User login
The Official Newspaper of the American Association for Thoracic Surgery
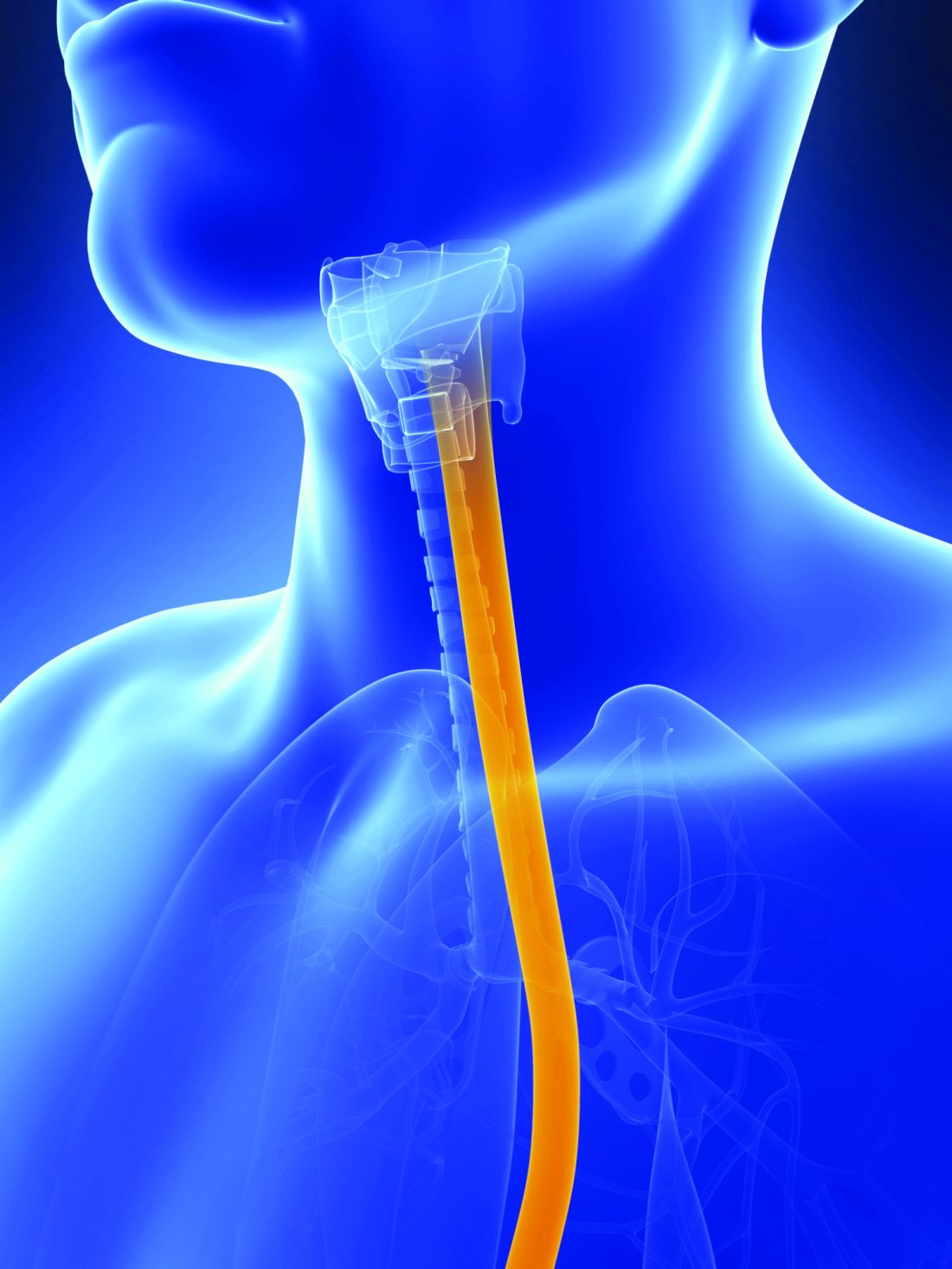
Esophageal cancers: Apples and oranges wrongly lumped together
Genomic analysis suggests that esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) are two separate diseases that should not be combined in clinical trials and may benefit from different treatments, according to the results of a molecular study of 559 esophageal and gastric carcinoma tumors obtained from around the world.
The comprehensive molecular analysis comprised 164 esophageal tumors, 359 gastric adenocarcinomas, and 36 additional adenocarcinomas spanning the gastroesophageal junction.
The results of their analysis “call into question the premise of envisioning esophageal carcinoma as a single entity” and “argue against approaches that combine EAC and ESCC for clinical trials of neoadjuvant, adjuvant, or systemic therapies,” wrote the members of The Cancer Genome Atlas Research Network under the coordination of the National Cancer Institute and the National Human Genome Research Institute project.
The researchers evaluated the 164 esophageal carcinomas using integrated clustering of somatic copy number aberrations, DNA methylation, mRNA, and microRNA expression.
Gene expression analysis showed EACs had increased E-cadherin (CDH1) signaling and upregulation of ARF6 and FOXA pathways, which regulate E-cadherin. In contrast, ESCCs showed upregulation of Wnt, syndecan; p63 pathways, which are essential for squamous epithelial cell differentiation, were also upregulated. “These data suggest the presence of lineage-specific alterations that drive progression in EACs and ESCCs,” according to the researchers.
Somatic genome alterations showed that many of the same genetic pathways were altered in both EAC and ESCC, but the specific genes affected were dissimilar, suggesting distinct pathophysiologies between the two types of cancer. This could signal the need for different treatment approaches and led the researchers to caution against lumping EAC and ESCC in the same clinical trials.
Molecular subtype analysis of the ESCC cancers showed three molecular subtypes: ESCC1 (50 tumors), ESCC2 (36) and ESCC3 (4), distinguished by their mutation types. ESCC1, for example, was characterized by alterations in the NRF2 pathway, mutations in which are associated with poor prognosis and resistance to chemotherapy.
The three subtypes also showed trends for geographic associations, with Vietnamese patients (the only Asian population studied) showing a predominance of ESCC1 (27/41), and all 4 ESCC3 tumors being derived from United States patients.
The researchers also evaluated the molecular association between ESCC and human papillomavirus (HPV), which has been shown to have a pathogenic role in cervical SCC and head and neck (HN)SCC. They found that ESCC mRNA sequencing showed that ESCC-HPV transcript levels were similar to HPV-negative HNSCC tumors, diminishing the likelihood of an etiological role for HPV in ESCC.
In evaluating EACs in comparison to chromosomal instability (CIN) gastric cancers, the researchers found “clear similarity between chromosomal aberrations” in the two cancer types, with a stronger similarity between EAC and CIN gastric cancers than between EAC and ESCC, further differentiating the two esophageal cancers.
“The notable molecular similarity between EACs and CIN gastric cancers provides indirect support for gastric origin of Barrett’s esophagus and EAC and indicates that we may view GEA [gastroesophageal adenocarcinoma] as a singular entity, analogous to colorectal adenocarcinoma,” the authors added.
A notable anatomic gradient showed up in the progression of DNA methylation as seen from proximal to distal GEA-CIN tumors, with the most frequent hypermethylation seen in EACs, compared with gastric CIN cancers, a significant difference.
“These molecular data show that EAC and ESCC are distinct in their molecular characteristics across all platforms tested. ESCC emerges as a disease more reminiscent of other SCCs than of EAC, which itself bears striking resemblance to CIN gastric cancer,” the researchers concluded.
The authors reported that they had no competing financial interests.
This article published in Nature summarizes an integrated genomic analysis of esophageal cancer with careful comparisons to other cancers in the neighborhood (head and neck, lung, and gastric cancer). While clinically apparent to physicians taking care of esophageal cancer throughout the world, these analyses confirm that esophageal squamous cell cancer and esophageal adenocarcinoma are essentially two different diseases with distinct genomic characteristics. This has an important implication in clinical trial design: These pathologies should not be analyzed together, but instead should be studied distinctly.
In addition to the above major conclusion, several other features deserve to be noted. First, esophageal cancer does not seem to be associated with HPV as the HPV transcript levels in these tumors resemble those in HPV-negative head and neck cancers. Second, there are significant differences in the genomic characteristics of esophageal squamous cell cancer depending on geographic location. Third, esophageal adenocarcinoma is most like one particular molecular variant of gastric cancer (chromosomal instability type) and as one moves from the gastric antrum to the esophagus, there is an enrichment of this type of cancer. Such a gradient is found in methylation patterns as well, suggesting a similar cell of origin between gastric and esophageal cancers.
This study brings into focus the overarching theme that cancers may soon be treated based on molecular characteristics rather than anatomic location and clinical trials may have to be grouped based on genetic changes rather than organ systems.
Sai Yendamuri, MD, FACS, is an attending surgeon at the department of thoracic surgery, and director, Thoracic Surgery Research Laboratory, and an associate professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y.
This article published in Nature summarizes an integrated genomic analysis of esophageal cancer with careful comparisons to other cancers in the neighborhood (head and neck, lung, and gastric cancer). While clinically apparent to physicians taking care of esophageal cancer throughout the world, these analyses confirm that esophageal squamous cell cancer and esophageal adenocarcinoma are essentially two different diseases with distinct genomic characteristics. This has an important implication in clinical trial design: These pathologies should not be analyzed together, but instead should be studied distinctly.
In addition to the above major conclusion, several other features deserve to be noted. First, esophageal cancer does not seem to be associated with HPV as the HPV transcript levels in these tumors resemble those in HPV-negative head and neck cancers. Second, there are significant differences in the genomic characteristics of esophageal squamous cell cancer depending on geographic location. Third, esophageal adenocarcinoma is most like one particular molecular variant of gastric cancer (chromosomal instability type) and as one moves from the gastric antrum to the esophagus, there is an enrichment of this type of cancer. Such a gradient is found in methylation patterns as well, suggesting a similar cell of origin between gastric and esophageal cancers.
This study brings into focus the overarching theme that cancers may soon be treated based on molecular characteristics rather than anatomic location and clinical trials may have to be grouped based on genetic changes rather than organ systems.
Sai Yendamuri, MD, FACS, is an attending surgeon at the department of thoracic surgery, and director, Thoracic Surgery Research Laboratory, and an associate professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y.
This article published in Nature summarizes an integrated genomic analysis of esophageal cancer with careful comparisons to other cancers in the neighborhood (head and neck, lung, and gastric cancer). While clinically apparent to physicians taking care of esophageal cancer throughout the world, these analyses confirm that esophageal squamous cell cancer and esophageal adenocarcinoma are essentially two different diseases with distinct genomic characteristics. This has an important implication in clinical trial design: These pathologies should not be analyzed together, but instead should be studied distinctly.
In addition to the above major conclusion, several other features deserve to be noted. First, esophageal cancer does not seem to be associated with HPV as the HPV transcript levels in these tumors resemble those in HPV-negative head and neck cancers. Second, there are significant differences in the genomic characteristics of esophageal squamous cell cancer depending on geographic location. Third, esophageal adenocarcinoma is most like one particular molecular variant of gastric cancer (chromosomal instability type) and as one moves from the gastric antrum to the esophagus, there is an enrichment of this type of cancer. Such a gradient is found in methylation patterns as well, suggesting a similar cell of origin between gastric and esophageal cancers.
This study brings into focus the overarching theme that cancers may soon be treated based on molecular characteristics rather than anatomic location and clinical trials may have to be grouped based on genetic changes rather than organ systems.
Sai Yendamuri, MD, FACS, is an attending surgeon at the department of thoracic surgery, and director, Thoracic Surgery Research Laboratory, and an associate professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y.
Genomic analysis suggests that esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) are two separate diseases that should not be combined in clinical trials and may benefit from different treatments, according to the results of a molecular study of 559 esophageal and gastric carcinoma tumors obtained from around the world.
The comprehensive molecular analysis comprised 164 esophageal tumors, 359 gastric adenocarcinomas, and 36 additional adenocarcinomas spanning the gastroesophageal junction.
The results of their analysis “call into question the premise of envisioning esophageal carcinoma as a single entity” and “argue against approaches that combine EAC and ESCC for clinical trials of neoadjuvant, adjuvant, or systemic therapies,” wrote the members of The Cancer Genome Atlas Research Network under the coordination of the National Cancer Institute and the National Human Genome Research Institute project.
The researchers evaluated the 164 esophageal carcinomas using integrated clustering of somatic copy number aberrations, DNA methylation, mRNA, and microRNA expression.
Gene expression analysis showed EACs had increased E-cadherin (CDH1) signaling and upregulation of ARF6 and FOXA pathways, which regulate E-cadherin. In contrast, ESCCs showed upregulation of Wnt, syndecan; p63 pathways, which are essential for squamous epithelial cell differentiation, were also upregulated. “These data suggest the presence of lineage-specific alterations that drive progression in EACs and ESCCs,” according to the researchers.
