User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Adherence and discontinuation limit triptan outcomes
a new Danish study shows.
“Few people continue on triptans either due to lack of efficacy or too many adverse events,” said Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles. “Some people overuse triptans when they are available and work well, but the patients are not properly informed, and do not listen.”
Migraine headaches fall among some of the most common neurologic disorders and claims the No. 2 spot in diseases that contribute to life lived with disability. An estimated 11.7% have migraine episodes annually, and the disorder carries a high prevalence through the duration of the patient’s life.
Triptans were noted as being a highly effective solution for acute migraine management when they were first introduced in the early 1990s and still remain the first-line treatment for acute migraine management not adequately controlled by ordinary analgesics and NSAIDs. As a drug class, the side-effect profile of triptans can vary, but frequent users run the risk of medication overuse headache, a condition noted by migraines of increased frequency and intensity.
25 years of triptan use
Study investigators conducted a nationwide, register-based cohort study using data collected from 7,435,758 Danish residents who accessed the public health care system between Jan. 1, 1994, and Oct. 31, 2019. The time frame accounts for a period of 139.0 million person-years when the residents were both alive and living in Denmark. Their findings were published online Feb. 14, 2021, in Cephalalgia.
Researchers evaluated and summarized purchases of all triptans in all dosage forms sold in Denmark during that time frame. These were sumatriptan, naratriptan, zolmitriptan, rizatriptan, almotriptan, eletriptan, and frovatriptan. Based on their finding, 381,695 patients purchased triptans at least one time. Triptan users were more likely to be female (75.7%) than male (24.3%).
Dr. Rapoport, who was not involved in the study, feels the differences in use between genders extrapolate to the U.S. migraine population as well. “Three times more women have migraines than men and buy triptans in that ratio,” he said.
Any patient who purchased at least one of any triptan at any point during the course of the study was classified as a triptan user. Triptan overuse is defined as using a triptan greater for at least 10 days a month for 3 consecutive months, as defined by the International Classification of Headache Disorders. It’s important to note that triptan are prescribed to patients for only two indications – migraines and cluster headaches. However, cluster headaches are extremely rare.
The study’s investigators summarized data collected throughout Denmark for more than a quarter of a century. The findings show an increase in triptan use from 345 defined daily doses to 945 defined daily doses per 1,000 residents per year along with an increased prevalence on triptan use from 5.17 to 14.57 per 1,000 inhabitants. In addition, 12.3% of the Danish residents who had migraines bought a triptan between 2014 and 2019 – data Dr. Rapoport noted falls in lines with trends in other Western countries, which range between 12% and 13%.
Nearly half of the first-time triptan buyers (43%) did not purchase another triptan for 5 years. In conflict with established guidelines, 90% of patients that discontinued triptan-based treatment had tried only one triptan type.
One important factor contributing to the ease of data collection is that the Danish population has free health care, coupled with sizable reimbursements for their spending. The country’s accessible health care system negates the effects of barriers related to price and availability while engendering data that more accurately reflects the patients’ experience based on treatment need and satisfaction.
“In a cohort with access to free clinical consultations and low medication costs, we observed low rates of triptan adherence, likely due to disappointing efficacy and/or unpleasant side effects rather than economic considerations. Triptan success continues to be hindered by poor implementation of clinical guidelines and high rates of treatment discontinuance,” the researchers concluded.
“The most surprising thing about this study is it is exactly what I would have expected if triptans in the U.S. were free,” Dr. Rapoport said.
Dr. Rapoport is the editor in chief of Neurology Reviews and serves as a consultant to several pharmaceutical companies.
a new Danish study shows.
“Few people continue on triptans either due to lack of efficacy or too many adverse events,” said Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles. “Some people overuse triptans when they are available and work well, but the patients are not properly informed, and do not listen.”
Migraine headaches fall among some of the most common neurologic disorders and claims the No. 2 spot in diseases that contribute to life lived with disability. An estimated 11.7% have migraine episodes annually, and the disorder carries a high prevalence through the duration of the patient’s life.
Triptans were noted as being a highly effective solution for acute migraine management when they were first introduced in the early 1990s and still remain the first-line treatment for acute migraine management not adequately controlled by ordinary analgesics and NSAIDs. As a drug class, the side-effect profile of triptans can vary, but frequent users run the risk of medication overuse headache, a condition noted by migraines of increased frequency and intensity.
25 years of triptan use
Study investigators conducted a nationwide, register-based cohort study using data collected from 7,435,758 Danish residents who accessed the public health care system between Jan. 1, 1994, and Oct. 31, 2019. The time frame accounts for a period of 139.0 million person-years when the residents were both alive and living in Denmark. Their findings were published online Feb. 14, 2021, in Cephalalgia.
Researchers evaluated and summarized purchases of all triptans in all dosage forms sold in Denmark during that time frame. These were sumatriptan, naratriptan, zolmitriptan, rizatriptan, almotriptan, eletriptan, and frovatriptan. Based on their finding, 381,695 patients purchased triptans at least one time. Triptan users were more likely to be female (75.7%) than male (24.3%).
Dr. Rapoport, who was not involved in the study, feels the differences in use between genders extrapolate to the U.S. migraine population as well. “Three times more women have migraines than men and buy triptans in that ratio,” he said.
Any patient who purchased at least one of any triptan at any point during the course of the study was classified as a triptan user. Triptan overuse is defined as using a triptan greater for at least 10 days a month for 3 consecutive months, as defined by the International Classification of Headache Disorders. It’s important to note that triptan are prescribed to patients for only two indications – migraines and cluster headaches. However, cluster headaches are extremely rare.
The study’s investigators summarized data collected throughout Denmark for more than a quarter of a century. The findings show an increase in triptan use from 345 defined daily doses to 945 defined daily doses per 1,000 residents per year along with an increased prevalence on triptan use from 5.17 to 14.57 per 1,000 inhabitants. In addition, 12.3% of the Danish residents who had migraines bought a triptan between 2014 and 2019 – data Dr. Rapoport noted falls in lines with trends in other Western countries, which range between 12% and 13%.
Nearly half of the first-time triptan buyers (43%) did not purchase another triptan for 5 years. In conflict with established guidelines, 90% of patients that discontinued triptan-based treatment had tried only one triptan type.
One important factor contributing to the ease of data collection is that the Danish population has free health care, coupled with sizable reimbursements for their spending. The country’s accessible health care system negates the effects of barriers related to price and availability while engendering data that more accurately reflects the patients’ experience based on treatment need and satisfaction.
“In a cohort with access to free clinical consultations and low medication costs, we observed low rates of triptan adherence, likely due to disappointing efficacy and/or unpleasant side effects rather than economic considerations. Triptan success continues to be hindered by poor implementation of clinical guidelines and high rates of treatment discontinuance,” the researchers concluded.
“The most surprising thing about this study is it is exactly what I would have expected if triptans in the U.S. were free,” Dr. Rapoport said.
Dr. Rapoport is the editor in chief of Neurology Reviews and serves as a consultant to several pharmaceutical companies.
a new Danish study shows.
“Few people continue on triptans either due to lack of efficacy or too many adverse events,” said Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles. “Some people overuse triptans when they are available and work well, but the patients are not properly informed, and do not listen.”
Migraine headaches fall among some of the most common neurologic disorders and claims the No. 2 spot in diseases that contribute to life lived with disability. An estimated 11.7% have migraine episodes annually, and the disorder carries a high prevalence through the duration of the patient’s life.
Triptans were noted as being a highly effective solution for acute migraine management when they were first introduced in the early 1990s and still remain the first-line treatment for acute migraine management not adequately controlled by ordinary analgesics and NSAIDs. As a drug class, the side-effect profile of triptans can vary, but frequent users run the risk of medication overuse headache, a condition noted by migraines of increased frequency and intensity.
25 years of triptan use
Study investigators conducted a nationwide, register-based cohort study using data collected from 7,435,758 Danish residents who accessed the public health care system between Jan. 1, 1994, and Oct. 31, 2019. The time frame accounts for a period of 139.0 million person-years when the residents were both alive and living in Denmark. Their findings were published online Feb. 14, 2021, in Cephalalgia.
Researchers evaluated and summarized purchases of all triptans in all dosage forms sold in Denmark during that time frame. These were sumatriptan, naratriptan, zolmitriptan, rizatriptan, almotriptan, eletriptan, and frovatriptan. Based on their finding, 381,695 patients purchased triptans at least one time. Triptan users were more likely to be female (75.7%) than male (24.3%).
Dr. Rapoport, who was not involved in the study, feels the differences in use between genders extrapolate to the U.S. migraine population as well. “Three times more women have migraines than men and buy triptans in that ratio,” he said.
Any patient who purchased at least one of any triptan at any point during the course of the study was classified as a triptan user. Triptan overuse is defined as using a triptan greater for at least 10 days a month for 3 consecutive months, as defined by the International Classification of Headache Disorders. It’s important to note that triptan are prescribed to patients for only two indications – migraines and cluster headaches. However, cluster headaches are extremely rare.
The study’s investigators summarized data collected throughout Denmark for more than a quarter of a century. The findings show an increase in triptan use from 345 defined daily doses to 945 defined daily doses per 1,000 residents per year along with an increased prevalence on triptan use from 5.17 to 14.57 per 1,000 inhabitants. In addition, 12.3% of the Danish residents who had migraines bought a triptan between 2014 and 2019 – data Dr. Rapoport noted falls in lines with trends in other Western countries, which range between 12% and 13%.
Nearly half of the first-time triptan buyers (43%) did not purchase another triptan for 5 years. In conflict with established guidelines, 90% of patients that discontinued triptan-based treatment had tried only one triptan type.
One important factor contributing to the ease of data collection is that the Danish population has free health care, coupled with sizable reimbursements for their spending. The country’s accessible health care system negates the effects of barriers related to price and availability while engendering data that more accurately reflects the patients’ experience based on treatment need and satisfaction.
“In a cohort with access to free clinical consultations and low medication costs, we observed low rates of triptan adherence, likely due to disappointing efficacy and/or unpleasant side effects rather than economic considerations. Triptan success continues to be hindered by poor implementation of clinical guidelines and high rates of treatment discontinuance,” the researchers concluded.
“The most surprising thing about this study is it is exactly what I would have expected if triptans in the U.S. were free,” Dr. Rapoport said.
Dr. Rapoport is the editor in chief of Neurology Reviews and serves as a consultant to several pharmaceutical companies.
FROM CEPHALALGIA
Anti-CD20s linked to higher COVID-19 severity in MS
Like other people, a biostatistician told neurologists. With the exception of anti-CD20s, registries also suggest that disease-modifying therapies (DMTs) don’t cause higher degrees of severity.
“It’s good news since it’s important for patients to stay on these treatments,” said Amber Salter, PhD, MPH, an assistant professor at Washington University, St. Louis, in a follow-up interview following her presentation at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Salter reported on the findings of several MS/COVID-19 registries from around the world, including the COViMS Registry, which is supported by the Consortium of MS Centers, the MS Society of Canada, and the National MS Society. It tracks patients who developed COVID-19 while also having MS, neuromyelitis optica, or MOG antibody disease.
The registry began collecting data in April 2020 and is ongoing. As of Jan. 29, 2021, 2,059 patients had been tracked; 85% of cases were confirmed by laboratory tests. Nearly all patients (97%) were from the United States, with about 21% from New York state. Nearly 76% were female, the average age was 48. About 70% were non-Hispanic White, 18% were African American; 83% had relapsing remitting MS, and 17% had progressive MS.
“We found that 11.5% of MS patients were reported being hospitalized, while 4.2% were admitted to the ICU or ventilated and 3% had died,” Dr. Salter said. Not surprisingly, the death rate was highest (21%) in patients aged 75 years or older, compared with 11% of those aged 65-74 years. Those with more severe cases – those who were nonambulatory – had a death rate of 18%, compared with 0.6% of those who were fully ambulatory and 4% of those who walked with assistance.
“A lot of the risks [for COVID-19 severity] we see in the general population are risks in the MS population,” Dr. Salter said.
Dr. Salter also summarized the results of other international registries. After adjustment, a registry in Italy linked the anti-CD20 drugs ocrelizumab or rituximab (odds ratio, 2.37, P = .015) and recent use of methylprednisolone (OR, 5.2; P = .001) to more severe courses of COVID-19, compared with other DMTs. And a global data-sharing project linked anti-CD20s to more severe outcomes, compared with other DMTs (hospitalization, adjusted prevalence ratio, 1.49; ICU admission, aPR, 2.55; and ventilation, aPR, 3.05).
In an interview, neurologist Lauren Gluck, MD, of Albert Einstein College of Medicine and Montefiore Medical Center, both in New York, cautioned that prescribing anti-CD20s now “requires a more complex informed consent process with patients and outlining of risk as well as strategies to minimize contracting the infection.”
Moving forward, she advised colleagues to “keep treating MS with DMTs. Preventing MS attacks will help keep patients out of the hospital and limit need for high-dose steroids.” And she cautioned that “avoiding action due to inaccurate fear of DMTs and COVID-19 may put your patients at unnecessary risk of relapses and accumulated disability. Educate your patients on the reality of the COVID19 pandemic, their personal risk of exposure, and strategies to minimize their risk.”
Fortunately, vaccinations offer protection against COVID-19 in patients with MS, although patients are clearly concerned about potential risks. “A frequent concern is whether the vaccines are safe for MS patients in general and if they could incite MS relapses,” neurologist Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, said in an interview. “The American Academy of Neurology guidelines have not found a connection between vaccination and MS relapses. Having COVID-19 infection can trigger MS relapses, so clearly the benefit from the vaccine outweighs any potential risks. Obviously, it is not advisable to take any vaccine during an active relapse, but vaccines are safe otherwise when given during remission.”
Dr. Salter and Dr. Gluck reported no relevant disclosures. Dr. Abboud reports consulting fees from Biogen, Genentech, Bristol-Myers Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myers Squibb, Genentech, and Sanofi-Genzyme.
