User login
The Official Newspaper of the American Association for Thoracic Surgery
Most cigarette smokers attempt to quit without evidence-based techniques
More than half of cigarette smokers have received advice to quit from a health care professional, but less than a third used medication or counseling in their cessation attempt, according to investigators from the Centers for Disease Control and Prevention.
In 2015, just over 57% of adult smokers said that a health care professional had advised them to quit in the past year. Of those who tried to quit, 29% used medication such as nicotine patches or gum, varenicline, or bupropion; 7% used counseling (including a stop-smoking clinic, class, or support group and a telephone help line); and 31% used counseling and/or medication, the investigators reported (MMWR 2017;65[52]:1457-64).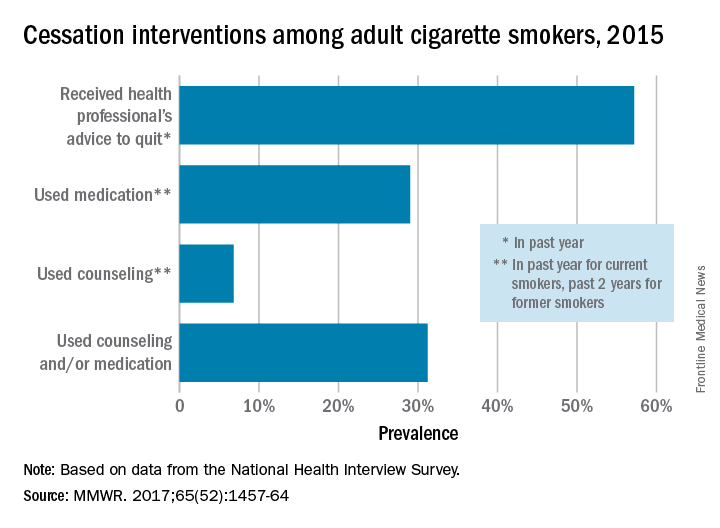
With the overall cessation rate at less than 10%, “it is critical for health care providers to consistently identify smokers, advise them to quit, and offer evidence-based cessation treatments, and for insurers to cover and promote the use of these treatments and remove barriers to accessing them,” the investigators wrote.
More than half of cigarette smokers have received advice to quit from a health care professional, but less than a third used medication or counseling in their cessation attempt, according to investigators from the Centers for Disease Control and Prevention.
In 2015, just over 57% of adult smokers said that a health care professional had advised them to quit in the past year. Of those who tried to quit, 29% used medication such as nicotine patches or gum, varenicline, or bupropion; 7% used counseling (including a stop-smoking clinic, class, or support group and a telephone help line); and 31% used counseling and/or medication, the investigators reported (MMWR 2017;65[52]:1457-64).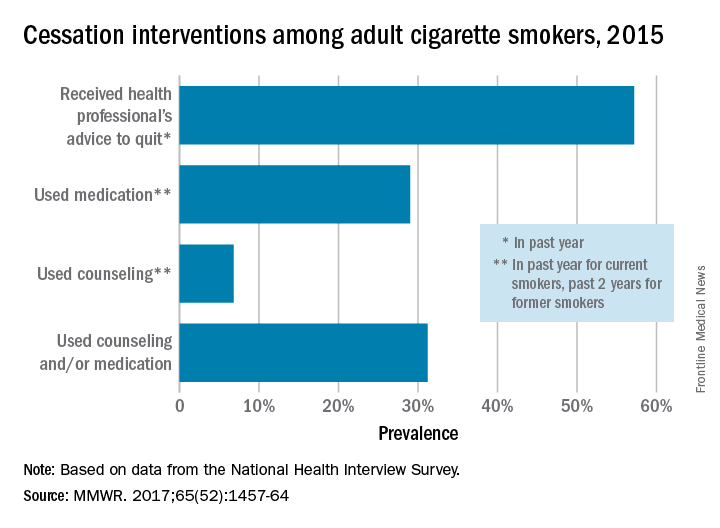
With the overall cessation rate at less than 10%, “it is critical for health care providers to consistently identify smokers, advise them to quit, and offer evidence-based cessation treatments, and for insurers to cover and promote the use of these treatments and remove barriers to accessing them,” the investigators wrote.
More than half of cigarette smokers have received advice to quit from a health care professional, but less than a third used medication or counseling in their cessation attempt, according to investigators from the Centers for Disease Control and Prevention.
In 2015, just over 57% of adult smokers said that a health care professional had advised them to quit in the past year. Of those who tried to quit, 29% used medication such as nicotine patches or gum, varenicline, or bupropion; 7% used counseling (including a stop-smoking clinic, class, or support group and a telephone help line); and 31% used counseling and/or medication, the investigators reported (MMWR 2017;65[52]:1457-64).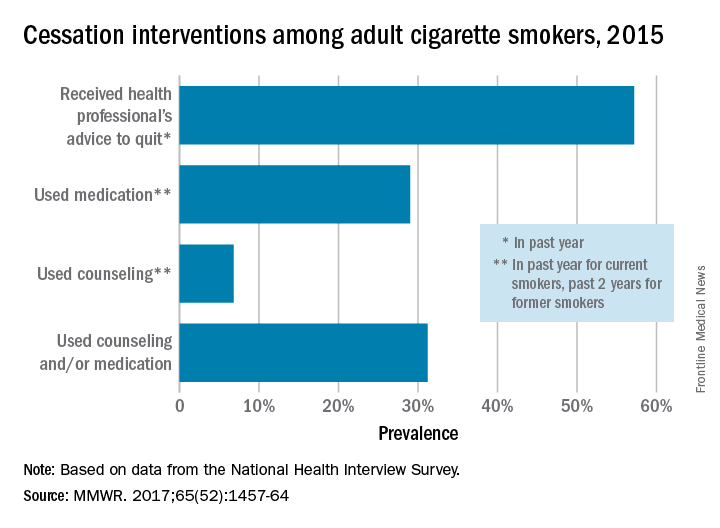
With the overall cessation rate at less than 10%, “it is critical for health care providers to consistently identify smokers, advise them to quit, and offer evidence-based cessation treatments, and for insurers to cover and promote the use of these treatments and remove barriers to accessing them,” the investigators wrote.
FROM MMWR
Senate, House take first step toward repealing ACA
With a Jan. 12 early morning procedural passed on party lines, the Senate has set the stage for the repeal of the revenue aspects of the Affordable Care Act. The House of Representatives passed similar legislation Jan. 13.*
Republicans will be using the budget reconciliation process, which will allow them to move forward with repealing certain provisions of the health care reform law without any Democratic support, although passage of any replacement will require some bipartisan support as Republicans do not have the required 60 votes to guarantee passage in the Senate.
The budget resolutions contain no details about what could be repealed or whether there will be a replacement, but it does direct the key committees to write draft legislation by Jan. 27.
Senate Republicans “plan to rescue those trapped in a failing system, to replace that system with a functional market, or markets, and then repeal Obamacare for good,” he said.
Sen. Alexander said the process will come in three parts. The first will protect the 11 million people who have purchased health insurance through the exchanges so that they don’t lose coverage.
“Second, we will build better systems providing Americans with more choices that cost less,” he said. “Note I say systems, not one system. If anyone is expecting [Senate Majority Leader Mitch] McConnell [R-Ky.] to roll a wheelbarrow on the Senate floor with a comprehensive Republican health care plan, they’re going to be waiting a long time because we don’t believe in that. We don’t want to replace a failed Obamacare federal system with another failed federal system.”
The last part will be to repeal what remains of the law after the new plan is in place.
Sen. Alexander reiterated that any future bill will keep the ban on coverage denials for preexisting conditions and the allowance of coverage of children up to the age of 26 who are on their parents’ plans.
He stated that this reform effort will not address Medicare reform, which will be the subject of separate legislative action.
*This story was updated Jan. 13 at 4:30 pm.