Somatic genome alterations showed that many of the same genetic pathways were altered in both EAC and ESCC, but the specific genes affected were dissimilar, suggesting distinct pathophysiologies between the two types of cancer. This could signal the need for different treatment approaches and led the researchers to caution against lumping EAC and ESCC in the same clinical trials.
Molecular subtype analysis of the ESCC cancers showed three molecular subtypes: ESCC1 (50 tumors), ESCC2 (36) and ESCC3 (4), distinguished by their mutation types. ESCC1, for example, was characterized by alterations in the NRF2 pathway, mutations in which are associated with poor prognosis and resistance to chemotherapy.
The three subtypes also showed trends for geographic associations, with Vietnamese patients (the only Asian population studied) showing a predominance of ESCC1 (27/41), and all 4 ESCC3 tumors being derived from United States patients.
The researchers also evaluated the molecular association between ESCC and human papillomavirus (HPV), which has been shown to have a pathogenic role in cervical SCC and head and neck (HN)SCC. They found that ESCC mRNA sequencing showed that ESCC-HPV transcript levels were similar to HPV-negative HNSCC tumors, diminishing the likelihood of an etiological role for HPV in ESCC.
In evaluating EACs in comparison to chromosomal instability (CIN) gastric cancers, the researchers found “clear similarity between chromosomal aberrations” in the two cancer types, with a stronger similarity between EAC and CIN gastric cancers than between EAC and ESCC, further differentiating the two esophageal cancers.
“The notable molecular similarity between EACs and CIN gastric cancers provides indirect support for gastric origin of Barrett’s esophagus and EAC and indicates that we may view GEA [gastroesophageal adenocarcinoma] as a singular entity, analogous to colorectal adenocarcinoma,” the authors added.
A notable anatomic gradient showed up in the progression of DNA methylation as seen from proximal to distal GEA-CIN tumors, with the most frequent hypermethylation seen in EACs, compared with gastric CIN cancers, a significant difference.
“These molecular data show that EAC and ESCC are distinct in their molecular characteristics across all platforms tested. ESCC emerges as a disease more reminiscent of other SCCs than of EAC, which itself bears striking resemblance to CIN gastric cancer,” the researchers concluded.
The authors reported that they had no competing financial interests.
Genomic analysis suggests that esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) are two separate diseases that should not be combined in clinical trials and may benefit from different treatments, according to the results of a molecular study of 559 esophageal and gastric carcinoma tumors obtained from around the world.
The comprehensive molecular analysis comprised 164 esophageal tumors, 359 gastric adenocarcinomas, and 36 additional adenocarcinomas spanning the gastroesophageal junction.
The results of their analysis “call into question the premise of envisioning esophageal carcinoma as a single entity” and “argue against approaches that combine EAC and ESCC for clinical trials of neoadjuvant, adjuvant, or systemic therapies,” wrote the members of The Cancer Genome Atlas Research Network under the coordination of the National Cancer Institute and the National Human Genome Research Institute project.
The researchers evaluated the 164 esophageal carcinomas using integrated clustering of somatic copy number aberrations, DNA methylation, mRNA, and microRNA expression.
Gene expression analysis showed EACs had increased E-cadherin (CDH1) signaling and upregulation of ARF6 and FOXA pathways, which regulate E-cadherin. In contrast, ESCCs showed upregulation of Wnt, syndecan; p63 pathways, which are essential for squamous epithelial cell differentiation, were also upregulated. “These data suggest the presence of lineage-specific alterations that drive progression in EACs and ESCCs,” according to the researchers.
Somatic genome alterations showed that many of the same genetic pathways were altered in both EAC and ESCC, but the specific genes affected were dissimilar, suggesting distinct pathophysiologies between the two types of cancer. This could signal the need for different treatment approaches and led the researchers to caution against lumping EAC and ESCC in the same clinical trials.
Molecular subtype analysis of the ESCC cancers showed three molecular subtypes: ESCC1 (50 tumors), ESCC2 (36) and ESCC3 (4), distinguished by their mutation types. ESCC1, for example, was characterized by alterations in the NRF2 pathway, mutations in which are associated with poor prognosis and resistance to chemotherapy.
The three subtypes also showed trends for geographic associations, with Vietnamese patients (the only Asian population studied) showing a predominance of ESCC1 (27/41), and all 4 ESCC3 tumors being derived from United States patients.
The researchers also evaluated the molecular association between ESCC and human papillomavirus (HPV), which has been shown to have a pathogenic role in cervical SCC and head and neck (HN)SCC. They found that ESCC mRNA sequencing showed that ESCC-HPV transcript levels were similar to HPV-negative HNSCC tumors, diminishing the likelihood of an etiological role for HPV in ESCC.
In evaluating EACs in comparison to chromosomal instability (CIN) gastric cancers, the researchers found “clear similarity between chromosomal aberrations” in the two cancer types, with a stronger similarity between EAC and CIN gastric cancers than between EAC and ESCC, further differentiating the two esophageal cancers.
“The notable molecular similarity between EACs and CIN gastric cancers provides indirect support for gastric origin of Barrett’s esophagus and EAC and indicates that we may view GEA [gastroesophageal adenocarcinoma] as a singular entity, analogous to colorectal adenocarcinoma,” the authors added.
A notable anatomic gradient showed up in the progression of DNA methylation as seen from proximal to distal GEA-CIN tumors, with the most frequent hypermethylation seen in EACs, compared with gastric CIN cancers, a significant difference.
“These molecular data show that EAC and ESCC are distinct in their molecular characteristics across all platforms tested. ESCC emerges as a disease more reminiscent of other SCCs than of EAC, which itself bears striking resemblance to CIN gastric cancer,” the researchers concluded.
The authors reported that they had no competing financial interests.
FROM NATURE
Key clinical point:
Major finding: Molecular analysis showed esophageal squamous cell carcinoma is more like other squamous cell carcinomas than esophageal adenocarcinoma, which itself resembles chromosomal-instability gastric cancer.
Data source: A molecular study of 559 esophageal and gastric carcinoma tumors obtained from around the world.
Disclosures: The authors reported that they had no competing financial interests.
21 Medicare health plans warned to fix provider directory errors
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.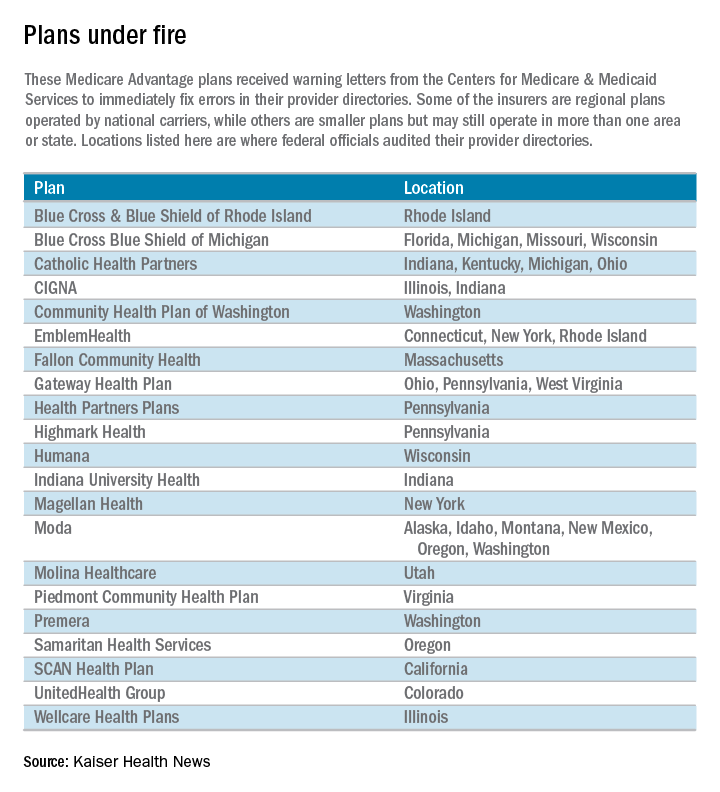
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.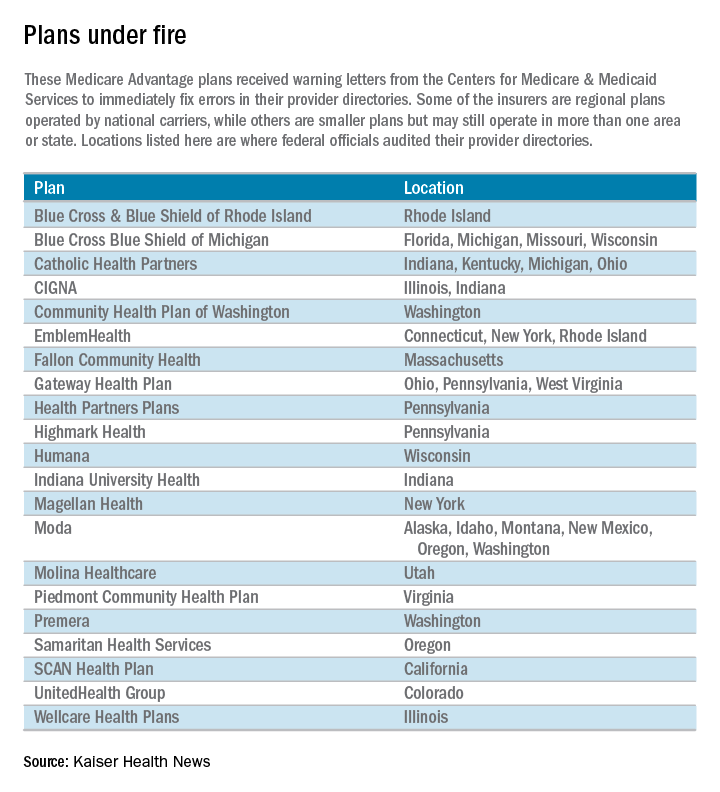
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.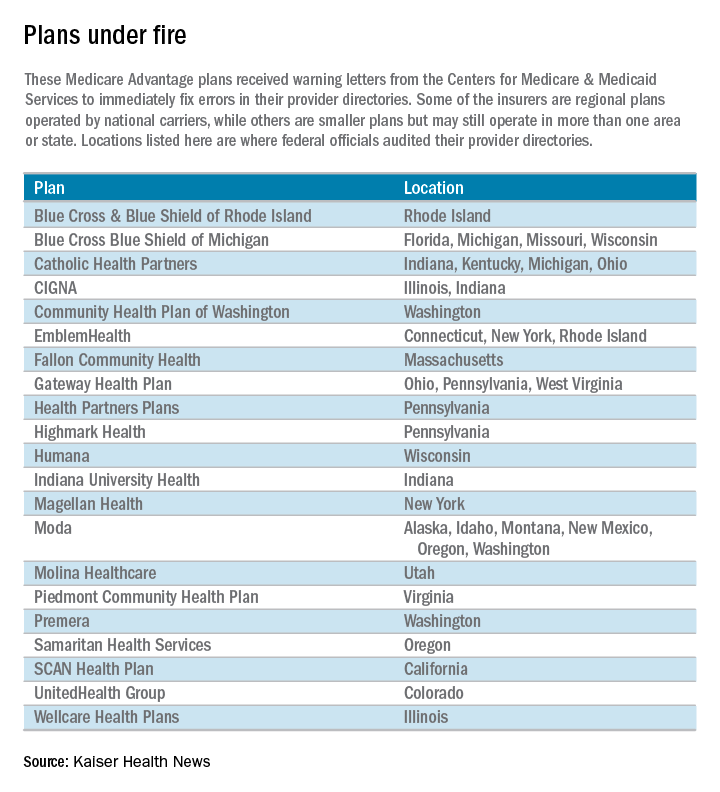
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Ultrashort course antibiotics may be enough in stable VAP
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Key clinical point: Ultrashort antibiotic courses yielded outcomes that were similar to those with longer courses in patients with suspected ventilator-associated pneumonia but minimal and stable ventilator settings.
Major finding: The groups did not significantly differ based on time to extubation alive (hazard ratio, 1.2), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).
Data source: A single-center retrospective observational study of 1,290 patients with suspected ventilator-associated pneumonia.
Disclosures: The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Repeal and replace: House bills offer potential road maps
As Republicans dig in to make good on their promise to repeal the Affordable Care Act, hints at what an eventual replacement may look like can be gleaned from legislation previously introduced in the House of Representatives.
One model could be the Empowering Patients First Act (H.R. 2300), sponsored by Rep. Tom Price (R-Ga.), a retired orthopedic surgeon and President-elect Trump’s nominee to head the Health and Human Services department. That legislation offers up a number of the usual GOP proposals related to health care, including refundable tax credits for low-income individuals buying insurance on the individual market; federal grants for states to provide health coverage through a high-risk pool, a reinsurance pool, or other mechanism to help subsidize the purchase of insurance; allowing individuals to purchase insurance through individual member associations; allowing small business owners to purchase insurance for their families and employees across state lines through their trade associations; and allowing insurance companies to sell coverage across state lines.
