User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Captopril questioned for diabetes patients in COVID-19 setting
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Lifestyle changes may explain skin lesions in pandemic-era patients
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
such as lockdown conditions, which may be clarified with additional research.
Lindy P. Fox, MD, professor of dermatology at the University of California, San Francisco, who was not an author of either study, urged caution in interpreting these results. Data from the American Academy of Dermatology and a recent paper from the British Journal of Dermatology suggest a real association exists, at in least some patients. “It’s going to be true that most patients with toe lesions are PCR [polymerase chain reaction]-negative because it tends to be a late phenomenon when patients are no longer shedding virus,” Dr. Fox said in an interview.
Reports about chickenpox-like vesicles, urticaria, and other skin lesions in SARS-CoV-2 patients have circulated in the clinical literature and the media. Acute acro-ischemia has been cited as a potential sign of infection in adolescents and children.
One of the European studies, which was published in JAMA Dermatology, explored this association in 20 patients aged 1-18 years (mean age, 12.3 years), who presented with new-onset acral inflammatory lesions in their hands and feet at La Fe University Hospital, in Valencia, during the country’s peak quarantine period in April. Investigators conducted blood tests and reverse transcriptase–PCR (RT-PCR) for SARS-CoV-2, and six patients had skin biopsies.
Juncal Roca-Ginés, MD, of the department of dermatology, at the Hospital Universitario y Politécnico in La Fe, and coauthors, identified acral erythema in 6 (30%) of the cases, dactylitis in 4 (20%), purpuric maculopapules in 7 (35%), and a mixed pattern in 3 (15%). Serologic and viral testing yielded no positive results for SARS-CoV-2 or other viruses, and none of the patients exhibited COVID-19 symptoms such as fever, dry cough, sore throat, myalgia, or taste or smell disorders. In other findings, 45% of the patients had a history of vascular reactive disease of the hands, and 75% reported walking barefoot in their homes while staying at home. Only two patients reported taking medications.
In the six patients who had a biopsy, the findings were characteristic of chillblains, “confirming the clinical impression,” the authors wrote. Concluding that they could not show a relationship between acute acral skin changes and COVID-19, they noted that “other studies with improved microbiologic tests or molecular techniques aimed at demonstrating the presence of SARS-CoV-2 in the skin may help to clarify this problem.”
The other case series, which was also published in JAMA Dermatology and included 31 adults at a hospital in Brussels, who had recently developed chillblains, also looked for a connection between SARS-CoV-2 and chilblains, in April. Most of the participants were in their teens or 20s. Lesions had appeared on hands, feet, or on both extremities within 1-30 days of consultation, presenting as erythematous or purplish erythematous macules, occasionally with central vesicular or bullous lesions or necrotic areas. Patients reported pain, burning, and itching.
Skin biopsies were obtained in 22 patients and confirmed the diagnosis of chilblains; of the 15 with immunofluorescence analyses, 7 patients were found to have vasculitis of small-diameter vessels.
Of the 31 patients, 20 (64%) reported mild symptoms consistent with SARS-CoV-2, yet none of the RT-PCR or serologic test results showed signs of the virus in all 31 patients. “Because some patients had experienced chilblains for more than 15 days [under 30 days or less] at the time of inclusion, we can reasonably exclude the possibility that serologic testing was done too soon,” observed the authors. They also didn’t find eosinopenia, lymphopenia, and hyperferritinemia, which have been associated with COVID-19, they added.
Changes in lifestyle conditions during the pandemic may explain the appearance of these lesions, according to the authors of both studies, who mentioned that walking around in socks or bare feet and reduced physical activity could have indirectly led to the development of skin lesions.
It’s also possible that young people have less severe disease and a delayed reaction to the virus, Ignacio Torres-Navarro, MD, a dermatologist with La Fe University and the Spanish study’s corresponding author, said in an interview. Their feet may lack maturity in neurovascular regulation and/or the eccrine glands, which can happen in other diseases such as neutrophilic idiopathic eccrine hidradenitis. “In this context, perhaps there was an observational bias of the parents to the children when this manifestation was reported in the media. However, nothing has been demonstrated,” he said.
In an accompanying editor’s note, Claudia Hernandez, MD, of the departments of dermatology and pediatrics, Rush University Medical Center, Chicago, and Anna L. Bruckner, MD, of the departments of dermatology and pediatrics at the University of Colorado, Aurora, wrote that “it is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for ‘COVID toes.’ ” Lack of confirmatory testing and reliance on indirect evidence of infection complicates this further, they noted, adding that “dermatologists must be aware of the protean cutaneous findings that are possibly associated with COVID-19, even if our understanding of their origins remains incomplete.”
In an interview, Dr. Fox, a member of the AAD’s’s COVID-19 Registry task force, offered other possible reasons for the negative antibody tests in the studies. The assay might not have been testing the correct antigen, or the timing of the test might not have been optimal. “More studies will help this become less controversial,” she said.
The authors of the two case series acknowledged potential limitations of their studies. Neither was large in scope: Both took place over a week’s time and included small cohorts. The Belgian study had no control group or long-term follow-up. Little is still known about the clinical manifestations and detection methods for SARS-CoV-2, noted the authors of the Spanish study.
The Spanish study received funding La Fe University Hospital’s department of dermatology, and the authors had no disclosures. The Belgian study received support from the Fondation Saint-Luc, which provided academic funding for its lead author, Marie Baeck, MD, PhD. Another author of this study received personal fees from the Fondation Saint-Luc and personal fees and nonfinancial support from Bioderma. The authors of the editor’s note had no disclosures.
SOURCES: Roca-Ginés J et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2340; Herman A et al. JAMA Dermatol. 2020 Jun 25. doi: 10.1001/jamadermatol.2020.2368.
FDA approves avelumab as maintenance for urothelial carcinoma
The Food and Administration has approved a new indication for the PD-L1 inhibitor avelumab.
Physicians can now prescribe avelumab (Bavencio) as maintenance treatment for patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed after first-line platinum-containing chemotherapy.
The new indication adds to avelumab use in other patient populations, including people with locally advanced or metastatic UC who experience disease progression during or following platinum-containing chemotherapy. The FDA also previously approved avelumab for patients who experienced UC progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
The FDA first approved marketing of avelumab in 2017. Other uses include treatment of metastatic Merkel cell carcinoma and first-line treatment of advanced renal cell carcinoma in combination with axitinib.
The new maintenance therapy indication for avelumab is based on efficacy demonstrated in the JAVELIN Bladder 100 trial. Results from this trial were presented as part of the American Society of Clinical Oncology virtual scientific program.
Investigators randomly assigned 700 patients with unresectable, locally advanced or metastatic UC to intravenous avelumab and best supportive care or best supportive care alone. All participants had UC that had not progressed after first-line platinum-containing chemotherapy.
The median overall survival was 21.4 months in the avelumab arm and 14.3 months in the best supportive care–alone arm (hazard ratio, 0.69; 95% confidence interval, 0.56-0.86). This difference was statistically significant (P = .001).
Avelumab also was associated with significantly longer overall survival in the 51% of participants with PD-L1–positive tumors (hazard ratio, 0.56; 95% confidence interval, 0.40-0.79; P < .001).
Results from the JAVELIN Bladder 100 trial allowed the FDA to convert an initial accelerated approval of avelumab to a regular approval.
Fatigue, musculoskeletal pain, urinary tract infection, and rash were the most common adverse events reported in 20% or more of trial participants. In all, 28% of patients experienced serious adverse events, and one patient died from sepsis during the trial.
Recommended avelumab dosing is 800 mg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progresses or toxicity becomes unacceptable.
See the full prescribing information for more details.
The Food and Administration has approved a new indication for the PD-L1 inhibitor avelumab.
Physicians can now prescribe avelumab (Bavencio) as maintenance treatment for patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed after first-line platinum-containing chemotherapy.
The new indication adds to avelumab use in other patient populations, including people with locally advanced or metastatic UC who experience disease progression during or following platinum-containing chemotherapy. The FDA also previously approved avelumab for patients who experienced UC progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
The FDA first approved marketing of avelumab in 2017. Other uses include treatment of metastatic Merkel cell carcinoma and first-line treatment of advanced renal cell carcinoma in combination with axitinib.
The new maintenance therapy indication for avelumab is based on efficacy demonstrated in the JAVELIN Bladder 100 trial. Results from this trial were presented as part of the American Society of Clinical Oncology virtual scientific program.
Investigators randomly assigned 700 patients with unresectable, locally advanced or metastatic UC to intravenous avelumab and best supportive care or best supportive care alone. All participants had UC that had not progressed after first-line platinum-containing chemotherapy.
The median overall survival was 21.4 months in the avelumab arm and 14.3 months in the best supportive care–alone arm (hazard ratio, 0.69; 95% confidence interval, 0.56-0.86). This difference was statistically significant (P = .001).
Avelumab also was associated with significantly longer overall survival in the 51% of participants with PD-L1–positive tumors (hazard ratio, 0.56; 95% confidence interval, 0.40-0.79; P < .001).
Results from the JAVELIN Bladder 100 trial allowed the FDA to convert an initial accelerated approval of avelumab to a regular approval.
Fatigue, musculoskeletal pain, urinary tract infection, and rash were the most common adverse events reported in 20% or more of trial participants. In all, 28% of patients experienced serious adverse events, and one patient died from sepsis during the trial.
Recommended avelumab dosing is 800 mg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progresses or toxicity becomes unacceptable.
See the full prescribing information for more details.
The Food and Administration has approved a new indication for the PD-L1 inhibitor avelumab.
Physicians can now prescribe avelumab (Bavencio) as maintenance treatment for patients with locally advanced or metastatic urothelial carcinoma (UC) that has not progressed after first-line platinum-containing chemotherapy.
The new indication adds to avelumab use in other patient populations, including people with locally advanced or metastatic UC who experience disease progression during or following platinum-containing chemotherapy. The FDA also previously approved avelumab for patients who experienced UC progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
The FDA first approved marketing of avelumab in 2017. Other uses include treatment of metastatic Merkel cell carcinoma and first-line treatment of advanced renal cell carcinoma in combination with axitinib.
The new maintenance therapy indication for avelumab is based on efficacy demonstrated in the JAVELIN Bladder 100 trial. Results from this trial were presented as part of the American Society of Clinical Oncology virtual scientific program.
Investigators randomly assigned 700 patients with unresectable, locally advanced or metastatic UC to intravenous avelumab and best supportive care or best supportive care alone. All participants had UC that had not progressed after first-line platinum-containing chemotherapy.
The median overall survival was 21.4 months in the avelumab arm and 14.3 months in the best supportive care–alone arm (hazard ratio, 0.69; 95% confidence interval, 0.56-0.86). This difference was statistically significant (P = .001).
Avelumab also was associated with significantly longer overall survival in the 51% of participants with PD-L1–positive tumors (hazard ratio, 0.56; 95% confidence interval, 0.40-0.79; P < .001).
Results from the JAVELIN Bladder 100 trial allowed the FDA to convert an initial accelerated approval of avelumab to a regular approval.
Fatigue, musculoskeletal pain, urinary tract infection, and rash were the most common adverse events reported in 20% or more of trial participants. In all, 28% of patients experienced serious adverse events, and one patient died from sepsis during the trial.
