User login
In Case You Missed It: COVID
FDA limits use of J&J COVID vaccine over blood clot risk
In a statement issued May 5, the FDA said the J&J vaccine should only be given to people 18 and older who don’t have access to other vaccines or for whom other vaccines are not clinically appropriate. People 18 and older can also get the J&J vaccine if they choose to because they wouldn’t otherwise receive any vaccine, the FDA said.
The FDA statement was similar to the recommendation made in December by a Centers for Disease Control and Prevention committee of experts.
The FDA said the decision was made after more information was shared about the occurrence of a rare blood clotting condition, thrombosis with thrombocytopenia syndrome (TTS), 1 or 2 weeks after people received the J&J vaccine. The finding “warrants limiting the authorized use of the vaccine,” the FDA said.
“We recognize that the Janssen COVID-19 vaccine still has a role in the current pandemic response in the United States and across the global community,” Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said in the statement.
“Our action reflects our updated analysis of the risk of TTS following administration of this vaccine and limits the use of the vaccine to certain individuals.”
The CDC says 16.9 million people are fully vaccinated with the J&J vaccine, compared with 76.5 million with Moderna and 126.3 million with Pfizer.
Through March 18, the CDC and FDA have detected 60 confirmed cases of TTS, including 9 fatal cases, ABC News reported.
The J&J vaccine was granted emergency authorization in February 2021. Health authorities hoped it would help spread vaccines across the nation because it only required one initial dose and didn’t need to be stored at extremely cold temperatures, unlike the two-dose Pfizer and Moderna vaccines.
But 2 months after authorization, the government paused its use for 10 days because of reports of TTS. In December 2021, the CDC’s Advisory Committee on Immunization Practices said the Pfizer and Moderna vaccines were preferred over J&J because J&J carried the rare risk of blood clots and bleeding in the brain.
The FDA said the cause of the blood clotting is not known. But the “known and potential benefits of the vaccine” outweigh the risks for those people now allowed to receive it, the FDA said.
A version of this article first appeared on WebMD.com.
In a statement issued May 5, the FDA said the J&J vaccine should only be given to people 18 and older who don’t have access to other vaccines or for whom other vaccines are not clinically appropriate. People 18 and older can also get the J&J vaccine if they choose to because they wouldn’t otherwise receive any vaccine, the FDA said.
The FDA statement was similar to the recommendation made in December by a Centers for Disease Control and Prevention committee of experts.
The FDA said the decision was made after more information was shared about the occurrence of a rare blood clotting condition, thrombosis with thrombocytopenia syndrome (TTS), 1 or 2 weeks after people received the J&J vaccine. The finding “warrants limiting the authorized use of the vaccine,” the FDA said.
“We recognize that the Janssen COVID-19 vaccine still has a role in the current pandemic response in the United States and across the global community,” Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said in the statement.
“Our action reflects our updated analysis of the risk of TTS following administration of this vaccine and limits the use of the vaccine to certain individuals.”
The CDC says 16.9 million people are fully vaccinated with the J&J vaccine, compared with 76.5 million with Moderna and 126.3 million with Pfizer.
Through March 18, the CDC and FDA have detected 60 confirmed cases of TTS, including 9 fatal cases, ABC News reported.
The J&J vaccine was granted emergency authorization in February 2021. Health authorities hoped it would help spread vaccines across the nation because it only required one initial dose and didn’t need to be stored at extremely cold temperatures, unlike the two-dose Pfizer and Moderna vaccines.
But 2 months after authorization, the government paused its use for 10 days because of reports of TTS. In December 2021, the CDC’s Advisory Committee on Immunization Practices said the Pfizer and Moderna vaccines were preferred over J&J because J&J carried the rare risk of blood clots and bleeding in the brain.
The FDA said the cause of the blood clotting is not known. But the “known and potential benefits of the vaccine” outweigh the risks for those people now allowed to receive it, the FDA said.
A version of this article first appeared on WebMD.com.
In a statement issued May 5, the FDA said the J&J vaccine should only be given to people 18 and older who don’t have access to other vaccines or for whom other vaccines are not clinically appropriate. People 18 and older can also get the J&J vaccine if they choose to because they wouldn’t otherwise receive any vaccine, the FDA said.
The FDA statement was similar to the recommendation made in December by a Centers for Disease Control and Prevention committee of experts.
The FDA said the decision was made after more information was shared about the occurrence of a rare blood clotting condition, thrombosis with thrombocytopenia syndrome (TTS), 1 or 2 weeks after people received the J&J vaccine. The finding “warrants limiting the authorized use of the vaccine,” the FDA said.
“We recognize that the Janssen COVID-19 vaccine still has a role in the current pandemic response in the United States and across the global community,” Peter Marks, MD, director of the FDA’s Center for Biologics Evaluation and Research, said in the statement.
“Our action reflects our updated analysis of the risk of TTS following administration of this vaccine and limits the use of the vaccine to certain individuals.”
The CDC says 16.9 million people are fully vaccinated with the J&J vaccine, compared with 76.5 million with Moderna and 126.3 million with Pfizer.
Through March 18, the CDC and FDA have detected 60 confirmed cases of TTS, including 9 fatal cases, ABC News reported.
The J&J vaccine was granted emergency authorization in February 2021. Health authorities hoped it would help spread vaccines across the nation because it only required one initial dose and didn’t need to be stored at extremely cold temperatures, unlike the two-dose Pfizer and Moderna vaccines.
But 2 months after authorization, the government paused its use for 10 days because of reports of TTS. In December 2021, the CDC’s Advisory Committee on Immunization Practices said the Pfizer and Moderna vaccines were preferred over J&J because J&J carried the rare risk of blood clots and bleeding in the brain.
The FDA said the cause of the blood clotting is not known. But the “known and potential benefits of the vaccine” outweigh the risks for those people now allowed to receive it, the FDA said.
A version of this article first appeared on WebMD.com.
Second COVID booster: Who should receive it and when?
The more boosters the better? Data from Israel show that immune protection in elderly people is strengthened even further after a fourth dose. Karl Lauterbach, MD, German minister of health, recently pleaded for a second booster for those aged 18 years and older, and he pushed for a European Union–wide recommendation. He has not been able to implement this yet.
Just as before, Germany’s Standing Committee on Vaccination (STIKO) is only recommending the second booster for people aged 70 years and older, the European Medicines Agency (EMA) is recommending the fourth vaccination for everyone aged 80 years and older, and the United States has set the general age limit at 50 years.
Specialists remain skeptical about expanding the availability of the second booster. “From an immunologic perspective, people under the age of 70 with a healthy immune system do not need this fourth vaccination,” said Christiane Falk, PhD, head of the Institute for Transplantation Immunology of the Hannover Medical School (Germany) and member of the German Federal Government COVID Expert Panel, at a Science Media Center press briefing.
After the second vaccination, young healthy people are sufficiently protected against a severe course of the disease. Dr. Falk sees the STIKO recommendation as feasible, since it can be worked with. People in nursing facilities or those with additional underlying conditions would be considered for a fourth vaccination, explained Dr. Falk.
Complete protection unrealistic
Achieving complete protection against infection through multiple boosters is not realistic, said Christoph Neumann-Haefelin, MD, head of the Working Group for Translational Virus Immunology at the Clinic for Internal Medicine II, University Hospital Freiburg, Germany. Therefore, this should not be pursued when discussing boosters. “The aim of the booster vaccination should be to protect different groups of people against severe courses of the disease,” said Dr. Neumann-Haefelin.
Neutralizing antibodies that are only present in high concentrations for a few weeks after infection or vaccination are sometimes able to prevent the infection on their own. The immunologic memory of B cells and T cells, which ensures long-lasting protection against severe courses of the disease, is at a high level after two doses, and a third dose increases the protection more.
While people with a weak immune system need significantly more vaccinations in a shorter period to receive the same protection, too many booster vaccinations against SARS-CoV-2 are not sensible for young healthy people.
Immune saturation effect
A recent study in macaques showed that an adjusted Omicron booster did not lead to higher antibody titers, compared with a usual booster. In January 2022, the EMA warned against frequent consecutive boosters that may no longer produce the desired immune response.
If someone receives a booster too early, a saturation effect can occur, warned Andreas Radbruch, PhD, scientific director of the German Rheumatism Research Center Berlin. “We know this from lots of experimental studies but also from lots of other vaccinations. For example, you cannot be vaccinated against tetanus twice at 3- or 4-week intervals. Nothing at all will happen the second time,” explained Dr. Radbruch.
If the same antigen is applied again and again at the same dose, the immune system is made so active that the antigen is directly intercepted and cannot have any new effect on the immune system. This mechanism has been known for a long time, said Dr. Radbruch.
‘Original antigenic sin’
Premature boosting could even be a handicap in the competition between immune response and virus, said Dr. Radbruch. This is due to the principle of “original antigenic sin.” If the immune system has already come into contact with a virus, contact with a new virus variant will cause it to form antibodies predominantly against those epitopes that were already present in the original virus. As a result of this, too many boosters can weaken protection against different variants.
“We have not actually observed this with SARS-CoV-2, however,” said Dr. Radbruch. “Immunity is always extremely broad. With a double or triple vaccination, all previously existing variants are covered by an affinity-matured immune system.”
Dr. Neumann-Haefelin confirmed this and added that all virus mutations, including Omicron, have different epitopes that affect the antibody response, but the T-cell response does not differ.
Dr. Radbruch said that the vaccine protection probably lasts for decades. Following an infection or vaccination, the antibody concentration in the bone marrow is similar to that achieved after a measles or tetanus vaccination. “The vaccination is already extremely efficient. You have protection at the same magnitude as for other infectious diseases or vaccinations, which is expected to last decades,” said Dr. Radbruch.
He clarified that the decrease in antibodies after vaccination and infection is normal and does not indicate a drop in protection. “Quantity and quality must not be confused here. There is simply less mass, but the grade of remaining antibody increases.”
In the competition around the virus antigens (referred to as affinity maturation), antibodies develop that bind 10 to 100 times better and are particularly protective against the virus. The immune system is thereby sustainably effective.
For whom and when?
Since the immune response is age dependent, it makes more sense to administer an additional booster to elderly people than to young people. Also included in this group, however, are people whose immune system still does not provide the same level of protection after the second or even third vaccination as that of younger, healthy people.
Dr. Radbruch noted that 4% of people older than 70 years exhibited autoantibodies against interferons. The effects are huge. “That is 20% of patients in an intensive care unit – and they all have a very poor prognosis,” said Dr. Radbruch. These people are extremely threatened by the virus. Multiple vaccinations are sensible for them.
Even people with a weak immune response benefit from multiple vaccinations, confirmed Dr. Neumann-Haefelin. “We are not seeing the antibody responses here that we see in young people with healthy immune systems until the third or fourth vaccination sometimes.”
Although for young healthy people, it is particularly important to ensure a sufficient period between vaccinations so that the affinity maturation is not impaired, those with a weak immune response can be vaccinated again as soon as after 3 months.
The “optimum minimum period of time” for people with healthy immune systems is 6 months, according to Dr. Neumann-Haefelin. “This is true for everyone in whom a proper response is expected.” The vaccine protection probably lasts significantly longer, and therefore, frequent boosting may not be necessary in the future, he said. The time separation also applies for medical personnel, for whom the Robert Koch Institute also recommends a second booster.
A version of this article first appeared on Medscape.com.
The more boosters the better? Data from Israel show that immune protection in elderly people is strengthened even further after a fourth dose. Karl Lauterbach, MD, German minister of health, recently pleaded for a second booster for those aged 18 years and older, and he pushed for a European Union–wide recommendation. He has not been able to implement this yet.
Just as before, Germany’s Standing Committee on Vaccination (STIKO) is only recommending the second booster for people aged 70 years and older, the European Medicines Agency (EMA) is recommending the fourth vaccination for everyone aged 80 years and older, and the United States has set the general age limit at 50 years.
Specialists remain skeptical about expanding the availability of the second booster. “From an immunologic perspective, people under the age of 70 with a healthy immune system do not need this fourth vaccination,” said Christiane Falk, PhD, head of the Institute for Transplantation Immunology of the Hannover Medical School (Germany) and member of the German Federal Government COVID Expert Panel, at a Science Media Center press briefing.
After the second vaccination, young healthy people are sufficiently protected against a severe course of the disease. Dr. Falk sees the STIKO recommendation as feasible, since it can be worked with. People in nursing facilities or those with additional underlying conditions would be considered for a fourth vaccination, explained Dr. Falk.
Complete protection unrealistic
Achieving complete protection against infection through multiple boosters is not realistic, said Christoph Neumann-Haefelin, MD, head of the Working Group for Translational Virus Immunology at the Clinic for Internal Medicine II, University Hospital Freiburg, Germany. Therefore, this should not be pursued when discussing boosters. “The aim of the booster vaccination should be to protect different groups of people against severe courses of the disease,” said Dr. Neumann-Haefelin.
Neutralizing antibodies that are only present in high concentrations for a few weeks after infection or vaccination are sometimes able to prevent the infection on their own. The immunologic memory of B cells and T cells, which ensures long-lasting protection against severe courses of the disease, is at a high level after two doses, and a third dose increases the protection more.
While people with a weak immune system need significantly more vaccinations in a shorter period to receive the same protection, too many booster vaccinations against SARS-CoV-2 are not sensible for young healthy people.
Immune saturation effect
A recent study in macaques showed that an adjusted Omicron booster did not lead to higher antibody titers, compared with a usual booster. In January 2022, the EMA warned against frequent consecutive boosters that may no longer produce the desired immune response.
If someone receives a booster too early, a saturation effect can occur, warned Andreas Radbruch, PhD, scientific director of the German Rheumatism Research Center Berlin. “We know this from lots of experimental studies but also from lots of other vaccinations. For example, you cannot be vaccinated against tetanus twice at 3- or 4-week intervals. Nothing at all will happen the second time,” explained Dr. Radbruch.
If the same antigen is applied again and again at the same dose, the immune system is made so active that the antigen is directly intercepted and cannot have any new effect on the immune system. This mechanism has been known for a long time, said Dr. Radbruch.
‘Original antigenic sin’
Premature boosting could even be a handicap in the competition between immune response and virus, said Dr. Radbruch. This is due to the principle of “original antigenic sin.” If the immune system has already come into contact with a virus, contact with a new virus variant will cause it to form antibodies predominantly against those epitopes that were already present in the original virus. As a result of this, too many boosters can weaken protection against different variants.
“We have not actually observed this with SARS-CoV-2, however,” said Dr. Radbruch. “Immunity is always extremely broad. With a double or triple vaccination, all previously existing variants are covered by an affinity-matured immune system.”
Dr. Neumann-Haefelin confirmed this and added that all virus mutations, including Omicron, have different epitopes that affect the antibody response, but the T-cell response does not differ.
Dr. Radbruch said that the vaccine protection probably lasts for decades. Following an infection or vaccination, the antibody concentration in the bone marrow is similar to that achieved after a measles or tetanus vaccination. “The vaccination is already extremely efficient. You have protection at the same magnitude as for other infectious diseases or vaccinations, which is expected to last decades,” said Dr. Radbruch.
He clarified that the decrease in antibodies after vaccination and infection is normal and does not indicate a drop in protection. “Quantity and quality must not be confused here. There is simply less mass, but the grade of remaining antibody increases.”
In the competition around the virus antigens (referred to as affinity maturation), antibodies develop that bind 10 to 100 times better and are particularly protective against the virus. The immune system is thereby sustainably effective.
For whom and when?
Since the immune response is age dependent, it makes more sense to administer an additional booster to elderly people than to young people. Also included in this group, however, are people whose immune system still does not provide the same level of protection after the second or even third vaccination as that of younger, healthy people.
Dr. Radbruch noted that 4% of people older than 70 years exhibited autoantibodies against interferons. The effects are huge. “That is 20% of patients in an intensive care unit – and they all have a very poor prognosis,” said Dr. Radbruch. These people are extremely threatened by the virus. Multiple vaccinations are sensible for them.
Even people with a weak immune response benefit from multiple vaccinations, confirmed Dr. Neumann-Haefelin. “We are not seeing the antibody responses here that we see in young people with healthy immune systems until the third or fourth vaccination sometimes.”
Although for young healthy people, it is particularly important to ensure a sufficient period between vaccinations so that the affinity maturation is not impaired, those with a weak immune response can be vaccinated again as soon as after 3 months.
The “optimum minimum period of time” for people with healthy immune systems is 6 months, according to Dr. Neumann-Haefelin. “This is true for everyone in whom a proper response is expected.” The vaccine protection probably lasts significantly longer, and therefore, frequent boosting may not be necessary in the future, he said. The time separation also applies for medical personnel, for whom the Robert Koch Institute also recommends a second booster.
A version of this article first appeared on Medscape.com.
The more boosters the better? Data from Israel show that immune protection in elderly people is strengthened even further after a fourth dose. Karl Lauterbach, MD, German minister of health, recently pleaded for a second booster for those aged 18 years and older, and he pushed for a European Union–wide recommendation. He has not been able to implement this yet.
Just as before, Germany’s Standing Committee on Vaccination (STIKO) is only recommending the second booster for people aged 70 years and older, the European Medicines Agency (EMA) is recommending the fourth vaccination for everyone aged 80 years and older, and the United States has set the general age limit at 50 years.
Specialists remain skeptical about expanding the availability of the second booster. “From an immunologic perspective, people under the age of 70 with a healthy immune system do not need this fourth vaccination,” said Christiane Falk, PhD, head of the Institute for Transplantation Immunology of the Hannover Medical School (Germany) and member of the German Federal Government COVID Expert Panel, at a Science Media Center press briefing.
After the second vaccination, young healthy people are sufficiently protected against a severe course of the disease. Dr. Falk sees the STIKO recommendation as feasible, since it can be worked with. People in nursing facilities or those with additional underlying conditions would be considered for a fourth vaccination, explained Dr. Falk.