With a Jan. 12 early morning procedural passed on party lines, the Senate has set the stage for the repeal of the revenue aspects of the Affordable Care Act. The House of Representatives passed similar legislation Jan. 13.*
Republicans will be using the budget reconciliation process, which will allow them to move forward with repealing certain provisions of the health care reform law without any Democratic support, although passage of any replacement will require some bipartisan support as Republicans do not have the required 60 votes to guarantee passage in the Senate.
The budget resolutions contain no details about what could be repealed or whether there will be a replacement, but it does direct the key committees to write draft legislation by Jan. 27.
Senate Republicans “plan to rescue those trapped in a failing system, to replace that system with a functional market, or markets, and then repeal Obamacare for good,” he said.
Sen. Alexander said the process will come in three parts. The first will protect the 11 million people who have purchased health insurance through the exchanges so that they don’t lose coverage.
“Second, we will build better systems providing Americans with more choices that cost less,” he said. “Note I say systems, not one system. If anyone is expecting [Senate Majority Leader Mitch] McConnell [R-Ky.] to roll a wheelbarrow on the Senate floor with a comprehensive Republican health care plan, they’re going to be waiting a long time because we don’t believe in that. We don’t want to replace a failed Obamacare federal system with another failed federal system.”
The last part will be to repeal what remains of the law after the new plan is in place.
Sen. Alexander reiterated that any future bill will keep the ban on coverage denials for preexisting conditions and the allowance of coverage of children up to the age of 26 who are on their parents’ plans.
He stated that this reform effort will not address Medicare reform, which will be the subject of separate legislative action.
*This story was updated Jan. 13 at 4:30 pm.
With a Jan. 12 early morning procedural passed on party lines, the Senate has set the stage for the repeal of the revenue aspects of the Affordable Care Act. The House of Representatives passed similar legislation Jan. 13.*
Republicans will be using the budget reconciliation process, which will allow them to move forward with repealing certain provisions of the health care reform law without any Democratic support, although passage of any replacement will require some bipartisan support as Republicans do not have the required 60 votes to guarantee passage in the Senate.
The budget resolutions contain no details about what could be repealed or whether there will be a replacement, but it does direct the key committees to write draft legislation by Jan. 27.
Senate Republicans “plan to rescue those trapped in a failing system, to replace that system with a functional market, or markets, and then repeal Obamacare for good,” he said.
Sen. Alexander said the process will come in three parts. The first will protect the 11 million people who have purchased health insurance through the exchanges so that they don’t lose coverage.
“Second, we will build better systems providing Americans with more choices that cost less,” he said. “Note I say systems, not one system. If anyone is expecting [Senate Majority Leader Mitch] McConnell [R-Ky.] to roll a wheelbarrow on the Senate floor with a comprehensive Republican health care plan, they’re going to be waiting a long time because we don’t believe in that. We don’t want to replace a failed Obamacare federal system with another failed federal system.”
The last part will be to repeal what remains of the law after the new plan is in place.
Sen. Alexander reiterated that any future bill will keep the ban on coverage denials for preexisting conditions and the allowance of coverage of children up to the age of 26 who are on their parents’ plans.
He stated that this reform effort will not address Medicare reform, which will be the subject of separate legislative action.
*This story was updated Jan. 13 at 4:30 pm.
LAA closure during cardiac surgery cuts late mortality
NEW ORLEANS – Surgical left atrial appendage closure at the time of open heart surgery in patients with atrial fibrillation doesn’t decrease patients’ early or late risk of stroke, but it does substantially reduce their risk of late mortality, Masahiko Ando, MD, reported at the American Heart Association scientific sessions.
Solid evidence demonstrates that percutaneous left atrial appendage (LAA) closure using the Watchman or other devices in patients with atrial fibrillation offers a potential alternative to lifelong oral anticoagulation.
In contrast, even though surgical LAA closure at the time of cardiac surgery is commonly done, the data as to its long-term impact are scanty. This was the impetus for Dr. Ando and his coinvestigators at Massachusetts General Hospital in Boston to perform a comprehensive systematic review of the medical literature. They also conducted a meta-analysis that involved 7,466 patients who underwent open-heart surgery with or without surgical LAA closure in 12 studies, 3 of which were randomized controlled trials, 2 propensity-matched comparisons, and the rest cohort studies.
At 30-day follow-up, LAA closure was not associated with any significant effect on the risks of stroke, death, reexploration for bleeding, or postoperative atrial fibrillation.
At the latest follow-up in the studies, however, surgical LAA closure was associated with a highly significant 36% reduction in mortality risk compared with the no–LAA-closure control group. This remained the case even after statistical adjustment for demographics, type of cardiac surgery, and the form of preoperative atrial fibrillation.
“Given that we generally add LAA closure to those who have a higher risk of embolization, which could have negatively affected the efficacy of LAA closure, this preventive effect of LAA closure on late mortality cannot be ignored,” said Dr. Ando.
The most likely explanation for the improved survival in surgical LAA closure recipients, he continued, is that the procedure enabled them to avoid aggressive lifelong oral anticoagulation, with its attendant risks.
Dr. Ando reported having no financial conflicts regarding his study.
NEW ORLEANS – Surgical left atrial appendage closure at the time of open heart surgery in patients with atrial fibrillation doesn’t decrease patients’ early or late risk of stroke, but it does substantially reduce their risk of late mortality, Masahiko Ando, MD, reported at the American Heart Association scientific sessions.
Solid evidence demonstrates that percutaneous left atrial appendage (LAA) closure using the Watchman or other devices in patients with atrial fibrillation offers a potential alternative to lifelong oral anticoagulation.
In contrast, even though surgical LAA closure at the time of cardiac surgery is commonly done, the data as to its long-term impact are scanty. This was the impetus for Dr. Ando and his coinvestigators at Massachusetts General Hospital in Boston to perform a comprehensive systematic review of the medical literature. They also conducted a meta-analysis that involved 7,466 patients who underwent open-heart surgery with or without surgical LAA closure in 12 studies, 3 of which were randomized controlled trials, 2 propensity-matched comparisons, and the rest cohort studies.
At 30-day follow-up, LAA closure was not associated with any significant effect on the risks of stroke, death, reexploration for bleeding, or postoperative atrial fibrillation.
At the latest follow-up in the studies, however, surgical LAA closure was associated with a highly significant 36% reduction in mortality risk compared with the no–LAA-closure control group. This remained the case even after statistical adjustment for demographics, type of cardiac surgery, and the form of preoperative atrial fibrillation.
“Given that we generally add LAA closure to those who have a higher risk of embolization, which could have negatively affected the efficacy of LAA closure, this preventive effect of LAA closure on late mortality cannot be ignored,” said Dr. Ando.
The most likely explanation for the improved survival in surgical LAA closure recipients, he continued, is that the procedure enabled them to avoid aggressive lifelong oral anticoagulation, with its attendant risks.
Dr. Ando reported having no financial conflicts regarding his study.
NEW ORLEANS – Surgical left atrial appendage closure at the time of open heart surgery in patients with atrial fibrillation doesn’t decrease patients’ early or late risk of stroke, but it does substantially reduce their risk of late mortality, Masahiko Ando, MD, reported at the American Heart Association scientific sessions.
Solid evidence demonstrates that percutaneous left atrial appendage (LAA) closure using the Watchman or other devices in patients with atrial fibrillation offers a potential alternative to lifelong oral anticoagulation.
In contrast, even though surgical LAA closure at the time of cardiac surgery is commonly done, the data as to its long-term impact are scanty. This was the impetus for Dr. Ando and his coinvestigators at Massachusetts General Hospital in Boston to perform a comprehensive systematic review of the medical literature. They also conducted a meta-analysis that involved 7,466 patients who underwent open-heart surgery with or without surgical LAA closure in 12 studies, 3 of which were randomized controlled trials, 2 propensity-matched comparisons, and the rest cohort studies.