Recommended avelumab dosing is 800 mg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progresses or toxicity becomes unacceptable.
See the full prescribing information for more details.
Sepsis readmissions risk linked to residence in a poor neighborhoods
according to a study published in Critical Care Medicine.
The association between living in a disadvantaged neighborhood and 30-day readmission remained significant even after adjustment for “individual demographic variables, active tobacco use, length of index hospitalization, severity of acute and chronic morbidity, and place of initial discharge,” wrote Panagis Galiatsatos, MD, of Johns Hopkins University in Baltimore, and colleagues.
“Our findings suggest the need for interventions that emphasize neighborhood-level socioeconomic variables in addition to individual-level efforts in an effort to promote and achieve health equity for patients who survive a hospitalization due to sepsis,” the authors wrote. “With a third of our cohort rehospitalized with infections, and other studies emphasizing that the most common readmission diagnosis was infection, attention toward both anticipating and attenuating the risk of infection in sepsis survivors, especially among those who live in higher risk neighborhoods, must be a priority for the prevention of readmissions.”
Although she did not find the study results surprising, Eva DuGoff, PhD, a senior managing consultant with the Berkeley Research Group and a visiting assistant professor at University of Maryland School of Public Health, College Park, said in an interview that she was impressed with how clinically rigorous the analysis was, both in confirming an accurate sepsis diagnosis and in using the more refined measure of the Area Deprivation Index (ADI) to assess neighborhood disadvantage.
“I think it makes sense that people who have less means and are in neighborhoods with fewer resources would run into more issues and would need to return to the hospital, above and beyond the clinical risk factors, such as smoking and chronic conditions,” said Dr. DuGoff, who studies health disparities but was not involved in this study.
Shayla N.M. Durfey MD, ScM, a pediatric resident at Hasbro Children’s Hospital in Providence, R.I., said in an interview she was similarly unsurprised by the findings.
“People who live in disadvantaged neighborhoods may have less access to walking spaces, healthy food, and safe housing and more exposure to poor air quality, toxic stress, and violence – any of which can negatively impact health or recovery from illness through stress responses, nutritional deficiencies, or comorbidities, such as reactive airway disease, obesity, hypertension, and diabetes,” said Dr. Durfey, who studies health disparities but was not involved in this study. “Our research has found these neighborhood-level factors often matter above and beyond individual social determinants of health.”
Dr. Galiatsatos and associates conducted a retrospective study in Baltimore that compared readmission rates in 2017 at Johns Hopkins Bayview Medical Center among patients discharged after a hospitalization for sepsis, coded via ICD-10. They relied on the ADI to categorize the neighborhoods of patients’ residential addresses. The ADI rates various socioeconomic components, including income, education, employment, and housing characteristics, on a scale of 1-100 in geographic blocks, with higher score indicating a greater level of disadvantage.
Among 647 hospitalized patients with an ICD-10 code of sepsis who also met criteria for sepsis or septic shock per the Sepsis-3 definition, 17.9% were excluded from the analysis because they died or were transferred to hospice care. The other 531 patients had an average age of 61, and just under one-third (30.9%) were active smokers. Their average length of stay was 6.9 days, with a mean Charlson Comorbidity Index of 4.2 and a mean Sequential Organ Failure Assessment score of 4.9.
The average ADI for all the patients was 54.2, but the average score was 63 for the 22% of patients who were readmitted within 30 days of initial discharge, compared with an average 51.8 for patients not readmitted (P < .001).
Among those 117 readmitted, “39 patients had a reinfection, 68 had an exacerbation of their chronic conditions, and 10 were admitted for ‘concerning symptoms’ without a primary admitting diagnosis,” the investigators reported. Because “a third of our cohort was readmitted with an infection, it is possible that more disadvantaged neighborhoods created more challenges for a person’s immune system, which may be compromised after recovering from sepsis.”
Dr. DuGoff further noted that health literacy may be lower among people living in less advantaged neighborhoods.
“A number of studies suggest when patients leave the hospital, they’re not sure what they need to do. The language is complicated, and it’s hard to know what kind of medication to take when, and when you’re supposed to return to the doctor or the hospital,” Dr. DuGoff said. “Managing all of that can be pretty scary for people, particularly after a traumatic experience with sepsis at the hospital.”
Most patients had been discharged home (67.3%), but the 31.6% discharged to a skilled nursing facility had a greater likelihood of readmission, compared with those discharged home (P < .01); 1% were discharged to acute rehabilitation. The average length of stay during the index hospitalization was also greater for those readmitted (8.7 days) than for those not readmitted (6.4 days). The groups did not differ in terms of their acute organ dysfunction or severity of their comorbidities.
However, even after adjustment for these factors, “neighborhood disadvantage remained significantly associated with 30-day rehospitalization in patients who were discharged with sepsis,” the authors said. Specifically, each additional standard deviation greater in patients’ ADI was associated with increased risk of 30-day readmission (P < .001).
“Given that the ADI is a composite score, we cannot identify which component is the predominant driver of rehospitalizations for patients who survive sepsis,” the authors wrote. “However, all components that make up the index are intertwined, and policy efforts targeting one (i.e., unemployment) will likely impact others (i.e., housing).”
Dr. Durfey said that medical schools have not traditionally provided training related to management of social risk factors, although this is changing in more recent curricula. But the findings still have clinical relevance for practitioners.
“Certainly, the first step is awareness of where and how patients live and being mindful of how treatment plans may be impacted by social factors at both the individual and community levels,” Dr. Durfey said. “An important part of this is working in partnership with social workers and case managers. Importantly, clinicians can also partner with disadvantaged communities to advocate for improved conditions through policy change and act as expert witnesses to how neighborhood level factors impact health.”
Dr. DuGoff also wondered what implications these findings might have currently, with regards to COVID-19.
“People living in disadvantaged neighborhoods are already at higher risk for getting the disease, and this study raises really good questions about how we should be monitoring discharge now in anticipation of these types of issues,” she said.
The authors noted that their study is cross-sectional and cannot indicate causation, and the findings of a single urban institution may not be generalizable elsewhere. They also did not consider what interventions individual patients had during their index hospitalization that could have increased frailty.
The study did not note external funding. One coauthor of the study, Suchi Saria, PhD, reported receiving honoraria and travel reimbursement from two dozen biotechnology companies for keynotes and advisory board service; she also holds equity in Patient Ping and Bayesian Health. The other authors reported no industry disclosures. In addition to consulting for Berkeley Research Group, Dr. DuGoff has received a past honorarium from Zimmer Biomet. Dr. Durfey has no disclosures.
SOURCE: Galiatsatos P et al. Crit Care Med. 2020 Jun;48(6):808-14.
according to a study published in Critical Care Medicine.
The association between living in a disadvantaged neighborhood and 30-day readmission remained significant even after adjustment for “individual demographic variables, active tobacco use, length of index hospitalization, severity of acute and chronic morbidity, and place of initial discharge,” wrote Panagis Galiatsatos, MD, of Johns Hopkins University in Baltimore, and colleagues.
“Our findings suggest the need for interventions that emphasize neighborhood-level socioeconomic variables in addition to individual-level efforts in an effort to promote and achieve health equity for patients who survive a hospitalization due to sepsis,” the authors wrote. “With a third of our cohort rehospitalized with infections, and other studies emphasizing that the most common readmission diagnosis was infection, attention toward both anticipating and attenuating the risk of infection in sepsis survivors, especially among those who live in higher risk neighborhoods, must be a priority for the prevention of readmissions.”
Although she did not find the study results surprising, Eva DuGoff, PhD, a senior managing consultant with the Berkeley Research Group and a visiting assistant professor at University of Maryland School of Public Health, College Park, said in an interview that she was impressed with how clinically rigorous the analysis was, both in confirming an accurate sepsis diagnosis and in using the more refined measure of the Area Deprivation Index (ADI) to assess neighborhood disadvantage.
“I think it makes sense that people who have less means and are in neighborhoods with fewer resources would run into more issues and would need to return to the hospital, above and beyond the clinical risk factors, such as smoking and chronic conditions,” said Dr. DuGoff, who studies health disparities but was not involved in this study.
Shayla N.M. Durfey MD, ScM, a pediatric resident at Hasbro Children’s Hospital in Providence, R.I., said in an interview she was similarly unsurprised by the findings.
“People who live in disadvantaged neighborhoods may have less access to walking spaces, healthy food, and safe housing and more exposure to poor air quality, toxic stress, and violence – any of which can negatively impact health or recovery from illness through stress responses, nutritional deficiencies, or comorbidities, such as reactive airway disease, obesity, hypertension, and diabetes,” said Dr. Durfey, who studies health disparities but was not involved in this study. “Our research has found these neighborhood-level factors often matter above and beyond individual social determinants of health.”
Dr. Galiatsatos and associates conducted a retrospective study in Baltimore that compared readmission rates in 2017 at Johns Hopkins Bayview Medical Center among patients discharged after a hospitalization for sepsis, coded via ICD-10. They relied on the ADI to categorize the neighborhoods of patients’ residential addresses. The ADI rates various socioeconomic components, including income, education, employment, and housing characteristics, on a scale of 1-100 in geographic blocks, with higher score indicating a greater level of disadvantage.
Among 647 hospitalized patients with an ICD-10 code of sepsis who also met criteria for sepsis or septic shock per the Sepsis-3 definition, 17.9% were excluded from the analysis because they died or were transferred to hospice care. The other 531 patients had an average age of 61, and just under one-third (30.9%) were active smokers. Their average length of stay was 6.9 days, with a mean Charlson Comorbidity Index of 4.2 and a mean Sequential Organ Failure Assessment score of 4.9.
The average ADI for all the patients was 54.2, but the average score was 63 for the 22% of patients who were readmitted within 30 days of initial discharge, compared with an average 51.8 for patients not readmitted (P < .001).
Among those 117 readmitted, “39 patients had a reinfection, 68 had an exacerbation of their chronic conditions, and 10 were admitted for ‘concerning symptoms’ without a primary admitting diagnosis,” the investigators reported. Because “a third of our cohort was readmitted with an infection, it is possible that more disadvantaged neighborhoods created more challenges for a person’s immune system, which may be compromised after recovering from sepsis.”
Dr. DuGoff further noted that health literacy may be lower among people living in less advantaged neighborhoods.
“A number of studies suggest when patients leave the hospital, they’re not sure what they need to do. The language is complicated, and it’s hard to know what kind of medication to take when, and when you’re supposed to return to the doctor or the hospital,” Dr. DuGoff said. “Managing all of that can be pretty scary for people, particularly after a traumatic experience with sepsis at the hospital.”
Most patients had been discharged home (67.3%), but the 31.6% discharged to a skilled nursing facility had a greater likelihood of readmission, compared with those discharged home (P < .01); 1% were discharged to acute rehabilitation. The average length of stay during the index hospitalization was also greater for those readmitted (8.7 days) than for those not readmitted (6.4 days). The groups did not differ in terms of their acute organ dysfunction or severity of their comorbidities.