Another model can be found in House Republican’s health reform plan, called “A Better Way.”
The plan includes a number of provisions similar to those in Dr. Price’s plan, such as expanding consumer-directed health care options, allowing sale of insurance across state lines, expanding opportunities for pooling, and bringing about medical liability reform.
It also increases health insurance portability, helps to preserve the employer-sponsored insurance market, preserves wellness programs, promotes greater use of health savings accounts, and provides for greater opportunities to contribute and use them.
The Better Way plan maintains a few of the popular aspects of the Affordable Care Act, including a ban on coverage denial for preexisting conditions and the ability to keep adult children on parents’ health insurance up to age 26 years, in certain situations.
In addition, the plan would roll back a premium adjustment for older patients. The ACA mandates that premiums for older individuals could be no more than three times that of a younger enrollee. Prior to the ACA, the GOP plan notes that it was generally a limit of five times that of a younger enrollee, and the GOP vision is to bring that limit back.
“The ill-advised three-to-one policy is leading to artificially higher premiums for millions of Americans, especially younger and healthier patients,” according to the GOP plan.
The plan aims to repeal several ACA provisions including the Independent Payment Advisory Board, the Center for Medicare & Medicaid Innovations, and the ban on physician-owned hospitals. It would also extend value-based insurance design to Medicare Advantage, combine Medicare Parts A & B, and reform to uncompensated care.
President-elect Trump also gave hints as to what might be contained in a health reform plan he is formulating. In a Jan. 14 interview with the Washington Post, Mr. Trump said his plan aims to provide “insurance for all” while requiring drug manufacturers to negotiate with Medicare and Medicaid on pricing.
As Republicans dig in to make good on their promise to repeal the Affordable Care Act, hints at what an eventual replacement may look like can be gleaned from legislation previously introduced in the House of Representatives.
One model could be the Empowering Patients First Act (H.R. 2300), sponsored by Rep. Tom Price (R-Ga.), a retired orthopedic surgeon and President-elect Trump’s nominee to head the Health and Human Services department. That legislation offers up a number of the usual GOP proposals related to health care, including refundable tax credits for low-income individuals buying insurance on the individual market; federal grants for states to provide health coverage through a high-risk pool, a reinsurance pool, or other mechanism to help subsidize the purchase of insurance; allowing individuals to purchase insurance through individual member associations; allowing small business owners to purchase insurance for their families and employees across state lines through their trade associations; and allowing insurance companies to sell coverage across state lines.
Another model can be found in House Republican’s health reform plan, called “A Better Way.”
The plan includes a number of provisions similar to those in Dr. Price’s plan, such as expanding consumer-directed health care options, allowing sale of insurance across state lines, expanding opportunities for pooling, and bringing about medical liability reform.
It also increases health insurance portability, helps to preserve the employer-sponsored insurance market, preserves wellness programs, promotes greater use of health savings accounts, and provides for greater opportunities to contribute and use them.
The Better Way plan maintains a few of the popular aspects of the Affordable Care Act, including a ban on coverage denial for preexisting conditions and the ability to keep adult children on parents’ health insurance up to age 26 years, in certain situations.
In addition, the plan would roll back a premium adjustment for older patients. The ACA mandates that premiums for older individuals could be no more than three times that of a younger enrollee. Prior to the ACA, the GOP plan notes that it was generally a limit of five times that of a younger enrollee, and the GOP vision is to bring that limit back.
“The ill-advised three-to-one policy is leading to artificially higher premiums for millions of Americans, especially younger and healthier patients,” according to the GOP plan.
The plan aims to repeal several ACA provisions including the Independent Payment Advisory Board, the Center for Medicare & Medicaid Innovations, and the ban on physician-owned hospitals. It would also extend value-based insurance design to Medicare Advantage, combine Medicare Parts A & B, and reform to uncompensated care.
President-elect Trump also gave hints as to what might be contained in a health reform plan he is formulating. In a Jan. 14 interview with the Washington Post, Mr. Trump said his plan aims to provide “insurance for all” while requiring drug manufacturers to negotiate with Medicare and Medicaid on pricing.
As Republicans dig in to make good on their promise to repeal the Affordable Care Act, hints at what an eventual replacement may look like can be gleaned from legislation previously introduced in the House of Representatives.
One model could be the Empowering Patients First Act (H.R. 2300), sponsored by Rep. Tom Price (R-Ga.), a retired orthopedic surgeon and President-elect Trump’s nominee to head the Health and Human Services department. That legislation offers up a number of the usual GOP proposals related to health care, including refundable tax credits for low-income individuals buying insurance on the individual market; federal grants for states to provide health coverage through a high-risk pool, a reinsurance pool, or other mechanism to help subsidize the purchase of insurance; allowing individuals to purchase insurance through individual member associations; allowing small business owners to purchase insurance for their families and employees across state lines through their trade associations; and allowing insurance companies to sell coverage across state lines.
Another model can be found in House Republican’s health reform plan, called “A Better Way.”
The plan includes a number of provisions similar to those in Dr. Price’s plan, such as expanding consumer-directed health care options, allowing sale of insurance across state lines, expanding opportunities for pooling, and bringing about medical liability reform.
It also increases health insurance portability, helps to preserve the employer-sponsored insurance market, preserves wellness programs, promotes greater use of health savings accounts, and provides for greater opportunities to contribute and use them.
The Better Way plan maintains a few of the popular aspects of the Affordable Care Act, including a ban on coverage denial for preexisting conditions and the ability to keep adult children on parents’ health insurance up to age 26 years, in certain situations.
In addition, the plan would roll back a premium adjustment for older patients. The ACA mandates that premiums for older individuals could be no more than three times that of a younger enrollee. Prior to the ACA, the GOP plan notes that it was generally a limit of five times that of a younger enrollee, and the GOP vision is to bring that limit back.
“The ill-advised three-to-one policy is leading to artificially higher premiums for millions of Americans, especially younger and healthier patients,” according to the GOP plan.
The plan aims to repeal several ACA provisions including the Independent Payment Advisory Board, the Center for Medicare & Medicaid Innovations, and the ban on physician-owned hospitals. It would also extend value-based insurance design to Medicare Advantage, combine Medicare Parts A & B, and reform to uncompensated care.
President-elect Trump also gave hints as to what might be contained in a health reform plan he is formulating. In a Jan. 14 interview with the Washington Post, Mr. Trump said his plan aims to provide “insurance for all” while requiring drug manufacturers to negotiate with Medicare and Medicaid on pricing.
Dr. Price light on ACA replacement details at Senate hearing
WASHINGTON – Rep. Tom Price (R-Ga.) was light on specifics as to what he would favor in ACA replacement efforts, instead focused on broad goals for reform at a courtesy hearing Jan. 18 before the Senate Committee on Health, Education, Labor & Pensions.
Democratic senators on committee sought firm commitments on many issues – maintaining insurance coverage, women’s access to reproductive health care, coverage of mental health/substance use treatment, drug pricing, and reducing racial disparities – from Dr. Price, President-elect Trump’s nominee to lead the Health & Human Service department and a retired orthopedic surgeon. They also challenged Dr. Price on financial conflicts of interest related to legislation he supported.
Dr. Price consistently avoided committing to specific policies, but insisted that “individuals [should] have the opportunity to gain access to the kind of coverage they desire.”
Senators specifically queried Dr. Price as to whether he would commit to maintaining copay-free insurance coverage of all 18 forms of birth control for women approved by the Food and Drug Administration, as mandated by the ACA.
“Every single American ought to have access to the coverage and care that they desire,” Dr. Price responded.
Similarly, regarding coverage of mental health and substance use disorders, Dr. Price called it an “absolutely an imperative” that “every single American” have access to the care for these health issues.
When pressed by Sen. Maggie Hassan (D-N.H.) to commit to ensuring that there would be no cuts to Medicaid funding for mental health care/substance use disorders, Dr. Price noted that “we will address that need.”
Senators also queried Dr. Price’s commitment to maintaining the HHS Office of Minority Health. Sen. Murray offered a number of statistics demonstrating how minority women in particular have benefited with coverage and access to health care under the ACA.
Dr. Price stopped well short of committing to keeping the office, but instead returned to his desire to pursue policies that ensure “every American has access to the care that they desire.”
Dr. Price did not commit to upholding Mr. Trump’s campaign promise that no dollars would be cut from Medicare; instead, he argued that money spent is the wrong metric to measure health care quality.
Regarding the Center for Medicare & Medicaid Innovation, Dr. Price said that the center has “great promise,” but he “opposed the mandatory nature” of some of its programs, highlighting the comprehensive joint replacement bundle, which he said limits how orthopedic surgeons practice.
Senators also paid special attention to Dr. Price’s potential conflicts of interest. Several pointed to medical industry stock purchases that occurred around the time he introduced legislation that could benefit these companies, including a device manufacturer that would potentially benefit from Dr. Price’s challenging of the comprehensive joint replacement bundle and of pharmaceutical companies that might see benefit from the drug provisions in the 21st Century Cures Act.
He vehemently denied any wrongdoing, noting that he regularly and consistently disclosed all security holdings as required by congressional ethics rules and said he did nothing different from what many people in Congress currently do.
Despite his assurances that his ethics have not been compromised, Sen. Murray called for an ethics probe to address any potential conflicts of interest before his confirmation vote.
In closing the hearing, Chairman Lamar Alexander (R-Tenn.) reiterated his plan for a phased timeline for ACA repeal and replacement, to be completed so that no one would lose coverage. He suggested that while legislative action could be swift, implementation could span years to minimize impact on insurance coverage and access to health care.
Dr. Price’s official confirmation hearing before the Senate Finance Committee is scheduled for Jan. 24.
WASHINGTON – Rep. Tom Price (R-Ga.) was light on specifics as to what he would favor in ACA replacement efforts, instead focused on broad goals for reform at a courtesy hearing Jan. 18 before the Senate Committee on Health, Education, Labor & Pensions.
Democratic senators on committee sought firm commitments on many issues – maintaining insurance coverage, women’s access to reproductive health care, coverage of mental health/substance use treatment, drug pricing, and reducing racial disparities – from Dr. Price, President-elect Trump’s nominee to lead the Health & Human Service department and a retired orthopedic surgeon. They also challenged Dr. Price on financial conflicts of interest related to legislation he supported.
Dr. Price consistently avoided committing to specific policies, but insisted that “individuals [should] have the opportunity to gain access to the kind of coverage they desire.”
Senators specifically queried Dr. Price as to whether he would commit to maintaining copay-free insurance coverage of all 18 forms of birth control for women approved by the Food and Drug Administration, as mandated by the ACA.
“Every single American ought to have access to the coverage and care that they desire,” Dr. Price responded.
Similarly, regarding coverage of mental health and substance use disorders, Dr. Price called it an “absolutely an imperative” that “every single American” have access to the care for these health issues.
When pressed by Sen. Maggie Hassan (D-N.H.) to commit to ensuring that there would be no cuts to Medicaid funding for mental health care/substance use disorders, Dr. Price noted that “we will address that need.”
Senators also queried Dr. Price’s commitment to maintaining the HHS Office of Minority Health. Sen. Murray offered a number of statistics demonstrating how minority women in particular have benefited with coverage and access to health care under the ACA.
Dr. Price stopped well short of committing to keeping the office, but instead returned to his desire to pursue policies that ensure “every American has access to the care that they desire.”
Dr. Price did not commit to upholding Mr. Trump’s campaign promise that no dollars would be cut from Medicare; instead, he argued that money spent is the wrong metric to measure health care quality.
Regarding the Center for Medicare & Medicaid Innovation, Dr. Price said that the center has “great promise,” but he “opposed the mandatory nature” of some of its programs, highlighting the comprehensive joint replacement bundle, which he said limits how orthopedic surgeons practice.
Senators also paid special attention to Dr. Price’s potential conflicts of interest. Several pointed to medical industry stock purchases that occurred around the time he introduced legislation that could benefit these companies, including a device manufacturer that would potentially benefit from Dr. Price’s challenging of the comprehensive joint replacement bundle and of pharmaceutical companies that might see benefit from the drug provisions in the 21st Century Cures Act.
He vehemently denied any wrongdoing, noting that he regularly and consistently disclosed all security holdings as required by congressional ethics rules and said he did nothing different from what many people in Congress currently do.
Despite his assurances that his ethics have not been compromised, Sen. Murray called for an ethics probe to address any potential conflicts of interest before his confirmation vote.
In closing the hearing, Chairman Lamar Alexander (R-Tenn.) reiterated his plan for a phased timeline for ACA repeal and replacement, to be completed so that no one would lose coverage. He suggested that while legislative action could be swift, implementation could span years to minimize impact on insurance coverage and access to health care.
Dr. Price’s official confirmation hearing before the Senate Finance Committee is scheduled for Jan. 24.
WASHINGTON – Rep. Tom Price (R-Ga.) was light on specifics as to what he would favor in ACA replacement efforts, instead focused on broad goals for reform at a courtesy hearing Jan. 18 before the Senate Committee on Health, Education, Labor & Pensions.