Like other people, a biostatistician told neurologists. With the exception of anti-CD20s, registries also suggest that disease-modifying therapies (DMTs) don’t cause higher degrees of severity.
“It’s good news since it’s important for patients to stay on these treatments,” said Amber Salter, PhD, MPH, an assistant professor at Washington University, St. Louis, in a follow-up interview following her presentation at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Salter reported on the findings of several MS/COVID-19 registries from around the world, including the COViMS Registry, which is supported by the Consortium of MS Centers, the MS Society of Canada, and the National MS Society. It tracks patients who developed COVID-19 while also having MS, neuromyelitis optica, or MOG antibody disease.
The registry began collecting data in April 2020 and is ongoing. As of Jan. 29, 2021, 2,059 patients had been tracked; 85% of cases were confirmed by laboratory tests. Nearly all patients (97%) were from the United States, with about 21% from New York state. Nearly 76% were female, the average age was 48. About 70% were non-Hispanic White, 18% were African American; 83% had relapsing remitting MS, and 17% had progressive MS.
“We found that 11.5% of MS patients were reported being hospitalized, while 4.2% were admitted to the ICU or ventilated and 3% had died,” Dr. Salter said. Not surprisingly, the death rate was highest (21%) in patients aged 75 years or older, compared with 11% of those aged 65-74 years. Those with more severe cases – those who were nonambulatory – had a death rate of 18%, compared with 0.6% of those who were fully ambulatory and 4% of those who walked with assistance.
“A lot of the risks [for COVID-19 severity] we see in the general population are risks in the MS population,” Dr. Salter said.
Dr. Salter also summarized the results of other international registries. After adjustment, a registry in Italy linked the anti-CD20 drugs ocrelizumab or rituximab (odds ratio, 2.37, P = .015) and recent use of methylprednisolone (OR, 5.2; P = .001) to more severe courses of COVID-19, compared with other DMTs. And a global data-sharing project linked anti-CD20s to more severe outcomes, compared with other DMTs (hospitalization, adjusted prevalence ratio, 1.49; ICU admission, aPR, 2.55; and ventilation, aPR, 3.05).
In an interview, neurologist Lauren Gluck, MD, of Albert Einstein College of Medicine and Montefiore Medical Center, both in New York, cautioned that prescribing anti-CD20s now “requires a more complex informed consent process with patients and outlining of risk as well as strategies to minimize contracting the infection.”
Moving forward, she advised colleagues to “keep treating MS with DMTs. Preventing MS attacks will help keep patients out of the hospital and limit need for high-dose steroids.” And she cautioned that “avoiding action due to inaccurate fear of DMTs and COVID-19 may put your patients at unnecessary risk of relapses and accumulated disability. Educate your patients on the reality of the COVID19 pandemic, their personal risk of exposure, and strategies to minimize their risk.”
Fortunately, vaccinations offer protection against COVID-19 in patients with MS, although patients are clearly concerned about potential risks. “A frequent concern is whether the vaccines are safe for MS patients in general and if they could incite MS relapses,” neurologist Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, said in an interview. “The American Academy of Neurology guidelines have not found a connection between vaccination and MS relapses. Having COVID-19 infection can trigger MS relapses, so clearly the benefit from the vaccine outweighs any potential risks. Obviously, it is not advisable to take any vaccine during an active relapse, but vaccines are safe otherwise when given during remission.”
Dr. Salter and Dr. Gluck reported no relevant disclosures. Dr. Abboud reports consulting fees from Biogen, Genentech, Bristol-Myers Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myers Squibb, Genentech, and Sanofi-Genzyme.
Like other people, a biostatistician told neurologists. With the exception of anti-CD20s, registries also suggest that disease-modifying therapies (DMTs) don’t cause higher degrees of severity.
“It’s good news since it’s important for patients to stay on these treatments,” said Amber Salter, PhD, MPH, an assistant professor at Washington University, St. Louis, in a follow-up interview following her presentation at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Dr. Salter reported on the findings of several MS/COVID-19 registries from around the world, including the COViMS Registry, which is supported by the Consortium of MS Centers, the MS Society of Canada, and the National MS Society. It tracks patients who developed COVID-19 while also having MS, neuromyelitis optica, or MOG antibody disease.
The registry began collecting data in April 2020 and is ongoing. As of Jan. 29, 2021, 2,059 patients had been tracked; 85% of cases were confirmed by laboratory tests. Nearly all patients (97%) were from the United States, with about 21% from New York state. Nearly 76% were female, the average age was 48. About 70% were non-Hispanic White, 18% were African American; 83% had relapsing remitting MS, and 17% had progressive MS.
“We found that 11.5% of MS patients were reported being hospitalized, while 4.2% were admitted to the ICU or ventilated and 3% had died,” Dr. Salter said. Not surprisingly, the death rate was highest (21%) in patients aged 75 years or older, compared with 11% of those aged 65-74 years. Those with more severe cases – those who were nonambulatory – had a death rate of 18%, compared with 0.6% of those who were fully ambulatory and 4% of those who walked with assistance.
“A lot of the risks [for COVID-19 severity] we see in the general population are risks in the MS population,” Dr. Salter said.
Dr. Salter also summarized the results of other international registries. After adjustment, a registry in Italy linked the anti-CD20 drugs ocrelizumab or rituximab (odds ratio, 2.37, P = .015) and recent use of methylprednisolone (OR, 5.2; P = .001) to more severe courses of COVID-19, compared with other DMTs. And a global data-sharing project linked anti-CD20s to more severe outcomes, compared with other DMTs (hospitalization, adjusted prevalence ratio, 1.49; ICU admission, aPR, 2.55; and ventilation, aPR, 3.05).
In an interview, neurologist Lauren Gluck, MD, of Albert Einstein College of Medicine and Montefiore Medical Center, both in New York, cautioned that prescribing anti-CD20s now “requires a more complex informed consent process with patients and outlining of risk as well as strategies to minimize contracting the infection.”
Moving forward, she advised colleagues to “keep treating MS with DMTs. Preventing MS attacks will help keep patients out of the hospital and limit need for high-dose steroids.” And she cautioned that “avoiding action due to inaccurate fear of DMTs and COVID-19 may put your patients at unnecessary risk of relapses and accumulated disability. Educate your patients on the reality of the COVID19 pandemic, their personal risk of exposure, and strategies to minimize their risk.”
Fortunately, vaccinations offer protection against COVID-19 in patients with MS, although patients are clearly concerned about potential risks. “A frequent concern is whether the vaccines are safe for MS patients in general and if they could incite MS relapses,” neurologist Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, said in an interview. “The American Academy of Neurology guidelines have not found a connection between vaccination and MS relapses. Having COVID-19 infection can trigger MS relapses, so clearly the benefit from the vaccine outweighs any potential risks. Obviously, it is not advisable to take any vaccine during an active relapse, but vaccines are safe otherwise when given during remission.”
Dr. Salter and Dr. Gluck reported no relevant disclosures. Dr. Abboud reports consulting fees from Biogen, Genentech, Bristol-Myers Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myers Squibb, Genentech, and Sanofi-Genzyme.
FROM ACTRIMS FORUM 2021
Certain DMTs in MS may attenuate COVID-19 vaccines
“There’s no reason to think any of the three authorized vaccines are in any way more dangerous in people with MS, or in the context of MS DMTs. It’s only a question of whether certain DMTs will influence the degree of benefit you get from the vaccine,” said Amit Bar-Or, MD, director of the Center for Neuroinflammation and Neurotherapeutics, chief of the multiple sclerosis division, and Melissa and Paul Anderson President’s Distinguished Professor at the University of Pennsylvania, Philadelphia. He spoke at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, and he also answered questions in a follow-up interview.
“The merits of being protected by the COVID-19 vaccines far outweigh any risks that one would consider associated with vaccines and individuals with MS,” said Dr. Bar-Or. “And there’s reason to think that the RNA vaccines may even be safer than prior, more traditional vaccines. They are nonlive, noninactivated vaccines, and there is no risk in terms of interacting with MS.”
Where do DMTs fit in? In an interview, Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, also in Cleveland, said there’s reason for caution regarding DMTs that deplete immune cells or entrap them in the lymph nodes. “What is not clearly known is the effect of the fumarates, which do not act through cell depletion but can occasionally deplete immune cells as a side effect. These likely have no negative effect on vaccine efficacy in patients with normal immune cell count but may have a negative effect in those with significant immune cell reduction. Luckily, significant immune cell reduction is rare in patients taking fumarates.”
In addition, he said, “interferons and natalizumab are generally thought to have no impact on vaccine efficacy while glatiramer acetate and teriflunomide are thought to have no or only little impact on vaccines. Most of these concepts are derived from studies of non–COVID-19 vaccines.”
Dr. Bar-Or highlighted specific DMTs. Teriflunomide (Aubagio) “has a relatively mild effect on the immune system and is not thought to be particularly immune suppressive or deplete immune cells,” Dr. Bar-Or said, as shown in a 2015 study he led (Neurol Neuroimmunol Neuroinflamm. 2015 Feb 12;2[2]:e70). In contrast, a 2020 study, also led by Dr. Bar-Or, showed that nonlive vaccinations given after treatment with ocrelizumab (Ocrevus) – an anti-CD20 monoclonal antibody – are “attenuated, compared with untreated or interferon-beta–treated patients, but they can still be expected to be protective.”
Dr. Bar-Or pointed to National MS Society guidelines about the timing of the Pfizer and Moderna mRNA vaccines for patients with MS who are on DMT. In patients with stable MS, the society recommends no adjustments in timing for patients starting or remaining on several DMTs. The list includes teriflunomide, glatiramer acetate (Copaxone), and dimethyl fumarate, among others.
Patients shouldn’t start fingolimod (Gilenya), siponimod (Mayzent), or ozanimod (Zeposia) until 4 weeks or more after their second vaccine dose, the guidelines suggest. Vaccine doses are recommended 3-5 days after the final dose of high-dose steroids. And there are more complicated recommendations regarding a number of other DMTs – ocrelizumab, ofatumumab (Kesimpta), alemtuzumab (Lemtrada), cladribine (Mavenclad), and rituximab (Rituxan).
Dr. Bar-Or cautioned that the guidelines are an imperfect “first pass” and are being updated.
He added that the guidelines are not set in stone: “Scheduling is not always possible in terms of adjusting the vaccine timing. Patients in general are recommended to take the vaccine when it becomes available, as it may be more important for them to get the vaccine than to try to time the vaccine relative to the DMT.”
Guidance regarding the newly authorized Johnson & Johnson vaccine is expected soon, said neurologist Barbara Giesser, MD, of Pacific Neuroscience Institute in Santa Monica, Calif., in an interview. As for her advice to patients, she said that, “in general, I am recommending that patients get [vaccinated] as soon as it is available to them with adjustment of timing of some DMTs as may be appropriate.”
Dr. Bar-Or has received consulting fees and/or grant support from – or participated as a speaker in events sponsored by – Accure, Atara Biotherapeutics, Biogen, Bristol-Myer Squibb/Celgene/Receptos, GlaxoSmithKline, Gossamer, Janssen/Actelion, Medimmune, Merck/EMD Serono, Novartis, Roche/Genentech, and Sanofi-Genzyme. He also receives research funding from various organizations and agencies. Dr. Abboud reported receiving consulting fees from Biogen, Genentech, Bristol-Myer Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myer Squibb, Genentech, and Sanofi-Genzyme. Dr. Giesser reports no disclosures.
“There’s no reason to think any of the three authorized vaccines are in any way more dangerous in people with MS, or in the context of MS DMTs. It’s only a question of whether certain DMTs will influence the degree of benefit you get from the vaccine,” said Amit Bar-Or, MD, director of the Center for Neuroinflammation and Neurotherapeutics, chief of the multiple sclerosis division, and Melissa and Paul Anderson President’s Distinguished Professor at the University of Pennsylvania, Philadelphia. He spoke at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, and he also answered questions in a follow-up interview.
“The merits of being protected by the COVID-19 vaccines far outweigh any risks that one would consider associated with vaccines and individuals with MS,” said Dr. Bar-Or. “And there’s reason to think that the RNA vaccines may even be safer than prior, more traditional vaccines. They are nonlive, noninactivated vaccines, and there is no risk in terms of interacting with MS.”
Where do DMTs fit in? In an interview, Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, also in Cleveland, said there’s reason for caution regarding DMTs that deplete immune cells or entrap them in the lymph nodes. “What is not clearly known is the effect of the fumarates, which do not act through cell depletion but can occasionally deplete immune cells as a side effect. These likely have no negative effect on vaccine efficacy in patients with normal immune cell count but may have a negative effect in those with significant immune cell reduction. Luckily, significant immune cell reduction is rare in patients taking fumarates.”
In addition, he said, “interferons and natalizumab are generally thought to have no impact on vaccine efficacy while glatiramer acetate and teriflunomide are thought to have no or only little impact on vaccines. Most of these concepts are derived from studies of non–COVID-19 vaccines.”
Dr. Bar-Or highlighted specific DMTs. Teriflunomide (Aubagio) “has a relatively mild effect on the immune system and is not thought to be particularly immune suppressive or deplete immune cells,” Dr. Bar-Or said, as shown in a 2015 study he led (Neurol Neuroimmunol Neuroinflamm. 2015 Feb 12;2[2]:e70). In contrast, a 2020 study, also led by Dr. Bar-Or, showed that nonlive vaccinations given after treatment with ocrelizumab (Ocrevus) – an anti-CD20 monoclonal antibody – are “attenuated, compared with untreated or interferon-beta–treated patients, but they can still be expected to be protective.”
Dr. Bar-Or pointed to National MS Society guidelines about the timing of the Pfizer and Moderna mRNA vaccines for patients with MS who are on DMT. In patients with stable MS, the society recommends no adjustments in timing for patients starting or remaining on several DMTs. The list includes teriflunomide, glatiramer acetate (Copaxone), and dimethyl fumarate, among others.