However, even after adjustment for these factors, “neighborhood disadvantage remained significantly associated with 30-day rehospitalization in patients who were discharged with sepsis,” the authors said. Specifically, each additional standard deviation greater in patients’ ADI was associated with increased risk of 30-day readmission (P < .001).
“Given that the ADI is a composite score, we cannot identify which component is the predominant driver of rehospitalizations for patients who survive sepsis,” the authors wrote. “However, all components that make up the index are intertwined, and policy efforts targeting one (i.e., unemployment) will likely impact others (i.e., housing).”
Dr. Durfey said that medical schools have not traditionally provided training related to management of social risk factors, although this is changing in more recent curricula. But the findings still have clinical relevance for practitioners.
“Certainly, the first step is awareness of where and how patients live and being mindful of how treatment plans may be impacted by social factors at both the individual and community levels,” Dr. Durfey said. “An important part of this is working in partnership with social workers and case managers. Importantly, clinicians can also partner with disadvantaged communities to advocate for improved conditions through policy change and act as expert witnesses to how neighborhood level factors impact health.”
Dr. DuGoff also wondered what implications these findings might have currently, with regards to COVID-19.
“People living in disadvantaged neighborhoods are already at higher risk for getting the disease, and this study raises really good questions about how we should be monitoring discharge now in anticipation of these types of issues,” she said.
The authors noted that their study is cross-sectional and cannot indicate causation, and the findings of a single urban institution may not be generalizable elsewhere. They also did not consider what interventions individual patients had during their index hospitalization that could have increased frailty.
The study did not note external funding. One coauthor of the study, Suchi Saria, PhD, reported receiving honoraria and travel reimbursement from two dozen biotechnology companies for keynotes and advisory board service; she also holds equity in Patient Ping and Bayesian Health. The other authors reported no industry disclosures. In addition to consulting for Berkeley Research Group, Dr. DuGoff has received a past honorarium from Zimmer Biomet. Dr. Durfey has no disclosures.
SOURCE: Galiatsatos P et al. Crit Care Med. 2020 Jun;48(6):808-14.
according to a study published in Critical Care Medicine.
The association between living in a disadvantaged neighborhood and 30-day readmission remained significant even after adjustment for “individual demographic variables, active tobacco use, length of index hospitalization, severity of acute and chronic morbidity, and place of initial discharge,” wrote Panagis Galiatsatos, MD, of Johns Hopkins University in Baltimore, and colleagues.
“Our findings suggest the need for interventions that emphasize neighborhood-level socioeconomic variables in addition to individual-level efforts in an effort to promote and achieve health equity for patients who survive a hospitalization due to sepsis,” the authors wrote. “With a third of our cohort rehospitalized with infections, and other studies emphasizing that the most common readmission diagnosis was infection, attention toward both anticipating and attenuating the risk of infection in sepsis survivors, especially among those who live in higher risk neighborhoods, must be a priority for the prevention of readmissions.”
Although she did not find the study results surprising, Eva DuGoff, PhD, a senior managing consultant with the Berkeley Research Group and a visiting assistant professor at University of Maryland School of Public Health, College Park, said in an interview that she was impressed with how clinically rigorous the analysis was, both in confirming an accurate sepsis diagnosis and in using the more refined measure of the Area Deprivation Index (ADI) to assess neighborhood disadvantage.
“I think it makes sense that people who have less means and are in neighborhoods with fewer resources would run into more issues and would need to return to the hospital, above and beyond the clinical risk factors, such as smoking and chronic conditions,” said Dr. DuGoff, who studies health disparities but was not involved in this study.
Shayla N.M. Durfey MD, ScM, a pediatric resident at Hasbro Children’s Hospital in Providence, R.I., said in an interview she was similarly unsurprised by the findings.
“People who live in disadvantaged neighborhoods may have less access to walking spaces, healthy food, and safe housing and more exposure to poor air quality, toxic stress, and violence – any of which can negatively impact health or recovery from illness through stress responses, nutritional deficiencies, or comorbidities, such as reactive airway disease, obesity, hypertension, and diabetes,” said Dr. Durfey, who studies health disparities but was not involved in this study. “Our research has found these neighborhood-level factors often matter above and beyond individual social determinants of health.”
Dr. Galiatsatos and associates conducted a retrospective study in Baltimore that compared readmission rates in 2017 at Johns Hopkins Bayview Medical Center among patients discharged after a hospitalization for sepsis, coded via ICD-10. They relied on the ADI to categorize the neighborhoods of patients’ residential addresses. The ADI rates various socioeconomic components, including income, education, employment, and housing characteristics, on a scale of 1-100 in geographic blocks, with higher score indicating a greater level of disadvantage.
Among 647 hospitalized patients with an ICD-10 code of sepsis who also met criteria for sepsis or septic shock per the Sepsis-3 definition, 17.9% were excluded from the analysis because they died or were transferred to hospice care. The other 531 patients had an average age of 61, and just under one-third (30.9%) were active smokers. Their average length of stay was 6.9 days, with a mean Charlson Comorbidity Index of 4.2 and a mean Sequential Organ Failure Assessment score of 4.9.
The average ADI for all the patients was 54.2, but the average score was 63 for the 22% of patients who were readmitted within 30 days of initial discharge, compared with an average 51.8 for patients not readmitted (P < .001).
Among those 117 readmitted, “39 patients had a reinfection, 68 had an exacerbation of their chronic conditions, and 10 were admitted for ‘concerning symptoms’ without a primary admitting diagnosis,” the investigators reported. Because “a third of our cohort was readmitted with an infection, it is possible that more disadvantaged neighborhoods created more challenges for a person’s immune system, which may be compromised after recovering from sepsis.”
Dr. DuGoff further noted that health literacy may be lower among people living in less advantaged neighborhoods.
“A number of studies suggest when patients leave the hospital, they’re not sure what they need to do. The language is complicated, and it’s hard to know what kind of medication to take when, and when you’re supposed to return to the doctor or the hospital,” Dr. DuGoff said. “Managing all of that can be pretty scary for people, particularly after a traumatic experience with sepsis at the hospital.”
Most patients had been discharged home (67.3%), but the 31.6% discharged to a skilled nursing facility had a greater likelihood of readmission, compared with those discharged home (P < .01); 1% were discharged to acute rehabilitation. The average length of stay during the index hospitalization was also greater for those readmitted (8.7 days) than for those not readmitted (6.4 days). The groups did not differ in terms of their acute organ dysfunction or severity of their comorbidities.
However, even after adjustment for these factors, “neighborhood disadvantage remained significantly associated with 30-day rehospitalization in patients who were discharged with sepsis,” the authors said. Specifically, each additional standard deviation greater in patients’ ADI was associated with increased risk of 30-day readmission (P < .001).
“Given that the ADI is a composite score, we cannot identify which component is the predominant driver of rehospitalizations for patients who survive sepsis,” the authors wrote. “However, all components that make up the index are intertwined, and policy efforts targeting one (i.e., unemployment) will likely impact others (i.e., housing).”
Dr. Durfey said that medical schools have not traditionally provided training related to management of social risk factors, although this is changing in more recent curricula. But the findings still have clinical relevance for practitioners.
“Certainly, the first step is awareness of where and how patients live and being mindful of how treatment plans may be impacted by social factors at both the individual and community levels,” Dr. Durfey said. “An important part of this is working in partnership with social workers and case managers. Importantly, clinicians can also partner with disadvantaged communities to advocate for improved conditions through policy change and act as expert witnesses to how neighborhood level factors impact health.”
Dr. DuGoff also wondered what implications these findings might have currently, with regards to COVID-19.
“People living in disadvantaged neighborhoods are already at higher risk for getting the disease, and this study raises really good questions about how we should be monitoring discharge now in anticipation of these types of issues,” she said.
The authors noted that their study is cross-sectional and cannot indicate causation, and the findings of a single urban institution may not be generalizable elsewhere. They also did not consider what interventions individual patients had during their index hospitalization that could have increased frailty.
The study did not note external funding. One coauthor of the study, Suchi Saria, PhD, reported receiving honoraria and travel reimbursement from two dozen biotechnology companies for keynotes and advisory board service; she also holds equity in Patient Ping and Bayesian Health. The other authors reported no industry disclosures. In addition to consulting for Berkeley Research Group, Dr. DuGoff has received a past honorarium from Zimmer Biomet. Dr. Durfey has no disclosures.
SOURCE: Galiatsatos P et al. Crit Care Med. 2020 Jun;48(6):808-14.
FROM CRITICAL CARE MEDICINE
Republican or Democrat, Americans vote for face masks
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
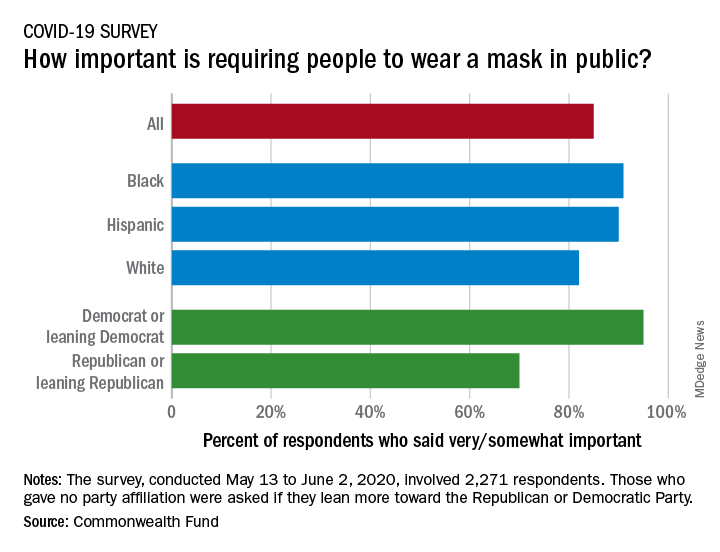
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
In that survey, conducted from May 13 to June 2, 2020, and involving 2,271 respondents, regular COVID-19 testing for everyone was supported by 81% of the sample as way to ensure a safe work environment until a vaccine is available, the researchers said in the report.
Support on both issues was consistently high across both racial/ethnic and political lines. Mandatory mask use gained 91% support among black respondents, 90% in Hispanics, and 82% in whites. There was greater distance between the political parties, but 70% of Republicans and Republican-leaning independents support mask use, compared with 95% of Democrats and Democratic-leaning independents, they said.
Regarding regular testing, 66% of Republicans and those leaning Republican said that it was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Hispanics offered the most support by race/ethnicity, with 90% saying that testing was very/somewhat important, compared with 86% of black respondents and 78% of white respondents, Dr. Collins and associates said.
Two-thirds of Republicans said that it was very/somewhat important for the government to trace the contacts of any person who tested positive for COVID-19, a sentiment shared by 91% of Democrats. That type of tracing was supported by 88% of blacks, 85% of Hispanics, and 79% of whites, based on the polling results.
The survey, conducted for the Commonwealth Fund by the survey and market research firm SSRS, had a margin of error of ± 2.4 percentage points.