Complete protection unrealistic
Achieving complete protection against infection through multiple boosters is not realistic, said Christoph Neumann-Haefelin, MD, head of the Working Group for Translational Virus Immunology at the Clinic for Internal Medicine II, University Hospital Freiburg, Germany. Therefore, this should not be pursued when discussing boosters. “The aim of the booster vaccination should be to protect different groups of people against severe courses of the disease,” said Dr. Neumann-Haefelin.
Neutralizing antibodies that are only present in high concentrations for a few weeks after infection or vaccination are sometimes able to prevent the infection on their own. The immunologic memory of B cells and T cells, which ensures long-lasting protection against severe courses of the disease, is at a high level after two doses, and a third dose increases the protection more.
While people with a weak immune system need significantly more vaccinations in a shorter period to receive the same protection, too many booster vaccinations against SARS-CoV-2 are not sensible for young healthy people.
Immune saturation effect
A recent study in macaques showed that an adjusted Omicron booster did not lead to higher antibody titers, compared with a usual booster. In January 2022, the EMA warned against frequent consecutive boosters that may no longer produce the desired immune response.
If someone receives a booster too early, a saturation effect can occur, warned Andreas Radbruch, PhD, scientific director of the German Rheumatism Research Center Berlin. “We know this from lots of experimental studies but also from lots of other vaccinations. For example, you cannot be vaccinated against tetanus twice at 3- or 4-week intervals. Nothing at all will happen the second time,” explained Dr. Radbruch.
If the same antigen is applied again and again at the same dose, the immune system is made so active that the antigen is directly intercepted and cannot have any new effect on the immune system. This mechanism has been known for a long time, said Dr. Radbruch.
‘Original antigenic sin’
Premature boosting could even be a handicap in the competition between immune response and virus, said Dr. Radbruch. This is due to the principle of “original antigenic sin.” If the immune system has already come into contact with a virus, contact with a new virus variant will cause it to form antibodies predominantly against those epitopes that were already present in the original virus. As a result of this, too many boosters can weaken protection against different variants.
“We have not actually observed this with SARS-CoV-2, however,” said Dr. Radbruch. “Immunity is always extremely broad. With a double or triple vaccination, all previously existing variants are covered by an affinity-matured immune system.”
Dr. Neumann-Haefelin confirmed this and added that all virus mutations, including Omicron, have different epitopes that affect the antibody response, but the T-cell response does not differ.
Dr. Radbruch said that the vaccine protection probably lasts for decades. Following an infection or vaccination, the antibody concentration in the bone marrow is similar to that achieved after a measles or tetanus vaccination. “The vaccination is already extremely efficient. You have protection at the same magnitude as for other infectious diseases or vaccinations, which is expected to last decades,” said Dr. Radbruch.
He clarified that the decrease in antibodies after vaccination and infection is normal and does not indicate a drop in protection. “Quantity and quality must not be confused here. There is simply less mass, but the grade of remaining antibody increases.”
In the competition around the virus antigens (referred to as affinity maturation), antibodies develop that bind 10 to 100 times better and are particularly protective against the virus. The immune system is thereby sustainably effective.
For whom and when?
Since the immune response is age dependent, it makes more sense to administer an additional booster to elderly people than to young people. Also included in this group, however, are people whose immune system still does not provide the same level of protection after the second or even third vaccination as that of younger, healthy people.
Dr. Radbruch noted that 4% of people older than 70 years exhibited autoantibodies against interferons. The effects are huge. “That is 20% of patients in an intensive care unit – and they all have a very poor prognosis,” said Dr. Radbruch. These people are extremely threatened by the virus. Multiple vaccinations are sensible for them.
Even people with a weak immune response benefit from multiple vaccinations, confirmed Dr. Neumann-Haefelin. “We are not seeing the antibody responses here that we see in young people with healthy immune systems until the third or fourth vaccination sometimes.”
Although for young healthy people, it is particularly important to ensure a sufficient period between vaccinations so that the affinity maturation is not impaired, those with a weak immune response can be vaccinated again as soon as after 3 months.
The “optimum minimum period of time” for people with healthy immune systems is 6 months, according to Dr. Neumann-Haefelin. “This is true for everyone in whom a proper response is expected.” The vaccine protection probably lasts significantly longer, and therefore, frequent boosting may not be necessary in the future, he said. The time separation also applies for medical personnel, for whom the Robert Koch Institute also recommends a second booster.
A version of this article first appeared on Medscape.com.
Impact of the COVID-19 Pandemic on Characteristics of Cutaneous Tumors Treated by Mohs Micrographic Surgery
The COVID-19 pandemic has brought about unprecedented changes and challenges to medical practice, including new public health measure legislation, local and national medical authority recommendations, nursing home and other ancillary health center protocols, and novel clinical decision-making considerations.1-3 In July 2020, the American Academy of Dermatology (AAD) addressed the changing landscape in dermatologic surgery, in part, by publishing recommendations on practice protocols during the COVID-19 pandemic.4 The guidelines recommended deferred treatment of superficial basal cell carcinomas (BCCs) for 6 months and all other BCC subtypes for 3 to 6 months. Furthermore, the guidelines recommended deferring treatment of all actinic keratoses and squamous cell carcinomas (SCCs) in situ “for now.” Squamous cell carcinoma treatment was to be guided by prognostic variables, such as location, size, depth, differentiation, perineural or lymphovascular invasion, recurrence, and immunosuppression. The guidelines recommended melanoma in situ (MIS) treatment be deferred for 3 months and invasive melanoma with histologic clearance obtained on excisional biopsy for 3 months. Other general recommendations included triaging clinics, rebooking according to clinical priority, using telehealth where possible, screening patients for COVID-19 signs and symptoms, staggering appointment times, spacing patient chairs, limiting support persons to 1, removing possible sources of infection in the waiting room, ensuring all patients sanitized their hands on arrival, rationing personal protective equipment, considering N95 masks for periorificial surgery, and using dissolving sutures to minimize multiple presentations.4
The American College of Mohs Surgery (ACMS), with guidance from its sister societies and the National Comprehensive Cancer Network, also communicated COVID-19–related recommendations to its members via intermittent newsletters during the initial peak of the pandemic in March and June 2020.5 General social distancing and office recommendations were similar to those released by the AAD. Recommendations for skin cancer treatment included deferring all BCCs for up to 3 months, with exceptions for highly symptomatic cancers and those with potential for substantial rapid growth. Squamous cell carcinoma in situ and small, well-differentiated SCCs were deferred, with priority placed on SCCs that were rapidly enlarging, poorly differentiated, demonstrated perineural invasion, were ulcerated, or were symptomatic. Patients with major risk factors were prioritized for treatment. Melanoma in situ was deferred for 2 to 3 months.5
State-level guidance from the Texas Dermatological Society (TDS) communicated in April 2020 stated that skin cancers with a potential for rapid progression and metastasis, such as melanoma and SCC, may require treatment as determined by the physician.6 The potential risk of serious adverse medical outcomes from not treating these cancers should be carefully documented. General practice measures for preventing the spread of COVID-19 were also recommended.6
In the setting of emerging novel recommendations, the practice of Mohs micrographic surgery (MMS) was notably impacted by the COVID-19 pandemic. According to one survey study from the United Kingdom conducted in April and May 2020, 49% of MMS services ceased and 36% were reduced during the infancy of the COVID-19 pandemic.7 Mohs micrographic surgery was largely suspended because of a lack of personal protective equipment and safety concerns, according to respondents. Additionally, respondents reported 77% of departments experienced redeployment of physicians and nurses to intensive care and medical wards. Thirty-five percent reported a reduction in the proportion of flaps/grafts to primary closures performed, 74% reported a decrease in outside referrals for repair by other specialties, 81% reported increased usage of dissolvable sutures, and 29% reported an increase in prophylactic antibiotic prescriptions.7 Another study from Italy reported a 46.5% reduction in dermatologic surgeries performed during the initial lockdown of the COVID-19 pandemic. Patients canceled 52.9% of procedures, and 12.5% were cancelled because of confirmed or suspected COVID-19 infection.8 Patient perceptions of MMS have also been impacted by the COVID-19 pandemic. According to a survey study of patients in the United Kingdom undergoing MMS during the pandemic, 47% were worried the hospital would cancel their surgery, 54% were anxious about using public transportation to attend their appointment, 30% were concerned about transmitting COVID-19 to household or family members, and 19% were worried about their ability to socially distance in the hospital.9
Evidence is also emerging that suggests the potential negative impact of the COVID-19 pandemic on morbidity and mortality outcomes in patients with skin cancer. One European study found an increase in Breslow thickness in primary melanomas diagnosed following the initial COVID-19 lockdown (0.88-mm average thickness prelockdown vs 1.96-mm average thickness postlockdown).10 An Italian study observed similar results—an increase in median Breslow thickness during the initial COVID-19 lockdown period of 0.5 mm from 0.4 mm during the prelockdown time period.11 Also providing evidence for potentially poor patient outcomes, one study modeled the impact of backlog in cutaneous melanoma referrals in the United Kingdom on patient survival and predicted 138 attributable lives lost for a 1-month delay and 1171 lives lost for a 6-month delay. The model further predicted a 3.1% to 12.5% reduction in 10-year net survival incurred from a 3-month delay in melanoma treatment, with the largest reduction seen in the patient population older than 80 years.12
Although the COVID-19 pandemic has been observed to impact MMS practice, patient perceptions, and clinical outcomes, it is unknown how the COVID-19 pandemic and corresponding rapidly evolving recommendations in dermatologic surgery have impacted the characteristics of cutaneous tumors treated by MMS.
Our study sought to determine the characteristics of skin cancers treated by MMS during the peak of government-mandated medical practice restrictions and business shutdowns in response to the COVID-19 pandemic and to compare them with characteristics of skin cancers treated during a prepandemic control period.
Methods
A retrospective chart review was conducted with approval from our institutional review board at the University of Texas Medical Branch (Galveston, Texas). Included in the chart review were all cutaneous malignancies treated by MMS at our outpatient, office-based surgical center from March 15, 2020, to April 30, 2020; this period corresponded to the peak of the COVID-19–related government-mandated medical and business shutdowns in our geographic region (southeast Texas). All cases performed were in compliance with national- and state-level guidance. Data were also collected for all cutaneous malignancies treated by MMS at our office from March 15, 2019, to April 30, 2019, as well as March 15, 2018, to April 30, 2018; these periods represented prepandemic control periods.
Data were collected for 516 surgeries performed on 458 patients and included patient age, preoperative clinical size, postoperative defect size, number of Mohs stages to achieve clearance, MMS appropriate use criteria (AUC) location (categorized as high-, medium-, or low-risk tumor location),13 and tumor type (categorized as BCC, SCC, or MIS). All variables were examined for unusual or missing values. Five patients with rare tumor types were observed and removed from the data set.
Statistical Analysis—An a priori power analysis for a power set at 0.85 determined sample sizes of 105 per group. Bivariate analyses were performed to compare variables for patients undergoing MMS during the pandemic vs prepandemic periods. Continuous outcome variables—Mohs stages, preoperative size, postoperative size, and patient age—were categorized for the analysis. Preoperative tumor size was dichotomized, with less than 2 cm2 as the referent category vs 2 cm2 or greater, and postoperative defect size was dichotomized with less than 3.6 cm2 as the referent category vs 3.6 cm2 or greater. Mohs stage was dichotomized as 1 stage (referent) vs more than 1 stage, and patient age was dichotomized as younger than 65 years (referent) vs 65 years or older.
Multivariate analyses were also performed to compare preoperative and postoperative sizes for patients undergoing MMS during the pandemic vs prepandemic periods, controlling for Mohs AUC location. Bivariate unadjusted and multivariate analyses were performed using a GENMOD logistic regression procedure in SAS (SAS Institute) to account for correlation in clustered data because a patient could be included for more than 1 surgery in the data set. Data were analyzed using SAS 9.4 for Windows. Because outcome variables tended to be skewed and not distributed normally, outcome variables were recorded as medians with interquartile ranges where possible to give a more accurate representation of the data than could be demonstrated with means with standard deviations.
Results
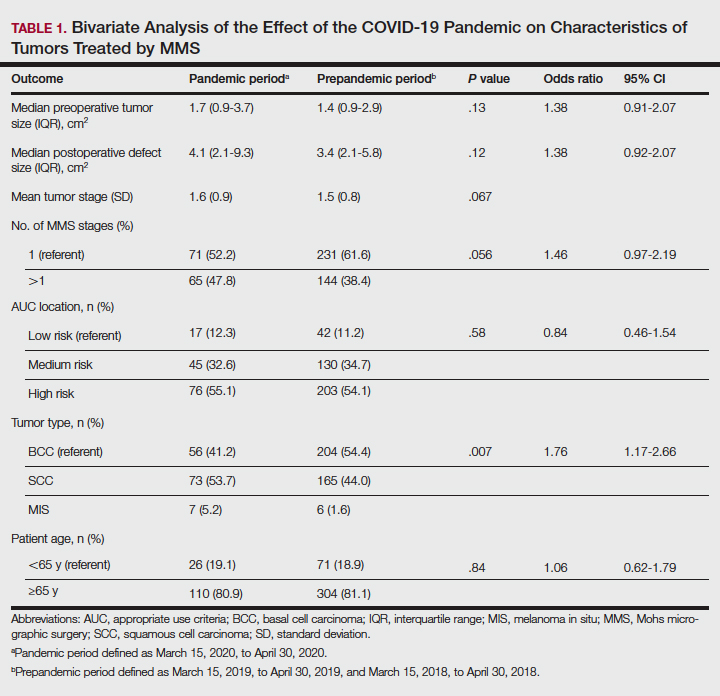
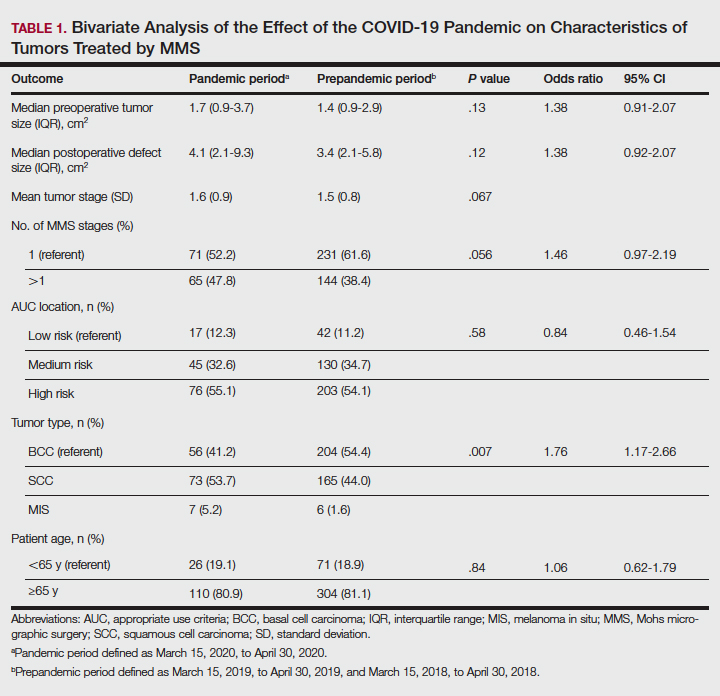
One hundred thirty-eight skin cancers were treated during the COVID-19 pandemic from March 15, 2020, to April 30, 2020, and 378 skin cancers were treated during the prepandemic control periods of March 15, 2019, to April 30, 2019, and March 15, 2018, to April 30, 2018. Tumor type treated during the pandemic period was more likely to be SCC or MIS (representing generally more severe tumor types) vs BCC when compared with the prepandemic periods, with an odds ratio (OR) of 1.763 (95% CI, 1.17-2.66). This outcome was statistically significant (P=.01).
Tumors treated during the pandemic period were more likely to have necessitated more than one Mohs stage for clearance compared to the prepandemic periods, though this difference was not statistically significant (OR, 1.461; 95% CI, 0.97-2.19; P=.056). Neither AUC location of treated tumors nor age were significantly different between prepandemic and pandemic periods (P=.58 and P=.84, respectively). Table 1 includes all bivariate analysis results.