Patients shouldn’t start fingolimod (Gilenya), siponimod (Mayzent), or ozanimod (Zeposia) until 4 weeks or more after their second vaccine dose, the guidelines suggest. Vaccine doses are recommended 3-5 days after the final dose of high-dose steroids. And there are more complicated recommendations regarding a number of other DMTs – ocrelizumab, ofatumumab (Kesimpta), alemtuzumab (Lemtrada), cladribine (Mavenclad), and rituximab (Rituxan).
Dr. Bar-Or cautioned that the guidelines are an imperfect “first pass” and are being updated.
He added that the guidelines are not set in stone: “Scheduling is not always possible in terms of adjusting the vaccine timing. Patients in general are recommended to take the vaccine when it becomes available, as it may be more important for them to get the vaccine than to try to time the vaccine relative to the DMT.”
Guidance regarding the newly authorized Johnson & Johnson vaccine is expected soon, said neurologist Barbara Giesser, MD, of Pacific Neuroscience Institute in Santa Monica, Calif., in an interview. As for her advice to patients, she said that, “in general, I am recommending that patients get [vaccinated] as soon as it is available to them with adjustment of timing of some DMTs as may be appropriate.”
Dr. Bar-Or has received consulting fees and/or grant support from – or participated as a speaker in events sponsored by – Accure, Atara Biotherapeutics, Biogen, Bristol-Myer Squibb/Celgene/Receptos, GlaxoSmithKline, Gossamer, Janssen/Actelion, Medimmune, Merck/EMD Serono, Novartis, Roche/Genentech, and Sanofi-Genzyme. He also receives research funding from various organizations and agencies. Dr. Abboud reported receiving consulting fees from Biogen, Genentech, Bristol-Myer Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myer Squibb, Genentech, and Sanofi-Genzyme. Dr. Giesser reports no disclosures.
“There’s no reason to think any of the three authorized vaccines are in any way more dangerous in people with MS, or in the context of MS DMTs. It’s only a question of whether certain DMTs will influence the degree of benefit you get from the vaccine,” said Amit Bar-Or, MD, director of the Center for Neuroinflammation and Neurotherapeutics, chief of the multiple sclerosis division, and Melissa and Paul Anderson President’s Distinguished Professor at the University of Pennsylvania, Philadelphia. He spoke at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, and he also answered questions in a follow-up interview.
“The merits of being protected by the COVID-19 vaccines far outweigh any risks that one would consider associated with vaccines and individuals with MS,” said Dr. Bar-Or. “And there’s reason to think that the RNA vaccines may even be safer than prior, more traditional vaccines. They are nonlive, noninactivated vaccines, and there is no risk in terms of interacting with MS.”
Where do DMTs fit in? In an interview, Hesham Abboud, MD, PhD, of University Hospitals of Cleveland and Case Western Reserve University, also in Cleveland, said there’s reason for caution regarding DMTs that deplete immune cells or entrap them in the lymph nodes. “What is not clearly known is the effect of the fumarates, which do not act through cell depletion but can occasionally deplete immune cells as a side effect. These likely have no negative effect on vaccine efficacy in patients with normal immune cell count but may have a negative effect in those with significant immune cell reduction. Luckily, significant immune cell reduction is rare in patients taking fumarates.”
In addition, he said, “interferons and natalizumab are generally thought to have no impact on vaccine efficacy while glatiramer acetate and teriflunomide are thought to have no or only little impact on vaccines. Most of these concepts are derived from studies of non–COVID-19 vaccines.”
Dr. Bar-Or highlighted specific DMTs. Teriflunomide (Aubagio) “has a relatively mild effect on the immune system and is not thought to be particularly immune suppressive or deplete immune cells,” Dr. Bar-Or said, as shown in a 2015 study he led (Neurol Neuroimmunol Neuroinflamm. 2015 Feb 12;2[2]:e70). In contrast, a 2020 study, also led by Dr. Bar-Or, showed that nonlive vaccinations given after treatment with ocrelizumab (Ocrevus) – an anti-CD20 monoclonal antibody – are “attenuated, compared with untreated or interferon-beta–treated patients, but they can still be expected to be protective.”
Dr. Bar-Or pointed to National MS Society guidelines about the timing of the Pfizer and Moderna mRNA vaccines for patients with MS who are on DMT. In patients with stable MS, the society recommends no adjustments in timing for patients starting or remaining on several DMTs. The list includes teriflunomide, glatiramer acetate (Copaxone), and dimethyl fumarate, among others.
Patients shouldn’t start fingolimod (Gilenya), siponimod (Mayzent), or ozanimod (Zeposia) until 4 weeks or more after their second vaccine dose, the guidelines suggest. Vaccine doses are recommended 3-5 days after the final dose of high-dose steroids. And there are more complicated recommendations regarding a number of other DMTs – ocrelizumab, ofatumumab (Kesimpta), alemtuzumab (Lemtrada), cladribine (Mavenclad), and rituximab (Rituxan).
Dr. Bar-Or cautioned that the guidelines are an imperfect “first pass” and are being updated.
He added that the guidelines are not set in stone: “Scheduling is not always possible in terms of adjusting the vaccine timing. Patients in general are recommended to take the vaccine when it becomes available, as it may be more important for them to get the vaccine than to try to time the vaccine relative to the DMT.”
Guidance regarding the newly authorized Johnson & Johnson vaccine is expected soon, said neurologist Barbara Giesser, MD, of Pacific Neuroscience Institute in Santa Monica, Calif., in an interview. As for her advice to patients, she said that, “in general, I am recommending that patients get [vaccinated] as soon as it is available to them with adjustment of timing of some DMTs as may be appropriate.”
Dr. Bar-Or has received consulting fees and/or grant support from – or participated as a speaker in events sponsored by – Accure, Atara Biotherapeutics, Biogen, Bristol-Myer Squibb/Celgene/Receptos, GlaxoSmithKline, Gossamer, Janssen/Actelion, Medimmune, Merck/EMD Serono, Novartis, Roche/Genentech, and Sanofi-Genzyme. He also receives research funding from various organizations and agencies. Dr. Abboud reported receiving consulting fees from Biogen, Genentech, Bristol-Myer Squibb, Alexion, and Viela Bio. He receives research support from Novartis, Bristol-Myer Squibb, Genentech, and Sanofi-Genzyme. Dr. Giesser reports no disclosures.
FROM ACTRIMS FORUM 2021
Routine vaccinations missed by older adults during pandemic
Physicians are going to have to play catch-up when it comes to getting older patients their routine, but important, vaccinations missed during the pandemic.
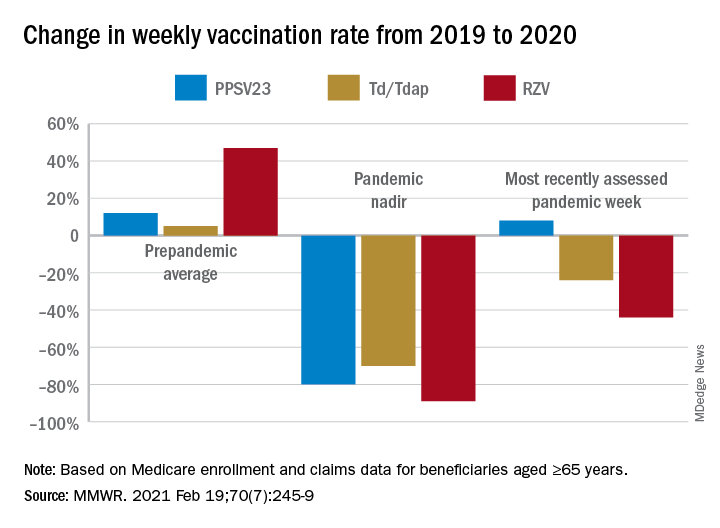
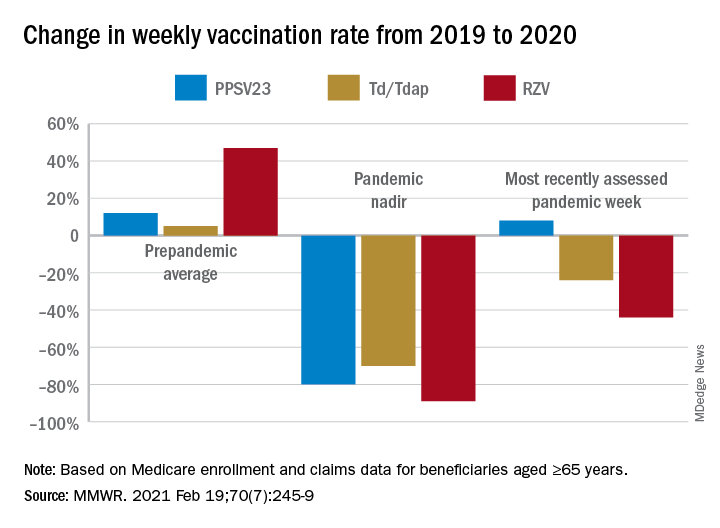
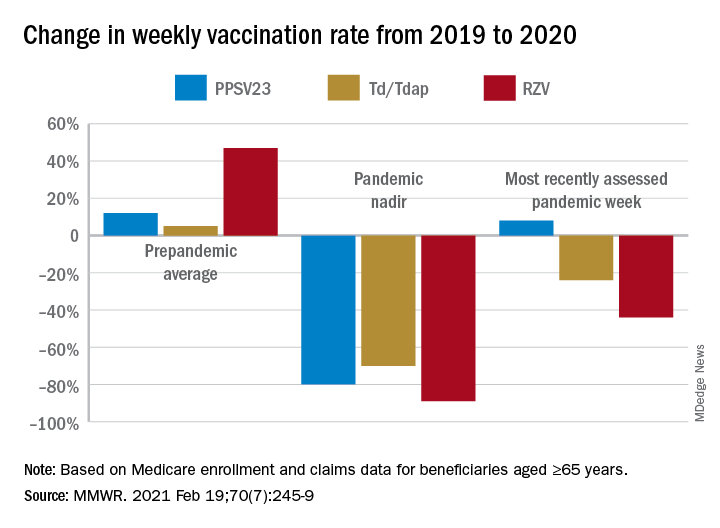
and have recovered only partially and gradually, according to a report by Kai Hong, PhD, and colleagues at the Centers for Disease Control and Prevention, published in the Morbidity and Mortality Weekly Report. “As the pandemic continues,” the investigators stated, “vaccination providers should continue efforts to resolve disruptions in routine adult vaccination.”
The CDC issued guidance recommending postponement of routine adult vaccination in response to the March 13, 2020, COVID-19 national emergency declaration by the U.S. government and also to state and local shelter-in-place orders. Health care facility operations were restricted because of safety concerns around exposure to the SARS-CoV-2 virus. The result was a significant drop in routine medical care including adult vaccinations.
The investigators examined Medicare enrollment and claims data to assess the change in weekly receipt of four routine adult vaccines by Medicare beneficiaries aged ≥65 during the pandemic: (13-valent pneumococcal conjugate vaccine [PCV13], 23-valent pneumococcal polysaccharide vaccine [PPSV23], tetanus-diphtheria or tetanus-diphtheria-acellular pertussis vaccine [Td/Tdap], and recombinant zoster vaccine [RZV]). The comparison periods were Jan. 6–July 20, 2019, and Jan. 5–July 18, 2020.
Of the Medicare enrollees in the study sample, 85% were White, 7% Black, 2% Asian, 2% Hispanic, and 4% other racial and ethnic groups. For each of the four vaccines overall, weekly rates of vaccination declined sharply after the emergency declaration, compared with corresponding weeks in 2019. In the period prior to the emergency declaration (Jan. 5–March 14, 2020), weekly percentages of Medicare beneficiaries vaccinated with PPSV23, Td/Tdap, and RZV were consistently higher than rates during the same period in 2019.
After the March 13 declaration, while weekly vaccination rates plummeted 25% for PPSV23 and 62% for RZV in the first week, the greatest weekly declines were during April 5-11, 2020, for PCV13, PPSV23, and Td/Tdap, and during April 12-18, 2020, for RZV. The pandemic weekly vaccination rate nadirs revealed declines of 88% for PCV13, 80% for PPSV23, 70% for Td/Tdap, and 89% for RZV.
Routine vaccinations increased midyear
Vaccination rates recovered gradually. For the most recently assessed pandemic week (July 12-18, 2020), the rate for PPSV23 was 8% higher than in the corresponding period in 2019. Weekly corresponding rates for other examined vaccines, however, remained much lower than in 2019: 44% lower for RZV, 24% lower for Td/Tdap and 43% lower for PCV13. The CDC Advisory Committee on Immunization Practices voted in June 2019 to stop recommending PCV13 for adults aged ≥65 years and so vaccination with PCV13 among this population declined in 2020, compared with that in 2019.
Another significant drop in the rates of adult vaccinations may have occurred because of the surge in COVID-19 infections in the fall of 2020 and subsequent closures and renewal of lockdown in many localities.
Disparities in routine vaccination trends
Dr. Hong and colleagues noted that their findings are consistent with prior reports of declines in pediatric vaccine ordering, administration, and coverage during the pandemic. While the reductions were similar across all racial and ethnic groups, the magnitudes of recovery varied, with vaccination rates lower among racial and ethnic minority adults than among White adults.
In view of the disproportionate COVID-19 pandemic effects among some racial and ethnic minorities, the investigators recommended monitoring and subsequent early intervention to mitigate similar indirect pandemic effects, such as reduced utilization of other preventive services. “Many members of racial and ethnic minority groups face barriers to routine medical care, which means they have fewer opportunities to receive preventive interventions such as vaccination,” Dr. Hong said in an interview. “When clinicians are following up with patients who have missed vaccinations, it is important for them to remember that patients may face new barriers to vaccination such as loss of income or health insurance, and to work with them to remove those barriers,” he added.
