User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Everything We Say and Do: Take time to leave a good impression
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I say “thank you” to each patient at the close of the clinical encounter and ask if there is something I can do for him or her before leaving the room.
Why I do it
The beginning and the end of a medical visit each have a significant impact on how patients view their overall experience with the physician. Devoting energy and thought to these critical moments during the patient-physician interaction is simple and rewarding, and helps leave patients with a good impression.
How I do it
At the close of each patient visit, whether in the emergency department with a new admission or during daily rounds, I incorporate a “thank you” prior to leaving the room.
For example, I thank the patient for going over the details of her history with me; I know she has repeated the same information several times already. I thank the patient who brought in a detailed home medication list that made medication reconciliation a breeze for this organization. If I discussed a sensitive or difficult topic with the patient, such as substance use, I thank the patient for being honest. Another option is to thank the patient for trusting me with his care during the hospitalization. My favorite “thank you,” and one that will work in any situation, is to thank a patient for his or her patience. Whether it is waiting for a procedure, waiting to eat, or waiting for the green light to go home, our patients’ patience is tremendous and absolutely deserves to be recognized.
After saying “thank you,” I close with a simple but powerful question: “Is there something I can do for you before I leave? I have time.” Perhaps I can assist with a refill of ice chips, help find the call button, or relay a message to the bedside nurse. Whatever the task may be, offering to help before departing humanizes the interaction between physician and patient and is sure to be appreciated and remembered. Furthermore, taking a pause in the hectic pace of the day to show patients that we care can give busy hospitalists a moment to recharge before moving on to the next item on the to-do list. Any way you look at it, thanking our patients and offering to help is time well spent.
Dr. Sebasky is assistant clinical professor at the University of California, San Diego.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I say “thank you” to each patient at the close of the clinical encounter and ask if there is something I can do for him or her before leaving the room.
Why I do it
The beginning and the end of a medical visit each have a significant impact on how patients view their overall experience with the physician. Devoting energy and thought to these critical moments during the patient-physician interaction is simple and rewarding, and helps leave patients with a good impression.
How I do it
At the close of each patient visit, whether in the emergency department with a new admission or during daily rounds, I incorporate a “thank you” prior to leaving the room.
For example, I thank the patient for going over the details of her history with me; I know she has repeated the same information several times already. I thank the patient who brought in a detailed home medication list that made medication reconciliation a breeze for this organization. If I discussed a sensitive or difficult topic with the patient, such as substance use, I thank the patient for being honest. Another option is to thank the patient for trusting me with his care during the hospitalization. My favorite “thank you,” and one that will work in any situation, is to thank a patient for his or her patience. Whether it is waiting for a procedure, waiting to eat, or waiting for the green light to go home, our patients’ patience is tremendous and absolutely deserves to be recognized.
After saying “thank you,” I close with a simple but powerful question: “Is there something I can do for you before I leave? I have time.” Perhaps I can assist with a refill of ice chips, help find the call button, or relay a message to the bedside nurse. Whatever the task may be, offering to help before departing humanizes the interaction between physician and patient and is sure to be appreciated and remembered. Furthermore, taking a pause in the hectic pace of the day to show patients that we care can give busy hospitalists a moment to recharge before moving on to the next item on the to-do list. Any way you look at it, thanking our patients and offering to help is time well spent.
Dr. Sebasky is assistant clinical professor at the University of California, San Diego.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively impact patients’ experience of care. Each article will focus on how the contributor applies one or more of the “key communication” tactics in practice to maintain provider accountability for “everything we say and do that affects our patients’ thoughts, feelings, and well-being.”
What I say and do
I say “thank you” to each patient at the close of the clinical encounter and ask if there is something I can do for him or her before leaving the room.
Why I do it
The beginning and the end of a medical visit each have a significant impact on how patients view their overall experience with the physician. Devoting energy and thought to these critical moments during the patient-physician interaction is simple and rewarding, and helps leave patients with a good impression.
How I do it
At the close of each patient visit, whether in the emergency department with a new admission or during daily rounds, I incorporate a “thank you” prior to leaving the room.
For example, I thank the patient for going over the details of her history with me; I know she has repeated the same information several times already. I thank the patient who brought in a detailed home medication list that made medication reconciliation a breeze for this organization. If I discussed a sensitive or difficult topic with the patient, such as substance use, I thank the patient for being honest. Another option is to thank the patient for trusting me with his care during the hospitalization. My favorite “thank you,” and one that will work in any situation, is to thank a patient for his or her patience. Whether it is waiting for a procedure, waiting to eat, or waiting for the green light to go home, our patients’ patience is tremendous and absolutely deserves to be recognized.
After saying “thank you,” I close with a simple but powerful question: “Is there something I can do for you before I leave? I have time.” Perhaps I can assist with a refill of ice chips, help find the call button, or relay a message to the bedside nurse. Whatever the task may be, offering to help before departing humanizes the interaction between physician and patient and is sure to be appreciated and remembered. Furthermore, taking a pause in the hectic pace of the day to show patients that we care can give busy hospitalists a moment to recharge before moving on to the next item on the to-do list. Any way you look at it, thanking our patients and offering to help is time well spent.
Dr. Sebasky is assistant clinical professor at the University of California, San Diego.
New drug choices emerging to battle antibiotic resistance
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
SAN FRANCISCO – When the Infectious Diseases Society of America released the “Bad Bugs, No Drugs” report in 2004, its authors warned that effective antibiotics may not be available to treat seriously ill patients in the near future.
It also proposed legislative, regulatory, and funding solutions with a goal of developing and licensing 10 new antibiotics by the year 2020.
One such advancement was the Generating Antibiotics Incentives Now Act, which was signed into law in 2012 and created a designation for new antibiotics that are used to treat serious and/or life-threatening diseases due to certain pathogens. It also extends the patent life of these antibiotics and allows for fast-track Food and Drug Administration approval.
According to Dr. Erlich, chief of staff and medical director of infection control and antibiotic stewardship at Mills Peninsula Medical Center, Burlingame, Calif., increasingly common antibiotic-resistant pathogens besides MRSA and VRE include penicillin-resistant Streptococcus pneumoniae, extended-spectrum beta-lactamase–producing gram-negative rods, carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Mycobacterium tuberculosis, Salmonella enterica serotype Typhimurium DT 104, and drug-resistant Candida species.
Since 2010, several new antibiotics have been introduced to the market, including three second-generation lipoglycopeptide antibiotics with gram-positive coverage that are approved primarily for skin and soft tissue infections: dalbavancin (Dalvance), telavancin (Vibativ), and oritavancin (Orbactiv).
Compared with vancomycin, these new agents have more convenient dosing and a longer half life, “but they’re also more expensive,” said Dr. Erlich. Dalbavancin can be dosed once a week intravenously, telavancin can be dosed once daily intravenously, and oritavancin requires just one dose.
Another new agent is tedizolid phosphate (Sivextro), a second-generation oxazolidinone that is in the same drug class as linezolid (Zyvox). Tedizolid phosphate has gram-positive coverage including MRSA, but it is not approved for VRE. “It’s FDA approved for skin and soft-tissue infections (SSTI) but can be used for other locations as well,” Dr. Erlich said. “It features once-daily dosing IV or PO.”
Ceftaroline fosamil (Teflaro), ceftolozane/tazobactam (Zerbaxa), and ceftazidime/avibactam (Avycaz) are broad-spectrum cephalosporins with or without beta-lactamase inhibitors resulting in extended gram-negative coverage. FDA-approved indications include complicated urinary tract infections, complicated abdominal infections, SSTI, and pneumonia.
The primary advantage of these drugs, compared with other agents, is for multidrug-resistant gram-negative bacteria such as extended-spectrum beta-lactamase producers and CRE. “We’re not using a lot of these drugs in clinical practice, but they are available for patients with multidrug-resistant gram-negative rods who have no other options,” Dr. Erlich said.
Practical ways that clinicians can prevent antibiotic resistance include prescribing antibiotics only when necessary. “Be aware of local resistance patterns, avoid antibiotics for probable viral infections, use narrow-spectrum choices when possible, use shorter durations when appropriate, and consult published guidelines for optimal empiric antibiotic therapy,” Dr. Erlich advised.
In addition, “advocate infection control measures to keep patients from developing infections, including proper wound care, hand washing, respiratory etiquette, vaccinations, and social isolation for symptomatic individuals,” he noted.
Dr. Erlich reported having no relevant financial disclosures.
AT THE ANNUAL ADVANCES IN INTERNAL MEDICINE
Study shows that 20% of inpatients given antibiotics develop adverse reactions
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
Twenty percent of hospitalized adults given antibiotics develop adverse drug events, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects, according to a report in JAMA Internal Medicine.
This high frequency of adverse reactions “may not be recognized by clinicians because [these events] have varied manifestations, clinicians may be unaware of the risks associated with specific antibiotic agents, or because they occur after patients are discharged from the hospital,” said Pranita D. Tamma, MD, of the division of pediatric infectious diseases, Johns Hopkins University, Baltimore, and her associates.
They assessed antibiotic-associated adverse drug events in all 1,488 adults admitted to four general medicine services at a single medical center during a 9-month period and given at least 24 hours of any antibiotic therapy. The most common indications for antibiotics were urinary tract infections (12%), skin and soft-tissue infections (8%), and community-acquired pneumonia (7%).
Perhaps as important, the researchers noted, 19% of these adverse drug events were attributed to unnecessary antibiotics – drugs given for conditions for which they were not clinically indicated according to the hospital’s own antibiotic guidelines. These included asymptomatic bacteriuria, aspiration pneumonitis, and heart failure (JAMA Intern. Med. 2017 June 12. doi: 10.1001/jamainternmed.2017.1938).