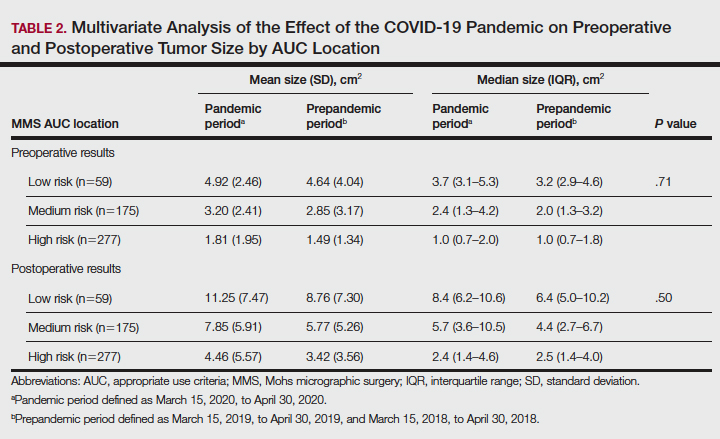
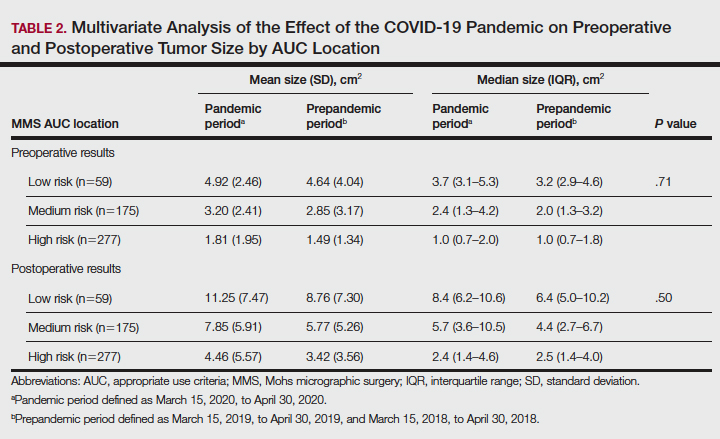
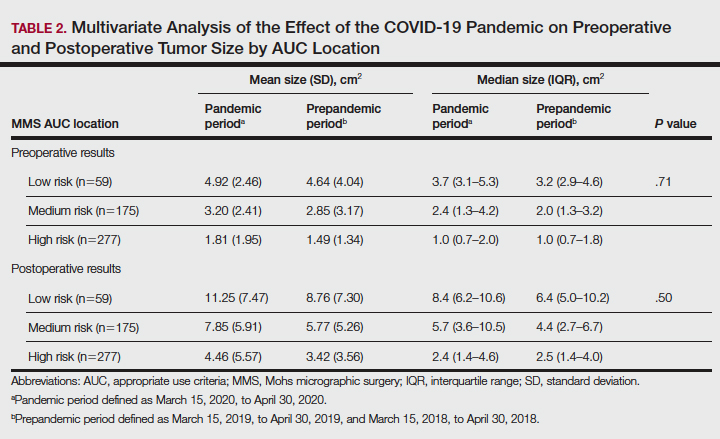
Additionally, although mean preoperative and postoperative sizes were larger for each AUC location during the pandemic vs prepandemic periods, these differences did not reach statistical significance on multivariate analysis (P=.71 and P=.50, respectively)(Table 2).
Comment
Our practice has followed best practice guidelines dictated by our governing professional societies during the COVID-19 pandemic in the treatment of skin cancers by MMS, specifically highly symptomatic BCCs (in accordance with ACMS guidance), SCCs with high-risk features (in accordance with AAD, ACMS, and TDS guidance), and tumors with high risk for progression and metastasis such as melanomas (in accordance with TDS guidance). Melanoma in situ was also treated during the COVID-19 pandemic in accordance with the latter TDS guidance, particularly in light of the potential for upstaging to melanoma following resection (a phenomenon demonstrated to occur in 5%–29% of biopsied MIS lesions).14
In following best practice guidelines, our results suggested tumors treated by MMS were more severe, as evidenced by a statistically significant higher proportion of SCC and MIS tumors (representing more severe tumor types) vs BCC when compared to the prepandemic period. Supporting this conclusion, we observed larger pretreatment and posttreatment tumor sizes for all AUC locations and more tumors necessitating 2 or more stages for clearance during the pandemic vs prepandemic periods, though these differences did not reach statistical significance. We postulate these findings may be attributed to allocation of finite medical resources to the treatment of larger and more aggressive skin cancers. Additionally, these findings may be explained, in part, by limitations on patient case load imposed by social distancing measures and governing body regulations in effect during the study period, including those put forth by the AAD, ACMS, and TDS. Of note, our practice observed no hospitalizations or 911 calls during the studied period. This suggests no allocation of precious hospital resources away from patients with COVID-19 in our treatment of high-risk skin cancers.
The changing characteristics of cutaneous tumors treated by MMS during the pandemic are of clinical relevance. Larger postoperative wound sizes as observed during the pandemic, albeit not statistically significant, presumably affect reconstructive decisions. With larger wounds tending to necessitate repair by techniques higher on the reconstructive ladder, greater patient morbidity and cost are expected.15 As the cost-effectiveness of dermatology services remains a critical issue, this is an area ripe for future follow-up research. Furthermore, our observation that tumors tended to necessitate 2 or more stages for clearance during the pandemic more often than prepandemic periods, though not statistically significant, presumably affected operating times. Longer operating times during the pandemic may be of importance when making clinical decisions for patients for whom limiting health care exposure may be of particular concern. With more SCC and MIS tumors being treated relative to BCCs during the pandemic, one might expect greater size and severity of the BCCs we observe in the proceeding months to years.
As the ongoing COVID-19 pandemic continues to impact the landscape of cutaneous oncology, the need for adaptability is imperative. With 3- and 6-month skin cancer treatment deferrals lapsed, uncertainty surrounds ideal management of existing and new skin cancers arising during the pandemic. This study adds to a growing body of literature elucidating the impact of the COVID-19 pandemic on MMS practice; however, further studies and a tincture of time are needed to guide future best practice standards.
Acknowledgment—The authors acknowledge Gwen Baillargeon, MS (Galveston, Texas), who was the statistician for this article.
- Gostin LO, Hodge JH. US emergency legal responses to novel coronavirus: balancing public health and civil liberties. JAMA. 2020;323:131-32.
- Barnett ML, Grabowski DC. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum. 2020;1:E200369.
- Perlis RH. Exercising heart and head in managing coronavirus disease 2019 in Wuhan. JAMA Netw Open. 2020;3:E204006.
- Sarkissian SA, Kim L, Veness M, et al. Recommendations on dermatologic surgery during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83:29-30.
- Billingsley EM. President’s message: COVID-19 (coronavirus) preparedness. American College of Mohs Surgery. March 30, 2020. Accessed April 14, 2022. https://www.mohscollege.org/UserFiles/AM20/Member%20Alert/COVIDAlert3March20.pdf
- Texas Dermatological Society Board of Directors. TDS Best Practice Recommendations—COVID-19. TDS Board Message. Texas Dermatologic Society. April 7, 2020.
- Nicholson P, Ali FR, Mallipeddi R. Impact of COVID‐19 on Mohs micrographic surgery: UK‐wide survey and recommendations for practice. Clin Exp Dermatol. 2020;45:901-902.
- Gironi LC, Boggio P, Giorgione R, et al. The impact of COVID-19 pandemics on dermatologic surgery: real-life data from the Italian Red-Zone [published online July 7, 2020]. J Dermatol Treat. doi:10.1080/09546634.2020.1789044
- Nicholson P, Ali FR, Craythorne E, et al. Patient perceptions of Mohs micrographic surgery during the COVID-19 pandemic and lessons for the next outbreak. Clin Exp Dermatol. 2021;46:179-180.
- Ricci F, Fania L, Paradisi A, et al. Delayed melanoma diagnosis in the COVID-19 era: increased breslow thickness in primary melanomas seen after the COVID-19 lockdown. J Eur Acad Dermatol Venereol. 2020;34:E778-E779.
- Gualdi G, Porreca A, Amoruso GF, et al. The effect of the COVID-19 lockdown on melanoma diagnosis in Italy. Clin Dermatol. 2021;39:911-919.
- Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21:1035-1044.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Higgins HW, Lee KC, Galan A, et al. Melanoma in situ: part II. histopathology, treatment, and clinical management. J Am Acad Dermatol. 2015;73:193-203.
- Cook J, Zitelli JA. Mohs micrographic surgery: a cost analysis. J Am Acad Dermatol. 1998;39:698-703.
The COVID-19 pandemic has brought about unprecedented changes and challenges to medical practice, including new public health measure legislation, local and national medical authority recommendations, nursing home and other ancillary health center protocols, and novel clinical decision-making considerations.1-3 In July 2020, the American Academy of Dermatology (AAD) addressed the changing landscape in dermatologic surgery, in part, by publishing recommendations on practice protocols during the COVID-19 pandemic.4 The guidelines recommended deferred treatment of superficial basal cell carcinomas (BCCs) for 6 months and all other BCC subtypes for 3 to 6 months. Furthermore, the guidelines recommended deferring treatment of all actinic keratoses and squamous cell carcinomas (SCCs) in situ “for now.” Squamous cell carcinoma treatment was to be guided by prognostic variables, such as location, size, depth, differentiation, perineural or lymphovascular invasion, recurrence, and immunosuppression. The guidelines recommended melanoma in situ (MIS) treatment be deferred for 3 months and invasive melanoma with histologic clearance obtained on excisional biopsy for 3 months. Other general recommendations included triaging clinics, rebooking according to clinical priority, using telehealth where possible, screening patients for COVID-19 signs and symptoms, staggering appointment times, spacing patient chairs, limiting support persons to 1, removing possible sources of infection in the waiting room, ensuring all patients sanitized their hands on arrival, rationing personal protective equipment, considering N95 masks for periorificial surgery, and using dissolving sutures to minimize multiple presentations.4
The American College of Mohs Surgery (ACMS), with guidance from its sister societies and the National Comprehensive Cancer Network, also communicated COVID-19–related recommendations to its members via intermittent newsletters during the initial peak of the pandemic in March and June 2020.5 General social distancing and office recommendations were similar to those released by the AAD. Recommendations for skin cancer treatment included deferring all BCCs for up to 3 months, with exceptions for highly symptomatic cancers and those with potential for substantial rapid growth. Squamous cell carcinoma in situ and small, well-differentiated SCCs were deferred, with priority placed on SCCs that were rapidly enlarging, poorly differentiated, demonstrated perineural invasion, were ulcerated, or were symptomatic. Patients with major risk factors were prioritized for treatment. Melanoma in situ was deferred for 2 to 3 months.5
State-level guidance from the Texas Dermatological Society (TDS) communicated in April 2020 stated that skin cancers with a potential for rapid progression and metastasis, such as melanoma and SCC, may require treatment as determined by the physician.6 The potential risk of serious adverse medical outcomes from not treating these cancers should be carefully documented. General practice measures for preventing the spread of COVID-19 were also recommended.6
In the setting of emerging novel recommendations, the practice of Mohs micrographic surgery (MMS) was notably impacted by the COVID-19 pandemic. According to one survey study from the United Kingdom conducted in April and May 2020, 49% of MMS services ceased and 36% were reduced during the infancy of the COVID-19 pandemic.7 Mohs micrographic surgery was largely suspended because of a lack of personal protective equipment and safety concerns, according to respondents. Additionally, respondents reported 77% of departments experienced redeployment of physicians and nurses to intensive care and medical wards. Thirty-five percent reported a reduction in the proportion of flaps/grafts to primary closures performed, 74% reported a decrease in outside referrals for repair by other specialties, 81% reported increased usage of dissolvable sutures, and 29% reported an increase in prophylactic antibiotic prescriptions.7 Another study from Italy reported a 46.5% reduction in dermatologic surgeries performed during the initial lockdown of the COVID-19 pandemic. Patients canceled 52.9% of procedures, and 12.5% were cancelled because of confirmed or suspected COVID-19 infection.8 Patient perceptions of MMS have also been impacted by the COVID-19 pandemic. According to a survey study of patients in the United Kingdom undergoing MMS during the pandemic, 47% were worried the hospital would cancel their surgery, 54% were anxious about using public transportation to attend their appointment, 30% were concerned about transmitting COVID-19 to household or family members, and 19% were worried about their ability to socially distance in the hospital.9
Evidence is also emerging that suggests the potential negative impact of the COVID-19 pandemic on morbidity and mortality outcomes in patients with skin cancer. One European study found an increase in Breslow thickness in primary melanomas diagnosed following the initial COVID-19 lockdown (0.88-mm average thickness prelockdown vs 1.96-mm average thickness postlockdown).10 An Italian study observed similar results—an increase in median Breslow thickness during the initial COVID-19 lockdown period of 0.5 mm from 0.4 mm during the prelockdown time period.11 Also providing evidence for potentially poor patient outcomes, one study modeled the impact of backlog in cutaneous melanoma referrals in the United Kingdom on patient survival and predicted 138 attributable lives lost for a 1-month delay and 1171 lives lost for a 6-month delay. The model further predicted a 3.1% to 12.5% reduction in 10-year net survival incurred from a 3-month delay in melanoma treatment, with the largest reduction seen in the patient population older than 80 years.12
Although the COVID-19 pandemic has been observed to impact MMS practice, patient perceptions, and clinical outcomes, it is unknown how the COVID-19 pandemic and corresponding rapidly evolving recommendations in dermatologic surgery have impacted the characteristics of cutaneous tumors treated by MMS.
Our study sought to determine the characteristics of skin cancers treated by MMS during the peak of government-mandated medical practice restrictions and business shutdowns in response to the COVID-19 pandemic and to compare them with characteristics of skin cancers treated during a prepandemic control period.
Methods
A retrospective chart review was conducted with approval from our institutional review board at the University of Texas Medical Branch (Galveston, Texas). Included in the chart review were all cutaneous malignancies treated by MMS at our outpatient, office-based surgical center from March 15, 2020, to April 30, 2020; this period corresponded to the peak of the COVID-19–related government-mandated medical and business shutdowns in our geographic region (southeast Texas). All cases performed were in compliance with national- and state-level guidance. Data were also collected for all cutaneous malignancies treated by MMS at our office from March 15, 2019, to April 30, 2019, as well as March 15, 2018, to April 30, 2018; these periods represented prepandemic control periods.
Data were collected for 516 surgeries performed on 458 patients and included patient age, preoperative clinical size, postoperative defect size, number of Mohs stages to achieve clearance, MMS appropriate use criteria (AUC) location (categorized as high-, medium-, or low-risk tumor location),13 and tumor type (categorized as BCC, SCC, or MIS). All variables were examined for unusual or missing values. Five patients with rare tumor types were observed and removed from the data set.
Statistical Analysis—An a priori power analysis for a power set at 0.85 determined sample sizes of 105 per group. Bivariate analyses were performed to compare variables for patients undergoing MMS during the pandemic vs prepandemic periods. Continuous outcome variables—Mohs stages, preoperative size, postoperative size, and patient age—were categorized for the analysis. Preoperative tumor size was dichotomized, with less than 2 cm2 as the referent category vs 2 cm2 or greater, and postoperative defect size was dichotomized with less than 3.6 cm2 as the referent category vs 3.6 cm2 or greater. Mohs stage was dichotomized as 1 stage (referent) vs more than 1 stage, and patient age was dichotomized as younger than 65 years (referent) vs 65 years or older.
Multivariate analyses were also performed to compare preoperative and postoperative sizes for patients undergoing MMS during the pandemic vs prepandemic periods, controlling for Mohs AUC location. Bivariate unadjusted and multivariate analyses were performed using a GENMOD logistic regression procedure in SAS (SAS Institute) to account for correlation in clustered data because a patient could be included for more than 1 surgery in the data set. Data were analyzed using SAS 9.4 for Windows. Because outcome variables tended to be skewed and not distributed normally, outcome variables were recorded as medians with interquartile ranges where possible to give a more accurate representation of the data than could be demonstrated with means with standard deviations.
Results
One hundred thirty-eight skin cancers were treated during the COVID-19 pandemic from March 15, 2020, to April 30, 2020, and 378 skin cancers were treated during the prepandemic control periods of March 15, 2019, to April 30, 2019, and March 15, 2018, to April 30, 2018. Tumor type treated during the pandemic period was more likely to be SCC or MIS (representing generally more severe tumor types) vs BCC when compared with the prepandemic periods, with an odds ratio (OR) of 1.763 (95% CI, 1.17-2.66). This outcome was statistically significant (P=.01).
Tumors treated during the pandemic period were more likely to have necessitated more than one Mohs stage for clearance compared to the prepandemic periods, though this difference was not statistically significant (OR, 1.461; 95% CI, 0.97-2.19; P=.056). Neither AUC location of treated tumors nor age were significantly different between prepandemic and pandemic periods (P=.58 and P=.84, respectively). Table 1 includes all bivariate analysis results.
Additionally, although mean preoperative and postoperative sizes were larger for each AUC location during the pandemic vs prepandemic periods, these differences did not reach statistical significance on multivariate analysis (P=.71 and P=.50, respectively)(Table 2).
Comment
Our practice has followed best practice guidelines dictated by our governing professional societies during the COVID-19 pandemic in the treatment of skin cancers by MMS, specifically highly symptomatic BCCs (in accordance with ACMS guidance), SCCs with high-risk features (in accordance with AAD, ACMS, and TDS guidance), and tumors with high risk for progression and metastasis such as melanomas (in accordance with TDS guidance). Melanoma in situ was also treated during the COVID-19 pandemic in accordance with the latter TDS guidance, particularly in light of the potential for upstaging to melanoma following resection (a phenomenon demonstrated to occur in 5%–29% of biopsied MIS lesions).14
In following best practice guidelines, our results suggested tumors treated by MMS were more severe, as evidenced by a statistically significant higher proportion of SCC and MIS tumors (representing more severe tumor types) vs BCC when compared to the prepandemic period. Supporting this conclusion, we observed larger pretreatment and posttreatment tumor sizes for all AUC locations and more tumors necessitating 2 or more stages for clearance during the pandemic vs prepandemic periods, though these differences did not reach statistical significance. We postulate these findings may be attributed to allocation of finite medical resources to the treatment of larger and more aggressive skin cancers. Additionally, these findings may be explained, in part, by limitations on patient case load imposed by social distancing measures and governing body regulations in effect during the study period, including those put forth by the AAD, ACMS, and TDS. Of note, our practice observed no hospitalizations or 911 calls during the studied period. This suggests no allocation of precious hospital resources away from patients with COVID-19 in our treatment of high-risk skin cancers.
The changing characteristics of cutaneous tumors treated by MMS during the pandemic are of clinical relevance. Larger postoperative wound sizes as observed during the pandemic, albeit not statistically significant, presumably affect reconstructive decisions. With larger wounds tending to necessitate repair by techniques higher on the reconstructive ladder, greater patient morbidity and cost are expected.15 As the cost-effectiveness of dermatology services remains a critical issue, this is an area ripe for future follow-up research. Furthermore, our observation that tumors tended to necessitate 2 or more stages for clearance during the pandemic more often than prepandemic periods, though not statistically significant, presumably affected operating times. Longer operating times during the pandemic may be of importance when making clinical decisions for patients for whom limiting health care exposure may be of particular concern. With more SCC and MIS tumors being treated relative to BCCs during the pandemic, one might expect greater size and severity of the BCCs we observe in the proceeding months to years.