“If vaccination is deferred, older adults and adults with underlying medical conditions who subsequently become infected with a vaccine-preventable disease are at increased risk for complications,” Dr. Hong said. “The most important thing clinicians can do is identify patients who are due for or who have missed vaccinations, and contact them to schedule visits. Immunization Information Systems and electronic health records may be able to support this work. In addition, the vaccination status of all patients should be assessed at every health care visit to reduce missed opportunities for vaccination.”
Physicians are going to have to play catch-up when it comes to getting older patients their routine, but important, vaccinations missed during the pandemic.
and have recovered only partially and gradually, according to a report by Kai Hong, PhD, and colleagues at the Centers for Disease Control and Prevention, published in the Morbidity and Mortality Weekly Report. “As the pandemic continues,” the investigators stated, “vaccination providers should continue efforts to resolve disruptions in routine adult vaccination.”
The CDC issued guidance recommending postponement of routine adult vaccination in response to the March 13, 2020, COVID-19 national emergency declaration by the U.S. government and also to state and local shelter-in-place orders. Health care facility operations were restricted because of safety concerns around exposure to the SARS-CoV-2 virus. The result was a significant drop in routine medical care including adult vaccinations.
The investigators examined Medicare enrollment and claims data to assess the change in weekly receipt of four routine adult vaccines by Medicare beneficiaries aged ≥65 during the pandemic: (13-valent pneumococcal conjugate vaccine [PCV13], 23-valent pneumococcal polysaccharide vaccine [PPSV23], tetanus-diphtheria or tetanus-diphtheria-acellular pertussis vaccine [Td/Tdap], and recombinant zoster vaccine [RZV]). The comparison periods were Jan. 6–July 20, 2019, and Jan. 5–July 18, 2020.
Of the Medicare enrollees in the study sample, 85% were White, 7% Black, 2% Asian, 2% Hispanic, and 4% other racial and ethnic groups. For each of the four vaccines overall, weekly rates of vaccination declined sharply after the emergency declaration, compared with corresponding weeks in 2019. In the period prior to the emergency declaration (Jan. 5–March 14, 2020), weekly percentages of Medicare beneficiaries vaccinated with PPSV23, Td/Tdap, and RZV were consistently higher than rates during the same period in 2019.
After the March 13 declaration, while weekly vaccination rates plummeted 25% for PPSV23 and 62% for RZV in the first week, the greatest weekly declines were during April 5-11, 2020, for PCV13, PPSV23, and Td/Tdap, and during April 12-18, 2020, for RZV. The pandemic weekly vaccination rate nadirs revealed declines of 88% for PCV13, 80% for PPSV23, 70% for Td/Tdap, and 89% for RZV.
Routine vaccinations increased midyear
Vaccination rates recovered gradually. For the most recently assessed pandemic week (July 12-18, 2020), the rate for PPSV23 was 8% higher than in the corresponding period in 2019. Weekly corresponding rates for other examined vaccines, however, remained much lower than in 2019: 44% lower for RZV, 24% lower for Td/Tdap and 43% lower for PCV13. The CDC Advisory Committee on Immunization Practices voted in June 2019 to stop recommending PCV13 for adults aged ≥65 years and so vaccination with PCV13 among this population declined in 2020, compared with that in 2019.
Another significant drop in the rates of adult vaccinations may have occurred because of the surge in COVID-19 infections in the fall of 2020 and subsequent closures and renewal of lockdown in many localities.
Disparities in routine vaccination trends
Dr. Hong and colleagues noted that their findings are consistent with prior reports of declines in pediatric vaccine ordering, administration, and coverage during the pandemic. While the reductions were similar across all racial and ethnic groups, the magnitudes of recovery varied, with vaccination rates lower among racial and ethnic minority adults than among White adults.
In view of the disproportionate COVID-19 pandemic effects among some racial and ethnic minorities, the investigators recommended monitoring and subsequent early intervention to mitigate similar indirect pandemic effects, such as reduced utilization of other preventive services. “Many members of racial and ethnic minority groups face barriers to routine medical care, which means they have fewer opportunities to receive preventive interventions such as vaccination,” Dr. Hong said in an interview. “When clinicians are following up with patients who have missed vaccinations, it is important for them to remember that patients may face new barriers to vaccination such as loss of income or health insurance, and to work with them to remove those barriers,” he added.
“If vaccination is deferred, older adults and adults with underlying medical conditions who subsequently become infected with a vaccine-preventable disease are at increased risk for complications,” Dr. Hong said. “The most important thing clinicians can do is identify patients who are due for or who have missed vaccinations, and contact them to schedule visits. Immunization Information Systems and electronic health records may be able to support this work. In addition, the vaccination status of all patients should be assessed at every health care visit to reduce missed opportunities for vaccination.”
Physicians are going to have to play catch-up when it comes to getting older patients their routine, but important, vaccinations missed during the pandemic.
and have recovered only partially and gradually, according to a report by Kai Hong, PhD, and colleagues at the Centers for Disease Control and Prevention, published in the Morbidity and Mortality Weekly Report. “As the pandemic continues,” the investigators stated, “vaccination providers should continue efforts to resolve disruptions in routine adult vaccination.”
The CDC issued guidance recommending postponement of routine adult vaccination in response to the March 13, 2020, COVID-19 national emergency declaration by the U.S. government and also to state and local shelter-in-place orders. Health care facility operations were restricted because of safety concerns around exposure to the SARS-CoV-2 virus. The result was a significant drop in routine medical care including adult vaccinations.
The investigators examined Medicare enrollment and claims data to assess the change in weekly receipt of four routine adult vaccines by Medicare beneficiaries aged ≥65 during the pandemic: (13-valent pneumococcal conjugate vaccine [PCV13], 23-valent pneumococcal polysaccharide vaccine [PPSV23], tetanus-diphtheria or tetanus-diphtheria-acellular pertussis vaccine [Td/Tdap], and recombinant zoster vaccine [RZV]). The comparison periods were Jan. 6–July 20, 2019, and Jan. 5–July 18, 2020.
Of the Medicare enrollees in the study sample, 85% were White, 7% Black, 2% Asian, 2% Hispanic, and 4% other racial and ethnic groups. For each of the four vaccines overall, weekly rates of vaccination declined sharply after the emergency declaration, compared with corresponding weeks in 2019. In the period prior to the emergency declaration (Jan. 5–March 14, 2020), weekly percentages of Medicare beneficiaries vaccinated with PPSV23, Td/Tdap, and RZV were consistently higher than rates during the same period in 2019.
After the March 13 declaration, while weekly vaccination rates plummeted 25% for PPSV23 and 62% for RZV in the first week, the greatest weekly declines were during April 5-11, 2020, for PCV13, PPSV23, and Td/Tdap, and during April 12-18, 2020, for RZV. The pandemic weekly vaccination rate nadirs revealed declines of 88% for PCV13, 80% for PPSV23, 70% for Td/Tdap, and 89% for RZV.
Routine vaccinations increased midyear
Vaccination rates recovered gradually. For the most recently assessed pandemic week (July 12-18, 2020), the rate for PPSV23 was 8% higher than in the corresponding period in 2019. Weekly corresponding rates for other examined vaccines, however, remained much lower than in 2019: 44% lower for RZV, 24% lower for Td/Tdap and 43% lower for PCV13. The CDC Advisory Committee on Immunization Practices voted in June 2019 to stop recommending PCV13 for adults aged ≥65 years and so vaccination with PCV13 among this population declined in 2020, compared with that in 2019.
Another significant drop in the rates of adult vaccinations may have occurred because of the surge in COVID-19 infections in the fall of 2020 and subsequent closures and renewal of lockdown in many localities.
Disparities in routine vaccination trends
Dr. Hong and colleagues noted that their findings are consistent with prior reports of declines in pediatric vaccine ordering, administration, and coverage during the pandemic. While the reductions were similar across all racial and ethnic groups, the magnitudes of recovery varied, with vaccination rates lower among racial and ethnic minority adults than among White adults.
In view of the disproportionate COVID-19 pandemic effects among some racial and ethnic minorities, the investigators recommended monitoring and subsequent early intervention to mitigate similar indirect pandemic effects, such as reduced utilization of other preventive services. “Many members of racial and ethnic minority groups face barriers to routine medical care, which means they have fewer opportunities to receive preventive interventions such as vaccination,” Dr. Hong said in an interview. “When clinicians are following up with patients who have missed vaccinations, it is important for them to remember that patients may face new barriers to vaccination such as loss of income or health insurance, and to work with them to remove those barriers,” he added.
“If vaccination is deferred, older adults and adults with underlying medical conditions who subsequently become infected with a vaccine-preventable disease are at increased risk for complications,” Dr. Hong said. “The most important thing clinicians can do is identify patients who are due for or who have missed vaccinations, and contact them to schedule visits. Immunization Information Systems and electronic health records may be able to support this work. In addition, the vaccination status of all patients should be assessed at every health care visit to reduce missed opportunities for vaccination.”
FROM MMWR
BMI, age, and sex affect COVID-19 vaccine antibody response
The capacity to mount humoral immune responses to COVID-19 vaccinations may be reduced among people who are heavier, older, and male, new findings suggest.
The data pertain specifically to the mRNA vaccine, BNT162b2, developed by BioNTech and Pfizer. The study was conducted by Italian researchers and was published Feb. 26 as a preprint.
The study involved 248 health care workers who each received two doses of the vaccine. Of the participants, 99.5% developed a humoral immune response after the second dose. Those responses varied by body mass index (BMI), age, and sex.
“The findings imply that female, lean, and young people have an increased capacity to mount humoral immune responses, compared to male, overweight, and older populations,” Raul Pellini, MD, professor at the IRCCS Regina Elena National Cancer Institute, Rome, and colleagues said.
“To our knowledge, this study is the first to analyze Covid-19 vaccine response in correlation to BMI,” they noted.
“Although further studies are needed, this data may have important implications to the development of vaccination strategies for COVID-19, particularly in obese people,” they wrote. If the data are confirmed by larger studies, “giving obese people an extra dose of the vaccine or a higher dose could be options to be evaluated in this population.”
Results contrast with Pfizer trials of vaccine
The BMI finding seemingly contrasts with final data from the phase 3 clinical trial of the vaccine, which were reported in a supplement to an article published Dec. 31, 2020, in the New England Journal of Medicine. In that study, vaccine efficacy did not differ by obesity status.
Akiko Iwasaki, PhD, professor of immunology at the Howard Hughes Medical Institute and an investigator at Yale University, New Haven, Conn., noted that, although the current Italian study showed somewhat lower levels of antibodies in people with obesity, compared with people who did not have obesity, the phase 3 trial found no difference in symptomatic infection rates.
“These results indicate that even with a slightly lower level of antibody induced in obese people, that level was sufficient to protect against symptomatic infection,” Dr. Iwasaki said in an interview.
Indeed, Dr. Pellini and colleagues pointed out that responses to vaccines against influenza, hepatitis B, and rabies are also reduced in those with obesity, compared with lean individuals.
However, they said, it was especially important to study the effectiveness of COVID-19 vaccines in people with obesity, because obesity is a major risk factor for morbidity and mortality in COVID-19.
“The constant state of low-grade inflammation, present in overweight people, can weaken some immune responses, including those launched by T cells, which can directly kill infected cells,” the authors noted.
Findings reported in British newspapers
The findings of the Italian study were widely covered in the lay press in the United Kingdom, with headlines such as “Pfizer Vaccine May Be Less Effective in People With Obesity, Says Study” and “Pfizer Vaccine: Overweight People Might Need Bigger Dose, Italian Study Says.” In tabloid newspapers, some headlines were slightly more stigmatizing.
The reports do stress that the Italian research was published as a preprint and has not been peer reviewed, or “is yet to be scrutinized by fellow scientists.”
Most make the point that there were only 26 people with obesity among the 248 persons in the study.
“We always knew that BMI was an enormous predictor of poor immune response to vaccines, so this paper is definitely interesting, although it is based on a rather small preliminary dataset,” Danny Altmann, PhD, a professor of immunology at Imperial College London, told the Guardian.
“It confirms that having a vaccinated population isn’t synonymous with having an immune population, especially in a country with high obesity, and emphasizes the vital need for long-term immune monitoring programs,” he added.
Antibody responses differ by BMI, age, and sex
In the Italian study, the participants – 158 women and 90 men – were assigned to receive a priming BNT162b2 vaccine dose with a booster at day 21. Blood and nasopharyngeal swabs were collected at baseline and 7 days after the second vaccine dose.
After the second dose, 99.5% of participants developed a humoral immune response; one person did not respond. None tested positive for SARS-CoV-2.
Titers of SARS-CoV-2–binding antibodies were greater in younger than in older participants. There were statistically significant differences between those aged 37 years and younger (453.5 AU/mL) and those aged 47-56 years (239.8 AU/mL; P = .005), those aged 37 years and younger versus those older than 56 years (453.5 vs 182.4 AU/mL; P < .0001), and those aged 37-47 years versus those older than 56 years (330.9 vs. 182.4 AU/mL; P = .01).
Antibody response was significantly greater for women than for men (338.5 vs. 212.6 AU/mL; P = .001).
Humoral responses were greater in persons of normal-weight BMI (18.5-24.9 kg/m2; 325.8 AU/mL) and those of underweight BMI (<18.5 kg/m2; 455.4 AU/mL), compared with persons with preobesity, defined as BMI of 25-29.9 (222.4 AU/mL), and those with obesity (BMI ≥30; 167.0 AU/mL; P < .0001). This association remained after adjustment for age (P = .003).
“Our data stresses the importance of close vaccination monitoring of obese people, considering the growing list of countries with obesity problems,” the researchers noted.
Hypertension was also associated with lower antibody titers (P = .006), but that lost statistical significance after matching for age (P = .22).