The most common adverse reactions that developed within 30 days were GI, renal, and hematologic abnormalities. Neurotoxic effects included encephalopathy and seizures; cardiotoxic effects included QTc prolongation. Less frequent adverse events included anaphylaxis, daptomycin-associated myositis, trimethoprim/sulfamethoxazole-associated pancreatitis, linezolid-associated neuropathy, and ciprofloxacin-related tendinitis. The most common adverse reactions that developed within 90 days were C. difficile infections and infections involving multidrug-resistant organisms.
“Our findings underscore the importance of avoiding unnecessary antibiotic prescribing to reduce the harm that can result from antibiotic-associated adverse drug events,” Dr. Tamma and her associates said.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Among hospitalized adults given antibiotics, 20% develop adverse reactions, including GI, nephrotoxic, hematologic, cardiac, and neurotoxic effects.
Major finding: Among 1,488 patients, 298 (20%) developed 324 adverse reactions to antibiotics – 73% during hospitalization and 27% after discharge – requiring prolonged hospitalization; a subsequent hospitalization; an ED visit; or additional lab tests, ECGs, or imaging studies.
Data source: A single-center retrospective cohort study involving all 1,488 general medicine inpatients admitted during a 9-month period who received any antibiotic for at least 24 hours.
Disclosures: This study was supported by Pfizer Independent Grants for Learning and Change and the Joint Commission. Dr. Tamma and her associates reported having no relevant financial disclosures.
Meet the two newest SHM board members
SHM’s two newest board members – pediatric hospitalist Kris Rehm, MD, SFHM, and perioperative specialist Rachel Thompson, MD, MPH, SFHM – will bring their expertise to bear on the society’s top panel.
However, neither woman sees her role as shaping the board. In fact, they see themselves as lucky to be joining the team.
“I really want to hear everyone’s voice, and I hope to see how we can all move to better places together,” added Dr. Rehm, associate professor of clinical pediatrics and director of the division of hospital medicine at Vanderbilt University in Nashville.
Both board members were officially seated for three-year terms at HM17 in Las Vegas. They replace former SHM president Robert Harrington, MD, SFHM, and veteran pediatric hospitalist Erin Stucky Fisher, MD, MHM.
Each of the new board members brings a strong perspective to the panel.
For Dr. Thompson, that viewpoint is based in engagement. She is the former chair of SHM’s Pacific Northwest chapter and has spent the past few years leading the perioperative issues for the society’s work group.
“We get to a certain point of our career as hospitalists, and if we’re just plugging in and working, doing our shifts, somewhere in that 8- to 10-year range, we might get a little bored, tired, worn out,” Dr. Thompson said. “I believe, if we have the community and professional home to keep us engaged, that helps us see the value in what we’re doing every day. It helps us continue to grow, so we don’t hit that wall.”
Given Dr. Thompson’s involvement both with her chapter and the society’s chapter support committee, she will likely continue that effort to make sure SHM’s board sees the value of encouraging and partnering with local chapters. She will also work with SHM president Ron Greeno, MD, FCCP, MHM, on policy issues, as her background in public health has aligned her interests on health care reform and other headwinds facing the specialty.
“I went in to do my masters in public health with the idea that I wanted to build the skill set so that I could be more analytical in how I approach our problem solving, our discovery in the hospital setting,” she said. “It really speaks to a part of me that has always been interested in finding ways to prevent illness and moving beyond that reactivity that we have in medicine into a prevention-based [approach].”
Dr. Thompson noted that her background in perioperative medicine helps her work as part of a team because it “entirely relies on collaboration and coordination of care, which is pretty much the basis of what we do in the hospital any day.”
Dr. Rehm, who serves as a pediatric hospitalist at the Monroe Carell Jr. Children’s Hospital at Vanderbilt, said she will also bring a teamwork-focused perspective to the SHM board.
She could be expected to view everything through the lens of inpatient pediatrics, but that’s not her style.
“I think we have so many similarities and so many things that [pediatric and adult hospitalists] can partner to do together,” she said. “We all are involved in, for example, medication reconciliation or discharge-management planning or postacute care follow-up. There’s a lot of synergy, and I think we can learn so much from each other.”
Dr. Rehm, who chairs SHM’s Pediatrics Committee and the 2017 Pediatric Hospital Medicine meeting, pointed out that working well with others is a natural skill set for hospitalists.
“Collaboration is probably my biggest skill set and that of many hospital medicine providers,” she said. “I think I do that in my job here at Vanderbilt in thinking about complicated patients that requirement multiple subspecialists and in bringing together people to figure out the question at hand. That is definitely my leadership style.”
If Dr. Rehm has one goal on the board, it is to become a little bit more like Dr. Thompson and focus on chapter development for pediatric hospitalists.
“I’m really interested in engaging with members to better understand the struggles on the front line so that we can make sure that, as an organization, we’re offering a brand of things that our membership needs,” she said. “So, I’m really looking forward to becoming more involved in the chapter engagement and development. The Nashville chapter is getting re-engaged now and I’m excited to be involved.”
To prepare for her debut board meeting in Las Vegas, Dr. Rehm attended SHM board meetings at the group’s Philadelphia headquarters over the past two years.
“I’ve been lucky enough to attend the fall board meeting in Philadelphia and observe the board in action, and I think that has helped me get to know some of the current board members and to have a little bit of a vision of what the meetings will be like,” she said.
SHM’s two newest board members – pediatric hospitalist Kris Rehm, MD, SFHM, and perioperative specialist Rachel Thompson, MD, MPH, SFHM – will bring their expertise to bear on the society’s top panel.
However, neither woman sees her role as shaping the board. In fact, they see themselves as lucky to be joining the team.
“I really want to hear everyone’s voice, and I hope to see how we can all move to better places together,” added Dr. Rehm, associate professor of clinical pediatrics and director of the division of hospital medicine at Vanderbilt University in Nashville.
Both board members were officially seated for three-year terms at HM17 in Las Vegas. They replace former SHM president Robert Harrington, MD, SFHM, and veteran pediatric hospitalist Erin Stucky Fisher, MD, MHM.
Each of the new board members brings a strong perspective to the panel.
For Dr. Thompson, that viewpoint is based in engagement. She is the former chair of SHM’s Pacific Northwest chapter and has spent the past few years leading the perioperative issues for the society’s work group.
“We get to a certain point of our career as hospitalists, and if we’re just plugging in and working, doing our shifts, somewhere in that 8- to 10-year range, we might get a little bored, tired, worn out,” Dr. Thompson said. “I believe, if we have the community and professional home to keep us engaged, that helps us see the value in what we’re doing every day. It helps us continue to grow, so we don’t hit that wall.”
Given Dr. Thompson’s involvement both with her chapter and the society’s chapter support committee, she will likely continue that effort to make sure SHM’s board sees the value of encouraging and partnering with local chapters. She will also work with SHM president Ron Greeno, MD, FCCP, MHM, on policy issues, as her background in public health has aligned her interests on health care reform and other headwinds facing the specialty.
“I went in to do my masters in public health with the idea that I wanted to build the skill set so that I could be more analytical in how I approach our problem solving, our discovery in the hospital setting,” she said. “It really speaks to a part of me that has always been interested in finding ways to prevent illness and moving beyond that reactivity that we have in medicine into a prevention-based [approach].”
Dr. Thompson noted that her background in perioperative medicine helps her work as part of a team because it “entirely relies on collaboration and coordination of care, which is pretty much the basis of what we do in the hospital any day.”
Dr. Rehm, who serves as a pediatric hospitalist at the Monroe Carell Jr. Children’s Hospital at Vanderbilt, said she will also bring a teamwork-focused perspective to the SHM board.
She could be expected to view everything through the lens of inpatient pediatrics, but that’s not her style.
“I think we have so many similarities and so many things that [pediatric and adult hospitalists] can partner to do together,” she said. “We all are involved in, for example, medication reconciliation or discharge-management planning or postacute care follow-up. There’s a lot of synergy, and I think we can learn so much from each other.”
Dr. Rehm, who chairs SHM’s Pediatrics Committee and the 2017 Pediatric Hospital Medicine meeting, pointed out that working well with others is a natural skill set for hospitalists.
“Collaboration is probably my biggest skill set and that of many hospital medicine providers,” she said. “I think I do that in my job here at Vanderbilt in thinking about complicated patients that requirement multiple subspecialists and in bringing together people to figure out the question at hand. That is definitely my leadership style.”
If Dr. Rehm has one goal on the board, it is to become a little bit more like Dr. Thompson and focus on chapter development for pediatric hospitalists.
“I’m really interested in engaging with members to better understand the struggles on the front line so that we can make sure that, as an organization, we’re offering a brand of things that our membership needs,” she said. “So, I’m really looking forward to becoming more involved in the chapter engagement and development. The Nashville chapter is getting re-engaged now and I’m excited to be involved.”
To prepare for her debut board meeting in Las Vegas, Dr. Rehm attended SHM board meetings at the group’s Philadelphia headquarters over the past two years.
“I’ve been lucky enough to attend the fall board meeting in Philadelphia and observe the board in action, and I think that has helped me get to know some of the current board members and to have a little bit of a vision of what the meetings will be like,” she said.
SHM’s two newest board members – pediatric hospitalist Kris Rehm, MD, SFHM, and perioperative specialist Rachel Thompson, MD, MPH, SFHM – will bring their expertise to bear on the society’s top panel.
However, neither woman sees her role as shaping the board. In fact, they see themselves as lucky to be joining the team.
“I really want to hear everyone’s voice, and I hope to see how we can all move to better places together,” added Dr. Rehm, associate professor of clinical pediatrics and director of the division of hospital medicine at Vanderbilt University in Nashville.
Both board members were officially seated for three-year terms at HM17 in Las Vegas. They replace former SHM president Robert Harrington, MD, SFHM, and veteran pediatric hospitalist Erin Stucky Fisher, MD, MHM.
Each of the new board members brings a strong perspective to the panel.