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
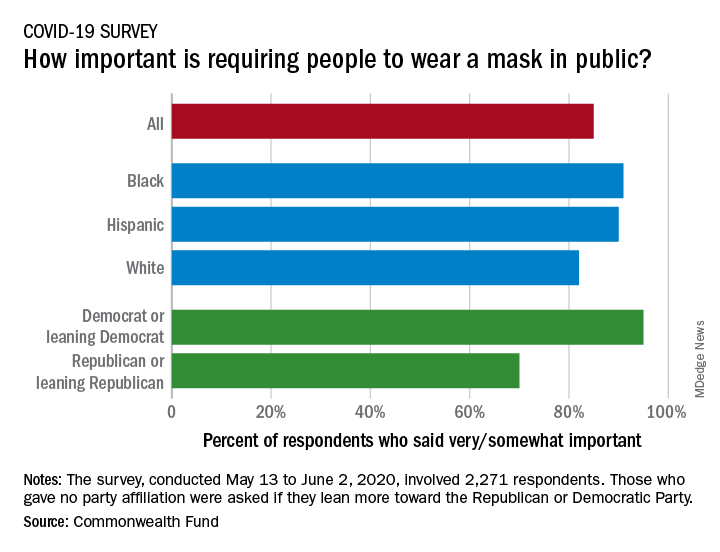
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
In that survey, conducted from May 13 to June 2, 2020, and involving 2,271 respondents, regular COVID-19 testing for everyone was supported by 81% of the sample as way to ensure a safe work environment until a vaccine is available, the researchers said in the report.
Support on both issues was consistently high across both racial/ethnic and political lines. Mandatory mask use gained 91% support among black respondents, 90% in Hispanics, and 82% in whites. There was greater distance between the political parties, but 70% of Republicans and Republican-leaning independents support mask use, compared with 95% of Democrats and Democratic-leaning independents, they said.
Regarding regular testing, 66% of Republicans and those leaning Republican said that it was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Hispanics offered the most support by race/ethnicity, with 90% saying that testing was very/somewhat important, compared with 86% of black respondents and 78% of white respondents, Dr. Collins and associates said.
Two-thirds of Republicans said that it was very/somewhat important for the government to trace the contacts of any person who tested positive for COVID-19, a sentiment shared by 91% of Democrats. That type of tracing was supported by 88% of blacks, 85% of Hispanics, and 79% of whites, based on the polling results.
The survey, conducted for the Commonwealth Fund by the survey and market research firm SSRS, had a margin of error of ± 2.4 percentage points.
Most Americans support the required use of face masks in public, along with universal COVID-19 testing, to provide a safe work environment during the pandemic, according to a new report from the Commonwealth Fund.
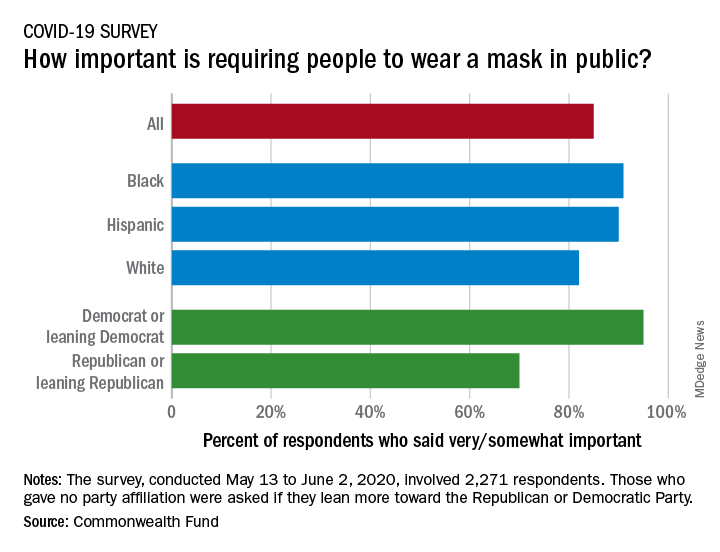
Results of a recent survey show that 85% of adults believe that it is very or somewhat important to require everyone to wear a face mask “at work, when shopping, and on public transportation,” said Sara R. Collins, PhD, vice president for health care coverage and access at the fund, and associates.
In that survey, conducted from May 13 to June 2, 2020, and involving 2,271 respondents, regular COVID-19 testing for everyone was supported by 81% of the sample as way to ensure a safe work environment until a vaccine is available, the researchers said in the report.
Support on both issues was consistently high across both racial/ethnic and political lines. Mandatory mask use gained 91% support among black respondents, 90% in Hispanics, and 82% in whites. There was greater distance between the political parties, but 70% of Republicans and Republican-leaning independents support mask use, compared with 95% of Democrats and Democratic-leaning independents, they said.
Regarding regular testing, 66% of Republicans and those leaning Republican said that it was very/somewhat important to ensure a safe work environment, as did 91% on the Democratic side. Hispanics offered the most support by race/ethnicity, with 90% saying that testing was very/somewhat important, compared with 86% of black respondents and 78% of white respondents, Dr. Collins and associates said.
Two-thirds of Republicans said that it was very/somewhat important for the government to trace the contacts of any person who tested positive for COVID-19, a sentiment shared by 91% of Democrats. That type of tracing was supported by 88% of blacks, 85% of Hispanics, and 79% of whites, based on the polling results.
The survey, conducted for the Commonwealth Fund by the survey and market research firm SSRS, had a margin of error of ± 2.4 percentage points.
Real-world data support adjuvant immunotherapy for stage III melanoma
Among patients with stage IIIC disease, the 2-year survival rate was 70% in those who received immunotherapy and 59% in those who did not (P < .01). The median overall survival in this group was 32.8 months with immunotherapy and 28 months without it (P < .01).
Among patients with stage IIIA disease, the 2-year survival rate was 94% with immunotherapy and 91% without it (P = .03).
There was a trend toward a 2-year survival benefit with immunotherapy in patients with stage IIIB disease and in all 4,094 stage III patients, but the differences were not significant. The 2-year survival rate was 84% with immunotherapy and 81% without it among patients with stage IIIB disease (P = .35). The survival rates were 83% and 80%, respectively, in all stage III patients (P = .051).
This was an early analysis, noted investigator Justin Moyers, MD, of Loma Linda (Calif.) University. Ipilimumab was approved as adjuvant therapy for stage III melanoma patients in 2015, the year patients from this analysis were diagnosed.
“There’s really only 2 full years of survival data,” Dr. Moyers said. “I think given time, we will see a benefit amongst all the substages.”
In the meantime, “I would definitely not use this data to say whether or not [immunotherapy] should be given,” Dr. Moyers said.
The researchers were just using the database – which captures 52% of U.S. melanoma cases – to see if “real-world data mimics the clinical trial data,” Dr. Moyers said.
Overall, the findings support “adjuvant immunotherapy in the real-world setting,” he said.
The researchers also looked at treatment patterns in 2015-2016 across 8,160 patients with stage III melanoma, 4,094 of whom were included in the aforementioned survival analysis. There were 2,260 patients (27.7%) who received immunotherapy after surgery during that time period.
Uptake of adjuvant immunotherapy “was low to start, but those patients did better than ones who did not get” it, said AACR president Antoni Ribas, MD, PhD, of the University of California, Los Angeles, who was not involved in the study.
Immunotherapy recipients were younger, on average (54.8 years vs. 62.4 years). Patients with Charlson comorbidity scores above zero and those on Medicare were less likely to receive immunotherapy (18.4% Medicare vs. over 30% with other payers). There also were trends of decreased use with lower income and lower high school graduation rates.
The finding “highlights the negative impact of socioeconomic [factors] on access to proven therapy,” Dr. Ribas said.
As for low use among Medicare patients, uptake of new treatments, in general, “seems to be faster with private insurance,” he noted.
The study excluded patients who received systemic therapies other than immunotherapy, as well as those who received immunotherapy before surgery. Among study limitations, the specific immunotherapies patients received was unknown.
There was no external funding for this study. Dr. Moyers reported travel compensation from Astellas Pharmaceuticals in 2018. Dr. Ribas disclosed relationships with Amgen, Chugai, Merck, Sanofi, Tango, Arcus, Bioncotech, Compugen, CytomX, FLX Bio, ImaginAb, Isoplexis, Merus, Rgenix, and PACT.
SOURCE: Moyers J et al. AACR 2020, Abstract 4338.
Among patients with stage IIIC disease, the 2-year survival rate was 70% in those who received immunotherapy and 59% in those who did not (P < .01). The median overall survival in this group was 32.8 months with immunotherapy and 28 months without it (P < .01).
Among patients with stage IIIA disease, the 2-year survival rate was 94% with immunotherapy and 91% without it (P = .03).
There was a trend toward a 2-year survival benefit with immunotherapy in patients with stage IIIB disease and in all 4,094 stage III patients, but the differences were not significant. The 2-year survival rate was 84% with immunotherapy and 81% without it among patients with stage IIIB disease (P = .35). The survival rates were 83% and 80%, respectively, in all stage III patients (P = .051).
This was an early analysis, noted investigator Justin Moyers, MD, of Loma Linda (Calif.) University. Ipilimumab was approved as adjuvant therapy for stage III melanoma patients in 2015, the year patients from this analysis were diagnosed.
“There’s really only 2 full years of survival data,” Dr. Moyers said. “I think given time, we will see a benefit amongst all the substages.”
In the meantime, “I would definitely not use this data to say whether or not [immunotherapy] should be given,” Dr. Moyers said.
The researchers were just using the database – which captures 52% of U.S. melanoma cases – to see if “real-world data mimics the clinical trial data,” Dr. Moyers said.
Overall, the findings support “adjuvant immunotherapy in the real-world setting,” he said.
The researchers also looked at treatment patterns in 2015-2016 across 8,160 patients with stage III melanoma, 4,094 of whom were included in the aforementioned survival analysis. There were 2,260 patients (27.7%) who received immunotherapy after surgery during that time period.
Uptake of adjuvant immunotherapy “was low to start, but those patients did better than ones who did not get” it, said AACR president Antoni Ribas, MD, PhD, of the University of California, Los Angeles, who was not involved in the study.
Immunotherapy recipients were younger, on average (54.8 years vs. 62.4 years). Patients with Charlson comorbidity scores above zero and those on Medicare were less likely to receive immunotherapy (18.4% Medicare vs. over 30% with other payers). There also were trends of decreased use with lower income and lower high school graduation rates.
The finding “highlights the negative impact of socioeconomic [factors] on access to proven therapy,” Dr. Ribas said.
As for low use among Medicare patients, uptake of new treatments, in general, “seems to be faster with private insurance,” he noted.
The study excluded patients who received systemic therapies other than immunotherapy, as well as those who received immunotherapy before surgery. Among study limitations, the specific immunotherapies patients received was unknown.
There was no external funding for this study. Dr. Moyers reported travel compensation from Astellas Pharmaceuticals in 2018. Dr. Ribas disclosed relationships with Amgen, Chugai, Merck, Sanofi, Tango, Arcus, Bioncotech, Compugen, CytomX, FLX Bio, ImaginAb, Isoplexis, Merus, Rgenix, and PACT.
SOURCE: Moyers J et al. AACR 2020, Abstract 4338.
Among patients with stage IIIC disease, the 2-year survival rate was 70% in those who received immunotherapy and 59% in those who did not (P < .01). The median overall survival in this group was 32.8 months with immunotherapy and 28 months without it (P < .01).