Democratic senators on committee sought firm commitments on many issues – maintaining insurance coverage, women’s access to reproductive health care, coverage of mental health/substance use treatment, drug pricing, and reducing racial disparities – from Dr. Price, President-elect Trump’s nominee to lead the Health & Human Service department and a retired orthopedic surgeon. They also challenged Dr. Price on financial conflicts of interest related to legislation he supported.
Dr. Price consistently avoided committing to specific policies, but insisted that “individuals [should] have the opportunity to gain access to the kind of coverage they desire.”
Senators specifically queried Dr. Price as to whether he would commit to maintaining copay-free insurance coverage of all 18 forms of birth control for women approved by the Food and Drug Administration, as mandated by the ACA.
“Every single American ought to have access to the coverage and care that they desire,” Dr. Price responded.
Similarly, regarding coverage of mental health and substance use disorders, Dr. Price called it an “absolutely an imperative” that “every single American” have access to the care for these health issues.
When pressed by Sen. Maggie Hassan (D-N.H.) to commit to ensuring that there would be no cuts to Medicaid funding for mental health care/substance use disorders, Dr. Price noted that “we will address that need.”
Senators also queried Dr. Price’s commitment to maintaining the HHS Office of Minority Health. Sen. Murray offered a number of statistics demonstrating how minority women in particular have benefited with coverage and access to health care under the ACA.
Dr. Price stopped well short of committing to keeping the office, but instead returned to his desire to pursue policies that ensure “every American has access to the care that they desire.”
Dr. Price did not commit to upholding Mr. Trump’s campaign promise that no dollars would be cut from Medicare; instead, he argued that money spent is the wrong metric to measure health care quality.
Regarding the Center for Medicare & Medicaid Innovation, Dr. Price said that the center has “great promise,” but he “opposed the mandatory nature” of some of its programs, highlighting the comprehensive joint replacement bundle, which he said limits how orthopedic surgeons practice.
Senators also paid special attention to Dr. Price’s potential conflicts of interest. Several pointed to medical industry stock purchases that occurred around the time he introduced legislation that could benefit these companies, including a device manufacturer that would potentially benefit from Dr. Price’s challenging of the comprehensive joint replacement bundle and of pharmaceutical companies that might see benefit from the drug provisions in the 21st Century Cures Act.
He vehemently denied any wrongdoing, noting that he regularly and consistently disclosed all security holdings as required by congressional ethics rules and said he did nothing different from what many people in Congress currently do.
Despite his assurances that his ethics have not been compromised, Sen. Murray called for an ethics probe to address any potential conflicts of interest before his confirmation vote.
In closing the hearing, Chairman Lamar Alexander (R-Tenn.) reiterated his plan for a phased timeline for ACA repeal and replacement, to be completed so that no one would lose coverage. He suggested that while legislative action could be swift, implementation could span years to minimize impact on insurance coverage and access to health care.
Dr. Price’s official confirmation hearing before the Senate Finance Committee is scheduled for Jan. 24.
Cancer risk six times higher in children with congenital heart defects
NEW ORLEANS – Children with congenital heart defects have a five- to sixfold increased risk of developing pediatric cancer, Matthew Oster, MD, reported at the American Heart Association scientific sessions.
“The absolute risk is small, but it’s still a five- to sixfold risk compared to the general pediatric population, and it does warrant monitoring and a high index of suspicion in our children with congenital heart defects,” said Dr. Oster of Children’s Healthcare of Atlanta.
The increased cancer risk in adults with congenital heart defects has recently been the focus of research attention. However, little is known about the risk of cancer during the childhood of patients with congenital heart defects.
This was the impetus for Dr. Oster’s nationwide retrospective study of 6.1 million children and adolescents continuously enrolled in private, employer-sponsored health insurance plans during 2009-2015. The data came from the Truven Health MarketScan administrative database.
Children with Down syndrome were excluded from the study because their condition is known to be associated with increased rates of both congenital heart defects and pediatric cancers.
Among 88,493 individuals under age 18 with a diagnosed congenital heart defect, the incidence of any neoplasm diagnosed at least 30 days after diagnosis of the heart defect was 3.91/1,000, compared with 0.79/1,000 in more than 6 million children and adolescents without congenital heart disease.
Thus, children with a congenital heart defect were at a 4.9-fold increased risk for developing a childhood cancer. The risk for bone tumors was 11.2-fold greater than in the general pediatric population, and their neuroblastoma risk was 9.8-fold greater. Their risks of lymphoma and leukemia were increased 5.2- and 2.8-fold, respectively. Of note, they had no increased risk of brain tumors.
To confirm their results, Dr. Oster and his coinvestigators also conducted a sensitivity analysis limited to the 55,079 children and adolescents with at least two outpatient or one inpatient ICD-9 diagnostic code for congenital heart disease. Here the incidence of childhood malignancies was 5.1/1,000 patients, for an overall 6.4-fold increased relative risk.
“Bedside-to-bench work is now needed to determine potential mechanisms,” he said. “We believe the increased risk is related more to a common genetic pathway than to an exposure or treatment pathway because it occurs so early. But there may be some impact of exposures or treatment as well. We think that radiation exposure is more of a longer-term risk.”
He and his coinvestigators next plan to look at the impact on pediatric cancer risk of specific types of congenital heart defects.
Dr. Oster reported having no financial conflicts of interest regarding this study, which received Centers for Disease Control and Prevention funding.
NEW ORLEANS – Children with congenital heart defects have a five- to sixfold increased risk of developing pediatric cancer, Matthew Oster, MD, reported at the American Heart Association scientific sessions.
“The absolute risk is small, but it’s still a five- to sixfold risk compared to the general pediatric population, and it does warrant monitoring and a high index of suspicion in our children with congenital heart defects,” said Dr. Oster of Children’s Healthcare of Atlanta.
The increased cancer risk in adults with congenital heart defects has recently been the focus of research attention. However, little is known about the risk of cancer during the childhood of patients with congenital heart defects.
This was the impetus for Dr. Oster’s nationwide retrospective study of 6.1 million children and adolescents continuously enrolled in private, employer-sponsored health insurance plans during 2009-2015. The data came from the Truven Health MarketScan administrative database.
Children with Down syndrome were excluded from the study because their condition is known to be associated with increased rates of both congenital heart defects and pediatric cancers.
Among 88,493 individuals under age 18 with a diagnosed congenital heart defect, the incidence of any neoplasm diagnosed at least 30 days after diagnosis of the heart defect was 3.91/1,000, compared with 0.79/1,000 in more than 6 million children and adolescents without congenital heart disease.
Thus, children with a congenital heart defect were at a 4.9-fold increased risk for developing a childhood cancer. The risk for bone tumors was 11.2-fold greater than in the general pediatric population, and their neuroblastoma risk was 9.8-fold greater. Their risks of lymphoma and leukemia were increased 5.2- and 2.8-fold, respectively. Of note, they had no increased risk of brain tumors.
To confirm their results, Dr. Oster and his coinvestigators also conducted a sensitivity analysis limited to the 55,079 children and adolescents with at least two outpatient or one inpatient ICD-9 diagnostic code for congenital heart disease. Here the incidence of childhood malignancies was 5.1/1,000 patients, for an overall 6.4-fold increased relative risk.
“Bedside-to-bench work is now needed to determine potential mechanisms,” he said. “We believe the increased risk is related more to a common genetic pathway than to an exposure or treatment pathway because it occurs so early. But there may be some impact of exposures or treatment as well. We think that radiation exposure is more of a longer-term risk.”
He and his coinvestigators next plan to look at the impact on pediatric cancer risk of specific types of congenital heart defects.
Dr. Oster reported having no financial conflicts of interest regarding this study, which received Centers for Disease Control and Prevention funding.
NEW ORLEANS – Children with congenital heart defects have a five- to sixfold increased risk of developing pediatric cancer, Matthew Oster, MD, reported at the American Heart Association scientific sessions.
“The absolute risk is small, but it’s still a five- to sixfold risk compared to the general pediatric population, and it does warrant monitoring and a high index of suspicion in our children with congenital heart defects,” said Dr. Oster of Children’s Healthcare of Atlanta.
The increased cancer risk in adults with congenital heart defects has recently been the focus of research attention. However, little is known about the risk of cancer during the childhood of patients with congenital heart defects.
This was the impetus for Dr. Oster’s nationwide retrospective study of 6.1 million children and adolescents continuously enrolled in private, employer-sponsored health insurance plans during 2009-2015. The data came from the Truven Health MarketScan administrative database.
Children with Down syndrome were excluded from the study because their condition is known to be associated with increased rates of both congenital heart defects and pediatric cancers.
Among 88,493 individuals under age 18 with a diagnosed congenital heart defect, the incidence of any neoplasm diagnosed at least 30 days after diagnosis of the heart defect was 3.91/1,000, compared with 0.79/1,000 in more than 6 million children and adolescents without congenital heart disease.
Thus, children with a congenital heart defect were at a 4.9-fold increased risk for developing a childhood cancer. The risk for bone tumors was 11.2-fold greater than in the general pediatric population, and their neuroblastoma risk was 9.8-fold greater. Their risks of lymphoma and leukemia were increased 5.2- and 2.8-fold, respectively. Of note, they had no increased risk of brain tumors.
To confirm their results, Dr. Oster and his coinvestigators also conducted a sensitivity analysis limited to the 55,079 children and adolescents with at least two outpatient or one inpatient ICD-9 diagnostic code for congenital heart disease. Here the incidence of childhood malignancies was 5.1/1,000 patients, for an overall 6.4-fold increased relative risk.
“Bedside-to-bench work is now needed to determine potential mechanisms,” he said. “We believe the increased risk is related more to a common genetic pathway than to an exposure or treatment pathway because it occurs so early. But there may be some impact of exposures or treatment as well. We think that radiation exposure is more of a longer-term risk.”
He and his coinvestigators next plan to look at the impact on pediatric cancer risk of specific types of congenital heart defects.
Dr. Oster reported having no financial conflicts of interest regarding this study, which received Centers for Disease Control and Prevention funding.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Children with congenital heart defects are at a roughly sixfold increased risk of developing a pediatric cancer.
Data source: A retrospective analysis of administrative health insurance plan data on 6.1 million U.S. subjects under age 18 years, more than 88,000 of whom had congenital heart defects.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study, which received Centers for Disease Control and Prevention funding.
Burnout: Time to stop blaming the victims
Most surgeons today are familiar with professional burnout – in their colleagues, in surgical trainees, and perhaps, in themselves. But the understanding of burnout is evolving. The discussion is moving away from blaming physicians for their poor coping skills toward identifying the structural and organizational roots of burnout.
Burnout is a syndrome cause by work-related stress that features emotional exhaustion, depersonalization, and a decreased sense of personal accomplishment. A recent study of nearly 7,000 physicians using the Maslach Burnout Inventory found that 54.4% of those surveyed reported at least one symptom of burnout (Mayo Clin Proc. 2015 Dec;90[12]:1600-19). Other studies have found similar rates of burnout in the surgical specialties such as orthopedic, oncologic, cardiothoracic, and plastic surgery (JAMA Surg. 2014 Sep;149:948-53; Ann Surg Oncol 2011 May;18:1229-35; Internat J Cardiol. 2015 Jan 20;179:7-72; Aesthet Surg J. 2016 Sep 27. E-pub ahead of print).
A new paradigm of burnout
The paradigm of burnout as a personal issue that can be managed by individual coping strategies is giving way to an understanding that the structural roots of burnout require the shared responsibility of individuals and their work organizations to solve the problem. A revised approach has emerged: Physician burnout as a symptom not of personal failure to cope, but of institutional failure to adapt to new circumstances in the health care milieu. The growing number of physicians employed in large group practices and medical centers has come with a whole array of management problems that are only beginning to be recognized, and burnout may be one of the most challenging.
Tait D. Shanafelt, MD, of the Mayo Foundation for Medical Education and Research, and John H. Noseworthy, MD, president and CEO of the Mayo Clinic, both in Rochester, Minn., have partnered to distill years of study and practice on the issue of burnout to a set of organizational strategies to tackle the problem and describe the Mayo Clinic experience. The study, “Executive Leadership and Physician Well-Being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout” (Mayo Clin Proc. 2016 Nov 18. doi. org/10.1016/j.mayocp.2016.10.004) reverses the conventional “blame the victim” approach and identifies instead institutional responsibility to address burnout.
“Increasing evidence over the last 10 years demonstrating links to quality of care, productivity, and turnover have raised appreciation … by organizations that they have a substantial stake in this issue and that they control many of the factors that contribute to this problem,” said Dr. Shanafelt in an interview.