As the ongoing COVID-19 pandemic continues to impact the landscape of cutaneous oncology, the need for adaptability is imperative. With 3- and 6-month skin cancer treatment deferrals lapsed, uncertainty surrounds ideal management of existing and new skin cancers arising during the pandemic. This study adds to a growing body of literature elucidating the impact of the COVID-19 pandemic on MMS practice; however, further studies and a tincture of time are needed to guide future best practice standards.
Acknowledgment—The authors acknowledge Gwen Baillargeon, MS (Galveston, Texas), who was the statistician for this article.
The COVID-19 pandemic has brought about unprecedented changes and challenges to medical practice, including new public health measure legislation, local and national medical authority recommendations, nursing home and other ancillary health center protocols, and novel clinical decision-making considerations.1-3 In July 2020, the American Academy of Dermatology (AAD) addressed the changing landscape in dermatologic surgery, in part, by publishing recommendations on practice protocols during the COVID-19 pandemic.4 The guidelines recommended deferred treatment of superficial basal cell carcinomas (BCCs) for 6 months and all other BCC subtypes for 3 to 6 months. Furthermore, the guidelines recommended deferring treatment of all actinic keratoses and squamous cell carcinomas (SCCs) in situ “for now.” Squamous cell carcinoma treatment was to be guided by prognostic variables, such as location, size, depth, differentiation, perineural or lymphovascular invasion, recurrence, and immunosuppression. The guidelines recommended melanoma in situ (MIS) treatment be deferred for 3 months and invasive melanoma with histologic clearance obtained on excisional biopsy for 3 months. Other general recommendations included triaging clinics, rebooking according to clinical priority, using telehealth where possible, screening patients for COVID-19 signs and symptoms, staggering appointment times, spacing patient chairs, limiting support persons to 1, removing possible sources of infection in the waiting room, ensuring all patients sanitized their hands on arrival, rationing personal protective equipment, considering N95 masks for periorificial surgery, and using dissolving sutures to minimize multiple presentations.4
The American College of Mohs Surgery (ACMS), with guidance from its sister societies and the National Comprehensive Cancer Network, also communicated COVID-19–related recommendations to its members via intermittent newsletters during the initial peak of the pandemic in March and June 2020.5 General social distancing and office recommendations were similar to those released by the AAD. Recommendations for skin cancer treatment included deferring all BCCs for up to 3 months, with exceptions for highly symptomatic cancers and those with potential for substantial rapid growth. Squamous cell carcinoma in situ and small, well-differentiated SCCs were deferred, with priority placed on SCCs that were rapidly enlarging, poorly differentiated, demonstrated perineural invasion, were ulcerated, or were symptomatic. Patients with major risk factors were prioritized for treatment. Melanoma in situ was deferred for 2 to 3 months.5
State-level guidance from the Texas Dermatological Society (TDS) communicated in April 2020 stated that skin cancers with a potential for rapid progression and metastasis, such as melanoma and SCC, may require treatment as determined by the physician.6 The potential risk of serious adverse medical outcomes from not treating these cancers should be carefully documented. General practice measures for preventing the spread of COVID-19 were also recommended.6
In the setting of emerging novel recommendations, the practice of Mohs micrographic surgery (MMS) was notably impacted by the COVID-19 pandemic. According to one survey study from the United Kingdom conducted in April and May 2020, 49% of MMS services ceased and 36% were reduced during the infancy of the COVID-19 pandemic.7 Mohs micrographic surgery was largely suspended because of a lack of personal protective equipment and safety concerns, according to respondents. Additionally, respondents reported 77% of departments experienced redeployment of physicians and nurses to intensive care and medical wards. Thirty-five percent reported a reduction in the proportion of flaps/grafts to primary closures performed, 74% reported a decrease in outside referrals for repair by other specialties, 81% reported increased usage of dissolvable sutures, and 29% reported an increase in prophylactic antibiotic prescriptions.7 Another study from Italy reported a 46.5% reduction in dermatologic surgeries performed during the initial lockdown of the COVID-19 pandemic. Patients canceled 52.9% of procedures, and 12.5% were cancelled because of confirmed or suspected COVID-19 infection.8 Patient perceptions of MMS have also been impacted by the COVID-19 pandemic. According to a survey study of patients in the United Kingdom undergoing MMS during the pandemic, 47% were worried the hospital would cancel their surgery, 54% were anxious about using public transportation to attend their appointment, 30% were concerned about transmitting COVID-19 to household or family members, and 19% were worried about their ability to socially distance in the hospital.9
Evidence is also emerging that suggests the potential negative impact of the COVID-19 pandemic on morbidity and mortality outcomes in patients with skin cancer. One European study found an increase in Breslow thickness in primary melanomas diagnosed following the initial COVID-19 lockdown (0.88-mm average thickness prelockdown vs 1.96-mm average thickness postlockdown).10 An Italian study observed similar results—an increase in median Breslow thickness during the initial COVID-19 lockdown period of 0.5 mm from 0.4 mm during the prelockdown time period.11 Also providing evidence for potentially poor patient outcomes, one study modeled the impact of backlog in cutaneous melanoma referrals in the United Kingdom on patient survival and predicted 138 attributable lives lost for a 1-month delay and 1171 lives lost for a 6-month delay. The model further predicted a 3.1% to 12.5% reduction in 10-year net survival incurred from a 3-month delay in melanoma treatment, with the largest reduction seen in the patient population older than 80 years.12
Although the COVID-19 pandemic has been observed to impact MMS practice, patient perceptions, and clinical outcomes, it is unknown how the COVID-19 pandemic and corresponding rapidly evolving recommendations in dermatologic surgery have impacted the characteristics of cutaneous tumors treated by MMS.
Our study sought to determine the characteristics of skin cancers treated by MMS during the peak of government-mandated medical practice restrictions and business shutdowns in response to the COVID-19 pandemic and to compare them with characteristics of skin cancers treated during a prepandemic control period.
Methods
A retrospective chart review was conducted with approval from our institutional review board at the University of Texas Medical Branch (Galveston, Texas). Included in the chart review were all cutaneous malignancies treated by MMS at our outpatient, office-based surgical center from March 15, 2020, to April 30, 2020; this period corresponded to the peak of the COVID-19–related government-mandated medical and business shutdowns in our geographic region (southeast Texas). All cases performed were in compliance with national- and state-level guidance. Data were also collected for all cutaneous malignancies treated by MMS at our office from March 15, 2019, to April 30, 2019, as well as March 15, 2018, to April 30, 2018; these periods represented prepandemic control periods.
Data were collected for 516 surgeries performed on 458 patients and included patient age, preoperative clinical size, postoperative defect size, number of Mohs stages to achieve clearance, MMS appropriate use criteria (AUC) location (categorized as high-, medium-, or low-risk tumor location),13 and tumor type (categorized as BCC, SCC, or MIS). All variables were examined for unusual or missing values. Five patients with rare tumor types were observed and removed from the data set.
Statistical Analysis—An a priori power analysis for a power set at 0.85 determined sample sizes of 105 per group. Bivariate analyses were performed to compare variables for patients undergoing MMS during the pandemic vs prepandemic periods. Continuous outcome variables—Mohs stages, preoperative size, postoperative size, and patient age—were categorized for the analysis. Preoperative tumor size was dichotomized, with less than 2 cm2 as the referent category vs 2 cm2 or greater, and postoperative defect size was dichotomized with less than 3.6 cm2 as the referent category vs 3.6 cm2 or greater. Mohs stage was dichotomized as 1 stage (referent) vs more than 1 stage, and patient age was dichotomized as younger than 65 years (referent) vs 65 years or older.
Multivariate analyses were also performed to compare preoperative and postoperative sizes for patients undergoing MMS during the pandemic vs prepandemic periods, controlling for Mohs AUC location. Bivariate unadjusted and multivariate analyses were performed using a GENMOD logistic regression procedure in SAS (SAS Institute) to account for correlation in clustered data because a patient could be included for more than 1 surgery in the data set. Data were analyzed using SAS 9.4 for Windows. Because outcome variables tended to be skewed and not distributed normally, outcome variables were recorded as medians with interquartile ranges where possible to give a more accurate representation of the data than could be demonstrated with means with standard deviations.
Results
One hundred thirty-eight skin cancers were treated during the COVID-19 pandemic from March 15, 2020, to April 30, 2020, and 378 skin cancers were treated during the prepandemic control periods of March 15, 2019, to April 30, 2019, and March 15, 2018, to April 30, 2018. Tumor type treated during the pandemic period was more likely to be SCC or MIS (representing generally more severe tumor types) vs BCC when compared with the prepandemic periods, with an odds ratio (OR) of 1.763 (95% CI, 1.17-2.66). This outcome was statistically significant (P=.01).
Tumors treated during the pandemic period were more likely to have necessitated more than one Mohs stage for clearance compared to the prepandemic periods, though this difference was not statistically significant (OR, 1.461; 95% CI, 0.97-2.19; P=.056). Neither AUC location of treated tumors nor age were significantly different between prepandemic and pandemic periods (P=.58 and P=.84, respectively). Table 1 includes all bivariate analysis results.
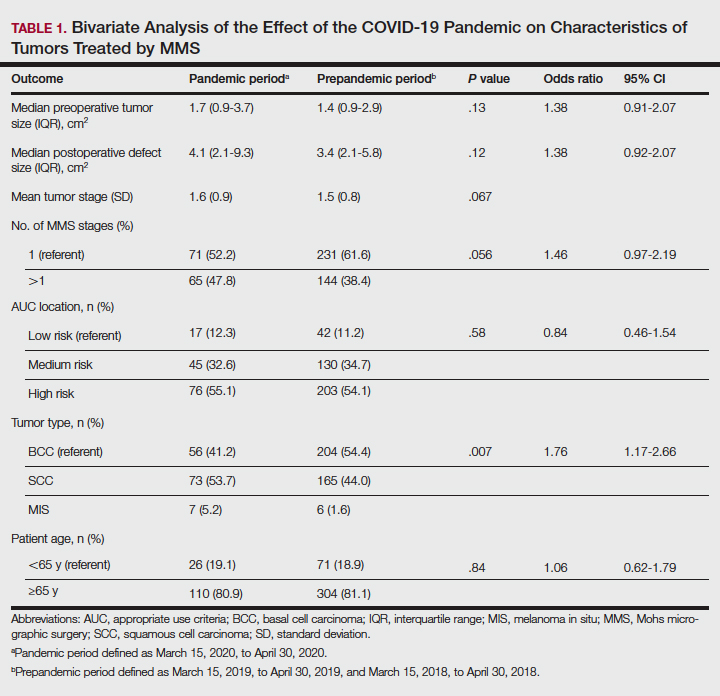
Additionally, although mean preoperative and postoperative sizes were larger for each AUC location during the pandemic vs prepandemic periods, these differences did not reach statistical significance on multivariate analysis (P=.71 and P=.50, respectively)(Table 2).
Comment
Our practice has followed best practice guidelines dictated by our governing professional societies during the COVID-19 pandemic in the treatment of skin cancers by MMS, specifically highly symptomatic BCCs (in accordance with ACMS guidance), SCCs with high-risk features (in accordance with AAD, ACMS, and TDS guidance), and tumors with high risk for progression and metastasis such as melanomas (in accordance with TDS guidance). Melanoma in situ was also treated during the COVID-19 pandemic in accordance with the latter TDS guidance, particularly in light of the potential for upstaging to melanoma following resection (a phenomenon demonstrated to occur in 5%–29% of biopsied MIS lesions).14
In following best practice guidelines, our results suggested tumors treated by MMS were more severe, as evidenced by a statistically significant higher proportion of SCC and MIS tumors (representing more severe tumor types) vs BCC when compared to the prepandemic period. Supporting this conclusion, we observed larger pretreatment and posttreatment tumor sizes for all AUC locations and more tumors necessitating 2 or more stages for clearance during the pandemic vs prepandemic periods, though these differences did not reach statistical significance. We postulate these findings may be attributed to allocation of finite medical resources to the treatment of larger and more aggressive skin cancers. Additionally, these findings may be explained, in part, by limitations on patient case load imposed by social distancing measures and governing body regulations in effect during the study period, including those put forth by the AAD, ACMS, and TDS. Of note, our practice observed no hospitalizations or 911 calls during the studied period. This suggests no allocation of precious hospital resources away from patients with COVID-19 in our treatment of high-risk skin cancers.
The changing characteristics of cutaneous tumors treated by MMS during the pandemic are of clinical relevance. Larger postoperative wound sizes as observed during the pandemic, albeit not statistically significant, presumably affect reconstructive decisions. With larger wounds tending to necessitate repair by techniques higher on the reconstructive ladder, greater patient morbidity and cost are expected.15 As the cost-effectiveness of dermatology services remains a critical issue, this is an area ripe for future follow-up research. Furthermore, our observation that tumors tended to necessitate 2 or more stages for clearance during the pandemic more often than prepandemic periods, though not statistically significant, presumably affected operating times. Longer operating times during the pandemic may be of importance when making clinical decisions for patients for whom limiting health care exposure may be of particular concern. With more SCC and MIS tumors being treated relative to BCCs during the pandemic, one might expect greater size and severity of the BCCs we observe in the proceeding months to years.
As the ongoing COVID-19 pandemic continues to impact the landscape of cutaneous oncology, the need for adaptability is imperative. With 3- and 6-month skin cancer treatment deferrals lapsed, uncertainty surrounds ideal management of existing and new skin cancers arising during the pandemic. This study adds to a growing body of literature elucidating the impact of the COVID-19 pandemic on MMS practice; however, further studies and a tincture of time are needed to guide future best practice standards.
Acknowledgment—The authors acknowledge Gwen Baillargeon, MS (Galveston, Texas), who was the statistician for this article.
- Gostin LO, Hodge JH. US emergency legal responses to novel coronavirus: balancing public health and civil liberties. JAMA. 2020;323:131-32.
- Barnett ML, Grabowski DC. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum. 2020;1:E200369.
- Perlis RH. Exercising heart and head in managing coronavirus disease 2019 in Wuhan. JAMA Netw Open. 2020;3:E204006.
- Sarkissian SA, Kim L, Veness M, et al. Recommendations on dermatologic surgery during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83:29-30.
- Billingsley EM. President’s message: COVID-19 (coronavirus) preparedness. American College of Mohs Surgery. March 30, 2020. Accessed April 14, 2022. https://www.mohscollege.org/UserFiles/AM20/Member%20Alert/COVIDAlert3March20.pdf
- Texas Dermatological Society Board of Directors. TDS Best Practice Recommendations—COVID-19. TDS Board Message. Texas Dermatologic Society. April 7, 2020.
- Nicholson P, Ali FR, Mallipeddi R. Impact of COVID‐19 on Mohs micrographic surgery: UK‐wide survey and recommendations for practice. Clin Exp Dermatol. 2020;45:901-902.
- Gironi LC, Boggio P, Giorgione R, et al. The impact of COVID-19 pandemics on dermatologic surgery: real-life data from the Italian Red-Zone [published online July 7, 2020]. J Dermatol Treat. doi:10.1080/09546634.2020.1789044
- Nicholson P, Ali FR, Craythorne E, et al. Patient perceptions of Mohs micrographic surgery during the COVID-19 pandemic and lessons for the next outbreak. Clin Exp Dermatol. 2021;46:179-180.
- Ricci F, Fania L, Paradisi A, et al. Delayed melanoma diagnosis in the COVID-19 era: increased breslow thickness in primary melanomas seen after the COVID-19 lockdown. J Eur Acad Dermatol Venereol. 2020;34:E778-E779.
- Gualdi G, Porreca A, Amoruso GF, et al. The effect of the COVID-19 lockdown on melanoma diagnosis in Italy. Clin Dermatol. 2021;39:911-919.
- Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21:1035-1044.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Higgins HW, Lee KC, Galan A, et al. Melanoma in situ: part II. histopathology, treatment, and clinical management. J Am Acad Dermatol. 2015;73:193-203.
- Cook J, Zitelli JA. Mohs micrographic surgery: a cost analysis. J Am Acad Dermatol. 1998;39:698-703.
- Gostin LO, Hodge JH. US emergency legal responses to novel coronavirus: balancing public health and civil liberties. JAMA. 2020;323:131-32.
- Barnett ML, Grabowski DC. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum. 2020;1:E200369.
- Perlis RH. Exercising heart and head in managing coronavirus disease 2019 in Wuhan. JAMA Netw Open. 2020;3:E204006.
- Sarkissian SA, Kim L, Veness M, et al. Recommendations on dermatologic surgery during the COVID-19 pandemic. J Am Acad Dermatol. 2020;83:29-30.
- Billingsley EM. President’s message: COVID-19 (coronavirus) preparedness. American College of Mohs Surgery. March 30, 2020. Accessed April 14, 2022. https://www.mohscollege.org/UserFiles/AM20/Member%20Alert/COVIDAlert3March20.pdf
- Texas Dermatological Society Board of Directors. TDS Best Practice Recommendations—COVID-19. TDS Board Message. Texas Dermatologic Society. April 7, 2020.
- Nicholson P, Ali FR, Mallipeddi R. Impact of COVID‐19 on Mohs micrographic surgery: UK‐wide survey and recommendations for practice. Clin Exp Dermatol. 2020;45:901-902.
- Gironi LC, Boggio P, Giorgione R, et al. The impact of COVID-19 pandemics on dermatologic surgery: real-life data from the Italian Red-Zone [published online July 7, 2020]. J Dermatol Treat. doi:10.1080/09546634.2020.1789044
- Nicholson P, Ali FR, Craythorne E, et al. Patient perceptions of Mohs micrographic surgery during the COVID-19 pandemic and lessons for the next outbreak. Clin Exp Dermatol. 2021;46:179-180.
