10% rate of complications. I have to make clear that these were radiographic abnormalities – tilting, migration, caval perforation – that didn’t have clinical consequences, but we were very aggressive in removing the IVC filters, and I’m guessing if they’d been left inside they would create problems in the long term,” Dr. Rodriguez said.
An important point about this study is that these were all sick patients, and most were hospitalized. The filter recipients and medical groups differed in key ways. For example, 49% of the filter patients had a malignancy, and 56% had a baseline history of venous thromboembolic events, compared with 26% and 16%, respectively, of the medical group. For that reason, the investigators performed propensity score matching and came up with 157 closely matched patient pairs. The outcomes remained unchanged.
Of course, this was a retrospective study, with its inherent limitations, but Dr. Rodriguez characterized the published randomized trials on management of CVT as “small and limited.” The most frequently quoted study is the double-blind multicenter CACTUS trial, which randomized 252 outpatients with symptomatic CVT to 6 weeks of low-molecular-weight heparin or placebo and found no difference in the rates of proximal extension of venous thromboembolic events (Lancet Haematol. 2016 Dec;3[12]:e556-62). But these were all low-risk patients. Prior DVT or malignancy were exclusion criteria, so this was a very different population than treated at Northwestern.
Based upon the results of the retrospective study at Northwestern, which have been published (J Vasc Surg Venous Lymphat Disord. 2017 Jan;5[1]:25-32), the vascular surgery service has developed a management algorithm for DVT management based upon the lesion site. If a patient is unable to undergo anticoagulation, venous duplex ultrasound is repeated at 1 week. If the imaging shows propagation into the popliteal vein and anticoagulation remains contraindicated, only then is placement of an IVC filter warranted.
Dr. Rodriguez reported serving as a paid speaker for Abbott, Endologix, and W.L. Gore.
CHICAGO – The use of therapeutic-dose anticoagulation in hospitalized patients with calf vein thrombosis significantly reduces the risk of venous thromboembolic complications, compared with lower-dose prophylactic anticoagulation or surveillance alone, Heron E. Rodriguez, MD, said at a symposium on vascular surgery sponsored by Northwestern University.
Moreover, placement of an inferior vena cava filter in patients with calf vein thrombosis when anticoagulation is contraindicated accomplishes nothing beneficial and had a 10% complication rate in a large retrospective single-center study, added Dr. Rodriguez of Northwestern University, Chicago.
Deep vein thrombosis (DVT) remains a significant source of morbidity and mortality despite worldwide awareness of the problem.
“Specifically, calf vein thrombosis [CVT] is very common, and we know that in some series up to 30% of patients end up propagating proximally if they’re not treated, and a good number of them develop chronic venous insufficiency, with long-term consequences,” he noted.
“Unfortunately there is no consensus regarding treatment. The guidelines are very vague. For example, there is no mention [in current American College of Chest Physicians guidelines] of how to manage muscular vein thrombosis and much ambiguity on how to treat calf vein thrombosis,” he continued.
Dr. Rodriguez cited as an indication of the lack of consensus on management of CVT a single-institution survey by other investigators of the practices of physicians in various specialties. Forty-nine percent of respondents indicated they anticoagulate patients with CVT; 51% don’t. Of those who did, 62% prescribed low-molecular-weight heparin and 11% intravenous heparin. Fifty-eight percent of physicians who anticoagulated did so for 3 months, 30% for 6. And 46% of physicians used an inferior vena cava (IVC) filter when anticoagulation was contraindicated (Vascular. 2014 Apr;22[2]:93-7).
That rate of IVC placement “seemed really high” given the paucity of supporting evidence for safety and efficacy of filter placement in the setting of CVT, so Dr. Rodriguez and coinvestigators decided to conduct a retrospective review of practices at Northwestern Memorial Hospital. He explained the study hypothesis: “Our thinking was that these kinds of thrombi are associated with low risk of propagation and pulmonary embolism, and they can and should be managed conservatively.”
Of 647 patients with isolated thrombosis of the anterior and posterior tibial, soleal, peroneal, or gastrocnemius veins, 44% received an IVC filter, and the rest got medical treatment alone. Of the 362 patients managed medically, 49% received therapeutic anticoagulation, 12% got low-dose prophylactic anticoagulation, and 39% underwent surveillance without anticoagulation.
The primary outcome was the incidence of venous thromboembolic complications – that is, propagation of DVT or pulmonary embolism. The incidence was 35% in the surveillance-only group, 30% with prophylactic anticoagulation, and 10% in patients who got therapeutic anticoagulation.
Of note, the rate of the most feared complication, pulmonary embolism, was low and similar in the filter recipients and medically managed group: 2.5% in the IVC group, 3.3% with medical management.
“Distal vein thromboses have low rates of pulmonary embolism, regardless of whether or not they are so-called protected with a filter. On the other hand, a filter was associated with a 10% rate of complications. I have to make clear that these were radiographic abnormalities – tilting, migration, caval perforation – that didn’t have clinical consequences, but we were very aggressive in removing the IVC filters, and I’m guessing if they’d been left inside they would create problems in the long term,” Dr. Rodriguez said.
An important point about this study is that these were all sick patients, and most were hospitalized. The filter recipients and medical groups differed in key ways. For example, 49% of the filter patients had a malignancy, and 56% had a baseline history of venous thromboembolic events, compared with 26% and 16%, respectively, of the medical group. For that reason, the investigators performed propensity score matching and came up with 157 closely matched patient pairs. The outcomes remained unchanged.
Of course, this was a retrospective study, with its inherent limitations, but Dr. Rodriguez characterized the published randomized trials on management of CVT as “small and limited.” The most frequently quoted study is the double-blind multicenter CACTUS trial, which randomized 252 outpatients with symptomatic CVT to 6 weeks of low-molecular-weight heparin or placebo and found no difference in the rates of proximal extension of venous thromboembolic events (Lancet Haematol. 2016 Dec;3[12]:e556-62). But these were all low-risk patients. Prior DVT or malignancy were exclusion criteria, so this was a very different population than treated at Northwestern.
Based upon the results of the retrospective study at Northwestern, which have been published (J Vasc Surg Venous Lymphat Disord. 2017 Jan;5[1]:25-32), the vascular surgery service has developed a management algorithm for DVT management based upon the lesion site. If a patient is unable to undergo anticoagulation, venous duplex ultrasound is repeated at 1 week. If the imaging shows propagation into the popliteal vein and anticoagulation remains contraindicated, only then is placement of an IVC filter warranted.
Dr. Rodriguez reported serving as a paid speaker for Abbott, Endologix, and W.L. Gore.
CHICAGO – The use of therapeutic-dose anticoagulation in hospitalized patients with calf vein thrombosis significantly reduces the risk of venous thromboembolic complications, compared with lower-dose prophylactic anticoagulation or surveillance alone, Heron E. Rodriguez, MD, said at a symposium on vascular surgery sponsored by Northwestern University.
Moreover, placement of an inferior vena cava filter in patients with calf vein thrombosis when anticoagulation is contraindicated accomplishes nothing beneficial and had a 10% complication rate in a large retrospective single-center study, added Dr. Rodriguez of Northwestern University, Chicago.
Deep vein thrombosis (DVT) remains a significant source of morbidity and mortality despite worldwide awareness of the problem.
“Specifically, calf vein thrombosis [CVT] is very common, and we know that in some series up to 30% of patients end up propagating proximally if they’re not treated, and a good number of them develop chronic venous insufficiency, with long-term consequences,” he noted.
“Unfortunately there is no consensus regarding treatment. The guidelines are very vague. For example, there is no mention [in current American College of Chest Physicians guidelines] of how to manage muscular vein thrombosis and much ambiguity on how to treat calf vein thrombosis,” he continued.
Dr. Rodriguez cited as an indication of the lack of consensus on management of CVT a single-institution survey by other investigators of the practices of physicians in various specialties. Forty-nine percent of respondents indicated they anticoagulate patients with CVT; 51% don’t. Of those who did, 62% prescribed low-molecular-weight heparin and 11% intravenous heparin. Fifty-eight percent of physicians who anticoagulated did so for 3 months, 30% for 6. And 46% of physicians used an inferior vena cava (IVC) filter when anticoagulation was contraindicated (Vascular. 2014 Apr;22[2]:93-7).