Unintended consequences of the individual solution
The focus on individual responsibility can have unintended consequences. A physician suffering from burnout can take action by leaving his or her job or cutting back. Staff turnover, a phenomenon closely tied to burnout, is costly and damaging to productivity and patient care (Physician Leadersh J. 2015 May-Jun;2[3]:22-5); Health Care Manage Rev. 2004;29[1]2-7). These personal strategies may help individuals cope but can end up harming the institution and the work life of other staff members. Physicians experiencing burnout in their own lives can trigger the same condition in their colleagues.
The Mayo paper by Dr. Shanafelt and Dr. Noseworthy states, “Mistakenly, most hospitals, medical centers, and practice groups operate under the framework that burnout and professional satisfaction are solely the responsibility of the individual physician. This frequently results in organizations pursuing a narrow list of ‘solutions’ that are unlikely to result in meaningful progress (e.g., stress management workshops and individual training in mindfulness/resilience). Such strategies neglect the organizational factors that are the primary drivers of physician burnout and are correctly viewed with skepticism by physicians as an insincere effort by the organization to address the problem.”
Organizational strategies to reduce burnout
Dr. Shanafelt and Dr. Noseworthy developed a list of nine organizational strategies that have been shown to reduce burnout among doctors. A critical piece of this approach is the accumulated evidence of the financial burden of burnout among physicians in health care institutions. The approach is based on an informed leadership that recognizes the costs of inaction, without which a systemic solution is unlikely to be achieved.
1. Naming the issue and assessing the problem
Acknowledgment of burnout as an institutional problem and meaningful measurement of physician well-being are the initial steps in tackling the problem. This requires a sincere commitment at the highest level of management to listen and to recognize what staff physicians are saying. “At Mayo Clinic, we have incorporated town halls, radio broadcasts, letters, and video interviews along with face-to-face meetings involving clinical divisions, work units, and small groups as formats or [by using] the CEO to reach the staff.” Assessing physician well-being and quality of work life using one or more of the many available tools has to be an ongoing “a barometer of organization health,” and not just a one-off, crisis management activity.
2. Harnessing the power of leadership
Studies have found that management behaviors and strategies of supervisors are key components of physician well-being. The bottom line is that physician supervisors must accept a share of responsibility for burnout in those they manage. Leaders can be chosen on the basis of their ability to listen, engage, develop, and lead, and but they can also be trained to improve. In addition, leaders should be regularly assessed by those whom they lead. Dr. Shanafelt and Dr. Noseworthy argue that a crucial element of successful leadership involves recognizing unique interests and talents of individual physicians whom they manage and facilitating professional development so that each staff member spends about 20% of work time engaged in activities that he or she finds most meaningful.
3. Developing targeted interventions
Just as all politics is local, the study suggests that many sources of burnout are local as well. For example, although a high clerical burden on physicians may be a universal driver of burnout, it manifests differently in each institutional setting. The key here is to dig into the specific structural driver at the unit or ward level, engage physicians in analysis and problem-solving, and implement a plan to address the problem.
Dr. Shanafelt noted, “We organize the drivers of engagement and burnout around seven dimensions: workload, efficiency, flexibility/control, community at work, organizational culture and values, work-life integration, and meaning in work. Each of these dimensions has organizational and individual components. Work units should begin by identifying which one or two dimensions are the biggest challenges for the group and then begin a stepwise process to address them.”
4. Cultivating community at work
Peer support, a long-standing source of strength among surgeons and other physicians, unintentionally has been eroded in many modern medical institutions. There is ample evidence that this loss of collegiality is tied to burnout. “These interactions have been an unintended casualty of increasing productivity expectations, documentation requirements, and clerical burden. [Many organizations have eliminated] formal spaces for physicians to interact (e.g., physicians’ lounge or dining room) without recognizing the important role that this dedicated space played in fostering interpersonal connections among physicians.” The Mayo Clinic and other institutions are reversing this trend by creating dedicated physician rooms for breaks, snacks, and a venue for peer interaction and camaraderie.
5. Rethinking rewards and incentives
Compensation is now commonly linked to productivity in many health care organizations, but this approach has some profound drawbacks: It can lead to physician burnout. Incentive structures based on patient satisfaction and quality metrics can have similar unintended consequences. All these incentive structures can combine to drive physicians to overwork. “Physicians may be particularly vulnerable to overwork due to high levels of education debt, their desire to ‘do everything for their patients,’ unhealthy role modeling by colleagues, and normalization of extreme work hours during the training process.” The investigators do not claim to have the ultimate answer to the problem of incentives that create unhealthy work patterns, but they argue that it is critical for leaders to recognize the potential unintended consequences of the productivity reward/incentive model and consider strategies to prevent overwork leading to burnout.
6. Aligning values and strengthening culture
The investigators also describe Mayo’s efforts to pursue self-appraisal of alignment of mission, values, and culture. They also describe the regular use of an all-staff survey, which has on occasion yielded candid feedback that, while not always flattering, has been the basis of a profound institutional rethink. The willingness of leadership to be receptive to hard truths from physicians is the foundation of institutional learning about burnout prevention and encourages engagement of the staff.
7. Promoting flexibility and work-life integration
Allowing employees greater flexibility in how and when they work is a management strategy that is gaining ground in many industries. Increasing part-time positions and expanding options for the work day have both been found to help prevent burnout and also help physicians recover from burnout. In addition, “institutions should also comprehensively examine the structure of their vacation benefits, coverage for life events (e.g., birth of a child, illness/death in family), approach to scheduling, and strategy for coverage of nights and weekends. Compensation practices that disincentivize using vacation time are shortsighted and should be eliminated.”
8. Providing resources to promote resilience and self-care
The solutions to burnout have been aimed at the individual and involve stress-reduction training and other personal management strategies. A metastudy of the interventions mentions psychoeducation, counseling, wellness management, interpersonal communication, and mindfulness meditation (J Nerv Ment Dis. 2014 May;202:353-9). But without concomitant structural reform, these individual solutions can backfire. “When individually focused offerings are not coupled with sincere efforts to address the system-based issues contributing to burnout, this approach is typically met with skepticism and resistance by physicians (‘They are implying I am the problem’). In this context, the response to well-intentioned ‘resilience training’ is frequently a cynical one (‘You only want to make me more resilient so you can further increase my workload’).”
9. Funding organizational research
Organizational science is a well-developed field of study. But cutting-edge management models such as the learning organization, participatory management, and collaborative action planning have been slow in coming to health care institutions. Dr. Shanafelt and Dr. Noseworthy argue that “vanguard institutions” such as the Mayo Clinic (which began its Program on Physician Well-Being in 2008), Stanford (Calif.) University, and other innovative institutions have the responsibility of developing evidence-based strategies to combat burnout that smaller institutions can implement.
Burnout among physicians is now on the radar of leadership in many health care institutions. Evidence on the cost and consequences is accumulating, and it becoming increasingly difficult to ignore what is happening to many physicians. Dr. Shanafelt projected an increasing need for operational solutions at the organizational level to address the problem. He said, “We need evidence to guide organizations to implement changes that truly make a difference, not well-intentioned but ineffective programs. Now that organizations recognize the strong business case, they are ready to invest resources to address this issue but they need to know it is money well spent and that there is an evidence-base to justify the investment.”
Most surgeons today are familiar with professional burnout – in their colleagues, in surgical trainees, and perhaps, in themselves. But the understanding of burnout is evolving. The discussion is moving away from blaming physicians for their poor coping skills toward identifying the structural and organizational roots of burnout.
Burnout is a syndrome cause by work-related stress that features emotional exhaustion, depersonalization, and a decreased sense of personal accomplishment. A recent study of nearly 7,000 physicians using the Maslach Burnout Inventory found that 54.4% of those surveyed reported at least one symptom of burnout (Mayo Clin Proc. 2015 Dec;90[12]:1600-19). Other studies have found similar rates of burnout in the surgical specialties such as orthopedic, oncologic, cardiothoracic, and plastic surgery (JAMA Surg. 2014 Sep;149:948-53; Ann Surg Oncol 2011 May;18:1229-35; Internat J Cardiol. 2015 Jan 20;179:7-72; Aesthet Surg J. 2016 Sep 27. E-pub ahead of print).
A new paradigm of burnout
The paradigm of burnout as a personal issue that can be managed by individual coping strategies is giving way to an understanding that the structural roots of burnout require the shared responsibility of individuals and their work organizations to solve the problem. A revised approach has emerged: Physician burnout as a symptom not of personal failure to cope, but of institutional failure to adapt to new circumstances in the health care milieu. The growing number of physicians employed in large group practices and medical centers has come with a whole array of management problems that are only beginning to be recognized, and burnout may be one of the most challenging.
Tait D. Shanafelt, MD, of the Mayo Foundation for Medical Education and Research, and John H. Noseworthy, MD, president and CEO of the Mayo Clinic, both in Rochester, Minn., have partnered to distill years of study and practice on the issue of burnout to a set of organizational strategies to tackle the problem and describe the Mayo Clinic experience. The study, “Executive Leadership and Physician Well-Being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout” (Mayo Clin Proc. 2016 Nov 18. doi. org/10.1016/j.mayocp.2016.10.004) reverses the conventional “blame the victim” approach and identifies instead institutional responsibility to address burnout.
“Increasing evidence over the last 10 years demonstrating links to quality of care, productivity, and turnover have raised appreciation … by organizations that they have a substantial stake in this issue and that they control many of the factors that contribute to this problem,” said Dr. Shanafelt in an interview.
Unintended consequences of the individual solution
The focus on individual responsibility can have unintended consequences. A physician suffering from burnout can take action by leaving his or her job or cutting back. Staff turnover, a phenomenon closely tied to burnout, is costly and damaging to productivity and patient care (Physician Leadersh J. 2015 May-Jun;2[3]:22-5); Health Care Manage Rev. 2004;29[1]2-7). These personal strategies may help individuals cope but can end up harming the institution and the work life of other staff members. Physicians experiencing burnout in their own lives can trigger the same condition in their colleagues.
The Mayo paper by Dr. Shanafelt and Dr. Noseworthy states, “Mistakenly, most hospitals, medical centers, and practice groups operate under the framework that burnout and professional satisfaction are solely the responsibility of the individual physician. This frequently results in organizations pursuing a narrow list of ‘solutions’ that are unlikely to result in meaningful progress (e.g., stress management workshops and individual training in mindfulness/resilience). Such strategies neglect the organizational factors that are the primary drivers of physician burnout and are correctly viewed with skepticism by physicians as an insincere effort by the organization to address the problem.”
Organizational strategies to reduce burnout
Dr. Shanafelt and Dr. Noseworthy developed a list of nine organizational strategies that have been shown to reduce burnout among doctors. A critical piece of this approach is the accumulated evidence of the financial burden of burnout among physicians in health care institutions. The approach is based on an informed leadership that recognizes the costs of inaction, without which a systemic solution is unlikely to be achieved.
1. Naming the issue and assessing the problem
Acknowledgment of burnout as an institutional problem and meaningful measurement of physician well-being are the initial steps in tackling the problem. This requires a sincere commitment at the highest level of management to listen and to recognize what staff physicians are saying. “At Mayo Clinic, we have incorporated town halls, radio broadcasts, letters, and video interviews along with face-to-face meetings involving clinical divisions, work units, and small groups as formats or [by using] the CEO to reach the staff.” Assessing physician well-being and quality of work life using one or more of the many available tools has to be an ongoing “a barometer of organization health,” and not just a one-off, crisis management activity.
2. Harnessing the power of leadership
Studies have found that management behaviors and strategies of supervisors are key components of physician well-being. The bottom line is that physician supervisors must accept a share of responsibility for burnout in those they manage. Leaders can be chosen on the basis of their ability to listen, engage, develop, and lead, and but they can also be trained to improve. In addition, leaders should be regularly assessed by those whom they lead. Dr. Shanafelt and Dr. Noseworthy argue that a crucial element of successful leadership involves recognizing unique interests and talents of individual physicians whom they manage and facilitating professional development so that each staff member spends about 20% of work time engaged in activities that he or she finds most meaningful.
3. Developing targeted interventions
Just as all politics is local, the study suggests that many sources of burnout are local as well. For example, although a high clerical burden on physicians may be a universal driver of burnout, it manifests differently in each institutional setting. The key here is to dig into the specific structural driver at the unit or ward level, engage physicians in analysis and problem-solving, and implement a plan to address the problem.
Dr. Shanafelt noted, “We organize the drivers of engagement and burnout around seven dimensions: workload, efficiency, flexibility/control, community at work, organizational culture and values, work-life integration, and meaning in work. Each of these dimensions has organizational and individual components. Work units should begin by identifying which one or two dimensions are the biggest challenges for the group and then begin a stepwise process to address them.”
4. Cultivating community at work
Peer support, a long-standing source of strength among surgeons and other physicians, unintentionally has been eroded in many modern medical institutions. There is ample evidence that this loss of collegiality is tied to burnout. “These interactions have been an unintended casualty of increasing productivity expectations, documentation requirements, and clerical burden. [Many organizations have eliminated] formal spaces for physicians to interact (e.g., physicians’ lounge or dining room) without recognizing the important role that this dedicated space played in fostering interpersonal connections among physicians.” The Mayo Clinic and other institutions are reversing this trend by creating dedicated physician rooms for breaks, snacks, and a venue for peer interaction and camaraderie.