- Ricci F, Fania L, Paradisi A, et al. Delayed melanoma diagnosis in the COVID-19 era: increased breslow thickness in primary melanomas seen after the COVID-19 lockdown. J Eur Acad Dermatol Venereol. 2020;34:E778-E779.
- Gualdi G, Porreca A, Amoruso GF, et al. The effect of the COVID-19 lockdown on melanoma diagnosis in Italy. Clin Dermatol. 2021;39:911-919.
- Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21:1035-1044.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Higgins HW, Lee KC, Galan A, et al. Melanoma in situ: part II. histopathology, treatment, and clinical management. J Am Acad Dermatol. 2015;73:193-203.
- Cook J, Zitelli JA. Mohs micrographic surgery: a cost analysis. J Am Acad Dermatol. 1998;39:698-703.
Practice Points
- Mohs surgeons should follow best practice guidelines dictated by our governing professional societies in selecting skin cancers for treatment by Mohs micrographic surgery (MMS) during the COVID-19 pandemic and beyond.
- The COVID-19 pandemic has impacted the characteristics of skin cancers treated by MMS, largely driven by new guidelines.
- Changing characteristics of skin cancers treated by MMS are of clinical significance, potentially affecting the extent of reconstructive surgery, cost, operating time, and future tumor characteristics.
Omicron sublineages evade immunity from past infection
A South African study based on blood samples found that the BA.4 and BA.5 sublineages of Omicron were more likely to evade antibodies produced by previous Omicron infections than the immunity provided by vaccinations.
Scientists took blood samples from 39 people infected with Omicron, with 24 people not vaccinated and 15 vaccinated with the Pfizer or the Johnson & Johnson vaccines, Reuters reported.
“The vaccinated group showed about a fivefold higher neutralization capacity ... and should be better protected,” the investigators found, according to Reuters.
There was an eightfold decrease in antibody protection in unvaccinated blood samples when exposed to the subvariants compared to a threefold decrease in the blood samples from vaccinated people.
“Based on neutralization escape, BA.4 and BA.5 have potential to result in a new infection wave,” the investigators found.
The finding is important because health authorities say cases caused by the sublineages are increasing in South Africa to a degree that the nation may be entering a fifth wave of COVID, Reuters said.
Health Minister Joe Phaahla said recently that hospitalizations were increasing but that ICU admissions had not greatly gone up yet.
A version of this article first appeared on WebMD.com.
A South African study based on blood samples found that the BA.4 and BA.5 sublineages of Omicron were more likely to evade antibodies produced by previous Omicron infections than the immunity provided by vaccinations.
Scientists took blood samples from 39 people infected with Omicron, with 24 people not vaccinated and 15 vaccinated with the Pfizer or the Johnson & Johnson vaccines, Reuters reported.
“The vaccinated group showed about a fivefold higher neutralization capacity ... and should be better protected,” the investigators found, according to Reuters.
There was an eightfold decrease in antibody protection in unvaccinated blood samples when exposed to the subvariants compared to a threefold decrease in the blood samples from vaccinated people.
“Based on neutralization escape, BA.4 and BA.5 have potential to result in a new infection wave,” the investigators found.
The finding is important because health authorities say cases caused by the sublineages are increasing in South Africa to a degree that the nation may be entering a fifth wave of COVID, Reuters said.
Health Minister Joe Phaahla said recently that hospitalizations were increasing but that ICU admissions had not greatly gone up yet.
A version of this article first appeared on WebMD.com.
A South African study based on blood samples found that the BA.4 and BA.5 sublineages of Omicron were more likely to evade antibodies produced by previous Omicron infections than the immunity provided by vaccinations.
Scientists took blood samples from 39 people infected with Omicron, with 24 people not vaccinated and 15 vaccinated with the Pfizer or the Johnson & Johnson vaccines, Reuters reported.
“The vaccinated group showed about a fivefold higher neutralization capacity ... and should be better protected,” the investigators found, according to Reuters.
There was an eightfold decrease in antibody protection in unvaccinated blood samples when exposed to the subvariants compared to a threefold decrease in the blood samples from vaccinated people.
“Based on neutralization escape, BA.4 and BA.5 have potential to result in a new infection wave,” the investigators found.
The finding is important because health authorities say cases caused by the sublineages are increasing in South Africa to a degree that the nation may be entering a fifth wave of COVID, Reuters said.
Health Minister Joe Phaahla said recently that hospitalizations were increasing but that ICU admissions had not greatly gone up yet.
A version of this article first appeared on WebMD.com.
Newly defined liver disorder associated with COVID mortality
People with metabolic dysfunction–associated fatty liver disease (MAFLD) – a newly defined condition – may be more likely to die from COVID-19, researchers say.
A cohort of people hospitalized for COVID-19 in Central Military Hospital, Mexico City, who met the criteria for MAFLD died at a higher rate than a control group without fatty liver disease, said Martín Uriel Vázquez-Medina, MSc, a researcher in the National Polytechnic Institute in Mexico City.
Patients who met only the criteria for the traditional classification, nonalcoholic fatty liver disease (NAFLD), also died of COVID-19 at a higher rate than the control group, but the difference was not statistically significant.
“It is important to screen for MAFLD,” Mr. Vázquez-Medina told this news organization. “It’s a new definition, but it has really helped us to identify which patients are going to get worse by COVID-19.”
The study was published in Hepatology Communications.
More evidence for clinical relevance of MAFLD
The finding lends support to an initiative to use MAFLD instead of NAFLD to identify patients whose liver steatosis poses a threat to their health, Mr. Vázquez-Medina said.
NAFLD affects as much as a quarter of the world’s population. No drugs have been approved to treat it. Some researchers have reasoned that the imprecision of the definition of NAFLD could be one reason for the lack of progress in treatment.
“NAFLD is something that doesn’t have positive criteria to be diagnosed,” said Mr. Vázquez-Medina. “You only say NAFLD when you don’t find hepatitis or another disease.”
In an article published in Gastroenterology, an international consensus panel proposed MAFLD as an alternative, arguing that a focus on metabolic dysfunction could more accurately reflect the pathogenesis of the disease and help stratify patients.
Previous research has suggested that patients with MAFLD have a higher risk of atherosclerotic cardiovascular disease and that the prevalence of colorectal adenomas is a higher in these patients, compared with patients with NAFLD.
The high prevalence of MAFLD in Mexico – about 30% – could help explain the country’s high rate of mortality from COVID-19, Mr. Vázquez-Medina said. Almost 6% of people diagnosed with COVID in Mexico have died from it, according to the Johns Hopkins University and Medical Center Coronavirus Resource Center.
Sorting COVID outcomes by liver steatosis
To understand the interaction of MAFLD, NAFLD, liver fibrosis, and COVID-19, Mr. Vázquez-Medina and his colleagues analyzed the records of all patients admitted to the Central Military Hospital with COVID-19 from April 4, 2020, to June 24, 2020.
They excluded patients for whom complete data were lacking or for whom a liver function test was not conducted in the first 24 hours of hospitalization. Also excluded were patients with significant consumption of alcohol (> 30 g/day for men and > 20 g/day for women) and those with a history of autoimmune liver disease, liver cancer, decompensated cirrhosis, platelet disorders, or myopathies.
The remaining patients were divided into three groups – 220 who met the criteria for MAFLD, 79 who met the criteria for NAFLD but not MAFLD, and 60 other patients as a control group.
The researchers defined MAFLD as the presence of liver steatosis detected with a noninvasive method and one of the following: overweight (body mass index, 25-29.9 kg/m2), type 2 diabetes, or the presence of two metabolic abnormalities (blood pressure > 140/90 mm Hg, plasma triglycerides > 150 mg/dL, plasma high-density lipoprotein cholesterol < 40 mg/dL in men and < 50 mg/dL in women, and prediabetes).
They defined NAFLD as the presence of liver steatosis without the other criteria for MAFLD.
The patients with MAFLD were the most likely to be intubated and were the most likely to die (intubation, 44.09%; mortality, 55%), followed by those with NAFLD (intubation, 40.51%; mortality, 51.9%) and those in the control group (intubation, 20%; mortality, 38.33%).
The difference in mortality between the MAFLD group and the control group was statistically significant (P = .02). The mortality difference between the NAFLD and the control group fell just short of statistical significance (P = .07).
For intubation, the difference between the MAFLD and the control group was highly statistically significant (P = .001), and the difference between the NAFLD and the control group was also statistically significant (P = .01)
Patients with advanced fibrosis and either MAFLD or NAFLD were also more likely to die than patients in the control group with advanced fibrosis.
That’s why screening for MAFLD is important, Mr. Vázquez-Medina said.
Next steps and new questions
Future research should examine whether patients with MAFLD have elevated levels of biomarkers for inflammation, such as interleukin 6, Mr. Vázquez-Medina said. A “chronic low proinflammatory state” may be the key to understanding the vulnerability of patients to MAFLD to COVID-19, he speculated.
The metabolic traits associated with MAFLD could explain the higher mortality and intubation rates with COVID, said Rohit Loomba, MD, MHSc, a professor of medicine in the division of gastroenterology at the University of California, San Diego, who was not involved in the study.
“Hypertension, diabetes, and obesity increase the risk of complications from COVID in all patients, whether they have been diagnosed with NAFLD or not,” he told this news organization in an email.
Mr. Vasquez-Medina pointed out that the patients with MAFLD had a higher risk of mortality even after adjusting for age, sex, type 2 diabetes, hypertension, overweight, and obesity (BMI ≥ 30 kg/m2). MAFLD also was more strongly associated with a poor outcome than either hypertension alone or obesity alone. Only age emerged as a significant independent covariate in the study.
Dr. Loomba also questioned whether the regression model used in this study for liver steatosis was “fully reflective of NAFLD.”
The researchers identified liver steatosis with a diagnostic formula that used noninvasive clinical BMI and laboratory tests (alanine aminotransferase), citing a study that found the regression formula was better at diagnosing NAFLD than FibroScan.
Mr. Vázquez-Medina reported no relevant financial relationships. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89bio, Terns Pharmaceuticals, and Viking Therapeutics. He is co-founder of LipoNexus.
A version of this article first appeared on Medscape.com.
People with metabolic dysfunction–associated fatty liver disease (MAFLD) – a newly defined condition – may be more likely to die from COVID-19, researchers say.
A cohort of people hospitalized for COVID-19 in Central Military Hospital, Mexico City, who met the criteria for MAFLD died at a higher rate than a control group without fatty liver disease, said Martín Uriel Vázquez-Medina, MSc, a researcher in the National Polytechnic Institute in Mexico City.
Patients who met only the criteria for the traditional classification, nonalcoholic fatty liver disease (NAFLD), also died of COVID-19 at a higher rate than the control group, but the difference was not statistically significant.
“It is important to screen for MAFLD,” Mr. Vázquez-Medina told this news organization. “It’s a new definition, but it has really helped us to identify which patients are going to get worse by COVID-19.”
The study was published in Hepatology Communications.
More evidence for clinical relevance of MAFLD
The finding lends support to an initiative to use MAFLD instead of NAFLD to identify patients whose liver steatosis poses a threat to their health, Mr. Vázquez-Medina said.
NAFLD affects as much as a quarter of the world’s population. No drugs have been approved to treat it. Some researchers have reasoned that the imprecision of the definition of NAFLD could be one reason for the lack of progress in treatment.
“NAFLD is something that doesn’t have positive criteria to be diagnosed,” said Mr. Vázquez-Medina. “You only say NAFLD when you don’t find hepatitis or another disease.”
In an article published in Gastroenterology, an international consensus panel proposed MAFLD as an alternative, arguing that a focus on metabolic dysfunction could more accurately reflect the pathogenesis of the disease and help stratify patients.
Previous research has suggested that patients with MAFLD have a higher risk of atherosclerotic cardiovascular disease and that the prevalence of colorectal adenomas is a higher in these patients, compared with patients with NAFLD.
The high prevalence of MAFLD in Mexico – about 30% – could help explain the country’s high rate of mortality from COVID-19, Mr. Vázquez-Medina said. Almost 6% of people diagnosed with COVID in Mexico have died from it, according to the Johns Hopkins University and Medical Center Coronavirus Resource Center.
Sorting COVID outcomes by liver steatosis
To understand the interaction of MAFLD, NAFLD, liver fibrosis, and COVID-19, Mr. Vázquez-Medina and his colleagues analyzed the records of all patients admitted to the Central Military Hospital with COVID-19 from April 4, 2020, to June 24, 2020.
They excluded patients for whom complete data were lacking or for whom a liver function test was not conducted in the first 24 hours of hospitalization. Also excluded were patients with significant consumption of alcohol (> 30 g/day for men and > 20 g/day for women) and those with a history of autoimmune liver disease, liver cancer, decompensated cirrhosis, platelet disorders, or myopathies.
The remaining patients were divided into three groups – 220 who met the criteria for MAFLD, 79 who met the criteria for NAFLD but not MAFLD, and 60 other patients as a control group.
The researchers defined MAFLD as the presence of liver steatosis detected with a noninvasive method and one of the following: overweight (body mass index, 25-29.9 kg/m2), type 2 diabetes, or the presence of two metabolic abnormalities (blood pressure > 140/90 mm Hg, plasma triglycerides > 150 mg/dL, plasma high-density lipoprotein cholesterol < 40 mg/dL in men and < 50 mg/dL in women, and prediabetes).
They defined NAFLD as the presence of liver steatosis without the other criteria for MAFLD.
The patients with MAFLD were the most likely to be intubated and were the most likely to die (intubation, 44.09%; mortality, 55%), followed by those with NAFLD (intubation, 40.51%; mortality, 51.9%) and those in the control group (intubation, 20%; mortality, 38.33%).
The difference in mortality between the MAFLD group and the control group was statistically significant (P = .02). The mortality difference between the NAFLD and the control group fell just short of statistical significance (P = .07).
For intubation, the difference between the MAFLD and the control group was highly statistically significant (P = .001), and the difference between the NAFLD and the control group was also statistically significant (P = .01)
Patients with advanced fibrosis and either MAFLD or NAFLD were also more likely to die than patients in the control group with advanced fibrosis.
That’s why screening for MAFLD is important, Mr. Vázquez-Medina said.
Next steps and new questions
Future research should examine whether patients with MAFLD have elevated levels of biomarkers for inflammation, such as interleukin 6, Mr. Vázquez-Medina said. A “chronic low proinflammatory state” may be the key to understanding the vulnerability of patients to MAFLD to COVID-19, he speculated.
The metabolic traits associated with MAFLD could explain the higher mortality and intubation rates with COVID, said Rohit Loomba, MD, MHSc, a professor of medicine in the division of gastroenterology at the University of California, San Diego, who was not involved in the study.
“Hypertension, diabetes, and obesity increase the risk of complications from COVID in all patients, whether they have been diagnosed with NAFLD or not,” he told this news organization in an email.
Mr. Vasquez-Medina pointed out that the patients with MAFLD had a higher risk of mortality even after adjusting for age, sex, type 2 diabetes, hypertension, overweight, and obesity (BMI ≥ 30 kg/m2). MAFLD also was more strongly associated with a poor outcome than either hypertension alone or obesity alone. Only age emerged as a significant independent covariate in the study.
Dr. Loomba also questioned whether the regression model used in this study for liver steatosis was “fully reflective of NAFLD.”
The researchers identified liver steatosis with a diagnostic formula that used noninvasive clinical BMI and laboratory tests (alanine aminotransferase), citing a study that found the regression formula was better at diagnosing NAFLD than FibroScan.
Mr. Vázquez-Medina reported no relevant financial relationships. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89bio, Terns Pharmaceuticals, and Viking Therapeutics. He is co-founder of LipoNexus.
A version of this article first appeared on Medscape.com.
People with metabolic dysfunction–associated fatty liver disease (MAFLD) – a newly defined condition – may be more likely to die from COVID-19, researchers say.
A cohort of people hospitalized for COVID-19 in Central Military Hospital, Mexico City, who met the criteria for MAFLD died at a higher rate than a control group without fatty liver disease, said Martín Uriel Vázquez-Medina, MSc, a researcher in the National Polytechnic Institute in Mexico City.
Patients who met only the criteria for the traditional classification, nonalcoholic fatty liver disease (NAFLD), also died of COVID-19 at a higher rate than the control group, but the difference was not statistically significant.
“It is important to screen for MAFLD,” Mr. Vázquez-Medina told this news organization. “It’s a new definition, but it has really helped us to identify which patients are going to get worse by COVID-19.”
The study was published in Hepatology Communications.
More evidence for clinical relevance of MAFLD
The finding lends support to an initiative to use MAFLD instead of NAFLD to identify patients whose liver steatosis poses a threat to their health, Mr. Vázquez-Medina said.
NAFLD affects as much as a quarter of the world’s population. No drugs have been approved to treat it. Some researchers have reasoned that the imprecision of the definition of NAFLD could be one reason for the lack of progress in treatment.
“NAFLD is something that doesn’t have positive criteria to be diagnosed,” said Mr. Vázquez-Medina. “You only say NAFLD when you don’t find hepatitis or another disease.”
In an article published in Gastroenterology, an international consensus panel proposed MAFLD as an alternative, arguing that a focus on metabolic dysfunction could more accurately reflect the pathogenesis of the disease and help stratify patients.
Previous research has suggested that patients with MAFLD have a higher risk of atherosclerotic cardiovascular disease and that the prevalence of colorectal adenomas is a higher in these patients, compared with patients with NAFLD.