That rate of IVC placement “seemed really high” given the paucity of supporting evidence for safety and efficacy of filter placement in the setting of CVT, so Dr. Rodriguez and coinvestigators decided to conduct a retrospective review of practices at Northwestern Memorial Hospital. He explained the study hypothesis: “Our thinking was that these kinds of thrombi are associated with low risk of propagation and pulmonary embolism, and they can and should be managed conservatively.”
Of 647 patients with isolated thrombosis of the anterior and posterior tibial, soleal, peroneal, or gastrocnemius veins, 44% received an IVC filter, and the rest got medical treatment alone. Of the 362 patients managed medically, 49% received therapeutic anticoagulation, 12% got low-dose prophylactic anticoagulation, and 39% underwent surveillance without anticoagulation.
The primary outcome was the incidence of venous thromboembolic complications – that is, propagation of DVT or pulmonary embolism. The incidence was 35% in the surveillance-only group, 30% with prophylactic anticoagulation, and 10% in patients who got therapeutic anticoagulation.
Of note, the rate of the most feared complication, pulmonary embolism, was low and similar in the filter recipients and medically managed group: 2.5% in the IVC group, 3.3% with medical management.
“Distal vein thromboses have low rates of pulmonary embolism, regardless of whether or not they are so-called protected with a filter. On the other hand, a filter was associated with a 10% rate of complications. I have to make clear that these were radiographic abnormalities – tilting, migration, caval perforation – that didn’t have clinical consequences, but we were very aggressive in removing the IVC filters, and I’m guessing if they’d been left inside they would create problems in the long term,” Dr. Rodriguez said.
An important point about this study is that these were all sick patients, and most were hospitalized. The filter recipients and medical groups differed in key ways. For example, 49% of the filter patients had a malignancy, and 56% had a baseline history of venous thromboembolic events, compared with 26% and 16%, respectively, of the medical group. For that reason, the investigators performed propensity score matching and came up with 157 closely matched patient pairs. The outcomes remained unchanged.
Of course, this was a retrospective study, with its inherent limitations, but Dr. Rodriguez characterized the published randomized trials on management of CVT as “small and limited.” The most frequently quoted study is the double-blind multicenter CACTUS trial, which randomized 252 outpatients with symptomatic CVT to 6 weeks of low-molecular-weight heparin or placebo and found no difference in the rates of proximal extension of venous thromboembolic events (Lancet Haematol. 2016 Dec;3[12]:e556-62). But these were all low-risk patients. Prior DVT or malignancy were exclusion criteria, so this was a very different population than treated at Northwestern.
Based upon the results of the retrospective study at Northwestern, which have been published (J Vasc Surg Venous Lymphat Disord. 2017 Jan;5[1]:25-32), the vascular surgery service has developed a management algorithm for DVT management based upon the lesion site. If a patient is unable to undergo anticoagulation, venous duplex ultrasound is repeated at 1 week. If the imaging shows propagation into the popliteal vein and anticoagulation remains contraindicated, only then is placement of an IVC filter warranted.
Dr. Rodriguez reported serving as a paid speaker for Abbott, Endologix, and W.L. Gore.
EXPERT ANALYSIS FROM NORTHWESTERN VASCULAR SYMPOSIUM
Is it time for health policy M&Ms?
What would happen if hospitalists began to incorporate health policy into morbidity and mortality (M&M) conferences? That was a question Chris Moriates, MD, explored in an entry for SHM’s The Hospital Leader blog1 and an idea that caused a minor stir on Twitter when he proposed it last summer.
In late July 2017, the U.S. Senate was debating a bill to repeal the Affordable Care Act, without a clear vision for replacing it. In response, physicians around the country took to Twitter to share their sentiments about repeal under the hashtag #DoctorsSpeakOut. In one such tweet, Dr. Moriates, assistant dean for health care value and an associate professor of internal medicine at Dell Medical School at the University of Texas, Austin, said this, in 140 characters: “We recently had idea: health policy M&M for residents to discuss adverse outcomes we see as result of lack of access.”
The idea began with a conversation Dr. Moriates had with Beth Miller, MD, program director for the Dell Medical School Internal Medicine Residency Program. “We were meeting and talking about revamping the [resident] M&M conference to have more learning objectives and put in place best practices,” Dr. Moriates said. “Dr. Miller suggested it could be a good forum [for health policy] because it’s an area where we all come together and there’s a natural hook to it, since it is case-based, thus we can use it to recognize the drivers within the system that lead to bad outcomes.”
In his SHM blog post, Dr. Moriates said he has increasingly observed adverse events that result from issues related to health policy. He provided an example: “A patient I admitted for ‘expedited work-up’ for rectal bleeding after he told me he had been trying to get a recommended colonoscopy for many months but could not get it scheduled due to his lack of insurance. He had colon cancer that had spread.”
In another example, he conjured a hypothetical (though not impractical) case where a patient prescribed blood thinners upon hospital discharge returns to the hospital soon after with a blood clot. Unable to afford the medication, or seek primary care follow-up, this kind of patient is readmitted through no direct fault of his physicians. Yet, the patient is worse off and the hospital takes the hit on readmissions penalties.
Dr. Moriates believes that viewing a case like this through a health policy lens is not only moving, but critical to better understanding health care delivery, particularly in an environment where physician performance is measured, in part, by outcomes. He now believes health policy M&Ms would be valuable to all hospital-based physicians, not just residents.
“Hospitalists are being asked to hit these value-based performance metrics, like readmissions and length of stay, and while we deal with the consequences, we are not always the best informed” with respect to policy, he said. “We could use this forum to teach health policy topics and continually update people and contribute, in real time, to all these different discussions and understand how things are changing or could change and impact our patients.”
“It’s important for physicians to know the policies that are aligned with, and the policies that may undermine, what they’re doing in their practice to improve their patients’ health,” Pourat said.
This knowledge can benefit physicians, too, Pourat added, because health policy M&Ms could help providers understand the goals of particular policies and in turn adjust their own behaviors and expectations.
“Physicians could discuss, what are the underlying issues or root causes, like the decision not to expand Medicaid here in Texas,” Dr. Moriates said. “Not all of these things you can fix, but you’re exposing those stories and perhaps we can come up with some actionable steps. How do we ensure in the future that our patients are able to fulfill their prescription so we’re not just sending someone out assuming they will but not knowing they’re unable to afford it?”
Similar to other domains in which physician leaders become champions, such as antibiotic stewardship, Dr. Pourat suggested that hospitalists could champion policy awareness through the kind of M&Ms Dr. Moriates proposed.
While journal clubs and lectures are great ways for hospitalists to learn more about health policy, the emotionally gripping nature of M&Ms could inspire more physicians to act in favor of policies that benefit their patients and themselves, Dr. Moriates said.
For example, physicians may write to or visit legislative offices, or author op-eds in their local newspapers. This collective action carries the potential to effect change. And it need not be partisan.
“I believe that if health policy issues were more explicitly integrated into M&Ms then clinicians would be more inclined and prepared to effectively advocate for specific policy changes,” he wrote in his blog post. “Perhaps entire groups would be moved to engage in the political process.”
On Twitter, even before Dr. Moriates’ first tweet about health policy M&Ms, New Jersey–based Jennifer Chuang, MD, an adolescent medicine physician, wrote: “M&M is heart-wrenching in academic hospitals. I dare @SenateGOP to present their role in M&M’s to come if ACA is repealed.”
While Dr. Moriates believes the chances are quite small that legislators and policymakers would attend health policy M&Ms, he called the notion “provocative and intriguing.”
In his blog post, Dr. Moriates invites state legislators and local members of Congress to join him in reviewing M&M cases where patients have been negatively affected by policy. He also emphasized that, like most modern M&Ms, the point should not be derision or finger-pointing, but an opportunity to learn how policy translates into practice.
Physicians may learn from legislators, too, he said in his blog post. “Just as policymakers could see legislation through the eyes of practitioners and their patients, this is where we as physicians could possibly learn from our legislators,” he wrote. “We may recognize the potential trade-offs, downsides, and barriers to proposals that to us may have seemed like no-brainers.”
What’s clear, said Dr. Pourat, who is also a professor in the UCLA Fielding School of Public Health and the School of Dentistry, is that Dr. Moriates’ blog post and tweet are “touching an important point for a lot of physicians during this whole debate over health reform.”