“We strongly believe that our results are extremely encouraging and useful for the scientific community,” Dr. Pellini and colleagues concluded.
The authors disclosed no relevant financial relationships. Dr. Iwasaki is a cofounder of RIGImmune and is a member of its scientific advisory board.
This article was updated on 3/8/21.
A version of this article first appeared on Medscape.com.
The capacity to mount humoral immune responses to COVID-19 vaccinations may be reduced among people who are heavier, older, and male, new findings suggest.
The data pertain specifically to the mRNA vaccine, BNT162b2, developed by BioNTech and Pfizer. The study was conducted by Italian researchers and was published Feb. 26 as a preprint.
The study involved 248 health care workers who each received two doses of the vaccine. Of the participants, 99.5% developed a humoral immune response after the second dose. Those responses varied by body mass index (BMI), age, and sex.
“The findings imply that female, lean, and young people have an increased capacity to mount humoral immune responses, compared to male, overweight, and older populations,” Raul Pellini, MD, professor at the IRCCS Regina Elena National Cancer Institute, Rome, and colleagues said.
“To our knowledge, this study is the first to analyze Covid-19 vaccine response in correlation to BMI,” they noted.
“Although further studies are needed, this data may have important implications to the development of vaccination strategies for COVID-19, particularly in obese people,” they wrote. If the data are confirmed by larger studies, “giving obese people an extra dose of the vaccine or a higher dose could be options to be evaluated in this population.”
Results contrast with Pfizer trials of vaccine
The BMI finding seemingly contrasts with final data from the phase 3 clinical trial of the vaccine, which were reported in a supplement to an article published Dec. 31, 2020, in the New England Journal of Medicine. In that study, vaccine efficacy did not differ by obesity status.
Akiko Iwasaki, PhD, professor of immunology at the Howard Hughes Medical Institute and an investigator at Yale University, New Haven, Conn., noted that, although the current Italian study showed somewhat lower levels of antibodies in people with obesity, compared with people who did not have obesity, the phase 3 trial found no difference in symptomatic infection rates.
“These results indicate that even with a slightly lower level of antibody induced in obese people, that level was sufficient to protect against symptomatic infection,” Dr. Iwasaki said in an interview.
Indeed, Dr. Pellini and colleagues pointed out that responses to vaccines against influenza, hepatitis B, and rabies are also reduced in those with obesity, compared with lean individuals.
However, they said, it was especially important to study the effectiveness of COVID-19 vaccines in people with obesity, because obesity is a major risk factor for morbidity and mortality in COVID-19.
“The constant state of low-grade inflammation, present in overweight people, can weaken some immune responses, including those launched by T cells, which can directly kill infected cells,” the authors noted.
Findings reported in British newspapers
The findings of the Italian study were widely covered in the lay press in the United Kingdom, with headlines such as “Pfizer Vaccine May Be Less Effective in People With Obesity, Says Study” and “Pfizer Vaccine: Overweight People Might Need Bigger Dose, Italian Study Says.” In tabloid newspapers, some headlines were slightly more stigmatizing.
The reports do stress that the Italian research was published as a preprint and has not been peer reviewed, or “is yet to be scrutinized by fellow scientists.”
Most make the point that there were only 26 people with obesity among the 248 persons in the study.
“We always knew that BMI was an enormous predictor of poor immune response to vaccines, so this paper is definitely interesting, although it is based on a rather small preliminary dataset,” Danny Altmann, PhD, a professor of immunology at Imperial College London, told the Guardian.
“It confirms that having a vaccinated population isn’t synonymous with having an immune population, especially in a country with high obesity, and emphasizes the vital need for long-term immune monitoring programs,” he added.
Antibody responses differ by BMI, age, and sex
In the Italian study, the participants – 158 women and 90 men – were assigned to receive a priming BNT162b2 vaccine dose with a booster at day 21. Blood and nasopharyngeal swabs were collected at baseline and 7 days after the second vaccine dose.
After the second dose, 99.5% of participants developed a humoral immune response; one person did not respond. None tested positive for SARS-CoV-2.
Titers of SARS-CoV-2–binding antibodies were greater in younger than in older participants. There were statistically significant differences between those aged 37 years and younger (453.5 AU/mL) and those aged 47-56 years (239.8 AU/mL; P = .005), those aged 37 years and younger versus those older than 56 years (453.5 vs 182.4 AU/mL; P < .0001), and those aged 37-47 years versus those older than 56 years (330.9 vs. 182.4 AU/mL; P = .01).
Antibody response was significantly greater for women than for men (338.5 vs. 212.6 AU/mL; P = .001).
Humoral responses were greater in persons of normal-weight BMI (18.5-24.9 kg/m2; 325.8 AU/mL) and those of underweight BMI (<18.5 kg/m2; 455.4 AU/mL), compared with persons with preobesity, defined as BMI of 25-29.9 (222.4 AU/mL), and those with obesity (BMI ≥30; 167.0 AU/mL; P < .0001). This association remained after adjustment for age (P = .003).
“Our data stresses the importance of close vaccination monitoring of obese people, considering the growing list of countries with obesity problems,” the researchers noted.
Hypertension was also associated with lower antibody titers (P = .006), but that lost statistical significance after matching for age (P = .22).
“We strongly believe that our results are extremely encouraging and useful for the scientific community,” Dr. Pellini and colleagues concluded.
The authors disclosed no relevant financial relationships. Dr. Iwasaki is a cofounder of RIGImmune and is a member of its scientific advisory board.
This article was updated on 3/8/21.
A version of this article first appeared on Medscape.com.
The capacity to mount humoral immune responses to COVID-19 vaccinations may be reduced among people who are heavier, older, and male, new findings suggest.
The data pertain specifically to the mRNA vaccine, BNT162b2, developed by BioNTech and Pfizer. The study was conducted by Italian researchers and was published Feb. 26 as a preprint.
The study involved 248 health care workers who each received two doses of the vaccine. Of the participants, 99.5% developed a humoral immune response after the second dose. Those responses varied by body mass index (BMI), age, and sex.
“The findings imply that female, lean, and young people have an increased capacity to mount humoral immune responses, compared to male, overweight, and older populations,” Raul Pellini, MD, professor at the IRCCS Regina Elena National Cancer Institute, Rome, and colleagues said.
“To our knowledge, this study is the first to analyze Covid-19 vaccine response in correlation to BMI,” they noted.
“Although further studies are needed, this data may have important implications to the development of vaccination strategies for COVID-19, particularly in obese people,” they wrote. If the data are confirmed by larger studies, “giving obese people an extra dose of the vaccine or a higher dose could be options to be evaluated in this population.”
Results contrast with Pfizer trials of vaccine
The BMI finding seemingly contrasts with final data from the phase 3 clinical trial of the vaccine, which were reported in a supplement to an article published Dec. 31, 2020, in the New England Journal of Medicine. In that study, vaccine efficacy did not differ by obesity status.
Akiko Iwasaki, PhD, professor of immunology at the Howard Hughes Medical Institute and an investigator at Yale University, New Haven, Conn., noted that, although the current Italian study showed somewhat lower levels of antibodies in people with obesity, compared with people who did not have obesity, the phase 3 trial found no difference in symptomatic infection rates.
“These results indicate that even with a slightly lower level of antibody induced in obese people, that level was sufficient to protect against symptomatic infection,” Dr. Iwasaki said in an interview.
Indeed, Dr. Pellini and colleagues pointed out that responses to vaccines against influenza, hepatitis B, and rabies are also reduced in those with obesity, compared with lean individuals.
However, they said, it was especially important to study the effectiveness of COVID-19 vaccines in people with obesity, because obesity is a major risk factor for morbidity and mortality in COVID-19.
“The constant state of low-grade inflammation, present in overweight people, can weaken some immune responses, including those launched by T cells, which can directly kill infected cells,” the authors noted.
Findings reported in British newspapers
The findings of the Italian study were widely covered in the lay press in the United Kingdom, with headlines such as “Pfizer Vaccine May Be Less Effective in People With Obesity, Says Study” and “Pfizer Vaccine: Overweight People Might Need Bigger Dose, Italian Study Says.” In tabloid newspapers, some headlines were slightly more stigmatizing.
The reports do stress that the Italian research was published as a preprint and has not been peer reviewed, or “is yet to be scrutinized by fellow scientists.”
Most make the point that there were only 26 people with obesity among the 248 persons in the study.
“We always knew that BMI was an enormous predictor of poor immune response to vaccines, so this paper is definitely interesting, although it is based on a rather small preliminary dataset,” Danny Altmann, PhD, a professor of immunology at Imperial College London, told the Guardian.
“It confirms that having a vaccinated population isn’t synonymous with having an immune population, especially in a country with high obesity, and emphasizes the vital need for long-term immune monitoring programs,” he added.
Antibody responses differ by BMI, age, and sex
In the Italian study, the participants – 158 women and 90 men – were assigned to receive a priming BNT162b2 vaccine dose with a booster at day 21. Blood and nasopharyngeal swabs were collected at baseline and 7 days after the second vaccine dose.
After the second dose, 99.5% of participants developed a humoral immune response; one person did not respond. None tested positive for SARS-CoV-2.
Titers of SARS-CoV-2–binding antibodies were greater in younger than in older participants. There were statistically significant differences between those aged 37 years and younger (453.5 AU/mL) and those aged 47-56 years (239.8 AU/mL; P = .005), those aged 37 years and younger versus those older than 56 years (453.5 vs 182.4 AU/mL; P < .0001), and those aged 37-47 years versus those older than 56 years (330.9 vs. 182.4 AU/mL; P = .01).
Antibody response was significantly greater for women than for men (338.5 vs. 212.6 AU/mL; P = .001).
Humoral responses were greater in persons of normal-weight BMI (18.5-24.9 kg/m2; 325.8 AU/mL) and those of underweight BMI (<18.5 kg/m2; 455.4 AU/mL), compared with persons with preobesity, defined as BMI of 25-29.9 (222.4 AU/mL), and those with obesity (BMI ≥30; 167.0 AU/mL; P < .0001). This association remained after adjustment for age (P = .003).
“Our data stresses the importance of close vaccination monitoring of obese people, considering the growing list of countries with obesity problems,” the researchers noted.
Hypertension was also associated with lower antibody titers (P = .006), but that lost statistical significance after matching for age (P = .22).
“We strongly believe that our results are extremely encouraging and useful for the scientific community,” Dr. Pellini and colleagues concluded.
The authors disclosed no relevant financial relationships. Dr. Iwasaki is a cofounder of RIGImmune and is a member of its scientific advisory board.
This article was updated on 3/8/21.
A version of this article first appeared on Medscape.com.
Sleep apnea and cognitive impairment are common bedfellows
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
“The study shows obstructive sleep apnea is common in patients with cognitive impairment. The results suggest that people with cognitive impairment should be assessed for sleep apnea if they have difficulty with sleep or if they demonstrate sleep-related symptoms,” said study investigator David Colelli, MSc, research coordinator at Sunnybrook Health Sciences Centre in Toronto.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology..
Linked to cognitive impairment
OSA is a common sleep disorder and is associated with an increased risk of developing cognitive impairment. It is also prevalent in the general population, but even more common among patients with dementia.
However, the investigators noted, the frequency and predictors of OSA have not been well established in Alzheimer’s disease and other related conditions such as vascular dementia.
The investigators had conducted a previous feasibility study investigating a home sleep monitor as an OSA screening tool. The current research examined potential correlations between OSA detected by this monitor and cognitive impairment.
The study included 67 patients with cognitive impairment due to neurodegenerative or vascular disease. The range of disorders included Alzheimer’s disease, mild cognitive impairment caused by Alzheimer’s disease, dementia caused by Parkinson’s or Lewy body disease, and vascular conditions.
Participants had a mean age of 72.8 years and 44.8% were male. The mean body mass index (BMI) was 25.6 kg/m2.
These participants completed a home sleep apnea test, which is an alternative to polysomnography for the detection of OSA.
Researchers identified OSA in 52.2% of the study population. This, Mr. Colelli said, “is in the range” of other research investigating sleep and cognitive impairment.
“In the general population, however, this number is a lot lower – in the 10%-20% range depending on the population or country you’re looking at,” Mr. Colelli said.
He emphasized that, without an objective sleep test, some patients may be unaware of their sleep issues. Those with cognitive impairment may “misjudge how they’re sleeping,” especially if they sleep without a partner, so it’s possible that sleep disorder symptoms often go undetected.
Bidirectional relationship?
Participants answered questionnaires on sleep, cognition, and mood. They also completed the 30-point Montreal Cognitive Assessment (MoCA) to assess language, visuospatial abilities, memory and recall, and abstract thinking.
Scores on this test range from 0 to 30, with a score of 26 or higher signifying normal, 18-25 indicating mild cognitive impairment, and 17 or lower indicating moderate to severe cognitive impairment. The average score for study participants with OSA was 20.5, compared with 23.6 for those without the sleep disorder.
Results showed OSA was significantly associated with a lower score on the MoCA scale (odds ratio, 0.40; P = .048). “This demonstrated an association of OSA with lower cognitive scores,” Mr. Colelli said.
The analysis also showed that OSA severity was correlated with actigraphy-derived sleep variables, including lower total sleep time, greater sleep onset latency, lower sleep efficiency, and more awakenings.
The study was too small to determine whether a specific diagnosis of cognitive impairment affected the link to OSA, Mr. Colelli said. “But definitely future research should be directed towards looking at this.”
Obesity is a risk factor for OSA, but the mean BMI in the study was not in the obese range of 30 and over. This, Mr. Colelli said, suggests that sleep apnea may present differently in those with cognitive impairment.
“Sleep apnea in this population might not present with the typical risk factors of obesity or snoring or feeling tired.”
While the new study “adds to the understanding that there’s a link between sleep and cognitive impairment, the direction of that link isn’t entirely clear,” Mr. Colelli said.