For Dr. Thompson, that viewpoint is based in engagement. She is the former chair of SHM’s Pacific Northwest chapter and has spent the past few years leading the perioperative issues for the society’s work group.
“We get to a certain point of our career as hospitalists, and if we’re just plugging in and working, doing our shifts, somewhere in that 8- to 10-year range, we might get a little bored, tired, worn out,” Dr. Thompson said. “I believe, if we have the community and professional home to keep us engaged, that helps us see the value in what we’re doing every day. It helps us continue to grow, so we don’t hit that wall.”
Given Dr. Thompson’s involvement both with her chapter and the society’s chapter support committee, she will likely continue that effort to make sure SHM’s board sees the value of encouraging and partnering with local chapters. She will also work with SHM president Ron Greeno, MD, FCCP, MHM, on policy issues, as her background in public health has aligned her interests on health care reform and other headwinds facing the specialty.
“I went in to do my masters in public health with the idea that I wanted to build the skill set so that I could be more analytical in how I approach our problem solving, our discovery in the hospital setting,” she said. “It really speaks to a part of me that has always been interested in finding ways to prevent illness and moving beyond that reactivity that we have in medicine into a prevention-based [approach].”
Dr. Thompson noted that her background in perioperative medicine helps her work as part of a team because it “entirely relies on collaboration and coordination of care, which is pretty much the basis of what we do in the hospital any day.”
Dr. Rehm, who serves as a pediatric hospitalist at the Monroe Carell Jr. Children’s Hospital at Vanderbilt, said she will also bring a teamwork-focused perspective to the SHM board.
She could be expected to view everything through the lens of inpatient pediatrics, but that’s not her style.
“I think we have so many similarities and so many things that [pediatric and adult hospitalists] can partner to do together,” she said. “We all are involved in, for example, medication reconciliation or discharge-management planning or postacute care follow-up. There’s a lot of synergy, and I think we can learn so much from each other.”
Dr. Rehm, who chairs SHM’s Pediatrics Committee and the 2017 Pediatric Hospital Medicine meeting, pointed out that working well with others is a natural skill set for hospitalists.
“Collaboration is probably my biggest skill set and that of many hospital medicine providers,” she said. “I think I do that in my job here at Vanderbilt in thinking about complicated patients that requirement multiple subspecialists and in bringing together people to figure out the question at hand. That is definitely my leadership style.”
If Dr. Rehm has one goal on the board, it is to become a little bit more like Dr. Thompson and focus on chapter development for pediatric hospitalists.
“I’m really interested in engaging with members to better understand the struggles on the front line so that we can make sure that, as an organization, we’re offering a brand of things that our membership needs,” she said. “So, I’m really looking forward to becoming more involved in the chapter engagement and development. The Nashville chapter is getting re-engaged now and I’m excited to be involved.”
To prepare for her debut board meeting in Las Vegas, Dr. Rehm attended SHM board meetings at the group’s Philadelphia headquarters over the past two years.
“I’ve been lucky enough to attend the fall board meeting in Philadelphia and observe the board in action, and I think that has helped me get to know some of the current board members and to have a little bit of a vision of what the meetings will be like,” she said.
FDA approves betrixaban for VTE prophylaxis
Betrixaban, a factor Xa inhibitor, has been approved for the prophylaxis of venous thromboembolism (VTE) in at-risk adult patients hospitalized with an acute illness, according to an announcement from the Food and Drug Administration.
Approval was based on results from a randomized, double-blind clinical trial in which over 7,000 hospitalized patients at risk for VTE received either extended-duration betrixaban (35-42 days) or short duration enoxaparin (6-14 days), a low molecular weight heparin administered subcutaneously. The rate of deep vein thrombosis, nonfatal pulmonary embolism, or VTE-related death was 4.4% among patients receiving betrixaban and 6% among patients receiving enoxaparin (relative risk, 0.75; 95% confidence interval: 0.61, 0.91).
The recommended dosage for betrixaban is 80 mg per day for 35-42 days at the same time every day with food, after a dose of 160 mg on the first day of treatment.
Betrixaban will be marketed as Bevyxxa by Portola.
Find the full FDA announcement and prescribing information on the FDA website.
Betrixaban, a factor Xa inhibitor, has been approved for the prophylaxis of venous thromboembolism (VTE) in at-risk adult patients hospitalized with an acute illness, according to an announcement from the Food and Drug Administration.
Approval was based on results from a randomized, double-blind clinical trial in which over 7,000 hospitalized patients at risk for VTE received either extended-duration betrixaban (35-42 days) or short duration enoxaparin (6-14 days), a low molecular weight heparin administered subcutaneously. The rate of deep vein thrombosis, nonfatal pulmonary embolism, or VTE-related death was 4.4% among patients receiving betrixaban and 6% among patients receiving enoxaparin (relative risk, 0.75; 95% confidence interval: 0.61, 0.91).
The recommended dosage for betrixaban is 80 mg per day for 35-42 days at the same time every day with food, after a dose of 160 mg on the first day of treatment.
Betrixaban will be marketed as Bevyxxa by Portola.
Find the full FDA announcement and prescribing information on the FDA website.
Betrixaban, a factor Xa inhibitor, has been approved for the prophylaxis of venous thromboembolism (VTE) in at-risk adult patients hospitalized with an acute illness, according to an announcement from the Food and Drug Administration.
Approval was based on results from a randomized, double-blind clinical trial in which over 7,000 hospitalized patients at risk for VTE received either extended-duration betrixaban (35-42 days) or short duration enoxaparin (6-14 days), a low molecular weight heparin administered subcutaneously. The rate of deep vein thrombosis, nonfatal pulmonary embolism, or VTE-related death was 4.4% among patients receiving betrixaban and 6% among patients receiving enoxaparin (relative risk, 0.75; 95% confidence interval: 0.61, 0.91).
The recommended dosage for betrixaban is 80 mg per day for 35-42 days at the same time every day with food, after a dose of 160 mg on the first day of treatment.
Betrixaban will be marketed as Bevyxxa by Portola.
Find the full FDA announcement and prescribing information on the FDA website.
Follow five tips to mitigate opioid prescribing risks
CHICAGO – As the epidemic of opioid addiction and overdose deaths continues to surge, state and federal authorities are keeping a close eye on physicians who prescribe controlled substances.
Experts offer the following guidance on how well-meaning doctors can avoid coming under scrutiny for prescribing opioids and successfully manage investigations and audits.
1. Know who’s on the radar: The Drug Enforcement Agency (DEA) compiles a “black list” yearly of physicians and health care providers they plan to target for audits, said Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law. For 2017, the list includes physicians who have prior noncompliance records, providers who specialize in pain management, and those who dispense or administer large quantities of controlled substances.
In addition, family physicians, psychiatrists, and other specialists who come under investigation by a state medical board because of suspected inappropriate prescribing or reporting violations may also come under the purview of federal authorities, Ms. Mazina said.
“If they come on the medical board radar, they may come on the [DEA’s] radar as well,” she said during the interview. “They just have to watch how many prescriptions they write for controlled substances and make sure they are legitimate prescriptions.”
2. Maintain proper records: Poor record keeping is a top reason that the DEA investigates health care providers for potential prescribing violations, said Dennis A. Wichern, a DEA agent with the Chicago Field Division. Federal law requires that registered practitioners who store or dispense controlled substances keep records of controlled substances coming in and out of the practice. That includes physicians who hand out samples of controlled substances to patients and also pertains to samples provided to doctors by pharmaceutical companies.
Records should include whether the inventory was taken at the beginning or close of business, names of controlled substances, each finished form of the substances, the number of dosage units of each finished form in the commercial container, the number of commercial containers of each finished form, and disposition of the controlled substances.
Law requires that physicians take a new inventory of all controlled substances on hand every 2 years. Doctors are not required to keep records of controlled substances that are merely prescribed, unless such substances are prescribed in the course of maintenance or detoxification treatment.
Ms. Mazina notes that there are many software platforms that can assist practices with proper inventory and record keeping for opioids and other drugs.
3. Check the state database: Before prescribing opioids, check your state’s prescription drug monitoring program (PDMP) database, advises Ms. Mazina. At least 37 states have operational PDMPs that receive and distribute controlled substance prescription information to authorized users. About 11 states have enacted legislation to establish a PDMP, but some databases are not fully operational.
A state’s PDMP can reveal whether patients may be obtaining multiple controlled substance prescriptions from different doctors or doctor-shopping, Ms. Mazina said. Such due diligence helps inform treatment decisions and can assist a doctor’s case if a medical board or DEA investigation later arises.
“Even if your state law does not require you to check a patient’s history prior to prescribing, you have to check it to protect yourself,” she said. “If you want to avoid controlled substances problems, PDMP is the way to go.”
4. Establish an audit response plan: Have an audit response plan ready to roll should an inquiry arise, experts advise. The policies ensure that only approved information is released to authorities, and that all staff members are on the same page about how to react to audits, Ms. Mazina said.
Plans should clearly state what information can be collected and what data should be kept confidential. Financial information, for example, should be off limits, she said. Government agents are entitled to inventory, dispensary data, and records of receipts.
“Agents very often do the mirror image of the database, and they get too much information,” she said. “You don’t want to [allow] that.”
Train staff members how to respond to government authorities seeking audit information, and explain they have the right to refuse being interviewed, Ms. Mazina said.
“Train your employees on what’s going to happen if the DEA comes in,” she said. “If I don’t have clear policies and procedures, and I’m not trained, I might disclose everything and blame someone. That puts everyone in a [bad] position, because [authorities] will record everything and use it against [the practice].”
5. Confer with the experts: It doesn’t hurt to consult with other medical professionals, such as emergency physicians or pain management specialists, for practical advice on inventory policies or software suggestions. But when it comes to staying updated on new drug laws and regulations, confer with a health law attorney or compliance officer, Ms. Mazina said. The DEA website also includes useful information about recent laws and rules pertaining to prescription drugs, as does the Centers for Disease Control and Prevention website.