President Donald Trump campaigned on a promise to fully repeal and replace the Affordable Care Act but Republican efforts have thus far been stymied. In the meantime, some physicians are watching closely, knowing that whatever comes next will continue to affect them and their patients.
Source
1. Moriates C. Is it time for health policy M&Ms? The Hospital Leader. Aug 16, 2017. http://thehospitalleader.org/is-it-time-for-health-policy-mms/. Accessed 2017 Sep 14.
What would happen if hospitalists began to incorporate health policy into morbidity and mortality (M&M) conferences? That was a question Chris Moriates, MD, explored in an entry for SHM’s The Hospital Leader blog1 and an idea that caused a minor stir on Twitter when he proposed it last summer.
In late July 2017, the U.S. Senate was debating a bill to repeal the Affordable Care Act, without a clear vision for replacing it. In response, physicians around the country took to Twitter to share their sentiments about repeal under the hashtag #DoctorsSpeakOut. In one such tweet, Dr. Moriates, assistant dean for health care value and an associate professor of internal medicine at Dell Medical School at the University of Texas, Austin, said this, in 140 characters: “We recently had idea: health policy M&M for residents to discuss adverse outcomes we see as result of lack of access.”
The idea began with a conversation Dr. Moriates had with Beth Miller, MD, program director for the Dell Medical School Internal Medicine Residency Program. “We were meeting and talking about revamping the [resident] M&M conference to have more learning objectives and put in place best practices,” Dr. Moriates said. “Dr. Miller suggested it could be a good forum [for health policy] because it’s an area where we all come together and there’s a natural hook to it, since it is case-based, thus we can use it to recognize the drivers within the system that lead to bad outcomes.”
In his SHM blog post, Dr. Moriates said he has increasingly observed adverse events that result from issues related to health policy. He provided an example: “A patient I admitted for ‘expedited work-up’ for rectal bleeding after he told me he had been trying to get a recommended colonoscopy for many months but could not get it scheduled due to his lack of insurance. He had colon cancer that had spread.”
In another example, he conjured a hypothetical (though not impractical) case where a patient prescribed blood thinners upon hospital discharge returns to the hospital soon after with a blood clot. Unable to afford the medication, or seek primary care follow-up, this kind of patient is readmitted through no direct fault of his physicians. Yet, the patient is worse off and the hospital takes the hit on readmissions penalties.
Dr. Moriates believes that viewing a case like this through a health policy lens is not only moving, but critical to better understanding health care delivery, particularly in an environment where physician performance is measured, in part, by outcomes. He now believes health policy M&Ms would be valuable to all hospital-based physicians, not just residents.
“Hospitalists are being asked to hit these value-based performance metrics, like readmissions and length of stay, and while we deal with the consequences, we are not always the best informed” with respect to policy, he said. “We could use this forum to teach health policy topics and continually update people and contribute, in real time, to all these different discussions and understand how things are changing or could change and impact our patients.”
“It’s important for physicians to know the policies that are aligned with, and the policies that may undermine, what they’re doing in their practice to improve their patients’ health,” Pourat said.
This knowledge can benefit physicians, too, Pourat added, because health policy M&Ms could help providers understand the goals of particular policies and in turn adjust their own behaviors and expectations.
“Physicians could discuss, what are the underlying issues or root causes, like the decision not to expand Medicaid here in Texas,” Dr. Moriates said. “Not all of these things you can fix, but you’re exposing those stories and perhaps we can come up with some actionable steps. How do we ensure in the future that our patients are able to fulfill their prescription so we’re not just sending someone out assuming they will but not knowing they’re unable to afford it?”
Similar to other domains in which physician leaders become champions, such as antibiotic stewardship, Dr. Pourat suggested that hospitalists could champion policy awareness through the kind of M&Ms Dr. Moriates proposed.
While journal clubs and lectures are great ways for hospitalists to learn more about health policy, the emotionally gripping nature of M&Ms could inspire more physicians to act in favor of policies that benefit their patients and themselves, Dr. Moriates said.
For example, physicians may write to or visit legislative offices, or author op-eds in their local newspapers. This collective action carries the potential to effect change. And it need not be partisan.
“I believe that if health policy issues were more explicitly integrated into M&Ms then clinicians would be more inclined and prepared to effectively advocate for specific policy changes,” he wrote in his blog post. “Perhaps entire groups would be moved to engage in the political process.”
On Twitter, even before Dr. Moriates’ first tweet about health policy M&Ms, New Jersey–based Jennifer Chuang, MD, an adolescent medicine physician, wrote: “M&M is heart-wrenching in academic hospitals. I dare @SenateGOP to present their role in M&M’s to come if ACA is repealed.”
While Dr. Moriates believes the chances are quite small that legislators and policymakers would attend health policy M&Ms, he called the notion “provocative and intriguing.”
In his blog post, Dr. Moriates invites state legislators and local members of Congress to join him in reviewing M&M cases where patients have been negatively affected by policy. He also emphasized that, like most modern M&Ms, the point should not be derision or finger-pointing, but an opportunity to learn how policy translates into practice.
Physicians may learn from legislators, too, he said in his blog post. “Just as policymakers could see legislation through the eyes of practitioners and their patients, this is where we as physicians could possibly learn from our legislators,” he wrote. “We may recognize the potential trade-offs, downsides, and barriers to proposals that to us may have seemed like no-brainers.”
What’s clear, said Dr. Pourat, who is also a professor in the UCLA Fielding School of Public Health and the School of Dentistry, is that Dr. Moriates’ blog post and tweet are “touching an important point for a lot of physicians during this whole debate over health reform.”
President Donald Trump campaigned on a promise to fully repeal and replace the Affordable Care Act but Republican efforts have thus far been stymied. In the meantime, some physicians are watching closely, knowing that whatever comes next will continue to affect them and their patients.
Source
1. Moriates C. Is it time for health policy M&Ms? The Hospital Leader. Aug 16, 2017. http://thehospitalleader.org/is-it-time-for-health-policy-mms/. Accessed 2017 Sep 14.
What would happen if hospitalists began to incorporate health policy into morbidity and mortality (M&M) conferences? That was a question Chris Moriates, MD, explored in an entry for SHM’s The Hospital Leader blog1 and an idea that caused a minor stir on Twitter when he proposed it last summer.
In late July 2017, the U.S. Senate was debating a bill to repeal the Affordable Care Act, without a clear vision for replacing it. In response, physicians around the country took to Twitter to share their sentiments about repeal under the hashtag #DoctorsSpeakOut. In one such tweet, Dr. Moriates, assistant dean for health care value and an associate professor of internal medicine at Dell Medical School at the University of Texas, Austin, said this, in 140 characters: “We recently had idea: health policy M&M for residents to discuss adverse outcomes we see as result of lack of access.”
The idea began with a conversation Dr. Moriates had with Beth Miller, MD, program director for the Dell Medical School Internal Medicine Residency Program. “We were meeting and talking about revamping the [resident] M&M conference to have more learning objectives and put in place best practices,” Dr. Moriates said. “Dr. Miller suggested it could be a good forum [for health policy] because it’s an area where we all come together and there’s a natural hook to it, since it is case-based, thus we can use it to recognize the drivers within the system that lead to bad outcomes.”
In his SHM blog post, Dr. Moriates said he has increasingly observed adverse events that result from issues related to health policy. He provided an example: “A patient I admitted for ‘expedited work-up’ for rectal bleeding after he told me he had been trying to get a recommended colonoscopy for many months but could not get it scheduled due to his lack of insurance. He had colon cancer that had spread.”
In another example, he conjured a hypothetical (though not impractical) case where a patient prescribed blood thinners upon hospital discharge returns to the hospital soon after with a blood clot. Unable to afford the medication, or seek primary care follow-up, this kind of patient is readmitted through no direct fault of his physicians. Yet, the patient is worse off and the hospital takes the hit on readmissions penalties.
Dr. Moriates believes that viewing a case like this through a health policy lens is not only moving, but critical to better understanding health care delivery, particularly in an environment where physician performance is measured, in part, by outcomes. He now believes health policy M&Ms would be valuable to all hospital-based physicians, not just residents.
“Hospitalists are being asked to hit these value-based performance metrics, like readmissions and length of stay, and while we deal with the consequences, we are not always the best informed” with respect to policy, he said. “We could use this forum to teach health policy topics and continually update people and contribute, in real time, to all these different discussions and understand how things are changing or could change and impact our patients.”