5. Rethinking rewards and incentives
Compensation is now commonly linked to productivity in many health care organizations, but this approach has some profound drawbacks: It can lead to physician burnout. Incentive structures based on patient satisfaction and quality metrics can have similar unintended consequences. All these incentive structures can combine to drive physicians to overwork. “Physicians may be particularly vulnerable to overwork due to high levels of education debt, their desire to ‘do everything for their patients,’ unhealthy role modeling by colleagues, and normalization of extreme work hours during the training process.” The investigators do not claim to have the ultimate answer to the problem of incentives that create unhealthy work patterns, but they argue that it is critical for leaders to recognize the potential unintended consequences of the productivity reward/incentive model and consider strategies to prevent overwork leading to burnout.
6. Aligning values and strengthening culture
The investigators also describe Mayo’s efforts to pursue self-appraisal of alignment of mission, values, and culture. They also describe the regular use of an all-staff survey, which has on occasion yielded candid feedback that, while not always flattering, has been the basis of a profound institutional rethink. The willingness of leadership to be receptive to hard truths from physicians is the foundation of institutional learning about burnout prevention and encourages engagement of the staff.
7. Promoting flexibility and work-life integration
Allowing employees greater flexibility in how and when they work is a management strategy that is gaining ground in many industries. Increasing part-time positions and expanding options for the work day have both been found to help prevent burnout and also help physicians recover from burnout. In addition, “institutions should also comprehensively examine the structure of their vacation benefits, coverage for life events (e.g., birth of a child, illness/death in family), approach to scheduling, and strategy for coverage of nights and weekends. Compensation practices that disincentivize using vacation time are shortsighted and should be eliminated.”
8. Providing resources to promote resilience and self-care
The solutions to burnout have been aimed at the individual and involve stress-reduction training and other personal management strategies. A metastudy of the interventions mentions psychoeducation, counseling, wellness management, interpersonal communication, and mindfulness meditation (J Nerv Ment Dis. 2014 May;202:353-9). But without concomitant structural reform, these individual solutions can backfire. “When individually focused offerings are not coupled with sincere efforts to address the system-based issues contributing to burnout, this approach is typically met with skepticism and resistance by physicians (‘They are implying I am the problem’). In this context, the response to well-intentioned ‘resilience training’ is frequently a cynical one (‘You only want to make me more resilient so you can further increase my workload’).”
9. Funding organizational research
Organizational science is a well-developed field of study. But cutting-edge management models such as the learning organization, participatory management, and collaborative action planning have been slow in coming to health care institutions. Dr. Shanafelt and Dr. Noseworthy argue that “vanguard institutions” such as the Mayo Clinic (which began its Program on Physician Well-Being in 2008), Stanford (Calif.) University, and other innovative institutions have the responsibility of developing evidence-based strategies to combat burnout that smaller institutions can implement.
Burnout among physicians is now on the radar of leadership in many health care institutions. Evidence on the cost and consequences is accumulating, and it becoming increasingly difficult to ignore what is happening to many physicians. Dr. Shanafelt projected an increasing need for operational solutions at the organizational level to address the problem. He said, “We need evidence to guide organizations to implement changes that truly make a difference, not well-intentioned but ineffective programs. Now that organizations recognize the strong business case, they are ready to invest resources to address this issue but they need to know it is money well spent and that there is an evidence-base to justify the investment.”
Most surgeons today are familiar with professional burnout – in their colleagues, in surgical trainees, and perhaps, in themselves. But the understanding of burnout is evolving. The discussion is moving away from blaming physicians for their poor coping skills toward identifying the structural and organizational roots of burnout.
Burnout is a syndrome cause by work-related stress that features emotional exhaustion, depersonalization, and a decreased sense of personal accomplishment. A recent study of nearly 7,000 physicians using the Maslach Burnout Inventory found that 54.4% of those surveyed reported at least one symptom of burnout (Mayo Clin Proc. 2015 Dec;90[12]:1600-19). Other studies have found similar rates of burnout in the surgical specialties such as orthopedic, oncologic, cardiothoracic, and plastic surgery (JAMA Surg. 2014 Sep;149:948-53; Ann Surg Oncol 2011 May;18:1229-35; Internat J Cardiol. 2015 Jan 20;179:7-72; Aesthet Surg J. 2016 Sep 27. E-pub ahead of print).
A new paradigm of burnout
The paradigm of burnout as a personal issue that can be managed by individual coping strategies is giving way to an understanding that the structural roots of burnout require the shared responsibility of individuals and their work organizations to solve the problem. A revised approach has emerged: Physician burnout as a symptom not of personal failure to cope, but of institutional failure to adapt to new circumstances in the health care milieu. The growing number of physicians employed in large group practices and medical centers has come with a whole array of management problems that are only beginning to be recognized, and burnout may be one of the most challenging.
Tait D. Shanafelt, MD, of the Mayo Foundation for Medical Education and Research, and John H. Noseworthy, MD, president and CEO of the Mayo Clinic, both in Rochester, Minn., have partnered to distill years of study and practice on the issue of burnout to a set of organizational strategies to tackle the problem and describe the Mayo Clinic experience. The study, “Executive Leadership and Physician Well-Being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout” (Mayo Clin Proc. 2016 Nov 18. doi. org/10.1016/j.mayocp.2016.10.004) reverses the conventional “blame the victim” approach and identifies instead institutional responsibility to address burnout.
“Increasing evidence over the last 10 years demonstrating links to quality of care, productivity, and turnover have raised appreciation … by organizations that they have a substantial stake in this issue and that they control many of the factors that contribute to this problem,” said Dr. Shanafelt in an interview.
Unintended consequences of the individual solution
The focus on individual responsibility can have unintended consequences. A physician suffering from burnout can take action by leaving his or her job or cutting back. Staff turnover, a phenomenon closely tied to burnout, is costly and damaging to productivity and patient care (Physician Leadersh J. 2015 May-Jun;2[3]:22-5); Health Care Manage Rev. 2004;29[1]2-7). These personal strategies may help individuals cope but can end up harming the institution and the work life of other staff members. Physicians experiencing burnout in their own lives can trigger the same condition in their colleagues.
The Mayo paper by Dr. Shanafelt and Dr. Noseworthy states, “Mistakenly, most hospitals, medical centers, and practice groups operate under the framework that burnout and professional satisfaction are solely the responsibility of the individual physician. This frequently results in organizations pursuing a narrow list of ‘solutions’ that are unlikely to result in meaningful progress (e.g., stress management workshops and individual training in mindfulness/resilience). Such strategies neglect the organizational factors that are the primary drivers of physician burnout and are correctly viewed with skepticism by physicians as an insincere effort by the organization to address the problem.”
Organizational strategies to reduce burnout
Dr. Shanafelt and Dr. Noseworthy developed a list of nine organizational strategies that have been shown to reduce burnout among doctors. A critical piece of this approach is the accumulated evidence of the financial burden of burnout among physicians in health care institutions. The approach is based on an informed leadership that recognizes the costs of inaction, without which a systemic solution is unlikely to be achieved.
1. Naming the issue and assessing the problem
Acknowledgment of burnout as an institutional problem and meaningful measurement of physician well-being are the initial steps in tackling the problem. This requires a sincere commitment at the highest level of management to listen and to recognize what staff physicians are saying. “At Mayo Clinic, we have incorporated town halls, radio broadcasts, letters, and video interviews along with face-to-face meetings involving clinical divisions, work units, and small groups as formats or [by using] the CEO to reach the staff.” Assessing physician well-being and quality of work life using one or more of the many available tools has to be an ongoing “a barometer of organization health,” and not just a one-off, crisis management activity.
2. Harnessing the power of leadership
Studies have found that management behaviors and strategies of supervisors are key components of physician well-being. The bottom line is that physician supervisors must accept a share of responsibility for burnout in those they manage. Leaders can be chosen on the basis of their ability to listen, engage, develop, and lead, and but they can also be trained to improve. In addition, leaders should be regularly assessed by those whom they lead. Dr. Shanafelt and Dr. Noseworthy argue that a crucial element of successful leadership involves recognizing unique interests and talents of individual physicians whom they manage and facilitating professional development so that each staff member spends about 20% of work time engaged in activities that he or she finds most meaningful.
3. Developing targeted interventions
Just as all politics is local, the study suggests that many sources of burnout are local as well. For example, although a high clerical burden on physicians may be a universal driver of burnout, it manifests differently in each institutional setting. The key here is to dig into the specific structural driver at the unit or ward level, engage physicians in analysis and problem-solving, and implement a plan to address the problem.
Dr. Shanafelt noted, “We organize the drivers of engagement and burnout around seven dimensions: workload, efficiency, flexibility/control, community at work, organizational culture and values, work-life integration, and meaning in work. Each of these dimensions has organizational and individual components. Work units should begin by identifying which one or two dimensions are the biggest challenges for the group and then begin a stepwise process to address them.”
4. Cultivating community at work
Peer support, a long-standing source of strength among surgeons and other physicians, unintentionally has been eroded in many modern medical institutions. There is ample evidence that this loss of collegiality is tied to burnout. “These interactions have been an unintended casualty of increasing productivity expectations, documentation requirements, and clerical burden. [Many organizations have eliminated] formal spaces for physicians to interact (e.g., physicians’ lounge or dining room) without recognizing the important role that this dedicated space played in fostering interpersonal connections among physicians.” The Mayo Clinic and other institutions are reversing this trend by creating dedicated physician rooms for breaks, snacks, and a venue for peer interaction and camaraderie.
5. Rethinking rewards and incentives
Compensation is now commonly linked to productivity in many health care organizations, but this approach has some profound drawbacks: It can lead to physician burnout. Incentive structures based on patient satisfaction and quality metrics can have similar unintended consequences. All these incentive structures can combine to drive physicians to overwork. “Physicians may be particularly vulnerable to overwork due to high levels of education debt, their desire to ‘do everything for their patients,’ unhealthy role modeling by colleagues, and normalization of extreme work hours during the training process.” The investigators do not claim to have the ultimate answer to the problem of incentives that create unhealthy work patterns, but they argue that it is critical for leaders to recognize the potential unintended consequences of the productivity reward/incentive model and consider strategies to prevent overwork leading to burnout.
6. Aligning values and strengthening culture
The investigators also describe Mayo’s efforts to pursue self-appraisal of alignment of mission, values, and culture. They also describe the regular use of an all-staff survey, which has on occasion yielded candid feedback that, while not always flattering, has been the basis of a profound institutional rethink. The willingness of leadership to be receptive to hard truths from physicians is the foundation of institutional learning about burnout prevention and encourages engagement of the staff.
7. Promoting flexibility and work-life integration
Allowing employees greater flexibility in how and when they work is a management strategy that is gaining ground in many industries. Increasing part-time positions and expanding options for the work day have both been found to help prevent burnout and also help physicians recover from burnout. In addition, “institutions should also comprehensively examine the structure of their vacation benefits, coverage for life events (e.g., birth of a child, illness/death in family), approach to scheduling, and strategy for coverage of nights and weekends. Compensation practices that disincentivize using vacation time are shortsighted and should be eliminated.”
8. Providing resources to promote resilience and self-care
The solutions to burnout have been aimed at the individual and involve stress-reduction training and other personal management strategies. A metastudy of the interventions mentions psychoeducation, counseling, wellness management, interpersonal communication, and mindfulness meditation (J Nerv Ment Dis. 2014 May;202:353-9). But without concomitant structural reform, these individual solutions can backfire. “When individually focused offerings are not coupled with sincere efforts to address the system-based issues contributing to burnout, this approach is typically met with skepticism and resistance by physicians (‘They are implying I am the problem’). In this context, the response to well-intentioned ‘resilience training’ is frequently a cynical one (‘You only want to make me more resilient so you can further increase my workload’).”
9. Funding organizational research
Organizational science is a well-developed field of study. But cutting-edge management models such as the learning organization, participatory management, and collaborative action planning have been slow in coming to health care institutions. Dr. Shanafelt and Dr. Noseworthy argue that “vanguard institutions” such as the Mayo Clinic (which began its Program on Physician Well-Being in 2008), Stanford (Calif.) University, and other innovative institutions have the responsibility of developing evidence-based strategies to combat burnout that smaller institutions can implement.
Burnout among physicians is now on the radar of leadership in many health care institutions. Evidence on the cost and consequences is accumulating, and it becoming increasingly difficult to ignore what is happening to many physicians. Dr. Shanafelt projected an increasing need for operational solutions at the organizational level to address the problem. He said, “We need evidence to guide organizations to implement changes that truly make a difference, not well-intentioned but ineffective programs. Now that organizations recognize the strong business case, they are ready to invest resources to address this issue but they need to know it is money well spent and that there is an evidence-base to justify the investment.”