The high prevalence of MAFLD in Mexico – about 30% – could help explain the country’s high rate of mortality from COVID-19, Mr. Vázquez-Medina said. Almost 6% of people diagnosed with COVID in Mexico have died from it, according to the Johns Hopkins University and Medical Center Coronavirus Resource Center.
Sorting COVID outcomes by liver steatosis
To understand the interaction of MAFLD, NAFLD, liver fibrosis, and COVID-19, Mr. Vázquez-Medina and his colleagues analyzed the records of all patients admitted to the Central Military Hospital with COVID-19 from April 4, 2020, to June 24, 2020.
They excluded patients for whom complete data were lacking or for whom a liver function test was not conducted in the first 24 hours of hospitalization. Also excluded were patients with significant consumption of alcohol (> 30 g/day for men and > 20 g/day for women) and those with a history of autoimmune liver disease, liver cancer, decompensated cirrhosis, platelet disorders, or myopathies.
The remaining patients were divided into three groups – 220 who met the criteria for MAFLD, 79 who met the criteria for NAFLD but not MAFLD, and 60 other patients as a control group.
The researchers defined MAFLD as the presence of liver steatosis detected with a noninvasive method and one of the following: overweight (body mass index, 25-29.9 kg/m2), type 2 diabetes, or the presence of two metabolic abnormalities (blood pressure > 140/90 mm Hg, plasma triglycerides > 150 mg/dL, plasma high-density lipoprotein cholesterol < 40 mg/dL in men and < 50 mg/dL in women, and prediabetes).
They defined NAFLD as the presence of liver steatosis without the other criteria for MAFLD.
The patients with MAFLD were the most likely to be intubated and were the most likely to die (intubation, 44.09%; mortality, 55%), followed by those with NAFLD (intubation, 40.51%; mortality, 51.9%) and those in the control group (intubation, 20%; mortality, 38.33%).
The difference in mortality between the MAFLD group and the control group was statistically significant (P = .02). The mortality difference between the NAFLD and the control group fell just short of statistical significance (P = .07).
For intubation, the difference between the MAFLD and the control group was highly statistically significant (P = .001), and the difference between the NAFLD and the control group was also statistically significant (P = .01)
Patients with advanced fibrosis and either MAFLD or NAFLD were also more likely to die than patients in the control group with advanced fibrosis.
That’s why screening for MAFLD is important, Mr. Vázquez-Medina said.
Next steps and new questions
Future research should examine whether patients with MAFLD have elevated levels of biomarkers for inflammation, such as interleukin 6, Mr. Vázquez-Medina said. A “chronic low proinflammatory state” may be the key to understanding the vulnerability of patients to MAFLD to COVID-19, he speculated.
The metabolic traits associated with MAFLD could explain the higher mortality and intubation rates with COVID, said Rohit Loomba, MD, MHSc, a professor of medicine in the division of gastroenterology at the University of California, San Diego, who was not involved in the study.
“Hypertension, diabetes, and obesity increase the risk of complications from COVID in all patients, whether they have been diagnosed with NAFLD or not,” he told this news organization in an email.
Mr. Vasquez-Medina pointed out that the patients with MAFLD had a higher risk of mortality even after adjusting for age, sex, type 2 diabetes, hypertension, overweight, and obesity (BMI ≥ 30 kg/m2). MAFLD also was more strongly associated with a poor outcome than either hypertension alone or obesity alone. Only age emerged as a significant independent covariate in the study.
Dr. Loomba also questioned whether the regression model used in this study for liver steatosis was “fully reflective of NAFLD.”
The researchers identified liver steatosis with a diagnostic formula that used noninvasive clinical BMI and laboratory tests (alanine aminotransferase), citing a study that found the regression formula was better at diagnosing NAFLD than FibroScan.
Mr. Vázquez-Medina reported no relevant financial relationships. Dr. Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Anylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, CohBar, Eli Lilly, Galmed, Gilead, Glympse Bio, Hightide, Inipharma, Intercept, Inventiva, Ionis, Janssen, Madrigal, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck, Pfizer, Sagimet, Theratechnologies, 89bio, Terns Pharmaceuticals, and Viking Therapeutics. He is co-founder of LipoNexus.
A version of this article first appeared on Medscape.com.
FROM HEPATOLOGY COMMUNICATIONS
When it’s not long, but medium COVID?
Symptom timelines surrounding COVID infection tend to center on either the immediate 5-day quarantine protocols for acute infection or the long-COVID symptoms that can last a month or potentially far longer.
People may return to work or daily routines, but something is off: What had been simple exercise regimens become onerous. Everyday tasks take more effort.
Does this ill-defined subset point to a “medium COVID?”
Farha Ikramuddin, MD, MHA, a physiatrist and rehabilitation specialist at the University of Minnesota and M Health Fairview in Minneapolis, points out there is no definition or diagnostic code or shared official understanding of a middle category for COVID.
“But am I seeing that? Absolutely,” she said in an interview.
“I have seen patients who are younger, healthier, [and] with not so many comorbidities have either persistence of symptoms or reappearance after the initial infection is done,” she said.
Some patients report they had very low infection or were nonsymptomatic and returned to their normal health fairly quickly after infection. Then a week later they began experiencing fatigue, lost appetite, loss of smell, and feeling full after a few bites, Dr. Ikramuddin said.
Part of the trouble in categorizing the space between returning to normal after a week and having symptoms for months is that organizations can’t agree on a timeline for when symptoms warrant a “long-COVID” label.
For instance, the Centers for Disease Control and Prevention defines it as 4 or more weeks after infection. The World Health Organization defines it as starting 3 months after COVID-19 symptom onset.
“I’m seeing ‘medium COVID’ – as one would call it – in younger and healthier patients. I’m also noticing that these symptoms are not severe enough to warrant stopping their job or changing their job schedules,” Dr. Ikramuddin said.
They go back to work, she said, but start noticing something is off.
“I am seeing that.”
“I discharge at least two patients a week from my clinic because they have moved on and no longer have symptoms,” Dr. Ikramuddin said.
In a story from Kaiser Health News published last month, WHYY health reporter Nina Feldman writes: “What I’ve come to think of as my ‘medium COVID’ affected my life. I couldn’t socialize much, drink, or stay up past 9:30 p.m. It took me 10 weeks to go for my first run – I’d been too afraid to try.”
She described a dinner with a friend after ending initial isolation protocols: “One glass of wine left me feeling like I’d had a whole bottle. I was bone-achingly exhausted but couldn’t sleep.”
Medical mystery
Dr. Ikramuddin notes the mechanism behind prolonged COVID-19 symptoms is still a medical mystery.
“In one scenario,” she said, “the question is being asked about whether the virus is staying dormant, similar to herpes zoster or HIV.”
“Right now, instead of getting more answers, we’re getting more questions,” Dr. Ikramuddin said.
Mouhib Naddour, MD, a pulmonary specialist with Sharp HealthCare in San Diego, said he’s seeing that it’s taking some patients who have had COVID longer to recover than it would for other viral infections.
Some patients fall between those recovering within 2-3 weeks and patients having long COVID. Those patients in the gap could be lumped into a middle-range COVID, he told this news organization.
“We try to put things into tables and boxes but it is hard with this disease,” Dr. Naddour said.
He agrees there’s no medical definition for “medium” COVID, but he said the idea should bring hope for patients to know that, if their symptoms are persisting they don’t necessarily have long COVID – and their symptoms may still disappear.
“This is an illness that may take longer to completely recover from,” he said. “The majority of patients we’re seeing in this group could be healthy young patients who get COVID, then 2-3 weeks after they test negative, still have lingering symptoms.”
Common symptoms
Some commonly reported symptoms of those with enduring illness, which often overlap with other stages of COVID, are difficulty breathing, chest tightness, dry cough, chest pain, muscle and joint pain, fatigue, difficulty sleeping, and mood swings, Dr. Naddour said.
“We need to do an extensive assessment to make sure there’s no other problem causing these symptoms,” he said.
Still, there is no set timeline for the medium-COVID range, he noted, so checking in with a primary care physician is important for people experiencing symptoms.
It’s a continuum, not a category
Fernando Carnavali, MD, coordinator for Mount Sinai’s Center for Post-COVID Care in New York, said he is not ready to recognize a separate category for a “medium” COVID.
He noted that science can’t even agree on a name for lasting post-COVID symptoms, whether it’s “long COVID” or “long-haul COVID,” “post-COVID syndrome” or “post-acute sequelae of COVID-19 (PASC ).” There’s no agreed-upon pathophysiology or biomarker.
“That creates these gaps of understanding on where we are,” Dr. Carnavali said in an interview.
He said he understands people’s need to categorize symptoms, but rather than a middle ground he sees a continuum.
It doesn’t mean what others may call COVID’s middle ground doesn’t exist, Dr. Carnavali said: “We are in the infancy of defining this. Trying to classify them may create more anxiety.”
The clinicians interviewed for this story report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Symptom timelines surrounding COVID infection tend to center on either the immediate 5-day quarantine protocols for acute infection or the long-COVID symptoms that can last a month or potentially far longer.
People may return to work or daily routines, but something is off: What had been simple exercise regimens become onerous. Everyday tasks take more effort.
Does this ill-defined subset point to a “medium COVID?”
Farha Ikramuddin, MD, MHA, a physiatrist and rehabilitation specialist at the University of Minnesota and M Health Fairview in Minneapolis, points out there is no definition or diagnostic code or shared official understanding of a middle category for COVID.
“But am I seeing that? Absolutely,” she said in an interview.
“I have seen patients who are younger, healthier, [and] with not so many comorbidities have either persistence of symptoms or reappearance after the initial infection is done,” she said.
Some patients report they had very low infection or were nonsymptomatic and returned to their normal health fairly quickly after infection. Then a week later they began experiencing fatigue, lost appetite, loss of smell, and feeling full after a few bites, Dr. Ikramuddin said.
Part of the trouble in categorizing the space between returning to normal after a week and having symptoms for months is that organizations can’t agree on a timeline for when symptoms warrant a “long-COVID” label.
For instance, the Centers for Disease Control and Prevention defines it as 4 or more weeks after infection. The World Health Organization defines it as starting 3 months after COVID-19 symptom onset.
“I’m seeing ‘medium COVID’ – as one would call it – in younger and healthier patients. I’m also noticing that these symptoms are not severe enough to warrant stopping their job or changing their job schedules,” Dr. Ikramuddin said.
They go back to work, she said, but start noticing something is off.
“I am seeing that.”
“I discharge at least two patients a week from my clinic because they have moved on and no longer have symptoms,” Dr. Ikramuddin said.
In a story from Kaiser Health News published last month, WHYY health reporter Nina Feldman writes: “What I’ve come to think of as my ‘medium COVID’ affected my life. I couldn’t socialize much, drink, or stay up past 9:30 p.m. It took me 10 weeks to go for my first run – I’d been too afraid to try.”
She described a dinner with a friend after ending initial isolation protocols: “One glass of wine left me feeling like I’d had a whole bottle. I was bone-achingly exhausted but couldn’t sleep.”
Medical mystery
Dr. Ikramuddin notes the mechanism behind prolonged COVID-19 symptoms is still a medical mystery.
“In one scenario,” she said, “the question is being asked about whether the virus is staying dormant, similar to herpes zoster or HIV.”
“Right now, instead of getting more answers, we’re getting more questions,” Dr. Ikramuddin said.
Mouhib Naddour, MD, a pulmonary specialist with Sharp HealthCare in San Diego, said he’s seeing that it’s taking some patients who have had COVID longer to recover than it would for other viral infections.
Some patients fall between those recovering within 2-3 weeks and patients having long COVID. Those patients in the gap could be lumped into a middle-range COVID, he told this news organization.
“We try to put things into tables and boxes but it is hard with this disease,” Dr. Naddour said.
He agrees there’s no medical definition for “medium” COVID, but he said the idea should bring hope for patients to know that, if their symptoms are persisting they don’t necessarily have long COVID – and their symptoms may still disappear.
“This is an illness that may take longer to completely recover from,” he said. “The majority of patients we’re seeing in this group could be healthy young patients who get COVID, then 2-3 weeks after they test negative, still have lingering symptoms.”
Common symptoms
Some commonly reported symptoms of those with enduring illness, which often overlap with other stages of COVID, are difficulty breathing, chest tightness, dry cough, chest pain, muscle and joint pain, fatigue, difficulty sleeping, and mood swings, Dr. Naddour said.
“We need to do an extensive assessment to make sure there’s no other problem causing these symptoms,” he said.
Still, there is no set timeline for the medium-COVID range, he noted, so checking in with a primary care physician is important for people experiencing symptoms.
It’s a continuum, not a category
Fernando Carnavali, MD, coordinator for Mount Sinai’s Center for Post-COVID Care in New York, said he is not ready to recognize a separate category for a “medium” COVID.
He noted that science can’t even agree on a name for lasting post-COVID symptoms, whether it’s “long COVID” or “long-haul COVID,” “post-COVID syndrome” or “post-acute sequelae of COVID-19 (PASC ).” There’s no agreed-upon pathophysiology or biomarker.
“That creates these gaps of understanding on where we are,” Dr. Carnavali said in an interview.
He said he understands people’s need to categorize symptoms, but rather than a middle ground he sees a continuum.
It doesn’t mean what others may call COVID’s middle ground doesn’t exist, Dr. Carnavali said: “We are in the infancy of defining this. Trying to classify them may create more anxiety.”
The clinicians interviewed for this story report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Symptom timelines surrounding COVID infection tend to center on either the immediate 5-day quarantine protocols for acute infection or the long-COVID symptoms that can last a month or potentially far longer.
People may return to work or daily routines, but something is off: What had been simple exercise regimens become onerous. Everyday tasks take more effort.
Does this ill-defined subset point to a “medium COVID?”
Farha Ikramuddin, MD, MHA, a physiatrist and rehabilitation specialist at the University of Minnesota and M Health Fairview in Minneapolis, points out there is no definition or diagnostic code or shared official understanding of a middle category for COVID.
“But am I seeing that? Absolutely,” she said in an interview.
“I have seen patients who are younger, healthier, [and] with not so many comorbidities have either persistence of symptoms or reappearance after the initial infection is done,” she said.
Some patients report they had very low infection or were nonsymptomatic and returned to their normal health fairly quickly after infection. Then a week later they began experiencing fatigue, lost appetite, loss of smell, and feeling full after a few bites, Dr. Ikramuddin said.
Part of the trouble in categorizing the space between returning to normal after a week and having symptoms for months is that organizations can’t agree on a timeline for when symptoms warrant a “long-COVID” label.
For instance, the Centers for Disease Control and Prevention defines it as 4 or more weeks after infection. The World Health Organization defines it as starting 3 months after COVID-19 symptom onset.
“I’m seeing ‘medium COVID’ – as one would call it – in younger and healthier patients. I’m also noticing that these symptoms are not severe enough to warrant stopping their job or changing their job schedules,” Dr. Ikramuddin said.
They go back to work, she said, but start noticing something is off.
“I am seeing that.”
“I discharge at least two patients a week from my clinic because they have moved on and no longer have symptoms,” Dr. Ikramuddin said.
In a story from Kaiser Health News published last month, WHYY health reporter Nina Feldman writes: “What I’ve come to think of as my ‘medium COVID’ affected my life. I couldn’t socialize much, drink, or stay up past 9:30 p.m. It took me 10 weeks to go for my first run – I’d been too afraid to try.”
She described a dinner with a friend after ending initial isolation protocols: “One glass of wine left me feeling like I’d had a whole bottle. I was bone-achingly exhausted but couldn’t sleep.”
Medical mystery
Dr. Ikramuddin notes the mechanism behind prolonged COVID-19 symptoms is still a medical mystery.
“In one scenario,” she said, “the question is being asked about whether the virus is staying dormant, similar to herpes zoster or HIV.”
“Right now, instead of getting more answers, we’re getting more questions,” Dr. Ikramuddin said.
Mouhib Naddour, MD, a pulmonary specialist with Sharp HealthCare in San Diego, said he’s seeing that it’s taking some patients who have had COVID longer to recover than it would for other viral infections.
Some patients fall between those recovering within 2-3 weeks and patients having long COVID. Those patients in the gap could be lumped into a middle-range COVID, he told this news organization.
“We try to put things into tables and boxes but it is hard with this disease,” Dr. Naddour said.
He agrees there’s no medical definition for “medium” COVID, but he said the idea should bring hope for patients to know that, if their symptoms are persisting they don’t necessarily have long COVID – and their symptoms may still disappear.
“This is an illness that may take longer to completely recover from,” he said. “The majority of patients we’re seeing in this group could be healthy young patients who get COVID, then 2-3 weeks after they test negative, still have lingering symptoms.”
Common symptoms
Some commonly reported symptoms of those with enduring illness, which often overlap with other stages of COVID, are difficulty breathing, chest tightness, dry cough, chest pain, muscle and joint pain, fatigue, difficulty sleeping, and mood swings, Dr. Naddour said.
“We need to do an extensive assessment to make sure there’s no other problem causing these symptoms,” he said.
Still, there is no set timeline for the medium-COVID range, he noted, so checking in with a primary care physician is important for people experiencing symptoms.
It’s a continuum, not a category
Fernando Carnavali, MD, coordinator for Mount Sinai’s Center for Post-COVID Care in New York, said he is not ready to recognize a separate category for a “medium” COVID.
He noted that science can’t even agree on a name for lasting post-COVID symptoms, whether it’s “long COVID” or “long-haul COVID,” “post-COVID syndrome” or “post-acute sequelae of COVID-19 (PASC ).” There’s no agreed-upon pathophysiology or biomarker.
“That creates these gaps of understanding on where we are,” Dr. Carnavali said in an interview.
He said he understands people’s need to categorize symptoms, but rather than a middle ground he sees a continuum.