At 30-day follow-up, LAA closure was not associated with any significant effect on the risks of stroke, death, reexploration for bleeding, or postoperative atrial fibrillation.
At the latest follow-up in the studies, however, surgical LAA closure was associated with a highly significant 36% reduction in mortality risk compared with the no–LAA-closure control group. This remained the case even after statistical adjustment for demographics, type of cardiac surgery, and the form of preoperative atrial fibrillation.
“Given that we generally add LAA closure to those who have a higher risk of embolization, which could have negatively affected the efficacy of LAA closure, this preventive effect of LAA closure on late mortality cannot be ignored,” said Dr. Ando.
The most likely explanation for the improved survival in surgical LAA closure recipients, he continued, is that the procedure enabled them to avoid aggressive lifelong oral anticoagulation, with its attendant risks.
Dr. Ando reported having no financial conflicts regarding his study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Late mortality risk was reduced by 36% in patients with atrial fibrillation who underwent surgical LAA closure during open heart surgery, compared with those who did not.
Data source: This meta-analysis included 12 published studies and 7,466 patients who either did or did not undergo surgical LAA closure during open heart surgery.
Disclosures: The study presenter reported having no financial conflicts.
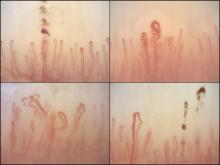
Nailfold analysis can predict cardiopulmonary complications in systemic sclerosis
Nailfold videocapillaroscopy can help to predict which patients with systemic sclerosis may develop serious cardiopulmonary complications, according to findings from a Dutch cross-sectional study.
While individual autoantibodies seen in systemic sclerosis (SSc) are known to be associated with greater or lesser risk of cardiopulmonary involvement, in this study nailfold vascularization patterns independently predicted pulmonary artery hypertension or interstitial lung disease.
All patients in the study had NVC pattern data as well as anti-extractable nuclear antigen (anti-ENA) antibodies. The mean age of the patients was 54 years; 82% were female, and median disease duration was 3 years. Just over half the cohort had interstitial lung disease, and 16% had pulmonary artery hypertension.
Among the anti-ENA autoantibody subtypes, anti-ACA was seen in 37% of patients, anti-Scl-70 in 24%, anti-RNP in 9%, and anti-RNAPIII in 5%; other subtypes were rarer. SSc-specific NVC patterns were seen in 88% of patients, with 10% of the cohort showing an early (less severe microangiopathy) pattern, 42% an active pattern, and 36% a late pattern.
One of the study’s objectives was to determine whether one or more mechanisms was responsible for both autoantibody production and the microangiopathy seen in SSc.
If a joint mechanism is implicated, “more severe NVC patterns would be determined in patients with autoantibodies (such as anti-Scl-70 and anti-RNAPIII) that are associated with more severe disease,” wrote Dr. Markusse and her colleagues. “On the other hand, if specific autoantibodies and stage of microangiopathy reflect different processes in the disease, a combination of autoantibody status and NVC could be helpful for identifying patients at highest risk for cardiopulmonary involvement.”
The investigators reported finding a similar distribution of NVC abnormalities across the major SSc autoantibody subtypes (except for anti–RNP-positive patients), suggesting that combinations of the two variables would be most predictive of cardiopulmonary involvement. More severe NVC patterns were associated with a higher risk of cardiopulmonary involvement, independent of the presence of a specific autoantibody.
Notably, the researchers wrote, “prevalence of ILD [interstitial lung disease] is generally lower among ACA-positive patients. According to our data, even among ACA-positive patients there was a trend for more ILD being associated with more severe NVC patterns (OR = 1.33).”
A similar pattern was seen for pulmonary artery hypertension. “Based on anti-RNP and anti-RNAPIII positivity, patients did not have an increased risk of a [systolic pulmonary artery pressure] greater than 35 mm Hg; however, with a severe NVC pattern, this risk was significantly increased (OR = 2.33).”
The investigators cautioned that their findings should be confirmed in larger cohorts. The study by Dr. Markusse and her colleagues was conducted without outside funding, though manufacturers donated diagnostic antibody tests. One of the 11 study coauthors disclosed receiving financial support from Actelion.
Systemic sclerosis is a profoundly heterogeneous disorder, with the overall prevalence of major organ-specific manifestations, such as pulmonary arterial hypertension (PAH), broadly adhering to a 15% rule. As such, the majority of patients with SSc will not develop any given organ-specific complication. The major challenge for clinicians during the early stages of the disease is predicting the future occurrence of potentially life-threatening organ-specific manifestations, such as PAH.
The complementary association of nailfold videocapillaroscopy changes and autoantibody profile in predicting cardiopulmonary involvement reported by Dr. Markusse and her colleagues is novel, but otherwise supports the findings of previous cross-sectional studies identifying associations between advanced NVC changes and SSc complications, such as digital ischemic lesions and PAH. These studies provide intriguing insight into the relationship between the evolution of microangiopathy and the emergence of organ-specific manifestations of SSc, but also represent a shift in focus from the diagnostic to the prognostic utility of NVC in SSc.
There is potential clinical utility in these observations that has yet to be unlocked fully; particularly should the predictive value and timing of NVC progression be further characterized in longitudinal studies better defining the natural history of SSc organ-specific manifestations. If evolving NVC changes (in high-risk serological subgroups) are shown to pre-date the emergence of overt organ-specific manifestations of SSc, then we might be provided with a window of opportunity for escalation of therapy with treatments targeting endothelial function (such as phosphodiesterase inhibitors and/or endothelin receptor antagonists) and/or possible immunomodulatory approaches. This could potentially usher in a new era of preventive disease-modifying therapeutic intervention in SSc.
John D. Pauling, MD, PhD, is a consultant rheumatologist at the Royal National Hospital for Rheumatic Diseases, Bath, England, and Visiting Senior Lecturer in the department of pharmacy and pharmacology at the University of Bath. His commentary is derived from an editorial accompanying the study by Dr. Markusse and her associates (Rheumatology [Oxford]. 2016 Dec 30. doi: 10.1093/rheumatology/kew461). He disclosed having received grants and consultancy income from Actelion.
Systemic sclerosis is a profoundly heterogeneous disorder, with the overall prevalence of major organ-specific manifestations, such as pulmonary arterial hypertension (PAH), broadly adhering to a 15% rule. As such, the majority of patients with SSc will not develop any given organ-specific complication. The major challenge for clinicians during the early stages of the disease is predicting the future occurrence of potentially life-threatening organ-specific manifestations, such as PAH.
The complementary association of nailfold videocapillaroscopy changes and autoantibody profile in predicting cardiopulmonary involvement reported by Dr. Markusse and her colleagues is novel, but otherwise supports the findings of previous cross-sectional studies identifying associations between advanced NVC changes and SSc complications, such as digital ischemic lesions and PAH. These studies provide intriguing insight into the relationship between the evolution of microangiopathy and the emergence of organ-specific manifestations of SSc, but also represent a shift in focus from the diagnostic to the prognostic utility of NVC in SSc.
There is potential clinical utility in these observations that has yet to be unlocked fully; particularly should the predictive value and timing of NVC progression be further characterized in longitudinal studies better defining the natural history of SSc organ-specific manifestations. If evolving NVC changes (in high-risk serological subgroups) are shown to pre-date the emergence of overt organ-specific manifestations of SSc, then we might be provided with a window of opportunity for escalation of therapy with treatments targeting endothelial function (such as phosphodiesterase inhibitors and/or endothelin receptor antagonists) and/or possible immunomodulatory approaches. This could potentially usher in a new era of preventive disease-modifying therapeutic intervention in SSc.
John D. Pauling, MD, PhD, is a consultant rheumatologist at the Royal National Hospital for Rheumatic Diseases, Bath, England, and Visiting Senior Lecturer in the department of pharmacy and pharmacology at the University of Bath. His commentary is derived from an editorial accompanying the study by Dr. Markusse and her associates (Rheumatology [Oxford]. 2016 Dec 30. doi: 10.1093/rheumatology/kew461). He disclosed having received grants and consultancy income from Actelion.