PD-L1 testing in NSCLC patients shows high concordance
VIENNA – Several different tests for PD-L1 levels in tumor cells of patients with metastatic non–small cell lung cancer showed high concordance when run at seven French centers, boosting confidence in the clinical utility of this testing to guide first-line pembrolizumab treatment of patients with this cancer.
Among 27 laboratory-developed tests for PD-L1 (programmed death–ligand 1) levels in tumor cells that used any one of three prespecified testing platforms (made by Dako, Ventana, or Leica), 14 (52%) had “similar” concordance when compared with reference assays, Julien Adam, MD, said at the World Conference on Lung Cancer, sponsored by the International Association for the Study of Lung Cancer. “These results will provide the basis for making national recommendations for PD-L1 testing in patients with non–small cell lung cancer [NSCLC]” in France, added Dr. Adam, a pathologist at Gustave Roussy Cancer Center in Paris. “We expect to produce recommendations by the second half of 2017.”
Although the results came entirely from French centers, the results will also likely influence U.S. practice, predicted Shirish M. Gadgeel, MD, a thoracic oncologist at the Karmanos Cancer Institute in Detroit. The approval pembrolizumab (Keytruda) received from the Food and Drug Administration in October specified that patients with metastatic NSCLC had to show PD-L1 expression in the tumor using a FDA-approved test to receive pembrolizumab as first-line treatment.
“Before pembrolizumab’s approval there was no incentive to do PD-L1 testing,” but now it is becoming routine, he said. “It has been challenging to U.S. laboratories to decide which platform and antibody to use. Harmonization gives us confidence that if you have a platform and appropriate antibody you should be able to use the results clinically. I think the French results can be extrapolated” to U.S. practice because the results “came from multiple labs using multiple antibodies and platforms,” Dr. Gadgeel said.
The French study arranged for PD-L1 testing of NSCLC specimens from 41 patients selected as broadly representative of PD-L1 expression levels. The seven participating centers used a Dako (three centers), Ventana (two centers), or Leica (two centers) testing platform and one of five available antibodies that bind PD-L1. Every center ran tests that depended on different antibodies, and tests occurred on both tumor cells and immune cells. In total the seven testing sites collectively performed 35 stainings on each specimen for a total of 1,435 slides. In tumor cells, the overall, weighted kappa coefficient for concordance was 0.81 for tests that used the SP263 antibody and 0.78 for those using the E1L3N antibody, both high enough to make them potential candidates for routine use, said Dr. Adam. The 28-8 and 22C3 antibodies also showed high concordance levels. In contrast, some antibodies used at certain centers produced unacceptable results with concordance coefficients of less than 0.5. The best performing antibody overall was SP263.
No test measuring PD-L1 level in immune cells had an acceptable concordance rate, Dr. Adam also reported.
[email protected]
On Twitter @mitchelzoler
Researchers have developed several different antibodies for measuring levels of PD-L1 in tumor cells and the antibodies can be used in several different testing platforms. Although most laboratories focus on using one specific immunohistochemical platform, the overall status of real-world PD-L1 testing is messy.
In the results reported by Dr. Adam, concordance weighted kappa coefficients of 0.8 or higher show extremely good concordance, and coefficients of 0.6-0.79 show good concordance. Several of the tests and testing sites reported by Dr. Adam showed concordance coefficients within these ranges. In certain other cases the concordance coefficients were very low, which prompts concern about the reliability of these low-scoring tests. The results show that the results you see in one laboratory with a specific antibody and platform test may not always remain consistent with the same antibody and platform used elsewhere.
Michael Boyer, MD, is a professor of medicine at the University of Sydney and a thoracic oncologist and chief clinical officer of the Chris O’Brien Lifehouse in Sydney. He has received research support from Merck and from AstraZeneca, Bristol-Myers Squibb, Clovis, Eli Lilly, Pfizer, and Roche. He made these comments as designated discussant for the report.
Researchers have developed several different antibodies for measuring levels of PD-L1 in tumor cells and the antibodies can be used in several different testing platforms. Although most laboratories focus on using one specific immunohistochemical platform, the overall status of real-world PD-L1 testing is messy.
In the results reported by Dr. Adam, concordance weighted kappa coefficients of 0.8 or higher show extremely good concordance, and coefficients of 0.6-0.79 show good concordance. Several of the tests and testing sites reported by Dr. Adam showed concordance coefficients within these ranges. In certain other cases the concordance coefficients were very low, which prompts concern about the reliability of these low-scoring tests. The results show that the results you see in one laboratory with a specific antibody and platform test may not always remain consistent with the same antibody and platform used elsewhere.
Michael Boyer, MD, is a professor of medicine at the University of Sydney and a thoracic oncologist and chief clinical officer of the Chris O’Brien Lifehouse in Sydney. He has received research support from Merck and from AstraZeneca, Bristol-Myers Squibb, Clovis, Eli Lilly, Pfizer, and Roche. He made these comments as designated discussant for the report.
Researchers have developed several different antibodies for measuring levels of PD-L1 in tumor cells and the antibodies can be used in several different testing platforms. Although most laboratories focus on using one specific immunohistochemical platform, the overall status of real-world PD-L1 testing is messy.
In the results reported by Dr. Adam, concordance weighted kappa coefficients of 0.8 or higher show extremely good concordance, and coefficients of 0.6-0.79 show good concordance. Several of the tests and testing sites reported by Dr. Adam showed concordance coefficients within these ranges. In certain other cases the concordance coefficients were very low, which prompts concern about the reliability of these low-scoring tests. The results show that the results you see in one laboratory with a specific antibody and platform test may not always remain consistent with the same antibody and platform used elsewhere.
Michael Boyer, MD, is a professor of medicine at the University of Sydney and a thoracic oncologist and chief clinical officer of the Chris O’Brien Lifehouse in Sydney. He has received research support from Merck and from AstraZeneca, Bristol-Myers Squibb, Clovis, Eli Lilly, Pfizer, and Roche. He made these comments as designated discussant for the report.
VIENNA – Several different tests for PD-L1 levels in tumor cells of patients with metastatic non–small cell lung cancer showed high concordance when run at seven French centers, boosting confidence in the clinical utility of this testing to guide first-line pembrolizumab treatment of patients with this cancer.
Among 27 laboratory-developed tests for PD-L1 (programmed death–ligand 1) levels in tumor cells that used any one of three prespecified testing platforms (made by Dako, Ventana, or Leica), 14 (52%) had “similar” concordance when compared with reference assays, Julien Adam, MD, said at the World Conference on Lung Cancer, sponsored by the International Association for the Study of Lung Cancer. “These results will provide the basis for making national recommendations for PD-L1 testing in patients with non–small cell lung cancer [NSCLC]” in France, added Dr. Adam, a pathologist at Gustave Roussy Cancer Center in Paris. “We expect to produce recommendations by the second half of 2017.”
Although the results came entirely from French centers, the results will also likely influence U.S. practice, predicted Shirish M. Gadgeel, MD, a thoracic oncologist at the Karmanos Cancer Institute in Detroit. The approval pembrolizumab (Keytruda) received from the Food and Drug Administration in October specified that patients with metastatic NSCLC had to show PD-L1 expression in the tumor using a FDA-approved test to receive pembrolizumab as first-line treatment.
“Before pembrolizumab’s approval there was no incentive to do PD-L1 testing,” but now it is becoming routine, he said. “It has been challenging to U.S. laboratories to decide which platform and antibody to use. Harmonization gives us confidence that if you have a platform and appropriate antibody you should be able to use the results clinically. I think the French results can be extrapolated” to U.S. practice because the results “came from multiple labs using multiple antibodies and platforms,” Dr. Gadgeel said.
The French study arranged for PD-L1 testing of NSCLC specimens from 41 patients selected as broadly representative of PD-L1 expression levels. The seven participating centers used a Dako (three centers), Ventana (two centers), or Leica (two centers) testing platform and one of five available antibodies that bind PD-L1. Every center ran tests that depended on different antibodies, and tests occurred on both tumor cells and immune cells. In total the seven testing sites collectively performed 35 stainings on each specimen for a total of 1,435 slides. In tumor cells, the overall, weighted kappa coefficient for concordance was 0.81 for tests that used the SP263 antibody and 0.78 for those using the E1L3N antibody, both high enough to make them potential candidates for routine use, said Dr. Adam. The 28-8 and 22C3 antibodies also showed high concordance levels. In contrast, some antibodies used at certain centers produced unacceptable results with concordance coefficients of less than 0.5. The best performing antibody overall was SP263.
No test measuring PD-L1 level in immune cells had an acceptable concordance rate, Dr. Adam also reported.
[email protected]
On Twitter @mitchelzoler
VIENNA – Several different tests for PD-L1 levels in tumor cells of patients with metastatic non–small cell lung cancer showed high concordance when run at seven French centers, boosting confidence in the clinical utility of this testing to guide first-line pembrolizumab treatment of patients with this cancer.
Among 27 laboratory-developed tests for PD-L1 (programmed death–ligand 1) levels in tumor cells that used any one of three prespecified testing platforms (made by Dako, Ventana, or Leica), 14 (52%) had “similar” concordance when compared with reference assays, Julien Adam, MD, said at the World Conference on Lung Cancer, sponsored by the International Association for the Study of Lung Cancer. “These results will provide the basis for making national recommendations for PD-L1 testing in patients with non–small cell lung cancer [NSCLC]” in France, added Dr. Adam, a pathologist at Gustave Roussy Cancer Center in Paris. “We expect to produce recommendations by the second half of 2017.”
Although the results came entirely from French centers, the results will also likely influence U.S. practice, predicted Shirish M. Gadgeel, MD, a thoracic oncologist at the Karmanos Cancer Institute in Detroit. The approval pembrolizumab (Keytruda) received from the Food and Drug Administration in October specified that patients with metastatic NSCLC had to show PD-L1 expression in the tumor using a FDA-approved test to receive pembrolizumab as first-line treatment.
“Before pembrolizumab’s approval there was no incentive to do PD-L1 testing,” but now it is becoming routine, he said. “It has been challenging to U.S. laboratories to decide which platform and antibody to use. Harmonization gives us confidence that if you have a platform and appropriate antibody you should be able to use the results clinically. I think the French results can be extrapolated” to U.S. practice because the results “came from multiple labs using multiple antibodies and platforms,” Dr. Gadgeel said.
The French study arranged for PD-L1 testing of NSCLC specimens from 41 patients selected as broadly representative of PD-L1 expression levels. The seven participating centers used a Dako (three centers), Ventana (two centers), or Leica (two centers) testing platform and one of five available antibodies that bind PD-L1. Every center ran tests that depended on different antibodies, and tests occurred on both tumor cells and immune cells. In total the seven testing sites collectively performed 35 stainings on each specimen for a total of 1,435 slides. In tumor cells, the overall, weighted kappa coefficient for concordance was 0.81 for tests that used the SP263 antibody and 0.78 for those using the E1L3N antibody, both high enough to make them potential candidates for routine use, said Dr. Adam. The 28-8 and 22C3 antibodies also showed high concordance levels. In contrast, some antibodies used at certain centers produced unacceptable results with concordance coefficients of less than 0.5. The best performing antibody overall was SP263.
No test measuring PD-L1 level in immune cells had an acceptable concordance rate, Dr. Adam also reported.
[email protected]
On Twitter @mitchelzoler
AT WCLC 2016
Key clinical point:
Major finding: The concordance weighted kappa coefficient was highest for tests using the SP263 antibody, with an average coefficient of 0.81.
Data source: Forty-one non–small cell lung cancer specimens subjected to a total of 35 different tests.
Disclosures: Funding for the study came from AstraZeneca, Bristol Myers Squibb, Merck Sharp and Dohme, and Roche. Dr. Adam has been a consultant to AstraZeneca, Bristol-Myers Squibb, HalioDx, Merck Sharp and Dohme, and Roche. Dr. Gadgeel has been a speaker on behalf of Eli Lilly, Genentech, and GlaxoSmithKline and has received research funding from AstraZeneca, Eli Lilly, and Genentech. Dr. Brahmer has served on an advisory board for Merck.
LMWH trumps unfractionated heparin in reducing posttrauma thrombotic events
HOLLYWOOD, FLA. – Low-molecular-weight heparin (LMWH) decreased the risk of venous thromboembolism in trauma patients significantly more than did unfractionated heparin, a large state database review has found.
It also was associated with a 37% decrease in overall mortality, compared with unfractionated heparin, Benjamin Jacobs, MD, said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
He extracted data describing thromboembolism prophylaxis among 37,868 trauma patients included in the Michigan Trauma Quality Improvement Program from 2012 to 2014. The patients were treated at 23 hospitals around the state. They received either unfractionated or LMWH as their only clot-preventing protocol.
The primary outcomes of the study were reductions in the risk of venous thromboembolism (VTE), deep vein thrombosis (DVT), pulmonary thrombosis (PT), and mortality.