“It’s slowly becoming appreciated that the relationship might be bidirectionality, where sleep apnea might be contributing to the cognitive impairment and cognitive impairment could be contributing to the sleep issues.”
The study highlights how essential sleep is to mental health, Mr. Colelli said. “I feel, and I’m sure you do too, that if you don’t get good sleep, you feel tired during the day and you may not have the best concentration or memory.”
Identifying sleep issues in patients with cognitive impairment is important, as treatment and management of these issues could affect outcomes including cognition and quality of life, he added.
“Future research should be directed to see if treatment of sleep disorders with continuous positive airway pressure (CPAP), which is the gold standard, and various other treatments, can improve outcomes.” Future research should also examine OSA prevalence in larger cohorts.
Common, undertreated
Commenting on the resaerch, Lei Gao, MD, assistant professor of anesthesia at Harvard Medical School, Boston, whose areas of expertise include disorders of cognition, sleep, and circadian rhythm, believes the findings are important. “It highlights how common and potentially undertreated OSA is in this age group, and in particular, its link to cognitive impairment.”
OSA is often associated with significant comorbidities, as well as sleep disruption, Dr. Gao noted. One of the study’s strengths was including objective assessment of sleep using actigraphy. “It will be interesting to see to what extent the OSA link to cognitive impairment is via poor sleep or disrupted circadian rest/activity cycles.”
It would also be interesting “to tease out whether OSA is more linked to dementia of vascular etiologies due to common risk factors, or whether it is pervasive to all forms of dementia,” he added.
A version of this article first appeared on Medscape.com.
FROM AAN 2021
JAMA podcast on racism in medicine faces backlash
Published on Feb. 23, the episode is hosted on JAMA’s learning platform for doctors and is available for continuing medical education credits.
“No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast,” JAMA wrote in a Twitter post to promote the episode. That tweet has since been deleted.

The episode features host Ed Livingston, MD, deputy editor for clinical reviews and education at JAMA, and guest Mitchell Katz, MD, president and CEO for NYC Health + Hospitals and deputy editor for JAMA Internal Medicine. Dr. Livingston approaches the episode as “structural racism for skeptics,” and Dr. Katz tries to explain how structural racism deepens health disparities and what health systems can do about it.
“Many physicians are skeptical of structural racism, the idea that economic, educational, and other societal systems preferentially disadvantage Black Americans and other communities of color,” the episode description says.
In the podcast, Dr. Livingston and Dr. Katz speak about health care disparities and racial inequality. Dr. Livingston, who says he “didn’t understand the concept” going into the episode, suggests that racism was made illegal in the 1960s and that the discussion of “structural racism” should shift away from the term “racism” and focus on socioeconomic status instead.
“What you’re talking about isn’t so much racism ... it isn’t their race, it isn’t their color, it’s their socioeconomic status,” Dr. Livingston says. “Is that a fair statement?”
But Dr. Katz says that “acknowledging structural racism can be helpful to us. Structural racism refers to a system in which policies or practices or how we look at people perpetuates racial inequality.”
Dr. Katz points to the creation of a hospital in San Francisco in the 1880s to treat patients of Chinese ethnicity separately. Outside of health care, he talks about environmental racism between neighborhoods with inequalities in hospitals, schools, and social services.
“All of those things have an impact on that minority person,” Dr. Katz says. “The big thing we can all do is move away from trying to interrogate each other’s opinions and move to a place where we are looking at the policies of our institutions and making sure that they promote equality.”
Dr. Livingston concludes the episode by reemphasizing that “racism” should be taken out of the conversation and it should instead focus on the “structural” aspect of socioeconomics.
“Minorities ... aren’t [in those neighborhoods] because they’re not allowed to buy houses or they can’t get a job because they’re Black or Hispanic. That would be illegal,” Dr. Livingston says. “But disproportionality does exist.”
Efforts to reach Dr. Livingston were unsuccessful. Dr. Katz distanced himself from Dr. Livingston in a statement released on March 4.
“Systemic and interpersonal racism both still exist in our country — they must be rooted out. I do not share the JAMA host’s belief of doing away with the word ‘racism’ will help us be more successful in ending inequities that exists across racial and ethnic lines,” Dr. Katz said. “Further, I believe that we will only produce an equitable society when social and political structures do not continue to produce and perpetuate disparate results based on social race and ethnicity.”
Dr. Katz reiterated that both interpersonal and structural racism continue to exist in the United States, “and it is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it.”
He also recommended JAMA use this controversy “as a learning opportunity for continued dialogue and create another podcast series as an open conversation that invites diverse experts in the field to have an open discussion about structural racism in healthcare.”
The podcast and JAMA’s tweet promoting it were widely criticized on Twitter. In interviews with WebMD, many doctors expressed disbelief that such a respected journal would lend its name to this podcast episode.
B. Bobby Chiong, MD, a radiologist in New York, said although JAMA’s effort to engage with its audience about racism is laudable, it missed the mark.
“I think the backlash comes from how they tried to make a podcast about the subject and somehow made themselves an example of unconscious bias and unfamiliarity with just how embedded in our system is structural racism,” he said.
Perhaps the podcast’s worst offense was its failure to address the painful history of racial bias in this country that still permeates the medical community, says Tamara Saint-Surin, MD, assistant professor at the University of North Carolina at Chapel Hill.
“For physicians in leadership to have the belief that structural racism does not exist in medicine, they don’t really appreciate what affects their patients and what their patients were dealing with,” Dr. Saint-Surin said in an interview. “It was a very harmful podcast and goes to show we still have so much work to do.”
Along with a flawed premise, she says, the podcast was not nearly long enough to address such a nuanced issue. And Dr. Livingston focused on interpersonal racism rather than structural racism, she said, failing to address widespread problems such as higher rates of asthma among Black populations living in areas with poor air quality.
The number of Black doctors remains low and the lack of representation adds to an environment already rife with racism, according to many medical professionals.
Shirlene Obuobi, MD, an internal medicine doctor in Chicago, said JAMA failed to live up to its own standards by publishing material that lacked research and expertise.
“I can’t submit a clinical trial to JAMA without them combing through methods with a fine-tooth comb,” Dr. Obuobi said. “They didn’t uphold the standards they normally apply to anyone else.”
Both the editor of JAMA and the head of the American Medical Association issued statements criticizing the episode and the tweet that promoted it.
JAMA Editor-in-Chief Howard Bauchner, MD, said, “The language of the tweet, and some portions of the podcast, do not reflect my commitment as editorial leader of JAMA and JAMA Network to call out and discuss the adverse effects of injustice, inequity, and racism in society and medicine as JAMA has done for many years.” He said JAMA will schedule a future podcast to address the concerns raised about the recent episode.
AMA CEO James L. Madara, MD, said, “The AMA’s House of Delegates passed policy stating that racism is structural, systemic, cultural, and interpersonal, and we are deeply disturbed – and angered – by a recent JAMA podcast that questioned the existence of structural racism and the affiliated tweet that promoted the podcast and stated ‘no physician is racist, so how can there be structural racism in health care?’ ”
He continued: “JAMA has editorial independence from AMA, but this tweet and podcast are inconsistent with the policies and views of AMA, and I’m concerned about and acknowledge the harms they have caused. Structural racism in health care and our society exists, and it is incumbent on all of us to fix it.”
This article was updated 3/5/21.
A version of this article first appeared on WebMD.com.
Published on Feb. 23, the episode is hosted on JAMA’s learning platform for doctors and is available for continuing medical education credits.
“No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast,” JAMA wrote in a Twitter post to promote the episode. That tweet has since been deleted.

The episode features host Ed Livingston, MD, deputy editor for clinical reviews and education at JAMA, and guest Mitchell Katz, MD, president and CEO for NYC Health + Hospitals and deputy editor for JAMA Internal Medicine. Dr. Livingston approaches the episode as “structural racism for skeptics,” and Dr. Katz tries to explain how structural racism deepens health disparities and what health systems can do about it.
“Many physicians are skeptical of structural racism, the idea that economic, educational, and other societal systems preferentially disadvantage Black Americans and other communities of color,” the episode description says.
In the podcast, Dr. Livingston and Dr. Katz speak about health care disparities and racial inequality. Dr. Livingston, who says he “didn’t understand the concept” going into the episode, suggests that racism was made illegal in the 1960s and that the discussion of “structural racism” should shift away from the term “racism” and focus on socioeconomic status instead.
“What you’re talking about isn’t so much racism ... it isn’t their race, it isn’t their color, it’s their socioeconomic status,” Dr. Livingston says. “Is that a fair statement?”
But Dr. Katz says that “acknowledging structural racism can be helpful to us. Structural racism refers to a system in which policies or practices or how we look at people perpetuates racial inequality.”
Dr. Katz points to the creation of a hospital in San Francisco in the 1880s to treat patients of Chinese ethnicity separately. Outside of health care, he talks about environmental racism between neighborhoods with inequalities in hospitals, schools, and social services.
“All of those things have an impact on that minority person,” Dr. Katz says. “The big thing we can all do is move away from trying to interrogate each other’s opinions and move to a place where we are looking at the policies of our institutions and making sure that they promote equality.”
Dr. Livingston concludes the episode by reemphasizing that “racism” should be taken out of the conversation and it should instead focus on the “structural” aspect of socioeconomics.
“Minorities ... aren’t [in those neighborhoods] because they’re not allowed to buy houses or they can’t get a job because they’re Black or Hispanic. That would be illegal,” Dr. Livingston says. “But disproportionality does exist.”
Efforts to reach Dr. Livingston were unsuccessful. Dr. Katz distanced himself from Dr. Livingston in a statement released on March 4.
“Systemic and interpersonal racism both still exist in our country — they must be rooted out. I do not share the JAMA host’s belief of doing away with the word ‘racism’ will help us be more successful in ending inequities that exists across racial and ethnic lines,” Dr. Katz said. “Further, I believe that we will only produce an equitable society when social and political structures do not continue to produce and perpetuate disparate results based on social race and ethnicity.”
Dr. Katz reiterated that both interpersonal and structural racism continue to exist in the United States, “and it is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it.”
He also recommended JAMA use this controversy “as a learning opportunity for continued dialogue and create another podcast series as an open conversation that invites diverse experts in the field to have an open discussion about structural racism in healthcare.”
The podcast and JAMA’s tweet promoting it were widely criticized on Twitter. In interviews with WebMD, many doctors expressed disbelief that such a respected journal would lend its name to this podcast episode.
B. Bobby Chiong, MD, a radiologist in New York, said although JAMA’s effort to engage with its audience about racism is laudable, it missed the mark.
“I think the backlash comes from how they tried to make a podcast about the subject and somehow made themselves an example of unconscious bias and unfamiliarity with just how embedded in our system is structural racism,” he said.
Perhaps the podcast’s worst offense was its failure to address the painful history of racial bias in this country that still permeates the medical community, says Tamara Saint-Surin, MD, assistant professor at the University of North Carolina at Chapel Hill.
“For physicians in leadership to have the belief that structural racism does not exist in medicine, they don’t really appreciate what affects their patients and what their patients were dealing with,” Dr. Saint-Surin said in an interview. “It was a very harmful podcast and goes to show we still have so much work to do.”
Along with a flawed premise, she says, the podcast was not nearly long enough to address such a nuanced issue. And Dr. Livingston focused on interpersonal racism rather than structural racism, she said, failing to address widespread problems such as higher rates of asthma among Black populations living in areas with poor air quality.
The number of Black doctors remains low and the lack of representation adds to an environment already rife with racism, according to many medical professionals.
Shirlene Obuobi, MD, an internal medicine doctor in Chicago, said JAMA failed to live up to its own standards by publishing material that lacked research and expertise.
“I can’t submit a clinical trial to JAMA without them combing through methods with a fine-tooth comb,” Dr. Obuobi said. “They didn’t uphold the standards they normally apply to anyone else.”
Both the editor of JAMA and the head of the American Medical Association issued statements criticizing the episode and the tweet that promoted it.
JAMA Editor-in-Chief Howard Bauchner, MD, said, “The language of the tweet, and some portions of the podcast, do not reflect my commitment as editorial leader of JAMA and JAMA Network to call out and discuss the adverse effects of injustice, inequity, and racism in society and medicine as JAMA has done for many years.” He said JAMA will schedule a future podcast to address the concerns raised about the recent episode.
AMA CEO James L. Madara, MD, said, “The AMA’s House of Delegates passed policy stating that racism is structural, systemic, cultural, and interpersonal, and we are deeply disturbed – and angered – by a recent JAMA podcast that questioned the existence of structural racism and the affiliated tweet that promoted the podcast and stated ‘no physician is racist, so how can there be structural racism in health care?’ ”
He continued: “JAMA has editorial independence from AMA, but this tweet and podcast are inconsistent with the policies and views of AMA, and I’m concerned about and acknowledge the harms they have caused. Structural racism in health care and our society exists, and it is incumbent on all of us to fix it.”
This article was updated 3/5/21.
A version of this article first appeared on WebMD.com.
Published on Feb. 23, the episode is hosted on JAMA’s learning platform for doctors and is available for continuing medical education credits.
“No physician is racist, so how can there be structural racism in health care? An explanation of the idea by doctors for doctors in this user-friendly podcast,” JAMA wrote in a Twitter post to promote the episode. That tweet has since been deleted.

The episode features host Ed Livingston, MD, deputy editor for clinical reviews and education at JAMA, and guest Mitchell Katz, MD, president and CEO for NYC Health + Hospitals and deputy editor for JAMA Internal Medicine. Dr. Livingston approaches the episode as “structural racism for skeptics,” and Dr. Katz tries to explain how structural racism deepens health disparities and what health systems can do about it.
“Many physicians are skeptical of structural racism, the idea that economic, educational, and other societal systems preferentially disadvantage Black Americans and other communities of color,” the episode description says.