If an investigation or audit emerges, work with an attorney as early as possible. Often, practices wait until too late after an investigation begins to contact legal counsel, Ms. Mazina noted. The earlier an attorney gets involved, the sooner that person can build a strong case for the practice and work toward the best resolution.
“Very often, the physician thinks they are right, and there’s nothing for them to fear,” she said. “There is something for you to fear. There’s a lot at stake.”
[email protected]
On Twitter @legal_med
CHICAGO – As the epidemic of opioid addiction and overdose deaths continues to surge, state and federal authorities are keeping a close eye on physicians who prescribe controlled substances.
Experts offer the following guidance on how well-meaning doctors can avoid coming under scrutiny for prescribing opioids and successfully manage investigations and audits.
1. Know who’s on the radar: The Drug Enforcement Agency (DEA) compiles a “black list” yearly of physicians and health care providers they plan to target for audits, said Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law. For 2017, the list includes physicians who have prior noncompliance records, providers who specialize in pain management, and those who dispense or administer large quantities of controlled substances.
In addition, family physicians, psychiatrists, and other specialists who come under investigation by a state medical board because of suspected inappropriate prescribing or reporting violations may also come under the purview of federal authorities, Ms. Mazina said.
“If they come on the medical board radar, they may come on the [DEA’s] radar as well,” she said during the interview. “They just have to watch how many prescriptions they write for controlled substances and make sure they are legitimate prescriptions.”
2. Maintain proper records: Poor record keeping is a top reason that the DEA investigates health care providers for potential prescribing violations, said Dennis A. Wichern, a DEA agent with the Chicago Field Division. Federal law requires that registered practitioners who store or dispense controlled substances keep records of controlled substances coming in and out of the practice. That includes physicians who hand out samples of controlled substances to patients and also pertains to samples provided to doctors by pharmaceutical companies.
Records should include whether the inventory was taken at the beginning or close of business, names of controlled substances, each finished form of the substances, the number of dosage units of each finished form in the commercial container, the number of commercial containers of each finished form, and disposition of the controlled substances.
Law requires that physicians take a new inventory of all controlled substances on hand every 2 years. Doctors are not required to keep records of controlled substances that are merely prescribed, unless such substances are prescribed in the course of maintenance or detoxification treatment.
Ms. Mazina notes that there are many software platforms that can assist practices with proper inventory and record keeping for opioids and other drugs.
3. Check the state database: Before prescribing opioids, check your state’s prescription drug monitoring program (PDMP) database, advises Ms. Mazina. At least 37 states have operational PDMPs that receive and distribute controlled substance prescription information to authorized users. About 11 states have enacted legislation to establish a PDMP, but some databases are not fully operational.
A state’s PDMP can reveal whether patients may be obtaining multiple controlled substance prescriptions from different doctors or doctor-shopping, Ms. Mazina said. Such due diligence helps inform treatment decisions and can assist a doctor’s case if a medical board or DEA investigation later arises.
“Even if your state law does not require you to check a patient’s history prior to prescribing, you have to check it to protect yourself,” she said. “If you want to avoid controlled substances problems, PDMP is the way to go.”
4. Establish an audit response plan: Have an audit response plan ready to roll should an inquiry arise, experts advise. The policies ensure that only approved information is released to authorities, and that all staff members are on the same page about how to react to audits, Ms. Mazina said.
Plans should clearly state what information can be collected and what data should be kept confidential. Financial information, for example, should be off limits, she said. Government agents are entitled to inventory, dispensary data, and records of receipts.
“Agents very often do the mirror image of the database, and they get too much information,” she said. “You don’t want to [allow] that.”
Train staff members how to respond to government authorities seeking audit information, and explain they have the right to refuse being interviewed, Ms. Mazina said.
“Train your employees on what’s going to happen if the DEA comes in,” she said. “If I don’t have clear policies and procedures, and I’m not trained, I might disclose everything and blame someone. That puts everyone in a [bad] position, because [authorities] will record everything and use it against [the practice].”
5. Confer with the experts: It doesn’t hurt to consult with other medical professionals, such as emergency physicians or pain management specialists, for practical advice on inventory policies or software suggestions. But when it comes to staying updated on new drug laws and regulations, confer with a health law attorney or compliance officer, Ms. Mazina said. The DEA website also includes useful information about recent laws and rules pertaining to prescription drugs, as does the Centers for Disease Control and Prevention website.
If an investigation or audit emerges, work with an attorney as early as possible. Often, practices wait until too late after an investigation begins to contact legal counsel, Ms. Mazina noted. The earlier an attorney gets involved, the sooner that person can build a strong case for the practice and work toward the best resolution.
“Very often, the physician thinks they are right, and there’s nothing for them to fear,” she said. “There is something for you to fear. There’s a lot at stake.”
[email protected]
On Twitter @legal_med
CHICAGO – As the epidemic of opioid addiction and overdose deaths continues to surge, state and federal authorities are keeping a close eye on physicians who prescribe controlled substances.
Experts offer the following guidance on how well-meaning doctors can avoid coming under scrutiny for prescribing opioids and successfully manage investigations and audits.
1. Know who’s on the radar: The Drug Enforcement Agency (DEA) compiles a “black list” yearly of physicians and health care providers they plan to target for audits, said Natalia Mazina, a San Francisco–based attorney who specializes in health and pharmacy law. For 2017, the list includes physicians who have prior noncompliance records, providers who specialize in pain management, and those who dispense or administer large quantities of controlled substances.
In addition, family physicians, psychiatrists, and other specialists who come under investigation by a state medical board because of suspected inappropriate prescribing or reporting violations may also come under the purview of federal authorities, Ms. Mazina said.
“If they come on the medical board radar, they may come on the [DEA’s] radar as well,” she said during the interview. “They just have to watch how many prescriptions they write for controlled substances and make sure they are legitimate prescriptions.”
2. Maintain proper records: Poor record keeping is a top reason that the DEA investigates health care providers for potential prescribing violations, said Dennis A. Wichern, a DEA agent with the Chicago Field Division. Federal law requires that registered practitioners who store or dispense controlled substances keep records of controlled substances coming in and out of the practice. That includes physicians who hand out samples of controlled substances to patients and also pertains to samples provided to doctors by pharmaceutical companies.
Records should include whether the inventory was taken at the beginning or close of business, names of controlled substances, each finished form of the substances, the number of dosage units of each finished form in the commercial container, the number of commercial containers of each finished form, and disposition of the controlled substances.
Law requires that physicians take a new inventory of all controlled substances on hand every 2 years. Doctors are not required to keep records of controlled substances that are merely prescribed, unless such substances are prescribed in the course of maintenance or detoxification treatment.
Ms. Mazina notes that there are many software platforms that can assist practices with proper inventory and record keeping for opioids and other drugs.
3. Check the state database: Before prescribing opioids, check your state’s prescription drug monitoring program (PDMP) database, advises Ms. Mazina. At least 37 states have operational PDMPs that receive and distribute controlled substance prescription information to authorized users. About 11 states have enacted legislation to establish a PDMP, but some databases are not fully operational.
A state’s PDMP can reveal whether patients may be obtaining multiple controlled substance prescriptions from different doctors or doctor-shopping, Ms. Mazina said. Such due diligence helps inform treatment decisions and can assist a doctor’s case if a medical board or DEA investigation later arises.
“Even if your state law does not require you to check a patient’s history prior to prescribing, you have to check it to protect yourself,” she said. “If you want to avoid controlled substances problems, PDMP is the way to go.”
4. Establish an audit response plan: Have an audit response plan ready to roll should an inquiry arise, experts advise. The policies ensure that only approved information is released to authorities, and that all staff members are on the same page about how to react to audits, Ms. Mazina said.
Plans should clearly state what information can be collected and what data should be kept confidential. Financial information, for example, should be off limits, she said. Government agents are entitled to inventory, dispensary data, and records of receipts.
“Agents very often do the mirror image of the database, and they get too much information,” she said. “You don’t want to [allow] that.”
Train staff members how to respond to government authorities seeking audit information, and explain they have the right to refuse being interviewed, Ms. Mazina said.
“Train your employees on what’s going to happen if the DEA comes in,” she said. “If I don’t have clear policies and procedures, and I’m not trained, I might disclose everything and blame someone. That puts everyone in a [bad] position, because [authorities] will record everything and use it against [the practice].”
5. Confer with the experts: It doesn’t hurt to consult with other medical professionals, such as emergency physicians or pain management specialists, for practical advice on inventory policies or software suggestions. But when it comes to staying updated on new drug laws and regulations, confer with a health law attorney or compliance officer, Ms. Mazina said. The DEA website also includes useful information about recent laws and rules pertaining to prescription drugs, as does the Centers for Disease Control and Prevention website.
If an investigation or audit emerges, work with an attorney as early as possible. Often, practices wait until too late after an investigation begins to contact legal counsel, Ms. Mazina noted. The earlier an attorney gets involved, the sooner that person can build a strong case for the practice and work toward the best resolution.
“Very often, the physician thinks they are right, and there’s nothing for them to fear,” she said. “There is something for you to fear. There’s a lot at stake.”
[email protected]
On Twitter @legal_med
AT THE PHYSICIANS LEGAL ISSUES CONFERENCE
For opioid-related hospitalizations, men and women are equal
Equality is not always a good thing, particularly with opioids.