“It’s important for physicians to know the policies that are aligned with, and the policies that may undermine, what they’re doing in their practice to improve their patients’ health,” Pourat said.
This knowledge can benefit physicians, too, Pourat added, because health policy M&Ms could help providers understand the goals of particular policies and in turn adjust their own behaviors and expectations.
“Physicians could discuss, what are the underlying issues or root causes, like the decision not to expand Medicaid here in Texas,” Dr. Moriates said. “Not all of these things you can fix, but you’re exposing those stories and perhaps we can come up with some actionable steps. How do we ensure in the future that our patients are able to fulfill their prescription so we’re not just sending someone out assuming they will but not knowing they’re unable to afford it?”
Similar to other domains in which physician leaders become champions, such as antibiotic stewardship, Dr. Pourat suggested that hospitalists could champion policy awareness through the kind of M&Ms Dr. Moriates proposed.
While journal clubs and lectures are great ways for hospitalists to learn more about health policy, the emotionally gripping nature of M&Ms could inspire more physicians to act in favor of policies that benefit their patients and themselves, Dr. Moriates said.
For example, physicians may write to or visit legislative offices, or author op-eds in their local newspapers. This collective action carries the potential to effect change. And it need not be partisan.
“I believe that if health policy issues were more explicitly integrated into M&Ms then clinicians would be more inclined and prepared to effectively advocate for specific policy changes,” he wrote in his blog post. “Perhaps entire groups would be moved to engage in the political process.”
On Twitter, even before Dr. Moriates’ first tweet about health policy M&Ms, New Jersey–based Jennifer Chuang, MD, an adolescent medicine physician, wrote: “M&M is heart-wrenching in academic hospitals. I dare @SenateGOP to present their role in M&M’s to come if ACA is repealed.”
While Dr. Moriates believes the chances are quite small that legislators and policymakers would attend health policy M&Ms, he called the notion “provocative and intriguing.”
In his blog post, Dr. Moriates invites state legislators and local members of Congress to join him in reviewing M&M cases where patients have been negatively affected by policy. He also emphasized that, like most modern M&Ms, the point should not be derision or finger-pointing, but an opportunity to learn how policy translates into practice.
Physicians may learn from legislators, too, he said in his blog post. “Just as policymakers could see legislation through the eyes of practitioners and their patients, this is where we as physicians could possibly learn from our legislators,” he wrote. “We may recognize the potential trade-offs, downsides, and barriers to proposals that to us may have seemed like no-brainers.”
What’s clear, said Dr. Pourat, who is also a professor in the UCLA Fielding School of Public Health and the School of Dentistry, is that Dr. Moriates’ blog post and tweet are “touching an important point for a lot of physicians during this whole debate over health reform.”
President Donald Trump campaigned on a promise to fully repeal and replace the Affordable Care Act but Republican efforts have thus far been stymied. In the meantime, some physicians are watching closely, knowing that whatever comes next will continue to affect them and their patients.
Source
1. Moriates C. Is it time for health policy M&Ms? The Hospital Leader. Aug 16, 2017. http://thehospitalleader.org/is-it-time-for-health-policy-mms/. Accessed 2017 Sep 14.
Multidisciplinary care improves surgical outcomes for elderly patients
and were able to leave the hospital after a shorter stay, according to findings from a case-control study of nearly 400 patients.
Data from previous studies suggest that preoperative assessment by geriatric experts can improve outcomes for the elderly, who are more likely than are younger patients to develop preventable postoperative complications, and “this evidence supports the formulation of a different approach to preoperative assessment and postoperative care for this population,” wrote Shelley R. McDonald, DO, of Duke University, Durham, N.C., and colleagues.
The intervention, known as the Perioperative Optimization of Senior Health (POSH), was described as “a quality improvement initiative with prospective data collection.” Patients in a geriatrics clinic within an academic center were selected for the study if they were at high risk for complications linked to elective abdominal surgery. High risk was defined as older than 85 years of age, or older than 65 years of age with conditions including cognitive impairment, recent weight loss, multiple comorbidities, and polypharmacy (JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513).
The POSH intervention patients received preoperative evaluation from a team including a geriatrician, geriatric resource nurse, social worker, program administrator, and nurse practitioner from the preoperative anesthesia testing clinic. Patients and families were advised on risk management and care optimization involving cognition, comorbidities, medications, mobility, functional status, nutrition, hydration, pain, and advanced care planning.
Patients in the POSH group were on average older, had more comorbidities, and were more likely to be smokers. But despite these disadvantaging characteristics, they still had better outcomes in several important variables than did those in the control group.
The POSH group had significantly shorter hospital stays, compared with controls (4 days vs. 6 days), and significantly lower all-cause readmission rates at both 7 days (2.8% vs. 9.9%) and 30 days (7.8% vs. 18.3%). The significance persisted whether the surgeries were laparoscopic or open.
The overall complication rate was lower in the POSH group, compared with the controls, but fell short of statistical significance (44.8% vs. 58.7%, P = .01). However, rates of specific complications were significantly lower in the POSH group, compared with controls, including postoperative cardiogenic or hypovolemic shock (2.2% vs. 8.4%), bleeding, either during or after surgery (6.1% vs. 15.4%), and postoperative ileus (4.9% vs. 20.3%).
“Delirium was identified in POSH patients at higher rates than in the control group, which is not unexpected because higher postoperative delirium rates are known to be identified with increased screening,” the researchers noted. “Collaborative care allows for increasing the recognition of geriatric syndromes like delirium, more focus on symptom management, and proactively anticipating complications,” they said.
The study results were limited by several factors including a long enrollment period for the POSH patients, and potential changes in surgical protocols, the researchers said. However, the findings support the need for further research and more refined analysis to identify the most beneficial aspects of care, and to support better clinical decision making about the timing of interventions and the type of patient who could benefit, they noted.
The researchers had no financial conflicts to disclose. The John A. Hartford Foundation Center of Excellence National Program Award provided salary and database support.
SOURCE: McDonald S et al. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513.
and were able to leave the hospital after a shorter stay, according to findings from a case-control study of nearly 400 patients.
Data from previous studies suggest that preoperative assessment by geriatric experts can improve outcomes for the elderly, who are more likely than are younger patients to develop preventable postoperative complications, and “this evidence supports the formulation of a different approach to preoperative assessment and postoperative care for this population,” wrote Shelley R. McDonald, DO, of Duke University, Durham, N.C., and colleagues.
The intervention, known as the Perioperative Optimization of Senior Health (POSH), was described as “a quality improvement initiative with prospective data collection.” Patients in a geriatrics clinic within an academic center were selected for the study if they were at high risk for complications linked to elective abdominal surgery. High risk was defined as older than 85 years of age, or older than 65 years of age with conditions including cognitive impairment, recent weight loss, multiple comorbidities, and polypharmacy (JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513).
The POSH intervention patients received preoperative evaluation from a team including a geriatrician, geriatric resource nurse, social worker, program administrator, and nurse practitioner from the preoperative anesthesia testing clinic. Patients and families were advised on risk management and care optimization involving cognition, comorbidities, medications, mobility, functional status, nutrition, hydration, pain, and advanced care planning.
Patients in the POSH group were on average older, had more comorbidities, and were more likely to be smokers. But despite these disadvantaging characteristics, they still had better outcomes in several important variables than did those in the control group.
The POSH group had significantly shorter hospital stays, compared with controls (4 days vs. 6 days), and significantly lower all-cause readmission rates at both 7 days (2.8% vs. 9.9%) and 30 days (7.8% vs. 18.3%). The significance persisted whether the surgeries were laparoscopic or open.
The overall complication rate was lower in the POSH group, compared with the controls, but fell short of statistical significance (44.8% vs. 58.7%, P = .01). However, rates of specific complications were significantly lower in the POSH group, compared with controls, including postoperative cardiogenic or hypovolemic shock (2.2% vs. 8.4%), bleeding, either during or after surgery (6.1% vs. 15.4%), and postoperative ileus (4.9% vs. 20.3%).
“Delirium was identified in POSH patients at higher rates than in the control group, which is not unexpected because higher postoperative delirium rates are known to be identified with increased screening,” the researchers noted. “Collaborative care allows for increasing the recognition of geriatric syndromes like delirium, more focus on symptom management, and proactively anticipating complications,” they said.