In the podcast, Dr. Livingston and Dr. Katz speak about health care disparities and racial inequality. Dr. Livingston, who says he “didn’t understand the concept” going into the episode, suggests that racism was made illegal in the 1960s and that the discussion of “structural racism” should shift away from the term “racism” and focus on socioeconomic status instead.
“What you’re talking about isn’t so much racism ... it isn’t their race, it isn’t their color, it’s their socioeconomic status,” Dr. Livingston says. “Is that a fair statement?”
But Dr. Katz says that “acknowledging structural racism can be helpful to us. Structural racism refers to a system in which policies or practices or how we look at people perpetuates racial inequality.”
Dr. Katz points to the creation of a hospital in San Francisco in the 1880s to treat patients of Chinese ethnicity separately. Outside of health care, he talks about environmental racism between neighborhoods with inequalities in hospitals, schools, and social services.
“All of those things have an impact on that minority person,” Dr. Katz says. “The big thing we can all do is move away from trying to interrogate each other’s opinions and move to a place where we are looking at the policies of our institutions and making sure that they promote equality.”
Dr. Livingston concludes the episode by reemphasizing that “racism” should be taken out of the conversation and it should instead focus on the “structural” aspect of socioeconomics.
“Minorities ... aren’t [in those neighborhoods] because they’re not allowed to buy houses or they can’t get a job because they’re Black or Hispanic. That would be illegal,” Dr. Livingston says. “But disproportionality does exist.”
Efforts to reach Dr. Livingston were unsuccessful. Dr. Katz distanced himself from Dr. Livingston in a statement released on March 4.
“Systemic and interpersonal racism both still exist in our country — they must be rooted out. I do not share the JAMA host’s belief of doing away with the word ‘racism’ will help us be more successful in ending inequities that exists across racial and ethnic lines,” Dr. Katz said. “Further, I believe that we will only produce an equitable society when social and political structures do not continue to produce and perpetuate disparate results based on social race and ethnicity.”
Dr. Katz reiterated that both interpersonal and structural racism continue to exist in the United States, “and it is woefully naive to say that no physician is a racist just because the Civil Rights Act of 1964 forbade it.”
He also recommended JAMA use this controversy “as a learning opportunity for continued dialogue and create another podcast series as an open conversation that invites diverse experts in the field to have an open discussion about structural racism in healthcare.”
The podcast and JAMA’s tweet promoting it were widely criticized on Twitter. In interviews with WebMD, many doctors expressed disbelief that such a respected journal would lend its name to this podcast episode.
B. Bobby Chiong, MD, a radiologist in New York, said although JAMA’s effort to engage with its audience about racism is laudable, it missed the mark.
“I think the backlash comes from how they tried to make a podcast about the subject and somehow made themselves an example of unconscious bias and unfamiliarity with just how embedded in our system is structural racism,” he said.
Perhaps the podcast’s worst offense was its failure to address the painful history of racial bias in this country that still permeates the medical community, says Tamara Saint-Surin, MD, assistant professor at the University of North Carolina at Chapel Hill.
“For physicians in leadership to have the belief that structural racism does not exist in medicine, they don’t really appreciate what affects their patients and what their patients were dealing with,” Dr. Saint-Surin said in an interview. “It was a very harmful podcast and goes to show we still have so much work to do.”
Along with a flawed premise, she says, the podcast was not nearly long enough to address such a nuanced issue. And Dr. Livingston focused on interpersonal racism rather than structural racism, she said, failing to address widespread problems such as higher rates of asthma among Black populations living in areas with poor air quality.
The number of Black doctors remains low and the lack of representation adds to an environment already rife with racism, according to many medical professionals.
Shirlene Obuobi, MD, an internal medicine doctor in Chicago, said JAMA failed to live up to its own standards by publishing material that lacked research and expertise.
“I can’t submit a clinical trial to JAMA without them combing through methods with a fine-tooth comb,” Dr. Obuobi said. “They didn’t uphold the standards they normally apply to anyone else.”
Both the editor of JAMA and the head of the American Medical Association issued statements criticizing the episode and the tweet that promoted it.
JAMA Editor-in-Chief Howard Bauchner, MD, said, “The language of the tweet, and some portions of the podcast, do not reflect my commitment as editorial leader of JAMA and JAMA Network to call out and discuss the adverse effects of injustice, inequity, and racism in society and medicine as JAMA has done for many years.” He said JAMA will schedule a future podcast to address the concerns raised about the recent episode.
AMA CEO James L. Madara, MD, said, “The AMA’s House of Delegates passed policy stating that racism is structural, systemic, cultural, and interpersonal, and we are deeply disturbed – and angered – by a recent JAMA podcast that questioned the existence of structural racism and the affiliated tweet that promoted the podcast and stated ‘no physician is racist, so how can there be structural racism in health care?’ ”
He continued: “JAMA has editorial independence from AMA, but this tweet and podcast are inconsistent with the policies and views of AMA, and I’m concerned about and acknowledge the harms they have caused. Structural racism in health care and our society exists, and it is incumbent on all of us to fix it.”
This article was updated 3/5/21.
A version of this article first appeared on WebMD.com.
Do antidepressants increase the risk of brain bleeds?
Contrary to previous findings, results of a large observational study show. However, at least one expert urged caution in interpreting the finding.
“These findings are important, especially since depression is common after stroke and SSRIs are some of the first drugs considered for people,” Mithilesh Siddu, MD, of the University of Miami/Jackson Memorial Hospital, also in Miami, said in a statement.
However, Dr. Siddu said “more research is needed to confirm our findings and to also examine if SSRIs prescribed after a stroke may be linked to risk of a second stroke.”
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Widely prescribed
SSRIs, the most widely prescribed antidepressant in the United States, have previously been linked to an increased risk of ICH, possibly as a result of impaired platelet function.
To investigate further, the researchers analyzed data from the Florida Stroke Registry (FSR). They identified 127,915 patients who suffered ICH from January 2010 to December 2019 and for whom information on antidepressant use was available.
They analyzed the proportion of cases presenting with ICH among antidepressant users and the rate of SSRI prescription among stroke patients discharged on antidepressant therapy.
The researchers found that 11% of those who had been prescribed antidepressants had an ICH, compared with 14% of those who had not.
Antidepressant users were more likely to be female; non-Hispanic White; have hypertension; have diabetes; and use oral anticoagulants, antiplatelets, and statins prior to hospital presentation for ICH.
In multivariable analyses adjusting for age, race, prior history of hypertension, diabetes and prior oral anticoagulant, antiplatelet and statin use, antidepressant users were just as likely to present with spontaneous ICH as nonantidepressant users (odds ratio, 0.92; 95% confidence interval, 0.85-1.01).
A total of 3.4% of all ICH patients and 9% of those in whom specific antidepressant information was available were discharged home on an antidepressant, most commonly an SSRI (74%).
The authors noted a key limitation of the study: Some details regarding the length, dosage, and type of antidepressants were not available.
Interpret with caution
In a comment, Shaheen Lakhan, MD, PhD, a neurologist in Newton, Mass., and executive director of the Global Neuroscience Initiative Foundation, urged caution in making any firm conclusions based on this study.
“We have two questions here: One, is SSRI use a risk factor for first-time intracerebral hemorrhage, and two, is SSRI use after an ICH a risk factor for additional hemorrhages,” said Dr. Lakhan, who was not involved with the study.
“This study incompletely addresses the first because it is known that SSRIs have a variety of potencies. For instance, paroxetine is a strong inhibitor of serotonin reuptake, whereas bupropion is weak. Hypothetically, the former has a greater risk of ICH. Because this study did not stratify by type of antidepressant, it is not possible to tease these out,” Dr. Lakhan said.
“The second question is completely unaddressed by this study and is the real concern in clinical practice, because the chance of rebleed is much higher than the risk of first-time ICH in the general population,” he added.
The study had no specific funding. Dr. Siddu and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Contrary to previous findings, results of a large observational study show. However, at least one expert urged caution in interpreting the finding.
“These findings are important, especially since depression is common after stroke and SSRIs are some of the first drugs considered for people,” Mithilesh Siddu, MD, of the University of Miami/Jackson Memorial Hospital, also in Miami, said in a statement.
However, Dr. Siddu said “more research is needed to confirm our findings and to also examine if SSRIs prescribed after a stroke may be linked to risk of a second stroke.”
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Widely prescribed
SSRIs, the most widely prescribed antidepressant in the United States, have previously been linked to an increased risk of ICH, possibly as a result of impaired platelet function.
To investigate further, the researchers analyzed data from the Florida Stroke Registry (FSR). They identified 127,915 patients who suffered ICH from January 2010 to December 2019 and for whom information on antidepressant use was available.
They analyzed the proportion of cases presenting with ICH among antidepressant users and the rate of SSRI prescription among stroke patients discharged on antidepressant therapy.
The researchers found that 11% of those who had been prescribed antidepressants had an ICH, compared with 14% of those who had not.
Antidepressant users were more likely to be female; non-Hispanic White; have hypertension; have diabetes; and use oral anticoagulants, antiplatelets, and statins prior to hospital presentation for ICH.
In multivariable analyses adjusting for age, race, prior history of hypertension, diabetes and prior oral anticoagulant, antiplatelet and statin use, antidepressant users were just as likely to present with spontaneous ICH as nonantidepressant users (odds ratio, 0.92; 95% confidence interval, 0.85-1.01).
A total of 3.4% of all ICH patients and 9% of those in whom specific antidepressant information was available were discharged home on an antidepressant, most commonly an SSRI (74%).
The authors noted a key limitation of the study: Some details regarding the length, dosage, and type of antidepressants were not available.
Interpret with caution
In a comment, Shaheen Lakhan, MD, PhD, a neurologist in Newton, Mass., and executive director of the Global Neuroscience Initiative Foundation, urged caution in making any firm conclusions based on this study.
“We have two questions here: One, is SSRI use a risk factor for first-time intracerebral hemorrhage, and two, is SSRI use after an ICH a risk factor for additional hemorrhages,” said Dr. Lakhan, who was not involved with the study.
“This study incompletely addresses the first because it is known that SSRIs have a variety of potencies. For instance, paroxetine is a strong inhibitor of serotonin reuptake, whereas bupropion is weak. Hypothetically, the former has a greater risk of ICH. Because this study did not stratify by type of antidepressant, it is not possible to tease these out,” Dr. Lakhan said.
“The second question is completely unaddressed by this study and is the real concern in clinical practice, because the chance of rebleed is much higher than the risk of first-time ICH in the general population,” he added.
The study had no specific funding. Dr. Siddu and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Contrary to previous findings, results of a large observational study show. However, at least one expert urged caution in interpreting the finding.
“These findings are important, especially since depression is common after stroke and SSRIs are some of the first drugs considered for people,” Mithilesh Siddu, MD, of the University of Miami/Jackson Memorial Hospital, also in Miami, said in a statement.
However, Dr. Siddu said “more research is needed to confirm our findings and to also examine if SSRIs prescribed after a stroke may be linked to risk of a second stroke.”
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Widely prescribed
SSRIs, the most widely prescribed antidepressant in the United States, have previously been linked to an increased risk of ICH, possibly as a result of impaired platelet function.
To investigate further, the researchers analyzed data from the Florida Stroke Registry (FSR). They identified 127,915 patients who suffered ICH from January 2010 to December 2019 and for whom information on antidepressant use was available.
They analyzed the proportion of cases presenting with ICH among antidepressant users and the rate of SSRI prescription among stroke patients discharged on antidepressant therapy.
The researchers found that 11% of those who had been prescribed antidepressants had an ICH, compared with 14% of those who had not.
Antidepressant users were more likely to be female; non-Hispanic White; have hypertension; have diabetes; and use oral anticoagulants, antiplatelets, and statins prior to hospital presentation for ICH.
In multivariable analyses adjusting for age, race, prior history of hypertension, diabetes and prior oral anticoagulant, antiplatelet and statin use, antidepressant users were just as likely to present with spontaneous ICH as nonantidepressant users (odds ratio, 0.92; 95% confidence interval, 0.85-1.01).
A total of 3.4% of all ICH patients and 9% of those in whom specific antidepressant information was available were discharged home on an antidepressant, most commonly an SSRI (74%).
The authors noted a key limitation of the study: Some details regarding the length, dosage, and type of antidepressants were not available.
Interpret with caution
In a comment, Shaheen Lakhan, MD, PhD, a neurologist in Newton, Mass., and executive director of the Global Neuroscience Initiative Foundation, urged caution in making any firm conclusions based on this study.
“We have two questions here: One, is SSRI use a risk factor for first-time intracerebral hemorrhage, and two, is SSRI use after an ICH a risk factor for additional hemorrhages,” said Dr. Lakhan, who was not involved with the study.
“This study incompletely addresses the first because it is known that SSRIs have a variety of potencies. For instance, paroxetine is a strong inhibitor of serotonin reuptake, whereas bupropion is weak. Hypothetically, the former has a greater risk of ICH. Because this study did not stratify by type of antidepressant, it is not possible to tease these out,” Dr. Lakhan said.
“The second question is completely unaddressed by this study and is the real concern in clinical practice, because the chance of rebleed is much higher than the risk of first-time ICH in the general population,” he added.
The study had no specific funding. Dr. Siddu and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2021
Natalizumab postinfusion reactions rare; is monitoring necessary?
new studies show.
Collectively, the results suggest the need to rethink the drug’s mandatory 1-hour postinfusion observation period – particularly when unnecessarily spending time in medical settings is discouraged because of concerns regarding COVID-19, the researchers concluded.
Their findings “highlight a potential opportunity to improve and streamline the infusion and postinfusion monitoring process,” reported the authors of one of the studies. The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Infusion reactions were rare
“In this systematic review of almost 10,000 natalizumab infusions, all infusion-related adverse events were mild, and no clinically relevant safety concerns were associated with natalizumab infusions,” they said.