Among patients with stage IIIA disease, the 2-year survival rate was 94% with immunotherapy and 91% without it (P = .03).
There was a trend toward a 2-year survival benefit with immunotherapy in patients with stage IIIB disease and in all 4,094 stage III patients, but the differences were not significant. The 2-year survival rate was 84% with immunotherapy and 81% without it among patients with stage IIIB disease (P = .35). The survival rates were 83% and 80%, respectively, in all stage III patients (P = .051).
This was an early analysis, noted investigator Justin Moyers, MD, of Loma Linda (Calif.) University. Ipilimumab was approved as adjuvant therapy for stage III melanoma patients in 2015, the year patients from this analysis were diagnosed.
“There’s really only 2 full years of survival data,” Dr. Moyers said. “I think given time, we will see a benefit amongst all the substages.”
In the meantime, “I would definitely not use this data to say whether or not [immunotherapy] should be given,” Dr. Moyers said.
The researchers were just using the database – which captures 52% of U.S. melanoma cases – to see if “real-world data mimics the clinical trial data,” Dr. Moyers said.
Overall, the findings support “adjuvant immunotherapy in the real-world setting,” he said.
The researchers also looked at treatment patterns in 2015-2016 across 8,160 patients with stage III melanoma, 4,094 of whom were included in the aforementioned survival analysis. There were 2,260 patients (27.7%) who received immunotherapy after surgery during that time period.
Uptake of adjuvant immunotherapy “was low to start, but those patients did better than ones who did not get” it, said AACR president Antoni Ribas, MD, PhD, of the University of California, Los Angeles, who was not involved in the study.
Immunotherapy recipients were younger, on average (54.8 years vs. 62.4 years). Patients with Charlson comorbidity scores above zero and those on Medicare were less likely to receive immunotherapy (18.4% Medicare vs. over 30% with other payers). There also were trends of decreased use with lower income and lower high school graduation rates.
The finding “highlights the negative impact of socioeconomic [factors] on access to proven therapy,” Dr. Ribas said.
As for low use among Medicare patients, uptake of new treatments, in general, “seems to be faster with private insurance,” he noted.
The study excluded patients who received systemic therapies other than immunotherapy, as well as those who received immunotherapy before surgery. Among study limitations, the specific immunotherapies patients received was unknown.
There was no external funding for this study. Dr. Moyers reported travel compensation from Astellas Pharmaceuticals in 2018. Dr. Ribas disclosed relationships with Amgen, Chugai, Merck, Sanofi, Tango, Arcus, Bioncotech, Compugen, CytomX, FLX Bio, ImaginAb, Isoplexis, Merus, Rgenix, and PACT.
SOURCE: Moyers J et al. AACR 2020, Abstract 4338.
FROM AACR 2020
Three stages to COVID-19 brain damage, new review suggests
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” lead author Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center in McLean, Va., said.
“Hospitalized patients with COVID-19 should have a neurological evaluation and ideally a brain MRI before leaving the hospital; and, if there are abnormalities, they should follow up with a neurologist in 3-4 months,” said Dr. Fotuhi, who is also affiliate staff at Johns Hopkins Medicine, Baltimore.
The review was published online June 8 in the Journal of Alzheimer’s Disease.
Wreaks CNS havoc
It has become “increasingly evident” that SARS-CoV-2 can cause neurologic manifestations, including anosmia, seizures, stroke, confusion, encephalopathy, and total paralysis, the authors wrote.
They noted that SARS-CoV-2 binds to ACE2, which facilitates the conversion of angiotensin II to angiotensin. After ACE2 has bound to respiratory epithelial cells and then to epithelial cells in blood vessels, SARS-CoV-2 triggers the formation of a “cytokine storm.”
These cytokines, in turn, increase vascular permeability, edema, and widespread inflammation, as well as triggering “hypercoagulation cascades,” which cause small and large blood clots that affect multiple organs.
If SARS-CoV-2 crosses the blood-brain barrier, directly entering the brain, it can contribute to demyelination or neurodegeneration.
“We very thoroughly reviewed the literature published between Jan. 1 and May 1, 2020, about neurological issues [in COVID-19] and what I found interesting is that so many neurological things can happen due to a virus which is so small,” said Dr. Fotuhi.
“This virus’ DNA has such limited information, and yet it can wreak havoc on our nervous system because it kicks off such a potent defense system in our body that damages our nervous system,” he said.
Three-stage classification
- Stage 1: The extent of SARS-CoV-2 binding to the ACE2 receptors is limited to the nasal and gustatory epithelial cells, with the cytokine storm remaining “low and controlled.” During this stage, patients may experience smell or taste impairments, but often recover without any interventions.
- Stage 2: A “robust immune response” is activated by the virus, leading to inflammation in the blood vessels, increased hypercoagulability factors, and the formation of blood clots in cerebral arteries and veins. The patient may therefore experience either large or small strokes. Additional stage 2 symptoms include fatigue, hemiplegia, sensory loss, , tetraplegia, , or ataxia.
- Stage 3: The cytokine storm in the blood vessels is so severe that it causes an “explosive inflammatory response” and penetrates the blood-brain barrier, leading to the entry of cytokines, blood components, and viral particles into the brain parenchyma and causing neuronal cell death and encephalitis. This stage can be characterized by seizures, confusion, , coma, loss of consciousness, or death.
“Patients in stage 3 are more likely to have long-term consequences, because there is evidence that the virus particles have actually penetrated the brain, and we know that SARS-CoV-2 can remain dormant in neurons for many years,” said Dr. Fotuhi.
“Studies of coronaviruses have shown a link between the viruses and the risk of multiple sclerosis or Parkinson’s disease even decades later,” he added.
“Based on several reports in recent months, between 36% to 55% of patients with COVID-19 that are hospitalized have some neurological symptoms, but if you don’t look for them, you won’t see them,” Dr. Fotuhi noted.
As a result, patients should be monitored over time after discharge, as they may develop cognitive dysfunction down the road.
Additionally, “it is imperative for patients [hospitalized with COVID-19] to get a baseline MRI before leaving the hospital so that we have a starting point for future evaluation and treatment,” said Dr. Fotuhi.
“The good news is that neurological manifestations of COVID-19 are treatable,” and “can improve with intensive training,” including lifestyle changes – such as a heart-healthy diet, regular physical activity, stress reduction, improved sleep, biofeedback, and brain rehabilitation, Dr. Fotuhi added.
Routine MRI not necessary
Kenneth Tyler, MD, chair of the department of neurology at the University of Colorado at Denver, Aurora, disagreed that all hospitalized patients with COVID-19 should routinely receive an MRI.
“Whenever you are using a piece of equipment on patients who are COVID-19 infected, you risk introducing the infection to uninfected patients,” he said. Instead, “the indication is in patients who develop unexplained neurological manifestations – altered mental status or focal seizures, for example – because in those cases, you do need to understand whether there are underlying structural abnormalities,” said Dr. Tyler, who was not involved in the review.
Also commenting on the review, Vanja Douglas, MD, associate professor of clinical neurology, University of California, San Francisco, described the review as “thorough” and suggested it may “help us understand how to design observational studies to test whether the associations are due to severe respiratory illness or are specific to SARS-CoV-2 infection.”
Dr. Douglas, who was not involved in the review, added that it is “helpful in giving us a sense of which neurologic syndromes have been observed in COVID-19 patients, and therefore which patients neurologists may want to screen more carefully during the pandemic.”
The study had no specific funding. Dr. Fotuhi disclosed no relevant financial relationships. One coauthor reported receiving consulting fees as a member of the scientific advisory board for Brainreader and reports royalties for expert witness consultation in conjunction with Neurevolution. Dr. Tyler and Dr. Douglas disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” lead author Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center in McLean, Va., said.
“Hospitalized patients with COVID-19 should have a neurological evaluation and ideally a brain MRI before leaving the hospital; and, if there are abnormalities, they should follow up with a neurologist in 3-4 months,” said Dr. Fotuhi, who is also affiliate staff at Johns Hopkins Medicine, Baltimore.
The review was published online June 8 in the Journal of Alzheimer’s Disease.
Wreaks CNS havoc
It has become “increasingly evident” that SARS-CoV-2 can cause neurologic manifestations, including anosmia, seizures, stroke, confusion, encephalopathy, and total paralysis, the authors wrote.
They noted that SARS-CoV-2 binds to ACE2, which facilitates the conversion of angiotensin II to angiotensin. After ACE2 has bound to respiratory epithelial cells and then to epithelial cells in blood vessels, SARS-CoV-2 triggers the formation of a “cytokine storm.”
These cytokines, in turn, increase vascular permeability, edema, and widespread inflammation, as well as triggering “hypercoagulation cascades,” which cause small and large blood clots that affect multiple organs.
If SARS-CoV-2 crosses the blood-brain barrier, directly entering the brain, it can contribute to demyelination or neurodegeneration.
“We very thoroughly reviewed the literature published between Jan. 1 and May 1, 2020, about neurological issues [in COVID-19] and what I found interesting is that so many neurological things can happen due to a virus which is so small,” said Dr. Fotuhi.
“This virus’ DNA has such limited information, and yet it can wreak havoc on our nervous system because it kicks off such a potent defense system in our body that damages our nervous system,” he said.
Three-stage classification
- Stage 1: The extent of SARS-CoV-2 binding to the ACE2 receptors is limited to the nasal and gustatory epithelial cells, with the cytokine storm remaining “low and controlled.” During this stage, patients may experience smell or taste impairments, but often recover without any interventions.
- Stage 2: A “robust immune response” is activated by the virus, leading to inflammation in the blood vessels, increased hypercoagulability factors, and the formation of blood clots in cerebral arteries and veins. The patient may therefore experience either large or small strokes. Additional stage 2 symptoms include fatigue, hemiplegia, sensory loss, , tetraplegia, , or ataxia.
- Stage 3: The cytokine storm in the blood vessels is so severe that it causes an “explosive inflammatory response” and penetrates the blood-brain barrier, leading to the entry of cytokines, blood components, and viral particles into the brain parenchyma and causing neuronal cell death and encephalitis. This stage can be characterized by seizures, confusion, , coma, loss of consciousness, or death.
“Patients in stage 3 are more likely to have long-term consequences, because there is evidence that the virus particles have actually penetrated the brain, and we know that SARS-CoV-2 can remain dormant in neurons for many years,” said Dr. Fotuhi.
“Studies of coronaviruses have shown a link between the viruses and the risk of multiple sclerosis or Parkinson’s disease even decades later,” he added.
“Based on several reports in recent months, between 36% to 55% of patients with COVID-19 that are hospitalized have some neurological symptoms, but if you don’t look for them, you won’t see them,” Dr. Fotuhi noted.
As a result, patients should be monitored over time after discharge, as they may develop cognitive dysfunction down the road.
Additionally, “it is imperative for patients [hospitalized with COVID-19] to get a baseline MRI before leaving the hospital so that we have a starting point for future evaluation and treatment,” said Dr. Fotuhi.
“The good news is that neurological manifestations of COVID-19 are treatable,” and “can improve with intensive training,” including lifestyle changes – such as a heart-healthy diet, regular physical activity, stress reduction, improved sleep, biofeedback, and brain rehabilitation, Dr. Fotuhi added.