In 2005, the rate of opioid-related inpatient hospital stays was 145.6 per 100,000 population for males of all ages and 127.8 for females of all ages. By 2014, however, equality had arrived: Females had a rate of 224.1 per 100,000, compared with 225 for males, according to the Agency for Healthcare Research and Quality. Those increases in hospital admissions work out to 75% for females and 55% for males.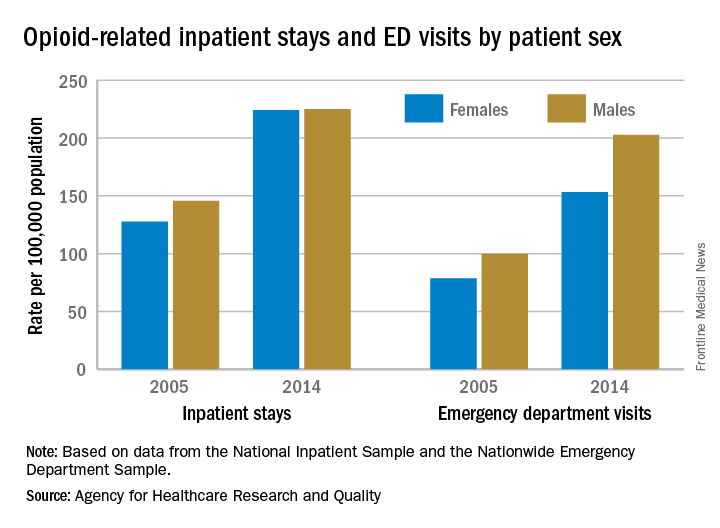
The states tell a similarly unequal story for opioid-related ED visits. In 2014, males had the higher rate in 23 states, and females had the higher rate in 7 states. (Washington, D.C., and 20 states do not participate in the State Emergency Department Databases and were not included in this analysis.)
Among the 30 participating states, Massachusetts had the highest visit rates for both males (598.8) and females (310.4), and Iowa had the lowest at 37 for males and 53.1 for females, AHRQ said.
The roles were reversed for opioid-related hospital admissions in the states in 2014: Females had the higher rate in 33 of the states participating in the State Inpatient Databases, compared with 11 states and the District of Columbia for males.
West Virginia had the highest rate for females at 371.2, and Washington, D.C., had the highest rate for males at 472. The lowest rates for both females (82.3) and males (63) were found in Iowa, according to the report.
Equality is not always a good thing, particularly with opioids.
In 2005, the rate of opioid-related inpatient hospital stays was 145.6 per 100,000 population for males of all ages and 127.8 for females of all ages. By 2014, however, equality had arrived: Females had a rate of 224.1 per 100,000, compared with 225 for males, according to the Agency for Healthcare Research and Quality. Those increases in hospital admissions work out to 75% for females and 55% for males.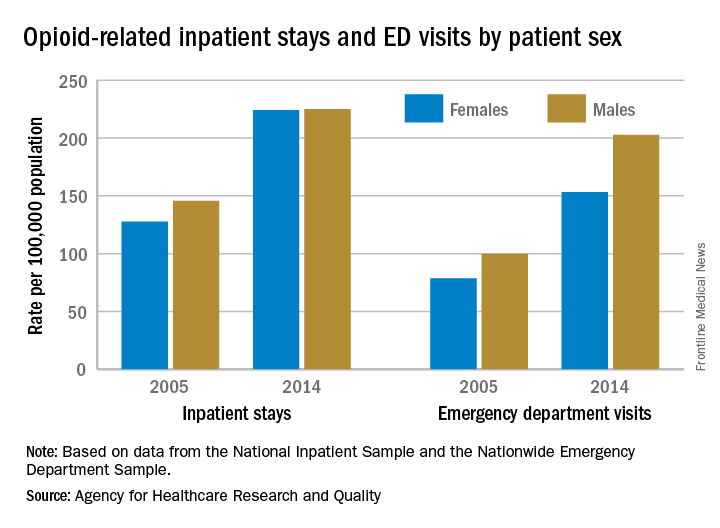
The states tell a similarly unequal story for opioid-related ED visits. In 2014, males had the higher rate in 23 states, and females had the higher rate in 7 states. (Washington, D.C., and 20 states do not participate in the State Emergency Department Databases and were not included in this analysis.)
Among the 30 participating states, Massachusetts had the highest visit rates for both males (598.8) and females (310.4), and Iowa had the lowest at 37 for males and 53.1 for females, AHRQ said.
The roles were reversed for opioid-related hospital admissions in the states in 2014: Females had the higher rate in 33 of the states participating in the State Inpatient Databases, compared with 11 states and the District of Columbia for males.
West Virginia had the highest rate for females at 371.2, and Washington, D.C., had the highest rate for males at 472. The lowest rates for both females (82.3) and males (63) were found in Iowa, according to the report.
Equality is not always a good thing, particularly with opioids.
In 2005, the rate of opioid-related inpatient hospital stays was 145.6 per 100,000 population for males of all ages and 127.8 for females of all ages. By 2014, however, equality had arrived: Females had a rate of 224.1 per 100,000, compared with 225 for males, according to the Agency for Healthcare Research and Quality. Those increases in hospital admissions work out to 75% for females and 55% for males.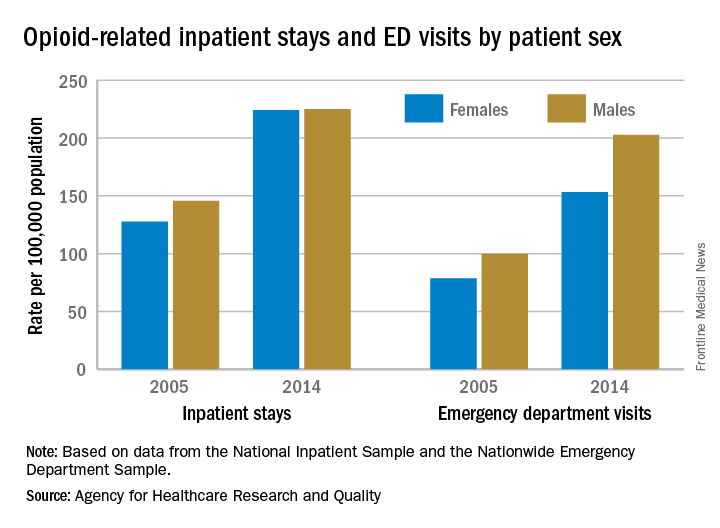
The states tell a similarly unequal story for opioid-related ED visits. In 2014, males had the higher rate in 23 states, and females had the higher rate in 7 states. (Washington, D.C., and 20 states do not participate in the State Emergency Department Databases and were not included in this analysis.)
Among the 30 participating states, Massachusetts had the highest visit rates for both males (598.8) and females (310.4), and Iowa had the lowest at 37 for males and 53.1 for females, AHRQ said.
The roles were reversed for opioid-related hospital admissions in the states in 2014: Females had the higher rate in 33 of the states participating in the State Inpatient Databases, compared with 11 states and the District of Columbia for males.
West Virginia had the highest rate for females at 371.2, and Washington, D.C., had the highest rate for males at 472. The lowest rates for both females (82.3) and males (63) were found in Iowa, according to the report.
Hospitalist meta-leader: Your new mission has arrived
If you are a hospitalist and leader in your health care organization, the ongoing controversies surrounding the Affordable Care Act repeal and replace campaign are unsettling. No matter your politics, Washington’s political drama and gamesmanship pose a genuine threat to the solvency of your hospital’s budget, services, workforce, and patients.
Health care has devolved into a political football, tossed from skirmish to skirmish. Political leaders warn of the implosion of the health care system as a political tactic, not an outcome that could cost and ruin lives. Both Democrats and Republicans hope that if or when that happens, it does so in ways that allow them to blame the other side. For them, this is a game of partisan advantage that wagers the well-being of your health care system.
For you, the situation remains predictably unpredictable. The future directives from Washington are unknowable. This makes your strategic planning – and health care leadership itself – a complex and puzzling task. Your job now is not simply leading your organization for today. Your more important mission is preparing your organization to perform in this unpredictable and perplexing future.
Forecasting is the life blood of leadership: Craft a vision and the work to achieve it; be mindful of the range of obstacles and opportunities; and know and coalesce your followers. The problem is that today’s prospects are loaded with puzzling twists and turns. The viability of both the private insurance market and public dollars are – maybe! – in future jeopardy. Patients and the workforce are understandably jittery. What is a hospitalist leader to do?
It is time to refresh your thinking, to take a big picture view of what is happening and to assess what can be done about it. There is a tendency for leaders to look at problems and then wonder how to fit solutions into their established organizational framework. In other words, solutions are cast into the mold of retaining what you have, ignoring larger options and innovative possibilities. Solutions are expected to adapt to the organization rather than the organization adapting to the solutions.
The hospitalist movement grew as early leaders – true innovators – recognized the problems of costly, inefficient and uncoordinated care. Rather than tinkering with what was, hospitalist leaders introduced a new and proactive model to provide care. It had to first prove itself and once it did, a once revolutionary idea evolved into an institutionalized solution.
No matter what emerges from the current policy debate, the national pressures on the health care system persist: rising expectations for access; decreasing patience for spending; increasing appetite for breakthrough technology; shifting workforce requirements; all combined with a population that is aging and more in need of care. These are meta-trends that will redefine how the health system operates and what it will achieve. What is a health care leader to do?
Think and act like a “meta-leader.” This framework, developed at the Harvard T.H. Chan School of Public Health, guides leaders facing complex and transformational problem solving. The prefix “meta-” encourages expansive analysis directed toward a wide range of options and opportunities. In keeping with the strategies employed by hospitalist pioneers, rather than building solutions around “what already is,” meta-leaders pursue “what could be.” In this way, solutions are designed and constructed to fit the problems they are intended to overcome.
There are three critical dimensions to the thinking and practices of meta-leadership.
The first is the Person of the meta-leader. This is who you are, your priorities and values. This is how other people regard your leadership, translated into the respect, trust, and “followership” you garner. Be a role model. This involves building your own confidence for the task at hand so that you gain and then foster the confidence of those you lead. As a meta-leader, you shape your mindset and that of others for innovation, sharpening the curiosity necessary for fostering discovery and exploration of new ideas. Be ready to take appropriate risks.