It doesn’t mean what others may call COVID’s middle ground doesn’t exist, Dr. Carnavali said: “We are in the infancy of defining this. Trying to classify them may create more anxiety.”
The clinicians interviewed for this story report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data confirm risk of Guillain-Barré with J&J COVID shot
The Janssen vaccine (Ad26.COV2.S) is a replication-incompetent adenoviral vector vaccine.
The data show no increased risk of GBS with the Pfizer (BNT162b2) or Moderna (mRNA-1273) shots – both mRNA vaccines.
“Our findings support the current guidance from U.S. health officials that preferentially recommend use of mRNA COVID-19 vaccines for primary and booster doses,” Nicola Klein, MD, PhD, with Kaiser Permanente Vaccine Study Center, Oakland, Calif., told this news organization.
“Individuals who choose to receive Janssen/J&J COVID-19 vaccine should be informed of the potential safety risks, including GBS,” Dr. Klein said.
The study was published online in JAMA Network Open.
Eleven cases
Between mid-December 2020 and mid-November 2021, roughly 15.1 million doses of COVID-19 vaccine were administered to nearly 7.9 million adults in the United States.
This includes roughly 483,000 doses of the Janssen vaccine, 8.8 million doses of the Pfizer vaccine, and 5.8 million doses of the Moderna vaccine.
The researchers confirmed 11 cases of GBS after the Janssen vaccine.
The unadjusted incidence of GBS (per 100,000 person-years) was 32.4 in the first 21 days after the Janssen vaccine – substantially higher than the expected background rate of 1 to 2 cases per 100,000 person-years.
There were 36 confirmed cases of GBS after mRNA vaccines. The unadjusted incidence in the first 21 days after mRNA vaccination was 1.3 per 100,000 person-years, similar to the overall expected background rate.
In an adjusted head-to-head comparison, GBS incidence during the 21 days after receipt of the Janssen vaccine was 20.6 times higher than the GBS incidence during the 21 days after the Pfizer or Moderna mRNA vaccines, amounting to 15.5 excess cases per million Janssen vaccine recipients.
Most cases of GBS after the Janssen vaccine occurred during the 1- to 21-day risk interval, with the period of greatest risk in the 1-14 days after vaccination.
The findings of this analysis of surveillance data of COVID-19 vaccines are “consistent with an elevated risk of GBS after primary Ad26.COV2.S vaccination,” the authors wrote.
Novel presentation?
The researchers note that nearly all individuals who developed GBS after the Janssen vaccine had facial weakness or paralysis, in addition to weakness and decreased reflexes in the limbs, suggesting that the presentation of GBS after COVID-19 adenoviral vector vaccine may be novel.
“More research is needed to determine if the presentation of GBS after adenoviral vector vaccine differs from GBS after other exposures such as Campylobacter jejuni, and to investigate the mechanism for how adenoviral vector vaccines may cause GBS,” Dr. Klein and colleagues said.
“The Vaccine Safety Datalink continues to conduct safety surveillance for all COVID-19 vaccines, including monitoring for GBS and other serious health outcomes after vaccination,” Dr. Klein said in an interview.
This study was supported by the Centers for Disease Control and Prevention. Dr. Klein reported receiving grants from Pfizer research support for a COVID vaccine clinical trial as well as other unrelated studies, grants from Merck, grants from GlaxoSmithKline, grants from Sanofi Pasteur, and grants from Protein Science (now Sanofi Pasteur) outside the submitted work.
A version of this article first appeared on Medscape.com.
The Janssen vaccine (Ad26.COV2.S) is a replication-incompetent adenoviral vector vaccine.
The data show no increased risk of GBS with the Pfizer (BNT162b2) or Moderna (mRNA-1273) shots – both mRNA vaccines.
“Our findings support the current guidance from U.S. health officials that preferentially recommend use of mRNA COVID-19 vaccines for primary and booster doses,” Nicola Klein, MD, PhD, with Kaiser Permanente Vaccine Study Center, Oakland, Calif., told this news organization.
“Individuals who choose to receive Janssen/J&J COVID-19 vaccine should be informed of the potential safety risks, including GBS,” Dr. Klein said.
The study was published online in JAMA Network Open.
Eleven cases
Between mid-December 2020 and mid-November 2021, roughly 15.1 million doses of COVID-19 vaccine were administered to nearly 7.9 million adults in the United States.
This includes roughly 483,000 doses of the Janssen vaccine, 8.8 million doses of the Pfizer vaccine, and 5.8 million doses of the Moderna vaccine.
The researchers confirmed 11 cases of GBS after the Janssen vaccine.
The unadjusted incidence of GBS (per 100,000 person-years) was 32.4 in the first 21 days after the Janssen vaccine – substantially higher than the expected background rate of 1 to 2 cases per 100,000 person-years.
There were 36 confirmed cases of GBS after mRNA vaccines. The unadjusted incidence in the first 21 days after mRNA vaccination was 1.3 per 100,000 person-years, similar to the overall expected background rate.
In an adjusted head-to-head comparison, GBS incidence during the 21 days after receipt of the Janssen vaccine was 20.6 times higher than the GBS incidence during the 21 days after the Pfizer or Moderna mRNA vaccines, amounting to 15.5 excess cases per million Janssen vaccine recipients.
Most cases of GBS after the Janssen vaccine occurred during the 1- to 21-day risk interval, with the period of greatest risk in the 1-14 days after vaccination.
The findings of this analysis of surveillance data of COVID-19 vaccines are “consistent with an elevated risk of GBS after primary Ad26.COV2.S vaccination,” the authors wrote.
Novel presentation?
The researchers note that nearly all individuals who developed GBS after the Janssen vaccine had facial weakness or paralysis, in addition to weakness and decreased reflexes in the limbs, suggesting that the presentation of GBS after COVID-19 adenoviral vector vaccine may be novel.
“More research is needed to determine if the presentation of GBS after adenoviral vector vaccine differs from GBS after other exposures such as Campylobacter jejuni, and to investigate the mechanism for how adenoviral vector vaccines may cause GBS,” Dr. Klein and colleagues said.
“The Vaccine Safety Datalink continues to conduct safety surveillance for all COVID-19 vaccines, including monitoring for GBS and other serious health outcomes after vaccination,” Dr. Klein said in an interview.
This study was supported by the Centers for Disease Control and Prevention. Dr. Klein reported receiving grants from Pfizer research support for a COVID vaccine clinical trial as well as other unrelated studies, grants from Merck, grants from GlaxoSmithKline, grants from Sanofi Pasteur, and grants from Protein Science (now Sanofi Pasteur) outside the submitted work.
A version of this article first appeared on Medscape.com.
The Janssen vaccine (Ad26.COV2.S) is a replication-incompetent adenoviral vector vaccine.
The data show no increased risk of GBS with the Pfizer (BNT162b2) or Moderna (mRNA-1273) shots – both mRNA vaccines.
“Our findings support the current guidance from U.S. health officials that preferentially recommend use of mRNA COVID-19 vaccines for primary and booster doses,” Nicola Klein, MD, PhD, with Kaiser Permanente Vaccine Study Center, Oakland, Calif., told this news organization.
“Individuals who choose to receive Janssen/J&J COVID-19 vaccine should be informed of the potential safety risks, including GBS,” Dr. Klein said.
The study was published online in JAMA Network Open.
Eleven cases
Between mid-December 2020 and mid-November 2021, roughly 15.1 million doses of COVID-19 vaccine were administered to nearly 7.9 million adults in the United States.
This includes roughly 483,000 doses of the Janssen vaccine, 8.8 million doses of the Pfizer vaccine, and 5.8 million doses of the Moderna vaccine.
The researchers confirmed 11 cases of GBS after the Janssen vaccine.
The unadjusted incidence of GBS (per 100,000 person-years) was 32.4 in the first 21 days after the Janssen vaccine – substantially higher than the expected background rate of 1 to 2 cases per 100,000 person-years.
There were 36 confirmed cases of GBS after mRNA vaccines. The unadjusted incidence in the first 21 days after mRNA vaccination was 1.3 per 100,000 person-years, similar to the overall expected background rate.
In an adjusted head-to-head comparison, GBS incidence during the 21 days after receipt of the Janssen vaccine was 20.6 times higher than the GBS incidence during the 21 days after the Pfizer or Moderna mRNA vaccines, amounting to 15.5 excess cases per million Janssen vaccine recipients.
Most cases of GBS after the Janssen vaccine occurred during the 1- to 21-day risk interval, with the period of greatest risk in the 1-14 days after vaccination.
The findings of this analysis of surveillance data of COVID-19 vaccines are “consistent with an elevated risk of GBS after primary Ad26.COV2.S vaccination,” the authors wrote.
Novel presentation?
The researchers note that nearly all individuals who developed GBS after the Janssen vaccine had facial weakness or paralysis, in addition to weakness and decreased reflexes in the limbs, suggesting that the presentation of GBS after COVID-19 adenoviral vector vaccine may be novel.
“More research is needed to determine if the presentation of GBS after adenoviral vector vaccine differs from GBS after other exposures such as Campylobacter jejuni, and to investigate the mechanism for how adenoviral vector vaccines may cause GBS,” Dr. Klein and colleagues said.
“The Vaccine Safety Datalink continues to conduct safety surveillance for all COVID-19 vaccines, including monitoring for GBS and other serious health outcomes after vaccination,” Dr. Klein said in an interview.
This study was supported by the Centers for Disease Control and Prevention. Dr. Klein reported receiving grants from Pfizer research support for a COVID vaccine clinical trial as well as other unrelated studies, grants from Merck, grants from GlaxoSmithKline, grants from Sanofi Pasteur, and grants from Protein Science (now Sanofi Pasteur) outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Children and COVID: New cases up for third straight week
Moderna submitted a request to the Food and Drug administration for emergency use authorization of its COVID-19 vaccine in children under the age of 6 years, according to this news organization, and Pfizer/BioNTech officially applied for authorization of a booster dose in children aged 5-11, the companies announced.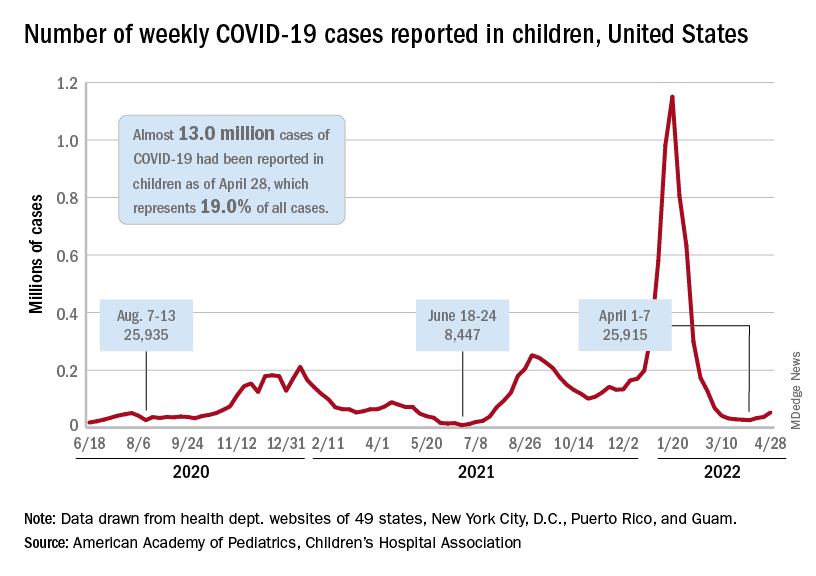
The FDA has tentatively scheduled meetings of its Vaccines and Related Biological Products Advisory Committee in June to consider the applications, saying that it “understands the urgency to authorize a vaccine for age groups who are not currently eligible for vaccination and will work diligently to complete our evaluation of the data. Should any of the submissions be completed in a timely manner and the data support a clear path forward following our evaluation, the FDA will act quickly” to convene the necessary meetings.
The need for greater access to vaccines seems to be increasing, as new pediatric COVID cases rose for the third consecutive week. April 22-28 saw over 53,000 new cases reported in children, up 43.5% from the previous week and up 105% since cases started rising again after dipping under 26,000 during the week of April 1-7, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
Hospital admissions involving diagnosed COVID also ticked up over the latter half of April, although the most recent 7-day average (April 24-30) of 112 per day was lower than the 117 reported for the previous week (April 17-23), the Centers for Disease Control and Prevention said, also noting that figures for the latest week “should be interpreted with caution.”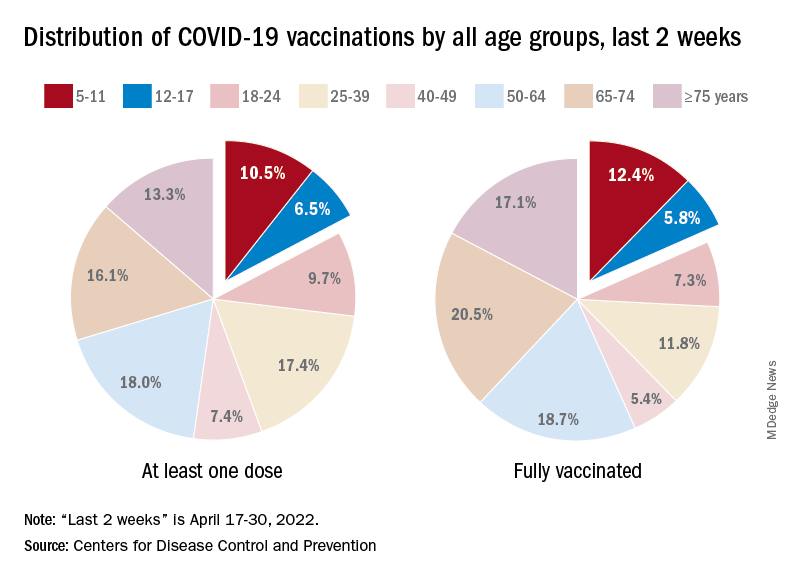
Vaccinations also were up slightly in children aged 5-11 years, with 52,000 receiving their first dose during the week of April 21-27, compared with 48,000 the week before. There was a slight dip, however, among 12- to 17-year-olds, who received 34,000 first doses during April 21-27, versus 35,000 the previous week, the AAP said in a separate report.
Cumulatively, almost 69% of all children aged 12-17 years have received at least one dose of the COVID-19 vaccine and 59% are fully vaccinated. Those aged 5-11 are well short of those figures, with just over 35% having received at least one dose and 28.5% fully vaccinated, the CDC said on its COVID Data Tracker.
A look at recent activity shows that children are not gaining on adults, who are much more likely to be vaccinated – full vaccination in those aged 50-64, for example, is 80%. During the 2 weeks from April 17-30, the 5- to 11-year-olds represented 10.5% of those who had initiated a first dose and 12.4% of those who gained full-vaccination status, both of which were well below the oldest age groups, the CDC reported.
Moderna submitted a request to the Food and Drug administration for emergency use authorization of its COVID-19 vaccine in children under the age of 6 years, according to this news organization, and Pfizer/BioNTech officially applied for authorization of a booster dose in children aged 5-11, the companies announced.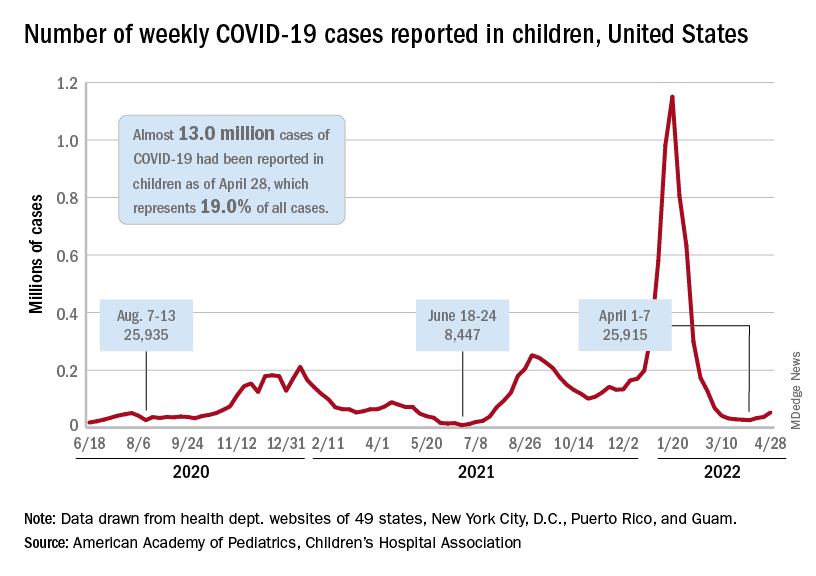
The FDA has tentatively scheduled meetings of its Vaccines and Related Biological Products Advisory Committee in June to consider the applications, saying that it “understands the urgency to authorize a vaccine for age groups who are not currently eligible for vaccination and will work diligently to complete our evaluation of the data. Should any of the submissions be completed in a timely manner and the data support a clear path forward following our evaluation, the FDA will act quickly” to convene the necessary meetings.