Routine MRI not necessary
Kenneth Tyler, MD, chair of the department of neurology at the University of Colorado at Denver, Aurora, disagreed that all hospitalized patients with COVID-19 should routinely receive an MRI.
“Whenever you are using a piece of equipment on patients who are COVID-19 infected, you risk introducing the infection to uninfected patients,” he said. Instead, “the indication is in patients who develop unexplained neurological manifestations – altered mental status or focal seizures, for example – because in those cases, you do need to understand whether there are underlying structural abnormalities,” said Dr. Tyler, who was not involved in the review.
Also commenting on the review, Vanja Douglas, MD, associate professor of clinical neurology, University of California, San Francisco, described the review as “thorough” and suggested it may “help us understand how to design observational studies to test whether the associations are due to severe respiratory illness or are specific to SARS-CoV-2 infection.”
Dr. Douglas, who was not involved in the review, added that it is “helpful in giving us a sense of which neurologic syndromes have been observed in COVID-19 patients, and therefore which patients neurologists may want to screen more carefully during the pandemic.”
The study had no specific funding. Dr. Fotuhi disclosed no relevant financial relationships. One coauthor reported receiving consulting fees as a member of the scientific advisory board for Brainreader and reports royalties for expert witness consultation in conjunction with Neurevolution. Dr. Tyler and Dr. Douglas disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In stage 1, viral damage is limited to epithelial cells of the nose and mouth, and in stage 2 blood clots that form in the lungs may travel to the brain, leading to stroke. In stage 3, the virus crosses the blood-brain barrier and invades the brain.
“Our major take-home points are that patients with COVID-19 symptoms, such as shortness of breath, headache, or dizziness, may have neurological symptoms that, at the time of hospitalization, might not be noticed or prioritized, or whose neurological symptoms may become apparent only after they leave the hospital,” lead author Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center in McLean, Va., said.
“Hospitalized patients with COVID-19 should have a neurological evaluation and ideally a brain MRI before leaving the hospital; and, if there are abnormalities, they should follow up with a neurologist in 3-4 months,” said Dr. Fotuhi, who is also affiliate staff at Johns Hopkins Medicine, Baltimore.
The review was published online June 8 in the Journal of Alzheimer’s Disease.
Wreaks CNS havoc
It has become “increasingly evident” that SARS-CoV-2 can cause neurologic manifestations, including anosmia, seizures, stroke, confusion, encephalopathy, and total paralysis, the authors wrote.
They noted that SARS-CoV-2 binds to ACE2, which facilitates the conversion of angiotensin II to angiotensin. After ACE2 has bound to respiratory epithelial cells and then to epithelial cells in blood vessels, SARS-CoV-2 triggers the formation of a “cytokine storm.”
These cytokines, in turn, increase vascular permeability, edema, and widespread inflammation, as well as triggering “hypercoagulation cascades,” which cause small and large blood clots that affect multiple organs.
If SARS-CoV-2 crosses the blood-brain barrier, directly entering the brain, it can contribute to demyelination or neurodegeneration.
“We very thoroughly reviewed the literature published between Jan. 1 and May 1, 2020, about neurological issues [in COVID-19] and what I found interesting is that so many neurological things can happen due to a virus which is so small,” said Dr. Fotuhi.
“This virus’ DNA has such limited information, and yet it can wreak havoc on our nervous system because it kicks off such a potent defense system in our body that damages our nervous system,” he said.
Three-stage classification
- Stage 1: The extent of SARS-CoV-2 binding to the ACE2 receptors is limited to the nasal and gustatory epithelial cells, with the cytokine storm remaining “low and controlled.” During this stage, patients may experience smell or taste impairments, but often recover without any interventions.
- Stage 2: A “robust immune response” is activated by the virus, leading to inflammation in the blood vessels, increased hypercoagulability factors, and the formation of blood clots in cerebral arteries and veins. The patient may therefore experience either large or small strokes. Additional stage 2 symptoms include fatigue, hemiplegia, sensory loss, , tetraplegia, , or ataxia.
- Stage 3: The cytokine storm in the blood vessels is so severe that it causes an “explosive inflammatory response” and penetrates the blood-brain barrier, leading to the entry of cytokines, blood components, and viral particles into the brain parenchyma and causing neuronal cell death and encephalitis. This stage can be characterized by seizures, confusion, , coma, loss of consciousness, or death.
“Patients in stage 3 are more likely to have long-term consequences, because there is evidence that the virus particles have actually penetrated the brain, and we know that SARS-CoV-2 can remain dormant in neurons for many years,” said Dr. Fotuhi.
“Studies of coronaviruses have shown a link between the viruses and the risk of multiple sclerosis or Parkinson’s disease even decades later,” he added.
“Based on several reports in recent months, between 36% to 55% of patients with COVID-19 that are hospitalized have some neurological symptoms, but if you don’t look for them, you won’t see them,” Dr. Fotuhi noted.
As a result, patients should be monitored over time after discharge, as they may develop cognitive dysfunction down the road.
Additionally, “it is imperative for patients [hospitalized with COVID-19] to get a baseline MRI before leaving the hospital so that we have a starting point for future evaluation and treatment,” said Dr. Fotuhi.
“The good news is that neurological manifestations of COVID-19 are treatable,” and “can improve with intensive training,” including lifestyle changes – such as a heart-healthy diet, regular physical activity, stress reduction, improved sleep, biofeedback, and brain rehabilitation, Dr. Fotuhi added.
Routine MRI not necessary
Kenneth Tyler, MD, chair of the department of neurology at the University of Colorado at Denver, Aurora, disagreed that all hospitalized patients with COVID-19 should routinely receive an MRI.
“Whenever you are using a piece of equipment on patients who are COVID-19 infected, you risk introducing the infection to uninfected patients,” he said. Instead, “the indication is in patients who develop unexplained neurological manifestations – altered mental status or focal seizures, for example – because in those cases, you do need to understand whether there are underlying structural abnormalities,” said Dr. Tyler, who was not involved in the review.
Also commenting on the review, Vanja Douglas, MD, associate professor of clinical neurology, University of California, San Francisco, described the review as “thorough” and suggested it may “help us understand how to design observational studies to test whether the associations are due to severe respiratory illness or are specific to SARS-CoV-2 infection.”
Dr. Douglas, who was not involved in the review, added that it is “helpful in giving us a sense of which neurologic syndromes have been observed in COVID-19 patients, and therefore which patients neurologists may want to screen more carefully during the pandemic.”
The study had no specific funding. Dr. Fotuhi disclosed no relevant financial relationships. One coauthor reported receiving consulting fees as a member of the scientific advisory board for Brainreader and reports royalties for expert witness consultation in conjunction with Neurevolution. Dr. Tyler and Dr. Douglas disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Weight loss failures drive bariatric surgery regrets
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD, of Harvard Medical School, Boston.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders, Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
However, postprocedure problems don’t always equal regrets, he said. “Although many women [in the 2014 study] reported negative thoughts and health issues after weight loss surgery, none of them said they regret undergoing the procedure,” he noted.
To further examine decision regret in patients who underwent gastric bypass and gastric banding, Dr. Jones participated in a study of patients’ attitudes 4 years after gastric bypass and gastric banding (Obes Surg. 2019;29:1624-31).
“Weight loss surgery is neither risk free nor universally effective, yet few studies have examined what proportion of patients regret having undergone weight loss surgery,” he noted.
Dr. Jones and colleagues interviewed patients at two weight loss surgery centers and used specific metrics and a multivariate analysis to examine associations among weight loss, quality of life, and decision regret.
A total of 205 Roux-en-Y gastric bypass (RYGB) patients responded at 1 year after surgery: 181, 156, and 134 patients responded at 2, 3, and 4 years, respectively.
At 1 year, 2% reported regret and that they would not choose the surgery again, and by 4 years, 5% reported regret, based on overall regret scores greater than 50. In addition, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects.
The researchers also interviewed gastric band patients: 170, 157, 146, and 123 responded at years 1,2,3, and 4.
Overall, 8% of these patients expressed regret at 1 year, and 20% expressed regret at 4 years, said Dr. Jones.
“Almost 20% did not think they made the right decision,” he said.
Dr. Jones noted. An average weight loss of 7.4% of excess body weight was associated with regret scores greater than 50, while an average weight loss of 21.1% was associated with regret scores less than 50, he said.
In addition, poor sexual function, but not weight loss or other quality-of-life factors was significantly associated with regret among RYGB patients.
Many surgeons are performing sleeve gastrectomies, which appear to yield greater weight loss than gastric banding and fewer complications than gastric bypass, said Dr. Jones. His study did not include sleeve gastrectomies, but “I expect a sleeve gastrectomy to do pretty well in this analysis,” and to be associated with less patient regret, he said.
Overall, better patient education is key to improving patients’ experiences and reducing feelings of regret, said Dr. Jones.
“The better patients understand the difference between band, bypass, and sleeve preoperatively, the better we can set expectations,” he said. Dr. Jones’ institution has developed an app for laparoscopic sleeve that guides patients through the process from preop through postoperative stay, he noted.
Given the association between amount of weight lost and regret, “setting expectations is very important,” and could include not only written consent but also webinars, information sessions, and apps for patients in advance to help mitigate regrets after the procedure, Dr. Jones concluded.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones disclosed serving on the medical advisory board for Allurion.
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD, of Harvard Medical School, Boston.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders, Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
However, postprocedure problems don’t always equal regrets, he said. “Although many women [in the 2014 study] reported negative thoughts and health issues after weight loss surgery, none of them said they regret undergoing the procedure,” he noted.
To further examine decision regret in patients who underwent gastric bypass and gastric banding, Dr. Jones participated in a study of patients’ attitudes 4 years after gastric bypass and gastric banding (Obes Surg. 2019;29:1624-31).
“Weight loss surgery is neither risk free nor universally effective, yet few studies have examined what proportion of patients regret having undergone weight loss surgery,” he noted.
Dr. Jones and colleagues interviewed patients at two weight loss surgery centers and used specific metrics and a multivariate analysis to examine associations among weight loss, quality of life, and decision regret.
A total of 205 Roux-en-Y gastric bypass (RYGB) patients responded at 1 year after surgery: 181, 156, and 134 patients responded at 2, 3, and 4 years, respectively.
At 1 year, 2% reported regret and that they would not choose the surgery again, and by 4 years, 5% reported regret, based on overall regret scores greater than 50. In addition, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects.
The researchers also interviewed gastric band patients: 170, 157, 146, and 123 responded at years 1,2,3, and 4.
Overall, 8% of these patients expressed regret at 1 year, and 20% expressed regret at 4 years, said Dr. Jones.
“Almost 20% did not think they made the right decision,” he said.
Dr. Jones noted. An average weight loss of 7.4% of excess body weight was associated with regret scores greater than 50, while an average weight loss of 21.1% was associated with regret scores less than 50, he said.
In addition, poor sexual function, but not weight loss or other quality-of-life factors was significantly associated with regret among RYGB patients.