The study results were limited by several factors including a long enrollment period for the POSH patients, and potential changes in surgical protocols, the researchers said. However, the findings support the need for further research and more refined analysis to identify the most beneficial aspects of care, and to support better clinical decision making about the timing of interventions and the type of patient who could benefit, they noted.
The researchers had no financial conflicts to disclose. The John A. Hartford Foundation Center of Excellence National Program Award provided salary and database support.
SOURCE: McDonald S et al. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513.
and were able to leave the hospital after a shorter stay, according to findings from a case-control study of nearly 400 patients.
Data from previous studies suggest that preoperative assessment by geriatric experts can improve outcomes for the elderly, who are more likely than are younger patients to develop preventable postoperative complications, and “this evidence supports the formulation of a different approach to preoperative assessment and postoperative care for this population,” wrote Shelley R. McDonald, DO, of Duke University, Durham, N.C., and colleagues.
The intervention, known as the Perioperative Optimization of Senior Health (POSH), was described as “a quality improvement initiative with prospective data collection.” Patients in a geriatrics clinic within an academic center were selected for the study if they were at high risk for complications linked to elective abdominal surgery. High risk was defined as older than 85 years of age, or older than 65 years of age with conditions including cognitive impairment, recent weight loss, multiple comorbidities, and polypharmacy (JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513).
The POSH intervention patients received preoperative evaluation from a team including a geriatrician, geriatric resource nurse, social worker, program administrator, and nurse practitioner from the preoperative anesthesia testing clinic. Patients and families were advised on risk management and care optimization involving cognition, comorbidities, medications, mobility, functional status, nutrition, hydration, pain, and advanced care planning.
Patients in the POSH group were on average older, had more comorbidities, and were more likely to be smokers. But despite these disadvantaging characteristics, they still had better outcomes in several important variables than did those in the control group.
The POSH group had significantly shorter hospital stays, compared with controls (4 days vs. 6 days), and significantly lower all-cause readmission rates at both 7 days (2.8% vs. 9.9%) and 30 days (7.8% vs. 18.3%). The significance persisted whether the surgeries were laparoscopic or open.
The overall complication rate was lower in the POSH group, compared with the controls, but fell short of statistical significance (44.8% vs. 58.7%, P = .01). However, rates of specific complications were significantly lower in the POSH group, compared with controls, including postoperative cardiogenic or hypovolemic shock (2.2% vs. 8.4%), bleeding, either during or after surgery (6.1% vs. 15.4%), and postoperative ileus (4.9% vs. 20.3%).
“Delirium was identified in POSH patients at higher rates than in the control group, which is not unexpected because higher postoperative delirium rates are known to be identified with increased screening,” the researchers noted. “Collaborative care allows for increasing the recognition of geriatric syndromes like delirium, more focus on symptom management, and proactively anticipating complications,” they said.
The study results were limited by several factors including a long enrollment period for the POSH patients, and potential changes in surgical protocols, the researchers said. However, the findings support the need for further research and more refined analysis to identify the most beneficial aspects of care, and to support better clinical decision making about the timing of interventions and the type of patient who could benefit, they noted.
The researchers had no financial conflicts to disclose. The John A. Hartford Foundation Center of Excellence National Program Award provided salary and database support.
SOURCE: McDonald S et al. JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513.
FROM JAMA SURGERY
Key clinical point: A preoperative surgical intervention improved outcomes and shortened hospital stays for seniors.
Major finding: The POSH group had significantly shorter hospital stays compared with controls (4 days vs. 6 days).
Study details: The data come from a study of 183 surgery patients and 143 controls.
Disclosures: The researchers had no financial conflicts to disclose.
Source: McDonald S JAMA Surg. 2018 Jan 3. doi: 10.1001/jamasurg.2017.5513
Short takes
Pacing in syncope for select patients only
The 2017 ACC/AHA/HRD guideline for syncope evaluation and management concludes that the evidence does not yet support the use of pacing for reflex-mediated except among those with both recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Citation: Varosy P et al. Pacing as a treatment for reflex-mediated (vasovagal, situational, or carotid sinus hypersensitivity) syncope: A systematic review for the 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J Am Coll Cardiol. 2017 Aug 1;20(5):664-79.
Postoperative opioids often underutilized
Between 67% and 92% of patients report postoperative opioid oversupply, defined as filled but unused opioid prescriptions or unfilled opioid prescriptions. Half of the filled prescriptions were unused, with the majority reporting that the narcotics were not stored in locked containers.
Citation: Bicket MC et al. Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017 Aug 2. doi: 10.1001/jamasurg.2017.0831
5-hour protocol for contrast allergy safe and effective
Observational study showing a 5-hour IV steroid protocol was noninferior to a traditional 13-hour oral premedication regimen in patients at high risk for IV contrast reactions.
Citation: Mervak BM et al. Intravenous corticosteroid premedication administered 5 hours before CT, compared with a traditional 13-hour oral regimen. Radiology. 2017 Nov;285(2):425-33.
Poor food intake and chills predict true bacteremia in hospitalized patients
Observational study showing that poor food consumption had a sensitivity of 93.7% and shaking chills a specificity of 95.1% in diagnosing true bacteremia based on blood culture results.
Citation: Komatsu T et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017 Jul;12(7),510-5.
Lower readmission rates do not lead to increased postdischarge mortality at 30 days
Post–Affordable Care Act reductions in 30-day hospital risk-adjusted readmission rates for heart failure, acute MI, and pneumonia among Medicare beneficiaries did not increase but were weakly associated with decreased 30-day post–hospital discharge risk-adjusted mortality.
Citation: Dharmarajan K et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017Jul 18;318(3):270-8.
Pacing in syncope for select patients only
The 2017 ACC/AHA/HRD guideline for syncope evaluation and management concludes that the evidence does not yet support the use of pacing for reflex-mediated except among those with both recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Citation: Varosy P et al. Pacing as a treatment for reflex-mediated (vasovagal, situational, or carotid sinus hypersensitivity) syncope: A systematic review for the 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J Am Coll Cardiol. 2017 Aug 1;20(5):664-79.
Postoperative opioids often underutilized
Between 67% and 92% of patients report postoperative opioid oversupply, defined as filled but unused opioid prescriptions or unfilled opioid prescriptions. Half of the filled prescriptions were unused, with the majority reporting that the narcotics were not stored in locked containers.
Citation: Bicket MC et al. Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017 Aug 2. doi: 10.1001/jamasurg.2017.0831
5-hour protocol for contrast allergy safe and effective
Observational study showing a 5-hour IV steroid protocol was noninferior to a traditional 13-hour oral premedication regimen in patients at high risk for IV contrast reactions.
Citation: Mervak BM et al. Intravenous corticosteroid premedication administered 5 hours before CT, compared with a traditional 13-hour oral regimen. Radiology. 2017 Nov;285(2):425-33.
Poor food intake and chills predict true bacteremia in hospitalized patients
Observational study showing that poor food consumption had a sensitivity of 93.7% and shaking chills a specificity of 95.1% in diagnosing true bacteremia based on blood culture results.
Citation: Komatsu T et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017 Jul;12(7),510-5.
Lower readmission rates do not lead to increased postdischarge mortality at 30 days
Post–Affordable Care Act reductions in 30-day hospital risk-adjusted readmission rates for heart failure, acute MI, and pneumonia among Medicare beneficiaries did not increase but were weakly associated with decreased 30-day post–hospital discharge risk-adjusted mortality.
Citation: Dharmarajan K et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017Jul 18;318(3):270-8.
Pacing in syncope for select patients only
The 2017 ACC/AHA/HRD guideline for syncope evaluation and management concludes that the evidence does not yet support the use of pacing for reflex-mediated except among those with both recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Citation: Varosy P et al. Pacing as a treatment for reflex-mediated (vasovagal, situational, or carotid sinus hypersensitivity) syncope: A systematic review for the 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. J Am Coll Cardiol. 2017 Aug 1;20(5):664-79.
Postoperative opioids often underutilized
Between 67% and 92% of patients report postoperative opioid oversupply, defined as filled but unused opioid prescriptions or unfilled opioid prescriptions. Half of the filled prescriptions were unused, with the majority reporting that the narcotics were not stored in locked containers.
Citation: Bicket MC et al. Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017 Aug 2. doi: 10.1001/jamasurg.2017.0831
5-hour protocol for contrast allergy safe and effective
Observational study showing a 5-hour IV steroid protocol was noninferior to a traditional 13-hour oral premedication regimen in patients at high risk for IV contrast reactions.