The 1-hour postinfusion observation period for natalizumab, approved for the treatment of relapsing remitting MS (RRMS), is mandated by the Food and Drug Administration, as well as the European Medicines Agency, and applies to each dose, regardless of treatment duration, owing to concerns of infusion reactions. However, previous evidence has indicated that reactions are rare and are usually mild.
In addition to adding burden to the treatment regimen for patients and providers alike, any extended time in an environment where there is concern of heightened risk for SARS-CoV-2 exposure is a concern.
To evaluate the frequency, severity, and timing of infusion reactions, Yujie Wang, MD, of the department of neurology at the University of Washington, Seattle, and colleagues reviewed medical records of all patients who received natalizumab at the University of Washington MS Center’s infusion suite between July 2012 and September 2020.
Among 333 patients with RRMS, 9,682 infusions of natalizumab were provided over the study period, with a mean of 27 infusions per patient (range, 1-174). The mean age of the patients was 41 years, and 87 (26%) were male.
Overall, 33 infusion-related adverse events were reported in 26 patients, representing 0.34% of total infusions and 7.8% of patients.
In 77% of cases, the adverse event occurred during the infusion. In 92% of cases, the adverse event occurred within the first 6 months of treatment.
All of the events were described as mild. The most common were itching, gastrointestinal problems, headache, and flushing.
None of the reactions required emergency care or hospitalization. Symptoms were either self-managed or were managed easily with standard care. The treatment was continued in all cases.
“For physicians and providers who care for patients with MS and are comfortable with infusible therapies, it is no surprise that rates of clinically significant infusion reactions were low,” Dr. Wang said. “It is indeed consistent with prior studies that reactions generally occur during rather than post infusion.”
The authors underscored the array of potential benefits in making changes to the requirement. “Anticipated benefits may include reducing SARS-CoV2 exposure risks for patients and staff, reducing patients’ treatment burden, increasing efficiency, as well as improving access to care without neglecting patient safety.”
Additional studies show consistent findings
Several other recent studies have shown similar results. In a study published in Multiple Sclerosis in October 2020, researchers with the Amsterdam University Medical Center found that, among 14,174 natalizumab infusions provided to 225 patients with RRMS between 2006 and 2018, 276 infusion-related adverse events occurred (1.95%) among 60 patients.
There were 11 severe infusion-related adverse events in nine patients (4.0%). All documented severe reactions occurred during the infusion. Among 19 moderate adverse events, 17 occurred during the infusion.
The researchers noted that the majority of patients who experienced severe infusion reactions had detectable antibodies against natalizumab. Such antibodies are associated with a higher risk for infusion-related adverse events.
Patients who did not have any symptoms of a reaction during the infusion had no clinically relevant moderate or severe reactions.
“Thus, the need for postinfusion observation will depend on the patients’ clinical status during the infusion,” they wrote. “Consequently, our data suggest that patients who do not have an infusion-related adverse event while receiving natalizumab treatment do not need to stay in the hospital for an additional observation hour.”
Rapid infusion protocol
In another recent study published in Multiple Sclerosis and Related Disorders in January 2021, researchers in Australia reported on the use of a rapid infusion protocol of natalizumab and ocrelizumab. The protocol was implemented to reduce the amount of time patients are required to spend in clinical settings during the COVID-19 pandemic.
In their analysis of 269 rapid infusions of natalizumab and 100 rapid infusions of ocrelizumab, there were two infusion-related reactions in the natalizumab group and eight in the ocrelizumab group.
All the reactions were mild to moderate, and no discontinuations were required. None of the reactions occurred during the postinfusion observation period.
“In the setting of COVID-19 pandemic, rapid infusion protocols could potentially save hospital resources and limit patient exposure to a high-risk clinical setting while still maintaining ongoing treatment of multiple sclerosis,” the authors wrote.
Under the rapid infusion protocol, patients receive three standard doses for 1 hour followed by 30 minutes of observation. In addition, infusions are reduced to 30 minutes, explained lead author Louise Rath, of clinical neurosciences, Alfred Health, in Melbourne.
“For our cohort of patients, the side effects were minimal,” she said.
“Rapid infusions allowed patients to have option of hospital in-home or office, ensuring work was not at risk by infusion,” she added. “Our governance has been very supportive, and we will be keeping rapid infusion post COVID.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new studies show.
Collectively, the results suggest the need to rethink the drug’s mandatory 1-hour postinfusion observation period – particularly when unnecessarily spending time in medical settings is discouraged because of concerns regarding COVID-19, the researchers concluded.
Their findings “highlight a potential opportunity to improve and streamline the infusion and postinfusion monitoring process,” reported the authors of one of the studies. The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Infusion reactions were rare
“In this systematic review of almost 10,000 natalizumab infusions, all infusion-related adverse events were mild, and no clinically relevant safety concerns were associated with natalizumab infusions,” they said.
The 1-hour postinfusion observation period for natalizumab, approved for the treatment of relapsing remitting MS (RRMS), is mandated by the Food and Drug Administration, as well as the European Medicines Agency, and applies to each dose, regardless of treatment duration, owing to concerns of infusion reactions. However, previous evidence has indicated that reactions are rare and are usually mild.
In addition to adding burden to the treatment regimen for patients and providers alike, any extended time in an environment where there is concern of heightened risk for SARS-CoV-2 exposure is a concern.
To evaluate the frequency, severity, and timing of infusion reactions, Yujie Wang, MD, of the department of neurology at the University of Washington, Seattle, and colleagues reviewed medical records of all patients who received natalizumab at the University of Washington MS Center’s infusion suite between July 2012 and September 2020.
Among 333 patients with RRMS, 9,682 infusions of natalizumab were provided over the study period, with a mean of 27 infusions per patient (range, 1-174). The mean age of the patients was 41 years, and 87 (26%) were male.
Overall, 33 infusion-related adverse events were reported in 26 patients, representing 0.34% of total infusions and 7.8% of patients.
In 77% of cases, the adverse event occurred during the infusion. In 92% of cases, the adverse event occurred within the first 6 months of treatment.
All of the events were described as mild. The most common were itching, gastrointestinal problems, headache, and flushing.
None of the reactions required emergency care or hospitalization. Symptoms were either self-managed or were managed easily with standard care. The treatment was continued in all cases.
“For physicians and providers who care for patients with MS and are comfortable with infusible therapies, it is no surprise that rates of clinically significant infusion reactions were low,” Dr. Wang said. “It is indeed consistent with prior studies that reactions generally occur during rather than post infusion.”
The authors underscored the array of potential benefits in making changes to the requirement. “Anticipated benefits may include reducing SARS-CoV2 exposure risks for patients and staff, reducing patients’ treatment burden, increasing efficiency, as well as improving access to care without neglecting patient safety.”
Additional studies show consistent findings
Several other recent studies have shown similar results. In a study published in Multiple Sclerosis in October 2020, researchers with the Amsterdam University Medical Center found that, among 14,174 natalizumab infusions provided to 225 patients with RRMS between 2006 and 2018, 276 infusion-related adverse events occurred (1.95%) among 60 patients.
There were 11 severe infusion-related adverse events in nine patients (4.0%). All documented severe reactions occurred during the infusion. Among 19 moderate adverse events, 17 occurred during the infusion.
The researchers noted that the majority of patients who experienced severe infusion reactions had detectable antibodies against natalizumab. Such antibodies are associated with a higher risk for infusion-related adverse events.
Patients who did not have any symptoms of a reaction during the infusion had no clinically relevant moderate or severe reactions.
“Thus, the need for postinfusion observation will depend on the patients’ clinical status during the infusion,” they wrote. “Consequently, our data suggest that patients who do not have an infusion-related adverse event while receiving natalizumab treatment do not need to stay in the hospital for an additional observation hour.”
Rapid infusion protocol
In another recent study published in Multiple Sclerosis and Related Disorders in January 2021, researchers in Australia reported on the use of a rapid infusion protocol of natalizumab and ocrelizumab. The protocol was implemented to reduce the amount of time patients are required to spend in clinical settings during the COVID-19 pandemic.
In their analysis of 269 rapid infusions of natalizumab and 100 rapid infusions of ocrelizumab, there were two infusion-related reactions in the natalizumab group and eight in the ocrelizumab group.
All the reactions were mild to moderate, and no discontinuations were required. None of the reactions occurred during the postinfusion observation period.
“In the setting of COVID-19 pandemic, rapid infusion protocols could potentially save hospital resources and limit patient exposure to a high-risk clinical setting while still maintaining ongoing treatment of multiple sclerosis,” the authors wrote.
Under the rapid infusion protocol, patients receive three standard doses for 1 hour followed by 30 minutes of observation. In addition, infusions are reduced to 30 minutes, explained lead author Louise Rath, of clinical neurosciences, Alfred Health, in Melbourne.
“For our cohort of patients, the side effects were minimal,” she said.
“Rapid infusions allowed patients to have option of hospital in-home or office, ensuring work was not at risk by infusion,” she added. “Our governance has been very supportive, and we will be keeping rapid infusion post COVID.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new studies show.
Collectively, the results suggest the need to rethink the drug’s mandatory 1-hour postinfusion observation period – particularly when unnecessarily spending time in medical settings is discouraged because of concerns regarding COVID-19, the researchers concluded.
Their findings “highlight a potential opportunity to improve and streamline the infusion and postinfusion monitoring process,” reported the authors of one of the studies. The findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Infusion reactions were rare
“In this systematic review of almost 10,000 natalizumab infusions, all infusion-related adverse events were mild, and no clinically relevant safety concerns were associated with natalizumab infusions,” they said.
The 1-hour postinfusion observation period for natalizumab, approved for the treatment of relapsing remitting MS (RRMS), is mandated by the Food and Drug Administration, as well as the European Medicines Agency, and applies to each dose, regardless of treatment duration, owing to concerns of infusion reactions. However, previous evidence has indicated that reactions are rare and are usually mild.
In addition to adding burden to the treatment regimen for patients and providers alike, any extended time in an environment where there is concern of heightened risk for SARS-CoV-2 exposure is a concern.
To evaluate the frequency, severity, and timing of infusion reactions, Yujie Wang, MD, of the department of neurology at the University of Washington, Seattle, and colleagues reviewed medical records of all patients who received natalizumab at the University of Washington MS Center’s infusion suite between July 2012 and September 2020.
Among 333 patients with RRMS, 9,682 infusions of natalizumab were provided over the study period, with a mean of 27 infusions per patient (range, 1-174). The mean age of the patients was 41 years, and 87 (26%) were male.
Overall, 33 infusion-related adverse events were reported in 26 patients, representing 0.34% of total infusions and 7.8% of patients.
In 77% of cases, the adverse event occurred during the infusion. In 92% of cases, the adverse event occurred within the first 6 months of treatment.
All of the events were described as mild. The most common were itching, gastrointestinal problems, headache, and flushing.
None of the reactions required emergency care or hospitalization. Symptoms were either self-managed or were managed easily with standard care. The treatment was continued in all cases.
“For physicians and providers who care for patients with MS and are comfortable with infusible therapies, it is no surprise that rates of clinically significant infusion reactions were low,” Dr. Wang said. “It is indeed consistent with prior studies that reactions generally occur during rather than post infusion.”
The authors underscored the array of potential benefits in making changes to the requirement. “Anticipated benefits may include reducing SARS-CoV2 exposure risks for patients and staff, reducing patients’ treatment burden, increasing efficiency, as well as improving access to care without neglecting patient safety.”
Additional studies show consistent findings
Several other recent studies have shown similar results. In a study published in Multiple Sclerosis in October 2020, researchers with the Amsterdam University Medical Center found that, among 14,174 natalizumab infusions provided to 225 patients with RRMS between 2006 and 2018, 276 infusion-related adverse events occurred (1.95%) among 60 patients.
There were 11 severe infusion-related adverse events in nine patients (4.0%). All documented severe reactions occurred during the infusion. Among 19 moderate adverse events, 17 occurred during the infusion.
The researchers noted that the majority of patients who experienced severe infusion reactions had detectable antibodies against natalizumab. Such antibodies are associated with a higher risk for infusion-related adverse events.
Patients who did not have any symptoms of a reaction during the infusion had no clinically relevant moderate or severe reactions.
“Thus, the need for postinfusion observation will depend on the patients’ clinical status during the infusion,” they wrote. “Consequently, our data suggest that patients who do not have an infusion-related adverse event while receiving natalizumab treatment do not need to stay in the hospital for an additional observation hour.”
Rapid infusion protocol
In another recent study published in Multiple Sclerosis and Related Disorders in January 2021, researchers in Australia reported on the use of a rapid infusion protocol of natalizumab and ocrelizumab. The protocol was implemented to reduce the amount of time patients are required to spend in clinical settings during the COVID-19 pandemic.
In their analysis of 269 rapid infusions of natalizumab and 100 rapid infusions of ocrelizumab, there were two infusion-related reactions in the natalizumab group and eight in the ocrelizumab group.
All the reactions were mild to moderate, and no discontinuations were required. None of the reactions occurred during the postinfusion observation period.
“In the setting of COVID-19 pandemic, rapid infusion protocols could potentially save hospital resources and limit patient exposure to a high-risk clinical setting while still maintaining ongoing treatment of multiple sclerosis,” the authors wrote.
Under the rapid infusion protocol, patients receive three standard doses for 1 hour followed by 30 minutes of observation. In addition, infusions are reduced to 30 minutes, explained lead author Louise Rath, of clinical neurosciences, Alfred Health, in Melbourne.
“For our cohort of patients, the side effects were minimal,” she said.
“Rapid infusions allowed patients to have option of hospital in-home or office, ensuring work was not at risk by infusion,” she added. “Our governance has been very supportive, and we will be keeping rapid infusion post COVID.”
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACTRIMS 2021
Docs become dog groomers and warehouse workers after COVID-19 work loss
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.