Many surgeons are performing sleeve gastrectomies, which appear to yield greater weight loss than gastric banding and fewer complications than gastric bypass, said Dr. Jones. His study did not include sleeve gastrectomies, but “I expect a sleeve gastrectomy to do pretty well in this analysis,” and to be associated with less patient regret, he said.
Overall, better patient education is key to improving patients’ experiences and reducing feelings of regret, said Dr. Jones.
“The better patients understand the difference between band, bypass, and sleeve preoperatively, the better we can set expectations,” he said. Dr. Jones’ institution has developed an app for laparoscopic sleeve that guides patients through the process from preop through postoperative stay, he noted.
Given the association between amount of weight lost and regret, “setting expectations is very important,” and could include not only written consent but also webinars, information sessions, and apps for patients in advance to help mitigate regrets after the procedure, Dr. Jones concluded.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones disclosed serving on the medical advisory board for Allurion.
Not all weight loss surgery patients “live happily ever after,” according to Daniel B. Jones, MD, of Harvard Medical School, Boston.
A 2014 study of 22 women who underwent weight loss surgery reported lower energy, worse quality of life, and persistent eating disorders, Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
However, postprocedure problems don’t always equal regrets, he said. “Although many women [in the 2014 study] reported negative thoughts and health issues after weight loss surgery, none of them said they regret undergoing the procedure,” he noted.
To further examine decision regret in patients who underwent gastric bypass and gastric banding, Dr. Jones participated in a study of patients’ attitudes 4 years after gastric bypass and gastric banding (Obes Surg. 2019;29:1624-31).
“Weight loss surgery is neither risk free nor universally effective, yet few studies have examined what proportion of patients regret having undergone weight loss surgery,” he noted.
Dr. Jones and colleagues interviewed patients at two weight loss surgery centers and used specific metrics and a multivariate analysis to examine associations among weight loss, quality of life, and decision regret.
A total of 205 Roux-en-Y gastric bypass (RYGB) patients responded at 1 year after surgery: 181, 156, and 134 patients responded at 2, 3, and 4 years, respectively.
At 1 year, 2% reported regret and that they would not choose the surgery again, and by 4 years, 5% reported regret, based on overall regret scores greater than 50. In addition, 13% of patients at 1 year and 4 years reported that weight loss surgery caused “some” or “a lot” of negative effects.
The researchers also interviewed gastric band patients: 170, 157, 146, and 123 responded at years 1,2,3, and 4.
Overall, 8% of these patients expressed regret at 1 year, and 20% expressed regret at 4 years, said Dr. Jones.
“Almost 20% did not think they made the right decision,” he said.
Dr. Jones noted. An average weight loss of 7.4% of excess body weight was associated with regret scores greater than 50, while an average weight loss of 21.1% was associated with regret scores less than 50, he said.
In addition, poor sexual function, but not weight loss or other quality-of-life factors was significantly associated with regret among RYGB patients.
Many surgeons are performing sleeve gastrectomies, which appear to yield greater weight loss than gastric banding and fewer complications than gastric bypass, said Dr. Jones. His study did not include sleeve gastrectomies, but “I expect a sleeve gastrectomy to do pretty well in this analysis,” and to be associated with less patient regret, he said.
Overall, better patient education is key to improving patients’ experiences and reducing feelings of regret, said Dr. Jones.
“The better patients understand the difference between band, bypass, and sleeve preoperatively, the better we can set expectations,” he said. Dr. Jones’ institution has developed an app for laparoscopic sleeve that guides patients through the process from preop through postoperative stay, he noted.
Given the association between amount of weight lost and regret, “setting expectations is very important,” and could include not only written consent but also webinars, information sessions, and apps for patients in advance to help mitigate regrets after the procedure, Dr. Jones concluded.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones disclosed serving on the medical advisory board for Allurion.
FROM MISS
Phase 3 COVID-19 vaccine trials launching in July, expert says
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
The race to develop a SARS-CoV-2 vaccine is unlike any other global research and development effort in modern medicine.
According to Paul A. Offit, MD, there are now 120 Investigational New Drug applications to the Food and Drug Administration for these vaccines, and researchers at more than 70 companies across the globe are interested in making a vaccine. The Biomedical Advanced Research and Development Authority (BARDA) has awarded $2.5 billion to five different pharmaceutical companies to make a vaccine.
“The good news is that the new coronavirus is relatively stable,” Dr. Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said during the virtual Pediatric Dermatology 2020: Best Practices and Innovations Conference. “Although it is a single-stranded RNA virus, it does mutate to some extent, but it doesn’t look like it’s going to mutate away from the vaccine. So, this is not going to be like influenza virus, where you must give a vaccine every year. I think we can make a vaccine that will last for several years. And we know the protein we’re interested in. We’re interested in antibodies directed against the spike glycoprotein, which is abundantly present on the surface of the virus. We know that if we make an antibody response to that protein, we can therefore prevent infection.”
Some research groups are interested in developing a whole, killed virus like those used in the inactivated polio vaccine, and vaccines for hepatitis A virus and rabies, said Dr. Offit, who is a member of Accelerating COVID-19 Technical Innovations And Vaccines, a public-private partnership formed by the National Institutes of Health. Other groups are interested in making a live-attenuated vaccine like those for measles, mumps, and rubella. “Some are interested in using a vectored vaccine, where you take a virus that is relatively weak and doesn’t cause disease in people, like vesicular stomatitis virus, and then clone into that the gene that codes for this coronavirus spike protein, which is the way that we made the Ebola virus vaccine,” Dr. Offit said. “Those approaches have all been used before, with success.”
Novel approaches are also being employed to make this vaccine, including using a replication-defective adenovirus. “That means that the virus can’t reproduce itself, but it can make proteins,” he explained. “There are some proteins that are made, but most aren’t. Therefore, the virus can’t reproduce itself. We’ll see whether or not that [approach] works, but it’s never been used before.”
Another approach is to inject messenger RNA that codes for the coronavirus spike protein, where that genetic material is translated into the spike protein. The other platform being evaluated is a DNA vaccine, in which “you give DNA which is coded for that spike protein, which is transcribed to messenger RNA and then is translated to other proteins.”
Typical vaccine development involves animal models to prove the concept, dose-ranging studies in humans, and progressively larger safety and immunogenicity studies in hundreds of thousands of people. Next come phase 3 studies, “where the proof is in the pudding,” he said. “These are large, prospective placebo-controlled trials to prove that the vaccine is safe. This is the only way whether you can prove or not a vaccine is effective.”
“Some companies may branch out on their own and do smaller studies than that,” he said. “We’ll see how this plays out. Keep your eyes open for that, because you really want to make sure you have a fairly large phase 3 trial. That’s the best way to show whether something works and whether it’s safe.”
The tried and true vaccines that emerge from the effort will not be FDA-licensed products. Rather, they will be approved products under the Emergency Use Authorization program. “Ever since the 1950s, every vaccine that has been used in the U.S. has been under the auspices of FDA licensure,” said Dr. Offit, who is also professor of pediatrics and the Maurice R. Hilleman professor of vaccinology at the University of Pennsylvania, Philadelphia. “That’s not going to be true here. The FDA is involved every step of the way but here they have a somewhat lighter touch.”
A few candidate vaccines are being mass-produced at risk, “meaning they’re being produced not knowing whether these vaccines are safe and effective yet or not,” he said. “But when they’re shown in a phase 3 trial to be safe and effective, you will have already produced it, and then it’s much easier to roll it out to the general public the minute you’ve shown that it works. This is what we did for the polio vaccine back in the 1950s. We mass-produced that vaccine at risk.”
Dr. Offit emphasized the importance of managing expectations once a COVID-19 vaccine gets approved for use. “Regarding safety, these vaccines will be tested in tens of thousands of people, not tens of millions of people, so although you can disprove a relatively uncommon side effect preapproval, you’re not going to disprove a rare side effect preapproval. You’re only going to know that post approval. I think we need to make people aware of that and to let them know that through groups like the Vaccine Safety Datalink, we’re going to be monitoring these vaccines once they’re approved.”
Regarding efficacy, he continued, “we’re not going know about the rates of immunity initially; we’re only going to know about that after the vaccine [has been administered]. My guess is the protection is going to be short lived and incomplete. By short lived, I mean that protection would last for years but not decades. By incomplete, I mean that protection will be against moderate to severe disease, which is fine. You don’t need protection against all of the disease; it’s hard to do that with respiratory viruses. That means you can keep people out of the hospital, and you can keep them from dying. That’s the main goal.”
Dr. Offit closed his remarks by noting that much is at stake in this effort to develop a vaccine so quickly and that it “could go one of two ways. We could find that the vaccine is a lifesaver, and [that] we can finally end this awful pandemic. Or, if we cut corners and don’t prove that the vaccines are safe and effective as we should before they’re released, we could shake what is a fragile vaccine confidence in this country. Hopefully, it doesn’t play out that way.”
FROM PEDIATRIC DERMATOLOGY 2020
Tiragolumab plus atezolizumab active in PD-L1+ NSCLC
The combination of the anti-TIGIT antibody tiragolumab with the PD-L1 inhibitor atezolizumab was well tolerated and showed preliminary activity in the phase 1b portion of the study, according to investigator Johanna C. Bendell, MD, of Sarah Cannon Research Institute/Tennessee Oncology in Nashville, Tenn.
Objective responses occurred mainly in chemoimmunotherapy-naive, PD-L1-positive tumors. In an expansion cohort of 13 patients with PD-L1-positive non–small cell lung cancer (NSCLC), the confirmed overall response rate was 46%, with several responses demonstrating durability.
Dr. Bendell reported these results at the AACR virtual meeting II.
While several important research questions remain, the results in the lung cancer expansion cohort were encouraging, particularly in patients who were smokers and previous smokers, said invited discussant Michele Teng, PhD, of QIMR Berghofer Medical Research Institute in Brisbane, Australia.
“Although it was [a] small cohort, the data suggest promising duration of response in some of the patients [n = 4] who have been under study for more than 700 days,” Dr. Teng said.
Based on the preliminary safety and activity seen in this study, the combination of tiragolumab and atezolizumab is being evaluated in a randomized, placebo-controlled phase 2 study, and a phase 3 study is recruiting.
Rationale, design, and safety
TIGIT is a novel inhibitory receptor expressed on multiple immune cells, especially CD8-positive T cells and natural killer cells, Dr. Bendell explained. She added that TIGIT is coexpressed with PD-1 on immune cells.
“Using anti-TIGIT antibodies to prevent TIGIT from binding, and cotargeting TIGIT and PD-L1, may restore antitumor response and enhance anti-PD-L1 effect,” Dr. Bendell said.
The phase 1 study Dr. Bendell presented, known as GO30103, was designed to evaluate tiragolumab as a single agent and in combination with atezolizumab in advanced solid tumors.
There were 24 patients in the phase 1a portion of GO30103, which was intended to determine the preliminary safety, tolerability, and recommended phase 2 dose of tiragolumab. There were 49 patients treated with tiragolumab plus atezolizumab in the phase 1b portion, which was intended to provide data on pharmacokinetics as well as preliminary antitumor activity of the combination.
No dose-limiting toxicities were seen in either cohort. The recommended phase 2 dose of tiragolumab was 600 mg every 3 weeks.