The second dimension of meta-leadership practice is the Situation. This is what is happening and what can be done about it. You did not create the complex circumstances that derive from the political showdown in Washington. However, it is your job to understand them and to develop effective strategies and operations in response. This is where the “think big” of meta-leadership comes into play. You distinguish the chasm between the adversarial policy confrontation in Washington and the collaborative solution building needed in your home institution. You want to set the stage to meaningfully coalesce the thinking, resources, and people in your organization. The invigorated shared mission is a health care system that leads into the future.
The third dimension of meta-leadership practice is about building the Connectivity needed to make that happen. This involves developing the communication, coordination, and cooperation necessary for constructing something new. Many of your answers lie within the walls of your organization, even the most innovative among them. This is where you sow adaptability and flexibility. It translates into necessary change and transformation. This is reorienting what you and others do and how you go about doing it, from shifts and adjustments to, when necessary, disruptive innovation.
A recent Harvard Business School and Harvard Medical School forum on health care innovation identified five imperatives for meeting innovation challenges in health care: 1) Creating value is the key aim for innovation and it requires a combination of care coordination along with communication; 2) Seek opportunities for process improvement that allows new ideas to be tested, accepting that failure is a step on the road to discovery; 3) Adopt a consumerism strategy for service organization that engages and involves active patients; 4) Decentralize problem solving to encourage field innovation and collaboration; and 5) Integrate new models into established institutions, introducing fresh thinking to replace outdated practices.
Meta-leadership is not a formula for an easy fix. While much remains unpredictable, an impending economic squeeze is a likely scenario. There is nothing easy about a shortage of dollars to serve more and more people in need of clinical care. This may very well be the prompt – today – that encourages the sort of innovative thinking and disruptive solution development that the future requires. Will you and your organization get ahead of this curve?
Your mission as a hospitalist meta-leader is in forging this process of discovery. Perceive what is going on through a wide lens. Orient yourself to emerging trends. Predict what is likely to emerge from this unpredictable policy environment. Take decisions and operationalize them in ways responsive to the circumstances at hand. And then communicate with your constituencies, not only to inform them of direction but also to learn from them what is working and what not. And then you start the process again, trying on ideas and practices, learning from them and through this continuous process, finding solutions that fit your situation at hand.
Health care meta-leaders today must keep both eyes firmly on their feet, to know that current operations are achieving necessary success. At the same time, they must also keep both eyes focused on the horizon, to ensure that when conditions change, their organizations are ready to adaptively innovate and transform.
Leonard J. Marcus, Ph.D. is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected]
If you are a hospitalist and leader in your health care organization, the ongoing controversies surrounding the Affordable Care Act repeal and replace campaign are unsettling. No matter your politics, Washington’s political drama and gamesmanship pose a genuine threat to the solvency of your hospital’s budget, services, workforce, and patients.
Health care has devolved into a political football, tossed from skirmish to skirmish. Political leaders warn of the implosion of the health care system as a political tactic, not an outcome that could cost and ruin lives. Both Democrats and Republicans hope that if or when that happens, it does so in ways that allow them to blame the other side. For them, this is a game of partisan advantage that wagers the well-being of your health care system.
For you, the situation remains predictably unpredictable. The future directives from Washington are unknowable. This makes your strategic planning – and health care leadership itself – a complex and puzzling task. Your job now is not simply leading your organization for today. Your more important mission is preparing your organization to perform in this unpredictable and perplexing future.
Forecasting is the life blood of leadership: Craft a vision and the work to achieve it; be mindful of the range of obstacles and opportunities; and know and coalesce your followers. The problem is that today’s prospects are loaded with puzzling twists and turns. The viability of both the private insurance market and public dollars are – maybe! – in future jeopardy. Patients and the workforce are understandably jittery. What is a hospitalist leader to do?
It is time to refresh your thinking, to take a big picture view of what is happening and to assess what can be done about it. There is a tendency for leaders to look at problems and then wonder how to fit solutions into their established organizational framework. In other words, solutions are cast into the mold of retaining what you have, ignoring larger options and innovative possibilities. Solutions are expected to adapt to the organization rather than the organization adapting to the solutions.
The hospitalist movement grew as early leaders – true innovators – recognized the problems of costly, inefficient and uncoordinated care. Rather than tinkering with what was, hospitalist leaders introduced a new and proactive model to provide care. It had to first prove itself and once it did, a once revolutionary idea evolved into an institutionalized solution.
No matter what emerges from the current policy debate, the national pressures on the health care system persist: rising expectations for access; decreasing patience for spending; increasing appetite for breakthrough technology; shifting workforce requirements; all combined with a population that is aging and more in need of care. These are meta-trends that will redefine how the health system operates and what it will achieve. What is a health care leader to do?
Think and act like a “meta-leader.” This framework, developed at the Harvard T.H. Chan School of Public Health, guides leaders facing complex and transformational problem solving. The prefix “meta-” encourages expansive analysis directed toward a wide range of options and opportunities. In keeping with the strategies employed by hospitalist pioneers, rather than building solutions around “what already is,” meta-leaders pursue “what could be.” In this way, solutions are designed and constructed to fit the problems they are intended to overcome.
There are three critical dimensions to the thinking and practices of meta-leadership.
The first is the Person of the meta-leader. This is who you are, your priorities and values. This is how other people regard your leadership, translated into the respect, trust, and “followership” you garner. Be a role model. This involves building your own confidence for the task at hand so that you gain and then foster the confidence of those you lead. As a meta-leader, you shape your mindset and that of others for innovation, sharpening the curiosity necessary for fostering discovery and exploration of new ideas. Be ready to take appropriate risks.
The second dimension of meta-leadership practice is the Situation. This is what is happening and what can be done about it. You did not create the complex circumstances that derive from the political showdown in Washington. However, it is your job to understand them and to develop effective strategies and operations in response. This is where the “think big” of meta-leadership comes into play. You distinguish the chasm between the adversarial policy confrontation in Washington and the collaborative solution building needed in your home institution. You want to set the stage to meaningfully coalesce the thinking, resources, and people in your organization. The invigorated shared mission is a health care system that leads into the future.
The third dimension of meta-leadership practice is about building the Connectivity needed to make that happen. This involves developing the communication, coordination, and cooperation necessary for constructing something new. Many of your answers lie within the walls of your organization, even the most innovative among them. This is where you sow adaptability and flexibility. It translates into necessary change and transformation. This is reorienting what you and others do and how you go about doing it, from shifts and adjustments to, when necessary, disruptive innovation.
A recent Harvard Business School and Harvard Medical School forum on health care innovation identified five imperatives for meeting innovation challenges in health care: 1) Creating value is the key aim for innovation and it requires a combination of care coordination along with communication; 2) Seek opportunities for process improvement that allows new ideas to be tested, accepting that failure is a step on the road to discovery; 3) Adopt a consumerism strategy for service organization that engages and involves active patients; 4) Decentralize problem solving to encourage field innovation and collaboration; and 5) Integrate new models into established institutions, introducing fresh thinking to replace outdated practices.
Meta-leadership is not a formula for an easy fix. While much remains unpredictable, an impending economic squeeze is a likely scenario. There is nothing easy about a shortage of dollars to serve more and more people in need of clinical care. This may very well be the prompt – today – that encourages the sort of innovative thinking and disruptive solution development that the future requires. Will you and your organization get ahead of this curve?
Your mission as a hospitalist meta-leader is in forging this process of discovery. Perceive what is going on through a wide lens. Orient yourself to emerging trends. Predict what is likely to emerge from this unpredictable policy environment. Take decisions and operationalize them in ways responsive to the circumstances at hand. And then communicate with your constituencies, not only to inform them of direction but also to learn from them what is working and what not. And then you start the process again, trying on ideas and practices, learning from them and through this continuous process, finding solutions that fit your situation at hand.
Health care meta-leaders today must keep both eyes firmly on their feet, to know that current operations are achieving necessary success. At the same time, they must also keep both eyes focused on the horizon, to ensure that when conditions change, their organizations are ready to adaptively innovate and transform.
Leonard J. Marcus, Ph.D. is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected]
If you are a hospitalist and leader in your health care organization, the ongoing controversies surrounding the Affordable Care Act repeal and replace campaign are unsettling. No matter your politics, Washington’s political drama and gamesmanship pose a genuine threat to the solvency of your hospital’s budget, services, workforce, and patients.
Health care has devolved into a political football, tossed from skirmish to skirmish. Political leaders warn of the implosion of the health care system as a political tactic, not an outcome that could cost and ruin lives. Both Democrats and Republicans hope that if or when that happens, it does so in ways that allow them to blame the other side. For them, this is a game of partisan advantage that wagers the well-being of your health care system.
For you, the situation remains predictably unpredictable. The future directives from Washington are unknowable. This makes your strategic planning – and health care leadership itself – a complex and puzzling task. Your job now is not simply leading your organization for today. Your more important mission is preparing your organization to perform in this unpredictable and perplexing future.
Forecasting is the life blood of leadership: Craft a vision and the work to achieve it; be mindful of the range of obstacles and opportunities; and know and coalesce your followers. The problem is that today’s prospects are loaded with puzzling twists and turns. The viability of both the private insurance market and public dollars are – maybe! – in future jeopardy. Patients and the workforce are understandably jittery. What is a hospitalist leader to do?
It is time to refresh your thinking, to take a big picture view of what is happening and to assess what can be done about it. There is a tendency for leaders to look at problems and then wonder how to fit solutions into their established organizational framework. In other words, solutions are cast into the mold of retaining what you have, ignoring larger options and innovative possibilities. Solutions are expected to adapt to the organization rather than the organization adapting to the solutions.
The hospitalist movement grew as early leaders – true innovators – recognized the problems of costly, inefficient and uncoordinated care. Rather than tinkering with what was, hospitalist leaders introduced a new and proactive model to provide care. It had to first prove itself and once it did, a once revolutionary idea evolved into an institutionalized solution.