Citation: Mervak BM et al. Intravenous corticosteroid premedication administered 5 hours before CT, compared with a traditional 13-hour oral regimen. Radiology. 2017 Nov;285(2):425-33.
Poor food intake and chills predict true bacteremia in hospitalized patients
Observational study showing that poor food consumption had a sensitivity of 93.7% and shaking chills a specificity of 95.1% in diagnosing true bacteremia based on blood culture results.
Citation: Komatsu T et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017 Jul;12(7),510-5.
Lower readmission rates do not lead to increased postdischarge mortality at 30 days
Post–Affordable Care Act reductions in 30-day hospital risk-adjusted readmission rates for heart failure, acute MI, and pneumonia among Medicare beneficiaries did not increase but were weakly associated with decreased 30-day post–hospital discharge risk-adjusted mortality.
Citation: Dharmarajan K et al. Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA. 2017Jul 18;318(3):270-8.
Heart attacks bring 12 weeks of higher stroke risk
LOS ANGELES – , based on a sample of Medicare beneficiaries.
The period of elevated stroke risk following an MI extends beyond the 30-day window that has traditionally been considered the interval of highest risk, Alexander E. Merkler, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Beyond 12 weeks after MI discharge, the stroke incidence showed no significant difference compared with people without a recent MI history, said Dr. Merkler, a neurologist at Weill Cornell Medicine in New York.
He calculated these statistically significant elevated risk rates after adjusting for demographic measures, stroke risk factors, and the comorbidities included in the Charlson Comorbidity Index.
These increased stroke rates were independent of periprocedural strokes that might have happened during MI interventions, as the analysis excluded MI patients with a history of a stroke either before or during their MI hospitalization.
To run this analysis, Dr. Merkler and his associates used data collected in a 5% sample of Medicare beneficiaries who were at least 66 years old during 2008-2015. Among these 1.7 million people were 46,182 who were hospitalized for an MI.
Several factors associated with an acute MI likely contribute to an elevated stroke risk, including stasis in the heart and generation of microthrombi, and a possibly systemic proinflammatory state, Dr. Merkler suggested.
Dr. Merkler had no disclosures.
SOURCE: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan; 49[Suppl 1]:A172).
LOS ANGELES – , based on a sample of Medicare beneficiaries.
The period of elevated stroke risk following an MI extends beyond the 30-day window that has traditionally been considered the interval of highest risk, Alexander E. Merkler, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Beyond 12 weeks after MI discharge, the stroke incidence showed no significant difference compared with people without a recent MI history, said Dr. Merkler, a neurologist at Weill Cornell Medicine in New York.
He calculated these statistically significant elevated risk rates after adjusting for demographic measures, stroke risk factors, and the comorbidities included in the Charlson Comorbidity Index.
These increased stroke rates were independent of periprocedural strokes that might have happened during MI interventions, as the analysis excluded MI patients with a history of a stroke either before or during their MI hospitalization.
To run this analysis, Dr. Merkler and his associates used data collected in a 5% sample of Medicare beneficiaries who were at least 66 years old during 2008-2015. Among these 1.7 million people were 46,182 who were hospitalized for an MI.
Several factors associated with an acute MI likely contribute to an elevated stroke risk, including stasis in the heart and generation of microthrombi, and a possibly systemic proinflammatory state, Dr. Merkler suggested.
Dr. Merkler had no disclosures.
SOURCE: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan; 49[Suppl 1]:A172).
LOS ANGELES – , based on a sample of Medicare beneficiaries.
The period of elevated stroke risk following an MI extends beyond the 30-day window that has traditionally been considered the interval of highest risk, Alexander E. Merkler, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
Beyond 12 weeks after MI discharge, the stroke incidence showed no significant difference compared with people without a recent MI history, said Dr. Merkler, a neurologist at Weill Cornell Medicine in New York.
He calculated these statistically significant elevated risk rates after adjusting for demographic measures, stroke risk factors, and the comorbidities included in the Charlson Comorbidity Index.
These increased stroke rates were independent of periprocedural strokes that might have happened during MI interventions, as the analysis excluded MI patients with a history of a stroke either before or during their MI hospitalization.
To run this analysis, Dr. Merkler and his associates used data collected in a 5% sample of Medicare beneficiaries who were at least 66 years old during 2008-2015. Among these 1.7 million people were 46,182 who were hospitalized for an MI.
Several factors associated with an acute MI likely contribute to an elevated stroke risk, including stasis in the heart and generation of microthrombi, and a possibly systemic proinflammatory state, Dr. Merkler suggested.
Dr. Merkler had no disclosures.
SOURCE: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan; 49[Suppl 1]:A172).
REPORTING FROM ISC 2018
Key clinical point: A patient’s stroke risk is elevated for 12 weeks following a myocardial infarction.
Major finding: The stroke rate was 2.7-fold, 2.0-fold, and 1.6-fold above background at 4, 8, and 12 weeks after an MI.
Study details: A review of 1.7 million Medicare beneficiaries during 2008-2015.
Disclosures: Dr. Merkler had no disclosures.
Source: Merkler AE et al., International Stroke Conference abstract 172 (Stroke. 2018 Jan;49[Suppl 1]:A172).
CDC: Flu levels highest since pandemic year 2009
according to data from the Centers for Disease Control and Prevention.
That season was dominated by influenza A (H3N2), and the 2017-2018 season seems to be going down that same path. For the week ending Jan. 20, the proportion of outpatient visits for influenza-like illness increased to 6.6%, which is, for the second consecutive week, the highest level reported since October of – you guessed it – 2009, when it hit 7.7%, the CDC said in its weekly flu surveillance report.
The level reported last week, 6.3%, has been revised downward and now stands at an even 6%.
It turns out that 2018 is something of a milestone for the H3N2 virus. The virus first emerged in 1968, so it has reached its 50th anniversary, Dan Jernigan, MD, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta, said on Jan. 26 in a weekly briefing.
H3N2 must not be happy about hitting the big 5-0, however, because the map of influenza-like illness activity looks pretty red and angry. For the week ending Jan. 20, there were 30 states at the highest level of flu activity on the CDC’s 1-10 scale, with another nine in the “high” range at levels 8 and 9.
Dr. Jernigan did suggest that activity may have peaked in some areas of the country, with California among them.
There were seven pediatric deaths reported for the week ending Jan. 20, although six occurred in previous weeks. There have been 37 flu-related deaths among children so far during the 2017-2018 season, the CDC said.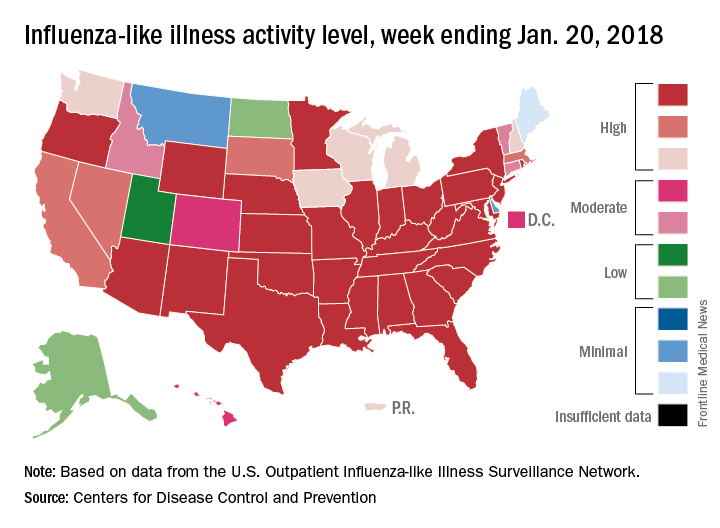
according to data from the Centers for Disease Control and Prevention.
That season was dominated by influenza A (H3N2), and the 2017-2018 season seems to be going down that same path. For the week ending Jan. 20, the proportion of outpatient visits for influenza-like illness increased to 6.6%, which is, for the second consecutive week, the highest level reported since October of – you guessed it – 2009, when it hit 7.7%, the CDC said in its weekly flu surveillance report.
The level reported last week, 6.3%, has been revised downward and now stands at an even 6%.
It turns out that 2018 is something of a milestone for the H3N2 virus. The virus first emerged in 1968, so it has reached its 50th anniversary, Dan Jernigan, MD, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta, said on Jan. 26 in a weekly briefing.