Systemic sclerosis is a profoundly heterogeneous disorder, with the overall prevalence of major organ-specific manifestations, such as pulmonary arterial hypertension (PAH), broadly adhering to a 15% rule. As such, the majority of patients with SSc will not develop any given organ-specific complication. The major challenge for clinicians during the early stages of the disease is predicting the future occurrence of potentially life-threatening organ-specific manifestations, such as PAH.
The complementary association of nailfold videocapillaroscopy changes and autoantibody profile in predicting cardiopulmonary involvement reported by Dr. Markusse and her colleagues is novel, but otherwise supports the findings of previous cross-sectional studies identifying associations between advanced NVC changes and SSc complications, such as digital ischemic lesions and PAH. These studies provide intriguing insight into the relationship between the evolution of microangiopathy and the emergence of organ-specific manifestations of SSc, but also represent a shift in focus from the diagnostic to the prognostic utility of NVC in SSc.
There is potential clinical utility in these observations that has yet to be unlocked fully; particularly should the predictive value and timing of NVC progression be further characterized in longitudinal studies better defining the natural history of SSc organ-specific manifestations. If evolving NVC changes (in high-risk serological subgroups) are shown to pre-date the emergence of overt organ-specific manifestations of SSc, then we might be provided with a window of opportunity for escalation of therapy with treatments targeting endothelial function (such as phosphodiesterase inhibitors and/or endothelin receptor antagonists) and/or possible immunomodulatory approaches. This could potentially usher in a new era of preventive disease-modifying therapeutic intervention in SSc.
John D. Pauling, MD, PhD, is a consultant rheumatologist at the Royal National Hospital for Rheumatic Diseases, Bath, England, and Visiting Senior Lecturer in the department of pharmacy and pharmacology at the University of Bath. His commentary is derived from an editorial accompanying the study by Dr. Markusse and her associates (Rheumatology [Oxford]. 2016 Dec 30. doi: 10.1093/rheumatology/kew461). He disclosed having received grants and consultancy income from Actelion.
Nailfold videocapillaroscopy can help to predict which patients with systemic sclerosis may develop serious cardiopulmonary complications, according to findings from a Dutch cross-sectional study.
While individual autoantibodies seen in systemic sclerosis (SSc) are known to be associated with greater or lesser risk of cardiopulmonary involvement, in this study nailfold vascularization patterns independently predicted pulmonary artery hypertension or interstitial lung disease.
All patients in the study had NVC pattern data as well as anti-extractable nuclear antigen (anti-ENA) antibodies. The mean age of the patients was 54 years; 82% were female, and median disease duration was 3 years. Just over half the cohort had interstitial lung disease, and 16% had pulmonary artery hypertension.
Among the anti-ENA autoantibody subtypes, anti-ACA was seen in 37% of patients, anti-Scl-70 in 24%, anti-RNP in 9%, and anti-RNAPIII in 5%; other subtypes were rarer. SSc-specific NVC patterns were seen in 88% of patients, with 10% of the cohort showing an early (less severe microangiopathy) pattern, 42% an active pattern, and 36% a late pattern.
One of the study’s objectives was to determine whether one or more mechanisms was responsible for both autoantibody production and the microangiopathy seen in SSc.
If a joint mechanism is implicated, “more severe NVC patterns would be determined in patients with autoantibodies (such as anti-Scl-70 and anti-RNAPIII) that are associated with more severe disease,” wrote Dr. Markusse and her colleagues. “On the other hand, if specific autoantibodies and stage of microangiopathy reflect different processes in the disease, a combination of autoantibody status and NVC could be helpful for identifying patients at highest risk for cardiopulmonary involvement.”
The investigators reported finding a similar distribution of NVC abnormalities across the major SSc autoantibody subtypes (except for anti–RNP-positive patients), suggesting that combinations of the two variables would be most predictive of cardiopulmonary involvement. More severe NVC patterns were associated with a higher risk of cardiopulmonary involvement, independent of the presence of a specific autoantibody.
Notably, the researchers wrote, “prevalence of ILD [interstitial lung disease] is generally lower among ACA-positive patients. According to our data, even among ACA-positive patients there was a trend for more ILD being associated with more severe NVC patterns (OR = 1.33).”
A similar pattern was seen for pulmonary artery hypertension. “Based on anti-RNP and anti-RNAPIII positivity, patients did not have an increased risk of a [systolic pulmonary artery pressure] greater than 35 mm Hg; however, with a severe NVC pattern, this risk was significantly increased (OR = 2.33).”
The investigators cautioned that their findings should be confirmed in larger cohorts. The study by Dr. Markusse and her colleagues was conducted without outside funding, though manufacturers donated diagnostic antibody tests. One of the 11 study coauthors disclosed receiving financial support from Actelion.
Nailfold videocapillaroscopy can help to predict which patients with systemic sclerosis may develop serious cardiopulmonary complications, according to findings from a Dutch cross-sectional study.
While individual autoantibodies seen in systemic sclerosis (SSc) are known to be associated with greater or lesser risk of cardiopulmonary involvement, in this study nailfold vascularization patterns independently predicted pulmonary artery hypertension or interstitial lung disease.
All patients in the study had NVC pattern data as well as anti-extractable nuclear antigen (anti-ENA) antibodies. The mean age of the patients was 54 years; 82% were female, and median disease duration was 3 years. Just over half the cohort had interstitial lung disease, and 16% had pulmonary artery hypertension.
Among the anti-ENA autoantibody subtypes, anti-ACA was seen in 37% of patients, anti-Scl-70 in 24%, anti-RNP in 9%, and anti-RNAPIII in 5%; other subtypes were rarer. SSc-specific NVC patterns were seen in 88% of patients, with 10% of the cohort showing an early (less severe microangiopathy) pattern, 42% an active pattern, and 36% a late pattern.
One of the study’s objectives was to determine whether one or more mechanisms was responsible for both autoantibody production and the microangiopathy seen in SSc.
If a joint mechanism is implicated, “more severe NVC patterns would be determined in patients with autoantibodies (such as anti-Scl-70 and anti-RNAPIII) that are associated with more severe disease,” wrote Dr. Markusse and her colleagues. “On the other hand, if specific autoantibodies and stage of microangiopathy reflect different processes in the disease, a combination of autoantibody status and NVC could be helpful for identifying patients at highest risk for cardiopulmonary involvement.”
The investigators reported finding a similar distribution of NVC abnormalities across the major SSc autoantibody subtypes (except for anti–RNP-positive patients), suggesting that combinations of the two variables would be most predictive of cardiopulmonary involvement. More severe NVC patterns were associated with a higher risk of cardiopulmonary involvement, independent of the presence of a specific autoantibody.
Notably, the researchers wrote, “prevalence of ILD [interstitial lung disease] is generally lower among ACA-positive patients. According to our data, even among ACA-positive patients there was a trend for more ILD being associated with more severe NVC patterns (OR = 1.33).”
A similar pattern was seen for pulmonary artery hypertension. “Based on anti-RNP and anti-RNAPIII positivity, patients did not have an increased risk of a [systolic pulmonary artery pressure] greater than 35 mm Hg; however, with a severe NVC pattern, this risk was significantly increased (OR = 2.33).”
The investigators cautioned that their findings should be confirmed in larger cohorts. The study by Dr. Markusse and her colleagues was conducted without outside funding, though manufacturers donated diagnostic antibody tests. One of the 11 study coauthors disclosed receiving financial support from Actelion.
FROM RHEUMATOLOGY
Key clinical point:
Major finding: Across the major autoantibody subtypes seen in an SSc cohort, NVC pattern showed a stable association with presence of interstitial lung disease (OR, 1.3-1.4) or elevated systolic pulmonary artery pressure (OR, 2.2-2.4).