No matter what emerges from the current policy debate, the national pressures on the health care system persist: rising expectations for access; decreasing patience for spending; increasing appetite for breakthrough technology; shifting workforce requirements; all combined with a population that is aging and more in need of care. These are meta-trends that will redefine how the health system operates and what it will achieve. What is a health care leader to do?
Think and act like a “meta-leader.” This framework, developed at the Harvard T.H. Chan School of Public Health, guides leaders facing complex and transformational problem solving. The prefix “meta-” encourages expansive analysis directed toward a wide range of options and opportunities. In keeping with the strategies employed by hospitalist pioneers, rather than building solutions around “what already is,” meta-leaders pursue “what could be.” In this way, solutions are designed and constructed to fit the problems they are intended to overcome.
There are three critical dimensions to the thinking and practices of meta-leadership.
The first is the Person of the meta-leader. This is who you are, your priorities and values. This is how other people regard your leadership, translated into the respect, trust, and “followership” you garner. Be a role model. This involves building your own confidence for the task at hand so that you gain and then foster the confidence of those you lead. As a meta-leader, you shape your mindset and that of others for innovation, sharpening the curiosity necessary for fostering discovery and exploration of new ideas. Be ready to take appropriate risks.
The second dimension of meta-leadership practice is the Situation. This is what is happening and what can be done about it. You did not create the complex circumstances that derive from the political showdown in Washington. However, it is your job to understand them and to develop effective strategies and operations in response. This is where the “think big” of meta-leadership comes into play. You distinguish the chasm between the adversarial policy confrontation in Washington and the collaborative solution building needed in your home institution. You want to set the stage to meaningfully coalesce the thinking, resources, and people in your organization. The invigorated shared mission is a health care system that leads into the future.
The third dimension of meta-leadership practice is about building the Connectivity needed to make that happen. This involves developing the communication, coordination, and cooperation necessary for constructing something new. Many of your answers lie within the walls of your organization, even the most innovative among them. This is where you sow adaptability and flexibility. It translates into necessary change and transformation. This is reorienting what you and others do and how you go about doing it, from shifts and adjustments to, when necessary, disruptive innovation.
A recent Harvard Business School and Harvard Medical School forum on health care innovation identified five imperatives for meeting innovation challenges in health care: 1) Creating value is the key aim for innovation and it requires a combination of care coordination along with communication; 2) Seek opportunities for process improvement that allows new ideas to be tested, accepting that failure is a step on the road to discovery; 3) Adopt a consumerism strategy for service organization that engages and involves active patients; 4) Decentralize problem solving to encourage field innovation and collaboration; and 5) Integrate new models into established institutions, introducing fresh thinking to replace outdated practices.
Meta-leadership is not a formula for an easy fix. While much remains unpredictable, an impending economic squeeze is a likely scenario. There is nothing easy about a shortage of dollars to serve more and more people in need of clinical care. This may very well be the prompt – today – that encourages the sort of innovative thinking and disruptive solution development that the future requires. Will you and your organization get ahead of this curve?
Your mission as a hospitalist meta-leader is in forging this process of discovery. Perceive what is going on through a wide lens. Orient yourself to emerging trends. Predict what is likely to emerge from this unpredictable policy environment. Take decisions and operationalize them in ways responsive to the circumstances at hand. And then communicate with your constituencies, not only to inform them of direction but also to learn from them what is working and what not. And then you start the process again, trying on ideas and practices, learning from them and through this continuous process, finding solutions that fit your situation at hand.
Health care meta-leaders today must keep both eyes firmly on their feet, to know that current operations are achieving necessary success. At the same time, they must also keep both eyes focused on the horizon, to ensure that when conditions change, their organizations are ready to adaptively innovate and transform.
Leonard J. Marcus, Ph.D. is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected]
Hospitalist movers and shakers - June/July 2017
Three members of the hospital medicine community – Thiruvoipati Nanda Kumar, MD; Anthony Aghenta, MD, MS, FACP; and Angela Aboutalib, MD – recently were honored for their work by the International Association of HealthCare Professionals, earning spots in its publication, The Leading Physicians of the World.
Hospitalist and internist Dr. Nanda Kumar serves patients at Vibra Hospital in Redding, Calif., where he is also a clinical associate professor at the University of California at Davis. He is a member of both the Society of Hospital Medicine and the American Diabetes Association.
Dr. Aghenta is a 17-year veteran internist who currently serves as medical director for Coronado Healthcare Center in Phoenix. There, he also is affiliated with St. Joseph’s Hospital and Medical Center. A member of SHM, Dr. Aghenta also has the title of Fellow of the American College of Physicians.
Dr. Aboutalib, whose experience as an internist includes expertise in hospital medicine, serves as hospitalist and medical director of clinical operations at U.S. Acute Care Solutions, Canton, Ohio. Previously, this member of the American College of Physicians served South Physicians as a hospitalist at Mercy Hospital in Chicago.
Andrew Dunn, MD, MPH, FACP, SFHM, recently was named chair-elect of the Board of Regents of the American College of Physicians (ACP), the national organization of internists. He assumed the role at the start of the ACP’s annual scientific meeting held in San Diego, March 30–April 1.
Susan Herson, MD, has been named the new chief of staff at the Bath, N.Y., Veterans Affairs Medical Center. Dr. Herson comes to Bath from the Sioux Falls (S.D.) VA, where she was a hospitalist, a hospitalist-clinician educator, and medical director of clinical documentation improvement, while also serving as clinical assistant professor for New York Medical College and medical director at Norwalk (Conn.) Hospital.
Dr. Herson served in the U.S. Navy, doing her training at Walter Reed Medical Center, Bethesda, Md. She was a general medical officer while stationed at U.S. Marine Corps Base Camp Lejeune in Jacksonville, N.C.
Chad Whelan, MD, has been elevated to president of the Loyola (Ill.) University Medical Center, moving up from his chair as senior vice president and chief medical officer. This longtime hospitalist also serves as a professor of medicine in the Loyola Chicago Stritch School of Medicine.
Kevin Tulipana, DO, recently was promoted to medical director of hospital medicine at Cancer Treatment Centers of America’s Southwest Regional Medical Center in Tulsa, Okla. Previously, Dr. Tulipana was a hospitalist in the special care unit at CTCA Tulsa.
Mustafa Sardini, MD, has been named Envision Physician Services’ 2017 Hospital Medicine Physician of the Year. Dr. Sardini is the site medical director as Baylor Scott & White Medical Center, Sunnyvale, Texas. EPS presents the award to a hospitalist who peers deem as a leader in the industry.
Business moves
Physicians’ Alliance, (PAL) recently announced plans to partner with Penn State Health. As the largest independent physician group in Lancaster County, Pa., they will bring its more than 120 physicians, hospitalists, and dieticians to central Pennsylvania giant Penn State.
The alliance will allow patients of PAL physicians access to advanced care at Milton S. Hershey Medical Center and Penn State Children’s Hospital in Hershey.
Envision Healthcare, Greenwood Village, Colo. has created the Envision Physical Services (EPS) as a result of a merger with AmSurg ambulatory surgical center in December 2016. EPS combines EmCare and Sheridan Healthcare’s physician services divisions.
EPS specializes in hospital medicine, anesthesia, emergency medicine, radiology, and surgical services.
Three members of the hospital medicine community – Thiruvoipati Nanda Kumar, MD; Anthony Aghenta, MD, MS, FACP; and Angela Aboutalib, MD – recently were honored for their work by the International Association of HealthCare Professionals, earning spots in its publication, The Leading Physicians of the World.
Hospitalist and internist Dr. Nanda Kumar serves patients at Vibra Hospital in Redding, Calif., where he is also a clinical associate professor at the University of California at Davis. He is a member of both the Society of Hospital Medicine and the American Diabetes Association.
Dr. Aghenta is a 17-year veteran internist who currently serves as medical director for Coronado Healthcare Center in Phoenix. There, he also is affiliated with St. Joseph’s Hospital and Medical Center. A member of SHM, Dr. Aghenta also has the title of Fellow of the American College of Physicians.
Dr. Aboutalib, whose experience as an internist includes expertise in hospital medicine, serves as hospitalist and medical director of clinical operations at U.S. Acute Care Solutions, Canton, Ohio. Previously, this member of the American College of Physicians served South Physicians as a hospitalist at Mercy Hospital in Chicago.
Andrew Dunn, MD, MPH, FACP, SFHM, recently was named chair-elect of the Board of Regents of the American College of Physicians (ACP), the national organization of internists. He assumed the role at the start of the ACP’s annual scientific meeting held in San Diego, March 30–April 1.
Susan Herson, MD, has been named the new chief of staff at the Bath, N.Y., Veterans Affairs Medical Center. Dr. Herson comes to Bath from the Sioux Falls (S.D.) VA, where she was a hospitalist, a hospitalist-clinician educator, and medical director of clinical documentation improvement, while also serving as clinical assistant professor for New York Medical College and medical director at Norwalk (Conn.) Hospital.
Dr. Herson served in the U.S. Navy, doing her training at Walter Reed Medical Center, Bethesda, Md. She was a general medical officer while stationed at U.S. Marine Corps Base Camp Lejeune in Jacksonville, N.C.
Chad Whelan, MD, has been elevated to president of the Loyola (Ill.) University Medical Center, moving up from his chair as senior vice president and chief medical officer. This longtime hospitalist also serves as a professor of medicine in the Loyola Chicago Stritch School of Medicine.
Kevin Tulipana, DO, recently was promoted to medical director of hospital medicine at Cancer Treatment Centers of America’s Southwest Regional Medical Center in Tulsa, Okla. Previously, Dr. Tulipana was a hospitalist in the special care unit at CTCA Tulsa.