H3N2 must not be happy about hitting the big 5-0, however, because the map of influenza-like illness activity looks pretty red and angry. For the week ending Jan. 20, there were 30 states at the highest level of flu activity on the CDC’s 1-10 scale, with another nine in the “high” range at levels 8 and 9.
Dr. Jernigan did suggest that activity may have peaked in some areas of the country, with California among them.
There were seven pediatric deaths reported for the week ending Jan. 20, although six occurred in previous weeks. There have been 37 flu-related deaths among children so far during the 2017-2018 season, the CDC said.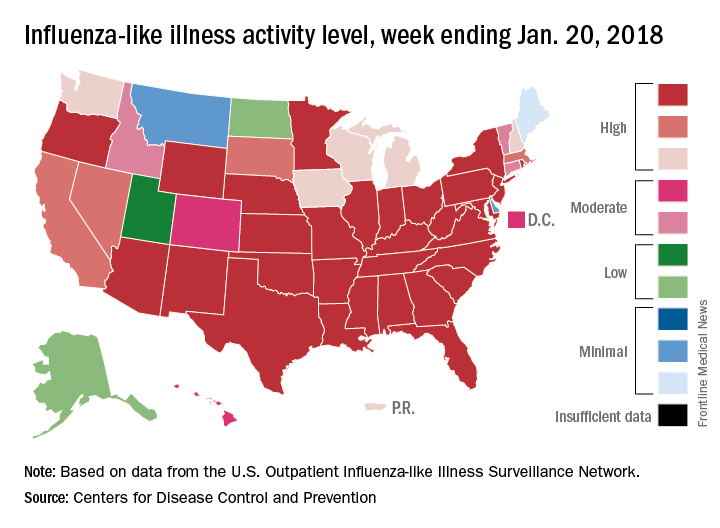
according to data from the Centers for Disease Control and Prevention.
That season was dominated by influenza A (H3N2), and the 2017-2018 season seems to be going down that same path. For the week ending Jan. 20, the proportion of outpatient visits for influenza-like illness increased to 6.6%, which is, for the second consecutive week, the highest level reported since October of – you guessed it – 2009, when it hit 7.7%, the CDC said in its weekly flu surveillance report.
The level reported last week, 6.3%, has been revised downward and now stands at an even 6%.
It turns out that 2018 is something of a milestone for the H3N2 virus. The virus first emerged in 1968, so it has reached its 50th anniversary, Dan Jernigan, MD, director of the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta, said on Jan. 26 in a weekly briefing.
H3N2 must not be happy about hitting the big 5-0, however, because the map of influenza-like illness activity looks pretty red and angry. For the week ending Jan. 20, there were 30 states at the highest level of flu activity on the CDC’s 1-10 scale, with another nine in the “high” range at levels 8 and 9.
Dr. Jernigan did suggest that activity may have peaked in some areas of the country, with California among them.
There were seven pediatric deaths reported for the week ending Jan. 20, although six occurred in previous weeks. There have been 37 flu-related deaths among children so far during the 2017-2018 season, the CDC said.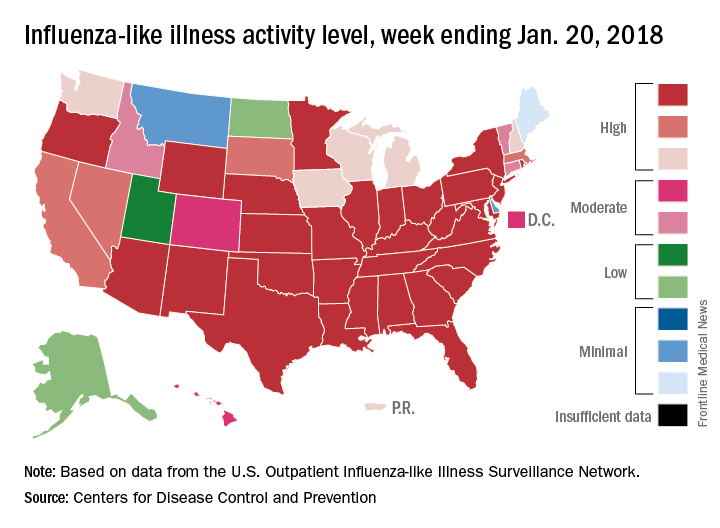
Contrast nephropathy after computed tomography
Clinical question: Do rates of acute kidney injury (AKI), renal replacement therapy (RRT), or mortality differ between adults receiving contrast-enhanced computed tomography (CT) versus those receiving noncontrast CT?
Background: Published estimates regarding the risk of postcontrast complications are highly variable and recent data show that the risk of postcontrast AKI may be lower than previously suggested.
Study design: Systematic review and meta-analysis..
Setting: Noninterventional studies assessing differences in AKI, new RRT, or mortality among adults who received contrast-enhanced CT, compared with those receiving noncontrast CT.
Synopsis: A search among six databases and Google Scholar from inception through 2016 yielded 28 observational studies meeting inclusion criteria that included 107,335 participants. Twenty-six assessed AKI, 13 assessed need for RRT, and 9 assessed all-cause mortality. Compared with noncontrast CT, contrast-enhanced CT was not significantly associated with AKI (odds ratio, 0.94; 95% confidence interval, 0.83-1.07), RRT (OR, 0.83; 95% CI 0.59-1.16), or all-cause mortality (OR, 1.0; 95% CI 0.73-1.36). The overall risk of bias ranged from low to serious among the included studies. Studies were observational in nature, they were conducted in multiple settings (for example, ICU, emergency department), and the baseline characteristics of included patients were highly variable.
Bottom line: This meta-analysis observed no difference in adverse events between patients receiving contrast-enhanced CT versus those receiving noncontrast CT but should be interpreted with caution given the observational nature of the studies and differing characteristics of the included patients and study settings.
Citation: Aycock RD et al. Acute kidney injury after computed tomography: a meta-analysis. Ann Emerg Med. 2017 Aug 12. doi: 10.1016/j.annemergmed.2017.06.041
Dr. Simonetti is a hospitalist at the University of Colorado School of Medicine.
Clinical question: Do rates of acute kidney injury (AKI), renal replacement therapy (RRT), or mortality differ between adults receiving contrast-enhanced computed tomography (CT) versus those receiving noncontrast CT?
Background: Published estimates regarding the risk of postcontrast complications are highly variable and recent data show that the risk of postcontrast AKI may be lower than previously suggested.
Study design: Systematic review and meta-analysis..
Setting: Noninterventional studies assessing differences in AKI, new RRT, or mortality among adults who received contrast-enhanced CT, compared with those receiving noncontrast CT.
Synopsis: A search among six databases and Google Scholar from inception through 2016 yielded 28 observational studies meeting inclusion criteria that included 107,335 participants. Twenty-six assessed AKI, 13 assessed need for RRT, and 9 assessed all-cause mortality. Compared with noncontrast CT, contrast-enhanced CT was not significantly associated with AKI (odds ratio, 0.94; 95% confidence interval, 0.83-1.07), RRT (OR, 0.83; 95% CI 0.59-1.16), or all-cause mortality (OR, 1.0; 95% CI 0.73-1.36). The overall risk of bias ranged from low to serious among the included studies. Studies were observational in nature, they were conducted in multiple settings (for example, ICU, emergency department), and the baseline characteristics of included patients were highly variable.
Bottom line: This meta-analysis observed no difference in adverse events between patients receiving contrast-enhanced CT versus those receiving noncontrast CT but should be interpreted with caution given the observational nature of the studies and differing characteristics of the included patients and study settings.
Citation: Aycock RD et al. Acute kidney injury after computed tomography: a meta-analysis. Ann Emerg Med. 2017 Aug 12. doi: 10.1016/j.annemergmed.2017.06.041
Dr. Simonetti is a hospitalist at the University of Colorado School of Medicine.
Clinical question: Do rates of acute kidney injury (AKI), renal replacement therapy (RRT), or mortality differ between adults receiving contrast-enhanced computed tomography (CT) versus those receiving noncontrast CT?
Background: Published estimates regarding the risk of postcontrast complications are highly variable and recent data show that the risk of postcontrast AKI may be lower than previously suggested.
Study design: Systematic review and meta-analysis..
Setting: Noninterventional studies assessing differences in AKI, new RRT, or mortality among adults who received contrast-enhanced CT, compared with those receiving noncontrast CT.