Data source: A cross-section of 287 patients in a Dutch SSc cohort.
Disclosures: The study was conducted without outside funding, though manufacturers donated diagnostic antibody tests. One of the 11 study coauthors disclosed receiving financial support from Actelion.
Surgical discharge data highlight stewardship need at transition
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
NEW ORLEANS – Most antibiotic prescriptions written at the time of patient discharge at an academic hospital were inappropriate, according to a retrospective review of 2014 discharge data.
These drugs were prescribed despite the existence of a robust inpatient antibiotic stewardship program (ASP) at the hospital, Sarah Scarpato, MD, reported at IDWeek, an annual scientific meeting on infectious diseases.
Of 9,750 prescriptions written during the study year, 86% were for oral antibiotics and 14% were for outpatient parenteral antibiotic therapy. Among a random sample of 150 patients discharged on antibiotics, 22.7% had no clinical indication of infection, 13% received an antibiotic with inappropriate spectrum of activity, 17% received an incorrect dose, 55% received an antibiotic course that was too long, and 7.3% received a course that was too short, Dr. Scarpato said at the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
A total of 57.7% of surgical patients and 57.6% of medical patients received an antibiotic prescription that was inappropriate.
“A whopping 70% of prescriptions had at least one error in drug choice, dose, indication, or duration,” she said.
“The most common scenarios in which an antibiotic use was not indicated were prolonged surgical prophylaxis and prolonged prophylaxis in patients who had neutropenic fever during their hospitalization but were no longer neutropenic on discharge. The most common infectious indications were consistent with previous data, with genitourinary, respiratory, and skin and soft tissue being the most common, followed by gastrointestinal,” Dr. Scarpato of the Hospital of the University of Pennsylvania, Philadelphia, said.
In addition, she noted, “100% of patients discharged from cardiothoracic surgery, ear/nose/throat surgery, oral and maxillofacial surgery, neurosurgery, and neurology had at least one error. Oncology was the medical service with the highest rate of inappropriate prescriptions at 80%. The rest, including infectious diseases, had error rates between 40% and 60%.”
Also in line with previous data, fluoroquinolones were the most commonly prescribed antibiotics, accounting for 23.5%, followed by cephalosporins, penicillins, trimethoprim-sulfamethoxazole, and metronidazole.
“Antibiotic prescription in the absence of an acceptable indication and inappropriate duration accounted for the vast majority – 76% – of inappropriate prescriptions,” Dr. Scarpato said, noting that this may be because of a failure by physicians to account for antibiotics given as an inpatient, a lack of familiarity with a patient’s course because of hand-offs, the writing of a prescription with a given duration expecting discharge on a different day, or a lack of familiarity with recommended treatment durations.
“On average, we saw an excess of 3.8 days of unnecessary antibiotics per patient,” she said. The range, however, was 18 days too few to 36 days too many. Further, readmission rates at days 7 and 30 were 6.4% and 19.4%, respectively, for patients discharged on antibiotics, compared with 3.70% and 13.79% hospital wide. The respective rates among those discharged on outpatient parenteral antibiotic therapy were 5.6% and 16.4%, compared with 6.5% and 19.9% among those on oral antibiotic therapy.
The higher rates among those on oral vs. parenteral therapy may be because patients on outpatient parenteral antibiotic therapy are followed closely by a team of infectious disease physicians and pharmacists, while those discharged on oral therapy are not routinely monitored, or it may reflect an unintended consequence of switching from parenteral to oral therapy at discharge, Dr. Scarpato said.
Transitions of care are vulnerable times for patients, she said, noting that “nearly a quarter of patients suffer an adverse event from an error in transition of care during hospital discharge, and up to half of those who suffer an adverse drug reaction at discharge are prescribed an antibiotic.”
Though limited by the retrospective and descriptive nature of the study, and the single-center design, the findings demonstrate “a significant and unmet need for antimicrobial stewardship at transition in care, even at institutions such as ours that have a substantial inpatient ASP,” Dr. Scarpato concluded.
Dr. Scarpato reported having no conflicts of interest.
AT IDWEEK 2016
Key clinical point:
Major finding: 70% of prescriptions had at least one error in drug choice, dose, indication, or duration.
Data source: A review of discharge data for 150 patients at an academic hospital.
Disclosures: Dr. Scarpato reported having no conflicts of interest.
What’s in store for CMS under Seema Verma?
WASHINGTON – Big changes could be in store for the Medicaid program under the potential leadership of Seema Verma as administrator of the Centers for Medicare & Medicaid Services.
In nominating Ms. Verma, President Trump called her a leading expert on Medicaid and Medicare who will help “transform our health care system for the benefit of all Americans.”
A relative unknown, Ms. Verma is a health policy consultant who has spent 20 years quietly designing policy projects involving Medicaid, including the crafting of Indiana’s Medicaid expansion under the Affordable Care Act in which she worked closely with Vice President Pence.
How the savvy consultant could alter the Medicaid program during her potential CMS tenure has been the source of much speculation. President Trump and Rep. Tom Price (R-Ga.), Health & Human Services secretary–designee, have called for the restructuring of Medicaid, including the possibility of block grants that would set limits on total annual spending regardless of enrollment or caps that would limit average spending per enrollee.
Ms. Verma’s role in the revamp will largely depend on what Congress allows, said Mark Polston, a Washington, D.C.–based health law attorney and former associate general counsel for litigation in the HHS Office of General Counsel, CMS division, under President George W. Bush.
“We don’t know what cards she has in her hands – let alone what’s in the deck for her to deal from,” Mr. Polston said at a meeting sponsored by the American Bar Association. “That’s really going to be set by Congress.”
“From a CMS perspective, the Medicaid program is in large part run by the states,” Mr. Blum said at the ABA meeting. “What the new nominee says to me is that there is going to be a very high priority placed upon working with states, working with governors to modify Medicaid programs and to shape them to meet different state priorities.”
Look no further than the Healthy Indiana Plan 2.0 to get an idea of what such plans could look like, said Leslie V. Norwalk, a Washington, D.C.–based health law attorney and a former acting CMS administrator under President George W. Bush. The Indiana plan requires patients to pay a small amount to receive health coverage and includes a lockout period if payments are missed. Ms. Verma could work with governors to develop similar model waivers, Ms. Norwalk said.
Mr. Blum said he believes a top priority for Ms. Verma will be limiting the disruption that could come if the ACA is repealed and finding ways to cover those who lose coverage.
“What the next team really needs to really realize [is] that those who sign up for coverage – with the exchanges or through the new state expansions – are sicker on average, have lower income on average, and they’re going to have to think very carefully about the transitions going on,” Mr. Blum said at the meeting. “How you think about the transitions, how you think about continuity of care, how you think about disruptions – those will be very real and very tangible for the next team.”
“If she’s smart, she’ll find a deputy who’s very strong on Medicare. She’ll probably also try to find a former Hill staffer who can help her on the Hill,” Mr. Scully said. “The best news for her is that they picked her really early, so she’s got a head start.”
Hiring a deputy with a strong insurance background will also be key, Ms. Norwalk said in an interview. Even if the exchanges are repealed, other CMS programs, such as Medicare Part D and Medicare Advantage rely heavily on insurers, she said.
Ms. Norwalk noted that Ms. Verma may be surprised to find that much of the CMS agenda is controlled by the requirements of Medicare’s regulatory cycle. “[It] will take up a lot of her time, perhaps more than she might anticipate,” she said. “But in addition, you’ll have governors coming in wanting to do waivers. ... The third component will be how much time she spends on Capitol Hill working on whether repeal is done or not, and certainly the replace function and how that works will be a critical component of what she does. [If she’s confirmed,] she’ll be a very busy lady.”
[email protected]
On Twitter @legal_med
WASHINGTON – Big changes could be in store for the Medicaid program under the potential leadership of Seema Verma as administrator of the Centers for Medicare & Medicaid Services.