Mustafa Sardini, MD, has been named Envision Physician Services’ 2017 Hospital Medicine Physician of the Year. Dr. Sardini is the site medical director as Baylor Scott & White Medical Center, Sunnyvale, Texas. EPS presents the award to a hospitalist who peers deem as a leader in the industry.
Business moves
Physicians’ Alliance, (PAL) recently announced plans to partner with Penn State Health. As the largest independent physician group in Lancaster County, Pa., they will bring its more than 120 physicians, hospitalists, and dieticians to central Pennsylvania giant Penn State.
The alliance will allow patients of PAL physicians access to advanced care at Milton S. Hershey Medical Center and Penn State Children’s Hospital in Hershey.
Envision Healthcare, Greenwood Village, Colo. has created the Envision Physical Services (EPS) as a result of a merger with AmSurg ambulatory surgical center in December 2016. EPS combines EmCare and Sheridan Healthcare’s physician services divisions.
EPS specializes in hospital medicine, anesthesia, emergency medicine, radiology, and surgical services.
Three members of the hospital medicine community – Thiruvoipati Nanda Kumar, MD; Anthony Aghenta, MD, MS, FACP; and Angela Aboutalib, MD – recently were honored for their work by the International Association of HealthCare Professionals, earning spots in its publication, The Leading Physicians of the World.
Hospitalist and internist Dr. Nanda Kumar serves patients at Vibra Hospital in Redding, Calif., where he is also a clinical associate professor at the University of California at Davis. He is a member of both the Society of Hospital Medicine and the American Diabetes Association.
Dr. Aghenta is a 17-year veteran internist who currently serves as medical director for Coronado Healthcare Center in Phoenix. There, he also is affiliated with St. Joseph’s Hospital and Medical Center. A member of SHM, Dr. Aghenta also has the title of Fellow of the American College of Physicians.
Dr. Aboutalib, whose experience as an internist includes expertise in hospital medicine, serves as hospitalist and medical director of clinical operations at U.S. Acute Care Solutions, Canton, Ohio. Previously, this member of the American College of Physicians served South Physicians as a hospitalist at Mercy Hospital in Chicago.
Andrew Dunn, MD, MPH, FACP, SFHM, recently was named chair-elect of the Board of Regents of the American College of Physicians (ACP), the national organization of internists. He assumed the role at the start of the ACP’s annual scientific meeting held in San Diego, March 30–April 1.
Susan Herson, MD, has been named the new chief of staff at the Bath, N.Y., Veterans Affairs Medical Center. Dr. Herson comes to Bath from the Sioux Falls (S.D.) VA, where she was a hospitalist, a hospitalist-clinician educator, and medical director of clinical documentation improvement, while also serving as clinical assistant professor for New York Medical College and medical director at Norwalk (Conn.) Hospital.
Dr. Herson served in the U.S. Navy, doing her training at Walter Reed Medical Center, Bethesda, Md. She was a general medical officer while stationed at U.S. Marine Corps Base Camp Lejeune in Jacksonville, N.C.
Chad Whelan, MD, has been elevated to president of the Loyola (Ill.) University Medical Center, moving up from his chair as senior vice president and chief medical officer. This longtime hospitalist also serves as a professor of medicine in the Loyola Chicago Stritch School of Medicine.
Kevin Tulipana, DO, recently was promoted to medical director of hospital medicine at Cancer Treatment Centers of America’s Southwest Regional Medical Center in Tulsa, Okla. Previously, Dr. Tulipana was a hospitalist in the special care unit at CTCA Tulsa.
Mustafa Sardini, MD, has been named Envision Physician Services’ 2017 Hospital Medicine Physician of the Year. Dr. Sardini is the site medical director as Baylor Scott & White Medical Center, Sunnyvale, Texas. EPS presents the award to a hospitalist who peers deem as a leader in the industry.
Business moves
Physicians’ Alliance, (PAL) recently announced plans to partner with Penn State Health. As the largest independent physician group in Lancaster County, Pa., they will bring its more than 120 physicians, hospitalists, and dieticians to central Pennsylvania giant Penn State.
The alliance will allow patients of PAL physicians access to advanced care at Milton S. Hershey Medical Center and Penn State Children’s Hospital in Hershey.
Envision Healthcare, Greenwood Village, Colo. has created the Envision Physical Services (EPS) as a result of a merger with AmSurg ambulatory surgical center in December 2016. EPS combines EmCare and Sheridan Healthcare’s physician services divisions.
EPS specializes in hospital medicine, anesthesia, emergency medicine, radiology, and surgical services.
Tipoffs that an infant hospitalized with pertussis may require ICU
MADRID – Infants hospitalized for pertussis are more likely to develop severe disease requiring pediatric ICU admission if they are experiencing apnea, are unvaccinated against pertussis, or are less than 2 months old, Maria Arranz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“The presence of these parameters on admission should warn us of possible severe disease,” said Dr. Arranz of Gregorio Maranon Hospital in Madrid.
Dr. Arranz presented a retrospective observational study of 101 children under 1 year of age who were hospitalized for pertussis at the Madrid tertiary center prior to the hospital’s 2016 shift to a strategy of maternal immunization during pregnancy as a means of preventing pertussis in infancy. Thirteen percent of the children required admission to the pediatric ICU and thus by definition had severe disease.
Half of infants in the study were not vaccinated against pertussis. That proved to be a powerful risk factor for severe disease requiring an ICU stay. Only 8% of children with severe pertussis were vaccinated, compared with a 58% vaccination rate among those who avoided the ICU.
Apneic pauses were noted in 67% of the severe disease group, compared with 28% of the infants who didn’t need the ICU.
The pertussis patients admitted to the pediatric ICU averaged 1 month of age, compared with age 2 months in the nonsevere group.
The maximum leukocyte, lymphocyte, and neutrophil counts during the hospital stay of the severe disease group averaged 23,600 cells/mm3, 18,000/mm3, and 5,000/mm3, respectively, significantly greater than the 15,300, 10,700, and 3,900 cells/mm3 in infants who did not require the ICU. Levels of all three cells also were higher at admission in the severe pertussis group than in those who didn’t make it to the ICU, albeit not statistically significantly so.
Dr. Arranz reported having no financial conflicts of interest regarding her study.
MADRID – Infants hospitalized for pertussis are more likely to develop severe disease requiring pediatric ICU admission if they are experiencing apnea, are unvaccinated against pertussis, or are less than 2 months old, Maria Arranz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“The presence of these parameters on admission should warn us of possible severe disease,” said Dr. Arranz of Gregorio Maranon Hospital in Madrid.
Dr. Arranz presented a retrospective observational study of 101 children under 1 year of age who were hospitalized for pertussis at the Madrid tertiary center prior to the hospital’s 2016 shift to a strategy of maternal immunization during pregnancy as a means of preventing pertussis in infancy. Thirteen percent of the children required admission to the pediatric ICU and thus by definition had severe disease.
Half of infants in the study were not vaccinated against pertussis. That proved to be a powerful risk factor for severe disease requiring an ICU stay. Only 8% of children with severe pertussis were vaccinated, compared with a 58% vaccination rate among those who avoided the ICU.
Apneic pauses were noted in 67% of the severe disease group, compared with 28% of the infants who didn’t need the ICU.
The pertussis patients admitted to the pediatric ICU averaged 1 month of age, compared with age 2 months in the nonsevere group.
The maximum leukocyte, lymphocyte, and neutrophil counts during the hospital stay of the severe disease group averaged 23,600 cells/mm3, 18,000/mm3, and 5,000/mm3, respectively, significantly greater than the 15,300, 10,700, and 3,900 cells/mm3 in infants who did not require the ICU. Levels of all three cells also were higher at admission in the severe pertussis group than in those who didn’t make it to the ICU, albeit not statistically significantly so.
Dr. Arranz reported having no financial conflicts of interest regarding her study.
MADRID – Infants hospitalized for pertussis are more likely to develop severe disease requiring pediatric ICU admission if they are experiencing apnea, are unvaccinated against pertussis, or are less than 2 months old, Maria Arranz, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“The presence of these parameters on admission should warn us of possible severe disease,” said Dr. Arranz of Gregorio Maranon Hospital in Madrid.
Dr. Arranz presented a retrospective observational study of 101 children under 1 year of age who were hospitalized for pertussis at the Madrid tertiary center prior to the hospital’s 2016 shift to a strategy of maternal immunization during pregnancy as a means of preventing pertussis in infancy. Thirteen percent of the children required admission to the pediatric ICU and thus by definition had severe disease.
Half of infants in the study were not vaccinated against pertussis. That proved to be a powerful risk factor for severe disease requiring an ICU stay. Only 8% of children with severe pertussis were vaccinated, compared with a 58% vaccination rate among those who avoided the ICU.
Apneic pauses were noted in 67% of the severe disease group, compared with 28% of the infants who didn’t need the ICU.
The pertussis patients admitted to the pediatric ICU averaged 1 month of age, compared with age 2 months in the nonsevere group.
The maximum leukocyte, lymphocyte, and neutrophil counts during the hospital stay of the severe disease group averaged 23,600 cells/mm3, 18,000/mm3, and 5,000/mm3, respectively, significantly greater than the 15,300, 10,700, and 3,900 cells/mm3 in infants who did not require the ICU. Levels of all three cells also were higher at admission in the severe pertussis group than in those who didn’t make it to the ICU, albeit not statistically significantly so.
Dr. Arranz reported having no financial conflicts of interest regarding her study.
AT ESPID 2017
Key clinical point:
Major finding: Among infants hospitalized for pertussis, apneic pauses were present in two-thirds of those with severe disease, ultimately resulting in admission to the pediatric ICU, compared with 28% of those who didn’t require an ICU stay.
Data source: This retrospective observational study sought to identify factors associated with severe pertussis requiring an ICU stay in a group of 101 Spanish infants hospitalized with the disease.
Disclosures: The presenter reported having no financial conflicts of interest regarding her study.

