Synopsis: A search among six databases and Google Scholar from inception through 2016 yielded 28 observational studies meeting inclusion criteria that included 107,335 participants. Twenty-six assessed AKI, 13 assessed need for RRT, and 9 assessed all-cause mortality. Compared with noncontrast CT, contrast-enhanced CT was not significantly associated with AKI (odds ratio, 0.94; 95% confidence interval, 0.83-1.07), RRT (OR, 0.83; 95% CI 0.59-1.16), or all-cause mortality (OR, 1.0; 95% CI 0.73-1.36). The overall risk of bias ranged from low to serious among the included studies. Studies were observational in nature, they were conducted in multiple settings (for example, ICU, emergency department), and the baseline characteristics of included patients were highly variable.
Bottom line: This meta-analysis observed no difference in adverse events between patients receiving contrast-enhanced CT versus those receiving noncontrast CT but should be interpreted with caution given the observational nature of the studies and differing characteristics of the included patients and study settings.
Citation: Aycock RD et al. Acute kidney injury after computed tomography: a meta-analysis. Ann Emerg Med. 2017 Aug 12. doi: 10.1016/j.annemergmed.2017.06.041
Dr. Simonetti is a hospitalist at the University of Colorado School of Medicine.
Elderly trauma patients at high risk for post-discharge mortality
LAKE BUENA VISTA, FLA. – Nearly one-quarter of discharge, according to a study presented at the Eastern Association for the Surgery of Trauma Scientific Assembly.
These findings emphasize a need to know more about geriatric patient outcomes, especially as a tide of elderly trauma patients has begun to sweep through trauma centers, according to presenter Ciara Huntington, MD, a surgical resident at the Carolinas Healthcare System, Charlotte, N.C.
Investigators studied 6,285 geriatric patients in the ACS-verified Level 1 trauma registry between 2009 and 2015, and cross-referenced those files with the Social Security Death Index.
Patients were an average of 78.6 years, and the majority were female (57%) and white (85.7%). Average length of stay of was 6.7 days with an average injury severity score of 11, with a median time to death of 225 days.
While 5,780 patients were alive at discharge, 1,519 (24.2%) were dead within 1 year of hospitalization.
In a comparison of geriatric trauma patients against those of similar age in the general population, geriatric patients within the trauma population had a significantly lower life expectancy across all ages.
For trauma patients aged 65-70 years, life expectancy was estimated at 1.52 years, compared with 18.79 years for those in the general population.
Discharge location may have an impact on mortality, according to Dr. Huntington and her colleagues, who found geriatric patients discharged to their homes had a 1-year mortality rate of 13.5%, compared with 22.6% of those discharged to acute inpatient rehab centers, and 53.7% of those sent to skilled nursing facilities.
Another factor may be mechanism of injury, as the 1-year mortality of trauma patients who had fallen (27%) was nearly double the rate of those in motor vehicle crashes (15%).
Falls also were the most common injury, accounting for around 75% of the hospitalizations in the study.
In a question-and-answer session after the presentation, audience members asked about how these findings will help improve palliative care for geriatric trauma patients.
“The goal of this research is to have better predictive models and also to have better conversations” with families about the potential outcomes of trauma in these elderly patients, Dr. Huntington responded. Knowing the risk of 1-year mortality can change “how families can plan to spend time with their loved ones and how to make more appropriate medical decisions by incorporating quantitative data into the conversation.”
Dr. Huntington and her colleagues reported no relevant financial disclosures.
SOURCE: EAST 2018, Abstract #47.
LAKE BUENA VISTA, FLA. – Nearly one-quarter of discharge, according to a study presented at the Eastern Association for the Surgery of Trauma Scientific Assembly.
These findings emphasize a need to know more about geriatric patient outcomes, especially as a tide of elderly trauma patients has begun to sweep through trauma centers, according to presenter Ciara Huntington, MD, a surgical resident at the Carolinas Healthcare System, Charlotte, N.C.
Investigators studied 6,285 geriatric patients in the ACS-verified Level 1 trauma registry between 2009 and 2015, and cross-referenced those files with the Social Security Death Index.
Patients were an average of 78.6 years, and the majority were female (57%) and white (85.7%). Average length of stay of was 6.7 days with an average injury severity score of 11, with a median time to death of 225 days.
While 5,780 patients were alive at discharge, 1,519 (24.2%) were dead within 1 year of hospitalization.
In a comparison of geriatric trauma patients against those of similar age in the general population, geriatric patients within the trauma population had a significantly lower life expectancy across all ages.
For trauma patients aged 65-70 years, life expectancy was estimated at 1.52 years, compared with 18.79 years for those in the general population.
Discharge location may have an impact on mortality, according to Dr. Huntington and her colleagues, who found geriatric patients discharged to their homes had a 1-year mortality rate of 13.5%, compared with 22.6% of those discharged to acute inpatient rehab centers, and 53.7% of those sent to skilled nursing facilities.
Another factor may be mechanism of injury, as the 1-year mortality of trauma patients who had fallen (27%) was nearly double the rate of those in motor vehicle crashes (15%).
Falls also were the most common injury, accounting for around 75% of the hospitalizations in the study.
In a question-and-answer session after the presentation, audience members asked about how these findings will help improve palliative care for geriatric trauma patients.
“The goal of this research is to have better predictive models and also to have better conversations” with families about the potential outcomes of trauma in these elderly patients, Dr. Huntington responded. Knowing the risk of 1-year mortality can change “how families can plan to spend time with their loved ones and how to make more appropriate medical decisions by incorporating quantitative data into the conversation.”
Dr. Huntington and her colleagues reported no relevant financial disclosures.
SOURCE: EAST 2018, Abstract #47.
LAKE BUENA VISTA, FLA. – Nearly one-quarter of discharge, according to a study presented at the Eastern Association for the Surgery of Trauma Scientific Assembly.
These findings emphasize a need to know more about geriatric patient outcomes, especially as a tide of elderly trauma patients has begun to sweep through trauma centers, according to presenter Ciara Huntington, MD, a surgical resident at the Carolinas Healthcare System, Charlotte, N.C.
Investigators studied 6,285 geriatric patients in the ACS-verified Level 1 trauma registry between 2009 and 2015, and cross-referenced those files with the Social Security Death Index.
Patients were an average of 78.6 years, and the majority were female (57%) and white (85.7%). Average length of stay of was 6.7 days with an average injury severity score of 11, with a median time to death of 225 days.
While 5,780 patients were alive at discharge, 1,519 (24.2%) were dead within 1 year of hospitalization.
In a comparison of geriatric trauma patients against those of similar age in the general population, geriatric patients within the trauma population had a significantly lower life expectancy across all ages.
For trauma patients aged 65-70 years, life expectancy was estimated at 1.52 years, compared with 18.79 years for those in the general population.
Discharge location may have an impact on mortality, according to Dr. Huntington and her colleagues, who found geriatric patients discharged to their homes had a 1-year mortality rate of 13.5%, compared with 22.6% of those discharged to acute inpatient rehab centers, and 53.7% of those sent to skilled nursing facilities.
Another factor may be mechanism of injury, as the 1-year mortality of trauma patients who had fallen (27%) was nearly double the rate of those in motor vehicle crashes (15%).
Falls also were the most common injury, accounting for around 75% of the hospitalizations in the study.
In a question-and-answer session after the presentation, audience members asked about how these findings will help improve palliative care for geriatric trauma patients.
“The goal of this research is to have better predictive models and also to have better conversations” with families about the potential outcomes of trauma in these elderly patients, Dr. Huntington responded. Knowing the risk of 1-year mortality can change “how families can plan to spend time with their loved ones and how to make more appropriate medical decisions by incorporating quantitative data into the conversation.”
Dr. Huntington and her colleagues reported no relevant financial disclosures.
SOURCE: EAST 2018, Abstract #47.
REPORTING FROM EAST 2018
Key clinical point: Short-term mortality rates do not show a full picture of the burden of trauma on elderly patients.
Major finding: While 92% of patients survived to discharge, 24.1% of patients died within 1 year after injury, and 41.9% died within 8 years of injury.
Data source: Study of 6,285 geriatric trauma patients collected from an ACS-verified Level 1 trauma center registry database during 2009-2015.
Disclosures: Presenters reported no relevant financial disclosures.
Source: EAST Scientific Assembly abstract #47.