In nominating Ms. Verma, President Trump called her a leading expert on Medicaid and Medicare who will help “transform our health care system for the benefit of all Americans.”
A relative unknown, Ms. Verma is a health policy consultant who has spent 20 years quietly designing policy projects involving Medicaid, including the crafting of Indiana’s Medicaid expansion under the Affordable Care Act in which she worked closely with Vice President Pence.
How the savvy consultant could alter the Medicaid program during her potential CMS tenure has been the source of much speculation. President Trump and Rep. Tom Price (R-Ga.), Health & Human Services secretary–designee, have called for the restructuring of Medicaid, including the possibility of block grants that would set limits on total annual spending regardless of enrollment or caps that would limit average spending per enrollee.
Ms. Verma’s role in the revamp will largely depend on what Congress allows, said Mark Polston, a Washington, D.C.–based health law attorney and former associate general counsel for litigation in the HHS Office of General Counsel, CMS division, under President George W. Bush.
“We don’t know what cards she has in her hands – let alone what’s in the deck for her to deal from,” Mr. Polston said at a meeting sponsored by the American Bar Association. “That’s really going to be set by Congress.”
“From a CMS perspective, the Medicaid program is in large part run by the states,” Mr. Blum said at the ABA meeting. “What the new nominee says to me is that there is going to be a very high priority placed upon working with states, working with governors to modify Medicaid programs and to shape them to meet different state priorities.”
Look no further than the Healthy Indiana Plan 2.0 to get an idea of what such plans could look like, said Leslie V. Norwalk, a Washington, D.C.–based health law attorney and a former acting CMS administrator under President George W. Bush. The Indiana plan requires patients to pay a small amount to receive health coverage and includes a lockout period if payments are missed. Ms. Verma could work with governors to develop similar model waivers, Ms. Norwalk said.
Mr. Blum said he believes a top priority for Ms. Verma will be limiting the disruption that could come if the ACA is repealed and finding ways to cover those who lose coverage.
“What the next team really needs to really realize [is] that those who sign up for coverage – with the exchanges or through the new state expansions – are sicker on average, have lower income on average, and they’re going to have to think very carefully about the transitions going on,” Mr. Blum said at the meeting. “How you think about the transitions, how you think about continuity of care, how you think about disruptions – those will be very real and very tangible for the next team.”
“If she’s smart, she’ll find a deputy who’s very strong on Medicare. She’ll probably also try to find a former Hill staffer who can help her on the Hill,” Mr. Scully said. “The best news for her is that they picked her really early, so she’s got a head start.”
Hiring a deputy with a strong insurance background will also be key, Ms. Norwalk said in an interview. Even if the exchanges are repealed, other CMS programs, such as Medicare Part D and Medicare Advantage rely heavily on insurers, she said.
Ms. Norwalk noted that Ms. Verma may be surprised to find that much of the CMS agenda is controlled by the requirements of Medicare’s regulatory cycle. “[It] will take up a lot of her time, perhaps more than she might anticipate,” she said. “But in addition, you’ll have governors coming in wanting to do waivers. ... The third component will be how much time she spends on Capitol Hill working on whether repeal is done or not, and certainly the replace function and how that works will be a critical component of what she does. [If she’s confirmed,] she’ll be a very busy lady.”
[email protected]
On Twitter @legal_med
WASHINGTON – Big changes could be in store for the Medicaid program under the potential leadership of Seema Verma as administrator of the Centers for Medicare & Medicaid Services.
In nominating Ms. Verma, President Trump called her a leading expert on Medicaid and Medicare who will help “transform our health care system for the benefit of all Americans.”
A relative unknown, Ms. Verma is a health policy consultant who has spent 20 years quietly designing policy projects involving Medicaid, including the crafting of Indiana’s Medicaid expansion under the Affordable Care Act in which she worked closely with Vice President Pence.
How the savvy consultant could alter the Medicaid program during her potential CMS tenure has been the source of much speculation. President Trump and Rep. Tom Price (R-Ga.), Health & Human Services secretary–designee, have called for the restructuring of Medicaid, including the possibility of block grants that would set limits on total annual spending regardless of enrollment or caps that would limit average spending per enrollee.
Ms. Verma’s role in the revamp will largely depend on what Congress allows, said Mark Polston, a Washington, D.C.–based health law attorney and former associate general counsel for litigation in the HHS Office of General Counsel, CMS division, under President George W. Bush.
“We don’t know what cards she has in her hands – let alone what’s in the deck for her to deal from,” Mr. Polston said at a meeting sponsored by the American Bar Association. “That’s really going to be set by Congress.”
“From a CMS perspective, the Medicaid program is in large part run by the states,” Mr. Blum said at the ABA meeting. “What the new nominee says to me is that there is going to be a very high priority placed upon working with states, working with governors to modify Medicaid programs and to shape them to meet different state priorities.”
Look no further than the Healthy Indiana Plan 2.0 to get an idea of what such plans could look like, said Leslie V. Norwalk, a Washington, D.C.–based health law attorney and a former acting CMS administrator under President George W. Bush. The Indiana plan requires patients to pay a small amount to receive health coverage and includes a lockout period if payments are missed. Ms. Verma could work with governors to develop similar model waivers, Ms. Norwalk said.
Mr. Blum said he believes a top priority for Ms. Verma will be limiting the disruption that could come if the ACA is repealed and finding ways to cover those who lose coverage.
“What the next team really needs to really realize [is] that those who sign up for coverage – with the exchanges or through the new state expansions – are sicker on average, have lower income on average, and they’re going to have to think very carefully about the transitions going on,” Mr. Blum said at the meeting. “How you think about the transitions, how you think about continuity of care, how you think about disruptions – those will be very real and very tangible for the next team.”
“If she’s smart, she’ll find a deputy who’s very strong on Medicare. She’ll probably also try to find a former Hill staffer who can help her on the Hill,” Mr. Scully said. “The best news for her is that they picked her really early, so she’s got a head start.”
Hiring a deputy with a strong insurance background will also be key, Ms. Norwalk said in an interview. Even if the exchanges are repealed, other CMS programs, such as Medicare Part D and Medicare Advantage rely heavily on insurers, she said.
Ms. Norwalk noted that Ms. Verma may be surprised to find that much of the CMS agenda is controlled by the requirements of Medicare’s regulatory cycle. “[It] will take up a lot of her time, perhaps more than she might anticipate,” she said. “But in addition, you’ll have governors coming in wanting to do waivers. ... The third component will be how much time she spends on Capitol Hill working on whether repeal is done or not, and certainly the replace function and how that works will be a critical component of what she does. [If she’s confirmed,] she’ll be a very busy lady.”
[email protected]
On Twitter @legal_med
AT THE AMERICAN BAR ASSOCIATION HEALTH LAW SUMMIT
First-trimester blood glucose predicts congenital heart disease risk
NEW ORLEANS – A single, random, first-trimester maternal plasma glucose measurement is superior to an oral glucose tolerance test later in pregnancy as a predictor of congenital heart disease in newborns, Emmi Helle, MD, reported at the American Heart Association scientific sessions.
This finding from a large retrospective study, if confirmed in a prospective data set, is likely to be practice changing. At present, a 1-hour oral glucose tolerance test in the second or third trimester is considered the best means of identifying pregnant women who ought to undergo fetal echocardiography for prenatal diagnosis of congenital heart disease, noted Dr. Helle of Stanford (Calif.) University.
An elevated random plasma glucose value in the first trimester was broadly predictive of increased risk for a variety of congenital heart anomalies, not just, for example, cyanotic conditions.
Fetal heart development is completed during the first trimester, Dr. Helle observed.
Her study received a warm reception. Michael A. Portman, MD, singled it out in his final-day wrap-up of the meeting’s highlights in the field of congenital heart disease.