The need for greater access to vaccines seems to be increasing, as new pediatric COVID cases rose for the third consecutive week. April 22-28 saw over 53,000 new cases reported in children, up 43.5% from the previous week and up 105% since cases started rising again after dipping under 26,000 during the week of April 1-7, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
Hospital admissions involving diagnosed COVID also ticked up over the latter half of April, although the most recent 7-day average (April 24-30) of 112 per day was lower than the 117 reported for the previous week (April 17-23), the Centers for Disease Control and Prevention said, also noting that figures for the latest week “should be interpreted with caution.”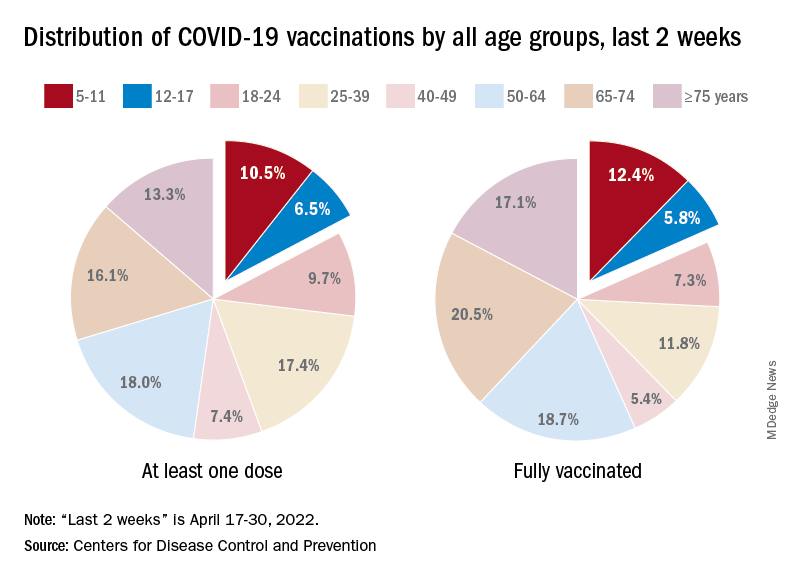
Vaccinations also were up slightly in children aged 5-11 years, with 52,000 receiving their first dose during the week of April 21-27, compared with 48,000 the week before. There was a slight dip, however, among 12- to 17-year-olds, who received 34,000 first doses during April 21-27, versus 35,000 the previous week, the AAP said in a separate report.
Cumulatively, almost 69% of all children aged 12-17 years have received at least one dose of the COVID-19 vaccine and 59% are fully vaccinated. Those aged 5-11 are well short of those figures, with just over 35% having received at least one dose and 28.5% fully vaccinated, the CDC said on its COVID Data Tracker.
A look at recent activity shows that children are not gaining on adults, who are much more likely to be vaccinated – full vaccination in those aged 50-64, for example, is 80%. During the 2 weeks from April 17-30, the 5- to 11-year-olds represented 10.5% of those who had initiated a first dose and 12.4% of those who gained full-vaccination status, both of which were well below the oldest age groups, the CDC reported.
Moderna submitted a request to the Food and Drug administration for emergency use authorization of its COVID-19 vaccine in children under the age of 6 years, according to this news organization, and Pfizer/BioNTech officially applied for authorization of a booster dose in children aged 5-11, the companies announced.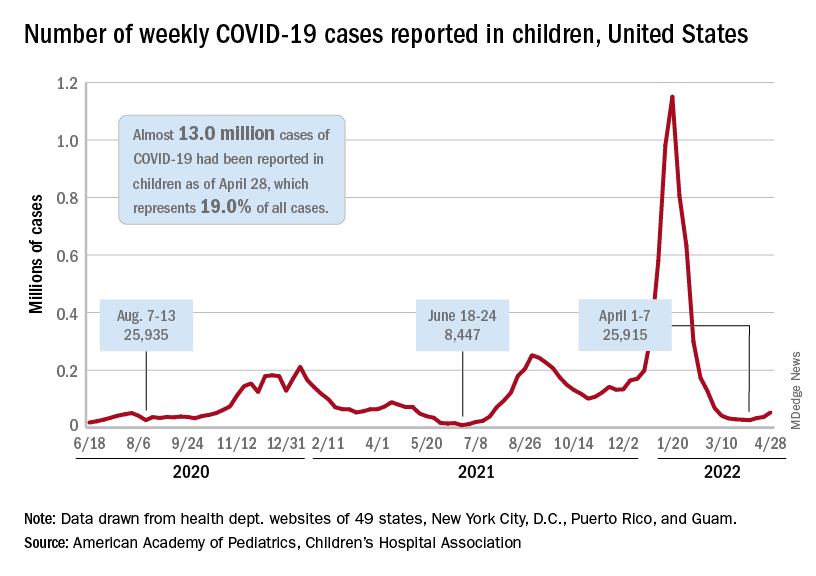
The FDA has tentatively scheduled meetings of its Vaccines and Related Biological Products Advisory Committee in June to consider the applications, saying that it “understands the urgency to authorize a vaccine for age groups who are not currently eligible for vaccination and will work diligently to complete our evaluation of the data. Should any of the submissions be completed in a timely manner and the data support a clear path forward following our evaluation, the FDA will act quickly” to convene the necessary meetings.
The need for greater access to vaccines seems to be increasing, as new pediatric COVID cases rose for the third consecutive week. April 22-28 saw over 53,000 new cases reported in children, up 43.5% from the previous week and up 105% since cases started rising again after dipping under 26,000 during the week of April 1-7, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
Hospital admissions involving diagnosed COVID also ticked up over the latter half of April, although the most recent 7-day average (April 24-30) of 112 per day was lower than the 117 reported for the previous week (April 17-23), the Centers for Disease Control and Prevention said, also noting that figures for the latest week “should be interpreted with caution.”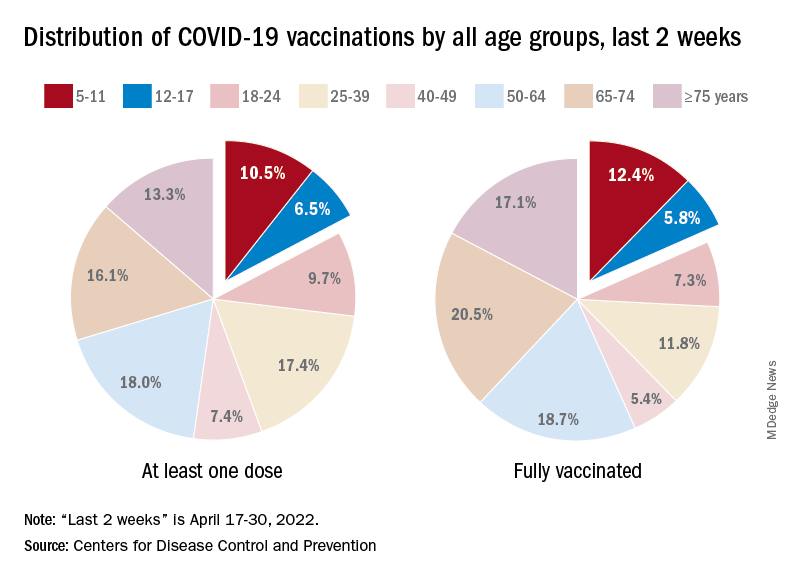
Vaccinations also were up slightly in children aged 5-11 years, with 52,000 receiving their first dose during the week of April 21-27, compared with 48,000 the week before. There was a slight dip, however, among 12- to 17-year-olds, who received 34,000 first doses during April 21-27, versus 35,000 the previous week, the AAP said in a separate report.
Cumulatively, almost 69% of all children aged 12-17 years have received at least one dose of the COVID-19 vaccine and 59% are fully vaccinated. Those aged 5-11 are well short of those figures, with just over 35% having received at least one dose and 28.5% fully vaccinated, the CDC said on its COVID Data Tracker.
A look at recent activity shows that children are not gaining on adults, who are much more likely to be vaccinated – full vaccination in those aged 50-64, for example, is 80%. During the 2 weeks from April 17-30, the 5- to 11-year-olds represented 10.5% of those who had initiated a first dose and 12.4% of those who gained full-vaccination status, both of which were well below the oldest age groups, the CDC reported.
Paxlovid doesn’t prevent infection in households, Pfizer says
Paxlovid works as a treatment for COVID-19 but not as a preventive measure, particularly if you’ve been exposed to the coronavirus through a household member who is infected, according to a new announcement from Pfizer.
In a clinical trial, the oral antiviral tablets were tested for postexposure prophylactic use, or tested for how well they prevented a coronavirus infection in people exposed to the virus. Paxlovid somewhat reduced the risk of infection, but the results weren’t statistically significant.
“We designed the clinical development program for Paxlovid to be comprehensive and ambitious with the aim of being able to help combat COVID-19 in a very broad population of patients,” Albert Bourla, PhD, Pfizer’s chairman and CEO, said in the announcement.
“While we are disappointed in the outcome of this particular study, these results do not impact the strong efficacy and safety data we’ve observed in our earlier trial for the treatment of COVID-19 patients at high risk of developing severe illness,” he said.
The trial included nearly 3,000 adults who were living with someone who recently tested positive for COVID-19 and had symptoms. The people in the trial, who tested negative and didn’t have symptoms, were given either Paxlovid twice daily for 5 or 10 days or a placebo. The study recruitment began in September 2021 and was completed during the peak of the Omicron wave.
Those who took the 5-day course of Paxlovid were found to be 32% less likely to become infected than the placebo group. Those who took the 10-day treatment had a 37% risk reduction. But the results weren’t statistically significant and may have been because of chance.
“Traditionally, it’s been difficult to use small-molecule antivirals for true prophylaxis because the biology of treating infection is different from the biology of preventing infection,” Daniel Barouch, MD, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center, told STAT News.
He also noted that the Omicron variant could have played a role.
“That hyperinfectiousness probably makes it more difficult to prevent infections,” Dr. Barouch said.
The safety data was consistent with that of previous studies, Pfizer said, which found that the treatment was about 90% effective at preventing hospitalization or death in COVID-19 patients with a high risk of severe illness if the pills were taken for 5 days soon after symptoms started.
Paxlovid is approved or authorized for conditional or emergency use in more than 60 countries to treat high-risk COVID-19 patients, Pfizer said. In the United States, the drug is authorized for emergency use for the treatment of mild to moderate COVID-19 in those aged 12 and older who face high risks for severe disease, hospitalization, or death.
The full study data will be released in coming months and submitted to a peer-reviewed publication, the company said. More details are on the ClinicalTrials.gov website (NCT05047601).
A version of this article first appeared on WebMD.com.
Paxlovid works as a treatment for COVID-19 but not as a preventive measure, particularly if you’ve been exposed to the coronavirus through a household member who is infected, according to a new announcement from Pfizer.
In a clinical trial, the oral antiviral tablets were tested for postexposure prophylactic use, or tested for how well they prevented a coronavirus infection in people exposed to the virus. Paxlovid somewhat reduced the risk of infection, but the results weren’t statistically significant.
“We designed the clinical development program for Paxlovid to be comprehensive and ambitious with the aim of being able to help combat COVID-19 in a very broad population of patients,” Albert Bourla, PhD, Pfizer’s chairman and CEO, said in the announcement.
“While we are disappointed in the outcome of this particular study, these results do not impact the strong efficacy and safety data we’ve observed in our earlier trial for the treatment of COVID-19 patients at high risk of developing severe illness,” he said.
The trial included nearly 3,000 adults who were living with someone who recently tested positive for COVID-19 and had symptoms. The people in the trial, who tested negative and didn’t have symptoms, were given either Paxlovid twice daily for 5 or 10 days or a placebo. The study recruitment began in September 2021 and was completed during the peak of the Omicron wave.
Those who took the 5-day course of Paxlovid were found to be 32% less likely to become infected than the placebo group. Those who took the 10-day treatment had a 37% risk reduction. But the results weren’t statistically significant and may have been because of chance.
“Traditionally, it’s been difficult to use small-molecule antivirals for true prophylaxis because the biology of treating infection is different from the biology of preventing infection,” Daniel Barouch, MD, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center, told STAT News.
He also noted that the Omicron variant could have played a role.
“That hyperinfectiousness probably makes it more difficult to prevent infections,” Dr. Barouch said.
The safety data was consistent with that of previous studies, Pfizer said, which found that the treatment was about 90% effective at preventing hospitalization or death in COVID-19 patients with a high risk of severe illness if the pills were taken for 5 days soon after symptoms started.
Paxlovid is approved or authorized for conditional or emergency use in more than 60 countries to treat high-risk COVID-19 patients, Pfizer said. In the United States, the drug is authorized for emergency use for the treatment of mild to moderate COVID-19 in those aged 12 and older who face high risks for severe disease, hospitalization, or death.
The full study data will be released in coming months and submitted to a peer-reviewed publication, the company said. More details are on the ClinicalTrials.gov website (NCT05047601).
A version of this article first appeared on WebMD.com.
Paxlovid works as a treatment for COVID-19 but not as a preventive measure, particularly if you’ve been exposed to the coronavirus through a household member who is infected, according to a new announcement from Pfizer.
In a clinical trial, the oral antiviral tablets were tested for postexposure prophylactic use, or tested for how well they prevented a coronavirus infection in people exposed to the virus. Paxlovid somewhat reduced the risk of infection, but the results weren’t statistically significant.
“We designed the clinical development program for Paxlovid to be comprehensive and ambitious with the aim of being able to help combat COVID-19 in a very broad population of patients,” Albert Bourla, PhD, Pfizer’s chairman and CEO, said in the announcement.
“While we are disappointed in the outcome of this particular study, these results do not impact the strong efficacy and safety data we’ve observed in our earlier trial for the treatment of COVID-19 patients at high risk of developing severe illness,” he said.
The trial included nearly 3,000 adults who were living with someone who recently tested positive for COVID-19 and had symptoms. The people in the trial, who tested negative and didn’t have symptoms, were given either Paxlovid twice daily for 5 or 10 days or a placebo. The study recruitment began in September 2021 and was completed during the peak of the Omicron wave.
Those who took the 5-day course of Paxlovid were found to be 32% less likely to become infected than the placebo group. Those who took the 10-day treatment had a 37% risk reduction. But the results weren’t statistically significant and may have been because of chance.
“Traditionally, it’s been difficult to use small-molecule antivirals for true prophylaxis because the biology of treating infection is different from the biology of preventing infection,” Daniel Barouch, MD, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center, told STAT News.
He also noted that the Omicron variant could have played a role.
“That hyperinfectiousness probably makes it more difficult to prevent infections,” Dr. Barouch said.
The safety data was consistent with that of previous studies, Pfizer said, which found that the treatment was about 90% effective at preventing hospitalization or death in COVID-19 patients with a high risk of severe illness if the pills were taken for 5 days soon after symptoms started.
Paxlovid is approved or authorized for conditional or emergency use in more than 60 countries to treat high-risk COVID-19 patients, Pfizer said. In the United States, the drug is authorized for emergency use for the treatment of mild to moderate COVID-19 in those aged 12 and older who face high risks for severe disease, hospitalization, or death.
The full study data will be released in coming months and submitted to a peer-reviewed publication, the company said. More details are on the ClinicalTrials.gov website (NCT05047601).
A version of this article first appeared on WebMD.com.
How to communicate effectively with patients when tension is high
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
“At my hospital, it was such a big thing to make sure that families are called,” said Dr. Nwankwo, in an interview following a session on compassionate communication at the annual meeting of the American College of Physicians. “So you have 19 patients, and you have to call almost every family to update them. And then you call, and they say, ‘Call this person as well.’ You feel like you’re at your wit’s end a lot of times.”
Sometimes, she has had to dig deep to find the empathy for patients that she knows her patients deserve.
“You really want to care by thinking about where is this patient coming from? What’s going on in their lives? And not just label them a difficult patient,” she said.
Become curious
Auguste Fortin, MD, MPH, offered advice for handling patient interactions under these kinds of circumstances, while serving as a moderator during the session.
“When the going gets tough, turn to wonder.” Become curious about why a patient might be feeling the way they are, he said.
Dr. Fortin, professor of internal medicine at Yale University, New Haven, Conn., said using the ADOBE acronym, has helped him more effectively communicate with his patients. This tool cues him to keep the following in mind: acknowledge, discover, opportunity, boundary setting, and extend.
He went on to explain to the audience why thinking about these terms is useful when interacting with patients.
First, acknowledge the feelings of the patient. Noting that a patient is angry, perhaps counterintuitively, helps, he said. In fact, not acknowledging the anger “throws gasoline on the fire.”
Then, discover the cause of their emotion. Saying "tell me more" and "help me understand" can be powerful tools, he noted.
Next, take this as an opportunity for empathy – especially important to remember when you’re being verbally attacked.
Boundary setting is important, because it lets the patient know that the conversation won’t continue unless they show the same respect the physician is showing, he said.
Finally, physicians can extend the system of support by asking others – such as colleagues or security – for help.
Use the NURS guide to show empathy
Dr. Fortin said he uses the “NURS” guide or calling to mind “name, express, respect, and support” to show empathy:
This involves naming a patient’s emotion; expressing understanding, with phrases like "I can see how you could be …"; showing respect, acknowledging a patient is going through a lot; and offering support, by saying something like, "Let’s see what we can do together to get to the bottom of this," he explained.
“My lived experience in using [these] in this order is that by the end of it, the patient cannot stay mad at me,” Dr. Fortin said.
“It’s really quite remarkable,” he added.
Steps for nonviolent communication
Rebecca Andrews, MD, MS, another moderator for the session, offered these steps for “nonviolent communication”:
- Observing the situation without blame or judgment.
- Telling the person how this situation makes you feel.
- Connecting with a need of the other person.
- Making a request that is specific and based on action, rather than a request not to do something, such as "Would you be willing to … ?"
Dr. Andrews, who is professor of medicine at the University of Connecticut, Farmington, said this approach has worked well for her, both in interactions with patients and in her personal life.
“It is evidence based that compassion actually makes care better,” she noted.
Varun Jain, MD, a member of the audience, expressed gratitude to the session’s speakers for teaching him something that he had not learned in medical school or residency.
“Every week you will have one or two people who will be labeled as ‘difficult,’ ” and it was nice to have some proven advice on how to handle these tough interactions, said the hospitalist at St. Francis Hospital in Hartford, Conn.
“We never got any actual training on this, and we were expected to know this because we are just physicians, and physicians are expected to be compassionate,” Dr. Jain said. “No one taught us how to have compassion.”
Dr. Fortin and Dr. Andrews disclosed no relevant financial relationships.
AT INTERNAL MEDICINE 2022