LMWH was given at either 40 mg every day or 30 mg twice a day. The comparator was unfractionated heparin at 5,000 U either two or three times a day.
The preferred method was LMWH, which 83% of patients received, compared with 17% who got the unfractionated heparin. Most patients who got LMWH received the 40 mg/day dose (70%). Most who got unfractionated heparin received 5,000 U three times a day (87%).
Both types of heparin reduced the risk of all thromboembolic outcomes, and both doses of LMWH significantly reduced the risks. However, the 40 mg/day dose was significantly more effective than the twice-daily 30-mg dose in reducing the risk of VTE and DVT. Risk reductions for PT and mortality were not significantly different between the doses.
Overall, compared with unfractionated heparin, LMWH decreased the risk of VTE by 33%; of PT by 48%; and of DVT by 27%. It also conferred a significant mortality benefit, reducing the risk of death by 37%, compared with the unfractionated type
When Dr. Jacobs grouped the patients according to Injury Severity Score (ISS), he saw a consistently higher benefit among patients with lower scores. For example, LMWH significantly reduced the risk of PT by 59% in patients with an ISS of 5-14. In those with an ISS of 25 or higher, the drug was associated with a 20% increased risk, although that wasn’t statistically significant.
There was a similar finding in DVT. LMWH reduced the risk by 18% in those with an ISS of 5-15, and by 50% among those with an score of 16-24 – both significant reductions. Among those with an ISS of at least 25, the risk was 18% higher, although, again, it was not a significant finding.
Curiously, the mortality benefit was stronger among sicker patients. The benefit was nonsignificant among those with an ISS of less than 25 but for those above 25, the mortality risk reduction was a significant 45%.
Dr Jacobs had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOLLYWOOD, FLA. – Low-molecular-weight heparin (LMWH) decreased the risk of venous thromboembolism in trauma patients significantly more than did unfractionated heparin, a large state database review has found.
It also was associated with a 37% decrease in overall mortality, compared with unfractionated heparin, Benjamin Jacobs, MD, said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
He extracted data describing thromboembolism prophylaxis among 37,868 trauma patients included in the Michigan Trauma Quality Improvement Program from 2012 to 2014. The patients were treated at 23 hospitals around the state. They received either unfractionated or LMWH as their only clot-preventing protocol.
The primary outcomes of the study were reductions in the risk of venous thromboembolism (VTE), deep vein thrombosis (DVT), pulmonary thrombosis (PT), and mortality.
LMWH was given at either 40 mg every day or 30 mg twice a day. The comparator was unfractionated heparin at 5,000 U either two or three times a day.
The preferred method was LMWH, which 83% of patients received, compared with 17% who got the unfractionated heparin. Most patients who got LMWH received the 40 mg/day dose (70%). Most who got unfractionated heparin received 5,000 U three times a day (87%).
Both types of heparin reduced the risk of all thromboembolic outcomes, and both doses of LMWH significantly reduced the risks. However, the 40 mg/day dose was significantly more effective than the twice-daily 30-mg dose in reducing the risk of VTE and DVT. Risk reductions for PT and mortality were not significantly different between the doses.
Overall, compared with unfractionated heparin, LMWH decreased the risk of VTE by 33%; of PT by 48%; and of DVT by 27%. It also conferred a significant mortality benefit, reducing the risk of death by 37%, compared with the unfractionated type
When Dr. Jacobs grouped the patients according to Injury Severity Score (ISS), he saw a consistently higher benefit among patients with lower scores. For example, LMWH significantly reduced the risk of PT by 59% in patients with an ISS of 5-14. In those with an ISS of 25 or higher, the drug was associated with a 20% increased risk, although that wasn’t statistically significant.
There was a similar finding in DVT. LMWH reduced the risk by 18% in those with an ISS of 5-15, and by 50% among those with an score of 16-24 – both significant reductions. Among those with an ISS of at least 25, the risk was 18% higher, although, again, it was not a significant finding.
Curiously, the mortality benefit was stronger among sicker patients. The benefit was nonsignificant among those with an ISS of less than 25 but for those above 25, the mortality risk reduction was a significant 45%.
Dr Jacobs had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOLLYWOOD, FLA. – Low-molecular-weight heparin (LMWH) decreased the risk of venous thromboembolism in trauma patients significantly more than did unfractionated heparin, a large state database review has found.
It also was associated with a 37% decrease in overall mortality, compared with unfractionated heparin, Benjamin Jacobs, MD, said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma.
He extracted data describing thromboembolism prophylaxis among 37,868 trauma patients included in the Michigan Trauma Quality Improvement Program from 2012 to 2014. The patients were treated at 23 hospitals around the state. They received either unfractionated or LMWH as their only clot-preventing protocol.
The primary outcomes of the study were reductions in the risk of venous thromboembolism (VTE), deep vein thrombosis (DVT), pulmonary thrombosis (PT), and mortality.
LMWH was given at either 40 mg every day or 30 mg twice a day. The comparator was unfractionated heparin at 5,000 U either two or three times a day.
The preferred method was LMWH, which 83% of patients received, compared with 17% who got the unfractionated heparin. Most patients who got LMWH received the 40 mg/day dose (70%). Most who got unfractionated heparin received 5,000 U three times a day (87%).
Both types of heparin reduced the risk of all thromboembolic outcomes, and both doses of LMWH significantly reduced the risks. However, the 40 mg/day dose was significantly more effective than the twice-daily 30-mg dose in reducing the risk of VTE and DVT. Risk reductions for PT and mortality were not significantly different between the doses.
Overall, compared with unfractionated heparin, LMWH decreased the risk of VTE by 33%; of PT by 48%; and of DVT by 27%. It also conferred a significant mortality benefit, reducing the risk of death by 37%, compared with the unfractionated type
When Dr. Jacobs grouped the patients according to Injury Severity Score (ISS), he saw a consistently higher benefit among patients with lower scores. For example, LMWH significantly reduced the risk of PT by 59% in patients with an ISS of 5-14. In those with an ISS of 25 or higher, the drug was associated with a 20% increased risk, although that wasn’t statistically significant.
There was a similar finding in DVT. LMWH reduced the risk by 18% in those with an ISS of 5-15, and by 50% among those with an score of 16-24 – both significant reductions. Among those with an ISS of at least 25, the risk was 18% higher, although, again, it was not a significant finding.
Curiously, the mortality benefit was stronger among sicker patients. The benefit was nonsignificant among those with an ISS of less than 25 but for those above 25, the mortality risk reduction was a significant 45%.
Dr Jacobs had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE EAST ANNUAL SCIENTIFIC ASSEMBLY
Key clinical point:
Major finding: Overall mortality was reduced by 37% with LMWH, compared with unfractionated heparin.
Data source: The review comprised 37,868 patients included in the Michigan Trauma Quality Improvement Program.
Disclosures: Dr. Jacobs had no financial disclosures.
Smoking-cessation interest and success vary by race, ethnicity
Just over 55% of adult cigarette smokers made an attempt to quit in the past year, and 7.4% said that they recently quit, according to investigators from the Centers or Disease Control and Prevention.
Data from the 2015 National Health Interview Survey (NHIS) show that 68% of cigarette smokers were interested in quitting, with considerable variation seen according to race and ethnicity (MMWR. 2017;65[52]:1457-64).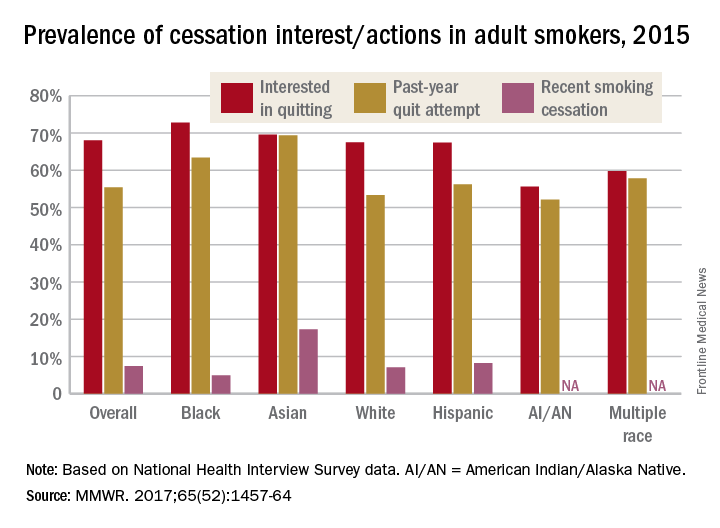
American Indian/Alaska Native smokers were the least likely to be interested in quitting (55.6%) and to have attempted to quit (52.1%), but the sample size was too small to report a reliable quit rate. The amount of survey participants of multiple races was also too small to report a reliable quit rate. Among that group, 59.8% were interested in quitting and 57.8% had attempted to quit in the past year, the NHIS data showed.
The sizes of surveyed populations for individual races and ethnicities were not reported, but the total sample size for the 2015 NHIS was 33,672.
Just over 55% of adult cigarette smokers made an attempt to quit in the past year, and 7.4% said that they recently quit, according to investigators from the Centers or Disease Control and Prevention.
Data from the 2015 National Health Interview Survey (NHIS) show that 68% of cigarette smokers were interested in quitting, with considerable variation seen according to race and ethnicity (MMWR. 2017;65[52]:1457-64).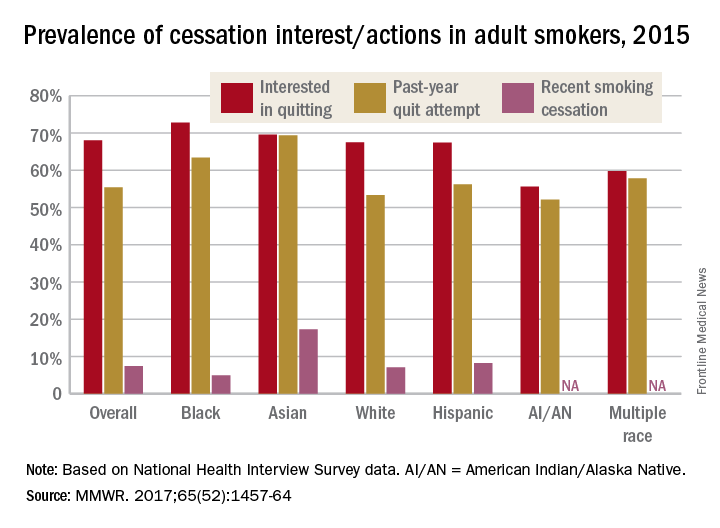
American Indian/Alaska Native smokers were the least likely to be interested in quitting (55.6%) and to have attempted to quit (52.1%), but the sample size was too small to report a reliable quit rate. The amount of survey participants of multiple races was also too small to report a reliable quit rate. Among that group, 59.8% were interested in quitting and 57.8% had attempted to quit in the past year, the NHIS data showed.
The sizes of surveyed populations for individual races and ethnicities were not reported, but the total sample size for the 2015 NHIS was 33,672.
Just over 55% of adult cigarette smokers made an attempt to quit in the past year, and 7.4% said that they recently quit, according to investigators from the Centers or Disease Control and Prevention.
Data from the 2015 National Health Interview Survey (NHIS) show that 68% of cigarette smokers were interested in quitting, with considerable variation seen according to race and ethnicity (MMWR. 2017;65[52]:1457-64).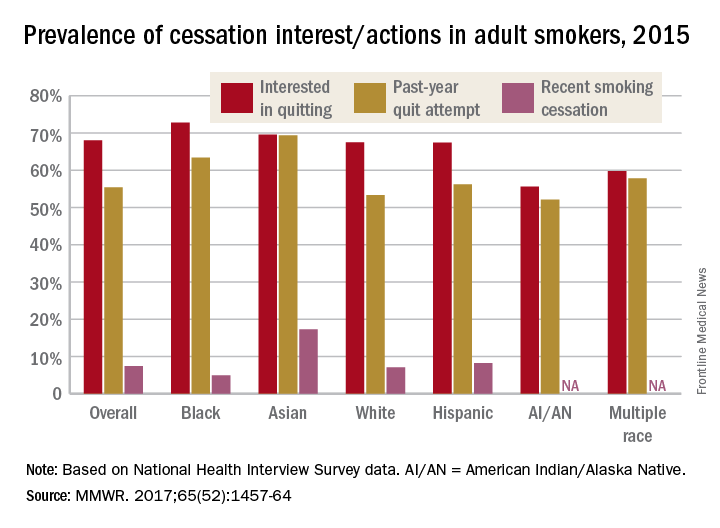
American Indian/Alaska Native smokers were the least likely to be interested in quitting (55.6%) and to have attempted to quit (52.1%), but the sample size was too small to report a reliable quit rate. The amount of survey participants of multiple races was also too small to report a reliable quit rate. Among that group, 59.8% were interested in quitting and 57.8% had attempted to quit in the past year, the NHIS data showed.
The sizes of surveyed populations for individual races and ethnicities were not reported, but the total sample size for the 2015 NHIS was 33,672.