Several studies have demonstrated that prenatal diagnosis of congenital heart disease results in improved surgical outcomes in newborns. The question is, how to get the right women – those at increased risk – to diagnostic fetal echocardiography. Guidelines suggest but don’t mandate on the basis of weak evidence that an oral glucose tolerance test performed in the second or early third trimester may be a useful means of screening mothers for fetal imaging. Dr. Helle’s study points to a better way.
“Hopefully we can change our guidelines and make them more scientific for identification of mothers who should undergo fetal echocardiography,” said Dr. Portman, professor of pediatrics at the University of Washington, Seattle, and director of pediatric cardiovascular research at Seattle Children’s Hospital.
Dr. Helle and Dr. Portman reported having no relevant financial interests.
NEW ORLEANS – A single, random, first-trimester maternal plasma glucose measurement is superior to an oral glucose tolerance test later in pregnancy as a predictor of congenital heart disease in newborns, Emmi Helle, MD, reported at the American Heart Association scientific sessions.
This finding from a large retrospective study, if confirmed in a prospective data set, is likely to be practice changing. At present, a 1-hour oral glucose tolerance test in the second or third trimester is considered the best means of identifying pregnant women who ought to undergo fetal echocardiography for prenatal diagnosis of congenital heart disease, noted Dr. Helle of Stanford (Calif.) University.
An elevated random plasma glucose value in the first trimester was broadly predictive of increased risk for a variety of congenital heart anomalies, not just, for example, cyanotic conditions.
Fetal heart development is completed during the first trimester, Dr. Helle observed.
Her study received a warm reception. Michael A. Portman, MD, singled it out in his final-day wrap-up of the meeting’s highlights in the field of congenital heart disease.
Several studies have demonstrated that prenatal diagnosis of congenital heart disease results in improved surgical outcomes in newborns. The question is, how to get the right women – those at increased risk – to diagnostic fetal echocardiography. Guidelines suggest but don’t mandate on the basis of weak evidence that an oral glucose tolerance test performed in the second or early third trimester may be a useful means of screening mothers for fetal imaging. Dr. Helle’s study points to a better way.
“Hopefully we can change our guidelines and make them more scientific for identification of mothers who should undergo fetal echocardiography,” said Dr. Portman, professor of pediatrics at the University of Washington, Seattle, and director of pediatric cardiovascular research at Seattle Children’s Hospital.
Dr. Helle and Dr. Portman reported having no relevant financial interests.
NEW ORLEANS – A single, random, first-trimester maternal plasma glucose measurement is superior to an oral glucose tolerance test later in pregnancy as a predictor of congenital heart disease in newborns, Emmi Helle, MD, reported at the American Heart Association scientific sessions.
This finding from a large retrospective study, if confirmed in a prospective data set, is likely to be practice changing. At present, a 1-hour oral glucose tolerance test in the second or third trimester is considered the best means of identifying pregnant women who ought to undergo fetal echocardiography for prenatal diagnosis of congenital heart disease, noted Dr. Helle of Stanford (Calif.) University.
An elevated random plasma glucose value in the first trimester was broadly predictive of increased risk for a variety of congenital heart anomalies, not just, for example, cyanotic conditions.
Fetal heart development is completed during the first trimester, Dr. Helle observed.
Her study received a warm reception. Michael A. Portman, MD, singled it out in his final-day wrap-up of the meeting’s highlights in the field of congenital heart disease.
Several studies have demonstrated that prenatal diagnosis of congenital heart disease results in improved surgical outcomes in newborns. The question is, how to get the right women – those at increased risk – to diagnostic fetal echocardiography. Guidelines suggest but don’t mandate on the basis of weak evidence that an oral glucose tolerance test performed in the second or early third trimester may be a useful means of screening mothers for fetal imaging. Dr. Helle’s study points to a better way.
“Hopefully we can change our guidelines and make them more scientific for identification of mothers who should undergo fetal echocardiography,” said Dr. Portman, professor of pediatrics at the University of Washington, Seattle, and director of pediatric cardiovascular research at Seattle Children’s Hospital.
Dr. Helle and Dr. Portman reported having no relevant financial interests.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: For every 10-mg/dL increase in maternal plasma glucose on a random first-trimester measurement, the risk of giving birth to a baby with congenital heart disease rose by 8%.
Data source: A retrospective study of 19,197 pregnancies, 811 of which resulted in congenital heart disease in the offspring.
Disclosures: The presenter reported having no financial conflicts of interest regarding the study.
Non-MD CT Surgical Team Scientific Poster Opportunity
Non-MD cardiothoracic team professionals can submit a scientific poster for the Perioperative/Team-Based Care Poster Competition. Winning posters will be displayed at the AATS Centennial, April 29 – May 3 in Boston, MA.
The competition winner will receive a $1,000 stipend to offset travel and accommodation costs.
Deadline: January 20, 2017
Share:
Non-MD cardiothoracic team professionals can submit a scientific poster for the Perioperative/Team-Based Care Poster Competition. Winning posters will be displayed at the AATS Centennial, April 29 – May 3 in Boston, MA.
The competition winner will receive a $1,000 stipend to offset travel and accommodation costs.
Deadline: January 20, 2017
Share:
Non-MD cardiothoracic team professionals can submit a scientific poster for the Perioperative/Team-Based Care Poster Competition. Winning posters will be displayed at the AATS Centennial, April 29 – May 3 in Boston, MA.
The competition winner will receive a $1,000 stipend to offset travel and accommodation costs.
Deadline: January 20, 2017
Share:
Non-MD CT Surgical Team Scientific Poster Opportunity
Non-MD cardiothoracic team professionals can submit a scientific poster for the Perioperative/Team-Based Care Poster Competition. Winning posters will be displayed at the AATS Centennial, April 29 – May 3 in Boston, MA.
The competition winner will receive a $1,000 stipend to offset travel and accommodation costs.
Deadline: January 20, 2017
Share:
Non-MD cardiothoracic team professionals can submit a scientific poster for the Perioperative/Team-Based Care Poster Competition. Winning posters will be displayed at the AATS Centennial, April 29 – May 3 in Boston, MA.
The competition winner will receive a $1,000 stipend to offset travel and accommodation costs.
Deadline: January 20, 2017
Share:
Non-MD cardiothoracic team professionals can submit a scientific poster for the Perioperative/Team-Based Care Poster Competition. Winning posters will be displayed at the AATS Centennial, April 29 – May 3 in Boston, MA.
The competition winner will receive a $1,000 stipend to offset travel and accommodation costs.
Deadline: January 20, 2017
Share:
In NSCLC, delayed chemo yields survival benefit comparable to early chemo
Patients with non–small-cell lung cancer (NSCLC) for whom adjuvant chemotherapy must be delayed for as long as 18 weeks have mortality outcomes that are no worse than those of patients who start chemotherapy soon after surgery, and those who undergo delayed chemotherapy have a significantly lower risk for death than patients who have no chemotherapy at all, investigators report.
A retrospective review of data on 12,473 patients with previously untreated NSCLC showed that there were no significant differences in 5-year overall survival (OS) estimates among patients who started multi-agent chemotherapy at 18-38 days postoperatively, from 39 to 56 days after surgery (the reference interval), or from 57 to 127 days after surgery, reported Daniel J. Boffa, MD, of Yale University, New Haven, Conn., and his colleagues.
In addition, when they used propensity score matching to pair patients who received chemotherapy with patients who did not undergo chemotherapy, they found that even late chemotherapy was associated with a significantly lower risk for death.
“Clinicians should still consider chemotherapy in appropriately selected patients that are healthy enough to tolerate it, up to 4 months after NSCLC resection. Further study is warranted to confirm these findings,” the investigators concluded (JAMA Oncol. 2017 Jan. 5 doi: 10.1001/jamaoncol.2016.5829).
In the retrospective review of records from the National Cancer Database, the investigators limited the study to patients for whom chemotherapy is typically prescribed: those with lymph node metastases, tumors 4 cm or larger, and/or local extension of disease. They looked at the association between the time to initiation of adjuvant chemotherapy and survival using Cox modeling with restricted cubic splines, a validated statistical method for evaluating links between survival and independent variables.