Tiragolumab was well tolerated in the phase 1a and 1b portions of the trial, according to Dr. Bendell.
“Immune-related adverse events were seen, but their incidence was not out of proportion to events seen with atezolizumab alone,” she said.
Treatment-related grade 3-4 adverse events occurred in one patient (4%) in the phase 1a portion of the trial and two patients (4%) in the phase 1b portion. There were no grade 5 adverse events related to treatment.
Efficacy and next steps
No objective responses were seen with tiragolumab monotherapy, although several patients did exhibit tumor reduction.
“We were not really expecting much single-agent activity of the anti-TIGIT drug,” Dr. Bendell said. “There’s some preclinical data that suggests that TIGIT may be more important as a single agent in earlier stages of cancer.”
In contrast, the combination of tiragolumab and atezolizumab resulted in several responses, including one in a patient with PD-L1-positive NSCLC who was previously treated with immunotherapy, according to Dr. Bendell.
The 13-patient expansion cohort of patients with PD-L1-positive NSCLC were treated at the recommended phase 2 dose of tiragolumab and atezolizumab. In these chemoimmunotherapy-naive patients, the overall response rate was 46%. Responses occurred in 6 of 13 patients and included 2 complete responses. Four patients had stable disease, so the disease control rate was 85% (11/13).
Based on that expansion cohort, a randomized, phase 2 study called CITYSCAPE was initiated. Results of CITYSCAPE were recently presented as part of the American Society of Clinical Oncology virtual scientific program.
In that study, tiragolumab plus atezolizumab improved the overall response rate and progression-free survival when compared with placebo plus atezolizumab. More substantial improvement was seen in the subgroup of patients with PD-L1 tumor proportion scores of 50% or greater.
The activity and safety of tiragolumab plus atezolizumab will be confirmed in the ongoing SKYSCRAPER-01 trial (NCT04294810), a phase 3 study of first-line treatment in patients with NSCLC and a PD-L1 tumor proportion score of 50% or greater, according to investigators.
The phase 1 study presented by Dr. Bendell was sponsored by Genentech. Dr. Bendell disclosed relationships with Genentech/Roche, Gilead, Five Prime, Lilly, and other companies.
SOURCE: Bendell JC et al. AACR 2020, Abstract CT302.
The combination of the anti-TIGIT antibody tiragolumab with the PD-L1 inhibitor atezolizumab was well tolerated and showed preliminary activity in the phase 1b portion of the study, according to investigator Johanna C. Bendell, MD, of Sarah Cannon Research Institute/Tennessee Oncology in Nashville, Tenn.
Objective responses occurred mainly in chemoimmunotherapy-naive, PD-L1-positive tumors. In an expansion cohort of 13 patients with PD-L1-positive non–small cell lung cancer (NSCLC), the confirmed overall response rate was 46%, with several responses demonstrating durability.
Dr. Bendell reported these results at the AACR virtual meeting II.
While several important research questions remain, the results in the lung cancer expansion cohort were encouraging, particularly in patients who were smokers and previous smokers, said invited discussant Michele Teng, PhD, of QIMR Berghofer Medical Research Institute in Brisbane, Australia.
“Although it was [a] small cohort, the data suggest promising duration of response in some of the patients [n = 4] who have been under study for more than 700 days,” Dr. Teng said.
Based on the preliminary safety and activity seen in this study, the combination of tiragolumab and atezolizumab is being evaluated in a randomized, placebo-controlled phase 2 study, and a phase 3 study is recruiting.
Rationale, design, and safety
TIGIT is a novel inhibitory receptor expressed on multiple immune cells, especially CD8-positive T cells and natural killer cells, Dr. Bendell explained. She added that TIGIT is coexpressed with PD-1 on immune cells.
“Using anti-TIGIT antibodies to prevent TIGIT from binding, and cotargeting TIGIT and PD-L1, may restore antitumor response and enhance anti-PD-L1 effect,” Dr. Bendell said.
The phase 1 study Dr. Bendell presented, known as GO30103, was designed to evaluate tiragolumab as a single agent and in combination with atezolizumab in advanced solid tumors.
There were 24 patients in the phase 1a portion of GO30103, which was intended to determine the preliminary safety, tolerability, and recommended phase 2 dose of tiragolumab. There were 49 patients treated with tiragolumab plus atezolizumab in the phase 1b portion, which was intended to provide data on pharmacokinetics as well as preliminary antitumor activity of the combination.
No dose-limiting toxicities were seen in either cohort. The recommended phase 2 dose of tiragolumab was 600 mg every 3 weeks.
Tiragolumab was well tolerated in the phase 1a and 1b portions of the trial, according to Dr. Bendell.
“Immune-related adverse events were seen, but their incidence was not out of proportion to events seen with atezolizumab alone,” she said.
Treatment-related grade 3-4 adverse events occurred in one patient (4%) in the phase 1a portion of the trial and two patients (4%) in the phase 1b portion. There were no grade 5 adverse events related to treatment.
Efficacy and next steps
No objective responses were seen with tiragolumab monotherapy, although several patients did exhibit tumor reduction.
“We were not really expecting much single-agent activity of the anti-TIGIT drug,” Dr. Bendell said. “There’s some preclinical data that suggests that TIGIT may be more important as a single agent in earlier stages of cancer.”
In contrast, the combination of tiragolumab and atezolizumab resulted in several responses, including one in a patient with PD-L1-positive NSCLC who was previously treated with immunotherapy, according to Dr. Bendell.
The 13-patient expansion cohort of patients with PD-L1-positive NSCLC were treated at the recommended phase 2 dose of tiragolumab and atezolizumab. In these chemoimmunotherapy-naive patients, the overall response rate was 46%. Responses occurred in 6 of 13 patients and included 2 complete responses. Four patients had stable disease, so the disease control rate was 85% (11/13).
Based on that expansion cohort, a randomized, phase 2 study called CITYSCAPE was initiated. Results of CITYSCAPE were recently presented as part of the American Society of Clinical Oncology virtual scientific program.
In that study, tiragolumab plus atezolizumab improved the overall response rate and progression-free survival when compared with placebo plus atezolizumab. More substantial improvement was seen in the subgroup of patients with PD-L1 tumor proportion scores of 50% or greater.
The activity and safety of tiragolumab plus atezolizumab will be confirmed in the ongoing SKYSCRAPER-01 trial (NCT04294810), a phase 3 study of first-line treatment in patients with NSCLC and a PD-L1 tumor proportion score of 50% or greater, according to investigators.
The phase 1 study presented by Dr. Bendell was sponsored by Genentech. Dr. Bendell disclosed relationships with Genentech/Roche, Gilead, Five Prime, Lilly, and other companies.
SOURCE: Bendell JC et al. AACR 2020, Abstract CT302.
The combination of the anti-TIGIT antibody tiragolumab with the PD-L1 inhibitor atezolizumab was well tolerated and showed preliminary activity in the phase 1b portion of the study, according to investigator Johanna C. Bendell, MD, of Sarah Cannon Research Institute/Tennessee Oncology in Nashville, Tenn.
Objective responses occurred mainly in chemoimmunotherapy-naive, PD-L1-positive tumors. In an expansion cohort of 13 patients with PD-L1-positive non–small cell lung cancer (NSCLC), the confirmed overall response rate was 46%, with several responses demonstrating durability.
Dr. Bendell reported these results at the AACR virtual meeting II.
While several important research questions remain, the results in the lung cancer expansion cohort were encouraging, particularly in patients who were smokers and previous smokers, said invited discussant Michele Teng, PhD, of QIMR Berghofer Medical Research Institute in Brisbane, Australia.
“Although it was [a] small cohort, the data suggest promising duration of response in some of the patients [n = 4] who have been under study for more than 700 days,” Dr. Teng said.
Based on the preliminary safety and activity seen in this study, the combination of tiragolumab and atezolizumab is being evaluated in a randomized, placebo-controlled phase 2 study, and a phase 3 study is recruiting.
Rationale, design, and safety
TIGIT is a novel inhibitory receptor expressed on multiple immune cells, especially CD8-positive T cells and natural killer cells, Dr. Bendell explained. She added that TIGIT is coexpressed with PD-1 on immune cells.
“Using anti-TIGIT antibodies to prevent TIGIT from binding, and cotargeting TIGIT and PD-L1, may restore antitumor response and enhance anti-PD-L1 effect,” Dr. Bendell said.
The phase 1 study Dr. Bendell presented, known as GO30103, was designed to evaluate tiragolumab as a single agent and in combination with atezolizumab in advanced solid tumors.
There were 24 patients in the phase 1a portion of GO30103, which was intended to determine the preliminary safety, tolerability, and recommended phase 2 dose of tiragolumab. There were 49 patients treated with tiragolumab plus atezolizumab in the phase 1b portion, which was intended to provide data on pharmacokinetics as well as preliminary antitumor activity of the combination.
No dose-limiting toxicities were seen in either cohort. The recommended phase 2 dose of tiragolumab was 600 mg every 3 weeks.
Tiragolumab was well tolerated in the phase 1a and 1b portions of the trial, according to Dr. Bendell.
“Immune-related adverse events were seen, but their incidence was not out of proportion to events seen with atezolizumab alone,” she said.
Treatment-related grade 3-4 adverse events occurred in one patient (4%) in the phase 1a portion of the trial and two patients (4%) in the phase 1b portion. There were no grade 5 adverse events related to treatment.
Efficacy and next steps
No objective responses were seen with tiragolumab monotherapy, although several patients did exhibit tumor reduction.
“We were not really expecting much single-agent activity of the anti-TIGIT drug,” Dr. Bendell said. “There’s some preclinical data that suggests that TIGIT may be more important as a single agent in earlier stages of cancer.”
In contrast, the combination of tiragolumab and atezolizumab resulted in several responses, including one in a patient with PD-L1-positive NSCLC who was previously treated with immunotherapy, according to Dr. Bendell.
The 13-patient expansion cohort of patients with PD-L1-positive NSCLC were treated at the recommended phase 2 dose of tiragolumab and atezolizumab. In these chemoimmunotherapy-naive patients, the overall response rate was 46%. Responses occurred in 6 of 13 patients and included 2 complete responses. Four patients had stable disease, so the disease control rate was 85% (11/13).
Based on that expansion cohort, a randomized, phase 2 study called CITYSCAPE was initiated. Results of CITYSCAPE were recently presented as part of the American Society of Clinical Oncology virtual scientific program.
In that study, tiragolumab plus atezolizumab improved the overall response rate and progression-free survival when compared with placebo plus atezolizumab. More substantial improvement was seen in the subgroup of patients with PD-L1 tumor proportion scores of 50% or greater.
The activity and safety of tiragolumab plus atezolizumab will be confirmed in the ongoing SKYSCRAPER-01 trial (NCT04294810), a phase 3 study of first-line treatment in patients with NSCLC and a PD-L1 tumor proportion score of 50% or greater, according to investigators.
The phase 1 study presented by Dr. Bendell was sponsored by Genentech. Dr. Bendell disclosed relationships with Genentech/Roche, Gilead, Five Prime, Lilly, and other companies.
SOURCE: Bendell JC et al. AACR 2020, Abstract CT302.
FROM AACR 2020