Dr. Boffa and his associates found that the unadjusted Kaplan-Meier 5-year OS estimates did not differ between the groups, at 53% for the early chemotherapy group (hazard ratio [HR] vs. the reference group, 1.009, P = .79), 55% for the reference group, and 53% for the later chemotherapy group (HR 1.037, P = .27).
Comparing adjuvant chemotherapy timing on the efficacy of surgery alone in patients matched by tumor stage and other features, the researchers found that chemotherapy started during any of the three intervals was associated with an approximately 34% reduction in risk of death compared with no chemotherapy (HR for the respective time intervals 0.672, 0.645, and 0.664; P less than .001 for each comparison).
The study helps to clarify for clinicians the benefits of adjuvant chemotherapy in select patients with NSCLC in a real-world setting, Howard (Jack) West, MD, of the Swedish Cancer Institute, Seattle, said in an accompanying editorial (JAMA Oncol. 2017 Jan. 5 doi: 10.1001/jamaoncol.2016.5798).
“While retrospective data cannot define the benefit of delayed adjuvant chemotherapy with the clarity of a prospective randomized trial, we must remember that in the land of the blind, the one-eyed man is king; these limited data inject an evidence-based answer for a very common clinical question for which we have been forced by necessity to rely only on our best judgments,” he wrote.
The study was internally supported. The authors and Dr. West reported no conflict of interest disclosures.
Patients with non–small-cell lung cancer (NSCLC) for whom adjuvant chemotherapy must be delayed for as long as 18 weeks have mortality outcomes that are no worse than those of patients who start chemotherapy soon after surgery, and those who undergo delayed chemotherapy have a significantly lower risk for death than patients who have no chemotherapy at all, investigators report.
A retrospective review of data on 12,473 patients with previously untreated NSCLC showed that there were no significant differences in 5-year overall survival (OS) estimates among patients who started multi-agent chemotherapy at 18-38 days postoperatively, from 39 to 56 days after surgery (the reference interval), or from 57 to 127 days after surgery, reported Daniel J. Boffa, MD, of Yale University, New Haven, Conn., and his colleagues.
In addition, when they used propensity score matching to pair patients who received chemotherapy with patients who did not undergo chemotherapy, they found that even late chemotherapy was associated with a significantly lower risk for death.
“Clinicians should still consider chemotherapy in appropriately selected patients that are healthy enough to tolerate it, up to 4 months after NSCLC resection. Further study is warranted to confirm these findings,” the investigators concluded (JAMA Oncol. 2017 Jan. 5 doi: 10.1001/jamaoncol.2016.5829).
In the retrospective review of records from the National Cancer Database, the investigators limited the study to patients for whom chemotherapy is typically prescribed: those with lymph node metastases, tumors 4 cm or larger, and/or local extension of disease. They looked at the association between the time to initiation of adjuvant chemotherapy and survival using Cox modeling with restricted cubic splines, a validated statistical method for evaluating links between survival and independent variables.
Dr. Boffa and his associates found that the unadjusted Kaplan-Meier 5-year OS estimates did not differ between the groups, at 53% for the early chemotherapy group (hazard ratio [HR] vs. the reference group, 1.009, P = .79), 55% for the reference group, and 53% for the later chemotherapy group (HR 1.037, P = .27).
Comparing adjuvant chemotherapy timing on the efficacy of surgery alone in patients matched by tumor stage and other features, the researchers found that chemotherapy started during any of the three intervals was associated with an approximately 34% reduction in risk of death compared with no chemotherapy (HR for the respective time intervals 0.672, 0.645, and 0.664; P less than .001 for each comparison).
The study helps to clarify for clinicians the benefits of adjuvant chemotherapy in select patients with NSCLC in a real-world setting, Howard (Jack) West, MD, of the Swedish Cancer Institute, Seattle, said in an accompanying editorial (JAMA Oncol. 2017 Jan. 5 doi: 10.1001/jamaoncol.2016.5798).
“While retrospective data cannot define the benefit of delayed adjuvant chemotherapy with the clarity of a prospective randomized trial, we must remember that in the land of the blind, the one-eyed man is king; these limited data inject an evidence-based answer for a very common clinical question for which we have been forced by necessity to rely only on our best judgments,” he wrote.
The study was internally supported. The authors and Dr. West reported no conflict of interest disclosures.
Patients with non–small-cell lung cancer (NSCLC) for whom adjuvant chemotherapy must be delayed for as long as 18 weeks have mortality outcomes that are no worse than those of patients who start chemotherapy soon after surgery, and those who undergo delayed chemotherapy have a significantly lower risk for death than patients who have no chemotherapy at all, investigators report.
A retrospective review of data on 12,473 patients with previously untreated NSCLC showed that there were no significant differences in 5-year overall survival (OS) estimates among patients who started multi-agent chemotherapy at 18-38 days postoperatively, from 39 to 56 days after surgery (the reference interval), or from 57 to 127 days after surgery, reported Daniel J. Boffa, MD, of Yale University, New Haven, Conn., and his colleagues.
In addition, when they used propensity score matching to pair patients who received chemotherapy with patients who did not undergo chemotherapy, they found that even late chemotherapy was associated with a significantly lower risk for death.
“Clinicians should still consider chemotherapy in appropriately selected patients that are healthy enough to tolerate it, up to 4 months after NSCLC resection. Further study is warranted to confirm these findings,” the investigators concluded (JAMA Oncol. 2017 Jan. 5 doi: 10.1001/jamaoncol.2016.5829).
In the retrospective review of records from the National Cancer Database, the investigators limited the study to patients for whom chemotherapy is typically prescribed: those with lymph node metastases, tumors 4 cm or larger, and/or local extension of disease. They looked at the association between the time to initiation of adjuvant chemotherapy and survival using Cox modeling with restricted cubic splines, a validated statistical method for evaluating links between survival and independent variables.
Dr. Boffa and his associates found that the unadjusted Kaplan-Meier 5-year OS estimates did not differ between the groups, at 53% for the early chemotherapy group (hazard ratio [HR] vs. the reference group, 1.009, P = .79), 55% for the reference group, and 53% for the later chemotherapy group (HR 1.037, P = .27).
Comparing adjuvant chemotherapy timing on the efficacy of surgery alone in patients matched by tumor stage and other features, the researchers found that chemotherapy started during any of the three intervals was associated with an approximately 34% reduction in risk of death compared with no chemotherapy (HR for the respective time intervals 0.672, 0.645, and 0.664; P less than .001 for each comparison).
The study helps to clarify for clinicians the benefits of adjuvant chemotherapy in select patients with NSCLC in a real-world setting, Howard (Jack) West, MD, of the Swedish Cancer Institute, Seattle, said in an accompanying editorial (JAMA Oncol. 2017 Jan. 5 doi: 10.1001/jamaoncol.2016.5798).
“While retrospective data cannot define the benefit of delayed adjuvant chemotherapy with the clarity of a prospective randomized trial, we must remember that in the land of the blind, the one-eyed man is king; these limited data inject an evidence-based answer for a very common clinical question for which we have been forced by necessity to rely only on our best judgments,” he wrote.
The study was internally supported. The authors and Dr. West reported no conflict of interest disclosures.
FROM JAMA ONCOLOGY
Key clinical point: Chemotherapy delayed for up to 18 weeks after surgery offers survival benefits comparable to those of earlier chemotherapy in non–small-cell lung cancer.
Major finding: There were no statistical differences in 5-year survival of patients with NSCLC started on chemotherapy either 18-38, 39-56, or 57-127 days after surgery.
Data source: Retrospective observational study of 12,473 patients with untreated NSCLC in the National Cancer Database.
Disclosures: The study was internally supported. The authors and Dr. West reported no conflict of interest disclosures.